*NURSING > STUDY GUIDE > NR566 Week 5 Study Outline Chapter 18: Drugs Affecting the Hematopoietic System_ lATEST,100% CORRECT (All)
NR566 Week 5 Study Outline Chapter 18: Drugs Affecting the Hematopoietic System_ lATEST,100% CORRECT
Document Content and Description Below
NR566 Week 5 Study Outline Chapter 18: Drugs Affecting the Hematopoietic System_ lATEST • Know the pharmacodynamics, pharmacotherapeutics clinical use, drug interactions and adverse drug reactions ... for: Anticoagulants • Pharmacodynamics • Oral anticoagulants such as warfarin (Coumadin) inhibit the hepatic synthesis of several clotting factors, including factor X. • Heparin inhibits the activity of several activated clotting factors by accelerating the activity of antithrombin III. • LMWH enoxaparin (Lovenox) potentiates the activity of antithrombin III and inactivates factors Xa and IIa (thrombin). • Dabigatran (Pradaxa) is a direct thrombin inhibitor. • Thrombin is required for the conversion of fibrinogen to fibrin in the clotting cascade, thus dabigatran's inhibition of thrombin prevents thrombi from forming. • Fondaparinux (Arixtra) is a selective inhibitor of antithrombin III and a factor Xa inhibitor. • Rivaroxaban (Xarelto) an anticoagulant, is a highly selective factor Xa inhibitor that inhibits thrombin formation and the development of thrombi. • Apixaban (Eliquis) is a selective inhibitor of factor Xa. • Aspirin antagonizes the cyclooxygenase pathway and interferes with platelet aggregation. • NSAIDs have this same action. • NSAIDs are not used as antiplatelet drugs, but this explains why concurrent use with anticoagulants is contraindicated • Ticlopidine (Ticlid) and clopidogrel (Plavix) reduce platelet aggregation by inhibiting the ADP pathway of platelets. • Unlike aspirin, they have no effect on prostaglandin metabolism. • Ticagrelor (Brilinta) reversibly interacts with the platelet P2Y12 ADP-receptor to prevent platelet activation. • Vorapaxar (Zontivity) is a protease-activated receptor-1 (PAR-1) antagonist, inhibiting thrombin-induced and thrombin receptor agonist peptide-induced platelet aggregation • Pharmacotherapeutics: • Precautions and Contraindications • All anticoagulants are contraindicated for patients who are hypersensitive to the drug or actively bleeding or who have hemophilia, thrombocytopenia, severe HTN, intracranial hemorrhage, infective endocarditis, active tuberculosis, or ulcerative lesions of the GI tract. • Heparins are contraindicated in advanced hepatic or renal disease. • They may be used in patients who are actively bleeding to treat DIC • Heparin is Pregnancy Category C: stillbirth, prematurity • Some heparin preparations contain benzyl alcohol: known to cause “gasping syndrome”: • fatal toxicity in neonates • Hyperkalemia may develop • Use for patient with DM or renal insufficiency requires care and frequent monitoring of aPTT • Has been associated with fatal medication errors r/t different strengths of preparations • JCo: anticoagulant therapy is a National patient Safety Goal: plan in place at each facility to reduce patient harm • LMWHs are contraindicated for patients with allergies to pork, sulfites, or benzyl alcohol; uncontrolled bleeding; and in patients who have antiplatelet antibodies • Renal impairment: cautious use • Body weight less than 50 kg associated with increased r/f bleeding: • enoxaparin dose adjustment • Cautious use: untreated HTN, retinopathy (HTN or DM caused), severe liver disease, recent Hx of ulcer, or malignancy • Not used for thromboprophylaxis in patients with mechanical heart values: especially pregnant (r/f heart value thrombosis) • Enoxaparin: Preg Cat B, tinzaparin: teratogenicity and fetal death, fondaparinux: Preg B • First line drug for women who require antithrombotic therapy during pregnancy: LMWH • Pharmacokinetics of LMWH is altered during pregnancy • Warfarin • Hepatic dysfunction potentiates response through impaired synthesis of coagulation factors • Use with caution: Hypermetabolic states produced by fever or hyperthyroidism increase responsiveness to warfarin: • r/t increased catabolism of vit K dependent coagulation factors • Increased r/f bleeding in older adults • Caution use based on balance between potential for decreased r/f thromboembolism and the risk for bleeding especially in those with dementia or severe cognitive impairment: Hx of three falls in the previous year or recurrent injurious falls, uncontrolled HTN, or non-adherent or unreliable • Warfarin is Pregnancy Category X: Crosses placenta and can cause hemorrhagic disorders in the fetus and serious birth defects • Safe during lactation • Rivaroxaban (Xarelto): Black-Box Warning: premature discontinuation of anticoagulants including rivaroxaban may lead to thrombotic events. • An increased risk of stroke is seen in patients with atrial fibrillation when transitioning to warfarin • Rivaroxaban is Pregnancy Category C and is not recommended for use in pregnant women. • Apixaban (Eliquis): Black Box warning premature discontinuation leading to thrombotic events • Although there are no well-controlled studies: Pregnancy Category B • Hypersensitivity to aspirin and cross-sensitivity with NSAIDs may occur, contraindicating the drug • Aspirin hypersensitivity is more prevalent in patients with asthma, nasal polyps, or chronic urticaria. • Reye syndrome has been associated with its use in children and teenagers who have influenza or chickenpox. • Reversible hepatotoxicity has occurred • Use with caution in liver damage, preexisting hypoprothrombinemia, or vit K deficiency • Preg Cat C and Cat D in third trimester • Avoid during lactation • Clopidogrel and ticlopidine: severe hepatic disease (r/f bleeding d/o), do not use in these patients • Not recommended for patients with GI d/o • Preg Category B • Ticlopidine: clearance increased with age, older adults increased sensitivity to this drug (closely monitor or ADRs) • Older adults: increased levels of clopidogrel: no dosage adjustments • In older adults clopidogrel is a safer drug • Ticlopidine: elevations in cholesterol and TC within 1 month of therapy: factor in HLD • Ticagrelor: Black-Box Warning to not use in a patient with active pathological bleeding or history of intracranial hemorrhage. • Ticagrelor should be discontinued 5 days prior to any surgery. • Dabigatran: Black-Box Warning concerning discontinuation increasing risk of thrombotic events. • There is no reversal agent available for dabigatran • Vorapaxar: Black-Box Warning to not use in patients with a history of stroke, TIA, intracranial hemorrhage, or active pathological bleeding. • Vorapaxar is Pregnancy Category B, with no congenital malformations found in animal studies • ADRs • All anticoagulants: excessive bleeding • Risk is higher early in therapy, with wide fluctuations in aPTT or INR, and older adults (especially women over 60) • Heparins: cause thrombocytopenia and anemia • More likely with bovine than with porcine • Early thrombocytopenia 2 to 3 days after starting therapy and delayed forms 7 to 12 days • Platelet below 100,000: d/c heparin • Enoxaparin antidote: protamine sulfate 1 mg for each mg of enoxaparin dalteparin and tinzaparin: 1 mg for each 100 anti-Xa IUs of dalteparin • Slow IV injection • Fondaparinux: no known antidote • Heparin has a short half-life: Tx is usually d/c of the drug • Protamine sulfate antidote for heparin OD • Warfarin: toxicity and OD Tx withholding one or more doses • Or 1 to 10 mg of vitamin K is the antidote for minor bleeding • 5 to 50 may be used for frank bleeding • Hemorrhagic skin necrosis in women and cyanotic toes in men have been reported • r/t transient inhibition in proteins S and C • Allergic reactions: symmetrical, maculopapular, erythematous lesions • Some are isolated and some confluent: face, neck, and torso • May not appear until 8 to 10 days • Ribaroxaban: bleeding is major ADR • No reversal agent • Back pain, upper ABD pain, osteoarthritis, dyspepsia, and fatigue • Apixaban: bleeding • No reversal agent • ASA: gastric erosions: increased r/f serious upper GI bleeding • More likely when used in combo with other anticoags such as warfarin • Salicylism (tinnitus) : serum levels above 200 mcg/mL • Toxicity: tinnitus, HA, hyperventilation, agitation, confusion, lethargy, diarrhea, and sweating • Ticagrelor: bleeding • Dyspnea: sometimes improves with use or must be d/c • HA, cough, dizziness, and nausea • Ticlopidine: reversible neutropenia at 3 weeks to 3 months after initiation of therapy • Severe neutropenia (<450) or thrombocytopenia (<80,000) d/c drug • Clopidogrel: ADRs similar to ASA, safe and effective • Dabigatran: bleeding • GI ADRs: dyspepsia and gastritis-like symptoms • Angioedema and thrombocytopenia • Vorapaxar: bleeding • Anemia, depression, and rashes or eruptions • Drug Interactions • Cephalosporins and PCNs given parenterally associated with coagulopathies, increased r/f bleeding when given with Heparin • Second and third gen cephalosporins and high doses of PCNs: increased r/f bleeding with Warfarin • Drugs that affect platelet functioning or cause hypoprothrombinemia (ASA, NSAIDS, dipyridamole, quinidine, and valproic acid: increased r/f bleeding • Heparin and LMWHs: similar drug interactions: also interact with antiplatelets including NSAIDS and dextran • Foods can effect anticoags • Warfarin: many drug interactions and increased INR monitoring within 4 to 7 days when other drugs are started or stopped even ABX • Vit K: antagonistic interaction with warfarin: decreases effectiveness • Inhibitors of CYP 1A2, CYP 2C9, or CYP 3A4 increase effect of warfarin • Inhibitors decrease the effectiveness of warfarin • Interacts with any other drug that increased bleeding: anticoags, antiplatelets, NSAIDS and SSRIs • ABX and antifungals may affect INR • Herbal Productions may increase bleeding: ginkgo biloba and garlic • Decrease effectiveness: St John’s wort, ginseng, and coenzyme Q10 • May influence metabolism of warfarin: St John’s wort, echinacea, ginkgo, goldenseal, AND GRAPEFRUIT JUICE • Dabigatran: rifampin (decreased levels of dabigatran) • Dronedarone increased dabigatran levels by 70 to 150% • CCB verapamil: increases dabigatran • Amiodarone increases dabigatran • Clopidogrel increases dabigatran • Ticagrelor: metabolized by CYP 3A4: avoid strong inhibitors ketoconazole, itraconazole, voriconazole, clarithromycin, nefazodone, ritonavir, saquinavir, nelfinavir, indinavir, atazanavir, and telithromycin • Avoid inducers: rifampin, dexamethasone, phenytoin carbamazepine, and phenobarbital • Vorapaxar: avoid with CYP3A inhibitors • Avoid use of inducers (rifampin, carbamazepine, St John’s Wort, and phenytoin • Clinical Use and Dosing Prevention and Treatment of Thromboembolism • Warfarin: drug of choice for prevention of venous thrombosis, systemic thrombosis, and pulmonary embolism o For prevention: give dose sufficient for INR between 2 and 3 o Beginning dose is 10 mg daily for the first 2 days with a recheck of INR in two to three doses o ICSI guidelines: recommend starting warfarin at 5 mg/day with a range of 2.5 mg to 7.5 mg/day o Further dosing is based on INR o Lower initiation doses for: ▪ Older than 75 ▪ Multiple comorbid conditions ▪ Poor nutrition (low albumin) ▪ Elevated INR when off warfarin ▪ Elevated LFTS ▪ Changing thyroid status o If INR is greater than 2 after the first 3 doses, consider decreased the dose by one half o If INR raises rapidly: search for reasons: drug interactions, poor nutrition, infection, or systemic disease process • Acute PE, DVT, or acute systemic embolization: admit to hospital for IV anticoagulation o Heparin, LMWH, or SC fondaparinux and then placed on oral anticoags o Treat while waiting on Dx tests o Acute PE: heparin, LMWH, or fondaparinux for at least 5 days until INR is greater than or equal to 2 for 24 hrs o ACCP recommends staring warfarin on the first day of Tx in conjunction with heparin, LMWH, or fondaparinux or SX heparin o PE due to transient (reversible) risk factor is warfarin for 3 months • Superficial Vein Thrombosis: 45 days of prophylaxis with fondaparinux or LMWH o Lower limb of at least 5 cm in length o ACCP recommends fondaparinux 2.5 mg/day over prophylactic LMWH • Deep Vein Thrombosis: Divided the Tx of acute DVT into acute treatment of DVT of the leg and Tx of the upper extremity DVT o Leg or UE: short term Tx with SC LMWHs, SC fondaparinux, or IV or SC heparin for at least 5 days and until the INR is 2 for 24 hr o LMWH and SC fondaparinux: preferred over heparin o Warfarin: initiated on the first Tx day (like PE) • Idiopathic DVT: maintained on warfarin with target of 2.5 (range 2.0 to 3.0) for 3 months • Indwelling Cline: at r/f DVT o Tx is the same as for leg DVT o After Cath removed: 3 months of anticoags (Warfarin) • All other patients requiring anticoags therapy can be started on Warfarin as OPs o 10 mg/day or 5 mg/day, o Unless patient wt. is less than 110 lbs., over 75, or at ARF bleeding ▪ Start these patients on 2.5 mg/day o Steady state is achieved in 5 to 7 days: dosage adjustments are made ATT based on INR • Goal of therapy is an INR of 2 to 3 for all Tx durations • For patients with DVT or PE and CA: LMWH for 3 to 6 months o Referral for management • Air travel time longer than 8 hrs: increases r/f thrombus formation o Wear loose clothing, avoid tight clothing around the waist or lower extremities, good hydration, and frequent calf muscle exercises o At high risk for DVT: wear compression stockings 15 to 30 mm Hg during air travel • Immobility (bedrest): ambulation as tolerated o Use of compression stocking with 30 to 40 mm Hg for 2 years after DVT episode Prevention of Embolic Stroke in AFib • Low risk for stroke: ASA 75 mg to 325 mg daily • Intermediate risk for stroke: oral anticoags o Anticoags or a combination of ASA and clopidogrel • High risk for stroke: oral anticoags o ACCP recommends: 150 mg of dabigatran BID rather than warfarin • For patients with paroxysmal AFib at high risk for stroke: warfarin target INR between 2 to 3 • For AFib and mitral stenosis: follow recommendation of those at high risk o If valve replacement: follow recommendations for those with heart valves regardless of AFib • Apixaban: to reduce risk of stroke and systemic embolism in non-valvular AFib o 5 mg BID o For those older than 80, less than 60 kg, or crt >1.5 dose at 2.5 mg BID Mitral Valve Disease • Rheumatic MVD but no AFib and left atrial diameter of less than 55 mm: no therapy • Rheumatic MVD with left atrial diameter of greater than 55 mm or left atrial thrombus or AFib or previous embolism: warfarin target INR of 2.5 • Therapy is continued indefinitely in all cases Antithrombotic Therapy for Ischemic Stroke • Acute ischemic stroke or TIA: early (within 48 hours) ASA therapy at 160 to 325 mg • ACCP has three options for long term therapy after noncardioembolic ischemic stroke or TIA • 75 to 100 mg ASA/day • Combo of ASA (25 mg) and ER dipyridamole or clopidogrel • Patients with Hx of ischemic stroke or TIA with AFib: 150 mg dabigatran BID over warfarin Recurrent Embolism or Prosthetic Heart Valves • Warfarin: drug of choice o Therapy initiated and maintained the same as for prevention of venous thrombosis o Except that the target INR is valve dependent • For patients with additional risk factors (AFib, MI, left atrial enlargement, endocardial damage, and low EF) o 75 to 100 mg/day of ASA should be added to Warfarin protocol o The same is true for patients with caged ball or caged disc valves • Bioprosthetic valves in SR: 75 to 100 mg/day of ASA o Therapy is continued indefinitely for mechanical heart valves • For systemic embolization that recurs after 6 months of therapy: therapy is continues for an additional 12 months • Pregnant patients with MHV: require anticoags o Use one of three treatment regiments ▪ LMWH BID ▪ SC heparin every 12 hours ▪ Or SX heparin or LMWH until the 13th week of pregnancy then warfarin until close to delivery with LMWH or heparin is resumed o Warfarin is a known teratogen: may cause fetal hemorrhage o Women with MHV at high risk of thromboembolism: ASA 75 to 100 mg/day added to anticoags regimen o Women on warfarin planning on pregnancy: frequent pregnancy tests and substitution of heparin or LMWH when pregnancy is achieved o Anticoagulation specialist and perinatologist Prevention of MI • Several protocols are effective in prevention of MI in patients with and w/o CAD o Over 50 w/o symptomatic CVD: ASA 75 to 100 mg/day o Established CAD (1 year post ACS, with prior revascularization, coronary stenoses greater than 50% by angiogram, and/or evidence for cardiac ischemia on Dx testing): ASA 75 to 100 mg/day or clopidogrel (75 mg/day) o Patients with ACS who have undergone PCI with or w/o stent placement: dual therapy: 90 mg ticagrelor BID plus ASA 75 to 100 mg/day ▪ ACCP: recommends use of ticagrelor over clopidogrel in PCI • Patient who have experienced an MI: anticlot therapy o STEMI: fibrinolytics then ongoing therapy after hospital d/c • Post-AMI TX: • Anterior AMI w/ r/f LV thrombus who do not get a stent: warfarin (INR target 2 to 3) and ASA 75-100 mg/day • Patients with an acute MI who have a bare metal stent: triple therapy o Warfarin (INR target 2-3), ASA low dose, and 75 mg daily clopidogrel for a month after stent placement o Then warfarin and one antiplatelet drug for months 2 and 3 o After 3 months: d/c warfarin and replaced with dual antiplatelet therapy (90 mg ticagrelor BID plus ASA 75 to 100 mg/day for up to 12 months • Patients with DM: ASA 75 to 162 mg/day • Vorapaxar: approved for reduction of thrombotic CV events in patients with Hx of MI or with PAD o Patient takes one 2.08 mg tablet daily in addition to ASA or clopidogrel Prevention of Post-Operative Thromboembolism • J Co requires that all hospital have a formal active strategy to prevent venous thrombosis • LMWH, low dose heparin, or fondaparinux o Moderate-risk major general surgery, higher risk patients who are having a major procedure for CA, major vascular surgery, major gynecological surgery, major urological procedures, bariatric surgery, thoracic surgery, and many orthopedic surgeries • Length of Tx: determined by the type of surgery, ranging from a single dose to 10 days for most orthopedic procedures, to 28 days in high risk patients, patients undergoing major gynecological surgery, and patients having major surgery for CA • Hip or knee replacement: Apixaban 2.5 mg BID Perioperative Therapy of Patients on Warfarin or Antiplatelet Therapy • Stop Warfarin 5 days before surgery and resume 12 to 24 hours after surgery • For prevention of thromboembolism (MHV, AFib): may require parenteral anticoags perioperatively o Decision to bridge with heparin is determined by balancing r/f bleeding due to the surgical procedure and clotting risk due to the underlying d/o • Low bleeding risk: skin biopsies, cataract surgery, and most dental procedures can remain on warfarin o Dental procedures: tranexamic acid mouthwash can be used w/o interrupting anticoags therapy • Low risk thromboembolic risk (AFib w/o prior stroke or remote Hx of venous thrombosis): warfarin stopped 5 days prior to surgery and resumed that evening of surgery • High thromboembolic risk (PHV): bridging with LMWH or unfractionated heparin may be indicated • Antiplatelets: do not d/c before surgery • Rational Drug Selection • Cost can be significant • PO anticoags are preferred: no special equipment or skills to administer, less expensive • Brands are not interchangeable • Monitoring • Dosage adjustments of warfarin is by INR o Daily INRs initially to guard against excessive anticoagulation until therapeutic range for 2 days o Testing interval is then lengthened to 2 or 3 times weekly for 1 or 2 weeks o Self-testing is increasing in popularity: competency using the equipment o Computer assisted, validated, decision, support tools for warfarin dose regulation: more effective than traditional dosing at maintaining therapeutic INR values o Evidence based dosing tools, patient Edu, follow up, and optimal patient communication: best patient outcomes o CYP 2C9 or VKORC1 gene variants: may require 2 to 4 weeks longer to reach target INR • Monitoring heparin adjustments: aPTT blood tests o Goal of therapy is 1.5 to 2.5 times the control o Platelet and Hct every 2 or 3 days o Thrombocytopenis: tends to occur about 4th day and resolves despite continued heparin therapy o Day 8: thrombocytopenia severe enough to require d/c med o After this time period: periodic testing of platelet and Hct and occult blood in stool o Low doses of SC heparin (5,000 U BID) do not require monitoring r/t does not prolong the aPTT • LMWH: same periodic monitoring of platelet and Hct: likelihood of thrombocytopenia is much less o Test for monitoring: anti factor Xa assay o aPTT may be prolonged: dopes not reliably reflect activity o Routine Xa not recommended: except in pregnant patients • ASA dose for antiplatelet therapy is low to moderate o Serum salicylate level is approximately 100 mcg/mL • Clopidogrel: safety profile similar to ASA, no routine monitoring • Ticlopidine: Severe neutropenia and thrombocytopenia have occurred o CBC, WBC with differential counts every 2 weeks, starting from the second week to the end of the third month of therapy o More frequent monitoring is necessary for patients whose absolute neutrophil counts consistently decline or are 30% lower than baseline o After the first 3 months: CBCs as needed for s/s of infection • Also know: Use of anticoagulants in pregnancy: • Enoxaparin is Pregnancy Category B. • Teratogenicity and fetal death have been reported as well for tinzaparin, although a clear cause-and-effect relationship was not established. • Fondaparinux is also listed as Pregnancy Category B but without adequate or well-controlled studies in pregnancy. • LMWHs do not cross the placenta and do not cause teratogenicity or fetal bleeding • The American College of Chest Physicians recommends LMWH as the first-line drug for women who require antithrombotic therapy during pregnancy: enoxaparin (Lovenox), dalteparin (Fragmin), and tinzaparin (Innohep) • The pharmacokinetics of LMWHs are altered during pregnancy. • LMWH passes in small amounts into breast milk but has low oral bioavailability and may be safely used during breastfeeding Thromboprophylaxis • Prevention and treatment of thromboembolism: o Warfarin is drug of choice for the prevention of venous thrombosis, systemic thrombosis, and pulmonary embolism • Prevention of embolic stroke in AFib: o Low risk for stroke: ASA 75 mg to 325 mg daily o Intermediate risk for stroke: oral anticoags ▪ Anticoags or a combination of ASA and clopidogrel o High risk for stroke: oral anticoags ▪ ACCP recommends: 150 mg of dabigatran BID rather than warfarin o For patients with paroxysmal AFib at high risk for stroke: warfarin target INR between 2 to 3 • Prevention of MI o Several protocols are effective in prevention of MI in patients with and w/o CAD ▪ Over 50 w/o symptomatic CVD: ASA 75 to 100 mg/day ▪ Established CAD (1 year post ACS, with prior revascularization, coronary stenoses greater than 50% by angiogram, and/or evidence for cardiac ischemia on Dx testing): ASA 75 to 100 mg/day or clopidogrel (75 mg/day) ▪ Patients with ACS who have undergone PCI with or w/o stent placement: dual therapy: 90 mg ticagrelor BID plus ASA 75 to 100 mg/day • ACCP: recommends use of ticagrelor over clopidogrel in PCI o Patient who have experienced an MI: anticlot therapy ▪ STEMI: fibrinolytics then ongoing therapy after hospital d/c o Post-AMI TX: o Anterior AMI w/ r/f LV thrombus who do not get a stent: warfarin (INR target 2 to 3) and ASA 75- 100 mg/day o Patients with an acute MI who have a bare metal stent: triple therapy ▪ Warfarin (INR target 2-3), ASA low dose, and 75 mg daily clopidogrel for a month after stent placement ▪ Then warfarin and one antiplatelet drug for months 2 and 3 ▪ After 3 months: d/c warfarin and replaced with dual antiplatelet therapy (90 mg ticagrelor BID plus ASA 75 to 100 mg/day for up to 12 months o Patients with DM: ASA 75 to 162 mg/day o Vorapaxar: approved for reduction of thrombotic CV events in patients with Hx of MI or with PAD ▪ Patient takes one 2.08 mg tablet daily in addition to ASA or clopidogrel • Prevention of Post-Operative Thromboembolism o J Co requires that all hospital have a formal active strategy to prevent venous thrombosis o LMWH, low dose heparin, or fondaparinux ▪ Moderate-risk major general surgery, higher risk patients who are having a major procedure for CA, major vascular surgery, major gynecological surgery, major urological procedures, bariatric surgery, thoracic surgery, and many orthopedic surgeries o Length of Tx: determined by the type of surgery, ranging from a single dose to 10 days for most orthopedic procedures, to 28 days in high risk patients, patients undergoing major gynecological surgery, and patients having major surgery for CA o Hip or knee replacement: Apixaban 2.5 mg BID • The ACCP recommends the use of LMWH, low-dose heparin, or fondaparinux as thromboprophylaxis in the following surgical procedures: moderate-risk major general surgery, higher-risk patients who are having a major procedure for cancer, major vascular surgery, major gynecological surgery, major urological procedures, bariatric surgery, thoracic surgery, and many orthopedic surgeries • LMWH should not be used for thromboprophylaxis in patients with mechanical prosthetic heart valves, especially pregnant women, as prosthetic heart valve thrombosis may occur. Population needed warfarin starting dose adjustment: Older than 75 years • Multiple comorbid conditions • Poor nutrition (low albumin) • Elevated INR when off warfarin • Elevated liver function tests • Changing thyroid status INR target goals o Prevention of DVT, PE, or systemic embolism: 2-3 o Prevention of embolic stoke in patient with AFib: 2-3 o Patients with St. Jude Medical bileaflet PHV: 2-3 o Patients with tilting disk valves and bileaflet PHV ion aortic position: 2.5-3.5 o Patients with CarboMedics bileaflet valve or Medtronic Hall tilting disk PHV: 2-3 o Patients with MHV and high risk (atrial thrombus, AFib, hypercoagulable state, and low EF): 2.5-3.5 o Patients with caged ball or caged disk PHV: 2.5 to 3.5 o Patients with bioprosthetic valve in mitral position: 2-3 o Patients with bioprosthetic vale in aortic position: 2-3 Anticoagulant preferred for patients at high risk for stroke with atrial fibrillation: • High risk for stroke: oral anticoags o ACCP recommends: 150 mg of dabigatran BID rather than warfarin • For patients with paroxysmal AFib at high risk for stroke: warfarin target INR between 2 to 3 o than 80, less than 60 kg, or crt >1.5 dose at 2.5 mg BID Drugs which decrease anticoagulant medication effectiveness: o Heparin: NTG decreases effect of heparin o Warfarin: oral contraceptives, barbiturates, carbamazepine, chlordiazepoxide, cholestyramine, dicloxacillin, griseofulvin, nafcillin, rifampin, flu vaccine, foods high in vitamin K, large amounts of avocado, soy milk, ginseng o Clopidogrel: phenytoin, tolbutamide, tamoxifen, torsemide, Fluvastatin, NSAIDS Chapter 19: Drugs Affecting the Immune System • Know the pharmacodynamics, pharmacotherapeutics clinical use, drug interactions and adverse drug reactions for: Immunizations Immunizations • Frequently encountered in primary care: Prevent the spread of infectious diseases • Single best technique for preventing infectious disease Attenuated Vaccines Influenza Live, Attenuated Influenza Vaccine • Pharmacodynamics o LAIV: included strains dependent upon predicted circulating influenza strains • Pharmacotherapeutics o Contraindicated: o Egg or egg product hypersensitivity, asthma, reactive airway disease, or other chronic d/o of the pulmonary or CV systems o Persons with underlying medical conditions: DM, renal dysfunction, and hemoglobinopathies o Known or suspected immunodeficiency diseases or immunosuppressive therapy ▪ Patients who are immune compromised or with HIV should not be vaccinated with LAIV o Do not administer to those with Guillain-Barre syndrome o Preg Cat C: should not be vaccinated with LAIV o Contraindicated: children under 2 y/o r/t increased incidence of RAD and asthma o Contraindicated in children or adolescents receiving ASA or other salicylates r/t Reye syndrome • ADRs o Usually well tolerated: mild and transient ADRs o Adults: reported resp symptoms: runny nose or nasal congestion, HA, sore throat, cough, and muscle aches o No serious ADRs have been reported in children older than 2 or adults • Drug Interactions o Wait 48 hrs after stopping antivirals to receiving LAIV o May be concurrently administered with MMR and varicella o May be given with any of the inactivated vaccines ▪ May be given with inactivated or live vaccines on the same day if not separate vaccines by 4 weeks • Clinical Use and Dosing o Children and adults aged 9 through 49: 0.2 mL LAIV o Children 5 to 8: w/o prior flu immunization: two doses (0.2 mL each) separated by 4 weeks o Children 8 years and younger who have previously received two doses in the same year need only one day annually o Intranasally: half of drug in each nostril • Monitoring and Patient Education o Lab monitoring not necessary o Live virus: stay away from close contact with immunocompromised persons for 7 days after admin o Report serious or moderate reactions: difficulty breathing, wheezing, hives, swelling, unusual weakness, and temp 38.9C or higher Measles, Mumps, and Rubella Vaccine (MMR) ▪ Pharmacodynamics o Stimulates the immune system to produce antibodies by inducing a subclinical infection with attenuated virus particles o Subclinical infection is not contagious o The antibodies are capable of virus neutralization by complement activation, induction of cell mediated immunity , and opsonization o M-R-Vax II: commonly used combo vaccine also ProQuad ▪ Pharmacotherapeutics o The virus has been detected 1 to 4 weeks in the pharynx or nose after vaccine administration: does not appear to cause virus transmission o Relatively few true contraindications o Previous anaphylactic reaction to the MMR, neomycin, or gelatin ▪ Hx of contact dermatitis to neomycin is not a contraindication o Not recommended for immunocompromised patients ▪ Do not give to patients who are severely immunocompromised r/t CA, leukemia, or lymphomas or on immunosuppressive drug therapy (high dose steroids or radiation) o May be given to close contacts of immune suppressed patients (health care workers) o Deferred if a patient has moderate or severe febrile illness ▪ Minor illnesses with or w/o fever (diarrhea, URI, or OM) are not contraindications o Patients who receive blood products should wait 3 months before getting the MMR o MMR should be given at least 2 weeks before immune globulin (IG) ▪ Those who receive IG should wait 3 to 11 months o Do not give to pregnant women or women who may become pregnant within 3 months ▪ r/t congenital rubella syndrome in the infant o Safely given to children of all given ▪ May not be immunogenic in infants under 12 months ▪ If given under age 12 months, revaccinate at 12 to 15 months, and a third dose at 4 to 6 y/o ▪ ADRs o Children: fever 7 to 12 days after vaccination, lasts 1 to 2 days otherwise asymptomatic o May cause transient maculopapular rash 7 to 10 days o May cause febrile seizure: highest risk at 6 to 14 days o Thrombocytopenia: rare and may occur within 2 month, generally benign and transient o Injection site pain, redness and swelling, muscle or joint aches, and dizziness or light headedness ▪ Drug Interactions o Do not give to patients receiving immunosuppressants (high dose corticosteroid, interferon, and antineoplastic drugs) r/t insufficient response to immunization o MMR may be inactivated by IG: give 14 to 30 days before or 3 months after o Delay PPD for 4 to 6 weeks after MMR: temporary decrease in tuberculin skin sensitivity o MMR and varicella: compatible if done the same day (different needles, separate sites) ▪ If not given the same day: separate by 1 month o MMRV (ProQuad): measles, mumps, rubella, and varicella in children 12 months to 12 y/o ▪ First dose separate MMR and varicella vaccines r/t risk of febrile seizures with MMRV o MMR can be given with LAIV on the same day, if not 4 weeks ▪ Clinical Use and Dosing o Routinely given SC at 12 to 15 months with repeat dose at age 4 to 6 y/o o Second dose: may be given as soon as 4 weeks after the first dose o Indicated ruing an epidemic or before international travel o CDC recommends second dose as MMRV o Adults: born in 1957 or later who are at least 18 should receive at least one dose of MMR if no serological proof of immunity or documentation of a dose given on or after the patient’s first birthday o High risk groups: students entering college, military, and international travelers, healthcare workers: two doses o Adults born before 1957 are considered immune but documentation of immunity is important ▪ Monitoring and Patient Education o Labs not needed o Rubella titer: to determine immunity o All patients or the parents/guardians: required by law to receive Vaccine Information Statements that are developed by the CDC o Provide adequate information to the patient before immunization should be made o Fever up to 103 7 to 12 days after admin o Patient may experience rash, malaise, or sore throat Measles, Mumps, Rubella, and Varicella Vaccine o Pharmacodynamics o Similar to MMR o MMRV (ProQuad): live attenuated virus, produces a subclinical infection o Creates active immunity to measles, mumps, rubella, and varicella o Pharmacotherapeutics o Same as for MMR: Hx of anaphylactic reaction to neomycin or gelatin or any other component of the vaccine ▪ Immediate Tx for anaphylaxis reaction should be available when administering MMRV o Contraindication: primary or acquired immunodeficiency (HIV/ADIS and patients with blood dyscrasias, leukemia, lymphomas, or other malignant neoplasms affecting the bone marrow or lymphatic system o Preg Cat C: do not administer, avoid pregnancy for at least 3 months o Untreated TB or febrile illness with temp greater than 101.3, deferred until well o Use with caution in patient with Hx of cerebral injury, seizures, or other conditions in which physiological stress due to fever should be avoided r/t increased risk of fever and febrile seizures with MMRV o Avoid for 3 months after blood transfusion or IG admin o ADRs o Similar to MMR o More likely to develop fever and rash o Injection site pain, erythema, and swelling o Drug Interactions o Same as MMR: immunosuppressants, IG, tuberculin skin tests, and salicylates o Clinical Use and Dosing o Given SC at 12 to 15 months o First dose may be given any time before age 12 o Three months should elapse before second dose of MMRV o MMRV: can be given 1 month after MMR o Patient Education o Talk with parents about increases risk of fever and febrile seizures with the combo vaccine Oral Poliovirus Vaccine (No longer used in the US but used in other countries) o Pharmacodynamics o Stimulates immune system to produce anti-poliovirus antibodies: Sabin poliovirus types 1, 2, and 3 o Live attenuated virus enters small intestine: replicates in villous epithelial cells o Specialized epithelial cells transport the viral antigens to the B cells and macrophages: produce antibodies in 1 to 2 weeks o Live attenuated poliovirus lingers in GI for 4 to 6 weeks o Two doses of PPV are needed for intestinal immunity ▪ Three doses for lifelong immunity o Pharmacotherapeutics o Contraindication: anaphylactic reaction to any previous dose of OPV o Do not use with neomycin or streptomycin hypersensitivity o Delay with moderate or severe febrile illness or severe resp infection o Contraindicated: viral GI infection, ongoing diarrhea, or vomiting o Immunocompromised patients may develop poliomyelitis from live poliovirus o Contraindicated: CA, leukemia, lymphoma, radiation therapy, immunodeficiency (HIV or AIDS) or drugs that effect immunity ▪ Use IVP in immune compromised patients and household members are immune compromised o Pregnancy Cat: C o ADRs o Low incidence of paralytic poliomyelitis (those who receive it and household contacts) o Most likely to occur after the first dose o Household members are exposed r/t virus shedding in feces o Drug Interactions o Do not administer to patients receiving immunosuppressants, r/t insufficient response to immunization ▪ Use IPV in these patients o MMR, MMRV, hep B, DTP, DTaP, influenza, and HIB may be given with OPV o Avoid concurrent administration with cholera vaccine, parenteral typhoid vaccine, or plague vaccine r/t increased ADRs o IG may be given with OPV o Clinical Use and Dosing o IPV is first choice for immunization o OPV: use only for special circumstances: mass vaccination campaigns to control outbreaks or in unvaccinated children who will be traveling in less than 4 weeks to endemic or epidemic areas Rotavirus Vaccine o Pharmacodynamics o Leading cause of gastroenteritis in infants and young children worldwide o RotaTeq live oral vaccine: contains five strains (Gi, G2, G3 or G4, P7) o Rotarix: G1, G3, G4, and G9 o Both vaccines are live vaccines that replicate in the small intestine and induce active immunity o Pharmacotherapeutics o Do not administer: ▪ Infants who are or may be potentially immunocompromised (including infants with blood dyscrasias, leukemia, lymphoma, or other malignant neoplasms, infants on immunosuppressive therapy) ▪ Infants with primary and acquired immunodeficiency states (HIV/AIDS) ▪ Infants who have received blood transfusion or blood products in the past 42 days o Delay vaccine with febrile illness except when withholding the vaccine creates greater risk to the patient o Minor URI with low grade fever (under 100.5) not a reason to withhold o Do not administer with acute gastroenteritis until it improves o Rotavirus may shed in stools: prudent to use caution if in contact with those with malignancies or otherwise immune compromised and contacts on immunosuppressive therapy o Hx of intussusception is a contraindication r/t increased risk of intussusception following the first dose o ADRs o ARF intussusception o RotaTeq: GI ADRs: vomiting, diarrhea o Rotarix: slight incidence of vomiting in the week after admin o Drug Interactions o Can be administered concurrently with DTaP, IPV, HIB, HBV, and pneumococcal conjugate vaccine o Clinical Use and Dosing o RotaTeq: series of three ready to use oral liquid doses ▪ 6 to 12 weeks first dose, second and third doses in 4 to 10 week intervals o Rotarix: two dose schedule of 1 mL/dose given at 2 to 4 months o May be given between 6 to 24 weeks, give the two doses 4 weeks apart o No considerations for blood products or IG Varicella Virus Vaccine o Pharmacodynamics o Varivax: live vaccine, produces IgG antibody humoral immune response to VZV o Also have cell mediated immune response: activation of CD41 helper T cells and CD 81 T lymphocytes o Efficacy is measured by protection against disease and protection against severe disease ▪ One dose: 94% over 10 years ▪ Two doses: 98% effective against any disease and 96% effective against household exposure o Vaccination appears to prevent serious illness even in those who do not seroconvert ▪ Post vaccination cases are mild, and recovery is quicker o Pharmacotherapeutics o Contraindicated: neomycin or gelatin hypersensitivity o Delay vaccine if moderate or severe illness present with or w/o fever o Immune compromised individuals: ARF development of varicella from use of live virus o Contraindicated: CA, leukemia, lymphoma, radiation therapy, and immunodeficiency, symptomatic HIV o Contraindicated: drugs that affect the immune system ▪ Those on low dose systemic steroids (asthma) if less than 2 mg/kg or less than 20 mg/day of prednisone and not otherwise immune compromised o May be given to a patient if an immune compromised person in the household o If a rash develops: avoid contact with immune compromised people for the duration of the rash o Avoid in pregnancy: Category C o Avoid pregnancy for 1 to 3 months o ADRs o Children and adults: fever, injection site reaction, and a vesicular rash o Adults and adolescents: two injections and have similar ADRs ▪ Fever, injection site reaction, generalized vesicular rash o Drug Interactions o Do not give to those taking immunosuppressants: r/t insufficient immunization o Avoid use during IG therapy, do not use for 3 to 11 months o Check for need to revaccinate if taken close together o MMR and varicella are compatible: given the same day, separate by 1 month if not o Can be given simultaneously with DTaP, DT, Td, HIB, IPV, OPV, PCV13, or HBV o Avoid ASA for 6 weeks after vaccination r/t Reye syndrome o Clinical Use and Dosing o Vaccinate at 12 to 15 months: all healthy children ▪ Second dose at 4 to 6 y/o (before kindergarten) ▪ Separate first and second dose by at least 3 months o Healthy adolescents age 13 and older w/o Hx of infection who have not been vaccinated: two doses 4 to 8 weeks apart o If a child is accidentally administered zoster vaccine (Zostavax) instead of varicella vaccine (Varivax): should be counted as a valid vaccine and reported to VAERS whether ADRs occur ▪ Child will still require two doses of varicella vaccine o Adults: w/o immunity should receive the vaccine ▪ Adults at high risk of exposure: live with children, live or work in an environment in which transmission is likely (teachers, healthcare workers, day care workers) or could occur (college dorm, correctional institution, military) or immune compromised household member ▪ Nonpregnant women of childbearing age, and international travelers o Adults should receive two doses: 4 to 8 weeks apart o Patient Education o ARF fever, injection site reaction, or vesicular rash Zoster Vaccine o Pharmacodynamics o Shingles is a localized and painful cutaneous eruption caused by reactivation of VZV o Latent in neuronal cell bodies and when reactivated causes shingles o Zoster vaccine (Zostavax): live attenuated VZV o Reduces risk of shingles by 50% and 66% effective in preventing post herpetic neuralgia o Reduces severity of zoster o Approved for adults aged 50 years and older o Most effective in patients aged 60 to 69 and least effective in those over age 80 o Pharmacotherapeutics o Contraindicated: Hx of anaphylactic reaction to neomycin, gelatin, or vaccine components o Do not give to those with primary immunodeficiency states o Do not give to those with leukemia, lymphoma, CA of the bone marrow or lymphatic system or AIDS r/t development of disseminated disease o Do not take while actively receiving high dose corticosteroids (prednisone), wait a month after stopping o Not approved for women of childbearing age and should not be used in pregnancy o Do not give to those with active TB or acute illness, or with fever o ADRs o Injection site pain/tenderness, erythema, swelling, and pruritis; HA o Drug Interactions o Stop antiviral drugs (acyclovir, famciclovir, and valacyclovir) 24 hours before vaccine admin o Do not use antiviral for at least 14 days after vaccination o Can be given before, after, or at the same time as blood products or antibody containing products o Stop long term/high dose prednisone for 1 month before vaccination o Short term or low dose may be vaccinated o Methotrexate low doses, azathioprine, or 6 mercaptopurine for Tx of RA, psoriasis, polymyositis, sarcoidosis, or IBD may be vaccinated with zoster vaccine o Clinical Use and Dosing o A single dose of zoster vaccine is recommended for all adults aged 60 years or older o SC tissue of deltoid o Can be given with Hx of herpes zoster o Can be given with Td, Tdap, and pneumococcal o Separate zoster vaccine and other live virus vaccines by 4 weeks o Zoster vaccine is not recommended for those who received the varicella vaccine o Patients with chronic medical conditions (CRF, DM, RA, and chronic pulmonary disease) may be vaccinated o Defer in severe illness or with fever o Can be given in minor acute illness w/o fever (URI) o Immunosuppressed: greater morbidity and mortality from herpes zoster o Give at least 14 days prior to immune suppressive therapy o Avoid for at least 24 months after stem cell transplant o Avoid antiviral meds for 14 days after vaccination o If a child is accidentally given zoster vaccine: valid vaccine, report to VAERS o If an adult is given varicella vaccine: not a valid dose and the zoster vaccine is given the same day o If not the same day 28 days later Oral Typhoid Vaccine Pharmacodynamics o Used to increase resistance to enteric fever caused by Salmonella typhi o Spread by ingesting water contaminated by feces from infected persons o Risk is greatest in travelers to South Asian, East and Southeast Asia, Africa, Caribbean, and Central and South America o OTV (Vivotif Berna): live attenuated vaccine Ty21a o Ingested and works in the small intestine to synthesize a lipopolysaccharide that evokes a protective immune response o 50 to 80% effective in preventing typhoid fever o Efficacy of protective immunity: dependent upon the size of the bacterial inoculum consumed Pharmacotherapeutics o Contraindication: hypersensitivity to typhoid vaccine o Do not give to immune compromised patients o Do not given during acute febrile illness or acute GI illness o Preg Cat C: if vaccine is needed use inactivated vaccine o Not recommended for children younger than 6 y/o: use inactivated vaccine in young children ADRs o Infrequent and transient and resolve with intervention o ABD pain, diarrhea, vomiting, fever, HA, and rash have been reported Drug Interactions o Mefloquine (Lariam) (antimalaria drug): can inhibit the growth of the live Ty21a strain: given either 24 hours before or after mefloquine o Immunosuppressants: insufficient response to the vaccine o OTV: do not given while receiving sulfonamides and ABX r/t prevention of sufficient degree of multiplication to induce a protective immune response Clinical Use and Dosing o Used for primary immunization against S. typhi in the following o Travelers to areas of increased risk o Household contact with a documented typhoid fever carrier o Lab workers o In patients over 6 y/o: dose is one capsule on alternative days for a total of four doses o Take 1 hour before meals (empty stomach) with a glass of cold water o Swallow whole o All four doses must be taken at least 1 week prior to travel Yellow Fever Vaccine Pharmacodynamics o Viral illness spread by some species of mosquitoes in Central and South America and in tropical regions of Africa o Endemic in sub Saharan African and tropical South America o Produces a hemorrhagic fever and is fatal in 20 to 50% of severe cases o All travelers should use personal protective measures to avoid mosquito bites o Vaccination is recommended for travel to endemic areas o Refer to current CDC guidelines for endemic areas because they can change o Certification of vaccination may be required to travel into some areas o Yellow fever vaccine (YF-Vax): live attenuated virus that is prepared by culturing the 17D strain virus in a living chick embryo Pharmacotherapeutics o Avoid in patient with Hx of egg hypersensitivity or sensitivity to chicken protein or gelatin o Contraindicated in immune compromised o Use with caution in HIV patients o Contraindicated: thymus d/o that affects immune function o Defer vaccination for 8 weeks following blood or plasma transfusion o Pregnancy Category C: use only if exposure risk is high o Contraindicated: infants younger than 6 months r/t increased r/f vaccine associated neurological disease o Use with caution in infants aged 6 to 8 months o Rare cases of encephalitis have occurred in infants at this age o Use with caution: aged 60 years and older r/t increased r/f serious ADRs after vaccination ADRs o Fever or malaise (7 to 14 days after vax) o Myalgia or HA o Anaphylaxis has occurred: keep epi on hand when given the vaccine o Very rare reaction: yellow fever vaccine associated viscerotropic disease: fever and multiple organ failure o Higher among those 60 and older o Case fatality ration is 53% o Yellow fever vaccine associated neurological disease: conglomerate of clinical syndromes including meningoencephalitis, GBS, encephalomyelitis, bulbar palsy, and Bell’s palsy o Adverse neuro outcomes are usually seen among infants as encephalitis but may occur at any age Drug Interactions o Concurrent vaccination with HAV, HBV, meningococcal vaccine, typhoid fever vaccine, DTaP, Tdap and measles vaccines is ok o Immunosuppressants: insufficient response to the yellow fever vaccine Clinical Use and Dosing o Immunization against yellow fever is recommended for all people over age 9 months who are living in or traveling to endemic areas o Dose is a single 0.5 mL dose given SC o Should be repeated every 10 years Bacillus Calmette-Guerin Vaccine Pharmacodynamics o BCG lowers the risk of serious complications of primary TB in children o Not widely used in the US but used in countries where TB is endemic o BCG stimulates natural infection with My tuberculosis and results in a T cell medicated immune reaction and immunity against TB but with variable degrees of protection o The protective effect of BCG used in children against military and meningeal TB is about 80% o It is less effective in adults Pharmacotherapeutics o Do not use in Active TB o PPD skin testing should be performed on all patients over 2 months of age o Contraindicated in CA, leukemia, lymphoma, radiation therapy, and immunodeficiency o Patients with symptomatic or asymptomatic HIV should not receive BCG o Drugs that affect the immune system: contraindicated o Take precautions to avoid accidental exposure to BCG solutions during preparation and administration because this is a live attenuated virus o Pregnancy Cat C: CDC does not recommend use ADRs o Normal reaction: skin lesions that appear within 10 to 14 days after the multiple puncture disc application o The lesions consist of small red papules at the site of admin o Papules reach max diameter (3 mm) after 4 to 6 weeks and then scale away and slowly subside o Lymphadenopathy: may occur in a regional lymph node and resolves spontaneously o Osteomyelitis: rare o BCG induced osteomyelitis: affects the epiphyses of the long bones and can occur from 4 months to 2 years after administration o Lupoid like skin reactions: Tx with INH for 3 months o Disseminated BCG infection and death are very rare and usually occurs in patients with impaired immune systems Drug Interactions o Anti-TB agents (RIF, INH, streptomycin) and immunosuppressives: interfere with development of an appropriate immune response o BCG: will cause PPD skin tests to give false positive readings for up to 10 years, after 10 years: a positive PPD usually indicates infection with M. Tuberculosis Clinical Use and Dosing o In the US: given only in very special circumstances: unavoidable risk of exposure to M. tuberculosis and failure of other methods of prevention and control of TB o Should be considered for infants and children who reside in settings in which the likelihood of TB transmission and subsequent infection is high provided no other measures can be implemented (removing children from the source of infection) o May be considered for health care workers who are employed in settings in which the likelihood of transmission and subsequent infection with TB strains resistant to INH and RIF is high o BCG: given to healthy infants from birth to 2 months w/o TB skin testing o After that, BCG is given only to children with negative Mantoux skin tests o Must be administered exactly as manufacturer suggests o Vaccine is dropped onto clean, dry skin over the deltoid muscle and spread over the area to be punctured, using the edge of the multipuncture disc o The prongs of the disc are coated with the virus by lightly dipping them into the spread vaccine o The prongs of the disc are pressing into the skin and held for 5 to 10 seconds o After the disc is removed: vaccine is respread to fill all the puncture areas o Additional vaccine may be applied to ensure a wet vaccine site o Keep the area dry for 24 hours, no dressing is required o The person administering: take precautions against coming into contact with the live virus o Educate not to touch the site r/t live virus o Keep clean until local reaction has resolved Inactivated Vaccines Diphtheria, Tetanus, and Pertussis Vaccine Pharmacodynamics o Various combinations of diphtheria, tetanus, and pertussis vaccines: basic pharmacodynamics are the same o Diphtheria toxoid: induces the production of antibodies against the exotoxin excreted by Corynebacterium diphtheria o Complete immunization (four doses, then boosters every 10 years) reduces incidence by 95% o Immunized persons who develop diphtheria have milder illness o Infection with C. diphtheria does not confer immunity: those previously infected should vax o Tetanus toxoid: contains antigens that induce the production of antibodies against the exotoxin excreted by Clostridium tetani o Duration of immunity: 10 years o Natural immunity to C. tetani does not occur in the US and patients with previous C. tetani infection should be vaccinated o Pertussis vaccine: inactivated pertussis antigens o Acellular pertussis vaccine contains one or more immunogens derived from Bordetella pertussis and unlike whole cell vaccine contains little or no endotoxin o Antibodies produced against B. pertussis Pharmacotherapeutics o In the US: DTaP be used for primary immunization of infants and children o DTaP contraindication: immediate anaphylactic reaction with a pervious dose o Encephalopathy w/in 7 days of a previous dose, unexplained by another cause: do not use ▪ In this case DT should be substituted for DTaP o Patients with unstable, progressive, neurological problems: defer until neuro status clarified o Precautions: previous temp of 105 or higher within 48 hours after a dose, Hx of continuous crying (more than 3 hours) within 48 hours of a dose, convulsions within 3 days of a previous dose, and collapse or shock like state (hypotonic-hyporesponsive episode) within 48 hours of a dose o Precautions: seizures 3 days or less after a previous dose of DTaP, persistent or inconsolable crying lasting more than 3 hours within 48 hours of a pervious dose, GBS less than 6 weeks after a previous dose of tetanus toxoid containing vaccine, or moderate or severe acute illness with or w/o fever o DTaP: may be given to immunocompromised patients or patients on immune suppressive drugs: immune response may be less than optimal o HIV infected patients may be immunized o Patients with minor acute or febrile illness may be immunized ▪ Delay in cases of moderate or severe illness, with or w/o fever o Infants born prematurely should begin series based on their DOB: first vaccine at 2 months o Pregnant women, including pregnant adolescents, receive a booster of Tdap with each pregnancy ideally between 27 and 36 weeks gestation: passive pertussis immunity, gives 2 to 3 months of protection o Td and Tdap are Pregnancy Cat C: but have been used extensively worldwide in pregnant women o DT contraindications: patients older than age 7, who should be given Td or Tdap, as appropriate o DT and Td: hypersensitivity to any component of the vaccine and moderate to severe illness, with or w/o fever: do not postpone for minor illnesses o Tdap contraindications: GBS 6 weeks or sooner after previous use of tetanus toxoid containing vaccine, previous arthus reaction after receiving tetanus or diphtheria vaccine, or a progressive neurological d/o o Tdap and Td should be deferred with moderate or severe illness, with or w/o fever ADRs o Injection site reactions of mild to moderate pain, erythema, swelling, and induration for a few days o Transient low grad fever, chills, malaise, generalized aches and pain, and HA may occur o Fever was common after DPT and less common after DTaP o Drowsiness, fretfulness, and GI upset may occur o Tdap: most frequent ADR pain at injection site o Seizures may occur and are more likely in children with a Hx of seizures: less common now that DPT is no longer used in the US o Seizures may be r/t fever: antipyretic prophylaxis after DTaP admin every 4 to 6 hrs Drug Interactions o Decreased immunological response: radiation, antineoplastic agents, or immune suppressive agents o DTaP, DT, Tdap, or Td may be coadministered with HBV, HIB, meningococcal, influenza, hep A, and pneumococcal vaccines o Do not co administer: cholera vaccine, typhoid vaccine, or plague vaccine r/t accentuated ADRs Clinical Use and Dosing o DTaP: routinely given at 2, 4, 6, and 15 to 18 months and 4 to 6 years old o Tdap: recommended at age 11 to 12 y/o o Patients should receive a booster dose of Td or Tdap Q 10 years o “Cocooning”: Parents, siblings, grandparents, childcare providers, and health care personnel who care for infants younger than 12 months receive Tdap vaccine to protect the infant against pertussis Haemophilus B Conjugate Vaccine Pharmacodynamics o HIB conjugate vaccine: consist of the HIB capsular polysaccharide covalently linked to another antigen to increase immunogenicity o Stimulates the immune system to produce antibodies that destroy the capsule: making the organism vulnerable to antibody and cell mediated immunity o Unconjugated capsule polysaccharide vaccines cause B cell stimulation only o Conjugation: T cell stimulation occurs as well o HIB conjugate vaccine comes singly and in combo with other vaccines (HBV/HIB, DTaP/HIB, DTaP/IPV/HIB, meningococcal/HIB Pharmacotherapeutics o Anaphylactic reaction to the vaccine or any component is contraindicated o Moderate to severe illness with or w/o fever may be reason to delay vaccination o Minor illness is not a reason to delay admin o HIB should only be given to children under the age of 6 ADRs o Pain, redness, and swelling at the injection site Drug Interactions o No known interactions Clinical Use and Dosing o Dosing depends on the vaccine used o The first dose can be given at 6 weeks but no earlier Inactivated Poliovirus Vaccine Pharmacodynamics o Parenteral noninfectious suspension of three types of inactivated poliovirus o All US poliovirus vaccines as inactivated polio: reduce risk of vaccine associated polio Pharmacotherapeutics o Hx of immediate hypersensitivity reaction after receiving IPV is a contraindication o Neomycin, streptomycin, or polymyxin B hypersensitivity should not receive the vaccine o IPV is preferred over OPV in immune suppressed patients however a protective immune response is not guaranteed o IPV can be administered to patients with HIV o IPV may be given in pregnancy: Category C o Can be used in infants as young as 6 weeks old ADRs o Injection site reaction o Systemic reactions are infrequent Drug Interactions o Immune response to IPV may be diminished by immunosuppressant medications o Revaccinate 3 months after d/c immunosuppressants o Can be coadministered with all other childhood vaccines Clinical Use and Dosing o Primary series of IPV is four doses given at 2, 4, and 6 to 18 months and 4 to 6 years o Four weeks between doses one and two and 2 to 3 o Minimal interval between dose three and four is 6 months Hepatitis B Virus Vaccine Pharmacodynamics o HBV is produced by recombinant DNA from common baker’s yeast that is genetically modified to synthesize HbsAg o Active immunization with HBV stimulates the immune system to produce anti-hepatitis B surface antigen antibodies Pharmacotherapeutics o Contraindication: hypersensitivity to yeast or other components of the vaccine o Moderate or severe illness with or w/o fever is a contraindication to HBV o Patients with renal disease requiring hemodialysis or patients with immunosuppression may require larger doses to achieve adequate serum levels of anti HBs o Pregnancy Cat C: CDC has stated that pregnancy is not a contraindication ADRs o Injection site reactions o Systemic complaints: fatigue, weakness, malaise, fever, HA, NVD, and pharyngitis o Serum sickness has occurred days to weeks after admin o Alopecia: a very rare side effect Drug Interactions o Immunosuppressants and antineoplastic agents may require larger doses or additional doses Clinical Use and Dosing o Vaccination with HBV is recommended for all ages particularly those at high risk of contracting hep B o IV drug users, infants born to mothers who are HbsAg positive, hemodialysis patients, sexually active people with multiple partners, incarcerated people, international travelers, household contacts of hep B carriers, and sexual contacts of hep B carriers o Patients getting tattoos, share razors, toothbrushes, or body piercing jewelry are also at risk o Healthcare workers, day care workers, and other people exposed to body fluids are at risk o Patients with DM are at increased risk and it is recommended they receive the HBV series o Universal vaccination of all infants as a comprehensive strategy to control hep B o Current childhood immunization: three dose HBV series to newborns or at age 11 to 12 o The series can be started at any age o Schedule for vaccinating infants: first dose at birth or before age 2 months, second dose at age 1 to 4 months, dose 3 at 6 to 18 months o The series can be completed in as little as four months o Series is never restarted: no matter how long since the previous dose Hepatitis A Virus Vaccine Pharmacodynamics • HAV vaccine is used to confer immunity to hep A in people at risk of contracting the disease • Stimulation of specific antibodies takes place w/o producing disease symptoms • Antibody titers after HAV are lower than those resulting from Hep A infection • Antibody titer of 20 mIU/mL is protective • Two products available: both have a two dose schedule Pharmacotherapeutics • Contraindication: Hx of severe reaction to HAV • Contraindication: Moderate or severe illness, w/ or w/o fever • Can be given to immunosuppressed but may have lower antibody titers • Pregnancy Category C: CDC has stated that HAV may be given in pregnancy if indicated and poses no risk to the fetus • Safety and effectiveness in children under 12 months have not been established ADRs • Soreness at the injection site, HA, malaise Drug Interactions • Decreased immunological response while taking immunosuppressants or antineoplastic agents Clinical Use and Dosing • Pre-exposure protection from hep A in adults and children • Recommended that all children begin HAV series at 12 months • Those at increased risk: o Traveling or working in endemic regions, over 12 months (S. America, Africa, Greenland, and Asia) o Men who have sex with men o Illegal drug users o Occupational risk for infection (research lab) o People with clotting factor d/os o People with chronic liver disease o Household members and close personal contact of internationally adopted children from endemic countries (start first dose as soon as the adoption planning process begins: at least 2 weeks before arrival • Two products available: HAVrix and VAQTA also combo products (HAV and HBV) • HAVrix: Two dose schedule 6 to 12 months apart • VAQTA: Adults 6 months apart, children 6 to 18 months apart • IM into deltoid: adults and children 3 y/o and older o Vastus lateralis: 12 months to 36 months old o Injection into gluteal region results in suboptimal response • Those with impaired immunity may require additional doses to obtain adequate response o Post immunization testing for those that are immune compromised, not for healthy adults r/t high seroconversion rates in both children and adults Human Papillomavirus Vaccine Pharmacodynamics • HPV causes cervical CA: HPV-16 and HPV 18 cause neoplasia • Two vaccines: o Gardisil (quadrivalent HPV recombinant vaccine for types 6, 11, 16, and 18) o Gardisil 9 (types 16, 18, 31, 33, 45, 52, and 58 Pharmacotherapeutics • Contraindication: severe allergic reactions • Contraindication: yeast allergy • Both vaccines: syncope, observe for 15 mins after admin put in supine or Trendelenburg is symptomatic • Preg Cat B: not recommended for use in pregnancy ADRs • Pain, redness, and swelling at injection site • Fatigue, HA, myalgias, and arthralgias • Serious reaction: syncopal episodes: reports of falling w/ injury Drug Interactions • No known interactions • Immunosuppressants may reduce immune response to the vaccine Clinical Use and Dosing • Dosing varies with the drug and patient gender • Gardasil: girls and women ages 9 to 26 y/o to prevent cervical, vulvar, and vaginal CA caused by HPV types 16, 18, and genital warts caused by HPV types 6 and 11 • Gardasil 9: girls and women ages 9 to 26 y/o to prevent cervical, vulvar, and vaginal CA caused by HPV types 16, 18, 33, 45, 52, and 58; genital warts caused by HPV 6 and 11. • Vax is recommended for all girls starting at age 11 to 12 y/o but may be started as young as 9 y/o • Dosing schedule: three doses of 0.5 mL IM 0, 2, and 6 months • Gardasil: approved for prevention of genital warts types 6 and 11 in males • Gardasil 9: approved for anal warts caused by 16, 18, 31, 33, 45, 52 and 58 and genital warts caused by 6 and 11 • In males 0.5 mL at 0, 2, and 6 months • Cervarix: approved to prevent cervical CA caused by types 16 and 18 in females aged 10 to 25 y/o, 0, 1, and 6 months Influenza Vaccine Pharmacodynamics • Influenza vaccine (Afluria, Fluarix, Flucelvax, FluLaval, Fluvirin, Fluzone, Fluzone Intradermal, Fluzone High-dose) • Multivalent vaccine that contains three different viral subtypes • Available as a trivalent or quadrivalent (Fluarix, Quadrivalent, Flulaval Quadrivalent, Fluzone Quadrivalent) • Flucelvax (trivalent): first cell based flu vaccine • FluBlok (trivalent recombinant hemagluten (HA) flu vaccine containing purified HA proteins: uses cell based technology • The WHO tells the FDA which strains to include for the year, flu virus consistently changes • Stimulates production of antibodies specific to the disease strain Pharmacotherapeutics • Contraindication: anaphylactic reaction to the flu vaccine, eggs, or egg products • CDC developed an algorithm to be used in those who report egg allergy o Recommendation: admin inactivated flu vaccine to patients who can eat lightly cooked eggs w/o a reaction o For those 18 to 49 who experience hives from eating eggs: admin recombinant flu vaccine (Flucelvax, FluBlok) or inactivated flu vaccine and observe for at least 30 mins o Patients with severe hypersensitivity to eggs: only admin the recombinant flu vaccine: produced using non egg technology • Thimerosal: used as a preservative, hypersensitivity contraindicates flu vaccine • Some vaccines contain sulfites: hypersensitivity contraindicates, choose a vaccine that does not contain sulfites • Patient w/ active neuro d/o should defer vaccine until stabilized • Any patient w/ Hx of GBS less than 6 weeks after a previous flu vaccine should not receive • HIV: can be immunized but may have lower vaccine induced antibody levels • Defer with acute febrile illness until symptoms subside • Preg Cat C: according to CDC can be safely administered to pregnant women • Safety not established in children younger than 6 months • Admin error: dosing schedules for children and adults for injectable flu vaccine are different • If an adult is given a peds dose the adult should receive an addition peds dose the same day. If not discovered until later, a full adult dose is given o If a child is given an adult dose: no action needed ADRs • Usually mild and more common in children • Local injection site reaction • Low grade fever, malaise, and myalgia • Hypersensitivity reaction: urticaria, angioedema, bronchospasm, and/or anaphylactic shock o Most likely result of hypersensitivity to residual egg protein Drug Interactions • Immunosuppressants or antineoplastic agents: decreased immune response • Theophylline, phenytoin, and warfarin: inhibited clearance, not a contraindication Clinical Use and Dosing • Admin annually to all persons aged 6 months and older (including pregnant women) • Optimal time is October through mid-November • Travelers to endemic flu zone: vax 2 to 4 weeks prior to travel • Dosing schedules vary by age and past immunization (children) Pneumococcal Vaccine Pharmacodynamics • Two types of pneumococcal vaccine: Pneumovax 23 and Prevnar • Polyvalent pneumococcal polysaccharide vaccine (PPV) contains 23 highly purified capsular polysaccharides from St. pneumoniae o These are the 23 most prevalent or invasive pneumococcal types o PPV stimulates immune system to produce pneumococcus capsule specific antibodies o These antibodies destroy the capsule: pneumococcus vulnerable to antibody and cell mediated immunity • Limited immunogenicity in children younger than 2 • Infants and children: 7-valent conjugate vaccine (Prevnar) o Targets the 7 most common strains in infants • 13-valent conjugate (Prevnar 13, PCV13): adults age 50 and older and age 19 and older with immunocompromising condition, functional or anatomic asplenia, cerebrospinal fluid leak, or cochlear implants Pharmacotherapeutics • Previous anaphylactic reaction contraindicates use • Moderate to severe illness, w/ or w/o fever, defer until patient improved • Should be given 10 to 14 days before elective splenectomy, organ transplant, immunosuppressive therapy, or chemo • Patients with Hodgkin’s disease and immune suppressed: suboptimal antibody response • PPV: use cautiously in patients w/ idiopathic thrombocytopenic purpura: associated w/ relapse • PPV: Preg cat C, avoid in first trimester • PCV13: Preg cat B: no adequate studies • PPV 23-valent: no recommended in children under 2 y/o ADRs • PPV: Local injection site reactions erythema, induration, and soreness for up to 48 hrs o Low grade fever (high grade fever is rare) and arthralgia • Prevnar: generally mild injection site reaction, irritability, drowsiness, and decreased appetite o Children: fever • PCV13: infants had redness, swelling and tenderness at injection site o Fever, irritability, and increased sleep after the first dose (same rate as infants vaxed w/ PCV7) Drug Interactions • No known drug interactions have occurred Clinical Use and Dosing • Dosing of PPV is based on age and medical condition o PPV: all adults aged 65 or older. Revax if original was 6 years ago or more and the patient was under age 65 o People aged 2 to 65 y/o w/ chronic illness and increased risk of morbidity or mortality PPV (chronic cardiac or pulmonary disease, chronic liver disease or alcoholism, DM, and CSF leaks) Revax is not recommended in these populations o Immunocompetent patients aged 2 to 65 y/o with asplenia, revax in 5 years or more after the first dose if the patient is under 10 y/o revaccinate in 5 years o Immunocompromised, CRF, hematological malignancy, Hodgkin’s disease, lymphoma, or multiple myeloma, immunosuppressive therapy and patients who have received an organ or bone marrow transplant. Revax in 5 years o Adult smoker between 19 and 64 (one dose) o Asthma 19 to 64 y/o (one dose) o One dose at 12 and 24 months following bone marrow transplant o A dose of {PPV is given 2 or more months after last dose of PCV13 to children age 2 years and older • PCV13 dosing o Infants and toddlers: four doses at 2, 4, 6, and 12-15 months of age o Children up to age 59 months who are not vaccinated with PCV13 at the routine infant vaccine times should be doses following the catch up schedule o Children aged 6 to 18 with asplenia, HIV infection, cochlear implant, CSF leak, or other immune compromising condition w/o previous PCV 13 should receiving one dose of PCV13 followed by PPV 8 weeks later o Immunocompromised adults age 19 and older who have not received pneumococcal vaccine should receive a dose of PCV13 followed by a dose of PPV 8 weeks later o Immune compromised adults age 19 and older who have received PPV should receive a dose of PCV 13 at least one year after last PPV dose o All adults age 65 or older: if not previously vaccinated dose of PCV13 followed by PPV in 6 to 12 months o Persons age 65 and older who have previously received PPV should be given a dose of PCV13 at least a year after the last PPV dose Meningococcal Vaccine Pharmacodynamics • Meningococcal polysaccharide vaccine (MPSV) for groups A, C, Y, and W135 (Menomune A/C/Y/W135) o Approved in the US for meningococcemia and meningitis caused by Neisseria meningitidis serogroups A,C,Y, and W135 • MCV4 (Menactra, Menveo): tetravalent meningococcal conjugate vaccine, provides protection against serogroups A C Y and W 135 • Hib-MenCY (MenHibrix): Neisseria meningitidis serogroups C and Y and H. influenza type b • Trumembra: used in 10 to 25 y/o, serogroup B meningococcal vaccine • Bexero: meningococcal serotype B: 10 to 25 y/os • In the US: N. meningitidis serogroup C Y and W 73% of infections aged 11 y/o or older o and serogroup B for 60% of cases in children 0 to 59 months old • Group A is rare in the US, most common in Africa and Asia, there have been 2 recent group A outbreaks in the US on college campuses • All the meningococcal vaccines induce the formation of bactericidal antibodies to meningococcal antibodies • Limitations of MVP (Menomune) group C polysaccharide is poorly immunogenic among child less than 2 y/o, does not confer long lasting immunity, and it does not cause a sustainable reduction of nasopharyngeal carriage of N meningitidis o Conjugation of polysaccharide (as in MCV4) to a protein carrier changes the immune response from T cell independent to T cell dependent: leads to stronger response to the vaccine and reduction of the asymptomatic carrier state Pharmacotherapeutics • Previous anaphylactic reaction to any component: contraindication • Moderate to severe illness w/ or w/o fever: defer until patient improved • Hx of GBS: precaution for MCV4: ACIP removed GBS as a precaution r/t benefits outweigh risk • Immunosuppressed patients: immune response may not be obtained • Menomune A/C/Y/W135 should not be given to pregnant women o Not recommended for children under age 2 • MCV4 (Menactra): approved for use in children 9 months and older and in adults: o not recommended in adults older than 55 y/o • MCV4 (Menveo): not recommended for children younger than 2 y/o or adults older than 55 y/o • HibMenCy: approved for children aged 6 weeks to 18 months o not approved in older children or adults • MPSV (Menomune): approved for adults older than 55 y/o • Both serotype B vaccines (Bexsero, Trumenba): Preg Cat C o Neither approved for children younger than 10 y/o ADRs • Mild: pain and tenderness at injection site for 1 to 2 days Drug Interactions • No known drug interactions Clinical Use and Dosing • The ACIP recommends routine vaccination of young adolescents (11 to 12 y/o) with MCV4 at the preadolescent health care visitor or on entering high school (age 15) o One booster MCV4 at 16 to 18 y/o to adolescents who received the first dose before age 16 o A catch up dose can be administered to those aged 19 to 21 y/o who have not received a dose after their 16th birthday • HibMenCY: infants aged 2 to 18 months with persistent complement deficiencies or asplenia o May also be used for infants 2 to 18 months during an outbreak of meningitis covered by the vaccine • ACIP: these high risk groups should be vaccinated o Patients with deficiencies in late complement components (C3, C5, to C9) o Persons with functional or actual asplenia o Research, industrial, and clinical laboratory personnel who routinely are exposed to N. meningitidis in solutions that may be aerosolized o Travelers to and residents of hyperendemic areas such as sub Saharan African. Epidemics have occurred recently in Saudi Arabia, Kenya, Tanzania, Burundi, and Mongolia o College freshmen living in dorms o Military recruits • HibMenCY: given as a primary series IM at age 2, 4, 6, and 12-15 months. • MCV4: IM single dose with a second dose in 12 weeks in children aged 9 to 23 months and at 8 to 12 weeks in patients aged 2 to 55 y/o • Menomune for all ages is a single SC dose • In patients aged 9 months to 10 years, MCV4 (Menactra) is the preferred vaccine • Adults over age 55 y/o: MPSV • Revaccination: o indicated for persons at high risk for infection (travel or living in epidemic areas) who were previously vaccinated with MPSV or MCV4 o Children vaccinated between age 2 months and 6 y/o should be revaccinated with Menactra in 3 years if they remain at high risk o If previous dose given at age 7 or older: either brand of MCV4 may be given after 5 years o Revaccination with MCV4 of high risk older children and adults is recommended every 5 years after the first dose of MPSV or MCV4 • A booster dose of MCV4 is recommended at age 16 years in children who received their first dose of MCV4 at age 11 to 12 y/o o Adolescents who receive their first dose of MCV4 at age 13 to 15: booster dose at age 16 to 18 y/o o Minimum interval between doses of MCV4 is 8 weeks • Serotype B vaccine: given to 10 to 18 y/o during an outbreak or to those at increased r/f meningococcal disease o Bexero: two does 1 month apart o Trumenba: three doses 1, 2, and 6 months Lyme Disease Vaccine Pharmacodynamics • Vector born illness caused by ticks infested with Borrelia burgdorferi • Recombinant Lyme disease vaccine (LYMErix, Immulyme): imparts immunity against B. burgdorferi by stimulating production of antibodies to the lipoprotein OspA o OspA: lipoprotein of the B. burgdorferi spirochete • MOA: antibody killing of the spirochete in the tick o Transmission of OspA antibody occurs while the tick is feeding on the blood of an immunized host, the antibodies kill the spirochete before transmission occurs • Production was d/c r/t ADRs of the vaccine o Although an FDA investigation did not find the vaccine to be dangerous • Long term immunity for patients previously vaccinated is unknown • New vaccine against B. burgdorferi is in clinical trials in Austria and Germany Typhoid Vaccine The best protection against typhoid fever is food and water precautions to prevent contracting S. Typhi Pharmacodynamics • Typhoid vaccines (Typhoid Vaccine, Typhim Vi) • Used to increase resistance to enteric fever caused by S. typhi o Efficacy of protective immunity depends on the size of the bacterial inoculum consumed • Two parenteral typhoid vaccines available o Heat and phenol inactivated vaccine (Typhoid Vaccine) o Purified Vi polysaccharide (Typhim Vi): used in the United States Pharmacotherapeutics • Hypersensitivity to typhoid vaccine is contraindication • Do not admin to patients w/ acute febrile illness • Preg Cat C: unknown if harmful to the fetus o If vaccination is necessary: inactivated vaccine is recommended • Typhim Vi and Typherix (Canada): not recommended for children under ag e2 ADRs • Local injection site reactions: erythema, induration, and soreness that begin w/in 24 hours and last 1-2 days • Systemic symptoms: low grade fever, HA, and myalgias o High fever is rare Drug Interactions • Plague vaccine should not be given at the same time as typhoid vaccine r/t avoidance of accentuated ARDs • Immunosuppressants: insufficient response to the vaccine Clinical Use and Dosing • Typhoid vaccine is used for primary immunization against S. typhi infection in the following o Travelers to areas where a risk of exposure to S. typhi is recognized o Persons w/ household contact w/ a documented typhoid fever carrier o Lab workers with frequent contact with s. typhi • Typhim Vi and Typherix in children older than age 2 years and adults is 0.5 mL SC o A booster dose should be given every 2 years to patients at continued risk of contracting typhoid Cholera Vaccine • No used in the US • Immunization for travelers not recommended r/t brief and incomplete immunity that the vaccine offers Japanese Encephalitis Virus Vaccine Pharmacodynamics • Japanese encephalitis (JE): most common form of viral encephalitis in Asian and is spread by mosquitoes • Usually severe resulting in death in 20-30% of cases, miscarriage in pregnant women, and serious neuro outcomes in 30 to 50% of those infected • US: inactivated Vero cell culture derived vaccine (JE-VC) or IXIARO Pharmacotherapeutics • Previous anaphylactic reaction to any component of the vaccine, including thimerosal, is a contraindication • Pregnancy is a contraindication to JE-VC use • IXIARO approved for children age 2 to 16 y/o ADRs • IXIARO: same ADRs as placebo or comparison vaccine (PCV7 or HAV) • Injection site tenderness and fever • Report any significant ADRs to VAERS • ADRs typically appear up to 10 days after immunization • Advise patients not to travel outside of the US for 10 days in case of ADRs Drug Interactions • No known drug interactions Clinical Use and Dosing • Prevention is best way to avoid JE o Wear long sleeved shirts and long pants, use repellents, apply permethrin to clothing • ACIP recommends JE-VC for those who plan on residing for more than a month in areas in which JE is endemic or epidemic o Probability of JE infection and illness increases with the duration of stay in rural endemic areas • Obtain information about locations from CDC Yellow Book • JE-VC: not recommended for all travelers to Asia o Those spending a month or longer in endemic areas during transmission season (rural areas especially) o Also, for those who will be spending extensive time outdoors during their travel • JE-VC in adults: two doses 28 days apart • Children aged 2 months to 2 years two doses • Complete at least 1 week before potential exposure to JEV Plague Vaccine Pharmacodynamics • Plague vaccine, a whole cell vaccine consisting of a suspension of inactivated plague bacilli (Yersinia pestis), no longer available in the US • Travelers who may be exposed to plague should carry prophylactic antibiotics (doxycycline, or trimethoprim- sulfamethoxazole for children under 8 y/o) and use them according to the CDC guidelines for plague Rabies Vaccine Pharmacodynamics • Rabies vaccine (Imovax, RabAvert): preparation of inactivated rabies virus that induces active immunity • Two products available differ only in the cell culture used to develop the vaccine o Imovax uses human diploid cell culture o and RabAvert uses purified chick embryo cell culture Pharmacotherapeutics • Previous anaphylactic reaction to any component of the vaccine, including neomycin, is a contraindication • Moderate to severe illness, w/ or w/o fever is reason to defer until patient improved • Immunosuppressed: expected immune response may not be obtained • Pregnancy Cat C: not a contraindication to post exposure vaccination of pregnant women • Safety in children under 6 y/o not established ADRs • Local reactions: pain, erythema, and swelling of the injection site • Systemic reactions: HA, nausea, ABD pain, muscle aches, and dizziness • Three cases of a neuro illness resembling GBS have been reported • Serum sickness like reaction who received booster dose of Imovax Drug Interactions • Long term therapy with chloroquine (Aralen) can interfere w/ the active antibody response • Immunosuppressants or antineoplastic agents: decreased immunological response to the vaccine • Rabies IG (RIG): can partially suppress the antibody response to rabies vaccine • Follow CEC recommendations for simultaneous administration exactly: give no more than the recommended dose of RIG Clinical Use and Dosing • Rabies vaccine can be given for primary or pre exposure vaccination or as part of a post exposure prophylaxis • Pre exposure vaccination is recommended to high risk groups (vets, animal handlers, and certain lab workers) o Three 1 mL IM injections of vaccine in the deltoid o Doses given on day 0, day 7, and either day 21 or 28 o Booster dose of 1 mL every 2 years to those considered at frequent risk of their serum antibody titer is less than 1:5 o High risk groups: vets, animal control officers, wildlife officers, and staff where rabies is enzootic o Ver high risk: research lab workers or vaccine production facilities: a serum rabies antibody test should be done every 6 months and vaccine administered if levels are less than 1:5 • Post-exposure prophylaxis is recommended if the patient has a bite from a rabid animal that penetrates the skin o Post exposure vaccine admin should always be accompanied by use of RIG o Always includes admin of both passive antibody and vaccine with the exception of those who have previously received complete vaccination o ACIP recommendation: four doses of rabies vaccine ▪ 1 mL given IM on days 0, 3, 7, and 14 ▪ And RIG given on day 0 o For those who have previously been vaccinated two doses of rabies vaccine are given on days 0 and 3, with no RIG needed Differentiate between the types of vaccines (live, attenuated, etc.) • Vaccines are divided into two different types: Attenuated or Inactivated • Attenuated (“modified-live”) o Attenuated vaccines include MMR; oral polio (OPV); varicella virus (Varivax, ProQuad); yellow fever (YF-Vax); live, attenuated virus influenza vaccine (Flumist); rotavirus (Rotarix, RotaTeq); varicella zoster (Zostavax); and bacilli Calmette–Guérin (BCG) • Inactivated (“killed”) infective agents o Inactivated vaccines include diphtheria, tetanus, and pertussis (DTP, DTaP, DT, Td, Tdap), H. influenzae type B (HIB), hepatitis A and B, influenza (Fluzone), meningococcal (Menactra, Menomune, Trumenba, Bexsero), inactivated polio vaccine (IPV), human papillomavirus vaccine (Gardasil, Cervarix), pneumococcal polysaccharide (PPV23), and pneumococcal conjugate vaccine (PCV13). Cholera, Japanese encephalitis virus, and plague vaccines are other inactivated vaccines. Typhoid vaccine is available in an inactivated form and an oral live, attenuated form. Immunization types and recommended administration schedule https://www.cdc.gov/vaccines/schedules/index.html Contraindications for each immunization: See above sections PPD administration • Diagnostic biological agent commonly used in primary care • Used to screen asymptomatic individuals for infection w/ M tuberculosis • PPD is administered intradermally to asymptomatic individuals • Once a person has become sensitized to mycobacterial antigens, a hypersensitivity reaction occurs to the administration of the intradermal PPD • In sensitive people, the reaction includes induration and erythema at the site of administration. o A positive reaction to PPD indicates that the person at some time has had a TB infection. o A positive test does not indicate an active infection but rather that further testing is indicated. • PPD testing is safe in pregnancy, during lactation, and in children of all ages, including infants. • The test consists of injecting 5 TU of PPD intradermally. o A small white bleb should appear at the injection site if it is done correctly. o Reactions are read in 48 to 72 hours after administration. o For patients who may be highly sensitized, a test dose of 1 TU is used. • Determining the results of the skin test is based on the likelihood of infection and the risk of active TB if infection has occurred. o If the patient is HIV-positive or has fibrotic lesions on chest x-ray, a reaction of 5 mm or more induration is considered positive. o A reaction of 10 mm or more induration is considered positive in other at-risk patients, including infants and children. o In patients who are not in any high-risk category or high-risk environment, a result of 15 mm or more induration is considered positive. Post-exposure prophylaxis for rabies • Post-exposure prophylaxis is recommended if the patient has a bite from a rabid animal that penetrates the skin o Post exposure vaccine admin should always be accompanied by use of RIG o Always includes admin of both passive antibody and vaccine except for those who have previously received complete vaccination o ACIP recommendation: four doses of rabies vaccine ▪ 1 mL given IM on days 0, 3, 7, and 14 ▪ And RIG given on day 0 o For those who have previously been vaccinated two doses of rabies vaccine are given on days 0 and 3, with no RIG needed Chapter 27: Anemia Differentiate between the types & etiologies of the anemias • Anemia is a sign of disease rather than a disease itself • Diagnosis and Tx of the various forms of anemia entails interpretation of blood studies and peripheral smears to correctly Dx the type of anemia • Underlying pathophysiology in all types of anemia is a decrease in the oxygen-carrying capacity of the blood • Anemias are classified by erythrocyte size and hemoglobin (Hgb) content. • Size is referred to by the terms microcytic (small), macrocytic (large), and normocytic. • Hgb content is referred to by the terms hypochromic (low Hgb) or normochromic. • Regardless of the disease process, the decreased oxygen transport to tissues carries the same results. • A reduction in the number of circulating red blood cells (RBCs) affects the consistency and volume of blood. • Less viscous blood flows faster and more turbulently and may cause ventricular dysfunction, cardiac dilation, and heart valve insufficiency Iron Deficiency Anemia: • IDA decreases oxygen carrying capacity r/t low hemoglobin concentration that is due to reduced RBC production (lack of adequate iron intake, poor absorption of iron by the body, or lead poisoning) or acute or chronic blood loss • This produces a microcytic-hypochromic anemia o Iron is essential for production of Hgb, myoglobin, and other enzymes. o IDA results in problems with oxygen transport that affect the energy metabolism of every cell • Commonly seen in infants, particularly premature infants, in children during rapid growth, and in pregnant and lactating women • After gastrectomy and with malabsorption d/os (particularly small bowel) • Most common cause in adults is blood loss: menstruation, occult blood loss from GI bleeding, and CA o Gastric and duodenal ulcers, diverticula, hemorrhoids, and ulcerative colitis are common sources of this bleeding o GI bleeding is such a common cause of IDA that it is recommended all men and postmenopausal women with IDA and all premenopausal women whose IDA cannot be explained by heavy menses should be evaluated for occult GI bleed • Individuals with RF (especially on dialysis) are at high risk r/t kidneys not secreting enough erythropoietin o Erythropoietin and iron can both be lost in dialysis • IDA develops slowly in three overlapping stages (develops slowly) • Stage 1: the body’s iron stores are depleted, and the patient has iron deficiency w/o anemia o Erythropoiesis proceeds normally with the Hgb content of RBS remaining normal o Few or any symptoms, vague (fatigue) o Dx by measuring serum ferritin (ferritin less than 30 ng/mL indicative of iron deficiency) • Stage 2: Iron deficiency with mild anemia, iron transportation to bone marrow is diminished and iron deficient erythropoiesis takes place o Lab values begin to change o Hgb 9-12, ferritin of less than 20, and iron le\vel less than 60 o Usually no symptoms or vague symptoms of fatigue or HA o Those with lower Hgb may have more definitive symptoms (weakness, SOB) • Stage 3: severe iron deficiency with severe anemia o The small, hemoglobin-deficient cells enter circulation in sufficient numbers and replace normal erythrocytes that have reached maturity and been removed from circulation o RBC lifespan: 120 days o Associated with depleted iron store and diminished Hgb production o Hgb levels are now 6 to 7, ferritin less than 10, and iron less than 40 o Earlobes, palms, and conjunctivae become pale o Nails are brittle, thin, coarsely ridged, and spoon shaped r/t impaired oxygen transport o Tongue becomes red, sore, and painful o Dry, sore skin at the \corners of the mouth and difficulty swallowing r/t decreased salivation o Confusion, memory loss, and disorientation secondary to poor O2 transport to cerebral tissue o Especially problematic in the older adult population o Severe Ida with Hgb below 7: postural hypotension, dizziness, weakness, gastritis, irritability, numbness, and lethargy Folic acid deficiency anemia • (FOA) decreases oxygen-carrying capacity because of a low Hgb concentration • Exogenous folate is required for nucleoprotein synthesis and maintenance of normal erythropoiesis o Folic acid stimulates production of erythrocytes, WBCs, and platelets • Macrocytic-normochromic anemia within 3 months of the start of an inadequate diet, because folate stores are rapidly depleted • Primary function of folate coenzymes is the synthesis of purines and pyrimidines (bases for DNA and RNA) o These coenzymes also involved with the synthesis of thymidylate (precursor of DNA) o Symptoms: become apparent when the synthesis of thymidylate is critically impaired o Apoptosis of RBCs in the late stages of differentiation occurs • Folate is a critical component of the diet of pregnant women and folate supplementation is recommended o r/t neural tube defects and heart disease • Folate is absorbed in the upper small intestine then circulated to the liver for storage • At risk groups: alcoholics (alcohol interferes w/ folate absorption and metabolism), patients w/ malabsorptive d/os and pregnant women o Inadequate dietary intake of green veggies or excessive boiling of veggies while cooking o Impaired absorption r/t ileal disease or phenytoin use, increased demand during pregnancy, hyperthyroidism, hemolytic anemia, or malignancy: impaired utilization for patients taking methotrexate, triamterene, and trimethoprim • Patients commonly c/o glossitis, stomatitis, nausea and anorexia, and diarrhea • Systolic ejection murmur may be heart • Positive Romberg’s sign and increased or decreased deep tendon reflexes • Mild confusion, depression, apathy, and intellectual loss Pernicious anemia (PA) • Also has a low Hgb concentration • Vitamin B12 is necessary for maturation and DNA synthesis in RBCs • When the cause of vitamin B12 deficiency is autoimmune and linked to heredity, it is PA • Associated with other autoimmune conditions, (particularly endocrine) Hashimoto's thyroiditis, type 1 DM, Addison's disease, and Graves’ disease. • Macrocytic-normochromic anemia that develops slowly, often over years, and it is frequently severe before it is diagnosed. • B12 is critical to 2 essential enzyme systems: o Cofactor in metabolism of methyl malonyl CoA: leads to abnormal fatty acids ▪ Responsible for the neurological manifestations of B12 deficiency o Other system involves folate metabolism: final steps in folate metabolism cannot occur ▪ Leads to megaloblastic anemia found in B12 deficiency • Causes: Vit B 12 deficiency: poor intake, impaired absorption, increased demand, or faulty utilization o Poor intake is rare: except in strict vegetarians (no eggs or dairy products) o Poor intake: vegetarians (vegans), Crohn’s disease or others with resection of the bowel (gastric bypass and pregnant women who are strict vegetarians) • Impaired absorption: lack of intrinsic factor excreted from gastric parietal cells o Absorption: impaired by disease of the ileum, bacterial overgrowth from statis (severe constipation), and altered digestive enzymes: gastrectomy • Faulty utilization: rare genetic defects • Symptoms: vague early symptoms (infections, mood swings, and GI, Cardiac, or kidney problems) o Classic symptoms not seen until Hgb approaches 7 to 8 o Neurological symptoms are the result of nerve demyelination: loss of position and vibratory sense, ataxia, and spasticity o Beefy red tongue, peripheral neuropathy o Liver enlargement (older adults especially): indicates right sided heart failure Anemia of Chronic Disease (ACD) • Develops secondary to a chronic disease, Ca, or long term infection and is the second most common form of anemia • ACD is also associated with low Hgb, but it is caused by destruction of RBCs by a hyperactive reticuloendothelial system, decreased production of RBCs by hypoactive bone marrow, or altered iron metabolism, with defective transfer of iron from stores to the plasma. o Appears to be produced by the activation of the cellular immune system • Specific cytokines that have been implicated in ACD include TNF alpha, interferon delta, IL 1 beta, and IL6 o Microvascular eruptions occur in the GI tract in response to the inflammatory mediators o Results in occult blood escaping into the intestines • Normocytic-normochromic anemia: develops slowly often mild or asymptomatic • Anemias that resemble ACD include anemias secondary to malignancy, chronic renal disease, HIV infection, and heart failure Sickle Cell anemia • SCA: normal amount of Hgb but their REBs contain an abnormal type of Hgb: hemoglobin S • Group of autosomal recessive genetic disorders characterized by the predominance of this Hgb. • Includes SCA (homozygous form that is most severe) • Sickle cell thalassemia syndrome and Sickle cell HbC: heterozygous forms in which the child also inherits another type of abnormal Hgb from one parent • Sickle cell trait, in which the child inherits HgbS from one parent and normal hemoglobin (HgbA) from the other parent, is a heterozygous carrier state. o It does not cause abnormalities in the blood count, and it does not produce vaso-occlusive symptoms under physiological conditions • Found in those of African, Mediterranean, Indian, and Middle Eastern heritage • Sickle cell Hgb: produced by a recessive allele of the gene encoding the beta chain of the protein hemoglobin o A single amino acid, glutamic acid, is replaced by valine at the sixth position of the pain • Two cardinal pathophysiological features: chronic hemolytic anemia and vaso-occlusion (results in ischemic tissue injury) • Low oxygen tension in the blood from ischemia or decreased partial pressures of oxygen in the air cause HgbS to crystallize: distorts the RBC into a sickle shape and makes them fragile and easily destroyed • Degree of deoxygenation required to produce sickling varies with the percentage of HgbS in the cells • Sickling is rarely permanent: regain a normal shape when reoxygenated and rehydrated o Some irreversible sickling occurs r/t damage to the plasma membrane of the RBC o Hemolytic anemia may be r/t repeated cycles of sickling and unsickling • Tissue injury is produced by hypoxia secondary to the obstruction of blood vessels by sickled erythrocytes • Sickled cells are unable to squeeze through the smaller blood vessels=tissue ischemia • Organs at greatest risk for damage are those with venous sinuses in which blood flow is low and oxygen tension and pH are low (spleen and bone marrow) • And those with limited terminal arterial blood supply (eye and head of the femur and humerus) • Kidneys are also a risk Relevant diagnostic tests hemoglobin, hematocrit, reticulocyte count, plasma iron, total iron binding capacity, ferritin, transferrin, mean corpuscular volume (MCV), serum B12, and folate Prevention & treatment for the anemias IDA: supplemental iron (ferrous salts should be used: better absorption) • Iron deficiency cannot be overcome with increased dietary intake alone • Adult dose: 150-300 mg//day in two or three divided doses • Premature breastfed neonates: 2 mg iron/kg/day until 12 months old • All breastfed infants: 1 mg/kg/day of iron beginning at 4 months and continued until the infant is consuming adequate iron containing food o Formula-fed infants do not need iron supplementation • Toddlers 1 to 3 y/o: 7 mg/day ideally from iron fortified foods o Check iron level at around 12 months • Infants and young children require 4 to 6 mg/kg/day divided in three doses for severe IDA o and 3 mg/kg/day for mild to moderate IDA • Tx continues for 3 to 4 months after hemoglobin/hematocrit return to normal to correct the anemia and replenish iron stores o Monitoring: reticulocyte count 7 to 10 days after initiation of therapy: first measurable response to therapy o Rise in RBCs 0.5 to 1.5 % o Hgb at 2 weeks: should indicate a rise of 0.1 to 0.2 g/100 mL/day o Normal Hgb: 14-18 in men and 12 to 16 in women reached in 1 to 3 months o Monitoring RBC and Hgb thereafter based on individual risks, response, and symptoms • Primary goal of management for IDA is prevention. o The key to prevention of IDA not due to a disease process is adequate nutrition. o Prevention, for infants, starts with breastfeeding o Children and adults need to eat enough iron-rich foods o Foods rich in iron that the body can readily absorb include raisins, lean meats, fish, poultry, eggs, legumes, soybeans, dark green leafy vegetables, blackstrap molasses, fortified cereals, and whole- grain rice. o The iron in many vegetables is poorly absorbed, so vegetarians must pay special attention to their intake of legumes and rice. o The recommended amount of iron for non-anemic pregnant women is 27 mg/d, with a recommendation that all pregnant women take a low dose (30 mg/d elemental iron) daily to prevent anemia o Learning energy conservation techniques, such as planning rest periods, pacing activities, keeping objects within reach when performing tasks, and sitting down when doing chores, are other important lifestyle modifications for the patient with IDA • Drug Therapy: once the decision is made to begin drug therapy choice of drug is based on age and gender variables o Iron is safe to use in preterm infants, infants, adolescents, adults, during pregnancy and lactation o doses range from 60 to 185 mg of elemental iron o Oral formulation of 325 mg (60 mg of elemental iron) TID with meals o Ferrous sulfate is the least expensive and the most easily absorbed o Slow release and EC compounds help decrease GI ADRs with only once/day dosing Folic Acid Deficiency • Eat food high ion folic acid: dark green leafy veggies, bran, yeast dried beans, fortified cereals, and nuts • For all females planning or capable of becoming pregnant: .4 to .8 mg/day • Well absorbed, doses of 1 to 2 mg/day result in correction of the deficiency in 4 to 5 weeks • Hgb levels begin to rise within the first week and complete correction in 1 to 2 months • When clinical symptoms have subsided, and labs normalized: maintenance doses 0.1 mg/day for infants to 0.8 mg/day for pregnant and lactating patients • Prevention: supplementation during pregnancy and lactation Pernicious Anemia • Eat foods high in B12: mollusks, fortified breakfast cereals, liver, trout, salmon, milk, and eggs • Prevention: 2.2 mcg/day during pregnancy • 2.6 mcg/day during lactation, 0.3 to 0.5 mcg/day for infants under age 1 • 0.7 to 1.4 mcg/day for children 1 to 10 • Pernicious Anemia: Malabsorption: therapy for life • Initial 1,000 mcg/day for 7 days: IM or deep SC • Response to injected B12 is rapid: reticulocytosis begins on the second or third day and maximal 5-10 days • If clinical improvement and appropriate reticulocyte response after 7 days: then 100 to 1,000 mcg IM weekly for a month • Hgb and Hct levels should return to normal within 1 to 2 months: may take up to 6 months for neurological symptoms to resolve • If neuro symptoms are present twice monthly dose is recommended for 6 months prior to beginning the monthly dose • B12 once monthly for life • Referral to or consultation with a hematologist and gastroenterologist should occur w/ Dx of PA Anemia of Chronic Disease • Most common form of anemia in older adults and associated with several specific chronic diseases including osteomyelitis, TB, Ra, hepatitis, carcinoma, myeloma, lymphoma, and leukemia, CRF • There is no effective therapy directed specifically at ACD o Tx of the underlying chronic disease is necessary to resolve the anemia • Can exist with IDA: Tx with iron • Energy conservation is important • When caused by CRF: decreased production of erythropoietin o Sufficient iron needed o Admin epoetin alfa (Epogen, Procrit) may increase Hct w/in 6 weeks • For CRF or zidovudine-treated HIV: epoetin alpha three times a week o Titrated to keep Hgb between 10 and 12 Sickle Cell Anemia • Prevention is focused on avoidance of precipitants of sickling crisis o Serious bacterial infections ▪ (S. pneumoniae, H. influenzae, and M. pneumoniae are major causes of sickling ▪ Teach early s/s of infections and early aggressive Tx is critical o Dehydration: adequate hydration especially during elevated temperature and physical activity o Exposure to cold: vasoconstriction, avoid • Children should receive all childhood immunizations: including pneumococcal vaccine o Infants are high risk and vaccinated with meningococcal vaccine and persons age 9 months to 55 are vaccinated o Annual flu vaccine starting at 6 months • Encourage patients to exercise: non-strenuous • Drug therapy • Daily MVI, diet rich in complex B vitamins and vitamin C, maintain hydration • 1 mg/day of folic acid during crisis • Infections: increase r/f vaso-occlusive events and subsequent ischemia o Oral PCN BK 125 mg bid until 3 y/o then 250 mg big until 5 • NIH: strong evidence for the use of hydroxyurea in the Tx of SCD in adults o No drug to cure SCD o Hydroxyurea: reduces frequency of sickle cell pain crisis in adults, reduced need for transfusion, and increase total hemoglobin and HgbF o Usually managed by a specialist in hematology o Toxicity can occur: absolute neutrophil counts lower than 2,000, absolute reticulocyte counts lower than 80,000, and platelet s lower than 80,000, or a fall in Hgb from 7 to 4.5-5 o ARF cytopenia: leukopenia and thrombocytopenia may occur w/in 10 days of starting therapy o WBC and platelet: monitor prior to and periodically during therapy o ADRs: stomatitis, anorexia, nausea, vomiting, and diarrhea may occur o Good oral hygiene and monitoring of nutritional status o Do not handle the hydroxyurea tablet w/ bare hands, wear gloves • Transfusions: With the mild to moderate anemia common to SCD, body systems except the eye and spleen adapt well to the reduced oxygen carrying capacity of the blood o Most SCD patients are relatively asymptomatic: do not require transfusions o Transfusions may be used for specific indications when anemia is severe or to prevent chronic complications Monitoring and outcome evaluation IDA • Monitoring: o Response to iron therapy is apparent within 10 days of initiation o First change noted in blood values is an increase in reticulocyte count as soon as 4 days after Tx is started, followed by a rise in Hgb of 1 to 2 g/dL/day o If the anemia is ever (Hgb less than 8): reticulocyte count obtained 5 to 10 days after starting therapy o If the anemia is not severe Hgb Hct, and ferritin checked a t 4 weeks o If mild: (Hgb 10 -12 and Hct 30-60%) follow up every 4 to 6 months o Referral is almost never required unless there is an inadequate response to therapy, there is a question of possible malabsorption that requires a GI specialist or the reason for inadequate response is unclear • Outcome evaluation: o Several weeks of therapy are required o Replenishing iron stores may take months o Speed is not the issue: unless there is rapid blood loss o In that case: consultation or referral o Hgb, Hct, and RBC at 4 weeks, 3 months, and annually o If Hgb does not return to normal w/in 6 weeks; evaluate for inadequate response o If dose is inadequate: increase dose Folic Acid Deficiency Anemia • Monitoring o Response to Tx is assessed after 2 weeks and then monthly until the condition stabilizes o A rapid rise in reticulocytes follows the initial Tx with a peak in 5 to 8 days, an improving Hgb and Hct within 1 week, and a normal Hct within 2 months o Only monitoring required: Hgb and Hct levels at regular intervals Pernicious Anemia (PA) • Monitoring: o Reticulocyte counts, Hgb, Hct, iron, folic acid, and B12 prior to Tx, between the 5th and 7th day of therapy and then frequently until Hgb and Hct are normal o Relapse of symptoms is not uncommon in the presence of continuing therapy o Blood counts at regular intervals throughout the patient’s lifetime (based on response to therapy) o Potassium levels: monitor at the same time as Hgb and Hct o LFTs should also be done (AST and ALT) ▪ If AST and ALT are elevated before the start of cobalamin therapy: evaluate every 2 to 4 weeks (monitor for liver dysfunction) ▪ If LFTs elevate after the start of therapy, more frequent testing might be required to assess for hepatotoxicity ▪ Schilling test: used for Dx but not as a monitoring tool o Consult with hematology and GI doc Sickle Cell Anemia • Hgb, Hct, reticulocyte counts, platelet counts, and WBC frequently during the first year of life to establish baseline • After the first year: Hgb and Hct only once or twice a year in stable patients • UA, BUN, crt, and liver enzyme studies to monitor for evidence of organ damage • Prior to transfusion: RBC antigens are needed, often difficult to crossmatch • Most adults with SCD should have regular medical evaluations every 3 to 6 months • Blood counts, UA, and routine chemistry done annually • With advancing age, complications such as chronic organ failure often require more frequent visits and more extensive labs • Focus on abnormalities in renal function and complications such as gallstones, aseptic necrosis, leg ulcers, and priapism • Goal of therapy: reduction in the number of sickling crises and prevention of organ damage • Hgb goal: 9 or greater but levels of at least 7 may be acceptable in asymptomatic patients • Goal for percentage of Hgb S: 30% or less Recommended amount of iron supplementation for breastfed infants • All breastfed infants 1 mg/kg/day of iron beginning at 4 months and continued until the infant is consuming adequate iron containing food • Formula-fed infants do not need iron supplementation Medication to reduce the number of acute sick cell crisis events: • Drug therapy • Infections: increase r/f vaso-occlusive events and subsequent ischemia o Oral PCN VK 125 mg bid until 3 y/o then 250 mg big until 5 y/o • NIH: strong evidence for the use of hydroxyurea in the Tx of SCD in adults o No drug to cure SCD o Hydroxyurea: reduces frequency of sickle cell pain crisis in adults, reduced need for transfusion, and increase total hemoglobin and HgbF o Usually managed by a specialist in hematology o Toxicity can occur: absolute neutrophil counts lower than 2,000, absolute reticulocyte counts lower than 80,000, and platelet s lower than 80,000, or a fall in Hgb from 7 to 4.5-5 o ARF cytopenia: leukopenia and thrombocytopenia may occur w/in 10 days of starting therapy o WBC and platelet: monitor prior to and periodically during therapy o ADRs: stomatitis, anorexia, nausea, vomiting, and diarrhea may occur o Good oral hygiene and monitoring of nutritional status o Do not handle the hydroxyurea tablet w/ bare hands, wear gloves Vitamin deficiency and risk for neural tube defects during pregnancy • Impaired thymidylate synthesis is thought to be the mechanism behind neural tube defects in the offspring of pregnant women with folic acid deficiency • Evidence suggests that maternal folic acid deficiency is associated with increased risk for neural tube defects in the fetus. • Folate deficiency is more common than vitamin B12 deficiency and often associated with alcoholics, chronic malnutrition, fad diets, and diets low in vegetables Folate requirements during pregnancy • 0.4 mg prior to conception and throughout pregnancy • Pregnant women have increased folate requirements (800 μg daily versus 50 to 100 μg per day) • Folate deficiency is more common than vitamin B12 deficiency and often associated with alcoholics, chronic malnutrition, fad diets, and diets low in vegetables Treatment for anemia of chronic disease: see above section: Tx of chronic disease/underlying cause sometimes iron is IDA and ACD happen together Chapter 37: HIV & Aids • Know the pharmacodynamics, pharmacotherapeutics clinical use, drug interactions and adverse drug reactions for: Antiretroviral medications • Antiretroviral therapy (ART) • ART can increase the number of circulating CD4 T cells: prolonged survival and diminished rate of opportunistic infections • Six classes: nucleoside reverse transcriptase inhibitors (NRTIs or nukes), nonnucleoside reverse transcriptase inhibitors (NNRTIs or non-nukes) protease inhibitors (PIs), fusion inhibitors (FI or entry inhibitors), integrase strand transfer inhibitors (INSTIs), and CCR5 antagonists o Each class inhibits replication in a different way Nucleoside reverse transcriptase inhibitors (NRTIs or nukes) • NRTI Drugs: abacavir, Didanosine, emtricitabine, lamivudine, stavudine, and zidovudine • NtRTI drugs (nucleotide): tenofovir • MOA: inhibition of replication of retroviruses by interfering w/ viral RNA-directed DNA polymerase (reverse transcriptase) o Require phosphorylation to become active in the body thus NtRTI are already chemically activated • Pharmacotherapeutics: eliminated via kidneys: require renal adjustment when CCR is less than 50 mL/min o Abacavir: eliminated by mechanism in the liver: does not require renal adjustment, half life is increased in mild hepatic impairment and must be dose adjust for Child-Pugh class A and contraindicated for classes B and C • ADRs: anemia, bone marrow suppression, flatulence, HA, myopathy, nausea, rash, renal issues, and vomiting o Symptomatic and life threatening lactic acidosis may occur: more common in patients with hepatomegaly and hepatic steatosis o Abacavir is contraindication in HLA B^5701 positive patients: genetic screening required hypersensitivity reaction can be fatal o Didanosine and stavudine: peripheral neuropathy and pancreatitis o Tenofovir: variety of ADRs, decreased bone mineral density, increased biochemical markers of bone metabolism, ARF, acute tubular necrosis, decreased urine volume, Fanconi syndrome, renal impairment, increased crt, interstitial nephritis, nephritis, nephrogenic DI, new onset or worsening renal, proximal renal tubulopathy, RF, and renal insufficiency Nonnucleoside reverse transcriptase inhibitors (NNRTIs or non-nukes) • Drugs: delavirdine, efavirenz, etravirine, nevirapine, and rilpivirine • MOA: Inhibit replication by acting as a specific, noncompetitive, reverse transcriptase inhibitor and disrupting the catalytic site of the enzyme o Attach themselves to reverse transcriptase and prevent the enzyme from converting RNA to DNA: results in HIV genetic material cannot be incorporated into host cell • Kinetics: metabolized in liver by CYP450 system o More prone to clinically significant drug interactions when combined with other ARTs o Interact with other concurrent medications and complementary/alternative medicines (inducers or inhibitors) o Follow guidelines • ADRs: difficulty sleeping, dizziness, drowsiness, fatigue, HA, liver problems (can be severe and life threatening), NVD, rash (can be severe), and vivid dreams Protease inhibitors (PIs) • Drugs: atazanavir, fosamprenavir, indinavir, lopinavir/ritonavir, nelfinavir, ritonavir, saquinavir, and tipranavir • MOA: Selective and competitive inhibitors of HIV protease o Plan an essential role in preventing cleavage of protein precursors essential for maturation, infection of new cells, and replication • Kinetics: Metabolized by CYP450 system: inducers and inhibitors o Ritonavir: very potent CYP450 inhibitor of other PIs (except nelfinavir) ▪ Commonly paired in low doses to intensify the half life of other PIs (ritonavir boosting) o Drug interactions with boosted and non-boosted PIs must be considered when devising an effective ART regimen o Do not require renal dosing adjustment • ADRs: bleeding problem, diarrhea, GI disturbance, hyperglycemia, HLD, lipodystrophy, and liver problem that can be severe Fusion inhibitors (FI or entry inhibitors) • Drugs: enfuvirtide • MOA: work by blocking an important step in the process of entry into CD4 cells known as fusion o By blocking fusion, FIs may prevent HIV from entering and infecting CD4 cells o Target gp120 and gp41 proteins • ADRs: skin itchiness, swelling, and pain at the injection site o Dizziness, fatigue, insomnia, and numbness in feet or legs Integrase strand transfer inhibitors (INSTIs) • Drugs: raltegravir and cobicistat-boosted elvitegravir • MOA: work by blocking the integrase enzyme that HIV needs to make more virus: blocks the virus ability to replicate • Therapeutics: Use with caution when administer with strong inducers of uridine diphosphate glucuronosyltransferase (RIF) o Reduce plasma concentrations of raltegravir • ADRs: raltegravir: CK elevations, diarrhea, HA, myopathy, nausea, pyrexia, and rhabdomyolysis o Elvitegravir: nausea and diarrhea, URI and bronchitis, back and joint pain, and UTI o Cobicistat: GIADRS: NVD, may exacerbate kidney impairment CCR5 antagonists • Drugs: Maraviroc • MOA: Work by blocking a molecule called CCR5 that is found on the surface of CD4 cells so HIV cannot enter • Kinetics: modulated by inhibitors and inducers of CYP3A/Pgp o Inhibitors: (ketoconazole, lopinavir/ritonavir, ritonavir, darunavir/ritonavir, saquinavir/ritonavir, and atazanavir) o Inducers: RIF, etravirine, and efavirenz o ADRs: cough, dizziness, pyrexia, rash, and URI, diarrhea, edema, esophageal candidiasis, flu, parasomnias, rhinitis, sleep d/os, and urinary abnormalities Goals of therapy • The goals of treatment with ART medication are o (Box 37-1) HIV Tx goals: Improve QOL, obtain maximal and durable suppression of HIV, prevent vertical HIV transmission, prolong survival, reduce HIV-related morbidity, reduce transmissibility of HIB, and restore and preserve immunological function • The most important goals are to (1) reduce HIV-associated morbidity and prolong the duration and quality of survival, (2) restore and preserve immunological function, (3) achieve maximal and durable suppression of plasma HIV viral load, (4) and prevent HIV transmission. • These goals are achieved by reducing HIV-related morbidity and mortality, improving quality of life, and restoring and preserving immunological function in persons infected with HIV • Complete eradication is not possible r/t latently infected CD4 T cells that are established during the earliest stages of acute HIV infection o persist with a long half-life despite prolonged suppression of HIV plasma viremia • Follow approved Tx guidelines and strategies: substantial reductions in HIV related morbidity and mortality and reduced vertical transmission • Higher viral loads are associated with more rapid disease progression o Other factors: heightened T cell activation w/ cellular turnover and expression of immune activation markers, probably contribute as well to clinical disease progression and the rate of Cd4 T cell decline • Goal of maximal viral suppression with ART may be difficult w/ pre-existing medication resistance o In 2007, About one of every six new HIV cases involved virus with ART drug resistant mutations • To successful, ART regimens need to contain at least two, and preferably three, active medicines from multiple medication classes. • If maximal initial suppression below the level of HIV detection (less than 50 copies/mL) is not achieved or is lost, it is important to change medication regimens to include at least two active medicines to achieve the maximal suppression goal • To achieve Tx goals, clinicians and patients must work together to define priorities, investigate options, and mutually determine the best Tx plan Treatment in special populations (pregnancy, children) • Dosing principles should be applied to HIV-infected children, adolescents, and adults. • The treatment of HIV-infected children involves unique pharmacological, virological, and immunological considerations • Women should receive optimal ART even if they are pregnant. • ART of the pregnant woman with zidovudine alone or with standard three-drug combinations has dramatically reduced the rates of vertical transmission from mother to child • Treatment of acute HIV infection should be considered optional at this time. Pretesting treatment • CD4 T-cell count • Pretreatment HIV genotypic resistance testing should be considering in selecting the best ART regimen Predictors of success • Predictors of ART Virological Success (Box 37-2) o High level patient adherence to ART regimen o High potency of antiretroviral medication regimen o Higher baseline CD4 T cell count o Low baseline HIB plasma viral RNA level o Rapid (i.e., equal to or greater than 1 log 10 in 1 to 4 months) reduction of viral RNA level in response to ART Phenotype assays • Phenotype assays are used to measure sensitivity to various antiretroviral agents. • The assay reports HIV sensitivity in terms of a ratio above the normal or wild-type IC50. • In other words, it is the half-maximal (50%) inhibitory concentration (IC) of a medicine (50% IC, or IC50). This information allows a provider to determine the relative extent of resistance. [Show More]
Last updated: 1 year ago
Preview 1 out of 87 pages
Reviews( 0 )
Document information
Connected school, study & course
About the document
Uploaded On
Mar 06, 2022
Number of pages
87
Written in
Additional information
This document has been written for:
Uploaded
Mar 06, 2022
Downloads
0
Views
43

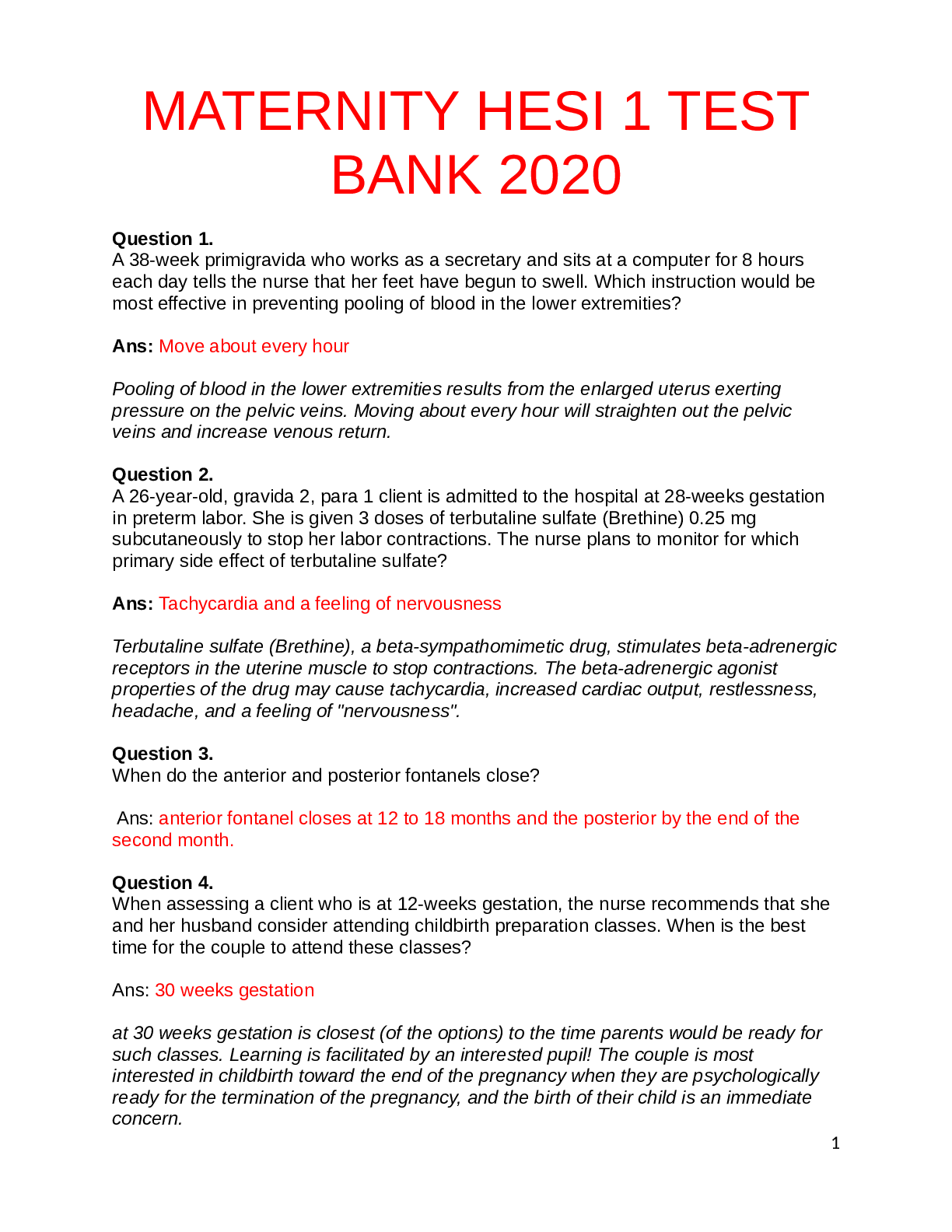
.png)