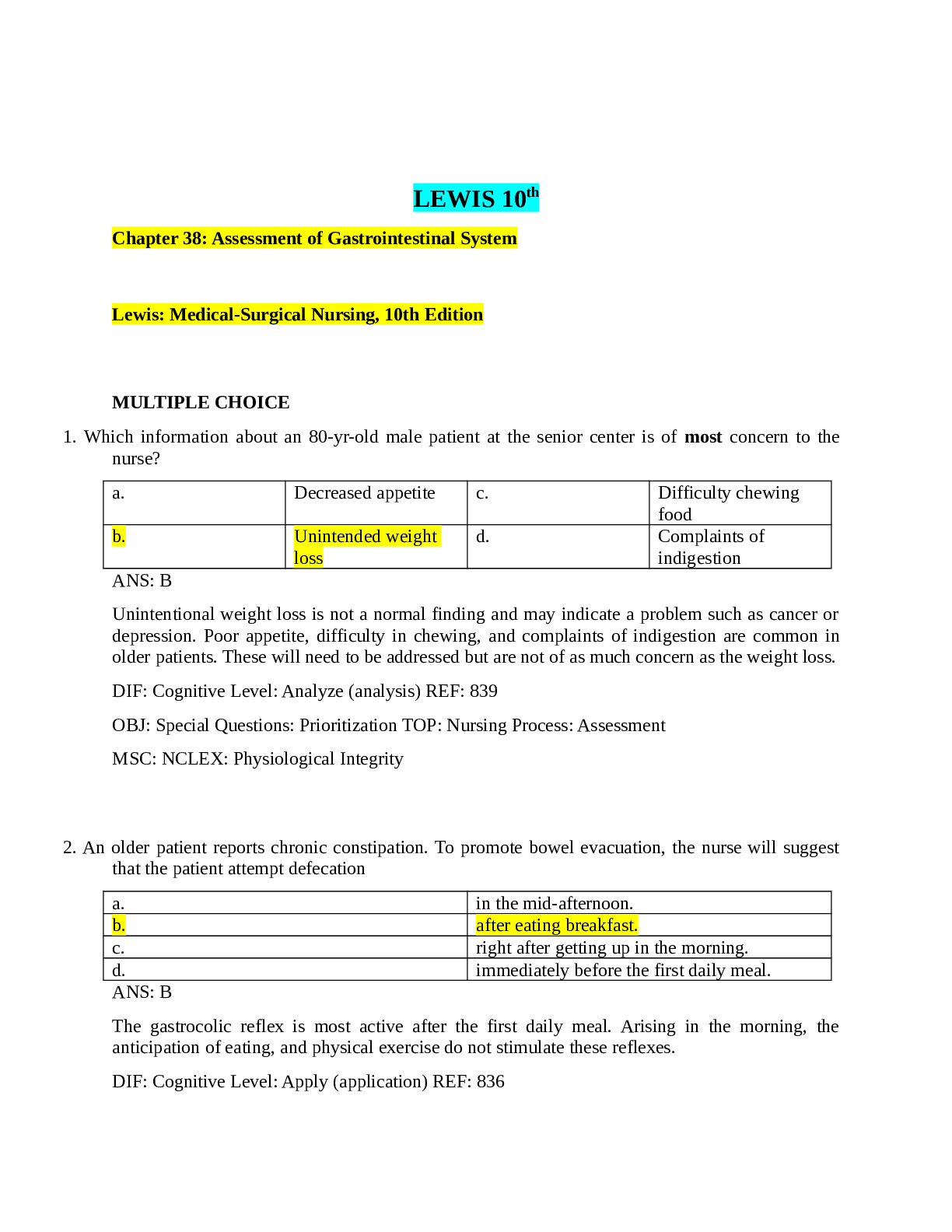
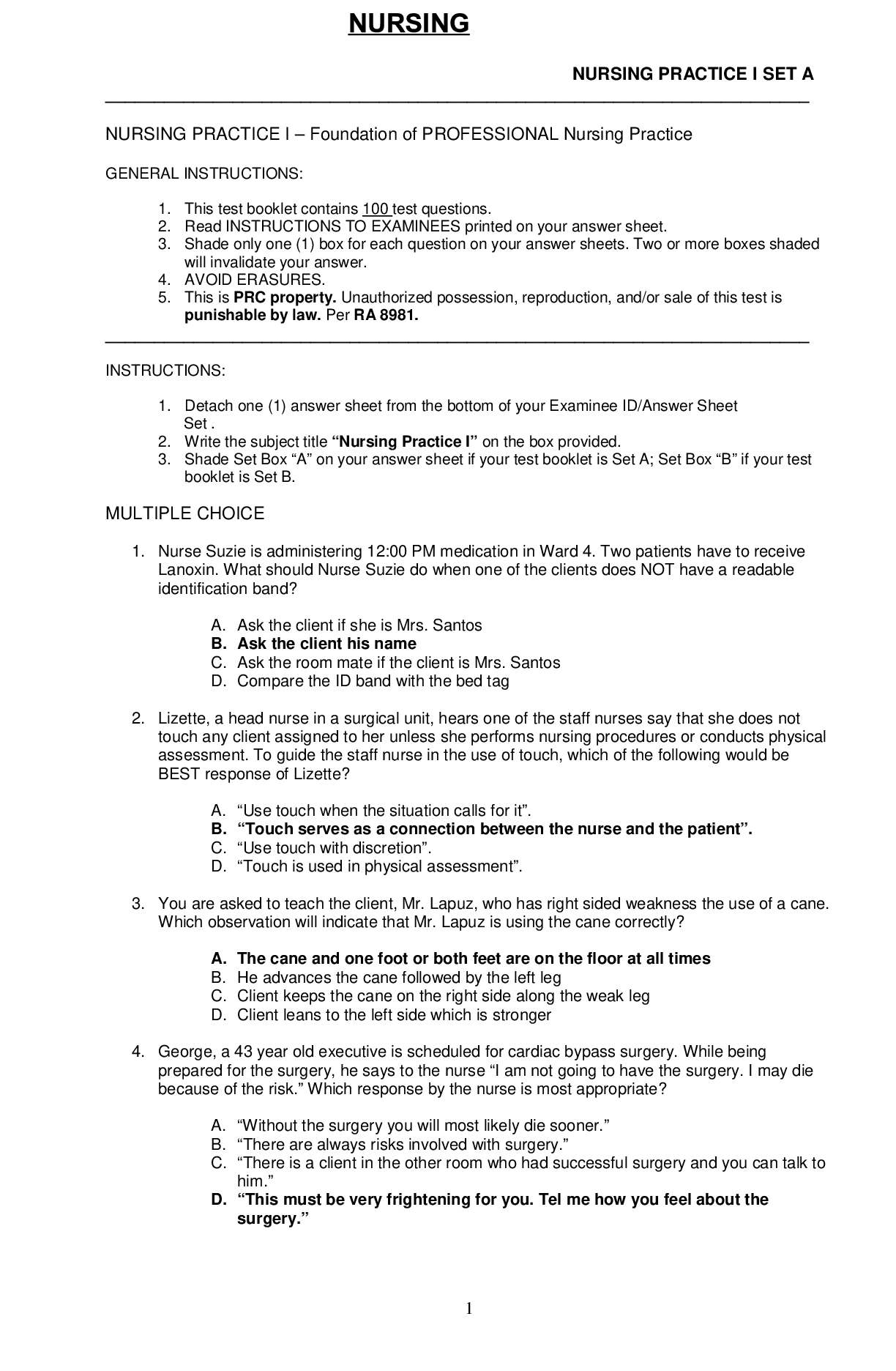
*NURSING > TEST BANK > Chapter 01: Professional Nursing Practice Lewis: Medical-Surgical Nursing, 10th Edition MULTIPLE CHO (All)
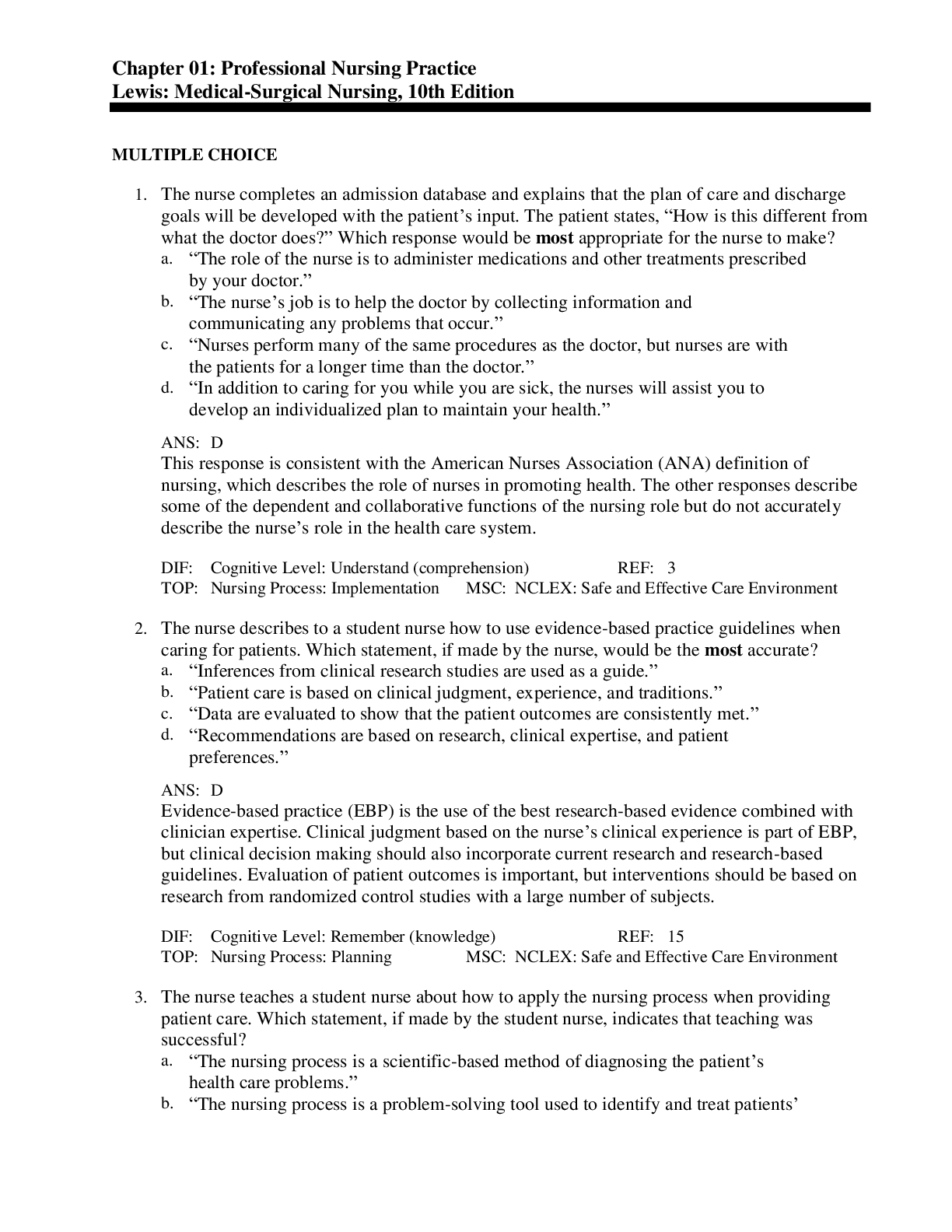
Chapter 01: Professional Nursing Practice Lewis: Medical-Surgical Nursing, 10th Edition MULTIPLE CHOICE
Document Content and Description Below
Chapter 01: Professional Nursing Practice Lewis: Medical-Surgical Nursing, 10th Edition MULTIPLE CHOICE 1. The nurse completes an admission database and explains that the plan of care and discharge... goals will be developed with the patient’s input. The patient states, “How is this different from what the doctor does?” Which response would be most appropriate for the nurse to make? a. “The role of the nurse is to administer medications and other treatments prescribed by your doctor.” b. “The nurse’s job is to help the doctor by collecting information and communicating any problems that occur.” c. “Nurses perform many of the same procedures as the doctor, but nurses are with the patients for a longer time than the doctor.” d. “In addition to caring for you while you are sick, the nurses will assist you to develop an individualized plan to maintain your health.” ANS: D This response is consistent with the American Nurses Association (ANA) definition of nursing, which describes the role of nurses in promoting health. The other responses describe some of the dependent and collaborative functions of the nursing role but do not accurately describe the nurse’s role in the health care system. DIF: Cognitive Level: Understand (comprehension) REF: 3 TOP: Nursing Process: Implementation MSC: NCLEX: Safe and Effective Care Environment 2. The nurse describes to a student nurse how to use evidence-based practice guidelines when caring for patients. Which statement, if made by the nurse, would be the most accurate? a. “Inferences from clinical research studies are used as a guide.” b. “Patient care is based on clinical judgment, experience, and traditions.” c. “Data are evaluated to show that the patient outcomes are consistently met.” d. “Recommendations are based on research, clinical expertise, and patient preferences.” ANS: D Evidence-based practice (EBP) is the use of the best research-based evidence combined with clinician expertise. Clinical judgment based on the nurse’s clinical experience is part of EBP, but clinical decision making should also incorporate current research and research-based guidelines. Evaluation of patient outcomes is important, but interventions should be based on research from randomized control studies with a large number of subjects. DIF: Cognitive Level: Remember (knowledge) REF: 15 TOP: Nursing Process: Planning MSC: NCLEX: Safe and Effective Care Environment 3. The nurse teaches a student nurse about how to apply the nursing process when providing patient care. Which statement, if made by the student nurse, indicates that teaching was successful? a. “The nursing process is a scientific-based method of diagnosing the patient’s health care problems.” b. “The nursing process is a problem-solving tool used to identify and treat patients’health care needs.” c. “The nursing process is used primarily to explain nursing interventions to other health care professionals.” d. “The nursing process is based on nursing theory that incorporates the biopsychosocial nature of humans.” ANS: B The nursing process is a problem-solving approach to the identification and treatment of patients’ problems. Diagnosis is only one phase of the nursing process. The primary use of the nursing process is in patient care, not to establish nursing theory or explain nursing interventions to other health care professionals. DIF: Cognitive Level: Understand (comprehension) REF: 5 TOP: Nursing Process: Implementation MSC: NCLEX: Safe and Effective Care Environment 4. A patient has been admitted to the hospital for surgery and tells the nurse, “I do not feel comfortable leaving my children with my parents.” Which action should the nurse take next? a. Reassure the patient that these feelings are common for parents. b. Have the patient call the children to ensure that they are doing well. c. Gather more data about the patient’s feelings about the child-care arrangements. d. Call the patient’s parents to determine whether adequate child care is being provided. ANS: C Because a complete assessment is necessary in order to identify a problem and choose an appropriate intervention, the nurse’s first action should be to obtain more information. The other actions may be appropriate, but more assessment is needed before the best intervention can be chosen. DIF: Cognitive Level: Apply (application) REF: 6 OBJ: Special Questions: Prioritization TOP: Nursing Process: Assessment MSC: NCLEX: Psychosocial Integrity 5. A patient who is paralyzed on the left side of the body after a stroke develops a pressure ulcer on the left hip. Which nursing diagnosis is most appropriate? a. Impaired physical mobility related to left-sided paralysis b. Risk for impaired tissue integrity related to left-sided weakness c. Impaired skin integrity related to altered circulation and pressure d. Ineffective tissue perfusion related to inability to move independently ANS: C The patient’s major problem is the impaired skin integrity as demonstrated by the presence of a pressure ulcer. The nurse is able to treat the cause of altered circulation and pressure by frequently repositioning the patient. Although left-sided weakness is a problem for the patient, the nurse cannot treat the weakness. The “risk for” diagnosis is not appropriate for this patient, who already has impaired tissue integrity. The patient does have ineffective tissue perfusion, but the impaired skin integrity diagnosis indicates more clearly what the health problem is. DIF: Cognitive Level: Apply (application) REF: 7 TOP: Nursing Process: Diagnosis MSC: NCLEX: Physiological Integrity6. A patient with a bacterial infection has a nursing diagnosis of deficient fluid volume related to excessive diaphoresis. Which outcome would the nurse recognize as appropriate for this patient? a. Patient has a balanced intake and output. b. Patient’s bedding is changed when it becomes damp. c. Patient understands the need for increased fluid intake. d. Patient’s skin remains cool and dry throughout hospitalization. ANS: A This statement gives measurable data showing resolution of the problem of deficient fluid volume that was identified in the nursing diagnosis statement. The other statements would not indicate that the problem of deficient fluid volume was resolved. DIF: Cognitive Level: Apply (application) REF: 7 TOP: Nursing Process: Planning MSC: NCLEX: Physiological Integrity 7. A nurse asks the patient if pain was relieved after receiving medication. What is the purpose of the evaluation phase of the nursing process? a. To determine if interventions have been effective in meeting patient outcomes b. To document the nursing care plan in the progress notes of the medical record c. To decide whether the patient’s health problems have been completely resolved d. To establish if the patient agrees that the nursing care provided was satisfactory ANS: A Evaluation consists of determining whether the desired patient outcomes have been met and whether the nursing interventions were appropriate. The other responses do not describe the evaluation phase. DIF: Cognitive Level: Understand (comprehension) REF: 5 TOP: Nursing Process: Evaluation MSC: NCLEX: Safe and Effective Care Environment 8. The nurse interviews a patient while completing the health history and physical examination. What is the purpose of the assessment phase of the nursing process? a. To teach interventions that relieve health problems b. To use patient data to evaluate patient care outcomes c. To obtain data with which to diagnose patient problems d. To help the patient identify realistic outcomes for health problems ANS: C During the assessment phase, the nurse gathers information about the patient to diagnose patient problems. The other responses are examples of the planning, intervention, and evaluation phases of the nursing process. DIF: Cognitive Level: Understand (comprehension) REF: 5 TOP: Nursing Process: Assessment MSC: NCLEX: Safe and Effective Care Environment 9. Which nursing diagnosis statement is written correctly? a. Altered tissue perfusion related to heart failure b. Risk for impaired tissue integrity related to sacral redness c. Ineffective coping related to response to biopsy test results d. Altered urinary elimination related to urinary tract infectionANS: C This diagnosis statement includes a NANDA nursing diagnosis and an etiology that describes a patient’s response to a health problem that can be treated by nursing. The use of a medical diagnosis as an etiology (as in the responses beginning “Altered tissue perfusion” and “Altered urinary elimination”) is not appropriate. The response beginning “Risk for impaired tissue integrity” uses the defining characteristic as the etiology. DIF: Cognitive Level: Understand (comprehension) REF: 7 TOP: Nursing Process: Diagnosis MSC: NCLEX: Safe and Effective Care Environment 10. The nurse admits a patient to the hospital and develops a plan of care. What components should the nurse include in the nursing diagnosis statement? a. The problem and the suggested patient goals or outcomes b. The problem with possible causes and the planned interventions c. The problem, its cause, and objective data that support the problem d. The problem with an etiology and the signs and symptoms of the problem ANS: D When writing nursing diagnoses, this format should be used: problem, etiology, and signs and symptoms. The subjective, as well as objective, data should be included in the defining characteristics. Interventions and outcomes are not included in the nursing diagnosis statement. DIF: Cognitive Level: Remember (knowledge) REF: 7 TOP: Nursing Process: Diagnosis MSC: NCLEX: Safe and Effective Care Environment 11. A nurse is caring for a patient with heart failure. Which task is appropriate for the nurse to delegate to experienced unlicensed assistive personnel (UAP)? a. Monitor for shortness of breath or fatigue after ambulation. b. Instruct the patient about the need to alternate activity and rest. c. Obtain the patient’s blood pressure and pulse rate after ambulation. d. Determine whether the patient is ready to increase the activity level. ANS: C UAP education includes accurate vital sign measurement. Assessment and patient teaching require registered nurse education and scope of practice and cannot be delegated. DIF: Cognitive Level: Apply (application) REF: 11 OBJ: Special Questions: Delegation TOP: Nursing Process: Planning MSC: NCLEX: Safe and Effective Care Environment 12. A nurse is caring for a group of patients on the medical-surgical unit with the help of one float registered nurse (RN), one unlicensed assistive personnel (UAP), and one licensed practical/vocational nurse (LPN/LVN). Which assignment, if delegated by the nurse, would be inappropriate? a. Measurement of a patient’s urine output by UAP b. Administration of oral medications by LPN/LVN c. Check for the presence of bowel sounds and flatulence by UAP d. Care of a patient with diabetes by RN who usually works on the pediatric unit ANS: CAssessment requires RN education and scope of practice and cannot be delegated to an LPN/LVN or UAP. The other assignments made by the RN are appropriate. DIF: Cognitive Level: Apply (application) REF: 11 OBJ: Special Questions: Delegation TOP: Nursing Process: Planning MSC: NCLEX: Safe and Effective Care Environment 13. Which task is appropriate for the nurse to delegate to a licensed practical/vocational nurse (LPN/LVN)? a. Complete the initial admission assessment and plan of care. b. Document teaching completed before a diagnostic procedure. c. Instruct a patient about low-fat, reduced sodium dietary restrictions. d. Obtain bedside blood glucose on a patient before insulin administration. ANS: D The education and scope of practice of the LPN/LVN include activities such as obtaining glucose testing using a finger stick. Patient teaching and the initial assessment and development of the plan of care are nursing actions that require registered nurse education and scope of practice. DIF: Cognitive Level: Apply (application) REF: 11 OBJ: Special Questions: Delegation TOP: Nursing Process: Planning MSC: NCLEX: Safe and Effective Care Environment 14. A nurse is assigned as a case manager for a hospitalized patient with a spinal cord injury. The patient can expect the nurse functioning in this role to perform which activity? a. Care for the patient during hospitalization for the injuries. b. Assist the patient with home care activities during recovery. c. Determine what medical care the patient needs for optimal rehabilitation. d. Coordinate the services that the patient receives in the hospital and at home. ANS: D The role of the case manager is to coordinate the patient’s care through multiple settings and levels of care to allow the maximal patient benefit at the least cost. The case manager does not provide direct care in either the acute or home setting. The case manager coordinates and advocates for care but does not determine what medical care is needed; that would be completed by the health care provider or other provider. DIF: Cognitive Level: Apply (application) REF: 9 TOP: Nursing Process: Implementation MSC: NCLEX: Safe and Effective Care Environment 15. The nurse is caring for an older adult patient who had surgery to repair a fractured hip. The patient needs continued nursing care and physical therapy to improve mobility before returning home. The nurse will help to arrange for transfer of this patient to which facility? a. A skilled care facility c. A transitional care facility b. A residential care facility d. An intermediate care facility ANS: CTransitional care settings are appropriate for patients who need continued rehabilitation before discharge to home or to long-term care settings. The patient is no longer in need of the more continuous assessment and care given in acute care settings. There is no indication that the patient will need the permanent and ongoing medical and nursing services available in intermediate or skilled care. The patient is not yet independent enough to transfer to a residential care facility. DIF: Cognitive Level: Apply (application) REF: 8 TOP: Nursing Process: Planning MSC: NCLEX: Safe and Effective Care Environment 16. A home care nurse is planning care for a patient who has just been diagnosed with type 2 diabetes mellitus. Which task is appropriate for the nurse to delegate to the home health aide? a. Assist the patient to choose appropriate foods. b. Help the patient with a daily bath and oral care. c. Check the patient’s feet for signs of breakdown. d. Teach the patient how to monitor blood glucose. ANS: B Assisting with patient hygiene is included in home health-aide education and scope of practice. Assessment of the patient and instructing the patient in new skills, such as diet and blood glucose monitoring, are complex skills that are included in registered nurse education and scope of practice. DIF: Cognitive Level: Apply (application) REF: 11 OBJ: Special Questions: Delegation TOP: Nursing Process: Implementation MSC: NCLEX: Safe and Effective Care Environment 17. The nurse is providing education to nursing staff on quality care initiatives. Which statement is an accurate description of the impact of health care financing on quality care? a. “If a patient develops a catheter-related infection, the hospital receives additional funding.” b. “Payment for patient care is primarily based on clinical outcomes and patient satisfaction.” c. “Hospitals are reimbursed for all costs incurred if care is documented electronically.” d. “Because hospitals are accountable for overall care, it is not nursing’s responsibility to monitor care delivered by others.” ANS: B Payment for health care services programs reimburses hospitals for their performance on overall quality-of-care measures. These measures include clinical outcomes and patient satisfaction. Nurses are responsible for coordinating complex aspects of patient care, including the care delivered by others, and identifying issues that are associated with poor quality care. Payment for care can be withheld if something happens to the patient that is considered preventable (e.g., acquiring a catheter-related urinary tract infection). DIF: Cognitive Level: Apply (application) REF: 4 TOP: Nursing Process: Implementation MSC: NCLEX: Safe and Effective Care Environment18. The nurse documenting the patient’s progress in the care plan in the electronic health record before an interprofessional discharge conference is demonstrating competency in which QSEN category? a. Patient-centered care c. Evidence-based practice b. Quality improvement d. Informatics and technology ANS: D The nurse is displaying competency in the QSEN area of informatics and technology. Using a computerized information system to document patient needs and progress and communicate vital information regarding the patient with the interprofessional care team members provides evidence that nursing practice standards related to the nursing process have been maintained during the care of the patient. DIF: Cognitive Level: Apply (application) REF: 13 TOP: Nursing Process: Implementation MSC: NCLEX: Safe and Effective Care Environment MULTIPLE RESPONSE 1. Which information will the nurse consider when deciding what nursing actions to delegate to a licensed practical/vocational nurse (LPN/LVN) who is working on a medical-surgical unit (select all that apply)? a. Institutional policies b. Stability of the patient c. State nurse practice act d. LPN/LVN teaching abilities e. Experience of the LPN/LVN ANS: A, B, C, E The nurse should assess the experience of LPN/LVNs when delegating. In addition, state nurse practice acts and institutional policies must be considered. In general, whereas the LPN/LVN scope of practice includes caring for patients who are stable, registered nurses should provide most of the care for unstable patients. Because the LPN/LVN scope of practice does not include patient education, this will not be part of the delegation process. DIF: Cognitive Level: Apply (application) REF: 11 OBJ: Special Questions: Delegation TOP: Nursing Process: Planning MSC: NCLEX: Safe and Effective Care Environment 2. The nurse is administering medications to a patient. Which actions by the nurse during this process are consistent with promoting safe delivery of care (select all that apply)? a. Throws away a medication that is not labeled b. Uses a hand sanitizer before preparing a medication c. Identifies the patient by the room number on the door d. Checks laboratory test results before administering a diuretic e. Gives the patient a list of current medications upon discharge ANS: A, B, D, ENational Patient Safety Goals have been established to promote safe delivery of care. The nurse should use at least two reliable ways to identify the patient such as asking the patient’s full name and date of birth before medication administration. Other actions that improve patient safety include performing hand hygiene, disposing of unlabeled medications, completing appropriate assessments before administering medications, and giving a list of the current medicines to the patient and caregiver before discharge. DIF: Cognitive Level: Apply (application) REF: 12 TOP: Nursing Process: Implementation MSC: NCLEX: Safe and Effective Care Environment OTHER 1. The nurse uses the Situation-Background-Assessment-Recommendation (SBAR) format to communicate a change in patient status to a health care provider. In which order should the nurse make the following statements? (Put a comma and a space between each answer choice [A, B, C, D].) a. “The patient needs to be evaluated immediately and may need intubation and mechanical ventilation.” b. “The patient was admitted yesterday with heart failure and has been receiving furosemide (Lasix) for diuresis, but urine output has been low.” c. “The patient has crackles audible throughout the posterior chest, and the most recent oxygen saturation is 89%. Her condition is very unstable.” d. “This is the nurse on the surgical unit. After assessing the patient, I am very concerned about increased shortness of breath over the past hour.” ANS: D, B, C, A The order of the nurse’s statements follows the SBAR format. DIF: Cognitive Level: Apply (application) REF: 11 OBJ: Special Questions: Prioritization TOP: Nursing Process: Implementation MSC: NCLEX: Safe and Effective Care EnvironmentChapter 02: Health Disparities and Culturally Competent Care Lewis: Medical-Surgical Nursing, 10th Edition MULTIPLE CHOICE 1. The nurse is obtaining a health history from a new patient. Which data will be the focus of patient teaching? a. Age and gender c. Hispanic/Latino ethnicity b. Saturated fat intake d. Family history of diabetes ANS: B Behaviors are strongly linked to many health care problems. The patient’s saturated fat intake is a behavior that the patient can change. The other information will be useful as the nurse develops an individualized plan for improving the patient’s health, but will not be the focus of patient teaching. DIF: Cognitive Level: Apply (application) REF: 18 TOP: Nursing Process: Planning MSC: NCLEX: Health Promotion and Maintenance 2. The nurse works in a clinic located in a community with many Hispanics. Which strategy, if implemented by the nurse, would decrease health care disparities for the Hispanic patients? a. Improve public transportation to the clinic. b. Update equipment and supplies at the clinic. c. Obtain low-cost medications for clinic patients. d. Teach clinic staff about Hispanic health beliefs. ANS: D Health care disparities are caused by stereotyping, biases, and prejudice of health care providers. The nurse can decrease these through staff education. The other strategies may also be addressed by the nurse but will not directly impact health disparities. DIF: Cognitive Level: Apply (application) REF: 19 TOP: Nursing Process: Planning MSC: NCLEX: Health Promotion and Maintenance 3. What information should the nurse collect when assessing the health status of a community? a. Air pollution levels c. Most common causes of death b. Number of health food stores d. Education level of the individuals ANS: C Health status measures of a community include birth and death rates, life expectancy, access to care, and morbidity and mortality rates related to disease and injury. Although air pollution, access to health food stores, and education level are factors that affect a community’s health status, they are not health measures. DIF: Cognitive Level: Understand (comprehension) REF: 18 TOP: Nursing Process: Assessment MSC: NCLEX: Health Promotion and Maintenance 4. The nurse is caring for a Native American patient who has traditional beliefs about health and illness. Which action by nurse is most appropriate? a. Avoid asking questions unless the patient initiates the conversation. b. Ask the patient whether it is important that cultural healers are contacted.c. Explain the usual hospital routines for meal times, care, and family visits. d. Obtain further information about the patient’s cultural beliefs from a family member. ANS: B Because the patient has traditional health care beliefs, it is appropriate for the nurse to ask whether the patient would like a visit by a shaman or other cultural healer. There is no cultural reason for the nurse to avoid asking the patient questions because these questions are necessary to obtain health information. The patient (rather than the family) should be consulted about personal cultural beliefs. The hospital routines for meals, care, and visits should be adapted to the patient’s preferences rather than expecting the patient to adapt to the hospital schedule. DIF: Cognitive Level: Apply (application) REF: 24 TOP: Nursing Process: Implementation MSC: NCLEX: Psychosocial Integrity 5. The nurse is caring for an Asian patient who is being admitted to the hospital. Which action would be most appropriate for the nurse to take when interviewing this patient? a. Avoid eye contact with the patient. b. Observe the patient’s use of eye contact. c. Look directly at the patient when interacting. d. Ask a family member about the patient’s cultural beliefs. ANS: B Observation of the patient’s use of eye contact will be most useful in determining the best way to communicate effectively with the patient. Looking directly at the patient or avoiding eye contact may be appropriate, depending on the patient’s individual cultural beliefs. The nurse should assess the patient, rather than asking family members about the patient’s beliefs. DIF: Cognitive Level: Apply (application) REF: 25 TOP: Nursing Process: Implementation MSC: NCLEX: Psychosocial Integrity 6. A female staff nurse is assessing a male patient of Arab descent who is admitted with complaints of severe headaches. It is most important for the charge nurse to intervene if the nurse takes which action? a. The nurse explains the 0 to 10 intensity pain scale. b. The nurse asks the patient when the headaches started. c. The nurse sits down at the bedside and closes the privacy curtain. d. The nurse calls for a male nurse to bring a hospital gown to the room. ANS: C Many men of Arab ethnicity do not believe it is appropriate to be alone with any female except for their spouse. The other actions are appropriate. DIF: Cognitive Level: Apply (application) REF: 25 TOP: Nursing Process: Implementation MSC: NCLEX: Psychosocial Integrity 7. The nurse is caring for a patient who speaks a different language. If an interpreter is not available, which action by the nurse is most appropriate? a. Talk slowly so that each word is clearly heard. b. Speak loudly in close proximity to the patient’s ears. c. Repeat important words so that the patient recognizes their significance.d. Use simple gestures to demonstrate meaning while talking to the patient. ANS: D The use of gestures will enable some information to be communicated to the patient. The other actions will not improve communication with the patient. DIF: Cognitive Level: Understand (comprehension) REF: 31 TOP: Nursing Process: Implementation MSC: NCLEX: Psychosocial Integrity 8. The nurse plans care for a hospitalized patient who uses culturally based treatments. Which action by the nurse is best? a. Encourage the use of diagnostic procedures. b. Coordinate the use of folk treatments with ordered medical therapies. c. Ask the patient to discontinue the cultural treatments during hospitalization. d. Teach the patient that folk remedies will interfere with orders by the health care provider. ANS: B Many culturally based therapies can be accommodated along with the use of Western treatments and medications. The nurse should attempt to use both traditional folk treatments and the ordered Western therapies as much as possible. Some culturally based treatments can be effective in treating “Western” diseases. Not all folk remedies interfere with Western therapies. It may be appropriate for the patient to continue some culturally based treatments while he or she is hospitalized. DIF: Cognitive Level: Apply (application) REF: 22 TOP: Nursing Process: Planning MSC: NCLEX: Psychosocial Integrity 9. The nurse is caring for a newly admitted patient. Which intervention is the best example of a culturally appropriate nursing intervention? a. Insist family members provide most of the patient’s personal care. b. Maintain a personal space of at least 2 feet when assessing the patient. c. Ask permission before touching a patient during the physical assessment. d. Consider the patient’s ethnicity as the most important factor in planning care. ANS: C Many cultures consider it disrespectful to touch a patient without asking permission, so asking a patient for permission is always culturally appropriate. The other actions may be appropriate for some patients but are not appropriate across all cultural groups or for all individual patients. Ethnicity may not be the most important factor in planning care, especially if the patient has urgent physiologic problems. DIF: Cognitive Level: Understand (comprehension) REF: 28 TOP: Nursing Process: Implementation MSC: NCLEX: Psychosocial Integrity 10. A staff nurse expresses frustration that a Native American patient always has several family members at the bedside. Which action by the charge nurse is most appropriate? a. Remind the nurse that family support is important to this family and patient. b. Have the nurse explain to the family that too many visitors will tire the patient. c. Suggest that the nurse ask family members to leave the room during patient care. d. Ask about the nurse’s personal beliefs about family support during hospitalization.ANS: D The first step in providing culturally competent care is to understand one’s own beliefs and values related to health and health care. Asking the nurse about personal beliefs will help achieve this step. Reminding the nurse that this cultural practice is important to the family and patient will not decrease the nurse’s frustration. The remaining responses (suggest that the nurse ask family members to leave the room and have the nurse explain to family that too many visitors will tire the patient) are not culturally appropriate for this patient. DIF: Cognitive Level: Apply (application) REF: 23 TOP: Nursing Process: Implementation MSC: NCLEX: Psychosocial Integrity 11. An older Asian American patient tells the nurse that she has lived in the United States for 50 years. The patient speaks English and lives in a predominantly Asian neighborhood. Which action by the nurse is most appropriate? a. Include a shaman when planning the patient’s care. b. Avoid direct eye contact with the patient during care. c. Ask the patient about any special cultural beliefs or practices. d. Involve the patient’s oldest son to assist with health care decisions. ANS: C Further assessment of the patient’s health care preferences is needed before making further plans for culturally appropriate care. The other responses indicate stereotyping of the patient based on ethnicity and would not be appropriate initial actions. DIF: Cognitive Level: Apply (application) REF: 23 TOP: Nursing Process: Planning MSC: NCLEX: Psychosocial Integrity 12. The nurse plans health care for a community with a large number of recent immigrants from Vietnam. Which intervention is the most important for the nurse to implement? a. Hepatitis testing c. Contraceptive teaching b. Tuberculosis screening d. Colonoscopy information ANS: B Tuberculosis (TB) is endemic in many parts of Asia, and the incidence of TB is much higher in immigrants from Vietnam than in the general U.S. population. Teaching about contraceptive use, colonoscopy, and testing for hepatitis may also be appropriate for some patients but is not generally indicated for all members of this community. DIF: Cognitive Level: Apply (application) REF: 28 TOP: Nursing Process: Planning MSC: NCLEX: Physiological Integrity 13. When doing an admission assessment for a patient, the nurse notices that the patient pauses before answering questions about the health history. Which action by the nurse is most appropriate? a. Interview a family member instead. b. Wait for the patient to answer the questions. c. Remind the patient that you have other patients who need care. d. Give the patient an assessment form listing the questions and a pen. ANS: BPatients from some cultures take time to consider a question carefully before answering. The nurse will show respect for the patient and help develop a trusting relationship by allowing the patient time to give a thoughtful answer. Asking the patient why the answers are taking so much time, stopping the assessment, and handing the patient a form indicate that the nurse does not have time for the patient. DIF: Cognitive Level: Apply (application) REF: 30 TOP: Nursing Process: Assessment MSC: NCLEX: Psychosocial Integrity 14. Which strategy should be a priority when the nurse is planning care for a diabetic patient who is uninsured? a. Obtain less expensive medications. b. Follow evidence-based practice guidelines. c. Assist with dietary changes as the first action. d. Teach about the impact of exercise on diabetes. ANS: B The use of standardized evidence-based guidelines will reduce the incidence of health care disparities among various socioeconomic groups. The other strategies may also be appropriate, but the priority concern should be that the patient receives care that meets the accepted standard. DIF: Cognitive Level: Apply (application) REF: 28 OBJ: Special Questions: Prioritization TOP: Nursing Process: Planning MSC: NCLEX: Health Promotion and Maintenance 15. A Hispanic patient complains of abdominal cramping caused by empacho. Which action should the nurse take first? a. Ask the patient what treatments are likely to help. b. Massage the patient’s abdomen until the pain is gone. c. Administer prescribed medications to decrease the cramping. d. Offer to contact a curandero(a) to make a visit to the patient. ANS: A Further assessment of the patient’s cultural beliefs is appropriate before implementing any interventions for a culture-bound syndrome such as empacho. Although medication, a visit by a curandero(a), or massage may be helpful, more information about the patient’s beliefs is needed to determine which intervention(s) will be most helpful. DIF: Cognitive Level: Apply (application) REF: 29 OBJ: Special Questions: Prioritization TOP: Nursing Process: Assessment MSC: NCLEX: Psychosocial Integrity 16. The nurse performs a cultural assessment with a patient from a different culture. Which action by the nurse should be taken first? a. Request an interpreter before interviewing the patient. b. Wait until a family member is available to help with the assessment. c. Ask the patient about any affiliation with a particular cultural group. d. Tell the patient what the nurse already knows about the patient’s culture. ANS: CAn early step in performing a cultural assessment is to determine whether the patient feels an affiliation with any cultural group. The other actions may be appropriate if the patient does identify with a particular culture. DIF: Cognitive Level: Apply (application) REF: 30 OBJ: Special Questions: Prioritization TOP: Nursing Process: Assessment MSC: NCLEX: Psychosocial Integrity 17. The nurse working in a clinic in a primarily African American community notes a higher incidence of uncontrolled hypertension in the patients. To correct this health disparity, which action should the nurse take first? a. Initiate a regular home-visit program by nurses working at the clinic. b. Schedule teaching sessions about low-salt diets at community events. c. Assess the perceptions of community members about the care at the clinic. d. Obtain low-cost antihypertensive drugs using funding from government grants. ANS: C Before other actions are taken, additional assessment data are needed to determine the reason for the disparity. The other actions also may be appropriate, but additional assessment is needed before the next action is selected. DIF: Cognitive Level: Apply (application) REF: 29 OBJ: Special Questions: Prioritization TOP: Nursing Process: Assessment MSC: NCLEX: Health Promotion and Maintenance MULTIPLE RESPONSE 1. The nurse is performing an admission assessment for a non–English-speaking patient who is from China. Which actions could the nurse take to enhance communication (select all that apply)? a. Use an electronic translation application. b. Use a telephone-based medical interpreter. c. Wait until an agency interpreter is available. d. Ask the patient’s teenage daughter to interpret. e. Use exaggerated gestures to convey information. ANS: A, B, C Electronic translation applications, telephone-based interpreters, and agency interpreters are all appropriate to use to communicate with non–English-speaking patients. When no interpreter is available, family members may be considered, but some information that will be needed in an admission assessment may be misunderstood or not shared if a child is used as the interpreter. Gestures are appropriate to use, but exaggeration of the gestures is not needed. DIF: Cognitive Level: Apply (application) REF: 31 TOP: Nursing Process: Assessment MSC: NCLEX: Psychosocial IntegrityChapter 03: Health History and Physical Examination Lewis: Medical-Surgical Nursing, 10th Edition MULTIPLE CHOICE 1. A patient who is actively bleeding is admitted to the emergency department. Which approach is best for the nurse to use to obtain a health history? a. Briefly interview the patient while obtaining vital signs. b. Obtain subjective data about the patient from family members. c. Omit subjective data collection and obtain the physical examination. d. Use the health care provider’s medical history to obtain subjective data. ANS: A In an emergency situation, the nurse may need to ask only the most pertinent questions for a specific problem and obtain more information later. A complete health history will include subjective information that is not available in the health care provider’s medical history. Family members may be able to provide some subjective data, but only the patient will be able to give subjective information about the bleeding. Because the subjective data about the cause of the patient’s bleeding will be essential, obtaining the physical examination alone will not provide sufficient information. DIF: Cognitive Level: Apply (application) REF: 40 TOP: Nursing Process: Assessment MSC: NCLEX: Health Promotion and Maintenance 2. Immediate surgery is planned for a patient with acute abdominal pain. Which question by the nurse will elicit the most complete information about the patient’s coping-stress tolerance pattern? a. “Can you rate your pain on a 0 to 10 scale?” b. “What do you think caused this abdominal pain?” c. “How do you feel about yourself and your hospitalization?” d. “Are there other major problems that are a concern right now?” ANS: D The coping–stress tolerance pattern includes information about other major stressors confronting the patient. The health perception–health management pattern includes information about the patient’s ideas about risk factors. Feelings about self and the hospitalization are assessed in the self-perception–self-concept pattern. Intensity of pain is part of the cognitive–perceptual pattern. DIF: Cognitive Level: Apply (application) REF: 37 TOP: Nursing Process: Assessment MSC: NCLEX: Psychosocial Integrity 3. During the health history interview, a patient tells the nurse about periodic fainting spells. Which question by the nurse will best elicit any associated clinical manifestations? a. “How frequently do you have the fainting spells?” b. “Where are you when you have the fainting spells?” c. “Do the spells tend to occur at any special time of day?” d. “Do you have any other symptoms along with the spells?” ANS: DAsking about other associated symptoms will provide the nurse more information about all the clinical manifestations related to the fainting spells. Information about the setting is obtained by asking where the patient was and what the patient was doing when the symptom occurred. The other questions from the nurse are appropriate for obtaining information about chronology and frequency. DIF: Cognitive Level: Apply (application) REF: 35 TOP: Nursing Process: Assessment MSC: NCLEX: Health Promotion and Maintenance 4. The nurse records the following general survey of a patient: “The patient is a 50-yr-old Asian female attended by her husband and two daughters. Alert and oriented. Does not make eye contact with the nurse and responds slowly, but appropriately, to questions. No apparent disabilities or distinguishing features.” What additional information should the nurse add to this general survey? a. Nutritional status b. Intake and output c. Reasons for contact with the health care system d. Comments of family members about his condition ANS: A The general survey also describes the patient’s general nutritional status. The other information will be obtained when doing the complete nursing history and examination but is not obtained through the initial scanning of a patient. DIF: Cognitive Level: Understand (comprehension) REF: 39 TOP: Nursing Process: Assessment MSC: NCLEX: Health Promotion and Maintenance 5. A nurse performs a health history and physical examination with a patient who has a right leg fracture. Which assessment would be a pertinent negative finding? a. Patient has several bruised and swollen areas on the right leg. b. Patient states that there have been no other recent health problems. c. Patient refuses to bend the right knee because of the associated pain. d. Patient denies having pain when the area over the fracture is palpated. ANS: D The nurse expects that a patient with a leg fracture will have pain over the fractured area. The bruising and swelling and pain with bending are positive findings. Having no other recent health problems is neither a positive nor a negative finding with regard to a leg fracture. DIF: Cognitive Level: Apply (application) REF: 39 TOP: Nursing Process: Assessment MSC: NCLEX: Health Promotion and Maintenance 6. The nurse who is assessing an older adult with rectal bleeding asks, “Have you ever had a colonoscopy?” The nurse is performing what type of assessment? a. Focused assessment c. Detailed health assessment b. Emergency assessment d. Comprehensive assessment ANS: AA focused assessment is an abbreviated assessment used to evaluate the status of previously identified problems and monitor for signs of new problems. It can be done when a specific problem is identified. An emergency assessment is done when the nurse needs to obtain information about life-threatening problems quickly while simultaneously taking action to maintain vital function. A comprehensive assessment includes a detailed health history and physical examination of one body system or many body systems. It is typically done on admission to the hospital or onset of care in a primary care setting. DIF: Cognitive Level: Understand (comprehension) REF: 40 TOP: Nursing Process: Assessment MSC: NCLEX: Health Promotion and Maintenance 7. The nurse is preparing to perform a focused assessment for a patient complaining of shortness of breath. Which equipment will be needed? a. Flashlight c. Tongue blades b. Stethoscope d. Percussion hammer ANS: B A stethoscope is used to auscultate breath sounds. The other equipment may be used for a comprehensive assessment but will not be needed for a focused respiratory assessment. DIF: Cognitive Level: Understand (comprehension) REF: 40 TOP: Nursing Process: Assessment MSC: NCLEX: Health Promotion and Maintenance 8. The nurse plans to complete a physical examination of an alert, older patient. Which adaptations to the examination technique should the nurse include? a. Avoid the use of touch as much as possible. b. Use slightly more pressure for palpation of the liver. c. Speak softly and slowly when talking with the patient. d. Organize the sequence to minimize the position changes. ANS: D Older patients may have age-related changes in mobility that make it more difficult to change position. There is no need to avoid the use of touch when examining older patients. Less pressure should be used over the liver. Because the patient is alert, there is no indication that there is any age-related difficulty in understanding directions from the nurse. DIF: Cognitive Level: Apply (application) REF: 40 TOP: Nursing Process: Assessment MSC: NCLEX: Health Promotion and Maintenance 9. While the nurse is taking the health history, a patient states, “My mother and sister both had double mastectomies and were unable to be very active for weeks.” Which functional health pattern is represented by this patient’s statement? a. Activity–exercise b. Cognitive–perceptual c. Coping–stress tolerance d. Health perception–health management ANS: D The information in the patient statement relates to risk factors and important information about the family history. Identification of risk factors falls into the health perception–health maintenance pattern.DIF: Cognitive Level: Understand (comprehension) REF: 37 TOP: Nursing Process: Assessment MSC: NCLEX: Health Promotion and Maintenance 10. A patient is seen in the emergency department with severe abdominal pain and hypotension. Which type of assessment should the nurse do at this time? a. Focused assessment c. Emergency assessment b. Subjective assessment d. Comprehensive assessment ANS: C Because the patient is hemodynamically unstable, an emergency assessment is needed. Comprehensive and focused assessments may be needed after the patient is stabilized. Subjective information is needed, but objective data such as vital signs are essential for the unstable patient. DIF: Cognitive Level: Understand (comprehension) REF: 40 TOP: Nursing Process: Assessment MSC: NCLEX: Health Promotion and Maintenance 11. The registered nurse (RN) cares for a patient who was admitted a few hours previously with back pain after falling. Which action can the RN delegate to unlicensed assistive personnel (UAP)? a. Finish documenting the admission assessment. b. Determine the patient’s priority nursing diagnoses. c. Obtain the health history from the patient’s caregiver. d. Take the patient’s temperature, pulse, and blood pressure. ANS: D The RN may delegate vital signs to the UAP. Obtaining the health history, documentation of the admission assessment, and determining nursing diagnoses require the education and scope of practice of the RN. DIF: Cognitive Level: Apply (application) REF: 36 OBJ: Special Questions: Delegation TOP: Nursing Process: Planning MSC: NCLEX: Safe and Effective Care Environment 12. When assessing for formation of a possible blood clot in the lower leg of a patient, which action should the nurse take first? a. Visually inspect the leg. b. Feel for the temperature of the leg. c. Check the patient’s pedal pulses using the fingertips. d. Compress the nail beds to determine capillary refill time. ANS: A Inspection is the first of the major techniques used in the physical examination. Palpation and auscultation are then used later in the examination. DIF: Cognitive Level: Apply (application) REF: 39 OBJ: Special Questions: Prioritization TOP: Nursing Process: Assessment MSC: NCLEX: Health Promotion and Maintenance 13. When assessing a patient’s abdomen during the admission assessment, which action should the nurse take first? a. Feel for any masses. c. Listen for bowel sounds.b. Palpate the abdomen. d. Percuss the liver borders. ANS: C When assessing the abdomen, auscultation is done before palpation or percussion because palpation and percussion can cause changes in bowel sounds and alter the findings. All of the techniques are appropriate, but auscultation should be done first. DIF: Cognitive Level: Understand (comprehension) REF: 39 OBJ: Special Questions: Prioritization TOP: Nursing Process: Assessment MSC: NCLEX: Health Promotion and Maintenance 14. When admitting a patient who has just arrived on the unit with a severe headache, what should the nurse do first? a. Complete only basic demographic data before addressing the patient’s pain. b. Inform the patient that the headache will be treated as soon as the health history is completed. c. Medicate the patient for the headache before doing the health history and examination. d. Take the initial vital signs and then address the headache before completing the health history. ANS: C The patient priority in this situation will be to decrease the pain level because the patient will be unlikely to cooperate in providing demographic data or the health history until the nurse addresses the pain. However, obtaining information about vital signs is essential before using either pharmacologic or nonpharmacologic therapies for pain control. The vital signs may indicate hemodynamic instability that would need to be addressed immediately. DIF: Cognitive Level: Apply (application) REF: 35 OBJ: Special Questions: Prioritization TOP: Nursing Process: Assessment MSC: NCLEX: Physiological Integrity OTHER 1. In what order will the nurse perform these actions when doing a physical assessment for a patient admitted with abdominal pain? (Put a comma and a space between each answer choice [A, B, C, D].) a. Percuss the abdomen to locate any areas of dullness. b. Palpate the abdomen to check for tenderness or masses. c. Inspect the abdomen for distention or other abnormalities. d. Auscultate the abdomen for the presence of bowel sounds. ANS: C, D, A, B When assessing the abdomen, the initial action is to inspect the abdomen. Auscultation is done next because percussion and palpation can alter bowel sounds and produce misleading findings. DIF: Cognitive Level: Understand (comprehension) REF: 39 TOP: Nursing Process: Assessment MSC: NCLEX: Physiological IntegrityChapter 04: Patient and Caregiver Teaching Lewis: Medical-Surgical Nursing, 10th Edition MULTIPLE CHOICE 1. A patient with newly diagnosed colon cancer has a nursing diagnosis of deficient knowledge about colon cancer. The nurse should initially focus on which learning goal for this patient? a. The patient will state ways of preventing the recurrence of the cancer. b. The patient will explore and select an appropriate colon cancer therapy. c. The patient will demonstrate coping skills needed to manage the disease. d. The patient will choose methods to minimize adverse effects of treatment. ANS: B Adults learn best when given information that can be used immediately. The first action the patient will need to take after a cancer diagnosis is to explore and choose a treatment option. The other goals may be appropriate as treatment progresses. DIF: Cognitive Level: Apply (application) REF: 47 TOP: Nursing Process: Planning MSC: NCLEX: Health Promotion and Maintenance 2. After the nurse provides diet instructions for a patient with diabetes, the patient can restate the information but fails to make the recommended diet changes. How would the nurse best evaluate the patient’s situation? a. Learning did not occur because the patient’s behavior did not change. b. Choosing not to follow the diet is the behavior that resulted from learning. c. The nurse’s responsibility for helping the patient make diet changes has been fulfilled. d. The teaching methods were ineffective in helping the patient learn about the necessary diet changes. ANS: B Although the patient behavior has not changed, the patient’s ability to restate the information indicates that learning has occurred, and the patient is choosing at this time not to change the diet. The patient may be in the contemplation or preparation stage in the transtheoretical model. The nurse should reinforce the need for change and continue to provide information and assistance with planning for change. DIF: Cognitive Level: Apply (application) REF: 47 TOP: Nursing Process: Evaluation MSC: NCLEX: Health Promotion and Maintenance 3. A patient is diagnosed with heart failure after being admitted to the hospital for shortness of breath and fatigue. Which teaching strategy, if implemented by the nurse, is most likely to be effective? a. Assure the patient that the nurse is an expert on management of heart failure. b. Teach the patient at each meal about the amounts of sodium in various foods. c. Discuss the importance of medication control in maintenance of long-term health. d. Refer the patient to a home health nurse for instructions on diet and fluid restrictions. ANS: BPrinciples of adult education indicate that readiness and motivation to learn are high when facing new tasks (e.g., learning about the sodium amounts in various food items) and when demonstration and practice of skills are available. Although a home health referral may be needed for this patient, teaching should not be postponed until discharge. Adult learners are independent. The nurse should act as a facilitator for learning, rather than as the expert. Adults learn best when the topic is of immediate usefulness. Long-term goals may not be very motivating. DIF: Cognitive Level: Apply (application) REF: 47 TOP: Nursing Process: Planning MSC: NCLEX: Health Promotion and Maintenance 4. A patient who was admitted to the hospital with hyperglycemia and newly diagnosed diabetes mellitus is scheduled for discharge the second day after admission. When implementing patient teaching, what is the priority action for the nurse? a. Instruct about the increased risk for cardiovascular disease. b. Provide detailed information about dietary control of glucose. c. Teach glucose self-monitoring and medication administration. d. Give information about the effects of exercise on glucose control. ANS: C When time is limited, the nurse should focus on the priorities of teaching. In this situation, the patient should know how to test blood glucose and administer medications to control glucose levels. The patient will need further teaching about the role of diet, exercise, various medications, and the many potential complications of diabetes, but these topics can be addressed through planning for appropriate referrals. DIF: Cognitive Level: Apply (application) REF: 49 TOP: Nursing Process: Implementation MSC: NCLEX: Health Promotion and Maintenance 5. A patient states, “I told my husband I wouldn’t buy as much prepared food snacks, so I will go the grocery store to buy fresh fruit, vegetables, and whole grains.” When using the Transtheoretical Model of Health Behavior Change, the nurse identifies that this patient is in which stage of change? a. Preparation c. Maintenance b. Termination d. Contemplation ANS: A The patient’s statement indicating that the plan for change is being shared with someone else indicates that the preparation stage has been achieved. Contemplation of a change would be indicated by a statement like “I know I should exercise.” Maintenance of a change occurs when the patient practices the behavior regularly. Termination would be indicated when the change is a permanent part of the lifestyle. DIF: Cognitive Level: Understand (comprehension) REF: 48 TOP: Nursing Process: Assessment MSC: NCLEX: Health Promotion and Maintenance 6. While admitting a patient to the medical unit, the nurse determines that the patient has a hearing impairment. How should the nurse use this information to plan teaching and learning strategies? a. Motivation and readiness to learn will be affected. b. The family must be included in the teaching process.c. The patient will have problems understanding information. d. Written materials should be provided with verbal instructions. ANS: D The information that the patient has a hearing impairment indicates that the nurse should use written and verbal materials in teaching along with other strategies. The patient does not indicate a lack of motivation or an inability to understand new information. The patient’s decreased hearing does not necessarily imply that the family must be included in the teaching process. DIF: Cognitive Level: Understand (comprehension) REF: 51 TOP: Nursing Process: Planning MSC: NCLEX: Health Promotion and Maintenance 7. A patient who is morbidly obese states, “I’ve recently made some changes in my life. I’ve decreased my fat intake, and I’ve stopped smoking.” Which statement, if made by the nurse, is the best initial response? a. “Although those are important, it is essential that you make other changes, too.” b. “Are you having any difficulty in maintaining the changes you have already made?” c. “Which additional changes in your lifestyle would you like to implement at this time?” d. “You have already accomplished changes that are important for the health of your heart.” ANS: D Positive reinforcement of the learner’s achievements is critical in making lifestyle changes. This patient is in the action stage of the Transtheoretical Model when reinforcement of the changes being made is an important nursing intervention. The other responses are also appropriate but are not the best initial response. DIF: Cognitive Level: Apply (application) REF: 53 TOP: Nursing Process: Implementation MSC: NCLEX: Health Promotion and Maintenance 8. The nurse is planning a teaching session with a patient newly diagnosed with migraine headaches. To assess a patient’s readiness to learn, which question should the nurse ask first? a. “What kind of work and leisure activities do you do?” b. “What information do you think you need right now?” c. “Can you describe the types of activities that help you learn new information?” d. “Do you have any religious beliefs that are inconsistent with the planned treatment?” ANS: B Motivation and readiness to learn depend on what the patient values and perceives as important. The other questions are also important in developing the teaching plan, but do not address what information most interests the patient at present. DIF: Cognitive Level: Apply (application) REF: 53 TOP: Nursing Process: Assessment MSC: NCLEX: Health Promotion and Maintenance 9. The nurse considers a nursing diagnosis of ineffective health maintenance related to low motivation for a patient with diabetes. Which finding would the nurse most likely use to support this nursing diagnosis?a. The patient does not perform capillary blood glucose tests as directed. b. The patient occasionally forgets to take the daily prescribed medication. c. The patient states that dietary changes have not made any difference at all. d. The patient cannot identify signs or symptoms of high and low blood glucose. ANS: C The patient’s motivation to follow a diabetic diet will be decreased if the patient believes that dietary changes do not affect symptoms. The other responses do not indicate that the ineffective health maintenance is caused by lack of motivation. DIF: Cognitive Level: Apply (application) REF: 48 TOP: Nursing Process: Diagnosis MSC: NCLEX: Health Promotion and Maintenance 10. A patient with diabetic neuropathy requires teaching about foot care. Which learning goal should the nurse include in the teaching plan? a. The nurse will demonstrate the proper technique for trimming toenails. b. The patient will list three ways to protect the feet from injury by discharge. c. The nurse will instruct the patient on appropriate foot care before discharge. d. The patient will understand the rationale for proper foot care after instruction. ANS: B Learning goals should state clear, measurable outcomes of the learning process. Demonstrating technique for trimming toenails and providing instructions on foot care are actions that the nurse will take rather than behaviors that indicate that patient learning has occurred. A learning goal that states that the patient will understand the rationale for proper foot care is too vague and nonspecific to measure whether learning has occurred. DIF: Cognitive Level: Apply (application) REF: 54 TOP: Nursing Process: Planning MSC: NCLEX: Health Promotion and Maintenance 11. A patient needs to learn how to instill eye drops. Which teaching strategy, if implemented by the nurse, would be most effective? a. Peer teaching b. Lecture-discussion c. Printed instructions d. Demonstration and return demonstration ANS: D Demonstration with return demonstration (show back) is best used to teach a patient how to learn to perform a skill. Lecture-discussion, peer teaching, and printed materials are more useful for other learning needs. DIF: Cognitive Level: Understand (comprehension) REF: 56 TOP: Nursing Process: Planning MSC: NCLEX: Health Promotion and Maintenance 12. The nurse and the patient who is diagnosed with hypertension develop this goal: “The patient will select a 2-gram sodium diet from the hospital menu for the next 3 days.” Which evaluation method will be best for the nurse to use when determining whether teaching was effective? a. Have the patient list substitutes for favorite foods that are high in sodium. b. Check the sodium content of the patient’s menu choices over the next 3 days.c. Ask the patient to identify which foods on the hospital menus are high in sodium. d. Compare the patient’s sodium intake before and after the teaching was implemented. ANS: B All of the answers address the patient’s sodium intake, but the desired patient behaviors in the learning objective are most clearly addressed by evaluating the sodium content of the patient’s menu choices. DIF: Cognitive Level: Apply (application) REF: 57 TOP: Nursing Process: Evaluation MSC: NCLEX: Health Promotion and Maintenance 13. The nurse prepares written handouts to be used as part of the standardized teaching plan for patients who have been recently diagnosed with diabetes. What statement would be most appropriate to include in the handouts? a. Eating the right foods can help in keeping blood glucose at a near-normal level. b. Polyphagia, polydipsia, and polyuria are common symptoms of diabetes mellitus. c. Some patients with diabetes control blood glucose with oral medications, injections, or dietary interventions. d. Diabetes mellitus is characterized by chronic hyperglycemia and the associated symptoms than can lead to long-term complications. ANS: A The reading level for patient teaching materials should be at the fifth grade level. The other responses have words with three or more syllables, use many medical terms, or are too long. DIF: Cognitive Level: Apply (application) REF: 52 TOP: Nursing Process: Planning MSC: NCLEX: Health Promotion and Maintenance 14. The hospital nurse implements a teaching plan to assist an older patient who lives alone to independently accomplish daily activities. How would the nurse best evaluate the patient’s long-term response to the teaching? a. Make a referral to the home health nursing agency for home visits. b. Have the patient demonstrate the learned skills at the end of the teaching session. c. Arrange a physical therapy visit before the patient is discharged from the hospital. d. Check the patient’s ability to bathe and get dressed without any assistance the next day. ANS: A A home health referral would allow for the assessment of the patient’s long-term response after discharge. The other actions allow evaluation of the patient’s short-term response to teaching. DIF: Cognitive Level: Apply (application) REF: 57 TOP: Nursing Process: Evaluation MSC: NCLEX: Health Promotion and Maintenance 15. A patient who smokes a pack of cigarettes per day tells the nurse, “I enjoy smoking and have no plans to quit.” Which nursing diagnosis is most appropriate? a. Health-seeking behaviors related to cigarette use b. Ineffective health maintenance related to tobacco use c. Readiness for enhanced self-health management related to smoking d. Deficient knowledge related to long-term effects of cigarette smokingANS: B The patient’s statement indicates that he or she is not considering smoking cessation. Ineffective health maintenance is defined as the inability to identify, manage, or seek out help to maintain health. DIF: Cognitive Level: Apply (application) REF: 47 TOP: Nursing Process: Diagnosis MSC: NCLEX: Health Promotion and Maintenance 16. An older Asian patient, who is seen at the health clinic, is diagnosed with protein malnutrition. What priority action should the nurse include in the teaching plan? a. Suggest the use of liquid supplements as a way to increase protein intake. b. Encourage the patient to increase the dietary intake of meat, cheese, and milk. c. Ask the patient to record the intake of all foods and beverages for a 3-day period. d. Focus on the use of combinations of beans and rice to improve daily protein intake. ANS: C Assessment is the first step in assisting a patient with health changes. The other answers may be appropriate for the patient, but the nurse will not be able to determine this until the assessment of the patient is complete. DIF: Cognitive Level: Apply (application) REF: 49 OBJ: Special Questions: Prioritization TOP: Nursing Process: Planning MSC: NCLEX: Health Promotion and Maintenance 17. A middle-aged patient who has diabetes tells the nurse, “I want to know how to give my own insulin so I don’t have to bother my wife all the time.” What is the priority action of the nurse? a. Demonstrate how to draw up and administer insulin. b. Discuss the use of exercise to decrease insulin needs. c. Teach about differences between the various types of insulin. d. Provide handouts about therapeutic and adverse effects of insulin. ANS: A Adult education is most effective when focused on information that the patient thinks is needed right now. All of the indicated information will need to be included when planning teaching for this patient, but the teaching will be most effective if the nurse starts with the patient’s stated priority topic. DIF: Cognitive Level: Apply (application) REF: 47 OBJ: Special Questions: Prioritization TOP: Nursing Process: Implementation MSC: NCLEX: Health Promotion and Maintenance 18. The nurse plans to teach a patient and the caregiver how to manage high blood pressure (BP). Which action should the nurse take first? a. Give written information about hypertension to the patient and caregiver. b. Have the dietitian meet with the patient and caregiver to discuss a low-sodium diet. c. Teach the caregiver how to take the patient’s BP using a manual blood pressure cuff. d. Ask the patient and caregiver to select information from a list of high BP teaching topics.ANS: D Because adults learn best when given information that they view as being needed immediately, asking the caregiver and patient to prioritize learning needs is likely to be the most successful approach to home management of health problems. The other actions may also be appropriate, depending on what learning needs the caregiver and patient have, but the initial action should be to assess what the learners feel is important. DIF: Cognitive Level: Apply (application) REF: 47 OBJ: Special Questions: Prioritization TOP: Nursing Process: Assessment MSC: NCLEX: Health Promotion and Maintenance 19. A postoperative patient and caregiver need discharge teaching. Which actions included in the teaching plan can the nurse delegate to unlicensed assistive personnel (UAP)? a. Evaluate whether the patient and caregiver understand the teaching. b. Show the caregiver how to accurately check the patient’s temperature. c. Schedule the discharge teaching session with the patient and caregiver. d. Give the patient a pamphlet reinforcing teaching already done by the nurse. ANS: D Providing a pamphlet to a patient to reinforce previously taught material does not require nursing judgment and can safely be delegated to UAP. Demonstration of how to take a temperature accurately, determining the best time for teaching, and evaluation of the success of patient teaching all require judgment and critical thinking and should be done by the registered nurse. DIF: Cognitive Level: Apply (application) REF: 46 OBJ: Special Questions: Delegation TOP: Nursing Process: Planning MSC: NCLEX: Safe and Effective Care Environment 20. A family caregiver tells the home health nurse, “I feel like I can never get away to do anything for myself.” Which action is best for the nurse to take? a. Assist the caregiver in finding respite services. b. Assure the caregiver that the work is appreciated. c. Encourage the caregiver to discuss feelings openly with the nurse. d. Tell the caregiver that family members provide excellent patient care. ANS: A Respite services allow family caregivers to have time away from their caregiving responsibilities. The other actions may also be helpful, but the caregiver’s statement clearly indicates the need for some time away. DIF: Cognitive Level: Apply (application) REF: 49 TOP: Nursing Process: Implementation MSC: NCLEX: Psychosocial Integrity MULTIPLE RESPONSE 1. The nurse plans to provide instructions about diabetes to a patient who has a low literacy level. Which teaching strategies should the nurse use (select all that apply)? a. Discourage use of the Internet as a source of health information. b. Avoid asking the patient about reading abilities and level of education. c. Provide illustrations and photographs showing various types of insulin.d. Schedule one-to-one teaching sessions to practice insulin administration. e. Obtain CDs and DVDs that illustrate how to perform blood glucose testing. ANS: C, D, E For patients with low literacy, visual and hands-on learning techniques are most appropriate. The nurse will need to obtain as much information as possible about the patient’s reading level in order to provide appropriate learning materials. The nurse should guide the patient to Internet sites established by reputable heath care organizations such as the American Diabetes Association. DIF: Cognitive Level: Apply (application) REF: 52 TOP: Nursing Process: Implementation MSC: NCLEX: Health Promotion and MaintenanceChapter 05: Chronic Illness and Older Adults Lewis: Medical-Surgical Nursing, 10th Edition MULTIPLE CHOICE 1. When caring for an older patient with hypertension who has been hospitalized after a transient ischemic (TIA), which topic is the most important for the nurse to include in the discharge teaching? a. Effect of atherosclerosis on blood vessels b. Mechanism of action of anticoagulant drug therapy c. Symptoms indicating that the patient should contact the health care provider d. Impact of the patient’s family history on likelihood of developing a serious stroke ANS: C One of the tasks for patients with chronic illnesses is to prevent and manage a crisis. The patient needs instruction on recognition of symptoms of hypertension and TIA and appropriate actions to take if these symptoms occur. The other information may also be included in patient teaching but is not as essential in the patient’s self-management of the illness. DIF: Cognitive Level: Analyze (analysis) REF: 60 OBJ: Special Questions: Prioritization TOP: Nursing Process: Implementation MSC: NCLEX: Physiological Integrity 2. The nurse performs a comprehensive assessment of an older patient who is considering admission to an assisted living facility. Which question is the most important for the nurse to ask? a. “Have you had any recent infections?” b. “How frequently do you see a doctor?” c. “Do you have a history of heart disease?” d. “Are you able to prepare your own meals?” ANS: D The patient’s functional abilities, rather than the presence of an acute or chronic illness, are more useful in determining how well the patient might adapt to an assisted living situation. The other questions will also provide helpful information but are not as useful in providing a basis for determining patient needs or for developing interventions for the older patient. DIF: Cognitive Level: Analyze (analysis) REF: 62 OBJ: Special Questions: Prioritization TOP: Nursing Process: Assessment MSC: NCLEX: Health Promotion and Maintenance 3. An alert older patient who takes multiple medications for chronic cardiac and pulmonary diseases lives with a daughter who works during the day. During a clinic visit, the patient verbalizes to the nurse that she has a strained relationship with her daughter and does not enjoy being alone all day. Which nursing diagnosis should the nurse assign as the priority for this patient? a. Social isolation related to fatigue b. Risk for injury related to drug interactions c. Caregiver role strain related to family employment scheduled. Compromised family coping related to the patient’s care needs ANS: B The patient’s age and multiple medications indicate a risk for injury caused by interactions between the multiple drugs being taken and a decreased drug metabolism rate. Problems with social isolation, caregiver role strain, or compromised family coping are not physiologic priorities. Drug–drug interactions could cause the most harm to the patient and are therefore the priority. DIF: Cognitive Level: Analyze (analysis) REF: 73 OBJ: Special Questions: Prioritization TOP: Nursing Process: Diagnosis MSC: NCLEX: Health Promotion and Maintenance 4. Which method should the nurse use to gather the most complete assessment of an older patient? a. Review the patient’s health record for previous assessments. b. Use a geriatric assessment instrument to evaluate the patient. c. Ask the patient to write down medical problems and medications. d. Interview both the patient and the primary caregiver for the patient. ANS: B The most complete information about the patient will be obtained through the use of an assessment instrument specific to the geriatric population, which includes information about both medical diagnoses and treatments and about functional health patterns and abilities. A review of the medical record, interviews with the patient and caregiver, and written information by the patient are all included in a comprehensive geriatric assessment. DIF: Cognitive Level: Analyze (analysis) REF: 74 OBJ: Special Questions: Prioritization TOP: Nursing Process: Assessment MSC: NCLEX: Health Promotion and Maintenance 5. Which intervention should the nurse implement to provide optimal care for an older patient who is hospitalized with pneumonia? a. Plan for transfer to a long-term care facility. b. Minimize activity level during hospitalization. c. Consider the preadmission functional abilities. d. Use an approved standardized geriatric nursing care plan. ANS: C The plan of care for older adults should be individualized and based on the patient’s current functional abilities. A standardized geriatric nursing care plan will not address individual patient needs and strengths. A patient’s need for discharge to a long-term care facility is variable. Activity level should be designed to allow the patient to retain functional abilities while hospitalized and also to allow any additional rest needed for recovery from the acute process. DIF: Cognitive Level: Apply (application) REF: 69 TOP: Nursing Process: Planning MSC: NCLEX: Physiological Integrity 6. The nurse cares for an older adult patient who lives in a rural area. Which intervention should the nurse plan to implement to meet this patient’s needs? a. Suggest that the patient move closer to health care providers.b. Obtain extra medications for the patient to last for 4 to 6 months. c. Ensure transportation to appointments with the health care provider. d. Assess the patient for chronic diseases that are unique to rural areas. ANS: C Transportation can be a barrier to accessing health services in rural areas. The patient living in a rural area may lose the benefits of a familiar situation and social support by moving to an urban area. There are no chronic diseases unique to rural areas. Because medications may change, the nurse should help the patient plan for obtaining medications through alternate means such as the mail or delivery services, not by purchasing large quantities of the medications. DIF: Cognitive Level: Apply (application) REF: 64 TOP: Nursing Process: Planning MSC: NCLEX: Health Promotion and Maintenance 7. Which nursing action will be most helpful in decreasing the risk for drug-drug interactions in an older adult? a. Teach the patient to have all prescriptions filled at the same pharmacy. b. Make a schedule for the patient as a reminder of when to take each medication. c. Instruct the patient to avoid taking over-the-counter (OTC) medications or supplements. d. Ask the patient to bring all medications, supplements, and herbs to each appointment. ANS: D The most information about drug use and possible interactions is obtained when the patient brings all prescribed medications, OTC medications, and supplements to every health care appointment. The patient should discuss the use of any OTC medications with the health care provider and obtain all prescribed medications from the same pharmacy, but use of supplements and herbal medications also need to be considered in order to prevent drug–drug interactions. Use of a medication schedule will help the patient take medications as scheduled, but will not prevent drug–drug interactions. DIF: Cognitive Level: Analyze (analysis) REF: 65 OBJ: Special Questions: Prioritization TOP: Nursing Process: Implementation MSC: NCLEX: Physiological Integrity 8. A patient who has just moved to a long-term care facility has a nursing diagnosis of relocation stress syndrome. Which action should the nurse include in the plan of care? a. Remind the patient that making changes is usually stressful. b. Discuss the reason for the move to the facility with the patient. c. Restrict family visits until the patient is accustomed to the facility. d. Have staff members write notes welcoming the patient to the facility. ANS: D Having staff members write notes will make the patient feel more welcome and comfortable at the long-term care facility. Discussing the reason for the move and reminding the patient that change is usually stressful will not decrease the patient’s stress about the move. Family member visits will decrease the patient’s sense of stress about the relocation. DIF: Cognitive Level: Apply (application) REF: 69 TOP: Nursing Process: Planning MSC: NCLEX: Psychosocial Integrity9. An older patient complains of having “no energy” and feeling increasingly weak. The patient has had a 12-lb weight loss over the past year. Which action should the nurse take initially? a. Ask the patient about daily dietary intake. b. Schedule regular range-of-motion exercise. c. Discuss long-term care placement with the patient. d. Describe normal changes associated with aging to the patient. ANS: A In a frail older patient, nutrition is frequently compromised, and the nurse’s initial action should be to assess the patient’s nutritional status. Active range of motion may be helpful in improving the patient’s strength and endurance, but nutritional assessment is the priority because the patient has had a significant weight loss. The patient may be a candidate for long-term care placement, but more assessment is needed before this can be determined. The patient’s assessment data are not consistent with normal changes associated with aging. DIF: Cognitive Level: Analyze (analysis) REF: 65 OBJ: Special Questions: Prioritization TOP: Nursing Process: Assessment MSC: NCLEX: Health Promotion and Maintenance 10. The nurse is admitting an acutely ill, older patient to the hospital. Which action should the nurse take? a. Speak slowly and loudly while facing the patient. b. Obtain a detailed medical history from the patient. c. Perform the physical assessment before interviewing the patient. d. Ask a family member to go home and retrieve the patient’s cane. ANS: C When a patient is acutely ill, the physical assessment should be accomplished first to detect any physiologic changes that require immediate action. Not all older patients have hearing deficits, and it is insensitive of the nurse to speak loudly and slowly to all older patients. To avoid tiring the patient, much of the medical history can be obtained from medical records. After the initial physical assessment to determine the patient’s current condition, then the nurse could ask someone to obtain any assistive devices for the patient if applicable. DIF: Cognitive Level: Apply (application) REF: 70 TOP: Nursing Process: Planning MSC: NCLEX: Health Promotion and Maintenance 11. The nurse cares for an alert, homeless older adult patient who was admitted to the hospital with a chronic foot infection. Which intervention is the most appropriate for the nurse to include in the discharge plan for this patient? a. Teach the patient how to assess and care for the foot infection. b. Refer the patient to social services for assessment of resources. c. Schedule the patient to return to outpatient services for foot care. d. Give the patient written information about shelters and meal sites. ANS: BAn interprofessional approach, including social services, is needed when caring for homeless older adults. Even with appropriate teaching, a homeless individual may not be able to maintain adequate foot care because of a lack of supplies or a suitable place to accomplish care. Older homeless individuals are less likely to use shelters or meal sites. A homeless person may fail to keep appointments for outpatient services because of factors such as fear of institutionalization or lack of transportation. DIF: Cognitive Level: Analyze (analysis) REF: 65 TOP: Nursing Process: Implementation MSC: NCLEX: Safe and Effective Care Environment 12. The home health nurse cares for an older adult patient who lives alone and takes several different prescribed medications for chronic health problems. Which intervention, if implemented by the nurse, would best encourage medication compliance? a. Use a marked pillbox to set up the patient’s medications. b. Discuss the option of moving to an assisted living facility. c. Remind the patient about the importance of taking medications. d. Visit the patient daily to administer the prescribed medications. ANS: A Because forgetting to take medications is a common cause of medication errors in older adults, the use of medication reminder devices is helpful when older adults have multiple medications to take. There is no indication that the patient needs to move to assisted living or that the patient does not understand the importance of medication compliance. Home health care is not designed for the patient who needs ongoing assistance with activities of daily living or instrumental ADLs. DIF: Cognitive Level: Apply (application) REF: 73 TOP: Nursing Process: Implementation MSC: NCLEX: Physiological Integrity 13. The home health nurse visits an older patient with mild forgetfulness. Which new information is of most concern to the nurse? a. The patient tells the nurse that a close friend recently died. b. The patient has lost 10 lb (4.5 kg) during the past month. c. The patient is cared for by a daughter during the day and stays with a son at night. d. The patient’s son uses a marked pillbox to set up the patient’s medications weekly. ANS: B A 10-pound weight loss may be an indication of elder neglect or depression and requires further assessment by the nurse. The use of a marked pillbox and planning by the family for 24-hour care are appropriate for this patient. It is not unusual that an 86-yr-old would have friends who have died. DIF: Cognitive Level: Apply (application) REF: 74 TOP: Nursing Process: Assessment MSC: NCLEX: Physiological Integrity 14. Which statement, if made by an older adult patient, would be of most concern to the nurse? a. “I prefer to manage my life without much help from other people.” b. “I take three different medications for my heart and joint problems.” c. “I don’t go on daily walks anymore since I had pneumonia 3 months ago.” d. “I set up my medications in a marked pillbox so I don’t forget to take them.” ANS: CInactivity and immobility lead rapidly to loss of function in older adults. The nurse should develop a plan to prevent further deconditioning and restore function for the patient. Self-management is appropriate for independently living older adults. On average, an older adult takes seven different medications so the use of three medications is not unusual for this patient. The use of memory devices to assist with safe medication administration is recommended for older adults. DIF: Cognitive Level: Apply (application) REF: 71 TOP: Nursing Process: Assessment MSC: NCLEX: Health Promotion and Maintenance 15. The nurse assesses an older patient who takes diuretics and has a possible urinary tract infection (UTI). Which action should the nurse take first? a. Palpate over the suprapubic area. b. Inspect for abdominal distention. c. Question the patient about hematuria. d. Request the patient empty the bladder. ANS: D Before beginning the assessment of an older patient with a UTI and on diuretics, the nurse should have the patient empty the bladder because bladder fullness or discomfort will distract from the patient’s ability to provide accurate information. The patient may seem disoriented if distracted by pain or urgency. The physical assessment data are obtained after the patient is as comfortable as possible. DIF: Cognitive Level: Analyze (analysis) REF: 69 OBJ: Special Questions: Prioritization TOP: Nursing Process: Assessment MSC: NCLEX: Physiological Integrity 16. Which patient is most likely to need long-term nursing care management? a. 72-yr-old who had a hip replacement after a fall at home b. 64-yr-old who developed sepsis after a ruptured peptic ulcer c. 76-yr-old who had a cholecystectomy and bile duct drainage d. 63-yr-old with bilateral knee osteoarthritis who weighs 350 lb (159 kg) ANS: D Osteoarthritis and obesity are chronic problems that will require planning for long-term interventions such as physical therapy and nutrition counseling. The other patients have acute problems that are not likely to require long-term management. DIF: Cognitive Level: Analyze (analysis) REF: 64 OBJ: Special Questions: Multiple Patients TOP: Nursing Process: Planning MSC: NCLEX: Safe and Effective Care Environment 17. An older adult being admitted is assessed at high risk for falls. Which action should the nurse take first? a. Use a bed alarm system on the patient’s bed. b. Administer the prescribed PRN sedative medication. c. Ask the health care provider to order a vest restraint. d. Place the patient in a “geri-chair” near the nurse’s station. ANS: AThe use of the least restrictive restraint alternative is required. Physical or chemical restraints may be necessary, but the nurse’s first action should be an alternative such as a bed alarm. DIF: Cognitive Level: Analyze (analysis) REF: 74 OBJ: Special Questions: Prioritization TOP: Nursing Process: Implementation MSC: NCLEX: Safe and Effective Care Environment 18. An older adult patient presents with a broken arm and visible scattered bruises healing at different stages. Which action should the nurse take first? a. Notify an elder protective services agency about possible abuse. b. Make a referral for a home assessment visit by the home health nurse. c. Have the family member stay in the waiting area while the patient is assessed. d. Ask the patient how the injury occurred and observe the family member’s reaction. ANS: C The initial action should be assessment and interviewing of the patient. The patient should be interviewed alone because the patient will be unlikely to give accurate information if the abuser is present. If abuse is occurring, the patient should not be discharged home for a later assessment by a home health nurse. The nurse needs to collect and document data before notifying the elder protective services agency. DIF: Cognitive Level: Analyze (analysis) REF: 69 OBJ: Special Questions: Prioritization TOP: Nursing Process: Assessment MSC: NCLEX: Safe and Effective Care Environment 19. The family of an older patient with chronic health problems and increasing weakness is considering placement in a long-term care (LTC) facility. Which action by the nurse will be most helpful in assisting the patient to make this transition? a. Have the family select a LTC facility that is relatively new. b. Ask the patient’s preference for the choice of a LTC facility. c. Explain the reasons for the need to live in LTC to the patient. d. Request that the patient be placed in a private room at the facility. ANS: B The stress of relocation is likely to be less when the patient has input into the choice of the facility. The age of the long-term care facility does not indicate a better fit for the patient or better quality of care. Although some patients may prefer a private room, others may adjust better when given a well-suited roommate. The patient should understand the reasons for the move but will make the best adjustment when involved with the choice to move and the choice of the facility. DIF: Cognitive Level: Analyze (analysis) REF: 69 TOP: Nursing Process: Implementation MSC: NCLEX: Psychosocial Integrity 20. The nurse manages the care of older adults in an adult health day care center. Which action can the nurse delegate to unlicensed assistive personnel (UAP)? a. Obtain information about food and medication allergies from patients. b. Take blood pressures daily and document in individual patient records. c. Choose social activities based on the individual patient needs and desires. d. Teach family members how to cope with patients who are cognitively impaired. ANS: BMeasurement and documentation of vital signs are included in UAP education and scope of practice. Obtaining patient health history, planning activities based on the patient assessment, and patient education are all actions that require critical thinking and will be done by the registered nurse. DIF: Cognitive Level: Apply (application) REF: 75 OBJ: Special Questions: Delegation TOP: Nursing Process: Planning MSC: NCLEX: Safe and Effective Care Environment MULTIPLE RESPONSE 1. Which nursing actions will the nurse take to assess for possible malnutrition in an older adult patient (select all that apply)? a. Assess for depression. b. Review laboratory results. c. Determine food preferences. d. Inspect teeth and oral mucosa. e. Ask about transportation needs. ANS: A, B, D, E The laboratory results, especially albumin and cholesterol levels, may indicate chronic poor protein intake or high-fat or high-cholesterol intake. Transportation affects the patient’s ability to shop for groceries. Depression may lead to decreased appetite. Oral sores or teeth in poor condition may decrease the ability to chew and swallow. Food likes and dislikes are not necessarily associated with malnutrition. DIF: Cognitive Level: Apply (application) REF: 65 TOP: Nursing Process: Assessment MSC: NCLEX: Health Promotion and MaintenanceChapter 06: Stress and Stress Management Lewis: Medical-Surgical Nursing, 10th Edition MULTIPLE CHOICE 1. An adult patient who arrived at the triage desk in the emergency department (ED) with minor facial lacerations after a motor vehicle accident has a blood pressure (BP) of 182/94. Which action by the nurse is appropriate? a. Start an IV line to administer antihypertensive medications. b. Recheck the blood pressure after the patient has been assessed. c. Discuss the need for hospital admission to control blood pressure. d. Teach the patient about the stroke risk associated with uncontrolled hypertension. ANS: B When a patient experiences an acute stressor, the BP increases. The nurse should plan to recheck the BP after the patient has stabilized and received treatment. This will provide a more accurate indication of the patient’s usual blood pressure. Elevated BP that occurs in response to acute stress does not increase the risk for health problems such as stroke, indicate a need for hospitalization, or indicate a need for IV antihypertensive medications. DIF: Cognitive Level: Apply (application) REF: 80 TOP: Nursing Process: Planning MSC: NCLEX: Physiological Integrity 2. A female patient who initially came to the clinic with incontinence was recently diagnosed with endometrial cancer. She is usually well organized and calm, but the nurse who is giving her preoperative instructions observes that the patient is irritable, has difficulty concentrating, and yells at her husband. Which action should the nurse take? a. Ask the health care provider for a psychiatric referral. b. Focus teaching on preventing postoperative complications. c. Try to calm the patient before repeating any information about the surgery. d. Encourage the patient to combine the hysterectomy with surgery for bladder repair. ANS: C Because behavioral responses to stress include temporary changes such as irritability, changes in memory, and poor concentration, patient teaching will need to be repeated. It is also important to try to calm the patient by listening to her concerns and fears. Psychiatric referral will not necessarily be needed for her but that can better be evaluated after surgery. Focusing on postoperative care does not address the need for preoperative instruction such as the procedure, NPO instructions before surgery, date and time of surgery, medications to be taken or discontinued before surgery, and so on. The issue of incontinence is not immediately relevant in the discussion of preoperative teaching for her hysterectomy. DIF: Cognitive Level: Apply (application) REF: 81 TOP: Nursing Process: Implementation MSC: NCLEX: Psychosocial Integrity 3. An adult patient who is hospitalized after a motorcycle crash tells the nurse, “I didn’t sleep last night because I worried about missing work at my new job and losing my insurance coverage.” Which nursing diagnosis is appropriate to include in the plan of care? a. Anxiety c. Ineffective denial b. Defensive coping d. Risk prone health behaviorANS: A The information about the patient indicates that anxiety is an appropriate nursing diagnosis. The patient data do not support defensive coping, ineffective denial, or risk prone health behavior as problems for this patient. DIF: Cognitive Level: Apply (application) REF: 78 TOP: Nursing Process: Diagnosis MSC: NCLEX: Psychosocial Integrity 4. A patient is extremely anxious about having a biopsy on a femoral lymph node. Which relaxation technique would be the best choice for the nurse to facilitate during the procedure? a. Yoga stretching c. Relaxation breathing b. Guided imagery d. Mindfulness meditation ANS: C Relaxation breathing is an easy relaxation technique to teach and use. The patient should remain still during the biopsy and not move or stretch any of his extremities. Meditation and guided imagery require more time to practice and learn. DIF: Cognitive Level: Apply (application) REF: 83 TOP: Nursing Process: Implementation MSC: NCLEX: Psychosocial Integrity 5. A patient who has frequent migraines tells the nurse, “My life feels chaotic and out of my control. I could not manage if anything else happens.” Which response should the nurse make initially? a. “Regular exercise may get your mind off the pain.” b. “Guided imagery can be helpful in regaining control.” c. “Tell me more about how your life has been recently.” d. “Your previous coping resources can be helpful to you now.” ANS: C The nurse’s initial strategy should be further assessment of the stressors in the patient’s life. Exercise, guided imagery, or understanding how to use coping strategies that worked in the past may be of assistance to the patient, but more assessment is needed before the nurse can determine this. DIF: Cognitive Level: Apply (application) REF: 86 OBJ: Special Questions: Prioritization TOP: Nursing Process: Implementation MSC: NCLEX: Psychosocial Integrity 6. A nurse prepares an adult patient with a severe burn injury for a dressing change. The nurse knows that this is a painful procedure and wants to try providing music to help the patient relax. Which action is best for the nurse to take? a. Use music composed by Mozart. b. Play music that does not have words. c. Ask the patient about music preferences. d. Select music that has 60 to 80 beats/minute. ANS: C Although music with 60 to 80 beats/min, music without words, and music composed by Mozart are frequently recommended to reduce stress, each patient responds individually to music and personal preferences are important.DIF: Cognitive Level: Analyze (analysis) REF: 85 TOP: Nursing Process: Implementation MSC: NCLEX: Psychosocial Integrity 7. The nurse teaches a patient who is experiencing stress at work how to use imagery as a relaxation technique. Which statement by the nurse would be appropriate? a. “Think of a place where you feel peaceful and comfortable.” b. “Place the stress in your life into an image that you can destroy.” c. “Repeatedly visualize yourself experiencing the distress in your workplace.” d. “Bring what you hear and sense in your work environment into your image.” ANS: A Imagery is the use of one’s mind to generate images that have a calming effect on the body. When using imagery for relaxation, the patient should visualize a comfortable and peaceful place. The goal is to offer a relaxing retreat from the actual work environment. Imagery that is not intended for relaxation purposes can target a disease, problem, or stressor. DIF: Cognitive Level: Apply (application) REF: 84 TOP: Nursing Process: Implementation MSC: NCLEX: Psychosocial Integrity 8. An obese female patient who had enjoyed active outdoor activities is stressed because osteoarthritis in her hips now limits her activity. Which action by the nurse will best assist the patient to cope with this situation? a. Have the patient practice frequent relaxation breathing. b. Ask the patient what outdoor activities she misses the most. c. Teach the patient to use imagery for reducing pain and stress. d. Encourage the patient to consider weight loss to improve symptoms. ANS: D For problems that can be changed or controlled, problem-focused coping strategies, such as encouraging the patient to lose weight, are most helpful. The other strategies also may assist the patient in coping with her problem, but they will not be as helpful as a problem-focused strategy. DIF: Cognitive Level: Analyze (analysis) REF: 86 TOP: Nursing Process: Implementation MSC: NCLEX: Psychosocial Integrity 9. A hospitalized patient with diabetes tells the nurse, “I don’t understand why I can keep my blood sugar under control at home with diet alone, but when I get sick, my blood sugar goes up. This is so frustrating.” Which response by the nurse is accurate? a. “The liver is not able to metabolize glucose as well during stressful times.” b. “Your diet at the hospital is the most likely cause of the increased glucose.” c. “The stress of illness causes release of hormones that increase blood glucose.” d. “It is probably coincidental that your blood glucose is higher when you are ill.” ANS: C The release of cortisol, epinephrine, and norepinephrine increase blood glucose levels. The increase in blood glucose is not coincidental. The liver does not control blood glucose. A patient with diabetes who is hospitalized will be on an appropriate diet to help control blood glucose. DIF: Cognitive Level: Apply (application) REF: 79TOP: Nursing Process: Implementation MSC: NCLEX: Physiological Integrity 10. A middle-aged male patient with usually well-controlled hypertension and diabetes visits the clinic. Today he has a blood pressure of 174/94 mm Hg and a blood glucose level of 190 mg/dL. What patient information may indicate that additional intervention by the nurse is needed? a. The patient states that he takes his prescribed antihypertensive medications daily. b. The patient states that both of his parents have high blood pressure and diabetes. c. The patient indicates that he does blood glucose monitoring several times each day. d. The patient reports that he and his wife are disputing custody of their 8-yr-old son. ANS: D The increase in blood pressure and glucose levels possibly suggests that stress caused by his divorce and custody battle may be adversely affecting his health. The nurse should assess this further and develop an appropriate plan to assist the patient in decreasing his stress. Although he has been very compliant with his treatment plan in the past, the nurse should assess whether the stress in his life is interfering with his management of his health problems. The family history will not necessarily explain why he has had changes in his blood pressure and glucose levels. DIF: Cognitive Level: Apply (application) REF: 79 TOP: Nursing Process: Assessment MSC: NCLEX: Physiological Integrity 11. A patient who is taking antiretroviral medication to control human immunodeficiency virus (HIV) infection tells the nurse about feeling mildly depressed and anxious. Which additional information about the patient is most important to communicate to the health care provider? a. The patient takes vitamin supplements and St. John’s wort. b. The patient recently experienced the death of a close friend. c. The patient’s blood pressure has increased to 152/88 mm Hg. d. The patient expresses anxiety about whether the drugs are effective. ANS: A St. John’s wort interferes with metabolism of medications that use the cytochrome P450 enzyme system, including many HIV medications. The health care provider will need to check for toxicity caused by the drug interactions. Teaching is needed about drug interactions. The other information will also be reported but does not have immediate serious implications for the patient’s health. DIF: Cognitive Level: Analyze (analysis) REF: 80 TOP: Nursing Process: Assessment MSC: NCLEX: Safe and Effective Care Environment MULTIPLE RESPONSE 1. A patient who is hospitalized with a pelvic fracture after a motor vehicle accident just received news that the driver of the car died from multiple injuries. What actions should the nurse take based on knowledge of the physiologic stress reactions that may occur in this patient (select all that apply)? a. Assess for bradycardia. b. Observe for decreased appetite.c. Ask about epigastric discomfort. d. Monitor for decreased respiratory rate. e. Check for elevated blood glucose levels. ANS: B, C, E The physiologic changes associated with the acute stress response can cause changes in appetite, increased gastric acid secretion, and increase blood glucose levels. In addition, stress causes an increase in respiratory and heart rates. DIF: Cognitive Level: Analyze (analysis) REF: 78 TOP: Nursing Process: Assessment MSC: NCLEX: Physiological IntegrityChapter 07: Sleep and Sleep Disorders Lewis: Medical-Surgical Nursing, 10th Edition MULTIPLE CHOICE 1. A patient complains of difficulty falling asleep and daytime fatigue for the past 6 weeks. What is the best initial action for the nurse to take in determining whether this patient has chronic insomnia? a. Schedule a polysomnograph (PSG). b. Teach the patient how to use an actigraph. c. Ask the patient to keep a 2-week sleep diary. d. Arrange for the patient to have a sleep study. ANS: C The diagnosis of insomnia is made on the basis of subjective complaints and an evaluation of a 1- to 2-week sleep diary completed by the patient. Actigraphy and PSG studies or sleep studies may be used for determining specific sleep disorders but are not necessary to make an initial insomnia diagnosis. DIF: Cognitive Level: Apply (application) REF: 91 OBJ: Special Questions: Prioritization TOP: Nursing Process: Implementation MSC: NCLEX: Physiological Integrity 2. A patient with chronic insomnia asks the nurse about ways to improve sleep quality. Which response by the nurse is accurate? a. Avoid exercise during the day. b. Keep the bedroom temperature warm. c. Read in bed for a few minutes each night. d. Go to bed at the same time every evening. ANS: D A regular evening schedule is recommended to improve sleep time and quality. Aerobic exercise may improve sleep quality but should occur at least 6 hours before bedtime. Reading in bed is discouraged for patients with insomnia. The bedroom temperature should be slightly cool. DIF: Cognitive Level: Apply (application) REF: 94 TOP: Nursing Process: Implementation MSC: NCLEX: Physiological Integrity 3. Which patient statement indicates a need for further teaching about extended-release zolpidem (Ambien CR)? a. “I should take the medication on an empty stomach.” b. “I will take the medication 1 to 2 hours before bedtime.” c. “I should not take this medication unless I can sleep for at least 6 hours.” d. “I will schedule activities that require mental alertness for later in the day.” ANS: B Benzodiazepine receptor agonists such as zolpidem work quickly and should be taken immediately before bedtime. The other patient statements are correct. DIF: Cognitive Level: Apply (application) REF: 94TOP: Nursing Process: Evaluation MSC: NCLEX: Physiological Integrity 4. The nurse cares for an unstable patient in the intensive care unit (ICU). Which intervention should the nurse include in the plan of care to improve this patient’s sleep quality? a. Ask all visitors to leave the ICU for the night. b. Lower the level of lighting from 8:00 PM until 7:00 AM. c. Avoid the use of opioids for pain relief during the evening. d. Schedule assessments to allow 4 hours of uninterrupted sleep. ANS: B Lowering the level of light will help mimic normal day/night patterns and maximize the opportunity for sleep. Although frequent assessments and opioid use can disturb sleep patterns, these actions are necessary for the care of unstable patients. For some patients, having a family member or friend at the bedside may decrease anxiety and improve sleep. DIF: Cognitive Level: Apply (application) REF: 96 TOP: Nursing Process: Planning MSC: NCLEX: Physiological Integrity 5. What teaching should be included in the plan of care for a patient with narcolepsy? a. Driving an automobile may be possible with appropriate treatment of narcolepsy. b. Changes in sleep hygiene are ineffective in improving sleep quality in narcolepsy. c. Antidepressant drugs are prescribed to treat the depression caused by the disorder. d. Stimulant drugs should be used for less than a month because of the risk for abuse. ANS: A The accident rate FOR patients with narcolepsy who are receiving appropriate treatment is similar to the general population. Stimulant medications are used on an ongoing basis for patients with narcolepsy. The purpose of antidepressant drugs in the treatment of narcolepsy is the management of cataplexy, not to treat depression. Changes in sleep hygiene are recommended for patients with narcolepsy to improve sleep quality. DIF: Cognitive Level: Apply (application) REF: 98 TOP: Nursing Process: Planning MSC: NCLEX: Physiological Integrity 6. Which action should the nurse manager promote as an evidence-based practice to support alertness for night shift nurses? a. Arrange for older staff members to work most night shifts. b. Provide a sleeping area for staff to use for napping at night. c. Post reminders about the relationship of sleep and alertness. d. Schedule nursing staff to rotate day and night shifts monthly. ANS: B Short onsite naps will improve alertness. Rotating shifts causes the most disruption in sleep habits. Reminding staff members about the impact of lack of sleep on alertness will not improve sleep or alertness. It is not feasible to schedule nurses based on their ages. DIF: Cognitive Level: Apply (application) REF: 100 TOP: Nursing Process: Implementation MSC: NCLEX: Safe and Effective Care Environment 7. Which information regarding a patient’s sleep is most important for the nurse to communicate to the health care provider? a. A 21-yr-old student who takes melatonin to assist in sleeping when traveling fromthe United States to Europe b. A 64-yr-old nurse who works the night shift reports drinking hot chocolate before going to bed in the morning c. A 41-yr-old librarian who has a body mass index (BMI) of 42 kg/m2 says that the spouse complains about snoring d. A 32-yr-old accountant who is experiencing a stressful week uses diphenhydramine (Benadryl) for several nights ANS: C The patient’s BMI and snoring suggest possible sleep apnea, which can cause complications such as cardiac dysrhythmias, hypertension, and right-sided heart failure. Melatonin is safe to use as a therapy for jet lag. Short-term use of diphenhydramine in young adults is not a concern. Hot chocolate contains only 5 mg of caffeine and is unlikely to affect this patient’s sleep quality. DIF: Cognitive Level: Analyze (analysis) REF: 96 TOP: Nursing Process: Assessment MSC: NCLEX: Safe and Effective Care Environment 8. What is the first action the nurse should take in addressing a patient’s concerns about insomnia and daytime fatigue? a. Question the patient about the use of over-the-counter sleep aids. b. Suggest that the patient decrease intake of caffeinated beverages. c. Advise the patient to get out of bed if unable to fall asleep in 10 to 20 minutes. d. Recommend that the patient use any prescribed sleep aids for only 2 to 3 weeks. ANS: A The nurse’s first action should be assessment of the patient for factors that may contribute to poor sleep quality or daytime fatigue such as the use of OTC medications. The other actions may be appropriate, but assessment is needed first to choose appropriate interventions to improve the patient’s sleep. DIF: Cognitive Level: Analyze (analysis) REF: 95 OBJ: Special Questions: Prioritization TOP: Nursing Process: Implementation MSC: NCLEX: Physiological Integrity 9. A patient with sleep apnea who uses a continuous positive airway pressure (CPAP) device is preparing to have inpatient surgery. Which instructions should the nurse provide to the patient? a. Schedule a preoperative sleep study. b. Take your home device to the hospital. c. Expect intubation with mechanical ventilation after surgery. d. Avoid requesting pain medication while you are hospitalized. ANS: B The patient should be told to take the CPAP device to the hospital if an overnight stay is expected. Many patients will be able to use their own CPAP equipment. Patients should be treated for pain and monitored for respiratory depression. Another sleep study is not required before surgery. A person with sleep apnea would not routinely be expected to require postoperative intubation and mechanical ventilation. DIF: Cognitive Level: Apply (application) REF: 96 TOP: Nursing Process: Implementation MSC: NCLEX: Physiological Integrity10. When caring for patients with sleep disorders, which activity can the nurse appropriately delegate to unlicensed assistive personnel (UAP)? a. Assist a patient to place the CPAP device on correctly at bedtime. b. Interview a patient about risk factors for obstructive sleep disorders. c. Discuss the benefits of oral appliances in decreasing obstructive sleep apnea. d. Help a patient choose a new continuous positive airway pressure (CPAP) mask. ANS: A Because a CPAP mask is consistently worn in the same way and will have been previously fitted by a licensed health professional, a UAP can assist the patient with putting the mask on. The other actions require critical thinking and nursing judgment by the RN. DIF: Cognitive Level: Apply (application) REF: 100 OBJ: Special Questions: Delegation TOP: Nursing Process: Planning MSC: NCLEX: Physiological Integrity MULTIPLE RESPONSE 1. Which information obtained by the nurse about an older adult who complains of occasional insomnia indicates a need for patient teaching (select all that apply)? a. Drinks a cup of coffee every morning with breakfast b. Eats a snack every evening 1 hour before going to bed c. Reads or watches television in bed on most evenings d. Takes a warm bath just before bedtime every night e. Uses diphenhydramine as an occasional sleep aid ANS: C, E Reading and watching television in bed may contribute to insomnia. Older adults should avoid the use of medications that have anticholinergic effects, such as diphenhydramine. Having a snack 1 hour before bedtime or coffee early in the day should not affect sleep quality. Rituals such as a warm bath before bedtime can enhance sleep quality. DIF: Cognitive Level: Apply (application) REF: 95 TOP: Nursing Process: Assessment MSC: NCLEX: Physiological IntegrityChapter 08: Pain Lewis: Medical-Surgical Nursing, 10th Edition MULTIPLE CHOICE 1. Which question asked by the nurse will give the most information about the patient’s metastatic bone cancer pain? a. “How long have you had this pain?” b. “How would you describe your pain?” c. “How often do you take pain medication?” d. “How much medication do you take for the pain?” ANS: B Because pain is a multidimensional experience, asking a question that addresses the patient’s experience with the pain will elicit more information than the more specific information asked in the other three responses. All of these questions are appropriate, but the response beginning “How would you describe your pain?” is the best initial question. DIF: Cognitive Level: Analysis (analyze) REF: 102 TOP: Nursing Process: Assessment MSC: NCLEX: Physiological Integrity 2. A patient who has had good control for chronic pain using a fentanyl (Duragesic) patch reports rapid onset pain at a level 9 (0 to 10 scale) and requests “something for pain that will work quickly.” How will the nurse document the type of pain reported by this patient? a. Somatic pain c. Neuropathic pain b. Referred pain d. Breakthrough pain ANS: D Pain that occurs beyond the chronic pain already being treated by appropriate analgesics is termed breakthrough pain. Neuropathic pain is caused by damage to peripheral nerves or the central nervous system. Somatic pain is localized and arises from bone, joint, muscle, skin, or connective tissue. Referred pain is pain that is localized in uninjured tissue. DIF: Cognitive Level: Apply (application) REF: 108 TOP: Nursing Process: Implementation MSC: NCLEX: Physiological Integrity 3. The nurse teaches a student nurse about the action of ibuprofen. Which statement, if made by the student, indicates that teaching was effective? a. “The drug decreases pain impulses in the spinal cord.” b. “The drug decreases sensitivity of the brain to painful stimuli.” c. “The drug decreases production of pain-sensitizing chemicals.” d. “The drug decreases the modulating effect of descending nerves.” ANS: C Nonsteroidal antiinflammatory drugs (NSAIDs) provide analgesic effects by decreasing the production of pain-sensitizing chemicals such as prostaglandins at the site of injury. Transmission of impulses through the spinal cord, brain sensitivity to pain, and the descending nerve pathways are not affected by NSAIDs. DIF: Cognitive Level: Understand (comprehension) REF: 104 TOP: Nursing Process: Implementation MSC: NCLEX: Physiological Integrity4. A nurse assesses a patient with chronic cancer pain who is receiving imipramine (Tofranil) in addition to long-acting morphine (MS Contin). Which statement, if made by the patient, indicates to the nurse that the patient is receiving adequate pain control? a. “I’m not anxious during the day.” b. “Every night I get 8 hours of sleep.” c. “I can accomplish activities without much discomfort.” d. “I feel less depressed since I’ve been taking the Tofranil.” ANS: C Imipramine is being used in this patient to manage chronic pain and improve functional ability. Although the medication is also prescribed for patients with depression, insomnia, and anxiety, the evaluation for this patient is based on improved pain control and activity level. DIF: Cognitive Level: Apply (application) REF: 116 TOP: Nursing Process: Evaluation MSC: NCLEX: Physiological Integrity 5. A patient with chronic back pain has learned to control the pain with the use of imagery and hypnosis. The patient’s spouse asks the nurse how these techniques work. Which response by the nurse is accurate? a. “The strategies work by affecting the perception of pain.” b. “These techniques block the pain pathways of the nerves.” c. “These strategies prevent transmission of stimuli from the back to the brain.” d. “The therapies slow the release of chemicals in the spinal cord that cause pain.” ANS: A Cognitive therapies affect the perception of pain by the brain rather than affecting efferent or afferent pathways or influencing the release of chemical transmitters in the dorsal horn. DIF: Cognitive Level: Apply (application) REF: 121 TOP: Nursing Process: Implementation MSC: NCLEX: Physiological Integrity 6. A patient who is receiving sustained-release morphine sulfate (MS Contin) every 12 hours for chronic pain experiences level 9 (0 to 10 scale) breakthrough pain and anxiety. Which action by the nurse is appropriate for treating this change in assessment? a. Suggest amitriptyline 10 mg orally. b. Administer lorazepam (Ativan) 1 mg orally. c. Give ibuprofen (Motrin) 400 to 800 mg orally. d. Offer immediate-release morphine 30 mg orally. ANS: D The severe breakthrough pain indicates that the initial therapy should be a rapidly acting opioid, such as the immediate-release morphine. Lorazepam and amitriptyline may be appropriate to use as adjuvant therapy, but they are not likely to block severe breakthrough pain. Use of antianxiety agents for pain control is inappropriate because this patient’s anxiety is caused by the pain. DIF: Cognitive Level: Apply (application) REF: 108 TOP: Nursing Process: Implementation MSC: NCLEX: Physiological Integrity 7. A patient with chronic neck pain is seen in the pain clinic for follow-up. To evaluate whether the pain management is effective, which question is best for the nurse to ask?a. “Has there been a change in pain location?” b. “Can you describe the quality of your pain?” c. “How would you rate your pain on a 0 to 10 scale?” d. “Does the pain keep you from activities that you enjoy?” ANS: D The goal for the treatment of chronic pain usually is to enhance function and quality of life. The other questions are also appropriate to ask, but information about patient function is more useful in evaluating effectiveness. DIF: Cognitive Level: Apply (application) REF: 107 TOP: Nursing Process: Evaluation MSC: NCLEX: Physiological Integrity 8. A patient with a deep partial thickness burn has been receiving hydromorphone through patient-controlled analgesia (PCA) for 1 week. The nurse caring for the patient during the previous shift reports that the patient wakes up frequently during the night complaining of pain. What action by the nurse is appropriate? a. Administer a dose of morphine every 1 to 2 hours from the PCA machine while the patient is sleeping. b. Consult with the health care provider about using a different treatment protocol to control the patient’s pain. c. Request that the health care provider order a bolus dose of morphine to be given when the patient awakens with pain. d. Teach the patient to push the button every 10 minutes for an hour before going to sleep, even if the pain is minimal. ANS: B PCAs are best for controlling acute pain. This patient’s history indicates a need for a pain management plan that will provide adequate analgesia while the patient is sleeping. Administering a dose of morphine when the patient already has severe pain will not address the problem. Teaching the patient to administer unneeded medication before going to sleep can result in oversedation and respiratory depression. It is illegal for the nurse to administer the morphine for a patient through PCA. DIF: Cognitive Level: Apply (application) REF: 107 TOP: Nursing Process: Implementation MSC: NCLEX: Physiological Integrity 9. The nurse assesses that a patient receiving epidural morphine has not voided for more than 10 hours. What action should the nurse take initially? a. Place an indwelling urinary catheter. b. Monitor for signs of narcotic overdose. c. Ask if the patient feels the need to void. d. Encourage the patient to drink more fluids. ANS: CUrinary retention is a common side effect of epidural opioids. Assess whether the patient feels the need to void. Because urinary retention is a possible side effect, there is no reason for concern of overdose symptoms. Placing an indwelling catheter requires an order from the health care provider. Usually an in-and-out catheter is performed to empty the bladder if the patient is unable to void because of the risk of infection with an indwelling catheter. Encouraging oral fluids may lead to bladder distention if the patient is unable to void, but might be useful if a patient who is able to void has a fluid deficit. DIF: Cognitive Level: Apply (application) REF: 114 OBJ: Special Questions: Prioritization TOP: Nursing Process: Implementation MSC: NCLEX: Physiological Integrity 10. The nurse assesses that a home hospice patient with terminal cancer who complains of severe pain has a respiratory rate of 11 breaths/min. Which action should the nurse take? a. Inform the patient that increasing the morphine will cause the respiratory drive to fail. b. Tell the patient that additional morphine can be administered when the respirations are 12. c. Titrate the prescribed morphine dose up until the patient indicates adequate pain relief. d. Administer a nonsteroidal antiinflammatory drug (NSAID) to improve patient pain control. ANS: C The goal of opioid use in terminally ill patients is effective pain relief regardless of adverse effects such as respiratory depression. A nonopioid analgesic such as ibuprofen would not provide adequate analgesia or be absorbed quickly. The rule of double effect provides ethical justification for administering an increased morphine dose to provide effective pain control even though the morphine may further decrease the patient’s respiratory rate. DIF: Cognitive Level: Apply (application) REF: 125 TOP: Nursing Process: Implementation MSC: NCLEX: Physiological Integrity 11. The nurse is completing the medication reconciliation form for a patient admitted with chronic cancer pain. Which medication is of most concern to the nurse? a. Amitriptyline 50 mg at bedtime b. Ibuprofen 800 mg 3 times daily c. Oxycodone (OxyContin) 80 mg twice daily d. Meperidine (Demerol) 25 mg every 4 hours ANS: D Meperidine is contraindicated for chronic pain because it forms a metabolite that is neurotoxic and can cause seizures when used for prolonged periods. The ibuprofen, amitriptyline, and oxycodone are appropriate medications for long-term pain management. DIF: Cognitive Level: Apply (application) REF: 114 TOP: Nursing Process: Assessment MSC: NCLEX: Physiological Integrity 12. Which medication should the nurse administer for a patient with cancer who describes the pain as “deep, aching and at a level 8 on a 0 to 10 scale”? a. Ketorolac tabletsb. Fentanyl (Duragesic) patch c. Hydromorphone (Dilaudid) IV d. Acetaminophen (Tylenol) suppository ANS: C The patient’s pain level indicates that a rapidly acting medication such as an IV opioid is needed. The other medications may also be appropriate to use but will not work as rapidly or as effectively as the IV hydromorphone. DIF: Cognitive Level: Apply (application) REF: 112 TOP: Nursing Process: Implementation MSC: NCLEX: Physiological Integrity 13. The nurse is caring for a patient who has diabetes and complains of chronic, burning leg pain even when taking oxycodone (OxyContin) twice daily. Which prescribed medication is the best choice for the nurse to administer as an adjuvant to decrease the patient’s pain? a. Aspirin c. Celecoxib (Celebrex) b. Amitriptyline d. Acetaminophen (Tylenol) ANS: B The patient’s pain symptoms are consistent with neuropathic pain and the tricyclic antidepressants are effective for treating this type of pain. The other medications are more effective for nociceptive pain. DIF: Cognitive Level: Apply (application) REF: 106 TOP: Nursing Process: Implementation MSC: NCLEX: Physiological Integrity 14. A patient who uses a fentanyl (Duragesic) patch for chronic abdominal pain caused by ovarian cancer asks the nurse to administer the prescribed hydrocodone tablets, but the patient is asleep when the nurse returns with the medication. Which action is best for the nurse to take? a. Wake the patient and administer the hydrocodone. b. Wait until the patient wakes up and reassess the pain. c. Suggest the use of nondrug therapies for pain relief instead of additional opioids. d. Consult with the health care provider about changing the fentanyl (Duragesic) dose. ANS: A Because patients with chronic pain frequently use withdrawal and decreased activity as coping mechanisms for pain, sleep is not an indicator that the patient is pain free. The nurse should wake the patient and administer the hydrocodone. DIF: Cognitive Level: Apply (application) REF: 107 TOP: Nursing Process: Implementation MSC: NCLEX: Physiological Integrity 15. The following medications are prescribed by the health care provider for a middle-aged patient who uses long-acting morphine (MS Contin) for chronic back pain but still has ongoing pain. Which medication should the nurse question? a. Morphine c. Pentazocine (Talwin) b. Dexamethasone d. Celecoxib (Celebrex) ANS: COpioid agonist-antagonists can precipitate withdrawal if used in a patient who is physically dependent on mu agonist drugs such as morphine. The other medications are appropriate for the patient. DIF: Cognitive Level: Apply (application) REF: 114 TOP: Nursing Process: Implementation MSC: NCLEX: Physiological Integrity 16. The nurse is caring for a patient who had abdominal surgery yesterday and is receiving morphine through patient-controlled analgesia (PCA). What action by the nurse is a priority? a. Assessing for nausea c. Checking the respiratory rate b. Auscultating bowel sounds d. Evaluating for sacral redness ANS: C The patient’s respiratory rate is the highest priority of care while using PCA medication because of the possible respiratory depression. The other areas also require assessment but do not reflect immediately life-threatening complications. DIF: Cognitive Level: Analysis (analyze) REF: 115 OBJ: Special Questions: Prioritization TOP: Nursing Process: Assessment MSC: NCLEX: Physiological Integrity 17. A patient who has fibromyalgia reports pain at level 7 (0 to 10 scale). The patient tells the nurse, “I feel depressed because I ache too much to play golf.” Which patient goal has the highest priority when the nurse is developing the treatment plan? a. The patient will report pain at a level 2 of 10. b. The patient will be able to play a round of golf. c. The patient will exhibit fewer signs of depression. d. The patient will say that the aching has decreased. ANS: B For chronic pain, patients are encouraged to set functional goals such as being able to perform daily activities and hobbies. The patient has identified playing golf as the desired activity, so a pain level of 2 of 10 or a decrease in aching would be less useful in evaluating successful treatment. The nurse should also assess for depression, but the patient has identified the depression as being due to the inability to play golf, so the goal of being able to play golf is the most appropriate. DIF: Cognitive Level: Apply (application) REF: 107 OBJ: Special Questions: Prioritization TOP: Nursing Process: Planning MSC: NCLEX: Physiological Integrity 18. A patient who has just started taking sustained-release morphine sulfate (MS Contin) for chronic arthritic joint pain after a traumatic injury complains of nausea and abdominal fullness. Which action should the nurse take initially? a. Administer the ordered antiemetic medication. b. Order the patient a clear liquid diet until the nausea decreases. c. Tell the patient that the nausea should subside in about a week. d. Consult with the health care provider about using a different opioid. ANS: ANausea is frequently experienced with the initiation of opioid therapy, and antiemetics usually are prescribed to treat this expected side effect. The best choice would be to administer the antiemetic medication so the patient can eat. There is no indication that a different opioid is needed, although if the nausea persists, the health care provider may order a change of opioid. Although tolerance develops and the nausea will subside in about a week, it is not appropriate to allow the patient to continue to be nauseated. A clear liquid diet may decrease the nausea but may not provide needed nutrients for injury healing. DIF: Cognitive Level: Analyze (analysis) REF: 114 OBJ: Special Questions: Prioritization TOP: Nursing Process: Implementation MSC: NCLEX: Physiological Integrity 19. A patient with terminal cancer–related pain and a history of opioid abuse complains of breakthrough pain 2 hours before the next dose of sustained-release morphine sulfate (MS Contin) is due. Which action should the nurse take first? a. Use distraction by talking about things the patient enjoys. b. Suggest the use of alternative therapies such as heat or cold. c. Administer the prescribed PRN immediate-acting morphine. d. Consult with the doctor about increasing the MS Contin dose. ANS: C The patient’s pain requires rapid treatment, and the nurse should administer the immediate-acting morphine. Increasing the MS Contin dose and use of alternative therapies and distraction may also be needed, but the initial action should be to use the prescribed analgesic medications. DIF: Cognitive Level: Analyze (analysis) REF: 126 OBJ: Special Questions: Prioritization TOP: Nursing Process: Implementation MSC: NCLEX: Physiological Integrity 20. Which nursing action could the nurse delegate to unlicensed assistive personnel (UAP) when caring for a patient who is using a fentanyl (Duragesic) patch and a heating pad for treatment of chronic back pain? a. Check the skin under the heating pad. b. Count the respiratory rate every 2 hours. c. Ask the patient whether pain control is effective. d. Monitor sedation using the sedation assessment scale. ANS: B Obtaining the respiratory rate is included in UAP education and scope of practice. Assessment for sedation, pain control, and skin integrity requires more education and scope of practice. DIF: Cognitive Level: Apply (application) REF: 123 OBJ: Special Questions: Delegation TOP: Nursing Process: Planning MSC: NCLEX: Safe and Effective Care Environment 21. A patient who is using both a fentanyl (Duragesic) patch and immediate-release morphine for chronic cancer pain develops new-onset confusion, dizziness, and a decrease in respiratory rate. Which action should the nurse take first? a. Remove the fentanyl patch. b. Obtain complete vital signs.c. Notify the health care provider. d. Administer prescribed PRN naloxone ANS: A The assessment data indicate a possible overdose of opioid. The first action should be to remove the patch. Naloxone administration in a patient who has been chronically using opioids can precipitate withdrawal and would not be the first action. Notification of the health care provider and continued monitoring are also needed, but the patient’s data indicate that more rapid action is needed. The respiratory rate alone is an indicator for immediate action before obtaining blood pressure, pulse, and temperature. DIF: Cognitive Level: Analyze (analysis) REF: 118 OBJ: Special Questions: Prioritization TOP: Nursing Process: Implementation MSC: NCLEX: Physiological Integrity 22. The nurse reviews the medication orders for an older patient with arthritis in both hips who reports level 3 (0 to 10 scale) hip pain while ambulating. Which medication should the nurse offer as initial therapy? a. Naproxen 200 mg orally b. Oxycodone 5 mg orally c. Acetaminophen 650 mg orally d. Aspirin (acetylsalicylic acid) 650 mg orally ANS: C Acetaminophen is the best first-choice medication. The principle of “start low, go slow” is used to guide therapy when treating older adults because the ability to metabolize medications is decreased and the likelihood of medication interactions is increased. Nonopioid analgesics are used first for mild to moderate pain, although opioids may be used later. Aspirin and nonsteroidal antiinflammatory drugs are associated with a high incidence of gastrointestinal bleeding in older patients. DIF: Cognitive Level: Analyze (analysis) REF: 112 OBJ: Special Questions: Prioritization TOP: Nursing Process: Implementation MSC: NCLEX: Physiological Integrity 23. The nurse on a surgical inpatient unit is caring for several patients. Which patient should the nurse assess first? a. Patient with postoperative pain who received morphine sulfate IV 15 minutes ago b. Patient who received hydromorphone (Dilaudid) 1 hour ago and is currently asleep c. Patient who was treated for pain just prior to return from the postanesthesia care unit d. Patient with neuropathic pain who is scheduled to receive a dose of hydrocodone (Lortab) now ANS: C The risk for oversedation is greatest in the first 4 hours after transfer from the postanesthesia care unit. Patients should be reassessed 30 minutes after receiving IV opioids for pain. A scheduled oral medication does not need to be administered exactly at the scheduled time. A patient who falls asleep after pain medication can be allowed to rest. DIF: Cognitive Level: Analyze (analysis) REF: 115 OBJ: Special Questions: Prioritization | Special Questions: Multiple PatientsTOP: Nursing Process: Planning MSC: NCLEX: Safe and Effective Care Environment MULTIPLE RESPONSE 1. The health care provider orders a patient-controlled analgesia (PCA) machine to provide pain relief for a patient with acute surgical pain who has never received opioids before. Which nursing actions regarding opioid administration are appropriate at this time (select all that apply)? a. Assess for signs that the patient is becoming addicted to the opioid. b. Monitor for therapeutic and adverse effects of opioid administration. c. Emphasize that the risk of some opioid side effects increases over time. d. Teach the patient about how analgesics improve postoperative activity levels. e. Provide instructions on decreasing opioid doses by the second postoperative day. ANS: B, D Monitoring for pain relief and teaching the patient about how opioid use will improve postoperative outcomes are appropriate actions when administering opioids for acute pain. Although postoperative patients usually need a decreasing amount of opioids by the second postoperative day, each patient’s response is individual. Tolerance may occur, but addiction to opioids will not develop in the acute postoperative period. The patient should use the opioids to achieve adequate pain control, so the nurse should not emphasize the adverse effects. DIF: Cognitive Level: Apply (application) REF: 115 OBJ: Special Questions: Alternate item format: Multiple response TOP: Nursing Process: Implementation MSC: NCLEX: Physiological Integrity 2. A nurse assesses a postoperative patient 2 days after chest surgery. What findings indicate that the patient requires better pain management (select all that apply)? a. Confusion b. Hypoglycemia c. Poor cough effort d. Shallow breathing e. Elevated temperature ANS: A, C, D, E Inadequate pain control can decrease tidal volume and cough effort, leading to complications such as pneumonia with increases in temperature. Poor pain control may lead to confusion through a variety of mechanism, including hypoventilation and poor sleep quality. Stressors such as pain cause increased release of corticosteroids that can result in hyperglycemia. DIF: Cognitive Level: Apply (application) REF: 103 OBJ: Special Questions: Alternate item format: Multiple response TOP: Nursing Process: Assessment MSC: NCLEX: Physiological Integrity OTHER1. A patient with chronic pain who has been receiving morphine sulfate 20 mg IV over 24 hours is to be discharged home on oral sustained-release morphine (MS Contin) administered twice a day. What dosage of MS Contin will be needed for each dose to obtain an equianalgesic dose for the patient? (Morphine sulfate 10 mg IV is equianalgesic to morphine sulfate 30 mg orally.) ANS: MS Contin 30 mg/dose Morphine sulfate 20 mg IV over 24 hours will be equianalgesic to MS Contin 60 mg in 24 hours. Because the total dose needs to be divided into two doses, each dose should be 30 mg. DIF: Cognitive Level: Apply (application) REF: 117 OBJ: Special Questions: Alternate item format: Fill in the blank TOP: Nursing Process: Implementation MSC: NCLEX: Physiological IntegrityChapter 09: Palliative Care at End of Life Lewis: Medical-Surgical Nursing, 10th Edition MULTIPLE CHOICE 1. The nurse is caring for an unresponsive terminally ill patient who has 20-second periods of apnea followed by periods of deep and rapid breathing. Which action by the nurse would be appropriate? a. Suction the patient’s mouth. b. Administer oxygen via face mask. c. Document Cheyne-Stokes respirations. d. Place the patient in high Fowler’s position. ANS: C Cheyne-Stokes respirations are characterized by periods of apnea alternating with deep and rapid breaths. Cheyne-Stokes respirations are expected in the last days of life and are not position dependent. There is also no need for supplemental oxygen by face mask or suctioning the patient. DIF: Cognitive Level: Apply (application) REF: 132 TOP: Nursing Process: Assessment MSC: NCLEX: Physiological Integrity 2. The nurse is caring for an adolescent patient who is dying. The patient’s parents are interested in organ donation and ask the nurse how the health care providers determine brain death. Which response by the nurse accurately describes brain death determination? a. “If CPR does not restore a heartbeat, the brain cannot function.” b. “Brain death has occurred if there is not any breathing or brainstem reflexes.” c. “Brain death has occurred if a person has flaccid muscles and does not awaken.” d. “If respiratory efforts cease and no apical pulse is audible, brain death is present.” ANS: B The diagnosis of brain death is based on irreversible loss of all brain functions, including brainstem functions that control respirations and brainstem reflexes. The other descriptions describe other clinical manifestations associated with death but are insufficient to declare a patient brain dead. DIF: Cognitive Level: Apply (application) REF: 131 TOP: Nursing Process: Assessment MSC: NCLEX: Physiological Integrity 3. A patient in hospice is manifesting a decrease in all body system functions except for a heart rate of 124 beats/min and a respiratory rate of 28 breaths/min. Which statement, if made by the nurse to the patient’s family member, is most appropriate? a. “These vital signs will continue to increase until death finally occurs.” b. “These vital signs are an expected response now but will slow down later.” c. “These vital signs may indicate an improvement in the patient’s condition.” d. “These vital signs are a helpful response to the slowing of other body systems.” ANS: BAn increase in heart and respiratory rate may occur before the slowing of these functions in a dying patient. Heart and respiratory rate typically slow as the patient progresses further toward death. In a dying patient, high respiratory and pulse rates do not indicate improvement or compensation, and it would be inappropriate for the nurse to indicate this to the family. DIF: Cognitive Level: Apply (application) R [Show More]
Last updated: 1 year ago
Preview 1 out of 698 pages
Instant download
Buy this document to get the full access instantly
Instant Download Access after purchase
Add to cartInstant download
Reviews( 0 )
Document information
Connected school, study & course
About the document
Uploaded On
Aug 24, 2022
Number of pages
698
Written in
Additional information
This document has been written for:
Uploaded
Aug 24, 2022
Downloads
0
Views
212