*NURSING > EXAM REVIEW > NR-511 Week 8 Final Exam (Review) | Download To Score An A (All)
NR-511 Week 8 Final Exam (Review) | Download To Score An A
Document Content and Description Below
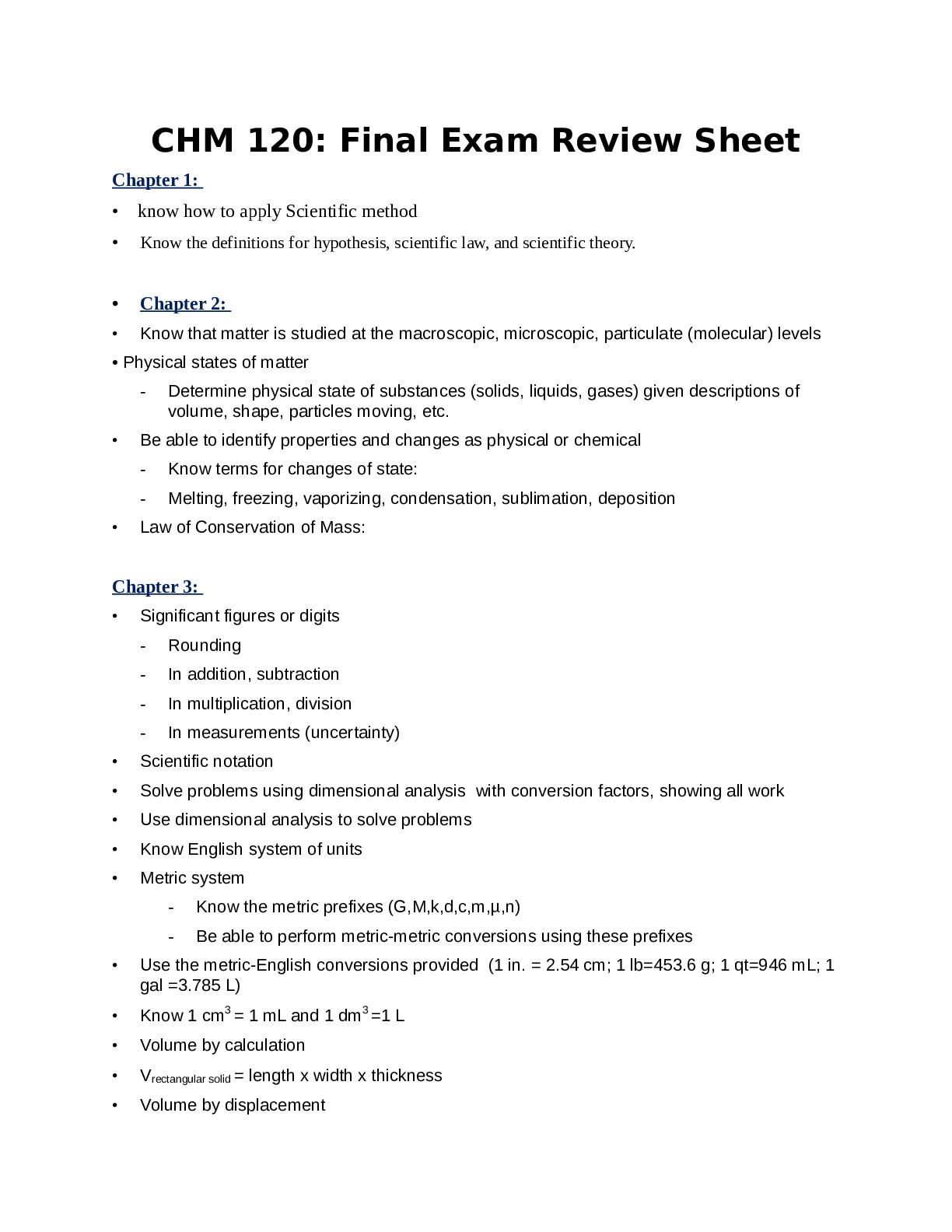
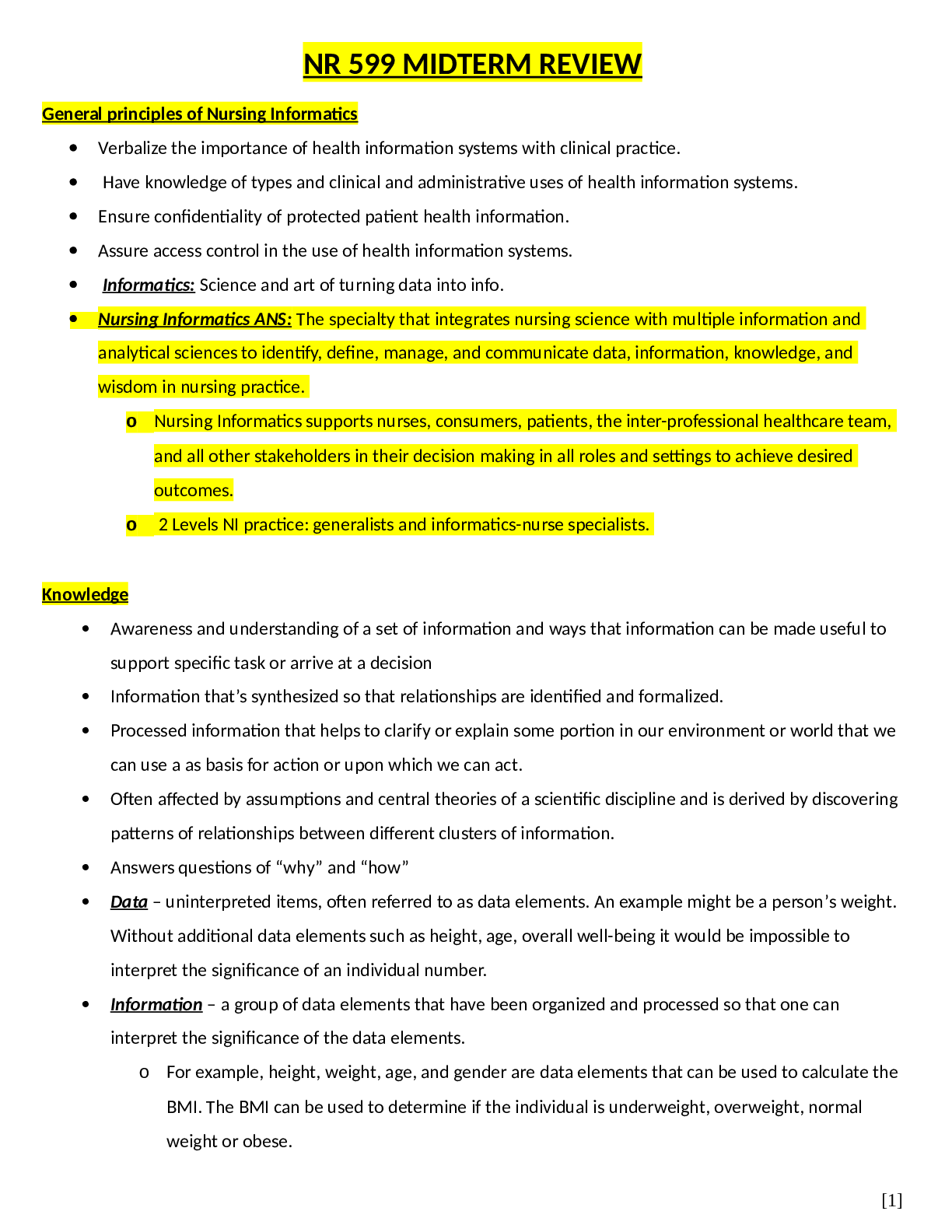
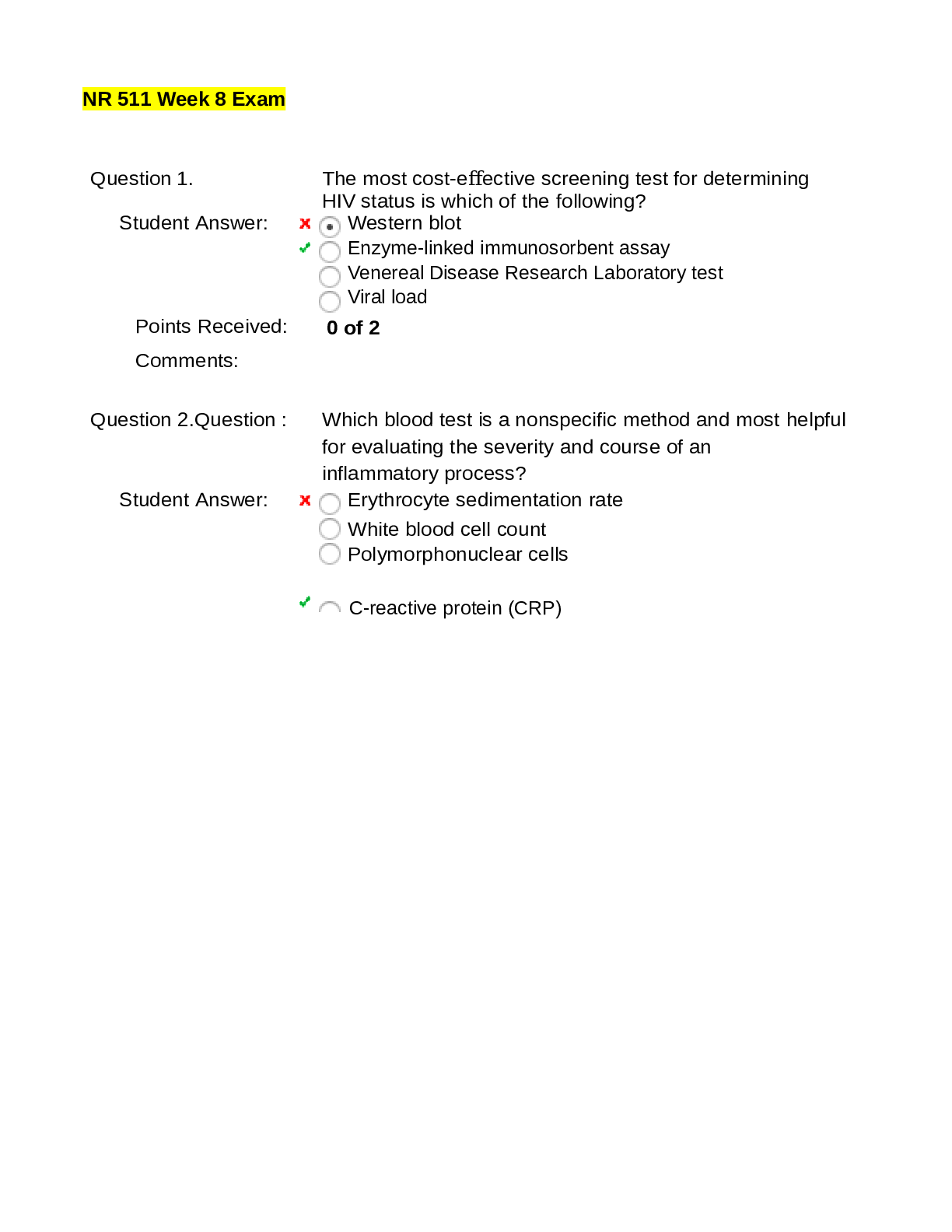
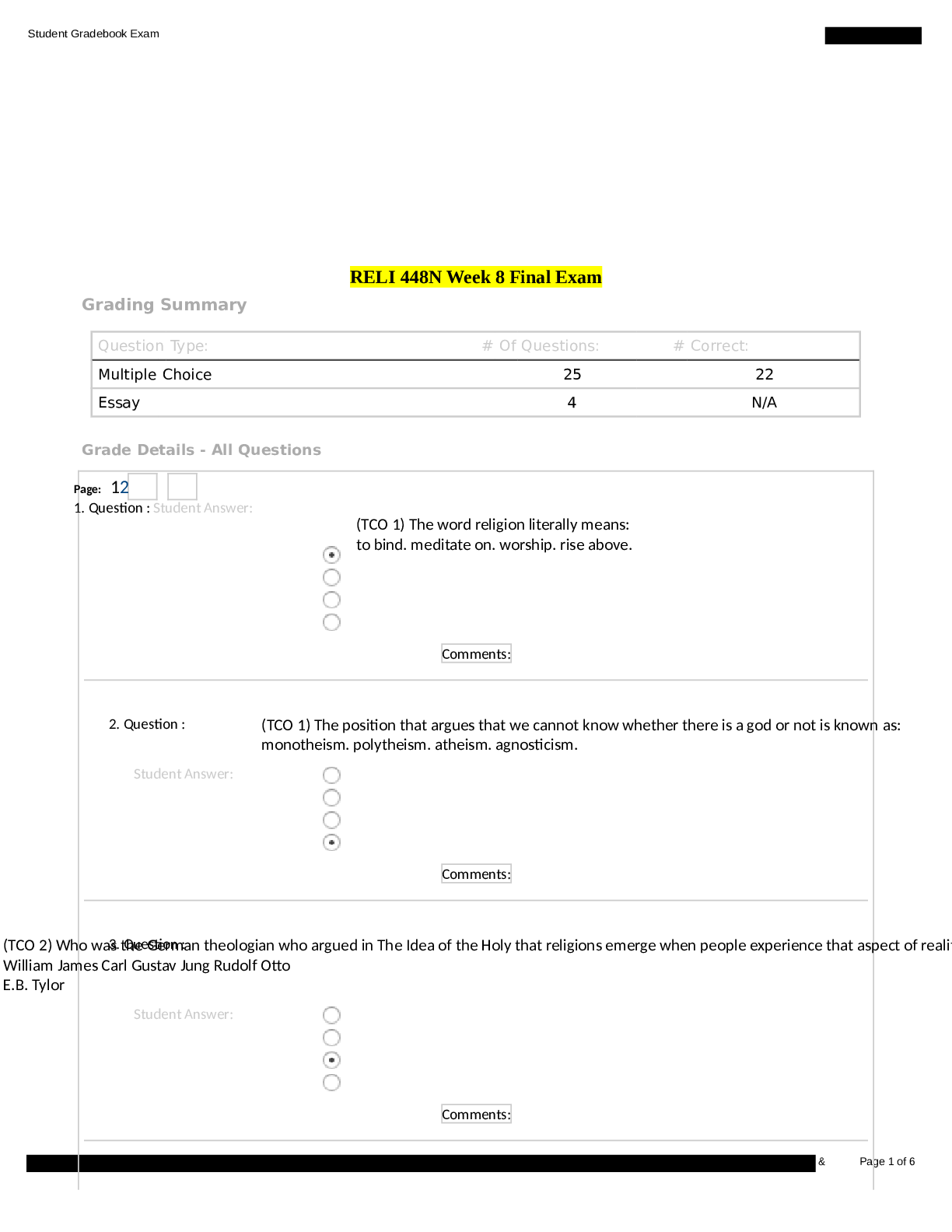
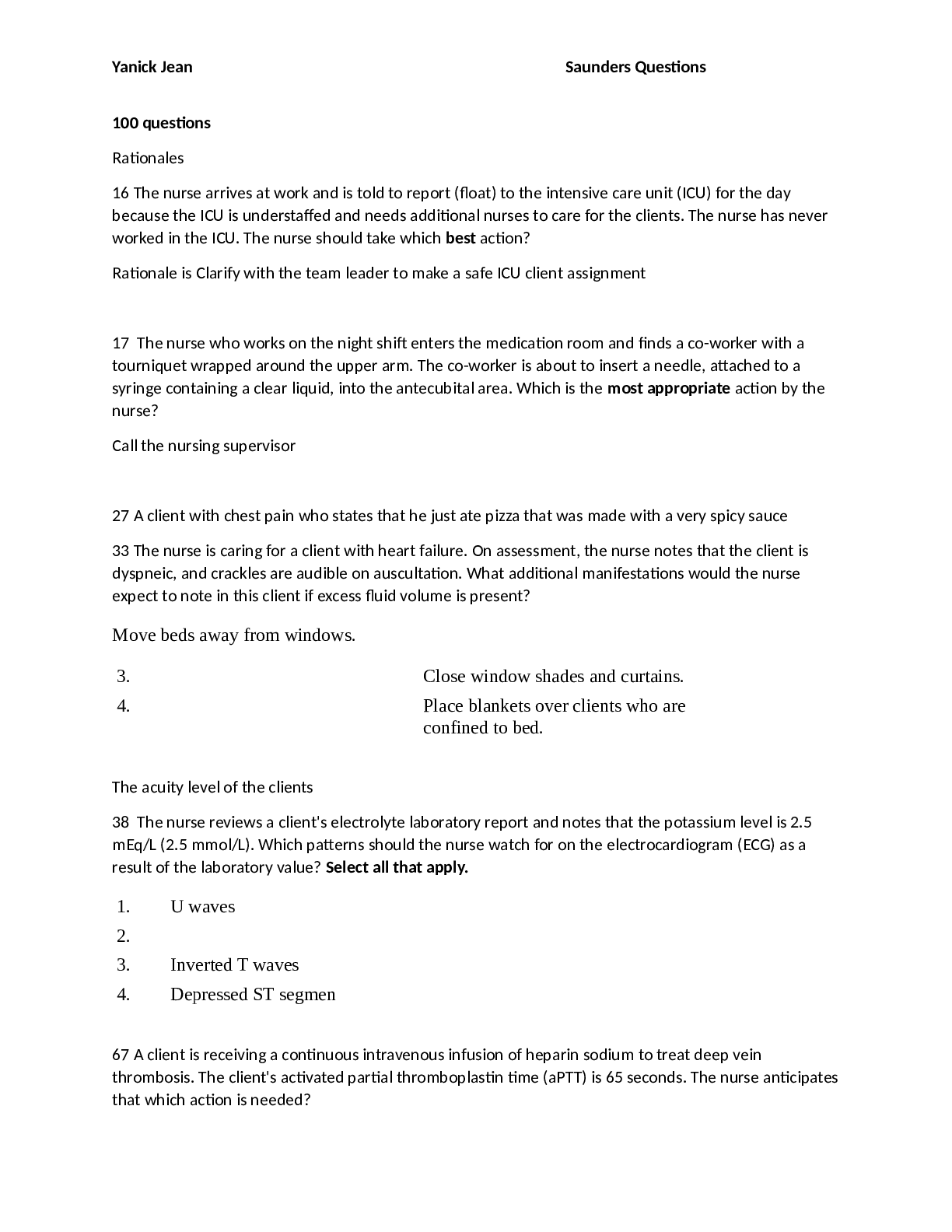
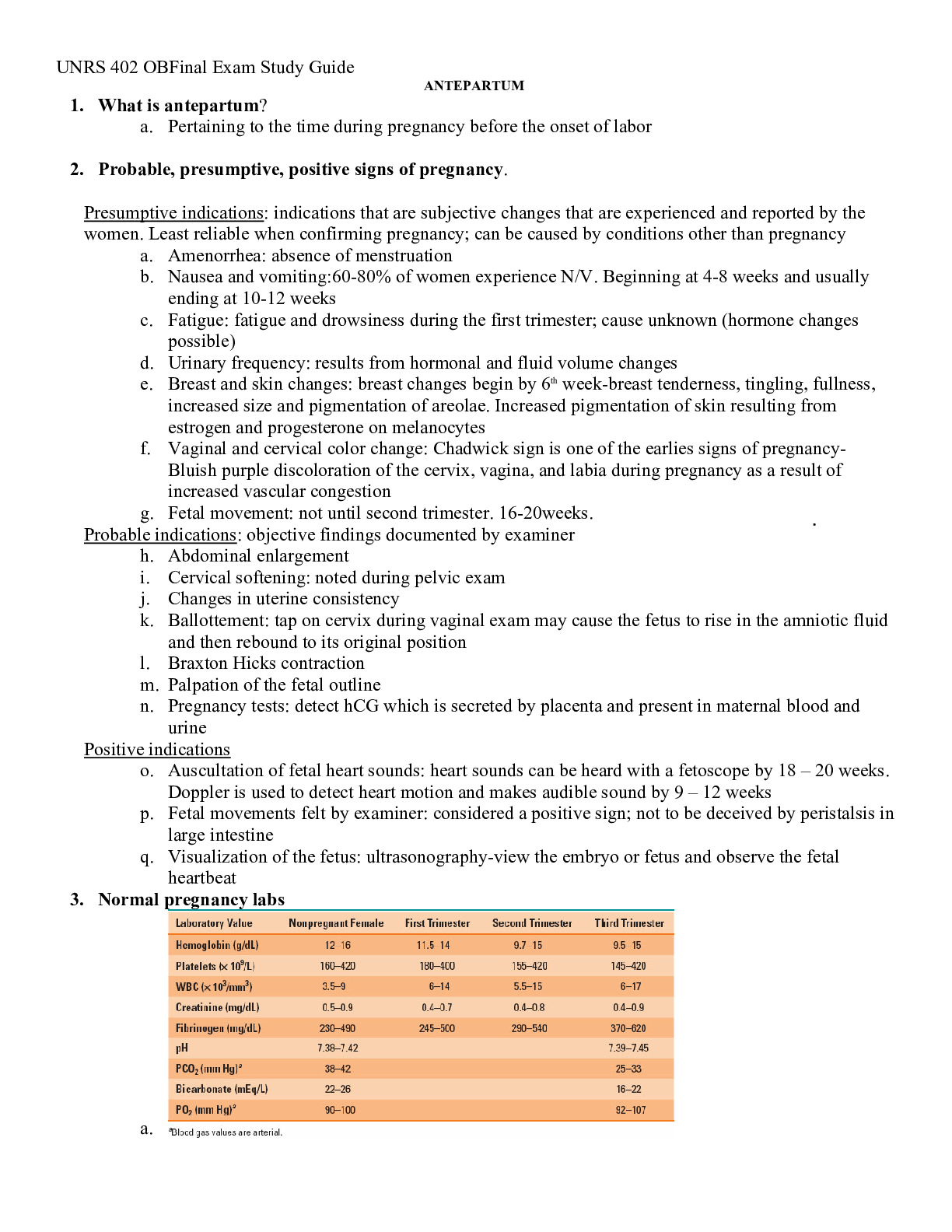
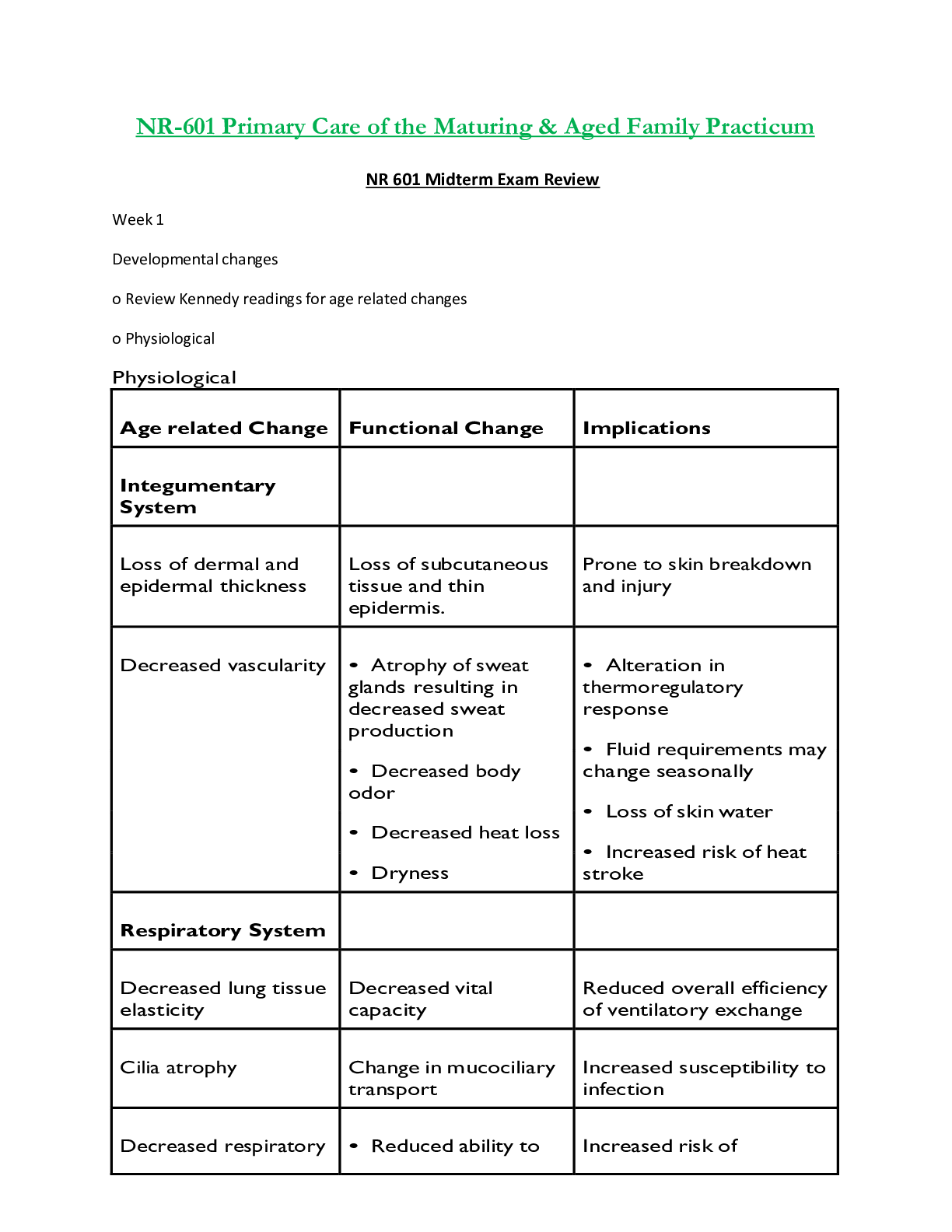
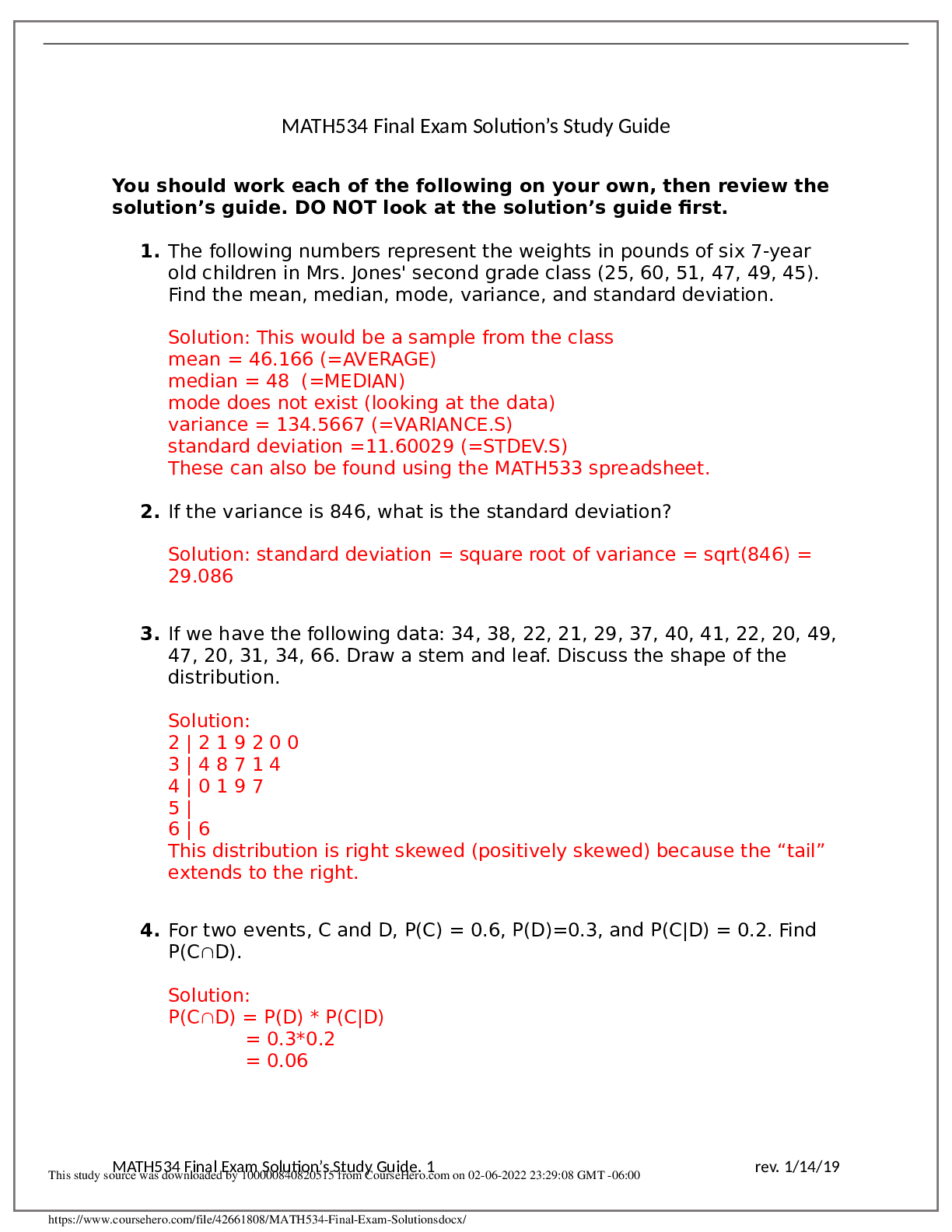
NR511 NP Café Final Exam Review Week 5 • Chapter 52: Common Musculoskeletal Complaints • Chapter 53: Spinal Disorders • Chapter 54: Soft-tissue Disorders Week 6 • Chapter 57: Glandu... lar Disorders (p.880-897 only) • Chapter 59: Metabolic Disorders • Chapter 73: Common Injuries (p.1210-1223 only) Week 7 • Chapter 46: Nocturia in Men (p.682) & Testicular pain (p.685) • Chapter 49: Prostate Disorders • Chapter 50: Penile & Testicular Disorders • Chapter 61: Hematological Disorders Musculoskeletal Disorders • Carpal Tunnel Syndrome • Herniated Disk • Shoulder Dislocation • Muscle Strain • Cauda Equine Syndrome • Spinal Fracture • Musculoskeletal exam • Back pain • Knee pain • Myofascial pain • Herniated nucleus pulposus • Lumbar spinal stenosis • Cervical spondylosis • Vertebral fractures • Tendonitis • Foot disorders • Meralgia parasthetica • Adhesive capsulitis • Tendon injury of the hand • Spinal stenosis Metabolic Disorders • Gout • Obesity Glandular Disorders • Hyperthyroidism • Hashimoto’s Thyroiditis • Hypothyroidism • Subclinical hypothyroidism Male GU Disorders • Priapism • Prostate Cancer • Hypospadias • BPH • Erectile Dysfunction • Prostatitis • Phimosis • Undescended Testes • Varicocele • Testicular Torsion • Epididymitis • Prostate Cancer Hematology • Anemia • Leukemia • Polycythemia The Musculoskeletal Exam (Chapter 52) Lachman maneuver: anterior cruciate ligament (ACL) injury (knee exam) McMurray sign: injury to the meniscus (knee exam); cause of meniscus injury: suddenly planting leg on ground and twisting; can cause immediate pain in the planted leg and inability to bear weight. Can lock up when trying to straighten it. Phalen’s test: numbness and tingling in the first 3 digits when pressing the dorsal surface of both hands together in a forced wrist flexion for at least 1 minute (wrist exam) Radial head fracture: palpate for tenderness, swelling, and crepitus just distal to the lateral epicondyle (wrist exam) Articular and non-articular musculoskeletal complaint-differentiation between the two is that non-articular complaints involves a point or focal tenderness Bulge test- use to check for knee joint effusion Carpal Tunnel Syndrome (Chapter 54 p. 839) Definition: Inflammation of the median nerve Initial treatment: wrist splint and NSAID Herniated Disk (Chapter 53 p.824) Most common area: L4-L5 (weakness in the great toe) Evaluation: straight leg test: patient in supine position and elevate the affected leg, positive if it elicits pain and sciatic nerve pain Shoulder Dislocation (Ch. 52 p.801) Assessment: shrugging shoulders should elicit pain if positive. Due to excessive pressure put on the shoulders Muscle Strains (Ch. 54 p.847) Degrees of Ankle Sprains: • 1st: ligaments are stretched but not torn • 2nd: most common; partial tearing of the ligament • 3rd: most severe; ligament is torn completely Risks: Strain can be due to not warming up prior to exercise; Teachable moment when the patient presents with strain is just to suggest stretching and warm-up exercises prior to the full exercise routine Assessment: Look for location (e.g. acute low back strain: low back pain not associated with sciatica; is aggravated by sitting, standing, and certain movements; alleviated with rest; pain locally on palpation and muscle spasms are felt Treatment: NSAID and recommend low back strengthening exercises; the type and intensity of the strengthening exercises depends on the patient’s pain tolerance. Be careful to not add insult to injury. Cauda Equine Syndrome (Ch. 53 p.828) Definition: occurs when the bundle of nerves below the end of the spinal cord known as the cauda equina is damaged Signs & Symptoms: low back pain, pain radiates down leg, numbness around the anus, and loss of bowel or bladder control. Referral: to the ER for evaluation- it’s going to require surgery (laminectomy) Spinal Fracture (Ch. 53 p.829) Presents: can present as low back pain Patient History Red Flags: hx of fall, prolonged steroid use, osteopenia, and osteoporosis Lumbar Spinal Stenosis (Ch. 53 p.827) Type of pain: often radicular complaints in the legs (with or without associated back pain) Symptoms: progress from proximal to distal direction and walking or prolonged standing causes pain and weakness in the legs and buttocks Relief: short term relief with leaning forward and often lean on counters when standing or grocery carts when shopping Cervical Spondylosis vs. Cervical Myelopathy (Ch. 53 p.816) Cervical spondylosis: known as degenerative arthritis, is a blanket term for the chronic degenerative processes that affect the vertebrae and facet joints; causes pain, stiffness and disability Cervical myelopathy: symptoms would include radicular symptoms of the upper extremities and weakness. In severe cases, leg weakness, gait disturbances, and loss of bowel and bladder control may occur Mixed: may have cervical spondylosis with myelopathy symptoms Cervical spondylosis w/o myelopathy symptoms: first line Tx: physical therapy Back Pain (Ch. 52 & 53 p.799) Assess: important to assess the cause of the back pain Red Flags: important to identify on the patient’s history (e.g. an individual who presents with back pain following a MVA, and it would warrant extensive investigation) Vertebral Fractures (Ch. 53 p.829) Risk Factors: most commonly associated with osteoporosis in susceptible individuals (older, Caucasian, small framed women) Knee Pain (Ch. 52 p. 805) Definition: patellofemoral dysfunction encompasses a continuum of disorders due to overuse Management: conservative with NSAID and quadriceps-strengthening exercises Myofascial Pain (Ch. 52 p.797) Definition: painful contractions of muscles after exertion, such as heat cramps; • may be R/T hyponatremia or other electrolyte imbalances • Usually the gastrocnemius and hamstring muscles are involved. • Tx of heat cramps: passive muscle stretching, cessation of activities, transfer to cooler environment, and drinking cool liquids. Sports drinks that contain electrolytes may be beneficial. Treatment: Identifying and eliminating aggravating factors; trigger point injections; dry needling; and massage therapy • Additional Tx: muscle relaxants, NSAIDs, COX-2 inhibitors, and tricyclic antidepressants in cases that do not respond to other treatments. • Narcotics and oral corticosteroids are not indicated Tendonitis (Ch.54 p. 836) Definition: lateral epicondylitis: elbow pain that is aggravated with movement especially with gripping objects or shaking hands. Associated with tenderness at the elbow and down the ulnar side of the forearm. Tendon injuries of the hand: mallet finger is caused by rupture or avulsion of the extensor digitorum tendon and is characterized by inability to actively extend the DIP joint. The joint typically resets at 30 degrees flexion Foot Disorders (Ch. 52 p.808) Morton’s Neuroma: localized pain on the sole of the foot, between the 3rd and 4th toes. • Pain is aggravated by weight bearing • Feels like a pebble in the shoe • On palpation: there will be a tender nodule in the metatarsal interspace on the left foot. • Not associated with redness and swelling Meralgia Parasthetica (Ch. 54, p. 846) Caused: By compression of the lateral femoral cutaneous nerve Risk Factors: commonly seen in overweight middle-aged men Symptoms: pain or parasthesias over the anterior superior iliac spine and the anterior lateral thigh, with decreased touch and pinprick sensation Treatment: analgesics and avoiding tight clothing around the waist and weight loss Adhesive Capsulitis (Frozen Shoulder) (Ch. 54 p. 843) Definition: painful condition in which the movement of the shoulder becomes limited. Frozen shoulder occurs when the strong connective tissue surrounding the shoulder joint (called the shoulder joint capsule) becomes thick, stiff, and inflamed. Risk Factors: • 40-60 years old • DM (especially type 1)- most common risk factor Metabolic Disorders Gout (Chapter 59 p. 946) Stages of Gout Stage Subjective Findings Objective Findings Diagnostic Findings I: Asymptomati c None None Microtophaceous deposits of urate in joints and bursae II: Acute Phase (inflammatory phase) • Extremely painful monoarticular or polyarticular attack. • Pruritus • Desquamation of the skin surrounding the affected joints as the inflammation subsides • Affected joints are red, warm, and swollen • Early acute attack subsides within a few days, but may last up to 2 weeks, as inflammation gradually subsides • 10% of patients experience only one acute attack during their lifetime • Elevated WBC • Elevated temperature • Elevated serum uric acid or normouricmia III: Intercritical (interval between acute attacks) None: patient is asymptomatic • Duration between attacks decreases as the disease progresses • If 2nd acute attack occurs, it usually presents within the first year after initial attack • Microtophaceous deposits of urate in joints and bursae • Serum urate levels should be below 6 mg/ dL if adequately treated IV: Chronic tophaceous (results from recurrent attacks with multiple sites or urate deposits [tophi] in articular and prearticular tissue) • May restrict movement of affected joints • Chronic pain, stiffness, decreased joint function, joint derangement, and secondary joint degeneration affected the upper and lower extremities • > 50% of patients progress to this acute stage within 20 years of initial attack if not properly managed • Occasionally, tophus ulceration and erosion with chalk- textured drainage observed. • Uric acid kidney stones in 5-10% of patients • Tophi Symptoms: severe great toe pain. Very painful to touch; painful on ambulation Physical Exam: erythema of the great toe at the interpharyngeal (IP) joint Gold standard diagnosis: joint aspiration with crystal analysis Other Diagnostics: • Hyperuricemia supports diagnosis but not in itself diagnosis • X-rays not diagnostics of gout Note: allopurinol lowers uric acid levels in the blood; this helps prevent gout flares but does not treat symptoms of an acute flare Acute Treatment: • Indomethacin, colchicine, prednisone o Colchicine is used to prevent further acute attacks triggered by changes in uric acid levels, but does not correct the underlying causes of an acute attack ▪ It is usually taken as 1 tablet every 1-2 hours until relief is obtained or until adverse GI effects occur Patient Education: high purine foods need to be avoided in order to reduce the risk of gout flares (fish, red meat, beans, beer) avoid alcohol Obesity (Chapter 59 p. 829) Secondary obesity: rare, possible causes include Cushing disease, polycystic ovary syndrome (PCOS), hypothalamic disease, hypothyroidism, and insulinoma Medications that are associated with weight gain: glucocorticoids, tricyclic antidepressants, and phenothiazines Glandular Disorders • Hyperthyroidism • Hashimoto’s Thyroiditis • Hypothyroidism • Subclinical hypothyroidism Who Needs Thyroid Screening? Recommendation: Recent clinical guidelines do not recommend routine screening of asymptomatic women before age 50 • No universally accepted screening recommendations for hypothyroidism • The American Thyroid Association recommends baseline screening at age 35, with close attention to high-risk patients (pregnant women, women > 60, and persons with autoimmune disease Prevalence: 1 in 5 women will develop an alteration in thyroid function in her lifetime Hyperthyroidism (Ch. 57 p. 880) Symptoms: heat intolerance, increase sweating, palpitations, tachycardia, nervousness, irritability, fatigue, and muscle weakness Diagnosis: TSH first when symptoms suggest hyperthyroidism (best test for hyperthyroidism • TSH: low • T4: High Treatment: • Anti-thyroid medication: methimazole, PTU o Can cause agranulocytosis and hepatic injury ▪ CBC and liver studies o Thyroid function test is needed taking ATDs; however, TSH are free T4 are preferred • Beta-blocker to treat any associated tachycardia and hypertension Grave’s Disease (Ch. 57) Definition: result of an autoimmune response wherein antibodies and produced that act against the body’s own organs and tissues (hyperthyroidism) Diagnosis: Thyroid-stimulating immunoglobulins are found in 95% of people with Grave’s disease and are evidence of this autoimmune process Hypothyroidism (Ch. 57 p. 889) Macroglossia: enlarged tongue Goal of Treatment: thyroid replacement to normalize the TSH (levothyroxine) • The absorption of levothyroxine from the GI tract may be slowed by concurrent use of certain drugs, such as ferrous sulfate, sucralfate, or antacids. • Start lower dose in the elderly to minimize cardiac effects Surgical Treatment: may be indicated for large, nonfunctional goiters that impair tracheoesophageal functioning Subclinical Hypothyroidism (Ch. 57) Definition: mild form of hypothyroidism. Indicates that only the serum TSH from the front of the pituitary gland is slightly above normal Labs: • TSH: elevated • Free T4: normal Hashimoto’s Thyroiditis (Ch. 57) Definition: autoimmune cause of hypothyroidism Incidence: • 7x more common in women than men • Can occur in teens and young women, but is more common in middle age Signs & Symptoms: enlarged thyroid is most often the first sign Diagnosis: antithyroid antibody titers- either for antimicrosomal (anti-TPO) antibodies or antithyroglobulin antibodies Male GU Disorders • Priapism • Prostate Cancer • Hypospadias • BPH • Erectile Dysfunction • Prostatitis • Phimosis • Undescended Testes • Varicocele • Testicular Torsion • Epididymitis • Prostate Cancer Priapism (Ch. 50) Definition: prolonged erection of the penis, usually w/o sexual arousal 1st Line Treatment: phenylephrine (Neo-Synephrine): for low-flow priapism because the drug has almost pure alpha-agonist effects and minimal beta activity Risk Factors Prostate Cancer (Ch. 49 p. 756) • Associated with human cytomegalovirus • Man with 1st degree relative with prostate cancer is 2x likely to develop disease • Men with diets high in fat, particularly animal fat • Men who smoke Treatment: both block the release of FSH and LH. Both are administered IM • Goserelin acetate (Zoladex) • Leuprolide acetate (Lupron) Hypospadias (Ch. 50 p.764) Definition: opening of the penis is on the underside of the organ Risk Factors: more common in infants with a FH of hypospadias Circumcision: Should never be done on a newborn with hypospadias because the surgeon who corrects the hypospadias may need the prepuce to repair the defect Surgical correction: should be done by the time the child enters 1st grade Benign Prostate Hyperplasia (BPH) (Ch. 49 p. 748) Treatment: after 6 months of therapy with finasteride (Proscar) for BPH, the PSA should decrease by about 50% Testing: Can then be repeated annually. If the PSA has not decreased, you should suspect prostate cancer and proceed to evaluate for such Surgery: within 4-6 weeks after surgery, it is safe to resume a full sex life, including intercourse. • Before this time, the spasmodic contractions that occur in the prostatic urethra at the time of ejaculation could trigger delayed bleeding. • After 6 weeks, the risk of delayed bleeding is very slight, however if the area has not completely healed, there may be slight discomfort because of the spasms Signs and symptoms: The prostate is usually diffusely smooth and enlarged • The size of the prostate does not correlate with urinary symptoms. • Lifestyle modifications and Rx medications are recommended for treatment of BPH Medications: • 5-alpha reductase inhibitors- finasteride (Proscar) and dutasteride (Avodart) • Alternative therapy such as saw palmetto: not considered 1st line treatment Erectile Dysfunction (Ch. 50 p. 761) Assessment: perform a medication Hx to determine if one of those could be causing the ED Medications that can cause ED: • Antiandrogens • Antihypertensives (B-Blockers and central sympatholytics (reserpine) • Anticholinergics • Antidepressants • Antipsychotics • CNS depressants • Drugs of abuse such as alcohol, tobacco, and heroin Bacterial Prostatitis (Ch. 49 p.754) Chronic bacterial prostatitis: recurrent bacterial infection of the prostate and urinary tract • Affects men 50-80 years old Accompanied by bladder obstruction: weak urine stream, hesitancy, or dribbling, hematuria, hematospermia, and/or panful ejaculation Most common offending pathogen: Escherichia coli Note: • The etiology of urethral discharge or difficulty voiding can include acute and chronic prostatitis and prostatic abscess • Young males in their 20s usually have acute prostatitis from gonorrhea or other bacterial infections Examination: a rectal exam should be performed gently because vigorous manipulation of the prostate can result in septicemia. Therefore, prostatic massage is contraindicated Acute bacterial prostatitis is always associated with a UTI and has a characteristically abrupt onset: fever, child, low-back pain, tenesmus, and urinary complaints typically of UTI are common Testicular Torsion (Ch. 50 p. 769) Most common sign: absence of the cremasteric reflex Phimosis (Ch. 50 p.764) Definition: unusually long foreskin or a foreskin that can’t be retracted over the glans penis during physical examination Risk Factors: uncircumcised males and is normal in infancy Referral: if anyone older than infancy, refer to urologist Undescended Testes Incidence: in boys with undescended testes, less than 1% have their testes descent after the first year Treatment: orchiopexy needs to be performed before age 6 to promote normal spermatogenesis and hormone production, prevent tumor formation, and leave the testis in a location where it can be easy palpated Varicocele (Ch. 50 p. 772) Description: May describe testicular pain and testicles that feel like a bag of worms Examination: There will be soft and moveable blood vessels underneath the scrotal skin upon palpation • Palpation of varicose veins, described as a “bag of worms”, in the scrotum is a classic example of a varicocele, an abnormal tortuosity and dilation of the veins of the pampiniform plexus within the spermatic cord Epididymitis (Ch. 50 p.767) Major complaint: scrotal pain that radiates along the spermatic cord Signs and Symptoms: • Urethral discharge • Other symptoms of UTI (frequency, dysuria, etc.) • Hematuria Relief of symptoms: elevation of the testes and the epididymis will relieve the discomfort Physical Exam: will reveal scrotal swelling and the testis may be indistinguishable from the epididymitis Hematology • Anemia • Leukemia • Polycythemia Anemia (Ch. 61) Macrocytic normochromic anemia: cell size is large and irregular • Folic acid and/or vitamin B12 deficiency Glucose-6 phosphate dehydrogenase (G6PD) deficiency: X-linked recessive disorder • Commonly seen in African American males • It is an enzyme defect that causes episodic hemolytic anemia because of the decreased ability of RBC to deal with oxidative stress Sickle-Cell Anemia: • An autosomal recessive disorder, which means both parents must have the gene to pass it on to child • Abdominal pain, pallor, tachycardia are all manifestations of splenic sequestration • Early recognition of splenic sequestration can be a lifesaving skill • Parents can be taught to recognize signs of increasing anemia and enlarging spleen o Teaching parents how to recognize increasing abdominal girth or abdominal pain, as well as how to palpate spleen • Gold standard Diagnostic: hemoglobin electrophoresis, a test that determines the presence of hemoglobin S. Iron Deficiency Anemia (Ch. 61 p. 959) Risk Factors: • > 60 years old • Live in poverty • Recent illness (ulcer, diverticulitis, colitis, hemorrhoids, and GI tumors Iron supplements: should be taken on empty stomach Signs & Symptoms • Pale conjunctivae and nail beds • Heart murmur • Cheilosis (reddened lips with fissures at the angles) • Stomatitis • Splenomegaly • Koilonychia (thin and concave fingernails with raised edges) • Glossitis • Esophageal webs (Plummer-Vinson syndrome) • Melena • Menorrhagia Labs: serum ferritin, the body’s iron-storing protein; can tell exactly how much iron is on hand in the body • Best way to spot iron deficiency early, before it progresses to full-blown anemia • If ferritin level is borderline, a dietary and supplemental regimen of iron will rebuild the iron stores Diagnostics: • fecal occult blood • Hemoglobin and hematocrit o Early stages will be normal to slightly reduced • It is necessary to determine whether the iron deficiency is related solely to inadequate dietary intake or to decreased absorption or chronic blood loss Pernicious Anemia (Ch. 61) Type: macrocytic (large cell size) and normochromic cells Most common cause: vitamin b12 deficiency is the most common cause of megaloblastic anemia Polycythemia (Ch. 61 p. 979) Definition: An increase in the # of RBC in the body. The extra cells cause the blood to be thicker, and this, in turn, increases the risk of other health issues, such as blood clots Incidence: increases with age • Men older than 70 more than women of the same age by a ratio of 2:1 • 1.9: 100,000 persons Risk Factors • Living in high altitudes, given the body’s compensation for the relatively lower environmental O2 tension through the upregulation of erythropoiesis Sideroblastic Anemia (Ch. 61 p. 960) Definition: group of blood disorders in which the body has enough iron but is unable to use it to make Hgb, which carries oxygen in the blood. Results in iron accumulation in the mitochondria of RBCs, giving a ringed appearance to the nucleus Diagnostics: The Prussian blue stain: ringed sideroblasts would be seen in this stain Lab Values for the Types of Anemia Test Iron Deficiency Anemia Thalassemia Anemia of Chronic Disease Sideroblastic Anemia Serum Ferritin Level Decreased Increased Normal to increased Normal to increased RBC distribution width Increased Normal to increased Normal Increased Serum iron level Decreased Normal to increased Normal to decreased Normal to increased Total iron-binding capacity Increased Normal Slightly decreased Normal Transferrin saturation Decreased Normal to increased Normal to slightly decreased Normal to increased Reticulocyte Count Definition: Indicates the percentage of newly maturing RBCs released into the circulating blood from the bone marrow. • As a RBC matures, it loses its endothelial reticulum Elevated In: • cases of blood loos as the body tries to replace the loss • treatment of anemias (e.g. iron, folic acid, and Vitamin B12) • Bone marrow disorders, when immature RBCs are displaced by other proliferating cells Mean Corpuscular Volume Definition: MVC indicates the average size of individual RBCs. • Normal (normocytic) range is 76-96 fL Increased (macrocytic) • Megaloblastic anemia (i.e. vitamin b12 deficiency and folate deficiency) • Liver disease (alcohol abuse) • Use of some drugs (e.g. zidovudine) Leukemia (Ch. 61 p. 984) Most common type in the U.S. Chronic lymphocytic leukemia (CLL) Rai classification system: • Stage 0: lymphocyte count > 10,000 mm3 • Stage I: enlarged lymph nodes • Stage II: enlarged liver and/or spleen • Stage III: anemia • Stage IV: thrombocytopenia Acute Lymphoblastic Leukemia (Ch. 61 p. 986) Most common: type of cancer in young children Signs & Symptoms: • Pallor • Fatigue • Bleeding • Fever • Bone pain • Adenopathy • Arthralgias • Hepatosplenomegaly Labs: • CBC with differential (leukopenia with lymphoblasts) Radiation therapy: increased risk for developing a brain tumor as a secondary malignancy • More often seen in children who are treated with radiation at age 5 or younger • 3-12% of children treated for cancer will develop a new cancer within 20 years of being treated for the primary cancer Wounds & Lacerations (Ch. 73 p. 1210) Immunizations: tetanus, ask when last was. • If > 5 years, a tetanus booster should be administered Suture removal time frames • Face: 4-6 days • Scalp: 6-10 days • Trunk: 7-10 days • Arms: 10-14 days • Legs: 10-14 days • Joints: 14 days Wound Closure: Dermabond tissue adhesive can be utilized for superficial lacerations < 6 cm in length and in low tension areas • Not be used over a joint or on any grossly contaminated wounds Antibiotic prophylaxis for wounds: • Patient with DM or have a Hx of vascular compromise should be started on prophylactic Abx o Initial Tx: Parental administration of ampicillin/sulbactam, cephalexin, or ceftriaxone o Followed by: oral therapy with amoxicillin/clavulanate, cephalexin, or cefadroxil • Allergy to penicillin or cephalosporins o Doxycycline with or w/o clindamycin or ciprofloxacin Animal Bites (Ch. 73 p. 1219) Cleansed: bites and scratches should be cleaned with mild soap and water or 1% povidone-iodine (Betadine) solution to remove the animal’s saliva from the wound • Irrigate with 500-2000mL of NS with a 30mL syringe with an 18-20G plastic catheter to achieve a pressure of 5-8 psi Bite wounds of the hand: should not be sutured Tetanus booster: if the patient received a primary immunization series but not a booster within the past 5 years, a booster should be administered. Prophylaxis Antibiotics: for 3-5 days if the wound is a fresh bite wound Healthy and available dog or cat: observe for 10 days for signs and symptoms of rabies, if no signs of rabies, no treatment of the exposed person is necessary [Show More]
Last updated: 1 year ago
Preview 1 out of 20 pages
Reviews( 0 )
Document information
Connected school, study & course
About the document
Uploaded On
Jun 26, 2022
Number of pages
20
Written in
Additional information
This document has been written for:
Uploaded
Jun 26, 2022
Downloads
0
Views
41

.png)
.png)