*NURSING > STUDY GUIDE > NURS 501 Study Guides(combined study guides for all chapters)Graded A study guides 2021 (All)
NURS 501 Study Guides(combined study guides for all chapters)Graded A study guides 2021
Document Content and Description Below
NURS 501 Study Guides NURS 501 Advanced Physiology and Pathophysiology Chapter 1: Cellular Biology Study Guide 1. Which statement best describes the cellular function of metabolic absorption... ? a. Cells can produce proteins. c. Cells can take in and use nutrients. b. Cells can secrete digestive enzymes. d. Cells can synthesize fats. 2. Most of a cell’s genetic information, including RNA and DNA, is contained in the: a. Mitochondria c. Nucleolus b. Ribosome d. Lysosome 3. Which component of the cell produces hydrogen peroxide (H2 O2 ) by using oxygen to remove hydrogen atoms from specific substrates in an oxidative reaction? a. Lysosomes c. Ribosomes b. Peroxisomes d. Oxyhydrosomes 4. Which cell component is capable of cellular autodigestion when it is released during cell injury? a. Ribosome c. Smooth endoplasmic reticulum b. Golgi complex d. Lysosomes 5. What is the sequence of steps in the development of a digestive enzyme by the pancreas cells from the initial transcription to the release from the cell? a. The enzyme is transcribed from DNA by RNA in the nucleus, proceeds to the ribosome for synthesis, and is transported in a secretory vesicle to the cell membrane. b. The enzyme is transcribed from RNA by DNA in the nucleus, proceeds to the lysosome for synthesis, and is transported in an encapsulated membrane to the cell membrane. c. The enzyme is transcribed by the mitochondria in the nucleus, proceeds to the ribosome for synthesis, and is transported in a cytoskeleton to the cell membrane. d. The enzyme is transcribed from DNA by RNA in the nucleus, proceeds to the Golgi complex for synthesis, and is transported in cytosol to the cell membrane. 6. During which phase of the cell cycle is DNA synthesized? a. G1 b. S c. G2 d. M 7. What organic compound facilitates transportation across cell membranes by acting as receptors, transport channels for electrolytes, and enzymes to drive active pumps? a. Lipids c. Proteins b. Proteases d. Carbohydrates 8. Understanding the various steps of proteolytic cascades, such as caspase-mediated apoptosis and complement cascades, may be useful in designing drug therapy for which human diseases? a. Cardiac and vascular disorders b. Autoimmune and malignant disorders c. Gastrointestinal and renal disorders d. Endocrine and gastrointestinal disorders 9. Which structure prevents water-soluble molecules from entering cells across the plasma membrane? a. Carbohydrate chains. b. Membrane channel proteins c. Glycoprotein channels d. Lipid bilayer (Phospholipids bi-layer) 10. The fluid mosaic model explains: a. How a cell membrane functions b. Why our bodies appear to be solid c. How tissue is differentiated d. How fluid moves between the intracellular and extracellular compartments 11. Which form of cell communication is used to communicate within the cell itself and with other cells in direct physical contact? a. Protein channel (gap junction) b. Plasma membrane-bound signaling molecules (involving receptors) c. Hormone secretion such as neurotransmitters d. Extracellular chemical messengers such as ligands 12. Which mode of chemical signaling uses blood to transport communication to cells some distance away? a. Paracrine c. Neurotransmitter b. Autocrine d. Hormonal 13. Which mode of chemical signaling uses local chemical mediators that are quickly taken up, destroyed, or immobilized? a. Paracrine c. Neurotransmitter b. Autocrine d. Hormone 14. Neurotransmitters affect the postsynaptic membrane by binding to: a. Lipids c. Amphipathic lipids b. Ribosomes d. Receptors 15. How do cells receive communication from the extracellular fluid surrounding them? a. Protein channel (gap junction) b. Plasma membrane-bound signaling molecules (involving receptors) c. Hormone secretion such as neurotransmitters d. Chemical messengers such as ligands 16. When a second message is necessary for extracellular communication to be activated, it is provided by which one? a. Guanosine triphosphate (GTP) c. Adenosine triphosphate (ATP) b. Adenosine monophosphate (AMP) d. Guanosine diphosphate (GDP) 17. Under anaerobic conditions, what process provides energy for the cell? A.. Oxidative phosphorylation B.. Lactolysis C. Glycolysis D. Passive transport 18. What is the mechanism by which the energy produced from carbohydrates, proteins, and lipids is transferred to adenosine triphosphate (ATP)? a. Anaerobic glycolysis c. Oxidative phosphorylation b. Oxidative cellular metabolism d. Tricarboxylic acid phosphorylation 19. Passive transport is best described with which statement? a. Being driven by osmosis, hydrostatic pressure, and diffusion. b. Involving receptors that can bind with substances being transported. c. Being capable of transporting macromolecules. d. Requiring energy generated by the cell 20. Active transport occurs across which type of membranes? a. Membranes that have a higher concentration of the solute on the outside of the cell b. Membranes that are semipermeable to water and small electrically uncharged molecules c. Membranes that have receptors that are capable of binding with the substances to be transported d. Membranes that have a cell membrane that is hydrophobic rather than hydrophilic 21. Which method of transport uses transmembrane proteins with receptors with a high degree of specificity for the substance being transported? a. Active c. Transmembranous b. Mediated d. Passive 22. The movement of fluid across the arterial end of capillary membranes into the interstitial fluid surrounding the capillary is an example of which fluid movement process? a. Hydrostatic pressure c. Diffusion b. Osmosis d. Active transport 23. Why is osmolality preferred over osmolarity as the measurement of osmotic activity in the clinical assessment of individuals? a. Plasma contains sodium and chloride, which influence the volume of solution. b. Volume affects perfusion more than the weight of solutes. c. More of the weight of plasma is influenced by solutes, such as protein and glucose, rather than by water. d. Osmotic activity depends on the concentration of solutes present in plasma, such as proteins and glucose. 24. A patient who has diarrhea receives a 3% saline solution intravenously to replace the sodium and chloride lost in the stool. What effect will this fluid replacement have on cells? a. Become hydrated c. Shrink b. Swell or burst d. Divide 25. The transport of glucose from the blood to the cell is accomplished by which process? a. Active-mediated transport (active transport) b. Active diffusion c. Passive osmosis d. Passive-mediated transport (facilitated diffusion) 26. Potassium and sodium are transported across plasma membranes by: a. Passive electrolyte channels b. Coupled channels c. Adenosine triphosphatase (ATPase) enzyme d. Diffusion 27. What occurs during exocytosis? a. Macromolecules can be secreted across eukaryotic cell membranes. b. All substances are secreted into the cellular matrix. c. No repairs in the plasma membrane can take place. d. Solute molecules flow freely into and out of the cell. 28. Why is it possible for potassium to diffuse easily into and out of cells? a. Potassium has a greater concentration in the intracellular fluid (ICF). b. Sodium has a greater concentration in the extracellular fluid (ECF). c. The resting plasma membrane is more permeable to potassium. d. An excess of anions are inside the cell. 29. The cellular uptake of the nutrient cholesterol depends on which process? a. Receptor-mediated exocytosis c. Receptor-mediated endocytosis b. Antiport system d. Passive transport 30. What causes the rapid change in the resting membrane potential to initiate an action potential? a. Potassium gates open, and potassium rushes into the cell, changing the membrane potential from negative to positive. b. Sodium gates open, and sodium rushes into the cell, changing the membrane potential from negative to positive. c. Sodium gates close, allowing potassium into the cell to change the membrane potential from positive to negative. d. Potassium gates close, allowing sodium into the cell to change the membrane potential from positive to negative. 31. The action of platelet-derived growth factor is to stimulate the production of which cells? a. Platelets c. Connective tissue cells b. Epidermal cells d. Fibroblast cells 32. The role of cytokines in cell reproduction is that they: a. Provide growth factor for tissue growth and development. b. Block progress of cell reproduction through the cell cycle. c. Restrain cell growth and development. d. Provide nutrients for cell growth and development. 33. What is the process of cellular reproduction? a. The process often takes months or years to complete. b. Cellular reproduction typically has a short interphase. c. Two diploid cells, called daughter cells, have been formed. d. The process involves the interaction of male and female cells. 34. Which statement is true about eukaryotic cells? a. They lack distinct nucleus. b. They contain compartments called organelles. c. They lack an encasing nuclear membrane. d. They are smaller than the typical prokaryote cell. 35. Which statement is true about phagocytosis? a. Phagocytosis is an example of exocytosis. b. Phagocytosis is dependent on small vesicles. c. Phagocytosis involves the ingestion of bacteria. d. Phagocytosis focuses on solute molecules. 36. A muscle cell possesses which specialized function? a. Movement c. Secretion b. Conductivity d. Respiration 37. When a mucous gland cell creates a new substance from previously absorbed material, this process is known as which specialized cellular function? a. Excretion c. Reproduction b. Metabolic absorption d. Secretion 38. All cells are capable of what process? a. Excretion c. Metabolic absorption b. Movement d. Continuous division Multiple Response Identify one or more choices that best complete the statement or answer the question. 39. What are the major chemical components of the cell membranes? (Select all that apply.) a. Lipids. b. Sodium ions c. Carbohydrates d. DNA e. Proteins 40. Which cells lose their ability to replicate and divide? (Select all that apply.) a. Intestines b. Nerves c. Skin d. Lens of the eye e. Skeletal muscle 41. Which statements are true concerning the process of facilitated diffusion? (Select all that apply). a. Facilitated diffusion is also referred to as passive mediated transport. b. This process expends no metabolic energy. c. Moving solute molecules through cellular membranes are involved in this process. d. Movement up a concentration gradient is necessary. e. Facilitated diffusion is the primary means for water transport. 42. Passive transport is dependent on: (Select all that apply.) a. Semipermeable barrier membrane b. The process of osmosis c. Diffusion as a driving force d. A living host e. Hydrostatic pressure 43. What is the primary function of proteins? (Select all that apply.) a. Proteins are binding units. b. Proteins are transport channels. c. Proteins are ribonucleoproteins. d. Proteins provide cell surface markers. e. Proteins are chemical reaction catalysts. Matching Match the structure with its function. Answers may be used more than once. A. Endoplasmic reticulum B. Ribosome C. Secretory vesicle D. Lysosomes 44. Packages and transports proteins. Endoplasmic reticulum, Ribosome 45. Fuses with the plasma membrane to release contents from the cell. Secretory Vesicle 46. Synthesizes and transports lipids. Endoplasmic reticulum 47. Provides energy to digest proteins into amino acids. Lysosomes Match the structure with its function. Answers may be used more than once. A. Passive-mediated transport B. Active-mediated transport C. Osmosis 48. Movement of water Osmosis 49. Protein carrier Passive-mediated transport & Active-mediated transport 50. Facilitated diffusion Passive-mediated transport Thought Questions 1. With respect to chemical communication and signal transduction, A. Describe three ways in which cells communicate with one another; give an example of each. 1. protein channels (gap junctions) coordinate activity with adjacent cells 2. PM-bound signaling molecules (receptors) affect itself and others in direct contact 3. secrete chemical signals (ligands) b. five forms of signaling mediated by secreted molecules; give an example of each. Intracrine ligands are produced by the target cell itself and bind to a receptor within. Autocrine ligands are finely distinct in that although they are also made by the target cell, they are first secreted and then later bind to the cell as well as neighboring cells (ex. Immune cells). Juxtacrine ligands target adjacent cells (often called “contact-dependent” signaling). Paracrine ligands target cells in the vicinity of the original emitting cell (ex. Neurotransmitters like Acetylcholine). Endocrine cells produce hormones that have the important task of targeting distant cells and often travel through our circulatory system. 2. Describe an example of a molecule(s) transported by active mediated transport (facilitated diffusion); describe active transport and the sodium-potassium pump. An example of facilitated diffusion is the movement of glucose into the cell, where it is used to make ATP. Their diffusion is facilitated by membrane proteins that form sodium channels (or “pores”) so that Na+ ions can move down their concentration gradient from outside the cells to inside the cells. 3. Describe the steps of the cAMP second messenger pathway and identify several cell responses to common neurotransmitters and steroids, which are first messenger molecules to cAMP second messenger pathway. -Second messengers are intracellular signaling molecules released by the cell in response to exposure to extracellular signaling molecules—the first messengers. First messengers are extracellular factors, often hormones or neurotransmitters, such as epinephrine, growth hormone, and serotonin. -AC Pathway. The AC pathway begins with an outside signal, such as a hormone, that binds to a receptor on a cell surface. The receptor then activates a G-protein by causing a change from GDP to GTP. The alpha piece of Gs, when activated, tells the AC to begin changing ATP to Cyclic adenosine monophosphate (cAMP, cyclic AMP, or 3',5'-cyclic adenosine monophosphate) . -cAMP is a second messenger important in many biological processes. cAMP is a derivative of adenosine triphosphate (ATP) and used for intracellular signal transduction in many different organisms, conveying the cAMP-dependent pathway for the activation of specific proteins. Chapter 2: Altered Cellular & Tissue Study Guide Multiple Choice Identify the choice that best completes the statement or answers the question. 1. Which type of cell adaptation occurs when normal columnar ciliated epithelial cells of the bronchial lining have been replaced by stratified squamous epithelial cells? a. Hyperplasia c. Dysplasia b. Metaplasia d. Anaplasia 2. The loss of adenosine triphosphate (ATP) during ischemia causes cells to: a. Shrink because of the influx of calcium (Ca). b. Shrink because of the influx of potassium (KCL). c. Swell because of the influx of sodium chloride (NaCl). d. Swell because of the influx of nitric oxide (NO). 3. The mammary glands enlarge during pregnancy primarily as a consequence of hormonal: a. Atrophy c. Hyperplasia c. Anaplasia d. Dysplasia 4. Free radicals play a major role in the initiation and progression of which diseases? a. Cardiovascular diseases such as hypertension and ischemic heart disease b. Renal diseases such as acute tubular necrosis and glomerulonephritis c. Gastrointestinal diseases such as peptic ulcer disease and Crohn disease d. Muscular disease such as muscular dystrophy and fibromyalgia 5. Free radicals cause cell damage by: a. Stealing the cell’s oxygen to stabilize the electron, thus causing hypoxia b. Stimulating the release of lysosomal enzymes that digest the cell membranes c. Transferring one of its charged, stabilized atoms to the cell membrane, which causes lysis d. Giving up an electron, which causes injury to the chemical bonds of the cell membrane 6. What is a consequence of plasma membrane damage to the mitochondria? a. Enzymatic digestion halts DNA synthesis. b. Influx of calcium ions halts ATP production. c. Edema from an influx in sodium causes a reduction in ATP production. d. Potassium shifts out of the mitochondria, which destroys the infrastructure. 7. What is a consequence of leakage of lysosomal enzymes during chemical injury? a. Enzymatic digestion of the nucleus and nucleolus occurs, halting DNA synthesis. b. Influx of potassium ions into the mitochondria occurs, halting the ATP production. c. Edema of the Golgi body occurs, preventing the transport of proteins out of the cell. d. Shift of calcium out of the plasma membrane occurs, destroying the cytoskeleton. 8. Lead causes damage within the cell by interfering with the action of: a. Sodium and chloride b. Calcium b. Potassium c. ATP 9. Which statement is a description of the characteristics of apoptosis? a. Programmed cell death of scattered, single cells b. Characterized by swelling of the nucleus and cytoplasm c. Unpredictable patterns of cell death d. Results in benign malignancies 10. Lead poisoning affects the nervous system by: a. Interfering with the function of neurotransmitters b. Inhibiting the production of myelin around nerves c. Increasing the resting membrane potential d. Altering the transport of potassium into the nerves 11. Carbon monoxide causes tissue damage by: a. Competing with carbon dioxide so that it cannot be excreted b. Binding to hemoglobin so that it cannot carry oxygen c. Destroying the chemical bonds of hemoglobin so it cannot carry oxygen d. Removing iron from hemoglobin so it cannot carry oxygen 12. Acute alcoholism mainly affects which body system? a. Hepatic c. Renal b. Gastrointestinal d. Central nervous 13. During cell injury caused by hypoxia, an increase in the osmotic pressure occurs within the cell because: a. Plasma proteins enter the cell. b. The adenosine triphosphatase (ATPase)–driven pump is stronger during hypoxia. c. Sodium chloride enters the cell. d. An influx of glucose occurs through the injured cell membranes. 14. Which statement is true regarding the difference between subdural hematoma and epidural hematoma? a. No difference exists, and these terms may be correctly used interchangeably. b. A subdural hematoma occurs above the dura, whereas an epidural hematoma occurs under the dura. c. A subdural hematoma is often the result of shaken baby syndrome, whereas an epidural hematoma rapidly forms as a result of a skull fracture. d. A subdural hematoma usually forms from bleeding within the skull, such as an aneurysm eruption, whereas an epidural hematoma occurs from trauma outside the skull, such as a blunt force trauma. 15. What physiologic change occurs during heat exhaustion? a. Hemoconcentration occurs because of the loss of salt and water. b. Cramping of voluntary muscles occurs as a result of salt loss. c. Thermoregulation fails because of high core temperatures. d. Subcutaneous layers are damaged because of high core temperatures. 16. In hypoxic injury, sodium enters the cell and causes swelling because: a. The cell membrane permeability increases for sodium during periods of hypoxia. b. ATP is insufficient to maintain the pump that keeps sodium out of the cell. c. The lactic acid produced by the hypoxia binds with sodium in the cell. d. Sodium cannot be transported to the cell membrane during hypoxia. 17. What is the most common site of lipid accumulation? a. Coronary arteries c. Liver b. Kidneys d. Subcutaneous tissue 18. What mechanisms occur in the liver cells as a result of lipid accumulation? a. Accumulation of lipids that obstruct the common bile duct, preventing flow of bile from the liver to the gallbladder b. Increased synthesis of triglycerides from fatty acids and decreased synthesis of apoproteins c. Increased binding of lipids with apoproteins to form lipoproteins d. Increased conversion of fatty acids to phospholipids 19. Hemoprotein accumulations are a result of the excessive storage of: a. Iron, which is transferred from the cells to the bloodstream b. Hemoglobin, which is transferred from the bloodstream to the cells c. Albumin, which is transferred from the cells to the bloodstream d. Amino acids, which are transferred from the cells to the bloodstream 20. Hemosiderosis is a condition that results in the excess of what substance being stored as hemosiderin in cells of many organs and tissues? a. Hemoglobin c. Iron b. Ferritin d. Transferrin 21. What is the cause of free calcium in the cytosol that damages cell membranes by uncontrolled enzyme activation? a. Activation of endonuclease interferes with the binding of calcium to protein. b. Activation of phospholipases, to which calcium normally binds, degrades the proteins. c. An influx of phosphate ions competes with calcium for binding to proteins. d. Depletion of ATP normally pumps calcium from the cell. 22. What two types of hearing loss are associated with noise? a. Acoustic trauma and noise-induced c. High frequency and acoustic trauma b. High frequency and low frequency d. Noise-induced and low frequency 23. What type of necrosis results from ischemia of neurons and glial cells? a. Coagulative c. Caseous b. Liquefactive d. Gangrene 24. What type of necrosis is often associated with pulmonary tuberculosis? a. Bacteriologic c. Liquefactive b. Caseous d. Gangrenous 25. What type of necrosis is associated with wet gangrene? a. Coagulative c. Caseous b. Liquefactive d. Gangrene 26. Current research supports the belief that, after heart muscle injury, the damage: a. Remains indefinitely because cardiac cells do not reproduce. b. Is repaired by newly matured cardiomyocytes. c. Gradually decreases in size as mitotic cell division occurs. d. Is replaced by hypertrophy of remaining cells. 27. After ovulation, the uterine endometrial cells divide under the influence of estrogen. This process is an example of hormonal: a. Hyperplasia c. Hypertrophy b. Dysplasia d. Anaplasia 28. The abnormal proliferation of cells in response to excessive hormonal stimulation is called: a. Dysplasia c. Hyperplasia b. Pathologic dysplasia d. Pathologic hyperplasia 29. Removal of part of the liver leads to the remaining liver cells undergoing compensatory: a. Atrophy c. Hyperplasia b. Metaplasia d. Dysplasia 30. What is the single most common cause of cellular injury? a. Hypoxic injury c. Infectious injury b. Chemical injury d. Genetic injury 31. During cell injury caused by hypoxia, sodium and water move into the cell because: a. Potassium moves out of the cell, and potassium and sodium are inversely related. b. The pump that transports sodium out of the cell cannot function because of a decrease in ATP levels. c. The osmotic pressure is increased, which pulls additional sodium across the cell membrane. d. Oxygen is not available to bind with sodium to maintain it outside of the cell. 32. In decompression sickness, emboli are formed by bubbles of: a. Oxygen b. Nitrogen c. Carbon monoxide d. Hydrogen 33. Which is an effect of ionizing radiation exposure? a. Respiratory distress b.Sun intolerance c. DNA aberrations d. Death 34. What is an example of compensatory hyperplasia? a. Hepatic cells increase cell division after part of the liver is excised. b. Skeletal muscle cells atrophy as a result of paralysis. c. The heart muscle enlarges as a result of hypertension. d. The size of the uterus increases during pregnancy. 35. It is true that nondividing cells are: a. Found in gastrointestinal lining c. Incapable of synthesizing DNA b. Affected by hyperplasia d. Affected by only hypertrophy 36.Dysplasia refers to a(n): a. Abnormal increase in the number of a specific cell type b. True adaptive process at the cellular level c. Modification in the shape of a specific cell type d. Lack of oxygen at the cellular level 37.Current research has determined that chemical-induced cellular injury: a. Affects the permeability of the plasma membrane. b. Is often the result of the damage caused by reactive free radicals. c. Is rarely influenced by lipid peroxidation. d. Seldom involves the cell’s organelles. Multiple Response Identify one or more choices that best complete the statement or answer the question. 38. Which organs are affected by lead consumption? (Select all that apply.) a. Bones b. Muscles c. Pancreas d. Nerves e. Eyes 39. What effect does fetal alcohol syndrome have on newborns? (Select all that apply.) a. Failure of alveoli to open b. Cognitive impairment c. Incompetent semilunar values d. Esophageal stricture e. Facial anomalies 40. What organs are affected by the type of necrosis that results from either severe ischemia or chemical injury? (Select all that apply.) a. Lungs b. Brain c. Kidneys d. Muscles e. Heart 41. It is true that melanin is: (Select all that apply.) a. Rarely found in epithelial cells b. Found in cells called keratinocytes, which are present in the retina c. A factor in the prevention of certain types of cancer d. Most influential in managing the effects of short-term sunlight exposure e. Accumulated in specific cells found in the skin 42. Examples of adaptive cellular responses include: (Select all that apply.) a. Atrophy b. Dysplasia c. Hypertrophy d. Hyperplasia e. Metaplasia 43. Blunt force injuries would include a: (Select all that apply.) a. Bruise to the upper arm, resulting from a fall b. Simple tibia fracture sustained in a skiing accident c. Cut on the finger while slicing vegetables for a salad d. Spleen laceration caused by a punch during a physical fight e. Small caliber gunshot wound to the foot while target shooting 44. Which statements are true regarding the effects of marijuana use? (Select all that apply.) a. Smoking the drug results in greater absorption that eating it. b. Heavy use can result in psychomotor impairments. c. Smoking four “joints” a day equals smoking approximately 20 cigarettes. d. Research does not support marijuana use as a factor in developing lung cancer. e. Fetal development appears to be unharmed by marijuana use. Thought Questions 1. Discuss the pathophysiologic processes of cellular injury from hypoxia. In hypoxic states, the lack of oxygen causes a decrease in mitochondrial phosphorylation. To maintain ATP production, the cell switches to anaerobic (glycolytic) metabolism. This results in rapid depletion of glycogen stores, and an accumulation of lactic acid (byproduct of anaerobic metabolism), which decreases the pH of the nucleus, and results in chromatin clumping. The reduction in ATP levels causes the ATP-reliant ion transport pumps in the plasma membrane to fail: Failure of the sodium-calcium exchanger results in intracellular calcium accumulation, while failure of the sodium-potassium pump results in sodium accumulation within the cell, cellular swelling, and diffusion of potassium out of the cell. The damage to the cell membrane changes its permeability, allowing rapid diffusion of even more calcium and water from the extracellular fluid into the cell. The influx of water causes dilation of the endoplasmic reticulum, subsequent ribosomal detachment, and reduced protein synthesis. As this cascade continues, the entire cell becomes swollen with increased concentrations of water, sodium, and chloride, and decreased concentrations of potassium. If oxygen is restored, these changes can be reversed, however with continued hypoxia, vacuolation occurs (formation of vacuoles: small cytoplasmic cavities) within the cytoplasm, there is swelling of the lysosomes and mitochondria, and calcium continues to accumulate. These processes ultimately result in the death of the cell: Digestive enzymes that leak from the swollen lysosomes cause autodigestion of intracellular contents, lysis of the plasma membrane, and cellular death. Alternatively, increased calcium levels activate multiple enzyme systems (proteases, nitric oxide synthase, phospholipases, endonuclease) that result in damage to the cytoskeleton, cellular membrane damage, inflammation, ATP depletion, and DNA and chromatin degradation, leading to cell death. 2. Briefly describe the differences between the various forms of cellular adaptations to disease (atrophy, hypertrophy, hyperplasia, dysplasia, metaplasia). Cellular adaptation is a reversible, structural, or functional response both to normal or physiologic conditions & to adverse or pathologic conditions 1.) Atrophy: decrease or shrinkage in cell size. Most common in skeletal, heart, secondary sex organs & brain. (Physiologic-occurs with early development such as when thymus gland undergoes atrophy during childhood. Pathologic-occurs as a result of decreases in workload, pressure, use, nerve stimulation) 2.) Hypertrophy: increase in size of cells and size of infected organ. Cells of the heart and kidneys are prone to enlargement. Increased size in associated with an increase in accumulation of protein in cellular components (plasma membrane, ER, mitochondria) and NOT with an increase in cellular fluid. can be physiologic or pathologic- caused by specific hormone stimulation or increased functional demand. Two types of signals- a. mechanical signals- stretch b. trophic signals- growth factors, hormones, and vasoactive agents. Ex. Kidney is removed, other kidney is larger. Physiologic- NORMAL, Pathologic- BAD. Pathologic example- hypertension. 3.) Hyperplasia: increase in number of cells resulting from an increased rate of cellular division. As a response to injury, occurs when injury has been severe and prolonged long enough to cause cell death. Hyperplasia and hypertrophy go hand in hand If cells can synthesize DNA. Two types of physiologic- compensatory (adaptative mechanism that causes cells to regenerate) Ex. Compensatory hyperplasia is the callus (thickening) of the skin as a result of hyperplasia of epidermal cells in response to a mechanical stimulus. Removing part of liver leads remaining cells to regenerate for loss and hormonal (in estrogen dependent organs such as uterus and breast. Pregnancy occurs- uterus enlarges. Pathological- abnormal proliferation of normal cells, usually in response to excessive hormonal stimulation or growth. Ex. Hyperplasia of endometrium= excessive menstrual bleeding. 4.) Dysplasia: abnormal changes in size, shape, and organization of mature cells. Not a true adaptive process but related to hyperplasia- called atypical hyperplasia. Does not indicate cancer and may not progress to cancer. 5.) Metaplasia: reversible replacement of 1 mature cell type by another, sometimes less differentiated cell type. Develop from a reprogramming of stem cells that exist on most epithelia or of undifferentiated mesenchymal cells present in connective tissue. EX cigarette smoke replaces cells. Bronchial tubes are normal ciliated epithelial cells replaced with stratified squamous epithelial cells. Bronchial metaplasia can be reversed if the inducing stimulus, usually cigarettes, is removed. With prolonged exposure to the inducing stimulus, dysplasia and cancerous transformation can occur Chapter 3: Fluids, Electrolytes, and Acid-Base Balance Study Guide Multiple Choice Identify the choice that best completes the statement or answers the question 1. Infants are most susceptible to significant losses in the total body water because of an infant’s: a. High body surface-to-body size ratio b. Slow metabolic rate c. Kidneys are not mature enough to counter fluid losses d. Inability to communicate adequately when he or she is thirsty 2. Obesity creates a greater risk for dehydration in people because: a. Adipose cells contain little water because fat is water repelling b. The metabolic rate of obese adults is slower than the rate of lean adults c. The rate of urine output of obese adults is higher than the rate of output of lean adults d. The thirst receptors of the hypothalamus do not function effectively 3. A patient’s blood gases reveal the following findings: pH 7.3; bicarbonate (HCo3) 27 mEq/L; carbon dioxide (CO2), 59 mmHg. What is the interpretation of these gases? a. Respiratory alkalosis b. Metabolic acidosis c. Respiratory acidosis d. Metabolic alkalosis 4. Water movement between the intracellular fluid (ICF) compartment and the extracellular fluid (ECF) compartment is primarily a function of: a. Osmotic forces b. Plasma oncotic pressure c. Antidiuretic hormone d. Hydrostatic forces 5. In addition to osmosis, what force is involved in the movement of water between the plasma and interstitial fluid spaces? a. Oncotic pressure b. Buffering c. Net filtration d. Hydrostatic pressure 6. Venous obstruction is a cause of edema because of an increase in which pressure? a. Capillary hydrostatic b. Interstitial hydrostatic c. Capillary oncotic d. Interstitial oncotic 7. At the arterial end of the capillaries, fluid moves from the intravascular space into the interstitial space because the: a. Interstitial hydrostatic pressure is higher than the capillary hydrostatic pressure b. Capillary hydrostatic pressure is higher than the capillary oncotic pressure c. Interstitial oncotic pressure is higher than the interstitial hydrostatic pressure d. Capillary oncotic pressure is lower than the interstitial hydrostatic pressure 8. Low plasma albumin causes edema as a result of a reduction in which pressure? a. Capillary hydrostatic b. Interstitial hydrostatic c. Plasma oncotic d. Interstitial oncotic 9. Secretion of antidiuretic hormone (ADH) and the perception of thirst are stimulated by a(n): a. Decrease in serum sodium b. Increase in plasma osmolality c. Increase in glomerular filtration rate d. Decrease in osmoreceptor stimulation 10. Thirst activates osmoreceptors by an increase in which blood plasma? a. Antidiuretic hormone b. Aldosterone c. Hydrostatic pressure d. Osmotic pressure 11. It is true that natriuretic peptides: a. Decrease blood pressure and increase sodium and water excretion b. Increase blood pressure and decrease sodium and water excretion c. Increase heart rate and decrease potassium excretion d. Decrease heart rate and increase potassium excretion 12. When changes in total body water are accompanied by proportional changes in electrolytes, what type of alternation occurs? a. Isotonic b. Hypertonic c. Hypotonic d. Normotonic 13. Which enzyme is secreted by the juxtaglomerular cells of the kidney when circulating blood volume is reduced? a. Angiotensin I b. Angiotensin II c. Aldosterone d. Renin 14. What mechanism can cause hypernatremia? a. Syndrome of inappropriate antiduretic hormone b. Hypersecretion of aldosterone c. Brief bouts of vomiting or diarrhea d. Excessive diuretic therapy 15. What causes the clinical manifestations of confusion, convulsions, cerebral hemorrhage, and coma in hypernatremia? a. High sodium in the blood vessels pulls water out of the brain cells into the blood vessels, causing brain cells to shrink b. High sodium in the brain cells pulls water out of the blood vessels into the brain cells, causing them to swell c. High sodium in the blood vessels pulls potassium out of the brain cells, which slows the synapses in the brain d. High sodium in the blood vessels draw chloride into the brain cells followed by water, causing the brain cells to swell 16. Vomiting-induced metabolic alkalosis, resulting in the loss of chloride, causes: a. Retained sodium to bind with the chloride b. Hydrogen to move into the cell and exchange with potassium to maintain cation Balance c. Retention of bicarbonate to maintain the anion balance d. Hypoventilation to compensate for the metabolic alkalosis 17. The pathophysiologic process of edema is related to which mechanism? a. Sodium depletion b. Decreased capillary hydrostatic pressure c. Increased plasma oncotic pressure d. Lymphatic obstruction 18. Insulin is used to treat hyperkalemia because it: a. Stimulates sodium to be removed from the cell in exchange for potassium b. Binds to potassium to remove it through the kidneys c. Transports potassium from the blood to the cell along with glucose d. Breaks down the chemical components of potassium, causing it to be no longer effective 19. A major determinant of the resting membrane potential necessary for the transmission of nerve impulses is the ratio between: a. Intracellular and extracellular Na+ b. Intracellular and extracellular K+ c. Intracellular Na+ and extracellular K+ d. Intracellular K+ and extracellular Na+ 20. During acidosis, the body compensates for the increase in serum hydrogen ions by shifting the hydrogen ions int to the cell in exchange for which electrolyte? a. Oxygen b. Sodium c. Potassium d. Magnesium 21. Causes of hyperkalemia include: a. Hyperparathyroidism and malnutrition b. Vomiting and diarrhea c. Renal failure and Addison disease d. Hyperaldosteronism and Cushing disease 22. In hyperkalemia, what change occurs to the cells’ resting membrane potential? a. Hypopolarization b. Hyperexcitability c. Depolarization d. Repolarization 23. The calcium and phosphate balance is influenced by which three substances? a. Parathyroid hormone, vasopressin, and vitamin D b. Parathyroid hormone, calcitonin, and vitamin D c. Thyroid hormone, vasopressin, and vitamin A d. Thyroid hormone, calcitonin, vitamin A 24. It is true that Kussmaul respirations indicate: a. Anxiety is a cause of respiratory acidosis b. A compensatory measure is needed to correct metabolic acidosis c. Diabetic ketoacidosis is the cause of the metabolic acidosis d. More oxygen is necessary to compensate for respiratory acidosis 25. Chvostek and Trousseau signs indicate which electrolyte imbalance? a. Hypokalemia b. Hyperkalemia c. Hypocalcemia d. Hypercalcemia 26. An excessive use of magnesium-containing antacids and aluminum-containing antacids can result in: a. Hypomagnesemia b. Hypophosphatemia c. Hyponatremia d. Hypokalemia 27. The most common cause of hypermagnesemia is: a. Hepatitis b. Renal failure c. Hyponatremia d. Hypokalemia c. Trauma to the hypothalamus d. Pancreatitis 28. Physiologic pH is maintained at approximately 7.4 because bicarbonate (HCO3) and carbonic acid (H2CO3) exist in a ratio of: a. 20:1 b. 1:20 c. 10:2 d. 10:5 29. Which arterial pH will initiate the formation of ammonium (NH4) from ammonia (NH3), referred to as academia, in the tubular lumen of the kidney? a. 7.25 b. 7.35 c. 7.55 d. 7.65 30. Two thirds of the body’s water is found in its: a. Interstitial fluid spaces b. Vascular system c. Intracellular fluid compartments d. Intraocular fluids 31. It is true that when insulin is administered: a. The Na+, K+–ATPase pump is turned off. b. Potassium is moved out of muscle cells. c. The liver increases its potassium levels. d. Glucose transport is impaired. 32. Increased capillary hydrostatic pressure results in edema because of: a. Losses or diminished production of plasma albumin b. Inflammation resulting from an immune response c. Blockage within the lymphatic channel system d. Sodium and water retention 33. The existence of hyperkalemia is likely to result in which changes to a person’s electrocardiogram (ECG)? a. Flattened U waves b. Peaked T waves c. Depressed ST segments d. Peaked P waves Multiple Response Identify one or more choices that best complete the statement or answer the question. 34. Which groups are at risk for fluid imbalance? (Select all that apply.) a. Women b. Infants c. Men d. Obese persons e. Older adults 35. Dehydration can cause which result? (Select all that apply.) a. Moist mucous membranes b. Weak pulses c. Tachycardia d. Polyuria e. Weight loss 36. Causes of hypocalcemia include: (Select all that apply.) a. Repeated blood administration b. Pancreatitis c. Decreased reabsorption of calcium d. Hyperparathyroidism e. Kidney stones 37. The electrolyte imbalance called hyponatremia exhibits which clinical manifestations? (Select all that apply.) a. Headache b. Seizures c. Paranoia d. Confusion e. Lethargy 38. The electrolyte imbalance hypercalcemia exhibits which clinical manifestations? (Select all that apply.) a. Diarrhea b. Calcium based kidney stones c. ECG showing narrow T waves d. Lethargy e. Bradycardia 39. The electrolyte imbalance hypokalemia exhibits which clinical manifestations? (Select all that apply.) a. Paralytic ileus b. Sinus bradycardia c. Atrioventricular block d. Dry mucous membranes e. Tetany 40. A third of the body’s fluid is contained in the extracellular interstitial fluid spaces that include: (Select all that apply.) a. Urine b.Intraocular fluids c.Lymph d.Blood plasma e.Sweat 41. An imbalance of potassium can produce which dysfunctions? (Select all that apply.) a. Weakness skeletal muscles b. Cardiac dysrhythmias c. Smooth muscle atony d. Visual impairment e. Hearing loss 42. Which statements regarding total body water (TBW) are true? (Select all that apply.) a. During childhood, TBW slowly decreases in relationship to body weight. b. Gender has no influence on TBW until old age. c. Men tend to have greater TBW as a result of their muscle mass. d. Estrogen plays a role in female TBW. e. Older adults experience a decrease in TBW as a result of decreased muscle mass. Matching Match the electrolytes with the corresponding descriptions. Terms may be used more than once. A. Sodium B. Chloride C. Potassium D. Magnesium E. Phosphate 43. Regulates osmolality in the extracellular fluid (ECF) space. A-Sodium 44. Is inversely related to HCO3 concentration. B- Chloride 45. Is a major determinant of resting membrane potential. C- Potassium 46. An intracellular metabolic form is adenosine triphosphate (ATP). E- Phosphate 47. Changes in hydrogen ion concentration affect this electrolyte. C- Potassium Thought Question Describe edema and the four most common mechanisms of edema formation. Edema is the excessive accumulation of fluid within the interstitial spaces. The four common mechanisms are: 1. Increased capillary hydrostatic pressure 2. Decreased capillary oncotic pressure 3. Increased capillary membrane permeability 4. Lymphatic obstruction Describe the three types of alterations in sodium, chloride and water imbalance (isotonic, hypertonic and hypotonic alterations) Isotonic: (isoosmolar) Gain or loss of extracellular fluid (ECF) resulting in a concentrated equivalent to a 0.9% sodium chloride solution (normal saline); no shrinkage or swelling of the cell. Hypertonic: (hyperosmolar) Imbalance that results in an ECF concentration >0.9% salt solution; that is, water loss or solute gain; cells shrink in a hypertonic fluid. Hypotonic: (hypoosmolar) Imbalance that results in an ECF <0.9% salt solution; that is, water gain or solute loss; cells swell in a hypotonic fluid. Describe the manifestations of alterations in potassium, calcium, phosphate and magnesium balance. Potassium: Hypokalemia Decreased neuromuscular excitability Skeletal muscle weakness Smooth muscle atony Cardiac dysrhythmias Hyperkalemia U wave on electrocardiogram (ECG) Increased intake Shift of K+ from ICF to ECF Decreased renal excretion Hypoxia Acidosis Insulin deficiency Cell trauma Digitalis overdose Calcium: Hypocalcemia Increased neuromuscular excitability (partial depolarization) Muscle spasms Chvostek and Trousseau signs Convulsions Tetany Hypercalcemia Decreased neuromuscular excitability Weakness Kidney stones Constipation Heart block Phosphate: Hypophosphatemia Diminished release of oxygen osteomalacia (soft bones) muscle weakness bleeding disorders (platelet impairment) leukocyte alterations rickets Hyperphosphatemia Same as hypocalcemia with possible calcification of soft tissue Magnesium: Hypomagnesemia From malabsorption Associated with hypocalcemia and hypokalemia Neuromuscular irritability Tetany, convulsions Increased reflexes Hypermagnesemia From renal failure Skeletal muscle depression Muscle weakness Hypotension Respiratory depression Bradycardia Chapter 7: Innate Immunity Study Guide Multiple Choice Identify the choice that best completes the statement or answers the question. Chapter 7 Multiple Choice Identify the choice that best completes the statement or answers the question. ____ 1. Which action is a purpose of the inflammatory process? a. To provide specific responses toward antigens b. To lyse cell membranes of microorganisms c. To prevent infection of the injured tissue d. To create immunity against subsequent tissue injury ____ 2. How do surfactant proteins A through D provide innate resistance? a. Initiate the complement cascade. b. Promote phagocytosis. c. Secrete mucus. d. Synthesize lysosomes. ____ 3. Which secretion is a first line of defense against pathogen invasion that involves antibacterial and antifungal fatty acids, as well as lactic acid? a. Optic tears b. Oral saliva c. Sweat gland perspiration d. Sebaceous gland sebum ____ 4. Which bacterium grows in the intestines after prolonged antibiotic therapy? a. Lactobacillus b. Candida albicans c. Clostridium difficile d. Helicobacter pylori ____ 5. What causes the edema that occurs during the inflammatory process? a. Vasodilation of blood vessels b. Increased capillary permeability c. Endothelial cell expansion d. Emigration of neutrophils ____ 6. What process causes heat and redness to occur during the inflammatory process? a. Vasodilation of blood vessels b. Platelet aggregation c. Decreased capillary permeability d. Endothelial cell contraction ____ 7. What does activation of the classical pathway begin with? a. Viruses b. Antigen-antibody complexes c. Mast cells d. Macrophages ____ 8. What plasma protein system forms a fibrinous meshwork at an inflamed site? a. Complement b. Coagulation c. Kinin d. Fibrinolysis ____ 9. Which component of the plasma protein system tags pathogenic microorganisms for destruction by neutrophils and macrophages? a. Complement cascade b. Coagulation system c. Kinin system d. Immune system ____ 10. What is the vascular effect of histamine released from mast cells? a. Platelet adhesion b. Initiation of the clotting cascade c. Vasodilation d. Increased endothelial adhesiveness ____ 11. What is an outcome of the complement cascade? a. Activation of the clotting cascade b. Prevention of the spread of infection to adjacent tissues c. Inactivation of chemical mediators such as histamine d. Lysis of bacterial cell membranes ____ 12. What is the function of opsonization related to the complement cascade? a. To tag pathogenic microorganisms for destruction by neutrophils and macrophages b. To process pathogenic microorganisms so that activated lymphocytes can be created for acquired immunity c. To destroy glycoprotein cell membranes of pathogenic microorganisms d. To promote anaphylatoxic activity, resulting in mast cell degranulation ____ 13. In the coagulation (clotting) cascade, the intrinsic and the extrinsic pathways converge at which factor? a. XII b. VII c. X d. V ____ 14. Which chemical interacts among all plasma protein systems by degrading blood clots, activating complement, and activating the Hageman factor? a. Kallikrein b. Histamine c. Bradykinin d. Plasmin ____ 15. How does the chemotactic factor affect the inflammatory process? a. By causing vasodilation around the inflamed area b. By stimulating smooth muscle contraction in the inflamed area c. By directing leukocytes to the inflamed area d. By producing edema around the inflamed area ____ 16. What effect does the process of histamine binding to the histamine-2 (H2) receptor have on inflammation? a. Inhibition b. Activation c. Acceleration d. Termination ____ 17. Frequently when H1 and H2 receptors are located on the same cells, they act in what fashion? a. Synergistically b. Additively c. Antagonistically d. Agonistically ____ 18. Some older adults have impaired inflammation and wound healing because of which problem? a. Circulatory system cannot adequately perfuse tissues. b. Complement and chemotaxis are deficient. c. Underlying chronic illness(es) exists. d. Number of mast cells is insufficient. ____ 19. Which chemical mediator derived from mast cells retracts endothelial cells to increase vascular permeability and to cause leukocyte adhesion to endothelial cells? a. Chemokines b. Prostaglandin E c. Platelet-activating factor d. Bradykinin ____ 20. What is the inflammatory effect of nitric oxide (NO)? a. Increases capillary permeability, and causes pain b. Increases neutrophil chemotaxis and platelet aggregation c. Causes smooth muscle contraction and fever d. Decreases mast cell function, and decreases platelet aggregation ____ 21. What is the correct sequence in phagocytosis? a. Engulfment, recognition, fusion, destruction b. Fusion, engulfment, recognition, destruction c. Recognition, engulfment, fusion, destruction d. Engulfment, fusion, recognition, destruction ____ 22. When considering white blood cell differentials, acute inflammatory reactions are related to elevations of which leukocyte? a. Monocytes b. Eosinophils c. Neutrophils d. Basophils ____ 23. In the later stages of an inflammatory response, which phagocytic cell is predominant? a. Neutrophils b. Monocytes c. Chemokines d. Eosinophils ____ 24. In regulating vascular mediators released from mast cells, the role of eosinophils is to release what? a. Arylsulfatase B, which stimulates the formation of B lymphocytes b. Histaminase, which limits the effects of histamine during acute inflammation c. Lysosomal enzymes, which activate mast cell degranulation during acute inflammation d. Immunoglobulin E, which defends the body against parasites ____ 25. What is a role of a natural killer (NK) cells? a. Initiation of the complement cascade b. Elimination of malignant cells c. Binding tightly to antigens d. Proliferation after immunization with antigen ____ 26. Which cytokine is produced and released from virally infected host cells? a. IL-1 b. IL-10 c. TNF-? d. IFN-? ____ 27. Which manifestation of inflammation is systemic? a. Formation of exudates b. Fever and leukocytosis c. Redness and heat d. Pain and edema ____ 28. The acute inflammatory response is characterized by fever that is produced by the hypothalamus being affected by what? a. Endogenous pyrogens b. Bacterial endotoxin c. Antigen-antibody complexes d. Exogenous pyrogens ____ 29. What occurs during the process of repair after tissue damage? a. Nonfunctioning scar tissue replaces destroyed tissue. b. Regeneration occurs; the original tissue is replaced. c. Resolution occurs; tissue is regenerated. d. Epithelialization replaces destroyed tissue. ____ 30. What is the role of fibroblasts during the reconstructive phase of wound healing? a. Generate new capillaries from vascular endothelial cells around the wound. b. Establish connections between neighboring cells and contract their fibers. c. Synthesize and secrete collagen and the connective tissue proteins. d. Provide enzymes that débride the wound bed of dead cells. ____ 31. A keloid is the result of which dysfunctional wound healing response? a. Epithelialization b. Contraction c. Collagen matrix assembly d. Maturation ____ 32. A student is preparing to irrigate a patient’s wound and gathers supplies, including hydrogen peroxide. What response by the health care professional is best? a. Help the student gather the rest of the supplies. b. Instruct the student to dilute the hydrogen peroxide. c. Tell the student to get some normal saline instead. d. Ask the patient if pain medication is needed first. ____ 33. Many neonates have a transient depressed inflammatory response as a result of which condition? a. The circulatory system is too immature to perfuse tissues adequately. b. Complement and chemotaxis are deficient. c. Mast cells are lacking. d. The respiratory system is too immature to deliver oxygen to tissues. ____ 34. During phagocytosis, what is occurring during the step referred to as opsonization? a. Phagocytes recognize and adhere to the bacteria. b. Microorganisms are ingested. c. Microorganisms are killed and digested. d. An intracellular phagocytic vacuole is formed. ____ 35. Fusion is the step of phagocytosis during which what happens? a. Microorganisms are killed and digested. b. An intracellular phagocytic vacuole is formed. c. Lysosomal granules enter the phagocyte. d. Microorganisms are ingested. ____ 36. What does the phagosome step result in during the process of endocytosis? a. Microorganisms are ingested. b. Microorganisms are killed and digested. c. Phagocytes recognize and adhere to bacteria. d. An intracellular phagocytic vacuole is formed. ____ 37. When cellular damage occurs and regeneration is minor with no significant complications, what is the process of returning the cells to preinjury function referred to as? a. Restoration b. Resolution c. Regrowth d. Replacement ____ 38. Newborns often have deficiencies in collectin-like proteins, making them more susceptible to what type of infection? a. Cardiac b. Urinary c. Respiratory d. Gastrointestinal ____ 39. Which cell is the body’s primary defense against parasite invasion? a. Eosinophil b. Neutrophils c. T lymphocytes d. B lymphocytes Multiple Response Identify one or more choices that best complete the statement or answer the question. ____ 40. Which chemical mediators induce pain during an inflammatory response? (Select all that apply.) a. Prostaglandins b. Leukotrienes c. Tryptase d. Phospholipase e. Bradykinin ____ 41. What do sebaceous glands secrete in order to protect the body from infection? (Select all that apply.) a. Antibacterial fatty acids b. Antifungal fatty acids c. Ascorbic acid d. Lactic acid e. Hydrochloric acid ____ 42. Which body fluids have the ability to attack the cell walls of gram-positive bacteria? (Select all that apply.) a. Perspiration b. Semen c. Tears d. Saliva e. Urine ____ 43. What do the main functions of NK cells include? (Select all that apply.) a. Recognizing virus-infected cells b. Eliminating virus-infected cells c. Recognizing bacteria-infected cells d. Eliminating bacteria-infected cells e. Eliminating previously identified cancer cells ____ 44. An individual’s acquired immunity is dependent on the function of which cells? (Select all that apply.) a. T lymphocytes b. B lymphocytes c. Macrophages d. Opsonins e. Neutrophils ____ 45. Examples of pathogens capable of surviving and even multiplying inside a macrophage include what? (Select all that apply.) a. Mycobacterium tuberculosis (tuberculosis) b. Mycobacterium leprae (leprosy) c. Salmonella typhi (typhoid fever) d. Clostridium difficile e. Brucella abortus (brucellosis) ____ 46. An older adult is particularly susceptible to infections of which body parts? (Select all that apply.) a. Lungs b. Skin c. Liver d. Eyes e. Bladder Chapter 8: Adaptive Immunity Study Guide Multiple Choice Identify the choice that best completes the statement or answers the question. ____ 1. Which primary characteristic is unique for the immune response? a. The immune response is similar each time it is activated. b. The immune response is specific to the antigen that initiates it. c. The response to a specific pathogen is short term. d. The response is innate, rather than acquired. ____ 2. In which structure does B lymphocytes mature and undergo changes that commit them to becoming B cells? a. Thymus gland b. Regional lymph nodes c. Bone marrow d. Spleen ____ 3. What is the term for the process during which lymphoid stem cells migrate and change into either immunocompetent T cells or immunocompetent B cells? a. Clonal diversity b. Clonal differentiation c. Clonal selection d. Clonal competence ____ 4. Which type of immunity is produced by an individual after either natural exposure to the antigen or after immunization against the antigen? a. Passive-acquired immunity b. Active-acquired immunity c. Passive-innate immunity d. Active-innate immunity ____ 5. What type of immunity is produced when an immunoglobulin crosses the placenta? a. Passive-acquired immunity b. Active-acquired immunity c. Passive-innate immunity d. Active-innate immunity ____ 6. The portion of the antigen that is configured for recognition and binding is referred to as what type of determinant? a. Immunotope b. Paratope c. Epitope d. Antigenitope ____ 7. Which characteristic is the most important determinant of immunogenicity when considering the antigen? a. Size b. Foreignness c. Complexity d. Quantity ____ 8. A student asks why some vaccinations are given orally and some are given by injection. What response by the professor is best? a. Different routes allow the speed of onset of the antigen to be varied, with the intravenous route being the fastest. b. Some individuals appear to be unable to respond to an antigen by a specific route, thus requiring the availability of different routes for the same antigen. c. Antigen-presenting cells are highly specialized and thus require stimulation by different routes. d. Each route stimulates a different lymphocyte-containing tissue, resulting in different types of cellular and humoral immunity. ____ 9. The functions of the major histocompatibility complex (MHC) and CD1 molecules are alike because both do what? a. Are antigen-presenting molecules b. Bind antigens to antibodies c. Secrete interleukins during the immune process d. Are capable of activating cytotoxic T lymphocytes ____ 10. Where are antibodies produced? a. Helper T lymphocytes b. Thymus gland c. Plasma cells d. Bone marrow ____ 11. Which immunoglobulin is present in blood, saliva, breast milk, and respiratory secretions? a. IgA b. IgE c. IgG d. IgM ____ 12. Which antibody initially indicates a typical primary immune response? a. IgG b. IgM c. IgA d. IgE ____ 13. An individual is more susceptible to infections of mucous membranes when he or she has a seriously low level of which immunoglobulin antibody? a. IgG b. IgM c. IgA d. IgE ____ 14. How does the B-cell receptor (BCR) complex function? a. Communicating information about the antigen to the helper T cell b. Secreting chemical signals to communicate between cells c. Releasing histamine and other vasoactive substances d. Communicating information about the antigen to the cell nucleus ____ 15. The generation of clonal diversity occurs primarily during which phase of life? a. Fetal b. Neonatal c. Infancy d. Puberty ____ 16. A student is confused about the process of the generation of clonal diversity. What description by the professor is best? a. It involves antigens that select those lymphocytes with compatible receptors. b. It allows the differentiation of cells into antibody-secreting plasma cells or mature Peyer patches. c. It takes place in the primary (central) lymphoid organs. d. It causes antigens to expand and diversify their populations. ____ 17. Which is an example of an endogenous antigen? a. Yeast b. Cancer cells c. Bacteria d. Fungus ____ 18. Which cytokine is needed for the maturation of a functional helper T cell? a. IL-1 b. IL-2 c. IL-4 d. IL-12 ____ 19. Th2 cells produce IL-4 and suppress which cells? a. B lymphocytes b. Cytotoxic T lymphocytes c. Th1 cells d. Memory T lymphocytes ____ 20. Which statement is believed to be true concerning Th1 cells? a. Th1 cells are induced by antigens derived from allergens. b. They are induced by antigens derived from cancer cells. c. Th1 cells produce IL-4, IL-5, IL-6, and IL-13. d. They assist in the development of humoral immunity. ____ 21. Which statement is believed to be true concerning Th2 cells? a. Th2 cells are induced by antigens derived from allergens. b. They are induced by antigens derived from cancer cells. c. Th2 cells produce IL-2, TNF-ß, and IFN-g. d. They assist in the development of cell-mediated immunity. ____ 22. When a person is exposed to most antigens, antibodies can be usually detected in their circulation within what timeframe? a. 12 hours b. 24 hours c. 3 days d. 6 days ____ 23. Vaccinations are able to provide protection against certain microorganisms because of what? a. Strong response from IgM b. Level of protection provided by IgG c. Memory cells for IgE d. Rapid response from IgA ____ 24. The healthcare professional working with older adults teaches general infection-prevention measures as a priority for this age group due to which change in lymphocyte function? a. Increased production of antibodies against self-antigens b. Decreased number of circulating T cells c. Decreased production of autoantibodies d. Increased production of helper T cells ____ 25. How do antibodies protect the host from bacterial toxins? a. Lysing the cell membrane of the toxins b. Binding to the toxins to neutralize their biologic effects c. Inhibiting the synthesis of DNA proteins needed for growth d. Interfering with the DNA enzyme needed for replication ____ 26. Which T cell controls or limits the immune response to protect the host’s own tissues against an autoimmune response? a. Cytotoxic T cells b. Th1 cells c. Th2 cells d. Regulatory T (Treg) cells ____ 27. Evaluation of umbilical cord blood can confirm that which immunoglobulin level is near adult levels? a. IgA b. IgG c. IgM d. IgE ____ 28. Which statement is true concerning IgM? a. IgM is the first antibody produced during the initial response to an antigen. b. IgM mediates many common allergic responses. c. IgM is the most abundant class of immunoglobulins. d. IgM is capable of crossing the human placenta. ____ 29. Which cell has the ability to recognize antigens presented by the MHC class I molecules? a. T cytotoxic b. CD 4 c. CD 8 d. T helper ____ 30. Which cell has a role in developing cell-mediated immunity? a. Th1 b. CD4 c. CD8 d. Th2 ____ 31. A student asks the healthcare professional how the aging process of the T-cell activity affects older adults. What response by the professional is best? a. Poor heat regulation abilities b. Increased risk for bone fractures c. Tendency to develop various infections d. Likelihood of experiencing benign skin lesions ____ 32. Which statement is true regarding maternal antibodies provided to the neonate? a. The antibodies enter into the fetal circulation by means of active transport. b. The antibodies are transferred to the fetus via the lymphatic system. c. The antibodies are directly related to the mother’s nutritional intake. d. The antibodies reach protective levels after approximately 6 months of age. ____ 33. Antibodies that are associated with mucosal immune system, such as immunoglobulins, function to prevent which type of infections? a. Infections that attack the respiratory system b. Infections that tend to be chronic in nature c. Infections likely to be resistant to antibiotics d. Infections that focus on epithelial surfaces of the body ____ 34. Cytokines are vital to a cell’s ability to do which function? a. Excrete b. Reproduce c. Metabolize d. Communicate Multiple Response Identify one or more choices that best complete the statement or answer the question. ____ 35. Which is an example of a bacterial toxin that has been inactivated but still retains its immunogenicity to protect the person? (Select all that apply.) a. Poliomyelitis b. Measles c. Tetanus d. Gonorrhea e. Diphtheria ____ 36. Which statements are true concerning the humoral immune response? (Select all that apply.) a. The humoral immune response is divided into major and minor phases. b. The response has IgG and IgM produced during each of its phrases. c. It has a greater presence of IgG than IgM in one of its phases. d. The humoral immune response is produced in reaction to the presence of an antigen. e. Phases differ in their response time as a result of the effect of memory cells. ____ 37. CD4 is a characteristic surface marker and a result of which of these? (Select all that apply.) a. Activity in the primary lymphoid organs b. Process of cellular differentiation c. Alterations to T cells d. Changes to B cells e. Clonal selection ____ 38. What are the necessary components of an adaptive immune response? (Select all that apply.) a. Antigen b. Gamma IgG c. Lymphocyte surface receptors d. Crystalline fragment e. Antibody Chapter 9 Alteration in Immunity and Inflammation Multiple Choice Identify the choice that best completes the statement or answers the question. ____ 1. How is hypersensitivity best defined? a. A disturbance in the immunologic tolerance of self-antigens b. An immunologic reaction of one person to the tissue of another person c. An altered immunologic response to an antigen that results in disease d. An undetectable immune response in the presence of antigens ____ 2. What is a hypersensitivity reaction that produces an allergic response called? a. Hemolytic shock b. Anaphylaxis c. Necrotizing vasculitis d. Systemic erythematosus ____ 3. The common hay fever allergy is expressed through a reaction that is mediated by which class of immunoglobulins? a. IgE b. IgG c. IgM d. T cells ____ 4. What are blood transfusion reactions an example of? a. Autoimmunity b. Alloimmunity c. Homoimmunity d. Hypersensitivity ____ 5. During an IgE-mediated hypersensitivity reaction, which leukocyte is activated? a. Neutrophils b. Monocytes c. Eosinophils d. T lymphocytes ____ 6. During an IgE-mediated hypersensitivity reaction, what causes bronchospasm? a. Bronchial edema caused by the chemotactic factor of anaphylaxis b. Bronchial edema caused by binding of the cytotropic antibody c. Smooth muscle contraction caused by histamine bound to H1 receptors d. Smooth muscle contraction caused by histamine bound to H2 receptors ____ 7. A patient is having an IgE-mediated hypersensitivity reaction. What action by the healthcare professional is best? a. Give the patient an antihistamine. b. Prepare to give the patient a blood transfusion. c. Ask the patient is he/she is having pain at the site. d. Apply warm, moist heat to the affected area. ____ 8. What characteristic do atopic individuals have that make them genetically predisposed to develop allergies? a. Greater quantities of histamine b. More histamine receptors c. Greater quantities of IgE d. A deficiency in epinephrine ____ 9. A student asks about the mechanism that results in type II hypersensitivity reactions. What description by the professor is best? a. Antibodies coat mast cells by binding to receptors that signal its degranulation, followed by a discharge of preformed mediators. b. Antibodies bind to soluble antigens that were released into body fluids, and the immune complexes are then deposited in the tissues. c. Cytotoxic T lymphocytes or lymphokine-producing helper T 1 cells directly attack and destroy cellular targets. d. Antibodies bind to the antigens on the cell surface. ____ 10. When mismatched blood is administered causing an ABO incompatibility, how are the erythrocytes destroyed? a. Complement-mediated cell lysis b. Phagocytosis by macrophages c. Phagocytosis in the spleen d. Natural killer cells ____ 11. When antibodies are formed against red blood cell antigens of the Rh system, how are the blood cells destroyed? a. Complement-mediated cell lysis b. Phagocytosis by macrophages c. Phagocytosis in the spleen d. Neutrophil granules and toxic oxygen products ____ 12. When soluble antigens from infectious agents enter circulation, what is tissue damage a result of? a. Complement-mediated cell lysis b. Phagocytosis by macrophages c. Phagocytosis in the spleen d. Neutrophil granules and toxic oxygen products ____ 13. How are target cells destroyed in a type II hypersensitivity reaction? a. Tissue damage from mast cell degranulation b. Antigen-antibody complexes deposited in vessel walls c. Cytotoxic T lymphocytes attack the cell directly. d. Natural killer cells ____ 14. Graves disease (hyperthyroidism) is an example of which type II hypersensitivity reaction? a. Modulation b. Antibody-dependent cell-mediated cytotoxicity c. Neutrophil-mediated damage d. Complement-mediated lysis ____ 15. Type III hypersensitivity reactions are a result of which of these? a. Antibodies coating mast cells by binding to receptors that signal its degranulation, followed by the discharge of preformed mediators b. Antibodies binding to soluble antigens that were released into body fluids and the immune complexes being deposited in the tissues c. Tc cells or lymphokine-producing Th1 cells directly attacking and destroying cellular targets d. Antibodies binding to the antigen on the cell surface ____ 16. A type IV hypersensitivity reaction causes which result? a. Antibodies coating mast cells by binding to receptors that signal its degranulation, followed by the discharge of preformed mediators b. Antibodies binding to soluble antigens that were released into body fluids and the immune complexes being deposited in the tissues c. Lymphokine-producing Th1 cells directly attacking and destroying cellular targets d. Antibodies binding to the antigen on the cell surface ____ 17. In a type III hypersensitivity reaction, the harmful effects after the immune complexes that are deposited in tissues are a result of what? a. Cytotoxic T cells b. Natural killer cells c. Complement activation d. Degranulation of mast cells ____ 18. A healthcare professional is teaching a patient about Raynaud phenomenon and instructs the patient to avoid cold. What is the best explanation of how cold impacts the manifestations of this disease? a. Immune complexes that are deposited in capillary beds, blocking circulation b. Mast cells that are bound to specific endothelial receptors, causing them to degranulate and creating a localized inflammatory reaction that occludes capillary circulation c. Cytotoxic T cells that attack and destroy the capillaries so that they are unable to perfuse local tissues d. Antibodies that detect the capillaries as foreign protein and destroy them using lysosomal enzymes and toxic oxygen species ____ 19. Deficiencies in which element can produce depression of both B- and T-cell function? a. Iron b. Zinc c. Iodine d. Magnesium ____ 20. An Rh-negative woman gave birth to an Rh-positive baby. When discussing Rho[D] immunoglobulin with her, what information should the healthcare professional provide? a. It provides protection against infection from poor immunity in the baby. b. It prevents alloimmunity and hemolytic anemia of the newborn. c. It provides necessary antibodies in case the mother doesn’t breastfeed. d. It causes the intestinal tract of the newborn to produce antibodies. ____ 21. Tissue damage caused by the deposition of circulating immune complexes containing an antibody against the host DNA is the cause of which disease? a. Hemolytic anemia b. Pernicious anemia c. Systemic lupus erythematosus d. Myasthenia gravis ____ 22. A patient asks the healthcare professional why tissue damage occurs in acute rejection after organ transplantation. What response by the professional is best? a. Th1 cells release cytokines that activate infiltrating macrophages, and cytotoxic T cells directly attack the endothelial cells of the transplanted tissue. b. Circulating immune complexes are deposited in the endothelial cells of transplanted tissue, where the complement cascade lyses tissue. c. Receptors on natural killer cells recognize antigens on the cell surface of transplanted tissue, which releases lysosomal enzymes that destroy tissue. d. Antibodies coat the surface of transplanted tissue to which mast cells bind and liberate preformed chemical mediators that destroy tissue. ____ 23. Which blood cell carries the carbohydrate antigens for blood type? a. Platelets b. Neutrophils c. Lymphocytes d. Erythrocytes ____ 24. A person with type O blood needs a blood transfusion. What blood type does the healthcare professional prepare to administer to the patient? a. A b. B c. AB d. O ____ 25. Which class of immunoglobulins forms isohemagglutinins? a. IgA b. IgE c. IgG d. IgM ____ 26. Which component of the immune system is deficient in individuals with infections caused by viruses, fungi, or yeast? a. Natural killer cells b. Macrophages c. B cells d. T cells ____ 27. A child in the clinic has an absence of a parathyroid gland, structural heart defects, and a shortened structure of the upper lip. What immune dysfunction does the healthcare professional suspect? a. Partial-to-complete absence of T-cell immunity b. X-linked recessive microcephaly c. An autoimmune disease like systemic lupus erythematosus d. Adenosine deaminase deficiency ____ 28. How many months does it take for the newborn to be sufficiently protected by antibodies produced by its own B cells? a. 1 to 2 b. 4 to 5 c. 6 to 8 d. 10 to 12 ____ 29. Considering the effects of nutritional deficiencies on the immune system, severe deficits in calories and protein lead to deficiencies in the formation of which immune cells? a. B cells b. T cells c. Natural killer cells d. Neutrophils ____ 30. Urticaria is a manifestation of a which type of hypersensitivity reaction? a. IV b. III c. II d. I ____ 31. What is Graves disease a result of? a. Increased levels of circulating immunoglobulins b. The infiltration of the thyroid with T lymphocytes c. Autoantibodies binding to thyroid-stimulating hormone (TSH)-receptor sites d. Exposure to acetylates in substances such as rubber ____ 32. Raynaud phenomenon is an example of which type of hypersensitivity? a. IV b. III c. II d. I ____ 33. Which statement is true concerning an atopic individual? a. They tend to produce less IgE. b. They tend to produce more Fc receptors. c. They tend to attract very few mast cells. d. They tend to produce very high levels of IgM. ____ 34. Which statement is true regarding immunodeficiency? a. Immunodeficiency is generally not present in other family members. b. Immunodeficiency is never acquired; rather, it is congenital. c. Immunodeficiency is almost immediately symptomatic. d. Immunodeficiency is a result of a postnatal mutation. ____ 35. A person with type O blood is considered to be the universal blood donor because type O blood contains which of these? a. No antigens b. No antibodies c. Both A and B antigens d. Both A and B antibodies ____ 36. Immunoglobulin E (IgE) is associated with which type of hypersensitivity reaction? a. I b. II c. III d. IV ____ 37. A pregnant woman has Graves disease. What test/s does the healthcare professional advise the woman about? a. Frequent tests of the newborn’s muscular strength and movement. b. Blood test for hyperthyroidism c. Monthly OB checkups for fetal anomalies or pregnancy loss d. Serum complete blood count including platelet count Multiple Response Identify one or more choices that best complete the statement or answer the question. ____ 38. When a tuberculin skin test is positive, the hard center and erythema surrounding the induration are a result of which of these? (Select all that apply.) a. Histamine b. T lymphocytes c. Immune complexes d. Products of complement e. Macrophages ____ 39. Exposure to which of these could result in a type IV hypersensitivity reaction? (Select all that apply.) a. Poison ivy b. Neomycin c. Dairy products d. Nickel e. Detergents ____ 40. Which disorders are considered autoimmune? (Select all that apply.) a. Crohn disease b. Addison disease c. Rheumatoid arthritis d. Systemic lupus erythematosus e. Type 2 diabetes ____ 41. Which statements best define acute rejection? (Select all that apply.) a. Acute rejection is a cell-mediated immune response. b. Acute rejection is usually a type III rejection. c. Immunosuppressive drugs delay or lessen the intensity of an acute rejection. d. Acute rejection is associated with the body’s response to an organ transplant. e. Acute rejection is a response against unmatched human leukocyte antigens (HLAs). Thought Questions Briefly compare and contrast the four different types of hypersensitivity reactions. Be able to discuss the mediators and responses to the mediators; provide an example of each reaction. Briefly describe the pathophysiologic mechanism of the autoimmune disorders SLE and transfusion reactions. What are the pathophysiologic principles on which gamma-globulin therapies are based? Chapter 10: Infection ____ 1. What is a significant cause of morbidity and mortality worldwide? a. Starvation b. Traumatic injury c. Cardiovascular disease d. Infectious disease ____ 2. What is the first stage in the infectious process? a. Invasion b. Colonization c. Spread d. Multiplication ____ 3. Which type of microorganism reproduces on the skin? a. Viruses b. Bacteria and fungi c. Protozoa and Rickettsiae d. Mycoplasma ____ 4. Phagocytosis involves neutrophils actively attacking, engulfing, and destroying which microorganisms? a. Bacteria b. Fungi c. Viruses d. Yeasts ____ 5. Once they have penetrated the first line of defense, which microorganisms do natural killer (NK) cells actively attack? a. Bacteria b. Fungi c. Viruses d. Mycoplasma ____ 6. A student asks the healthcare professional to describe exotoxins. Which statement by the professional is best? a. Exotoxins are contained in cell walls of gram-negative bacteria. b. Exotoxins are released during the lysis of bacteria. c. Exotoxins are able to initiate the complement and coagulation cascades. d. Exotoxins are released during bacterial growth. ____ 7. A healthcare professional student is learning about fungal infections. What information should the student use to help another student understand? a. Fungal infections occur only on skin, hair, and nails. b. Phagocytes and T lymphocytes control fungal infections. c. Fungal infections release endotoxins. d. Vaccines prevent fungal infections. ____ 8. Cytokines are thought to cause fevers by stimulating the synthesis of which chemical mediator? a. Leukotriene b. Histamine c. Prostaglandin d. Bradykinin ____ 9. Considering the hypothalamus, what is a fever produced by? a. Endogenous pyrogens acting directly on the hypothalamus b. Exogenous pyrogens acting directly on the hypothalamus c. Immune complexes acting indirectly on the hypothalamus d. Cytokines acting indirectly on the hypothalamus ____ 10. A healthcare professional is conducting community education on vaccinations. Which statement about vaccines does the professional include in the presentation? a. Most bacterial vaccines contain attenuated organisms. b. Most viral vaccines are made by using dead organisms. c. Vaccines require booster injections to maintain life-long protection. d. Vaccines provide effective protection against most infections. ____ 11. What are vaccines against viruses created from? a. Killed organisms or extracts of antigens b. Live organisms weakened to produce antigens c. Purified toxins that have been chemically detoxified d. Recombinant pathogenic protein ____ 12. What does the student learn about HIV? a. HIV only infects T-helper (Th) cells. b. HIV is a retrovirus. c. HIV carries genetic information in its DNA. d. HIV has five identified strains. ____ 13. What is the role of reverse transcriptase in HIV infection? a. Reverse transcriptase converts single-stranded DNA into double-stranded DNA. b. It is needed to produce integrase. c. It transports the RNA into the cell nucleus. d. It converts RNA into double-stranded DNA. ____ 14. After sexual transmission of HIV, how soon can lab results detect the infection? a. 1 to 2 days b. 4 to 10 days c. 4 to 8 weeks d. 2 to 4 months ____ 15. Which cells are primary targets for HIV? a. CD4+ Th cells only b. CD4+ Th cells, macrophages, and dendritic cells c. CD8-positive cytotoxic T (Tc) cells and plasma cells d. CD8-positive Tc cells only ____ 16. What area in the body may act as a reservoir in which HIV can be relatively protected from antiviral drugs? a. Central nervous system b. Bone marrow c. Thymus gland d. Lungs ____ 17. What is the final stage of the infectious process? a. Colonization b. Invasion c. Multiplication d. Spread ____ 18. How is toxigenicity defined? a. The ability of the pathogen to invade and multiply in the host b. The pathogen’s ability to produce disease by the production of a soluble toxin c. The ability of an agent to produce disease d. The potency of a pathogen measured in terms of the number of microorganisms required to kill the host ____ 19. What is the ability of the pathogen to invade and multiply in the host referred to as? a. Infectivity b. Toxigenicity c. Pathogenicity d. Virulence ____ 20. Some bacterial surface proteins bind with the crystalline fragment (Fc) portion of an antibody to do what? a. Hide in cells to avoid triggering an immune response b. Form self-protecting toxins c. Make staining possible for microscopic observation d. Produce a protective “self” protein ____ 21. Which organism is a common sexually transmitted bacterial infection? a. Staphylococcus aureus b. Clostridium perfringens c. Helicobacter pylori d. Treponema pallidum ____ 22. Which disease is an example of a rickettsial infection? a. Cholera b. Candida c. Sleeping sickness d. Rocky Mountain spotted fever Multiple Response Identify one or more choices that best complete the statement or answer the question. ____ 23. Which secretions transmit HIV? (Select all that apply.) a. Semen b. Urine c. Saliva d. Breast milk e. Sweat ____ 24. Which infections are fungal? (Select all that apply.) a. Ringworm b. Candida c. Cholera d. Athlete’s foot e. Aspergillus ____ 25. Which statements are true regarding the development of HIV symptoms? (Select all that apply.) a. Symptoms generally appear in the clinical latency stage. b. Symptoms are generally observable within 5 years of the initial infection. c. T cells levels, particularly those of memory T cells, progressively decrease. d. Untreated infected individuals may remain asymptomatic for up to 10 years. e. Secondary lymphoid organs experience damage and resulting malfunction. ____ 26. Which statements are true regarding endotoxins? (Select all that apply.) a. Endotoxins are lipopolysaccharides. b. Endotoxins are located in the walls of bacteria. c. Endotoxins are created during the process of lysis. d. Endotoxins are found in gram-negative microorganisms. e. Endotoxins are released during the destruction of its host. ____ 27. Which statements are true regarding viruses? (Select all that apply.) a. Viruses are very complex microorganisms. b. Viruses are referred to as eukaryotes. c. Viruses are capable of producing messenger RNA (mRNA). d. Viruses penetrate plasma membranes via endocytosis. e. Viruses are capable of uncoating cytoplasmic nucleocapsid. ____ 28. Which of these play a role in the control of fungal infections? (Select all that apply.) a. Cytokines b. Macrophages c. Natural killer cells d. Neutrophils e. T lymphocytes ____ 29. Which are complications of AIDS? (Select all that apply.) a. Kaposi sarcoma b. Helicobacter pylori c. Cytomegalovirus retinitis d. Herpes simplex infection e. Legionella pneumophila Thought Questions Describe the pathophysiologic mechanisms of lipopolysaccharide injury after gram-negative bacteria lysis/destruction. Vascular permeability is increased, allowing blood borne substances involved in the destruction to enter the infected site. Endotoxins increase the permeability of the vasculature which causes leakage of large volumes of plasma. This action of will cause hypotension and possible sepsis as well as cardiogenic shock. In addition, the endotoxins released can create a cascade effect of coagulation and cause dissemented intravascular coagulation (DIC) Candida is the most common fungal infection in people with cancer, transplantation, and HIV/AIDs. Briefly describe the ways in which candida contributes to tissue destruction. Initial step consists of the adhesion of single fungal yeast cells to the substrate forming a foundation of a basal yeast cell layer. This is followed by a phase of cell proliferation across the surface and filamentation where cells form elongated projections that continue to grow into the filamentous hyphal forms (initiation step). The production of hyphae is a hallmark of the initiation of biofilm formation followed by the accumulation of an extracellular polysaccharide matrix as the biofilm matures. Non-adherent yeast cells are released from the biofilm into the surroundings where they can colonize other surfaces (dispersal step). Dispersion of biofilm-associated cells carries great clinical significance as released cells can initiate formation of new biofilms or disseminate into host tissues and therefore, they are associated with candidemia and disseminated invasive disease Chapter 11: Stress & Disease Study Guide Multiple Choice: Identify the choice that best completes the statement or answers the question. ____ 1. Exhaustion occurs if stress continues when which stage of the general adaptation syndrome is not successful? a. Flight or fight b. Alarm c. Adaptation d. Arousal ____ 2. Which organ is stimulated during the alarm phase of the general adaptation syndrome (GAS)? a. Adrenal cortex b. Hypothalamus c. Anterior pituitary d. Limbic system ____ 3. During an anticipatory response to stress, what is the reaction from the limbic system stimulated by? a. The retronucleus of the anterior pituitary b. The anterior nucleus of the hippocampus c. The paraventricular nucleus of the hypothalamus d. The prefrontal nucleus of the amygdala ____ 4. Which hormone prompts increased anxiety, vigilance, and arousal during a stress response? a. Norepinephrine b. Epinephrine c. Cortisol d. Adrenocorticotropic hormone (ACTH) ____ 5. Perceived stress elicits an emotional, anticipatory response that begins where? a. Prefrontal cortex b. Anterior pituitary c. Limbic system d. Hypothalamus ____ 6. A student asks the healthcare professional how immunity is decreased by stress. The professional responds that during a stress response, the helper T (Th) 1 response is suppressed by which hormone? a. ACTH b. Cortisol c. Prolactin d. Growth hormone ____ 7. Stress-induced sympathetic stimulation of the adrenal medulla causes the secretion of what? a. Epinephrine and aldosterone b. Norepinephrine and cortisol c. Epinephrine and norepinephrine d. Acetylcholine and cortisol ____ 8. A severely stressed patient has cold, clammy skin. The healthcare professional quizzes the student about this effect. The student correctly answers that this effect is directly from which action? a. Epinephrine dilating blood vessels leading to the vital organs b. Norepinephrine constricting blood vessels in the skin c. Dilating the airways to increased oxygenation of the tissues d. Dysfunctional temperature regulation from cortisol secretion ____ 9. Released stress-induced cortisol results in the stimulation of gluconeogenesis by affecting which structure? a. Adrenal cortex b. Pancreas c. Liver d. Anterior pituitary ____ 10. What effect of increased secretions of epinephrine, glucagon, and growth hormone would the healthcare professional assess for? a. Hyperglycemia b. Hypertension c. Bronchodilation d. Pupil dilation ____ 11. A severely stressed patient has hypoglycemia each time the patient’s blood glucose is checked. The healthcare professional should order laboratory tests to measure which hormone in the patient’s blood? a. Epinephrine b. Norepinephrine c. Cortisol d. Growth hormone ____ 12. What effect do androgens have on lymphocytes? a. Suppression of B-cell responses and enhancement of T-cell responses b. Suppression of T-cell responses and enhancement of B-cell responses c. Suppression of B- and T-cell responses d. Enhancement of B- and T-cell responses ____ 13. The action of which hormone helps explain increases in affective anxiety and eating disorders, mood cycles, and vulnerability to autoimmune and inflammatory diseases in women as a result of stimulation of the CRH gene promoter and central norepinephrine system? a. Progesterone b. Cortisol c. Estrogen d. Prolactin ____ 14. Which statement is true concerning the differences between stress-induced hormonal alterations of men and women? a. After injury, women produce more proinflammatory cytokines than men, a profile that is associated with poor outcomes. b. Androgens appear to induce a greater degree of immune cell apoptosis after injury, creating greater immunosuppression in injured men than in injured women. c. Psychologic stress associated with some types of competition decreases both testosterone and cortisol, especially in athletes older than 45 years of age. d. After stressful stimuli, estrogen is increased in women, but testosterone is decreased in men. ____ 15. A patient perceives living in a state of chronic stress. What will diagnostic blood work ordered by the healthcare professional likely demonstrate? a. Decreased Th lymphocytes b. Increased erythrocytes c. Decreased Tc cells d. Increased platelets ____ 16. What are the signs that a patient is in the adaptive stage of the general adaptation syndrome? a. He or she begins to experience elevated heart and respiratory rates. b. He or she finds it difficult to concentrate on a solution for the stress. c. The patient perceives his or her only options are to run away or fight back. d. The patient has exceeded his or her ability to cope with the current situation. ____ 17. What is the most influential factor in whether a person will experience a stress reaction? a. General state of physical health b. Spiritual belief system c. Intellectual abilities d. Ability to cope ____ 18. A reduction in an individual’s number of natural killer (NK) cells appears to correlate with an increased risk for the development of what? a. Depression b. Type 1 diabetes c. Obsessive compulsive disorder (OCD) d. Gastroesophageal reflux disorder (GERD) Multiple Response Identify one or more choices that best complete the statement or answer the question. ____ 19. The effect epinephrine has on the immune system during the stress response is to increase which cells? (Select all that apply.) a. NK cells b. Immunoglobulins c. Cytokines d. T cells e. Th cells ____ 20. The increased production of proinflammatory cytokines is associated with which considerations? (Select all that apply.) a. Chronic respiratory dysfunction b. Elevated anxiety levels c. Immune disorders d. Age and gender e. Dementia ____ 21. Which statements are true regarding lymphocytes? (Select all that apply.) a. Lymphocytes are involved in the production of the human growth hormone. b. Elevated catecholamine levels influence lymphocytes. c. Lymphocytes are synthesized in the anterior pituitary gland. d. Lymphocytes have receptors for the hormone prolactin. e. Lymphocytes produce endorphins in large amounts. ____ 22. Which cytokines initiate the production of corticotropin-releasing hormone (CRH)? (Select all that apply.) a. IL-1 b. IL-6 c. TNF-ß d. IFN e. IL-12 Thought Question 1. A highly educated patient with known cardiovascular disease (CVD) and type 2 diabetes (T2D) asks you to describe the pathophysiologic mechanism of why stress is “bad” for them. You have no more than 15 minutes to spend with the patient. Focusing on the two diseases this patient has (CVD and T2D), how would you succinctly, and in a scholarly way, answer this patient? When someone is experiencing stress, the body releases hormones that trigger the “fight or flight” response. While these effects can sometimes be helpful, such as when a mother experiencing the hormonal surge can muster the strength to lift a car off of her child, over the long term, they can wreak havoc on the body. Some of the main stress hormones are epinephrine, or adrenaline, norepinephrine, and cortisol. Cortisol puts gas in the body’s tank: It is released in times of stress to help supply the body with as much energy as possible in response to immediate threats by directing a series of actions that increase the energy available in the body for muscles to burn. Cortisol tells the body to increase blood glucose by breaking down glycogen stores in the body, directs cells to resist insulin’s signals to absorb and store glucose in the blood, and prompts cravings for high-calorie foods. At the same time, epinephrine works to increase the concentration of glucose in the blood by stimulating glucose production in the liver. When cortisol and epinephrine levels are consistently high, it results in higher blood sugar and higher insulin resistance, forcing the pancreas to produce more and more insulin to get a response. With ongoing insulin resistance and high blood sugars, the insulin-producing beta cells wear out, causing or worsening type 2 diabetes. Epinephrine, along with norepinephrine, also impacts the cardiovascular system to make sure the body’s muscles have enough oxygen. Epinephrine causes the heart to beat harder and faster, while norepinephrine increases blood pressure by constricting the smaller blood vessels in the body. This increases the work that your heart has to do, and over time, can cause hypertension, heart dysrhythmias, and heart attack from the increased cardiac workload. Chapter 12 Multiple Choice Identify the choice that best completes the statement or answers the question. ____ 1. Which cancer originates from connective tissue? a. Osteogenic sarcoma b. Basal cell carcinoma c. Multiple myeloma d. Adenocarcinoma ____ 2. Carcinoma refers to abnormal cell proliferation originating from which tissue origin? a. Blood vessels b. Epithelial cells c. Connective tissue d. Glandular tissue ____ 3. Carcinoma in situ is characterized by which changes? a. Cells have broken through the local basement membrane. b. Cells have invaded immediate surrounding tissue. c. Cells remain localized in the glandular or squamous cells. d. Cellular and tissue alterations indicate dysplasia. ____ 4. Which term is used to describe a cell showing a loss of cellular differentiation? a. Dysplasia b. Hyperplasia c. Metaplasia d. Anaplasia ____ 5. What are tumor cell markers? a. Hormones, enzymes, antigens, and antibodies that are produced by cancer cells b. Receptor sites on tumor cells that can be identified and marked c. Cytokines that are produced against cancer cells d. Identification marks that are used in administering radiation therapy ____ 6. What is one function of the tumor cell marker? a. To provide a definitive diagnosis of cancer b. To treat certain types of cancer c. To predict where cancers will develop d. To screen individuals at high risk for cancer ____ 7. Which statement supports the hypothesis that intestinal polyps are benign neoplasms and the first stage in the development of colon cancer? a. Cancer cells accumulate slower than noncancer cells. b. An accumulation of mutations in specific genes is required to develop cancer. c. Tumor invasion and metastasis progress more slowly in the gastrointestinal tract. d. Apoptosis is triggered by diverse stimuli, including excessive growth. ____ 8. Autocrine stimulation is the ability of cancer cells to do what? a. Stimulate angiogenesis to create their own blood supply b. Encourage secretions that turn off normal growth inhibitors c. Secrete growth factors that stimulate their own growth d. Divert nutrients away from normal tissue for their own use ____ 9. What is apoptosis? a. Normal mechanism for cells to self-destruct when growth is excessive b. Antigrowth signal activated by the tumor-suppressor gene Rb c. Mutation of cell growth stimulated by the TP53 gene d. Transformation of cells from dysplasia to anaplasia ____ 10. A student studying biology asks the professor to describe how the ras gene is involved in cancer proliferation. What explanation by the professor is best? a. It suppresses the action of the tumor-suppressor genes. b. It changes the way the growth promotion genes work. c. A mutation in this gene allows continuous cell growth. d. It activates a cell surface receptor that allows signaling to the nucleus. ____ 11. The professor explains to students that oncogenes are genes that are capable of what? a. Undergoing mutation that directs the synthesis of proteins to accelerate the rate of tissue proliferation b. Directing synthesis of proteins to regulate growth and to provide necessary replacement of tissue c. Encoding proteins that negatively regulate the synthesis of proteins to slow or halt the replacement of tissue d. Undergoing mutation that directs malignant tissue toward blood vessels and lymph nodes for metastasis ____ 12. Burkitt lymphomas designate a chromosome that has a piece of chromosome 8 fused to a piece of chromosome 14. This is an example of which mutation of normal genes to oncogenes? a. Point mutation b. Chromosome translocation c. Gene amplification d. Chromosome fusion ____ 13. In childhood neuroblastoma, the N-myc oncogene undergoes which type of mutation of normal gene to oncogene? a. Point mutation b. Chromosome fusion c. Gene amplification d. Chromosome translocation ____ 14. What aberrant change causes the abnormal growth in retinoblastoma? a. Proto-oncogenes are changed to oncogenes. b. The tumor-suppressor gene is turned off. c. Genetic amplification causes the growth. d. Chromosomes 9 and 21 are fused. ____ 15. Why are two “hits” required to inactivate tumor-suppressor genes? a. Each allele must be altered, and each person has two copies, or alleles, of each gene, one from each parent. b. The first hit stops tissue growth, and the second hit is needed to cause abnormal tissue growth. c. Tumor-suppressor genes are larger than proto-oncogenes, requiring two hits to affect carcinogenesis. d. The first hit is insufficient to cause enough damage to cause a mutation. ____ 16. How does the ras gene convert from a proto-oncogene to an oncogene? a. Designating a chromosome that has a piece of one chromosome fused to a piece of another chromosome b. Duplicating a small piece of a chromosome, repeatedly making numerous copies c. Altering one or more nucleotide base pairs d. Promoting proliferation of growth signals by impairing tumor-suppressor genes ____ 17. How do cancer cells use the enzyme telomerase? a. To repair the telomeres to restore somatic cell growth b. As an intracellular signaling chemical to stimulate cell division c. To switch off the telomerase to enable cells to divide indefinitely d. To switch on the telomerase to enable cells to divide indefinitely ____ 18. What are characteristics of benign tumors? a. Benign tumors invade local tissues. b. Benign tumors spread through the lymph nodes. c. Benign tumors cause systemic symptoms. d. Benign tumors include the suffix -oma. ____ 19. What is the major virus involved in the development of cervical cancer? a. Herpes simplex virus type 6 b. Herpes simplex virus type 2 c. Human papillomavirus d. Human immunodeficiency virus ____ 20. The Papanicolaou (Pap) test is used to screen for which cancer? a. Ovarian b. Uterine c. Cervical d. Vaginal ____ 21. A healthcare professional is caring for a patient undergoing chemotherapy. What is the skin-related health risk the professional should assess the patient for and be prepared to treat? a. Infection b. Ultraviolet damage c. Pain d. Erythema ____ 22. Inherited mutations that predispose to cancer are almost invariably what kind of gene? a. Proto-oncogenes b. Oncogenes c. Tumor-suppressor genes d. Growth-promoting genes ____ 23. What is the consequence for cells when the functioning TP53 gene is lost as a result of mutation? a. Cells undergo apoptosis. b. Cells escape apoptosis. c. Cells receive less oxygen. d. Cells adhere more readily. ____ 24. Which gastrointestinal tract condition can be an outcome of both chemotherapy and radiation therapy? a. Increased cell turnover b. Constipation c. Stomatitis d. Bloody stool ____ 25. What is the role of vascular endothelial growth factor (VEGF) and basic fibroblast growth factor (bFGF) in cell metastasis? a. To stimulate growth of nearby tumor cells b. To develop new blood vessels to feed cancer cells c. To prevent cancer cells from escaping apoptosis d. To act as a chemical gradient to guide cells to blood vessels ____ 26. It has been determined that a patient’s tumor is in stage 2. How does the healthcare professional describe this finding to the patient? a. Cancer is confined to the organ of origin. b. Cancer has spread to regional structures. c. Cancer is locally invasive. d. Cancer has spread to distant sites. ____ 27. A cancer patient has pain at the tumor site and is worried the tumor has metastasized. What does the healthcare provider understand about this patient’s complaint? a. Pain is primarily a result of pressure caused by the tumor. b. Pain indicates the metastasis of a cancer. c. Pain is usually the initial symptom of cancer. d. Pain is generally associated with late-stage cancer. ____ 28. A healthcare professional is caring for four patients with cancer. Which patient does the professional educate about brachytherapy? a. Lung b. Colon c. Cervical d. Brain ____ 29. A child has been diagnosed with acute lymphoblastic leukemia (ALL). What does the healthcare professional tell the parents about the survival rate at 5 years for this disease? a. 90% b. 70% c. 40% d. 20% ____ 30. By what process do cancer cells multiply in the absence of external growth signals? a. Proto-oncogene b. Autocrine stimulation c. Reliance on caretaker genes d. Pleomorphology ____ 31. What is the role of caretaker genes? a. Maintenance of genomic integrity b. Proliferation of cancer cells c. Secretion of growth factors d. Restoration of normal tissue structure ____ 32. In a normal, nonmutant state, what is an oncogene referred to as? a. Basal cell b. Target cell c. Caretaker gene d. Proto-oncogene ____ 33. What does the student learn about pleomorphic cells? a. Pleomorphic cells are similar in size. b. They have different sizes and shapes. c. They are a result of anaplasia. d. Pleomorphic cells differentiate uniformly. ____ 34. What is the most commonly reported symptom of cancer treatment? a. Nausea b. Fatigue c. Hair loss d. Weight loss ____ 35. What does the health professions student learn about benign tumors? a. The resulting pain is severe. b. Benign tumors are not encapsulated. c. Benign tumors are fast growing. d. The cells are well-differentiated. Multiple Response Identify one or more choices that best complete the statement or answer the question. ____ 36. Normally, which cells are considered immortal? (Select all that apply.) a. Germ b. Stem c. Blood d. Epithelial e. Muscle ____ 37. What is the most common route for distant metastasis? (Select all that apply.) a. Seeding b. Blood c. Lymphatic vessels d. Invasion e. Proliferation ____ 38. What cellular characteristics are affected by anaplasia? (Select all that apply.) a. Size b. Ability to differentiate c. Life expectancy d. Tissue structure e. Shape ____ 39. What are the most common causes of nosocomial infections among patients with cancer? (Select all that apply.) a. Indwelling medical devices b. Suppressed immune system c. Visitor-introduced microorganisms d. Poor appetite e. Inadequate wound care ____ 40. Which statements concerning aging and the occurrence of cancer are true? (Select all that apply.) a. Decline in immunologic functions b. Predisposition to nutritional inadequacies c. Unwillingness to access healthcare services d. Reluctance to engage in cancer screenings e. Effects of immobility on the immune system ____ 41. Which cancers are associated with chronic inflammation? (Select all that apply.) a. Brain b. Colon c. Bone d. Thyroid gland e. Urinary bladder ____ 42. A healthcare professional is assessing a patient who has cancer and a hemoglobin of 8.8 mg/dL. What factors should the professional assess the patient for? a. Chronic bleeding b. Malabsorption of iron c. Malnutrition d. Recent blood transfusion e. Current infection Thought Questions 1. What is a tumor cell marker? Tumor (biologic) markers are substances produced by both benign and malignant cells that are found either in or on the tumor cells or in the blood, spinal fluid, or urine. Tumor markers may include hormones, enzymes, genes, antigens, and antibodies. The function of tumor cell markers is to help screen individuals at high risk for cancer. 2. Is the prostate-specific antigen (PSA) an ideal tumor cell marker? Why or why not? No because there are cancer-prostate patients with normal PSA concentrations in serum and patients with BPH with elevated PSA concentrations. 3. Are there breast cancer tumor markers? There are three tumor markers: cancer antigen 15-3 (CA15-3), cancer antigen 27.29 (CA27.29), and carcinoembryonic antigen (CEA) used to help monitor metastatic breast cancer (advanced breast CA) but they have not been found to be useful to find a breast cancer recurrence or to help lengthen lives in patients who had early stage breast cancer and who are now disease free. 4. What do you think is an ideal tumor cell marker? An ideal tumor cell marker would be highly sensitive, specific, reliable with high prognostic value, organ specificity and should correlate with tumor stages. Chapter 13 Multiple Choice Identify the choice that best completes the statement or answers the question. ____ 1. In teaching a women’s community group, which risk factor does the healthcare professional teach is related to high morbidity of cancer of the colon, uterus, and kidney? a. Women older than 45 years of age b. Women who have never had children c. Women who have a high body mass index d. Woman who have smoked for more than 10 years ____ 2. Which substance has been shown to increase the risk of cancer when used in combination with tobacco smoking? a. Alcohol b. Steroids c. Antihistamines d. Antidepressants ____ 3. Which cancers pose the highest risk for radiologists? a. Thyroid b. Breast c. Leukemia d. Brain ____ 4. Research has shown a link between cancer and which sexually transmitted disease? a. Syphilis b. Gonorrhea c. Human papillomavirus d. Pelvic inflammatory disease ____ 5. Research has supported that alcohol consumption has a convincing impact on increasing the risk of which cancer? a. Lung b. Breast c. Pharynx d. Pancreas ____ 6. A healthcare professional advises patients to exercise because it has a probable impact on reducing which cancer? a. Liver b. Endometrial c. Stomach d. Colon ____ 7. The World Health Organization (WHO) defines grade 1 (overweight) as which BMI range? a. 18.5 to 24.9 b. 25 to 29.9 c. 30 to 39.9 d. 40 to 50.9 Multiple Response Identify one or more choices that best complete the statement or answer the question. ____ 8. Tobacco smoking is associated with which cancers? (Select all that apply.) a. Lung b. Skin c. Bladder d. Kidney e. Pancreas ____ 9. What are the significant risk factors associated with the development of skin cancers? (Select all that apply.) a. Light-colored hair b. Pale eyes c. Fair skin d. Freckles e. History of acne ____ 10. Which environmental factors have been shown to have greatest significant effect on the frequency of genetic mutations in humans? (Select all that apply.) a. Tobacco use b. Radiation exposure c. Obesity d. Severe allergies e. Stressful occupation ____ 11. Research data support the relationship between the exposure of ultraviolet light (UVL) and the development of what? (Select all that apply.) a. Basal cell carcinoma b. Squamous cell carcinoma c. Hodgkin lymphoma d. Non-Hodgkin lymphoma e. Soft tissue sarcoma ____ 12. The healthcare professional teaches a community group that alcohol consumption has been proven to be a consistent risk factor in the development of which major cancers? (Select all that apply.) a. Colorectal b. Kidney c. Breast d. Esophageal e. Pancreatic ____ 13. Nutritional counseling regarding cancer stem cell repopulation must stress the importance of including sufficient quantities of what in a daily diet? (Select all that apply.) a. Vitamin A b. Vitamin D c. Protein d. Vitamin C e. Water ____ 14. The healthcare professional advises clients to make which personal lifestyle choices in order to likely reduce the risk for developing cancer? (Select all that apply.) a. Avoiding crowds b. Wearing a hat while golfing c. Eating a strict vegetarian diet d. Having regular health screenings e. Staying indoors during smog alerts ____ 15. Which individuals are at risk for developing lung and respiratory tract cancers because of exposure to known cancer-inducing environmental factors? (Select all that apply.) a. A patient whose partner smokes 1 1/2 packs of cigarettes a day b. A 10-year employee of an asbestos fiber manufacturer c. A farmer whose equipment is primarily driven by diesel engines d. An older adult with a family history of lung cancer and chronic obstructive pulmonary disease (COPD) e. A 10-year delivery employee for a paper manufacturing company ____ 16. A healthcare professional wants to work on community projects that would include strategies to reduce the risk of developing cancer. Which projects should the professional volunteer for? (Select all that apply.) a. Offering free smoking cessation classes to college students b. Establishing a support group for patients receiving chemotherapy c. Providing a breast cancer screening at a senior center twice a year d. Supplying low sugar, low-fat snacks at an after-school tutoring program e. Funding a support service that offers transportation to cancer treatment centers ____ 17. When considering topics for a series of community discussions related to cancer prevention strategies, what should the healthcare professional include? (Select all that apply.) a. Healthy eating b. Tobacco avoidance c. Importance of early diagnosis d. Impact of obesity on one’s health e. Age-appropriate exercise routines Thought Question Mr. Benson, 60 years old, lives near phosphate and uranium deposits. His father was a uranium miner. Mr. Benson has worked in a phosphate processing plant since his early 20s. (Phosphate ore is combined with low-grade uranium and emits constant low α-radiation.) He is a pack-a-day smoker and drinks alcohol moderately. He describes himself as a “meat and potatoes man” and likes to barbecue. Explain the contributing factors for Mr. Benson developing a lung tumor. Frame your answer in terms of initiation, promotion and progression of his lung tumor. Initiation- Interaction of a carcinogen with DNA. Genetic alteration caused by living near phosphate and uranium deposits, his father being a uranium miner Promotion- Carcinogens that promote growth of the tumor. Continued work in a phosphate processing plant. Progression- Tumor undergoes a genetic event that causes a permanent growth advantage like being exposed to additional carcinogens. Being a pack-a-day smoker and using alcohol Chapter 14 Multiple Choice Identify the choice that best completes the statement or answers the question. ____ 1. What congenital malformation is commonly linked to acute leukemia in children? a. Down syndrome b. Wilms tumor c. Retinoblastoma d. Neuroblastoma ____ 2. When are childhood cancers most often diagnosed? a. During infancy b. At peak times of physical growth c. After diagnosis of a chronic illness d. After an acute illness ____ 3. Prenatal exposure to diethylstilbestrol (DES) can result in which type of cancer? a. Breast cancer b. Leukemia c. Vaginal cancer d. Lymphoma ____ 4. Currently, what percentage of children with cancer can be cured? a. 40% b. 50% c. 60% d. 85% ____ 5. What do most childhood cancers arise from? a. Epithelium b. Mesodermal germ layer c. Embryologic ectodermal layer d. Viscera ____ 6. Which form of cancer is linked to congenital malformation syndromes? a. Wilms tumor b. Retinoblastoma c. Osteosarcoma d. Rhabdomyosarcoma ____ 7. Research data support a carcinogenic relationship in children resulting from exposure to which virus? a. Herpes simplex virus b. Influenza c. Varicella-zoster virus d. Epstein-Barr virus ____ 8. What does a child diagnosed with acquired immunodeficiency syndrome (AIDS) have an increased risk of developing? a. Non-Hodgkin lymphoma b. Retinoblastoma c. Epstein-Barr d. Leukemia ____ 9. Which intervention has the greatest effect on a child’s mortality rate when diagnosed with cancer? a. Age at the time of diagnosis b. Participation in clinical trials c. Proximity to a major cancer treatment center d. Parental involvement in the treatment planning ____ 10. Which statement is likely true regarding children being treated for cancer with radiation therapy? a. They will most likely have a successful remission of tumor growth. b. They seldom require follow-up maintenance treatments. c. They are prone to experience severe developmental delays. d. They are at increased risk for developing childhood cancers. ____ 11. How should the healthcare professional reply when parents question why a computed tomographic (CT) scan of the head was not ordered for their 5-year-old child after a minor fall? a. Physicians are cautious about ordering CT scan on children younger than 10 years of age. b. CT scans are seldom conclusive when used to diagnosis head injuries in young children. c. The child’s symptoms will determine whether a CT scan is necessary and worth the expense. d. Research suggests that repeated CT scans can increase the risk of developing brain cancer. Multiple Response Identify one or more choices that best complete the statement or answer the question. ____ 12. Childhood exposure to which risk factors is known to increase the susceptibility for developing cancers? (Select all that apply.) a. Low birth weight b. Chemotherapy c. Ionizing radiation d. Cigarette smoke e. Epstein-Barr virus ____ 13. Which statement is true concerning the difference between adult and childhood cancers? (Select all that apply.) a. Numerous differences exist between these two categories of cancer. b. Genetic risk factors and congenital conditions are more related in childhood cancers. c. Environmental risks are strongly associated with childhood cancers. d. Exposure to pesticides is a minor risk for the development of adult cancers. e. Maternal exposure to carcinogenic substances presents little risk to the fetus. ____ 14. Most childhood cancers originate from the mesodermal germ layer that ultimately produces which of these? (Select all that apply.) a. Connective tissue b. Digestive system c. Muscles d. Kidneys e. Blood ____ 15. Which statements are true regarding cancers that develop in children? (Select all that apply.) a. Childhood cancers tend to be fast growing. b. Childhood cancers are diagnosed during growth spurts. c. Childhood cancer generally metastasizes by the time of diagnosis. d. Childhood cancer is typically at low risk for aggressive metastasis. e. Childhood cancers respond well to standardized treatment modalities. ____ 16. The healthcare professional is preparing a discussion on cancer and its occurrence among high school students. Which cancers will the professional include in the discussion? (Select all that apply.) a. Colorectal b. Brain c. Thyroid d. Breast e. Lung Thought Question Compare the risk of developing leukemia in two children, one with no family history of leukemia and the other with a sibling with leukemia. Siblings (brothers and sisters) of children with leukemia have a slightly increased chance (2 to 4 times normal) of developing leukemia A child who has a sibling with leukemia has a risk for the development of leukemia that is 2 to 4 times greater than that for children with healthy siblings. The occurrence of leukemia in monozygous twins is estimated as being as high as 25%. Chapter 28: Structure and Function of Hematologic System Study Guide Multiple Choice Identify the choice that best completes the statement or answers the question. 1. What is the most abundant class of plasma protein? a.Globulin c. Clotting factors b. Albumin d. Complement proteins 2. What is the effect of low plasma albumin? a. Clotting factors decrease, thus increasing the chance of prolonged bleeding. b. Fewer immunoglobulins are synthesized, thus impairing the immune function. c. Less iron is stored, thus increasing the incidence of iron deficiency anemia. d. Osmotic pressure decreases, thus water moves from the capillaries to the interstitium. 3. What is the life span of an erythrocyte (in days)? a. 20 to 30 c. 100 to 120 b. 60 to 90 d. 200 to 240 4. Which statement concerning erythrocytes is true? a. Erythrocytes contain a nucleus, mitochondria, and ribosomes. b. Erythrocytes synthesize proteins. c. Erythrocytes have the ability to change shape to squeeze through microcirculation. d. Erythrocyte colony-stimulating factor (E-CSF) stimulates erythrocytes. 5. Granulocytes that contain granules of vasoactive amines, such as histamine, are called: a. Neutrophils c. Monocytes b. Eosinophils d. Basophils 6. Which of the following are formed elements of the blood that are not cells but are disk-shaped cytoplasmic fragments essential for blood clotting? a. Monocytes c. Macrophages b. Platelets d. Erythrocytes 7. Blood cells that differentiate into macrophages are known as: a. Monocytes c. Eosinophils b. Neutrophils d. Basophils 8. Without prior exposure to an antigen, which cells are able to destroy some types of tumor cells and some virus-infected cells? a. Lymphocytes c. Megakaryocytes b. Plasma cells d. Natural killer (NK) cells 9. What is the life span of platelets (in days)? a. 10 c. 90 b. 30 d. 120 10. Fetal hematopoiesis occurs in which structure? a. Gut b. Spleen c. Bone marrow d. Thymus 11. What is the consequence of a splenectomy? a. The level of iron in circulation increases. b. Antibody production increases to improve immune function. c. The number of defective cells in circulation increases. d. The number of clotting factors increases. 12. During an infection, why do lymph nodes enlarge and become tender? a. B lymphocytes proliferate. b. The nodes are inflamed. c. The nodes fill with purulent exudate. d. The nodes are not properly functioning. 13. Which blood cells are the chief phagocytes involved in the early inflammation process? a. Neutrophils c. Eosinophils b. Monocytes d. Erythrocytes 14. Which blood cells are biconcave in shape and have the capacity to be reversibly deformed? a. Neutrophils c. Eosinophils b. Monocytes d. Erythrocytes 15. Which hemoglobin is made from oxidized ferric iron (Fe3+) and lacks the ability to bind oxygen? a. Deoxyhemoglobin c. Methemoglobin b. Oxyhemoglobin d. Glycosylated hemoglobin 16. The absence of parietal cells would prevent the absorption of an essential nutrient necessary to prevent which type of anemia? a. Iron deficiency c. Folic acid deficiency anemia b. Pernicious anemia d. Aplastic anemia 17. Which nutrients are necessary for the synthesis of DNA and the maturation of erythrocytes? a. Protein and niacin c. Cobalamin (vitamin B12) and folate b. Iron and vitamin B6 (pyridoxine) d. Pantothenic acid and vitamin C 18. Which nutrients are necessary for hemoglobin synthesis? a. Protein and niacin c. Cobalamin (vitamin B12) and folate b. Iron and vitamin B6 (pyridoxine) d. Pantothenic acid and vitamin C 19. Recycling of iron from erythrocytes is made possible by which of the following? a. Transferrin c. Apoferritin b. Hemosiderin d. Erythropoietin 20. By which structure are mature erythrocytes removed from the bloodstream? a. Liver c. Thymus b. Lymph nodes d. Spleen 21. Which substance is used to correct the chronic anemia associated with chronic renal failure? a. Iron c. Cobalamin (vitamin B12) b. Erythropoietin d. Folate 22. What is the role of thromboxane A (TXA2) in the secretion stage of hemostasis? a. Stimulates the synthesis of serotonin. b. Promotes vasodilation. c. Stimulates platelet aggregation. d. Promotes formation of cyclooxygenase. 23. Which of the following is the role of nitric oxide (NO) in hemostasis? a. Stimulates the release of fibrinogen to maintain the platelet plug. b. Stimulates the release of clotting factors V and VII. c. Causes vasoconstriction and stimulates platelet aggregation. d. Controls platelet activation through cyclic guanosine monophosphate (cGMP)–mediated signaling. 24. The drug heparin acts in hemostasis by which processes? a. Inhibiting thrombin and antithrombin III (AT-III) b. Preventing the conversion of prothrombin to thrombin c. Shortening the fibrin strands to retract the blood clot d. Degrading the fibrin within blood clots 25. What is plasmin’s role in the clotting process? a. Stimulates platelet aggregation. b. Inhibits platelet adhesion and aggregation. c. Prevents the conversion of prothrombin to degrade the fibrin within blood clots. d. Degrades the fibrin within blood clots. 26. What does polycythemia at birth indicate? a. Hypoxia in utero b. Dysfunctional bone marrow c. Congenitally absent spleen d. Dehydration in utero 27. Where are Kupffer cells located? a. Kidneys b. Liver c. Pancreas d. Spleen 28. Where are Langerhans cells found? a. Skin b. Intestinal lining c. Kidney d. Thyroid 29. What is the role of collagen in the clotting process? a. Initiates the clotting cascade. c. Stimulates fibrin. b. Activates platelets. d. Deactivates fibrinogen. 30. Which form of iron (Fe) can be used in the formation of normal hemoglobin? Fe+ Fe 2+ Fe 3+ Fe 4+ 31. Where are alveolar macrophages found? a. Skin b. Breasts c. Gastrointestinal tract d. Lungs 32. What changes to the hematologic system is related to age? a. Platelet adhesiveness decreases. b. Lymphocyte function decreases. c. Cellular immunity increases. d. Erythrocyte reproduction accelerates. 33. What is the function of erythrocytes? a. Tissue oxygenation b. Hemostasis c. Infection control d. Allergy response Multiple Response Identify one or more choices that best complete the statement or answer the question. 34. Which characteristics allow erythrocytes to function as gas carriers? (Select all that apply.) a. Permanent shape b. Compactness c. Reversible deformability d. Presence of hyperactive mitochondria e. Biconcavity 35. Which statements about plasma proteins are correct? (Select all that apply.) a. Provide clotting factors. b. Transport triglycerides. c. Synthesize complement proteins. d. Create hydrostatic pressure. e. Transport cholesterol. 36. What are the primary anticoagulant mechanisms? (Select all that apply.) a. Antithrombin III b. Tissue factor pathway inhibitor c. Hematopoiesis d. Protein C e. Phagocytosis 37. Which statements are true regarding the role of the endothelium in clot formation? (Select all that apply.) a. The surface of the endothelium produces plasma protease inhibitors. b. Plasma protease inhibitors assist in preventing clot formation. c. Thrombomodulin is a protein that is converted on the surface of endothelial cells. d. Protein A binds to thrombomodulin. e. Activated protein C enhances the adhesion ability of neutrophils. 38. Which statements characterize albumin? (Select all that apply.) a. Retains sodium to maintain water balance. b. Provides colloid osmotic pressure. c. Is synthesized in the liver. d. Is a carrier for drugs that have low water solubility. e. Is a small molecule Matching Match the descriptions with the corresponding terms. A. Clotting B. Red blood cell development C. Red blood cell destruction D. Platelet formation E. Blood cell production 39. D-Endomitosis 40. A-Hemostasis 41. E-Hematopoiesis 42. B-Erythropoiesis 43. C-Phagocytosis Concept Question: 1. A physician has advised Justin’s father to take an aspirin a day to reduce the risk of having a heart attack. Why would the physician tell him that? What causes a platelet adhesion? Aspirin reduces clumping action of platelets and reduces the risk of having a heart attack as it will help blood flow in the arteries especially in people with atherosclerosis. Platelet adhesion is caused by vascular injury. 2. Bobby, 6 years old, fell off his bike and skinned his knee. His mother notices that the injury is not deep but is bleeding. What kind of damage has probably occurred with his blood vessels and how will the blood react to mitigate the bleeding? Bobby caused an abrasion to his knee which would trigger the clotting cascade. The clotting cascade is made of 3 steps: 1. Vasoconstriction 2. Temporary blockage of a platelet plug 3. Formation of a fibrin clot to prevent further bleeding. Chapter 29 Alterations of Erythrocyte Function Multiple Choice Identify the choice that best completes the statement or answers the question. 1. What term is used to describe the capacity of some erythrocytes to vary in size, especially in relationship to some anemias? a. Poikilocytosis c. Anisocytosis b. Isocytosis d. Microcytosis 2. What is the fundamental physiologic manifestation of anemia? a. Hypotension c. Hypoxia b. Hyperesthesia d. Ischemia 3. The paresthesia that occurs in vitamin B12 deficiency anemia is a result of which of the following? a. Reduction in acetylcholine receptors in the postsynaptic nerves b. Myelin degeneration in the spinal cord c. Destruction of myelin in peripheral nerves d. Altered function of neurons in the parietal lobe 4. Which of the following describes how the body compensates for anemia? a. Increasing rate and depth of breathing b. Decreasing capillary vasoconstriction c. Hemoglobin holding more firmly onto oxygen d. Kidneys releasing more erythropoietin 5. Which of the following is classified as a megaloblastic anemia? a. Iron deficiency c. Sideroblastic b. Pernicious d. Hemolytic 6. Deficiencies in folate and vitamin B12 alter the synthesis of which of the following? a. RNA c. DNA b. Cell membrane d. Mitochondria 7. The underlying disorder of which anemia is a result of the defective secretion of the intrinsic factor, which is essential for the absorption of vitamin B12? a. Microcytic c. Hypochromic b. Pernicious d. Hemolytic 8. After a person has a subtotal gastrectomy for chronic gastritis, which type of anemia will result? a. Iron deficiency c. Folic acid b. Aplastic d. Pernicious 9. What causes the atrophy of gastric mucosal cells that result in pernicious anemia? a. Erythrocyte destruction c. Vitamin B12 malabsorption b. Folic acid malabsorption d. Poor nutritional intake 10. Which statement best describes a Schilling test? a. Administration of radioactive cobalamin and the measurement of its excretion in the urine to test for vitamin B12 deficiency b. Measurement of antigen-antibody immune complexes in the blood to test for hemolytic anemia c. Measurement of serum ferritin and total iron-binding capacity in the blood to test for iron deficiency anemia d. Administration of folate and measurement in 2 hours of its level in a blood sample to test for folic acid deficiency anemia. 11. What is the treatment of choice for pernicious anemia (PA)? a. Cyanocobalamin by oral intake b. Vitamin B12 by injection c. Ferrous fumarate by Z-track injection d. Folate by oral intake 12. Which condition resulting from untreated pernicious anemia (PA) is fatal? a. Brain hypoxia c. Heart failure b. Liver hypoxia d. Renal failure 13. How is the effectiveness of vitamin B12 therapy measured? a. Reticulocyte count c. Hemoglobin b. Serum transferring d. Serum vitamin B12 14. Which statement about folic acid is false? a. Folic acid absorption is dependent on the enzyme folacin. b. Folic acid is stored in the liver. c. Folic acid is essential for RNA and DNA synthesis within erythrocytes. d. Folic acid is absorbed in the upper small intestine. 15. Which anemia produces small, pale erythrocytes? a. Folic acid c. Iron deficiency b. Hemolytic d. Pernicious 16. Which type of anemia is characterized by fatigue, weakness, and dyspnea, as well as conjunctiva of the eyes and brittle, concave nails? a. Pernicious c. Aplastic b. Iron deficiency d. Hemolytic 17. What is the most common cause of iron deficiency anemia (IDA)? a. Decreased dietary intake c. Vitamin deficiency b. Chronic blood loss d. Autoimmune disease 18. Continued therapy of pernicious anemia (PA) generally lasts how long? a. 6 to 8 weeks c. Until the iron level is normal b. 8 to 12 months d. The rest of one’s life 19. Sideroblastic anemia can occasionally result from an autosomal recessive transmission inherited from which relative? a. Mother c. Grandfather b. Father d. Grandmother 20. Clinical manifestations of mild-to-moderate splenomegaly and hepatomegaly, bronze-colored skin, and cardiac dysrhythmias are indicative of which anemia? a. Iron deficiency c. Sideroblastic b. Pernicious d. Aplastic 21. Considering sideroblastic anemia, what would be the expected effect on the plasma iron levels? a. Plasma iron levels would be high. b. Levels would be low. c. Levels would be normal. d. Levels would be only minimally affected. 22. In aplastic anemia (AA), pancytopenia develops as a result of which of the following? a. Suppression of erythropoietin to produce adequate amounts of erythrocytes b. Suppression of the bone marrow to produce adequate amounts of erythrocytes, leukocytes, and thrombocytes c. Lack of DNA to form sufficient quantities of erythrocytes, leukocytes, and thrombocytes d. Lack of stem cells to form sufficient quantities of leukocytes 23. What is the most common pathophysiologic process that triggers aplastic anemia (AA)? a. Autoimmune disease against hematopoiesis by activated cytotoxic T (Tc) cells b. Malignancy of the bone marrow in which unregulated proliferation of erythrocytes crowd out other blood cells c. Autoimmune disease against hematopoiesis by activated immunoglobulins d. Inherited genetic disorder with recessive X-linked transmission 24. An allogenic bone marrow transplantation remains the preferred method for treating which anemia? a. Polycythemia vera c. Sideroblastic b. Aplastic d. Anemia of chronic disease (ACD) 25. Which statement is true regarding warm autoimmune hemolytic anemia? a. Warm autoimmune hemolytic anemia occurs primarily in men. b. It is self-limiting and rarely produces hemolysis. c. Erythrocytes are bound to macrophages and sequestered in the spleen. d. Immunoglobulin M coats erythrocytes and binds them to receptors on monocytes. 26. When considering hemolytic anemia, which statement is true regarding the occurrence of jaundice? a. Erythrocytes are destroyed in the spleen. b. Heme destruction exceeds the liver’s ability to conjugate and excrete bilirubin. c. The patient has elevations in aspartate transaminase (AST) and alanine transaminase (ALT). d. The erythrocytes are coated with an immunoglobulin. 27. Erythrocyte life span of less than 120 days, ineffective bone marrow response to erythropoietin, and altered iron metabolism describe the pathophysiologic characteristics of which type of anemia? a. Aplastic c. Anemia of chronic disease b. Sideroblastic d. Iron deficiency 28. What is the primary cause of the symptoms of polycythemia vera? a. Decreased erythrocyte count c. Increased blood viscosity b. Destruction of erythrocytes d. Neurologic involvement 29. Treatment for polycythemia vera involves which of the following? a. Therapeutic phlebotomy and radioactive phosphorus b. Restoration of blood volume by plasma expanders c. Administration of cyanocobalamin d. Blood transfusions 30. Considering iron replacement therapy prescribed for iron deficiency anemia, who is likely to require long-term daily maintenance dosage? a. A woman who has not yet experienced menopause b. A teenager who is involved in strenuous athletics c. A middle-aged man who smokes two packs of cigarettes a day d. An older person demonstrating signs of dementia 31. Which statement is true regarding the physical manifestations of vitamin B12 deficiency anemia? a. Vitamin B12 deficiency anemia seldom results in neurologic symptoms. b. The chances of a cure are good with appropriate treatment. c. The condition is reversible in 75% of the cases. d. Symptoms are a result of demyelination. Multiple Response Identify one or more choices that best complete the statement or answer the question. 32. A 2000 ml blood loss will produce which assessment finding? (Select all that apply.) a. Air hunger b. Normal blood pressure in the supine position c. Rapid thready pulse d. Cold clammy skin e. lactic acidosis 33. Which medications are associated with an intermediate increase in a person’s risk for developing aplastic anemia? (Select all that apply.) a. Penicillin b. Chloramphenicol (Chloromycetin) c. Phenytoin (Dilantin) d. Trimethoprim-sulfamethoxazole (Bactrim) e. Thiazides 34. Which conditions are generally included in the symptoms of pernicious anemia (PA)? (Select all that apply.) a. Weakness b. Weight gain c. Low hemoglobin d. Paresthesias e. Low hematocrit 35. What are the clinical manifestations of folate deficiency anemia? (Select all that apply.) a. Constipation b. Flatulence c. Dysphagia d. Stomatitis e. Cheilosis 36. Which diseases are commonly associated with anemia of chronic disease? (Select all that apply.) a. Rheumatoid arthritis b. Acquired immunodeficiency syndrome (AIDS) c. Polycythemia vera d. Systemic lupus erythematosus e. Chronic hepatitis Matching Match the phrases with the corresponding terms. Options may be used more than once. A. Normocytic-normochromic anemia B. Microcytic-hypochromic anemia C. Macrocytic-normochromic anemia 37. Pernicious anemia C 38. Sideroblastic anemia B 39. Aplastic anemia A Thought Questions 1. A physician informs a 48-year-old male smoker that he consistently has a hematocrit of 56%. Why might his hematocrit always 4% to 5% higher than normal values? The patient has secondary absolute polycythemia. Given the choice, hemoglobin prefers carbon monoxide over oxygen. As the patient smokes, the binding sites for oxygen are taken up by carbon monoxide. Because of the decreased oxygen-carrying capacity, the patient becomes hypoxic. The hypoxia is detected by the kidneys, erythropoietin is released, and more red cells are made to compensate for the lack of oxygen. The patient is now at risk for thrombus and embolus formation, heart failure, coronary artery disease, etc. 2. What are the pathophysiologic mechanisms in drug-induced hemolytic anemia? The causes of drug-induced hemolytic anemia can be divided into two categories, immune or metabolic. Those in the first category may operate much like the process that leads to immune-mediated agranulocytosis, or they can suppress regulator cells, which can lead to the production of autoantibodies. The second category involves the induction of hemolysis by metabolic abnormalities in the RBCs. Patients with drug-induced hemolytic anemia can present with signs of intravascular or extravascular hemolysis 3. Compare and contrast microcytic-hypochromic anemias with macrocytic-normochromic anemias. Microcytic anemia, the erythrocytes are smaller than normal. In a macrocytic anemia, the larger red cells are always associated with insufficient numbers of cells and often also insufficient hemoglobin content per cell Chapter 30 Alterations of Leukocyte, Lymphoid, and Hemostatic Function Multiple Choice Identify the choice that best completes the statement or answers the question. 1. What change is observed in leukocytes during an allergic disorder (type I hypersensitivity) often caused by asthma, hay fever, and drug reactions? a. Neutrophilia c. Eosinophilia b. Basophilia d. Monocytosis 2. In infectious mononucleosis (IM), what does the Monospot test detect? a. Immunoglobulin E (IgE) c. Immunoglobulin G (IgG) b. Immunoglobulin M (IgM) d. Immunoglobulin A (IgA) 3. Which description is consistent with acute lymphocytic leukemia (ALL)? a. ALL is a progressive neoplasm defined by the presence of greater than 30% lymphoblasts in the bone marrow or blood. b. Leukocytosis and a predominance of blast cells characterize the bone marrow and peripheral blood. As the immature blasts increase, they replace normal myelocytic cells, megakaryocytes, and erythrocytes. c. B cells fail to mature into plasma cells that synthesize immunoglobulins. d. The translocation of genetic material from genes 9 and 22 create an abnormal, fused gene identified as BCR-ABL. 4. Which description is consistent with chronic myelogenous leukemia (CML)? a. Defects exist in the ras oncogene, TP53 tumor-suppressor gene, and INK4A, the gene encoding a cell-cycle regulatory protein. b. Leukocytosis and a predominance of blast cells characterize the bone marrow and peripheral blood. As the immature blasts increase, they replace normal myelocytic cells, megakaryocytes, and erythrocytes. c. B cells fail to mature into plasma cells that synthesize immunoglobulins. d. The translocation of genetic material from genes 9 and 22 creates an abnormal, fused protein identified as BCR-ABL1. 5. Which description is consistent with chronic lymphocytic leukemia (CLL)? a. Defects exist in the ras oncogene, TP53 tumor-suppressor gene, and INK4A, the gene encoding a cell-cycle regulatory protein. b. Leukocytosis and a predominance of blast cells characterize the bone marrow and peripheral blood. As the immature blasts increase, they replace normal myelocytic cells, megakaryocytes, and erythrocytes. c. B cells fail to mature into plasma cells that synthesize immunoglobulins. d. The translocation of genetic material from genes 9 and 22 creates an abnormal, fused protein identified as BCR-ABL. 6. Which electrolyte imbalance accompanies multiple myeloma (MM)? a. Hyperkalemia c. Hyperphosphatemia b. Hypercalcemia d. Hypernatremia 7. Reed-Sternberg (RS) cells represent malignant transformation and proliferation of which of the following? a. Interleukin (IL)–1, IL-2, IL-5, and IL-6 b. Tumor necrosis factor–beta c. B cells d. T cells 8. Local signs and symptoms of Hodgkin disease–related lymphadenopathy are a result of which of the following? a. Pressure and ischemia c. Inflammation and ischemia b. Pressure and obstruction d. Inflammation and pressure 9. Which virus is associated with Burkitt lymphoma in African children? a. Cytomegalovirus c. Human papillomavirus b. Adenovirus d. Epstein-Barr virus 10. Which term is used to describe a red-purple discoloration caused by diffuse hemorrhage into the skin tissue? a. Petechiae c. Ecchymosis b. Hematoma d. Purpura 11. Which statement best describes heparin-induced thrombocytopenia (HIT)? a. Immunoglobulin G immune–mediated adverse drug reaction that reduces circulating platelets b. Hematologic reaction to heparin in which the bone marrow is unable to produce sufficient platelets to meet the body’s needs c. Immunoglobulin E–mediated allergic drug reaction that reduces circulating platelets d. Cell-mediated drug reaction in which macrophages process the heparin and platelet complexes that are then destroyed by activated cytotoxic T cells. 12. Immune thrombocytopenia (ITP) is a(n) condition in adults and a(n) condition in children. a. Acute; acute c. Acute; chronic b. Chronic; chronic d. Chronic; acute 13. Vitamin is required for normal clotting factor synthesis by the . a. K; kidneys c. K; liver b. D; kidneys d. D; liver 14. What is the most common cause of vitamin K deficiency? a. Administration of warfarin (Coumadin) b. Total parenteral nutrition with antibiotic therapy c. An immunoglobulin G–mediated autoimmune disorder d. Liver failure 15. Which disorder is described as an unregulated release of thrombin with subsequent fibrin formation and accelerated fibrinolysis? a. Disseminated intravascular coagulation (DIC) b. Immune thrombocytopenic purpura (ITP) c. Heparin-induced thrombocytopenia (HIT) d. Essential thrombocythemia (ET) 16. In disseminated intravascular coagulation (DIC), what activates the coagulation cascade? a. Cytokines, such as platelet-activating factor (PAF), and tumor necrosis factor-alpha (TNF-α) b. Thromboxane A, causing platelets to aggregate and consume clotting factors c. Tissue factor (TF) located in the endothelial layer of blood vessels and subcutaneous tissue d. Endotoxins from gram-negative and gram-positive bacteria circulating in the bloodstream 17. Which proinflammatory cytokines are responsible for the development and maintenance of disseminated intravascular coagulation (DIC)? a. Granulocyte colony-stimulating factor (G-CSF); interleukin (IL)–2, IL-4, and IL-10; and tumor necrosis factor-gamma (IFN-γ) b. Granulocyte-macrophage colony-stimulating factor (GM-CSF); and IL-3, IL-5, IL-9, and IFN-γ c. Macrophage colony-stimulating factor (M-CSF); IL-7, IL-11, and IL-14; and PAF d. Tumor necrosis factor-alpha (TNF-α); IL-1, IL-6, and IL-8; and platelet-activating factor (PAF) 18. In disseminated intravascular coagulation (DIC), what are the indications of microvascular thrombosis? a. Reduced amplitude in peripheral pulses b. Symmetric cyanosis of fingers and toes c. Numbness and tingling in fingers and toes d. Bilateral pallor and edema of fingers and toes 19. What is the most reliable and specific test for diagnosing disseminated intravascular coagulation (DIC)? a. Prothrombin time (PT) b. Activated partial thromboplastin time (aPTT) c. Fibrin degradation products (FDP) d. D-dimer 20. What term is used to identify thrombi that occlude arterioles and capillaries and are made up of platelets with minimal fibrin and erythrocytes? a. Essential (primary) thrombocythemia (ET) b. Acute idiopathic thrombotic thrombocytopenic purpura c. Thrombotic thrombocytopenic purpura (TTP) d. Immune thrombocytopenic purpura (ITP) 21. Which of the following is characterized by what is referred to as pathognomonic pentad of symptoms? a. Acute idiopathic thrombotic thrombocytopenic purpura b. Essential (primary) thrombocythemia (ET) c. Immune thrombocytopenic purpura (ITP) d. Thrombotic thrombocytopenic purpura (TTP) 22. Which statement relates to immune thrombocytopenic purpura (ITP)? a. ITP is formed in conditions of low flow and is made up of mostly red cells with larger amounts of fibrin and few platelets. b. An alteration of multipotent stem cells, resulting in an excess production of platelets, causes ITP. c. Mononuclear phagocytes in the spleen remove antibody-coated platelets from circulation. d. Arterial clots are made up of mostly platelet aggregates held together by fibrin strands. 23. When the demand for mature neutrophils exceeds the supply, immature neutrophils are released indicating: a. A shift to the right c. Leukocytosis b. A shift to the left d. Leukemia 24. Hodgkin disease is characterized by the presence of which of the following? a. Philadelphia chromosome c. Microvascular thrombi b. Virchow triad d. Reed-Sternberg (RS) cells Multiple Response Identify one or more choices that best complete the statement or answer the question. 25. Which classic clinical manifestations are symptoms of IM? (Select all that apply.) a. Lymph node enlargement b. Hepatitis c. Pharyngitis d. Edema in the area of the eyes e. Fever 26. Early detection of acute leukemia would include which of the following symptoms? (Select all that apply.) a. Dizziness b. Paresthesia c. Anorexia d. Bruising e. Bone pain 27. What are the most significant risk factors for the development of thrombus formation as referred to by the Virchow triad? (Select all that apply.) a. Endothelial injury to blood vessels b. Turbulent arterial blood flow c. Rapid coagulation of the blood d. Stagnant venous blood flow e. History of obesity 28. Which statements are true regarding leukemias? (Select all that apply.) a. A single progenitor cell undergoes a malignant change. b. Leukemia is a result of uncontrolled cellular proliferation. c. Bone marrow becomes overcrowded. d. Leukocytes are under produced. e. Hematopoietic cell production is decreased. 29. The two major forms of leukemia, acute and chronic, are classified by which criteria? (Select all that apply.) a. Predominant cell type b. Rate of progression c. Age of individual when cells differentiation occurs d. Stage of cell development when malignancy first occurs e. Serum level of leukocytes 30. What are the clinical manifestations of advanced non-African Burkitt lymphoma? (Select all that apply.) a. Abdominal swelling b. Night sweats c. Fever d. Weight gain e. Dementia Matching Match the causes or diagnostic tests with the hematologic disorders. A. Epstein-Barr virus B. Bence Jones protein C. Diagnosed by the Reed-Sternberg cell D. Diagnosed by the Philadelphia chromosome 31. Infectious mononucleosis A 32. Chronic myelogenous leukemia D 33. Multiple myeloma B 34. Hodgkin lymphoma C Thought Question 1. Example of hypercoagulation state: Heparin-induced thrombocytopenia (HIT) is the development of a low platelet count due to the administration of various forms of heparin. HIT predisposes to thrombosis because platelets release microparticles that activate thrombin, thereby leading to thrombosis. When thrombosis is identified the condition is called heparin-induced. HIT is a clotting disorder. After heparin is administered to a patient, an immune complex can form between heparin and a specific blood factor, known as platelet factor 4, or “PF4”, that is released by platelets. The body views this “heparin-PF4” complex as a foreign substance, and forms an antibody against the heparin-PF4 complex. The antibody binds to the complex and the platelets are destroyed. This disruption of platelets can lead to the formation of new blood clots in patients with immune-mediated HIT. The results can be DVT, PE, or even a heart attack or stroke. Example of hypcoagulation state: Hemophilia A is a rare disorder in which the blood does not clot normally. It is usually inherited. People with hemophilia have insufficient amounts or a defective factor VIII-clotting factor. Clotting factor is a protein needed for normal blood clotting. Provide an example of an hypercoagulation state and an hypocoagulation state, and identify what portion (or portions) of the coagulation cascade is/are affected in each state you provide. Chapter 31 Alterations of Hematologic Function in Children Multiple Choice Identify the choice that best completes the statement or answers the question. C 1. What is the cause of polycythemia in the fetus? a. Fetal hemoglobin has a greater affinity for oxygen as a result of diphosphoglycerate (DPG). b. The fetus has a different hemoglobin structure of two α- and two γ-chains rather than two α-and two β-chains. c. Increased erythropoiesis occurs in response to the hypoxic intrauterine environment. d. The lungs of the fetus are undeveloped and unable to diffuse oxygen adequately to the pulmonary capillaries. C 2. Why does fetal hemoglobin have a greater affinity for oxygen than adult hemoglobin? a. The fetus does not have its own oxygen supply and must rely on oxygen from the maternal vascular system. b. The fetus has two γ-chains on the hemoglobin, rather than two β-chains as in the adult. c. Fetal hemoglobin interacts less readily with diphosphoglycerate (DPG), which inhibits hemoglobin-oxygen binding. d. Fetal hemoglobin production occurs in the vessels and liver rather than in the bone marrow as in the adult. A 3. Which blood cell type is elevated at birth but decreases to adult levels during the first year of life? a. Monocytes c. Neutrophils b. Platelets d. Lymphocytes B 4. In a full-term infant, the normal erythrocyte life span is days, whereas the adult erythrocyte life span is days. a. 30 to 50; 80 c. 90 to 110; 140 b. 60 to 80; 120 d. 120 to 130; 150 B 5. What is the most common cause of insufficient erythropoiesis in children? a. Folic acid deficiency c. Hemoglobin abnormality b. Iron deficiency d. Erythrocyte abnormality B 6. How does hemolytic disease of the newborn (HDN) cause acquired congenital hemolytic anemia? a. HDN develops when hypoxia or dehydration causes the erythrocytes to change shapes, which are then recognized as foreign and removed from circulation. b. HDN is an alloimmune disease in which the mother’s immune system produces antibodies against fetal erythrocytes, which are recognized as foreign and removed from circulation. c. HDN develops when the polycythemia present in fetal life continues after birth, causing the excessive number of erythrocytes to be removed from circulation. d. HDN is an autoimmune disease in which the fetus’s immune system produces antibodies against fetal erythrocytes, which are recognized as foreign and removed from circulation. B 7. Erythroblastosis fetalis is defined as an: a. Allergic disease in which maternal blood and fetal blood are antigenically incompatible b. Alloimmune disease in which maternal blood and fetal blood are antigenically incompatible c. Autoimmune disease in immature nucleated cells that are released into the bloodstream d. Autosomal dominant hereditary disease D 8. An infant’s hemoglobin must fall below g/dl before signs of pallor, tachycardia, and systolic murmurs occur. a. 11 c. 7 b. 9 d. 5 C 9. Which vitamin improves the absorption of oral iron taken to treat iron deficiency anemia in children? a. A c. C b. B d. E B 10. Hemolytic disease of the newborn (HDN) can occur if the mother: a. Is Rh-positive and the fetus is Rh-negative b. Is Rh-negative and the fetus is Rh-positive c. Has type A blood and the fetus has type O d. Has type AB blood and the fetus has type B A 11. When diagnosed with hemolytic disease of the newborn (HDN), why does the newborn develop hyperbilirubinemia after birth but not in utero? a. Excretion of unconjugated bilirubin through the placenta into the mother’s circulation is no longer possible. b. Hemoglobin does not break down into bilirubin in the intrauterine environment. c. The liver of the fetus is too immature to conjugate bilirubin from a lipid-soluble to water-soluble form. d. The destruction of erythrocytes producing bilirubin is greater after birth. D 12. Fetuses who do not survive anemia in utero are usually stillborn with gross edema of the entire body. Which term is used to identify this condition? a. Spherocytosis c. Erythroblastosis fetalis b. Icterus gravis neonatorum d. Hydrops fetalis A 13. What is the name of the disorder in which levels of bilirubin remain excessively high in the newborn and are deposited in the brain? a. Kernicterus c. Jaundice b. Icterus neonatorum d. Icterus gravis neonatorum B 14. What treatment prevents the development of kernicterus in an infant born with hemolytic disease of the newborn (HDN)? a. Administration of intravenous fluids to dilute the blood b. Replacement transfusion of new Rh-positive blood that is not contaminated with anti-Rh antibodies c. Performance of a splenectomy to prevent the destruction of abnormal erythrocytes d. Replacement transfusion of Rh-negative erythrocytes B 15. Glucose 6-phosphate dehydrogenase (G6PD) deficiency is what type of inherited disorder? a. X-linked dominant c. Autosomal dominant b. X-linked recessive d. Autosomal recessive C 16. Sickle cell disease is classified as a(an): a. Inherited X-linked recessive disorder b. Inherited autosomal recessive disorder c. Disorder initiated by hypoxemia and acidosis d. Disorder that is diagnosed equally in men and women C 17. Hemoglobin S (HbS) is formed in sickle cell disease as a result of which process? a. Deficiency in glucose 6-phosphate dehydrogenase (G6PD) that changes hemoglobin A (HbA) to HbS. b. Genetic mutation in which two amino acids (histidine and leucine) are missing. c. Genetic mutation in which one amino acid (valine) is replaced by another (glutamic acid). d. Autoimmune response in which one amino acid (proline) is detected as an antigen by abnormal immunoglobulin G (IgG). B 18. Sickle cell disease (SCD) is what type of inherited disorder? a. Autosomal dominant c. X-linked dominant b. Autosomal recessive d. X-linked recessive A 19. What is the reason most children diagnosed with sickle cell anemia are not candidates for either bone marrow or stem cell transplants? a. Well-matched stem cell donors are difficult to find. b. The child is usually too weak to survive the procedure. c. The child’s immune system will not appropriately respond to the antirejection medications. d. Although effective for adults, neither procedure has been proven effective for children. B 20. Which manifestations of vasoocclusive crisis are associated with sickle cell disease (SCD) in infants? a. Atelectasis and pneumonia b. Edema of the hands and feet c. Stasis ulcers of the hands, ankles, and feet d. Splenomegaly and hepatomegaly B 21. What is the chance with each pregnancy that a child born to two parents with the sickle trait will have sickle cell disease (SCD)? a. 20% c. 33% b. 25% d. 50% A 22. Which type of anemia occurs as a result of thalassemia? a. Microcytic, hypochromic c. Macrocytic, hyperchromic b. Microcytic, normochromic d. Macrocytic, normochromic B 23. What is the fundamental defect that results in beta-thalassemia major? a. The spleen prematurely destroys the precipitate-carrying cells. b. A severe uncoupling of α- and β-chain synthesis occurs. c. All four beta-forming genes are defective. d. Hemoglobin H (HbH) develops when three genes are defective. A 24. The alpha- and beta-thalassemias are considered what types of inherited disorder? a. Autosomal recessive c. X-linked recessive b. Autosomal dominant d. X-linked dominant C 25. Hemophilia B is caused by a deficiency of which clotting factor? a. V c. IX b. VIII d. X C 26. Hemophilia A is considered to be what type of inherited disorder? a. Autosomal dominant c. X-linked recessive b. Autosomal recessive d. X-linked dominant B 27. Which disease is an autosomal dominant inherited hemorrhagic disease? a. Hemophilia A c. Christmas disease b. von Willebrand disease d. Hemophilia B C 28. Idiopathic thrombocytopenic purpura (ITP) is an autoimmune process involving antibodies attacking which type of cells? a. Neutrophils c. Platelets b. Eosinophils d. Basophils B 29. Which disorder results in decreased erythrocytes and platelets with changes in leukocytes and has clinical manifestations of pallor, fatigue, petechiae, purpura, bleeding, and fever? a. Idiopathic thrombocytopenic purpura (ITP) b. Acute lymphocytic leukemia (ALL) c. Non-Hodgkin lymphoma (NHL) d. Iron deficiency anemia (IDA) B 30. When does fetal erythrocyte production shift from the liver to the bone marrow? a. Fourth month of gestation c. Eighth month of gestation b. Fifth month of gestation d. At birth D 31. Which disease is caused by clotting factor VIII deficiency and is an autosomal dominant trait? a. Hemophilia A c. Hemophilia C b. Hemophilia B d. von Willebrand disease A 32. Which type of hemophilia affects only men? a. Hemophilia A c. Hemophilia C b. Hemophilia B d. von Willebrand disease C 33. Which hemophilia occurs equally in both men and women? a. Hemophilia A c. Hemophilia C b. Hemophilia B d. von Willebrand disease B 34. During childhood, when is dietary iron deficiency commonly diagnosed? a. Between 2 months and 1 year c. Between 12 months and 3 years b. Between 6 months and 2 years d. Between 18 months and 4 years A 35. What is the significance of hyperdiploidy when diagnosing and treating leukemia? a. Hyperdiploidy indicates a good prognosis. b. Hyperdiploidy indicates a poor prognosis. c. Hyperdiploidy indicates poor response to a specific treatment. d. Hyperdiploidy indicates the achievement of remission. Multiple Response Identify one or more choices that best complete the statement or answer the question. 36. What are the common triggers for sickle cell crisis? (Select all that apply.) a. Fever b. Infection c. Dehydration d. Alkalosis e. Exposure to the cold Matching Match each sickle cell crisis with its description. Terms may be used more than once. A. Vasoocclusive crisis B. Aplastic crisis C. Sequestration crisis D. Hyperhemolytic crisis C 37. Large amounts of blood become acutely pooled in the liver and spleen. A 38. Blood flow is impaired by tangled masses of rigid, sickled cells. D 39. Crisis occurs in association with certain drugs or infection. B 40. Compensatory erythropoiesis is compromised, thus limiting the number of erythrocytes that are replaced. Thought Questions 1. A woman who is Rh-negative just delivered a baby that is Rh-positive. Should she be concerned? If so, explain why. [Show More]
Last updated: 1 year ago
Preview 1 out of 102 pages
Reviews( 0 )
Document information
Connected school, study & course
About the document
Uploaded On
Jan 24, 2021
Number of pages
102
Written in
Additional information
This document has been written for:
Uploaded
Jan 24, 2021
Downloads
0
Views
21

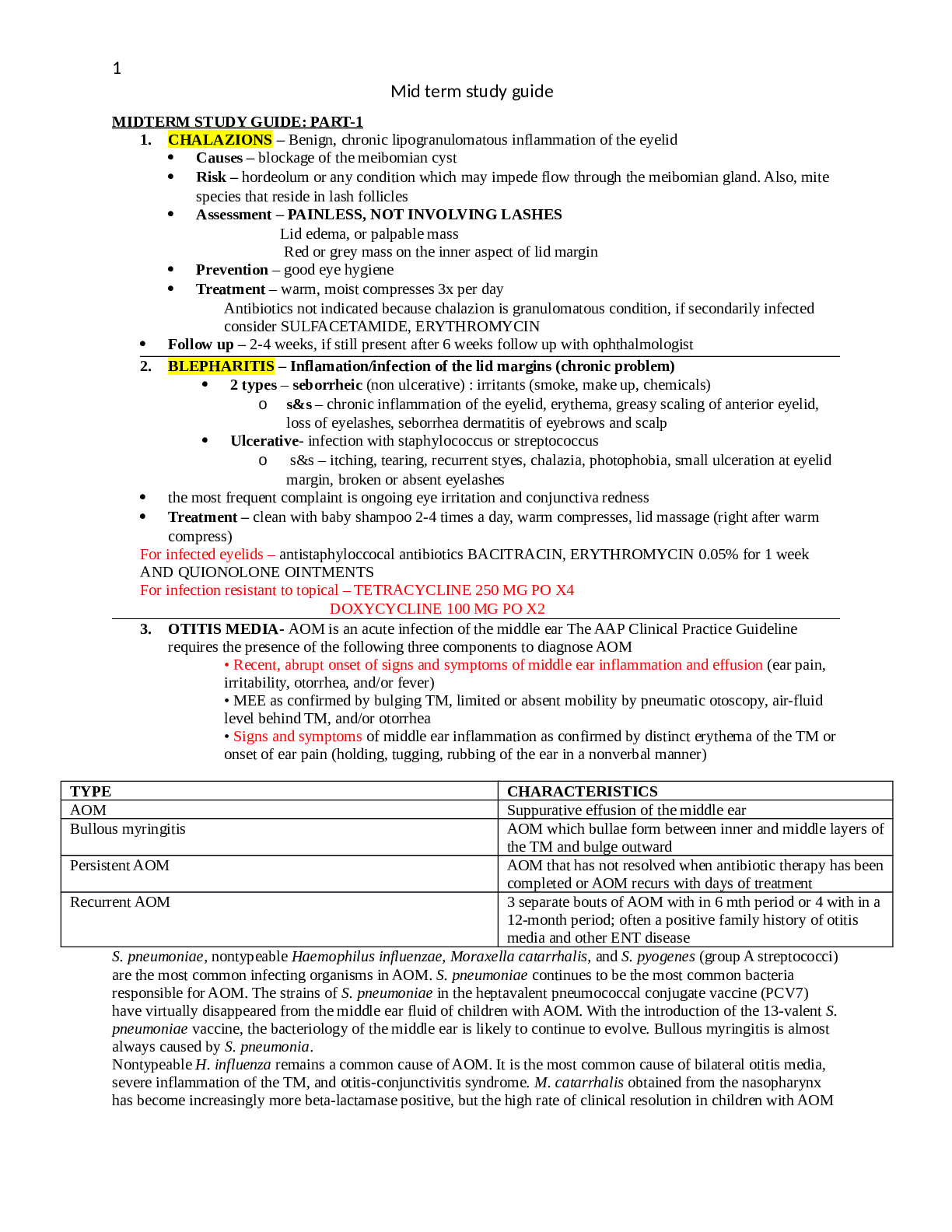
 (2).png)
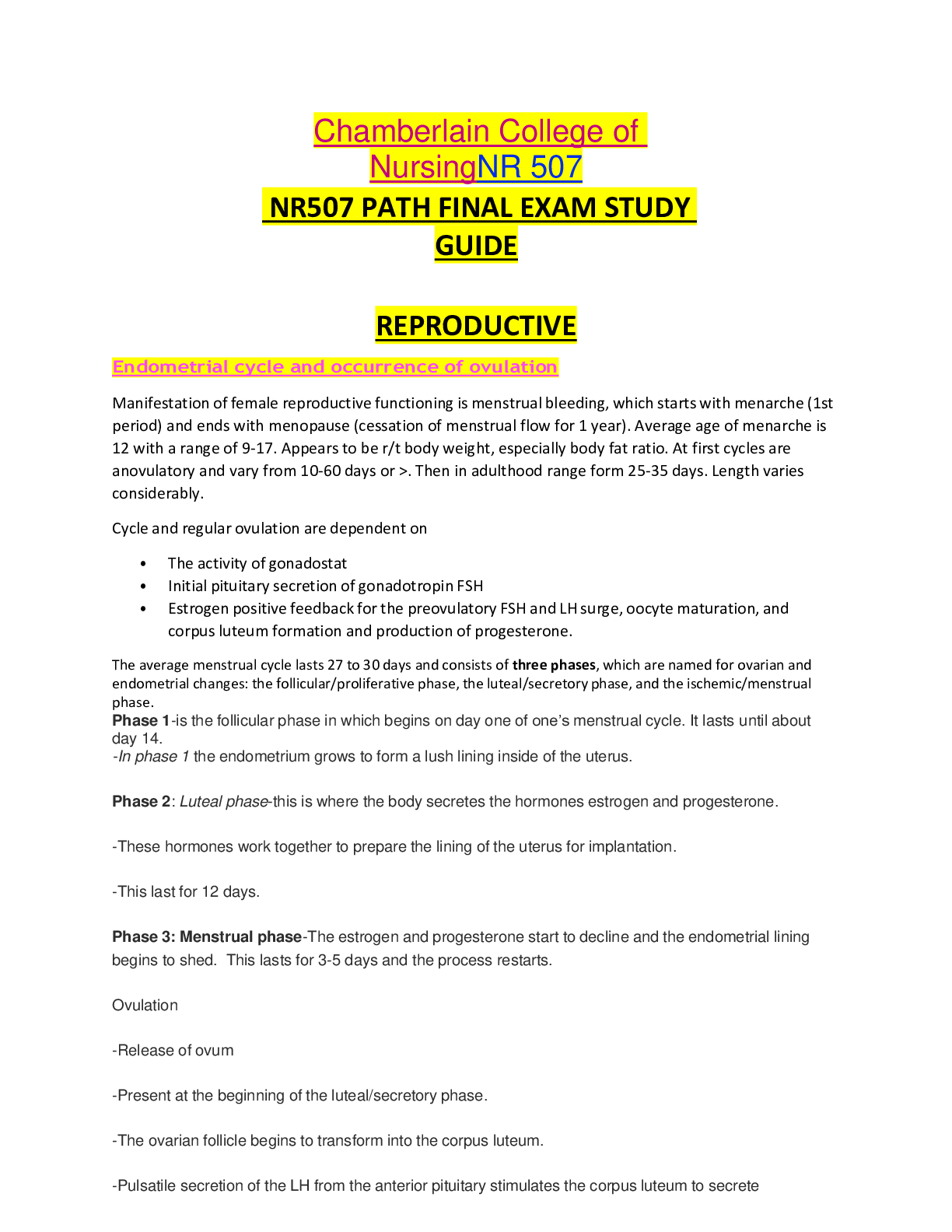
.png)
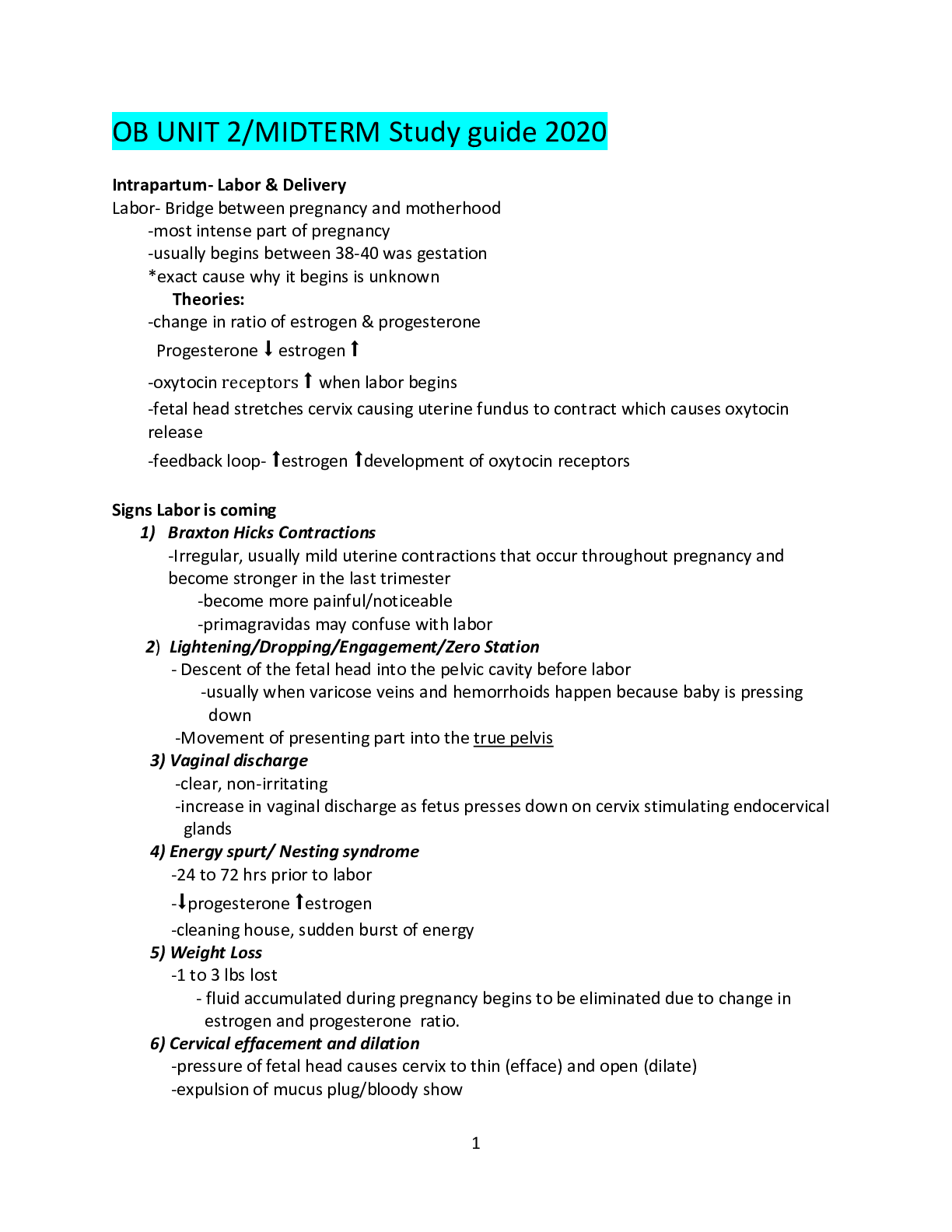
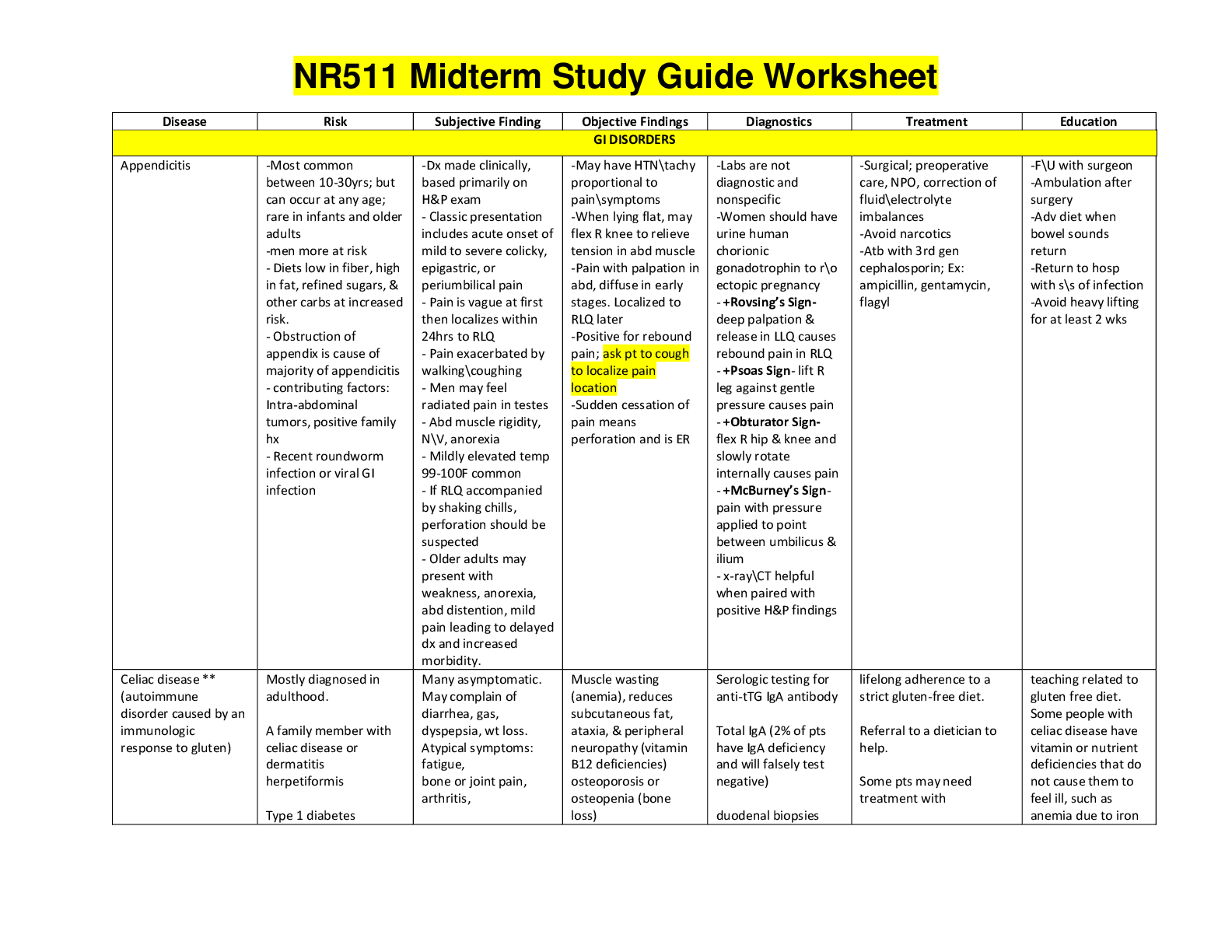
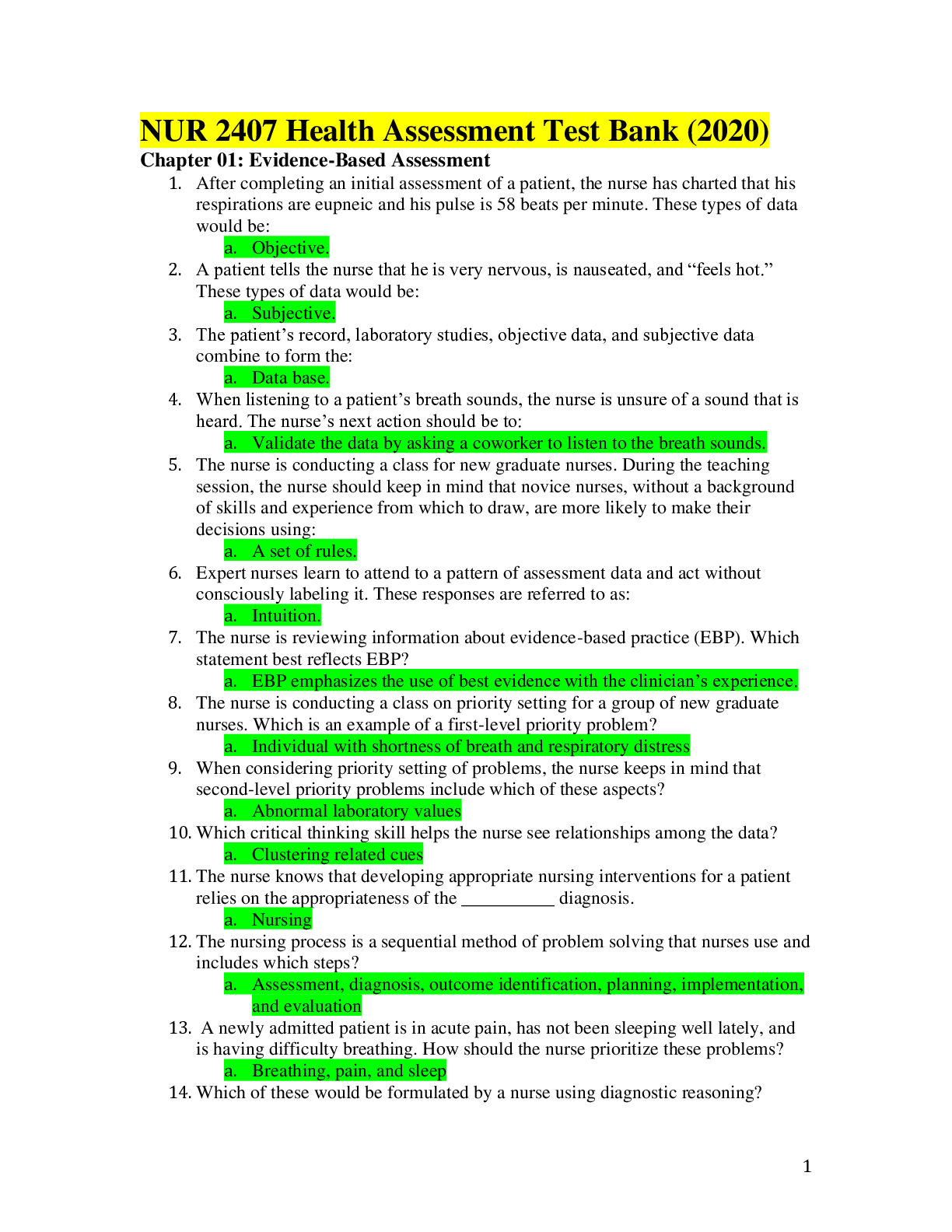
.png)
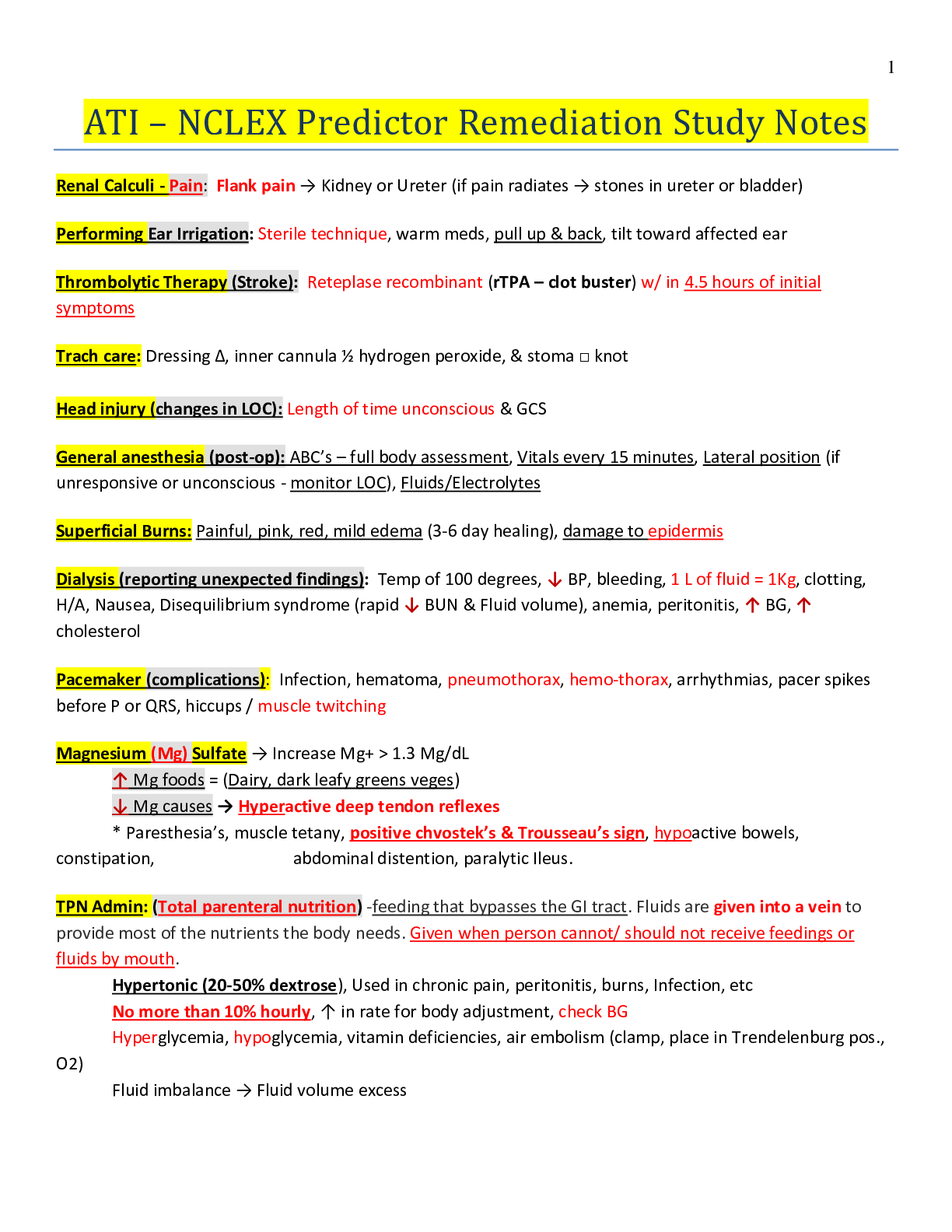
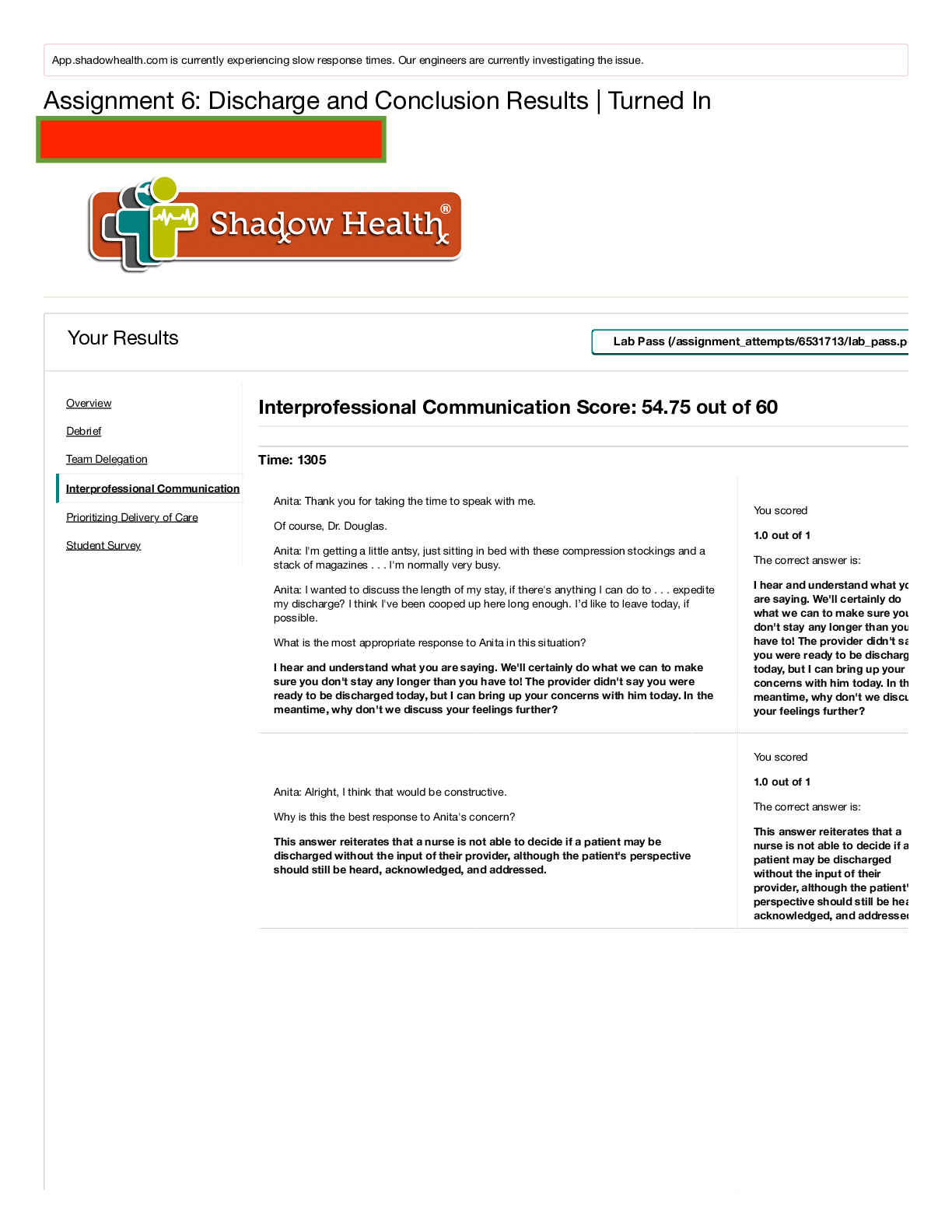
 Rasmussen College.png)