GASTRO NCLEX QUESTIONS AND ANSWERS LATEST UPDATE 2022/2023
Document Content and Description Below
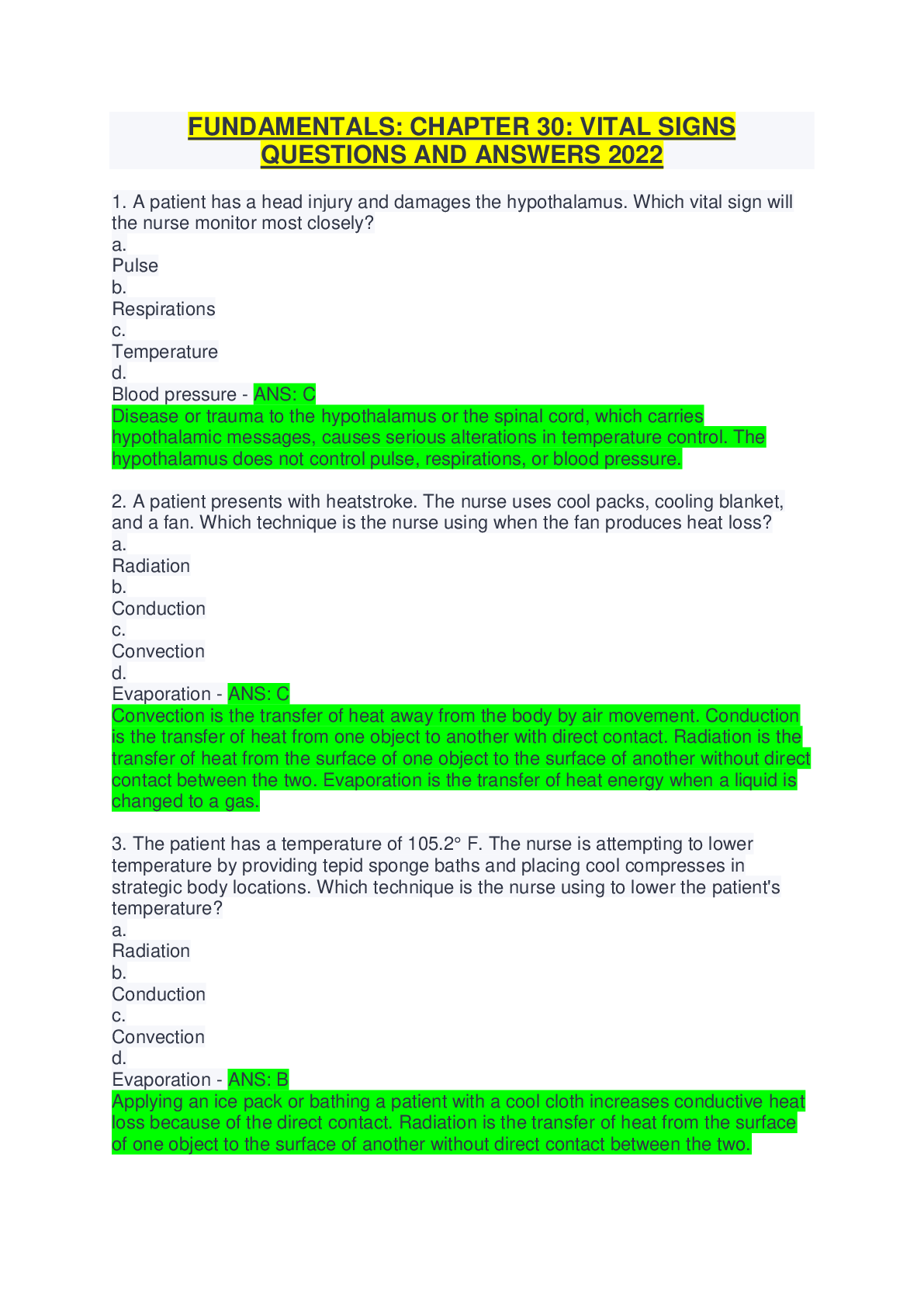
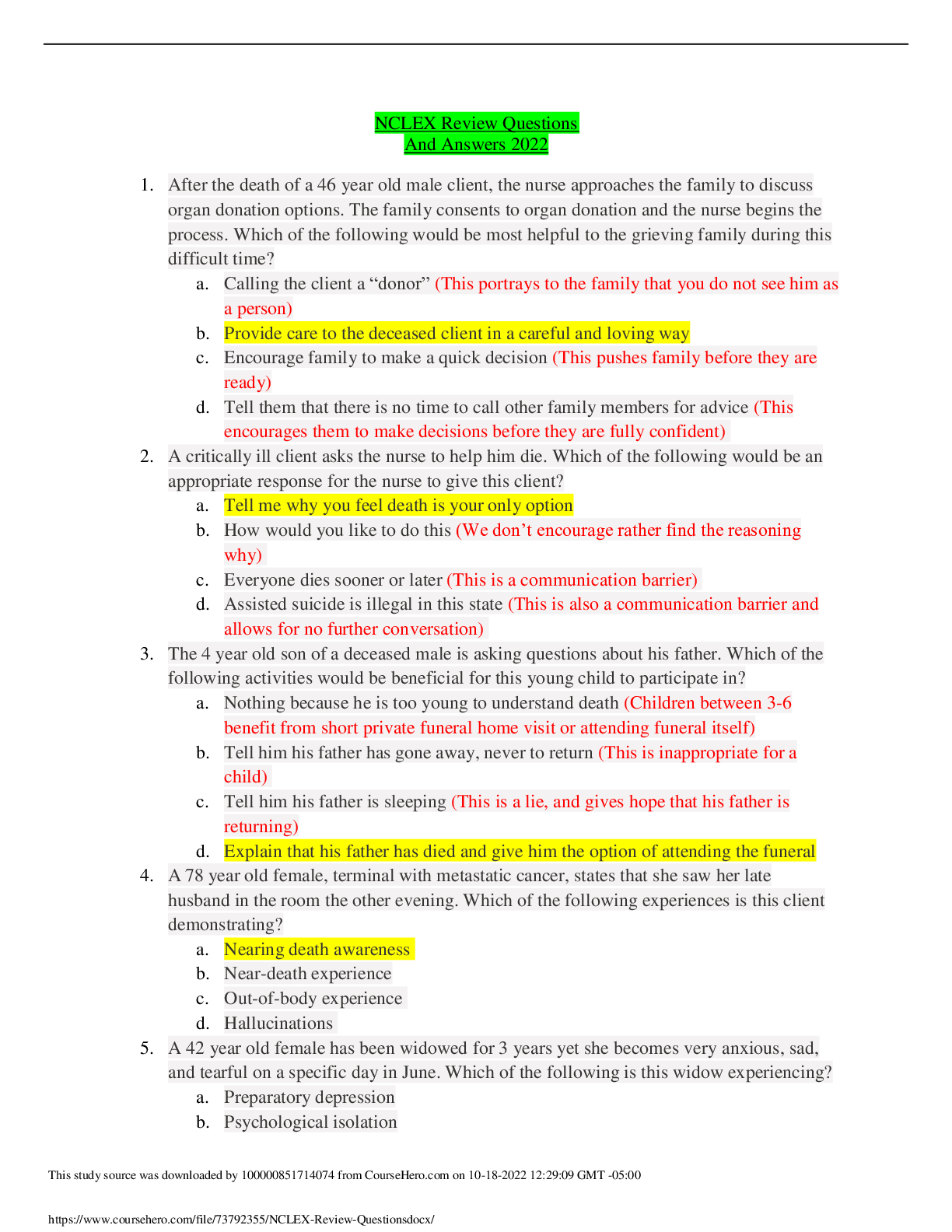
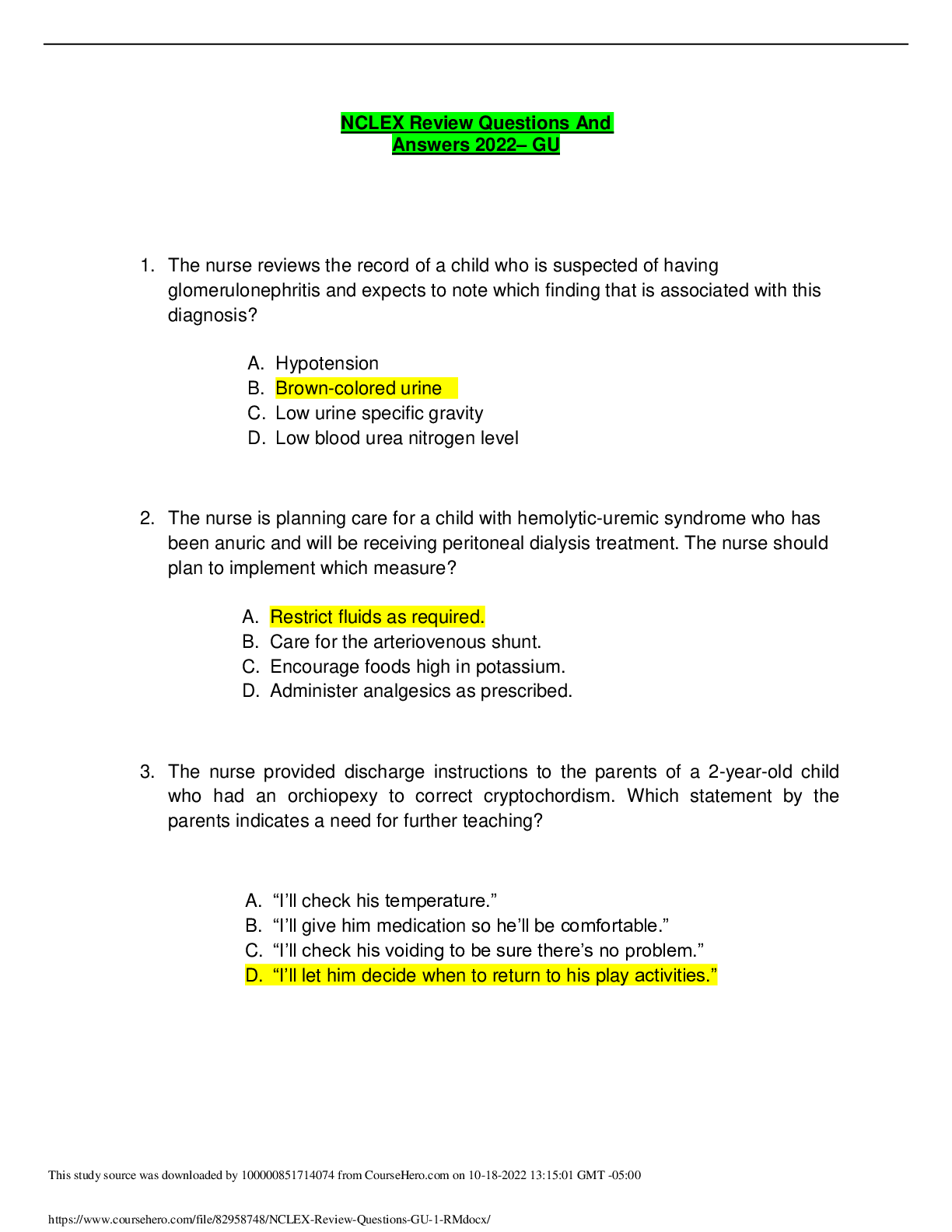
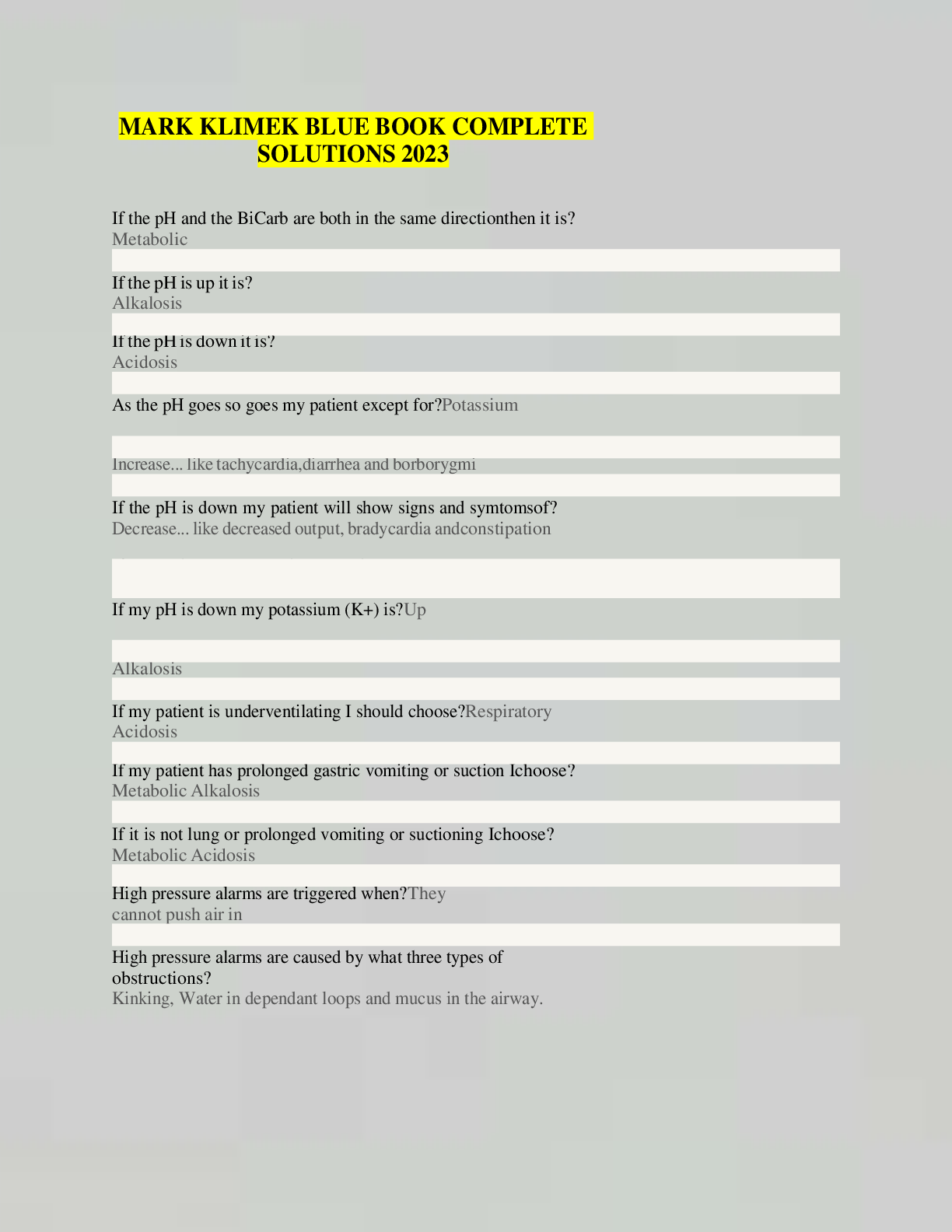
GASTRO NCLEX QUESTIONS AND ANSWERS LATEST UPDATE 2022/2023 Which of the following complications is thought to be the most common cause of appendicitis? A. A fecalith B. Bowel kinking C. Intern... al bowel occlusion D. Abdominal bowel swelling - ANS-A. A fecalith is a fecal calculus, or stone, that occludes the lumen of the appendix and is the most common cause of appendicitis. Bowel wall swelling, kinking of the appendix, and external occlusion, not internal occlusion, of the bowel by adhesions can also be causes of appendicitis. Which of the following terms best describes the pain associated with appendicitis? A. Aching B. Fleeting C. Intermittent D. Steady - ANS-D. The pain begins in the epigastrium or periumbilical region, then shifts to the right lower quadrant and becomes steady. The pain may be moderate to severe. Which of the following nursing interventions should be implemented to manage a client with appendicitis? A. Assessing for pain B. Encouraging oral intake of clear fluids C. Providing discharge teaching D. Assessing for symptoms of peritonitis - ANS-D. The focus of care is to assess for peritonitis, or inflammation of the peritoneal cavity. Peritonitis is most commonly caused by appendix rupture and invasion of bacteria, which could be lethal. The client with appendicitis will have pain that should be controlled with analgesia. The nurse should discourage oral intake in preparation of surgery. Discharge teaching is important; however, in the acute phase, management should focus on minimizing preoperative complications and recognizing when such may be occurring. Which of the following definitions best describes gastritis? A. Erosion of the gastric mucosa B. Inflammation of a diverticulum C. Inflammation of the gastric mucosa D. Reflux of stomach acid into the esophagus - ANS-C. Gastritis is an inflammation of the gastric mucosa that may be acute (often resulting from exposure to local irritants) or chronic (associated with autoimmune infections or atrophic disorders of the stomach). Erosion of the mucosa results in ulceration. Inflammation of a diverticulum is called diverticulitis; reflux of stomach acid is known as gastroesophageal disease. Which of the following substances is most likely to cause gastritis? A. Milk B. Bicarbonate of soda, or baking soda C. Enteric coated aspirin D. Nonsteriodal anti-imflammatory drugs - ANS-D. NSAIDS are a common cause of gastritis because they inhibit prostaglandin synthesis. Milk, once thought to help gastritis, has little effect on the stomach mucosa. Bicarbonate of soda, or baking soda, may be used to neutralize stomach acid, but it should be used cautiously because it may lead to metabolic acidosis. ASA with enteric coating shouldn't contribute significantly to gastritis because the coating limits the aspirin's effect on the gastric mucosa. Which of the following definitions best describes diverticulosis? A. An inflamed outpouching of the intestine B. A noninflamed outpouching of the intestine C. The partial impairment of the forward flow of intestinal contents D. An abnormal protrusion of an organ through the structure that usually holds it. - ANS-B. Diverticulosis involves a noninflamed outpouching of the intestine. Diverticulitis involves an inflamed outpouching. The partial impairment of forward flow of the intestine is an obstruction; abnormal protrusion of an organ is a hernia. Which of the following types of diets is implicated in the development of diverticulosis? A. Low-fiber diet B. High-fiber diet C. High-protein diet D. Low-carbohydrate diet - ANS-A. Low-fiber diets have been implicated in the development of diverticula because these diets decrease the bulk in the stool and predispose the person to the development of constipation. A high-fiber diet is recommended to help prevent diverticulosis. A high-protein or low-carbohydrate diet has no effect on the development of diverticulosis. Which of the following mechanisms can facilitate the development of diverticulosis into diverticulitis? A. Treating constipation with chronic laxative use, leading to dependence on laxatives B. Chronic constipation causing an obstruction, reducing forward flow of intestinal contents C. Herniation of the intestinal mucosa, rupturing the wall of the intestine D. Undigested food blocking the diverticulum, predisposing the area to bacteria invasion. - ANS-D. Undigested food can block the diverticulum, decreasing blood supply to the area and predisposing the area to invasion of bacteria. Chronic laxative use is a common problem in elderly clients, but it doesn't cause diverticulitis. Chronic constipation can cause an obstruction—not diverticulitis. Herniation of the intestinal mucosa causes an intestinal perforation. Which of the following symptoms indicated diverticulosis? A. No symptoms exist B. Change in bowel habits C. Anorexia with low-grade fever D. Episodic, dull, or steady midabdominal pain - ANS-A. Diverticulosis is an asymptomatic condition. The other choices are signs and symptoms of diverticulitis. Which of the following tests should be administered to a client suspected of having diverticulosis? A. Abdominal ultrasound B. Barium enema C. Barium swallow D. Gastroscopy - ANS-B. A barium enema will cause diverticula to fill with barium and be easily seen on x-ray. An abdominal US can tell more about structures, such as the gallbladder, liver, and spleen, than the intestine. A barium swallow and gastroscopy view upper GI structures. Medical management of the client with diverticulitis should include which of the following treatments? A. Reduced fluid intake B. Increased fiber in diet C. Administration of antibiotics D. Exercises to increase intra-abdominal pressur - ANS-C. Antibiotics are used to reduce the inflammation. The client isn't typically isn't allowed anything orally until the acute episode subsides. Parenteral fluids are given until the client feels better; then it's recommended that the client drink eight 8-ounce glasses of water per day and gradually increase fiber in the diet to improve intestinal motility. During the acute phase, activities that increase intra-abdominal pressure should be avoided to decrease pain and the chance of intestinal obstruction... [Show More]
Last updated: 1 year ago
Preview 1 out of 33 pages
Reviews( 0 )
Document information
Connected school, study & course
About the document
Uploaded On
Sep 26, 2022
Number of pages
33
Written in
Additional information
This document has been written for:
Uploaded
Sep 26, 2022
Downloads
0
Views
29

 (1).png)