*NURSING > STUDY GUIDE > RNSG 1430 Elimination and Nutrition Study guide 2020 – Weatherford College | RNSG1430 Elimination (All)
RNSG 1430 Elimination and Nutrition Study guide 2020 – Weatherford College | RNSG1430 Elimination and Nutrition Study guide 2020
Document Content and Description Below
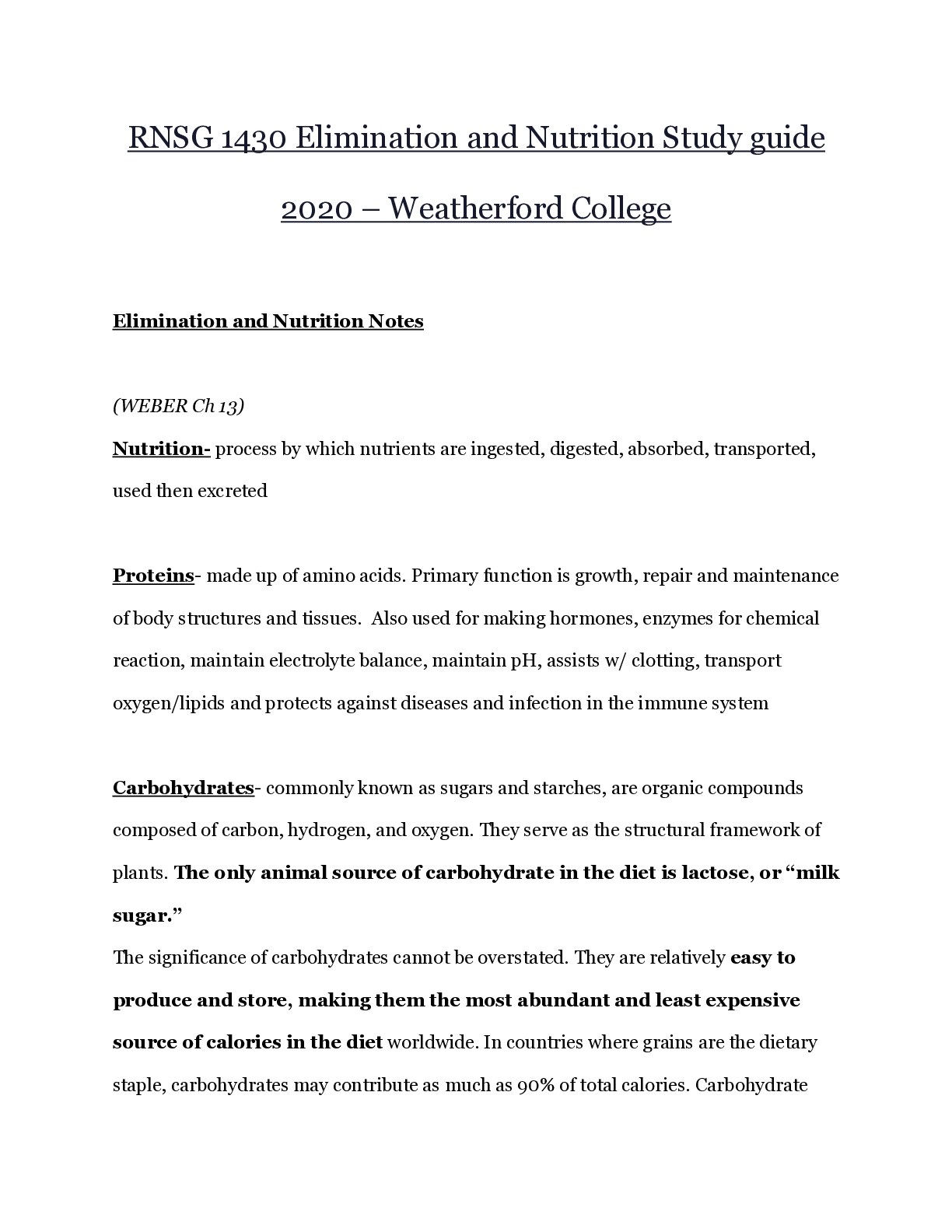
RNSG 1430 Elimination and Nutrition Study guide 2020 – Weatherford College Elimination and Nutrition Notes (WEBER Ch 13) Nutrition- process by which nutrients are ingested, digested, absorbed... , transported, used then excreted Proteins- made up of amino acids. Primary function is growth, repair and maintenance of body structures and tissues. Also used for making hormones, enzymes for chemical reaction, maintain electrolyte balance, maintain pH, assists w/ clotting, transport oxygen/lipids and protects against diseases and infection in the immune system Carbohydrates- commonly known as sugars and starches, are organic compounds composed of carbon, hydrogen, and oxygen. They serve as the structural framework of plants. The only animal source of carbohydrate in the diet is lactose, or “milk sugar.” The significance of carbohydrates cannot be overstated. They are relatively easy to produce and store, making them the most abundant and least expensive source of calories in the diet worldwide. In countries where grains are the dietary staple, carbohydrates may contribute as much as 90% of total calories. Carbohydrate intake is often correlated to income. As income increases, carbohydrate intake decreases and protein intake, a more expensive form of energy, increases. Fats- Stored in adipose tissue and classified as triglycerides which make up 95% of fats in food, phospholipids or sterols. They provide energy (double of proteins and carbs), aid in absorption of fat soluble vitamins, supply essential fatty acids for healthy skin, insulate skin and nerve fibers, protect internal organs, lubricate skin to slow water loss Cholesterol- fat like substance produced by the liver. Found in animal food sources Vitamins- required for energy to be releases from carbs, proteins and fats. Necessary for forming RBC’s Minerals- Promote growth and maintain health. Classified as major (Ca, Na, K) or trace (Zn, Fe, Fl) Water- one of the most important nutritional needs accounting for 50-80% of bodies weight Functions in transporting nutrients, electrolytes, and oxygen; excreting wastes; regulating body temperature; lubricating joints and membranes; and acting as a medium for digestion recommended 2000-3000mL/day Risk Factors Malnutrition - Lower socioeconomic status, lifestyle w/ long working hours, poor food choices, chronic dieting, chronic diseases (cancer), dental factors, limited access to sufficient food, disorders (anorexia, bulimia, depression), illness or trauma. Cachexia- wasting syndrome, malignant cachexia may develop in pts w/ cancer AIDS- vulnerable for malnutrition Obesity- affects 2/3 of the adults in U.S pop, 17% of children between 2-19 or obese. Can lead to diabetes, osteoarthritis, heart risk, certain cancers, and sleep apnea. Anyone 10% over their ideal body weight is considered overweight, 20% over is obese (Taylor Ch 35) Definitions: 1) Absorption- process where drugs transfer from site of entry into the body then bloodstream 2) Anorexia- lack or loss of appetite for food 3) Anthropometric- measurements of the body and body parts 4) Aspiration- misdirection of oropharyngeal secretions or gastric contents into larynx or lower respiratory tract 5) Basal metabolism- amount of energy required to carry out involuntary activities of the body at rest (BMR is increased w/ growth, infections, fever, emotional tension, extreme env temps, elevated epinephrine and thyroid hormones) 6) Body Mass Index (BMI)- ratio of height to weight (may show increase risk for heart disease, diabetes and hypertension) -18.5-24.9= healthy -25-29.9=overweight -30+= obesity -40+= extreme obesity 7) Calorie- measure of heat or energy 8) Kilocalorie- commonly referred to as a calorie, amount of heat required to raise 1 kg of water 1 degree Celsius 9) Carbohydrate- organic compound (sugars and starches) composed of Carbon, Hydrogen and Oxygen: most abundant and least expensive source of calories 10) Cholesterol- fat like substance only found in animal tissues, important for cell membrane structure - - - - - - - - - - - - - - - - - 1) NPO- nothing by mouth 2) Nutrient- specific biochemical substance used by the body for growth, dev, activity, reproduction, lactation, health maintenance and recovery from illness or injury 3) Nutrition-study of nutrients and how they are handled by the body, as well as the impact of human behavior and environment on the process of nourishment 4) Obesity- weight greater than 20% above normal 5) Parenteral nutrition- nourishment, provide via IV therapy 6) Percutaneous endoscopic gastrostomy tube (PEG)- surgically or laparoscopically placed gastrostomy tube 7) Peripheral Parenteral Nutrition- prescribed for patients who require nutrient supplement through a peripheral vein from inadequate oral feedings 8) Protein- vital component of every living cell, composed of carbon, hydrogen, oxygen and nitrogen 9) Recommended dietary allowance (RDA)- recommendations for avg daily amounts of essential nutrients that healthy pop groups should consume over time 10) Total parenteral nutrition- Nutritional therapy that bypasses the GI tract for patients who are unable to take food orally: highly concentrated, hypertonic nutrient solution adm IV thru central vein 11) Trans Fat- partially hydrogenated liquid: raises serum cholesterol 12) Triglycerides- predominant form of fat in food and the major storage form of fat in the body 13) Vitamins- organic substances needed by the body in small amounts to help regulate body processes 14) Waist circumference- a numerical measurement of the waist, used to assess an individual’s abdominal fat and establish ideal body weight Essential nutrients- not synthesized by the body or not made in sufficient amounts - - - - - - - - - - - - - -- - - Water Soluble Vitamins Vitamins B and C Vitamin C- citrus fruits, broccoli, green peppers, strawberries and greens -collagen -enhances iron absorption -antioxidant Signs and Symptoms of Vit C deficiency; scurvy, hemorrhaging, delayed wound healing Signs and Symptoms of Vit C excessiveness; hot flashes, headache, nausea and diarrhea Vitamin B Complex (thiamin) -pork, liver, whole grains, enriched grains, legumes -coenzyme in key reactions that produce energy from glucose - S/S of Deficiency- beriberi, mental confusion and fatigue -S/S of excess- NONE Elimination Toilet training- voluntary control of urethral sphincters occurs between 18-24 months of age. Toilet training begins between 2-3 yrs old when: a child can hold urine for 2 hrs, child recognized when bladder is full, child can communicate the need to control urination until seated at toilet. - Motivation from wanting to be like parents - Some cultures start at 1 yr, other at 5 yrs - Occasional day time urination is not cause for concern - Enuresis- Continued incontinence past the age of toilet training - Nocturnal enuresis is usually gone by 6 yrs old Types of Incontinence 1) Transient- appears suddenly and last for 6 months, caused by confusion secondary to acute illness, infection as a result of medical tx?, such as use of diuretics or I.V fluids 2) Stress- occurs when there is an involuntary loss of urine related to an increase in intraabdominal pressure; coughing, sneezing, laughing, child birth, menopause, obesity or straining from constipation. Leakage does not occur when supine 3) Urge- involuntary loss of urine occurring soon after feeling urgent need to void; pts. Experience loss before getting to toilet 4) Mixed- 2 or more types combined 5) Overflow- chronic retention of urine, involuntary loss associated w/ over distention and overflow of bladder; signal to empty bladder may be underactive or absent. The bladder fills and dribbling occurs. May be caused by drugs, fecal impaction or neurological conditions 6) Functional- urine loss caused by the inability to reach the toilet because of loss of memory, disorientation 7) Reflex- emptying the bladder w/out the sensation of the need to void; Spinal Cord injuries 8) Total- continuous and unpredictable loss of urine resulting from surgery, trauma or physical malformation; Cannot be controlled due to a anatomic abnormality Impact of incontinence on Ind- diminished self-concept, feeling like an outcast, discomfort, odor, embarrassment Interventions -Eliminate caffeine and drink more water. If you don’t drink enough water the bladder may become irritated and cause incontinence -Collagen substances benefit incontinence by adding bulk to the tissue around urethra Differences in normal based on age -Infants are born w/out voluntary control of urination and have little ability to concentrate urine -@ 6 weeks nephrons are able to control reabsorption of fluids into tubules and effectively concentrate urine -Most children develop urinary control between 2-5 yrs old - girls develop control earlier than boys - Older children and adults control urination voluntarily, kidneys are able to concentrate urine and produce less urine @ night as a result of decreased renal blood flow -Older Adults, diminished abilities of kidneys to concentrate urine results in nocturia, decreased bladder tone/contractibility, neuromuscular problems, degenerative joint problems, weakness and alteration of thought process RN strategies for older adults Assessment of status/alterations -Collection of data about the patients voiding patterns, habits and difficulties and a history of current or past urinary problems -Physical examination of the bladder and urethral meatus -Assessment of skin and hydration -Diagnostic tests and procedures for examining the urine and urinary tract Nursing History -Voiding habits, current or past voiding problems -Infants, assess # of wet diapers per day (newborns 6-8) -In young children see if they have bladder control -Adults, note any problems, how they handle the problems and your judgment regarding adequacy of their solution Bowel Elimination -GI Tract extends from mouth to anus -Major organ involved in bowel movements is the large intestine Stomach (J-Shaped) -Stores food, churns fluid, secretes digestive fluid, pushes food. -Pyloric Sphincter-muscle ring at the end of the stomach that controls the movement of food (chime) from the stomach to the small intestines Small Intestine (20ft long) -responsible for digestion of food and absorption of nutrients into the bloodstream -secretes enzymes that digest proteins and carbs - - - - - - - - - - - - - - - - - - - - - - - - - - - - - CH 37 1. A nurse is assessing the abdomen of a patient who is experiencing frequent bouts of diarrhea. The nurse first observes the contour of the abdomen, noting any masses, scars, or areas of distention. What action would the nurse perform next? a. Auscultate the abdomen using an orderly clockwise approach in all abdominal quadrants. b. Percuss all quadrants of the abdomen in a systematic clockwise manner to identify masses, fluid, or air in the abdomen. c. Lightly palpate over the abdominal quadrants; first checking for any areas of pain or discomfort. d. Deeply palpate over the abdominal quadrants, noting muscular resistance, tenderness, organ enlargement, or masses. 2. A nurse is administering a large-volume cleansing enema to a patient prior to surgery. Once the enema solution is introduced, the patient complains of severe cramping. What would be the appropriate nursing intervention in this situation? a. Elevate the head of the bed 30 degrees and reposition the rectal tube. b. Place the patient in a supine position and modify the amount of solution. c. Lower the solution container and check the temperature and flow rate. d. Remove the rectal tube and notify the primary care provider. 3. A nurse working in a hospital includes abdominal assessment as part of patient assessment. In which patients would a nurse expect to find decreased or absent bowel sounds after listening for 5 minutes? Select all that apply. a. A patient diagnosed with peritonitis b. A patient who is on prolonged bedrest c. A patient who has diarrhea d. A patient who has gastroenteritis e. A patient who has an early bowel obstruction f. A patient who has paralytic ileus caused by surgery 4. A nurse assesses the stool of patients who are experiencing gastrointestinal problems. In which patients would diarrhea be a possible finding? Select all that apply. a. A patient who is taking narcotics for pain b. A patient who is taking laxatives c. A patient who is taking diuretics d. A patient who is dehydrated e. A patient who is taking amoxicillin for an infection f. A patient taking over-the-counter antacids 5. A patient has a fecal impaction. The nurse correctly administers an oil-retention enema by: a. Administering a large volume of solution (500–1,000 mL) b. Mixing milk and molasses in equal parts for an enema c. Instructing the patient to retain the enema for at least 30 minutes d. Administering the enema while the patient is sitting on the toilet 6. A nurse prepares to assist a patient with her newly created ileostomy. Which recommended patient teaching points would the nurse stress? Select all that apply. a. “When you inspect the stoma, it should be dark purple-blue.” b. “The size of the stoma will stabilize within 2 weeks.” c. “Keep the skin around the stoma site clean and moist.” d. “The stool from an ileostomy is normally liquid.” e. “You should eat dark green vegetables to control the odor of the stool.” f. “You may have a tendency to develop food blockages.” 7. A nurse is preparing a hospitalized patient for a colonoscopy. Which nursing action is the recommended preparation for this test? a. Have the patient follow a clear liquid diet 24 to 48 hours before the test. b. Have the patient take Dulcolax and ingest a gallon of bowel cleaner on day 1. c. Prepare the patient for the use of general anesthesia during the test. d. Explain that barium contrast mixture will be given to drink before the test. 8. A nurse is performing digital removal of stool on a 74-year old female patient with a fecal impaction. During the procedure the patient tells the nurse she is feeling dizzy and nauseated, and then she vomits. What should be the nurse’s next action? a. Reassure the patient that this is a normal reaction to the procedure. b. Stop the procedure, prepare to administer CPR, and notify the physician. c. Stop the procedure, assess vital signs, and notify the physician. d. Stop the procedure, wait five minutes, and then resume the procedure. 9. A nurse is scheduling tests for a patient who has been experiencing epigastric pain. The physician ordered the following tests: (a) barium enema, (b) fecal occult blood test, (c) endoscopic studies, and (d) upper gastrointestinal series. Which is the correct order in which the tests would normally be performed? a. c, b, d, a b. d, c, a, b c. a, b, d, c d. b, a, d, c 10. A nurse is caring for a patient who has a nasogastric tube in place for gastric decompression. Which nursing actions are appropriate when irrigating a nasogastric tube connected to suction? Select all that apply. a. Draw up 30 mL of saline solution into the syringe. b. Unclamp the suction tubing near the connection site to instill solution. c. Place the tip of the syringe in the tube to gently insert saline solution. d. Place syringe in the blue air vent of a Salem sump or double-lumen tube. e. After instilling irrigant, hold the end of the NG tube over an irrigation tray. f. Observe for return flow of NG drainage into an available container. 11. A nurse is teaching a patient with frequent constipation how to implement a bowel-training program. What is a recommended teaching point? a. Using a diet that is low in bulk b. Decreasing fluid intake to 1,000 mL c. Administering an enema once a day to stimulate peristalsis d. Allowing ample time for evacuation 12. A nurse caring for patients with bowel alterations formulates a nursing diagnosis for a patient with a new ileostomy. Which diagnosis is most appropriate? a. Disturbed Body Image b. Constipation c. Delayed Growth and Development 13. A nurse is irrigating the colostomy of a patient and is unable to get the irrigation solution to flow. What would be the nurse’s next action in this situation? a. Assist the patient to a prone position on a waterproof pad and try again. b. Check the clamp on the tubing to make sure that the tubing is open. c. Quickly pull the cone from the stoma and check for bleeding. d. Remove the equipment and call the primary care provider. 14. A nurse is assisting a patient to empty and change an ostomy appliance. When the procedure is finished, the nurse notes that the stoma is protruding into the bag. What would be the nurse’s first action in this situation? a. Reassure the patient that this is a normal finding with a new ostomy. b. Notify the primary care provider that the stoma is prolapsed. c. Have the patient rest for 30 minutes to see if the prolapse resolves. d. Remove the appliance and redo the procedure using a larger appliance. 15. A nurse is caring for a postpartum patient who has stitches in the perineum from an episotomy (surgically planned incision to prevent vaginal tears). Which medication would the nurse most likely administer to this patient? a. A stool softener (Colace) b. An osmotic laxative (Miralax) c. A bulk-forming laxative (Metamucil) d. An emollient laxative (mineral oil) Pyelonephritis (kidney infection)– Treatment and Nursing care Bacteria, if detected in the urine, are eradicated if possible. Long-term use of prophylactic antimicrobial therapy may help limit recurrence of infections and renal scarring. Impaired renal function alters the excretion of antimicrobial agents and necessitates careful monitoring of renal function, especially if the medications are potentially toxic to the kidneys. Nursing Management The patient may require hospitalization or may be treated as an outpatient. When the patient requires hospitalization, fluid intake and output are carefully measured and recorded. Unless contraindicated, 3 to 4 L of fluids per day is encouraged to dilute the urine, decrease burning on urination, and prevent dehydration. The nurse assesses the patient’s temperature every 4 hours and administers antipyretic and antibiotic agents as prescribed. Symptomatic patients are often more comfortable on bed rest. Patient education focuses on prevention of further infection by consuming adequate fluids, emptying the bladder regularly, and performing recommended perineal hygiene. The importance of taking antimicrobial medications exactly as prescribed is stressed, as is the need for keeping follow-up appointments. Promoting Normal Urination Nursing care to promote normal urination includes interventions to support normal voiding habits, fluid intake, strengthening of muscle tone, stimulating urination and resolving urinary retention, and assisting with toileting. Nurses working with patients to promote appropriate behaviors related to urine elimination should examine their own behaviors as factors in the success of the plan. Nurses who role model good health behaviors are more effective teachers. MAINTAINING NORMAL VOIDING HABITS If the patient’s voiding habits are adequate, provide care or teach the patient to maintain these habits to ensure comfort and satisfactory urine output. Attention to the following variables is helpful: Schedule: Some patients report urinating on demand in no apparent pattern. Others have inflexible patterns that have developed over the years and become anxious if these are interrupted. Some patients need assistance to urinate and may experience urgency. Nursing actions should support the patient’s usual urinating pattern as much as possible. Urge to void: Assist the patient to void when the patient first feels the urge to void. Routinely delaying urination may result in difficulty initiating a stream and/or urinary stasis. Urinary stasis can contribute to the development of urinary tract infections. Privacy: Many adults and children cannot urinate in the presence of another person. Unless the patient is extremely weak and requires assistance, provide privacy in the health care facility and in the home. Position: Helping patients assume their usual voiding position may be all that is necessary to resolve an inability to urinate. Some male patients cannot use a urinal while lying down or sitting; encourage them to void while standing at the bedside unless this is contraindicated. Similarly, some female patients cannot void easily on a bedpan but respond favorably with a bedside commode. Hygiene: Patients who are confined to bed find it difficult to perform their usual genital hygiene. Careful cleansing of the perineal and genital areas is needed for patient comfort and to prevent infection. This is easily accomplished for patients on bedrest by using warmed, moistened disposable washcloths and skin cleanser or by pouring warm, soapy water over the perineal area while the patient is still on the bedpan, followed by clear water. Families providing care for ill members at home may be taught this technique. Treatment Options For Urinary Incontinence Behavioral Techniques Pelvic floor exercises: Kegel exercises to strengthen pelvic floor muscles and sphincter muscles. Kegel exercises can be done alone, with weighted cones, or with biofeedback. Biofeedback: Measuring devices are used to help patient become aware of when pelvic floor muscles are contracting. Electrical stimulation: Electrodes are placed in the vagina or rectum that then stimulate nearby muscles to contract. Timed voiding or bladder training: May be used with biofeedback. Patient keeps track of when voiding and leaking occur to enable oneself to plan when to void, with increasing length of voiding intervals. Bladder training involves biofeedback and muscle training. Urgency control is addressed using distraction and relaxation techniques. Pharmacologic Treatment [Show More]
Last updated: 1 year ago
Preview 1 out of 49 pages
Instant download
Buy this document to get the full access instantly
Instant Download Access after purchase
Add to cartInstant download
Reviews( 0 )
Document information
Connected school, study & course
About the document
Uploaded On
Nov 01, 2020
Number of pages
49
Written in
Additional information
This document has been written for:
Uploaded
Nov 01, 2020
Downloads
0
Views
55




.png)