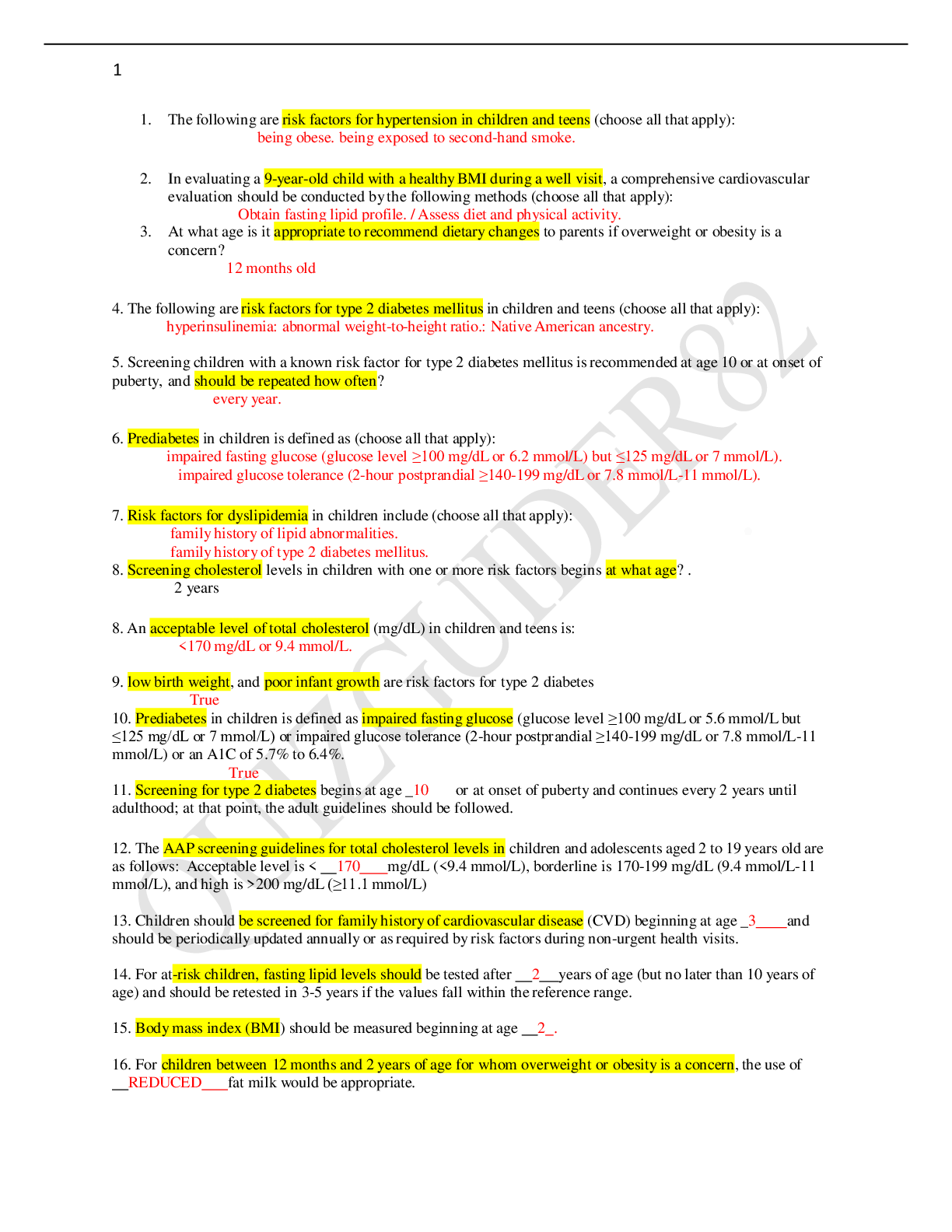
Exam Elaborations NR 566 final study guide
Document Content and Description Below
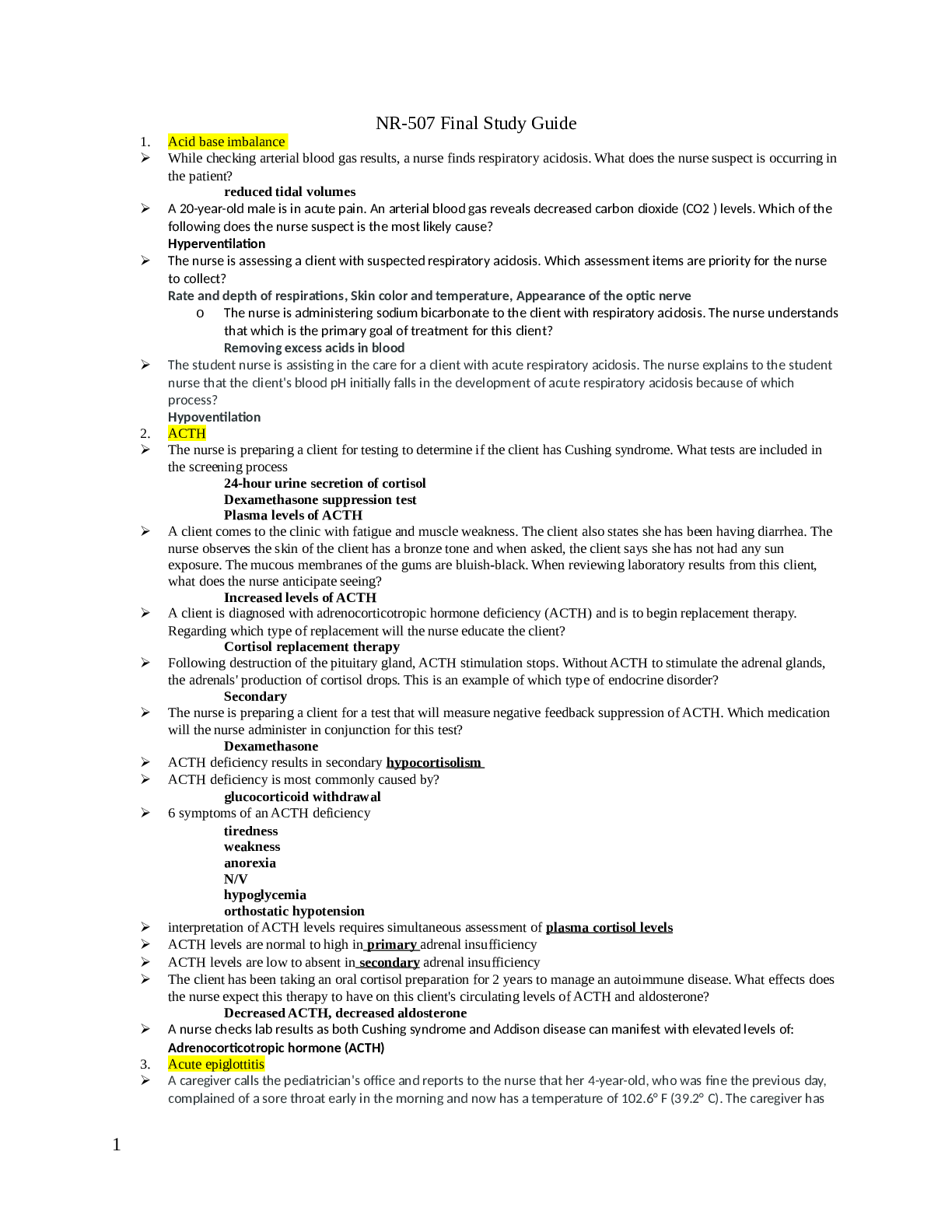
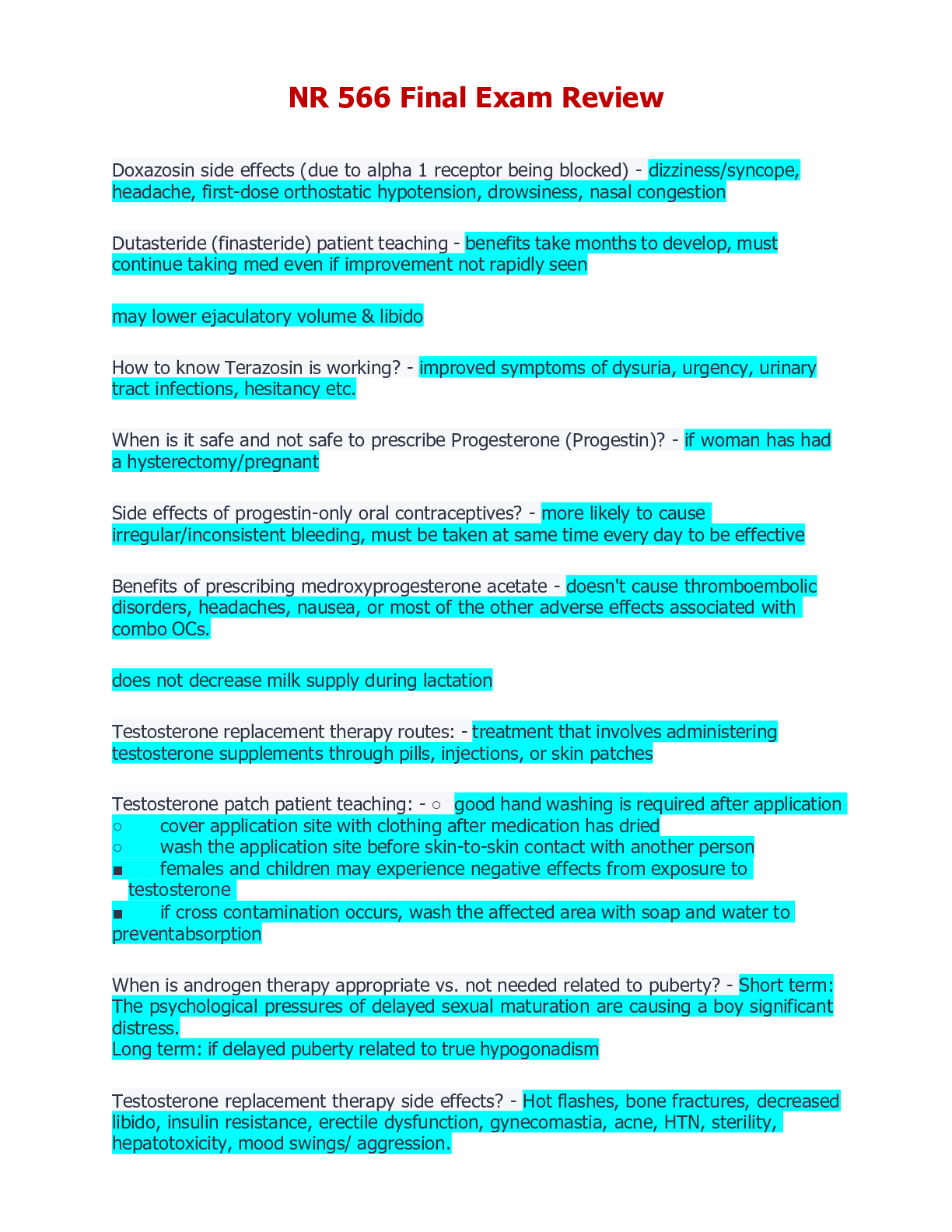
Know the pharmacodynamics, pharmacotherapeutics clinical use, drug interactions and adverse drug reactions for: Anticoagulants • Pharmacodynamics • Oral anticoagulants such as warfarin (Coumad in)... inhibit the hepatic synthesis of several clotting factors, including factor X. • Heparin inhibits the activity of several activated clotting factors by accelerating the activity of antithrombin III. • LMWH enoxaparin (Lovenox) potentiates the activity of antithrombin III and inactivates factors Xa and IIa (thrombin). • Dabigatran (Pradaxa) is a direct thrombin inhibitor. • Thrombin is required for the conversion of fibrinogen to fibrin in the clotting cascade, thus dabigatran's inhibition of thrombin prevents thrombi from forming. Fondaparinux (Arixtra) is a selective inhibitor of antithrombin III and a factor Xa inhibitor. Rivaroxaban (Xarelto) an anticoagulant, is a highly selective factor Xa inhibitor that inhibits thrombin formation and the development of thrombi. Apixaban (Eliquis) is a selective inhibitor of factor Xa. • Aspirin antagonizes the cyclooxygenase pathway and interferes with platelet aggregation. • NSAIDs have this same action. • NSAIDs are not used as antiplatelet drugs, but this explains why concurrent use with anticoagulants is contraindicated • Ticlopidine (Ticlid) and clopidogrel (Plavix) reduce platelet aggregation by inhibiting the ADP pathway of platelets. • Unlike aspirin, they have no effect on prostaglandin metabolism. • Ticagrelor (Brilinta) reversibly interacts with the platelet P2Y12 ADP-receptor to prevent platelet activation. • Vorapaxar (Zontivity) is a protease-activated receptor-1 (PAR-1) antagonist, inhibiting thrombin-induced and thrombin receptor agonist peptide-induced platelet aggregation • Pharmacotherapeutics: • Precautions and Contraindications • All anticoagulants are contraindicated for patients who are hypersensitive to the drug or actively bleeding or who have hemophilia, thrombocytopenia, severe HTN, intracranial hemorrhage, infective endocarditis, active tuberculosis, or ulcerative lesions of the GI tract. • Heparins are contraindicated in advanced hepatic or renal disease. • They may be used in patients who are actively bleeding to treat DIC • Heparin is Pregnancy Category C: stillbirth, prematurity • Some heparin preparations contain benzyl alcohol: known to cause “gasping syndrome”: • fatal toxicity in neonates • Hyperkalemia may develop • Use for patient with DM or renal insufficiency requires care and frequent monitoring of aPTT • Has been associated with fatal medication errors r/t different strengths of preparations • JCo: anticoagulant therapy is a National patient Safety Goal: plan in place at each facility to reduce patient harm • LMWHs are contraindicated for patients with allergies to pork, sulfites, or benzyl alcohol; uncontrolled bleeding; and in patients who have antiplatelet antibodies • Renal impairment: cautious use • Body weight less than 50 kg associated with increased r/f bleeding: • enoxaparin dose adjustment • Cautious use: untreated HTN, retinopathy (HTN or DM caused), severe liver disease, recent Hx of ulcer, or malignancy • Not used for thromboprophylaxis in patients with mechanical heart values: especially pregnant (r/f heart value thrombosis) • Enoxaparin: Preg Cat B, tinzaparin: teratogenicity and fetal death, fondaparinux: Preg B • First line drug for women who require antithrombotic therapy during pregnancy: LMWH • Pharmacokinetics of LMWH is altered during pregnancy • Warfarin • Hepatic dysfunction potentiates response through impaired synthesis of coagulation factors • Use with caution: Hypermetabolic states produced by fever or hyperthyroidism increase responsiveness to warfarin: • r/t increased catabolism of vit K dependent coagulation factors • Increased r/f bleeding in older adults • Caution use based on balance between potential for decreased r/f thromboembolism and the risk for bleeding especially in those with dementia or severe cognitive impairment: Hx of three falls in the previous year or recurrent injurious falls, uncontrolled HTN, or non-adherent or unreliable • Warfarin is Pregnancy Category X: Crosses placenta and can cause hemorrhagic disorders in the fetus and serious birth defects • Safe during lactation • Rivaroxaban (Xarelto): Black-Box Warning: premature discontinuation of anticoagulants including rivaroxaban may lead to thrombotic events. • An increased risk of stroke is seen in patients with atrial fibrillation when transitioning to warfarin • Rivaroxaban is Pregnancy Category C and is not recommended for use in pregnant women. • Apixaban (Eliquis): Black Box warning premature discontinuation leading to thrombotic events • Although there are no well-controlled studies: Pregnancy Category B • Hypersensitivity to aspirin and cross-sensitivity with NSAIDs may occur, contraindicating the drug • Aspirin hypersensitivity is more prevalent in patients with asthma, nasal polyps, or chronic urticaria. • Reye syndrome has been associated with its use in children and teenagers who have influenza or chickenpox. • Reversible hepatotoxicity has occurred • Use with caution in liver damage, preexisting hypoprothrombinemia, or vit K deficiency • Preg Cat C and Cat D in third trimester • Avoid during lactation • Clopidogrel and ticlopidine: severe hepatic disease (r/f bleeding d/o), do not use in these patients • Not recommended for patients with GI d/o • Preg Category B • Ticlopidine: clearance increased with age, older adults increased sensitivity to this drug (closely monitor or ADRs) • Older adults: increased levels of clopidogrel: no dosage adjustments • In older adults clopidogrel is a safer drug • Ticlopidine: elevations in cholesterol and TC within 1 month of therapy: factor in HLD • Ticagrelor: Black-Box Warning to not use in a patient with active pathological bleeding or history of intracranial hemorrhage. • Ticagrelor should be discontinued 5 days prior to any surgery. • Dabigatran: Black-Box Warning concerning discontinuation increasing risk of thrombotic events. • There is no reversal agent available for dabigatran • Vorapaxar: Black-Box Warning to not use in patients with a history of stroke, TIA, intracranial hemorrhage, or active pathological bleeding. • Vorapaxar is Pregnancy Category B, with no congenital malformations found in animal studies • ADRs • All anticoagulants: excessive bleeding • Risk is higher early in therapy, with wide fluctuations in aPTT or INR, and older adults (especially women over 60) • Heparins: cause thrombocytopenia and anemia • More likely with bovine than with porcine • Early thrombocytopenia 2 to 3 days after starting therapy and delayed forms 7 to 12 days • Platelet below 100,000: d/c heparin • Enoxaparin antidote: protamine sulfate 1 mg for each mg of enoxaparin dalteparin and tinzaparin: 1 mg for each 100 anti-Xa IUs of dalteparin • Slow IV injection • Fondaparinux: no known antidote • Heparin has a short half-life: Tx is usually d/c of the drug • Protamine sulfate antidote for heparin OD • Warfarin: toxicity and OD Tx withholding one or more doses • Or 1 to 10 mg of vitamin K is the antidote for minor bleeding • 5 to 50 may be used for frank bleeding • Hemorrhagic skin necrosis in women and cyanotic toes in men have been reported • r/t transient inhibition in proteins S and C • Allergic reactions: symmetrical, maculopapular, erythematous lesions • Some are isolated and some confluent: face, neck, and torso • May not appear until 8 to 10 days • Ribaroxaban: bleeding is major ADR • No reversal agent • Back pain, upper ABD pain, osteoarthritis, dyspepsia, and fatigue • Apixaban: bleeding • No reversal agent • ASA: gastric erosions: increased r/f serious upper GI bleeding • More likely when used in combo with other anticoags such as warfarin • Salicylism (tinnitus) : serum levels above 200 mcg/mL • Toxicity: tinnitus, HA, hyperventilation, agitation, confusion, lethargy, diarrhea, and sweating • Ticagrelor: bleeding • Dyspnea: sometimes improves with use or must be d/c • HA, cough, dizziness, and nausea • Ticlopidine: reversible neutropenia at 3 weeks to 3 months after initiation of therapy • Severe [Show More]
Last updated: 1 year ago
Preview 1 out of 93 pages

Reviews( 0 )
Document information
Connected school, study & course
About the document
Uploaded On
May 19, 2022
Number of pages
93
Written in
Additional information
This document has been written for:
Uploaded
May 19, 2022
Downloads
0
Views
47



 Complete solutions.png)
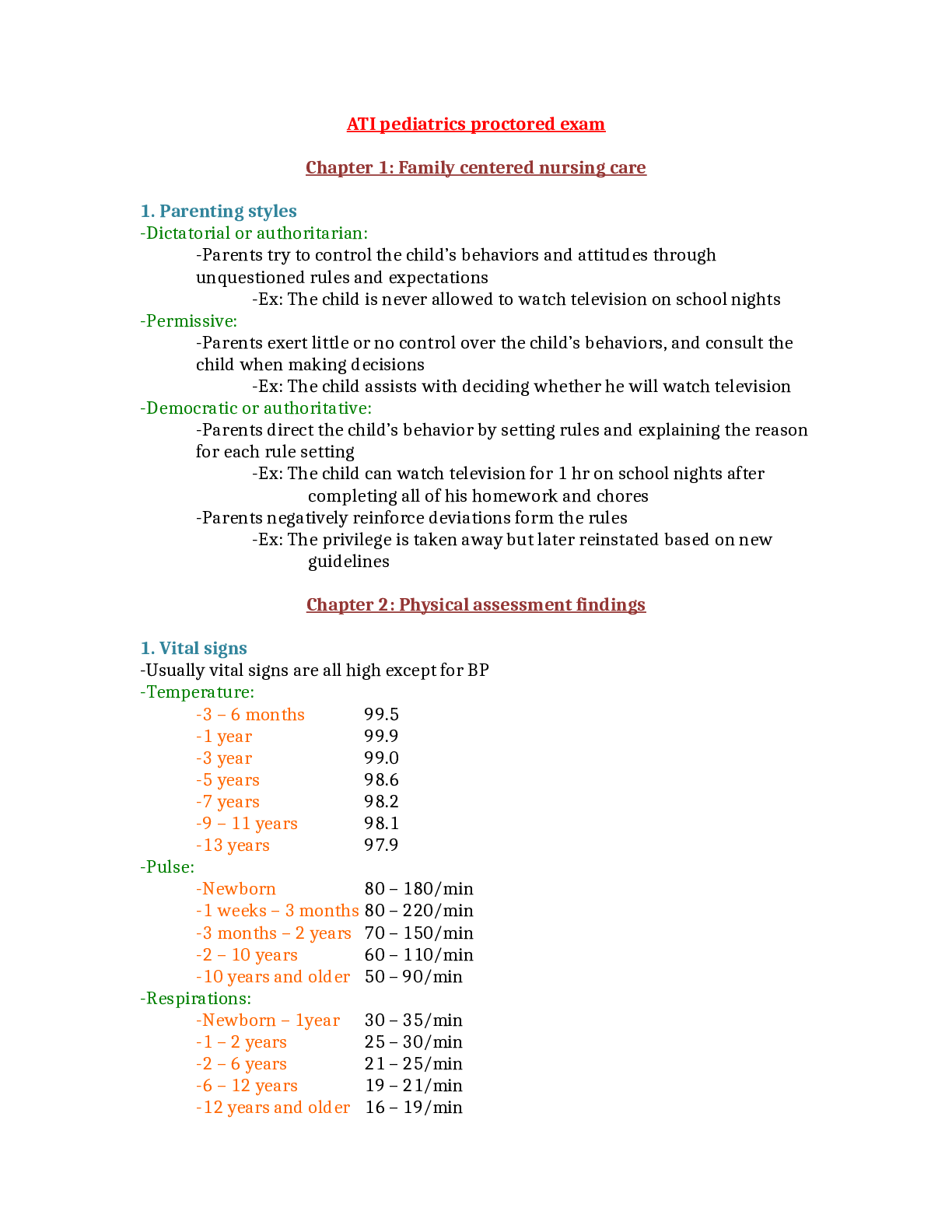
 NURS 3247Pharmacology - Proctored Assessment,.png)
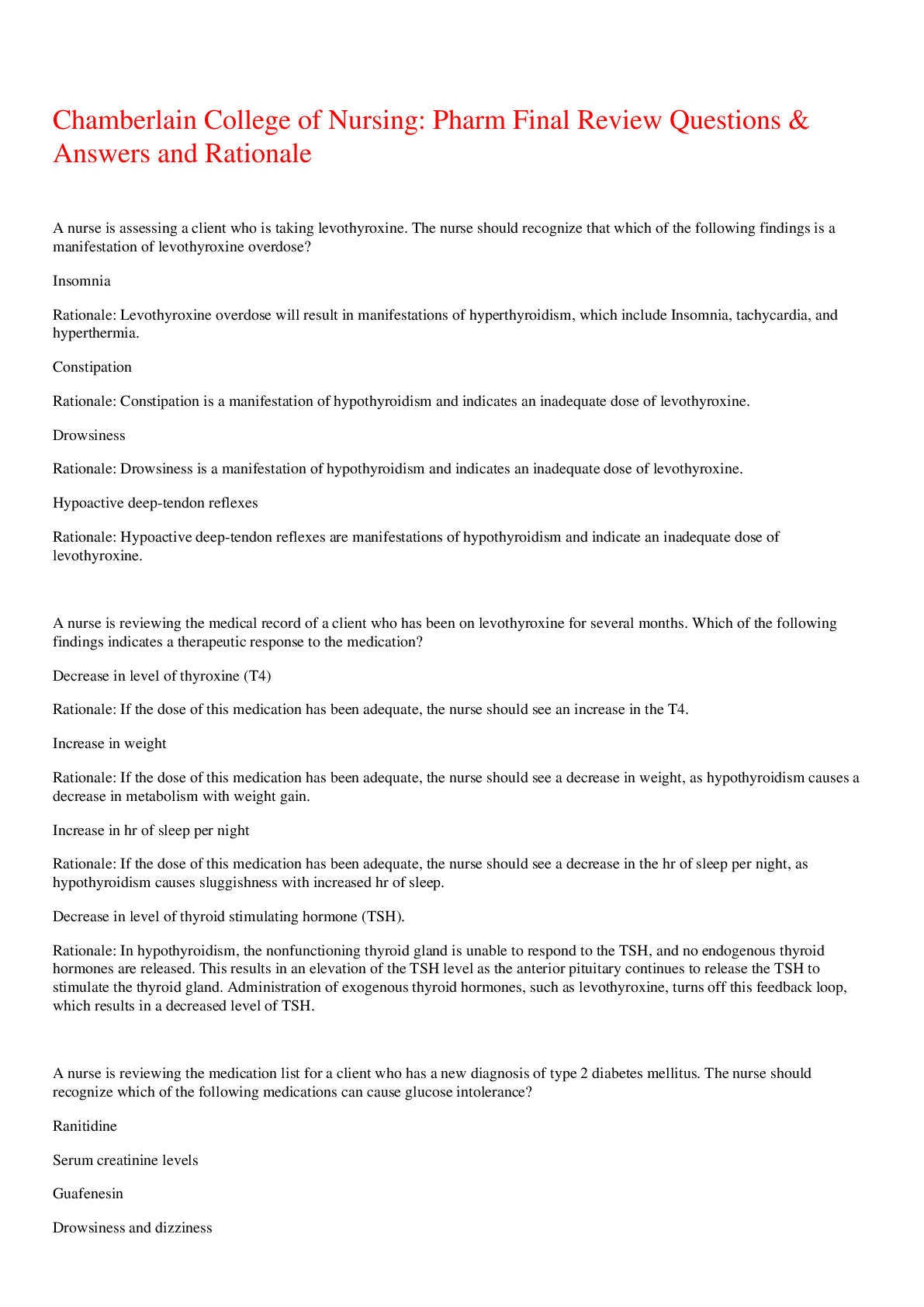
 Advanced Pharmacology for Care of the Family- Chamberlain.png)