*NURSING > TEST BANK > NUR 3294 Essentials Exam 2 Review Questions and Answers Latest,100% CORRECT (All)
NUR 3294 Essentials Exam 2 Review Questions and Answers Latest,100% CORRECT
Document Content and Description Below
NUR 3294 Essentials Exam 2 Review Questions and Answers Latest Essentials Exam 2 Summer Chapters 24, 15, 16, 17, 6, 7, 10, 11, 12, 13, 14, 36, 37, 38 Chapter 24 1. When working with an older adul... t who is hearing-impaired, the use of which techniques would improve communication? (Select all that apply.) 1. Check for needed adaptive equipment. 2. Exaggerate lip movements to help the patient lip read. 3. Give the patient time to respond to questions. 4. Keep communication short and to the point. 5. Communicate only through written information. 2. Nurses must communicate effectively with the health care team for which of the following reasons? (Select all that apply.) 1. Improve the nurse's status with the health team members 2. Reduce the risk of errors to the patient 3. Provide optimum level of patient care 4. Improve patient outcomes 5. Prevent issues that need to be reported to outside agencies 3. A new nurse complains to her preceptor that she has no time for therapeutic communication with her patients. Which of the following is the best strategy to help the nurse find more time for this communication? 1. Include communication while performing tasks such as changing dressings and checking vital signs. 2. Ask the patient if you can talk during the last few minutes of visiting hours. 3. Ask Pastoral care to come back a little later in the day. 4. Remind the nurse to complete all her tasks and then set up remaining time for communication. 4. Motivational interviewing (MI) is a technique that applies understanding a patient's values and goals in helping the patient make behavior changes. What are other benefits of using MI techniques? (Select all that apply.) 1. Gaining an understanding of patient's motivations 2. Focusing on opportunities to avoid poor health choices 3. Recognizing patient's strengths and supporting their efforts 4. Providing assessment data that can be shared with families to promote change 5. Identifying differences in patient's health goals and current behaviors 5. A nurse is talking with a young-adult patient about the purpose of a new medication. The nurse says, “I want to be clear. Can you tell me in your words the purpose of this medicine?” This exchange is an example of which element of the transactional communication process? 1. Message 2. Obtaining feedback 3. Channel 4. Referent 6. A patient who is Spanish-speaking does not appear to understand the nurse's information on wound care. Which action should the nurse take? 1. Arrange for a Spanish-speaking social worker to explain the procedure 2. Ask a fellow Spanish-speaking patient to help explain the procedure 3. Use a professional interpreter to provide wound care education in Spanish 4. Ask the patient to write down questions that he or she has for the nurse 7. A nurse prepares to contact a patient's physician about a change in the patient's condition. Put the following statements in the correct order using SBAR (Situation, Background, Assessment, and Recommendation) communication. B 1. “She is a 53-year-old female who was admitted 2 days ago with pneumonia and was started on Levaquin at 5 PM yesterday. She complains of a poor appetite.” A 2. “The patient reported feeling very nauseated after her dose of Levaquin an hour ago.” R 3. “Would you like to make a change in antibiotics, or could we give her a nutritional supplement before her medication?” S 4. “The patient started complaining of nausea yesterday evening and has vomited several times during the night.” 8. A nurse is assigned to care for a patient for the first time and states, “I don't know a lot about your culture and want to learn how to better meet your health care needs.” Which therapeutic communication technique did the nurse use in this situation? 1. Validation 2. Empathy 3. Sarcasm 4. Humility 9. A new nurse is experiencing lateral violence at work. Which steps could the nurse take to address this problem? 1. Challenge the nurses in a public forum to embarrass them and change their behavior 2. Talk with the department secretary and ask if this has been a problem for other nurses 3. Talk with the preceptor or manager and ask for assistance in handling this issue 4. Say nothing and hope things get better 10. A nurse has been gathering physical assessment data on a patient and is now listening to the patient's concerns. The nurse sets a goal of care that incorporates the patient's desire to make treatment decisions. This is an example of the nurse engaged in which phase of the nurse-patient relationship? 1. Working phase 2. Preinteraction phase 3. Termination phase 4. Orientation phase 11. A patient is evaluated in the emergency department after causing an automobile accident while being under the influence of alcohol. While assessing the patient, which statement would be the most therapeutic? 1. “Why did you drive after you had been drinking?” 2. “We have multiple patients to see tonight as a result of this accident.” 3. “Tell me what happened before, during, and after the automobile accident tonight.” 4. “It will be okay. No one was seriously hurt in the accident.” 12. A nursing student is reviewing a process recording with the instructor. The student engaged the patient in a discussion about availability of family members to provide support at home once the patient is discharged. The student reviews with the instructor whether the comments used encouraged openness and allowed the patient to “tell his story.” This is an example of which step of the nursing process? 1. Planning 2. Assessment 3. Intervention 4. Evaluation 13. Which strategies should a nurse use to facilitate a safe transition of care during a patient's transfer from the hospital to a skilled nursing facility? (Select all that apply.) 1. Collaboration between staff members from sending and receiving departments 2. Requiring that the patient visit the facility before a transfer is arranged 3. Using a standardized transfer policy and transfer tool 4. Arranging all patient transfers during the same time each day 5. Relying on family members to share information with the new facility 15. The nurse uses silence as a therapeutic communication technique. What is the purpose of the nurse's silence? (Select all that apply.) 1. Prevent the nurse from saying the wrong thing 2. Prompt the patient to talk when he or she is ready 3. Allow the patient time to think and gain insight 4. Allow time for the patient to drift off to sleep 5. Determine if the patient would prefer to talk with another staff member Chapter 15 1. Two patient deaths have occurred on a medical unit in the last month. The staff notices that everyone feels pressured and team members are getting into more arguments. As a nurse on the unit, what will best help you manage this stress? 1. Keep a journal 2. Participate in a unit meeting to discuss feelings about the patient deaths 3. Ask the nurse manager to assign you to less difficult patients 4. Review the policy and procedure manual on proper care of patients after death 2. A nurse has seen many cancer patients struggle with pain management because they are afraid of becoming addicted to the medicine. Pain control is a priority for cancer care. By helping patients focus on their values and beliefs about pain control, a nurse can best make clinical decisions. This is an example of: 1. Creativity. 2. Fairness. 3. Clinical reasoning. 4. Applying ethical criteria. 3. A nurse prepares to insert a Foley catheter. The procedure manual calls for the patient to lie in the dorsal recumbent position. The patient complains of having back pain when lying on her back. Despite this, the nurse positions the patient supine with knees flexed as the manual recommends and begins to insert the catheter. This is an example of: 1. Accuracy. 2. Reflection. 3. Risk taking. 4. Basic critical thinking. 4. A nurse is preparing medications for a patient. The nurse checks the name of the medication on the label with the name of the medication on the doctor's order. At the bedside the nurse checks the patient's name against the medication order as well. The nurse is following which critical thinking attitude: 1. Responsible 2. Complete 3. Accurate 4. Broad 5. A nurse on a busy medicine unit is assigned to four patients. It is 10 AM. Two patients have medications due and one of those has a specimen of urine to be collected. One patient is having complications from surgery and is being prepared to return to the operating room. The fourth patient requires instructions about activity restrictions before going home this afternoon. Which of the following should the nurse use in making clinical decisions appropriate for the patient group? (Select all that apply.) 1. Consider availability of assistive personnel to obtain the specimen 2. Combine activities to resolve more than one patient problem 3. Analyze the diagnoses/problems and decide which are most urgent based on patients' needs 4. Plan a family conference for tomorrow to make decisions about resources the patient will need to go home 5. Identify the nursing diagnoses for the patient going home 6. By using known criteria in conducting an assessment such as reviewing with a patient the typical characteristics of pain, a nurse is demonstrating which critical thinking attitude? 1. Curiosity 2. Adequacy 3. Discipline 4. Thinking independently 7. A nurse just started working at a well-baby clinic. One of her recent experiences was to help a mother learn the steps of breastfeeding. During the first clinic visit the mother had difficulty positioning the baby during feeding. After the visit the nurse considers what affected the inability of the mother to breastfeed, including the mother's obesity and inexperience. The nurse's review of the situation is called: 1. Reflection. 2. Perseverance. 3. Intuition. 4. Problem solving. 8. Place the steps of the scientific method in their correct order with number 1 being the first step of the process. 3 1. Formulate a question or hypothesis. 5 2. Evaluate results of the study. 2 3. Collect data. 1 4. Identify the problem. 4 5. Test the question or hypothesis. 9. A nurse changed a patient's surgical wound dressing the day before and now prepares for another dressing change. The nurse had difficulty removing the gauze from the wound bed yesterday, causing the patient discomfort. Today he gives the patient an analgesic 30 minutes before the dressing change. Then he adds some sterile saline to loosen the gauze for a few minutes before removing it. The patient reports that the procedure was much more comfortable. Which of the following describes the nurse's approach to the dressing change? (Select all that apply.) 1. Clinical inference 2. Basic critical thinking 3. Complex critical thinking 4. Experience 5. Reflection 10. Which of the following describes a nurse's application of a specific knowledge base during critical thinking? (Select all that apply.) 1. Initiative in reading current evidence from the literature 2. Application of nursing theory 3. Reviewing policy and procedure manual 4. Considering holistic view of patient needs 5. Previous time caring for a specific group of patients 11. Fill in the Blank. When a nurse tries to understand a patient's and family caregiver's perspective of why a patient is falling at home, the nurse applies the intellectual standard of Broad to understand all viewpoints. 12. An aspect of clinical decision making is knowing the patient. Which of the following is the most critical aspect of developing the ability to know the patient? 1. Working in multiple health care settings 2. Learning good communication skills 3. Spending time establishing relationships with patients 4. Relying on evidence in practice 13. In which of the following examples is a nurse applying critical thinking skills in practice? (Select all that apply.) 1. The nurse thinks back about a personal experience before administering a medication subcutaneously. 2. The nurse uses a pain-rating scale to measure a patient's pain. 3. The nurse explains a procedure step by step for giving an enema to a patient care technician. 4. The nurse gathers data on a patient with a mobility limitation to identify a nursing diagnosis. 5. A nurse offers support to a colleague who has witnessed a stressful event. 14. A nurse enters a 72-year-old patient's home and begins to observe her behaviors and examine her physical condition. The nurse learns that the patient lives alone and notices bruising on the patient's leg. When watching the patient walk, the nurse notes that she has an unsteady gait and leans to one side. The patient admits to having fallen in the past. The nurse identifies the patient as having the nursing diagnosis of Risk for Falls. This scenario is an example of: 1. Inference. 2. Basic critical thinking. 3. Evaluation. 4. Diagnostic reasoning. 15. Match the concepts for a critical thinker on the right with the application of the term on the left. Truth seeking (Be objective in asking questions of a patient) Open-mindedness (Be tolerant of the patient's views and beliefs) Analyticity (Anticipate how a patient might respond to a treatment) Systematicity (Organize assessment on the basis of patient priorities) Chapter 16 1. Which of the following examples are steps of nursing assessment? (Select all that apply.) 1. Collection of information from patient's family members 2. Recognition that further observations are needed to clarify information 3. Comparison of data with another source to determine data accuracy 4. Complete documentation of observational information 5. Determining which medications to administer based on a patient’s assessment data 2. A nurse assesses a patient who comes to the pulmonary clinic. “I see that it's been over 6 months since you've been here, but your appointment was for every 2 months. Tell me about that. Also I see from your last visit that the doctor recommended routine exercise. Can you tell me how successful you've been in following his plan?” The nurse's assessment covers which of Gordon's functional health patterns? 1. Value-belief pattern 2. Cognitive-perceptual pattern 3. Coping–stress-tolerance pattern 4. Health perception–health management pattern 3. When a nurse conducts an assessment, data about a patient often comes from which of the following sources? (Select all that apply.) 1. An observation of how a patient turns and moves in bed 2. The unit policy and procedure manual 3. The care recommendations of a physical therapist 4. The results of a diagnostic x-ray film 5. Your experiences in caring for other patients with similar problems 4. The nurse observes a patient walking down the hall with a shuffling gait. When the patient returns to bed, the nurse checks the strength in both of the patient's legs. The nurse applies the information gained to suspect that the patient has a mobility problem. This conclusion is an example of: 1. Cue. 2. Reflection. 3. Clinical inference. 4. Probing. 5. A 72-year-old male patient comes to the health clinic for an annual follow-up. The nurse enters the patient's room and notices him to be diaphoretic, holding his chest and breathing with difficulty. The nurse immediately checks the patient's heart rate and blood pressure and asks him, “Tell me where your pain is.” Which of the following assessment approaches does this scenario describe? 1. Review of systems approach 2. Use of a structured database format 3. Back channeling 4. A problem-oriented approach 6. The nurse asks a patient, “Describe for me a typical night's sleep. What do you do to fall asleep? Do you have difficulty falling or staying asleep? This series of questions would likely occur during which phase of a patient-centered interview? 1. Orientation 2. Working phase 3. Data validation 4. Termination 7. A nurse is assigned to a 42-year-old mother of 4 who weighs 136.2 kg (300 lbs), has diabetes, and works part time in the kitchen of a restaurant. The patient is facing surgery for gallbladder disease. Which of the following approaches demonstrates the nurse's cultural competence in assessing the patient's health care problems? 1. “I can tell that your eating habits have led to your diabetes. Is that right?” 2. “It's been difficult for people to find jobs. Is that why you work part time?” 3. “You have four children; do you have any concerns about going home and caring for them?” 4. “I wish patients understood how overeating affects their health.” 8. Which type of interview question does the nurse first use when assessing the reason for a patient seeking health care? 1. Probing 2. Open-ended 3. Problem-oriented 4. Confirmation 9. A nurse gathers the following assessment data. Which of the following cues together form(s) a pattern suggesting a problem? (Select all that apply.) 1. The skin around the wound is tender to touch. 2. Fluid intake for 8 hours is 800 mL. 3. Patient has a heart rate of 78 beats/min and regular. 4. Patient has drainage from surgical wound. 5. Body temperature is 38.3° C (101° F). 6. Patient states, “I'm worried that I won't be able to return to work when I planned.” 10. A nurse is checking a patient's intravenous line and, while doing so, notices how the patient bathes himself and then sits on the side of the bed independently to put on a new gown. This observation is an example of assessing: 1. Patient's level of function. 2. Patient's willingness to perform self-care. 3. Patient's level of consciousness. 4. Patient's health management values. 11. A nurse makes the following statement during a change-of-shift report to another nurse. “I assessed Mr. Diaz, my 61-year-old patient from Chile. He fell at home and hurt his back 3 days ago. He has some difficulty turning in bed, and he says that he has pain that radiates down his leg. He rates his pain at a 6, and he moves slowly as he transfers to a chair.” What can the nurse who is beginning a shift do to validate the previous nurse's assessment findings when she conducts rounds on the patient? (Select all that apply.) 1. The nurse asks the patient to rate his pain on a scale of 0 to 10. 2. The nurse asks the patient what caused his fall. 3. The nurse asks the patient if he has had pain in his back in the past. 4. The nurse assesses the patient's lower-limb strength. 5. The nurse asks the patient what pain medication is most effective in managing his pain. 12. A patient who visits the surgery clinic 4 weeks after a traumatic amputation of his right leg tells the nurse practitioner that he is worried about his ability to continue to support his family. He tells the nurse he feels that he has let his family down after having an auto accident that led to the loss of his left leg. The nurse listens and then asks the patient, “How do you see yourself now?” On the basis of Gordon's functional health patterns, which pattern does the nurse assess? 1. Health perception–health management pattern 2. Value-belief pattern 3. Cognitive-perceptual pattern 4. Self-perception–self-concept pattern 13. A nurse is conducting a patient-centered interview. Place the statements from the interview in the correct order, beginning with the first statement a nurse would ask. “My name is Todd. I'll be the nurse taking care of you today. I'm going to ask you a series of questions to gather your health history.”, “Tell me what brought you to the hospital.”, “You say you've lost weight. Tell me how much weight you've lost in the last month.”, “So, to summarize, you've lost about 6 lbs in the last month, and your appetite has been poor—correct?”, “I have no further questions. Thank you for your patience.” 14. During a visit to the clinic, a patient tells the nurse that he has been having headaches on and off for a week. The headaches sometimes make him feel nauseated. Which of the following responses by the nurse is an example of probing? 1. So you've had headaches periodically in the last week and sometimes they cause you to feel nauseated— correct? 2. Have you taken anything for your headaches? 3. Tell me what makes your headaches begin. 4. Uh huh, tell me more. 15. The nurse enters the room of an 82-year-old patient for whom she has not cared previously. The nurse notices that the patient wears a hearing aid. The patient looks up as the nurse approaches the bedside. Which of the following approaches are likely to be effective with an older adult? (Select all that apply.) 1. Listen attentively to the patient's story. 2. Use gestures that reinforce your questions or comments. 3. Stand back away from the bedside. 4. Maintain direct eye contact. 5. Ask questions quickly to reduce the patient's fatigue. Chapter 17 2. Review the following problem-focused nursing diagnoses and identify the diagnoses that are stated correctly. (Select all that apply.) 1. Impaired Skin Integrity related to physical immobility 2. Fatigue related to heart disease 3. Nausea related to gastric distention 4. Need for improved Oral Mucosa Integrity related to inflamed mucosa 5. Risk for Infection related to surgery 3. A nurse reviews data gathered regarding a patient's ability to cope with loss. The nurse compares the defining characteristics for Ineffective Coping with those for Readiness for Enhanced Coping and selects Ineffective Coping as the correct diagnosis. This is an example of the nurse avoiding an error in: (Select all that apply.) 1. Data collection. 2. Data clustering. 3. Data interpretation. 4. Making a diagnostic statement. 5. Goal setting. 4. The nursing diagnosis Impaired Parenting related to mother's developmental delay is an example of a(n): 1. Risk nursing diagnosis. 2. Problem-focused nursing diagnosis. 3. Health promotion nursing diagnosis. 4. Wellness nursing diagnosis. 5. A nurse interviewed and conducted a physical examination of a patient. Among the assessment data the nurse gathered were an increased respiratory rate, the patient reporting difficulty breathing while lying flat, and pursed-lip breathing. This data set is an example of: 1. Collaborative data set. 2. Diagnostic label. 3. Related factors. 4. Data cluster. 6. In which of the following examples are nurses making diagnostic errors? (Select all that apply.) 1. The nurse who observes a patient wincing and holding his left side and gathers no additional assessment data 2. The nurse who measures joint range of motion after the patient reports pain in the left elbow 3. The nurse who considers conflicting cues in deciding which diagnostic label to choose 4. The nurse who identifies a diagnosis on the basis of a patient reporting difficulty sleeping 5. The nurse who makes a diagnosis of Ineffective Airway Clearance related to pneumonia. 7. A nurse is reviewing a patient's list of nursing diagnoses in the medical record. The most recent nursing diagnosis is Diarrhea related to intestinal colitis. For which of the following reasons is this an incorrectly stated diagnostic statement? 1. Identifying the clinical sign instead of an etiology 2. Identifying a diagnosis on the basis of prejudicial judgment 3. Identifying the diagnostic study rather than a problem caused by the diagnostic study 4. Identifying the medical diagnosis instead of the patient's response to the diagnosis. 8. A nurse is assigned to a new patient admitted to the nursing unit following admission through the emergency department. The nurse collects a nursing history and interviews the patient. Place the following steps for making a nursing diagnosis in the correct order, beginning with the first step. 1 Reviews assessment data, noting objective and subjective clinical information, 2 Clusters clinical cues that form a pattern, 3 Chooses diagnostic label, 4 Considers context of patient's health problem and selects a related factor 9. A nursing student reports to a lead charge nurse that his assigned patient seems to be less alert and his blood pressure is lower, dropping from 140/80 to 110/60. The nursing student states, “I believe this is a nursing diagnosis of Deficient Fluid Volume.” The lead charge nurse immediately goes to the patient's room with the student to assess the patient's orientation, heart rate, skin turgor, and urine output for last 8 hours. The lead charge nurse suspects that the student has made which type of diagnostic error? 1. Insufficient cluster of cues 2. Disorganization 3. Insufficient number of cues 4. Evidence that another diagnosis is more likely 10. A nurse in a mother-baby clinic learns that a 16-year-old has given birth to her first child and has not been to a well-baby class yet. The nurse's assessment reveals that the infant cries when breastfeeding and has difficulty latching on to the nipple. The infant has not gained weight over the last 2 weeks. The nurse identifies the patient's nursing diagnosis as Ineffective Breastfeeding. Which of the following is the best “related to” factor? 1. Infant crying at breast 2. Infant unable to latch on to breast correctly 3. Mother's deficient knowledge 4. Lack of infant weight gain 11. A nurse is getting ready to assess a patient in a neighborhood community clinic. He was newly diagnosed with diabetes just a month ago. He has other health problems and a history of not being able to manage his health. Which of the following questions reflects the nurse's cultural competence in making an accurate diagnosis? (Select all that apply.) 1. How is your diabetic diet affecting you and your family? 2. You seem to not want to follow health guidelines. Can you explain why? 3. What worries you the most about having diabetes? 4. What do you expect from us when you do not take your insulin as instructed? 5. What do you believe will help you control your blood sugar? 12. A nurse assesses a young woman who works part time but also cares for her mother at home. The nurse reviews clusters of data that include the patient's report of frequent awakenings at night, reduced ability to think clearly at work, and a sense of not feeling well rested. Which of the following diagnoses is in the correct PES format? 1. Disturbed Sleep Pattern evidenced by frequent awakening 2. Disturbed Sleep Pattern related to family caregiving responsibilities 3. Disturbed Sleep Pattern related to need to improve sleep habits 4. Disturbed Sleep Pattern r/t caregiving responsibilities as evidenced by frequent awakening and not feeling rested 13. A nursing student is working with a faculty member to identify a nursing diagnosis for an assigned patient. The student has assessed that the patient is undergoing radiation treatment and has had liquid stool and the skin is clean and intact; therefore she selects the nursing diagnosis Impaired Skin Integrity. The faculty member explains that the student has made a diagnostic error for which of the following reasons? 1. Incorrect clustering 2. Wrong diagnostic label 3. Condition is a collaborative problem. 4. Premature closure of clusters 14. The use of standard formal nursing diagnostic statements serves several purposes in nursing practice, including which of the following? (Select all that apply.) 1. Defines a patient's problem, giving members of the health care team a common language for understanding the patient's needs 2. Allows physicians and allied health staff to communicate with nurses how they provide care among themselves 3. Helps nurses focus on the scope of nursing practice 4. Creates practice guidelines for collaborative health care activities 5. Builds and expands nursing knowledge 15. Which of the following nursing diagnoses is stated correctly? (Select all that apply.) 1. Fluid Volume Excess related to heart failure 2. Sleep Deprivation related to sustained noisy environment 3. Impaired Bed Mobility related to postcardiac catheterization 4. Ineffective Protection related to inadequate nutrition 5. Diarrhea related to frequent, small, watery stools. Chapter 6 1. A nurse is presenting a program to workers in a factory covering safety topics, including the wearing of hearing protectors when workers are in the factory. Which level of prevention is the nurse practicing? 1. Primary prevention 2. Secondary prevention 3. Tertiary prevention 4. Quaternary prevention 2. A patient had surgery for a total knee replacement a week ago and is currently participating in daily physical rehabilitation sessions at the surgeon's office. In what level of prevention is the patient participating? 1. Primary prevention 2. Secondary prevention 3. Tertiary prevention 4. Quaternary prevention 3. Based on the transtheoretical model of change, what is the most appropriate response to a patient who states: “Me, stop smoking? I've been smoking since I was 16!” 1. “That's fine. Some people who smoke live a long life.” 2. “OK. I want you to decrease the number of cigarettes you smoke by one each day, and I'll see you in 1 month.” 3. “I understand. Can you think of the greatest reason why stopping smoking would be challenging for you?” 4. “I'd like you to attend a smoking cessation class this week and use nicotine replacement patches as directed.” 4. A patient comes to the local health clinic and states: “I've noticed how many people are out walking in my neighborhood. Is walking good for you?” What is the best response to help the patient through the stages of change for exercise? 1. “Walking is OK. I really think running is better.” 2. “Yes, walking is great exercise. Do you think you could go for a 5-minute walk next week?” 3. “Yes, I want you to begin walking. Walk for 30 minutes every day and start to eat more fruits and vegetables.” 4. “They probably aren't walking fast enough or far enough. You need to spend at least 45 minutes if you are going to do any good.” 5. A male patient has been laid off from his construction job and has many unpaid bills. He is going through a divorce from his marriage of 15 years and has been seeing his pastor to help him through this difficult time. He does not have a primary health care provider because he has never really been sick and his parents never took him to a physician when he was a child. Which external variables influence the patient's health practices? (Select all that apply.) 1. Difficulty paying his bills 2. Seeing his pastor as a means of support 3. Age of patient (46 years) 4. Stress from the divorce and the loss of a job 5. Family practice of not routinely seeing a health care provider 6. A nurse is conducting a home visit with an older-adult couple. While in the home the nurse weighs each individual and reviews the 3-day food diary with them. She also checks their blood pressure and encourages them to increase their fluids and activity levels to help with their voiced concern about constipation. The nurse is addressing which level of need according to Maslow? 1. Physiological 2. Safety and security 3. Love and belonging 4. Self-actualization 7. When taking care of patients, a nurse routinely asks if they take any vitamins or herbal medications, encourages family members to bring in music that the patient likes to help the patient relax, and frequently prays with her patients if that is important to them. The nurse is practicing which model? 1. Holistic 2. Health belief 3. Transtheoretical 4. Health promotion 8. Using the Transtheoretical Model of Change, order the steps that a patient goes through to make a lifestyle change related to physical activity. 1 The individual becomes angry when the physician tells him that he needs to increase his activity to lose 30 lbs., 2 The individual recognizes that he is out of shape when his daughter asks him to walk with her after school., 3 The individual visits the local running store to purchase walking shoes and obtain advice on a walking plan., 4 The individual walks 2 to 3 miles, 5 nights a week, with his wife., 5 Eight months after beginning walking, the individual participates with his wife in a local 5K race. 9. Which statement made by a nurse shows that the nurse is engaging in an activity to help cope with secondary traumatic stress and burnout? 1. “I don't need time for lunch since I am not very hungry.” 2. “I am enjoying my quilting group that meets each week at my church.” 3. “I am going to drop my gym membership because I don't have time to go.” 4. “I don't know any of the other nurses who met today to discuss hospital-wide problems with nurse satisfaction.” 10. Which of the following are symptoms of secondary traumatic stress and burnout that commonly affect nurses? (Select all that apply.) 1. Regular participation in a book club 2. Lack of interest in exercise 3. Difficulty falling asleep 4. Lack of desire to go to work 5. Anxiety while working 11. After a class on Pender's health promotion model, students make the following statements. Which statement does the faculty member need to clarify? 1. “The desired outcome of the model is health-promoting behavior.” 2. “Perceived self-efficacy is not related to the model.” 3. “The individual has unique characteristics and experiences that affect his or her actions.” 4. “Patients need to commit to a plan of action before they adopt a health-promoting behavior.” 12. A patient registered at the local fitness center and purchased a pair of exercise shoes. The patient is in what stage of behavioral change? 1. Precontemplation 2. Contemplation 3. Preparation 4. Action 13. As part of a faith community nursing program in her church, a nurse is developing a health promotion program on breast self-examination for the women's group. Which statement made by one of the participants is related to the individual's perception of susceptibility to an illness? 1. “I have a door hanging tag in my bathroom to remind me to do my breast self-examination monthly.” 2. “Since my mother had breast cancer, I know that I am at increased risk for developing breast cancer.” 3. “Since I am only 25 years of age, the risk of breast cancer for me is very low.” 4. “I participate every year in our local walk/run to raise money for breast cancer research.” 14. The nurse assesses the following risk factors for coronary artery disease (CAD) in a female patient. Which factors are classified as genetic and physiological? (Select all that apply.) 1. Sedentary lifestyle 2. Mother died from CAD at age 48 3. History of hypertension 4. Eats diet high in sodium 5. Elevated cholesterol level 15. Which activity shows a nurse engaged in primary prevention? 1. A home health care nurse visits a patient's home to change a wound dressing. 2. A nurse is assessing risk factors of a patient in the emergency department admitted with chest pain. 3. A school health nurse provides a program to the first-year students on healthy eating. 4. A nurse schedules a patient who had a myocardial infarction for cardiac rehabilitation sessions weekly. Chapter 7 1. A nurse hears a colleague tell a nursing student that she never touches a patient unless she is performing a procedure or doing an assessment. The nurse tells the student that from a caring perspective: 1. She does not touch the patients either. 2. Touch is a type of verbal communication. 3. Touch is only used when a patient is in pain. 4. Touch forms a connection between nurse and patient. 2. Of the five caring processes described by Swanson, which describes “knowing the patient?” 1. Anticipating the patient's cultural preferences 2. Determining the patient's physician preference 3. Establishing an understanding of a specific patient 4. Gathering task-oriented information during assessment 3. A Muslim woman enters the clinic to have a woman's health examination for the first time. Which nursing behavior applies Swanson's caring process of “knowing the patient?” 1. Sharing feelings about the importance of having regular woman's health examinations 2. Gaining an understanding of what a woman's health examination means to the patient 3. Recognizing that the patient is modest; and obtaining gender-congruent caregiver 4. Explaining the risk factors for cervical cancer 4. Fill-in-the-Blank. Swanson's caring process of _enabling is demonstrated by a nurse helping a new mother through the birthing experience. 5. A patient is fearful of upcoming surgery and a possible cancer diagnosis. He discusses his love for the Bible with his nurse, who recommends a favorite Bible verse. Another nurse tells the patient's nurse that there is no place in nursing for spiritual caring. The patient's nurse replies: 1. “You're correct; spiritual care should be left to a pastoral care professional.” 2. “You're correct; religion is a personal decision.” 3. “Nurses should explain their own religious beliefs to patients.” 4. “Spiritual, mind, and body connections can affect health.” 6. Which of the following is a strategy for creating work environments that enable nurses to demonstrate more caring behaviors? (Select all that apply.) 1. Decreasing the number of consecutive shifts of the nursing staff 2. Increasing salary and vacation benefits of the nursing staff 3. Increasing the number of nurses who work each shift to decrease the nurse-patient ratio 4. Encouraging increased input concerning nursing functions from health care providers 5. Providing nursing staff an opportunity to discuss practice changes they can implement to enhance opportunities for patient caring 7. When a nurse helps a patient find the meaning of cancer by supporting beliefs about life, this is an example of: 1. Instilling hope and faith. 2. Forming a human-altruistic value system. 3. Cultural caring. 4. Being with. 8. An example of a nurse caring behavior that families of acutely ill patients perceive as important to patients' well-being is: 1. Making health care decisions for patients. 2. Having family members provide a patient's total personal hygiene. 3. Injecting the nurse's perceptions about the level of care provided. 4. Asking permission before performing a procedure on a patient. 9. A nurse demonstrated caring by helping family members to: (Select all that apply.) 1. Become active participants in care. 2. Remove themselves from personal care. 3. Make health care decisions for the patient. 4. Have uninterrupted time for family and patient to be together. 5. Have opportunities for the family to discuss their concerns. 10. Listening is not only “taking in” what a patient says, but it also includes: 1. Incorporating the views of the physician. 2. Correcting any errors in the patient's understanding. 3. Injecting the nurse's personal views and statements. 4. Interpreting and understanding what the patient means. 11. A nurse is caring for an older adult who needs to enter an assisted-living facility following discharge from the hospital. Which of the following is an example of listening that displays caring? 1. The nurse encourages the patient to talk about his concerns while reviewing the computer screen in the room. 2. The nurse sits at the patient's bedside, listens as he relays his fear of never seeing his home again, and then asks if he wants anything to eat. 3. The nurse listens to the patient's story while sitting on the side of the bed and then summarizes the story. 4. The nurse listens to the patient talk about his fears of not returning home and then tells him to think positively. 12. Presence involves a person-to-person encounter that: 1. Enables patients to care for self. 2. Provides personal care to a patient. 3. Conveys a closeness and a sense of caring. 4. Describes being in close contact with a patient. 13. A nurse enters a patient's room, arranges the supplies for a Foley catheter insertion, and explains the procedure to the patient. She tells the patient what to expect; just before inserting the catheter, she tells the patient to relax and that, once the catheter is in place, she will not feel the bladder pressure. The nurse then proceeds to skillfully insert the Foley catheter. This is an example of what type of touch? 1. Caring touch 2. Protective touch 3. Task-oriented touch 4. Interpersonal touch 14. A hospice nurse sits at the bedside of a male patient in the final stages of cancer. He and his parents made the decision that he would move home and they would help him in the final stages of his disease. The family participates in his care, but lately the nurse has increased the amount of time she spends with the family. Whenever she enters the room or approaches the patient to give care, she touches his shoulder and tells him that she is present. This is an example of what type of touch? 1. Caring touch 2. Protective touch 3. Task-oriented touch 4. Interpersonal touch 15. Match the following caring behaviors with their definitions. b. Striving to understand an event as meaning for another person 1. Knowing c. Being emotionally there for another person 2. Being with d. Providing for another as he or she would do for themselves 3. Doing for a. Sustaining faith in one's capacity to get through a situation 4. Maintaining belief Chapter 10 1. The Collins family includes a mother; stepfather, two teenage biological daughters of the mother; and a 25- year-old biological daughter of the father. The father's daughter just moved home following the loss of her job in another city. The family is converting a study into Stacey's bedroom and is in the process of distributing household chores. When you talk to members of the family, they all think that their family can adjust to lifestyle changes. This is an example of family: 1. Diversity. 2. Durability. 3. Resiliency. 4. Configuration. 2. What is the most common reason for calling on grandparents to raise their grandchildren? 1. Single parenthood 2. Legal interventions 3. Dual-income families 4. Increased divorce rate 3. Which of the following most greatly affects a family's access to adequate health care, opportunity for education, and sound nutrition? 1. Development 2. Family function 3. Family structure 4. Economic stability 4. You are caring for a family that consists of a father and 3-year-old boy who has well-managed asthma but misses care infrequently. They live in state-supported housing. The father is in school studying to be an information technology professional. His income and time are limited, and he admits to going to fast-food restaurants frequently for dinner. However, he and his son spend a lot of time together. The family receives state-supported health care for his son, but he does not have health insurance or a personal physician. He has his son enrolled in a government-assisted day care program. Which of the following are risks to this family's level of health? (Select all that apply.) 1. Economic status 2. Chronic illness 3. Underinsured 4. Government-assisted day care 5. Frequency of fast-food dinners 6. State-supported housing 5. Which of the following family assessments are most important for successful family caregiving? (Select all that apply.) 1. Educational level of family members 2. Cultural food preferences 3. Collaboration between family members 4. Social support 5. Conflict resolution practices 6. Which of the following are possible outcomes with clear family communication? (Select all that apply.) 1. Family goals 2. Increased socialization 3. Decision making 4. Methods of discipline 5. Improved education 6. Impaired coping 7. A family has decided to care for a grandparent with terminal cancer in the daughter's home. Family caregiving is new to the family. When helping this family as they begin to plan for their caregiving roles, what are the two top priority assessments to best learn about family functioning? (Select all that apply.) 1. Communication 2. Decision making 3. Development 4. Economic status 5. Family structure 8. A family is facing job loss of the father, who is the major wage earner, and relocation to a new city where there is a new job. The children will have to switch schools, and his wife will have to resign from the job she likes. Which of the following contribute to this family's hardiness? (Select all that apply.) 1. Family meetings 2. Established family roles 3. New neighborhood 4. Willingness to change in time of stress 5. Passive orientation to life 9. A family is undergoing a major change. Just as twins graduate from college and leave home to begin their careers, the husband loses his executive well-paying job. Because the family had two children in college at the same time, they did not save for retirement. They planned to save aggressively after the children left college. In this situation, which of the following demonstrate family resiliency? (Select all that apply.) 1. Resuming full-time work when spouse loses job 2. Increasing problems among siblings 3. Developing hobbies when children leave home 4. Placing blame on family members 5. Expecting children to help financially 6. Consulting a financial planner 10. In viewing the family as context, what is the primary focus? 1. Family members within a system 2. Family process and relationships 3. Family relational and transactional concepts 4. Health needs of an individual member 11. A hospice nurse is caring for a family that is providing end-of-life care for their grandmother, who has terminal breast cancer. When the nurse visits, the focus is on symptom management for the grandmother and helping the family with coping skills. This approach is an example of which of the following? 1. Family as context 2. Family as patient 3. Family as system 4. Family as structure 12. A new immigrant family consisting of a grandparent, two adults, and three school-age children has decided to receive their health promotion care at the Community Wellness Center. This is their first visit, and a family assessment, a health history, and a physical of each family member are needed. Which of the following are included in a family function assessment? (Select all that apply.) 1. Cultural practices 2. Decision making 3. Neighborhood services 4. Rituals and celebrations 5. Neighborhood crime data 6. Availability of parks 13. Two single mothers are active professionals and have teenage daughters. They also have busy social lives and date occasionally. Three years ago they decided to share a house and housing costs, living expenses, and child care responsibilities. The children consider one another as their family. What type of family form does this represent? 1. Diverse family relationship 2. Blended family relationships 3. Extended family relationship 4. Alternative family relationship 14. During a visit to a family clinic, a nurse teaches a mother about immunizations, car-seat use, and home safety for an infant and toddler. Which type of nursing interventions are these? 1. Health promotion activities 2. Acute care activities 3. Restorative care activities 4. Growth and development care activities 15. A family has decided to care for their father who is in the last stages of a debilitating neurological illness. Although he is alert, he cannot speak clearly or carry out self-care activities; he indicates that he wants to remain involved in family life as long as possible and loves spending time with his wife and two teenage children. Which best defines family caregiving? (Select all that apply.) 1. Designing a nurturing family to raise children 2. Providing physical and emotional care for a family member 3. Establishing a safe physical environment for a family 4. Monitoring for side effects of illness and treatments 5. Reducing the use of community resources Chapter 11 1. The nurse is aware that preschoolers often display a developmental characteristic that makes them treat dolls or stuffed animals as if they have thoughts and feelings. This is an example of: 1. Logical reasoning. 2. Egocentrism. 3. Concrete thinking. 4. Animism. 2. An 18-month-old child is noted by the parents to be “angry” about any change in routine. This child's temperament is most likely to be described as: 1. Slow to warm up. 2. Difficult. 3. Hyperactive. 4. Easy. 3. Nine-year-old Brian has a difficult time making friends at school and being chosen to play on the team. He also has trouble completing his homework and, as a result, receives little positive feedback from his parents or teacher. According to Erikson's theory, failure at this stage of development results in: 1. A sense of guilt. 2. A poor sense of self. 3. Feelings of inferiority. 4. Mistrust. 4. The nurse teaches parents how to have their children learn impulse control and cooperative behaviors. This would be during which of Erikson's stages of development? 1. Trust versus mistrust 2. Initiative versus guilt 3. Industry versus inferiority 4. Autonomy versus sense of shame and doubt 5. When Ryan was 3 months old, he had a toy train; when his view of the train was blocked, he did not search for it. Now that he is 9 months old, he looks for it, reflecting the presence of: 1. Object permanence. 2. Sensorimotor play. 3. Schemata. 4. Magical thinking. 6. When preparing a 4-year-old child for a procedure, which method is developmentally most appropriate for the nurse to use? 1. Allowing the child to watch another child undergoing the same procedure 2. Showing the child pictures of what he or she will experience 3. Talking to the child in simple terms about what will happen 4. Preparing the child through play with a doll and toy medical equipment 7. Which of the following are examples of the conventional reasoning form of cognitive development? (Select all that apply.) 1. A 35-year-old woman is speaking with you about her recent diagnosis of a chronic illness. She is concerned about her treatment options in relation to her ability to continue to care for her family. As she considers the options and alternatives, she incorporates information, her values, and emotions to decide which plan will be the best fit for her. 2. A young father is considering whether or not to return to school for a graduate degree. He considers the impact the time commitment may have on the needs of his wife and infant son. 3. A teenage girl is encouraged by her peers to engage in shoplifting. She decides not to join her peers in this activity because she is afraid of getting caught in the act. 4. A single mother of two children is unhappy with her employer. She has been unable to secure alternate employment but decides to quit her current job. 8. You are caring for a recently retired man who appears withdrawn and says he is “bored with life.” Applying the work of Havinghurst, you would help this individual find meaning in life by: 1. Encouraging him to explore new roles. 2. Encouraging relocation to a new city. 3. Explaining the need to simplify life. 4. Encouraging him to adopt a new pet. 9. Place the following stages of Freud's psychosexual development in the proper order by age progression. 4 1. Oedipal 3 2. Latency 1 3. Oral 5 4. Genital 2 5. Anal 10. According to Piaget's cognitive theory, a 12-year-old child is most likely to engage in which of the following activities? 1. Using building blocks to determine how houses are constructed 2. Writing a story about a clown who wants to leave the circus 3. Drawing pictures of a family using stick figures 4. Writing an essay about patriotism 11. Allison, age 15 years, calls her best friend Laura and is crying. She has a date with John, someone she has been hoping to date for months, but now she has a pimple on her forehead. Laura firmly believes that John and everyone else will notice the blemish right away. This is an example of the: 1. Imaginary audience. 2. False-belief syndrome. 3. Personal fable. 4. Personal absorption syndrome. 12. Elizabeth, who is having unprotected sex with her boyfriend, comments to her friends, “Did you hear about Kathy? You know, she fools around so much; I heard she was pregnant. That would never happen to me!” This is an example of adolescent: 1. Imaginary audience. 2. False-belief syndrome. 3. Personal fable. 4. Sense of invulnerability. 13. Which of the following activities are examples of the use of activity theory in older adults? (Select all that apply.) 1. Teaching an older adult how to use e-mail to communicate with a grandchild who lives in another state 2. Introducing golf as a new hobby 3. Leading a group walk of older adults each morning 4. Engaging an older adult in a community project with a short-term goal 5. Directing a community play at the local theater 14. Dave reports being happy and satisfied with his life. What do we know about him? 1. He is in one of the later developmental periods, concerned with reviewing his life. 2. He is atypical, since most people in any of the developmental stages report significant dissatisfaction with their lives. 3. He is in one of the earlier developmental periods, concerned with establishing a career and satisfying long-term relationships. 4. It is difficult to determine Dave's developmental stage since most people report overall satisfaction with their lives in all stages. 15. You are working in a clinic that provides services for homeless people. The current local regulations prohibit providing a service that you believe is needed by your patients. You adhere to the regulations but at the same time are involved in influencing authorities to change the regulation. This action represents Social contract orientation stage of moral development. Chapter 12 1. In an interview with a pregnant patient, the nurse discussed the three risk factors that have been cited as having a possible effect on prenatal development. They are: 1. Nutrition, stress, and mother's age. 2. Prematurity, stress, and mother's age. 3. Nutrition, mother's age, and fetal infections. 4. Fetal infections, prematurity, and placenta previa. 2. A parent has brought her 6-month-old infant in for a well-child check. Which of her statements indicates a need for further teaching? 1. “I can start giving her whole milk at about 12 months.” 2. “I can continue to breastfeed for another 6 months.” 3. “I've started giving her plenty of fruit juice as a way to increase her vitamin intake.” 4. “I can start giving her solid food now.” 3. The type of injury to which a child is most vulnerable at a specific age is most closely related to which of the following? 1. Provision of adult supervision 2. Educational level of the parent 3. Physical health of the child 4. Developmental level of the child 4. Which approach would be best for a nurse to use with a hospitalized toddler? 1. Always give several choices. 2. Set few limits to allow for open expression. 3. Use noninvasive methods when possible. 4. Establish a supportive relationship with the mother. 5. A nurse is providing information on prevention of sudden infant death syndrome (SIDS) to the mother of a young infant. Which of the following statements indicates that the mother has a good understanding? (Select all that apply.) 1. “I won't use a pacifier to help my baby sleep.” 2. “I'll be sure that my baby doesn't spend any time sleeping on her abdomen.” 3. “I'll place my baby on her back for sleep.” 4. “I'll be sure to keep my baby's room cool.” 5. “I'll keep a crib bumper in the bed to prevent drafts.” 6. Sequence the skills in the expected order of gross-motor development in an infant beginning with the earliest skill: 4 1. Move from prone to sitting unassisted 5 2. Sit down from standing position 3 3. Sit upright without support 2 4. Roll from abdomen to back 1 5. Can turn from side to back 7. Parents are concerned about their toddler's negativism. To avoid a negative response, which of the following is the best way for a nurse to demonstrate asking the toddler to eat his or her lunch? 1. Would you like to eat your lunch now? 2. When would you like to eat your lunch? 3. Would you like apple slices or applesauce with your sandwich? 4. Would you like to sit at the big table to eat? 8. When nurses are communicating with adolescents, they should: 1. Be alert to clues to their emotional state. 2. Ask closed-ended questions to get straight answers. 3. Avoid looking for meaning behind adolescents' words or actions. 4. Avoid discussing sensitive issues such as sex and drugs. 9. Which of the following statements is most descriptive of the psychosocial development of school-age children? 1. Boys and girls play equally with each other. 2. Peer influence is not yet an important factor to the child. 3. They like to play games with rigid rules. 4. Children frequently have “best friends.” 10. You are caring for a 4-year-old child who is hospitalized for an infection. He tells you that he is sick because he was “bad.” Which is the most correct interpretation of his comment? 1. Indicative of extreme stress 2. Representative of his cognitive development 3. Suggestive of excessive discipline at home 4. Indicative of his developing sense of inferiority 11. At a well-child examination, the mother comments that her toddler eats little at mealtime, will only sit briefly at the table, and wants snacks all the time. Which of the following should the nurse recommend? 1. Provide nutritious snacks. 2. Offer rewards for eating at mealtimes. 3. Avoid snacks so she is hungry at mealtime. 4. Explain to her firmly why eating at mealtime is important. 12. An 8-year-old child is being admitted to the hospital from the emergency department with an injury from falling off her bicycle. Which of the following will most help her adjust to the hospital? 1. Explain hospital routines such as mealtimes to her. 2. Use terms such as “honey” and “dear” to show a caring attitude. 3. Explain when her parents can visit and why siblings cannot come to see her. 4. Since she is young, orient her parents to her room and hospital facility. 13. A school nurse is counseling an obese 10-year-old child. Which factors would be important to consider when planning an intervention to support the child's health? (Select all that apply.) 1. Consider both the child and the family when addressing the issue. 2. Consider the use of medications to suppress the appetite. 3. First plan for weight loss through dieting and then add activity as tolerated. 4. Plan food intake to allow for growth. 5. Consider consulting a bariatric surgeon if other measures fail. 14. You are working in an adolescent health center when a 15-year-old patient shares with you that she thinks she is pregnant and is worried that she may now have a sexually transmitted infection (STI). Her pregnancy test is negative. What is your next priority of care? 1. Contact her parents to alert them of her need for birth control. 2. Refer her to a primary health care provider to obtain a prescription for birth control. 3. Counsel her on safe sex practices. 4. Ask her to have her partner come to the clinic for sexually transmitted infection testing. 15. A 4-month-old infant has not been feeling well for 2 days. His mother has brought him to the clinic to be seen by his health care provider. Which number identifies the area of the infant's head where the nurse can assess for dehydration? 1. 1 2. 2 3. 3 middle front opening 4. 4 5. 5 Chapter 13 1. With the exception of pregnant or lactating women, the young adult has usually completed physical growth by the age of: 1. 18. 2. 20. 3. 25. 4. 30. 2. A nurse is completing an assessment on a male patient, age 24. Following the assessment, the nurse notes that his physical and laboratory findings are within normal limits. Because of these findings, nursing interventions are directed toward activities related to: 1. Instructing him to return in 2 years. 2. Instructing him in secondary prevention. 3. Instructing him in health promotion activities. 4. Implementing primary prevention with vaccines. 3. When determining the amount of information that a patient needs to make decisions about the prescribed course of therapy, many factors affect his or her compliance with the regimen, including educational level and socioeconomic factors. Which additional factor affects compliance? 1. Gender 2. Lifestyle 3. Motivation 4. Family history 4. A patient is laboring with her first baby, who is about to be delivered 2 weeks early. Her husband is in the military and might not get back in time, and both families are unable to be with her during labor. The doctor decides to call in which of the following people employed by the birthing area as a support person to be present during labor? 1. Nurse 2. Midwife 3. Geneticist 4. Lay doula 5. A single young adult interacts with a group of close friends from college and work. They celebrate birthdays and holidays together. In addition, they help one another through many stressors. These individuals are viewed as: 1. Family. 2. Siblings. 3. Substitute parents. 4. Alternative family structure. 6. Sharing eating utensils with a person who has a contagious illness increases the risk of illness. This type of health risk arises from: 1. Lifestyle. 2. Community. 3. Family history. 4. Personal hygiene habits. 7. A 50-year-old woman has elevated serum cholesterol levels that increase her risk for cardiovascular disease. One method to control this risk factor is to identify current diet trends and describe dietary changes to reduce the risk. This nursing activity is a form of: 1. Referral. 2. Counseling. 3. Health education. 4. Stress-management techniques. 8. A 34-year-old female executive has a job with frequent deadlines. She notes that, when the deadlines appear, she has a tendency to eat high-fat, high-carbohydrate foods. She also explains that she gets frequent headaches and stomach pain during these deadlines. The nurse provides a number of options for the executive, and she chooses yoga. In this scenario yoga is used as a (n): 1. Outpatient referral. 2. Counseling technique. 3. Health promotion activity. 4. Stress-management technique. 9. A 50-year-old male patient is seen in the clinic. He tells a nurse that he has recently lost his job and his wife of 26 years has asked for a divorce. He has a flat affect. Family history reveals that his father committed suicide at the age of 53. The nurse assesses for the following: 1. Cardiovascular disease 2. Depression 3. Sexually transmitted infection 4. Iron deficiency anemia 10. Middle-age adults frequently find themselves trying to balance responsibilities related to employment, family life, care of children, and care of aging parents. People finding themselves in this situation are frequently referred to as being a part of: 1. The sandwich generation. 2. The millennial generation. 3. Generation X. 4. Generation Y. 11. Intimate partner violence (IPV) is linked to which of the following factors? (Select all that apply.) 1. Alcohol abuse 2. Marriage 3. Pregnancy 4. Unemployment 5. Drug use 12. Sexually transmitted infections (STIs) continue to be a major health problem in young adults. Men ages 20 to 24 years have the highest rate of which STI? 1. Chlamydia 2. Syphilis 3. Gonorrhea 4. Herpes zoster 13. Formation of positive health habits may prevent the development of chronic illness later in life. Which of the following are examples of positive health habits? (Select all that apply.) 1. Routine screening and diagnostic tests 2. Unprotected sexual activity 3. Regular exercise 4. Excess alcohol consumption 5. Consistent seat belt use 14. Chronic illness (e.g., diabetes mellitus, hypertension, rheumatoid arthritis) may affect a person's roles and responsibilities during middle adulthood. When assessing the health-related knowledge base of both the middle-age patient with a chronic illness and his family, your assessment includes which of the following? (Select all that apply.) 1. The medical course of the illness 2. The prognosis for the patient 3. Socioeconomic status 4. Coping mechanisms of the patient and family 5. The need for community and social services 15. A 45-year-old woman who is obese tells a nurse that she wants to lose weight. After conducting a thorough assessment, the nurse concludes that which of the following may be contributing factors to the woman's obesity? (Select all that apply.) 1. The woman works in an executive position that is very demanding. 2. The woman works out at the corporate gym at 5 AM two mornings per week. 3. The woman says that she has little time to prepare meals at home and eats out at least four nights a week. 4. The woman says that she tries to eat “low-cholesterol” foods to help lose weight. 5. The woman says that she vacations annually to reduce stress. Chapter 14 1. A nursing student is caring for a 78-year-old patient with multiple sclerosis. The patient has had an indwelling Foley catheter in for 3 days. Eight hours ago the patient's temperature was 37.1° C (98.8° F). The student reports her recent assessment to the registered nurse (RN): the patient's temperature is 37.2° C (99° F); the Foley catheter is still in place, draining dark urine; and the patient is uncertain what time of day it is. From what the RN knows about presentation of symptoms in older adults, what should he recommend first? 1. Tell the student that temporary confusion is normal and simply requires reorientation 2. Tell the student to increase the patient's fluid intake since the urine is concentrated 3. Tell the student that her assessment findings are normal for an older adult 4. Tell the student that he will notify the patient's health care provider of the findings and recommend a urine culture 2. A patient's family member is considering having her mother placed in a nursing center. The nurse has talked with the family before and knows that this is a difficult decision. Which of the following criteria does the nurse recommend in choosing a nursing center? (Select all that apply.) 1. The center needs to be clean, and rooms should look like a hospital room. 2. Adequate staffing is available on all shifts. 3. Social activities are available for all residents. 4. The center provides three meals daily with a set menu and serving schedule. 5. Staff encourage family involvement in care planning and assisting with physical care. 3. A nurse conducted an assessment of a new patient who came to the medical clinic. The patient is 82 years old and has had osteoarthritis for 10 years and diabetes mellitus for 20 years. He is alert but becomes easily distracted during the assessment. He recently moved to a new apartment, and his pet beagle died just 2 months ago. He is most likely experiencing: 1. Dementia. 2. Depression. 3. Delirium. 4. Hypoglycemic reaction. 4. The nurse is completing a health history with the daughter of a newly admitted patient who is confused and agitated. The daughter reports that her mother was diagnosed with Alzheimer's disease 1 year ago but became extremely confused last evening and was hallucinating. She was unable to calm her, and her mother thought she was a stranger. On the basis of this history, the nurse suspects that the patient is experiencing: 1. Delirium. 2. Depression. 3. New-onset dementia. 4. Worsening dementia. 5. Sexuality is maintained throughout our lives. Which of the following answers best explains sexuality in an older adult? 1. When the sexual partner passes away, the survivor no longer feels sexual. 2. A decrease in an older adult's libido occurs. 3. Any outward expression of sexuality suggests that the older adult is having a developmental problem. 4. All older adults, whether healthy or frail, need to express sexual feelings. 6. Older adults frequently experience a change in sexual activity. Which best explains this change? 1. The need to touch and be touched is decreased. 2. The sexual preferences of older adults are not as diverse. 3. Physical changes usually do not affect sexual functioning. 4. Frequency and opportunities for sexual activity may decline. 7. The nurse sees a 76-year-old woman in the outpatient clinic. She states that she recently started noticing a glare in the lights at home. Her vision is blurred; and she is unable to play cards with her friends, read, or do her needlework. The nurse suspects that the woman may have: 1. Presbyopia. 2. Presbycusis 3. Cataract(s). 4. Depression. 8. A nurse is caring for a patient preparing for discharge from the hospital the next day. The patient does not read. His family caregiver will be visiting before discharge. What can the nurse do to facilitate the patient's understanding of his discharge instructions? (Select all that apply.) 1. Yell so the patient can hear you. 2. Sit facing the patient so he is able to watch your lip movements and facial expressions. 3. Present one idea or concept at a time. 4. Send a written copy of the instructions home with him and tell him to have the family review them. 5. Include the family caregiver in the teaching session. 9. A 63-year-old patient is retiring from his job at an accounting firm where he was in a management role for the past 20 years. He has been with the same company for 42 years and was a dedicated employee. His wife is a homemaker. She raised their five children, babysits for her grandchildren as needed, and belongs to numerous church committees. What are the major concerns for this patient? (Select all that apply.) 1. The loss of his work role 2. The risk of social isolation 3. A determination if the wife will need to start working 4. How the wife expects household tasks to be divided in the home in retirement 5. The age the patient chose to retire 10. A nurse is assessing an older adult brought to the emergency department following a fall and wrist fracture. She notes that the patient is very thin and unkempt, has a stage 3 pressure ulcer to her coccyx, and has old bruising to the extremities in addition to her new bruises from the fall. She defers all of the questions to her caregiver son who accompanied her to the hospital. The nurse's next step is to: 1. Call social services to begin nursing home placement. 2. Ask the son to step out of the room so she can complete her assessment. 3. Call adult protective services because you suspect elder mistreatment. 4. Assess patient's cognitive status. 11. A nurse is participating in a health and wellness event at the local community center. A woman approaches and relates that she is worried that her widowed father is becoming more functionally impaired and may need to move in with her. The nurse inquires about his ability to complete activities of daily living (ADLs). ADLs include independence with: (Select all that apply.) 1. Driving. 2. Toileting. 3. Bathing. 4. Daily exercise. 5. Eating. 12. During a home health visit a nurse talks with a patient and his family caregiver about the patient's medications. The patient has hypertension and renal disease. Which of the following findings place him at risk for an adverse drug event? (Select all that apply.) 1. Taking two medications for hypertension 2. Taking a total of eight different medications during the day 3. Having one physician who reviews all medications 4. Patient's health history of renal disease 5. Involvement of the caregiver in helping with medication administration 13. The nurse is completing an admission assessment with an 80-year-old man who experienced a hip fracture following a fall. He is alert, lives alone, and has very poor hygiene. He reports a 20-pound weight loss in the last 6 months following his wife's death, as well as estrangement from his only child. He admits to falls before this most recent fall. What should the nurse suspect? 1. Dementia. 2. Elder abuse. 3. Delirium. 4. Alcohol abuse. 14. The nurse is working with an older adult after an acute hospitalization. The goal is to help this person be more in touch with time, place, and person. Which intervention will likely be most effective? 1. Reminiscence 2. Validation therapy 3. Reality orientation 4. Body image interventions 15. A 71-year-old patient enters the emergency department after falling down stairs in the home. The nurse is conducting a fall history with the patient and his wife. They live in a one-level ranch home. He has had diabetes for over 15 years and experiences some numbness in his feet. He wears bifocal glasses. His blood pressure is stable at 130/70. The patient does not exercise regularly and states that he experiences weakness in his legs when climbing stairs. He is alert, oriented, and able to answer questions clearly. What are the fall risk factors for this patient? (Select all that apply.) 1. Impaired vision 2. Residence design 3. Blood pressure 4. Leg weakness 5. Exercise history Chapter 36 1. A student nurse is telling a faculty member that her patient talked about gaining spiritual comfort from being focused on her inner self, including her values and principles. The instructor explains that this is an example of: 1. Faith. 2. Community. 3. Interpersonal connection. 4. Self-transcendence. 2. Health care agencies often have assessment tools to use in clarifying patient values and assess spirituality. Using the FICA assessment tool, match the criteria on the left with the appropriate assessment question on the right. Faith 1a. Tell me if you have a higher power or authority that helps you act on your beliefs Interventions to spiritual needs 4b. Describe which activities give you comfort spiritually? Community 3c. To whom do you go for support in times of difficulty? Importance of spirituality 2d. Your illness has kept you from attending church. Is that a problem for you? 3. A nurse is caring for a 78-year-old patient with chronic multiple sclerosis. The patient has severe fatigue, muscle weakness, severe muscle spasms, and difficulties with coordination and balance. Her disease will likely worsen. The nurse has gained the patient's trust and wants to assess her life satisfaction. Which of the following questions should the nurse ask? (Select all that apply.) 1. How often are you able to attend your synagogue? 2. What about your family makes you proudest? 3. What does your husband do for you at home? 4. Looking back, what is your greatest accomplishment? 5. How has your illness affected the way you live your life spiritually at home? 4. You are caring for a hospitalized patient who is Muslim and has diabetes. Which of the following items do you need to remove from the meal tray when it is delivered to the patient? 1. Small container of vanilla ice cream 2. A dozen red grapes 3. Bacon and eggs 4. Garden salad with ranch dressing 5. A 44-year-old male patient has just been told that his wife and child were killed in an auto accident while coming to visit him in the hospital. Which of the following statements are defining characteristics that support a nursing diagnosis of Spiritual Distress related to loss of family members? (Select all that apply.) 1. “I need to call my sister for support.” 2. “I have nothing to live for now.” 3. “Why would my God do this to me?” 4. “I need to pray for a miracle.” 5. “I want to be more involved in my church.” 6. A patient has just learned she has been diagnosed with a malignant brain tumor. She is alone; her family will not be arriving from out of town for an hour. You have cared for her for only 2 hours but have a good relationship with her. What might be the most appropriate intervention for support of her spiritual well-being at this time? 1. Make a referral to a professional spiritual care advisor 2. Sit down and talk with the patient; have her discuss her feelings and listen attentively 3. Move the patient's bible from her bedside cabinet drawer to the top of the over-bed table 4. Ask the patient if she would like to learn more about the implications of having this type of tumor 7. A nurse is preparing to teach an older adult who has chronic arthritis how to practice meditation. Which of the following strategies are appropriate? (Select all that apply.) 1. Encourage family members to participate in the exercise. 2. Have patient identify a quiet room in the home that has minimal interruptions. 3. Suggest use of a quiet fan running in the room. 4. Explain that it is best to meditate about 5 minutes 4 times a day. 5. Show the patient how to sit comfortably with the limitation of his arthritis and focus on a prayer. 8. A student nurse is developing a plan of care for a 74-year-old-female patient who has spiritual distress over losing a spouse. As the nurse develops appropriate interventions, which characteristics of older adults should be considered? (Select all that apply.) 1. Older adults do not routinely use complementary medicine to cope with illness. 2. Older adults dislike discussing the afterlife and what might have happened to people who have passed on. 3. Older adults achieve spiritual resilience through frequent expressions of gratitude. 4. Have the patient determine if her husband left a legacy behind. 5. Offer the patient her choice of rituals or participation in exercise. 9. A patient states that he does not believe in a higher power but instead believes that people bring meaning to what they do. This patient most likely is an: 1. Academic. 2. Atheist. 3. Agnostic. 4. Anarchist. 10. A nurse begins a night shift, assuming care for a critically ill patient who was resuscitated earlier in the day from cardiac arrest. He survived and is physically stable, alert, oriented, and responding appropriately to the nurse's questions. Knowing that the patient experienced a period when his heart stopped beating, what would be the best approach for the nurse to use with him? 1. Have family come to visit and focus discussion about their gratitude that the patient survived 2. Change the subject when the patient begins talking about entering a dark tunnel when the doctors were resuscitating him 3. Sit and encourage the patient to share what he experienced during resuscitation 4. Provide the patient the opportunity to have passages from the bible read to him 11. A nurse is caring for a patient with a seriously advanced infection who asks to have a spiritual care provider come who can offer Blessingway, a practice that attempts to remove ill health. This patient is likely a member of which religion or culture? 1. Hinduism 2. Navajo 3. Sikhism 4. Judaism 12. Evaluation of spiritual care is necessary to determine if a patient's level of spiritual health has changed following intervention. If the use of rituals was part of a nurse's care plan, which of the following questions is most appropriate to evaluate its efficacy? 1. Do you feel the need to forgive your wife over your loss? 2. What can I do to help you feel more at peace? 3. Were prayer or meditation helpful to you? 4. Should we plan on having your family try to visit you more often in the hospital? 13. A patient who is recovering from a bilateral amputation of the legs below the knee shows transcendence when she states: 1. “My pain medicine helps me feel better.” 2. “I know I'll get better if I just keep trying.” 3. “I see God's grace and become relaxed when I watch the sun set at night.” 4. “I have had a great life and a good marriage. My husband has been so helpful in my healing.” 14. The nurse is caring for a 50-year-old woman visiting the outpatient medicine clinic. The patient has had type 1 diabetes since age 13. She has numerous complications from her disease, including reduced vision, heart disease, and severe numbness and tingling of the extremities. Knowing that spirituality helps patients cope with their chronic illness, which of the following principles should the nurse apply in practice? (Select all that apply.) 1. Pay attention to the patient's spiritual identity throughout the course of her illness 2. Select interventions that you know scientifically support spiritual well-being 3. Listen to the patient's story each visit to the clinic and offer a compassionate presence 4. When the patient questions the reason for her long-time suffering, try to provide answers 5. Consult with a spiritual care advisor and have the advisor recommend useful interventions 15. Select the three factors that are evident when a healing relationship develops between nurse and patient. 1. The nurse being able to realistically mobilize hope for the patient 2. The patient being able to share fears of loss with significant others 3. Finding an interpretation or understanding of the patient's illness that is acceptable to the patient 4. Understanding your own beliefs about spirituality 5. Helping the patient use spiritual resources that he or she chooses Chapter 37 1. To best assist a patient in the grieving process, which of the following is most helpful to determine? 1. Previous experiences with grief and loss 2. Religious affiliation and denomination 3. Ethnic background and cultural practices 4. Current financial status. 2. Which of the following is the best intervention to help a hospitalized patient maintain some autonomy? 1. Use therapeutic techniques when communicating with the patient. 2. Allow the patient to determine timing and scheduling of interventions. 3. Encourage family to only visit for short periods of time. 4. Provide the patient with a private room close to the nurse's station. 3. Which factors influence a person's approach to death? (Select all that apply.) 1. Culture 2. Age 3. Spirituality 4. Personal beliefs 5. Previous experiences with death 6. Gender 7. Level of education 8. Degree of social support 4. A family member of a dying patient talks casually with the nurse and expresses relief that she will not have to visit at the hospital anymore. Which theoretical description of grief best applies to this family member? 1. Denial 2. Anticipatory grief 3. Yearning and searching 4. Dysfunctional grief 5. On entering a room the nurse sees the patient crying softly. What is the most therapeutic response? 1. Using silence 2. Asking, “Why are you crying today?” 3. Using therapeutic touch 4. Stating, “I see that you're crying.” 6. A young mother is dying of breast cancer with bone metastasis and tells the nurse, “My body hurts so much. I can hardly move. Why is God making me suffer when I have done nothing bad in my life? I feel like giving up. How can I care for my children when I can't even care for myself?” What is the most appropriate nursing diagnosis for this patient? 1. Spiritual Distress related to questioning God 2. Hopelessness related to terminal diagnosis 3. Pain related to disease process 4. Anticipatory Grief related to impending death 7. A nurse has the responsibility of managing a deceased patient's postmortem care. What is the proper order for postmortem care? 1 Ensure that the request for organ/tissue donation and/or autopsy was completed., 2 Elevate the head of the bed., 3 Collect any needed specimens., 4 Speak to the family members about their possible participation., 5 Notify support person (e.g., spiritual care provider, bereavement specialist) for the family., 6 Remove all tubes and indwelling lines., 7 Bathe the body of the deceased., 8 Position the body for family viewing., 9 Accurately tag the body, including the identity of the deceased and safety issues regarding infection control. 8. Which comment to a patient by a new nurse regarding palliative care needs to be corrected? 1. “Even though you're continuing treatment, palliative care is something we might want to talk about.” 2. “Palliative care is appropriate for people with any diagnosis.” 3. “Only people who are dying can receive palliative care.” 4. “Children are able to receive palliative care.” 9. A patient is receiving palliative care for symptom management related to anxiety and pain. A family member asks if the patient is dying and now in “hospice.” What does the nurse tell the family member about palliative care? (Select all that apply.) 1. Palliative care and hospice are the same thing. 2. Palliative care is for any patient, any time, any disease, in any setting. 3. Palliative care strategies are primarily designed to treat the patient's illness. 4. Palliative care relieves the symptoms of illness and treatment. 5. Palliative care selects home health care services. 10. A grieving patient complains of confusion, inability to concentrate, and insomnia. What do these symptoms indicate? 1. These are normal symptoms of grief. 2. There is a need for pharmacological support for insomnia. 3. The patient is experiencing complicated grief. 4. These are common complaints of the admitted patient. 11. When planning care for the dying patient, which interventions promote the patient's dignity? (Select all that apply.) 1. Providing respect 2. Viewing patients as a whole 3. Providing symptom management 4. Showing interest 5. Being present 6. Using a preferred name 12. What are the physical changes that occur as death approaches? (Select all that apply.) 1. Unresponsiveness 2. Erythema 3. Mottling 4. Restlessness 5. Increased urine output 6. Weakness 7. Incontinence 13. What is the palliative care team's primary obligation for the patient with severe pain? 1. Providing postmortem care. 2. Teaching about grief stages. 3. Enhancing the patient's quality of life. 4. Supporting the family after the death. 14. A year after her husband's death, a widow visits the unit on which he died. She talks about the anniversary and how much she misses him. Which type of grief is she experiencing? 1. Normal 2. Complicated 3. Chronic 4. Disenfranchised 15. When providing postmortem care, which action is a priority for the nurse? 1. Locating the patient's clothing 2. Providing culturally and religiously sensitive care in body preparation 3. Transporting the body to the morgue as soon as possible 4. Providing postmortem care to protect the family of the deceased from having to view the body Chapter 38 1. When teaching a patient about the negative feedback response to stress, the nurse includes which of the following to describe the benefits of this stress response? 1. Results in neurophysiological response 2. Reduces body temperature 3. Causes a person to be hypervigilant 4. Reduces level of consciousness to conserve energy. 2. The nurse is interviewing a patient in the community clinic and gathers the following information about her: she is intermittently homeless, a single parent with two children who have developmental delays, and is suffering from chronic asthma. She does not laugh or smile, does not volunteer any information, and at times appears close to tears. She has no support system and does not work. She is experiencing an allostatic load. As a result, which of the following would be present during complete patient assessment? (Select all that apply.) 1. Post-traumatic stress disorder 2. Rising hormone levels 3. Chronic illness 4. Return of vital signs to normal 5. Depression 3. A patient who is having difficulty managing his diabetes mellitus responds to the news that his hemoglobin A1C, a measure of blood sugar control over the past 90 days, has increased by saying, “The hemoglobin A1C is wrong. My blood sugar levels have been excellent for the last 6 months.” Which defense mechanism is the patient using? 1. Denial. 2. Conversion. 3. Dissociation. 4. Displacement. 4. When doing an assessment of a young woman who was a victim of a home invasion 3 months earlier, the nurse learns that the woman has vivid images of the crash whenever she hears loud yelling or a sudden noise. The nurse recognizes this as Post-traumatic stress disorder (PTSD) . 5. A grandfather living in Japan worries about his two young grandsons who disappeared after a tsunami. This is an example of: 1. A situational crisis. 2. A maturational crisis. 3. An adventitious crisis. 4. A developmental crisis. 6. During the assessment interview of an older woman who is recently widowed, the nurse suspects that this woman is experiencing a developmental crisis. Which of the following questions provide information about the impact of this crisis? (Select all that apply.) 1. With whom do you talk on a routine basis? 2. What do you do when you feel lonely? 3. How is having diabetes affecting your life? 4. I know this must be hard for you. Let me tell you what might help. 5. Do you have any changes in lifestyle habits: sleeping, eating, smoking, and drinking? 7. The nurse plans care for a 16-year-old male, taking into consideration that stressors experienced most commonly by adolescents include which of the following? 1. Loss of autonomy caused by health problems 2. Physical appearance, family, friends, and school 3. Self-esteem issues, changing family structure 4. Search for identity with peer groups and separation from family 8. A 10-year-old girl was playing on a slide at a playground during a summer camp. She fell and broke her arm. The camp notified the parents and took the child to the emergency department according to the camp protocol for injuries. The parents arrive at the emergency department and are stressed and frantic. The 10- year-old is happy in the treatment room, eating a Popsicle and picking out the color of her cast. List in order of priority what the nurse should say to the parents? 1 “Your daughter is happy in the treatment room, eating a Popsicle and picking out the color of her cast.”, 2 “Let me help you two calm down a bit so I can take you to your daughter.”, 3 “I'll have the doctor come out and talk to you as soon as possible.”, 4 “Can I contact someone to help you?” 9. When assessing an older adult who is showing symptoms of anxiety, insomnia, anorexia, and mild confusion, one of the first assessments includes which of the following? 1. The amount of family support 2. A 3-day diet recall 3. A thorough physical assessment 4. Threats to safety in her home 10. After a health care provider has informed a patient that he has colon cancer, the nurse enters the room to find the patient gazing out the window in thought. Which of the following are appropriate responses or actions of the nurse? (Select all that apply.) 1. “I know another patient whose colon cancer was cured by surgery.” 2. Straighten the patient's bed and room 3. “Have you thought about how you are going to tell your family?” 4. “Would you like for me to sit down with you for a few minutes so you can talk about this?” 5. Sit quietly with the patient 11. A 34-year-old single father who is anxious, tearful, and tired from caring for his three young children tells the nurse that he feels depressed and doesn't see how he can go on much longer. Which of the following would be the nurse's best response? 1. “Are you thinking of suicide?” 2. “You've been doing a good job raising your children. You can do it!” 3. “Is there someone who can help you during the evenings and weekends?” 4. “What do you mean when you say you can't go on any longer?” 12. The nurse is evaluating the coping success of a patient experiencing stress from being newly diagnosed with multiple sclerosis and psychomotor impairment. Which of the following statements indicate that the patient is beginning to cope with the diagnosis? (Select all that apply.) 1. “I'm going to learn to drive a car so I can be more independent.” 2. “My sister says she feels better when she goes shopping, so I'll go shopping.” 3. “I'm going to let the occupational therapist assess my home to improve efficiency.” 4. “I've always felt better when I go for a long walk. I'll do that when I get home.” 5. “I'm going to attend a support group to learn more about multiple sclerosis.” 13. A patient with type 2 diabetes is experiencing a lot of work-related stress and is fearful of losing his job. In addition, his wife is threatening divorce. His blood sugar is elevating, and his doctors want him to attend some stress-management classes. He says, “My blood sugar can't be high because of my work stress.” What causes blood glucose to rise during stress? (Select all that apply.) 1. Increases in antidiuretic hormone (ADH) 2. Increases in cortisol 3. Increases in aldosterone 4. Increases in adrenocorticotropic hormone (ACTH) 5. Increases in epinephrine 14. A staff nurse is talking with the nursing supervisor about the stress that she feels on the job. Which of the following are true about work-related stress? (Select all that apply.) 1. Job-related stress can affect the quality of patient care. 2. Stress can affect nurses' efficiency and decision making. 3. Nurses who talk about feeling stress are unprofessional and should calm down. 4. Nurses frequently experience stress with the rapid changes in health care technology. 5. Nurses cannot resolve job-related stress. 15. A crisis intervention nurse is working with a mother whose Down syndrome child has been hospitalized with pneumonia and who has lost her child's disability payment while the child is hospitalized. The mother worries that her daughter will fall behind in special-school classes during hospitalization. Which strategies are effective in helping this mother cope with these stressors? (Select all that apply.) 1. Referral to social service process reestablishing the child's disability payment 2. Sending the child home in 72 hours and having the child return to school 3. Coordinating hospital-based and home-based schooling with the child's teacher 4. Teaching the mother signs and symptoms of a respiratory tract infection 5. Telling the mother that the stress will decrease in 6 weeks when everything is back to normal [Show More]
Last updated: 1 year ago
Preview 1 out of 61 pages
Reviews( 0 )
Document information
Connected school, study & course
About the document
Uploaded On
Sep 22, 2022
Number of pages
61
Written in
Additional information
This document has been written for:
Uploaded
Sep 22, 2022
Downloads
0
Views
36


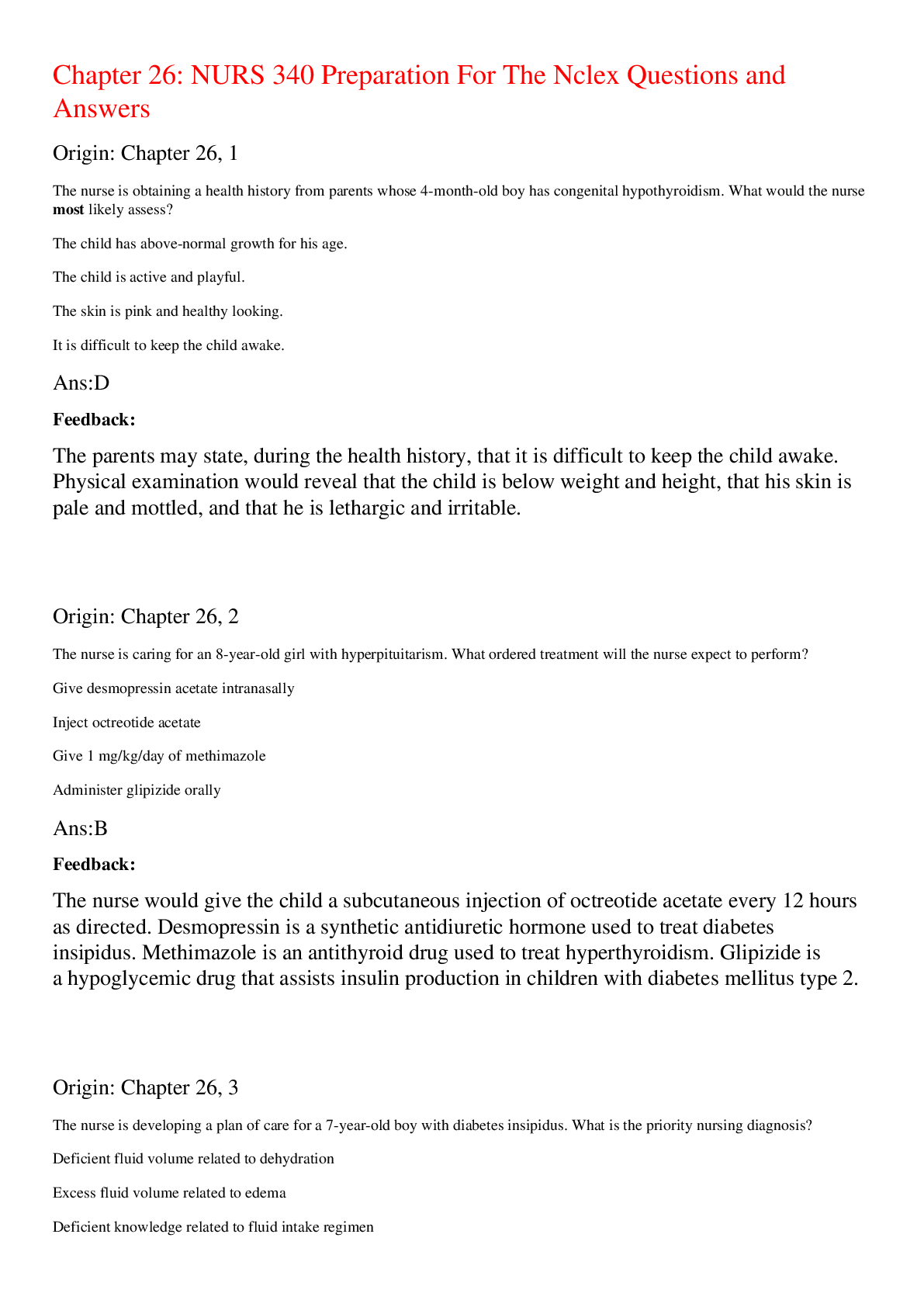
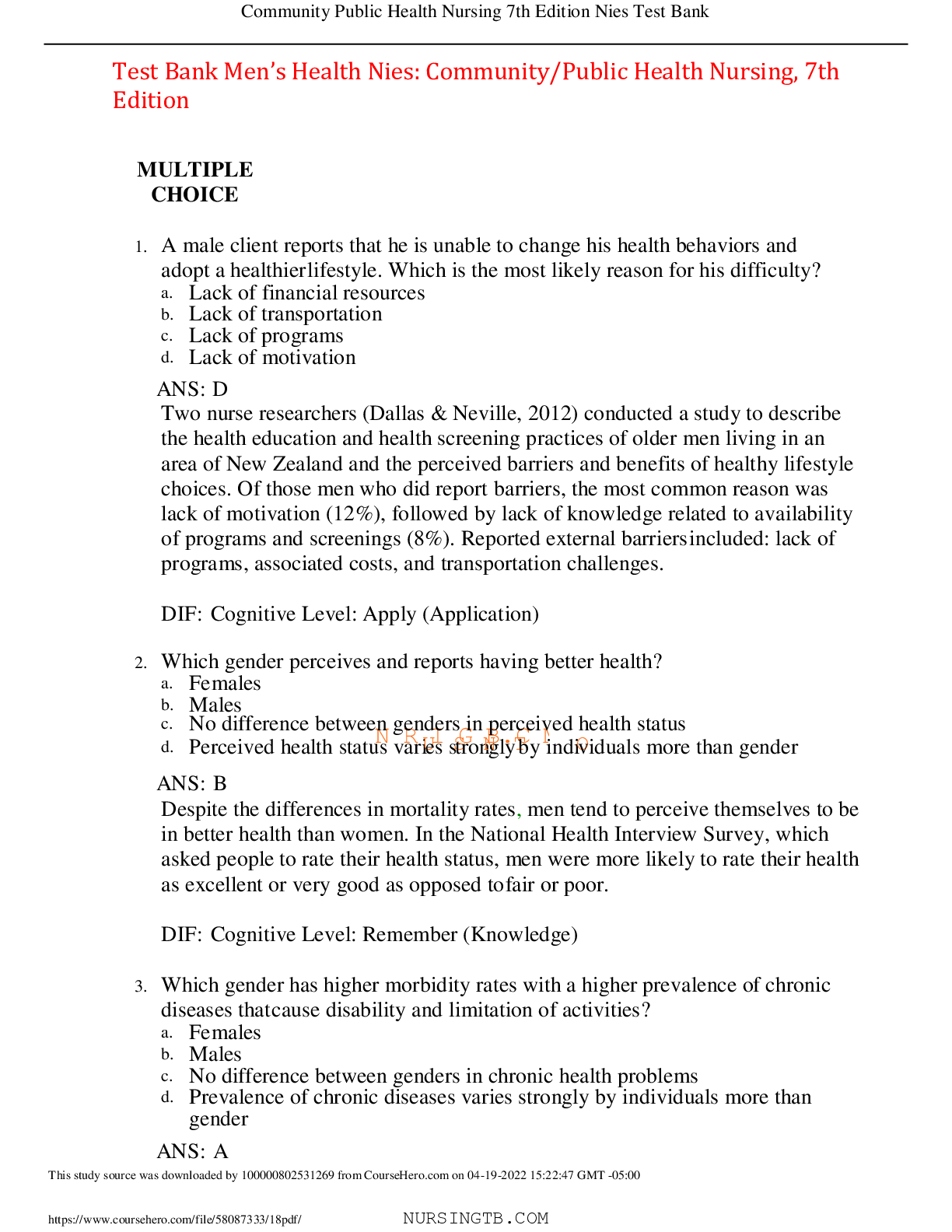

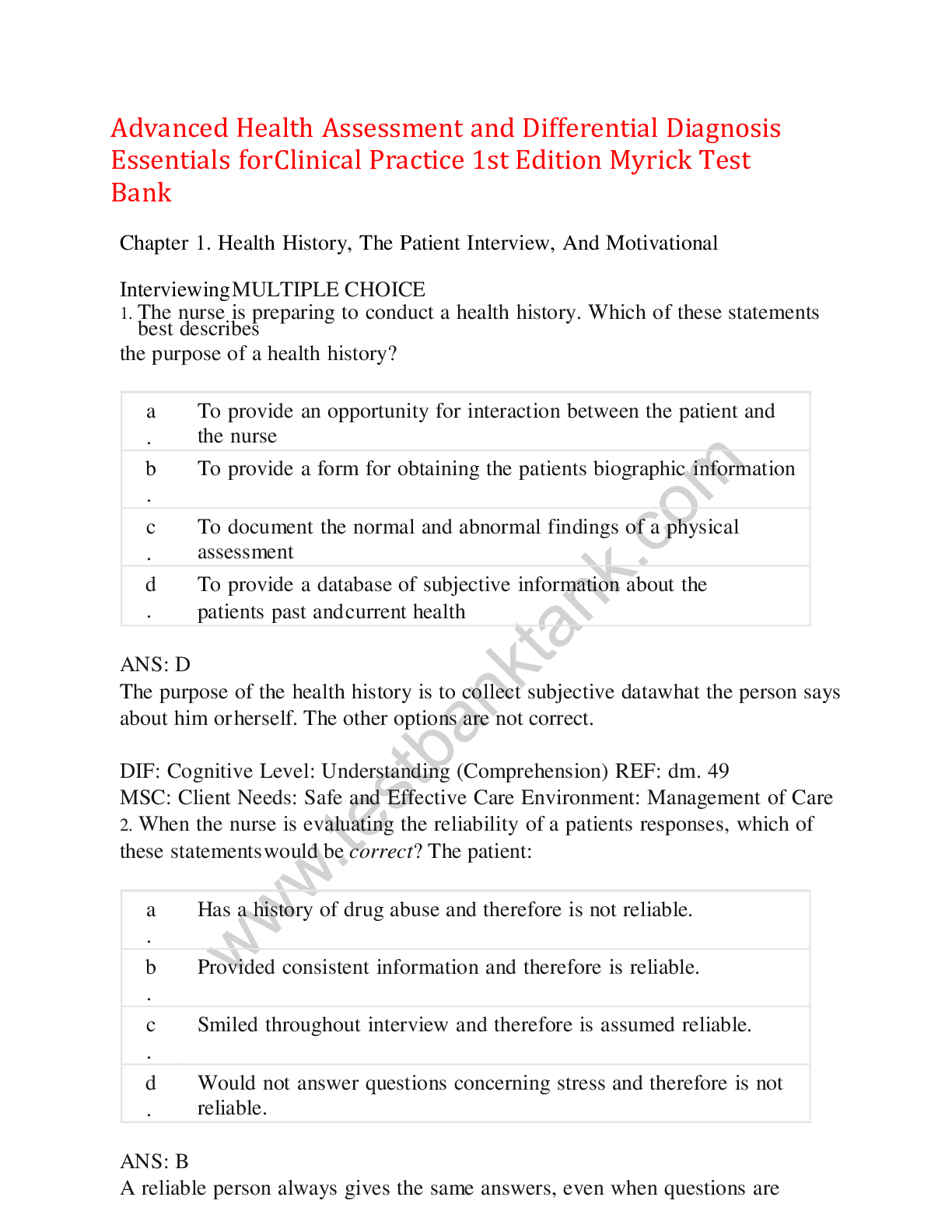
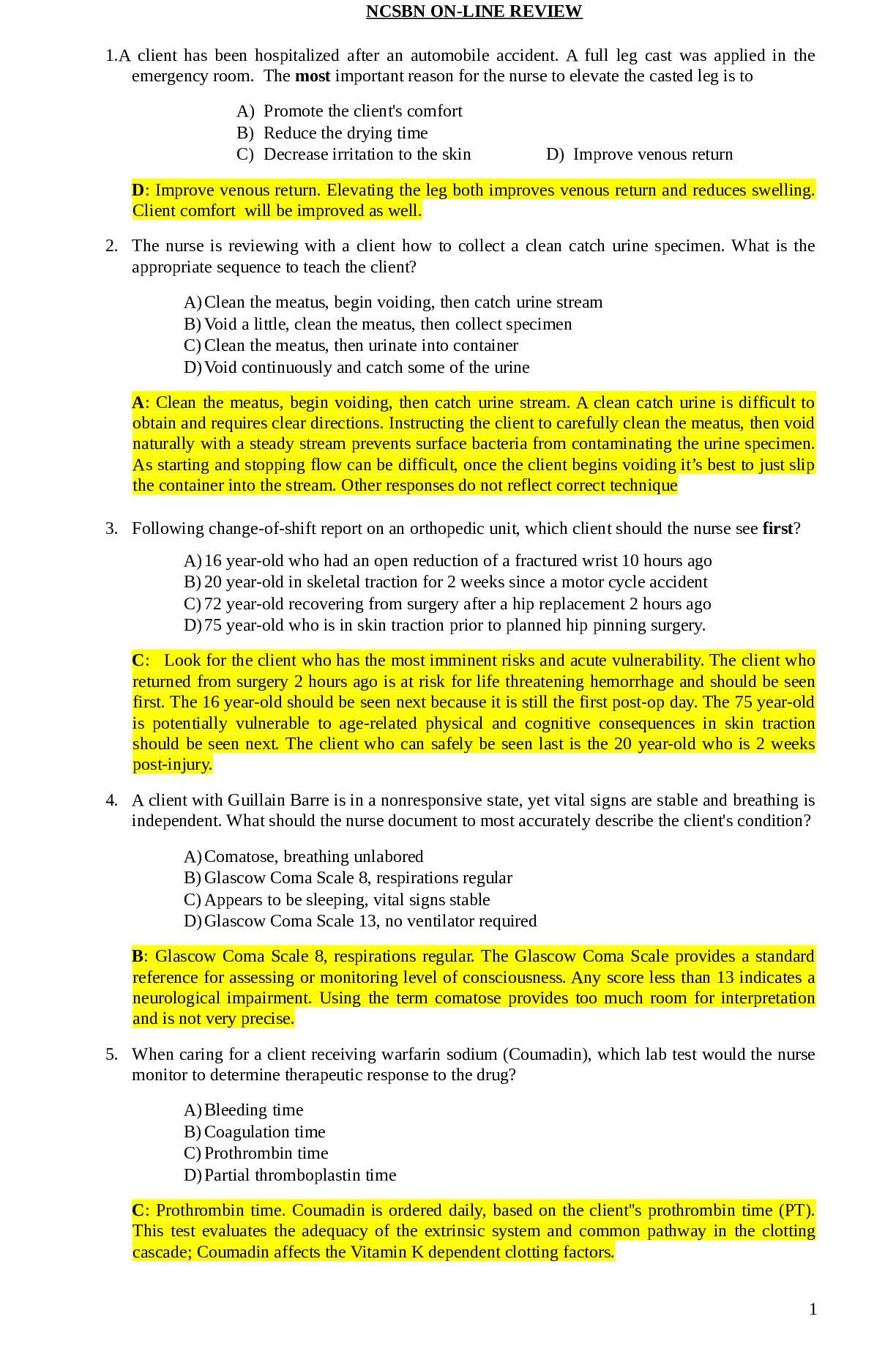
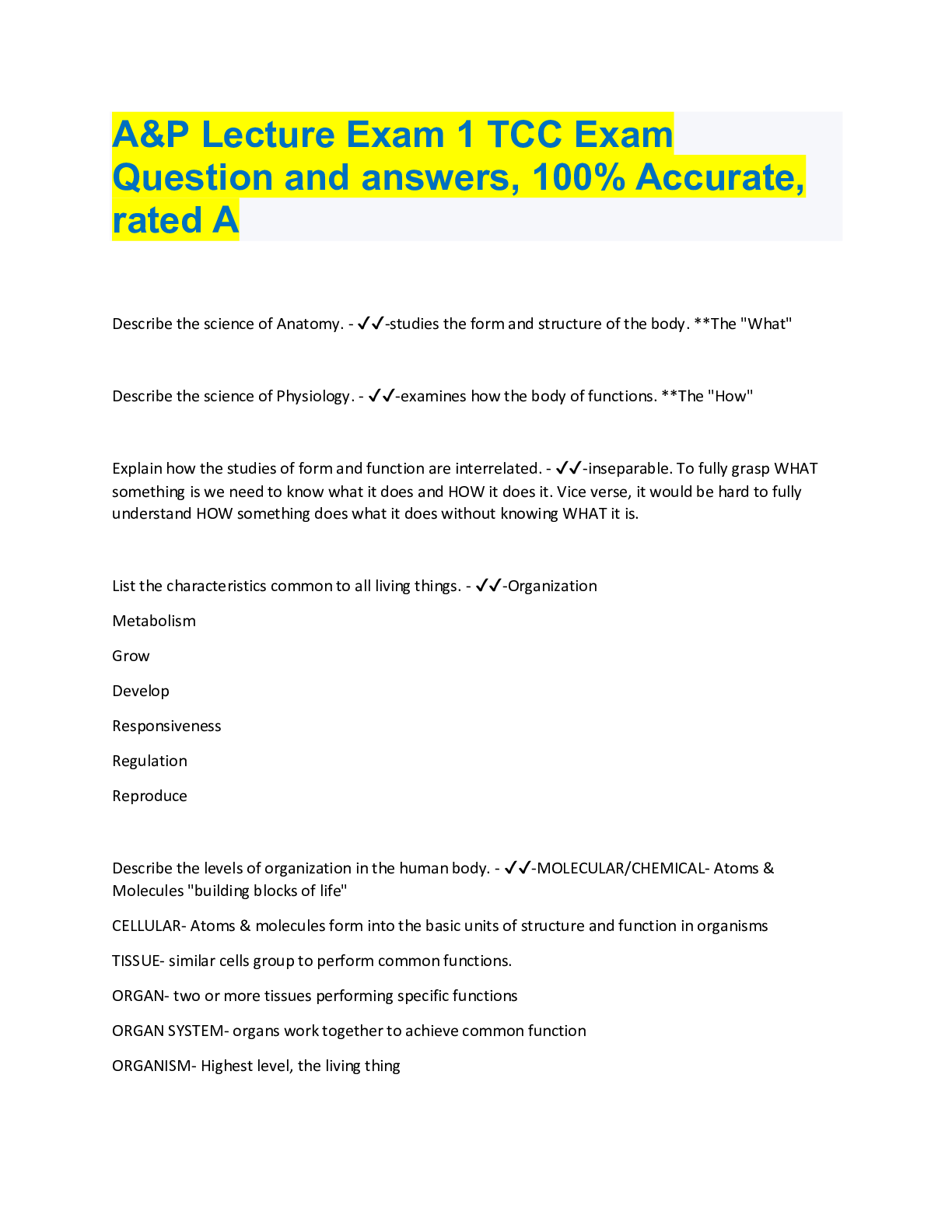
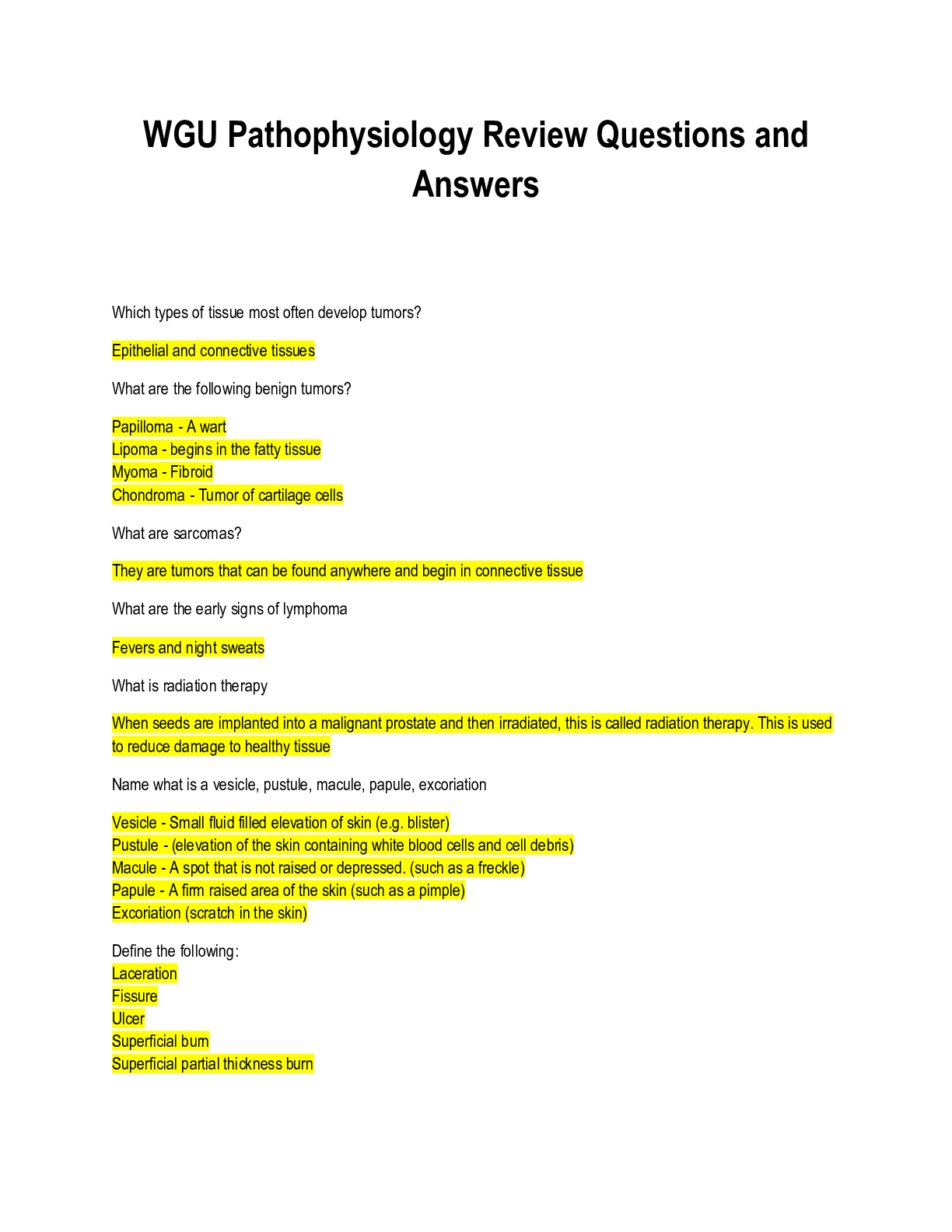
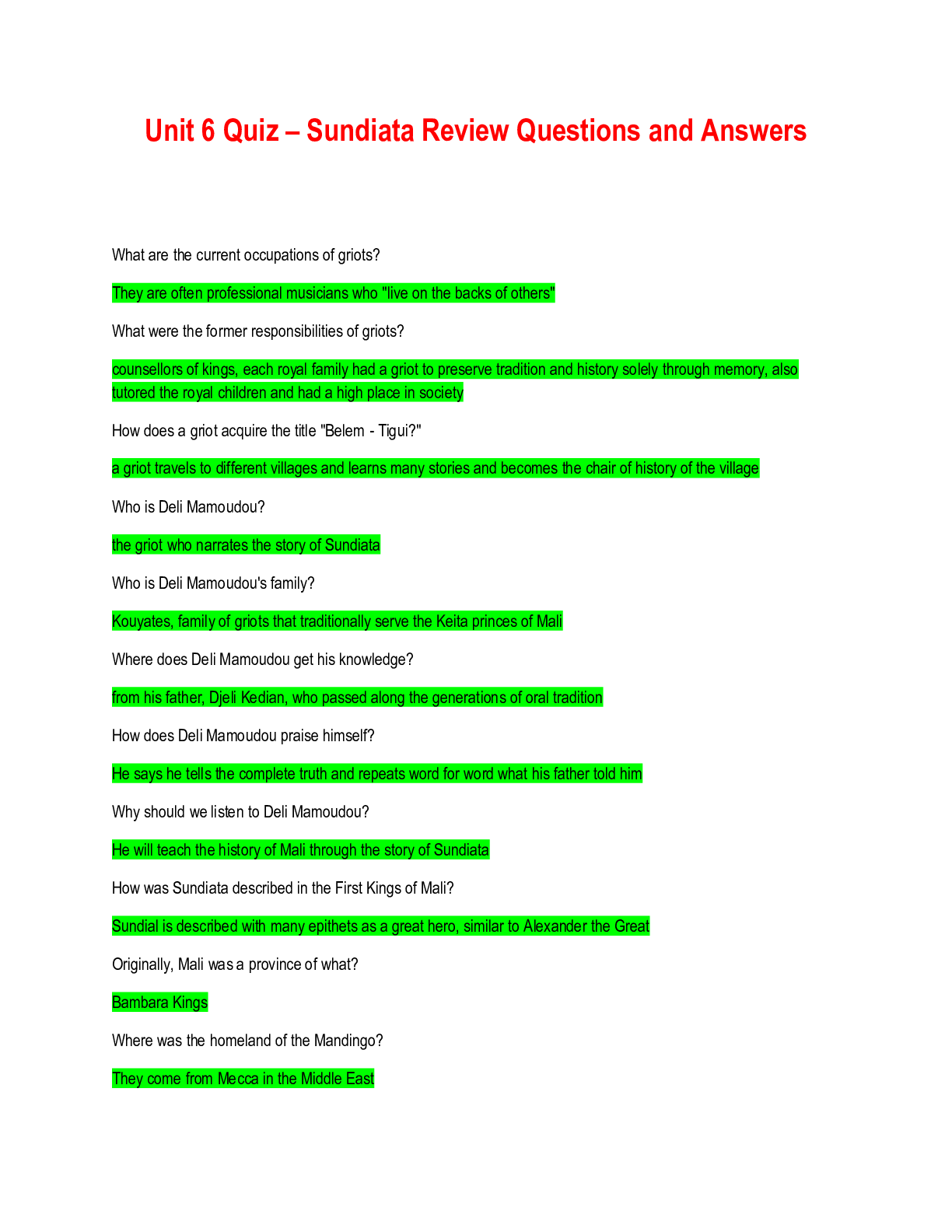
 (1).png)