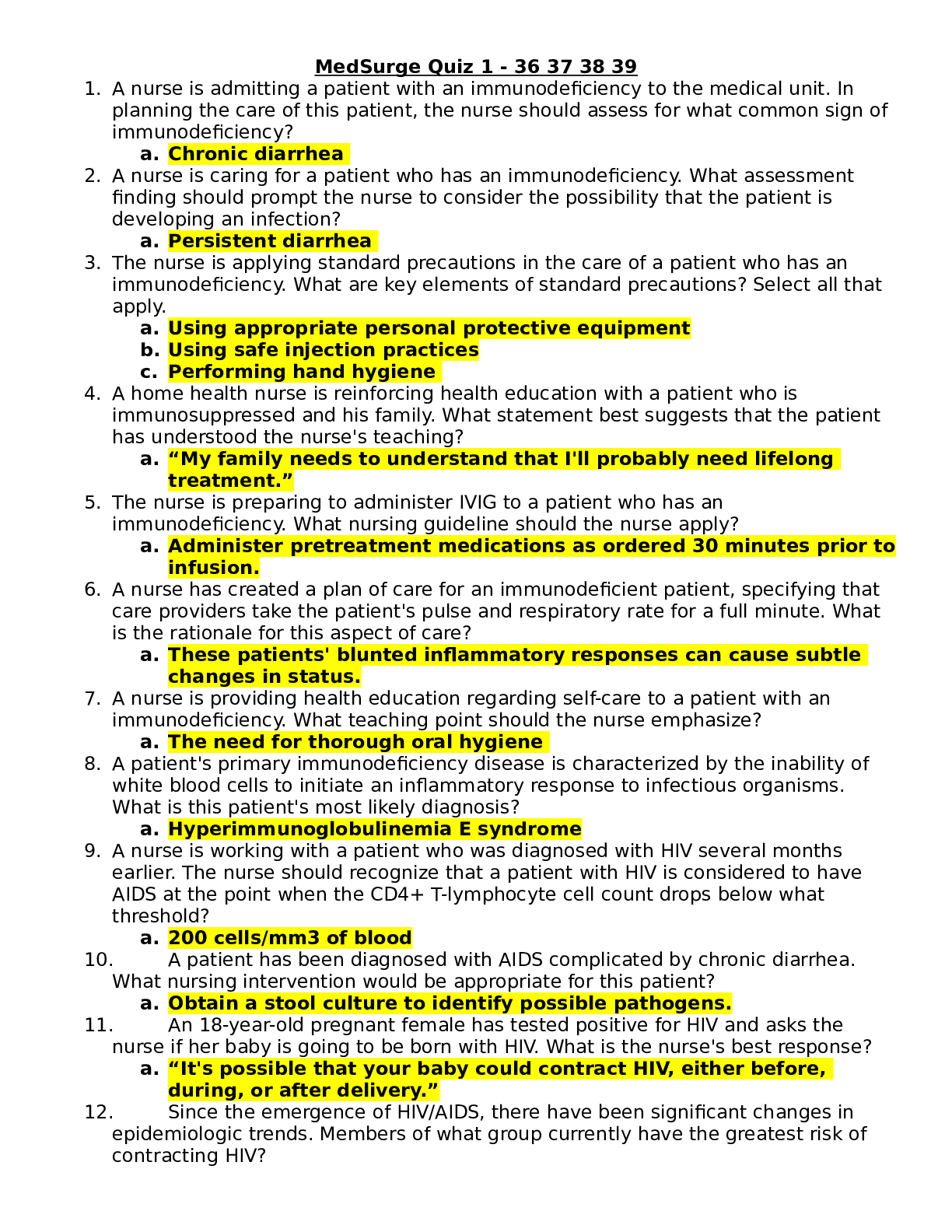
*NURSING > MED-SURG EXAM > NURS 3320 MED SURG EXAM 1 {2020} – Northeastern University | NURS3320 MED SURG EXAM 1 (All)
NURS 3320 MED SURG EXAM 1 {2020} – Northeastern University | NURS3320 MED SURG EXAM 1
Document Content and Description Below
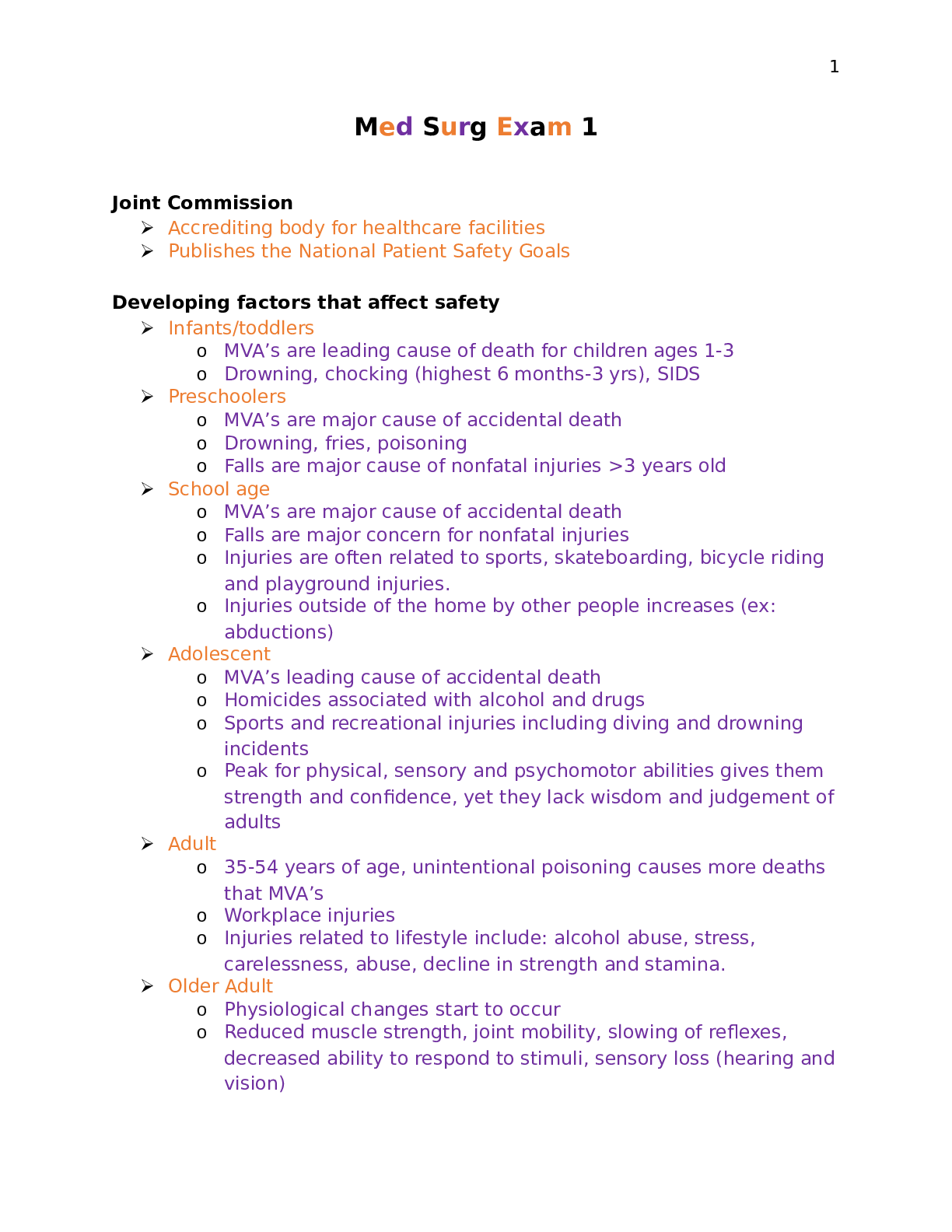
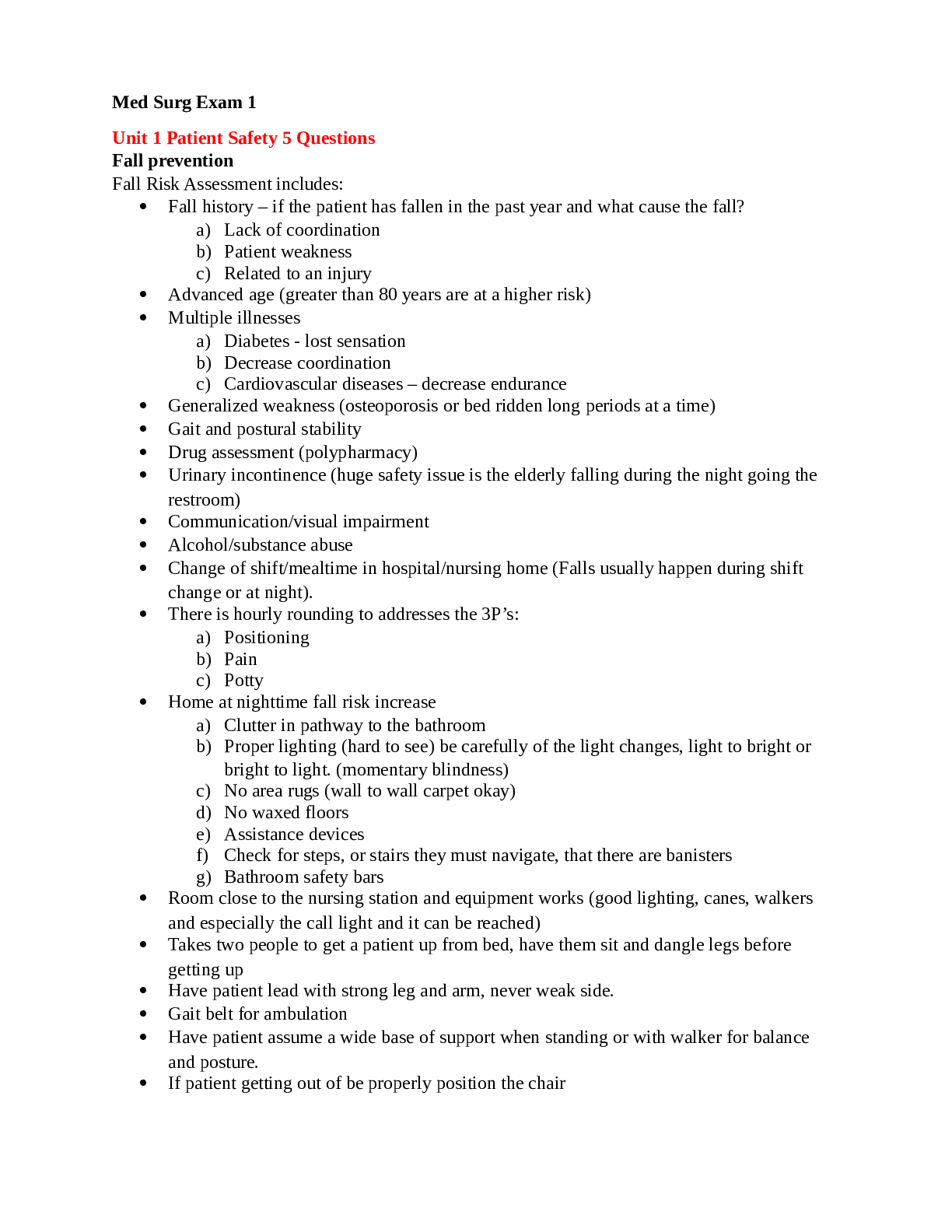
NURS 3320 MED SURG EXAM 1 – Northeastern University MED SURG EXAM 1 Module 1: Pain Pain Management • Pain is #1 reason to seek medical care • What is pain • What are the different ... types of pain • How ill you assess, treat, and reassess • What are the nursing implications for managing pain The Fundamental concepts • Acute: tissue damage as a result of surgery, trauma, or burns (expected to have relatively short duration and resolve with normal healing • Chronic: (persistent)- cancer or non-cancer origin and can be time limited (may resolve within months) or persist throughout the course of a person’s life • Nociceptive: physiologic pain o May be described as “normal” pain transmission o Normal functioning of physiologic systems that leads to the perception of noxious stimuli (tissue injury) as being painful o INCLUDES 4 SPECIFIC PROCESSES 1. Transduction- the processes by which noxious stimuli, such as a surgical incision or burn, activate primary afferent nercous called nociceptors, which are located throughout body in skin, subcutaneous tissue, and visceral and somatic structures o the conversion of chemical info at the cellular level into electrical impulses that move toward spinal cord o begins when cells injured o cells release chemicals o chemical excite norciceptors 2. Transmission- second process involved in nociception. o Stimuli move from the peripheral nervous system toward the brain o A-delta fibers- carry impulses rapidly o C-Fibers-carry impulses slower o In the thalamus, within the brain Transmits the message to the cortex Notifies norciceptors that message was received To discontinue the transmission 3. Perception-third process- is the result of the neural activity associated with transmission of noxious stimuli o Requires activation of higher brain structures for the occurrence of awareness, emotions, and drives associated with pain. o Each person tolerates pain differently o Pain is influenced by o Genetic o Learned behavior o Culture 4. Modulation-last phase of the pain impulse o Brain interacts with the spinal nerves to alter the pain experience o Involves many different neurochemicals • Neuropathic o Pathologic and results from abnormal processing of sensory input by the nervous system as a result of damage to the peripheral or central nervous system or both • Mixed o A combination of. nociceptive and neuropathic • Somatic o Caused by injury to skin, muscles, bone, joint, and connective tissues. Deep somatic pain is usually described as dull or aching, and localized in one area. • Visceral o Results from the activation of nociceptors of the thoracic, pelvic, or abdominal viscera (organs). Visceral structures are highly sensitive to distension (stretch), ischemia and inflammation, but relatively insensitive to other stimuli that normally evoke pain such as cutting or burning. • Central o Syndrome is a neurological condition caused by damage to or dysfunction of the central nervous system (CNS), which includes the brain, brainstem, and spinal cord. This syndrome can be caused by stroke, multiple sclerosis, tumors, epilepsy, brain or spinal cord trauma, or Parkinson's disease. • Peripheral neuropathic pain: o Refers to the conditions that result when nerves that carry messages to and from the brain and spinal cord from and to the rest of the body are damaged or diseased o They range from carpal tunnel syndrome (a traumatic injury common after chronic repetitive use of the hands and wrists, such as with computer use) to nerve damage linked to diabetes. • Harmful effects of unrelieved pain: o Cardiac and respiratory: Increased HR Increased cardiac workload Increased vascular resistance Decreased respiratory volume Increased cough reflex o Endocrine and metabolism Fight or flight response Increased glycogenesis Hyper glycaemia Decreased urine output Decreased motility and GI issues Fatigue, poor muscle function Decreased immune response Depression o Quality of life decrease Pain Assessment • Self report o Best use o Do not judge always believe when a patient report pain • Conduct through assessment o COLD ERA/ OLD CART o Location o Intensity (Pain Scale) ask pain level using scale Numeric Rating Scale Wong-Baker FACES Face pain scale revises Visual analog scale o Quality Stabbing, sharp, throbbing o Onset and Duration When did it start How long did it last o Aggravating/ Reliving factors Anything make it worse Anything make it better o Comfort function Goals Function goal: • Example: ambulate to the bathroom Comfort goal • Where they want to be on the pain scale Patient Education • Educating patients and their family on how to use a pain rating scale o Show pain scale and explain why using it o Explain how it works o Explain what you are measuring Tell them to report all types of pain • Tingling, pulling, tightness o Be sure patient understanding Teach back method of examples of pain in lifetime o Practice using scale Current pain or past pain • Purpose of pain scale o Quality of life Want to give them best quality of life possible • Goals o Determine goals for their comfort and quality of life o What pain rating will get them there Assess and then Reassess • Make goals, make interventions and reassess to see if its working Choosing a Method • Analgesics: opioid • Analgesics: non-opioid • Alternative therapies • RN not writing orders but can make suggestions Non-Opioid Analgesics • NSIDS o Aspirin, Aleve, Ibuprofen, Tylenol What are considerations for administration o Given for mild-moderate pain or given with opioids when there is severe pain o Can be administered: PO, IV, rectally o Side effects: Tylenol • Hepatotoxicity risk • Part of Percocet (pay attention to total dose) NSIDS: • GI complications • Renal toxicity • Cardiovascular problems • Administer with food and water • Things to consider: o What options do you have for non-opioid pain management o When would you use these and why o What are your nursing considerations Opioid Analgesics • Mu aganoist: o Morphine and morphine like drugs • Agonist antagonist o Nalbuphine and buprenophine o Interact with opioid receptor • Antagonist: o Bind same receptor but produce no effects Use to reverse effects of opioids • GOAL: o Improve maintain pain control and improve activity Keep pain level low so they can function o When administering re-assess pain o Consider leas invasive route and what will work best for pt to keep goals • Adverse effects o Constipation o Respiratory depression • Watch for sing of o Withdrawal o Tolerance • Considerations: o What options do you have for opioid pain management o When would you use these and why o What are your nursing considerations • Physical Dependence o Opioids over 2 weeks o Not addiction o When its stops there are withdrawal symptoms o Needs to tapper off medication so it doesn’t happen drastically • Tolerance o Decreased effects of administration • Addiction o Disease o Crave substance and take despite results o Not associated with pain relief o Usually doesn’t happen without other drug use Person will not develop this just from being prescribed opioids Alternative therapies • Local/ topical anesthetics o Lidocane patches o Anticonvulsants and antidepressants Good for diabetic for neuropathic pain - - - - - - - -- - - - - - - - - - - - - - - - - - - - - - - - - -Respiratory • The Pathophysiology of emphysema involves destruction of the walls of the alveoli leading to impaired oxygen diffusion- TRUE • Smoking cessation is the single most cost-effective intervention to reduce the risk of developing COPD and to stop its progression-TRUE • Administering oxygen to patients with COPD will result in cardiopulmonary arrest by suppressing the drive to breathe-FALSE • The strongest predisposing factor for asthma is allergy-TRUE • The risk of having a child with cystic fibrosis is 100% if both parents are carriers of the cystic fibrosis gene-FALSE • COPD is generally a progressive disease characterized by three primary symptoms: chronic cough, sputum production and dyspnea • Patients who have difficulty coordinating inspiration with activation of their metered dose inhaler can be helped by use of a spacer • If a rapid onset of shortness of breath occurs in a patient with COPD, the nurse should quickly evaluate the patient for the potential complication of pneumothorax by assessing the symmetry of chest movement, differences in breath sounds, and pulse oximetry. • The cornerstone pharmacologic therapy of bronchiectasis management is the use of ANTIBIOTICS • The most potent and effective anti-inflammatory medications currently available to treat asthma are CORTICOSTEROIDS • The clinic nurse is explaining to the patient with asthma what prednisone is used for. What would be the best explanation the nurse could give: To gain prompt control of inadequately controlled, persistent asthma • The admitting nurse is assessing a client with COPD. The nurse auscultates diminished breath sounds, which signify changes in the airway. These changes indicate to the nurse to monitor the patient for: Dyspnea and hypoxemia • You are the nurse caring for a patient with asthma hospitalized with an acute asthma exacerbation. What drugs would you expect to have ordered for this patient to gain underlying control of persistent asthma: anti-inflammatory drugs • You are taking a course in lung sounds. You are learning about the lungs of a child with asthma. You learn that the most common symptoms of asthma are: bilateral wheezes Cardiac • Recent research has shown that cigarette smoking causes high blood pressure, especially in men- FALSE • The dietary approach to stop hypertension (DASH) diet recommends 4 to 5 servings of fruit and vegetables a day (based on 2,000 cal diet)-TRUE • The patient who is adjusting to reduced salt intake should be advised that it takes up to 1 year for taste buds to adapt to changes in salt intake-FALSE • A hypertensive urgency describes a situation in which BP is very elevated, but no evidence seen of impending or progressive target organ damage-TRUE • Aldactone, an aldosterone receptor blocker that I prescribed for hypertension, is contraindicated for patients with hyperkalemia and impaired renal function-TRUE • Hypertension is defined by the 7th report of the joint national committee on prevention, detection, evaluation and treatment of high blood pressure as a systolic over 140 mm Hg. • Prolonged BO elevation gradually damages blood vessels throughout the body, particularly in target organs such as the heart, kidneys, brain, and EYES • The recommended initial medication regimen for patients with uncomplicated hypertension, and no indications for another medication, includes DIURETICS and beta-blockers, or both • Patients need to be informed that REBOUND hypertension can occur if antihypertensive medications are suddenly stopped • A hypertensive emergency is a situation in which the systolic BP is above 180 mm Hg and must be lowered immediately • While assessing a patient the nurse notes that the patient's ankle-brachial index (ABI) of the right leg is 0.40. The nurse is aware that this may indicate: Arterial narrowing • Which assessment would be most appropriate for a patient who is receiving a loop diuretic for heart failure: Monitor for hypotension. • A patient with primary hypertension complains of dizziness with ambulation. The patient is currently on an alpha-adrenergic blocker. The nurse assesses postural hypotension. When teaching this patient about risks associated with postural hypotension, what should the emphasis be placed on: Rising slowly from a lying or sitting position • A patient who has undergone a femoral to popliteal bypass graft surgery returns to your unit. Which assessments should be performed during the first postoperative day: Assess pulse of affected extremity every 15 minutes at first. • When caring for a patient with leg ulcers, the positioning of the legs depends on whether the ulcer is arterial or venous in origin. How would you position a patient who has leg ulcers that are venous in origin: Elevate lower extremities • You are assessing a patient suspected of having right-sided heart failure. What assessment finding may indicate right-sided heart failure: Distended neck veins • The nurse is taking a health history on a new patient. The patient reports experiencing pain in the left lower leg and foot when walking. This pain is relieved with rest. The nurse notes that the left lower leg is slightly edematous and is hairless. What does the nurse suspects that the patient may be experiencing: Intermittent claudication • A patient is placed on a low-sodium diet. Which statement by the patient indicates that the nurse's nutritional teaching plan has been effective: "I will have a baked potato with broiled chicken for dinner." • A patient presents to the emergency department complaining of increasing shortness of breath. The nurse assessing the patient notes a history of left-sided heart failure. The patient is agitated and coughing up pink-tinged, foamy sputum. What should the nurse recognize these as signs and symptoms of: Acute pulmonary edema • You are caring for an adult patient with heart failure who is prescribed digoxin. What adverse side effects should the nurse explain to the patient that he or she should watch for: Fatigue and nausea Fluid and Electrolyte • Osmosis is the natural tendency of a substance to move from an area of higher concentration to one of lower concentration-FALSE • Nursing interpretation of fluid and electrolyte changes in the older adult is based on the knowledge that muscle mass decrease with age results in a lower concentration of body fluid-TRUE • A nurse should assess a patient with hypervolemia for indicators of hypotension, bradypnea, and oliguria-FALSE • When monitoring a patient’s potassium level, the nurse is aware that tall, tented, “T” waves on an ECG are indicative of hyperkalemia-TRUE • The major electrolytes in the extracellular fluid are SODIUM and chloride • A nurse, who is caring for a patient with a serum sodium level of 150mEq/L, can estimate at t bedside that the patient would have a serum OSMOLALITY of 280 mOsm/kg. • When monitoring daily body weights to assess fluid volume deficit, the nurse understands that a los of 1 pound (0.5kg) represents a fluid loss of approximately 500 mL. • Hyperventilation, with a resulting decrease in PaCo2, is an expected compensatory reaction to the acid-base disorder of METABOLIC acidosis. • Systemic complications of intravenous solutions include Circulatory overload, AIR embolism, febrile reaction, and infection • In the human body, water and electrolytes move from the arterial capillary bed to the interstitial fluid. What causes this to occur: The hydrostatic pressure resulting from the pumping action of the heart • A patient with anxiety presents to the emergency room. The triage nurse notes upon assessment that the patient is hyperventilating. The triage nurse is aware that hyperventilation is the most common cause of which acid-base imbalance: Respiratory alkalosis • You are making initial shift assessments on your patients. While assessing one patient's peripheral IV site, you note edema around the insertion site. How will you document this complication related to IV therapy: Infiltration • While admitting a new patient to your medical-surgical unit, you note that the patient is oliguric. You notify the acute-care nurse practitioner who orders a fluid challenge of 100 to 200 mL of normal saline solution over 15 minutes. What do you know this intervention will do: Help distinguish reduced renal blood flow from decreased renal function • A patient in the ICU starts complaining of being ìshort of breath.î An arterial blood gas (ABG) is drawn. The ABG has the following values: pH = 7.21, PaCO2 = 64 mm Hg, HCO3 = 24 mm Hg. What does the ABG reflect: Respiratory acidosis • You are the nurse caring for a 65-year-old female patient who is in renal failure. During your shift assessment, the patient complains of tingling in her lips and fingers whenever anyone takes her blood pressure. She tells you that she gets a spasm in her wrist and hand and that it is very painful. What would you suspect: Hypocalcemia • You are working on a burn unit. One of your patients is exhibiting signs and symptoms of third spacing, which occurs when fluid moves out of the intravascular space but not into the intracellular space. Based upon this fluid shift, what would you expect the patient to demonstrate: Hypervolemia • You are caring for a patient with a diagnosis of syndrome of inappropriate antidiuretic hormone secretion. Your patient has specific gravities ordered every 4 hours. What does this test detect: Fluid volume status • You are the nurse evaluating a new patient's laboratory results. Based upon the laboratory findings, what will cause the release of antidiuretic hormone (ADH): Increased serum sodium • You are doing an admission assessment on an elderly patient newly admitted for end-stage liver disease. You must assess the patient's skin turgor. What should you remember when evaluating skin turgor: Inelastic skin turgor is a normal part of aging • A nurse in the medical ICU has orders to infuse a hypertonic solution into her patient with low blood pressure. This solution will increase the number of dissolved particles in the patient's blood, creating pressure for fluids in the tissues to shift into the capillaries and increase the blood volume. Which term or terms is/are associated with this process: Osmosis and osmolality • You are the nurse caring for a 77-year-old male who fell off his roof. You note that the patient's labs indicate minimally elevated serum creatinine levels. What can this indicate in older adults: Substantially reduced renal function [Show More]
Last updated: 1 year ago
Preview 1 out of 46 pages
Reviews( 0 )
Document information
Connected school, study & course
About the document
Uploaded On
Jan 16, 2021
Number of pages
46
Written in
Additional information
This document has been written for:
Uploaded
Jan 16, 2021
Downloads
0
Views
61





 Updated 2022.png)
.png)

.png)
.png)