*NURSING > EXAM REVIEW > Rasmussen College : NUR 2488 Mental Health Final Exam Review Latest Updated 2021,100% CORRECT (All)
Rasmussen College : NUR 2488 Mental Health Final Exam Review Latest Updated 2021,100% CORRECT
Document Content and Description Below
Rasmussen College : NUR 2488 Mental Health Final Exam Review Latest Updated 2021 NUR 2488 Mental Health Nursing Final Exam Key Concepts • Introduction in Psychiatric Nursing • Basic ... Brain Anatomy- what do the different part of brain control? o Frontal Lobe: Thought Processes & Voluntary Movement (decision making) o Temporal Lobe: Auditory Processes (language, speech, connects to Limbic system) o Occipital Lobe: Vision (interprets visual images) o Parietal Lobe: Sensory & Motor (L/R orientation, reading, math, proprioception) o Hypothalamus: maintains homeostasis, regulates BP, Temp, libido, hunger, thirst, and sleep/wake cycles. o Cerebellum: Balance, Skeletal Muscle Coordination o Neurons: Nerves that translate electrical impulses into chemical signals released at the synapse ▪ Synapse- (pg. 51)- The space between neurons in which neurotransmitters are released and either inhibit/excite the adjacent neuron. The 4 NT’s are dopamine, norepinephrine, serotonin and acetylcholine. • Milieu Therapy: Creating a SAFE, structured inpatient/outpatient setting where the mentally ill can test new behaviors and coping mechanisms with others. o Creating a SAFE, structured inpatient/outpatient setting where patients with mental illness can test new behaviors and interactions. o Climate is essential to healing: paint color, relaxed environments are conducive to the healing process. o Florence Nightingale believed that the environment helps heal • Maslow’s Hierarchy of needs o Basic Needs: food, oxygen, water, sleep, sex, and a constant body temperature. If all the needs were deprived, this level would take priority. o Safety Needs: Security, protection, freedom from fear/anxiety/chaos, and the need for law, order, and limits. o Belonging and Love Needs: intimate relationship, love, affection, and belonging, having a family and a home and being part of identifiable groups. o Esteem Needs: If self-esteem needs are met, we feel confident, valued, and valuable. When self-esteem is compromised, we feel inferior, worthless, and helpless. o Self-actualization: Reaching our full potential to feel inner peace and fulfillment. • Peplau’s Theory of Interpersonal Relations o Created the Nurse-Patient Partnership increasing individual and family roles in recovery. (Based off of Sullivan’s Interpersonal Theory). Relationships greatly influence recovery • Freud- what did he contribute to psychiatric setting? (Unconscious thoughts) o Id – unconscious mind, instincts (this is dominant) o Ego – sense of self, use of defense mechanisms o Superego – our conscious and is greatly influenced by our parents morals and ethical stances o Erickson’s ▪ Trust vs. Mistrust (infant 0- 1 ½) trust developed if caregivers give affection, love, care, attention, and reliability. (Feeding) ▪ Autonomy vs. Shame (toddlers 1 ½ - 3) kids need to develop a sense of personal control. (Toilet Training) ▪ Initiative vs. Guilt (children 3-6) children need to have power to explore their environment and not receive disapproval from parents. (Exploration) ▪ Industry vs. Inferiority: (school aged kids 6-12) Kids dealing with new social and academic demands. Success leads to a sense of competence. (School) ▪ Identity vs. Role Confusion (teens 12-20) Teens need to develop self-identity and personal identity to stay true to themselves. (Social Relationships) ▪ Intimacy & Solidarity vs. Isolation (young adults 20- 30) Young Adults need to form intimate, loving relationships. (Relationships) ▪ Generativity vs. Self-Absorption: (adults 30-65) Need to create/nurture things by having children. (Work & Parenthood) ▪ Integrity vs. Despair (elderly 65+) Need to look back and feel fulfilled by accomplishments; have wisdom and no regrets (Reflection on Life) o Sullivan ▪ Personalities are influenced during childhood and mostly by the MOTHER. (Page 31 in book for more information) • Therapeutic Communication • Therapeutic Communication: goal directed, professional, scientifically based. Goal is to get information so that you can plan care for the patient. o Active Listening ▪ Clarifying: promotes understanding of the patient’s statement ▪ Restating: repeating the same key words the patient has just spoken to echo their feelings. (Ex: If a patient remarks, “My life is empty…it has no meaning,” additional information may be gained by restating, “Your life has no meaning?”) ▪ Reflecting: helps people understand their own thoughts better; summarizes (Ex: For example, to reflect a patient's feelings about his or her life, a good beginning might be, “You sound as if you have had many disappointments.”) ▪ Exploring: use of open-ended questions or statements to allow the patient to express thoughts/feelings. (Ex: “Tell me more…”, “Give me an example of…”) • Communication Technique Examples in Different Scenarios o For Suicidal Patients: “These thoughts are very serious Mr. Adams. I do not want any harm to come to you. Can you tell me what you were feeling and if there were any circumstances that led you to this decision?” o For Patients who start Crying: Stay with your patient and reinforce that it is all right to cry & offer tissues. “You seem upset, what are you thinking right now?” o For Patients who say they “don’t want to talk”: “Its alright. I would like to spend time with you. We don’t have to talk.” Or reapproach at a later time, “Our 5 minutes is up. I will be back at 10am and spend another 5 minutes with you.” o For Patients who ask the nurse to keep a secret: Nurses cannot make such promises, as it may be important to share that information with other staff for safety reasons. “I cannot make that promise Mr. Adams as it might be important for me to share it with the other staff”. o Non-Verbal: ▪ Tone of voice (tone, pitch, intensity, stuttering, silence, pausing) ▪ Facial expressions (frown, smile, grimaces, raises eyebrows, licks lips) ▪ Posture (slumps over, puts face in hands, taps feet, fidgets with fingers) ▪ Amount of eye contact (angry, suspicious or accusatory looks, wandering) ▪ Sighs ▪ Hand gestures (fidgeting, snapping fingers) ▪ Yawning • Non-Therapeutic Communication: not goal-directed, false reassurances, double messages, giving personal opinions, making assumptions of feelings, asking “Why” questions, showing disapproval, excessive questioning, non-attending behaviors, poor non-verbal communication (eye rolling, staring off into distance, ignoring patient). o Double Bind Messages: intent of the message is to cause confusion o Double Messages: conflicting/mixed messages • Phases of the Nurse-Patient Relationships o Orientation Phase: first time the nurse & patient meet, interact according to their own backgrounds/standards/values/beliefs, roles of the patient and nurse are clarified, confidentiality is discussed and assumed, nurse becomes aware of transferences & countertransference issues, goals are established, termination terms are introduced. o Working Phase: exploration of feelings or situations that are causing the problems, re-experiencing of old conflicts can awaken high levels of anxiety, intense emotional states may surface, defense mechanisms, denying, manipulation, evaluation of problems and goals, promote alternative reactions/behaviors to situations, etc. The nurse’s awareness of his or her own personal feelings and reactions to the patient are VITAL for effective interaction with the patient. o Termination Phase: summarization of goals, review of what was achieved during communication, discussing new ways to implement new coping strategies, evokes strong feelings in both client & nurse. • Legal, Ethical, and Cultural o Negligence –or malpractice is an act or an omission to act that breaches the duty of due care and results in or is responsible for a person’s injuries. The five elements required to prove negligence are: (1) duty, (2) breach of duty, (3) cause in fact, (4) proximate cause, and (5) damages. ▪ Example – A nurse know that a patient’s IV is malfunctioning and the wires are frayed, but decides not to act in a timely manner and leaves the IV on the patient and doesn’t tag it for repair, this results in the patient dying. o Beneficence - This relates to the quality of doing good and can be described as charity. ▪ Example - A nurse helps a newly admitted client who has psychosis feel safe in the environment of the mental health facility. o Autonomy - This refers to the client’s right to make her own decisions. But the client must accept the consequences of those decisions. The client must also respect the decisions of others. ▪ Example - Rather than giving advice to a client who has difficulty making decisions, a nurse helps the client explore all alternatives and arrive at a choice. o Justice - This is defined as fair and equal treatment for all. ▪ Example - During a treatment team meeting, a nurse leads a discussion regarding whether or not two clients who broke the same facility rule were treated equally. o Fidelity - This relates to loyalty and faithfulness to the client and to one’s duty. ▪ Example - A client asks a nurse to be present when he talks to his mother for the first time in a year. The nurse remains with the client during this interaction. o Veracity - This refers to being honest when dealing with a client. ▪ Example - A client states, “You and that other staff member were talking about me, weren’t you?” The nurse truthfully replies, “We were discussing ways to help you relate to the other clients in a more positive way.” • Rights for Voluntary and Involuntary Admission o Voluntary Commitment – The client or client’s guardian chooses commitment to a mental health facility in order to obtain treatment. A voluntarily committed client has the right to apply for release at any time. This client is considered competent, and so has the right to refuse medication and treatment. o Involuntary (civil) Commitment – The client enters the mental health facility against her will for an indefinite period of time. The commitment is based on the client’s need for psychiatric treatment, the risk of harm to self or others, or the inability to provide self-care. The need for commitment could be determined by a judge of the court or by another agency. The number of physicians, which is usually two, required to certify that the client’s condition requires commitment varies from state to state. Clients admitted under involuntary commitment are still considered competent and have the right to refuse treatment, unless they have gone through a legal competency hearing and have been judged incompetent. • Informed Consent o The principle of informed consent is based on a person’s right to self- determination, as enunciated in the landmark case of Canterbury v. Spence (1972): True consent to what happens to one’s self is the informed exercise of choice, and that entails an opportunity to evaluate knowledgeably the options available and the risks attendant on each. Proper orders for specific therapies and treatments are required and must be documented in the patient’s chart. Consent for surgery, electroconvulsive treatment, or the use of experimental drugs or procedures must be obtained • Confidentiality/HIPAA o Therefore, you may not, without the patient’s consent, disclose information obtained from the patient or information in the medical record to anyone except those individuals for whom it is necessary for implementation of the patient’s treatment plan. • Psychiatric Nursing Assessment – priority interventions, nursing dx, etc. (pg 101) • Mood Disorders • Primary vs. Secondary Depression o Primary Depression: due to family history, female gender, 40yrs +, post-partum, chronic illness, ETOH abuse, stressful life events. o Secondary Depression: Resultant from another mental health disorder or debilitating chronic illness. Person is depressed BECAUSE of their decline in physical or mental functioning. • Review table 15-2/Nursing Diagnosis for Depression: *Risk for Suicide, Risk for Self-Mutilation, Ineffective Coping, Hopelessness, Powerlessness, Social Isolation, Risk for Loneliness, Situational Low Self-Esteem. • First-line treatment for Depression: o TCA’s are #1 (Amitriptyline, Imipramine, Doxepin). o Next choice is SSRI/SNRI’s (citalopram, fluoxetine, sertraline, bupropion, Buspirone) o Last option is MAROI (phenelzine, isocarboxazid) • Review box 15-2: • • Suicidal Ideation – Assessment, Risk Factors & Interventions (pg 437) o Suicide Risk Factors: presence of a plan, previous suicide attempt, recent loss/life event, TBI/Brain Injury, recent visit to PCP, WHITE MALES. Patient will say/do: “Everything will be okay now”, “Things will never work out”, giving away prized possessions, making a living will, suddenly increase in happy mood/euphoria. o Assessment: ▪ Are you thinking of harming yourself? ▪ Do you have a plan? ▪ Precipitating Event? ▪ History of attempts? Why did they fail? ▪ Any MH dx that puts them at higher risk? o Diagnosis: ▪ RISK FOR SUICIDE (outcome would be “Self Restraint from Suicide”) this is a priority diagnosis! o Interventions: ▪ #1 is suicide precautions ( 1:1 monitoring, keep an arm’s length from pt, no suicide contract) ▪ Make environment safe (remove sharp objects, metal silverware, mirrors, glass, cords, belts) o After Crisis Period: ▪ Have friend stay the night or have pt stay with family ▪ Remove weapons and pills from the house ▪ Encourage the patient to talk openly about their feelings. ▪ Don’t give person more than 1-3 days supply of a medication due to overdose (SSRI’s are least lethal) • Lithium Levels & Toxicity o Therapeutic Range: 0.8-1.4 (fine hand tremors & mild N/V are normal) o Maintenance Range: 0.4 – 1.3 o Toxic Range: 1.5 and over o Toxicity: slurred speech, blurry vision, seizures, coarse tremors, severe N/V, thirst o Patient Teaching: regular salt diet, don’t get dehydrated, stay out of hot climates, avoid excessive exercise, take with food. • Anxiety Disorders • Anxiety Levels & Stages o Mild: Everyday anxiety, better focusing, more alert and in-tune with surroundings (nail biting, fidgeting, foot tapping are common) o Moderate: Narrowed perceptual field, hears/sees/grasps less info. (Pacing, pounding heart, banging hands on table) o Severe: Cannot learn or problem solve. Confusion, hyperventilation, making threats and feeling of “impending doom”. (Stomach aches & physical symptoms are common: dizziness, H/A, insomnia, nausea) o Panic: Extreme Anxiety. Cannot problem solve/learn, Dilated Pupils, shouting, screaming, and hallucinations. Lost touch with reality. • Nursing Interventions for Anxiety o Mild/Moderate: Be calm and listen! Find out what worked before. Clarify, use open-ended questions, have the patient NAME the anxiety/trigger, “what were you thinking right before the attack?”. o Severe/Panic: Firm, Short Answers, Set Limits (you cannot hit me or anyone else), move patient to quiet room, low pitch voice & speak slow, reinforce reality, remain with the patient (don’t leave them alone), Prevent dehydration & exhaustion (high calorie fluids). Gross motor activities to drain some of the tension (ping pong, dancing, etc) • Anxiety/Depression Meds: o Antidepressants - is a substance that prevents/relieves depression. ▪ SSRI’s– (Ex: fluoxetine, citalopram, sertraline). Black Box Warning: increased suicidal thoughts are possible. Takes 2- 4 weeks to work. Helps treat Depression, ETOH withdrawal, OCD, ▪ Side Effects: Anxiety, tremors, sexual dysfunction, H/A, agitation, sleeplessness. Dry mouth. ▪ S/Sx of Overdose: Serotonin Syndrome (fever, Hyper- Reflexia, sweating, high BP, delirium, hostility). Wait 2 weeks before starting an MAOI or vice-versa. ▪ Contraindications: Those who have attempted suicide don’t use! Pregnancy, Renal/Liver issues, Elderly (due to increase of osteoporosis/fractures) ▪ Patient Teaching: OTC drug interactions, slow standing, don’t take w/in 2 weeks of MAOI, monitor for suicidal ideations ▪ Serotonin Syndrome Treatment: • STOP medication. •Serotonin receptor blockade: cyproheptadine, methysergide, propranolol •Cooling blankets, chlorpromazine for hyperthermia •Dantrolene, diazepam for muscle rigidity or rigors •Anticonvulsants •Artificial ventilation • Paralysis o TCA’s – Used for Depression, anorexia, insomnia, ODC, Panic disorder, and neurogenic pain. Takes 10-14 days to become effective. Provider will chose this drug if (1) it worked on family member in past and (2) severity of adverse effects. “Start low and go slow” ▪ Side Effects: Anticholinergic effects (urinary retention, dry mouth, blurred vision, dizziness, tachycardia, constipation, reflux), Postural Hypotension. ▪ S/Sx of Overdose: tachycardia, MI, heart block, dysrhythmias ▪ Contraindications: Elderly and those with Cardiac Disease ▪ Patient Teaching: takes 6-8 for full effect, get up slowly from sitting position, take at BEDTIME to reduce side effects, good mouth care/lozenges for dry mouth, don’t stop cold turkey o MAOI–. (ex: Phenelzine/Nardil, Isocarboxazid, Parnate) ▪ Side Effects: insomnia, palpitations, H/A, loss of libido, Orthostatic Hypotension ▪ Contraindications: Foods with Tyramine (causes Hypertensive Crisis. Food Ex: avocados, figs, bananas, smoked meats, organs, lunch meat, yeast, aged cheese, beer/wine, smoked fish, soy sauce), Pregnancy!!! ▪ Patient Teaching: Hypotension is HUGE – get up slowly from sitting, avoid Tyramine foods, avoid cold medications, go to ER if pounding H/A, avoid eating at Chinese restaurants. • Benzodiazepines – commonly given & teaching needed for patients o (Ex: Alprazolam, Diazepam, Lorazepam)(“Pam and Lam sisters”) o Very sedating, quick onset o Dependence on meds is HUGE. Don’t use a Benzo with a patient who has a history of drug abuse. Adverse Reactions: sedation, dry mouth, decreased cognitive function. Patient Teaching: increase fluids for dry mouth, don’t take if breastfeeding or if you have a drug abuse problem (ETOH too). Taper off the med. Take with or shortly after meals. Don’t take with Antacids, alcohol or caffeine. • Defense Mechanisms o Altruism – emotional conflict are addressed by meeting the needs of others. o Sublimation – substituting something constructive for something they feel they lack or are inadequate at o Suppression – denial of something disturbing o Repression – forgetting/excluding unpleasant things from memory (forgetting a death of a parent, etc) o Displacement – transferring feelings from a particular person/event to something non-threatening (Boss yells at man man yells at wife wife yells at child child kicks the dog). o Undoing – compensation for a negative action, common in OCD (Ex: giving a gift to undo an argument. Washing hands frequently to reduce anxiety about dirty thoughts). o Somatization – turning anxiety into physical symptoms o Dissociation – the pain/anxiety is too much to deal with, so the patient dissociates to get away from it (an “out of body” experience). o Projection – blaming another PERSON for your own issues o Reaction Formation – unacceptable feelings are kept out of awareness by doing the opposite behavior (Ex: person who doesn’t like children becomes a boy scout leader) o Passive Aggressive – aggression towards others is expressed by procrastination, failure, and illness that affect others more than themselves. o Splitting – qualities of a person are either all good, or all bad – not a healthy mix. (either good, loving, nurturing or bad, mean, hateful). o Idealization – emotional issues are dealt with by exaggerated qualities to others (putting someone on a pedestal, AKA “the perfect man”). When other person doesn’t hold up to their idealization, they are disappointed. o Denial – ignoring the existence of realities (Ex: denying the diagnosis of cancer, even when presented with the lab work and diagnostics) • Discuss the benefits of Buspirone o Less sedating than Benzodiazepines. Takes 3+ weeks to become effective (slow onset). No physical dependence (patients who have drug abuse problems can safely take this medication). Patient Teaching: Taper off the med. Take with or shortly after meals. Don’t take with Antacids, alcohol or caffeine. • Thought Disorders • Positive and Negative Symptoms of Schizophrenia o Positive: delusions, paranoia, hallucinations, unreal perceptions o Negative: flat affect, loss of joy (anhedonia), no motivation, laziness o Cognitive: cant concentrate, poor judgment, focus & memory impaired o Affective: hopeless, suicide ideations, inadequacy, poor social skills • EPS/Tardive Dyskinesia o Tardive Dyskinesia: spasms of the mouth, tongue, lip- smacking, facial grimacing (not reversible, no antidote/cure) o Acute Dystonia: muscle stiffness (especially neck and head) o Akathisia: restlessness, pill rolling, pacing (rocking back in forth in a chair, shifting weight from side to side) • Neuroleptic Malignancy Syndrome o Results from use of Typical Antipsychotics (Ex: Haldol) o Symptoms: Severe muscle rigidity, confusion, agitation, increased temperature (103+), pulse and BP o Interventions: 1. Stop the medication 2. Dantrolene (fever reducing agents) 3. Cool body to reduce fever 4. Maintain hydration with IV fluids 5. Treat cardiac dysrhythmias • Summary of Delusions o Thought broadcasting—belief that one's thoughts can be heard by others (e.g., “My brain is connected to the world mind. I can control all heads of state through my thoughts.”) o Thought insertion—belief that thoughts of others are being inserted into one's mind (e.g., “They make me think bad thoughts.”) o Thought withdrawal—belief that thoughts have been removed from one's mind by an outside agency (e.g., “The devil takes my thoughts away and leaves me empty.”) o Delusion of being controlled—belief that one's body or mind is controlled by an outside agency (e.g., “There is a man from darkness who controls my thoughts with electrical waves”) and made to feel emotions or sensations (e.g., sexual) that are not one's own. o Nursing Interventions: Don’t try to correct the patient. DON’T TOUCH the patient because they already are untrusting of people. Offer fluids and foods in containers so that people can see that you haven’t tampered with it (or “poisoned it”). Good options are soda in the can, food in wrappers, fruit, yogurts, and hard-boiled eggs. Use 1:1, PRN meds and seclusion instead of restraints. • Summary of Hallucinations o Auditory: hearing voices or sounds that aren’t there but are projections of inner thoughts or feelings o Visual – seeing a person or object that isn’t there o Olfactory - smelling things that aren’t there o Gustatory – tasting sensations are altered (Ex: Sam wont eat his food because he “tastes” the poison the FBI is putting in his food) o Tactile – feeling strange sensations from an object that wouldn’t feel that way o Nursing Interventions: (1) What are the voices saying to do? (2) Do you recognize the voices? (3) Do you plan to follow the command? *Speak in louder voice, remind the patient that the voices are not real (Ex: “your voices….”, take safety measures ASAP if patient is harm to self/others* • Antipsychotic Medications o Atypical Antipsychotics/ 2nd Gen. ▪ (Ex: Clozapine, Risperidone, Quetiapine (Seroquel), Olanzapine, Abilify) Targets both POSITIVE and NEGATIVE symptoms. Adverse Effects: weight gain, hypertension, increased glucose levels, Heart Disease o Typical Antipsychotics/1st Gen. ▪ (Ex: Haldol, Chlorpromazine) Targets POSTITIVE symptoms only. Adverse Effects: Highly sedating, EPS, TD, Neuroleptic Malignant Syndrome (give Cogentin & lower drug dose), Check blood sugars regularly, falls risk. • Personality, Somatoform, and Eating Disorders • Personality Disorders: Traits of a person exaggerated to the point in which they interfere or cause destruction in one’s life. Your “Difficult Patient”. Have issues working and with relationships/loving. Use Primitive (Immature) Defenses. Don’t treat with Benzos! Use 2nd Gen Antipsychotics and Antidepressants. o Histrionic: (think Marilyn Monroe – sex icon) flamboyant, wears a ton of make-up, tight clothes, and seductive behavior, seeking attention/love/admiration. Throws tantrums if attention needs not met. o Schizotypal – eccentric, magical thinking, odd/strange behavior, illogical speech. o Obsessive-Compulsive: concerned with order, neatness, rules, perfection, and lack sense of humor, superficial intimacy in relationships. o Narcissistic: (assholes) attention seeking, grandiosity (sense of entitlement), shallow relationships focused on what others can do for them, arrogant. o Borderline: (self-mutilation & suicide prone behaviors) emotional instability, sees relationships to not feel abandoned/alone. o Antisocial: (manipulators & con-artists), no remorse, no moral values, lie, steal, feel no responsibility. Don’t let them be in a position of power (judge, public speaker, etc.). o Dependent: afraid of being alone, cannot survive if left alone, stays in abusive relationships or may “relationship-jump”, have high anxiety. • Manipulation Interventions o Set clear rules on behaviors and enforce them CONSISTENTLY o DON’T make promises, keep secrets, do special favors or accept gifts • Highest nursing priority with these dx o SAFETY is #1 o Diagnosis depends on the type of PD the person has o Think Maslow….Basic Needs/Safety/Love & Belonging • What comorbidities exist with Anorexia and Bulimia? o Depression, OCD, Social Phobia, Anxiety (feelings of emptiness and helplessness). Always assess for suicide/self-harm in these patients. • Eating Disorder S/Sx: o Anorexia S/Sx: Terrified of gaining weight, moving food around plate, cutting food into tiny pieces, wearing baggy clothes to hide body, sunken eyes, protruding bones, views self as fat, exercising to exhaustion, lanugo, amenorrhea, osteoporosis. (Test Question for Select All that Apply (was on Exam 3): Milieu Therapy for Anorexia: (1) Scheduled meal times, (2) Scheduled weights (3) Selects from a specific menu (4) Observe before/after meals & in bathroom o Bulimia S/Sx: Erosion of teeth, GERD, stomach pain, frequent trips to bathroom to purge (especially after meals), Russell’s sign (calluses on knuckles), cardiac dysrhythmias • Conversion Disorder o Patient has motor/sensory deficits with no medical reason (blindness, loss of function of limbs, seizures, abnormal gait, deafness). o “La Belle Indifference” – patient wants MD care, but not concerned with their symptoms. o Patient Example: “ I woke up this morning and I couldn’t move my arm” • Conduct Disorder o Aggressive behavior towards others (cruelty to animals, using weapons), destructive behaviors, lying, manipulating, running away from home, truancy, sexually active at very young age o Nursing Intervention: #1 is protection from harm, provide positive feedback for acceptable behavior, provide immediate non-threatening feedback for negative behavior, and Help child use tools to control impulses and toleration of frustration, use ROLE PLAY to help them learn how to respond to feelings. • Addiction, Abuse and Violence • Signs of Alcohol Withdrawal o Peak: 24-48 hours o Symptoms: hyper-alert, jerky movements, irritability, startles easy, “shaking inside”, tachycardia, sweating, increased: BP, HR, hallucinations, disorientated, agitation, small pupils o Seizures: 7hrs – 48 hours after stopping drinking • Alcohol Dependence – know associated dx o Risk for Suicide, Risk for other-directed Violence, Hopelessness, Denial, Low-Self-Esteem, Anxiety o Depression & Alcohol go hand in hand. • Nursing Interventions & Assessment tools o Keep them SAFE while they are withdrawing from drugs o BAL (blood alcohol levels) o Seizure precautions • Medications for Alcohol Withdrawal o Chlordiazepoxide (Librium) – provides SAFE withdrawal and has anticonvulsant effects. Used for ACUTE withdrawal. #1st Choice Med o Disulfiram (Antabuse) – Used for MAINTENANCE. Makes you severely ill/sick if you drink alcohol. (Negative feedback) Metallic aftertaste. o Naltrexone (Revia)- Used to reduce cravings. Used in the first 12 weeks of ACUTE recovery. • Interventions for Pre-Assaultive Patient o Respond early and consistently to angry/aggressive behavior o Leave door open, stay between the door and the patient (never let patient get between you and the exit!), low tone voice, talk slowly and calmly, appear calm & collected, ask “What will help now?”, sit at 45 degree angle to patient o Reintegration: gradual increase in the ability of the patient to handle stimulus. • Cognitive and Degenerative Disorders • Alzheimer’s - Understand Pathology o Slow deterioration. NOT REVERSABLE. Results in impaired memory (from death of neurons), judgment, agnosia, forgetfulness, inattention, Short Term Memory Goes First, “Sundowning”, Preservation (repetition of phrases or behaviors) o HEAD TRAUMA– Big influence in Dementia/Alzheimer’s!!! o Use Confabulation to fill in gaps of memory (putting truth and made up stores into the same sentence and they don’t know the difference) o 4 A’s of Dementia/AD: ▪ Amnesia, Aphasia, Apraxia, Agnosia • Alzheimer’s – Meds used o Aricept (Donepezil) – slows down the deterioration/cognitive decline, but only for a short while. o Rivastigmine (Exelon)– slows down the deterioration/cognitive decline, but only for a short while. o Memantine (Namenda) – targets symptoms of Alzheimer’s disease in the moderate to severe stages. • Stages of Dementia: 1. Stage 1: mild/forgetfulness 2. Stage 2: moderate/confusion 3. Stage 3: severe/unable to identify objects/people 4. Stage 4: late/end-stage • Defense mechanism: Confabulation (making up stories or answers to maintain self-esteem when they do not remember), Perseveration (repetition of phrases or behavior) • Nursing Interventions: Always introduce yourself, call patient by name with every contact, expectations should be clear and explained in simple, step-by-step instructions, simple appropriate choices. Example “Do you want to wash your face before or after you brush your teeth.” • Family teaching/education: Nurses need to teach the families about dementia, where to get help, community resources, etc. Gradually take the car away, NO throw rugs, tape cords to the floors, mattress on the floor/bed alarms, keep it simple & Familiar as possible. • Nursing Diagnosis for Alzheimer’s o Risk for Injury, Fear, Acute Confusion, Disturbed Sleep Patterns, Impaired Memory, Powerlessness, Impaired Verbal Communication • Impulsive Behaviors: o Short Periods between thoughts and actions. (Person doesn’t stop and think, they just act to relieve anxiety/stress). o Stealing, fire setting, gambling, and sexting are examples. Person feels relief of anxiety once they complete the behavior. • Nursing Interventions for Impulsive Behavior: (Impulsive Behavior: short periods between thoughts and actions) ▪ What precedes the event? (Find the trigger) ▪ How do they feel AFTER they do the act? Any repercussions? ▪ Teach patient coping skills ▪ Discuss alternative behaviors • Patients in Crisis, Grief, Complementary Therapy • Discuss factors that influence the grieving process o Lack of support/empathy from others o Trying to hurry through the process to get back to their responsibilities o Failure to accept reality of loss or denying themselves the right to grieve/mourn. • Describe alarm, exhaustion, fight or flight o Alarm – trigger of the fight or flight mechanism o Exhaustion – extreme fatigue (mentally, emotionally, physically) o Fight or Flight – (Sympathetic Nervous System triggered by hypothalamus). Is a survival mechanism that alerts our bodies to be ready to meet a threat or stress. Increased pulse, BP, respirations, HR, alertness. • Identify forms of complementary therapies o Herbals, aromatherapy, acupuncture, pressure point therapy • Stress Reduction Techniques o Meditation, Yoga, Massage, Deep Breathing, exercise, nature, sunlight therapy, Reframing, Decrease Caffeine intake, SLEEP!, Meaningful work/satisfying work, live with who you want, love who you want, set your own life goals • 5 Stages of Grief 1. Denial – person cannot accept his/her painful loss (feels numb or may be emotionally dry). Lasts a few hours or days. 2. Anger – person places feelings on medical/nursing staff, or towards the deceased. Usually peaks during the 1st month after death. 3. Bargaining – hope that one can avoid grief by making a bargain (I will change the way I live, if mom can live just one more year). 4. Depression – extreme sadness and despair. Ex: “I miss my loved one, so why go on with life” 5. Acceptance – Moving forward with one’s life (“It’s going to be okay”.) • Crisis - Environmental Disasters & Situational Crisis o Environmental: floods, earthquakes, tornadoes, volcanoes, tsunamis, hurricanes, avalanches, mudslides, fires, snow emergencies o Situational: loss of a job, death of a loved one, unwanted pregnancy, financial changes, divorce, and severe physical/mental illness. • Crisis Nursing Interventions – Highest Priority o Physical Safety is #1 Priority. (This can be either keeping the patient safe from self-harm/suicide, or securing them to safety where food/shelter/clothing are available. o Crisis is an acute, time limited occurrence. Usually resolves in 4-6 weeks. o Patient Safety & Anxiety Reduction are two basic goals • Nursing Assessment Priority during Crisis o Can the patient identify: Precipitating event, situational supports and coping skills? o AFTER ruling out suicide/self-harm, assess: 1. Patient’s perception of the event (Questions to ask: What leads you to seek help now? Describe how you are feeling now. Has anything upsetting happened to you within the past few days/weeks? How do you see this event affecting your future?) 2. Patient’s support system (Questions to ask: Whom do you live with? Who can you trust? Who is available to help you? Who do you talk to when you feel overwhelmed? Do you have other family?) 3. Patient’s coping skills (Questions to ask: Have you thought of killing yourself or someone else? If yes, do you have a plan? What do you do to feel better? What do you think might happen now?) • Interventions for Patients in Crisis 1. Assess for suicide/self-harm. SAFETY #1 ALWAYS! 2. Lower patient anxiety 3. Listen & summarize what patient says at the end 4. Contact social worker/shelter/babysitting, etc. 5. Assess support systems 6. Identify coping skills that patient has and ones they need to learn 7. Plan f/u visits/phone calls/etc. • Nursing Diagnosis for Crisis: o Risk for Self-Directed Violence, Hopelessness, Social Isolation, Risk for Loneliness, Ineffective Coping, Powerlessness, Chronic Sorrow • Primary, Secondary and Tertiary Nursing Care o Primary: promoting mental health (ex: teaching coping skills, stress reducing techniques, meditation, reducing life changes) o Secondary: interventions during an acute crisis to prevent prolonged anxiety (ex: working to assess problem, support systems, and coping styles). Happens in an ER, clinic, hospital, MH center, etc. o Tertiary: providing support for those in recovery from crisis/facilitating optimal levels of functioning & emotional wellbeing (ex: rehab centers, outpatient services, workshops, etc) • Disenfranchised Grief o Grief experienced by a NURSE regarding a PATIENT who dies (or over an abortion, death from AIDS or execution, war heroes, divorced spouse, suicides). The nurse cannot openly grieve, it may not be acknowledged by others, so it may be difficult to deal with. • Caring for a Dying Patient o #1: Assess your own skill level and seek help from other nurses is necessary o Good Listening Skills & Sensitivity towards patients and family o Conservation of Dignity (access to wigs, clothing, cosmetics, discussing their legacy, allow patient as much control over their situation as possible, food/music/friends visiting, and spiritual comfort access) • Nursing Interventions for Acute Grief (lasts 4-8 weeks) o Be present. Listen to them. Sharing painful feelings during periods of silence help with healing and convey concern. o Share information on the Grieving Process (let them know these feelings are normal). Provide handouts for reference and support information. o Encourage support of friends and family or even Bereavement Groups o Spiritual support o Empathetic Words are ALWAYS helpful! Examples are: ▪ This must hurt terribly. ▪ I hear anger in your voice. Most people go through periods of anger when their loved one dies. Are you feeling angry now? ▪ Are you feeling guilty? This is a common reaction many people have. What are some of your thoughts about this? ▪ This must be very difficult for you. [Show More]
Last updated: 1 year ago
Preview 1 out of 20 pages
Reviews( 0 )
Recommended For You
*NURSING> EXAM REVIEW > NUR2063 / NUR 2063 Essentials of Pathophysiology Exam Review Latest Update Rasmussen College (All)
NUR2063 / NUR 2063 Essentials of Pathophysiology Exam Review Latest Update Rasmussen College
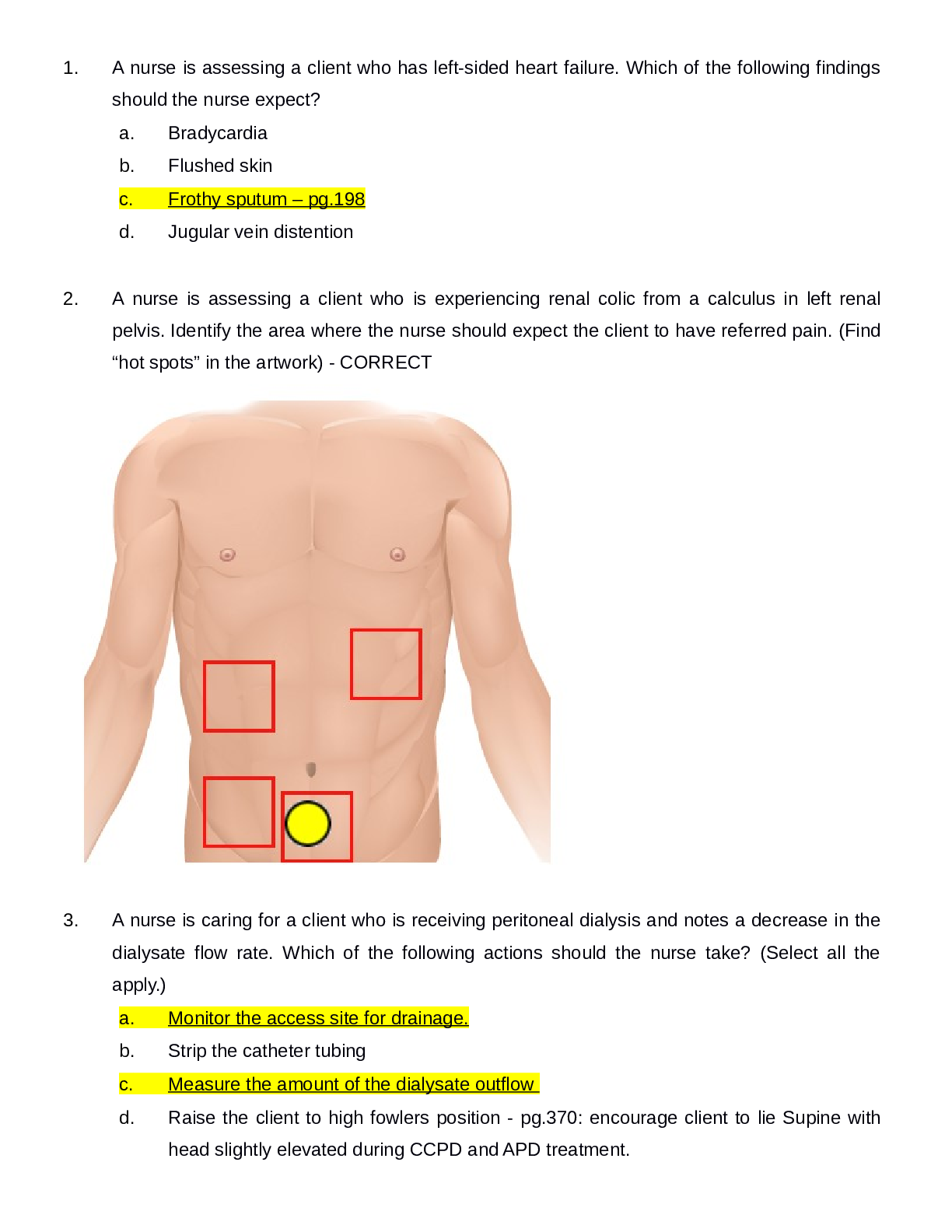
NUR 2063 Essentials of Pathophysiology Exam Review 1. A potentially lethal condition in which there is an acute elevation of circulating thyroid hormones is called _______________ - ANS: Thy...
By quiz_bit , Uploaded: Oct 28, 2020
$12
*NURSING> EXAM REVIEW > NUR2488 / NUR 2488 Mental Health Final Exam Review | Highly Rated Guide |LATEST, 2021/2022 | Rasmussen College (All)
NUR2488 / NUR 2488 Mental Health Final Exam Review | Highly Rated Guide |LATEST, 2021/2022 | Rasmussen College
NUR2488 / NUR 2488 Mental Health Final Exam Review | Highly Rated Guide |LATEST, 2021/2022 | Rasmussen College Defense mechanisms: a) Compensation: emphasize strengths to make up for weaknesse...
By nurse_steph , Uploaded: Sep 08, 2021
$12
*NURSING> EXAM REVIEW > NUR 2488 Mental Health Final Exam Review. DownloadTo Score A | Rasmussen College. (All)
NUR 2488 Mental Health Final Exam Review. DownloadTo Score A | Rasmussen College.
NUR 2488 Mental Health Final Exam Review. DownloadTo Score A | Rasmussen College.
By A+ Solutions , Uploaded: Oct 27, 2021
$12
*NURSING> EXAM REVIEW > Ati Med-Surg Final Exam Review Latest 2021. 100% Correct. (All)
Ati Med-Surg Final Exam Review Latest 2021. 100% Correct.
Ati Med-Surg Final Exam Review Latest 2021. 100% Correct.
By Rose Babyface , Uploaded: Aug 05, 2021
$15
*NURSING> EXAM REVIEW > Mental Health Final (All)
Mental Health Final
Introduction in Psychiatric Nursing Basic Brain Anatomy- what do the different part of brain control? Hypothalamus? Neurons/ synapse- pg. 51 Hypothalamus: Regulates temperature, blood pressure, per...
By Dr Fiona , Uploaded: Apr 27, 2021
$11
*NURSING> EXAM REVIEW > NUR 2488 Mental Health Final Exam Review (Download To Score) (All)
NUR 2488 Mental Health Final Exam Review (Download To Score)
NUR 2488 Mental Health Final Exam Review
By Good grade , Uploaded: Feb 13, 2021
$15
*NURSING> EXAM REVIEW > NSG 6020 APEA 3P Week 3 Exam Review Latest Update (All)

NSG 6020 APEA 3P Week 3 Exam Review Latest Update
NSG 6020 APEA 3P Week 3 Exam Review
By Good grade , Uploaded: Dec 30, 2020
$18
*NURSING> EXAM REVIEW > NSG 6020 APEA 3P Week 3 Exam Review Latest Update (All)

NSG 6020 APEA 3P Week 3 Exam Review Latest Update
NSG 6020 APEA 3P Week 3 Exam Review
By Good grade , Uploaded: Dec 30, 2020
$18
*NURSING> EXAM REVIEW > NR302 / NR 302: Health Assessment EXAM REVIEW Latest Update Chamberlain College of Nursing (All)
NR302 / NR 302: Health Assessment EXAM REVIEW Latest Update Chamberlain College of Nursing
NR-302 Health Assessment Health assessment Exam Review 1. Which finding would require immediate reaction from the nurse If found during the physical assessment - Oxygen saturation of 88%...
By quiz_bit , Uploaded: Nov 20, 2020
$13.5
*NURSING> EXAM REVIEW > NR224 / NR 224: Fundamentals Final Exam Review Latest Update Chamberlain College of Nursing (All)
NR224 / NR 224: Fundamentals Final Exam Review Latest Update Chamberlain College of Nursing
NR-224 Fundamentals Final Review 1. critical thinking - continuous process characterized by open-minded, continual inquiry and perseverance 2. levels of critical thinking - basic (concrete...
By quiz_bit , Uploaded: Nov 13, 2020
$9
Document information
Connected school, study & course
About the document
Uploaded On
Feb 08, 2022
Number of pages
20
Written in
Additional information
This document has been written for:
Uploaded
Feb 08, 2022
Downloads
0
Views
146






