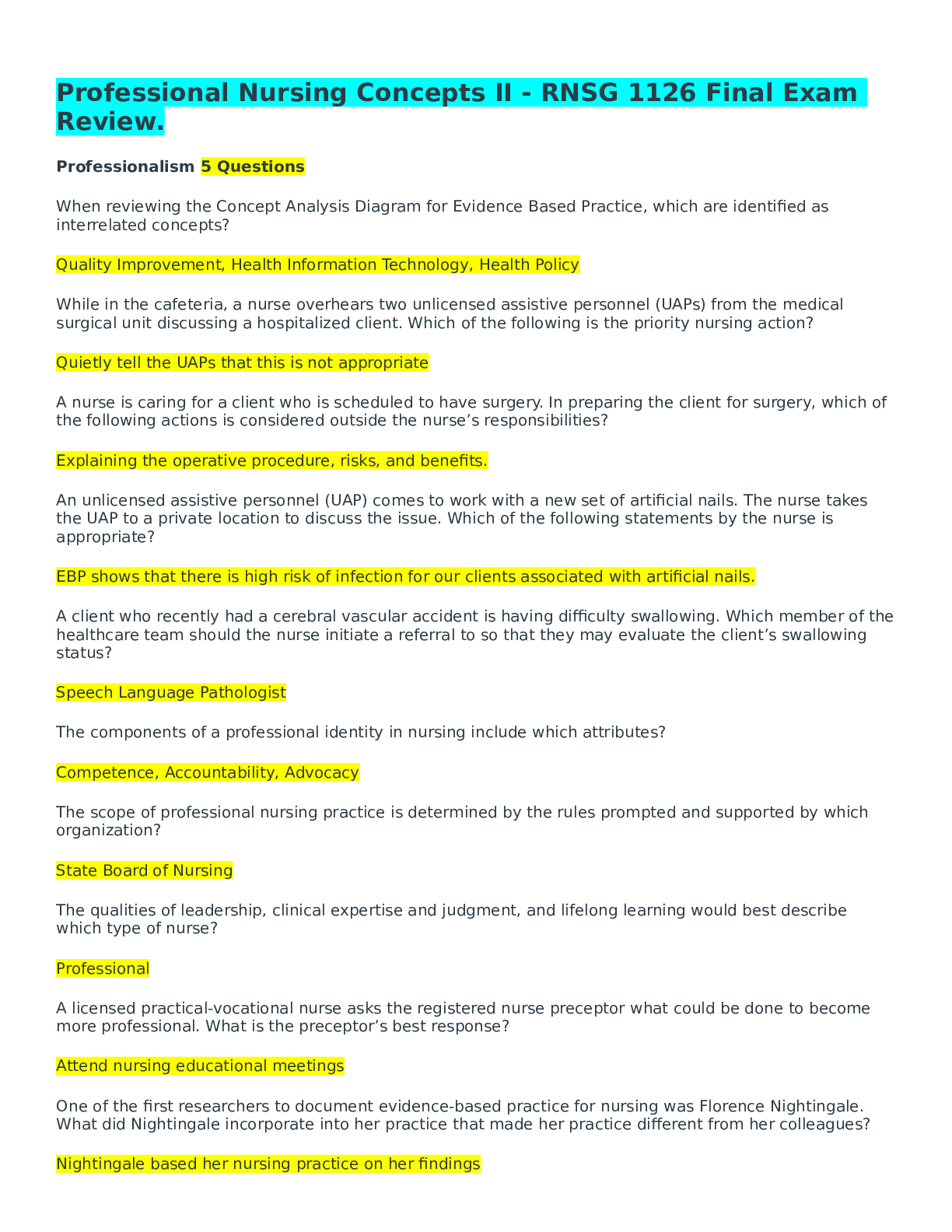
*NURSING > EXAM REVIEW > Chamberlain College: NR566 weeks 1-3 midterm review questions_ LATEST,100% CORRECT (All)
Chamberlain College: NR566 weeks 1-3 midterm review questions_ LATEST,100% CORRECT
Document Content and Description Below
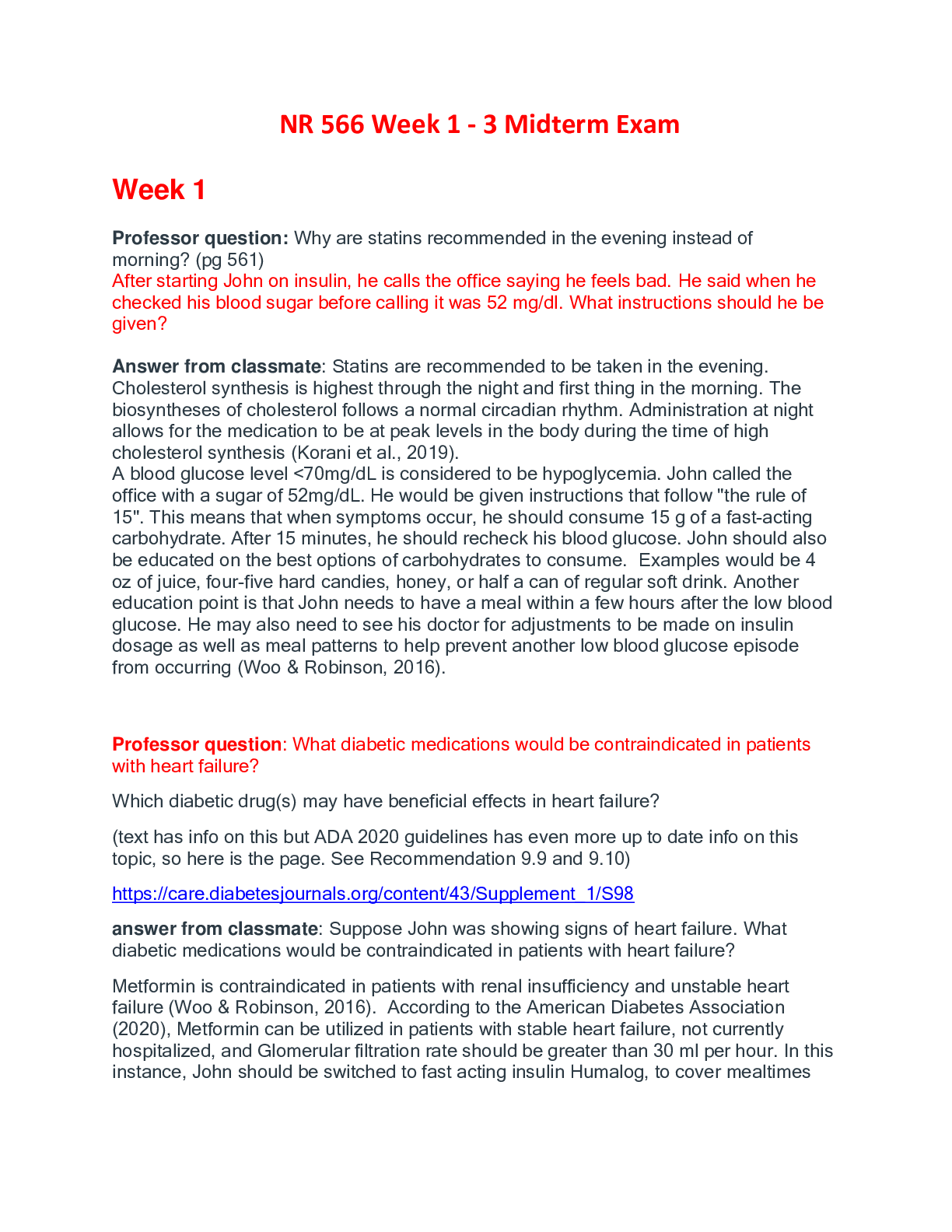
Chamberlain College: NR566 weeks 1-3 midterm review questions_ LATEST Week 1 Professor question: Why are statins recommended in the evening instead of morning? (pg 561) After starting John on ins... ulin, he calls the office saying he feels bad. He said when he checked his blood sugar before calling it was 52 mg/dl. What instructions should he be given? Answer from classmate: Statins are recommended to be taken in the evening. Cholesterol synthesis is highest through the night and first thing in the morning. The biosyntheses of cholesterol follows a normal circadian rhythm. Administration at night allows for the medication to be at peak levels in the body during the time of high cholesterol synthesis (Korani et al., 2019). A blood glucose level <70mg/dL is considered to be hypoglycemia. John called the office with a sugar of 52mg/dL. He would be given instructions that follow "the rule of 15". This means that when symptoms occur, he should consume 15 g of a fast-acting carbohydrate. After 15 minutes, he should recheck his blood glucose. John should also be educated on the best options of carbohydrates to consume. Examples would be 4 oz of juice, four-five hard candies, honey, or half a can of regular soft drink. Another education point is that John needs to have a meal within a few hours after the low blood glucose. He may also need to see his doctor for adjustments to be made on insulin dosage as well as meal patterns to help prevent another low blood glucose episode from occurring (Woo & Robinson, 2016). Professor question: What diabetic medications would be contraindicated in patients with heart failure? Which diabetic drug(s) may have beneficial effects in heart failure? (text has info on this but ADA 2020 guidelines has even more up to date info on this topic, so here is the page. See Recommendation 9.9 and 9.10) answer from classmate: Suppose John was showing signs of heart failure. What diabetic medications would be contraindicated in patients with heart failure? Metformin is contraindicated in patients with renal insufficiency and unstable heart failure (Woo & Robinson, 2016). According to the American Diabetes Association (2020), Metformin can be utilized in patients with stable heart failure, not currently hospitalized, and Glomerular filtration rate should be greater than 30 ml per hour. In this instance, John should be switched to fast acting insulin Humalog, to cover mealtimes and if his HgbA1C is not sufficiently controlled at the 3 month follow up then, long acting Lantus insulin should be added to the regime. Additionally, John should be placed on an Angiotensin Converting Enzyme inhibitor or Angiotensin Receptor Blocker and likely increase his atorvastatin to 20mg tablet (ADA, 2020). Which diabetic drug(s) may have beneficial effects in heart failure? With the scenario presented previously and with the addition of heart failure, John should be placed on either a sodium-glucose cotransporter 2 inhibitor (SGLTi) or a glucagon-like peptide 1 receptor agonist (GLP-1 RA) to improve glycemic management (ADA, 2020a). Both SGLT2i and GLP-1 RA have demonstrated cardiovascular disease benefits by reducing CVD events and HF hospitalizations in association with diabetes mellitus (ADA, 2020b). The differential in which medication to use for John would be based on his Glomerular Filtration Rate (GFR), decreasing GFR rates or worsening chronic kidney disease would indicate stoppage of SGLT2i and use of GLP-1 RA. Per the American Diabetes Association (2020), John with mild HF would be initially placed on a GLP 1- RA Liraglutide (Victoza). Victoza is a once daily injection that aids in treating T2DM by increasing insulin synthesis and release, decreasing amount of glucagon and gastric emptying, and reducing food intake (Woo & Robinson, 2016). Additionally, placing John on a GLP-1 RA would help decrease his obesity with its proven beneficial tendency to increase metabolism and improve weight loss (Woo & Robinson, 2016). Professor question: What lab do we need to check prior to starting metformin? (hint: which organ function needs to be evaluated?) What other potential adverse effects are there associated with metformin? (Micromedex in the library is a good source for this info) Answer: The most important lab is eGFR/renal function since this determines whether we can safely use metformin. See recommendations below. I also included information on contrast administration. The concern is that if dye impairs renal function, the risk of lactic acidosis is increased. Another potential adverse effect is B12 deficiency. "Clinical recommendations based upon the patient’s renal function • Before initiating therapy, obtain an eGFR • Initiation of therapy is not recommended in patients with eGFR between 30 –45 mL/minute/1.73 m² • Obtain an eGFR at least annually in all patients receiving therapy • In patients at increased risk for development of renal impairment (e.g., the elderly), renal function should be assessed more frequently • If eGFR later falls below 45 mL/minute/1.73 m², assess benefit and risk of continuing therapy Iodinated contrast imaging procedures • Discontinue metformin at the time of or before an iodinated contrast imaging procedure in patients with an eGFR between 30-60 mL/minute/1.73 m²; in patients with a history of liver disease, alcoholism, or heart failure; or in patients who will be administered intra-arterial iodinate contrast • Reevaluate eGFR 48 hr after the imaging procedure; restart metformin if renal function is stable" Professor question: The GLP1RA class drugs end with "-tide". They are highly recommended as a second agent after metformin by both ADA and AACE/ACE guidelines. Per ADA guidelines: • 9.9 Among patients with type 2 diabetes who have established atherosclerotic cardiovascular disease or indicators of high risk, established kidney disease, or heart failure, a sodium–glucose cotransporter 2 inhibitor or glucagon-like peptide 1 receptor agonist with demonstrated cardiovascular disease benefit is recommended as part of the glucose-lowering regimen independent of A1C and in consideration of patient-specific factors A • 9.10 In patients with type 2 diabetes who need greater glucose lowering than can be obtained with oral agents, glucagon-like peptide 1 receptor agonists are preferred to insulin when possible. B Unfortunately these agents are very expensive, from about $700-1,200/month which will make them unaffordable for many patients if insurance does not cover the cost. It is such a shame that cost factors into prescribing! according to the text, what effect does carbamazepine have on thyroid function tests? What is the difference b/w total and free T4? P 1181 Table 41-1 Answer from classmate: According to the text, carbamazepine decreases the serum concentration of thyroid hormones. It is proposed that carbamazepine increases the extra-thyroidal metabolism of thyroid hormones (Woo & Robinson, 2016). Total T4 measures the bound and free thyroid hormone and can change when binding proteins differ. Free T4 measure what is not bound and able to enter and affect the body tissues. The normal range for Free T4 is 0.7-1,86 ng.dL (9-24 pmol/L) In hypothyroidism, you would expect the Free T4 to be low whereas in hyperthyroidism, you would expect the Free T4 to be high. Professor question: Can you review in our text the sulfonylurea class? What is the MOA, what are some examples? What are the adverse effects? Thanks!! Answer from classmate: According to the text, the sulfonylurea class was the first class of oral drugs developed to help manage blood glucose levels in patients with type 2 diabetes mellitus. This class of drug has shown to be similarly effective as metformin and have the ability to reduce HbA1c levels by about 1,5%(Woo & Robinson, 2016). This class of drug’s mechanism of action is the increase the secretion of insulin via the stimulation of beta cells of the pancreas (Costello & Shivkumar, 2020) thus it is important that the patient is still able to produce some endogenous insulin. The drugs improve the binding between the insulin and the insulin receptors thus improve the utilization of the insulin to a certain extent (Woo & Robinson, 2016). These drugs may also enhance the effect of the diuretic hormone and have a slight diuresis effect. Sulfonylureas are recommended as a co-therapy, the drug is not as effective as a monotherapy since it is unable to sustain glycemic targets over time(Woo & Robinson, 2016). Some examples of sulfonylurea drugs are: Chlorpropamide, Tolazamide, Glipizide, and Glimepiride Professor question: If our patient had HF and Afib, he might be on digoxin. What medication for DM can decrease digoxin levels? (class and examples) Pg 579 Classmate answer: Acarbose and miglitol decrease digoxin levels when given together. Acarbose and Miglitol are oral antihyperglycemic drugs that treat type II diabetes and are classified as alpha-glucosidase inhibitors. These drugs competitively inhibit the absorption of complex carbohydrate from the small intestines. This result in delayed digestion of carbohydrates causing flatulence. Alpha-glucosidase inhibitors lower blood glucose after meals. Since this class of drugs reduce digoxin concentrations thus reduce effect, it is recommended to choose another antihyperglycemic drug that does not interact with digoxin. These drugs are gives as an adjunct with other therapy for type II diabetes. The most common adverse reactions are GI disturbances but these side effects cab be reduces if the dose is titrated slowly. Professor question: Jason- glad you recognized that contrast dye can be an issue for patients on metformin. Can you read this (older, I know) article that explains why it is a concern rather than binding with contrast dye? Classmate answer: Wow, I am glad you brought that to my attention. I work in the emergency room and have heard radiology give the speech over and over. It usually goes something like "don't take your glucophage for 48 hours because it binds with the dye and makes it harder to pass" and they hand them a piece of paper that tells them when to start taking it again. Now I know this is not the case. In the emergency room we check the patient's kidney function prior to giving the contrast. We have an acceptable range for non diabetic patients and a range for diabetic patients. On occasion we give IV contrast to patients with poor kidney function with the understanding that they will have dialysis afterwards. "There is controversy about the causal relationship between exposure to IV CM and PC-AKI" (Van der Molen et. al, 2018). In the ER setting there is no follow up to check kidney function post IV contrast. It has been mentioned that the patient can start their glucophage after 48 hours as long as kidney function remains acceptable but this seems like a step that is skipped. Making sure the patient is hydrated seems to be emphasized more, either through PO or IV routes. This will help maintain proper kidney function after receiving IV contrast. Professor question: Can you review for us what the ADA criteria for diagnosis of T2DM are? Classmate answer: The ADA diagnoses T2DM based on several criteria. The patient may have a fasting glucose of 126mg/dL (7.0 mmol/L) or higher. A 2-hour plasma glucose level of 200 mg/dL (11.1 mmol/L) or higher in the midst of a 75-g oral glucose clearance test. Also, a random plasma glucose of 200mg/dL (11.1 mmol/L) or higher with a patient that is also displaying signs of hyperglycemia or that they maybe in a hyperglycemic crisis. And lastly, the patient has a hemoglobin A1c level of 6.5% (48 mmol/dL) or higher (ADA, 2020). Professor question: If John’s A1C remains elevated and he does not have any indicators or at high-risk for ASCVD, CKD, or HF, a thiazolidinedione (TZD) could be prescribed (American Diabetes Association, 2020). How do thiazolidinediones help control blood sugar? Why is it important that there is little to no risk indicators for cardiovascular involvement when prescribing TZDs? pg 581-2 Classmate answer: Pioglitazone (Actos) and rosiglitazone (Avandia) are the two thiazolidinedione (TZD) that are available in the United States. TZD’s help by improving insulin sensitivity. The presence of insulin is needed for TZD’s to work which makes them ideal in the management of Type II Diabetics. TZD’s act on the peroxisome proliferator-activated receptor gamma. This receptor helps regulate gene transcription resulting in expression of proteins that improve insulin action in the cell. This mechanism of action provides an increased utilization of available insulin by the liver and muscle cells as well as that in adipose tissue (Micromedex, 2020). TZD’s prescription use is contraindicated in patients with NYHA class III or IV heart failure. Initiating or increasing dose of TZD’s requires the observation of any possible signs of heart failure. Heart failure signs and symptoms can include, rapid weight gain, dyspnea, and edema (Teri Moser Woo Phd Aprn Cnl Cpnp-pc Faanp et al., 2015, p. 581). Professor question: One class of diabetic drugs sometimes used is meglitinides. What is an important teaching point about this drug for patients to make sure the drug is most effective? pg 585 table 21-22 classmate answer: Hello Professor and class, what I gather from the readings is that Meglitinides may be given in conjunction with Metformin. Research states that Meglitinides should be given within 15 to 30 minutes before eating. I the patient is not going to eat, then this medication should not be taken. Also, this medication is not to replace any current medications. The patient also needs to monitor glucose regularly (Pakkir, 2018). Professor question: What side effects are most common for GLP-1 receptor agonists? What diseases would be contraindicated to have with the administration of GLP-1 receptor agonists? pg596 classmate answer: Glucagon-like peptide 1 receptor agonists (GLP-1RAs) are beneficial in the treatment of type 2 diabetes due to their glucose-lowering effects. Examples of GLP-1RAs are lixisenatide, liraglutide, exenatide, semaglutide, and dulaglutide. However, GLP-1RAs may cause side effects with some being serious. Common side effects include nausea, diarrhea, vomiting, headaches, mild tachycardia, headaches, dizziness, and dyspepsia (Collins & Costello, 2020). Rare side effects such as the development of pancreatitis and thyroid C-cell tumors have also been reported (Hinnen, 2017). Close monitoring is thus necessary to prevent the development of adverse effects. Owing to such side effects, healthcare professionals should consider certain contraindications when selecting GLP-1RAs. Notably, some animal studies have shown thyroid C-cell hyperplasia, medullary thyroid carcinomas, and adenomas with the use of some GLP-1RAs such as liraglutide in mice (Hinnen, 2017; Collins & Costello, 2020). As such, GLP-1RAs are contraindicated in individuals with a family or personal history of medullary thyroid carcinoma as well as among those with multiple endocrine neoplasia syndrome type 2 (Hinnen, 2017). GLP-1RAs should also be used with caution in those with severe gastroesophageal reflux disease, inflammatory bowel disease, and gastroparesis (Hinnen, 2017). The medication is also contraindicated in cases of hypersensitivity and pregnancy (Collins & Costello, 2020). Discontinuation of GLP-1RA therapy is, therefore, necessary if patients receiving this medication develop the contraindicated diseases or conditions. Professor question: If John is started on insulin and he still struggles to meet A1C goals, a sodium–glucose cotransporter 2 (SGLT2) inhibitor to insulin therapy has shown the ability to improve A1C levels while also aiding in decreasing body weight when compared with insulin therapy alone (American Diabetic Association, 2020). How do SFLT2 drugs work and what are some examples of drugs in that class? Pg 589 Classmate answer: Sodium-glucose cotransporter-2 inhibitors also referred to as SGLT- 2 inhibitors or gliflozins work through a mechanism of action that prevents SGLT2 in the kidney from reabsorbing glucose from the glomerular filtrate for its return back to the plasma resulting in increased urinary glucose excretion and lower plasma glucose concentrations (U.S. Food and Drug Administration, 2018). In normoglycemic individuals, renal filtration handles 160 -180 grams of glucose daily of which more than 99% is reabsorbed and returned to the systemic circulation through the proximal tubules (Seufert, 2015). The SGLT2 acting on the proximal convoluted tubules regulate the major pathway for renal glucose reabsorption and its inhibition by medications in this drug category promote therapeutic glucosuria, thereby achieving desired plasma glucose levels (Garber et al., 2020). This mechanism of action is unique to this class of drugs enabling plasma glucose lowering activity that is independent of insulin secretion, pancreatic beta-cell mass, and insulin sensitivity (Seufert, 2015). SGLT2 inhibitors are prescription glucose lowering agents in tablet form and are FDA-approved for use with diet and exercise to decrease blood sugar levels in type 2 adult diabetics (U.S. Food and Drug Administration, 2018). Utilization of these medications demonstrate reductions in plasma glucose, HgbA1c, body weight, and blood pressure (Garber et al., 2020). Studies also show statistically significant results in lowering rates of all-cause cardiovascular death, myocardial infarction, non-fatal stroke, lower risk of associated hospitalizations for heart failure, and reduced progression of renal disease (Garber et al., 2020). The American Diabetes Association (2019) has recommended to consider the use of SGLT2 inhibitors in type 2 diabetes patients with an estimated glomerular filtration rate of greater than or equal to 30 ml / minute / 1.73 m2 and particularly in cases with greater than 300 mg / g albuminuria to reduce the risk of diabetic kidney disease progression, cardiovascular events, or both. Contraindications to this medications include prior hypersensitivity to its components, severe renal impairment, and patients on dialysis (U.S. Food and Drug Administration, 2018). Precautions for SGLT2 inhibitors include risks for volume depletion, ketoacidosis, urosepsis and pyelonephritis, hypoglycemia, necrotizing fasciitis of the perineum (Fournier’s Gangrene), risk of leg and foot amputations, and urogenital mycotic infections (U.S. Food and Drug Administration, 2018). The drug listing in this class include: canagliflozin, dapagliflozin, empagliflozin, ertugliflozin, sotagliflozin, luseogliflozin, tofoglifozin, ipragliflozin, and remogliflozin (Giugliano & Esposito, 2019). Week 2 Professor FACTS: The current IDSA guidelines (2019) recommend the following 3 options when treating CAP in a previously healthy patient: 1. Beta-lactam (eg high dose Amox) 2. Doxycycline 3. Macrolide (if the resistance in the community is not too high). If a patient has comorbidities (eg DM, COPD) or recent antibiotic use, the recommendation is to use one of the following options: 1. A respiratory fluoroquinolone Diagnosis and Treatment of Adults with Community-acquired Pneumonia. An Official Clinical Practice Guideline of the American Thoracic Society and Infectious Diseases Society of America 2. Beta-lactam plus either doxy or a macrolide Prednisone should not be prescribed routinely for viral or bacterial pneumonia. Guidelines recommend use in the severely ill ICU patient. Classmate response: I followed the link to the American Thoracic Society and Infectious Diseases Society of American and reviewed the current official clinical practice guidelines for treating an otherwise healthy adult with community-acquired pneumonia. Previously, when researching, I believe I used articles found within our Chamberlain Library. After reviewing the official clinical practice, I see that the first line of treatment would be high dose Amoxicillin, doxycycline, or like I listed above, a macrolide antibiotic. One of the primary reasons I mentioned prednisone as an additional treatment option is due to reflection of past experience. It is good to see that in the official clinical practice guidelines, that is not routinely prescribed for viral or bacterial pneumonia. I have been prescribed a respiratory fluoroquinolone, levofloxacin, in the past to treat pneumonia. Levofloxacin is generally a safe, well-tolerated, broad-spectrum antibiotic that has a good pharmacodynamic profile and pharmacokinetic profile, and exhibits low potential for resistance against S. pneumoniae (Metlay, et al., 2019). Important patient teaching for levofloxacin includes the risk that the patient will develop tendonitis or a tendon rupture during the course of treatment or for several months after treatment. It is the recommendation of the FDA that at the first sign of tendon pain, swelling, or inflammation, patients should discontinue the levofloxacin, avoid exercise, and use of the affected area, and contact their provider immediately for a tendon evaluation as well as a change to a non-fluoroquinolone antibiotic (2016). While taking this medication it is important for patients to remain aware of their bodies so that they can quickly notice when there has been a change. Professor response to classmate: So glad you reviewed the guidelines! They just came out the end of last year. I was surprised that Amox made it into the guidelines, but it is related to resistance and that the higher dose can overcome that resistance. Fluoroquinolones are a very useful class used for pyelonephritis (eg Cipro) or the respiratory fluoroquinolones used for CAP in those at higher risk. Unfortunately there is also resistance to fluoroquinolones as well. Thanks for pointing out the risk of tendon rupture. We must not take likely the Rx of fluoroquinolones. There is a black box warning against using them for bronchitis and cystitis, yet it is still something seen in practice. Fluoroquinolones should be avoided in children and pregnant women. Professor FACTS: Clarithromycin and azithromycin are both macrolides. Unfortunately, with overuse, we are now seeing S. pneumoniae resistance to this class which is important to keep in mind if using for treatment of CAP or acute otitis media. Some important points about doxy: avoid in children and pregnant women, and the tetracyclines increase sun sensitivity. Professor Facts: The role of ipratropium/anticholinergics for the management of asthma is relatively new. Its place has been under study for years. The GINA 2020 asthma guidelines give further information regarding use of ipratropium for asthma: 1. It can be used acutely (short acting) to decrease hospital admissions when added to a SABA when that is insufficient for an acute exacerbation 2. Long acting anticholinergics can be used as a Step 4 or 5 add-on. More professor facts: One big change recommended by the GINA guidelines 2020 is that ALL patients with asthma should use an ICS, even if it is on a PRN basis whenever a SABA is used. Previous guidelines only recommended an ICS for persistent asthma and not for intermittent asthma. Professor question: Can you tell us (from the text), what is the definition of drug- resistant TB? Classmate answer: There is an increase in drug-resistant tuberculosis (TB) for over 2 decades. Drug resistance can be either primary or acquired. Primary resistance occurs in patients who have never been treated for TB and risk factors include exposure to someone who has drug resistant TB, immigration from a country with a high prevalence of drug-resistant TB, and a greater than 4% incidence of resistant TB in the community (Woo, & Robinson, 2016). Drug-resistant TB occurs when bacteria become resistant to the drugs used to treat TB. This means that the drug can no longer kill the TB bacteria. Drug-resistant TB can occur when the drugs used to treat TB are misused or mismanaged. Examples of misuse or mismanagement include: People do not complete a full course of TB treatment, Health care providers prescribe the wrong treatment (the wrong dose or length of time), drugs for proper treatment are not available, drugs are of poor quality (Centers for Disease Control and Prevention, 2020). Acquired or secondary resistance occurs in a patient who has been previously treated for TB. Poorly or inadequately treated TB is the leading cause of secondary resistance. Extensively resistant TB (resistant to multiple second-line drugs) is resistant both to isoniazid and rifampin and to any fluoroquinolone drug and at least one of three second- line injectable drugs (amikacin, kanamycin, or capreomycin). Drug resistance can be proved only by susceptibility testing (Woo, & Robinson, 2016). If INH resistance is documented in a patient on a 9-month regimen (without PZA), then INH should be discontinued. If EMB was included in the initial regimen, then treatment with RIF and EMB should continue for a minimum of 12 months. If the initial treatment did not include EMB, then testing for drug susceptibility should be repeated, and INH needs to be discontinued and two new drugs should be added (Woo, & Robinson, 2016). The regimen may need to be adjusted when drug susceptibility test results are available. Any patient whose TB demonstrates resistance must be seen by an infectious disease specialist who treats patients with TB. Inadequate treatment is one of the leading causes of secondary resistant TB (Woo, & Robinson, 2016). Professor question: From our text can you tell us the findings of the SMART trial regaring salmeterol use? Classmate answer: The Salmeterol Multicentre Asthma Research Trial was a large random controlled trial in asthma patients that evaluated the safety of salmeterol use. The findings showed that a non-significant increase in combined respiratory-related deaths and/or life-threatening events found in patients using salmeterol. The SMART trial also had findings of a statistically significant increase of death and life-threatening situations among African American patients. According to Rottenkolber (2015), "a significantly increased risk for “combined respiratory-related death or life-threatening experience and combined asthma-related deaths or life-threatening experience was found for African Americans who had no prescription of inhaled corticosteroids at baseline." In the conclusion of the SMART trial contrast, at baseline no significant differences between patients receiving salmeterol or placebo were found in the results as well as previous and current published guidelines. Long-acting beta-2-agonist was recommended to be prescribed only to patients receiving inhaled corticosteroids. After results were given to the public, according to Rottenkolber (2015), "information for health care providers were sent out by the FDA stating that long-acting beta-2-agonist should be prescribed to asthma patients only if other medicines, including low-or- medium dose inhaled corticosteroids do not control asthma." The FDA imposed a Black box’ warning on long-acting beta-2-agonists. Professor question: According to our text, what is the advantage of using transdermal nicotine over nicotine gum? Classmate answer: The transdermal nicotine has its advantages over the use of nicotine gum. The patch delivers a constant level o f nicotine to help prevent the occurrence of withdrawal symptoms. When the patient uses the gum, they are putting something in their mouth which does not take away the behavioral aspect of cigarette smoking. The oral aspect is not reinforced. The transdermal patch is also easier in the aspect of administration. Compared to gum that needs to be chewed anywhere from 20-30 times a day, the patch is applied once a day and the dose is of the patch is weaned on a scheduled basis (Woo & Robinson, 2016). Professor question: Theophylline is not used very often anymore but we may see it used by a specialist when inhaled therapy is insufficient. The reason is that this is a drug with a narrow therapeutic window- it is associated with toxicities including seizures. It is a drug that requires monitoring of drug levels. According to our text, are there any considerations regarding theophylline and type of diet? Classmate response: According to our textbook, theophylline can interact with beta- blockers because it can increase serum theophylline if taken together. Another interacting drug is the inhalation of anesthetics which can cause increased arrthymia. Smoking can increase theophylline clearance. A diet that is low in carbohydrates and high in protein can decrease the elimination of the drug. A diet that is high in carbohydrates and low in protein causes the drug to lengthen its half-life. Charcoal broiled foods should be avoided because it accelerates the hepatic metabolism of the drug. Any caffeine elimination may be increased as well. Theophylline considerations include monitoring closely for any signs of toxicity as well as frequent levels need to be checked when a new medication is being added. Signs of toxicity include any jitteriness, headaches, rashes, restlessness, convulsions, nausea and vomiting (Woo & Robinson, 2016). Professor question: If a woman is pregnant and taking INH, what supplement do we need to advise? (see text) Classmate answer: Pregnant women who are taking INH need to be prescribed Pyridoxine (vitamin B6) 25mg/d to decrease the incidence of peripheral neuropathy which is linked to patients taking INH Professor question: What type of medication is Spiriva? What is the generic name? Classmate answer: Spiriva is a trade name for tiotropium bromide. This medication is an anticholinergic agent which exerts a long-acting antimuscarinic action and showing affinity to the M1 to M5 muscarinic receptor sub-types (Radovanovic et al., 2017). In the lungs, it demonstrates therapeutic effects through the inhibition of M3 receptors on smooth muscles resulting in bronchodilation (U.S. Food and Drug Administration, 2016). Tiotropium bromide is indicated for once-daily, long-term maintenance regimen to prevent bronchospasms associated with chronic obstructive pulmonary disease (COPD), and for mitigating COPD exacerbations (U.S. Food and Drug Administration, 2016). It is also indicated for the once-daily, and long-term, maintenance treatment for asthmatics 6 years of age and older (U.S. Food and Drug Administration, 2016). Tiotropium bromide comes in the form of an inhalation spray known as Spiriva Respimat inhaler which produces a soft mist (U.S. Food and Drug Administration, 2016). Another dose administration form is the HandiHaler which emits a dry powder when activated and inhaled (U.S. Food and Drug Administration, 2016). Professor FYI: The IDSA guidelines are a terrific source for most type of infections (eg skin, bladder, etc) Week 3 Professor question: As we discuss medications for HTN this week let's consider a pregnant women and women of childbearing age who might become pregnant. What classes are contraindicated for pregnant woman? Classmate answer: According to the FDA, angiotensin converting enzyme (ACE) inhibitors and angiotensin II receptor blockers (ARBs) are contraindicated in pregnancy due to the associate with adverse fetal effects (Brown & Garovic, 2016). ACE inhibitors are labeled FDA class C for the duration of the first trimester of pregnancy and FDA class D for the duration of the second and third trimesters. Medications to treat hypertension that are considered safe in pregnancy include methyldopa, labetalol, nifedipine, and beta blockers. Professor question: One of our reading topics this week is reduction of lipids. Can you tell us about fenofibric acid? What is it used for and how does it work? At what level of hypertriglyceridemia should it be considered to reduce the risk of pancreatitis? Classmate answer: (this one is long but this girl gave some really good information in this response)!!! Thank you Pamela for the response!! Lipids represent an essential molecule concerning the role of certain lipids such as low-density lipoproteins (LDLs) in the development of cardiovascular diseases. Owing to this known risk, there are multiple guidelines and recommendations aimed at lowering lipids (Alagona Jr, 2010). For many years, statins were used to lower LDLs (Alagona Jr, 2010). However, non-statin drugs such as fenofibric acid have also been developed. Fenofibric acid is an antilipemic drug that is categorized as a fibric acid derivative. Fibric acids such as fenofibric acid are potent ligands of peroxisome proliferator receptor alpha (PPAR- α), which plays an important role in fatty acid metabolism regulation (Mathew & Singh, 2020). I will address this role in the next paragraph which focuses on how fenofibric acid works. Fenofibric acid is usually utilized as an adjunct to diet therapy to lower triglyceride levels in adults diagnosed with severe hypertriglyceridemia (Alagona Jr, 2010). Another use regards lowering of elevated total cholesterol, triglycerides, alipoprotein B, and LDL and to increase high-density lipoproteins (HDLs) in individuals with mixed dyslipidemia or hypercholesterolemia (Alagona Jr, 2010). Fenofibric acid can also be used to lower hypertriglyceridemia (HTG) to decrease pancreatitis risk (Scherer et al., 2014). Notably, fenofibric acid can be used alone or in combination therapy with statins. The drug is available in several brand names including Trilipix, Lipofen, and Antara among others. To understand how fenofibric acid works, we have to understand its mechanism of action. Clinical studies have demonstrated that fenofibric acid works by activating PPAR- α (Alagona Jr, 2010). PPAR-α is a transcription factor involved in the regulation of multiple genes with activation by an agonist resulting in increased gene transcription and protein synthesis (Mathew & Singh, 2020). Likewise, fenofibric acid binds to PPAR- α thereby activating it. Consequently, lipolysis as well as triglyceride-rich particles elimination from plasma increase (Mathew & Singh, 2020). This happens because of the activation of lipoprotein lipase and a curtailment of the production of apoprotein C- III, which is a known inhibitor of lipoprotein lipase activity (Alagona Jr, 2010). With the consequent reduction in triglycerides, the size and composition of low-density lipoproteins (LDLs) are altered since small-LDL particles are eliminated resulting in low LDL levels. (Alagona Jr, 2010). Furthermore, PPAR- α results in an induction of increased HDL through the upregulation of apoproteins apo A-I, and apo A-II (Alagona Jr, 2010). Fenofibric acid, therefore, realizes its benefits through multiple mechanisms. As indicated earlier, fenofibric acid is used to reduce HTG to lower the risk of pancreatitis. However, it must be noted that indications for this benefit are for those with severe hypertriglyceridemia because not all patients with hypertriglyceridemia are at risk of developing pancreatitis (Chait & Subramanian, 2019). The rationale is that there is a 5% and 10-20% pancreatitis risk in individuals with serum triglycerides >1000mg/dl and >2000 mg/dl respectively (Scherer et al., 2014). The Endocrine Society considers HTG levels 1000-1999 mg/dl as severe and levels ≥2000 mg/dl as very severe (Berglund et al., 2012). Since pancreatitis risk is highest in severe and very severe HTG, it is reasonable to argue that these are the levels of HTG when fenofibric acid should be considered to lower pancreatitis risk (Scherer et al., 2014; Chait & Subramanian, 2019). Nevertheless, secondary causes of HTG should be addressed before initiating fenofibric acid therapy. Maintaining low triglyceride levels is necessary to prevent recurrent pancreatitis. Professor question: Thanks! To help with our topic of lipid management this week, what lab test should we order if a patient on a statin develops muscle pain? Classmate answer: One of the most common adverse reaction with statin use is muscle pain. It can be defined based on a spectrum of severity that includes myalgia, myopathy, myositis, myonecrosis, and rhabdomyolysis. The risk factors for this to occur is those patients on higher doses, females, lower BMI, older age, diabetes, hypothyroidism, hypertension, hepatic and renal disease. If a patient develops muscle pain, the provider will order a serum creatine kinase lab draw. Creatine kinase is a substance that is released into the blood when there is inflammation or damage to muscles. The normal is 22-198 U/L. If the lab value is more than five times the normal level, the provider may advise the patient to discontinue statin use (Yuet, Knine, & Ahmad, 2015). . Professor question: To help with our review of lipid therapies this week, will you tell us about ezetimibe (Zetia)? What is it MOA and is it a first line agent? Classmate answer: Ezetimibe is a antilipemic agent used to lower high cholesterol agents. Adverse reactions include: increased liver enzymes, cholecystitis, angioedema, HA, myopathy, rhabdomolysis, and upper respiratory infection. Patient education: Follow your diet, medication, and exercise routines very closely. Store at room temperature away from moisture and heat. Avoid eating foods that are high in fat or cholesterol. What is it MOA and is it a first line agent? Mechanism of action: According to IBM Micromedex (2020), "Ezetimibe reduces blood cholesterol by acting at the brush border of the small intestine to inhibit the absorption of cholesterol, leading to a decrease in the delivery of intestinal cholesterol to the liver." This reduces hepatic cholesterol stores and increases the clearance of cholesterol from the blood. Ezetimibe (Zetia) is a non-statin agent which reduces cholesterol. According to IBM Micromedex (2020), "Statins are the first-line therapy for pharmacological lipid modification." Zetia is a second line agent. Further professor FACTS in regards to above question: This is an important drug to be aware of since it is prescribed often. It is indicated when a patient either is not achieving desired results with a statin alone OR if they are not able to take a statin. Thanks for your research! Professor question: If a patient has heart failure why would we need to be cautious about prescribing calcium channel blockers? Which CCB have the strongest neg inotropic effect? Classmate answer: In a patient with heart failure prescribing Calcium Channel Blockers (CCB) can reduce the ejection fraction of the heart, second or third-degree AV blockade, and sick sinus syndrome because of the possibility of causing bradycardia and worsening cardiac output. In a study of 2,466 patient with recent myocardial infarction randomized to diltiazem or placebo, the patient that took diltiazem increased the risk of adverse cardiac events. These drugs may exacerbate the disease. Verapamil has the most pronounced negative inotropic effect and needs to be avoided in Heart Failure patients and it also can worsen the disorder (Tang, 2018). Verapamil also has the strongest nodal conduction and make bradycardia worse. Patients that have ventricular dysrhythmias, and conduction disturbances in the SA or AV, patients who have systolic blood pressures below 90 mmHg because of the high risk for induction of heart failure and severe hypotension if prescribed CCB (Woo & Robinson, 2016). Professor question: Can you review the discussion of angina which discusses imbalance between myocardial oxygen supply (MOS) and demand (MOD) in the myocardium. Which of the following drugs affect MOS? Which affect MOD? Classmate answer: Angina is a syndrome that is characterized by the patient reporting a deep, poorly localized chest or arm pain that is associated with physical exertion or emotional stress (Woo & Robinson, 2016, p. 881). The patient will feel immediate relief with either rest or nitroglycerin. The cause of this angina is an imbalance between myocardial oxygen supply (MOS) and myocardial oxygen demand (MOD). Ischemia (angina) occurs when demand exceeds supply. There are multiple medication regimens that we can provide to the patient to help the supply and the demand of the heart. Nitrates Nitrates affect the myocardial oxygen supply and myocardial oxygen demand. Low dose nitroglycerin⟶⟶ dilate veins (more than arteries)venous return to the heartL-ventricular end diastolic pressure (preload) results in decreased wall tension and increased transmyocardial gradientincreased oxygen supply to the myocardium relieve angina pain (Woo & Robinson, 2016). Beta Blockers Beta blockers work to help the myocardial oxygen demand of angina. Beta blockers decrease myocardial contractility force decrease heart rate and conduction velocity decrease systemic vascular resistance decrease blood pressure (afterload) reduce MOD relieve angina pain (Woo & Robinson, 2016, p. 884). CCB CCB work on the MOD side of angina. Calcium into cells blocked dihydropyridines cause arterial smooth muscle relaxation results in peripheral vasodilation results in decrease afterload decreased MOD (Woo & Robinson, 2016, p. 884). • Non-dihydropyridine CCB (verapamil and diltiazem) reduce the SA node rate of depolarization and slow AV conduction which results in lowering heart rate in the smooth muscle of the heart (Woo & Robinson, 2016). These two actions will also effect the myocardium oxygen demand. ACE inhibitors Ace inhibitors work on angina by helping to solve the MOD and the MOS problems. Ace inhibitors block angiotensin II formation (vasoconstrictor) decreases peripheral vascular resistance decreased afterload decrease MOD (Woo & Robinson, 2016, p. 884). Coronary artery wall thickness is also reduced by the blocking of angiotensin II which will result in myocardium oxygen supply. Direct Renin Inhibitors (DRIs) DRI work to help reduce MOD in angina. The only approved DRI is Aliskiren (Tekturna). This medication will provide the patient with less cough and angioedema risk factors then patients who take ACE inhibitors. This medication is contraindicated for pregnant women (Woo & Robinson, 2016). DRIs decrease plasma renin activityblock conversion of angiotensinogen to angiotensin Idecrease angiotensin Idecrease conversion of angiotensin II which decreases peripheral vascular resistancedecrease MOD (Woo & Robinson, 2016, p. 884). ASA Since angina is mainly from atherosclerosis which causes vasodilation and plaque buildup. ASA helps stop the formation of thromboxane A2 in the formation of platelets. This helps in the fight to stop platelet buildup. ASA 81 to 162 mg are recommended for patients with angina (Woo & Robinson, 2016). Statin’s should also be included in the treatment regimen for angina. By reducing the patients LDL cholesterol, the patient will begin to have a decrease in atherosclerotic plaque which is causing the narrowing of the arteries which causes the ischemia (angina) (Woo & Robinson, 2016). professor question: What antihypertensive class is indicated in a patient with DM who has microalbuminuria? According to the text, what are conditions would this class be indicated for? Classmate answer: The antihypertensive class that has been recommended for diabetics with microalbuminuria is the Angiotensin-Converting Enzyme Inhibitor (ACEI) Lisinopril (Woo & Robinson, 2016). ACEIs reduce the effects of the Renin-Angiotensin-Aldosterone System (RAAS) on the kidneys, which with the additional volume and vasoconstriction associated with hypertension, can alter glomerular hemodynamics and their rate of perfusion. By reducing the amount of Renin, ACEI inhibits the converting enzyme from forming Angiotensin I, the precursor to Angiotensin II, a powerful vasoconstricting chemical messenger (Woo & Robinson, 2016). Without Angiotensin II affecting the adrenal glands, one of four target cell types, aldosterone is not released causing sodium and water retention. Thus, ACEIs reduce both vasoconstriction and fluid volume that would increase the progression rate of diabetic nephropathy. The advent of microalbuminuria is considered to be a hallmark of impending diabetic nephropathy following proteinuria. ACEI is indicated a first-line antihypertensive medication and will its ability to positively effect both the peripheral vascular resistance and the total fluid volume, makes this medication a potent medication in alleviating patients from their symptoms of hypertension and reducing the progression of the disease. In initiating ACEI in a diabetic patient, if it wasn't the initial medication then would require a positive proteinuria result from a urinalysis. Professor question: What is the dosing schedule for long acting isosorbide mononitrate and why? Classmate answer: The dosing schedule for long acting isosorbide mononitrate is once daily in the morning. This is due to the medication being extended release. The normal dosage is 30 - 60 mg once daily in the morning. Elderly patients should be started on the lower dosage. The extended release releases the medication over an 8 -10 hour period and it works best if there is a period of time that the medication is not in the patient's system. To provide for the period of time without the medication in the patient's system, it is prescribed to be taken in the morning so that the patient is sleeping during the time that they do not have medication on board. Professor question: According to our text, what lipid abnormality is most likely to benefit from omega 3 FA supplementation? Classmate answer: According to our text omega 3 FA are best at treating very high triglyceride levels. This is defined as greater than 500mg/dL. Omega 3 FA have also shown that LDL levels may rise but not affect HDL levels with omega 3 FA treatment (Woo & Robinson, 2015). Professor question: To help with this week's study can you review from the text the causes of systolic heart failure? Classmate answer: According to the text, Woo & Robinson (2015), systolic heart failure or left ventricular dysfunction is due to an injury to the myocardium, in two thirds of patients, the cause is coronary artery disease (CAD) . Other causes of left ventricular dysfunction is a myocardial infarction (MI) or non-ischemic cardiomyopathy from drugs or chemotherapy that weaken the myocardium. The injury to the myocardium leads to hypertrophy or the thickening of the myocardium wall which then results in the decreased cardiac output or systolic heart failure(Woo & Robinson, 2015). Professor question: What is the dosing schedule for ACEIs? (how many times per day are they taken?) Classmate answer: Captopril is a short acting ACEI with a half-life of less than 2 hours; It requires 2-3 times daily dosing. All other members ACEIs are dosed once a day because they have a longer-half-life of 6 – 12 hours that require more time to achieve steady state. Losartan has a 2-hour half-life, and its active metabolite has a 6 to 9-hour half-life. Dosing may be daily or in two divided doses. Steady state is achieved in 3 to 6 weeks (Woo & Robinson, 2016). Professor question: According to the text, what labs should be checked in a week after initiating an ACEI? Why? Classmate answer: The labs that need to be checked in a week for patients who take ACE inhibitors are Serum Creatinine, BUN levels and electrolytes, particularly the potassium levels. ACE tends to increase the potassium levels causing hyperkalemia. This is when the levels are above 5.5. This will cause AKI (Acute Kidney Injury). If the levels of all 3 are elevated, then discontinuation of the ACE is needed. The labs need to be checked 1-2 weeks of initiation and after the dose is increased. If levels are stable, then the recheck can occur in 4 weeks. According to Woo & Robinson (2016), ACE inhibitors decrease proteinuria in those with CKD and help with blood pressure control. Adding an ACE inhibitor for patients with known CKD commonly results in increased serum creatinine. The improvement in proteinuria happens despite this effect. It is acceptable to have an 30% increase in SCr with the discontinuation of the ACE inhibitor. Professor question: What anti-arrhythmic medication in the reading this week requires pulmonary and thyroid function monitoring every 6 months? Classmate answer: Amiodarone (Cordarone) is a medication that treats or prevent abnormal rhythms of the heart (Amiodarone, 2020). This medication is an extremely effective anti-arrhythmia medication, but like all medication it comes with the potential of adverse effects. Taking Amiodarone puts you at high risk for pulmonary fibrosis, so a chest x-ray and pulmonary function studies are recommended every 3-6 months (Woo & Robinson, 2016). Amiodarone also requires close monitoring for thyroid dysfunction. It is also recommended to assess thyroid-stimulating hormone (TSH) and free T4 for potential impairment (Woo & Robinson, 2016). Professor question: Can you review the classes of angina from our text? Classmate answer: Woo and Robinson (2016), identifies two forms of angina- chronic stable angina and Low-risk unstable angina. The New York Heart Association and the CCS have developed a classification system that helps providers grade the severity of angina. The classification identifies several classes; Class I, II, III, and IV. Class, I is proven coronary artery disease without symptoms, class II is angina only with usually strenuous physical excretion, class III is angina during routine physical activity while Class IV is angina that occurs during minimal activity or rest. (p. 885) Professor question: From our text, can you review the statin strength from weakest to highest? Classmate answer: no answer from classmate given but from the quiz: correct answer was rosuvastatin, lovastatin, atorvastatin (lowest to highest strength) [Show More]
Last updated: 1 year ago
Preview 1 out of 37 pages
Instant download
Buy this document to get the full access instantly
Instant Download Access after purchase
Add to cartInstant download
Reviews( 0 )
Document information
Connected school, study & course
About the document
Uploaded On
Mar 12, 2022
Number of pages
37
Written in
Additional information
This document has been written for:
Uploaded
Mar 12, 2022
Downloads
0
Views
51