Health Care > TEST BANK > TEST BANK FOR NURSING INTERVENTIONS AND CLINICAL SKILLS 7TH EDITION BY POTTER |GRADED A+2022 (All)
TEST BANK FOR NURSING INTERVENTIONS AND CLINICAL SKILLS 7TH EDITION BY POTTER |GRADED A+2022
Document Content and Description Below
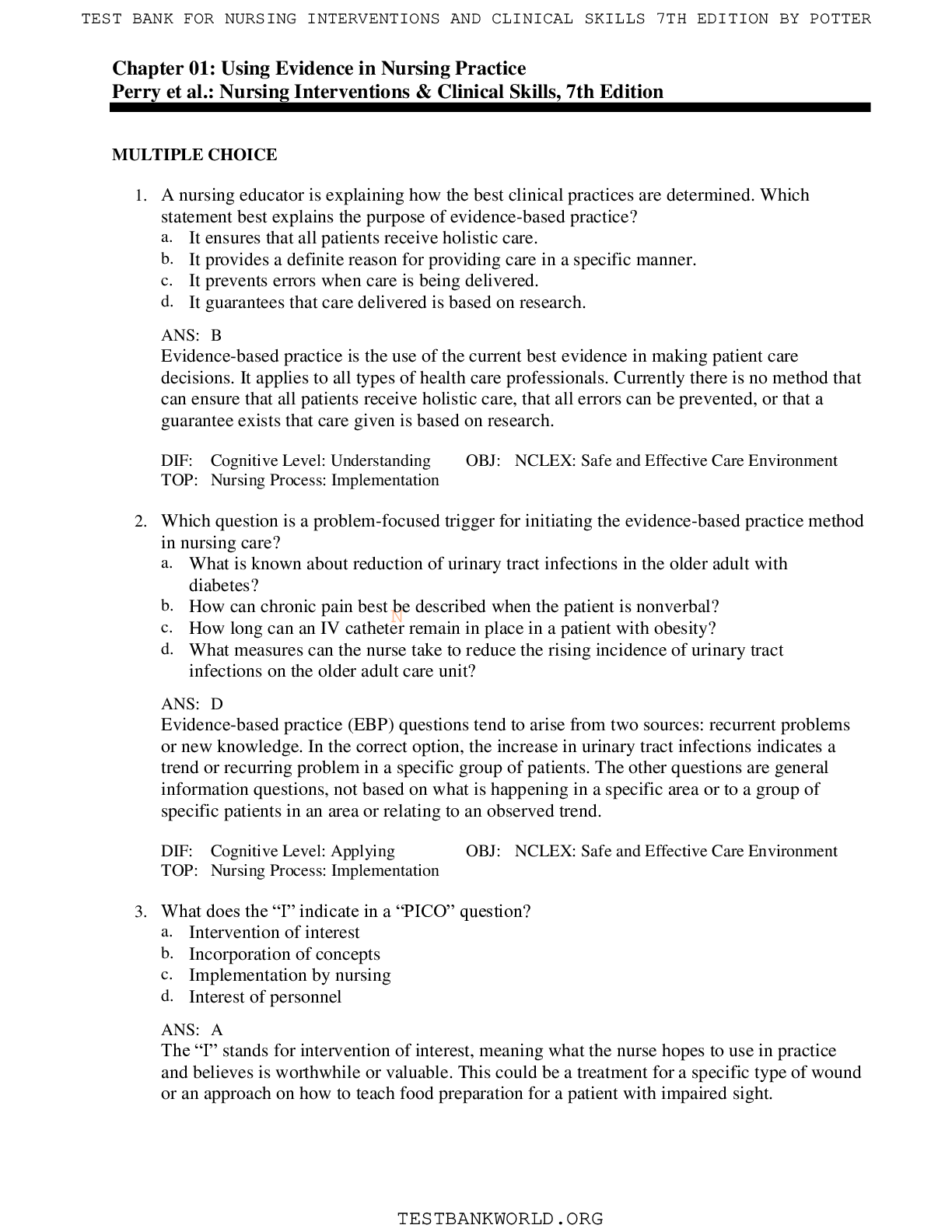
TEST BANK FOR NURSING INTERVENTIONS AND CLINICAL SKILLS 7TH EDITION BY POTTER TEST BANK FOR NURSING INTERVENTIONS AND CLINICAL SKILLS 7TH EDITION BY POTTER N Chapter 01: Using Evidence in Nursing Prac... tice Perry et al.: Nursing Interventions & Clinical Skills, 7th Edition MULTIPLE CHOICE 1. A nursing educator is explaining how the best clinical practices are determined. Which statement best explains the purpose of evidence-based practice? a. It ensures that all patients receive holistic care. b. It provides a definite reason for providing care in a specific manner. c. It prevents errors when care is being delivered. d. It guarantees that care delivered is based on research. ANS: B Evidence-based practice is the use of the current best evidence in making patient care decisions. It applies to all types of health care professionals. Currently there is no method that can ensure that all patients receive holistic care, that all errors can be prevented, or that a guarantee exists that care given is based on research. DIF: Cognitive Level: Understanding OBJ: NCLEX: Safe and Effective Care Environment TOP: Nursing Process: Implementation 2. Which question is a problem-focused trigger for initiating the evidence-based practice method in nursing care? a. What is known about reduction of urinary tract infections in the older adult with diabetes? b. How can chronic pain best be described when the patient is nonverbal? c. How long can an IV catheter remain in place in a patient with obesity? d. What measures can the nurse take to reduce the rising incidence of urinary tract infections on the older adult care unit? ANS: D Evidence-based practice (EBP) questions tend to arise from two sources: recurrent problems or new knowledge. In the correct option, the increase in urinary tract infections indicates a trend or recurring problem in a specific group of patients. The other questions are general information questions, not based on what is happening in a specific area or to a group of specific patients in an area or relating to an observed trend. DIF: Cognitive Level: Applying OBJ: NCLEX: Safe and Effective Care Environment TOP: Nursing Process: Implementation 3. What does the “I” indicate in a “PICO” question? a. Intervention of interest b. Incorporation of concepts c. Implementation by nursing d. Interest of personnel ANS: A The “I” stands for intervention of interest, meaning what the nurse hopes to use in practice and believes is worthwhile or valuable. This could be a treatment for a specific type of wound or an approach on how to teach food preparation for a patient with impaired sight. DIF: Cognitive Level: Remembering OBJ: NCLEX: Safe and Effective Care Environment TOP: Nursing Process: Implementation 4. Who will the clinical research nurse contact to search relevant databases in preparation for an upcoming study? a. The physician whose patients may be involved in the study b. The medical librarian c. The nurse manager of the unit where the study will be conducted d. The director of nursing of the facility ANS: B The medical librarian is most knowledgeable regarding databases relevant to a study. The other individuals do not have the knowledge regarding relevant databases. DIF: Cognitive Level: Understanding OBJ: NCLEX: Safe and Effective Care Environment TOP: Nursing Process: Implementation 5. Which database contains summaries of clinical guidelines and their development? a. MEDLINE b. CINAHL c. Cochrane Database of Systematic Reviews d. The National Guideline Clearinghouse ANS: D The National Guideline Clearinghouse is a database supported by the Agency for Healthcare Research and Quality. It contains summaries of clinical guidelines for practice. MEDLINE is a database for studies in medicNine, nursing, dentistry, psychiatry, veterinary medicine, and allied health. CINAHL (Cumulative Index of Nursing and Allied Health Literature) includes studies in nursing, allied health, and biomedicine. The Cochrane Database Full text of regularly updated systematic reviews prepared by the Cochrane Collaboration includes completed reviews and protocols. DIF: Cognitive Level: Remembering OBJ: NCLEX: Safe and Effective Care Environment TOP: Nursing Process: Implementation 6. Which does the nurse researcher identify as the strongest type of research? a. Randomized controlled trials b. A qualitative study c. A descriptive study d. A case controlled study ANS: A Individual randomized controlled trials are close to the top of the research pyramid. Only systematic reviews and meta-analyses are higher. This type of study tests an intervention against the usual standard of care. The other types of studies are useful but do not give the same type of information as a randomized controlled trial provides. DIF: Cognitive Level: Remembering OBJ: NCLEX: Safe and Effective Care Environment TOP: Nursing Process: Assessment 7. What is the nurse attempting to determine when critiquing the evidence related to a PICOT question? a. The ethical conduct of the research the nurse read b. The strength of the evidence found in the literature c. If there are any experts in the clinical question needing to be researched d. If the study demonstrates cost-effectiveness if a change in practice occurs ANS: B Once a literature search is complete and data are gathered about the question, it is time to critique the evidence. Critiquing the evidence involves a systematic approach to looking at the strength of the work reviewed and its relevance. The other questions are not applicable to critiquing the evidence. DIF: Cognitive Level: Understanding OBJ: NCLEX: Safe and Effective Care Environment TOP: Nursing Process: Implementation 8. A nurse finds a cohort study comparing one group taking hormone treatment with another group not taking hormone treatment to determine the incidence of changes in bone density of the lower spine. What can the nurse imply from this study? a. Low level of strength makes the study limited in value. b. Moderate level of strength makes the study probably useful. c. Opinions of the individuals in the cohort are not research. d. This could be the basis for a Quality Improvement project. ANS: B A cohort study is Level 4 evidence as it is a single, non-experimental study. This moderate level of evidence makes the study probably useful but the nurse should strive to find stronger evidence. N DIF: Cognitive Level: Applying OBJ: NCLEX: Safe and Effective Care Environment TOP: Nursing Process: Evaluation 9. Which question would be the best example of a knowledge-focused trigger for conducting an evidence-based practice project? a. What is the best method for treatment of leg swelling when a patient is taking gabapentin (Neurontin)? b. How can we decrease the incidence of skin cancer in adults over the age of 65? c. What is the current evidence for improving oral intake for cancer patients with stomatitis? d. What is the maximal length of time our hospital allows irrigation kits to be used? ANS: C Evidence-based practice (EBP) questions tend to arise from two sources: recurrent problems or new knowledge. In this example, the new knowledge that drives the question is the one looking at current evidence. The other questions do not look at the newest knowledge to form a question to research. DIF: Cognitive Level: Analyzing OBJ: NCLEX: Safe and Effective Care Environment TOP: Nursing Process: Implementation MULTIPLE RESPONSE 1. When planning to implement an evidence-based practice strategy, what factors are most important for the nurse to consider and include? (Select all that apply.) a. Time required to perform the strategy b. Patient preferences and values c. Clinical expertise d. Scientific knowledge e. Historical practices ANS: B, C, D When implementing evidence-based practice, the nurse considers and includes clinical expertise and patient preferences and values in addition to the scientific knowledge. Time required to perform the new strategy and customary practices are not vital to this approach. In fact, EBP seeks to ensure practices are based on evidence and not just historical practice. DIF: Cognitive Level: Remembering OBJ: NCLEX: Safe and Effective Care Environment TOP: Nursing Process: Implementation 2. A new nurse wants to ensure practice is based on the best knowledge available. What actions are best for this nurse to be involved in evidence-based practice? (Select all that apply.) a. Design and conduct a study based on interest. b. Join the hospital’s policy review committee. c. Remain vigilant for recurring problems. d. Maintain a spirit of inquiry. e. Read current literature appropriate to practice area. ANS: B, C, D, E This novice nurse would best mNaintain an evidence-based nursing practice by joining policy review committees, watching for and taking note of recurring problems in the practice area, maintaining a spirit of inquiry, and staying current in the literature. The nurse would not need to design and conduct a study. DIF: Cognitive Level: Applying OBJ: NCLEX: Safe and Effective Care Environment TOP: Nursing Process: Implementation 3. When explaining the value of evidence-based practice, what benefits does the nurse include? (Select all that apply.) a. Improves quality of care. b. Improves patient outcomes. c. Improves stakeholder satisfaction. d. Incorporates near real-time data in practice. e. Helps nurses remain current in practice. ANS: A, B, D, E There are five ways that EBP adds value to the health care system: helps clinicians remain current on standardized, evidence-based protocols; uses near real-time scientific data to make care decisions; improves transparency, accountability, and value (e.g. safe care); improves quality of care; and improves outcomes. One would hope all stakeholders would be more satisfied with this method of determining care but that is not one of the specific benefits. DIF: Cognitive Level: Remembering OBJ: NCLEX: Safe and Effective Care Environment TOP: Nursing Process: Implementation Chapter 02: Communication and Collaboration Perry et al.: Nursing Interventions & Clinical Skills, 7th Edition MULTIPLE CHOICE 1. The nurse interviews a patient during admission. Which observation by the nurse identifies consistency between the patient’s verbal and nonverbal communication? a. Asserts she is eager to answer questions while reading a magazine. b. States that he wants information while frequently changing the subject. c. Asks the nurse to explain a surgical procedure while she listens intently. d. Explains that he is relaxed while continuously shifting in his chair. ANS: C The patient demonstrates congruency, or consistency, between her verbal statement asking for an explanation and her nonverbal cue of listening intently. The verbal and nonverbal messages match; each indicates that the nurse’s response is important to her. If she is eager to answer questions, the patient should focus on the nurse’s questions or note taking; reading a magazine is a distraction and indicates a lack of interest. Changing the subject may indicate discomfort or reluctance to address the issue. Continually shifting position may be an indication of anxiety. DIF: Cognitive Level: Applying OBJ: NCLEX: Safe and Effective Care Environment TOP: Nursing Process: Assessment 2. The nurse is interviewing a newly admitted patient. Which statement by the nurse is most likely to result in effective patient communication? a. “I’m not sure why you’re here. Can you explain it to me?” b. “Tell me about things and people that are important to you.” c. “Tell me more about your pain. Where does it start?” d. “If you think it’s important, I’ll try to notify the provider.” ANS: C The nurse communicates effectively by using focused questions. This encourages the patient to give more information about the specific topic of concern. The remaining options are ineffective communication techniques because each potentially impairs the exchange of information between the nurse and the patient regarding care needs. The patient may be unwilling to express concerns openly after the nurse expresses lack of understanding and empathy. The patient will also likely lose confidence in the nurse if the nurse expresses confusion about suitability of the patient’s presence. By asking what is important to the patient, the nurse loses focus of the objective of the communication and is likely to confuse the patient. DIF: Cognitive Level: Applying OBJ: NCLEX: Safe and Effective Care Environment TOP: Integrated Process: Communication and Documentation 3. After receiving a diagnosis of a fatal disease, the patient expresses sadness and states “I don’t know what to do next”. Which action by the nurse best facilitates communication at this time? a. Sit quietly with the patient and observe nonverbal communication. b. Reassure the patient that his family will take care of him. c. Refer the patient to a church for spiritual counseling. d. Tell the patient that hospice care is available immediately. ANS: A Because of the grim diagnosis, the patient expresses confusion and lacks a clear direction. The patient is not able to process information at this time and is overwhelmed. Sitting quietly with the patient shows acceptance, empathy, and allows the nurse to observe nonverbal communication. The patient can benefit from a calming atmosphere and time to process the new information. Assuring the patient of family involvement requires consultation with the family first. Spiritual counseling may not be indicated for this patient if the patient does not wish to participate. Discussing hospice at this early stage is premature; the patient needs time to process the news and gather information but is not able to do so right now. DIF: Cognitive Level: Applying OBJ: NCLEX: Safe and Effective Care Environment TOP: Integrated Process: Communication and Documentation 4. The nurse is preparing to begin the patient hand-off procedure for five patients. Who should the nurse include in this process? a. Only the licensed nurses b. The nursing personnel caring for the patients c. The entire interdisciplinary team d. The nurses and health care provider ANS: B All the nursing personnel on the unit who will be interacting with this group of patients should actively participate in the patient hand-off. This would include nursing assistive personnel (NAP) and the nurses. An interdisciplinary team usually meets when there is a problem with a patient and all the team members need to discuss approaches and plans with and for a patient or as a routine meeting. The heNalth care provider does not participate in the patient hand-off procedure. DIF: Cognitive Level: Remembering OBJ: NCLEX: Safe and Effective Care Environment TOP: Integrated Process: Communication and Documentation 5. The nurse brings the patient’s medications into the room, and the patient shouts, “You don’t care if I take these, so get out of my room!” Which response by the nurse is most appropriate? a. “Who misinformed you about my feelings?” b. “You seem very angry about the medications.” c. “We know each other; why are you saying this?” d. “I cannot leave until you take these medications.” ANS: B Stating observations encourages the patient to be aware of his or her behavior. This neutral response would allow the patient time to explain the meaning behind the anger. Asking who misinformed the patient is confrontational. “Why” questions tend to put people on the defensive. Stating that the nurse cannot leave until the medications are taken is also confrontational and would set up a possible power struggle between the two. DIF: Cognitive Level: Applying OBJ: NCLEX: Safe and Effective Care Environment TOP: Integrated Process: Communication and Documentation 6. The patient shouts at the nurse, “No one answered my nurse call system all night!” Which response would the nurse use with this patient to restore therapeutic communication? a. “Shouting is going to disturb other patients.” b. “I see how that would make you very angry.” c. “Are you sure the nurses were avoiding you?” d. “The unit has many very sick patients right now.” ANS: B Regardless of whether the nurses answered the patient’s nurse call system during the night, the patient felt ignored. By empathizing with the patient’s distress and reflecting feelings, the nurse displays respect and understanding of his or her experience. Reprimanding the patient is humiliating and conveys the nurse’s lack of regard for the patient’s feelings. Quieting the patient is achievable by displaying empathy, caring, respect, and willingness to hear his or her complaints. Questioning the patient’s perception is demeaning and forces the patient to justify feelings, similar to asking a “why” question. Stating that the unit has very sick patients implies that the patient is not as important as the others are. DIF: Cognitive Level: Applying OBJ: NCLEX: Safe and Effective Care Environment TOP: Integrated Process: Communication and Documentation 7. A patient with a history of violence directed toward others becomes very excited and agitated during the nurse’s interview. Which intervention does the nurse implement to foster therapeutic communication? a. Call the security staff for assistance. b. Ask the patient to use self-control. c. Lean forward and touch the patient’s arm. d. Assume an open, nonthreatening posture. ANS: D The nurse should use neutraliziNng skills and assume an open, nonthreatening posture that conveys respect and acceptance, creating an atmosphere in which the patient can communicate without feeling threatened or defensive. Calling security in the patient’s presence is likely to aggravate the patient and escalate the potential for violence because it is humiliating, conveys the nurse’s rejection of the patient, and threatens to take all control away. Asking the patient to use self-control is reprimanding, humiliating, and conveys rejection and lack of respect by the nurse. The patient can perceive leaning in and touching as threatening. DIF: Cognitive Level: Applying OBJ: NCLEX: Safe and Effective Care Environment TOP: Integrated Process: Communication and Documentation 8. The nurse admits a patient who is nonverbal and agitated. What can the nurse do to communicate effectively with the patient? a. Use a communication aid. b. Wait for family to arrive. c. Call interpreter services. d. Treat the patient for pain. ANS: A Patients with sensory losses require communication techniques that maximize existing sensory and motor functions. Some patients are unable to speak because of physical or neurological alterations such as paralysis; a tube in the trachea to facilitate breathing; or a stroke resulting in aphasia, difficulty understanding, or verbalizing. Many types of communication aids are available for use, including writing boards, flash cards, and picture boards. The nurse needs to determine what will work for the patient. Waiting for family is unacceptable because the patient needs care and the family may be delayed or not come at all. Interpreter services are for patients who do not speak the language. The nurse should not assume the patient has pain before completing an assessment. DIF: Cognitive Level: Applying OBJ: NCLEX: Safe and Effective Care Environment TOP: Nursing Process: Assessment 9. A patient’s mother died several days ago. The patient begins to cry and states, “The pain of her death is impossible to bear.” Which statement by the nurse is the most effective response? a. “I was depressed last year when my mother died, too.” b. “I know things seem bleak, but you are doing so well.” c. “I can see this is a very difficult time for you right now.” d. “Should I cancel your appointment with the cardiologist?” ANS: C The nurse conveys empathy and respect by acknowledging the patient’s grief. This is an effective response and is likely to enhance the nurse–patient relationship because it is patient centered, displays caring and respect, and helps to make the patient feel accepted. Relating personal details about the nurse’s life redirects the focus of the communication to the nurse and fails to support the objectives of the nurse–patient relationship. Responding with a comment about the patient’s prN ogress and asking about the cardiologist’s appointment ignores the patient’s grief and conveys a lack of respect and consideration. DIF: Cognitive Level: Applying OBJ: NCLEX: Safe and Effective Care Environment TOP: Integrated Process: Communication and Documentation 10. A patient who says that both parents died of heart disease early in life is waiting for diagnostic testing results. The patient is biting fingernails and pacing around the room. Which statement should the nurse use to clarify patient information? a. “I can see that you are anxious about dying.” b. “Tell me more about your family’s history.” c. “Do you have your parents’ medical records?” d. “I’m not sure that I understand what you mean.” ANS: B Asking for more information about the family’s history directs the patient to expand on a specific, pertinent topic and relate key details before moving to another topic. “Early in life” and “heart disease” need to be defined by the patient; “early in life” can indicate a wide range of ages, depending on the definition of “early,” and “heart disease” can mean conditions such as heart failure, coronary artery disease, valve disease, and arrhythmias. Until the patient discusses his particular concerns, the nurse cannot be sure about the source of his anxiety. Asking for the records can display a lack of respect by implying that the patient is an unreliable source for information. Stating that the nurse is not sure what the patient means is vague, leaving the patient to guess what the nurse wants to know. DIF: Cognitive Level: Applying OBJ: NCLEX: Safe and Effective Care Environment TOP: Integrated Process: Communication and Documentation 11. The patient tells the nurse, “I must be very sick because so many tests are being performed.” Which statement does the nurse use to clarify the patient’s message? a. “I sense that you are very worried.” b. “Why do you mention this so frequently?” c. “We should talk about this more.” d. “Are you saying you think you are seriously ill?” ANS: D The nurse clarifies the patient’s message. This encourages the patient to expand on a thought or feeling that seems vague to the nurse. Pointing out that the patient has stated this before can be misinterpreted to mean that the patient is forgetful or annoying, and “why” questions tend to put people on the defensive. Stating that the nurse feels that the patient is worried is a suitable response but does not clarify what the patient actually said. Telling the patient he or she “should” talk about this topic is confrontational. DIF: Cognitive Level: Applying OBJ: NCLEX: Safe and Effective Care Environment TOP: Integrated Process: Communication and Documentation 12. The patient tells the nurse, “I want to die.” Which is the best response by the nurse to facilitate therapeutic communication? a. “Now why would you say a thing like that?” b. “Tell me more about how you’re feeling.” c. “We need to tell the provider how you feel.” d. “You have too much to live for to say that.” N ANS: B The patient’s statement warrants further investigation to determine how serious the patient is about dying and whether he or she has a plan. To elicit more information from the patient in a respectful and caring manner, the nurse allows the patient to expand on the statement, “I want to die” by stating, “Tell me more.” The statement displays concern for and value of the patient by acknowledging the patient’s message and encouraging him or her to continue. Safety is a major concern when a patient wants to die, and the remaining options are likely to be perceived as patronizing and/or dismissive. DIF: Cognitive Level: Applying OBJ: NCLEX: Safe and Effective Care Environment TOP: Integrated Process: Communication and Documentation 13. The nurse is explaining a procedure to a 3-year-old patient. Which strategy would the nurse use for patient teaching? a. Ask the patient to draw her feelings. b. Show needles, syringes, and bandages. c. Tell the patient about postoperative pain. d. Use dolls and stories to explain surgery. ANS: D Using dolls, stuffed animals, or puppets with stories is a suitable way to explain surgery to the 3-year-old patient because storytelling is a familiar communication method for the toddler’s developmental stage. A 3-year-old child is unlikely to understand an explanation about the surgery suited for an adult, and the discussion can frighten the child and upset the family or guardian. A 3-year-old child lacks the fine motor and cognitive skills to draw an abstract concept. A toddler is unlikely to understand and probably would be frightened by a discussion about postoperative pain. DIF: Cognitive Level: Applying OBJ: NCLEX: Safe and Effective Care Environment TOP: Integrated Process: Communication and Documentation 14. The nurse is caring for a patient who states, “I don’t feel well today.” Which is the best response by the nurse? a. Ask the patient to continue to describe the feeling. b. Measure the blood pressure and temperature. c. State that the patient’s diagnostic testing had normal results. d. Compare recent laboratory results with the prior results. ANS: A Because the patient’s statement is too vague, the nurse asks him or her to continue describing, “I don’t feel well today,” because many disorders begin with nonspecific complaints. Depending on the details the patient shares, the nurse plans and implements nursing care individualized to his or her description. This may include taking vital signs, and reviewing lab data, but before taking action the nurse needs more information. Telling the patient that test results are normal is dismissive of the concern. DIF: Cognitive Level: ApplyingN OBJ: NCLEX: Safe and Effective Care Environment TOP: Integrated Process: Communication and Documentation 15. The nurse is caring for a patient who refuses to participate in physical therapy (PT) and states, “I really don’t like to exercise.” Which response by the nurse is most likely to help engage the patient in PT? a. “It makes the pain worse, doesn’t it?” b. “What don’t you like about exercise?” c. “You really should do these exercises.” d. “Do you like to do any other activities?” ANS: B The nurse asks an open-ended question using the patient’s words to uncover information about the patient’s refusal to participate in PT by asking what the patient dislikes about exercise. Using the patient’s words conveys acceptance and value because the nurse listened closely enough to repeat what the patient said. Asking the patient a yes-or-no question such as, “It makes the pain worse, doesn’t it?” is unlikely to promote further discussion because it is a closed, yes/no question. Telling the patient to do the exercises is giving advice; rather the nurse can tell the patient the reason for the therapy and the benefits of doing it or the risks of not doing it. Asking about other activities moves the focus away from the patient’s need for physical therapy. This is also a yes/no question. DIF: Cognitive Level: Applying OBJ: NCLEX: Safe and Effective Care Environment TOP: Integrated Process: Communication and Documentation 16. The nursing staff are using the SBAR communication technique during patient hand-off communication. The circumstances leading up to the current status would be explained by the nurses during which step of the technique? a. Situation b. Background c. Assessment d. Recommendations ANS: B The background explains circumstances leading up to the situation. The situation explains what is happening at the present time. The assessment phase identifies what the problem is thought to be. The recommendations explain how to correct the problem. DIF: Cognitive Level: Remembering OBJ: NCLEX: Safe and Effective Care Environment TOP: Integrated Process: Communication and Documentation 17. The nursing staff are working with a postoperative patient from another culture who does not understand or speak the English language well. Which approach by the nurse would be best? a. Act out what the patient needs to do. b. Obtain a medical interpreter. c. Assess if the patient can read or write. d. Talk slowly when instructions are given. ANS: B A medical interpreter would be most helpful for effective communication. Acting out what the patient needs to do is ineffective and may be embarrassing to both the patient and the nurse. Since the patient and nurse do not speak a common language, defining the patient’s ability to read or write in his native languNage does not solve the communication problem. Talking slowly will not improve the patient’s ability to understand an unfamiliar language. DIF: Cognitive Level: Applying OBJ: NCLEX: Safe and Effective Care Environment TOP: Integrated Process: Communication and Documentation 18. The nurse is working toward discharging a patient. Which of following demonstrates patient engagement during the discharge process? a. Teaching the patient how to use his equipment b. Having the patient establish daily goals c. Reviewing the discharge instructions with the patient d. Including the family in the discharge planning ANS: B All of the answers are important to the discharge process but having the patient set his or her own daily goals establishes true patient engagement. The other interventions are performed by the nurse and do not really engage the patient. Patient engagement requires that the patient’s preferences be incorporated. DIF: Cognitive Level: Applying OBJ: NCLEX: Safe and Effective Care Environment TOP: Integrated Process: Communication and Documentation 19. The registered nurse is orienting a new nurse to the unit. They are completing paperwork on a newly admitted patient. When the experienced nurse asks what the new nurse thinks the patient will need to learn for self-care at home, the new nurse expresses surprise. What statement by the registered nurse is most appropriate? a. “You should always at least start thinking about discharge planning.” b. “We don’t want to wait too long because unexpected things happen.” c. “The admitting nurse has to fill in all sections of this document.” d. “Best practice is to begin discharge planning on admission.” ANS: D Discharge planning should begin on admission to be accurate, thorough, and to allow the patient and/or family enough time to learn information or to master skills they will need at home. The other options may be at least partially true, but the only comprehensive answer is that it is best practice. DIF: Cognitive Level: Understanding OBJ: NCLEX: Safe and Effective Care Environment TOP: Integrated Process: Communication and Documentation 20. A student is watching a nurse perform a medication reconciliation prior to transferring the patient to a skilled nursing facility. What explanation of this process to the student is best? a. “It is required by the Joint Commission before discharge or transfer.” b. “It creates an accurate list of medications so errors do not occur later.” c. “It helps us recognize lapses in patients’ ability to remember their medications.” d. “Receiving facilities won’t accept patients without a reconciliation.” ANS: B Medication reconciliation is the process of creating the most accurate list of medications a patient is taking and comparingNit to provider admission, transfer, and discharge orders. This is done in order to prevent medication errors at each transition. DIF: Cognitive Level: Understanding OBJ: NCLEX: Safe and Effective Care Environment TOP: Integrated Process: Communication and Documentation 21. A nurse is reviewing medications and treatments one final time before the patient goes home. The patient becomes agitated and says “I just can’t do this! I’m too upset to ever be able to learn this!” What action by the nurse is best? a. Provide immediate remediation on the knowledge and skills. b. Ask the patient if home health care might be acceptable. c. Request the provider re-examine all the discharge orders. d. Tell the patient you would like to understand what is most difficult. ANS: D Just prior to discharge, the nurse reviews the discharge orders and plans with the patient. When the patient cannot recall information or perform needed skills, the nurse can provide immediate re-teaching and skills practice. However, this patient is upset, so the nurse must first determine the most bothersome aspect of the situation, which may or may not include the instructions. The nurse must first assess this before deciding if home health care is acceptable or before asking the provider to review the orders to see if they are all necessary. DIF: Cognitive Level: Applying OBJ: NCLEX: Safe and Effective Care Environment TOP: Integrated Process: Communication and Documentation MULTIPLE RESPONSE 1. During a home care visit, the patient experiences an angry outburst and hits the nurse on the thigh and yells at her. The patient continues to be threatening. What are the most appropriate initial actions by the nurse? (Select all that apply.) a. Increase the personal space between the nurse and patient. b. Call law enforcement to take the patient to the hospital. c. Restrain the patient’s hands to the chair. d. Be empathetic to the patient’s feelings and concerns. e. Call the nursing agency to ask for advice in working with this patient. f. Use a calm, quiet voice when talking with the patient. ANS: A, D, F The priority in this situation is the safety of both nurse and patient. The nurse should ensure there is adequate personal space between the two of them so the patient cannot strike the nurse. Being empathetic displays respect; even if the nurse disagrees with the patient’s perception, it is real to that person. Using a calm, quiet voice is a de-escalation technique. The patient may or may not need hospitalization, but calling the police would not be the first action. The patient’s hands should not be restrained as this could cause the patient to escalate and perhaps feel assaulted. The nursing agency should be consulted, but not as an initial action. The nurse needs to create an environment that is safe for both parties. DIF: Cognitive Level: Applying OBJ: NCLEX: Safe and Effective Care Environment TOP: Integrated Process: Communication and Documentation 2. Which of the following pieces Nof information should be included in a hand-off to ensure patient safety? (Select all that apply.) a. Code status b. Recent changes in condition c. Age d. Family visitation e. Use of oxygen ANS: A, B, E It is important to include information on a patient’s background, assessment, nursing diagnosis, interventions (including the patient’s response), family information, discharge plans, and current priorities when handing off your patient to another unit or area. However, only code status, recent changes in patient’s condition, and use of oxygen directly impact patient safety. DIF: Cognitive Level: Applying OBJ: NCLEX: Safe and Effective Care Environment TOP: Integrated Process: Communication and Documentation 3. A faculty member is explaining personal factors that influence communication. What factors does the faculty member include? (Select all that apply.) a. Perceptions b. Values c. Emotions d. Relationships e. Pain ANS: A, B, C, D Although a patient’s pain may affect communication, it is not a personal factor as are perceptions, values, emotions, and relationships. DIF: Cognitive Level: Remembering OBJ: NCLEX: Safe and Effective Care Environment TOP: Integrated Process: Communication and Documentation N N Chapter 03: Documentation and Informatics Perry et al.: Nursing Interventions & Clinical Skills, 7th Edition MULTIPLE CHOICE 1. The nurse discovers a medication error on another nurse’s documentation, so the nurse completes an incident report. Which statement should the nurse include in the report? a. “Nurse mistakenly gave the wrong dose of medication for pain.” b. “Nurse gave incorrect dose of pain medication, but patient is all right.” c. “Morphine 10 mg IM given rather than morphine 5 mg IM as ordered.” d. “Physician will be notified of error when he makes rounds tomorrow.” ANS: C Stating that the patient received morphine 10 mg instead of 5 mg is a factual statement to include on an incident report because it is objective and provides no interpretation or conjecture from the nurse. The remaining choices are incorrect statements that do not accurately reflect what occurred. The physician needs to be notified as soon as the patient has been assessed, not the following day. DIF: Cognitive Level: Applying OBJ: NCLEX: Safe and Effective Care Environment TOP: Integrated Process: Communication and Documentation 2. The nurse is documenting the care of a patient. Which entry would be characteristic of charting by exception (CBE) as a documentation method? a. The patient needed to be turned every hour because of increasing pain. b. The patient’s vital signs are stable. c. The patient’s gait was steady with assistance from physical therapy. d. There was no odor when the dressing was removed. ANS: A CBE allows the nurse to specify exceptions to normal nursing assessments efficiently without documenting the normal assessment data and reducing the amount of narrative writing in patient documentation. The emphasis is on recording abnormal findings and trends in clinical care. It is a shorthand method for documenting based on defined standards for normal nursing assessments and interventions. CBE simply involves completing a flow sheet that incorporates these standards, thus minimizing the need for lengthy narrative notes. Increasing pain would not be expected and would be outside the “normal” or “expected.” DIF: Cognitive Level: Understanding OBJ: NCLEX: Safe and Effective Care Environment TOP: Integrated Process: Communication and Documentation 3. The nurse is documenting on a patient with a respiratory problem. Which patient datum documented by the nurse is the least objective? a. Cool and dusky skin b. Low flow rate oxygen c. 30 breaths per minute d. Very restless and drowsy ANS: B Low flow rate oxygen is the least objective datum and the datum most subject to interpretation because the quantity of oxygen is not as precise as “liters/minute” or the “percentage” of oxygen. The remaining options provide more verifiable data. DIF: Cognitive Level: Understanding OBJ: NCLEX: Safe and Effective Care Environment TOP: Integrated Process: Communication and Documentation 4. The nurse runs into a co-worker whose family friend is a patient on the unit. The co-worker asks about the friend’s health problems. Which is the correct response by the nurse? a. “Your friend told us to say nothing.” b. “Why don’t you ask your friend now?” c. “You know I can’t talk about the patients.” d. “Well, it was really a very difficult surgery.” ANS: C The nurse can’t talk about the co-worker’s friend or acknowledge the friend’s presence in the agency without breaching the friend’s right to privacy, so the nurse reminds the co-worker about confidentiality. DIF: Cognitive Level: Applying OBJ: NCLEX: Safe and Effective Care Environment TOP: Integrated Process: Communication and Documentation 5. The nurse is providing home care for a patient with an infection that is not improving. The patient refuses to see an infectious disease specialist. What should the nurse include in the documentation of the patient teaching provided? a. The discussion about the consequences of refusing to see a specialist and the patient’s response. b. The explanation that avoidiNng the specialist will most likely lead to a worse outcome. c. A hopeful explanation that this will most likely be the last medical specialist that the patient will need to see. d. The recommendation that the patient should discuss the decision with the family. ANS: A The nurse documents the discussion about the consequences of refusing to see a specialist and the patient’s response. Documenting the factual information presented about the risks of refusing treatment and the patient’s specific response to it (continued refusal to seek a specialist) are key pieces of information to include. The nurse should neither try to scare the patient into seeing the specialist nor provide false hope that only one consultation will be required. As long as the patient is competent to make a decision, the nurse must accept his or her choice. It is a requirement to document the facts surrounding that choice. DIF: Cognitive Level: Applying OBJ: NCLEX: Safe and Effective Care Environment TOP: Integrated Process: Communication and Documentation 6. At 0915 the nurse repeatedly instructs the patient to remain in bed. At 0930 the nurse enters the patient’s room, finds the patient on the floor, and hears the patient say, “I need pain medicine.” Which should the nurse do to document this event? a. Label the late entry using the time of 9:15 AM. b. Enclose the patient statement within quotations. c. Document completion of an incident report. d. Record plan to administer pain medication. ANS: B The nurse documents patient statements in quotations to indicate the patient’s precise statement. The nurse should document instructions given at 0915 and verify any indications of patient comprehension. A second entry noted at 0930 documents finding patient on floor. Completion of an incidence report is not documented in the patient record since it is an internal evaluation report. Administration of medication is only documented after it occurs to make sure that the documentation is accurate in terms of time and patient response. DIF: Cognitive Level: Applying OBJ: NCLEX: Safe and Effective Care Environment TOP: Integrated Process: Communication and Documentation 7. A nurse passes by a computer screen that has patient information that can be seen by visitors. What is the appropriate action for the nurse to take at this time? a. Leave the computer screen alone. b. Try to find the nurse caring for this patient. c. Document this situation on an incident report. d. Close the computer screen. ANS: D All agency staff have a responsibility to maintain patient confidentiality and should not leave a computer displaying patient information open. The nurse should minimize or close the computer screen so patient information cannot be seen by visitors. He or she should talk with the nurse caring for this patient about what happened. Incident reports are only filed when a patient experiences an adverse event. This situation does not require an incident report. DIF: Cognitive Level: ApplyingN OBJ: NCLEX: Safe and Effective Care Environment TOP: Integrated Process: Communication and Documentation 8. Nursing assistive personnel (NAP) finds a patient on the floor 30 minutes after the patient ambulated with physical therapy. What information should be charted by the NAP on the incident report? a. “Patient fell out of bed and landed on the floor.” b. “Patient found on floor. Upper side rails up. Bed in low position.” c. “Patient got dizzy and fell although ambulated with physical therapy earlier.” d. “Patient unfortunately slipped and fell.” ANS: B Documentation should state facts: “Patient found on floor. Upper side rails up. Bed in low position.” Only objective data with no interpretation can be documented by the NAP. The NAP does not evaluate the situation. Words such as “unfortunately” are never used in documentation. The NAP found the patient on the floor and did not see the patient slip and fall. DIF: Cognitive Level: Applying OBJ: NCLEX: Safe and Effective Care Environment TOP: Integrated Process: Communication and Documentation 9. An incident report is completed as a result of the pharmacy sending the wrong medication to the unit, even though the medication wasn’t administered. A student asks the nurse why this was needed. What response by the nurse is best? a. To make sure that the pharmacy was blamed for the error and not the nurse b. To help the pharmacy identify risks and prevent this situation from occurring again c. To prevent the hospital from a medical malpractice suit d. To get the health care provider’s attention about ordering medications ANS: B The incident report is a risk-management tool that enables health care providers to identify risks within an agency, analyze them, and act to reduce the risks and evaluate the results. This is also true when deviations from standards occur and not only when actual adverse events happen. Alerting the pharmacy to this type of error should help prevent it from occurring again. There was no problem with the health care provider’s order, only with how it was filled. DIF: Cognitive Level: Applying OBJ: NCLEX: Safe and Effective Care Environment TOP: Integrated Process: Communication and Documentation 10. The nursing staff have been using the SBAR format to structure communication for the past few months. Successful implementation of this system would be present if the nurse manager made which statement? a. “There are fewer omissions in patient care than before implementing this system.” b. “Fewer nurses are coming in late when they are scheduled to work.” c. “The medications are given on time now.” d. “The patient length of stay has decreased since last year.” ANS: A Noting fewer omissions in patient care would indicate successful implementation of the SBAR format. SBAR promotes the provision of safe, efficient, timely, and patient-centered communication. Staff timeliness, medication preparation, and length of patient stays are not affected by implementation of NSBAR. DIF: Cognitive Level: Evaluating OBJ: NCLEX: Safe and Effective Care Environment TOP: Nursing Process: Evaluation 11. The nursing staff are assisting nursing students in learning military time for documenting. Instruction by the nurses has been effective if the students identify that which entry reflects 40 minutes after midnight? a. 0040 b. 1240 c. 0004 d. 0400 ANS: A 0040 is 12:40 AM. 1240 is 12:40 PM. 0004 is 12:04 AM. 0400 is 4:00 AM. DIF: Cognitive Level: Understanding OBJ: NCLEX: Safe and Effective Care Environment TOP: Nursing Process: Evaluation 12. The following is an example of what part of the SBAR communication mnemonic? “Her blood pressure has decreased from 140/90 to 100/50 and she vomited 400 mL of bright red blood.” a. S b. A c. R d. B ANS: A This is an example of S-Situation—what is happening at the present time. Background (explain the circumstances leading up to the situation). Assessment (what you think the problem is). Recommendation (what you would do to correct the problem). DIF: Cognitive Level: Remembering OBJ: NCLEX: Safe and Effective Care Environment TOP: Integrated Process: Communication and Documentation MULTIPLE RESPONSE 1. Electronic health records (EHRs) can improve patient care. The following is an example of an alert in an EHR. (Select all that apply.) a. Notification of medication being overdue b. Change in patient’s blood pressure that exceeds parameters c. Order entered for a medication the patient is allergic to d. Routine lab orders e. Critical lab value ANS: A, B, C, E Alerts in EHRs notify nurses of critical changes in data that affect patient care and can be used to help nurses prioritize care. Overdue medications, critical lab values, and medication allergies are some of the examples of standard alerts. Alerts can also be tailored to patients to monitor for changes in their vital signs above certain parameters. When electronic health record alerts are used in the nurse’s practice, patient outcomes can be improved. DIF: Cognitive Level: Rememb Nering OBJ: NCLEX: Safe and Effective Care Environment TOP: Integrated Process: Communication and Documentation 2. The Joint Commission standards require all patients admitted to a health care agency to have the following documented. (Select all that apply.) a. Self-care assessment b. Discharge planning needs c. Environment assessment d. Physical assessment e. Religious practices ANS: A, B, C, D Current TJC (2012) standards require that all patients who are admitted to a health care agency have an assessment of physical, psychosocial, environmental, self-care, patient education, and discharge planning needs. Religious practices are not a specific assessment although it could be included in the psychosocial assessment. DIF: Cognitive Level: Remembering OBJ: NCLEX: Safe and Effective Care Environment TOP: Integrated Process: Communication and Documentation 3. The following is an excerpt of a discharge planning note. What elements of discharge planning are present in this example? (Select all that apply.) “Discussed learning about insulin injection technique. Patient will administer his own injection next time.” a. Measurable patient goal b. Progress toward goal c. Need for referral d. Discharge date ANS: A, B The information within a recorded entry must be complete, containing appropriate and essential information. There are criteria for thorough communication for certain health situations. For example, when recording discharge planning, measurable patient goals or expected outcomes, progress toward goals, and need for referrals are always included. DIF: Cognitive Level: Understanding OBJ: NCLEX: Safe and Effective Care Environment TOP: Integrated Process: Communication and Documentation 4. In a POMR charting method of documentation, which of the following items are used? (Select all that apply.) a. Progress notes b. Database c. Medical diagnosis d. Problem list e. Care plan ANS: A, B, D, E The problem-oriented medical record (POMR) is a structured method of documentation that emphasizes a patient’s problems. It is organized using the nursing process. Organization of data is by problem or diagnosis. Ideally each member of the health care team contributes to a single list of identified patient problems. Each recording includes a database, problem list, care plan, and progress notes. N DIF: Cognitive Level: Remembering OBJ: NCLEX: Safe and Effective Care Environment TOP: Integrated Process: Communication and Documentation Chapter 04: Patient Safety and Quality Improvement Perry et al.: Nursing Interventions & Clinical Skills, 7th Edition MULTIPLE CHOICE 1. The nurse is caring for an older patient who has a non–weight-bearing cast on the left lower extremity. The patient ambulates without using a walker despite repeated instruction from the nurse to call for assistance. Which response by the nurse is most likely to keep the patient from falling? a. Apply a vest restraint and offer frequent toileting. b. Plan fall prevention with patient, family, and health care provider. c. Inform family that the patient needs physical restraints. d. Document that the patient has a high potential for falling. ANS: B Planning an individualized fall prevention program with the help of the patient, family, and health care provider is more likely to reduce the patient’s risk of falls because the patient gains some control over the plan of care and still benefits from the input of the provider, family, and nurse. A combination of interventions is more useful in preventing falls. Including the patient in planning also gives him or her ownership of the plan, making it less likely the patient will disregard this plan. Restraints are associated with serious injuries and are not recommended for use unless nothing else has worked. Alternative methods of engaging the patient in a care plan that minimizes risks should be exhausted before resorting to restraints. Documenting the patient’s risk is important because it communicates the information and records the nurse’s acknowledgment of the risk, but it is not as effective as engaging the patient in planning care as a prevention technique becauNse it is indirect. DIF: Cognitive Level: Applying OBJ: NCLEX: Safe and Effective Care Environment TOP: Nursing Process: Planning 2. The nurse plans a fall prevention program for a confused patient. Which task from the program is suitable for the nurse to delegate to nursing assistive personnel (NAP)? a. Evaluating patient understanding of fall prevention plan b. Keeping the patient’s bed in the low position at all times c. Assessing the patient’s circulatory and respiratory status d. Instructing the patient’s family about alternatives to restraints ANS: B The nurse may delegate keeping the bed lowered to the NAP because the NAP is trained to perform the task with proper nursing supervision. Skills used to prevent falls can often be delegated. The nurse does not delegate the remaining options because they involve aspects of the nursing process that require the advanced training of a nurse to perform. DIF: Cognitive Level: Applying OBJ: NCLEX: Safe and Effective Care Environment TOP: Nursing Process: Planning 3. The nurse plans care for a patient who requires physical restraint. Which is a suitable goal for this patient? a. The patient remains free of any injury. b. The nurse checks the restraint every hour. c. The nurse uses the least restrictive restraint. d. The patient allows the nurse to apply restraints. ANS: A When restraints become necessary, the patient must remain free of injury; thus the nurse plans frequent neurovascular checks and removes the restraint on a regular basis to inspect the skin for pressure points and breakdown and perform range-of-motion exercises to maintain joint flexibility. Checking the restraint is a nursing intervention; it is not a goal because it is not patient centered. Using the least restrictive restraint can defeat the purpose of a restraint. When a restraint is required, the nurse uses the proper restraint to keep the patient safe and facilitate the therapeutic regimen. This is not a suitable goal because it focuses on the nurse. If the patient or staff members’ safety is at risk, the nurse applies restraints without the patient’s permission. DIF: Cognitive Level: Understanding OBJ: NCLEX: Safe and Effective Care Environment TOP: Nursing Process: Planning 4. The nurse applies a physical restraint to the patient. Which entry should the nurse make after applying the restraint? a. Performed restraint application reluctantly b. Applied bilateral soft lamb’s wool wrist restraints; skin pink, moist, and intact c. Will perform a neurovascular assessment every 4 hours d. Checked provider’s prescription for prn restraints ANS: B The nurse documents the type of restraint applied and the condition of the skin where the restraint was placed in the progress notes to communicate the information to the health care team. The nurse does not documNent subjective statements about the nurse. Neurovascular assessments of a patient’s extremity must take place at least every 2 hours because skin breakdown can occur very quickly. The nurse does not accept prn prescriptions for restraints according to nursing standards and federal regulations. DIF: Cognitive Level: Applying OBJ: NCLEX: Safe and Effective Care Environment TOP: Integrated Process: Communication and Documentation 5. The patient sustains a minor leg abrasion and stops breathing for a few seconds during a tonic-clonic seizure. Which is the best nursing documentation after the patient’s seizure? a. Type of muscle contractions b. Size and description of the abrasion c. Length of the patient’s apneic episode d. Description of the seizure in detail ANS: D Describing the seizure in detail is the best documentation after a seizure because it is the most comprehensive item listed and includes the type of muscle contractions observed during the seizure, the description of injuries, how the injuries occurred, and the description of any breathing abnormalities. DIF: Cognitive Level: Applying OBJ: NCLEX: Safe and Effective Care Environment TOP: Integrated Process: Communication and Documentation 6. A patient at risk for falling is being ambulated. Which action by the nurse is most important to prevent the patient from falling? a. Raising the bed to an appropriate working height b. Placing nonskid shoes on the patient c. Dangling the patient on the side of the bed for 10 minutes d. Turning on the brightest lights in the room ANS: B Placing nonskid surfaces on the patient’s feet helps to prevent falls. The height of the bed should be as low as possible before attempting to have the patient stand. Dangling prevents dizziness, but the length of time differs, and it is not required for all patients. Adequate light is important, but the brightest lights are not needed. DIF: Cognitive Level: Applying OBJ: NCLEX: Safe and Effective Care Environment TOP: Nursing Process: Implementation 7. The nurse is orienting a group of new nurses and explaining the concept of sentinel events and their causes. What should the nurse explain as a common root cause of all sentinel event? a. Medication errors b. Falls c. Communication failures d. High patient-to-nurse ratios ANS: C Communication failures are one of the most common root causes of all sentinel events. A sentinel event is an unexpected occurrence involving death, serious physical or psychological injury, or risk thereof. Although the other elements may cause sentinel events, they are not as frequent as communication failNures. DIF: Cognitive Level: Remembering OBJ: NCLEX: Safe and Effective Care Environment TOP: Integrated Process: Communication and Documentation 8. The nurse discovers smoke in the second-floor utility room. What intervention should he or she implement first? a. Find the fire extinguisher and try to extinguish the fire. b. Evacuate the entire second floor to the first-floor lobby. c. Rescue any patients, visitors, or staff in immediate danger. d. Pull the nearest alarm box and call the telephone operator. ANS: C The first step after identifying an actual or potential fire is to rescue victims at risk for injury from the fire, including patients, visitors, or staff, to reduce injuries from the fire. The second step is to activate the alarm. The third step is to contain the fire: find the extinguisher and empty the container onto the fire or source of the smoke. Finally the evacuation begins if the fire is uncontrolled or the smoke is excessive. This follows the acronym RACE. DIF: Cognitive Level: Remembering OBJ: NCLEX: Safe and Effective Care Environment TOP: Nursing Process: Implementation 9. The daughter of a patient tells the nurse that using the bathroom is embarrassing for the patient and she refuses to use a nurse call system when she needs to get up. Which is the best response by the nurse? a. Ask the patient why she does not use the nurse call system. b. Instruct the daughter to remain at the patient’s side. c. Tell the patient that getting up requires cooperation. d. Discuss nurse call system alternatives with patient and daughter. ANS: D Discussing nurse call system alternatives with the patient and daughter is the best method of engaging the patient in planning nursing care. This recognizes the patient as the source of control and full partner in providing compassionate and coordinated care based on respect for the patient’s preferences, values, and needs. Including the patient in planning alternatives also gives him or her ownership of the plan and increases the likelihood of cooperation. Asking a “why” question is not an ideal response because it is confrontational and requires the patient to justify feelings. Remaining with the patient is an impractical solution. DIF: Cognitive Level: Analyzing OBJ: NCLEX: Safe and Effective Care Environment TOP: Nursing Process: Implementation 10. Although the interdisciplinary team is responsible for the safety of the patient, who has the ultimate responsibility for making the patient’s bedside area safe? a. The nurse b. Housekeeping c. Nursing assistive personnel (NAP) d. The maintenance department ANS: A The nurse has the ultimate responsibility for making the patient’s bedside area safe. Other personnel assist with their specific roles, but the nurse oversees the safety. N DIF: Cognitive Level: Remembering OBJ: NCLEX: Safe and Effective Care Environment TOP: Nursing Process: Implementation 11. The nurse listens to a family’s request to bring a few familiar items into the room of a patient who is confused. What response by the nurse is best? a. No, because personal items can increase patient agitation. b. No, because personal items can create too much clutter. c. Yes, personal items are likely to restore cognitive function. d. Yes, personal items can comfort a confused person. ANS: D Personal items can comfort and calm a confused person because familiar items are part of the patient’s customary environment, patterns, and habits; in addition, these items personalize an otherwise strange environment and surround the patient with recognizable things. The personal items are likely to engage the patient but on their own do nothing to restore cognitive function. DIF: Cognitive Level: Analyzing OBJ: NCLEX: Safe and Effective Care Environment TOP: Nursing Process: Planning 12. The nurse plans a restraint-free environment but cannot find activities to engage an agitated middle-aged patient. Which should the nurse implement to maintain the patient’s safety? a. Request help from interdisciplinary team members. b. Transfer the patient to a private room to protect others. c. Document that the patient is uncooperative and hostile. d. Ask the health care provider for a sedation prescription. ANS: A A nurse’s expertise does not include all facets of health care, so the nurse collaborates with other experts to meet the patient’s safety and psychosocial needs. After assessing the patient, the experts make recommendations, and the nurse incorporates the activities into the patient’s plan of care. Putting the patient in a private room decreases the risk of injury to other patients; but it isolates the patient, increases the need for distraction, and increases the risks to the staff and patient. Documentation should always be descriptive and never judgmental. In this case the nurse would document the patient’s own words in quotation marks. Sedation increases the risk of falls from potential adverse effects, including hypotension, dizziness, and confusion. DIF: Cognitive Level: Applying OBJ: NCLEX: Safe and Effective Care Environment TOP: Nursing Process: Planning 13. A patient has been wandering and is at risk for falling. Which approach by the nurse regarding the use of chemical and physical restraints in the long-term care setting should be considered initially? a. Use nonprescription restraints first. b. Obtain with a telephone prescription. c. Implement alternative measures first. d. Notify patient’s family within 24 hours. ANS: C According to the standards governing the use of restraints, the nurse must implement several alternative measures in a serious attempt to avoid applying restraints. The patient must be assessed by the health care proNvider before restraints are implemented unless the patient is a serious and imminent risk to self and others. The patient’s family is notified in a timely manner but is not an initial consideration. DIF: Cognitive Level: Remembering OBJ: NCLEX: Safe and Effective Care Environment TOP: Nursing Process: Planning 14. The nurse plans a safety program for the patients on a medical-surgical unit. Which patient has the greatest likelihood of falling? a. A 79-year-old after a pacemaker battery replacement b. A 68-year-old anemic patient who is dehydrated and has heart failure c. A 21-year-old 2 hours postarthroscopy after a college football injury d. A 33-year-old patient post–right salpingectomy for ectopic pregnancy ANS: B The patient with anemia and dehydration with heart failure is the sickest patient and has the highest risk of falling. The patient will be taking other medications, including antihypertensive agents that increase the risk of falls caused by confusion, dizziness, or orthostatic hypotension. The replac [Show More]
Last updated: 1 year ago
Preview 1 out of 334 pages
Reviews( 0 )
Document information
Connected school, study & course
About the document
Uploaded On
Aug 29, 2022
Number of pages
334
Written in
Additional information
This document has been written for:
Uploaded
Aug 29, 2022
Downloads
0
Views
41


.png)
.png)