*NURSING > CASE STUDY > CaseStudy -Dementia-UNFOLDING_Reasoning William “Butch” Welka, 72 years old (GRADED A) (All)
CaseStudy -Dementia-UNFOLDING_Reasoning William “Butch” Welka, 72 years old (GRADED A)
Document Content and Description Below
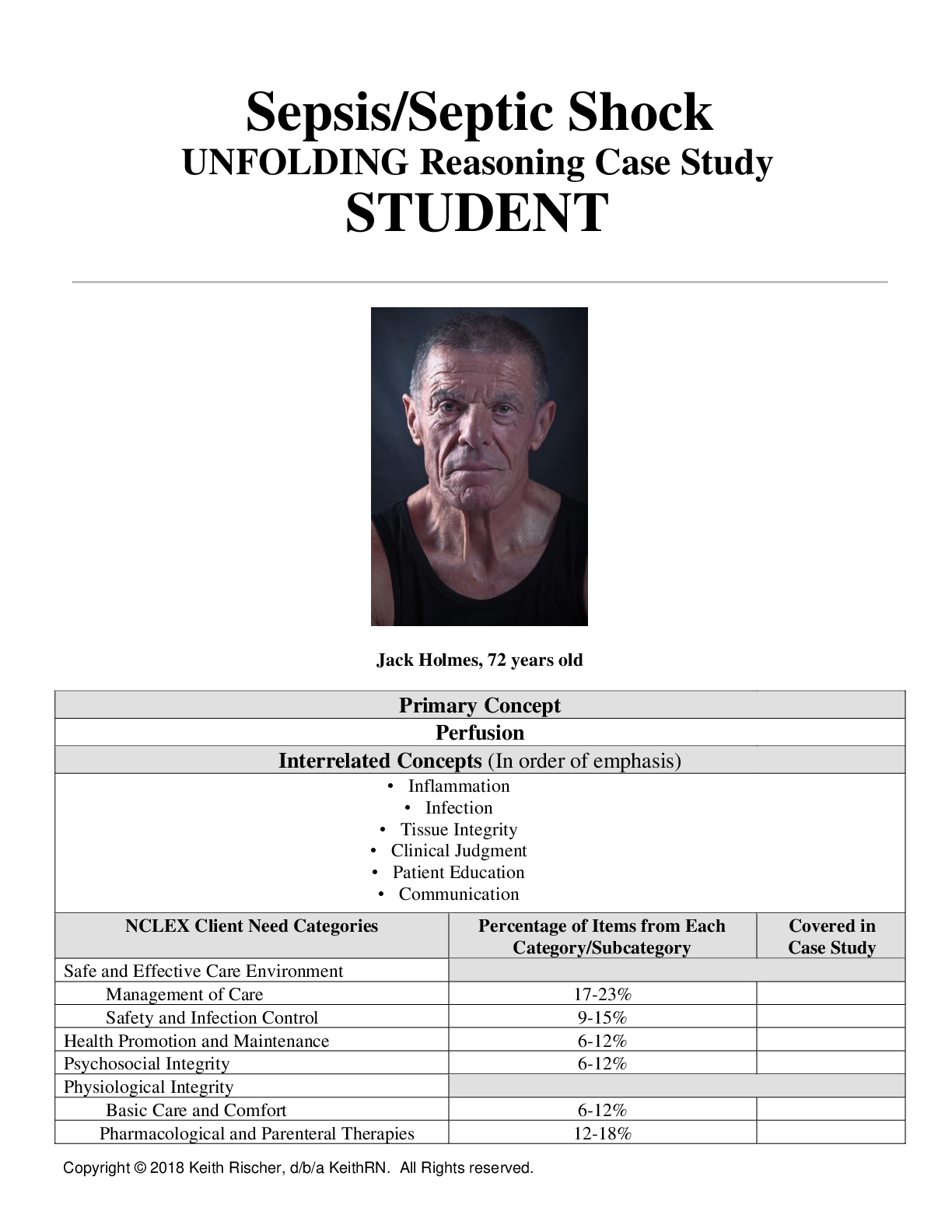
Dementia UNFOLDING Reasoning ####### William “Butch” Welka, 72 years old Primary Concept Cognition Interrelated Concepts (In order of emphasis) Pain Mood and Affect Psychosis Clinical Judgment Pat... ient Education Communication Collaboration ####### NCLEX Client Need Categories Percentage of Items from Each ####### Category/Subcategory ####### Covered in ####### Case Study Safe and Effective Care Environment Management of Care 17-23% ✓ Safety and Infection Control 9-15% Health Promotion and Maintenance 6-12% ✓ Psychosocial Integrity 6-12% ✓ Physiological Integrity Basic Care and Comfort 6-12% ✓ Pharmacological and Parenteral Therapies 12-18% ✓ Reduction of Risk Potential 9-15% ✓ Physiological Adaptation 11-17% ✓ History of Present Problem: William “Butch” Welka is a 72-year-old male with a history of heart failure, COPD, hypertension, diabetes type II and dementia who has been hospitalized for exacerbation of heart failure three times the past six months. He is now a resident of Pineville Estates, a local long-term care facility the past four months because his dementia progressed and his wife Rita was unable to care for him. When Rita visited Butch this morning, she reports to the nurse that he is more confused and is concerned because Butch is easily angered. Butch insists that he sees his friend Roger, who served with him in the Navy, is in the room, but he died ten years ago. Rita approaches the nursing station with tears in her eyes and states, “What is happening to my husband? This just isn’t like Butch to act like this! Please do something to help him!” Personal/Social History: Butch has been married to Rita for 51 years. They have three adult children who visit him weekly. Rita comes to visit Butch every day after work. Butch was a salesman for 35 years before he retired seven years ago. Butch believes he is at Pineville Estates for rehab, but his family is concerned that it is no longer safe at home if he were alone. Rita was just awarded guardianship due to his declining mental status. 1. What data from the histories are RELEVANT and have clinical significance to the nurse? (Reduction of Risk Potential) RELEVANT Data from Present Problem: Clinical Significance: History of heart failure, COPD, HTN, DM II and dementia Has been hospitalized for exacerbation of heart failure three times the past six months. Angry, confused, and hallucinaing All these condiions afect the vascular components of the body and increase the risk of stroke. COPD and HF can also cause him to not receive enough oxygen and blood low to the brain which could cause the demenia to advance at a quicker rate. End stages of HF S&S include confusion and impaired thinking. COPD could be the cause of the HF exacerbaions. S&S of end stage heart failure and is also a S&S of vascular demenia. RELEVANT Data from Social History: Clinical Significance: Married for 51 years 3 adult children that visit regularly Wife visits daily Thinks he in rehab Wife awarded guardianship Has support at home Has family that visit rouinely, rouine is important for demenia paients Has coninued support at the hospital Could be upset when he inds out why he is in the hospital Wife is the person in charge of decisions related to his care 3. One disease process often influences the development of other illnesses. Based on your knowledge of pathophysiology, (if applicable), which disease likely developed FIRST that created a “domino effect” in Butch’s life? COPD likely occurred first. COPD can eventually cause heart failure due to chronic lowered oxygen levels, which will create increased blood pressure in the lung’s arteries. DM will also cause damage to the vessels if not well controlled. He likely has CAD or is a high risk for CAD as well. This causes damages to the vascular system ad the heart becomes weaker. This will make the body’s blood harder to pump throughout the body (HTN). Body tissues and organs such as the brain do not perfuse adequately leading to oxygen deficits in the brain, increasing the risk of dementia. Patient Care Begins: ####### Current VS: P-Q-R-S-T Pain Assessment: ####### T: 99.8 F/37.7 C (oral) P rovoking/Palliative: “Standing and moving.” ####### P: 60 ( regular) Q uality: “Dull” ####### R: 16 (regular) R egion/Radiation: “Lower back” ####### BP: 115/72 S everity: “4/10” ####### O2 sat: 96% room air T iming: “It is always there.” 4. What VS data are RELEVANT and must be interpreted as clinically significant by the nurse? (Reduction of Risk Potential/Health Promotion and Maintenance) RELEVANT VS Data: Clinical Significance: T: 99. O2: 96% Pain: Lower back, 4/10, dull May have a UTI based on slightly elevated temp, location of pain and sudden confusion. Confusion could also be due to an exacerbation of COPD, r/t lower O2. ####### Mental Status Examination (MSE): APPEARANCE: Dressed in t-shirt and pants. His pants are urine soaked. Wearing a sweater even though it is summer. MOTOR BEHAVIOR: Ambulates with a walker, shuffling gait SPEECH: Clear MOOD/AFFECT: Pleasant, except when talking about being at Pineville Estates, becomes agitated Anxiety increases, and angry affect displayed; emotionally labile – can become easily angered THOUGHT PROCESS: Generally coherent conversation; can make himself understood THOUGHT CONTENT: Preoccupied with not wanting to be at Pine Estates. Talks about how they are not helping him. Wants to go home and get his hunting license so he can go hunting. PERCEPTION: Reports having seen a friend, Roger, from the Navy climbing down the side of the building yesterday. No other current evidence of hallucinations INSIGHT/JUDGMENT: Insight – poor- not understanding why he needs to be at a facility and not at home. (thinks he is here for rehab) Unable to recognize own deficits in functioning Judgment Poor-often asks his wife to bring him take-out food (which she does), then he eats an additional dinner in the cafeteria. COGNITION: Alert and Oriented to person and place. Not oriented to time or purpose. Believes it is 2017. Able to recognize it is spring. Short-term memory impaired: Doesn’t always remember that he has eaten; sometimes forgets when wife visits. Long-term memory seems to be intact. Remembers personal history Attention span is adequate when tested. Able to state months backwards INTERACTIONS: Pleasant when spoken to. Hesitant to initiate conversation. SUICIDAL/HOMICIDAL: “If I don’t get out of here soon, I might just walk into traffic.” 5. What MSE assessment data are RELEVANT and must be interpreted as clinically significant by the nurse? (Reduction of Risk Potential/Health Promotion & Maintenance) RELEVANT Assessment Data: Clinical Significance: 1. Appearance: Urine soaked pants; sweater in summer Speech: Clear Motor behavior: Shuffling gait Mood & affect: Agitated & angered at mention of his current residence Thought Process: Generally coherent Thought content: Wants to go home; wants to go hunting Perception: Hallucinations of seeing Navy friend that has died Insight/Judgement: Unable to recognize decrease in function; does not remember eating; does not know why he is at facility. Cognition: Limited to person and place, short term memory impaired Interactions: Hesitant to initiate conversation Suicidal/homicidal: “I might walk into traffic 1.-Incontinent and possibly unaware of it. If he has a fever, he may have chills, explaining the sweater. 2.-Loss of muscular coordination, S&S of dementia or a SA of his meds 3.-Able to communicate somewhat effectively and make his needs known when aware 4.-Agitation, anxiety, anger could be due to fear of not knowing why he is at the facility. 5.-Thought process is intact 6.-Wants to be at home where he is familiar with his surroundings and calm 7.- Hallucinations and confusion can indicate signs of delirium which could be due to an infection 8.-Does not understand why he needs to adhere to treatments and what is best for himself 9.-Shows a progression in dementia 10.- Shows discomfort in surroundings, lack of confidence due to not understanding why he is there. May be more likely to engage if at home. 11.-Frustrated with current circumstances and scared. Current Assessment: GENERAL ####### APPEARANCE: Calm, body relaxed, no grimacing, appears to be resting comfortably in chair. Most Recent: 5.8 14.5 198 52 0% 8. What lab results are RELEVANT and must be interpreted as clinically significant by the nurse? ####### (Reduction of Risk Potential/Physiologic Adaptation) ####### RELEVANT Lab(s): Clinical Significance: TREND: ####### Improve/Worsening/Stable: WBC 6. HGB 15. PLT 202 % Neut 55 Bands 0% Fight infecion but WNL Carry Oxygen, WNL Helps blood to clot, WNL Type of WBC, WBL WNL Stable Stable Stable Stable Stable Misc. HGB A1C Current: 7. Most Recent: 5. 9. What lab results are RELEVANT and must be recognized as clinically significant by the nurse? ####### (Reduction of Risk Potential/Physiologic Adaptation) ####### RELEVANT Lab(s): Clinical Significance: TREND: Improve/Worsening/Stable: HGB 7. Large increase for A1C. Could cause kidney issues Worsening Urinalysis + UA Micro Color: Clarity: Sp. Gr. Protein Nitrite LET RBCs WBCs Bacteria Epithelial Current: Yellow Clear 1.015 Neg Neg Neg 0 4 Trace Few Most Recent: Yellow Clear 1.018 Neg Neg Neg 0 0 None None 10.What lab results are RELEVANT and must be recognized as clinically significant by the nurse? (Reduction of Risk Potential/Physiologic Adaptation) ####### RELEVANT Lab(s): Clinical Significance: TREND: ####### Improve/Worsening/Stable: All values are normal Need to assess UA frequently d/t trending issues with WBC’s, bacteria, and epithelial current lab results Color: Stable Clarity: Stable SP gravity: Stable Protein: Stable Nitrite: Stable LET: Stable RBC: Stable WBC: Worsening Bacteria: Worsening Epithelial: Worsening 11.Lab Planning: Creating a Plan of Care with a PRIORITY Lab: (Reduction of Risk Potential/Physiologic Adaptation) Lab: Normal Value: Clinical Significance: Nursing Assessments/Interventions Required: Hgb A1C Value: 7.8 % 4-5.9% Critical Value: ####### <6% >9% Critical Levels >9% indicate poor diabetes control and damage to the eyes and other systems start to happen 7.8% is close to the critical value. This can indicate kidney damage. Patient is close to critical Hgb A1C values. Patient/family education is essential. His wife continues to bring him meals without checking if he has been fed or what his current A1C is. Possible change in medication may be needed as well. Clinical Reasoning Begins... 12. Interpreting relevant clinical data, what is the primary problem? What primary health related concepts does this primary problem represent? (Management of Care/Physiologic Adaptation) ####### Problem: Pathophysiology of Problem in OWN Words: Primary ####### Concept: Neuropsychiatric evaluation Urinalysis (UA) Haloperidol 2.5 mg PO BID Acetaminophen 325mg two tablets PO every 6 hours PRN Insulin glargine 10 units sub q HS Increase memantine to 10 mg PO daily Donepezil 5 mg PO daily Trazodone 50 mg PO at HS PRN Neuro eval: Measures the progression of dementia, assesses for delirium & possible cause of hallucinations, and assesses for suicide potential. UA: Continuous monitoring of UA will continue to evaluate if the patient has a Urinary tract infection or inflammation of the GU. Haloperidol: Antipsychotic which relieves positive symptoms of a psychotic episode (hallucinations). Acetaminophen is a mild analgesic and antipyretic. Insulin is an exogenous hormone replacement for the management of diabetes. Memantine increased to treat increasing symptoms if dementia Donepezil is in addition to treat dementia. Trazodone: Antidepressant to deal with feelings of hopelessness and helplessness. Demonstrate decrease in the rapid progression of dementia, to treat the factors that are contributing to confusion and/or delirium, to evaluate potential for suicide/self-harm. If the patient has an infection of the GU, antibiotics can be started treat the infection. Absence of hallucinations Reduction in the patient’s temp and pain. Management of hyperglycemia. Increasing memantine treats dementia by blocking the glutamate receptors on NMDA. Decrease in dementia S&S. Donepezil inhibits ACh- esterase. Decrease the S&S of dementia from two different angles so that the patient can continue as independently as possible. Improvement in mood and decreased or nonexistent suicidal ideations. Trazadone is used off-label as a sleep aid, which will help the patient’s insomnia. 14.PRIORITY Setting: Which Orders Do You Implement First and Why? (Management of Care) Care Provider Orders: Order of Priority: Rationale: Neuropsychiatric evaluation Urinalysis (UA) Haloperidol 2.5 mg PO BID Acetaminophen 325mg two tablets PO every 6 hours PRN Insulin glargine 10 units sub q HS Increase memantine to 10 mg PO daily Donepezil 5 mg PO daily 1)Neuropsychiatric Evaluation 2) UA 3) Insulin 4) Increase memantine 5) Add donepezil 6) Acetaminophen 7) Haloperidol 1) The basis of all current medical exacerbations is tied to his mental status 2) UA is important in case he is in current need of treatment for an infection and would need to be treated as soon as possible 3) The patient’s blood sugars should be managed to prevent HHNS, more confusion, kidney injury or DKA. 4.) Increasing memanine will also help the paient maintain independent funcion for as long as possible. 5.) Treating dementia via a different neurotransmitter will help the patient maintain independent function through his dementia for as long as he can 6) Pain and possible temperature will be addressed and will aid to promote patient’s comfort 7.) If hallucinations persist after all the priorities have been addressed, then Haloperidol will help address the hallucinations. Collaborative Care: Nursing 15.What nursing priority (ies) will guide your plan of care? (Management of Care) ####### Nursing PRIORITY: Safety ####### PRIORITY Nursing Interventions: Rationale: Expected Outcome: Assess the degree of impaired ability of competence, emergence of impulsive behavior, and a decrease in visual percepion. Assess the level of cogniive disorders such as change to orientaion to people, places and imes, range, atenion, thinking skills. Assess paient’s surroundings for hazards and remove them. 1. Impairment of visual percepion increase the risk of falling. Idenify potenial risks in the environment and heighten awareness so that caregivers more aware of the danger. (Ackley et al., 2020) 2. Provide the basis for the evaluaion / comparison that will come and inluencing the choice of intervenion. (Ackley et al., 2020) 3. Demenia decreases awareness of potenial dangers, and disease progression coupled with hazardous environment that could lead to accidents. (Ackley et al., 2020) 1. Patient will remain in a safe environment with no complications or injuries obtained. 2. Paient will remain safe from environmental hazards resuling from cogniive impairment. 3. Paient will remain in a safe environment with no complicaions or injuries obtained 16.What body system(s) will you assess most thoroughly based on the primary/priority concern? (Reduction of Risk Potential/Physiologic Adaptation) ####### PRIORITY Body System: PRIORITY Nursing Assessments: ####### Psychosocial PRIORITIES: Risk for self-harm ####### PRIORITY Nursing Interventions: Rationale: Expected Outcome: 1.) Provide a safe environment. Weapons and pills should be removed by friends, relaives, or the nurse. 2.) Present opportuniies for the paient to express thoughts, and feelings in a nonjudgmental environment. 3.) Stay with the paient more oten. 1.) Removing potentially harmful objects prevents the patient from acting or sudden self- destructive impulses. (Ackley et al., 2020) 2.) It is helpful for the paient to talk about suicidal thoughts and intenions to harm themselves. Expressing their thoughts and feelings may lessen their intensity. Also, they need to see that staf are open to discussion. (Ackley et al., 2020) 3.) This approach provides the paient with a sense of security and strengthens self-worth. (Ackley et al., 2020) 1.) Paient will remain safe and free from self- harm 2.) Paient will idenify feelings of negaivity and how to cope with those 3.) Paient will form a therapeuic relaionship with the staf Evaluation: Three days later... ####### Current VS: Most Recent: Current PQRST: T: 97.8 F/36.6 C (oral) T: 97.4 F/36.3 C (oral) P rovoking/Palliative: “Standing and moving” P: 66 (reg) P: 68 (reg) Q uality: “Dull” R: 16 (reg) R: 16 (reg) R egion/Radiation: “Lower back” BP: 104/68 BP: 120/74 S everity: “6/10” O2 sat: 98% room air O2 sat: 99% room air T iming: “All the time.” Blood Glucose: 165 ####### Current Assessment: GENERAL APPEARANCE: Resting comfortably appears in no acute distress RESP: Breath sounds clear with equal aeration bilaterally, nonlabored respiratory effort CARDIAC: Pink, warm & dry, no edema, heart sounds regular with no abnormal beats, pulses strong, equal with palpation at radial/pedal/post-tibial landmarks GI: Abdomen soft/nontender, bowel sounds audible per auscultation in all four quadrants GU: Continues to be incontinent but is agreeable to be changed. The results of the urinalysis returned and were negative. SKIN: Skin folds in the peri area are red and irritated. ####### Mental Status Examination (MSE): APPEARANCE: Dressed in a clean t-shirt and pants. Patient has a new adult diaper in place MOTOR BEHAVIOR: Ambulates with walker, shuffling gait SPEECH: Clear MOOD/AFFECT: Pleasant, except when talking about Pineville Estates, then becomes agitated. Anxiety increases, and angry affect displayed; easily becomes angry. THOUGHT PROCESS: Generally coherent conversation; can make himself understood. THOUGHT CONTENT: Continues to display some agitation about Pineville Estates. States, “I can take care of myself. There is nothing they do for me that I can’t do for myself. It is against the law for them to keep me here.” PERCEPTION: No other current evidence of hallucinations INSIGHT/JUDGMENT: Insight – poor as evidenced by not understanding why he needs to be at a facility and not at home. (Thinks he is here for rehab) Unable to recognize own deficits in functioning. Judgment Poor Continues to ask his wife to bring him in takeout food. Stated, “I don’t eat dinner in the cafeteria.” COGNITION: The client’s neuropsychiatric evaluation was completed, and it was determined that the cause of the patient’s dementia is Alzheimer’s disease. Oriented to person and place. Not oriented to time or purpose. Believes it is 2017. Able to recognize it is spring. Short-term memory impaired: Doesn’t always remember that he has eaten a meal, forgets that wife visits; forgets to use a walker. Long-term memory seems to be intact. Remembers personal history. INTERACTIONS: Pleasant when spoken to. Hesitant to initiate conversation. SUICIDAL/HOMICIDAL: Stated, “I would rather die than live in a nursing home.” Also expressed that he would never do anything to hurt himself because of his Catholic faith. 19.What clinical data are RELEVANT that must be recognized as clinically significant? (Reduction of Risk Potential/Health Promotion and Maintenance) RELEVANT VS Data: Clinical Significance: BP is low (104/68) and has dropped quite a bit Current blood glucose is starting to climb again. (from 148 to 165) Pain 6/10 shows an increase BP and hyperglycemia can be inversely related. When blood glucose levels are increase, blood volume and BP can become low. It is also suspected that both may be having an impact on the kidneys. Lower back pain may be related to kidney issues, which would relate to the blood glucose and could affect BP as well. RELEVANT Assessment Data: Clinical Significance: Incontinence continues to be an issue. There is some irritation and redness in the peri area. Incontinence continues, UTI has been ruled out. Wearing an adult diaper is causing some skin breakdown which can lead to an infection. RELEVANT MSE Assessment Data: Clinical Significance: Sill agitated; resistant to the idea of being at the Pineville. Does not realize he needs assistance with ADLS, poor judgement. Paient diagnosed with AD AOx2, short term impaired Depressed but not suicidal Does not want to be there and is less likely to adhere to treatment plans. Less likely to ask for help with ADLs because of pride or does not realize he needs help which increases his risk for injury. Paients with AD have problems with short term memory and AO. Paient is depressed which can lead to lack of moivaion 20.Has the status improved or not as expected to this point? Does your nursing priority or plan of care need ####### to be modified in any way after this evaluation assessment? (Management of Care, Physiological Adaptation) ####### Evaluation of Current Status: Modifications to Current Plan of Care: The patient has shown some improvement in areas and worsened in some systems. Blood pressure medications should be adjusted to prevent hypotension. ####### Day of admission/post-op #: Admitted 4 months ago B ackground: ####### Primary problem/diagnosis: ####### RELEVANT past medical history: Patient has a history of heart failure. He was hospitalized 3x in the ####### past 6 months exacerbation of HF, COPD, hypertension, type 2 diabetes. DM has been uncontrolled ####### for the past few days. Patient was taken off oral antidiabetics to insulin glargine 10 units SQ but BS ####### remains elevated. He has experienced problems with depression, insomnia, hallucinations, and ####### confusion. He was recently put on trazadone 50mg PO HS PRN for insomnia, haloperidol 2.5mg PO ####### BID for hallucinations and is on memantine 10mg PO QD, which was increased recently and ####### donepezil 5 mg PO QD. Receiving acetaminophen prn 325mg q6h for lower back pain 6/10. Takes ####### fluticasone/salmeterol 1 puff q12h for and Albuterol 2 puffs q4h PRN for COPD, Lisinopril 10 mg PO ####### QD and Atenolol 25 mg PO bid, but BP has been low today. Monitor VS if BP gets too low. Furosemide ####### 20mg PO QD and HCTZ 25 mg QD PO for HF. ####### RELEVANT background data: A&O x 2. Patient has been urine incontinent and wearing an adult ####### diaper as a result. Peri areas is red and irritated due to increased moisture of adult diaper, may need ####### some barrier cream. He is agitated and angered easily when talking about living here and struggles ####### with some suicidal type thoughts but says his faith will not permit him to carry out a plan. Otherwise ####### pleasant to speak with. Patient is on fall precautions due to increased fall risk. Patient has shuffling ####### gait and requires a walker to ambulate but forgets. He will sometimes eat two dinners because he ####### forgets that he ate so wife brings him fast food. Married x 51 years to his wife Rita, who has ####### guardianship over him, and has 3 adult children visit him regularly. Patient is hesitant to initiate ####### conversations but can still communicate. A ssessment: ####### Most recent vital signs: T: 97.8 F, P: 66/reg, R: 16/reg, BP: 104/68, O2 sat: 98% RA, Pain 6/10, dull lower back pain ####### RELEVANT body system nursing assessment data: ####### GU: Continue to monitor back pain, urinary incontinence, and along with peri skin. Dementia: ####### monitor S&S of anger and depression and possibly trying to leave facility. CV: BP is trending towards ####### hypotension. Monitor VS closely. Endo: Monitor blood glucose closely and pay attention to dining ####### habits. Neuro: Assess for fall risk and help patient to ambulate ####### RELEVANT lab values: K 3.4 may need to treat and continue to observe, Creatinine 1.2, previous Hgb ####### A1c of 7.8 current blood glucose: 165. ####### TREND of any abnormal clinical data (stable increasing/decreasing): Blood glucose: increasing, ####### BP: decreasing, Pain: increasing, Mood: stable but easily angered ####### How have you advanced the plan of care? Memantine has been increased and added donepezil. AD ####### symptoms more controlled, added insulin glargine, initial decrease in blood glucose now on the climb. ####### Patient response: Trazadone has helped sundowning/insomnia symptoms but not the depression. Had ####### a UA done, but shows no infection. Administered haloperidol resulting in no more hallucinations. ####### INTERPRETATION of current clinical status (stable/unstable/worsening): Blood glucose is ####### worsening/unstable. BP is unstable, continuing to trend towards being hypotensive. Pain in lower ####### back is worsening. Need to check kidney funcion. R ecommendation: ####### Suggestions to advance the plan of care: Need to assess for etiology of blood glucose increase and monitor for blood glucose changes. Alert physician if BP falls below 100/60, and potentially decrease antihypertensive dosages. Possible referral for renal US and more kidney function tests- BUN, creatinine, GFR. Education Priorities/Discharge Planning 22.What educational/discharge priorities will be needed to develop a teaching plan for this patient and/or family? (Health Promotion and Maintenance) ####### Education PRIORITY: Patient needs to be educated about his blood glucose and the ####### impact of eating too many meals. ####### PRIORITY Topics to Teach: Rationale: Needs to manage if he had eaten his dinner already using a food diary so that he can remember that he had eaten. Teach wife/family to look at food diary before bringing meals to the patient and log that meal on the food diary so that staff can be aware of his meal status. Wife also needs to be educated on what types of food are best for his health. Eating too many meals is adversely increasing the patient’s blood glucose, which can negatively affect his kidney function, continuing to deteriorate brain function The family needs to be able to help the paient adhere to food restricions and medicaion management so educaing them is imperaive as well. Caring and the “Art” of Nursing 23.What is the patient likely experiencing/feeling right now in this situation? What can you do to engage ####### yourself with this patient’s experience, and show that he/she matters to you as a person? ( Psychosocial Integrity) ####### What Patient is Experiencing: How to Engage: The paient seems to be frustrated and helpless. The paient is feeling like his independence is being stripped and is confused as to why he needs the long-term care. This can also cause fear and paranoia. Help promote the paient’s independence by helping to do bladder training to get him out of adult diapers and back to self-toileing. Give the paient charge of self-care whenever possible. Talk to paient when he is feeling frustrated or sad and form a therapeuic relaionship. Help paient come to terms with his deicits. Use Reflection to THINK Like a Nurse Reflection-IN-action (Tanner, 2006) is the nurse’s ability to accurately interpret the patient’s response to an intervention at the moment as the events are unfolding to make a correct clinical judgment. [Show More]
Last updated: 1 year ago
Preview 1 out of 18 pages
Instant download
Buy this document to get the full access instantly
Instant Download Access after purchase
Add to cartInstant download
Reviews( 0 )
Document information
Connected school, study & course
About the document
Uploaded On
Jul 26, 2022
Number of pages
18
Written in
Additional information
This document has been written for:
Uploaded
Jul 26, 2022
Downloads
0
Views
53




 Correct Study Guide, Download to Score A.png)
 Correct Study Guide, Download to Score A.png)
 Correct Study Guide, Download to Score A.png)
 Correct Study Guide, Download to Score A.png)
 Correct Study Guide, Download to Score A.png)
 Correct Study Guide, Download to Score A.png)

