NR-509 Week 7 Comprehensive Health History SOAP Note
Document Content and Description Below
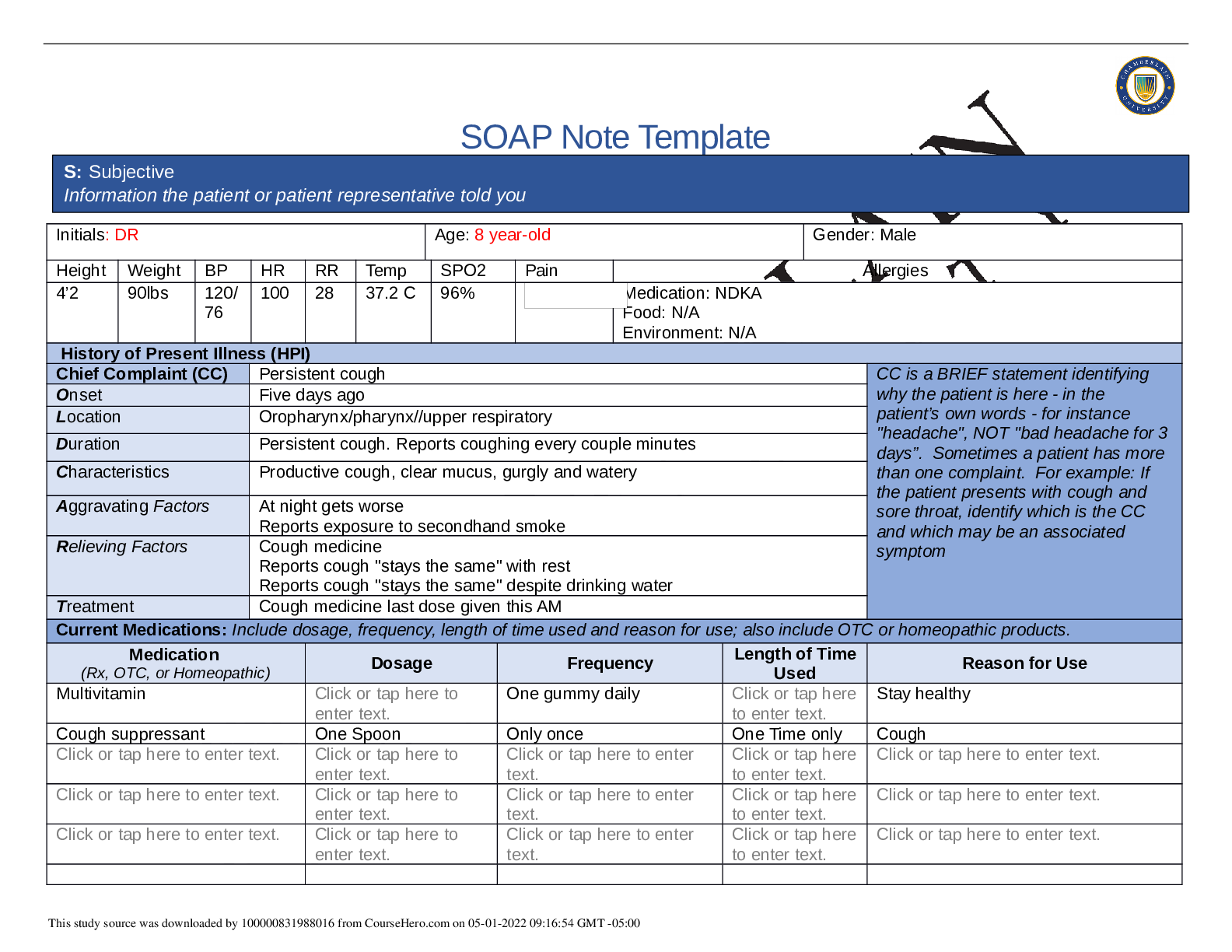
SOAP Note Template Initials: DR Age: 8 year-old Gender: Male Height Weight BP HR RR Temp SPO2 Pain Allergies 4’2 90lbs 120/ 76 100 28 37.2 C 96% Medication: NDKA Food: N/A Environment: N/A ... History of Present Illness (HPI) Chief Complaint (CC) Persistent cough CC is a BRIEF statement identifying why the patient is here - in the patient’s own words - for instance "headache", NOT "bad headache for 3 days”. Sometimes a patient has more than one complaint. For example: If the patient presents with cough and sore throat, identify which is the CC and which may be an associated symptom Onset Five days ago Location Oropharynx/pharynx//upper respiratory Duration Persistent cough. Reports coughing every couple minutes Characteristics Productive cough, clear mucus, gurgly and watery Aggravating Factors At night gets worse Reports exposure to secondhand smoke Relieving Factors Cough medicine Reports cough "stays the same" with rest Reports cough "stays the same" despite drinking water Treatment Cough medicine last dose given this AM Current Medications: Include dosage, frequency, length of time used and reason for use; also include OTC or homeopathic products. Medication (Rx, OTC, or Homeopathic) Dosage Frequency Length of Time Used Reason for Use Multivitamin Click or tap here to enter text. One gummy daily Click or tap here to enter text. Stay healthy Cough suppressant One Spoon Only once One Time only Cough Click or tap here to enter text. Click or tap here to enter text. Click or tap here to enter text. Click or tap here to enter text. Click or tap here to enter text. Click or tap here to enter text. Click or tap here to enter text. Click or tap here to enter text. Click or tap here to enter text. Click or tap here to enter text. Click or tap here to enter text. Click or tap here to enter text. Click or tap here to enter text. Click or tap here to enter text. Click or tap here to enter text. S: Subjective Information the patient or patient representative told you This study source was downloaded by 100000831988016 from CourseHero.com on 05-01-2022 09:16:54 GMT -05:00 Past Medical History (PMHx) – Includes but not limited to immunization status (note date of last tetanus for all adults), past major illnesses, hospitalizations, and surgeries. Depending on the CC, more info may be needed. - No surgical history - No prior hospitalizations - Pneumonia last year(treated at urgent care unit) - Earaches - No influenza vaccine in the last 12 months - Last physical exam exam two months ago - Denies ER visit - Hep B- 3- dose series completed at 6 mos. - Hep A- 2-dose series completed at 15 mos. - Pneumococcal -4-dose series completed at 15 mos. - DTaP- 5 dose series completed at 6 years - MMR- 2-dose series completed at 6 years - Varicella-2-dose series completed at 6 years - Polio- 4-dose series completed at 6 years Social History (Soc Hx) - Includes but not limited to occupation and major hobbies, family status, tobacco and alcohol use, and any other pertinent data. Include health promotion such as use seat belts all the time or working smoke detectors in the house. -3rd grade -Attendance record: out for two weeks last year due to Pneumonia -Lives with mother, father, grandmother, and grandpather. Grandmother provides care when parents working. -English primarily spoken at home, but some Spanish is used -Hobbies: Likes to play video games, read and write stories -Exposure to secondhand smoke Family History (Fam Hx) - Includes but not limited to illnesses with possible genetic predisposition, contagious or chronic illnesses. Reason for death of any deceased first degree relatives should be included. Include parents, grandparents, siblings, and children. Include grandchildren if pertinent. Mother: Type II DM, HTN, hypercholesterolemia, spinal stenosis, obesity Father: Smoker, HTN, hypercholesterolemia, asthma as a child. Maternal grandmother: Type 2 diabetes & HTN Maternal grandfather: Smoker, eczema Paternal grandmother: Died in a car accident (52 years old) This study source was downloaded by 100000831988016 from CourseHero.com on 05-01-2022 09:16:54 GMT -05:00 Paternal grandfather: No known history Review of Systems (ROS): Address all body systems that may help rule in or out a differential diagnosis Check the box next to each positive symptom and provide additional details. Constitutional Skin HEENT ☐Fatigue denies ☐Weakness denies ☐Fever/Chills denies ☐Weight Gain denies ☐Weight Loss denies ☒Trouble Sleeping Due to cough ☐Night Sweats denies ☒Other: More tired because cough keeps him up during at night ☐Itching denies ☐Rashes denies ☐Nail Changes denies ☐Skin Color Changes denies ☐Other: Click or tap here to enter text. ☐Diplopia denies ☐Eye Pain denies ☐Eye redness denies ☐Vision changes denies ☐Photophobia denies ☐Eye discharge denies ☒Earache 3/10 Right ear, since yesterday ☐Tinnitus denies ☐Epistaxis denies ☐Vertigo Click or tap here to enter text. ☐Hearing Changes denies ☐Hoarseness denies ☐Oral Ulcers denies ☒Sore Throat For five days ☐Congestion denies ☒Rhinorrhea Click or tap here to enter text. ☐Other: Click or tap here to enter text. Respiratory Neuro Cardiovascular ☒Cough For five days ☐Hemoptysis denies ☐Dyspnea denies ☐Wheezing Click or tap here to enter text. ☐Pain on Inspiration denies ☒Sputum Production ☒Other: Clear color sputum production ☐Syncope or Lightheadedness denies ☐Headache denies ☐Numbness denies ☐Tingling denies ☐Sensation Changes ☐Speech Deficits denies ☐Other: Click or tap here to enter text. ☐Chest pain denies ☐SOB denies ☐Exercise Intolerance denies ☐Orthopnea denies ☐Edema denies ☐Murmurs denies ☐Palpitations denies ☐Faintness denies ☐OC Changes denies ☐Claudications denies ☐PND denies ☐Other: Click or tap here to enter text. MSK GI GU PSYCH This study source was downloaded by 100000831988016 from CourseHero.com on 05-01-2022 09:16:54 GMT -05:00 ☐Pain denies ☐Stiffness denies ☐Crepitus denies ☐Swelling denies ☐Limited ROM ☐Redness denines ☐Misalignment denies ☐Other: Click or tap here to enter text. ☐Nausea/Vomiting denies ☐Dysphasia denies ☐Diarrhea denies ☐Appetite Change denies ☐Heartburn denies ☐Blood in Stool denies ☐Abdominal Pain denies ☐Excessive Flatus denies ☐Food Intolerance denies ☐Rectal Bleeding denies ☐Other: Click or tap here to enter text. ☐Urgency denies ☐Dysuria denies ☐Burning denies ☐Hematuria denies ☐Polyuria denies ☐Nocturia denies ☐Incontinence denies ☒Other: urinate every two hours ☐Stress denies ☐Anxiety denies ☐Depression denies ☐Suicidal/Homicidal Ideation denies ☐Memory Deficits denies ☐Mood Changes denies ☐Trouble Concentrating denies ☐Other: Click or tap here to enter text. GYN ☐Rash Click or tap here to enter text. ☐Discharge Click or tap here to enter text. ☐Itching Click or tap here to enter text. ☐Irregular Menses n/a ☐Dysmenorrhea n/a ☐Foul Odor Click or tap here to enter text. ☐Amenorrhea n//a ☐LMP: n/a ☐Contraception Click or tap here to enter text. ☐Other: O: Objective Information gathered during the physical examination by inspection, palpation, auscultation, and palpation. If unable to assess a body system, write “Unable to assess”. Document pertinent positive and negative assessment findings. This study source was downloaded by 100000831988016 from CourseHero.com on 05-01-2022 09:16:54 GMT -05:00 Body System Positive Findings Negative Findings General Patient present to the clinic complaining of persistent cough for the last 5 days, sore throat, and ear pain. AAOX3, pleasant and cooperative, 8 year-old Hispanic male, seated on the exam table without acute physical distress Skin Click or tap here to enter text. Skin warm, dry and intact HEENT Nasal cavities with clear discharge Erythemic color observed on right auditory canal Erythemic color observed on right tympanic membrane. Erythema present on tonsils Erythemic posterior oropharynx color. Cobblestoning Posterior Oropharynx Texture Cervical lymph nodes enlarged on right side -Head normocephalic and atraumatic -Inspected eyes and sclera: -Orbital area with no visible abnormal findings bilaterally. Sclera white on both eyes. Conjuctiva moist and pink -Nasal cavities, pink color, turbinates are patent B/L with no additional visible abnormal findings. -Ears: No visible abnormal findings on Right tympanic membrane. Right cone of light: 5:00. No discharge observed on right ear. -Pink color observed on Left auditory canal and left tympanic membrane pearly gray No visible abnormal findings on L tympanic membrane. Left cone of light: 7:00 No discharge observe on left ear. Oral mucosa moist and pink. No post nasal drip observed Neck symmetric with no vissible abnormal findings, trachea midline, no thyroid enlargement or tenderness Palpated frontal sinuses: no tenderness reported Palpated maxillary sinuses: No tenderness reported Supraclavicular lymph nodes: Not palpable Axillary lymph nodes: Not palpable [Show More]
Last updated: 1 year ago
Preview 1 out of 9 pages
Also available in bundle (1)
NR 509 SOAP Note Altogether Weeks 1 – 7
NR 509 SOAP Note Altogether Weeks 1 – 7
By Nutmegs 1 year ago
$35
9
Reviews( 0 )
Recommended For You
*NURSING> SOAP NOTE > Summary NR 509 Week 1 Health History SOAP Note (All)
Summary NR 509 Week 1 Health History SOAP Note
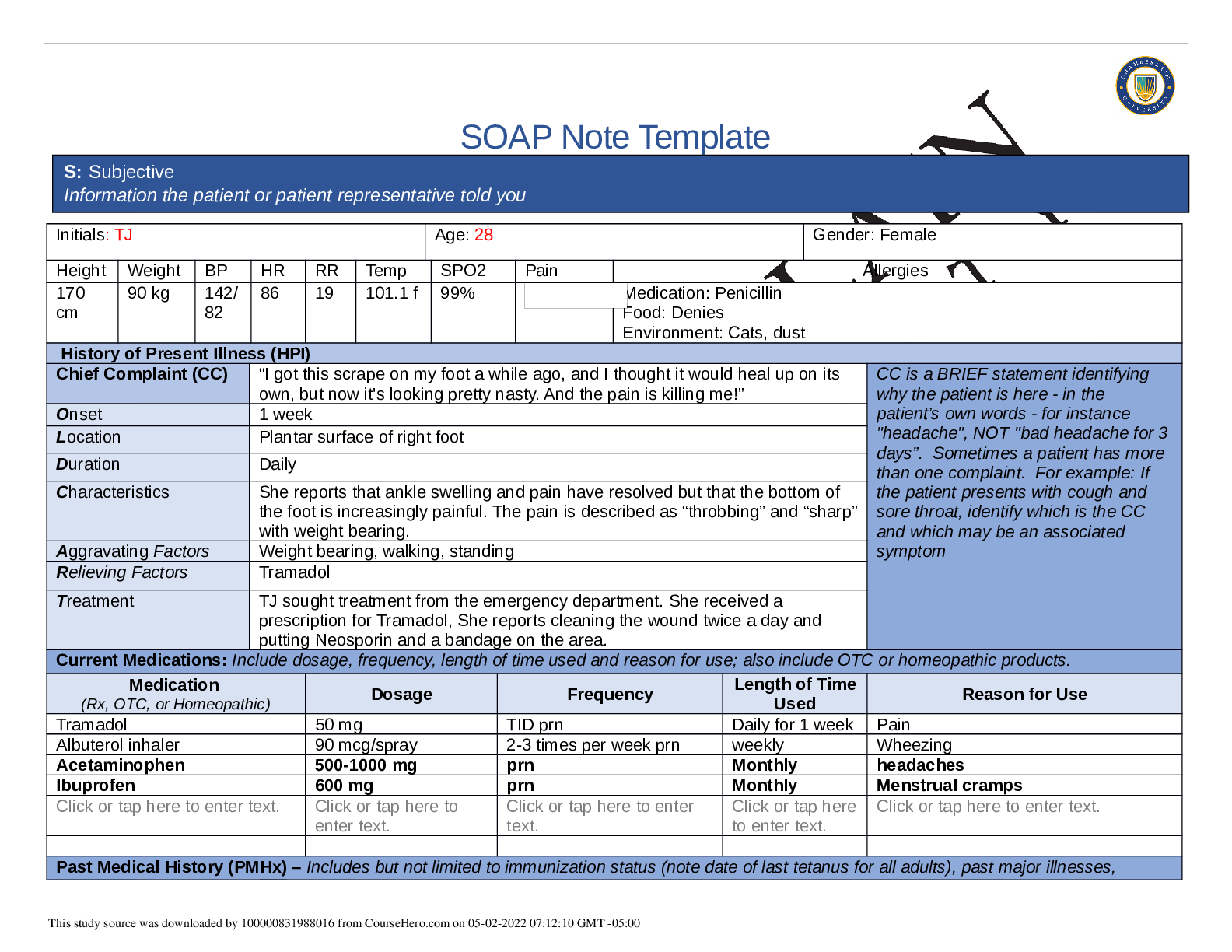
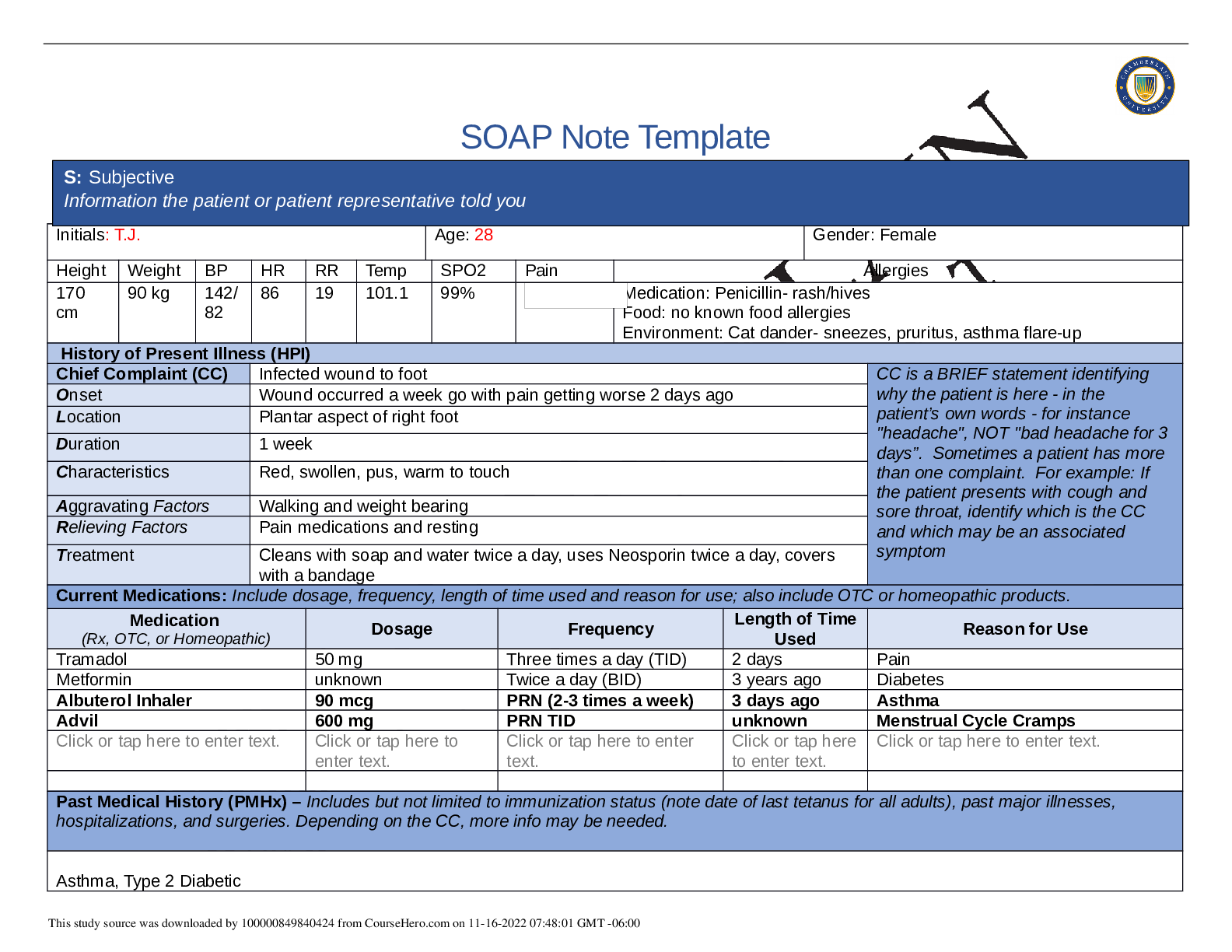
SOAP Note Template Initials: TJ Age: 28 Gender: Female Height Weight BP HR RR Temp SPO2 Pain Allergies 170 cm 90 kg 142/ 82 86 19 101.1 f 99% Medication: Penicillin Food: Denies Environment:...
By Nutmegs , Uploaded: May 02, 2022
$9
*NURSING> SOAP NOTE > NR 509 Week 1 Health History SOAP Note (All)
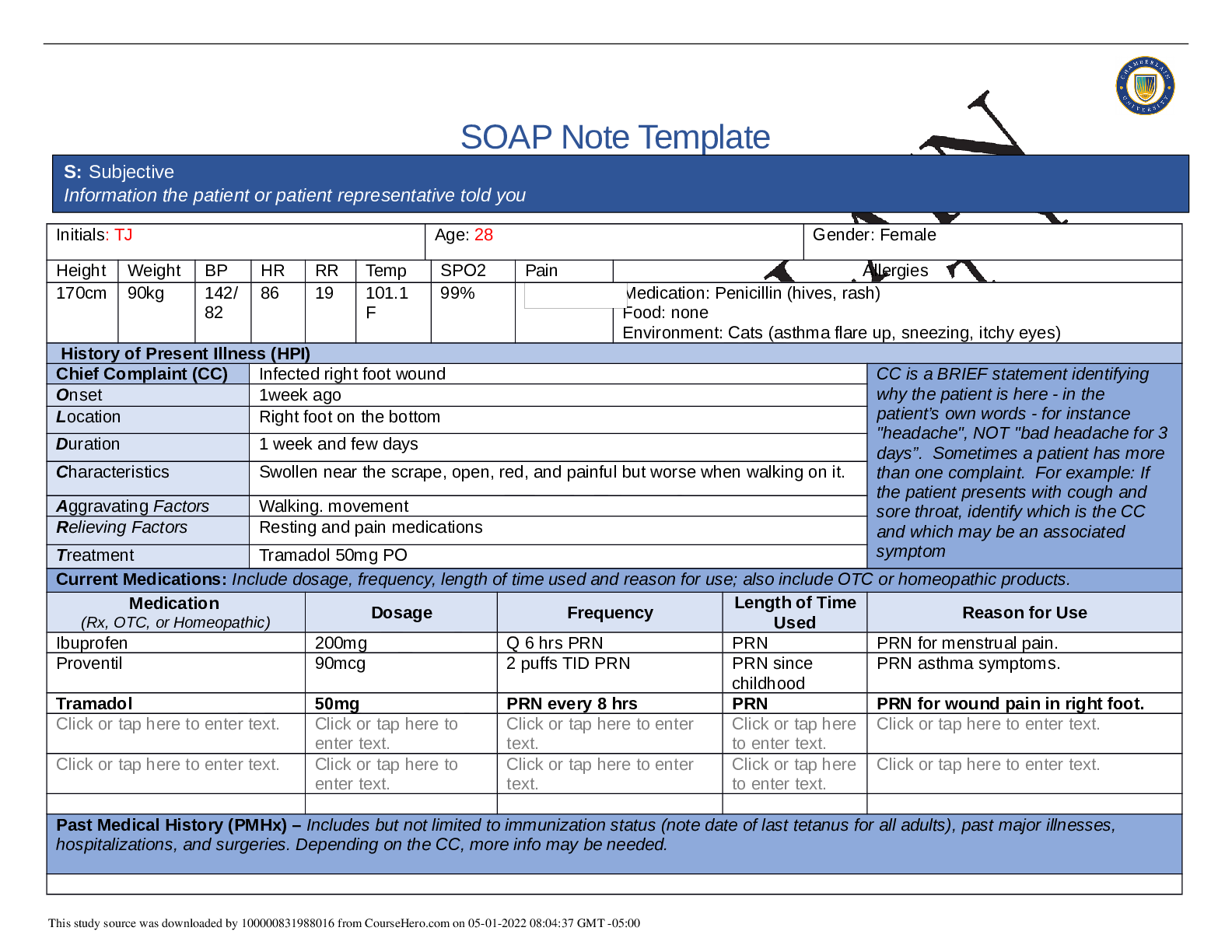
NR 509 Week 1 Health History SOAP Note
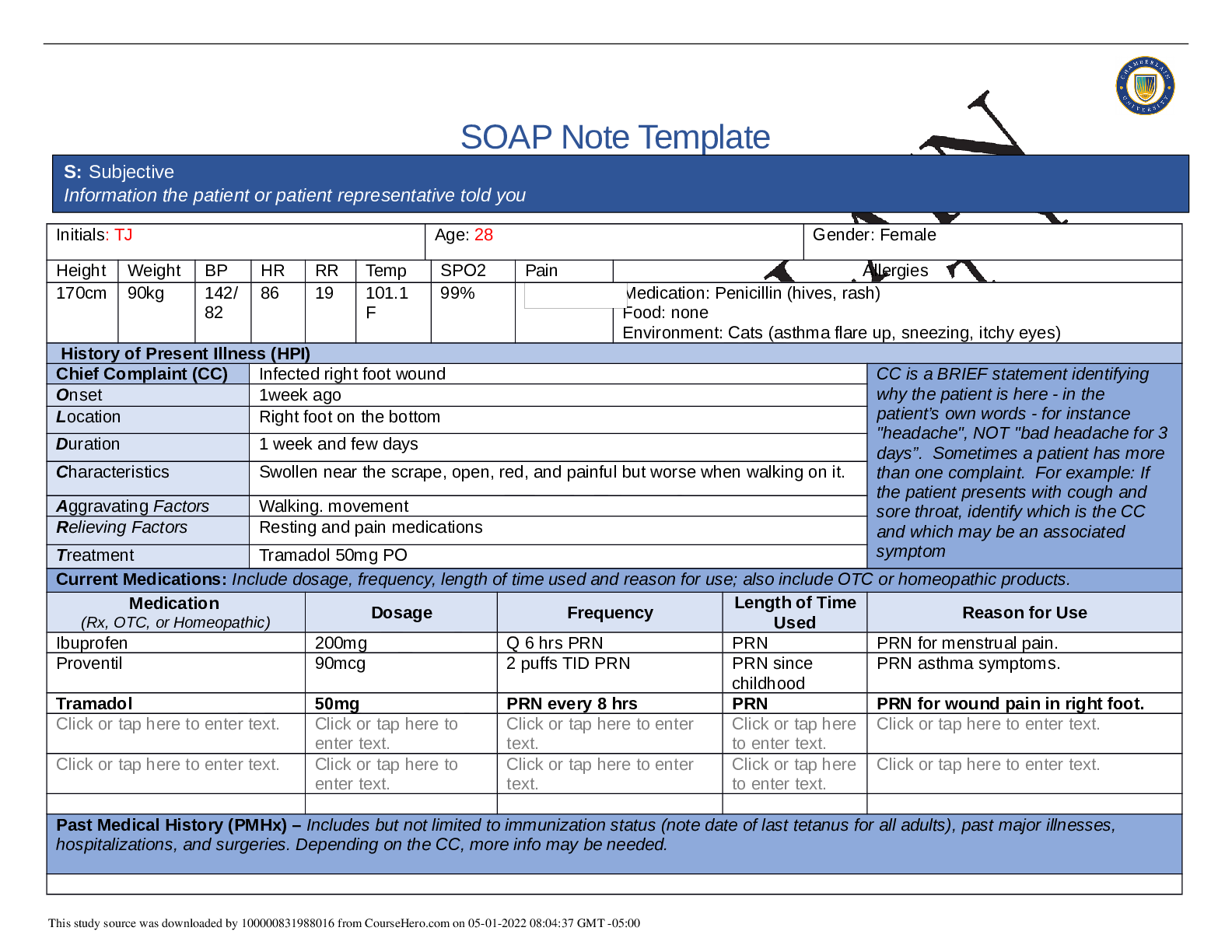
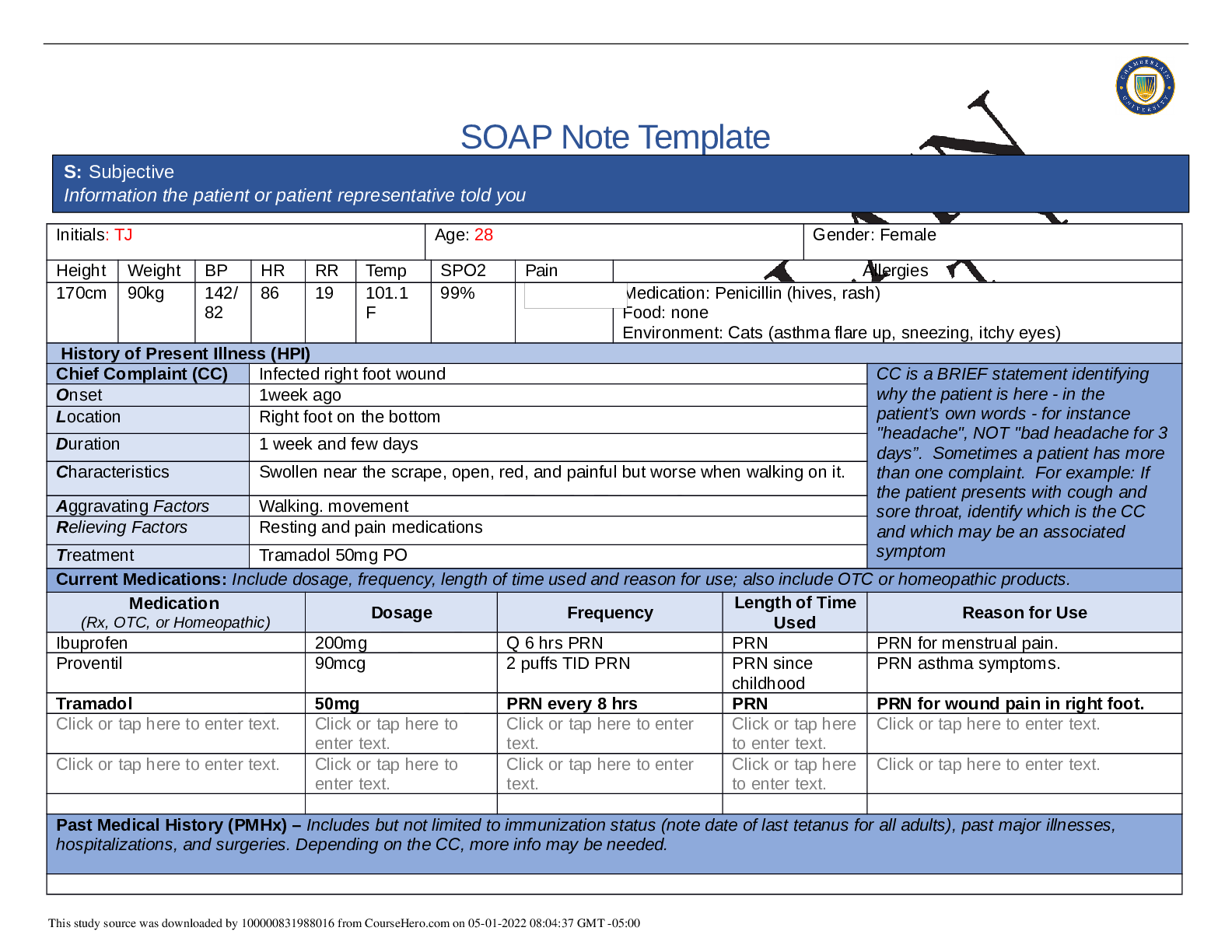
SOAP Note Template Initials: TJ Age: 28 Gender: Female Height Weight BP HR RR Temp SPO2 Pain Allergies 170cm 90kg 142/ 82 86 19 101.1 F 99% Medication: Penicillin (hives, rash) Food: none Env...
By Nutmegs , Uploaded: May 01, 2022
$9
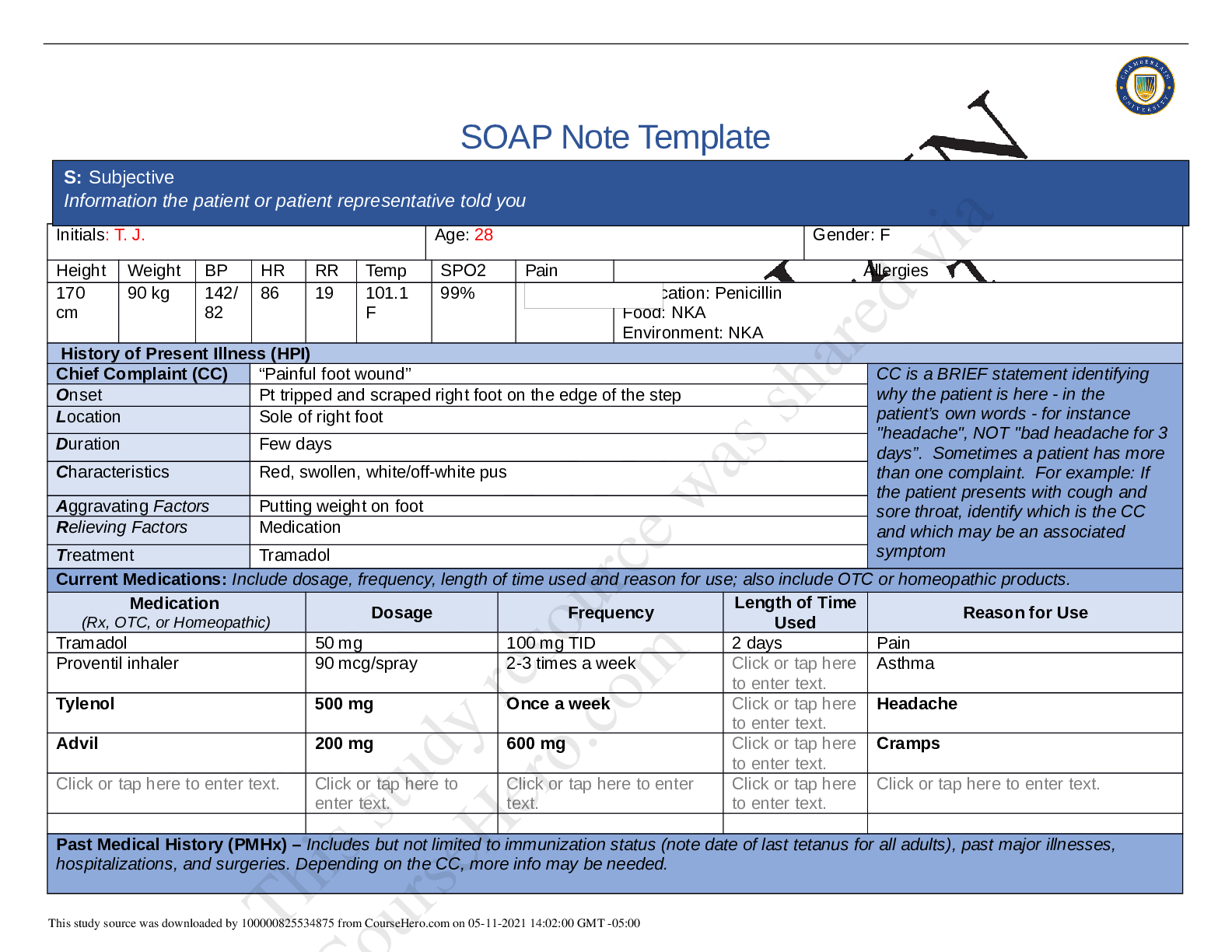
*NURSING> SOAP NOTE > NR 509 Week 1 Health History SOAP Note (All)
NR 509 Week 1 Health History SOAP Note
NR 509 SOAP Notes/NR 509 Advanced Physical Assessment/NR 509 SOAP Notes/NR 509 Advanced Physical Assessment/NR 509 SOAP Notes/NR 509 Advanced Physical Assessment/NR 509 SOAP Notes/NR 509 Advanced Phys...
By LAVIE , Uploaded: Apr 18, 2021
$13
*NURSING> SOAP NOTE > NR 509 Week 1 Health History SOAP Note (All)
NR 509 Week 1 Health History SOAP Note
NR 509 Week 1 Health History SOAP Note
By PROF , Uploaded: Feb 19, 2021
$17
*NURSING> SOAP NOTE > NR-509 Week 7 Comprehensive Health History SOAP Note (All)
NR-509 Week 7 Comprehensive Health History SOAP Note
NR-509 Week 7 Comprehensive Health History SOAP Note
By PROF , Uploaded: Feb 19, 2021
$15
*NURSING> SOAP NOTE > Summary NR 509 Week 1 Health History SOAP Note (All)

Summary NR 509 Week 1 Health History SOAP Note
NR 509 Week 1 Health History SOAP Note S: Subjective – Information the patient or patient representative told you O: Objective – Information gathered during the physical examination by inspection, pal...
By Quality Suppliers , Uploaded: Nov 04, 2020
$9
*NURSING> SOAP NOTE > NR 509 Week 1 Health History SOAP Note (GRADED A) (All)
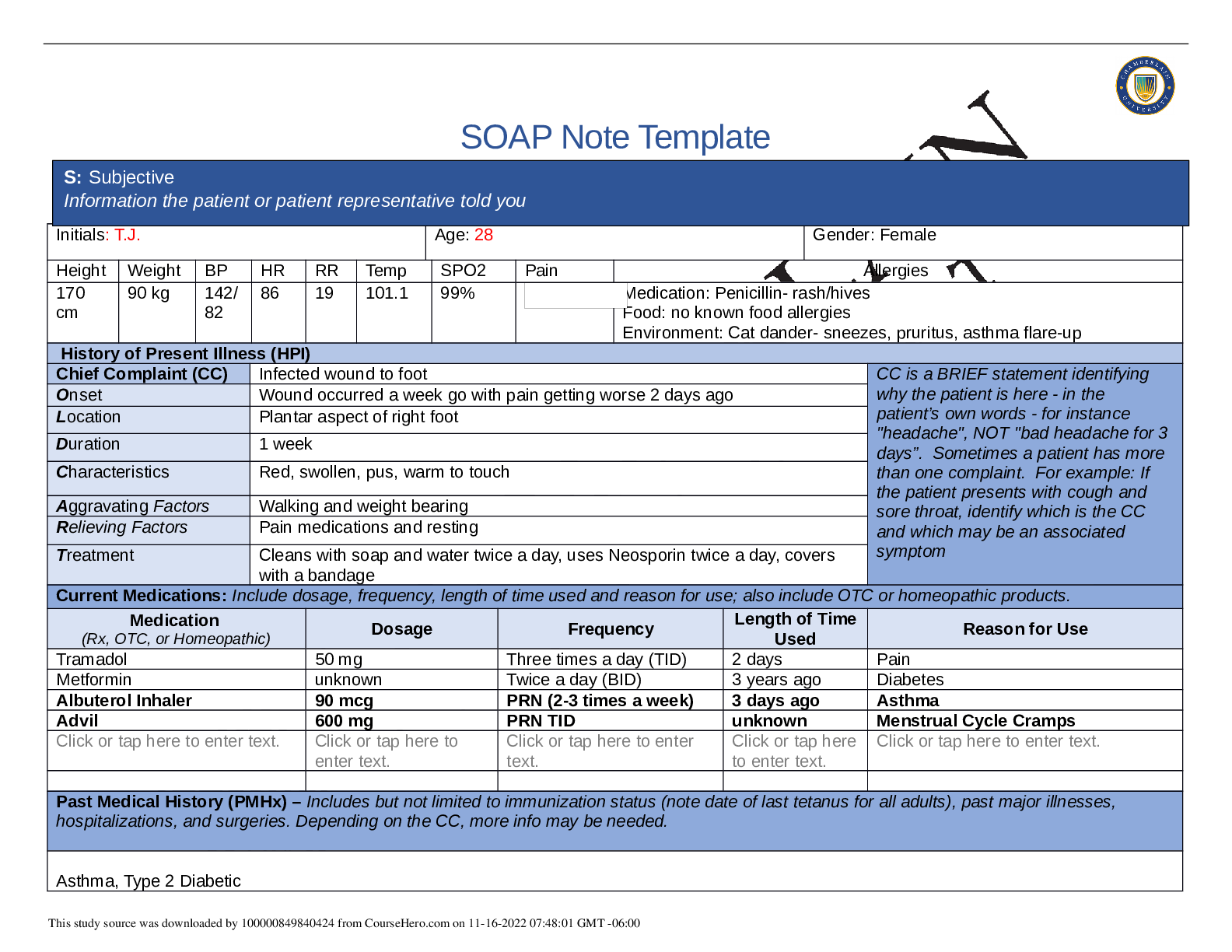
NR 509 Week 1 Health History SOAP Note (GRADED A)
SOAP Note Template S: Subjective Information the patient or patient representative told you Initials: T.J. Age: 28 Gender: Female Height Weight BP HR RR Temp SPO2 Pain Allergies 170 cm 90 kg 142...
By A+ Solutions , Uploaded: Nov 16, 2022
$12
*NURSING> SOAP NOTE > NRP 531Tom Walker, Episodic SOAP Note: Already graded A. (All)
NRP 531Tom Walker, Episodic SOAP Note: Already graded A.
Episodic SOAP Note: Tom Walker|NRP 531,Latest 2020 complete, Already graded A.
By Expert1 , Uploaded: Jul 18, 2020
$10
*NURSING> SOAP NOTE > NURS 112 SOAP Note Chest Pain Pennsylvania State University -Download To Score An A (All)
NURS 112 SOAP Note Chest Pain Pennsylvania State University -Download To Score An A
SOAP Note Chest Pain 1. Identifying data: Brain Foster is a 58-year-old Caucasian male. 2. Chief Complaint or Reason for Visit: he c/o having chest pain for 1 month. 3. History...
By Succeed , Uploaded: Aug 03, 2020
$9.5
Health Care> SOAP NOTE > SOAP Note: Cardiovascular Patient: Liam Fitzgerald SUBJECTIVE CC: “Routine follow up for his chronic conditions” (All)
SOAP Note: Cardiovascular Patient: Liam Fitzgerald SUBJECTIVE CC: “Routine follow up for his chronic conditions”
HPI: Mr. Fitzgerald is a 66-year-old male who presents via telehealth for a routine follow up on his chronic heart failure. He provided verbal consent for this telehealth visit. Mr. Fitzgerald repor...
By STUDY-GUIDENOTES , Uploaded: Oct 05, 2022
$7
Document information
Connected school, study & course
About the document
Uploaded On
May 01, 2022
Number of pages
9
Written in
Additional information
This document has been written for:
Uploaded
May 01, 2022
Downloads
0
Views
75






