Health Care > TEST BANK > Test Bank for Bontragers Textbook of Radiographic Positioning and Related Anatomy 9th Edition Lampig (All)
Test Bank for Bontragers Textbook of Radiographic Positioning and Related Anatomy 9th Edition Lampignano
Document Content and Description Below
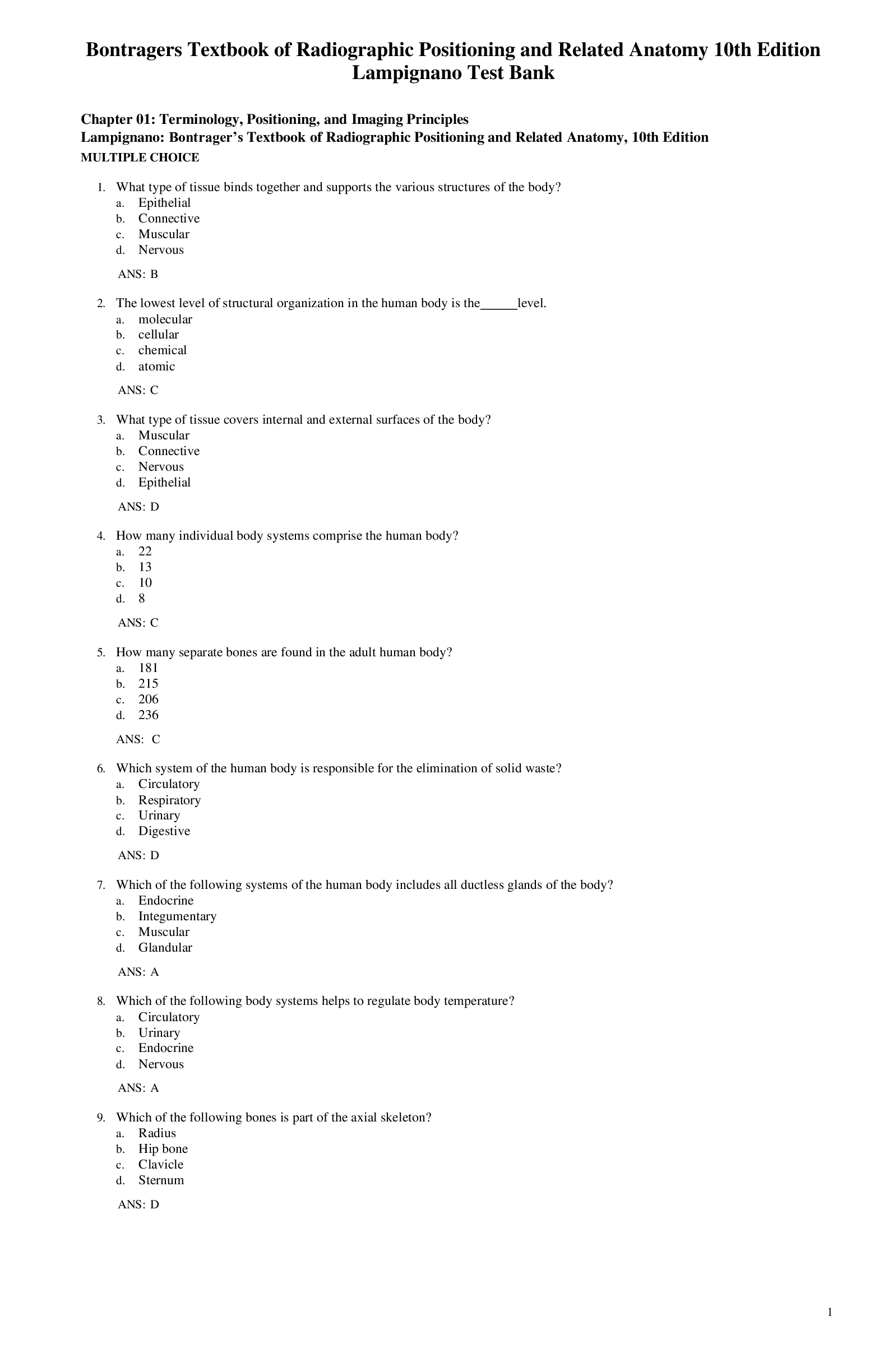
Test Bank for Bontragers Textbook of Radiographic Positioning and Related Anatomy 9th Edition Lampignano Test Bank for Bontragers Textbook of Radiographic Positioning and Related Anatomy 9th Edition L... ampignano Test Bank for Bontragers Textbook of Radiographic Positioning and Related Anatomy 9th Edition Lampignano Test Bank for Bontragers Textbook of Radiographic Positioning and Related Anatomy 9th Edition Lampignano Test Bank for Bontragers Textbook of Radiographic Positioning and Related Anatomy 9th Edition Lampignano Chapter 01: Terminology, Positioning, and Imaging Principles Lampignano: Bontrager’s Textbook of Radiographic Positioning and Related Anatomy, 10th Edition MULTIPLE CHOICE 1. What type of tissue binds together and supports the various structures of the body? a. Epithelial b. Connective c. Muscular d. Nervous ANS: B 2. The lowest level of structural organization in the human body is the _____ level. a. molecular b. cellular c. chemical d. atomic ANS: C 3. What type of tissue covers internal and external surfaces of the body? a. Muscular b. Connective c. Nervous d. Epithelial ANS: D 4. How many individual body systems comprise the human body? a. 22 b. 13 c. 10 d. 8 ANS: C 5. How many separate bones are found in the adult human body? a. 181 b. 215 c. 206 d. 236 ANS: C 6. Which system of the human body is responsible for the elimination of solid waste? a. Circulatory b. Respiratory c. Urinary d. Digestive ANS: D 7. Which of the following systems of the human body includes all ductless glands of the body? a. Endocrine b. Integumentary c. Muscular d. Glandular ANS: A 8. Which of the following body systems helps to regulate body temperature? a. Circulatory b. Urinary c. Endocrine d. Nervous ANS: A 9. Which of the following bones is part of the axial skeleton? a. Radius b. Hip bone c. Clavicle d. Sternum ANS: D 10. How many bones are there in the adult axial skeleton? a. 206 b. 80 c. 54 d. 126 ANS: B 11. What is the name of the small oval-shaped bone found in tendons? a. Wormian b. Tendinous c. Irregular d. Sesamoid ANS: D 12. Which of the following bones is classified as a long bone? a. Carpal bone b. Scapula c. Cranium d. Humerus ANS: D 13. What is the name of the dense fibrous membrane that covers bone? a. Cancellous portion b. Periosteum c. Diploë d. Medullary portion ANS: B 14. Which of the following bones is classified as a short bone? a. Vertebrae b. Phalanges (toes) c. Scapulae d. Carpal (wrist bones) ANS: D 15. Which of the following is a secondary growth center for endochondral ossification? a. Diaphysis b. Epiphyses c. Metaphysis d. Articular cartilage ANS: B 16. Which aspect of the long bones is responsible for the production of red blood cells? a. Compact bone b. Periosteum c. Medullary cavity d. Spongy or cancellous bone ANS: D 17. Examples of “flat” bones are the: a. calvaria, ribs, scapulae, and sternum. b. ribs, sternum, patella, and ilia of pelvis. c. sternum, scapulae, ilia of pelvis, and base of cranium. d. sternum and ilia of pelvis only. ANS: A 18. What is the primary center for bone growth termed? a. Epiphyses b. Diaphysis c. Metaphysis d. Epiphyseal plate ANS: B 19. Which of the following is NOT a functional classification of joints? a. Synarthrosis b. Amphiarthrosis c. Cartilaginous d. Diarthrosis ANS: C 20. The structural term for a freely movable joint is: a. fibrous. b. cartilaginous. c. synovial. d. gomphosis. ANS: C 21. Which of the following joints displays flexion and extension type of movement primarily? a. Pivot b. Ellipsoidal c. Saddle d. Ginglymus ANS: D 22. Which of the following joints is NOT a synovial joint? a. Skull sutures b. Elbow joint c. Hip joint d. Proximal radioulnar joint ANS: A 23. Which of the following is classified as a saddle (sellar) joint? a. Ankle joint b. Temporomandibular joint c. Knee joint d. Intercarpal joint ANS: A 24. Which of the following is classified as a bicondylar joint? a. Shoulder joint b. Temporomandibular joint c. First and second cervical vertebra joint d. Distal radioulnar joint ANS: B 25. An upright position with the arms abducted, palms forward, and head forward describes the _____ position. a. anteroposterior (AP) b. decubitus c. anatomic d. oblique ANS: C 26. A representation of the patient’s anatomic structures that can be obtained, viewed, manipulated, and stored digitally is the definition for: a. radiographic film. b. radiography. c. radiographic image. d. radiographic examination. ANS: C 27. The vertical plane that divides the body into equal right and left halves describes the _____ plane. a. coronal b. median or midsagittal c. longitudinal d. horizontal ANS: B 28. A longitudinal plane that divides the body into equal anterior and posterior parts is the _____ plane. a. midcoronal b. midsagittal c. horizontal d. oblique ANS: A 29. Which of the following terms describes the sole of the foot? a. Palmar b. Dorsum c. Volar d. Plantar ANS: D 30. Which term describes the back or posterior aspect of the hand? a. Dorsum pedis b. Dorsum manus c. Palmar d. Volar ANS: B 31. The position in which the head is lower than the feet: a. Trendelenburg. b. lithotomy. c. Fowler. d. recumbent. ANS: A 32. Which term describes lying down in any position? a. Horizontal b. Fowler c. Recumbent d. Anatomic ANS: C 33. A recumbent position in which the patient is lying on the right anterior surface with the body rotated toward the image receptor is termed: a. right posterior oblique. b. left anterior oblique. c. Sims’ position. d. Fowler position. ANS: A 34. A patient is lying on her back facing the x-ray tube. The right side of her body is turned 20 degrees toward the image receptor. What is this radiographic position? a. LPO (left posterior oblique) b. RPO (right posterior oblique) c. RAO (right anterior oblique) d. LAO (left anterior oblique) ANS: B 35. A patient is erect with the left side directly against the image receptor. The central ray (CR) enters the right side of the body. What is this radiographic position? a. Right lateral b. Left lateral decubitus c. Left lateral d. Dorsal decubitus ANS: C 36. A patient is lying on her back. The x-ray tube is horizontally directed with the CR entering the right side of the body. The image receptor is adjacent to the left side of the body. What is the radiographic position? a. Left lateral decubitus b. Left lateral c. Right lateral decubitus d. Dorsal decubitus ANS: D 37. A patient is erect facing the image receptor. The left side of the body is turned 45 degrees toward the image receptor. The CR enters the posterior aspect of the body and exits the anterior. What is this radiographic position? a. LAO b. LPO c. Left lateral d. Posteroanterior (PA) ANS: A 38. What type of projection is created with the CR directed along or parallel to the long axis of a structure or anatomic part? a. Axial b. Tangential c. Lordotic d. Transthoracic ANS: A 39. A projection in which the CR skims a body part to project it in profile is termed: a. tangential. b. lordotic. c. axial. d. decubitus. ANS: A 40. What is the general term for a position in which the long axis of the body is angled in relationship to the image receptor rather than the central ray (e.g., special chest projection)? a. Axial b. Trendelenburg c. Decubitus d. Lordotic ANS: D 41. The opposite term for supination is: a. protraction. b. adduction. c. pronation. d. retraction. ANS: C 42. Which of the following positions is often used to insert a rectal enema tip before a barium enema study? a. Fowler b. Modified Sims’ c. Lithotomy d. Trendelenburg ANS: B 43. A dorsoplantar projection would be a radiographic study of: a. any anatomic region. b. the hand. c. the foot. d. the skull. ANS: C 44. Moving the foot and toes downward is: a. eversion. b. inversion. c. dorsiflexion. d. plantar flexion. ANS: D 45. Movement in the form of a circle is the definition for: a. rotation. b. retraction. c. circumduction. d. protraction. ANS: C 46. Which of the following terms is the opposite of ipsilateral? a. Medial b. Deviation c. Contralateral d. Axiolateral ANS: C 47. The radiographic term projection is defined as: a. general position of the patient. b. path or direction of the central ray. c. radiographic image as seen from the vantage of the image receptor. d. computer-assisted image. ANS: B 48. Which of following is NOT one of the evaluation criteria applied in the evaluation of images? a. Patient condition b. Anatomy demonstrated c. Collimation and CR d. Exposure criteria ANS: A 49. A patient enters the emergency department (ED) with a piece of wire in the palm of the hand. What is the minimum number of projections required to be taken for this radiographic study? a. One b. Two c. Three d. Four or more ANS: B 50. Which of the following radiographic procedures often only requires a single AP projection be taken? a. Finger b. Ribs c. Chest d. Pelvis ANS: D 51. What is the final step taken before making the exposure during a positioning routine? a. Image receptor centering b. Placing anatomic markers on image receptor c. Ensuring correct gonadal shield placement d. Collimation adjustments ANS: C 52. What is the minimal number of projections taken for a study of the femur? a. One b. Two c. Three d. Four ANS: B 53. What is the minimal number of projections taken for a study of the right hip? a. One b. Two c. Three d. Four ANS: B 54. What is the minimal number of projections taken for a postreduction (to realign a fracture) study of the ankle? a. One b. Two c. Three d. Four ANS: B 55. What is the minimal number of projections taken for a study of the elbow? a. One b. Two c. Three d. Four ANS: C 56. A patient is erect with the left side of his chest placed against the image receptor. The central ray enters the right side of the upper chest and exits the left. Which specific position has been performed? a. Dorsal decubitus b. Transthoracic lateral c. Right lateral d. Ventral decubitus ANS: B 57. A patient is erect facing the x-ray tube and leaning the shoulders backward 20 to 30 degrees toward the IR. The central ray is perpendicular to the IR. What specific position has been performed? a. Lordotic b. Oblique c. Kyphotic d. Tangential ANS: A 58. The top of the foot is placed against the image receptor with the perpendicular central ray entering the sole of the foot. What specific projection has been performed? a. Transpedal b. Plantodorsal c. Axial dorsoplantar d. Tangential plantodorsal ANS: B 59. The patient is lying on her right side on a cart. The anterior surface of the patient is against the image receptor. A horizontal central ray enters the posterior surface and exits the anterior surface of the body. What specific projection/position has been performed? a. AP b. PA c. Right lateral decubitus d. Left lateral decubitus ANS: C 60. The patient’s head and neck are hyperextended with the top of the skull directly against the image receptor. The central ray enters just below the chin. Which specific projection has been performed? a. Submentovertical b. Acanthioparietal c. Parietoacanthial d. Verticosubmental ANS: A 61. Which of the following is NOT one of the four image quality factors of an analog radiograph? a. Contrast b. Spatial resolution c. Source–image receptor distance (SID) d. Distortion ANS: C 62. The amount of blackness seen on a radiograph is called: a. fog. b. scatter. c. contrast. d. density. ANS: D 63. Which of the following factors primarily controls radiographic density in the analog image? a. kVp b. mAs c. Film-screen speed d. Optimal immunomodulating dose (OID) ANS: B 64. A radiograph of the hand is underexposed and nondiagnostic. The following analog (film-screen) exposure factors were used: 50 kVp, 2 mAs, 40-inch (100 cm) SID. Which of the following sets of exposure factors should be used during the repeat exposure? a. 50 kVp, 8 mAs, 40 inches (100 cm) b. 50 kVp, 1 mAs, 40 inches (100 cm) c. 60 kVp, 4 mAs, 40 inches (100 cm) d. 50 kVp, 4 mAs, 40 inches (100 cm) ANS: D 65. A ____% increase in kVp will increase density the same as doubling the mAs (analog imaging). a. 15 b. 10 c. 100 d. 25 ANS: A 66. Exposure time is usually expressed in units of: a. seconds. b. nanoseconds. c. microseconds. d. milliseconds. ANS: D 67. What is the primary controlling factor for radiographic contrast in analog imaging? a. kVp b. mA c. Exposure time d. SID ANS: A 68. Which of the following radiographic studies would best benefit by applying the anode heel effect? a. Hand b. Skull c. Thoracic spine d. Ribs ANS: C 69. Which of the following devices can be used rather than applying the anode heel effect to compensate for anatomic part thickness differences? a. Compensating filters b. Copper filters c. Graded screens d. Added filtration ANS: A 70. Short scale contrast (in the analog image) is the result of: a. scatter radiation. b. collimation. c. high kVp. d. low kVp. ANS: D 71. What is the most effective method to reduce the production of scatter radiation? a. Increase kVp. b. Increase mAs. c. Collimate. d. Use a grid. ANS: C 72. A radiograph of the abdomen is underexposed and must be repeated. The original analog exposure factors used were 65 kVp with 25 mAs. The technologist decides to keep the mA at the same level but change the kVp to increase radiographic density. How much of an increase is needed in kVp to double the density? a. 3 to 5 kVp b. 9 to 10 kVp c. 10 to 15 kVp d. 15 to 20 kVp ANS: B 73. What type of radiographic contrast is produced with a high kVp (>100 kVp) technique? a. Low contrast, short scale b. High contrast, short scale c. Low contrast, long scale d. High contrast, long scale ANS: C 74. Which of the following controlling factors will most affect radiographic resolution? a. kVp b. mAs c. Filtration d. Focal spot size ANS: D 75. The unsharp edge of the projected image is termed: a. distortion. b. penumbra. c. edge loss. d. margin distortion. ANS: B 76. A radiograph of the abdomen demonstrates involuntary motion caused by bowel peristalsis (involuntary contractions). Which of the following factors will best eliminate this problem during the repeat exposure? a. Decrease SID. b. Turn patient into prone position rather than supine. c. Use higher kVp. d. Decrease exposure time. ANS: D 77. Which of the following changes will improve spatial resolution? a. Decrease SID. b. Decrease OID. c. Decrease kVp. d. None of the options. ANS: B 78. Increasing the SID to 48 inches (120 cm) from 40 inches (100 cm) and adjusting the mAs accordingly will: a. increase penumbra. b. along with the use of a small focal spot, decrease penumbra. c. decrease patient skin dose but increase internal dose because of an increase in scatter radiation. d. have no effect on image sharpness or on patient dose. ANS: B 79. Each digital image is two dimensional and is formed by a matrix of: a. bytes. b. algorithms. c. voxels. d. pixels. ANS: D 80. Highly complex mathematical formulas applied during digital processing of the image are termed: a. pixels. b. algorithms. c. digital filters. d. matrices. ANS: B 81. The intensity of light that represents the individual pixels in the digital image on the monitor is the definition for: a. contrast. b. spatial resolution. c. brightness. d. noise. ANS: C 82. Which of the following factors has the greatest effect on the brightness of the digital image? a. kVp b. mAs c. Processing software d. Matrix size ANS: C 83. The ability of a digital imaging system to distinguish between similar tissues is the definition for: a. edge enhancement. b. contrast resolution. c. sensitivity. d. system response. ANS: B 84. Contrast in the digital image is primarily affected by: a. kVp. b. mAs. c. matrix size. d. predetermined algorithms. ANS: D 85. The greater the bit depth of a digital system, the greater the: a. brightness. b. resolution. c. exposure index. d. contrast resolution. ANS: D 86. Which of the following factors has the greatest effect on spatial resolution of the digital image? a. Acquisition pixel size b. Display pixel size c. Use of a grid d. SID ANS: A 87. Misrepresentation of object size or shape as projected onto radiographic recording media is the general definition for: a. penumbra. b. distortion. c. magnification. d. margin loss. ANS: B 88. The number of x-ray photons that strike the digital receptor can be considered as: a. noise. b. kVp. c. signal. d. density. ANS: C 89. A numerical value that is representative of the exposure projected on the digital image receptor is termed: a. algorithm. b. variance. c. signal-to-noise ratio (SNR). d. exposure indicator. ANS: D 90. A random disturbance that obscures or reduces clarity is termed: a. signal. b. noise. c. electrical fluctuation. d. variance. ANS: B 91. The intensity of light that represents the individual pixels in the image on the monitor defines: a. density. b. brightness. c. contrast. d. spatial resolution. ANS: B 92. Which of the following factors has the greatest negative impact on SNR? a. Excessive kVp b. Collimation c. Insufficient mAs d. Long SID ANS: C 93. Which device or technique is most effective in controlling scatter radiation in digital imaging? a. Focal spot size b. Added filtration c. Postprocessing algorithm d. Grid ANS: D 94. The application of specific image processing that alters pixel values to the edges of structures is: a. smoothing. b. edge enhancement. c. magnification. d. image reversal. ANS: B 95. The adjustment of contrast and brightness of the displayed image is: a. brightness. b. equalization. c. edge enhancement. d. bit depth. ANS: D 96. The term portrait describes the long dimension of the image receptor that is aligned ____ to the long axis of the anatomy. a. perpendicular b. diagonal c. parallel d. transverse ANS: C 97. What type of material makes up the receptor in the FPD-TFT system? a. Amorphous selenium b. Amorphous silicon c. Calcium tungstate d. Both amorphous selenium and amorphous silicon ANS: D 98. Which of the following energy sources will erase any residual latent image from an exposed PSP imaging plate? a. Low-dose radiation b. Bright light c. Heat d. Ultraviolet light ANS: B 99. A digital storage and image management system defines a: a. radiology information system. b. digital archive. c. hospital information system. d. workstation. ANS: B 100. A network system with an array of hardware and software that connects all imaging modalities is termed a(n): a. archive. b. HIS. c. network. d. PACS. ANS: D 101. A standard that ensures that all digital imaging equipment can communicate with each other is referred to as: a. RIS. b. PACS. c. DICOM and HL7. d. HIS. ANS: C 102. Which of the following is NOT an advantage of a PACS? a. Simultaneous viewing of images at multiple locations b. Elimination of misplaced, damaged, or missing films c. Rapid chemical processing of images d. Rapid (electronic) transfer of images within the hospital ANS: C 103. A “soft-copy radiograph” is defined as a: a. radiographic image viewed on a computer monitor. b. radiographic image printed on film. c. radiographic image placed on a CD. d. latent radiographic image on a CR imaging plate. ANS: A 104. The application of specific image processing to reduce noise in an image is termed: a. filtration. b. photon degradation. c. attenuation. d. smoothing. ANS: D 105. A series of “boxes” that gives form to the image is the definition for: a. acquisition matrix. b. pixels. c. bit depth. d. display matrix. ANS: D 106. The range of exposure intensities that will produce an acceptable image is the definition for exposure: a. latitude. b. level. c. index. d. range. ANS: A 107. Changing or enhancing the electronic image to view it from a different perspective or improve its diagnostic quality is the general definition for: a. smoothing. b. edge enhancement. c. postprocessing. d. algorithmic conversion. ANS: C 108. What is the complete term for RIS? a. Radiographic imaging system b. Radiology interpretation system c. Radiology information system d. Reduced intensity system ANS: C 109. The complete term for SNR is signal-to-noise: a. relationship. b. ratio. c. rationale. d. reaction. ANS: B 110. Which term has replaced exposure in describing the amount of energy transferred to a mass of air by the photons? a. REM b. Air kerma c. Coulomb per kilogram d. Roentgen ANS: B 111. Which radiation unit of measurement is used to describe absorbed dose? a. Coulomb per kilogram b. Gray c. Sievert d. Curie ANS: B 112. Which traditional unit of radiation measurement describes patient dose? a. Roentgen b. Rem c. Coulombs d. Rad ANS: D 113. What is the annual whole body effective dose (ED) for a technologist? a. 10 mSv (1 rem) times the years of age b. 20 mSv (200 mrem) c. 50 mSv (5000 mrem) d. 500 mSv (50 rem) ANS: C 114. The annual occupational dose limit for the lens of the eye is: a. 150 mSv (15,000 mrem). b. 1 mSv (100 mrem). c. 50 mSv (5 rem). d. 500 mSv (50 rem). ANS: A 115. Where should a personnel dosimeter be worn during fluoroscopy? a. On collar inside the lead apron b. On waist inside the lead apron c. On collar outside the lead apron d. On sleeve outside the lead apron ANS: C 116. Which of the following is NOT an ALARA concept? a. Collimate when feasible. b. Always wear a personnel dosimeter. c. Use optimal kVp techniques. d. Have older technologists rather than younger technologists hold patients. ANS: D 117. Which of the following is NOT one of the cardinal principles of radiation protection? a. Shielding b. Filtration c. Time d. Distance ANS: B 118. Pregnant technologists should not exceed ____ dose per month. a. 1 mSv (0.1 rem) b. 0.5 mSv (50 mrem) c. 10 mSv (1 rem) d. 300 mSv (30 rem) ANS: B 119. Which of the following patient dose categories carries the highest numerical value of all patient doses? a. Effective dose b. Gonadal dose c. Midline dose d. Entrance skin exposure ANS: D 120. The cumulative (ED) lifetime dose for an occupationally exposed worker is _____ mSv × years of age. a. 100 b. 50 c. 10 d. 1 ANS: C 121. Which of the following radiographic projections will provide the greatest amount of effective dose (without shielding)? a. AP pelvis b. Barium enema c. AP skull d. AP abdomen (using 70 kVp) ANS: B 122. What type of collimator will automatically restrict the x-ray beam to the size of the image cassette or image receptor? a. Diaphragm b. Positive beam limiting c. Manual collimator d. Electronic focused beam ANS: B 123. What type of protective shield is NOT in direct contact with the patient’s body? a. Shadow shield b. Shaped shield c. Lead mat d. Gonadal flat shield ANS: A 124. A 20-year-old woman is brought into radiology from the ED with a possible fracture of the pelvis. What should the technologist do regarding gonadal shielding? a. Perform a PA projection of the pelvis and use gonadal shielding. b. Take an AP projection of the pelvis without using any shielding. c. Cover the area of the ovaries and uterus with a gonad shield for the AP pelvis projection. d. Ask the patient if she wishes to have shielding placed across her pelvis. ANS: B 125. Which of the following precautions reduces radiation exposure to the technologist during a fluoroscopic procedure to the greatest degree? a. Wearing a protective lead apron of 1-mm lead thickness b. Wearing a thyroid shield c. Standing as far away as possible from the radiation scatter fields d. Turning your back to the fluoroscopy table ANS: C 126. When correctly placed, gonadal shielding will reduce dose by ____ if gonads are in the primary x-ray field. a. 20% to 50% b. 50% to 90% c. 100% d. None of the options ANS: B 127. Use of gonadal shielding is necessary when the anatomical region of interest lies within or near _____ of the primary beam unless such shielding obscures essential diagnostic information. a. 10 inches (25 cm) b. 2 inches (5 cm) c. 1 inch (2.5 cm) d. 6 inches (15 cm) ANS: B 128. The minimum total filtration (inherent plus added) required for diagnostic x-ray equipment producing 70 kVp or greater is _____ mm aluminum equivalent. a. 1.5 b. 2.5 c. 0.5 d. 4 ANS: B MATCHING Select the correct definition for the terms listed below. (Use each choice only once.) a. Caudad b. Proximal c. Extension d. Radial deviation e. Inversion f. Dorsiflexion g. Adduction h. Abduction i. Pronation 1. Movement of an arm or leg toward the midline 2. An inward stress movement of foot 3. Near the source or the beginning 4. A CR angle away from the head end 5. Increasing the angle of a joint 6. Movement of an arm or leg away from the midline 7. Decrease angle between foot and lower leg 8. Turn or bend hand and wrist toward radius 9. Rotation of hand with palm down 1. ANS: G 2. ANS: E 3. ANS: B 4. ANS: A 5. ANS: C 6. ANS: H 7. ANS: F 8. ANS: D 9. ANS: I Select the minimum number of projections generally required for each of the anatomic structures. a. One projection b. Two projections c. Three projections 10. Femur 11. Chest 12. Foot 13. Finger 14. Forearm 15. Ankle 16. Elbow 17. Pelvis 10. ANS: B 11. ANS: B 12. ANS: C 13. ANS: C 14. ANS: B 15. ANS: C 16. ANS: C 17. ANS: A Match the analog image receptor (IR) sizes to their metric equivalent. a. 35 × 43 cm b. 18 × 24 cm c. 30 × 35 cm d. 24 × 24 cm e. 24 × 30 cm 18. 10 × 12 inches 19. 14 × 17 inches 20. 8 × 10 inches 21. 9 × 9 inches 22. 11 × 14 inches 18. ANS: E 19. ANS: A 20. ANS: B 21. ANS: D 22. ANS: C TRUE/FALSE 1. A body system consists of an association of organs that share a common function. ANS: T 2. A lateromedial projection is one in which the lateral aspect of the anatomy part is closest to the image receptor (IR). ANS: F 3. Tangential and axial projections are the same type of projection. ANS: F 4. Radiographic view is NOT a valid positioning term in the United States. ANS: T 5. The term position can be used for both a lateral and an oblique body position. ANS: T 6. According to the American Registry of Radiologic Technologists (ARRT) Code of Ethics, a radiologic technologist may render a diagnosis during a radiographic examination if requested by the patient. ANS: F 7. According to the ARRT Code of Ethics, radiologic technologists must participate in continuing education activities throughout their professional career. ANS: T 8. According to the ARRT Code of Ethics, a radiologic technologist may discuss a patient’s clinical history with a family member. ANS: F 9. It is legally acceptable to annotate “right” or “left” on a digital image if the anatomic side marker is not visible. ANS: F 10. The radiographer has the responsibility of communicating with the patient to obtain pertinent clinical information. ANS: T 11. The radiographer may provide a preliminary interpretation of the radiographic study if requested by the patient. ANS: F 12. It is common practice to view a PA projection with the patient’s left facing the viewer’s right. ANS: T 13. PA or AP oblique projections are aligned on the monitor with the patient’s right side of the body facing the viewer’s right. ANS: F 14. Decubitus chest projections are aligned for viewing the way the image receptor “sees” them. ANS: F 15. When aligning images of the hand on the monitor, the digits should be pointing upward. ANS: T 16. When aligning images of the lower leg on the monitor, the toes of the foot must be pointing upward. ANS: F 17. When viewing a CT (computed tomography) or MRI (magnetic resonance imaging) image, the patient’s right is facing the viewer’s left. ANS: T 18. The intensity of the x-ray beam is greatest under the anode as defined by the anode heel effect. ANS: F 19. Increasing the SID will increase distortion of the anatomy. ANS: F 20. A 40-inch (100 cm) SID should be the minimal distance used for most radiographic projections. ANS: T 21. Using a table Bucky device will increase magnification of the anatomy as compared with performing the same study on the tabletop. ANS: T 22. The least possible distortion of the anatomy occurs at the point of the central ray. ANS: T 23. The wide dynamic range of digital imaging systems results in fewer repeat exposures, increased efficiency, and operating cost reduction as compared with analog (film-screen) systems. ANS: T 24. In digital imaging, the term exposure indicator replaces the analog (film-based) term density. ANS: F 25. A low SNR is desirable in digital imaging. ANS: F 26. The photostimulable storage phosphor (PSP) imaging plate is light sensitive and must be processed in a dark environment. ANS: F 27. A PSP-based digital imaging system may be cassette based or cassetteless. ANS: T 28. Thin film transistor (FPD-TFT) digital imaging systems are commonly referred to as digital radiography (DR). ANS: T 29. PSP imaging plates are scanned with an ultra-bright light source to produce the visible digital image. ANS: F 30. Depending on the manufacturer, the PSP image may be viewed on the technologist workstation within 5 seconds following plate reading. ANS: T 31. FPD-TFT–based systems can be used for both grid and nongrid examinations. ANS: T 32. Lead masking/mats should be used when recording multiple images on the same cassette-based PSP system. ANS: T 33. Close collimation is not recommended when using a PSP imaging system. ANS: F 34. As a general rule, exposure factors are decreased 5 to 15 kVp with digital systems as compared with analog imaging systems. ANS: F 35. Digital radiography systems are hypersensitive to the effects of scatter radiation. ANS: T 36. An image receptor placed lengthwise to the long axis of the structure or body is in the portrait orientation. ANS: T 37. A grid can be left in place for most digital radiographic procedures. ANS: T 38. The acronym PACS refers to picture archiving connection system. ANS: F 39. Exposure indicator is a numeric value that is representative of the level of exposure the image receptor has acquired. ANS: T 40. PACS should be integrated with an HIS. ANS: T 41. One gray is equivalent to 1000 rad. ANS: F 42. Système International (SI) has been the national standard for units of radiation measurement since 1958. ANS: T 43. Thermoluminescent and optically stimulated luminescence dosimeters must be changed every 14 days to ensure an accurate recording of exposure to the technologist. ANS: F 44. The adjustable collimator light field must be accurate within 5% of the selected SID. ANS: F 45. Recent studies indicate that the breasts are more radiosensitive than the gonads. ANS: T 46. The ImageWisely® program is focused on reducing unnecessary exposure in children during imaging procedures. ANS: F 47. The ACE® initiative is a reminder to maintain professional communication between technologists and their patients. ANS: T 48. PACS permits simultaneous viewing of images at multiple locations. ANS: T 49. A Deviation Index (DI) of zero indicates no radiation has reached the digital image receptor. ANS: F [Show More]
Last updated: 1 year ago
Preview 1 out of 338 pages
Reviews( 0 )
Document information
Connected school, study & course
About the document
Uploaded On
Oct 21, 2022
Number of pages
338
Written in
Additional information
This document has been written for:
Uploaded
Oct 21, 2022
Downloads
0
Views
53


.png)

.png)
.png)


.png)
.png)

