100 Burn / fluid balance NCLEX Question latest update 2021(A level work)
Document Content and Description Below
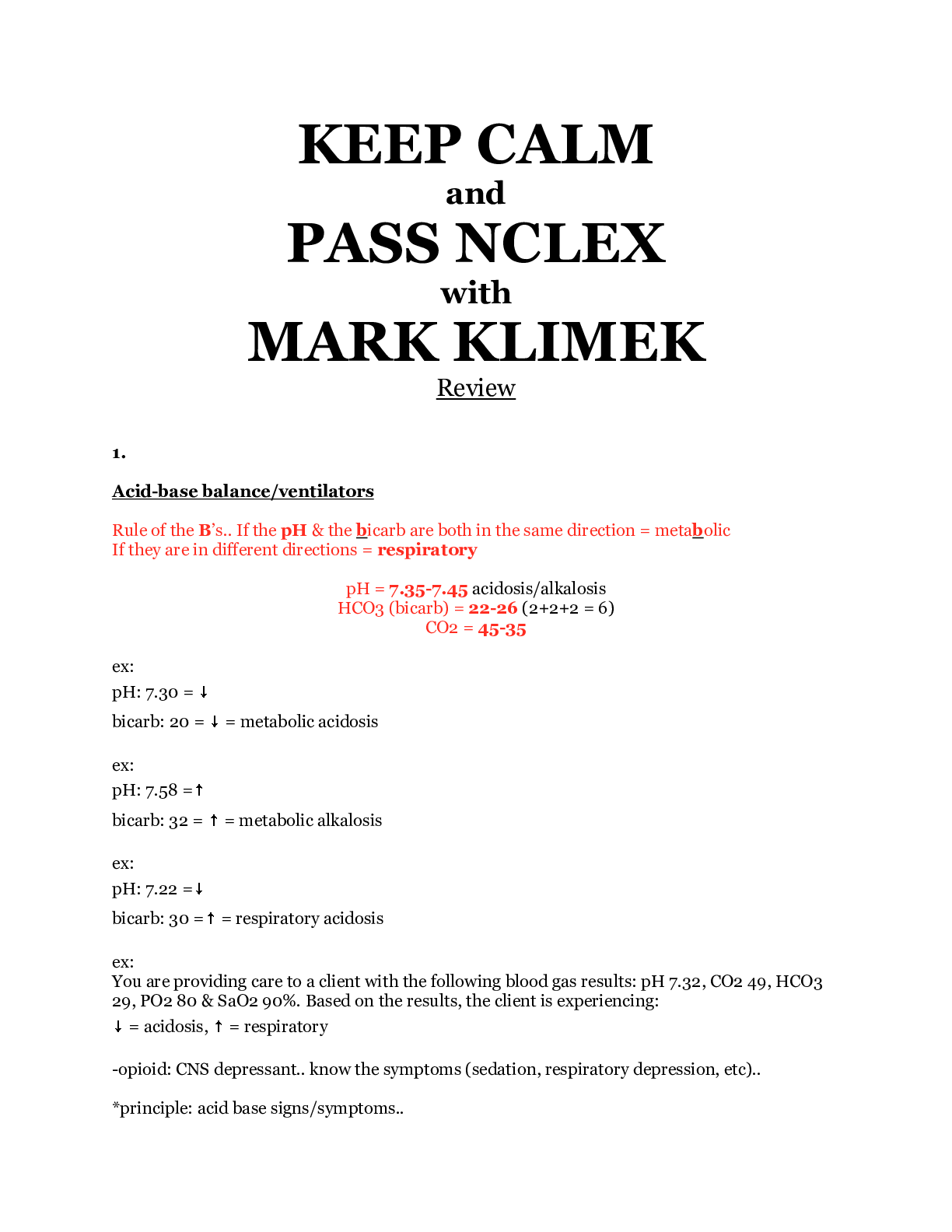
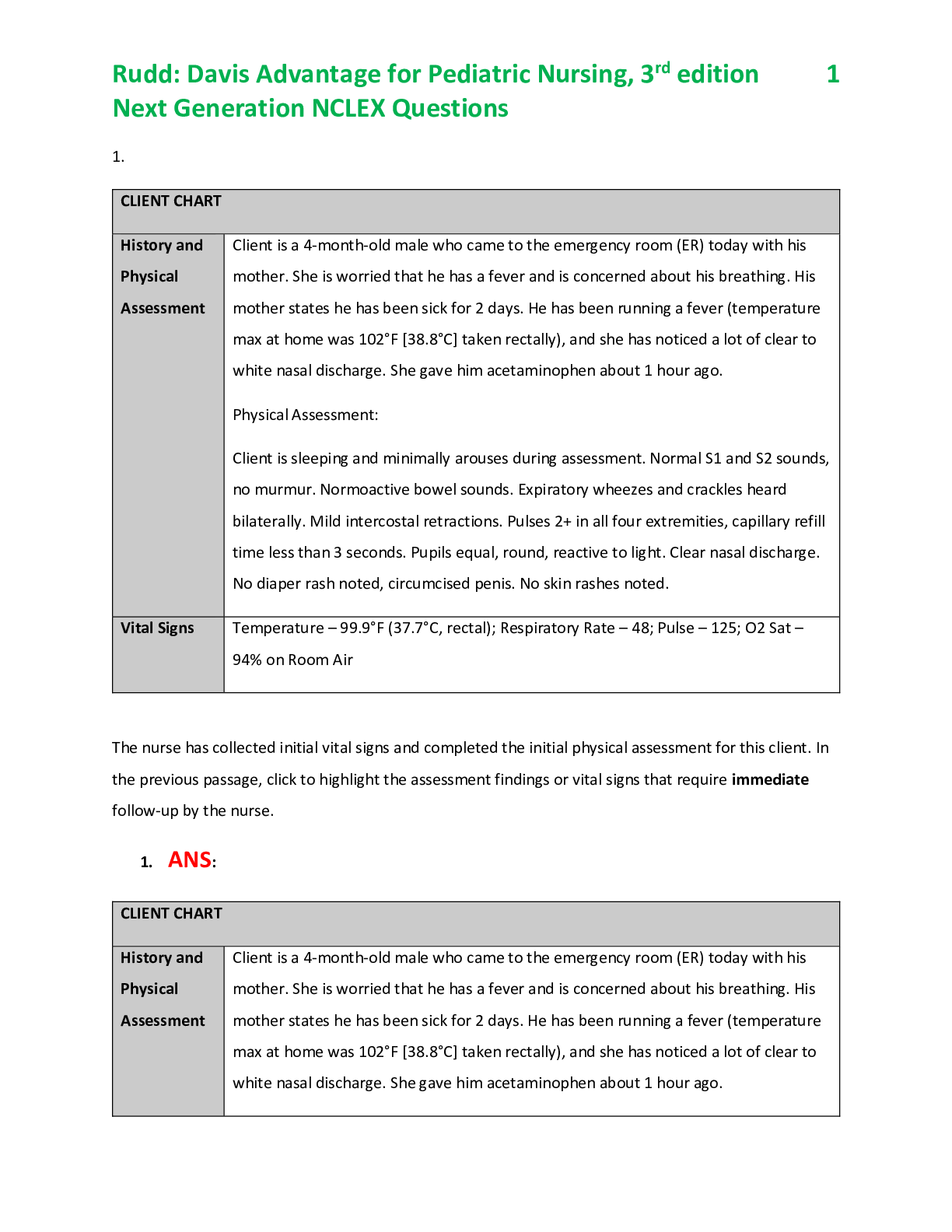
100 Burn / fluid balance NCLEX Question 1. The newly admitted client has burns on both legs. The burned areas appear white and leather-like. No blisters or bleeding are present, and the client stat... es that he or she has little pain. How should this injury be categorized? A. Superficial B. Partial-thickness superficial C. Partial-thickness deep D. Full thickness 2. The newly admitted client has a large burned area on the right arm. The burned area appears red, has blisters, and is very painful. How should this injury be categorized? A. Superficial B. Partial-thickness superficial C. Partial-thickness deep D. Full thickness 3. The burned client newly arrived from an accident scene is prescribed to receive 4 mg of morphine sulfate by IV push. What is the most important reason to administer the opioid analgesic to this client by the intravenous route? A. The medication will be effective more quickly than if given intramuscularly. B. It is less likely to interfere with the client’s breathing and oxygenation. C. The danger of an overdose during fluid remobilization is reduced. D. The client delayed gastric emptying. 4. Which vitamin deficiency is most likely to be a long-term consequence of a full-thickness burn injury? A. Vitamin A B. Vitamin B C. Vitamin C D. Vitamin D 5. Which client factors should alert the nurse to potential increased complications with a burn injury? A. The client is a 26-year-old male. B. The client has had a burn injury in the past. C. The burned areas include the hands and perineum. D. The burn took place in an open field and ignited the client’s clothing. 6. The burned client is ordered to receive intravenous cimetidine, an H2 histamine blocking agent, during the emergent phase. When the client’s family asks why this drug is being given, what is the nurse’s best response? A. “To increase the urine output and prevent kidney damage.” B. “To stimulate intestinal movement and prevent abdominal bloating.” C. “To decrease hydrochloric acid production in the stomach and prevent ulcers.” D. “To inhibit loss of fluid from the circulatory system and prevent hypovolemic shock.” 7. At what point after a burn injury should the nurse be most alert for the complication of hypokalemia? A. Immediately following the injury B. During the fluid shift C. During fluid remobilization D. During the late acute phase 8. What clinical manifestation should alert the nurse to possible carbon monoxide poisoning in a client who experienced a burn injury during a house fire? A. Pulse oximetry reading of 80% B. Expiratory stridor and nasal flaring C. Cherry red color to the mucous membranes D. Presence of carbonaceous particles in the sputum 9. What clinical manifestation indicates that an escharotomy is needed on a circumferential extremity burn? A. The burn is full thickness rather than partial thickness. B. The client is unable to fully pronate and supinate the extremity. C. Capillary refill is slow in the digits and the distal pulse is absent. D. The client cannot distinguish the sensation of sharp versus dull in the extremity. 10. What additional laboratory test should be performed on any African American client who sustains a serious burn injury? A. Total protein B. Tissue type antigens C. Prostate-specific antigen D. Hemoglobin S electrophoresis 11. Which type of fluid should the nurse expect to prepare and administer as fluid resuscitation during the emergent phase of burn recovery? A. Colloids B. Crystalloids C. Fresh-frozen plasma D. Packed red blood cells 12. The client with a dressing covering the neck is experiencing some respiratory difficulty. What is the nurse’s best first action? A. Administer oxygen. B. Loosen the dressing. C. Notify the emergency team. D. Document the observation as the only action. 13. The client who experienced an inhalation injury 6 hours ago has been wheezing. When the client is assessed, wheezes are no longer heard. What is the nurse’s best action? A. Raise the head of the bed. B. Notify the emergency team. C. Loosen the dressings on the chest. D. Document the findings as the only action. 14. Ten hours after the client with 50% burns is admitted, her blood glucose level is 90 mg/dL. What is the nurse’s best action? A. Notify the emergency team. B. Document the finding as the only action. C. Ask the client if anyone in her family has diabetes mellitus. D. Slow the intravenous infusion of dextrose 5% in Ringer’s lactate. 15. On admission to the emergency department the burned client’s blood pressure is 90/60, with an apical pulse rate of 122. These findings are an expected result of what thermal injury–related response? A. Fluid shift B. Intense pain C. Hemorrhage D. Carbon monoxide poisoning 16. Twelve hours after the client was initially burned, bowel sounds are absent in all four abdominal quadrants. What is the nurse’s best action? A. Reposition the client onto the right side. B. Document the finding as the only action. C. Notify the emergency team. D. Increase the IV flow rate. 17. Which clinical manifestation indicates that the burned client is moving into the fluid remobilization phase of recovery? A. Increased urine output, decreased urine specific gravity B. Increased peripheral edema, decreased blood pressure C. Decreased peripheral pulses, slow capillary refill D. Decreased serum sodium level, increased hematocrit 18. What is the priority nursing diagnosis during the first 24 hours for a client with full-thickness chemical burns on the anterior neck, chest, and all surfaces of the left arm? A. Risk for Ineffective Breathing Pattern B. Decreased Tissue Perfusion C. Risk for Disuse Syndrome D. Disturbed Body Image 19. All of the following laboratory test results on a burned client’s blood are present during the emergent phase. Which result should the nurse report to the physician immediately? A. Serum sodium elevated to 131 mmol/L (mEq/L) B. Serum potassium 7.5 mmol/L (mEq/L) C. Arterial pH is 7.32 D. Hematocrit is 52% 20. The client has experienced an electrical injury, with the entrance site on the left hand and the exit site on the left foot. What are the priority assessment data to obtain from this client on admission? A. Airway patency B. Heart rate and rhythm C. Orientation to time, place, and person D. Current range of motion in all extremities 21. In assessing the client’s potential for an inhalation injury as a result of a flame burn, what is the most important question to ask the client on admission? A. “Are you a smoker?” B. “When was your last chest x-ray?” C. “Have you ever had asthma or any other lung problem?” D. “In what exact place or space were you when you were burned?” 22. Which information obtained by assessment ensures that the client’s respiratory efforts are currently adequate? A. The client is able to talk. B. The client is alert and oriented. C. The client’s oxygen saturation is 97%. D. The client’s chest movements are uninhibited 23. Which information obtained by assessment ensures that the client’s respiratory efforts are currently adequate? A. The client is able to talk. B. The client is alert and oriented. C. The client’s oxygen saturation is 97%. D. The client’s chest movements are uninhibited 24. The burned client’s family ask at what point the client will no longer be at increased risk for infection. What is the nurse’s best response? A. “When fluid remobilization has started.” B. “When the burn wounds are closed.” C. “When IV fluids are discontinued.” D. “When body weight is normal.” 25. The burned client relates the following history of previous health problems. Which one should alert the nurse to the need for alteration of the fluid resuscitation plan? A. Seasonal asthma B. Hepatitis B 10 years ago C. Myocardial infarction 1 year ago D. Kidney stones within the last 6 month 26. The burned client on admission is drooling and having difficulty swallowing. What is the nurse’s best first action? A. Assess level of consciousness and pupillary reactions. B. Ask the client at what time food or liquid was last consumed. C. Auscultate breath sounds over the trachea and mainstem bronchi. D. Measure abdominal girth and auscultate bowel sounds in all four quadrants. 27. Which intervention is most important for the nurse to use to prevent infection by cross-contamination in the client who has open burn wounds? A. Handwashing on entering the client’s room B. Encouraging the client to cough and deep breathe C. Administering the prescribed tetanus toxoid vaccine D. Changing gloves between cleansing different burn areas 28. In reviewing the burned client’s laboratory report of white blood cell count with differential, all the following results are listed. Which laboratory finding indicates the possibility of sepsis? A. The total white blood cell count is 9000/mm3. B. The lymphocytes outnumber the basophils. C. The “bands” outnumber the “segs.” D. The monocyte count is 1,800/mm3. 29. The client has a deep partial-thickness injury to the posterior neck. Which intervention is most important to use during the acute phase to prevent contractures associated with this injury? A. Place a towel roll under the client’s neck or shoulder. B. Keep the client in a supine position without the use of pillows. C. Have the client turn the head from side to side 90 degrees every hour while awake. D. Keep the client in a semi-Fowler’s position and actively raise the arms above the head every hour while awake. 30. The client has severe burns around the right hip. Which position is most important to be emphasized by the nurse that the client maintains to retain maximum function of this joint? A. Hip maintained in 30-degree flexion, no knee flexion B. Hip flexed 90 degrees and knee flexed 90 degrees C. Hip, knee, and ankle all at maximum flexion D. Hip at zero flexion with leg flat 31. During the acute phase, the nurse applied gentamicin sulfate (topical antibiotic) to the burn before dressing the wound. The client has all the following manifestations. Which manifestation indicates that the client is having an adverse reaction to this topical agent? A. Increased wound pain 30 to 40 minutes after drug application B. Presence of small, pale pink bumps in the wound beds C. Decreased white blood cell count D. Increased serum creatinine level 32. The client, who is 2 weeks postburn with a 40% deep partial-thickness injury, still has open wounds. On taking the morning vital signs, the client is found to have a below-normal temperature, is hypotensive, and has diarrhea. What is the nurse’s best action? A. Nothing, because the findings are normal for clients during the acute phase of recovery. B. Increase the temperature in the room and increase the IV infusion rate. C. Assess the client’s airway and oxygen saturation. D. Notify the burn emergency team. 33. Which intervention is most important to use to prevent infection by autocontamination in the burned client during the acute phase of recovery? A. Changing gloves between wound care on different parts of the client’s body. B. Avoiding sharing equipment such as blood pressure cuffs between clients. C. Using the closed method of burn wound management. D. Using proper and consistent handwashing. 34. When should ambulation be initiated in the client who has sustained a major burn? A. When all full-thickness areas have been closed with skin grafts B. When the client’s temperature has remained normal for 24 hours C. As soon as possible after wound debridement is complete D. As soon as possible after resolution of the fluid shift 35. What statement by the client indicates the need for further discussion regarding the outcome of skin grafting (allografting) procedures? A. “For the first few days after surgery, the donor sites will be painful.” B. “Because the graft is my own skin, there is no chance it won’t ‘take’.” C. “I will have some scarring in the area when the skin is removed for grafting.” D. “Once all grafting is completed, my risk for infection is the same as it was before I was burned.” 36. Which statement by the client indicates a correct understanding of rehabilitation after burn injury? A. “I will never be fully recovered from the burn.” B. “I am considered fully recovered when all the wounds are closed.” C. “I will be fully recovered when I am able to perform all the activities I did before my injury.” D. “I will be fully recovered when I achieve the highest possible level of functioning that I can.” 37. Which statement made by the client with facial burns who has been prescribed to wear a facial mask pressure garment indicates a correct understanding of the purpose of this treatment? A. “After this treatment, my ears will not stick out.” B. “The mask will help protect my skin from sun damage.” C. “Using this mask will prevent scars from being permanent.” D. “My facial scars should be less severe with the use of this mask.” 38. What is the priority nursing diagnosis for a client in the rehabilitative phase of recovery from a burn injury? A. Acute Pain B. Impaired Adjustment C. Deficient Diversional Activity D. Imbalanced Nutrition: Less than Body Requirements 39. Nurse Faith should recognize that fluid shift in an client with burn injury results from increase in the: A. Total volume of circulating whole blood B. Total volume of intravascular plasma C. Permeability of capillary walls D. Permeability of kidney tubules 40. Louie, with burns over 35% of the body, complains of chilling. In promoting the client’s comfort, the nurse should: A. Maintain room humidity below 40% B. Place top sheet on the client C. Limit the occurrence of drafts D. Keep room temperature at 80 degrees 41. Patient X is diagnosed with constipation. As a knowledgeable nurse, which nursing intervention is appropriate for maintaining normal bowel function? A. Assessing dietary intake B. Decreasing fluid intake C. Providing limited physical activity D. Turning, coughing, and deep breathing 42. A 12-year-old boy was admitted in the hospital two days ago due to hyperthermia. His attending nurse, Dennis, is quite unsure about his plan of care. Which of the following nursing intervention should be included in the care of plan for the client? A. Room temperature reduction B. Fluid restriction of 2,000 ml/day C. Axillary temperature measurements every 4 hours D. Antiemetic agent administration 43. Tom is ready to be discharged from the medical-surgical unit after 5 days of hospitalization. Which client statement indicates to the nurse that Tom understands the discharge teaching about cellular injury? A. “I do not have to see my doctor unless i have problems.” B. “I can stop taking my antibiotics once I am feeling better.” C. “If I have redness, drainage, or fever, I should call my healthcare provider.” D. “I can return to my normal activities as soon as I go home.” 44. Nurse Katee is caring for Adam, a 22-year-old client, in a long-term facility. Which nursing intervention would be appropriate when identifying nursing interventions aimed at promoting and preventing contractures? Select all that apply. A. Clustering activities to allow uninterrupted periods of rest B. Maintaining correct body alignment at all times C. Monitoring intake and output, using a urometer if necessary D. Using a footboard or pillows to keep feet in correct position E. Performing active and passive range-of-motion exercises F. Weighing the client daily at the same time and in the same clothes 45. A 36-year-old male client is about to be discharged from the the hospital after 5 days due to surgery. Which intervention should be included in the home health care nurse’s instructions about measures to prevent constipation? A. Discouraging the client from eating large amounts of roughage-containing foods in the diet. B. Encouraging the client to use laxatives routinely to ensure adequate bowel elimination. C. Instructing the client to establish a bowel evacuation schedule that changes every day. D. Instructing the client to fill a 2-L bottle with water every night and drink it the next day. 46. Mr. McPartlin suffered abrasions and lacerations after a vehicular accident. He was hospitalized and was treated for a couple of weeks. When planning care for a client with cellular injury, the nurse should consider which scientific rationale? A. Nutritional needs remain unchanged for the well-nourished adult. B. Age is an insignificant factor in cellular repair. C. The presence of infection may slow the healing process. D. Tissue with inadequate blood supply may heal faster. 47. A 22-year-old lady is displaying facial grimaces during her treatment in the hospital due to burn trauma. Which nursing intervention should be included for reducing pain due to cellular injury? A. Administering anti-inflammatory agents as prescribed B. Elevating the injured area to decrease venous return to the heart C. Keeping the skin clean and dry D. Applying warm packs initially to reduce edema 48. Lisa, a client with altered urinary function, is under the care of nurse Tine. Which intervention is appropriate to include when developing a plan of care for Lisa who is experiencing urinary dribbling? A. Inserting an indwelling Foley catheter B. Having the client perform Kegel exercises C. Keeping the skin clean and dry D. Using pads or diapers on the client 49. Jeron is admitted in the hospital due to bacterial pneumonia. He is febrile, diaphoretic, and has shortness of breath and asthma. Which goal is the most important for the client? A. Prevention of fluid volume excess B. Maintenance of adequate oxygenation C. Education about infection prevention D. Pain reduction 50. Rogelio, a 32-year-old patient, is about to be discharged from the acute care setting. Which nursing intervention is the most important to include in the plan of care? A. Stress-reduction techniques B. Home environment evaluation C. Skin-care measures D. Participation in activities of daily living 51. Mrs. dela Riva is in her first trimester of pregnancy. She has been lying all day because her OB-GYN requested her to have a complete bed rest. Which nursing intervention is appropriate when addressing the client’s need to maintain skin integrity? A. Monitoring intake and output accurately B. Instructing the client to cough and deep-breathe every 2 hours C. Keeping the linens dry and wrinkle free D. Using a foot board to maintain correct anatomic position 52. Maya, who is admitted in a hospital, is scheduled to have her general checkup and physical assessment. Nurse Timothy observed a reddened area over her left hip. Which should the nurse do first? A. Massage the reddened are for a few minutes B. Notify the physician immediately C. Arrange for a pressure-relieving device D. Turn the client to the right side for 2 hours 53. Pierro was noted to be displaying facial grimaces after nurse Kara assessed his complaints of pain rated as 8 on a scale of 1 (no pain) 10 10 (worst pain). Which intervention should the nurse do? A. Administering the client’s ordered pain medication immediately B. Using guided imagery instead of administering pain medication C. Using therapeutic conversation to try to discourage pain medication D. Attempting to rule out complications before administering pain medication 54. Nurse Marthia is teaching her students about bacterial control. Which intervention is the most important factor in preventing the spread of microorganism? A. Maintenance of asepsis with indwelling catheter insertion B. Use of masks, gowns, and gloves when caring for clients with infection C. Correct handwashing technique D. Cleanup of blood spills with sodium hydrochloride 55. A patient with tented skin turgor, dry mucous membranes, and decreased urinary output is under nurse Mark’s care. Which nursing intervention should be included the care plan of Mark for his patient? A. Administering I.V. and oral fluids B. Clustering necessary activities throughout the day C. Assessing color, odor, and amount of sputum D. Monitoring serum albumin and total protein levels 56. Khaleesi is admitted in the hospital due to having lower than normal potassium level in her bloodstream. Her medical history reveals vomiting and diarrhea prior to hospitalization. Which foods should the nurse instruct the client to increase? A. Whole grains and nuts B. Milk products and green, leafy vegetables C. Pork products and canned vegetables D. Orange juice and bananas 57. Mary Jean, a first year nursing student, was rushed to the clinic department due to hyperventilation. Which nursing intervention is the most appropriate for the client who is subsequently developing respiratory alkalosis? A. Administering sodium chloride I.V. B. Encouraging slow, deep breaths C. Preparing to administer sodium bicarbonate D. Administer low-flow oxygen therapy 58. Nurse John Joseph is totaling the intake and output for Elena Reyes, a client diagnosed with septicemia who is on a clear liquid diet. The client intakes 8 oz of apple juice, 850 ml of water, 2 cups of beef broth, and 900 ml of half-normal saline solution and outputs 1,500 ml of urine during the shift. How many milliliters should the nurse document as the client’s intake. A. 2,230 B. 2,740 C. 2,470 D. 2,320 59. Marie Joy’s lab test revealed that her serum calcium is 2.5 mEq/L. Which assessment data does the nurse document when a client diagnosed with hypocalcemia develops a carpopedal spasm after the blood-pressure cuff is inflated? A. Positive Trousseau’s sign B. Positive Chvostek’s sign C. Tetany D. Paresthesia 60. Lab tests revealed that patient Z’s [Na+] is 170 mEq/L. Which clinical manifestation would nurse Natty expect to assess? A. Tented skin turgor and thirst B. Muscle twitching and tetany C. Fruity breath and Kussmaul’s respirations D. Muscle weakness and paresthesia 61. Mang Teban has a history of chronic obstructive pulmonary disease and has the following arterial blood gas results: partial pressure of oxygen (PO2), 55 mm Hg, and partial pressure of carbon dioxide (PCO2), 60 mm Hg. When attempting to improve the client’s blood gas values through improved ventilation and oxygen therapy, which is the client’s primary stimulus for breathing? A. High PCO2 B. Low PO2 C. Normal pH D. Normal bicarbonate (HCO3) 62. A client with very dry mouth, skin and mucous membranes is diagnosed of having dehydration. Which intervention should the nurse perform when caring for a client diagnosed with fluid volume deficit? A. Assessing urinary intake and output B. Obtaining the client’s weight weekly at different times of the day C. Monitoring arterial blood gas (ABG) results D. Maintaining I.V. therapy at the keep-vein-open rate 63. Which client situation requires the nurse to discuss the importance of avoiding foods high in potassium? A. 14-year-old Elena who is taking diuretics B. 16-year-old John Joseph with ileostomy C. 16-year-old Gabriel with metabolic acidosis D. 18-year-old Albert who has renal disease 64. Genevieve is diagnosed with hypomagnesemia, which nursing intervention would be appropriate? A. Instituting seizure precaution to prevent injury B. Instructing the client on the importance of preventing infection C. Avoiding the use of tight tourniquet when drawing blood D. Teaching the client the importance of early ambulation 65. Which electrolyte would the nurse identify as the major electrolyte responsible for determining the concentration of the extracellular fluid? A. Potassium B. Phosphate C. Chloride D. Sodium 66. Jon has a potassium level of 6.5 mEq/L, which medication would nurse Wilma anticipate? A. Potassium supplements B. Kayexalate C. Calcium gluconate D. Sodium tablets 67. Which clinical manifestation would lead the nurse to suspect that a client is experiencing hypermagnesemia? A. Muscle pain and acute rhabdomyolysis B. Hot, flushed skin and diaphoresis C. Soft-tissue calcification and hyperreflexia D. Increased respiratory rate and depth 68. Joshua is receiving furosemide and Digoxin, which laboratory data would be the most important to assess in planning the care for the client? A. Sodium level B. Magnesium level C. Potassium level D. Calcium level 69. Mr. Salcedo has the following arterial blood gas (ABG) values: pH of 7.34, partial pressure of arterial oxygen of 80 mm Hg, partial pressure of arterial carbon dioxide of 49 mm Hg, and a bicarbonate level of 24 mEq/L. Based on these results, which intervention should the nurse implement? A. Instructing the client to breathe slowly into a paper bag B. Administering low-flow oxygen C. Encouraging the client to cough and deep breathe D. Nothing, because these ABG values are within normal limits. 70. A client is diagnosed with metabolic acidosis, which would the nurse expect the health care provider to order? A. Potassium B. Sodium bicarbonate C. Serum sodium level D. Bronchodilator 71.The net diffusion of water from one solution of water from one solution through a semipermeable membrane to another solution containing a lower concentration of water is termed: A. filtration B. diffusion C. osmosis D. brownian motion 72. When assessing a patient’s total body water percentage, the nurse is aware that all of the following factors influence this except: A. age B. fat tissue C. muscle mass D. gender 73. Orly Khan is suffering from fluid volume deficit (FVD), which of the following symptoms would the nurse expect to assess in the patient? A. rales B. bounding pulse C. tachycardia D. bulging neck veins 74. John Reid is admitted in the hospital and is currently receiving hypertonic fluids. Nursing management for the client includes monitoring for all of the following potential complications except: A. water intoxication B. fluid volume excess (FVE) C. cellular dehydration D. cell shrinkage 75. Mr. Wenceslao is scheduled to receive an isotonic solution; which one of the following is an example of such solution? A. D10% W B. 0.45% saline C. 0.9% saline D. 3% normal saline W 76. Which of the following arterial blood gas (ABG) values indicates uncompensated metabolic alkalosis? A. pH 7.48, PaCO2 42, HCO3 30 B. pH 7.48, PaCO2 46, HCO3 30 C. pH 7.48, PaCO2 34, HCO3 20 D. pH 7.48, PaCO2 34, HCO3 26 77. The body’s compensation of metabolic alkalosis involves: A. increasing the respiratory rate B. decreasing the respiratory rate C. increasing urine output D. decreasing urine output 78. When assessing a patient for metabolic alkalosis, the nurse would expect to find: A. low serum potassium B. changes in urine output C. hypotension D. increased CVP 79. Which of the following blood products should be infused rapidly? A. packed red blood cells (PRBC) B. fresh frozen plasma (FFP) C. platelets D. dextran 80. Which of the following statements provides the rationale for using a hypotonic solution for a patient with FVD? A. A hypotonic solution provides free water to help the kidneys eliminate the solute. B. A hypotonic solution supplies an excess of sodium and chloride ions. C. Excessive volumes are recommended in the early postoperative period. D. A hypotonic solution is used to treat hyponatremia. 81. Redd is receiving a blood transfusion. When monitoring the patient, the nurse would analyze an elevated body temperature as indicating: A. a normal physiologic process B. evidence of sepsis C. a possible transfusion reaction D. an expected response to the transfusion 82. The process of endocrine regulation of electrolytes involves: A. sodium reabsorption and chloride excretion B. chloride reabsorption and sodium excretion C. potassium reabsorption and sodium excretion D. sodium reabsorption and potassium excretion 83. The chief anion in the intracellular fluid (ICF) is: A. phosphorus B. potassium C. sodium D. chloride 84. The major cation in the ICF is: A. potassium B. sodium C. phosphorus D. magnesium 85. Hypophosphatemia may result from which of the following diseases? A. liver cirrhosis B. renal failure C. Paget’s disease D. alcoholism 86. A patient with which of the following disorders is at high risk for developing hyperphosphatemia? A. hyperkalemia B. hyponatremia C. hypocalcemia D. hyperglycemia 87. Normal calcium levels must be analyzed in relation to: A. sodium B. glucose C. protein D. fats 88. Calcium is absorbed in the GI tract under the influence of: A. vitamin D B. glucose C. HCl D. vitamin C 89. Which of the following diagnoses is most appropriate for a patient with hypo calcemia? A. constipation, bowel B. high risk for injury: bleeding C. airway clearance, ineffective D. high risk for injury: confusion 90. When serum calcium levels rise, which of the following hormones is secreted? A. aldosterone B. renin C. parathyroid hormone D. calcitonin 91. The presence of which of the following electrolytes contributes to acidosis? A. sodium B. potassium C. hydrogen D. chloride 92. The lungs participate in acid-base balance by: A. reabsorbing bicarbonate B. splitting carbonic acid in two C. using CO2 to regulate hydrogen ions D. sending hydrogen ions to the renal tubules 93. The respiratory system regulates acid-base balance by: A. increasing mucus production B. changing the rate and depth of respirations C. forming bicarbonate D. reabsorbing bicarbonate 94. Which of the following is a gas component of the ABG measurement? A. carbon dioxide B. bicarbonate C. hydrogen D. pH 95. Chloride helps maintain acid-base balance by performing which of the following roles? A. participating in the chloride shift B. following sodium to maintain serum osmolarity C. maintaining the balance of cations in the ICF and ECF D. separating carbonic acid 96. Which of the following hormones helps regulate chloride reabsorption? A. antidiuretic hormone B. renin C. estrogen D. aldosterone 97. Chloride is absorbed in the: A. stomach B. bowel C. liver D. kidney 98. When chloride concentration drops below 95 mEq/L, reabsorption of which of the following electrolytes increases proportionally? A. hydrogen B. potassium C. sodium D. bicarbonate 99. Jonas is admitted with 1,000 ml of diarrhea per day for the last 3 days. An IV of 0.45% NaCl mixed with 5% dextrose is infusing. Which of the following nursing interventions is the most appropriate? A. Get an infusion controller from central supply. B. Mix all antibiotics in 0.45% NaCl with 5% dextrose. C. Check the patient’s potassium level and contact the doctor for IV additive orders. D. Assess the patient for signs of hyperkalemia. 100. Mrs. Waltraud is receiving digoxin and Lasix daily. Today, she complains of nausea, and her apical pulse is 130 and irregular. Which of the following nursing interventions is the most appropriate? A. Hold the digoxin and check the patient’s potassium level. B. Remove the orange juice from the patient’s tray. C. Identify the patient as high risk for hyperkalemia. D. Assess the patient for other signs of hypernatremia. [Show More]
Last updated: 1 year ago
Preview 1 out of 28 pages
Reviews( 0 )
Document information
Connected school, study & course
About the document
Uploaded On
Jan 12, 2021
Number of pages
28
Written in
Additional information
This document has been written for:
Uploaded
Jan 12, 2021
Downloads
0
Views
64


.png)