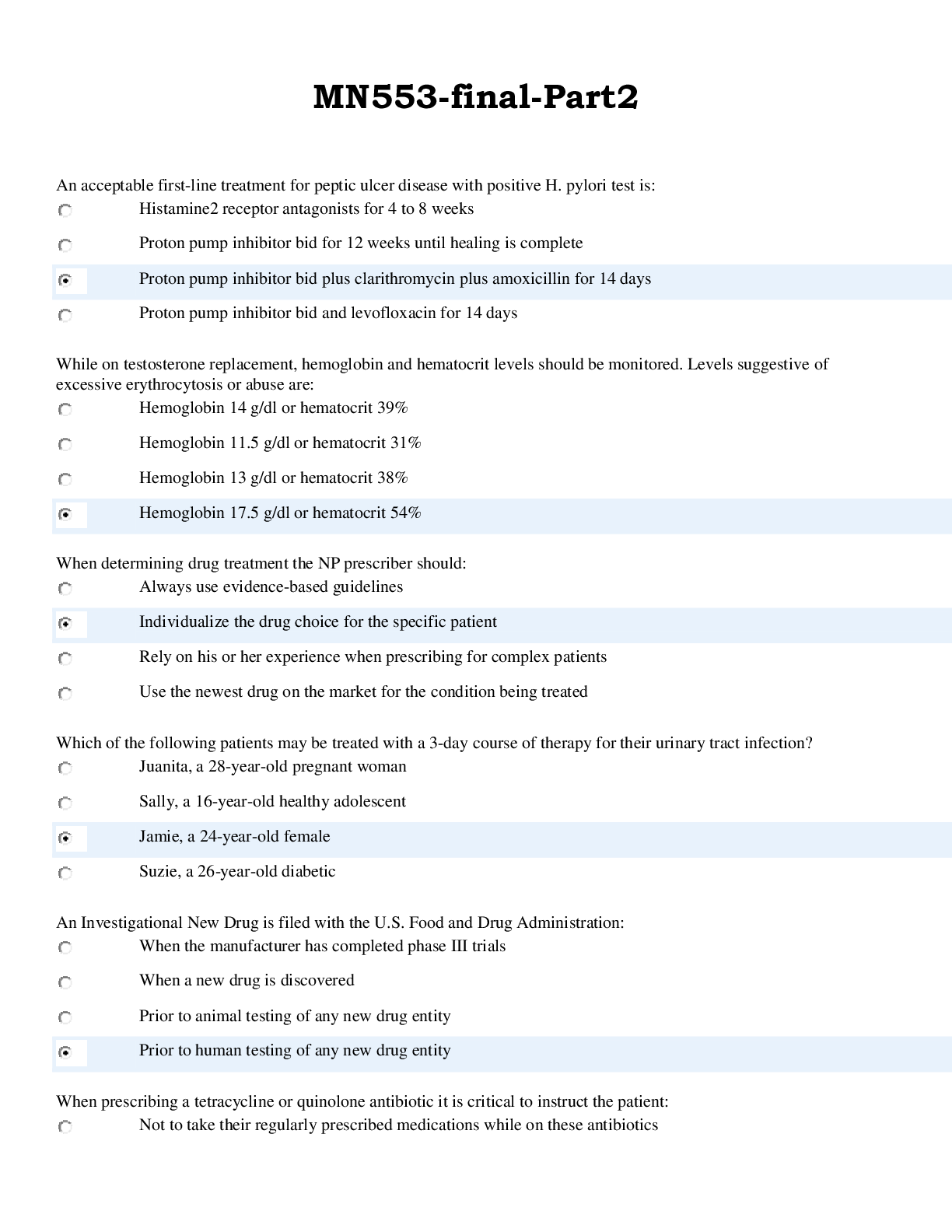
*NURSING > EXAM > NUR 2392 Module 9 Assignment: Endocrine Disorders Guide Rasmussen College NUR: 2392 Multidimensional (All)
NUR 2392 Module 9 Assignment: Endocrine Disorders Guide Rasmussen College NUR: 2392 Multidimensional Care II
Document Content and Description Below
NUR 2392 Module 9 Assignment: Endocrine Disorders Guide Rasmussen College NUR: 2392 Multidimensional Care II Running head: MODULE 9 ASSIGNMENT- ENDOCRINE DISORDERS GUIDE 1 Module 9 Assignment: End... ocrine Disorders Guide Rasmussen College NUR: 2392 Multidimensional Care II DateENDOCRINE DISORDERS GUIDE 2 Hyperthyroidism Hyperparathyroidism Causes of Disorder *Most common cause is Graves’ disease (toxic diffuse goiter)- an autoimmune disorder resulting from Hashimoto’s thyroiditis (HT); the production of autoantibodies to different substances & structures within the thyroid. *Caused by multiple thyroid nodules (toxic multinodular goiter)- enlarged thyroid tissues or benign tumors. *Caused by excessive use of thyroid replacement hormones (exogenous hyperthyroidism), (Rebar, Ignatavicius, & Workman, 2017, p 1265) *Parathyroid tumor or cancer *Congenital hyperplasia *Neck trauma or radiation *Vitamin D deficiency *Chronic kidney disease with hypocalcemia *Parathyroid hormone-secreting carcinomas of the lung, kidney, or GI tract, (Rebar, Ignatavicius, & Workman, 2017, p 1275) Diagnostic Tests • Thyroid scan- evaluates the position, size, & functioning of the thyroid gland • Ultrasonography- determine the size of the thyroid gland & the general composition of any masses or nodules. • ECG- usually shows supraventricular tachycardia, but other ECG changes can include atrial fibrillation, dysrhythmias, & premature ventricular contractions. • Lab tests such as Serum T3 (increased), T4 (total) (increased), free T4 index (increased), TSI (elevated in Graves’ disease; normal in other types of hyperthyroidism), TRAb (80%- 95% indicated Graves’ disease), & TSH (low in Graves’ disease; high in secondary or tertiary hyperthyroidism), (Rebar, Ignatavicius, & Workman, 2017 p 1266). • Arteriography • CT scan • Venous sampling of the thyroid for blood PTH levels • Ultrasonography • X-ray- may show kidney stones, calcium deposits, & bone lesions • EKG- usually shows short QT interval • Bone mineral density test • Lab tests such as 24-hour urine collection, serum calcium (increased in primary hyperparathyroidism), serum phosphorus (decreased), serum magnesium (increased), serum parathyroid hormone (increased), Vitamin D (calciferol) (variable), urine cAMP (increased), (Rebar, Ignatavicius, & Workman, 2017, p 1276). Signs & Symptoms • Diaphoresis • Thinning of scalp hair • Smooth, warm, moist skin • Palpitations • Chest pain • Increased systolic BP • GI problems (anorexia, nausea, vomiting, epigastric pain, constipation, weight loss) • Fatigue & lethargy • Psychosis & confusion • Bone fracturesENDOCRINE DISORDERS GUIDE 3 • Tachycardia • Dysrhythmias • Rapid, shallow respirations • Weight loss • Increased appetite • Increased stools • Eye fatigue • Insomnia • Tremors • Blurred or double vision • Increased tears • Hyperactive DTRs • Exophthalmos • Increased basal metabolic rate • Heat intolerance • Low-grade fever • Fatigue • Restlessness & irritability • Manic behavior • Decreased attention span • Enlarged spleen • Goiter • Muscle weakness & wasting • Increased libido • Amenorrhea • Inability to perform ADLs, (Rebar, Ignatavicius, & Workman, 2017, p 1264) • Arthritis • Psychological stress • Kidney stones • Excessive urination • Abdominal pain • Bone & joint pain • Depression • Forgetfulness, (Rebar, Ignatavicius, & Workman, 2017 p 1276) Nursing Role in Multidimensional Care • Monitor orthostatic BP (lying, sitting, & standing) • Assess HR & pulse when patient is sleeping • Auscultate heart sounds • Monitor ECG • Auscultate breath sounds • Monitor temperature • Observe s/s of polydipsia, dry mucous membranes, weak or thread pulse, poor capillary refill, oliguria, & hypotension • Weigh daily • Avoid foods that increase peristalsis & that cause diarrhea • Provide information about s/s of hypothyroidism & the need for continuous follow-up care, (Vera, • Monitor vitals, EKG, renal stones (strain urine), calcium, & phosphate levels • Monitor I&Os & fluid status • Diet low in calcium & high in phosphate • Provide IV fluids (normal saline for hydration & loop diuretics to decrease calcium levels • Adjust activities & reduce intensity level • Assist patients with activities/monitor clients use of assistive device such as a walker, cane, (RegisteredNurseRN, 2017).ENDOCRINE DISORDERS GUIDE 4 2019). Evaluate Responses to Interventions Taken • Nonsurgical management: • Monitoring includes measuring the patient’s apical pulse, BP, & temperature at least Q4H. Instruct patient to report immediately any palpitations, dyspnea, vertigo, or chest pain. Increases in temperature may indicate a rapid worsening of the patient’s condition & the onset of thyroid storm. If patient has a cardiac monitor, check for dysrhythmias. • Reducing stimulation helps prevent increasing the symptoms of hyperthyroidism & the risk for cardiac complications. Encourage the patient to rest. Keep the environment as quiet as possible. • Promoting comfort includes reducing the room temperature to decrease discomfort cause by heat intolerance. Suggest the patient take a cool shower or sponge bather several times each day. Patients with exophthalmos, prevent eye dryness by encouraging use of artificial tears. • Drug therapy (antithyroid drugs) initial treatment, such as thionamides, esp. methimazole (Tapazole). Propylthiouracil (PTU) is used less often because of its liver toxic effects. Response to these drugs are delayed because the patient may have large amounts of stored thyroid hormones that continue to be released. • Radioactive iodine (RAI) therapy not used in pregnant women. Can be given in oral form, with dosage depending on the thyroid gland’s size & sensitivity to radiation. Radiation precautions are needed to prevent exposure to family • Nonsurgical management: • Diuretic & hydration therapies help reduce serum calcium levels in patients who have milder disease. Usually furosemide (Lasix), a diuretic that increases kidney secretion of calcium, is used along with IV saline in large volumes to promote calcium excretion. • Drug therapy for patients who have more severe symptoms of hyperparathyroidism involves the use of cinacalcet (Sensipar), a calcimimetic. For patients who do not respond to cinacalcet, oral phosphates are used to inhibit bone resorption & interfere with calcium absorption. • Monitor cardiac function & I&O Q2H during hydration therapy. Compare recent ECG tracings with the patient’s baseline tracings. • Preventing injury is important because the patient with chronic hyperparathyroidism often has significant bone density loss & is at risk for fractures, (Rebar, Ignatavicius, & Workman, 2017, p 1276). • Surgical management: (parathyroidectomy) calcium levels are decreased to near normal for the patient. Nursing care before & after surgical removal of the parathyroid glands is the same as that for thyroidectomy. Check serum calcium levels whenever they are drawn until calcium levels stabilize. Monitor for hypocalcemia, check for Trousseau’s & Chvostek’s signs, which indicate potential tetany.ENDOCRINE DISORDERS GUIDE 5 members & other people, (Rebar, Ignatavicius, & Workman, 2017, p 1267). • Surgical management: • Preoperative- patient is treated with thionamide drug therapy first. • Monitoring the patient for complications is the most important nursing action after thyroid surgery. (Monitor vital signs every 15 minutes until the patient is stable & then every 30 minutes. • Hemorrhage is most likely to occur during the first 24 hours after surgery. Inspect the neck dressing & behind the patient’s neck for blood. A moderate amount of serosanguineous drainage is normal. • Respiratory distress & reduced gas exchange can result from swelling, tetany, or damage to the laryngeal nerve, resulting in spasms. Monitor the patient to identify symptoms of obstruction & poor gas exchange after thyroid surgery. • Hypocalcemia & tetany may occur if the parathyroid glands are removed or damaged or their blood supply is impaired during thyroid surgery, resulting in decreased PTH levels. • Laryngeal nerve damage may occur during surgery. This results in hoarseness & a weak voice. Assess patients voice at 2-hour intervals, (Rebar, Ignatavicius, & Workman, 2017, p 1269). Assess the patient for changes in voice patterns & hoarseness due to possible recurrent laryngeal nerve damage during surgery. If all else fails, lifelong treatment with calcium & vitamin D will be necessary, (Rebar, Ignatavicius, & Workman, 2017, p 1277).ENDOCRINE DISORDERS GUIDE 6 [Show More]
Last updated: 1 year ago
Preview 1 out of 6 pages

Reviews( 0 )
Document information
Connected school, study & course
About the document
Uploaded On
Apr 14, 2022
Number of pages
6
Written in
Additional information
This document has been written for:
Uploaded
Apr 14, 2022
Downloads
0
Views
39

.png)








 Rasmussen College.png)