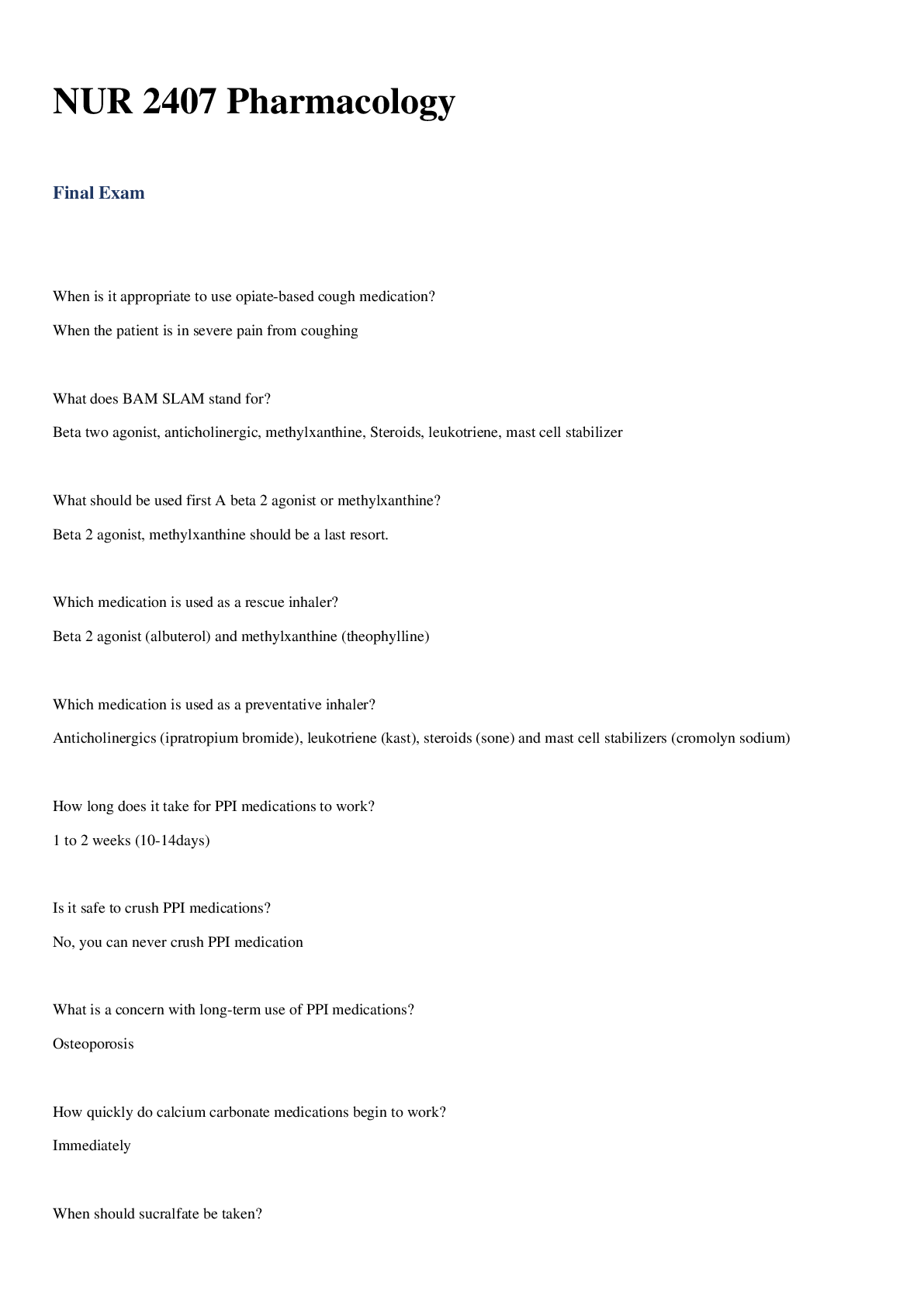
*NURSING > STUDY GUIDE > Rasmussen College: NURSING NUR2356/MCD-1 Final Exam Study Guide_LATEST UPDATED 2021/2022,100% CORREC (All)
Rasmussen College: NURSING NUR2356/MCD-1 Final Exam Study Guide_LATEST UPDATED 2021/2022,100% CORRECT
Document Content and Description Below
Rasmussen College: NURSING NUR2356/MCD-1 Final Exam Study Guide_LATEST UPDATED 2021/2022 Hygiene: Benefits of Bathing: Bathe clients to cleanse body, stimulate circulation, provide re... laxation, and enhance healing. Bathe clients whose health problems have exhausted them or limited their mobility Give a complete bath to clients who can tolerate it and whose hygiene needs warrant it. Allow rest periods for clients who become tired. Partial baths are useful when clients cannot tolerate a complete bath, need cleanings of odorous or uncomfortable areas, and can perform part of the bath independently. Therapeutic baths are used to promote comfort and provide treatment. Giving a Bed Bath: Collect supplies, provide privacy, explain procedure, apply gloves. Lock wheels on the hospital bed and adjust the height to a comfortable working position. Place a blanket over the client, and remove gown. Obtain warm bath water. Start by washing clients face first and allow client to perform this task if able. Perform the bath systematically by starting with the client’s trunk and upper extremities and continuing to the lower extremities. Keep clean area covered with a blanket or towel. Wash with long, firm strokes from distal to proximal and light strokes over lower extremities for clients who have a history of deep vein thrombosis. Apply a lotion and powder (If needed) and a clean gown. Replace water if he becomes cool, and use fresh water for perineal care. Document skin assessment, type of bath, and the clients response. Oral Hygiene: • Proper oral hygiene helps decrease the risk of infection, especially from the transmission of pathogens that can cause pneumonia. • Other populations who require meticulous oral hygiene include those who are seriously ill, injured, unconscious, dehydrated, and have an altered mental status or limited upper body movement. Autonomy for a Client Requiring Oral Care? • Brush the teeth twice a day. • Use a soft toothbrush. • Moisturize oral mucosa and lips every 2 to 4 hours. • Use a chlorhexidine gluconate (0.12%) rinse twice a day during the perioperative period for patients who undergo cardiac surgery (adult patients). • Use mouthwash inside the mouth twice a day for adult patients who are on a ventilator. • Give the patients the oral supplies. Perineal Care: (Reduces Urinary Tract Infection) • Perineal care helps maintain skin integrity, relieve discomfort, and prevent transmission of microorganisms (catheter care). • Provide privacy, maintain a professional demeanor, remove any fecal materials from the skin. • Cleanse the perineal area from front to back (perineum to rectum). • Dry thoroughly. • *On a MALE client* Retract foreskin of male clients to wash the tip of the penis, clean from the meatus outwards in a circular motion, then replace foreskin. Skin Care: • Perform a daily inspection of the patient's entire skin. • Document and report any manifestations of skin infection. • Use moisturizers daily on dry skin and apply when skin is damp. • Keep moisture from prolonged contact with skin. • Dry areas where two skin surfaces touch, such as the axillae and under the breasts. • Place absorbent pads under areas where perspiration collects. • Use moisture barriers on skin areas where wound drainage or incontinence occurs. • Do not massage bony prominences. • Humidify the room. Skin Cleaning • Clean the skin as soon as possible after soiling occurs and at routine intervals. • Use a mild, heavily fatted soap or gentle commercial cleanser for incontinence. • Use tepid rather than hot water. • In the perineal area, use a disposable cleaning cloth that contains a skin-barrier agent. • While cleaning, use the minimum scrubbing force necessary to remove soil. • Gently pat rather than rub the skin dry. • Do not use powders or talc directly on the perineum. • After cleaning, apply a commercial skin barrier to areas in frequent contact with urine or feces. Foot Care: - Foot care prevents skin breakdown, pain and infection. - Foot care is extremely important for clients who have diabetes mellitus, and a qualified professional must perform it. Must be performed for clients with peripheral vascular disease, or immunosuppression to evaluate the feet and prevent injury. - Inspect feet daily, paying attention to the area between the toes. Use lukewarm water, and dry the feet thoroughly. - Apply moisturizer to the feet, but avoid applying it between the toes. - Avoid over-the-counter products that contain alcohol or other strong chemicals. - Wear clean cotton socks DAILY. - Check shoes for any objects that may harm the feet, Cut the nails straight across and use an emery board to file nail edges. Avoid self-treating corns or calluses. - Wear comfortable shoes that don’t restrict circulation, do not apply heat unless prescribed, and contact provider if any infection or inflammation appears. Sleep and Rest: o Adequate amounts of sleep and rest promote health. Too little sleep leads to an inability to concentrate, poor judgement, moodiness, irritability, and increased risk for accidents. Chronic sleep loss can increase risks of obesity, depression, hypertension, diabetes mellitus, heart attack, and stroke. Non-rapid Eye Movement (NREM): Muscles begin to relax, light sleep, etc. Rapid Eye Movement (REM): Vivid dreaming, about 90 mins after falling asleep, reoccurring. o Ask about sleep patterns, history, or any recent changes. o Client education: Establish a bedtime routine, exercise regularly 2 hours before bedtime, make sleep environment comfortable, limit alcohol, caffeine, and nicotine at least 4 hours before bedtime, limit fluids, and relax. Nutrition: Assessment: Number of meals per day, fluid intake, food preferences and amounts, food preparation, purchasing practices, history of indigestion, heart burn or gas. Allergies, taste, chewing, swallowing, appetite, elimination patterns, medication use, activity levels, religious, cultural food preferences and restrictions, and nutritional screening tools. Nursing Interventions: Assist in advancing the diet as the provider prescribes, instruct clients about the appropriate diet regimen, provide interventions to promote appetite (good oral hygiene, favorite foods, minimal environment odors.) Educate clients about meds that can affect nutritional intake, assist clients with feedings, individualize client preferences. Assist with preventing aspiration, provide therapeutic diets, administer and monitor enteral feedings via nasogastric, gastrostomy or jejunostomy tubes, maintain fluid balance, encourage oral intake of fluids. Ensure a fluid intake between 2000 and 3000 mL/day. Maintain adequate intake of protein and calories. Pain Management: Medication: Non-Opioid analgesics: Example is NSAIDS, treating mild to moderate pain. Opioid Analgesics: Treating moderate to severe pain, such as postoperative pain. Adjuvant Analgesics: Help alleviate other manifestations that aggravate pain, treating neuropathic pain. Patient-Controlled Analgesia: Allows clients to self-administer safe doses of opioids. Acute Pain- protective, temporary, usually self-limiting, has a direct cause and results in tissue healing. Chronic Pain: is NOT protective, ongoing or recurs frequently, lasting longer than 6 months and persisting beyond tissue healing. Nociceptive Pain- arises from damage to or inflammation of tissue. Usually throbbing, aching, and localized. Neuropathic Pain- arises from abnormal or damaged pain in nerves. Includes phantom limb pain, pain below level of spinal cord injury, and diabetic neuropathy. Bowel Elimination: Many factors can alter bowel function. Interventions (surgery, immobility, medications, therapeutic diets) can affect bowel elimination. Fiber requirement: 25-38 g/day. Fluid requirement: 2 L/day for females, 3 L/day for males from fluid and food sources. Laxatives: Soften stool Diarrhea: Is a bowel pattern of frequent, loose or liquid stools. Causes include- viral or bacterial gastroenteritis, antibiotic therapy, inflammatory bowel disease, irritable bowel disease. Urinary Elimination: • Complications: Urinary Tract Infection (UTI); Most due to Escherichia Coli. And Incontinence. Risk Factors include: In females, close proximity of the urethral meatus to the anal, frequent sexual intercourse, menopause which decrease estrogen levels, uncircumcised clients, use of indwelling catheters. Manifestations: Urinary frequency, urgency, nocturia, flank pain, etc. Nursing Actions: Females wipe front to back, cleanse beneath male foreskin, provide catheter care regularly. • More Complications: Skin breakdown (from chronic exposure to urine). Nursing Actions: Keep the skin clean and dry, assess for manifestations of breakdown, apply protective barrier creams (Vaseline), implement a bladder-retraining program, assist with measures of conceal urinary leaking (perineal pads, external catheters, adult incontinence garments). • Client Education Teaching on Urinary Elimination: Maintain regular bowel movements, try to empty bladder completely with each void, keep incontinence diary, perform kegel exercises, perform bladder compression techniques, avoid caffeine and alcohol consumption, adverse effects of medications can affect urination, and conduct vaginal cone therapy, WIPE FRONT TO BACK, keep perineum clean (proper cleaning). • Drink 2 to 3 L of fluid daily, try to hold urine and stay on schedule for bladder retraining, drink cranberry juice to decrease risk of infection, if obese lose weight, intake meds to help resolve incontinence, get a catheter placed. Verbal and Nonverbal Communication Skills: Verbal Communication: Is the use of spoken and written words. Nonverbal Communication: Sometimes called body language, communicates how someone is feeling and gives a more accurate account of an individual’s true sentiment. Personal Space: The physical space immediately surrounding someone, into which any encroachment feels threatening to or uncomfortable for them. Therapeutic Relationships: Therapeutic communication occurs in the context of a helping relationship. The helping relationship has four phases: pre-interaction, orientation, working phase, and termination. • Pre-Interaction: Gathering data, diagnosis, lab work, gathers information, etc. • Orientation: First contact with patient. Introduce each other. • Working Phase: Start care plan. Work on getting patient to end goal. Maintain personal relationship. Shows respect, expresses concerns. • Termination: End at the nurse shift, discharge of patient, making sure they are following all the correct precautions before leaving. Therapeutic communication: is client centered communication directed to achieve the patients’ goal. Key skills to establish a therapeutic relationship include expressing interest, concern, caring, perception, and provide as well as obtain healthcare information. Therapeutic Key Characteristics: Therapeutic communication is the use of communication skills that results in a positive effect on client care; it is the foundation of professional nursing practice. Ex: Empathy: sharing and understanding how the patient feels. Sympathy: Feeling bad for someone. To Enhance Communication: Listen actively, establish trust, be assertive, restate messages, clarify and validate messages, interpret body language, share observations, explore issues, use silence, summarize the conversation, and make use of process recordings while you are learning. Barriers to Communication: Include asking too many questions; asking why; fire- hosing information; changing the subject inappropriately; failing to listen; failing to probe; expressing approval or disapproval; offering advice; providing false reassurance; stereotyping; and using patronizing language. Cultural and Religious Beliefs in Clients: Christian Scientist Beliefs in the ED Will most likely only encounter these patients following an accident because they do follow Western Medicine as first choice to promote health. Most adults are not likely to accept a blood transfusion. Asian Cultures and Space People stand farther apart and touch less. Jehovah’s Witness and Blood Transfusions View accepting blood transfusions or blood products as morally wrong. However, it is vital for the nurse to educate the client on the reasons why the blood transfusion is needed. Hindu Client and Bathing Hindus prefer to wash in free-flowing water (a shower instead of a tub bath). If a shower is not available, provide a jug of water for the person to use in the bath. Women are modest and usually prefer to be treated by female medical staff. Catholics and Last Rights A Roman Catholic who is seriously ill might wish to receive the sacrament of anointing the sick. This sacrament, once known as the last rights, can be repeated if the person recovers and then becomes ill at a later time. Only a priest can hear the sacrament of reconciliation (confession), during which God, through the agency of the priest, grants forgiveness for past sins. Importance of Safety: SAFETY IS FIRST. Safety is a basic human need. A person’s safety is influenced by developmental factors as well as individual factors, such as lifestyle, cognitive awareness, sensor perceptual status, ability to communicate, mobility status, and sensory losses, particularly hearing and vision losses. Safety Hazards in the Home: The main safety hazards in the home are poisoning, carbon monoxide poisoning, scalds and burns, fires, falls, firearm injuries, suffocation and drowning, and take-home toxins. When a Client Falls? • 1st Priority is to check the patient for any injuries. • Before you check, guide the patient to the floor. Interventions for Fall Risks: • Place client in a room close to the nurse’s station. • Place client with a sitter. • Orient client to room & surroundings & do not reposition furniture. • Keep bed in lowest position. • Remove rugs & keep floors clutter free. • Use proper fitting non-skid footwear. • Keep top 2 bed rails up; maximum 3 bed rails total. • Keep call light within reach. • Ensure proper lighting for patient to see at night. Education for an Elderly Client at Risk for Falls at Home: • Physical activity/exercise, weight bearing for bone strength. • Home modifications: handrails, slip-proof rugs, adequate lighting, avoid scatter rugs, slippery floors, clutter, encourage use of visual, hearing, ambulatory assistive devices. Prolonged Bedrest Can Result in What Types of Physical Issues? • Atrophy/muscle discomfort • pressure wounds/skin breakdown • immunosuppression (pneumonia) • DVT/damage to superficial nerves & blood vessels • Contractures Fire Safety Measures and Priorities: o Fires • Home fires are the major cause of death and injuries • Older adults & children < 5y/o have the highest risk. • Most common causes of fires: - Cooking fires. - Smoking. - Heating Equipment. - Home oxygen administration equipment: 75% of home fires involves oxygen, smoking materials are the ignition source. - Remove the client from the area. o RACE (priority when patient is in fire situation) Rescue – remove patient from danger. Alarm – pull the alarm. Contain - close doors. Extinguish fire (if possible). o PASS (How to use the fire extinguisher) Pull the pin. Aim at the base of the fire. Squeeze the handles. Sweep back and forth. Restraints: *Last Resort* RN may determine the need for restraints, Provider must sign the order within 24 hours. Nursing Interventions: Review medications, provide consistency, encourage family members to interact with patient, use relaxation techniques, reduce noise, frequent assessment, and surveillance communication. RN Responsibilities when using restraints: • Assess the initial restraint placement. • Periodically assess the circulation and skin integrity. • Remove the restraints ASAP when no longer needed • Modify the plan of care to reflect. Unlicensed Professional (UAP) responsibilities when using restraints: o The application of restraints o Period removal of restraints (If UAP is knowledgeable and skilled to.) o Verify the patient’s needs while restrained. Body Mechanics: Body mechanics is a term used to describe the way we move our bodies. It includes four components: body alignment, balance, coordination, and joint mobility. You should always use good body mechanics and teach them to patients for back safety and injury prevention. Body Alignment: Body alignment, also known as posture, is an important aspect of body mechanics. Proper posture places the spine in a neutral (resting) position. Maintain Proper Posture: ➤Avoid standing in one position for a lengthy period. If you cannot change positions, elevate one foot on a stool or box, and alternate foot placement frequently. ➤ Do not lock your knees when standing upright. ➤ Keep your stomach muscles tight to support your back. ➤ Do not bend forward at the waist or neck when you are working in a low position. ➤ When you are seated at your desk, work at a comfortable height. ➤ Do not wear high-heeled or platform shoes for long periods of time. ➤ Do not slump when you sit. ➤ Sit close to your work. ➤ Use a chair that supports your back in a slightly arched position. ➤ Sit with your feet flat on the floor and your knees below your hips. ➤ Sleep on a mattress that is firm but not extremely hard. Balance: The body achieves balance when it is in alignment. For your body to be balanced, your line of gravity must pass through your center of gravity, and your center of grav ity must be close to your base of support. -To avoid injury when moving objects: Place center of gravity closest to base of support, use wide stance, keep object close to body. Coordination: Smooth movement requires coordination between the nervous system and the musculoskeletal system. o Voluntary movement is initiated in the cerebral cortex. o The cerebellum coordinates movements. o Proprioception is the awareness of posture, movement, and position sense. o Basal Ganglia assists with coordination of movement. Benefits of Regular Exercise: Regular physical activity each week, sustained for months and years, can produce long-term health benefits. Strong evidence links regular physical activity with a lower risk for early death, heart disease, stroke, type 2 diabetes, hypertension, hyperlipidemia, metabolic syndrome, colon and breast cancers, and depression. Can promote older adults to help weight loss and maintenance of normal weight when combined with diet; lowers the risk of disability; and promotes better heart and lung function and muscular fitness. Bone reformation and growth, Cardiovascular health promotion, promotes balance and stability, reduces stress and increase energy levels, improve pulmonary circulation, skeletal development, skin tone, reduces systemic inflammation. Diseases Related to Bone Formation or Metabolism Bone formation abnormalities may be congenital, related to dietary deficiencies, or the result of bone disease. Osteogenesis imperfecta (OI): is a congenital disorder of bone and connective tissue that is characterized by brittle bones that fracture easily. Infants with OI are often born with fractures and continue to fracture with minimal trauma or even spontaneously. Prompt recognition and treatment of fractures helps prevent deformities. Achondroplasia, or dwarfism: occurs when the bones ossify (harden) prematurely. Paget’s Disease: is a metabolic bone disease in which increased bone loss results in pain, pathological fractures, and deformities. This disorder usually affects the skull, vertebrae, femur, and pelvis. Vitamin D and Calcium: are needed to form and maintain bone. Deficiencies lead to porous bones. In children, prolonged deficiencies can cause the long bones of the legs to become bowed, retard growth, and lead to frequent fractures. Diseases Affecting Joint Mobility • Diseases of the joints may be degenerative or inflammatory. Osteoarthritis: Progressive deterioration & loss of cartilage & bone in one or more joints (crepitus). The most prevalent type of degenerative joint disease is osteoarthritis (OA). OA involves a loss of articular cartilage in the joint, with pain and stiffness as the primary symptoms. Patients may also have decreased ROM and crepitus, a creaking or grating sound, with joint motion. Symptoms are aggravated by weight-bearing and joint use and are relieved by resting the affected joints. OA is more common in women, older adults, and people who are overweight. Rheumatoid arthritis (RA): is a systemic autoimmune disease involving chronic inflammation of the joints and surrounding connective tissue, frequently resulting in difficulty in performing activities of daily living (ADLs). RA causes joint pain, deformity, and loss of function; patients may also experience fever, fatigue, weakness, and weight loss. RA occurs most frequently in the fingers, wrists, elbows, ankles, and knees. It occurs in 1% to 2% of the population, with a greater incidence in women. The illness usually begins in mid-life, but persons in any age group can be affected. Those in the 30- to 50-year-old range are the most frequently affected age group. Unlike OA, RA does NOT improve with rest. Pain is most intense when the person arises from bed. Pain and joint deformities may so severely affect mobility that patients cannot care for themselves. Non-Pharmacological Interventions for Rheumatoid Arthritis: • Proper positioning, heat/cold therapy, hypnosis, imagery, music therapy, adequate nutrition, gradual weight loss. Continue…Diseases Affecting Joint Mobility Ankylosing Spondylitis: is a chronic inflammatory joint disease characterized by stiffening and fusion of the spine and sacroiliac joints. The inflammation occurs where the ligaments, tendons, and joint capsule insert into the bone. The disease usually develops in young adults, equally in men and women. Signs and symptoms include low back pain and stiffness and decreased ROM of the spine. The convex lumbar curve is lost, and the upper spine curve increases, causing kyphosis. Gout: is an inflammatory response to high levels of uric acid. Crystals form in the synovial fluid, and small white nodules, or tophi, form in the subcutaneous tissues. Gout produces painful joints and severely limits activity during acute flare-ups. Positioning Devices: Healthy people regularly shift position to maintain comfort. However, many patients are unable to move without assistance. They require a change of position at least every 2 hours to prevent skin breakdown, muscle discomfort, damage to superficial nerves and blood vessels, and contractures. Immobile people are more prone to pressure injury as a result of reduced circulation, impaired oxygen exchange to the tissues, and edema. A firm mattress provides support to the patient’s body and makes it easier to turn the patient (because he does not sink down into the mattress). A clean, dry bed also makes it easier to turn the patient and decreases the risk of skin maceration or pressure ulcer formation. Devices to use Adjustable Beds, pillows, side rails, trapeze bar, foot board, etc. Positioning Techniques: Fowler’s Positions: Fowler’s position is a semisitting position, in which the head of the bed is elevated 45° to 60°. • Semi-Fowler’s position, in which the head of the bed is elevated only 30° • High-Fowler’s position, in which the head is elevated 90°. • The lateral position is a side-lying position with the top hip and knee flexed and placed in front of the rest of the body. • Prone laying on stomach • Sims’ position is a semiprone position. The lower arm is positioned behind the patient, and the upper arm is flexed. • Supine laying on back. Range of Motion: Patients with limited mobility are at risk for developing complications of disuse, such as muscle atrophy, joint stiffness, and contractures. To limit the complications of immobility, patients recovering from illness, injury, or surgery often perform Active range of motion (AROM): as a rehabilitation procedure. Additionally, movement with ADLs improves joint mobility, circulation, muscular strength. AROM also improves and respiratory and cardiac function. MOVE ON YOUR OWN. Passive range of motion (PROM): is movement of the joints through their range of motion by another person. SOMEONE HELPING YOU MOVE. Both AROM and PROM improve joint mobility, increase circulation to the area exercised, and help maintain function. Continuous passive motion, also called CPM, is a device that repetitively but gently flexes and extends the knee joint. The CPM machine is often used after knee re- placement or other knee procedures to allow the joint to improve range of motion, eliminate the problem of stiff- ness, and prevent the development of adhesions, which can limit motion further. Diagnostic and Imaging Assessment: Imaging studies for patients who report mild nonspecific back pain may not be done, depending on the nature of the pain. Patients with severe or progressive motor or SENSORY PERCEPTION deficits or who are thought to have other underlying conditions (e.g., cancer, infection) require complete diagnostic assessment. To determine the exact cause of the pain, a number of diagnostic tests may be used, including: • Plain X-Rays (show general arthritis changes and bony alignment) • CT Scan (shows spinal bones, nerves, disks, and ligaments) • MRI (provides images of the spinal tissue, bones, spinal cord, nerves, ligaments, musculature, and disks) • Bone Scan (shows bone changes by injecting radioactive tracers, which attach to areas of increased bone production or show increased vascularity associated with tumor or infection) • Myelogram/post-myelogram CT (evaluates nerve root lesions and any other mass, lesion, or infection of the meninges or spinal cord). Electro diagnostic Testing, such as electromyography (EMG) and nerve-conduction studies, may help distinguish motor neuron diseases from peripheral neuropathies and radiculopathies (spinal nerve root involvement). These tests are especially useful in chronic diseases of the spinal cord or associated nerves. Labs Table (49-2): TEST NORMAL RANGE FOR ADULTS SIGNIFICANCE OF ABNORMAL FINDINGS Serum calcium 9.0-10.5 mg/dL (2.25- 2.75 mmol/L) Older adults: decreased Hypercalcemia(increased calcium) • Metastatic cancers of the bone • Paget's disease • Bone fractures in healing stage Hypocalcemia(decreased calcium) • Osteoporosis • Osteomalacia Serum phosphorus (phosphate) 3.0-4.5 mg/dL (0.97- 1.45 mmol/L) Older adults: decreased Hyperphosphatemia(increased phosphorus) • Bone fractures in healing stage • Bone tumors • Acromegaly Hypophosphatemia(decreased phosphorus) • Osteomalacia Alkaline phosphatase (ALP) 30-120 units/L Older adults: slightly increased Elevations may indicate: • Metastatic cancers of the bone or liver • Paget's disease • Osteomalacia Serum muscle enzymes Creatine kinase (CK-MM) Total CK: Men: 55-170 units/L Elevations may indicate: • Muscle trauma • Progressive muscular dystrophy TEST NORMAL RANGE FOR ADULTS SIGNIFICANCE OF ABNORMAL FINDINGS Women: 30- 135 units/L CK-MM: 96%- 100% • Effects of electromyography Lactic dehydrogenase (LDH) Total LDH: 100- 190 units/L LDH1: 17%- 27% LDH2: 27%- 37% LDH3: 18%- 25% LDH4: 3%-8% LDH5: 0%-5% Elevations may indicate: • Skeletal muscle necrosis • Extensive cancer • Progressive muscular dystrophy Aspartate aminotransferase (AST) 0-35 units/L Older adults: slightly increased Elevations may indicate: • Skeletal muscle trauma • Progressive muscular dystrophy Aldolase (ALD) 3.0-8.2 units/dL Elevations may indicate: • Polymyositis and dermatomyositis • Muscular dystrophy Osteoporosis: Osteoporosis: Osteoporosis is a chronic disease of CELLULAR REGULATION in which bone loss causes significant decreased density and possible fracture. It is often referred to as a silent disease or silent thief because the first sign of osteoporosis in most people follows some kind of a fracture. The spine, hip, and wrist are most often at risk, although any bone can fracture. Primary osteoporosis is caused by a combination of genetic, lifestyle, and environmental factors. The Joint Commission's National Patient Safety Goals (NPSGs) specify the need to reduce risk for harm to patients resulting from falls. People with osteoporosis are at an increased risk for fracture if a fall occurs. Health History- Body build, weight, and race/ethnicity seem to influence who gets the disease. Osteoporosis occurs most often in older, lean-built Euro-American and Asian women, particularly those who do not exercise regularly. However, African Americans are at risk for decreased vitamin D, which is needed for adequate calcium absorption in the small intestines. Education on reducing the risk of Osteoporosis: Prevent obesity, proper nutrition, avoid injuries, weight baring exercises. Active lifestyle, avoid staying (sitting or lying) in one spot for too long, participate in ADL’S Osteomyelitis: Osteomyelitis: Infection in bony tissue can be acute or chronic as well as difficult to treat problem. Bone infection can result in chronic recurrence of infection, loss of function and MOBILITY, amputation, and even death. Bacteria, viruses, or fungi can cause infection in bone, known as osteomyelitis. Invasion by one or more pathogenic microorganisms stimulates the inflammatory response in bone tissue. Osteomyelitis may be categorized as exogenous, in which infectious organisms enter from outside the body as in an open fracture, in which organisms are carried by the bloodstream from other areas of infection in the body. The most common cause of contiguous spread in older adults is found in those who have slow-healing foot ulcers. Assessment- Bone pain, with or without other signs and symptoms, is a common concern of patients with osteomyelitis. The pain is described as a constant, localized, pulsating sensation that worsens with movement. The patient with acute osteomyelitis has fever, usually with temperature greater than 101° F (38.3° C). Older adults may not have an extreme temperature elevation because of a lower core body temperature and compromised immune system that occur with normal aging. The area around the infected bone swells and is tender when palpated. Priorities in discharge instructions for Osteomyelitis: • 4-6 weeks of antibiotic therapy for acute osteomyelitis. • May require wound irrigation & medicated beads that are directly in contact with the wound. • May be in contact isolation precautions if area is draining copious amounts of drainage. • Hyperbaric oxygen therapy. Plantar Fasciitis: Plantar Fasciitis: Plantar Fasciitis is an inflammation of the plantar fascia, which is located in the area of the arch of the foot. It is often seen in middle-age and older adults, as well as in athletes, especially runners. Obesity is also a contributing factor. Patients report severe pain in the arch of the foot, especially when getting out of bed. The pain is worsened with weight bearing. Although most patients have unilateral plantar fasciitis, the problem can affect both feet. Most patients respond to conservative management, which includes rest, ice, stretching exercises, strapping of the foot to maintain the arch, shoes with good support, and orthotics. NSAIDs or steroids may be needed to control impaired COMFORT and inflammation. If conservative measures are unsuccessful, endoscopic surgery to remove the inflamed tissue may be required. Teach the patient about the importance of adhering to the treatment plan and coordinating care with the physical therapist for instruction in exercise. Upper and Lower Extremity Fractures: • Complete Fracture: Complete fracture. The break is across the entire width of the bone in such a way that the bone is divided into two distinct sections. • Displaced Fracture: If bone alignment is altered or disrupted, the fracture is also referred to as a displaced fracture. The ends of bone sections of a displaced fracture are more likely to damage surrounding nerves, blood vessels, and other soft tissues. • Incomplete Fracture: The fracture does NOT divide the bone into two portions because the break is through only part of the bone. This type of fracture is not typically displaced. A fracture can also be described by the extent of associated soft-tissue damage; open ( compound) or closed ( simple). The skin surface over the broken bone is disrupted in a compound fracture, which causes an external wound. These fractures are often graded to define the extent of tissue damage. A simple fracture does not extend through the skin and therefore has no visible wound. Open fractures- Interventions in Reducing Infection: 1. Hand washing or strict infection control. 2. Dressing changes with aseptic technique. 3. Monitor vital signs especially temperature & heart rate. 4. Administer broad spectrum antibiotics if ordered (Clindamycin & Gentamycin) 5. If irrigating open wound may be used using an antibiotic solution. 6. For chronic infections – adherence to antibiotic regimen. Describe Stages of Bone Healing: • Stage 1: 24-72 hours after injury hematoma formation. • Stage 2: 3 days-2 weeks granulation tissue invades hematoma forming fibrocartilage. • Stage 3: 3-6 weeks callus formation. • Stage 4: 3-8 weeks callus is gradually reabsorbed and transformed into bone. • Stage 5: 4-6 weeks to a year consolidation and remodeling of bone to continue to meet mechanical demands. Carpal Tunnel Syndrome (CTS): is a common condition in which the median nerve in the wrist becomes compressed, causing pain and a numb sensation. The carpal tunnel is a rigid canal that lies between the carpal bones and a fibrous tissue sheet. A group of tendons surround the synovium and share space with the median nerve in the carpal tunnel. When the synovium becomes swollen or thickened, this nerve is compressed. first three fingers of the hand and the palmar aspect of the fourth (ring) finger. Because the median nerve is close to other structures, wrist flexion causes nerve impingement, and extension causes increased pressure in the lower portion. Is the most common type of repetitive stress injury (RPI). People whose jobs require repetitive hand activities such as pinching or grasping during wrist flexion (e.g., factory workers, computer operators, jackhammer operators) are predisposed to CTS. It can also result from overuse in sports activities such as golf, tennis, or racquetball. CTS usually presents as a chronic problem. Rotator Cuff Injuries: The musculotendinous, or rotator, cuff of the shoulder functions to stabilize the head of the humerus in the glenoid cavity during shoulder abduction. Young adults usually sustain a tear of the cuff by substantial trauma, such as may occur during a fall, while throwing a ball, or with heavy lifting. Older adults tend to have small tears related to aging, repetitive motions, or falls; and the tears are usually painless. The patient with a torn rotator cuff has shoulder pain and cannot easily abduct the arm at the shoulder. When the arm is abducted, he or she usually drops it because abduction cannot be maintained (drop arm test). Pain is more intense at NIGHT. Partial-thickness tears are more painful than full-thickness tears, but full-thickness tears result in more weakness and loss of function. Patients then begin rehabilitation in the ambulatory-care occupational therapy department. Teach them that they may not have full function for several months. Physical Assessment: • Assess the head for any hair distribution, lesions, bumps, or redness. • Examine the eyebrows and eyelashes for hair distribution and determine the direction of the eyelashes. Eyelashes normally point outward and away from the eyelid. Assess the eyelids for ptosis(drooping), redness, lesions, or swelling. • Assess for symmetry in the appearance of the eyes. Check them to determine whether they are equally distant from the nose, are the same size, and have the same degree of prominence. • Look for head tilting, squinting, or other actions that indicate that the patient is trying to attain clear vision. For example, patients with double vision may cock the head to the side to focus the two images into one, or they may close one eye to see clearly. • Scleral and corneal assessment require a penlight. Examine the sclera for color; it is usually white. A yellow color may indicate jaundice or systemic problems. • Assess the responses for each eye. (You may see the abbreviation “PERRLA” in a patient's electronic health record, which stands for pupils equal, round, reactive to light, and accommodation.) • Assess for accommodation by holding your finger about 18 cm from the patient's nose and move it toward the nose. The patient's eyes normally converge during this movement, and the pupils constrict equally. • Visual acuity tests measure both distance and near vision. The Snellen eye chart measures distance vision. This chart has letters, numbers, pictures, or a single letter presented in various positions. • Assess balance by using the Romberg Test. Psychosocial Assessment: A patient with changes in visual SENSORY PERCEPTION may be anxious about possible vision loss. Patients with severe visual defects may be unable to perform ADLs. Dependency from reduced vision can affect self-esteem. Ask the patient how he or she feels about the vision changes and assess coping techniques. Assess the family to determine available support. Provide information about local resources and services for patients with reduced vision. Cataracts: A cataract is a lens opacity that distorts the image. With aging, the lens gradually loses water and increases in density. With time, as lens density increases and transparency is lost, visual SENSORY PERCEPTION is greatly reduced. Both eyes may have cataracts, but the rate of progression in each eye is different. Cataracts may be present at birth or develop at any time. They may be age related or caused by trauma or exposure to toxic agents. the onset of cataract formation occurs earlier with heavy sun exposure or exposure to other sources of ultraviolet (UV) light. Reduce the risk of UV light damage outside by wearing sunglasses. Early signs and symptoms of cataracts are slightly blurred vision and decreased color perception. At first the patient may think that his or her glasses or contact lenses are smudged. As lens cloudiness continues, blurred and double vision occurs, and the patient may have difficulty with ADLs. Without surgical intervention, visual impairment progresses to blindness. No pain or eye redness is associated with age-related cataract formation. Instruct patients to contact the surgeon if pain occurs with nausea or vomiting. To prevent increases in IOP, teach the patient and family about activity restrictions. Activities that can cause a sudden rise in IOP such as: bending from the waist, lifting objects that weigh more than 10 lbs, sneezing, coughing, blowing the nose, etc. Nursing interventions focus on helping the patient and family plan the eye drop schedule and daily home eye examination. Cataracts Continue… Teach the patient about activity restrictions. Cooking and light housekeeping are permitted, but vacuuming should be avoided for several weeks because of the forward flexion involved and the rapid, jerky movements required. Advise him or her to refrain from driving until vision is not blurry. Describe Symptoms of Bilateral Cataracts. • Blurred/clouded vision • Double vision • Decreased color perception • Problems with ADLs • Decreased visual acuity, recent in prescription change • Difficulty with night vision and sensitivity to light/glare • Rate and development of cataracts vary in each eye • May think glasses are smudged. • Halos around objects Refractive Errors: The main types of refractive errors are: Myopia (nearsightedness) The eye over refracts the light and bent images fall in front of, not on the retina causing far away objects to appear blurry. Hyperopia (farsightedness) Presbyopia (loss of near vision with age), and astigmatism. Glaucoma: Glaucoma is a group of eye disorders resulting in increased intraocular pressure (IOP). The gel in the posterior segment (vitreous humor) and the fluid in the anterior segment (aqueous humor) must be present in set amounts that apply pressure inside the eye to keep it ball shaped. There are several causes and types of glaucoma; classified as primary, secondary, or associated. The most common type is primary glaucoma. • Primary OPEN-angle glaucoma (POAG), the most common form of primary glaucoma, usually affects both eyes and has no signs or symptoms in the early stages. • Primary angle-CLOSURE glaucoma (PACG or acute glaucoma): has a sudden onset and is an emergency. The problem is a forward displacement of the iris, which presses against the cornea and closes the chamber angle, suddenly preventing outflow of aqueous humor. The best prevention against damage that glaucoma can cause is for adults to have eye examinations with glaucoma checks done every 2 to 4 years before age 40. The priority nursing intervention for the patient with glaucoma is teaching. Teach the patient that the benefit of drug therapy occurs only when the drugs are used on the prescribed schedule, usually every 12 hours. Teach patients the importance of instilling the drops on time and not skipping doses. When more than one drug is prescribed, teach the patient to wait 5 to 10 minutes between drug instillations to prevent one drug from “washing out” or diluting another drug. Stress the need for good handwashing, keeping the eye drop container tip clean, and avoiding touching the tip to any part of the eye. Also teach the technique of punctal occlusion (placing pressure on the corner of the eye near the nose) immediately after eye drop instillation to prevent systemic absorption of the drug. Glaucoma (open and closed angle) which test determines the difference? Gonioscopy is used when IOP is high and can determine whether a patient has open or close angled glaucoma. A special lens eliminates the corneal curve and allows for visualization of where the iris meets the cornea. The procedure is painless. Or ultrasonic imaging. Education for the reason that glaucoma is irreversible. Continued retinal hypoxia as result of glaucoma results in necrosis of photoreceptors and nerve fibers leading to permanent nerve damage. Meaning these nerves cannot be repaired and the damage that has been done is nonreversible. Additionally, extensive loss of photoreceptors and nerve fibers can result in permanent blindness. What is normal intra-ocular eye pressure (IOP)? • 12-22mmHg Orientation to a new room for a blind client? • Use clock wise or compass direction. • Ask the patient if describing the layout would help. • Speak to patient in normal tone and normal voice. Eye Drops contain beta blockers (Timolol-used to treat glaucoma). What precautions need to be taken by the nurse when administering these drops? • Nurse must monitor glucose levels and vital signs. If blood pressure or HR too low, hold medication. • Additional side effects include hives, difficulty breathing, swelling of the face, lips, tongue, and/or throat. • Nurse must assess airway and breathing and for signs of swelling of the face, lips, tongue and/or the throat. • Ask whether the patient has moderate to severe asthma or COPD. If these drugs are absorbed systemically, they constrict the pulmonary smooth muscle and narrow airways. • Warn the patients with diabetes to check their blood glucose levels more often with this medication. Induces hypoglycemia and can mask symptoms of hypoglycemia • Teach patients who also take oral beta-blockers to check their pulse at least 2x daily and to notify a provider if their pulse is consistently below 58 beats/min. Timolol can cause an unsafe drop in pulse and BP. Hearing Loss: Conductive Hearing Loss: Is an alteration in the middle ear that blocks sound waves before they reach the cochlea of the inner ear. Usually a history of middle ear infections and older age. Expected findings- hears better in a noisy environment, speaks softly, packed cerumen, etc. Sensorineural Hearing Loss: Is an alteration in the inner ear, auditory nerve, or hearing center of the brain. Risk factors include; prolonged exposure to loud noise, ototoxic medications, infectious process, and older age. Expected Findings are tinnitus (ringing of the ear), dizziness, hears poorly in a noisy environment, speaks loudly, etc. Hearing assessment begins while observing the patient listening to and answering questions. The patient's posture and responses can provide information about hearing acuity. Other indicators of hearing difficulty include frequently asking the speaker to repeat statements or frequently saying, “What?” or “Huh?” Notice whether the patient responds to whispered questions and startles when an unexpected sound occurs in the environment. . Teach patients the safe way to clean their ears, stressing that nothing smaller than his or her own fingertip should be inserted into the canal. Hearing Loss Continue… What is another word for earwax? • Cerumen What is Vertigo? • Feeling of a spinning sensation What medical term is used to describe ringing in the ears? • Tinnitus How do you apply ear drops? • Pull upper ear up and back. Education for a client with Meniere’s disease? (inner ear disorder that causes episodes of vertigo). • Teach patient to move head slowly to prevent worsening of vertigo • Encourage nutritional and lifestyle changes (stop smoking), such as reducing sodium intake to help reduce excess retention of endolymphatic fluid, adhere to medications. Hearing Loss Continue… How can communication be improved with a client wearing hearing aids? • Position yourself directly in front of the patient. • Ensure that you are not sitting or standing in front of a bright light or window, which can interfere with the patient's ability to see your lips move. • Make sure that the room is well lighted. • Get the patient's attention before you begin to speak. • Move closer to the better-hearing ear. • Speak clearly and slowly. • Do not shout (shouting often makes understanding more difficult). • Keep hands and other objects away from your mouth when talking to the patient. • Have conversations in a quiet room with minimal distractions. • Have the patient repeat your statements, not just indicate assent. • Rephrase sentences and repeat information to aid understanding. • Use appropriate hand motions. • Write messages on paper if the patient is able to read. • Remove distractions like turning off the television. Pressure Injuries: A pressure injury is a loss of TISSUE INTEGRITY caused when the skin and underlying soft tissue are compressed between a bony prominence and an external surface for an extended period. Tissue compression from pressure restricts blood flow to the skin, resulting in reduced tissue perfusion and gas exchange, which eventually leads to cell death. Ulcers occur most often in adults with limited mobility because they cannot change their position to relieve pressure. Friction and shear are mechanical forces that impair skin TISSUE INTEGRITY and cause skin tears, which set the stage for skin breakdown. Excessive skin moisture, such as urinary or fecal incontinence, also increases the risk for skin damage. Nutrition status is an important concern. Protein malnutrition makes normal tissue more prone to breakdown and also delays healing A pressure injury prevention program consists of two steps: (1) early identification of high-risk patients. (2) implementation of aggressive intervention for prevention with the use of pressure-relief or pressure-reduction devices. RISK FACTORS FOR PRESSURE INJURIES: Mental status changes and decreased sensation determine whether the patient is a partner in pressure injury prevention. Impaired mobility is a factor in the risk for pressure injury formation. Nutrition status is a critical risk factor for pressure injury development and for successful healing Incontinence results in prolonged contact of the skin with substances that irritate the skin, destroy TISSUE INTEGRITY, and predispose to skin breakdown Pressure Injuries Continue… Stage 2 • Skin is not intact. • There is partial-thickness skin loss of the epidermis or dermis. • Ulcer is superficial and may be characterized as an abrasion, a blister (open or fluid-filled), or a shallow crater. • Bruising is not present. Stage 3 • Skin loss is full thickness. • Subcutaneous tissues may be damaged or necrotic. • Damage extends down to but not through the underlying fascia; bone, tendon, and muscle are not exposed. • The depth can vary with anatomic location; areas of thin skin (e.g., the bridge of the nose) may show only a shallow crater, whereas thicker tissue areas with larger amounts of subcutaneous fat may show a deep, crater-like appearance. • Undermining and tunneling may or may not be present. Stage 4 • Skin loss is full thickness with exposed or palpable muscle, tendon, or bone. • Often includes undermining and tunneling. • Sinus tracts may develop. • Slough and eschar are often present on at least part of the wound. Unstageable Skin loss is full thickness; and the base is completely covered with slough or eschar, obscuring the true depth of the wound. Pressure Injuries Continue… How to Prevent Pressure Injuries by Positioning? • Pad contact surfaces with foam, silicone gel, air pads, or other materials with pressure-redistribution properties. • Do not keep the head of the bed elevated above 30 degrees to prevent shearing. • Use a lift sheet to move a patient in the bed. Avoid dragging or sliding him or her. • When positioning a patient on his or her side, position at a 30-degree tilt. • Re-position an immobile patient at a frequency consistent with assessed needs. • Do not place a rubber ring or donut under the patient's sacral area. • When moving an immobile patient from a bed to another surface, use a designated slide board well lubricated with talc or use a mechanical lift. • Place pillows or foam wedges between two bony surfaces. • Keep the patient's skin directly off plastic surfaces. • Keep the patient's heels off the bed surface using bed pillow under ankles or a heel-suspension device. Explain why certain medications place clients at risk for pressure ulcers? • Some medications alter the blood flow. This causes less blood to go to pressure areas. May lead to necrosis. Pressure Injuries Continue… Reducing Shear (Skin) Injury? • Avoid pulling, tugging, and sliding patient against the bed. • Keep head of bed at a slight elevation. • Make sure sheets and blanket DON’T have ripples in then that rub against the patient’s skin. • Use others to assist in moving patient to protect from shearing. Positioning to reduce injury to bony prominences? • Place pillows under areas and elevate. • Change positioning every 2 hours. • Elevate calves to protect heels. How Do Pressure Ulcers Develop? Patients at risk for developing pressure ulcers are those with immobility, friction and shear, moisture, incontinence, poor nutrition, perfusion, age, skin condition, and altered level of consciousness. Pressure ulcers are caused by unrelieved pressure, or pressure in combination with shearing forces. These compromise blood flow to an area, resulting in ischemia (inadequate blood supply) in the underlying tissue. Tissue ischemia leads to tissue anoxia (lack of oxygen) and cell death. Pressure ulcers can occur in as little time as 2 hours, though they may take as long as 5 days for the full extent of tissue dam- age to be known. Nutrition and Hydration of Skin Integrity: Skin condition reflects overall nutritional status, and at the same time nutritional intake affects the skin. Adequate intake of protein, cholesterol, calories, fluid, vitamin C, and minerals is essential to maintaining skin integrity. Protein: Healthy skin depends on adequate protein levels to maintain the skin, repair minor defects, and preserve intravascular volume. Edema (excess fluid in the tissues) develops. Edema decreases skin elasticity and interferes with the diffusion of oxygen to the cells. Therefore, the skin becomes prone to breakdown. Cholesterol: Low cholesterol levels predispose patients to skin breakdown and inhibit wound healing. Patients on low-fat tube feedings may experience deficiencies in cholesterol, fatty acids, and linoleic acid. Together, these fats aid in providing fuel for wound healing and maintain a waterproof barrier in the stratum corneum. Calorie Intake: If calorie intake is inadequate, the body uses proteins for energy (catabolism); they are then unavailable for building and maintenance functions (anabolism). When under nutrition is prolonged, the person experiences weight loss, loss of subcutaneous tissue, and muscle atrophy. As a result, padding between the skin and the bones decreases, predisposing the skin to pressure ulcers. Nutrition and Hydration of Skin Integrity: Ascorbic Acid, Zinc, and Copper: Vitamin C or ascorbic acid, is involved in the formation and maintenance of collagen, so a deficiency can delay wound healing. Zinc and copper are also involved in collagen formation, and deficiencies of either may impair healing. Hydration: Skin turgor depends on hydration. Poor skin turgor may occur as a result of dehydration, whereas edema may result from over hydration. Both dry, dehydrated, as well as edematous, overhydrated skin is prone to injury, especially when exposed to pressure, shearing, friction, and moisture. For further discussion on fluid requirements. Types of Wound Drainage: Drainage is the flow of fluids from a wound or cavity. It is often referred to as exudate and is fluid that oozes as a result of inflammation. Exudate may take several forms. • Serous Exudate: Clean wounds typically drain serous exudate. It is watery in consistency and contains very little cellular matter. Serous exudate consists of serum, the straw- colored fluid that separates out of blood when a clot is formed. • Sanguineous Exudate: You will often see sanguineous exudate with deep wounds or wounds in highly vas- cular areas. Sanguineous exudate is bloody drainage. It indicates damage to capillaries. Fresh bleeding pro- duces bright red drainage, whereas older, dried blood is a darker, red-brown color • Serosanguineous Drainage: In new wounds, you will most commonly see serosanguineous drainage, a combination of bloody and serous drainage. • Purulent Exudate: The thick, often malodorous, drainage that is seen in infected wounds is called pu- rulent exudate. It contains pus, a protein-rich fluid filled with WBCs, bacteria, and cellular debris. It is commonly caused by infection from pyogenic (pus- forming) bacteria, such as streptococci or staphylo- cocci. Normally, pus is yellow in color, although it may take on a blue-green color if the bacterium Pseudomonas aeruginosa is present. • Purosanguineous Exudate: Red-tinged pus is called purosanguineous exudate. It indicates that small vessels in the wound area have ruptured. Wounds: Stages of Wounds (I, II, III, IV): 1. Hemostasis- clotting 2. Inflammatory Phase- Cleaning (also forms a scab to protect) 3. Proliferative phase- granulation (a beefy red tissue that bleeds readily and is easily damaged.) “regeneration or healing” (occurs 5- 21 days) 4. Maturation phase- scar (a scar is only 80% as strong as the original tissue.) Priority actions with Wound Assessment: • Identify reason for impaired skin integrity. • Assess the wound: location, size, color, extent of tissue involvement, wound base and margins, exudate, condition of surrounding tissue. • Presence of foreign body. • pain level. • Nutritional status. Appropriate Diet for a Client with a Healing Wound: • Well-balanced diet, emphasizing protein, • Vegetables, fruits, whole grains and vitamins. Increase caloric intake. Primary Intention Healing: When a wound involves minimal or no tissue loss and has edges that are well approximated (closed), primary (first) intention healing takes place. Little scarring is expected. A clean surgical incision heals by this method. Secondary Intention Healing: Healing by secondary (second) intention occurs when a wound (1) involves extensive tissue loss, which prevents wound edges from approximating, or (2) should not be closed (e.g., because it is infected). Because the wound is left open, it heals from the inner layer to the surface by filling in with beefy red granulation tissue (a form of connective tissue with an abundant blood supply). Epithelial tissue may appear in the wound as small pink or pearl- like areas. Key Point: Do not mistake this as a sign of infection. Wounds that heal by secondary intention heal more slowly, are more prone to infection, and develop more scar tissue. Pressure ulcers (discussed later) and infected wounds are examples. Tertiary Intention Healing: A wound heals by tertiary (third) healing, also called delayed primary closure, when two surfaces of granulation tissue are brought together. This technique may be used when the wound is clean-contaminated or contaminated. Initially the wound is allowed to heal by secondary intention. When there is no evidence of edema, infection, or foreign matter, the wound edges are closed by bringing together the granulating tissue and suturing the surface. Such wounds require strict aseptic technique during all dressing changes because they are prone to infection. Tertiary intention healing creates less scarring than does secondary, but more than primary intention healing. Types of Wounds: Abrasion- A scrape of the superficial layers of the skin; usually unintentional but may be performed intentionally for cosmetic purposes to smooth skin surfaces. Abscess- A localized collection of pus resulting from invasion from a pyogenic bacterium or other pathogen; must be opened and drained to heal. Contusion- A closed wound caused by blunt trauma. May be referred to as a bruise or ecchymotic area. Crushing- A wound caused by force leading to compression or disruption of tissues. Often associated with fracture. Usually there is minimal or no break in the skin. Incision- An open, intentional wound caused by a sharp instrument. Laceration- The skin or mucous membranes are torn open, resulting in a wound with jagged margins. Penetrating- An open wound in which the agent causing the wound lodges in body tissue. Puncture- An open wound caused by a sharp object. Often there is collapse of tissue around the entry point, making this wound prone to infection. Tunnel- A wound with an entrance and exit site. Know Appropriate Nursing Interventions for Wounds: • Physical Assessment- Noticing signs and symptoms. • Wound Care Assessment- Record the location and size of wound measuring length, width, and depth. • Change synthetic dressings when exudate cause the adhesive seal to break and leakage to occur. • Assessing for infection and inflammation- monitor for signs of infection (cellulitis, progressive increase in ulcer size and depth, change in exudate, signs of bacteria (fever, elevated WBC count). • Reducing mechanical forces- Obtain pressure reduction devices. Protects against the mechanical forces of pressure, sheer, friction. • Interpreting Lab values- Evaluate WBCs, prealbumin, and total protein levels. • Pain- medicate the client with pain medication for deep wounds such as tunneling. Client Education for Cellulitis: • Take prescribed antibiotic until gone. • Keep the infected area clean. • Raise the infected area above the level of heart to keep swelling down. • Apply clean bandage as advised. • Take temperature once a day. • Wash your hands often to prevent spreading the infection. • Advise how to apply cool compress for discomfort alternating with warm and moist compress. Depth of the Wound: Superficial wounds: involve only the epidermal layer of the skin. The injury is usu- ally the result of friction, shearing, or burning. Partial Thickness: wounds extend through the epidermis but not through the dermis. Full-thickness: wounds extend into the subcutaneous tissue and beyond. The descriptor penetrating is sometimes added to indicate that the wound involves internal organs. Wound depth is a major determinant of healing time: The deeper the wound, the longer the healing time. The Braden Scale: Used to identify persons at risk for developing pressure ulcers. The Braden scale evaluates six major risk factors: sensory perception, moisture, activity, mobility, nutrition, and friction and sheer. The final score reflects the patient’s risk; the lower the score, the more likely the patient will develop a pressure ulcer. A score of 18 or less for hospitalized patients indicates risk. Interventions should be based on individual risk factors, as well as the total score. You should use this scale to assess the patient on admission to the facility and again in 48 to 72 hours or per facility policy. Studies have shown the second score to be more predictive, probably related to an increased awareness of the patient’s status. The Braden Q is a modified scale used in children. The Norton Scale: Assesses risk based on the patient’s physical condition, mental state, activity, mobility, and incontinence. A low score indicates a high risk. Some have suggested that the Norton scale should be modified by adding categories for skin appearance, medication, and nutrition. Analysis/Nursing Diagnosis: The following nursing diagnoses are appropriate for patients who are at risk for skin breakdown or for patients who have wounds. • Risk for Impaired Skin Integrity is appropriate for patients who have one or more risk factors for skin breakdown (e.g., immobility, incontinence, extremes of age, impaired circulation, impaired sensation, under nutrition, emaciation). NANDA International (2009) recommends that you use a risk assessment tool (e.g., Norton or Braden scale) to identify these patients. • Impaired Skin Integrity is appropriate for patients who have experienced damage to the epidermis or dermis, for example, patients who have superficial wounds or stage I or II pressure ulcers. • Impaired Tissue Integrity is appropriate for patients with wounds that extend into the subcutaneous tissue, muscle, or bone. Use this diagnosis for patients with deep wounds or stage III or IV pressure ulcers. • Risk for Impaired Tissue Integrity is appropriate for clients with Impaired Skin Integrity who are at risk for delayed healing. • Skin problems and wounds can be the etiology for other nursing diagnoses as well. • Risk for Infection is an appropriate diagnosis if the patient has a traumatic wound or is immunosuppressed, undernourished, or immobile. • Pain is a diagnosis that may be used for patients who are experiencing discomfort from the wound or from the treatments required to heal the wound. • Disturbed Body Image should be used if the patient is experiencing distress about the wound. Consider this diagnosis even if the patient is expected to make a complete recovery. Some patients experience extreme distress about wounds. You will certainly want to consider this diagnosis if the patient experiences an injury that is expected to result in disfigurement. Human Immune Deficiency Virus (HIV/AIDS): What Fluid DOESN’T Transmit HIV? -Saliva What Is Commonly Held as a False Belief? -Myth What does the I in HIV Stand For? -immunodeficiency What T cell count is Associated with Aids? -200 Can You Be Born With HIV? -True What is a Lymphocyte? -White Blood Cell What is One Way HIV is NOT transmitted? -Sharing a Water Fountain Which of the Following is NOT a Mucous Membranes? -Nails Which Bodily Fluid Has the Highest Viral Load? -Blood Which Test Confirms HIV? -ELISA What is the Treatment for HIV? -Anti-Retroviral Where Did HIV Start? -Western Africa Is There is a cure for HIV/AIDS? -False Human Immune Deficiency Virus (HIV/AIDS): An Infection That a Healthy Immune System Would Normally Be Able to Fight Off and Get Rid Of? -Opportunistic Infections A Rare Type of Skin Cancer That is HIV Related? -Kaposi’s Sarcoma What Has the Highest Rate of Transmission? -Injection Drug Use (sharing needles) Anti-Retro Viral Therapy Helps to Decrease the Viral Load in the Body? -True What are Ways to Reduce Transmission? -Condom, Getting Tested, Monogamous Relationships. The cause of HIV infection is a virus—the human immune deficiency virus. This virus, just like all other viruses, is an intracellular parasite because it must use the infected cell's resources to reproduce. The HIV can infect a cell and take over its functions to force the cell to make more copies of the virus (viral particles). These new viral particles are able to infect more cells, repeating the cycle as long as there are new host cells to infect. Human immune deficiency virus (HIV) infection and disease can progress to acquired immune deficiency syndrome (AIDS). This common chronic disorder of impaired immunity is a serious worldwide epidemic. Effects of HIV infection are related to the new genetic instructions that now direct CD4+ T-cells to change their role in immune system defenses. The new role is to be an “HIV factory,” making up to 10 billion new viral particles daily. For adults who have been transfused with HIV-contaminated blood, AIDS often develops quickly. For those who become HIV positive as a result of a single sexual encounter, progression to AIDS takes much longer. Other personal factors that influence progression to AIDS include frequency of re-exposure to HIV, presence of other sexually transmitted infections (STIs), NUTRITION status, and stress. Enhancing Nutrition: Many patients with AIDS have difficulty maintaining their weight and NUTRITION status, and a registered dietitian is part of the inter-professional health care team. This problem may be caused by fatigue, anorexia, nausea and vomiting, difficult or painful swallowing, diarrhea, intestinal malabsorption, or wasting syndrome. Opportunistic Infections: Opportunistic Infections are those caused by overgrowth of the patient's microbiome (normal flora). Only when IMMUNITY is depressed are such organisms capable of causing infection. Opportunistic Infections occur because of the profound reduced IMMUNITY of the adult with HIV disease. Opportunistic Infections account for many of the signs and symptoms observed in HIV/AIDS and can be protozoan, fungal, bacterial, or viral. These infections can result in death if appropriate treatment is not started quickly. - Priority nursing actions when caring for a patient who is HIV positive are continually assessing for and documenting the presence of an opportunistic infection and monitoring the patient's response to therapy. - Report to the primary health care provider any signs and symptoms that may indicate an infection. Bacterial infection: are acquired from other people or sources and as overgrowth of skin flora. That invade tissue. Occur after minor cuts or scrapes. Ex: UTI, strep throat. Viral Infection: is a proliferation of a harmful virus inside the body. Viruses cannot reproduce without the assistance of a host. Viruses infect a host by introducing their genetic material into the cells and hijacking the cell's internal machinery to make more virus particles. Ex: Chicken pox, measles, herpes. Fungal Infection: A fungus that invades the tissue can cause a disease that's confined to the skin, spreads into tissue, bones, and organs, or affects the whole body. Ex: athletes foot, jock itch, ringworms, pneumonia. Healthcare-Associated Infections: The term healthcare-associated infections (HAIs) refers to infections associated with healthcare given in any setting (e.g., hospitals, home care, long-term care, and ambulatory settings). Healthcare-associated infections aggravate existing illness and lengthen hospital stay and recovery time. HAIs are the leading complication of hospital care and one of the 10 leading causes of death in the United States and are preventable. Approximately 1 out of every 20 hospitalized patients will contract an HAI. Ill patients are vulnerable to infection, and they are a source of infection for others. In addition, they undergo invasive procedures (e.g., injections), which can introduce infectious organisms into their body. • What is Nosocomial Infection? - Hospital-Acquired Infection. Mode of Transmission: Contact, either direct or indirect, is the most frequent mode of transmission of infection. Direct contact between two people usually involves touching, kissing, or sexual intercourse. Animals commonly transmit infection via scratching and biting as well. Indirect contact involves contact with a fomite, a contaminated object that transfers a pathogen. For example, suppose that while you are charting you begin to sneeze or cough. If you cover your nose and mouth with your hand and then resume charting, you may transmit pathogens to the pen, paper, and chart. Droplet Transmission Infection: is passed when the pathogen travels in water droplets expelled as an infected person exhales; coughs, sneezes, or talks. Airborne Transmission: Microorganisms that float considerable distances on air currents can pass infection to vulnerable hosts. Airborne pathogens can travel through heating and air- conditioning systems to infect large numbers of people. Sweeping a floor or shaking out contaminated bed linens can stir up airborne microorganisms and launch them on air currents. Vector Transmission: This is an organism that carries a pathogen to a susceptible host, typically by biting or stinging, creating another portal of entry into the body. The mosquito is a common vector for diseases. Halo Traction: The patient may be placed in fixed skeletal traction to realign the vertebrae, facilitate bone healing, and prevent further injury, often after surgical stabilization. The most commonly used device for immobilization of the cervical spine is the halofixator device, which is worn for 8 to 12 weeks. This static device is affixed by four pins (or screw) into the outer aspect of the skull. For patients not having surgery, the addition of traction helps reduce the fracture. Halo traction and problems with infection. What are priority steps? Follow hospital policy for pin site care which may specify use of solutions such as saline, and Vaseline dressings. Monitor vital signs for indications of possible infection, fever, purulent drainage from pin site. Send cultures prior to the start of an antibiotic. Buck’s Traction: The two most common types of traction are skin and skeletal traction. Skin traction involves the use of a Velcro boot (Buck’s Traction), belt, or halter, which is usually secured around the affected leg. The primary purpose of skin traction is to decrease painful muscle spasms that accompany hip and proximal femur fractures. A weight is used as a pulling force, which is limited to 5 to 10 lb (2.3 to 4.5 kg) to prevent injury to the skin. Spinal Column: Lordosis- Is defined as an excessive inward curve of the spine. Closer to lower part of the back. Scoliosis- Is a sideways curvature of the spine. Kyphosis: Is a forward rounding of the back. Closer to the neck. Amputations: Complications of Amputations? • Hematomas, infections, necrosis, contractures, stump pain, phantom sensation, stump edema, bone overgrowth, causalgia, etc. Amputation Pain? • Possibility of Phantom Pain. Vital Signs indicating Post-Surgical Pain? Elevated Heart Rate Elevated Blood Pressure Elevated Respiratory Rate (Breathing) What are Complications of Hip Surgery? Blood clots, infection. Normal Vital Signs: • Blood Pressure: 90/60 mm Hg to 120/80 mm Hg. (anything higher is abnormal) • Breathing (Respiratory Rate): 12 to 20 Breaths per minute. • Pulse: 60 to 100 BPM • Pulse (Oximetry): “Saturation” 94 to 100% • Temperature: 96.4 F to 99.5 F, Average 98.6 F (Depending on site) Normal Temperatures for All Ages: Infant 97.7- 99.5 Adults 96.4 to 99.5 Elderly 96.8 average (due to loss of subcutaneous fat) Normal PH IS 7.35-7.45 Below is acidosis. Above is alkalosis. Measures in Taking Oral Temperature: Oral Temp: Don’t eat or drink 30 mins before taking temperature, do not use glass thermometer, safe for everyone, Bradypnea may cause false high temps. Temporal Temp: Most accurate. Rectal Temp: Accurately represents “core” temperature, not recommended as first choice. Axillary Temp: Not core temperature, doesn’t accurately diagnosis fever. Methicillin-Resistant Staphylococcus aureus (MRSA): Staphylococcus aureus lives on the skin and in the nose, usually without causing problems. If a person does have a “staph” infection it is normally treated with methicillin, but methicillin-resistant S. aureus (MRSA) can’t be killed by this drug. More than a million hospitalized patients acquire MRSA infection each year in the United States; it can be fatal. The organism is spread by skin-to-skin contact, and by living in crowded conditions. Control of MRSA has become a national priority. PPE for MRSA: Healthcare institutions are targeting MRSA with staff education, aggressive handwashing and use of alcohol- based hand rubs for 20 to 30 seconds for hand hygiene before touching a patient, increased use of protective gloves and gowns, and targeted screening. Be Able To Explain the Meaning of “Highly Virulent” • Virulence: power of the agent to cause a disease Interventions In Reducing Infection: Proper dental care. Maintaining clean & intact skin. Proper hand hygiene. Not leaving catheters in long term. Understanding who is at risk. Using proper standard and contact precautions. Reduce caffeine and stop smoking. Sterile Techniques in Nursing Care: Healthcare providers use sterile technique to perform a variety of procedures. Some of the procedures require full surgical attire; others do not. The following procedures, for example, use both sterile technique and principles of medical asepsis: administering an injection, starting an IV line, and performing a sterile dressing change. Administering an injection: you prepare the patient, cleanse the injection site, and remove the needle cap using standard precautions. You do not don sterile gloves, but for the rest of the procedure you observe sterile technique by taking care not to touch or otherwise contaminate the exposed needle. Before performing a sterile procedure, determine what supplies you will need and whether you will need assistance. If the patient is unable to maintain a position required for the procedure, you will need a helper to hold the patient during the procedure. • Wash your hands before gathering materials from the sterile supply area • gather the other required supplies and equipment. • Check the expiration date on each package. • Check the package to make sure it is intact. If it has paper or cloth wrapping, be sure there are no indications that it has ever been wet. WHAT ARE THE BODY’S DEFENSE AGAINST INFECTION? The human body has three “lines of defense” against infectious disease: Primary Defenses— The “soldiers” in the first line of defense are the structural barriers of the human body. These primary defenses prevent organisms from entering the body. The normal flora of the body provides one such defense. Ex: Skin, eyes, mouth, respiratory tree. Secondary Defenses— Protective biochemical processes fight pathogens that do enter. Pathogens that dodge the primary defenses and gain entry into the body begin to release wastes and secretions and to cause the breakdown of cells and tissues. The presence of such chemicals activates a set of secondary defenses. Ex: Inflammation, fever. Tertiary Defenses— The presence of pathogens activates immune responses against specific, recognized invaders. Immunity against an infection is achieved through the presence of antibodies that neutralize or destroy toxins or disease-producing organisms. Active Immunity: occurs when the body makes its own antibodies or T cells to protect the body against a pathogen. Ex: Immunization. Passive Immunity: Can also be achieved when a person is given antibodies to a pathogen rather than producing them through her own immune system. Ex: Breastfeeding. Key Point: Remember that T cells mature in the Thymus; and B cells mature in Bone marrow. Lupus Erythematosus: Lupus is thought to be an autoimmune process. Immune complexes form in the serum and organ tissues, which cause inflammation, damage, and destruction. These complexes invade organs directly or cause vasculitis (vessel inflammation), which deprives the organs of arterial blood and oxygen. The two main classifications of lupus are: Discoid Lupus Erythematosus (DLE): A small percentage of patients with lupus have the DLE type, which affects only the skin. is a chronic skin condition of sores with inflammation and scarring favoring the face, ears, and scalp and at times on other body areas. These lesions develop as a red, inflamed patch with a scaling and crusty appearance. Systemic Lupus Erythematosus (SLE): is a chronic, progressive, inflammatory connective tissue disorder that can cause major body organs and systems to fail. Like RA, it is characterized by spontaneous remissions and exacerbations (“flare-ups”), and the onset may be acute or insidious (slow). is an autoimmune disease. In this disease, the immune system of the body mistakenly attacks healthy tissue. It can affect the skin, joints, kidneys, brain, and other organs. “Immune system attacks its own tissues”. The major skin manifestation of DLE and SLE is a dry, scaly, raised rash on the face (“butterfly” rash) Systemic Sclerosis: Systemic sclerosis (SSc), also called scleroderma, is another chronic, inflammatory, autoimmune connective tissue disease, Chronic hardening and tightening of the skin and connective tissues. The onset of the disease is usually between 25 and 55 years of age, with most women getting it in their 40s. Scleroderma means hardening of the skin, which is only one sign of the problem. Some patients, often children, have only skin involvement, or localized scleroderma (also called linear scleroderma). However, adults usually have skin and other body system involvement. ^Late-stage skin changes seen in patients^ Education for a Client Who Has Scleroderma Receiving an Organ Transplant Should Take What Precautions? • Teach patients that the drug increases their risk for serious infections. • Teach them not to receive live vaccines for 30 days before treatment. • Do not receive live flowers, do not visit ill people, wear a mask when visiting others. What is Crest Syndrome? • • Calcinosis (calcium deposits) • • Raynaud's phenomenon (first symptom that occurs) • • Esophageal dysmotility • • Sclerodactyly (scleroderma of the digits) • • Telangiectasia (spider-like hemangiomas) Explain the Typical Assessment Findings of Systemic Sclerosis/Lupus? Physical Assessment: • Alopecia • Mouth ulcers • Polyarthritis • Hardened skin- scleroderma Signs and Symptoms: • Inflamed red rash across the nose (butterfly rash) • Nephritis • Pericarditis • Raynaud’s phenomenon • Pleural effusions • Pneumonia • Abdominal pain • Join inflammation • Fever • Fatigue • Anorexia • Weight loss • Generalized weakness Lab Assessment: • Same as for RA • Other test • Anti-SS-a • Anti-SS-b • Anti-smith • Anti-DNA and extractable nuclear antigens • CBC Psychosocial Assessment: • Altered body image • Decreased activity-social isolation • Assess support system Caring for A Patient With Dementia, Specific Nursing Interventions Would You Use? • Promote patient orientation, use simple communication, decrease anxiety, keep the patient safe, and provide continuity of care. As for assistance with procedures such as indwelling catheters or IV insertions. Interventions For A Patient With Deep Vein Thrombosis (DVT)? • Patient education • Leg exercises • Early ambulation • Adequate hydration • Graduated compression stockings • Intermittent pneumatic compression, such as sequential compression devices (SCDs) • Venous plexus foot pump • Anticoagulant therapy What Types of Clients Are at Greatest Risk for A DVT? • Decreased mobility or immobility • Older adults (40 years or older) • Family history or history of DVT, VTE, PE varicose veins, or edema • Oral contraceptives use • Smoking • Decreased cardiac output • Hip fracture or total hip or total knee surgery • Obesity • Cancer • Spinal cord injury • Heart disease What Exercises Can Improve Mobility? Range of Motion (Passive & Active) Weight baring exercise. Describe Different Types of Passive Range 0f Motion Exercises. (flexion, extension, abduction, adduction, circumduction, internal/external rotation, opposition). What Are The Negative Effects of Immobility? Osteoarthritis, Rheumatoid Arthritis, Loss of muscle strength, Impaired balance, altered join mobility, decreased stability, Osteoporosis, Depression, isolation, anxiety, and mood change, can cause decreased peristalsis, DVT. What Are The Effects of Immobility On The Respiratory System? Pulmonary embolisms, pneumonia. Decreased depth of respirations, decreased ability to cough, atelectasis. Interventions to Reduce the risk of Contractures: • Gently straighten out contracted extremity, fingers. • Mobility: Encouraging interventions such as passive ROM, and rotation. Flexion and extension exercises, these interventions should be performed about every 2hrs and as needed if the contractures are present. Education of a Client Using a Walker From a Lying/Sitting Position? • Feet firmly on the floor, one hand on the chair the other on the walker. Stand up slowly. How Does a Nurse Perform a Neurovascular Assessment? If Negative Findings Occur, What Should the Nurse Do Next? Assessment of the extremities to evaluate sensory & motor function (neuro) & peripheral circulation (vascular). Components: (bilateral comparison) pulses, capillary refill, skin color, temperature, sensation, & motor function (movement). Pain & edema are also assessed. (5 P’s: Pain, Pulse, Pallor, Paresthesia, & Paralysis) A doppler is used to determine blood flow. Negative Findings: • Assess BAC & provide as needed. • Expose the area of injury to assure accurate assessment. • Control any bleeding. Apply direct pressure to bleeding site or pressure artery above the fracture. • To prevent shock, position patient in a supine position. • Splint the injury. • Manage pain with an opioid medication. What Is the Normal Aging Process for Bones? It undergoes a continuous process of formation & resorption, or destruction, at equal rates until the age of 35 years. In later years, bone resorption increases, decreasing bone mass & predisposing patients to injury, especially older women. Osteopenia, less synovial joint cartilage, muscle atrophy. Appropriate Interventions for A Patient with A Cast (Negative) Assessment: • Teach patient and family to smell area for mustiness/unpleasant odor. • teach to never put anything inside cast (hanger, pencil). • Teach patient to assess for circulation at least daily, including the ability to move the area distal to the extremity, note numbness, increased pain. What Is Compartment Syndrome? • Limb threatening complication caused by severe neurovascular impairment manifested by increasing alterations in levels of comfort (pain even after analgesics are given) and paresthesia (painful tingling and numbness). Articulate Typical Assessment Findings for A Client with an Infection? • Observe the patient’s general appearance: • Does he seem fatigued? Is he diaphoretic? Is he wrapped in blankets or complaining of feeling chilled? Does the patient appear well nourished? Are the mucous membranes dry? Does the skin have normal elasticity (turgor)? Physical assessment includes a thorough examination of the skin. Look for signs of local infection evidenced by pain, redness, swelling, and warmth. Note the presence or absence of any rashes, along with any breaks or reddened areas of the skin. Patients with poor peripheral circulation often have various skin discolorations, rather than signs of inflammation, when experiencing an infection. Swollen lymph nodes indicate the possible presence of an infection in the area that drains into the nodes. Elevated temperature and pulse rate are classic signs of an infection. Appropriate Nursing Interventions for a Client With A Lowered Immunity: • Reduce exposure to pathogens through the use of aseptic technique. • Maintain skin integrity and support natural defenses against infection. • Reduce stress. • Promote immune function through collaborative care. • Provide supportive measures to decrease the length of time that invasive devices, such as intravenous lines and urinary catheters, are needed by a patient. • For clients who have had surgery and general anesthesia or who are at risk for pneumonia, promote coughing and deep breathing on a regular basis. • For clients being mechanically ventilated, provide special oral care designed to prevent ventilator-associated pneumonia. • For older adults, especially those who or frail or in a debilitated state and those living in a group residence, encourage immunizations that can help them to acquire immunity from some communicable diseases, such as influenza. • For clients who have breaks in the skin or incision sites, provide regular assessment for infection status and follow appropriate medical or surgical asepsis guidelines. • For all clients at risk for infection, provide care that is based on principles of medical asepsis. Explain the Differences Between Acquired, Adaptive, Innate, and Specific Immunity: • Acquired- Antibody-mediated immunity, acquired by infection (active) or by the transfer of antibody or lymphocytes from an immune donor (passive). • Adaptive- A person's body learns to make as an adaptive response to invasion by organisms or foreign proteins, occurs either naturally or artificially through lymphocyte responses and can be either active or passive. • Innate- Nonspecific defense mechanisms that come into play immediately or within hours of an antigen's appearance in the body, already present in the body. • Specific- Acquired during the organism's lifetime and involves the activation of white blood cells (B and T lymphocytes), which distinguish and react to foreign substances. B lymphocytes (or B cells) operate by producing antibodies, proteins that neutralize foreign molecules. Proper Education for Reducing The Spread of Chicken Pox? • Private room required with monitored negative airflow (with appropriate number of air exchanges and air discharge to outside or through HEPA filter); keep door(s) closed. Special Respiratory Protection: • Wear PAPR for known or suspected TB. • Susceptible people not to enter room of patient with known or suspected measles or varicella unless immune caregivers are not available. • Susceptible people who must enter room must wear PAPR or N95 HEPA filter*. • Transport: patient to leave room only for essential clinical reasons, wearing surgical mask. • Wiping any objects or surfaces with a sterilizing solution and making sure that any infected clothing or bedding is washed regularly. • Vaccination. Nursing Interventions for a Client with Fibromyalgia: • Recognize that patients with fibromyalgia syndrome (FMS) are often frustrated because they have not been diagnosed or have been misdiagnosed. Therefore, inform them about the National Fibromyalgia Association for additional information and patient and family support. • Teach the patient that these drugs can cause drowsiness and sleepiness and that alcohol should be avoided while taking them. • Promote comfort with help of NSAID and physical therapy • Encourage at home low impact exercise such as walking, swimming, rowing, biking, and water exercise. Help establish regular sleep patterns. Nursing Process: • Assessment/Data Collection: Information collection/gathering data about patient condition. • Analysis/ Data Collection (Diagnosis): Identify the patient problems, interpreting information. • Planning: Set goals of care and patients desired outcome, identify appropriate nursing actions. • Implementation: Perform the nursing actions identified in nursing planning. • Evaluation: Determine if goals and expected outcomes are achieved. Delegation to an Unlicensed Assistive Personnel (UAP): o Anytime there is concern over a finding from an unlicensed person assess the patient yourself to confirm the concern. o Things that can be delegated to unlicensed personnel: Vital signs on a non-critical patient. Moving/ambulating a patient. Bedside glucose monitoring. Bathing and documenting tasks. Provide instructions about high calorie, protein diet. Priorities: (Think of Maslow’s Hierarchy) How Can a Nurse Best Meet Psychosocial Needs for a Client? • involve clients in daily care. • Provide stimuli such as newspapers, TV, magazines. • Assist with grooming and hygiene such as shaving and makeup. • Involve the client in planning of daily routine. • Maintain orientation to time such as a clock, and calendar. Main Causes of Accidental Poisoning: • Young Children exposure is mainly due to improper storage of household chemicals, medicines, vitamins & cosmetics. • Older children and adolescents cause is due to suicide attempt, accidental experiment with recreational or prescription drugs. • Adults poisoning occurs by misuse or abuse or prescription drugs, especially narcotics, tranquilizers and antidepressants. Main Purpose of Incident Report: To give the health care facility and the healthcare professionals the opportunity to address the issue and prevent the occurrence of future incidents. a) Infant Safety- Education for new moms in keeping babies safe. • Don’t Sleep with baby. • Car seat faces backwards for 2 years. • Baby should sleep on their back. • Do not use microwave to heat formula or breast milk. Client Orientation to a New Room, May Include What Specifics? • Ensure they can use call light before you leave. • Show them where their personal items are and place them near to them. • Show them where all the furniture is at and walk them around it. • Also show them where the bathroom is and how to get to it. Non-Compliant Clients- What Are Best The Best Responses By The Nurse? • Find out the reason why. Provide education. Document. Extras: -Inflammation is a non-specific reaction. -Infection is when a pathogen is involved. -Wound contamination -> Colonization -> Infection. -Infection is the main cause of impaired healing. -All skin layers have to be intact, any disruption in skin integrity leads to the formation of a wound. -Pressure creates ischemia which results in impaired circulation and breaks in the skin barrier. What is Osteopenia? Osteopenia is considered a midway point to osteoporosis; the bone density is lower than normal but not as severe and treating it may slow the progression bone loss that leads to osteoporosis. Bone mineral density (BMD) measures the level of calcium in the bones. -A condition that occurs when the body doesn't make new bone as quickly as it reabsorbs old bone. [Show More]
Last updated: 1 year ago
Preview 1 out of 118 pages
Instant download
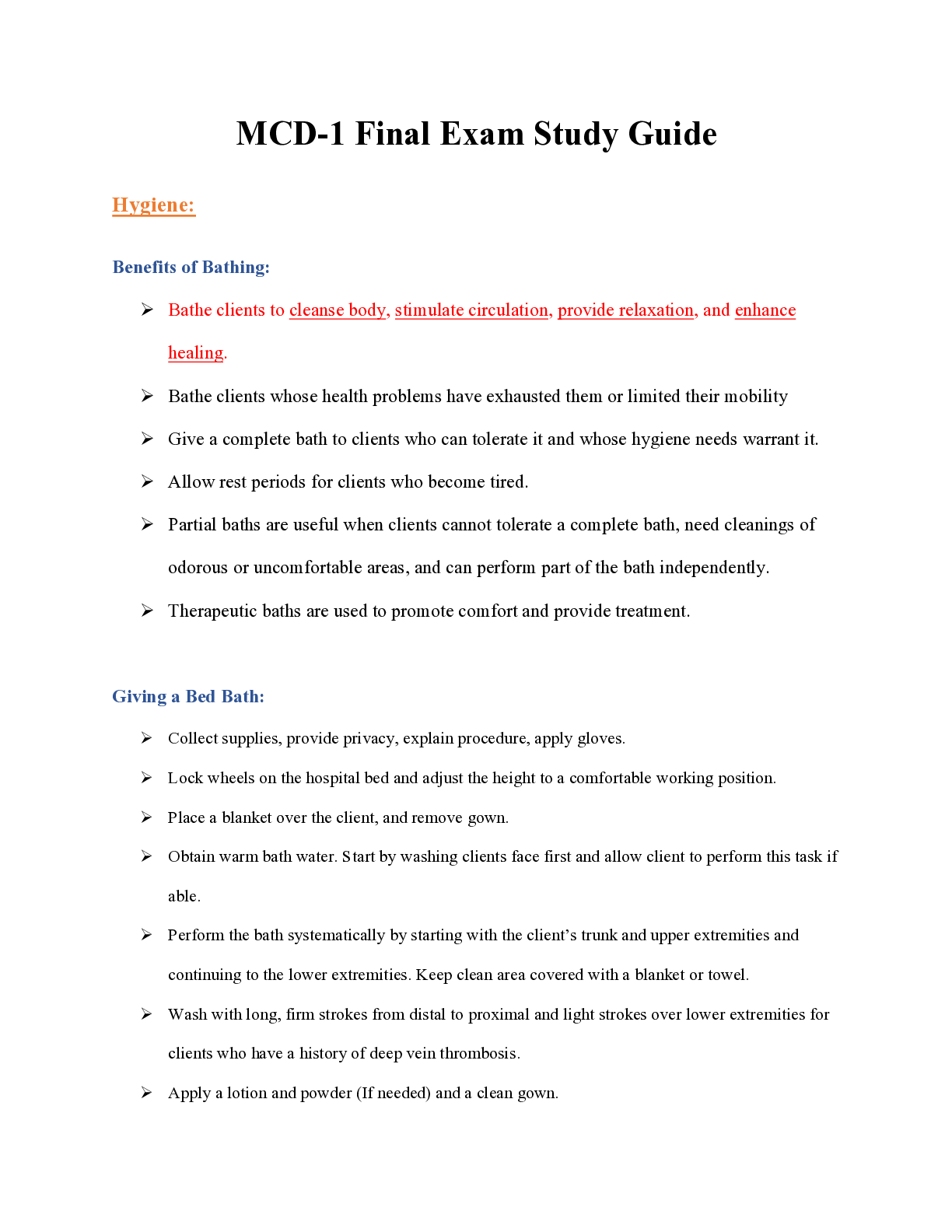
Buy this document to get the full access instantly
Instant Download Access after purchase
Add to cartInstant download
Reviews( 0 )
Document information
Connected school, study & course
About the document
Uploaded On
Feb 16, 2022
Number of pages
118
Written in
Additional information
This document has been written for:
Uploaded
Feb 16, 2022
Downloads
0
Views
41

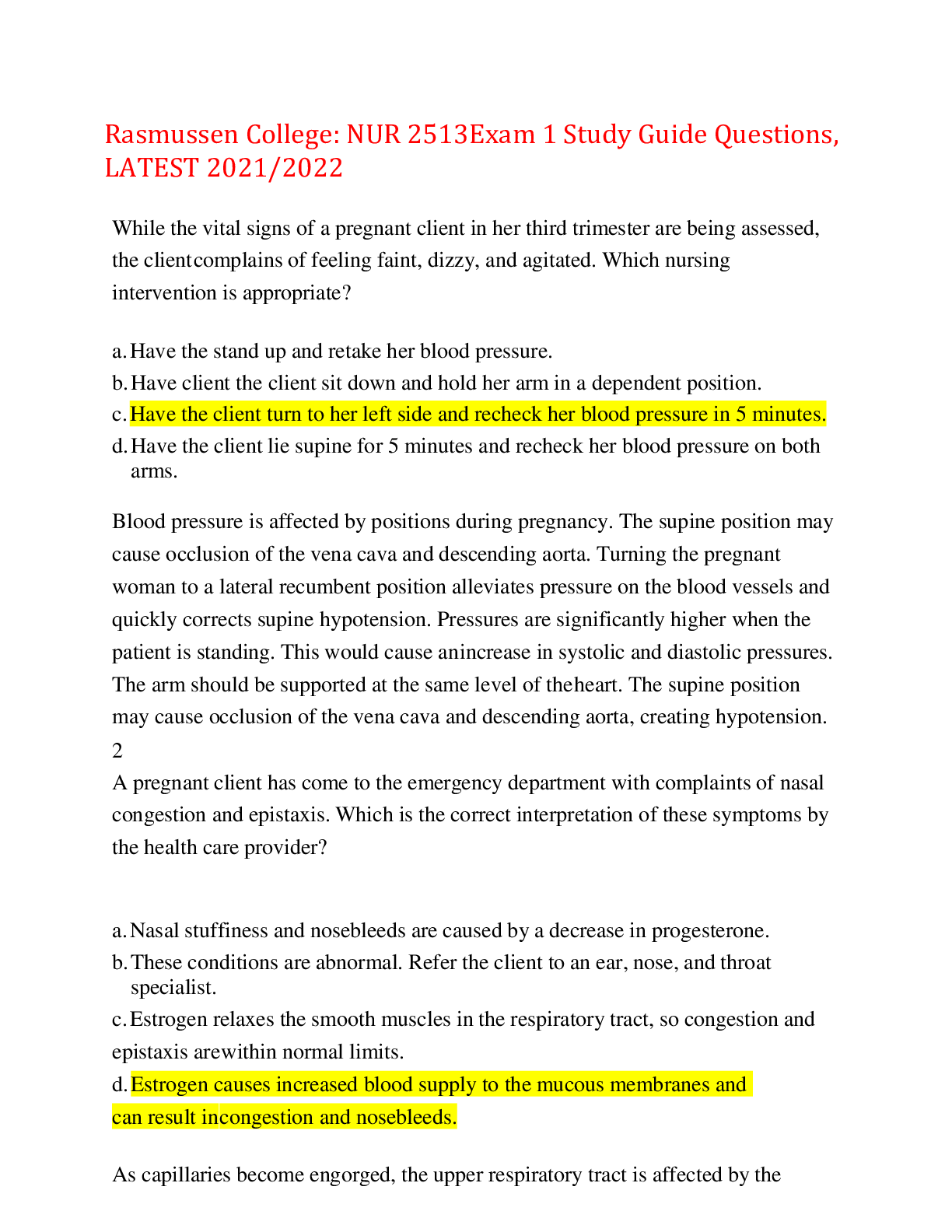
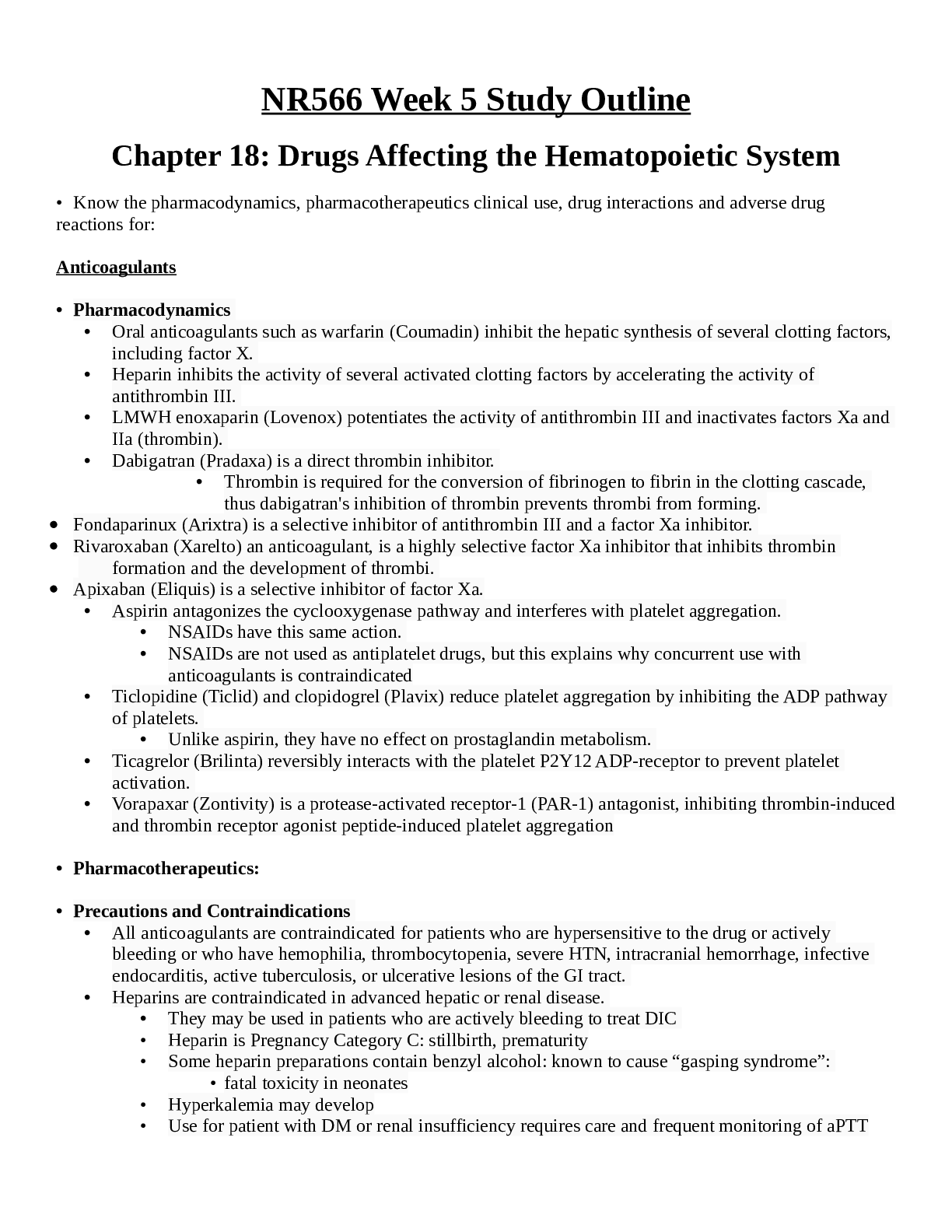
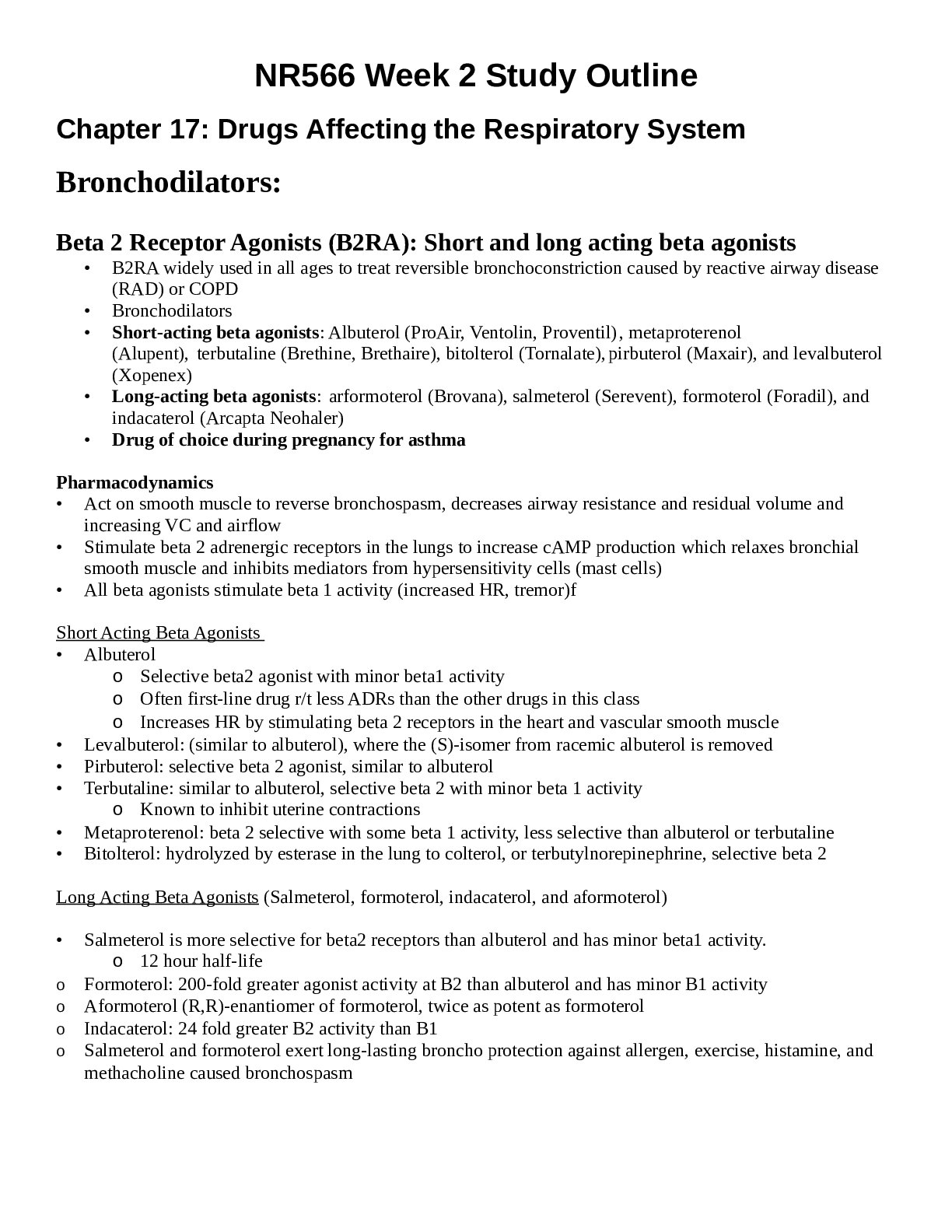
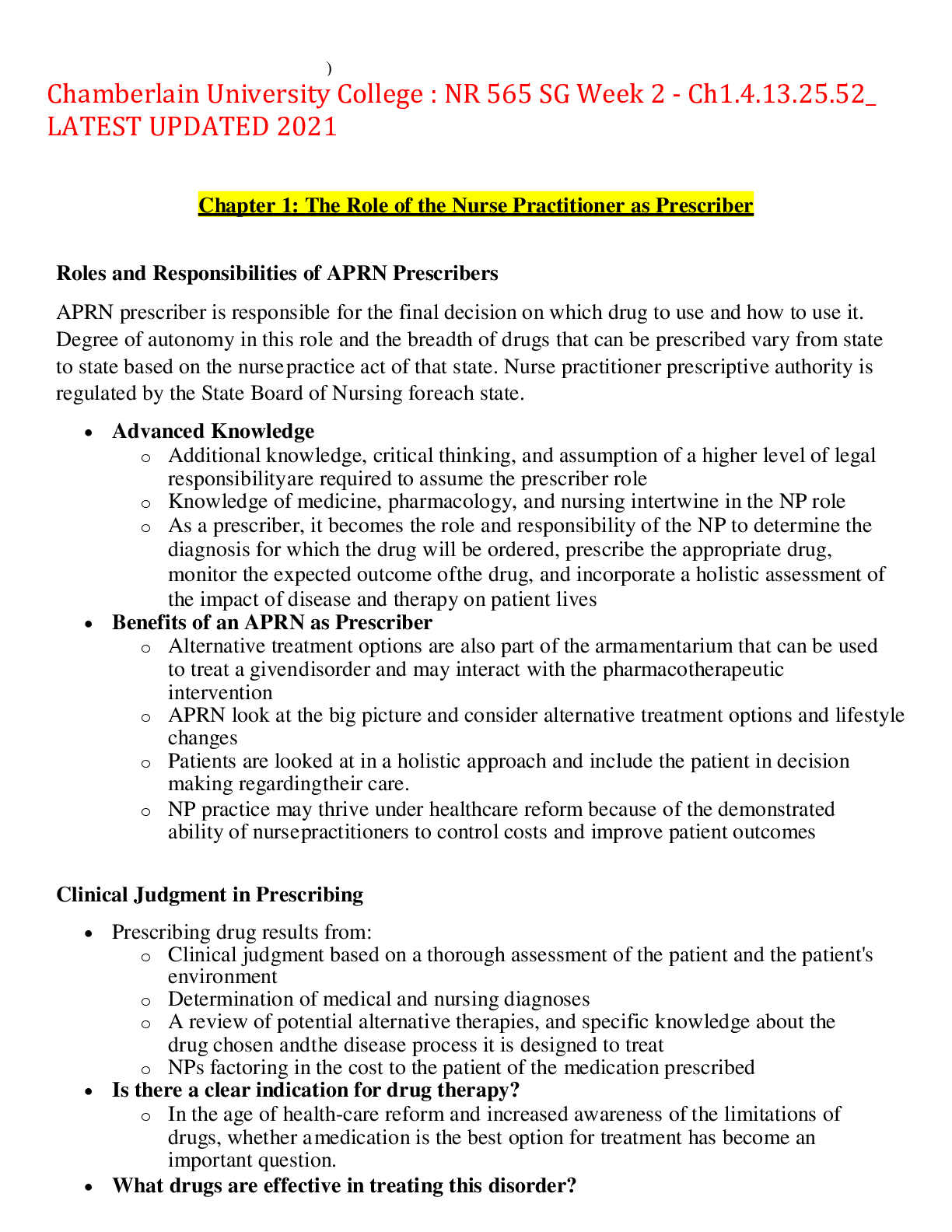
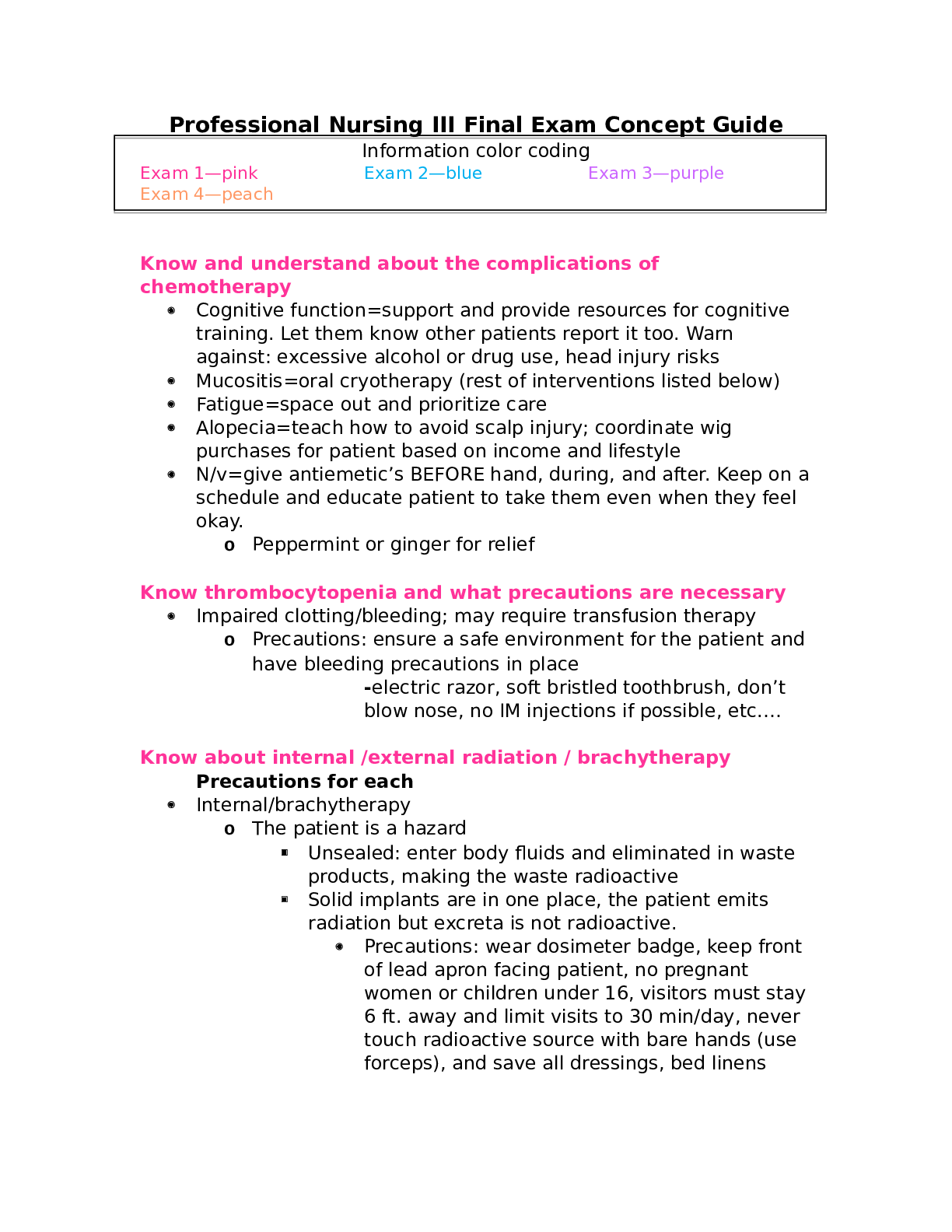
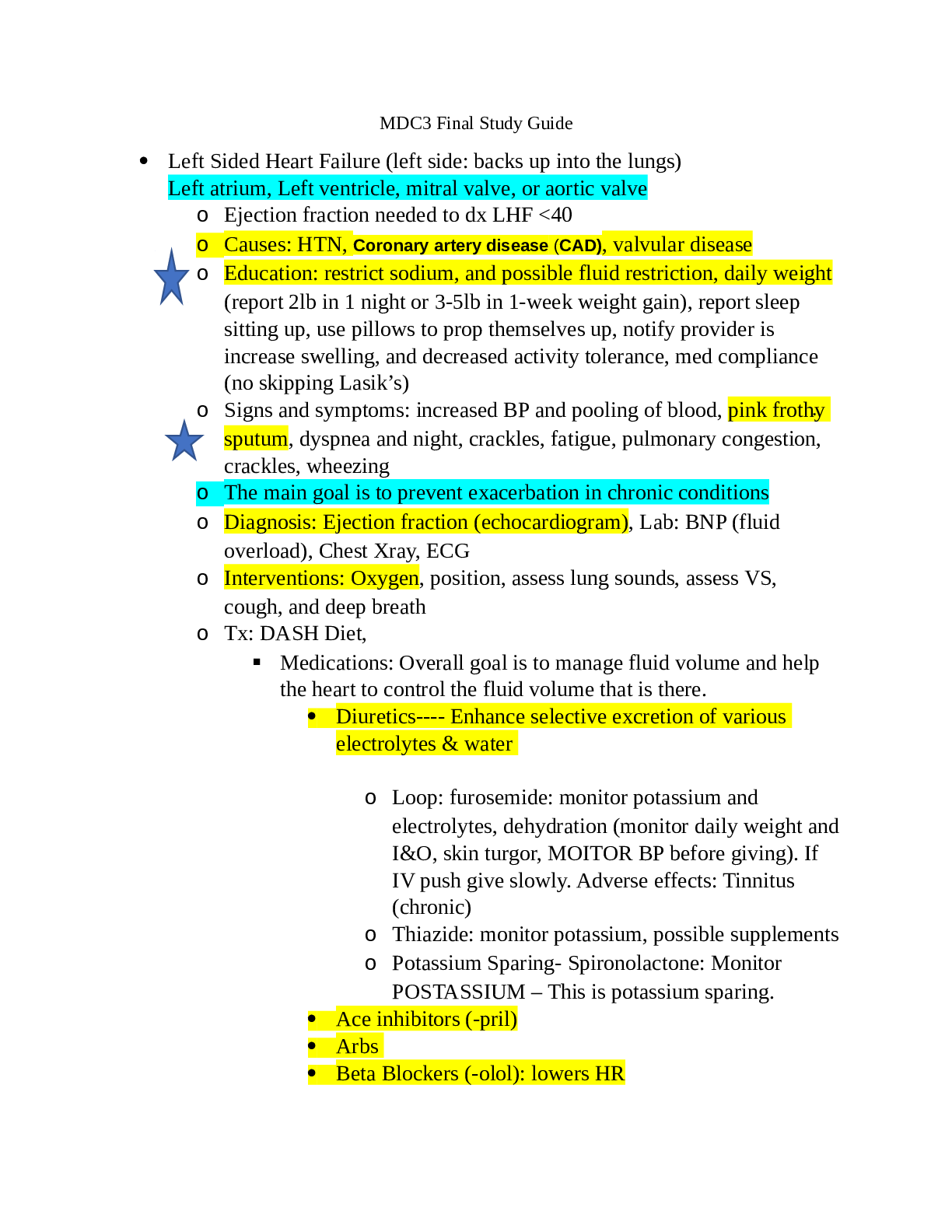
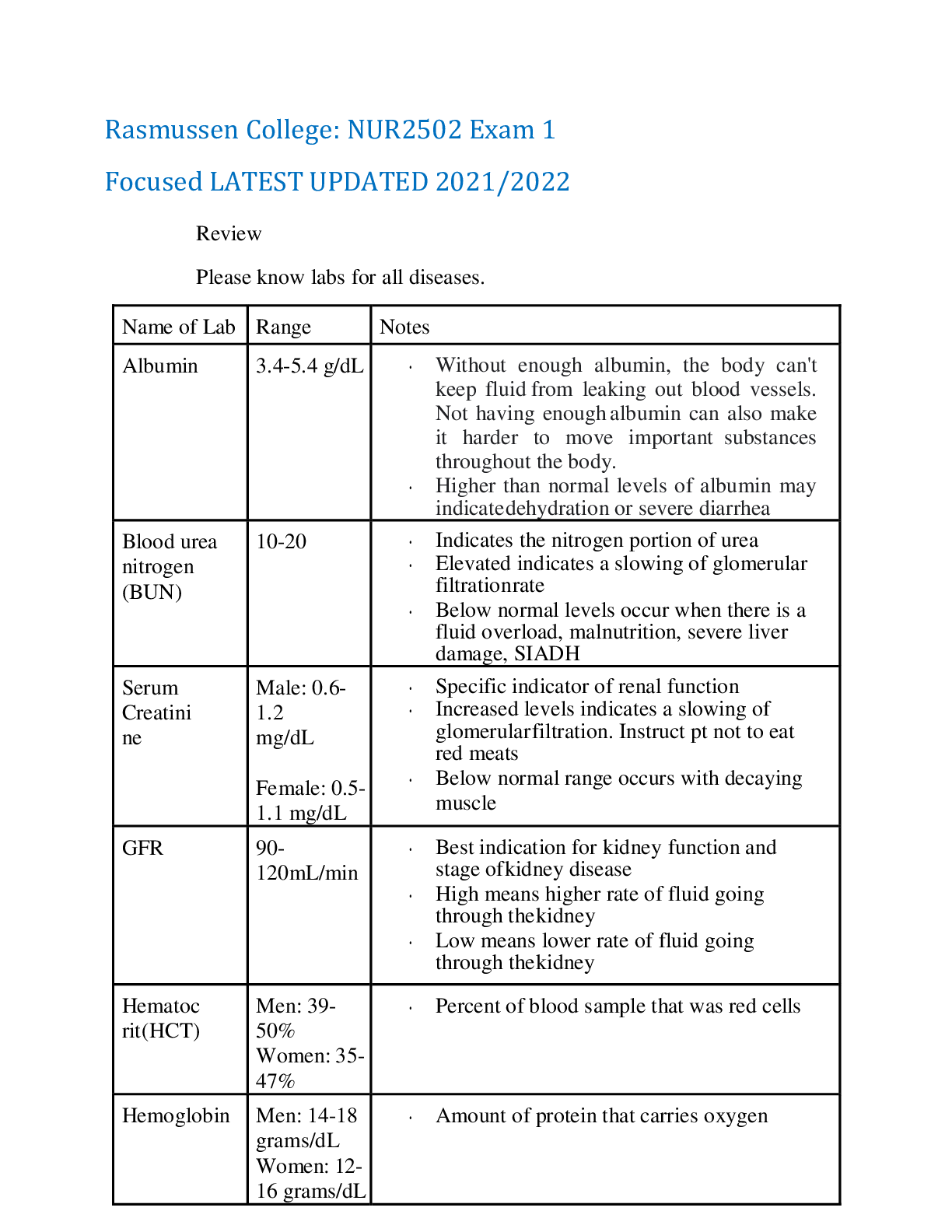
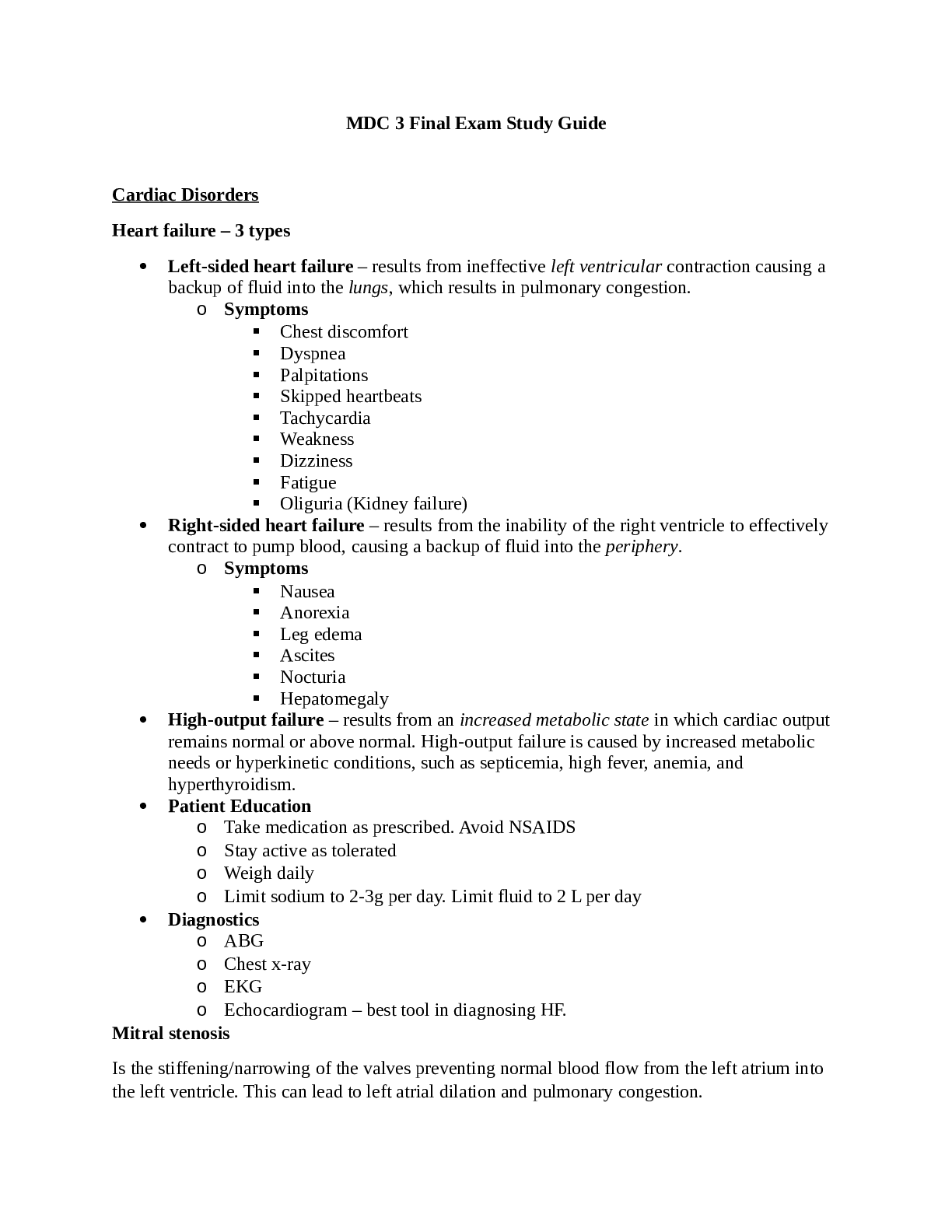
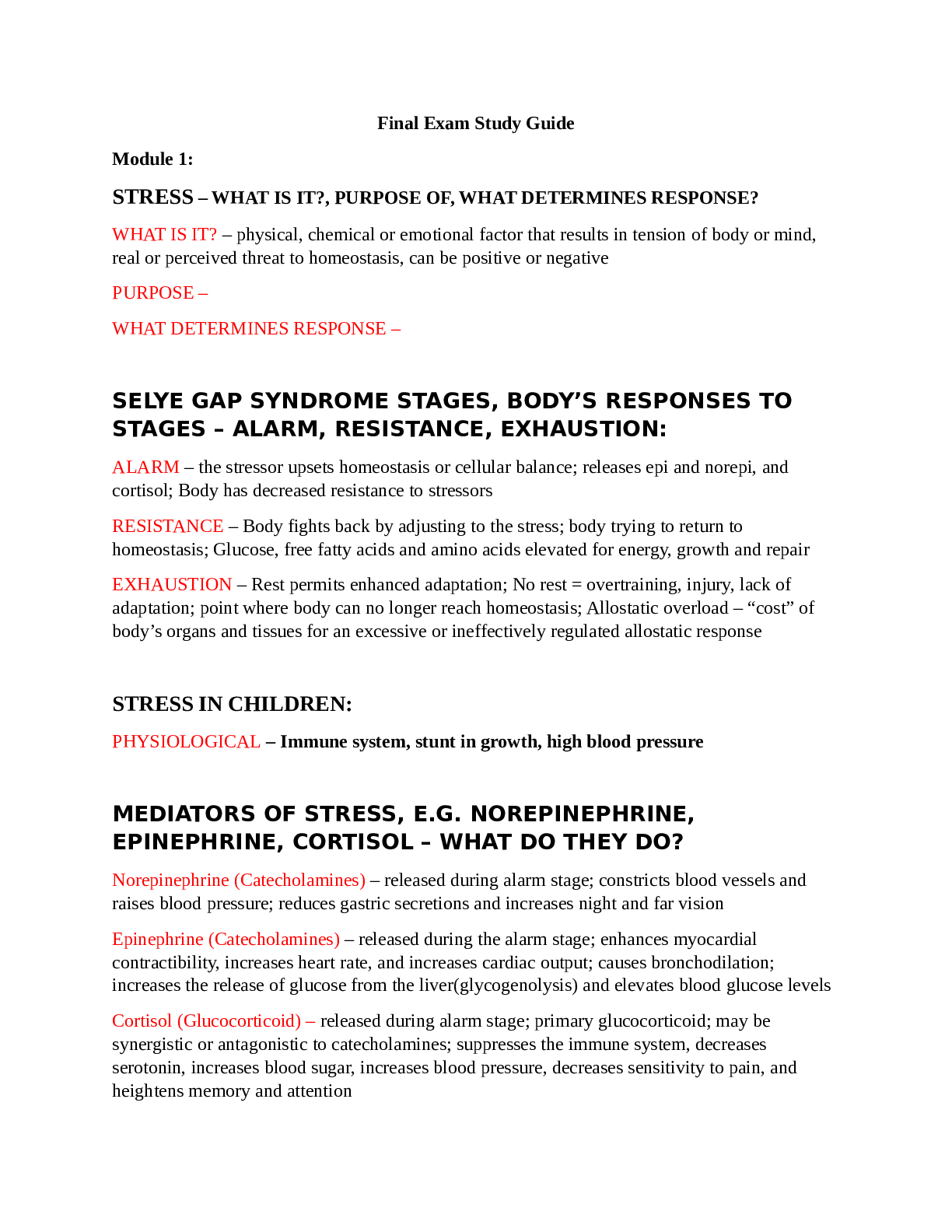
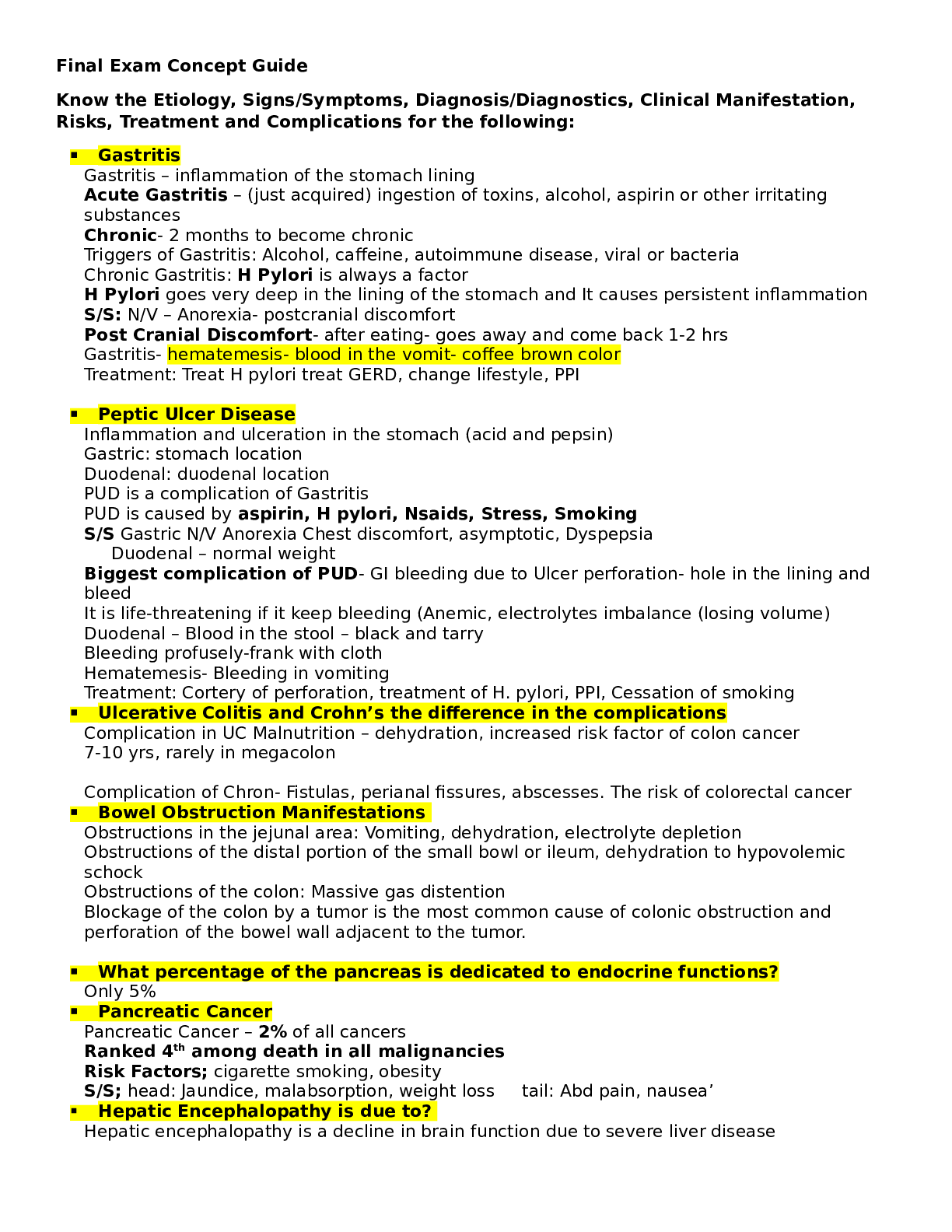



.png)