*NURSING > TEST BANK > TEST BANK Perspectives of Pediatric Nursing Hockenberry: Wong’s Essentials of Pediatric Nursing, 1 (All)
TEST BANK Perspectives of Pediatric Nursing Hockenberry: Wong’s Essentials of Pediatric Nursing, 10th Edition ,100% CORRECT
Document Content and Description Below
TEST BANK Perspectives of Pediatric Nursing Hockenberry: Wong’s Essentials of Pediatric Nursing, 10th Edition Chapter 01 MULTIPLE CHOICE 1. A nurse is planning a teaching session for paren... ts of preschool children. Which statement explains why the nurse should include information about morbidity and mortality? a. Life span statistics are included in the data. b. It explains effectiveness of treatment. c. Cost-effective treatment is detailed for the general population. d. High-risk age groups for certain disorders or hazards are identified. ANS: D Analysis of morbidity and mortality data provides the parents with information about which groups of individuals are at risk for which health problems. Life span statistics is a part of the mortality data. Treatment modalities and cost are not included in morbidity and mortality data. DIF: Cognitive Level: Apply REF: p. 11 TOP: Integrated Process: Nursing Process: Planning MSC: Area of Client Needs: Health Promotion and Maintenance 2. A clinic nurse is planning a teaching session about childhood obesity prevention for parents of school-age children. The nurse should include which associated risk of obesity in the teaching plan? a. Type I diabetes b. Respiratory disease c. Celiac disease d. Type II diabetes ANS: D NURSINGDOC.COM Childhood obesity has been associated with the rise of type II diabetes in children. Type I diabetes is not associated with obesity and has a genetic component. Respiratory disease is not associated with obesity, and celiac disease is the inability to metabolize gluten in foods and is not associated with obesity. DIF: Cognitive Level: Apply REF: p. 2 TOP: Integrated Process: Nursing Process: Planning MSC: Area of Client Needs: Health Promotion and Maintenance 3. Which is the leading cause of death in infants younger than 1 year? a. Congenital anomalies b. Sudden infant death syndrome c. Respiratory distress syndrome d. Bacterial sepsis of the newborn ANS: A Congenital anomalies account for 20.1% of deaths in infants younger than 1 year. Sudden infant death syndrome accounts for 8.2% of deaths in this age group. Respiratory distress syndrome accounts for 3.4% of deaths in this age group. Infections specific to the perinatal period account for 2.7% of deaths in this age group. DIF: Cognitive Level: Remember REF: p. 6 TOP: Integrated Process: Nursing Process: Assessment MSC: Area of Client Needs: Health Promotion and Maintenance 4. Which leading cause of death topic should the nurse emphasize to a group of African-American boys ranging in age from 15 to 19 years? a. Suicide b. Cancer c. Firearm homicide d. Occupational injuries ANS: C Firearm homicide is the second overall cause of death in this age group and the leading cause of death in African-American males. Suicide is the third-leading cause of death in this population. Cancer, although a major health problem, is the fourth-leading cause of death in this age group. Occupational injuries do not contribute to a significant death rate for this age group. DIF: Cognitive Level: Understand REF: p. 7 TOP: Integrated Process: Nursing Process: Planning MSC: Area of Client Needs: Health Promotion and Maintenance 5. Which is the major cause of death for children older than 1 year? a. Cancer b. Heart disease c. Unintentional injuries d. Congenital anomalies ANS: C NURSINGDOC.COM Unintentional injuries (accidents) are the leading cause of death after age 1 year through adolescence. Congenital anomalies are the leading cause of death in those younger than 1 year. Cancer ranks either second or fourth, depending on the age group, and heart disease ranks fifth in the majority of the age groups. DIF: Cognitive Level: Remember REF: p. 7 TOP: Integrated Process: Nursing Process: Planning MSC: Area of Client Needs: Health Promotion and Maintenance 6. Which is the leading cause of death from unintentional injuries for females ranging in age from 1 to 14? a. Mechanical suffocation b. Drowning c. Motor vehicle–related fatalities d. Fire- and burn-related fatalities ANS: C Motor vehicle–related fatalities are the leading cause of death for females ranging in age from 1 to 14, either as passengers or as pedestrians. Mechanical suffocation is fourth or fifth, depending on the age. Drowning is the second- or third-leading cause of death, depending on the age. Fire- and burn-related fatalities are the second-leading cause of death. DIF: Cognitive Level: Remember REF: p. 3 TOP: Integrated Process: Nursing Process: Assessment MSC: Area of Client Needs: Health Promotion and Maintenance 7. Which factor most impacts the type of injury a child is susceptible to, according to the child’s age? a. Physical health of the child b. Developmental level of the child c. Educational level of the child d. Number of responsible adults in the home ANS: B The child’s developmental stage determines the type of injury that is likely to occur. The child’s physical health may facilitate the child’s recovery from an injury but does not impact the type of injury. Educational level is related to developmental level, but it is not as important as the child’s developmental level in determining the type of injury. The number of responsible adults in the home may affect the number of unintentional injuries, but the type of injury is related to the child’s developmental stage. DIF: Cognitive Level: Understand REF: p. 3 TOP: Integrated Process: Nursing Process: Planning MSC: Area of Client Needs: Health Promotion and Maintenance 8. Which is now referred to as the “new morbidity”? a. Limitations in the major activities of daily living b. Unintentional injuries that cause chronic health problems c. Discoveries of new therapies to treat health problems d. Behavioral, social, and educational problems that alter health NURSINGDOC.COM ANS: D The new morbidity reflects the behavioral, social, and educational problems that interfere with the child’s social and academic development. It is currently estimated that the incidence of these issues is from 5% to 30%. Limitations in major activities of daily living and unintentional injuries that result in chronic health problems are included in morbidity data. Discovery of new therapies would be reflected in changes in morbidity data over time. DIF: Cognitive Level: Remember REF: p. 2 TOP: Integrated Process: Nursing Process: Assessment MSC: Area of Client Needs: Health Promotion and Maintenance 9. A nurse on a pediatric unit is practicing family-centered care. Which is most descriptive of the care the nurse is delivering? a. Taking over total care of the child to reduce stress on the family b. Encouraging family dependence on health care systems c. Recognizing that the family is the constant in a child’s life d. Excluding families from the decision-making process ANS: C The three key components of family-centered care are respect, collaboration, and support. Family-centered care recognizes the family as the constant in the child’s life. Taking over total care does not include the family in the process and may increase stress instead of reducing stress. The family should be enabled and empowered to work with the health care system. The family is expected to be part of the decision-making process. DIF: Cognitive Level: Remember REF: p. 7 TOP: Integrated Process: Nursing Process: Implementation MSC: Area of Client Needs: Health Promotion and Maintenance 10. The nurse is preparing an in-service education to staff about atraumatic care for pediatric patients. Which intervention should the nurse include? a. Prepare the child for separation from parents during hospitalization by reviewing a video. b. Prepare the child before any unfamiliar treatment or procedure by demonstrating on a stuffed animal. c. Help the child accept the loss of control associated with hospitalization. d. Help the child accept pain that is connected with a treatment or procedure. ANS: B Preparing the child for any unfamiliar treatments, controlling pain, allowing privacy, providing play activities for expression of fear and aggression, providing choices, and respecting cultural differences are components of atraumatic care. In the provision of atraumatic care, the separation of child from parents during hospitalization is minimized. The nurse should promote a sense of control for the child. Preventing and minimizing bodily injury and pain are major components of atraumatic care. DIF: Cognitive Level: Understand REF: p. 8 TOP: Integrated Process: Nursing Process: Implementation MSC: Area of Client Needs: Psychosocial Integrity 11. Which is most suggestive that a nurse has a nontherapeutic relationship with a patient and family? NURSINGDOC.COM a. Staff is concerned about the nurse’s actions with the patient and family. b. Staff assignments allow the nurse to care for same patient and family over an extended time. c. Nurse is able to withdraw emotionally when emotional overload occurs but still remains committed. d. Nurse uses teaching skills to instruct patient and family rather than doing everything for them. ANS: A An clue to a nontherapeutic staff-patient relationship is concern of other staff members. Allowing the nurse to care for the same patient over time would be therapeutic for the patient and family. Nurses who are able to somewhat withdraw emotionally can protect themselves while providing therapeutic care. Nurses using teaching skills to instruct patient and family will assist in transitioning the child and family to self-care. DIF: Cognitive Level: Analyze REF: p. 8 TOP: Integrated Process: Nursing Process: Assessment MSC: Area of Client Needs: Psychosocial Integrity 12. Which is most descriptive of clinical reasoning? a. A simple developmental process b. Purposeful and goal-directed c. Based on deliberate and irrational thought d. Assists individuals in guessing what is most appropriate ANS: B Clinical reasoning is a complex, developmental process based on rational and deliberate thought. Clinical reasoning is not a developmental process. Clinical reasoning is based on rational and deliberate thought. Clinical reasoning is not a guessing process. DIF: Cognitive Level: Understand REF: p. 10 TOP: Integrated Process: Nursing Process: Planning MSC: Area of Client Needs: Safe and Effective Care Environment: Management of Care 13. A nurse makes the decision to apply a topical anesthetic to a child’s skin before drawing blood. Which ethical principle is the nurse demonstrating? a. Autonomy b. Beneficence c. Justice d. Truthfulness ANS: B Beneficence is the obligation to promote the patient’s well-being. Applying a topical anesthetic before drawing blood promotes reducing the discomfort of the venipuncture. Autonomy is the patient’s right to be self-governing. Justice is the concept of fairness. Truthfulness is the concept of honesty. DIF: Cognitive Level: Understand REF: p. 10 TOP: Integrated Process: Nursing Process: Implementation MSC: Area of Client Needs: Physiological Integrity NURSINGDOC.COM 14. Which action by the nurse demonstrates use of evidence-based practice (EBP)? a. Gathering equipment for a procedure b. Documenting changes in a patient’s status c. Questioning the use of daily central line dressing changes d. Clarifying a physician’s prescription for morphine ANS: C The nurse who questions the daily central line dressing change is ascertaining whether clinical interventions result in positive outcomes for patients. This demonstrates EBP, which implies questioning why something is effective and whether a better approach exists. Gathering equipment for a procedure and documenting changes in a patient’s status are practices that follow established guidelines. Clarifying a physician’s prescription for morphine constitutes safe nursing care. DIF: Cognitive Level: Apply REF: p. 10 TOP: Integrated Process: Nursing Process: Evaluation MSC: Area of Client Needs: Safe and Effective Care Environment: Management of Care 15. A nurse is admitting a toddler to the hospital. The toddler is with both parents and is currently sitting comfortably on a parent’s lap. The parents state they will need to leave for a brief period. Which type of nursing diagnosis should the nurse formulate for this child? a. Risk for anxiety b. Anxiety c. Readiness for enhanced coping d. Ineffective coping ANS: A A potential problem is categorized as a risk. The toddler has a risk to become anxious when the parents leave. Nursing interventions will be geared toward reducing the risk. The child is not showing current anxiety or ineffective coping. The child is not at a point for readiness for enhanced coping, especially because the parents will be leaving. DIF: Cognitive Level: Remember REF: p. 11 TOP: Integrated Process: Nursing Process: Diagnosis MSC: Area of Client Needs: Health Promotion and Maintenance 16. A child has a postoperative appendectomy incision covered by a dressing. The nurse has just completed a prescribed dressing change for this child. Which description is an accurate documentation of this procedure? a. Dressing change to appendectomy incision completed, child tolerated procedure well, parent present b. No complications noted during dressing change to appendectomy incision c. Appendectomy incision non-reddened, sutures intact, no drainage noted on old dressing, new dressing applied, procedure tolerated well by child d. No changes to appendectomy incisional area, dressing changed, child complained of pain during procedure, new dressing clean, dry and intact ANS: C The nurse should document assessments and reassessments. Appearance of the incision described in objective terms should be included during a dressing change. The nurse should document patient’s response and the outcomes of the care provided. In this example, these include drainage on the old dressiNngU,RtShIeNaGpTpBli.cCaOtMion of the new dressing, and the child’s response. The other statements partially fulfill the requirements of documenting assessments and reassessments, patient’s response, and outcome, but do not include all three. DIF: Cognitive Level: Analyze REF: p. 12 TOP: Integrated Process: Nursing Process: Implementation MSC: Area of Client Needs: Safe and Effective Care Environment: Management of Care 17. A nurse is planning a class on accident prevention for parents of toddlers. Which safety topic is the priority for this class? a. Appropriate use of car seat restraints b. Safety crossing the street c. Helmet use when riding a bicycle d. Poison control numbers ANS: A Motor vehicle accidents (MVAs) continue to be the most common cause of death in children older than 1 year, therefore the priority topic is appropriate use of car seat restraints. Safety crossing the street and bicycle helmet use are topics that should be included for preschool parents but are not priorities for parents of toddlers. Information about poison control is important for parents of toddlers and would be a safety topic to include but is not the priority over appropriate use of car seat restraints. DIF: Cognitive Level: Apply REF: p. 3 TOP: Integrated Process: Nursing Process: Planning MSC: Area of Client Needs: Health Promotion and Maintenance 18. A nurse is collecting subjective and objective information about target populations to diagnose problems based on community needs. This describes which step in the community nursing process? a. Planning b. Diagnosis c. Assessment d. Establishing objectives ANS: C The nursing process stages are similar, whether the client is one child or a population of children. The assessment phase of the nursing process focuses on collecting subjective and objective data. Planning is the development of community-centered goals and objectives. Diagnosis is the identification of problems specific to the community. DIF: Cognitive Level: Understand REF: p. 11 TOP: Integrated Process: Communication and Documentation MSC: Area of Client Needs: Safe and Effective Care Environment: Management of Care 19. A nurse is establishing several health programs, such as bicycle safety, to improve the health status of a target population. This describes which step in the community nursing process? a. Planning b. Evaluation c. Assessment d. Implementation ANS: D NURSINGDOC.COMThe nurse working with the community to put into practice a program to reach community goals is the implementation phase of the community nursing process. Planning involves designing the program to meet community-centered goals. The evaluation stage would determine the effectiveness of the program. During the assessment phase, the nurse would identify the resources necessary and the barriers that would interfere with implementation. DIF: Cognitive Level: Understand REF: p. 11 TOP: Integrated Process: Nursing Process: Implementation MSC: Area of Client Needs: Safe and Effective Care Environment: Management of Care 20. A school nurse is conducting vision and hearing testing on fifth-grade children. Which level of prevention is the nurse demonstrating? a. Primary b. Secondary c. Tertiary d. Health promotion ANS: B Secondary prevention focuses on screening and early diagnosis of disease. Vision and hearing testing are screening tests to detect problems. Primary prevention focuses on health promotion and prevention of disease or injury. Tertiary prevention focuses on optimizing function for children with a disability or chronic disease. Health promotion is focused on preventing disease or illness. DIF: Cognitive Level: Understand REF: p. 2 TOP: Integrated Process: Nursing Process: Implementation MSC: Area of Client Needs: Health Promotion and Maintenance 21. The home health nurse asks a child’s mother many questions as part of the assessment. The mother answers many questions, then stops and says, “I don’t know why you ask me all this. Who gets to know this information?” The nurse should take which action? a. Determine why the mother is so suspicious. b. Determine what the mother does not want to tell. c. Explain who will have access to the information. d. Explain that everything is confidential and that no one else will know what is said. ANS: C Communication with the family should not be invasive. The nurse needs to explain the importance of collecting the information, its applicability to the child’s care, and who will have access to the information. The mother is not being suspicious and is not necessarily withholding important information. She has a right to understand how the information she provides will be used. The nurse will need to share, through both oral and written communication, clinically relevant information with other involved health professionals. DIF: Cognitive Level: Apply REF: p. 9 TOP: Integrated Process: Communication and Documentation MSC: Area of Client Needs: Safe and Effective Care Environment: Management of Care 22. When communicating with other professionals, what is important for the nurse to do? a. Ask others what they want to know. b. Share everything known about the family. c. Restrict communication to clinNiUcaRlSlyINrGelTeBv.aCnOtMinformation. d. Recognize that confidentiality is not possible. ANS: C The nurse will need to share, through both oral and written communication, clinically relevant information with other involved health professionals. Asking others what they want to know and sharing everything known about the family is inappropriate. Patients have a right to confidentiality. The nurse is not permitted to share information about clients, except clinically relevant information that pertains to the child’s care. Confidentiality permits the disclosure of information to other health professionals on a need-to-know basis. DIF: Cognitive Level: Apply REF: p. 9 TOP: Integrated Process: Communication and Documentation MSC: Area of Client Needs: Safe and Effective Care Environment: Management of Care 23. A nurse manager at a home-care agency is planning a continuing education program for the home-care staff nurses. Which type of continuing education program should the nurse manager plan? a. On-line training modules b. A structured written teaching module each nurse completes individually c. A workshop training day, with a professional speaker, where nurses can interact with each other d. One-on-one continuing education training with each nurse ANS: C Because of the unique practice environment of home care nurses, it is important for an agency to facilitate sharing among peers to decrease work-related stress, increase job satisfaction, and support high-quality patient care. On-line training, written teaching modules, and one-on-one training would not allow for any sharing with peers. DIF: Cognitive Level: Apply REF: p. 7 TOP: Integrated Process: Nursing Process: Planning MSC: Area of Client Needs: Safe and Effective Care Environment: Management of Care MULTIPLE RESPONSE 1. Which behaviors by the nurse indicate a therapeutic relationship with children and families? (Select all that apply.) a. Spending off-duty time with children and families b. Asking questions if families are not participating in the care c. Clarifying information for families d. Buying toys for a hospitalized child e. Learning about the family’s religious preferences ANS: B, C, E Asking questions if families are not participating in the care, clarifying information for families, and learning about the family’s religious preferences are positive actions and foster therapeutic relationships with children and families. Spending off-duty time with children and families and buying toys for a hospitalized child are negative actions and indicate overinvolvement with children and families, which is nontherapeutic. DIF: Cognitive Level: Understand NURSINRGETFB:.CpO.M8 TOP: Integrated Process: Nursing Process: Evaluation MSC: Area of Client Needs: Psychosocial Integrity 2. Which behaviors by the nurse indicate therapeutic nurse-family boundaries? (Select all that apply.) a. Nurse visits family on days off. b. House rules are negotiated. c. Nurse buys child expensive gifts. d. Communication is open and two-way. ANS: B, D A home care nurse can establish therapeutic nurse-family boundaries by negotiating house rules and ensuring that communication is open and two-way. Visiting the family of off-duty days and buying expensive gifts for the child would be boundary crossing and nontherapeutic. DIF: Cognitive Level: Analyze REF: p. 8 TOP: Integrated Process: Nursing Process: Implementation MSC: Area of Client Needs: Psychosocial Integrity OTHER 1. A nurse is formulating a clinical question for evidence-based practice. Place in order the steps the nurse should use to clarify the scope of the problem and clinical topic of interest. Begin with the first step of the process and proceed ordering the steps ending with the final step of the process. Provide answer as lowercase letters separated by commas (e.g., a, b, c, d, e). a. Intervention b. Outcome c. Population d. Time e. Control ANS: c, a, e, b, d When formulating a clinical question for evidence-based practice, the nurse should follow a concise, organized way that allows for clear answers. Good clinical questions should be asked in the PICOT (population, intervention, control, outcome, time) format to assist with clarity and literature searching. PICOT questions assist with clarifying the scope of the problem and clinical topic of interest. DIF: Cognitive Level: Understand REF: p. 10 TOP: Integrated Process: Nursing Process: Assessment MSC: Area of Client Needs: Health Promotion and Maintenance NURSINGDOC.COM Chapter 03: Developmental and Genetic Influences on Child Health Promotion Hockenberry: Wong’s Essentials of Pediatric Nursing, 10th Edition MULTIPLE CHOICE 1. An infant gains head control before sitting unassisted. The nurse recognizes that this is which type of development? a. Cephalocaudal b. Proximodistal c. Mass to specific d. Sequential ANS: A The pattern of development that is head-to-tail, or cephalocaudal, direction is described by an infant’s ability to gain head control before sitting unassisted. The head end of the organism develops first and is large and complex, whereas the lower end is smaller and simpler, and development takes place at a later time. Proximodistal, or near to far, is another pattern of development. Limb buds develop before fingers and toes. Postnatally, the child has control of the shoulder before achieving mastery of the hands. Mass to specific is not a specific pattern of development. In all dimensions of growth, a definite, sequential pattern is followed. DIF: Cognitive Level: Understand REF: p. 38 TOP: Integrated Process: Nursing Process: Assessment MSC: Area of Client Needs: Health Promotion and Maintenance NURSINGDOC.COM 2. Which refers to those times in an individual’s life when he or she is more susceptible to positive or negative influences? a. Sensitive period b. Sequential period c. Terminal points d. Differentiation points ANS: A Sensitive periods are limited times during the process of growth when the organism will interact with a particular environment in a specific manner. These times make the organism more susceptible to positive or negative influences. The sequential period, terminal points, and differentiation points are developmental times that do not make the organism more susceptible to environmental interaction. DIF: Cognitive Level: Remember REF: p. 39 TOP: Integrated Process: Nursing Process: Planning MSC: Area of Client Needs: Health Promotion and Maintenance 3. An infant who weighs 7 pounds at birth would be expected to weigh how many pounds at age 1 year? a. 14 b. 16 c. 18 TestBankWorld.org d. 21 ANS: D In general, birth weight triples by the end of the first year of life. For an infant who was 7 pounds at birth, 21 pounds would be the anticipated weight at the first birthday; 14, 16, or 18 pounds is below what would be expected for an infant with a birth weight of 7 pounds. DIF: Cognitive Level: Understand REF: p. 41 TOP: Integrated Process: Nursing Process: Assessment MSC: Area of Client Needs: Health Promotion and Maintenance 4. By what age does birth length usually double? a. 1 year b. 2 years c. 4 years d. 6 years ANS: C Linear growth or height occurs almost entirely as a result of skeletal growth and is considered a stable measurement of general growth. On average, most children have doubled their birth length at age 4 years. One and 2 years are too young for doubling of length. Most children will have achieved the doubling by age 4 years. DIF: Cognitive Level: Remember REF: p. 41 TOP: Integrated Process: Nursing Process: Assessment MSC: Area of Client Needs: Health Promotion and Maintenance NURSINGDOC.COM 5. Parents of an 8-year-old child ask the nurse how many inches their child should grow each year. The nurse bases the answer on the knowledge that after age 7 years, school-age children usually grow what number of inches per year? a. 1 b. 2 c. 3 d. 4 ANS: B The growth velocity after age 7 years is approximately 5 cm (2 inches) per year. One inch is too small an amount. Three and 4 inches are greater than the average yearly growth after age 7 years. DIF: Cognitive Level: Apply REF: p. 41 TOP: Integrated Process: Nursing Process: Implementation MSC: Area of Client Needs: Health Promotion and Maintenance 6. Parents express concern that their pubertal daughter is taller than the boys in her class. The nurse should respond with which statement regarding how the onset of pubertal growth spurt compares in girls and boys? a. It occurs earlier in boys. b. It occurs earlier in girls. c. It is about the same in both boys and girls. TestBankWorld.org d. In both boys and girls, the pubertal growth spurt depends on growth in infancy. ANS: B Usually, the pubertal growth spurt begins earlier in girls. It typically occurs between the ages of 10 and 14 years for girls and 11 and 16 years for boys. The average earliest age at onset is 1 year earlier for girls. There does not appear to be a relation to growth during infancy. DIF: Cognitive Level: Apply REF: p. 41 TOP: Integrated Process: Nursing Process: Implementation MSC: Area of Client Needs: Health Promotion and Maintenance 7. A 13-year-old girl asks the nurse how much taller she will get. She has been growing about 2 inches per year but grew 4 inches this past year. Menarche recently occurred. The nurse should base her response on which statement? a. Growth cannot be predicted. b. Pubertal growth spurt lasts about 1 year. c. Mature height is achieved when menarche occurs. d. Approximately 95% of mature height is achieved when menarche occurs. ANS: D At the time of the beginning of menstruation or the skeletal age of 13 years, most girls have grown to about 95% of their adult height. They may have some additional growth (5%) until the epiphyseal plates are closed. Although growth cannot be definitively predicted, on average, 95% of adult height has been reached with the onset of menstruation. Pubertal growth spurt lasts about 1 year does not address the girl’s question. Young women usually will grow approximately 5% moreNaUfRteSrINthGeToBn.CseOtMof menstruation. DIF: Cognitive Level: Apply REF: p. 41 TOP: Integrated Process: Teaching/Learning MSC: Area of Client Needs: Health Promotion and Maintenance 8. How is a child’s skeletal age best determined? a. Assessment of dentition b. Assessment of height over time c. Facial bone development d. Radiographs of the hand and wrist ANS: D The most accurate measure of skeletal age is radiologic examinations of the growth plates. These are the epiphyseal cartilage plates. Radiographs of the hand and wrist provide the most useful screening to determine skeletal age. Age of tooth eruption has considerable variation in children. It would not be a good determinant of skeletal age. Assessment of height over time will provide a record of the child’s height but not skeletal age. Facial bone development will not reflect the child’s skeletal age, which is determined by radiographic assessment. DIF: Cognitive Level: Remember REF: p. 41 TOP: Integrated Process: Nursing Process: Assessment MSC: Area of Client Needs: Health Promotion and Maintenance 9. Trauma to which site can result in a growth problem for children’s long bones? TestBankWorld.org a. Matrix b. Connective tissue c. Calcified cartilage d. Epiphyseal cartilage plate ANS: D The epiphyseal cartilage plate is the area of active growth. Bone injury at the epiphyseal plate can significantly affect subsequent growth and development. Trauma or infection can result in deformity. The matrix, connective tissue, and calcified cartilage are not areas of active growth. Trauma in these sites will not result in growth problems for the long bones. DIF: Cognitive Level: Comprehend REF: p. 41 TOP: Integrated Process: Nursing Process: Assessment MSC: Area of Client Needs: Health Promotion and Maintenance 10. A nurse has completed a teaching session for adolescents regarding lymphoid tissue growth. Which statement, by the adolescents, indicates understanding of the teaching? a. The tissue reaches adult size by age 1 year. b. The tissue quits growing by 6 years of age. c. The tissue is poorly developed at birth. d. The tissue is twice the adult size by ages 10 to 12 years. ANS: D Lymphoid tissue continues growing until it reaches maximal development at ages 10 to 12 years, which is twice its adult size. A rapid decline in size occurs until it reaches adult size by the end of adolescence. The tissueNrUeRacShINesGaTdBu.CltOsMize at 6 years of age but continues to grow. The tissue is well developed at birth. DIF: Cognitive Level: Analyze REF: p. 42 TOP: Integrated Process: Nursing Process: Evaluation MSC: Area of Client Needs: Health Promotion and Maintenance 11. Which statement is true about the basal metabolic rate (BMR) in children? a. It is reduced by fever. b. It is slightly higher in boys than in girls at all ages. c. It increases with age of child. d. It decreases as proportion of surface area to body mass increases. ANS: B The BMR is the rate of metabolism when the body is at rest. At all ages, the rate is slightly higher in boys than in girls. The rate is increased by fever. The BMR is highest in infancy and then closely relates to the proportion of surface area to body mass. As the child grows, the proportion decreases progressively to maturity. DIF: Cognitive Level: Understand REF: p. 42 TOP: Integrated Process: Nursing Process: Assessment MSC: Area of Client Needs: Health Promotion and Maintenance: Growth and Development TestBankWorld.org 12. A mother reports that her 6-year-old child is highly active, irritable, and irregular in habits and that the child adapts slowly to new routines, people, or situations. How should the nurse chart this type of temperament? a. Easy b. Difficult c. Slow-to-warm-up d. Fast-to-warm-up ANS: B Being highly active, irritable, irregular in habits, and adapting slowly to new routines, people, or situations is a description of difficult children, which compose about 10% of the population. Negative withdrawal responses are typical of this type of child, who requires a more structured environment. Mood expressions are usually intense and primarily negative. These children exhibit frequent periods of crying and often violent tantrums. Easy children are even tempered, regular, and predictable in their habits. They are open and adaptable to change. Approximately 40% of children fit this description. Slow-to-warm-up children typically react negatively and with mild intensity to new stimuli and adapt slowly with repeated contact. Approximately 10% of children fit this description. “Fast-to-warm-up” is not one of the categories identified. DIF: Cognitive Level: Apply REF: p. 43 TOP: Integrated Process: Communication and Documentation MSC: Area of Client Needs: Health Promotion and Maintenance 13. A 12-year-old child enjoys collecting stamps, playing soccer, and participating in Boy Scout activities. The nurse recognizes thNaUt tRhSeINchGiTldB.iCsOdMisplaying which developmental task? a. Identity b. Industry c. Integrity d. Intimacy ANS: B Industry is engaging in tasks that can be carried through to completion, learning to compete and cooperate with others, and learning rules. Industry is the developmental task characteristic of the school-age child. Identity is the developmental task of adolescence. Integrity and intimacy are not developmental tasks of childhood. DIF: Cognitive Level: Understand REF: p. 38 TOP: Integrated Process: Nursing Process: Assessment MSC: Area of Client Needs: Health Promotion and Maintenance 14. A nurse is conducting parenting classes for parents of children ranging in ages 2 to 7 years. The parents understand the term egocentrism when they indicate it means: a. selfishness. b. self-centeredness. c. preferring to play alone. d. unable to put self in another’s place. ANS: D TestBankWorld.org According to Piaget, children ages 2 to 7 years are in the preoperational stage of development. Children interpret objects and events not in terms of their general properties but in terms of their relationships or their use to them. This egocentrism does not allow children of this age to put themselves in another’s place. Selfishness, self-centeredness, and preferring to play alone do not describe the concept of egocentricity. DIF: Cognitive Level: Apply REF: p. 45 TOP: Integrated Process: Nursing Process: Evaluation MSC: Area of Client Needs: Health Promotion and Maintenance 15. The nurse is observing parents playing with their 10-month-old child. Which should the nurse recognize as evidence that the child is developing object permanence? a. Looks for the toy that parents hide under the blanket b. Returns the blocks to the same spot on the table c. Recognizes that a ball of clay is the same when flattened out d. Bangs two cubes held in her hands ANS: A Object permanence is the realization that items that leave the visual field still exist. When the infant searches for the toy under the blanket, it is an indication that object permanence has developed. Returning the blocks to the same spot on the table is not an example of object permanence. Recognizing that a ball of clay is the same when flattened out is an example of conservation, which occurs during the concrete operations stage from 7 to 11 years. Banging two cubes together is a simple repetitive activity characteristic of developing a sense of cause and effect. NURSINGDOC.COM DIF: Cognitive Level: Apply REF: p. 45 TOP: Integrated Process: Nursing Process: Assessment MSC: Area of Client Needs: Health Promotion and Maintenance 16. A father tells the nurse that his child is “filling up the house with collections” like seashells, bottle caps, baseball cards, and pennies. What should the nurse recognize the child is developing? a. Object permanence b. Preoperational thinking c. Concrete operational thinking d. Ability to use abstract symbols ANS: C During concrete operations, children develop logical thought processes. They are able to classify, sort, order, and otherwise organize facts about the world. This ability fosters the child’s ability to create collections. Object permanence is the realization that items that leave the visual field still exist. This is a task of infancy and does not contribute to collections. Preoperational thinking is concrete and tangible. Children in this age group cannot reason beyond the observable, and they lack the ability to make deductions or generalizations. Collections are not typical for this developmental level. The ability to use abstract symbols is a characteristic of formal operations, which develops during adolescence. These children can develop and test hypotheses. TestBankWorld.org DIF: Cognitive Level: Understand REF: p. 45 TOP: Integrated Process: Teaching/Learning MSC: Area of Client Needs: Health Promotion and Maintenance 17. A visitor arrives at a daycare center during lunchtime. The preschool children think that every time they have lunch a visitor will arrive. Which preoperational characteristic is being displayed? a. Egocentrism b. Transductive reasoning c. Intuitive reasoning d. Conservation ANS: B Transductive reasoning is when two events occur together, they cause each other. The expectation that every time lunch is served a visitor will arrive is descriptive of transductive reasoning. Egocentrism is the inability to see things from any perspective than their own. Intuitive reasoning (e.g., the stars have to go to bed just as they do) is predominantly egocentric thought. Conservation (able to realize that physical factors such as volume, weight, and number remain the same even though outward appearances are changed) does not occur until school age. DIF: Cognitive Level: Analyze REF: p. 44 TOP: Integrated Process: Nursing Process: Diagnosis MSC: Area of Client Needs: Health Promotion and Maintenance 18. Which behavior is most characteriNsUticRSoIfNtGhTeBc.oCnOcMrete operations stage of cognitive development? a. Progression from reflex activity to imitative behavior b. Inability to put oneself in another’s place c. Increasingly logical and coherent thought processes d. Ability to think in abstract terms and draw logical conclusions ANS: C During the concrete operations stage of development, which occurs approximately between ages 7 and 11 years, increasingly logical and coherent thought processes occur. This is characterized by the child’s ability to classify, sort, order, and organize facts to use in problem solving. The progression from reflex activity to imitative behavior is characteristic of the sensorimotor stage of development. The inability to put oneself in another’s place is characteristic of the preoperational stage of development. The ability to think in abstract terms and draw logical conclusions is characteristic of the formal operations stage of development. DIF: Cognitive Level: Understand REF: p. 45 TOP: Integrated Process: Nursing Process: Assessment MSC: Area of Client Needs: Health Promotion and Maintenance 19. According to Kohlberg, children develop moral reasoning as they mature. Which statement is most characteristic of a preschooler’s stage of moral development? a. Obeying the rules of correct behavior is important. b. Showing respect for authority is important behavior. TestBankWorld.org c. Behavior that pleases others is considered good. d. Actions are determined as good or bad in terms of their consequences. ANS: D Preschoolers are most likely to exhibit characteristics of Kohlberg’s preconventional level of moral development. During this stage, they are culturally oriented to labels of good or bad, right or wrong. Children integrate these concepts based on the physical or pleasurable consequences of their actions. Obeying the rules of correct behavior, showing respect for authority, and engaging in behavior that pleases others are characteristics of Kohlberg’s conventional level of moral development. DIF: Cognitive Level: Understand REF: p. 46 TOP: Integrated Process: Nursing Process: Planning MSC: Area of Client Needs: Health Promotion and Maintenance 20. A school nurse notes that school-age children generally obey the rules at school. The nurse recognizes that the children are displaying which stage of moral development? a. Preconventional b. Conventional c. Postconventional d. Undifferentiated ANS: B Conventional stage of moral development is described as obeying the rules, doing one’s duty, showing respect for authority, and maintaining the social order. This stage is characteristic of school-age children’s behavior. ThNeUpRrSeIcNoGnTvBe.nCtOioMnal stage is characteristic of the toddler and preschool age. At this stage, the child has no concept of the basic moral order that supports being good or bad. The postconventional level is characteristic of an adolescent and occurs at the formal stage of operation. Undifferentiated describes an infant’s understanding of moral development. DIF: Cognitive Level: Analyze REF: p. 46 TOP: Integrated Process: Nursing Process: Evaluation MSC: Area of Client Needs: Health Promotion and Maintenance 21. A nurse observes a toddler playing with sand and water. How should the nurse document this type of play? a. Skill b. Dramatic c. Social-affective d. Sense-pleasure ANS: D The toddler playing with sand and water is engaging in sense-pleasure play. This is characterized by nonsocial situations in which the child is stimulated by objects in the environment. Infants engage in skill play when they persistently demonstrate and exercise newly acquired abilities. Dramatic play is the predominant form of play in the preschool period. Children pretend and fantasize. Social-affective play is one of the first types of play in which infants engage. The infant responds to interactions with people. TestBankWorld.org DIF: Cognitive Level: Apply REF: p. 47 TOP: Integrated Process: Communication and Documentation MSC: Area of Client Needs: Health Promotion and Maintenance 22. In which type of play are children engaged in similar or identical activity, without organization, division of labor, or mutual goal? a. Solitary b. Parallel c. Associative d. Cooperative ANS: C In associative play, no group goal is present. Each child acts according to his or her own wishes. Although the children may be involved in similar activities, no organization, division of labor, leadership assignment, or mutual goal exists. Solitary play describes children playing alone with toys different from those used by other children in the same area. Parallel play describes children playing independently but being among other children. Cooperative play is organized. Children play in a group with other children who play in activities for a common goal. DIF: Cognitive Level: Understand REF: p. 48 TOP: Integrated Process: Nursing Process: Assessment MSC: Area of Client Needs: Health Promotion and Maintenance 23. The nurse observes some childrenNiUnRthSeINpGlaTyBr.oCoOmM. Which play situation exhibits the characteristics of parallel play? a. Kimberly and Amanda sharing clay to each make things b. Brian playing with his truck next to Kristina playing with her truck c. Adam playing a board game with Kyle, Steven, and Erich d. Danielle playing with a music box on her mother’s lap ANS: B Playing with trucks next to each other but not together is an example of parallel play. Both children are engaged in similar activities in proximity to each other; however, they are each engaged in their own play. Sharing clay to make things is characteristic of associative play. Friends playing a board game together is characteristic of cooperative play. A child playing with something by herself on her mother’s lap is an example of solitary play. DIF: Cognitive Level: Analyze REF: p. 48 TOP: Integrated Process: Nursing Process: Assessment MSC: Area of Client Needs: Health Promotion and Maintenance 24. A nurse is planning play activities for school-age children. Which type of a play activity should the nurse plan? a. Solitary b. Parallel c. Associative d. Cooperative TestBankWorld.org ANS: D School-age children engage in cooperative play where it is organized and interactive. Playing a game is a good example of cooperative play. Solitary play is appropriate for infants, parallel play is an activity appropriate for toddlers, and associative play is an activity appropriate for preschool-age children. DIF: Cognitive Level: Apply REF: p. 48 TOP: Integrated Process: Nursing Process: Planning MSC: Area of Client Needs: Health Promotion and Maintenance 25. Which following function of play is a major component of play at all ages? a. Creativity b. Socialization c. Intellectual development d. Sensorimotor activity ANS: D Sensorimotor activity is a major component of play at all ages. Active play is essential for muscle development and allows the release of surplus energy. Through sensorimotor play, children explore their physical world by using tactile, auditory, visual, and kinesthetic stimulation. Creativity, socialization, and intellectual development are each functions of play that are major components at different ages. DIF: Cognitive Level: Understand REF: p. 49 TOP: Integrated Process: Nursing Process: Assessment MSC: Area of Client Needs: Health NPUroRmSoINtioGnTaBn.CdOMMaintenance: Developmental Stages and Transitions 26. Parents are asking the clinic nurse about an appropriate toy for their toddler. Which response by the nurse is appropriate? a. “Your child would enjoy playing a board game.” b. “A toy your child can push or pull would help develop muscles.” c. “An action figure toy would be a good choice.” d. “A 25-piece puzzle would help your child develop recognition of shapes.” ANS: B Toys should be appropriate for the child’s age. A toddler would benefit from a toy he or she could push or pull. The child is too young for a board game, action figure, or 25-piece puzzle. DIF: Cognitive Level: Apply REF: p. 50 TOP: Integrated Process: Teaching/Learning MSC: Area of Client Needs: Health Promotion and Maintenance 27. Which is probably the single most important influence on growth at all stages of development? a. Nutrition b. Heredity c. Culture d. Environment TestBankWorld.org ANS: A Nutrition is the single most important influence on growth. Dietary factors regulate growth at all stages of development, and their effects are exerted in numerous and complex ways. Adequate nutrition is closely related to good health throughout life. Heredity, culture, and environment contribute to the child’s growth and development. However, good nutrition is essential throughout the life span for optimal health. DIF: Cognitive Level: Understand REF: p. 43 TOP: Integrated Process: Nursing Process: Planning MSC: Area of Client Needs: Health Promotion and Maintenance 28. A nurse is counseling an adolescent, in her second month of pregnancy, about the risk of teratogens. The adolescent has understood the teaching if she makes which statement? a. “I will be able to continue taking isotretinoin (Accutane) for my acne.” b. “I can continue to clean my cat’s litter box.” c. “I should avoid any alcoholic beverages.” d. “I will ask my physician to adjust my phenytoin (Dilantin) dosage.” ANS: C Teratogens are agents that cause birth defects when present in the prenatal period. Avoidance of alcoholic beverages is recommended to prevent fetal alcohol syndrome. Isotretinoin (Accutane) and phenytoin (Dilantin) have been shown to have teratogenic effects and should not be taken during pregnancy. Cytomegalovirus, an infectious agent and a teratogen, can be transmitted through cat feces, and cleaning the litter box during pregnancy should be avoided. NURSINGDOC.CO DIF: Cognitive Level: Analyze M REF: p. 52 TOP: Integrated Process: Teaching/Learning MSC: Area of Client Needs: Health Promotion and Maintenance 29. What should the nurse consider when discussing language development with parents of toddlers? a. Sentences by toddlers include adverbs and adjectives. b. The toddler expresses himself or herself with verbs or combination words. c. The toddler uses simple sentences. d. Pronouns are used frequently by the toddler. ANS: B The first parts of speech used are nouns, sometimes verbs (e.g., “go”), and combination words (e.g., “bye-bye”). Responses are usually structurally incomplete during the toddler period. The preschool child begins to use adjectives and adverbs to qualify nouns followed by adverbs to qualify nouns and verbs. Pronouns are not added until the later preschool years. By the time children enter school, they are able to use simple, structurally complete sentences that average five to seven words. DIF: Cognitive Level: Apply REF: p. 46 TOP: Integrated Process: Teaching/Learning MSC: Area of Client Needs: Health Promotion and Maintenance 30. A nurse is observing children at play. Which figure depicts associative play? TestBankWorld.org a. b. c. d. NURSINGTB.COM ANS: C The children depicted in the figure at the carnival ride are demonstrating associative play. They are engaged in similar or identical activities. The child depicted playing alone is demonstrating solitary play. The children playing on the beach depict parallel play. They are playing side by side but are participating in different activities. The children depicted playing a board game are engaging in cooperative play. DIF: Cognitive Level: Analyze REF: p. 48 TOP: Integrated Process: Nursing Process: Evaluation MSC: Area of Client Needs: Health Promotion and Maintenance 31. Which syndrome involves a common sex chromosome defect? a. Down b. Turner c. Marfan d. Hemophilia TestBankWorld.org ANS: B Turner syndrome is caused by an absence of one of the X chromosomes. Down syndrome is caused by trisomy 21, three copies rather than two copies of chromosome 21. Marfan syndrome is a connective tissue disorder inherited in an autosomal dominant pattern. Hemophilia is a disorder of blood coagulation inherited in an X-linked recessive pattern. DIF: Cognitive Level: Understand REF: p. 52 TOP: Integrated Process: Nursing Process: Assessment MSC: Area of Client Needs: Physiologic Integrity: Physiologic Adaptation 32. Turner syndrome is suspected in an adolescent girl with short stature. What is the cause of this syndrome? a. Absence of one of the X chromosomes b. Presence of an incomplete Y chromosome c. Precocious puberty in an otherwise healthy child d. Excess production of both androgens and estrogens ANS: A Turner syndrome is caused by an absence of one of the X chromosomes. Most girls who have this disorder have one X chromosome missing from all cells. No Y chromosome is present in individuals with Turner syndrome. This young woman has 45 rather than 46 chromosomes. DIF: Cognitive Level: Understand REF: p. 52 TOP: Integrated Process: Nursing Process: Assessment MSC: Area of Client Needs: Physiologic Integrity: Physiologic Adaptation NURSINGDOC.COM MULTIPLE RESPONSE 1. Play serves many purposes. In teaching parents about appropriate activities, the nurse should inform them that play serves which of the following function? (Select all that apply.) a. Intellectual development b. Physical development c. Socialization d. Creativity e. Temperament development ANS: A, C, D A common statement is that play is the work of childhood. Intellectual development is enhanced through the manipulation and exploration of objects. Socialization is encouraged by interpersonal activities and learning of social roles. In addition, creativity is developed through the experimentation characteristic of imaginative play. Physical development depends on many factors; play is not one of them. Temperament refers to behavioral tendencies that are observable from the time of birth. The actual behaviors, but not the child’s temperament attributes, may be modified through play. DIF: Cognitive Level: Understand REF: p. 49 TOP: Integrated Process: Nursing Process: Assessment MSC: Area of Client Needs: Health Promotion and Maintenance TestBankWorld.org 2. What factors indicate parents should seek genetic counseling for their child? (Select all that apply.) a. Abnormal newborn screen b. Family history of a hereditary disease c. History of hypertension in the family d. Severe colic as an infant e. Metabolic disorder ANS: A, B, E Factors that are indicative parents should seek genetic counseling for their child include an abnormal newborn screen, family history of a hereditary disease, and a metabolic disorder. A history of hypertension or severe colic as an infant is not an indicator of a genetic disease. DIF: Cognitive Level: Understand REF: p. 53 TOP: Integrated Process: Nursing Process: Assessment MSC: Area of Client Needs: Health Promotion and Maintenance 3. A nurse is preparing to administer a Denver II. Which is a correct statement about the Denver II? (Select all that apply.) a. All items intersected by the age line should be administered. b. There is no correction for a child born preterm. c. The tool is an intelligence test. d. Toddlers and preschoolers should be prepared by presenting the test as a game. e. Presentation of the toys from the kit should be done one at a time. NURSINGDOC.COM ANS: A, D, E To identify “cautions,” all items intersected by the age line are administered. Toddlers and preschoolers should be tested by presenting the Denver II as a game. Because children are easily distracted, perform each item quickly and present only one toy from the kit at a time. Before beginning the screening, ask whether the child was born preterm and correctly calculate the adjusted age. Up to 24 months of age, allowances are made for preterm infants by subtracting the number of weeks of missed gestation from their present age and testing them at the adjusted age. Explain to the parents and child, if appropriate, that the screenings are not intelligence tests but rather are a method of showing what the child can do at a particular age. DIF: Cognitive Level: Apply REF: p. 50 TOP: Integrated Process: Nursing Process: Implementation MSC: Area of Client Needs: Health Promotion and Maintenance COMPLETION 1. The nurse is recording a normal interpretation of a Denver II assessment. The nurse understands that the maximum number of cautions determined for a normal interpretation is . (Record your answer in a whole number.) ANS: TestBankWorld.org 1 Interpretation of normal for a Denver II is no delays and a maximum of one caution. DIF: Cognitive Level: Apply REF: p. 50 TOP: Integrated Process: Nursing Process: Implementation MSC: Area of Client Needs: Health Promotion and Maintenance OTHER 1. Place in order the sequence of cephalocaudal development that the nurse expects to find in the infant. Begin with the first development expected, sequencing to the final. Provide answers using lowercase letters separated by commas (e.g., a, b, c, d). a. Crawl b. Sit unsupported c. Lift head when prone d. Gain complete head control e. Walk ANS: c, d, b, a, e Cephalocaudal development is head-to-tail. Infants achieve structural control of the head before they have control of their trNuUnRkSsIaNnGdTeBx.CtrOeMmities, they lift their head while prone, obtain complete head control, sit unsupported, crawl, and walk sequentially. DIF: Cognitive Level: Apply REF: p. 38 TOP: Integrated Process: Nursing Process: Implementation MSC: Area of Client Needs: Health Promotion and Maintenance TestBankWorld.org Chapter 04: Communication and Physical Assessment of the Child and Family Hockenberry: Wong’s Essentials of Pediatric Nursing, 10th Edition MULTIPLE CHOICE 1. The nurse is seeing an adolescent boy and his parents in the clinic for the first time. What should the nurse do first? a. Introduce self. b. Make family comfortable. c. Explain purpose of interview. d. Give assurance of privacy. ANS: A The first thing that nurses should do is to introduce themselves to the patient and family. Parents and other adults should be addressed with appropriate titles unless they specify a preferred name. During the initial part of the interview, the nurse should include general conversation to help make the family feel at ease. Clarification of the purpose of the interview and the nurse’s role is the next thing that should be done. The interview should take place in an environment as free of distraction as possible. In addition, the nurse should clarify which information will be shared with other members of the health care team and any limits to the confidentiality. DIF: Cognitive Level: Apply REF: p. 57 TOP: Integrated Process: Communication and Documentation MSC: Area of Client Needs: PsychoNsoUcRiaSlIINnGteTgBri.tCyOM 2. Which is most likely to encourage parents to talk about their feelings related to their child’s illness? a. Be sympathetic. b. Use direct questions. c. Use open-ended questions. d. Avoid periods of silence. ANS: C Closed-ended questions should be avoided when attempting to elicit parents’ feelings. Open-ended questions require the parent to respond with more than a brief answer. Sympathy is having feelings or emotions in common with another person rather than understanding those feelings (empathy). Sympathy is not therapeutic in helping the relationship. Direct questions may obtain limited information. In addition, the parent may consider them threatening. Silence can be an effective interviewing tool. It allows sharing of feelings in which two or more people absorb the emotion in depth. Silence permits the interviewee to sort out thoughts and feelings and search for responses to questions. DIF: Cognitive Level: Apply REF: p. 58 TOP: Integrated Process: Communication and Documentation MSC: Area of Client Needs: Psychosocial Integrity TestBankWorld.org 3. Which communication technique should the nurse avoid when interviewing children and their families? a. Using silence b. Using clichés c. Directing the focus d. Defining the problem ANS: B Using stereotyped comments or clichés can block effective communication, and this technique should be avoided. After use of such trite phrases, parents will often not respond. Silence can be an effective interviewing tool. Silence permits the interviewee to sort out thoughts and feelings and search for responses to questions. To be effective, the nurse must be able to direct the focus of the interview while allowing maximal freedom of expression. By using open-ended questions, along with guiding questions, the nurse can obtain the necessary information and maintain the relationship with the family. The nurse and parent must collaborate and define the problem that will be the focus of the nursing intervention. DIF: Cognitive Level: Understand REF: p. 59 TOP: Integrated Process: Communication and Documentation MSC: Area of Client Needs: Psychosocial Integrity 4. What is the single most important factor to consider when communicating with children? a. The child’s physical condition b. Presence or absence of the child’s parent c. The child’s developmental level d. The child’s nonverbal behavioNrsURSINGTB.COM ANS: C The nurse must be aware of the child’s developmental stage to engage in effective communication. The use of both verbal and nonverbal communication should be appropriate to the developmental level. Although the child’s physical condition is a consideration, developmental level is much more important. The parents’ presence is important when communicating with young children but may be detrimental when speaking with adolescents. Nonverbal behaviors will vary in importance, based on the child’s developmental level. DIF: Cognitive Level: Understand REF: p. 60 TOP: Integrated Process: Communication and Documentation MSC: Area of Client Needs: Psychosocial Integrity 5. Which approach would be best to use to ensure a positive response from a toddler? a. Assume an eye-level position and talk quietly. b. Call the toddler’s name while picking him or her up. c. Call the toddler’s name and say, “I’m your nurse.” d. Stand by the toddler, addressing him or her by name. ANS: A TestBankWorld.org It is important that the nurse assume a position at the child’s level when communicating with the child. By speaking quietly and focusing on the child, the nurse should be able to obtain a positive response. The nurse should engage the child and inform the toddler what is going to occur. If the nurse picks up the child without explanation, the child is most likely going to become upset. The toddler may not understand the meaning of the phrase, “I’m your nurse.” If a positive response is desired, the nurse should assume the child’s level when speaking if possible. DIF: Cognitive Level: Apply REF: p. 60 TOP: Integrated Process: Communication and Documentation MSC: Area of Client Needs: Psychosocial Integrity 6. What is an important consideration for the nurse who is communicating with a very young child? a. Speak loudly, clearly, and directly. b. Use transition objects, such as a doll. c. Disguise own feelings, attitudes, and anxiety. d. Initiate contact with child when parent is not present. ANS: B Using a transition object allows the young child an opportunity to evaluate an unfamiliar person (the nurse). This will facilitate communication with a child this age. Speaking in this manner will tend to increase anxiety in very young children. The nurse must be honest with the child. Attempts at deception will lead to a lack of trust. Whenever possible, the parent should be present for interactions with young children. NURSINGDOC.COM DIF: Cognitive Level: Understand REF: p. 61 TOP: Integrated Process: Nursing Process: Planning MSC: Area of Client Needs: Psychosocial Integrity 7. A nurse is preparing to assess a 3-year-old child. What communication technique should the nurse use for this child? a. Focus communication on child. b. Explain experiences of others to child. c. Use easy analogies when possible. d. Assure child that communication is private. ANS: A Because children of this age are able to see things only in terms of themselves, the best approach is to focus communication directly on them. Children should be provided with information about what they can do and how they will feel. With children who are egocentric, experiences of others, analogies, and assurances that the communication is private will not be effective because the child is not capable of understanding. DIF: Cognitive Level: Apply REF: p. 61 TOP: Integrated Process: Communication and Documentation MSC: Area of Client Needs: Psychosocial Integrity TestBankWorld.org 8. A nurse is assigned to four children of different ages. In which age group should the nurse understand that body integrity is a concern? a. Toddler b. Preschooler c. School-age child d. Adolescent ANS: C School-age children have a heightened concern about body integrity. They place importance and value on their bodies and are oversensitive to anything that constitutes a threat or suggestion of injury. Body integrity is not as important a concern to toddlers, preschoolers, or adolescents. DIF: Cognitive Level: Understand REF: p. 61 TOP: Integrated Process: Nursing Process: Planning MSC: Area of Client Needs: Health Promotion and Maintenance 9. An 8-year-old girl asks the nurse how the blood pressure apparatus works. What is the most appropriate nursing action? a. Ask her why she wants to know. b. Determine why she is so anxious. c. Explain in simple terms how it works. d. Tell her she will see how it works as it is used. ANS: C School-age children require explaNnaUtRioSnINs GanTdB.rCeOasMons for everything. They are interested in the functional aspect of all procedures, objects, and activities. It is appropriate for the nurse to explain how equipment works and what will happen to the child. A nurse should respond positively for requests for information about procedures and health information. By not responding, the nurse may be limiting communication with the child. The child is not exhibiting anxiety, just requesting clarification of what will be occurring. The nurse must explain how the blood pressure cuff works so that the child can then observe during the procedure. DIF: Cognitive Level: Apply REF: p. 61 TOP: Integrated Process: Teaching/Learning MSC: Area of Client Needs: Health Promotion and Maintenance 10. When the nurse interviews an adolescent, which is especially important? a. Focus the discussion on the peer group. b. Allow an opportunity to express feelings. c. Emphasize that confidentiality will always be maintained. d. Use the same type of language as the adolescent. ANS: B TestBankWorld.org Adolescents, like all children, need an opportunity to express their feelings. Often they will interject feelings into their words. The nurse must be alert to the words and feelings expressed. Although the peer group is important to this age group, the focus of the interview should be on the adolescent. The nurse should clarify which information will be shared with other members of the health care team and any limits to confidentiality. The nurse should maintain a professional relationship with adolescents. To avoid misinterpretation of words and phrases that the adolescent may use, the nurse should clarify terms frequently. DIF: Cognitive Level: Understand REF: p. 62 TOP: Integrated Process: Communication and Documentation MSC: Area of Client Needs: Psychosocial Integrity 11. The nurse is having difficulty communicating with a hospitalized 6-year-old child. What technique might be most helpful? a. Suggest that the child keep a diary. b. Suggest that the parent read fairy tales to the child. c. Ask the parent if the child is always uncommunicative. d. Ask the child to draw a picture. ANS: D Drawing is one of the most valuable forms of communication. Children’s drawings tell a great deal about them because they are projections of the child’s inner self. It would be difficult for a 6-year-old child who is most likely learning to read to keep a diary. Parents reading fairy tales to the child is a passive activity involving the parent and child. It would not facilitate communication with the nurse. The child is in a stressful situation and is probably uncomfortable with strangers. NURSINGDOC.COM DIF: Cognitive Level: Apply REF: p. 64 TOP: Integrated Process: Communication and Documentation MSC: Area of Client Needs: Psychosocial Integrity 12. The nurse is meeting a 5-year-old child for the first time and would like the child to cooperate during a dressing change. The nurse decides to do a simple magic trick using gauze. How should this action be interpreted? a. Inappropriate, because of child’s age b. A way to establish rapport c. Too distracting, when cooperation is important d. Acceptable, if there is adequate time ANS: B A magic trick or other simple game may help alleviate anxiety for a 5-year-old. It is an excellent method to build rapport and facilitate cooperation during a procedure. Magic tricks appeal to the natural curiosity of young children. The nurse should establish rapport with the child. Failure to do so may cause the procedure to take longer and be more traumatic. DIF: Cognitive Level: Analyze REF: p. 64 TOP: Integrated Process: Communication and Documentation MSC: Area of Client Needs: Psychosocial Integrity TestBankWorld.org 13. The nurse must assess a 10-month-old infant. The infant is sitting on the father’s lap and appears to be afraid of the nurse and of what might happen next. Which initial action by the nurse would be most appropriate? a. Initiate a game of peek-a-boo. b. Ask father to place the infant on the examination table. c. Undress the infant while he is still sitting on his father’s lap. d. Talk softly to the infant while taking him from his father. ANS: A Peek-a-boo is an excellent means of initiating communication with infants while maintaining a safe, nonthreatening distance. The child will most likely become upset if separated from his father. As much of the assessment as possible should be done on the father’s lap. The nurse should have the father undress the child as needed for the examination. DIF: Cognitive Level: Apply REF: p. 62 TOP: Integrated Process: Communication and Documentation MSC: Area of Client Needs: Psychosocial Integrity 14. The nurse is taking a health history on an adolescent. Which best describes how the chief complaint should be determined? a. Ask for detailed listing of symptoms. b. Ask adolescent, “Why did you come here today?” c. Use what adolescent says to determine, in correct medical terminology, what the problem is. d. Interview parent away from adolescent to determine chief complaint. NURSINGDOC.COM ANS: B The chief complaint is the specific reason for the child’s visit to the clinic, office, or hospital. Because the adolescent is the focus of the history, this is an appropriate way to determine the chief complaint. A detailed listing of symptoms will make it difficult to determine the chief complaint. The adolescent should be prompted to tell which symptom caused him to seek help at this time. The chief complaint is usually written in the words that the parent or adolescent uses to describe the reason for seeking help. The parent and adolescent may be interviewed separately, but the nurse should determine the reason the adolescent is seeking attention at this time. DIF: Cognitive Level: Apply REF: p. 62 TOP: Integrated Process: Nursing Process: Assessment MSC: Area of Client Needs: Health Promotion and Maintenance 15. Where in the health history should the nurse describe all details related to the chief complaint? a. Past history b. Chief complaint c. Present illness d. Review of systems ANS: C TestBankWorld.org The history of the present illness is a narrative of the chief complaint from its earliest onset through its progression to the present. The focus of the present illness is on all factors relevant to the main problem, even if they have disappeared or changed during the onset, interval, and present. Past history refers to information that relates to previous aspects of the child’s health, not to the current problem. The chief complaint is the specific reason for the child’s visit to the clinic, office, or hospital. It does not contain the narrative portion describing the onset and progression. The review of systems is a specific review of each body system. DIF: Cognitive Level: Understand REF: p. 64 TOP: Integrated Process: Communication and Documentation MSC: Area of Client Needs: Health Promotion and Maintenance 16. The nurse is interviewing the mother of an infant. She reports, “I had a difficult delivery, and my baby was born preterm.” This information should be recorded under which of the following headings? a. Past history b. Present illness c. Chief complaint d. Review of systems ANS: A The past history refers to information that relates to previous aspects of the child’s health, not to the current problem. The mother’s difficult delivery and prematurity are important parts of the past history of an infant. The history of the present illness is a narrative of the chief complaint from its earliest onset through its progression to the present. Unless the chief complaint is directly related to theNpUrReSmINatGuTriBty.C, OthMis information is not included in the history of present illness. The chief complaint is the specific reason for the child’s visit to the clinic, office, or hospital. It would not include the birth information. The review of systems is a specific review of each body system. It does not include the preterm birth. Sequelae such as pulmonary dysfunction would be included. DIF: Cognitive Level: Understand REF: p. 65 TOP: Integrated Process: Communication and Documentation MSC: Area of Client Needs: Health Promotion and Maintenance 17. Which is most important to document about immunizations in the child’s health history? a. Dosage of immunizations received b. Occurrence of any reaction after an immunization c. The exact date the immunizations were received d. Practitioner who administered the immunizations ANS: B The occurrence of any reaction after an immunization was given is the most important to document in a history because of possible future reactions, especially allergic reactions. Exact dosage of the immunization received may not be recorded on the immunization record. Exact dates are important to obtain but not as important as a history of reaction to an immunization. The practitioner who administered the immunization does not need to be recorded in the health history. A potentially severe physiologic response is the most threatening and most important information to document for safety reasons. TestBankWorld.org DIF: Cognitive Level: Analyze REF: p. 65 TOP: Integrated Process: Communication and Documentation MSC: Area of Client Needs: Health Promotion and Maintenance 18. When interviewing the mother of a 3-year-old child, the nurse asks about developmental milestones such as the age of walking without assistance. How should this question be considered? a. Unnecessary information because child is age 3 years b. An important part of the family history c. An important part of the child’s past history d. An important part of the child’s review of systems ANS: C Information about the attainment of developmental milestones is important to obtain. It provides data about the child’s growth and development that should be included in the past history. Developmental milestones provide important information about the child’s physical, social, and neurologic health and should be included in the history for a 3-year-old child. If pertinent, attainment of milestones by siblings would be included in the family history. The review of systems does not include the developmental milestones. DIF: Cognitive Level: Understand REF: p. 65 TOP: Integrated Process: Communication and Documentation MSC: Area of Client Needs: Health Promotion and Maintenance 19. The nurse is taking a sexual historNyUoRnSaINnGaTdBo.lCeOscMent girl. Which is the best way to determine whether she is sexually active? a. Ask her, “Are you sexually active?” b. Ask her, “Are you having sex with anyone?” c. Ask her, “Are you having sex with a boyfriend?” d. Ask both the girl and her parent whether she is sexually active. ANS: B Asking the adolescent girl whether she is having sex with anyone is a direct question that is well understood. The phrase sexually active is broadly defined and may not provide specific information to the nurse to provide necessary care. The word anyone is preferred to using gender-specific terms such as boyfriend or girlfriend. Because homosexual experimentation may occur, it is preferable to use gender-neutral terms. Questioning about sexual activity should occur when the adolescent is alone. DIF: Cognitive Level: Apply REF: p. 65 TOP: Integrated Process: Nursing Process: Assessment MSC: Area of Client Needs: Health Promotion and Maintenance 20. When doing a nutritional assessment on a Hispanic family, the nurse learns that their diet consists mainly of vegetables, legumes, and starches. How should the nurse assess this diet? a. Indicates they live in poverty b. Is lacking in protein c. May provide sufficient amino acids TestBankWorld.org d. Should be enriched with meat and milk ANS: C The diet that contains vegetable, legumes, and starches may provide sufficient essential amino acids, even though the actual amount of meat or dairy protein is low. Many cultures use diets that contain this combination of foods. It is not indicative of poverty. Combinations of foods contain the essential amino acids necessary for growth. A dietary assessment should be done, but many vegetarian diets are sufficient for growth. DIF: Cognitive Level: Understand REF: p. 66 TOP: Integrated Process: Nursing Process: Assessment MSC: Area of Client Needs: Health Promotion and Maintenance 21. Which following parameters correlates best with measurements of the body’s total protein stores? a. Height b. Weight c. Skinfold thickness d. Upper arm circumference ANS: D Upper arm circumference is correlated with measurements of total muscle mass. Muscle serves as the body’s major protein reserve and is considered an index of the body’s protein stores. Height is reflective of past nutritional status. Weight is indicative of current nutritional status. Skinfold thickness is a measurement of the body’s fat content. NURSINGDOC.COM DIF: Cognitive Level: Understand REF: p. 72 TOP: Integrated Process: Nursing Process: Assessment MSC: Area of Client Needs: Health Promotion and Maintenance 22. A nurse is preparing to perform a physical assessment on a toddler. Which approach should the nurse use for this child? a. Always proceed in a head-to-toe direction. b. Perform traumatic procedures first. c. Use minimal physical contact initially. d. Demonstrate use of equipment. ANS: C Parents can remove clothing, and the child can remain on the parent’s lap. The nurse should use minimal physical contact initially to gain the child’s cooperation. The head-to-toe assessment can be done in older children but usually must be adapted in younger children. Traumatic procedures should always be performed last. These will most likely upset the child and inhibit cooperation. The nurse should introduce the equipment slowly. The child can inspect the equipment, but demonstrations are usually too complex for toddlers. DIF: Cognitive Level: Apply REF: p. 77 TOP: Integrated Process: Nursing Process: Planning MSC: Area of Client Needs: Health Promotion and Maintenance TestBankWorld.org 23. The nurse is preparing to perform a physical assessment on a 10-year-old girl. The nurse gives her the option of her mother either staying in the room or leaving. How should this action be interpreted? a. Appropriate because of child’s age b. Appropriate because mother would be uncomfortable making decisions for child c. Inappropriate because of child’s age d. Inappropriate because child is same sex as mother ANS: A The older school-age child should be given the option of having the parent present or not. During the examination, the nurse should respect the child’s need for privacy. Although the question was appropriate for the child’s age, the mother is responsible for making decisions for the child. It is appropriate because of the child’s age. During the examination, the nurse must respect the child’s privacy. The child should help determine who is present during the examination. DIF: Cognitive Level: Apply REF: p. 77 TOP: Integrated Process: Nursing Process: Assessment MSC: Area of Client Needs: Health Promotion and Maintenance 24. A nurse is counseling parents of a child beginning to show signs of being overweight. The nurse accurately relates which body mass index (BMI)-for-age percentile indicates a risk for being overweight? a. 10th percentile b. 9th percentile c. 85th percentile NURSINGDOC.COM d. 95th percentile ANS: C Children who have BMI-for-age greater than or equal to the 85th percentile and less than the 95th percentile are at risk for being overweight. Children in the 9th and 10th percentiles are within normal limits. Children who are greater than or equal to the 95th percentile are considered overweight. DIF: Cognitive Level: Apply REF: p. 79 TOP: Integrated Process: Nursing Process: Implementation MSC: Area of Client Needs: Health Promotion and Maintenance 25. The nurse is using the Centers for Disease Control and Prevention (CDC) growth chart for an African-American child. Which statement should the nurse consider? a. This growth chart should not be used. b. Growth patterns of African-American children are the same as for all other ethnic groups. c. A correction factor is necessary when the CDC growth chart is used for non-Caucasian ethnic groups. d. The CDC charts are accurate for US African-American children. ANS: D TestBankWorld.org The CDC growth charts can serve as reference guides for all racial or ethnic groups. US African-American children were included in the sample population. The growth chart can be used with the perspective that different groups of children have varying normal distributions on the growth curves. No correction factor exists. DIF: Cognitive Level: Understand REF: p. 77 TOP: Integrated Process: Nursing Process: Assessment MSC: Area of Client Needs: Health Promotion and Maintenance 26. Which tool measures body fat most accurately? a. Stadiometer b. Calipers c. Cloth tape measure d. Paper or metal tape measure ANS: B Calipers are used to measure skinfold thickness, which is an indicator of body fat content. Stadiometers are used to measure height. Cloth tape measures should not be used because they can stretch. Paper or metal tape measures can be used for recumbent lengths and other body measurements that must be made. DIF: Cognitive Level: Understand REF: p. 80 TOP: Integrated Process: Nursing Process: Assessment MSC: Area of Client Needs: Health Promotion and Maintenance 27. The nurse is using calipers to meaNsuUrReSsIkNiGnTfoBl.dCOthMickness over the triceps muscle in a school-age child. What is the purpose of doing this? a. To measure body fat b. To measure muscle mass c. To determine arm circumference d. To determine accuracy of weight measurement ANS: A Measurement of skinfold thickness is an indicator of body fat. Arm circumference is an indirect measure of muscle mass. The accuracy of weight measurement should be verified with a properly balanced scale. Body fat is just one indicator of weight. DIF: Cognitive Level: Remember REF: p. 80 TOP: Integrated Process: Nursing Process: Assessment MSC: Area of Client Needs: Health Promotion and Maintenance 28. A nurse notes that a 10-month-old infant has a larger head circumference than chest. The nurse interprets this as a normal finding because the head and chest circumference become equal at which age? a. 1 month b. 6 to 9 months c. 1 to 2 years d. to 3 years TestBankWorld.org ANS: C Head circumference begins larger than chest circumference. Between ages 1 and 2 years, they become approximately equal. Head circumference is larger than chest circumference before age 1. Chest circumference is larger than head circumference at to 3 years. DIF: Cognitive Level: Remember REF: p. 80 TOP: Integrated Process: Nursing Process: Assessment MSC: Area of Client Needs: Health Promotion and Maintenance 29. Which would be best for the nurse to use when determining the temperature of a preterm infant under a radiant heater? a. Axillary sensor b. Tympanic membrane sensor c. Rectal mercury glass thermometer d. Rectal electronic thermometer ANS: A The axillary sensor measures the infrared heat energy radiating from the axilla. It can be used on wet skin, in incubators, or under radiant warmers. Ear thermometry does not show sufficient correlation with established methods of measurement. It should not be used when body temperature must be assessed with precision. Mercury thermometers should never be used. The release of mercury, should the thermometer be broken, can cause harmful vapors. Rectal temperatures should be avoided unless no other suitable way exists for the temperature to be measured. DIF: Cognitive Level: Apply NURSINRGETFB:.CpO.M85 TOP: Integrated Process: Nursing Process: Assessment MSC: Area of Client Needs: Health Promotion and Maintenance 30. What is the earliest age at which a satisfactory radial pulse can be taken in children? a. 1 year b. 2 years c. 3 years d. 6 years ANS: B Satisfactory radial pulses can be used in children older than 2 years. In infants and young children, the apical pulse is more reliable. The apical pulse can be used for assessment at these ages. DIF: Cognitive Level: Remember REF: p. 103 TOP: Integrated Process: Nursing Process: Assessment MSC: Area of Client Needs: Health Promotion and Maintenance 31. Pulses can be graded according to certain criteria. Which is a description of a normal pulse? a. 0 b. +1 c. +2 d. +3 TestBankWorld.org ANS: D A normal pulse is described as +3. A pulse that is easy to palpate and not easily obliterated with pressure is considered normal. A pulse graded 0 is not palpable. A pulse graded +1 is difficult to palpate, thready, weak, and easily obliterated with pressure. A pulse graded +2 is difficult to palpate and may be easily obliterated with pressure. DIF: Cognitive Level: Remember REF: p. 85 TOP: Integrated Process: Nursing Process: Assessment MSC: Area of Client Needs: Health Promotion and Maintenance: Techniques of Physical Assessment 32. Where is the best place to observe for the presence of petechiae in dark-skinned individuals? a. Face b. Buttocks c. Oral mucosa d. Palms and soles ANS: C Petechiae, small distinct pinpoint hemorrhages, are difficult to see in dark skin unless they are in the mouth or conjunctiva. DIF: Cognitive Level: Remember REF: p. 89 TOP: Integrated Process: Nursing Process: Assessment MSC: Area of Client Needs: Health Promotion and Maintenance: Techniques of Physical Assessment 33. The nurse observes yellow staining in the sclera of eyes, soles of feet, and palms of hands. How should the nurse document tNheUsReSfIiNnGdiTnBg.sC?OM a. Normal b. Erythema c. Jaundice d. Ecchymosis ANS: C Jaundice is defined as the yellow staining of the skin, usually by bile pigments. Yellow staining is not a normal appearance of the skin. Erythema is redness that results from increased blood flow to the area. Ecchymosis is large, diffuse areas, usually black and blue, caused by hemorrhage of blood into the skin. DIF: Cognitive Level: Understand REF: p. 89 TOP: Integrated Process: Nursing Process: Assessment MSC: Area of Client Needs: Health Promotion and Maintenance 34. When palpating the child’s cervical lymph nodes, the nurse notes that they are tender, enlarged, and warm. What is the best explanation for this? a. Some form of cancer b. Local scalp infection common in children c. Infection or inflammation distal to the site d. Infection or inflammation close to the site ANS: D TestBankWorld.org Small nontender nodes are normal. Tender, enlarged, and warm lymph nodes may indicate infection or inflammation close to their location. Tender lymph nodes are not usually indicative of cancer. A scalp infection would usually not cause inflamed lymph nodes. The lymph nodes close to the site of inflammation or infection would be inflamed. DIF: Cognitive Level: Analyze REF: p. 89 TOP: Integrated Process: Nursing Process: Assessment MSC: Area of Client Needs: Health Promotion and Maintenance 35. During a routine health assessment, the nurse notes that an 8-month-old infant has significant head lag. Which is the nurse’s most appropriate action? a. Teach parents appropriate exercises. b. Recheck head control at next visit. c. Refer child for further evaluation. d. Refer child for further evaluation if anterior fontanel is still open. ANS: C Significant head lag after age 6 months strongly indicates cerebral injury and is referred for further evaluation. Reduction of head lag is part of normal development. Exercises will not be effective. The lack of achievement of this developmental milestone must be evaluated. DIF: Cognitive Level: Apply REF: p. 89 TOP: Integrated Process: Nursing Process: Assessment MSC: Area of Client Needs: Health Promotion and Maintenance 36. The nurse has just started assessinNgUaRySoINuGngTBc.hCiOldMwho is febrile and appears very ill. There is hyperextension of the child’s head (opisthotonos) with pain on flexion. Which is the most appropriate action? a. Refer for immediate medical evaluation. b. Continue assessment to determine cause of neck pain. c. Ask parent when neck was injured. d. Record “head lag” on assessment record, and continue assessment of child. ANS: A Hyperextension of the child’s head with pain on flexion is indicative of meningeal irritation and needs immediate evaluation; it is not descriptive of head lag. The pain is indicative of meningeal irritation. No indication of injury is present. DIF: Cognitive Level: Apply REF: p. 90 TOP: Integrated Process: Nursing Process: Assessment MSC: Area of Client Needs: Health Promotion and Maintenance 37. At what age should the nurse expect the anterior fontanel to close? a. 2 months b. 2 to 4 months c. 6 to 8 months d. 12 to 18 months ANS: D TestBankWorld.org The anterior fontanel normally closes between ages 12 and 18 months. Two to 8 months is too early. The expected closure of the anterior fontanel occurs between ages 12 and 18 months; if it closes between ages 2 and 8 months, the child should be referred for further evaluation. DIF: Cognitive Level: Remember REF: p. 90 TOP: Integrated Process: Nursing Process: Assessment MSC: Area of Client Needs: Health Promotion and Maintenance 38. During a funduscopic examination of a school-age child, the nurse notes a brilliant, uniform red reflex in both eyes. How should the nurse interpret this finding? a. Normal finding b. Abnormal finding, so child needs referral to ophthalmologist c. Sign of possible visual defect, so child needs vision screening d. Sign of small hemorrhages, which will usually resolve spontaneously ANS: A A brilliant, uniform red reflex is an important normal finding. It rules out many serious defects of the cornea, aqueous chamber, lens, and vitreous chamber. DIF: Cognitive Level: Understand REF: p. 91 TOP: Integrated Process: Nursing Process: Assessment MSC: Area of Client Needs: Health Promotion and Maintenance 39. Parents of a newborn are concerned because the infant’s eyes often “look crossed” when the infant is looking at an object. The nurse’s response is that this is normal based on the knowledge that binocularity is norNmUaRllSyINpGreTsBe.nCtObMy what age? a. 1 month b. 3 to 4 months c. 6 to 8 months d. 12 months ANS: B Binocularity is usually achieved by ages 3 to 4 months. 1 month is too young. If binocularity is not achieved by ages 6 to 12 months, the child must be observed for strabismus. DIF: Cognitive Level: Understand REF: p. 91 TOP: Integrated Process: Nursing Process: Assessment MSC: Area of Client Needs: Health Promotion and Maintenance 40. A nurse is preparing to test a school-age child’s vision. Which eye chart should the nurse use? a. Denver Eye Screening Test b. Allen picture card test c. Ishihara vision test d. Snellen letter chart ANS: D The Snellen letter chart, which consists of lines of letters of decreasing size, is the most frequently used test for visual acuity for school-age children. Single cards (Denver—letter E; Allen—pictures) are used for children ages 2 years and older who are unable to use the Snellen letter chart. The Ishihara vision test is used for color vision. TestBankWorld.org DIF: Cognitive Level: Apply REF: p. 92 TOP: Integrated Process: Nursing Process: Assessment MSC: Area of Client Needs: Health Promotion and Maintenance 41. Which is the most appropriate vision acuity test for a child who is in preschool? a. Cover test b. Ishihara test c. HOTV chart d. Snellen letter chart ANS: C The HOTV test consists of a wall chart of these letters. The child is asked to point to a corresponding card when the examiner selects one of the letters on the chart. The cover test determines ocular alignment. The Ishihara test is used for the detection of color blindness. The Snellen letter chart is usually used for older children. DIF: Cognitive Level: Understand REF: p. 93 TOP: Integrated Process: Nursing Process: Planning MSC: Area of Client Needs: Health Promotion and Maintenance 42. The nurse is testing an infant’s visual acuity. By what age should the infant be able to fix on and follow a target? a. 1 month b. 1 to 2 months c. 3 to 4 months NURSINGDOC.COM d. 6 months ANS: C Visual fixation and following a target should be present by ages 3 to 4 months. One to 2 months is too young for this developmental milestone. If the infant is not able to fix and follow by 6 months, further ophthalmologic evaluation is needed. DIF: Cognitive Level: Understand REF: p. 93 TOP: Integrated Process: Nursing Process: Problem Identification MSC: Area of Client Needs: Health Promotion and Maintenance 43. Where is the appropriate placement of a tongue blade for assessment of the mouth and throat? a. Center back area of tongue b. Side of the tongue c. Against the soft palate d. On the lower jaw ANS: B Side of the tongue is the correct position. It avoids the gag reflex yet allows visualization. Placement in the center back area of the tongue will elicit the gag reflex. Against the soft palate and on the lower jaw are not appropriate places for the tongue blade. DIF: Cognitive Level: Understand REF: p. 98 TOP: Integrated Process: Nursing Process: Assessment TestBankWorld.org MSC: Area of Client Needs: Health Promotion and Maintenance: Techniques of Physical Assessment 44. What is an appropriate screening test for hearing that can be administered by the nurse to a 5-year-old child? a. The Rinne test b. The Weber test c. Conventional audiometry d. Eliciting the startle reflex ANS: C Conventional audiometry is a behavioral test that measures auditory thresholds in response to speech and frequency-specific stimuli presented through earphones. The Rinne and Weber tests measure bone conduction of sound. Eliciting the startle reflex may be useful in infants. DIF: Cognitive Level: Understand REF: p. 97 TOP: Integrated Process: Nursing Process: Assessment MSC: Area of Client Needs: Health Promotion and Maintenance 45. What type of breath sound is normally heard over the entire surface of the lungs except for the upper intrascapular area and the area beneath the manubrium? a. Vesicular b. Bronchial c. Adventitious d. Bronchovesicular ANS: A NURSINGDOC.COMVesicular breath sounds are heard over the entire surface of lungs, with the exception of the upper intrascapular area and the area beneath the manubrium. Bronchial breath sounds are heard only over the trachea near the suprasternal notch. Adventitious breath sounds are not usually heard over the chest. These sounds occur in addition to normal or abnormal breath sounds. Bronchovesicular breath sounds are heard over the manubrium and in the upper intrascapular regions where trachea and bronchi bifurcate. DIF: Cognitive Level: Remember REF: p. 101 TOP: Integrated Process: Nursing Process: Assessment MSC: Area of Client Needs: Health Promotion and Maintenance 46. A nurse is assessing a patient admitted for an asthma exacerbation. Which breath sounds does the nurse expect to assess? a. Rubs b. Rattles c. Wheezes d. Crackles ANS: C TestBankWorld.org Asthma causes bronchoconstriction and narrowed passageways. Wheezes are produced as air passes through narrowed passageways. Rubs are the sound created by the friction of one surface rubbing over another. Pleural friction rub is caused by inflammation of the pleural space. Rattles is the term formerly used for crackles. Crackles are the sounds made when air passes through fluid or moisture. DIF: Cognitive Level: Analyze REF: p. 102 TOP: Integrated Process: Nursing Process: Assessment MSC: Area of Client Needs: Health Promotion and Maintenance 47. While caring for a critically ill child, the nurse observes that respirations are gradually increasing in rate and depth, with periods of apnea. What pattern of respiration will the nurse document? a. Dyspnea b. Tachypnea c. Cheyne-Stokes respirations d. Seesaw (paradoxic) respirations ANS: C Cheyne-Stokes respirations are a pattern of respirations that gradually increase in rate and depth, with periods of apnea. Dyspnea is defined as distress during breathing. Tachypnea is an increased respiratory rate. In seesaw respirations, the chest falls on inspiration and rises on expiration. DIF: Cognitive Level: Understand REF: p. 102 TOP: Integrated Process: CommuniNcaUtiRoSnINanGdTDBo.CcOumMentation MSC: Area of Client Needs: Health Promotion and Maintenance 48. How does the nurse assess a child’s capillary refill time? a. Inspecting the chest b. Auscultating the heart c. Palpating the apical pulse d. Palpating the skin to produce a slight blanching ANS: D Capillary refill time is assessed by pressing lightly on the skin to produce blanching, and then noting the amount of time it takes for the blanched area to refill. Inspecting the chest, auscultating the heart, and palpating the apical pulse will not provide an assessment of capillary refill time. DIF: Cognitive Level: Understand REF: p. 102 TOP: Integrated Process: Nursing Process: Assessment MSC: Area of Client Needs: Health Promotion and Maintenance 49. A nurse is assessing a child with an unrepaired ventricular septal defect. Which heart sound does the nurse expect to assess? a. S3 b. S4 c. Murmur TestBankWorld.org d. Physiologic splitting ANS: C Murmurs are the sounds that are produced in the heart chambers or major arteries from the back-and-forth flow of blood. These are the sounds expected to be heard in a child with a ventricular septal defect because of the abnormal opening between the ventricles. S3 is a normal heart sound sometimes heard in children. S4 is rarely heard as a normal heart sound. If heard, medical evaluation is required. Physiologic splitting is the distinction of the two sounds in S2, which widens on inspiration. It is a significant normal finding. DIF: Cognitive Level: Analyze REF: p. 103 TOP: Integrated Process: Nursing Process: Assessment MSC: Area of Client Needs: Health Promotion and Maintenance 50. The nurse has determined the rate of both the child’s radial pulse and heart. What is the normal finding when comparing the two rates? a. Are the same b. Differ, with heart rate faster c. Differ, with radial pulse faster d. Differ, depending on quality and intensity ANS: A Pulses are the fluid wave through the blood vessel as a result of each heartbeat. Therefore, they should be the same. DIF: Cognitive Level: Understand NURSINRGETFB:.CpO.M103 TOP: Integrated Process: Nursing Process: Assessment MSC: Area of Client Needs: Health Promotion and Maintenance 51. A nurse is performing an otoscopic exam on a school-age child. Which direction should the nurse pull the pinna for this age of child? a. Up and back b. Down and back c. Straight back d. Straight up ANS: A With older children, usually those older than 3 years of age, the canal curves downward and forward. Therefore, pull the pinna up and back during otoscopic examinations. In infants, the canal curves upward. Therefore, pull the pinna down and back to straighten the canal. Pulling the pinna straight back or straight up will not open the inner ear canal. DIF: Cognitive Level: Understand REF: p. 95 TOP: Integrated Process: Nursing Process: Assessment MSC: Area of Client Needs: Health Promotion and Maintenance 52. The nurse has a 2-year-old boy sit in “tailor” position during palpation for the testes. What is the rationale for this position? a. It prevents cremasteric reflex. b. Undescended testes can be palpated. TestBankWorld.org c. This tests the child for an inguinal hernia. d. The child does not yet have a need for privacy. ANS: A The tailor position stretches the muscle responsible for the cremasteric reflex. This prevents its contraction, which pulls the testes into the pelvic cavity. Undescended testes cannot be predictably palpated. Inguinal hernias are not detected by this method. This position is used for inhibiting the cremasteric reflex. Privacy should always be provided for children. DIF: Cognitive Level: Understand REF: p. 107 TOP: Integrated Process: Nursing Process: Assessment MSC: Area of Client Needs: Health Promotion and Maintenance: Techniques of Physical Assessment 53. During examination of a toddler’s extremities, the nurse notes that the child is bowlegged. What should the nurse recognize regarding this finding? a. Abnormal and requires further investigation b. Abnormal unless it occurs in conjunction with knock-knee c. Normal if the condition is unilateral or asymmetric d. Normal because the lower back and leg muscles are not yet well developed ANS: D Lateral bowing of the tibia (bowlegged) is common in toddlers when they begin to walk. It usually persists until all their lower back and leg muscles are well developed. Further evaluation is needed if it persists beyond ages 2 to 3 years, especially in African-American children. NURSINGDOC.COM DIF: Cognitive Level: Understand REF: p. 108 TOP: Integrated Process: Nursing Process: Problem Identification MSC: Area of Client Needs: Health Promotion and Maintenance 54. At about what age does the Babinski sign disappear? a. 4 months b. 6 months c. 1 year d. 2 years ANS: C The presence of the Babinski reflex after about age 1 year, when walking begins, is abnormal. Four to 6 months is too young for the disappearance of the Babinski reflex. Persistence of the Babinski reflex requires further evaluation. DIF: Cognitive Level: Understand REF: p. 109 TOP: Integrated Process: Nursing Process: Assessment MSC: Area of Client Needs: Health Promotion and Maintenance 55. A 5-year-old girl is having a checkup before starting kindergarten. The nurse asks her to do the “finger-to-nose” test. What is the nurse testing for? a. Deep tendon reflexes b. Cerebellar function c. Sensory discrimination TestBankWorld.org d. Ability to follow directions ANS: B The finger-to-nose test is an indication of cerebellar function. This test checks balance and coordination. Each deep tendon reflex is tested separately. Each sense is tested separately. Although this test enables the nurse to evaluate the child’s ability to follow directions, it is used primarily for cerebellar function. DIF: Cognitive Level: Apply REF: p. 109 TOP: Integrated Process: Nursing Process: Assessment MSC: Area of Client Needs: Health Promotion and Maintenance 56. Which figure depicts a nurse performing a test for the triceps reflex? a. b. NURSINGTB.COM c. TestBankWorld.org d. ANS: A To test the triceps reflex, the child is placed supine, with the forearm resting over the chest and the triceps tendon is struck with the reflex hammer. The other figures depict tests for biceps reflex (slightly above the antecubital space) patellar (knee), and Achilles (behind the foot). DIF: Cognitive Level: Analyze REF: p. 110 TOP: Integrated Process: Nursing Process: Assessment MSC: Area of Client Needs: Health Promotion and Maintenance MULTIPLE RESPONSE NURSINGDOC.COM 1. The nurse must check vital signs on a 2-year-old boy who is brought to the clinic for his 24-month checkup. What criteria should the nurse use in determining the appropriate-size blood pressure cuff? (Select all that apply.) a. The cuff is labeled “toddler.” b. The cuff bladder width is approximately 40% of the circumference of the upper arm. c. The cuff bladder length covers 80% to 100% of the circumference of the upper arm. d. The cuff bladder covers 50% to 66% of the length of the upper arm. ANS: B, C Research has demonstrated that cuff selection with a bladder width that is 40% of the arm circumference will usually have a bladder length that is 80% to 100% of the upper arm circumference. This size cuff will most accurately reflect measured radial artery pressure. The name of the cuff is a representative size that may not be suitable for any individual child. Choosing a cuff by limb circumference more accurately reflects arterial pressure than choosing a cuff by length. DIF: Cognitive Level: Understand REF: p. 86 TOP: Integrated Process: Nursing Process: Assessment MSC: Area of Client Needs: Health Promotion and Maintenance TestBankWorld.org 2. Which of the following data would be included in a health history? (Select all that apply.) a. Review of systems b. Physical assessment c. Sexual history d. Growth measurements e. Nutritional assessment f. Family medical history ANS: A, C, E, F The review of systems, sexual history, nutritional assessment, and family medical history are part of the health history. Physical assessment and growth measurements are components of the physical examination. DIF: Cognitive Level: Apply REF: p. 64 TOP: Integrated Process: Nursing Process: Assessment MSC: Area of Client Needs: Health Promotion and Maintenance 3. A nurse is performing an assessment on a school-age child. Which findings suggest the child is getting an excess of vitamin A? (Select all that apply.) a. Delayed sexual development b. Edema c. Pruritus d. Jaundice e. Paresthesia ANS: A, C, D NURSINGDOC.COM Excess vitamin A can cause delayed sexual development, pruritus, and jaundice. Edema is seen with excess sodium. Paresthesia occurs with excess riboflavin. DIF: Cognitive Level: Apply REF: p. 73 TOP: Integrated Process: Nursing Process: Assessment MSC: Area of Client Needs: Health Promotion and Maintenance 4. A nurse is planning to use an interpreter during a health history interview of a non-English speaking patient and family. Which nursing care guidelines should the nurse include when using an interpreter? (Select all that apply.) a. Elicit one answer at a time. b. Interrupt the interpreter if the response from the family is lengthy. c. Comments to the interpreter about the family should be made in English. d. Arrange for the family to speak with the same interpreter, if possible. e. Introduce the interpreter to the family. ANS: A, D, E TestBankWorld.org When using an interpreter, the nurse should pose questions to elicit only one answer at a time, such as: “Do you have pain?” rather than “Do you have any pain, tiredness, or loss of appetite?” Refrain from interrupting family members and the interpreter while they are conversing. Introduce the interpreter to family and allow some time before the interview for them to become acquainted. Refrain from interrupting family members and the interpreter while they are conversing. Avoid commenting to the interpreter about family members because they may understand some English. DIF: Cognitive Level: Apply REF: p. 60 TOP: Integrated Process: Nursing Process: Assessment MSC: Area of Client Needs: Health Promotion and Maintenance OTHER 1. What is the correct sequence used when performing an abdominal assessment? Begin with the first technique and end with the last. Provide answer using lowercase letters separated by commas (e.g., a, b, c, d). a. Auscultation b. Palpation c. Inspection d. Percussion ANS: c, a, d, b NURSINGDOC.COM The correct order of abdominal examination is inspection, auscultation, percussion, and palpation. Palpation is always performed last because it may distort the normal abdominal sounds. DIF: Cognitive Level: Apply REF: p. 104 TOP: Integrated Process: Nursing Process: Assessment MSC: Area of Client Needs: Health Promotion and Maintenance TestBankWorld.org Chapter 05: Pain Assessment and Management in Children Hockenberry: Wong’s Essentials of Pediatric Nursing, 10th Edition MULTIPLE CHOICE 1. A 2-year-old child has been returned to the nursing unit after an inguinal hernia repair. Which pain assessment tool should the nurse use to assess this child for the presence of pain? a. FACES pain rating tool b. Numeric scale c. Oucher scale d. FLACC tool ANS: D A behavioral pain tool should be used when the child is preverbal or doesn’t have the language skills to express pain. The FLACC (face, legs, activity, cry, consolability) tool should be used with a 2-year-old child. The FACES, numeric, and Oucher scales are all self-report pain rating tools. Self-report measures are not sufficiently valid for children younger than 3 years of age because many are not able to accurately self-report their pain. DIF: Cognitive Level: Apply REF: p. 115 TOP: Integrated Process: Nursing Process: Assessment MSC: Area of Client Needs: Physiologic Integrity 2. The nurse is caring for a 6-year-old girl who had surgery 12 hours ago. The child tells the nurse that she does not have pain,NbUuRt SaIfNeGwTBm.CinOuMtes later she tells her parents that she does. Which should the nurse consider when interpreting this? a. Truthful reporting of pain should occur by this age. b. Inconsistency in pain reporting suggests that pain is not present. c. Children use pain experiences to manipulate their parents. d. Children may be experiencing pain even though they deny it to the nurse. ANS: D Children may deny pain to the nurse because they fear receiving an injectable analgesic or because they believe they deserve to suffer as a punishment for a misdeed. They may refuse to admit pain to a stranger but readily tell a parent. Truthfully reporting pain and inconsistency in pain reporting suggesting that pain is not present are common fallacies about children and pain. Pain is whatever the experiencing person says it is, whenever the person says it exists. Pain would not be questioned in an adult 12 hours after surgery. DIF: Cognitive Level: Analyze REF: p. 116 TOP: Integrated Process: Nursing Process: Planning MSC: Area of Client Needs: Physiologic Integrity 3. A nurse is gathering a history on a school-age child admitted for a migraine headache. The child states, “I have been getting a migraine every 2 or 3 months for the last year.” The nurse documents this as which type of pain? a. Acute b. Chronic TestBankWorld.org c. Recurrent d. Subacute ANS: C Pain that is episodic and reoccurs is defined as recurrent pain. The time frame within which episodes of pain recur is at least 3 months. Recurrent pain in children includes migraine headache, episodic sickle cell pain, recurrent abdominal pain (RAP), and recurrent limb pain. Acute pain is pain that lasts for less than 3 months. Chronic pain is pain that lasts, on a daily basis, for more than 3 months. Subacute is not a term for documenting type of pain. DIF: Cognitive Level: Understand REF: p. 118 TOP: Integrated Process: Communication and Documentation MSC: Area of Client Needs: Physiologic Integrity 4. Physiologic measurements in children’s pain assessment are: a. the best indicator of pain in children of all ages. b. essential to determine whether a child is telling the truth about pain. c. of most value when children also report having pain. d. of limited value as sole indicator of pain. ANS: D Physiologic manifestations of pain may vary considerably, not providing a consistent measure of pain. Heart rate may increase or decrease. The same signs that may suggest fear, anxiety, or anger also indicate pain. In chronic pain, the body adapts, and these signs decrease or stabilize. Physiologic measurements are of limited value and must be viewed in the context of a pain-rating scale, behavioral assNesUsRmSeInNtG, TanBd.CpOaMrental report. When the child states that pain exists, it does. That is the truth. DIF: Cognitive Level: Understand REF: p. 119 TOP: Integrated Process: Nursing Process: Assessment MSC: Area of Client Needs: Physiologic Integrity 5. Nonpharmacologic strategies for pain management: a. may reduce pain perception. b. make pharmacologic strategies unnecessary. c. usually take too long to implement. d. trick children into believing they do not have pain. ANS: A Nonpharmacologic techniques provide coping strategies that may help reduce pain perception, make the pain more tolerable, decrease anxiety, and enhance the effectiveness of analgesics. Nonpharmacologic techniques should be learned before the pain occurs. With severe pain, it is best to use both pharmacologic and nonpharmacologic measures for pain control. The nonpharmacologic strategy should be matched with the child’s pain severity and taught to the child before the onset of the painful experience. Some of the techniques may facilitate the child’s experience with mild pain, but the child will still know the discomfort was present. DIF: Cognitive Level: Understand REF: p. 124 TOP: Integrated Process: Nursing Process: Planning TestBankWorld.org MSC: Area of Client Needs: Physiologic Integrity 6. Which drug is usually the best choice for patient-controlled analgesia (PCA) for a child in the immediate postoperative period? a. Codeine b. Morphine c. Methadone d. Meperidine ANS: B The most commonly prescribed medications for PCA are morphine, hydromorphone, and fentanyl. Parenteral use of codeine is not recommended. Methadone is not available in parenteral form in the United States. Meperidine is not used for continuous and extended pain relief. DIF: Cognitive Level: Remember REF: p. 129 TOP: Integrated Process: Nursing Process: Implementation MSC: Area of Client Needs: Physiologic Integrity 7. A lumbar puncture is needed on a school-age child. What should the nurse apply to provide the most appropriate analgesia during this procedure? a. TAC (tetracaine-adrenaline-cocaine) 15 minutes b. Transdermal fentanyl (Duragesic) patch immediately c. EMLA (eutectic mixture of local anesthetics) 1 hour d. EMLA (eutectic mixture of local anesthetics) 30 minutes NURSINGDOC.COM ANS: C EMLA is an effective analgesic agent when applied to the skin 60 minutes before a procedure. It eliminates or reduces the pain from most procedures involving skin puncture. TAC provides skin anesthesia about 15 minutes after application to nonintact skin. The gel can be placed on the wound for suturing. Transdermal fentanyl patches are useful for continuous pain control, not rapid pain control. For maximal effectiveness, EMLA must be applied approximately 60 minutes in advance. DIF: Cognitive Level: Apply REF: p. 143 TOP: Integrated Process: Nursing Process: Implementation MSC: Area of Client Needs: Physiologic Integrity 8. The nurse is caring for a child receiving intravenous (IV) morphine for severe postoperative pain. The nurse observes a slower respiratory rate, and the child cannot be aroused. What is the priority nursing action? a. Administer naloxone (Narcan) b. Discontinue IV infusion c. Discontinue morphine until child is fully awake d. Stimulate child by calling name, shaking gently, and asking to breathe deeply ANS: A TestBankWorld.org The management of opioid-induced respiratory depression includes lowering the rate of infusion and stimulating the child. If the respiratory rate is depressed and the child cannot be aroused, then IV naloxone should be administered. The child will be in pain because of the reversal of the morphine. The morphine should be discontinued, but naloxone is indicated if the child is unresponsive. The child is unresponsive, therefore naloxone is indicated. DIF: Cognitive Level: Apply REF: p. 143 TOP: Integrated Process: Nursing Process: Implementation MSC: Area of Client Needs: Physiologic Integrity 9. The nurse is completing a pain assessment on a 4-year-old child. Which of the depicted pain scale tools should the nurse use with a child this age? a. b. c. d. ANS: A NURSINGDOC.COM The pain scale appropriate for a 4-year-old child is the FACES pain scale. Numeric pain scales can be used on children as young as age 5 as long as they can count and have some concept of numbers and their values in relation to other numbers. Word graphic scales and visual analogue scales are used preferably for school-age children. DIF: Cognitive Level: Analyze REF: p. 115 TOP: Integrated Process: Nursing Process: Implementation MSC: Area of Client Needs: Physiologic Integrity 10. Fentanyl and midazolam (Versed) are given before débridement of a child’s burn wounds. Which is the rationale for administration of these medications? a. Promote healing b. Prevent infection c. Provide pain relief d. Limit amount of débridement that will be necessary ANS: C Fentanyl and midazolam provide excellent intravenous sedation and analgesia to control procedural pain in children with burns. These drugs are for sedation and pain control, not healing, preventing infection, or limiting the amount of débridement. DIF: Cognitive Level: Understand REF: p. 127 TOP: Integrated Process: Nursing Process: Implementation MSC: Area of Client Needs: Physiologic Integrity: Pharmacologic and Parenteral Therapies 11. Nitrous oxide is being administered to a child with extensive burn injuries. Which is the purpose of this medication? a. Promote healing b. Prevent infection c. Provide anesthesia d. Improve urinary output ANS: C The use of short-acting anesthetic agents, such as propofol and nitrous oxide, has proven beneficial in eliminating procedural pain. Nitrous oxide is an anesthetic agent. DIF: Cognitive Level: Understand REF: p. 144 TOP: Integrated Process: Nursing Process: Implementation MSC: Area of Client Needs: Physiologic Integrity: Pharmacologic and Parenteral Therapies MULTIPLE RESPONSE 1. A nurse recognizes which physiologic responses as a manifestation of pain in a neonate? (Select all that apply.) a. Decreased respirations b. Diaphoresis c. Decreased SaO2 d. Decreased blood pressure e. Increased heart rate ANS: B, C, E NURSINGDOC.COM The physiologic responses that indicate pain in neonates are increased heart rate, increased blood pressure, rapid, shallow respirations, decreased arterial oxygen saturation (SaO2), pallor or flushing, diaphoresis, and palmar sweating. DIF: Cognitive Level: Apply REF: p. 120 TOP: Integrated Process: Nursing Process: Assessment MSC: Area of Client Needs: Physiologic Integrity 2. A nurse is monitoring a patient for side effects associated with opioid analgesics. Which side effects should the nurse expect to monitor for? (Select all that apply.) a. Diarrhea b. Respiratory depression c. Hypertension d. Pruritus e. Sweating ANS: B, D, E Side effects of opioids include respiratory depression, pruritus, and sweating. Constipation may occur, not diarrhea, and orthostatic hypotension may occur but not hypertension. DIF: Cognitive Level: Understand REF: p. 131 TOP: Integrated Process: Nursing Process: Implementation MSC: Area of Client Needs: Physiologic Integrity 3. Which dietary recommendations should a nurse make to an adolescent patient to manage constipation related to opioid analgesic administration? (Select all that apply.) a. Bran cereal b. Decrease fluid intake c. Prune juice d. Cheese e. Vegetables ANS: A, C, E To manage the side effect of constipation caused by opioids, fluids should be increased, and bran cereal and vegetables are recommended to increase fiber. Prune juice can act as a nonpharmacologic laxative. Fluids should be increased, not decreased, and cheese can cause constipation so it should not be recommended. DIF: Cognitive Level: Apply REF: p. 132 TOP: Integrated Process: Nursing Process: Implementation MSC: Area of Client Needs: Physiologic Integrity 4. Surgery has informed a nurse that the patient returning to the floor after spinal surgery has an opioid epidural catheter for pain management. The nurse should prepare to monitor the patient for which side effects of an opioid epidural catheter? (Select all that apply.) a. Urinary frequency b. Nausea c. Itching d. Respiratory depression ANS: B, C, D NURSINGDOC.COM Respiratory depression, nausea, itching, and urinary retention are dose-related side effects from an epidural opioid. Urinary retention, not urinary frequency, would be seen. DIF: Cognitive Level: Apply REF: p. 132 TOP: Integrated Process: Nursing Process: Planning MSC: Area of Client Needs: Physiologic Integrity SHORT ANSWER 1. A dose of oxycodone (OxyContin) 2 mg/kg has been ordered for a child weighing 33 lb. How many milligrams of OxyContin should the nurse administer? (Record your answer as a whole number.) ANS: 30 The child’s weight is divided by 2.2 to get the weight in kilograms. Kilograms in weight are then multiplied by the prescribed 2 mg. 33 lb/2.2 = 15 kg. 15 kg 2 mg = 30 mg. DIF: Cognitive Level: Apply REF: p. 128 TOP: Integrated Process: Nursing Process: Implementation MSC: Area of Client Needs: Physiologic Integrity 2. A nurse is using the FLACC scale to evaluate pain in a preverbal child. The nurse makes the following assessment: Face: occasional grimace; Leg: relaxed; Activity: squirming, tense; Cry: no cry; Consolability: content, relaxed. The nurse records the FLACC assessment as which number? (Record your answer as a whole number.) ANS: 2 The FLACC scale is recorded per the following table: 0 1 2 Face No particular expression or smile Occasional grimace or frown, withdrawn, disinterested Frequent to constant frown, clenched jaw, quivering chin Legs Normal position or relaxed Uneasy, restless, tense Kicking, or legs drawn up Activity Lying quietly, normal position, moves easily Squirming, shifting back and forth, tense Arched, rigid, or jerking Cry No cry (awake or asleep) Moans or whimpers, NocUcRaSsIiNonGaTlBc.oCmOMplaint Crying steadily, screams or sobs, frequent complaints Consolability Content, relaxed Reassured by occasional touching, hugging, or talking to; distractible Difficult to console or comfort Because the child has a grimace and is squirming and tense, 2 total points are given. Relaxed legs, no cry, and content and relaxed consolability get 0 points. DIF: Cognitive Level: Apply REF: p. 141 TOP: Integrated Process: Nursing Process: Implementation MSC: Area of Client Needs: Physiologic Integrity OTHER 1. A patient on an intravenous opioid analgesic has become apneic. The nurse should implement which interventions? Place the interventions in order from the highest priority (first intervention) to the lowest priority (last intervention). Provide your answer using lowercase letters separated by commas (e.g., a, b, c, d). a. Place the patient on continuous pulse oximetry to assess SaO2. b. Administer the prescribed naloxone (Narcan) dose by slow IV push. c. Ensure oxygen is available. TestBankWorld.org d. Prepare to calm the child as analgesia is reversed. ANS: b, a, c, d The Narcan prescribed dose should be given, first by slow IV push every 2 minutes until effect is obtained. The second intervention should be assessment of the patient’s SaO2 status. Oxygen should be made available and administered if the SaO2 status indicates hypoxemia. Last, the child should be calmed as the analgesia is reversed. DIF: Cognitive Level: Apply REF: p. 135 TOP: Integrated Process: Nursing Process: Implementation MSC: Area of Client Needs: Physiologic Integrity TestBankWorld.org Chapter 06: Childhood Communicable and Infectious Diseases Hockenberry: Wong’s Essentials of Pediatric Nursing, 10th Edition MULTIPLE CHOICE 1. Which term best describes the identification of the distribution and causes of disease, injury, or illness? a. Nursing process b. Epidemiologic process c. Community-based statistics d. Mortality and morbidity statistics ANS: B Epidemiology is the science of population health applied to the detection of morbidity and mortality in a population. It identifies the distribution and causes of diseases across a population. Nursing process is a systematic problem-solving approach for the delivery of nursing care. Morbidity and mortality statistics, along with natal rates, may provide an objective picture of a community’s health status. DIF: Cognitive Level: Remember REF: p. 157 TOP: Integrated Process: Nursing Process: Assessment MSC: Area of Client Needs: Health Promotion and Maintenance 2. The nurse is taking care of a 7-year-old child with a skin rash called a papule. Which clinical finding should the nurse expect to assess with this type of skin rash? a. A lesion that is elevated, palpaNbUleR,SfIiNrmGT, Ban.CdOcMircumscribed; less than 1 cm in diameter b. A lesion that is elevated, flat-topped, firm, rough, and superficial; greater than 1 cm in diameter c. An elevated lesion, firm, circumscribed, palpable; 1 to 2 cm in diameter d. An elevated lesion, circumscribed, filled with serous fluid; less than 1 cm in diameter ANS: A A papule is elevated; palpable; firm; circumscribed; less than 1 cm in diameter; and brown, red, pink, tan, or bluish red. A plaque is an elevated, flat-topped, firm, rough, superficial papule greater than 1 cm in diameter. It may be coalesced papules. A nodule is elevated, 1 to 2 cm in diameter, firm, circumscribed, palpable, and deeper in the dermis than a papule. A vesicle is elevated, circumscribed, superficial, less than 1 cm in diameter, and filled with serous fluid. DIF: Cognitive Level: Understand REF: p. 178 TOP: Integrated Process: Nursing Process: Assessment MSC: Area of Client Needs: Physiologic Integrity: Reduction of Risk Potential 3. The nurse is teaching nursing students about childhood skin lesions. Which is an elevated, circumscribed skin lesion that is less than 1 cm in diameter and filled with serous fluid? a. Cyst b. Papule c. Pustule d. Vesicle ANS: D A vesicle is elevated, circumscribed, superficial, less than 1 cm in diameter, and filled with serous fluid. A cyst is elevated, circumscribed, palpable, encapsulated, and filled with liquid or semisolid material. A papule is elevated, palpable, firm, circumscribed, less than 1 cm in diameter, and brown, red, pink, tan, or bluish red. A pustule is elevated, superficial, and similar to a vesicle but filled with purulent fluid. DIF: Cognitive Level: Remember REF: p. 178 TOP: Integrated Process: Teaching/Learning MSC: Area of Client Needs: Physiologic Integrity: Reduction of Risk Potential 4. The nurse is taking care of a 2-year-old child with a macule skin lesion. Which clinical finding should the nurse expect to assess with this type of lesion? a. Flat, nonpalpable, and irregularly shaped lesion that is greater than 1 cm in diameter b. Heaped-up keratinized cells, flaky exfoliation, irregular, thick or thin, dry or oily, varied in size c. Flat, brown mole less than 1 cm in diameter d. Elevated, flat-topped, firm, rough, superficial papule greater than 1 cm in diameter ANS: C A macule is flat; nonpalpable; circumscribed; less than 1 cm in diameter; and brown, red, purple, white, or tan. A patch is a flat, nonpalpable, and irregularly shaped macule that is greater than 1 cm in diameter. Scale is heaped-up keratinized cells, flaky exfoliation, irregular, thick or thin, dry or oily, varied in size, and silver white or tan. A plaque is an elevated, flat-topped, firm, rough, superficiaNlUpRaSpIuNlGe TgBre.CaOteMr than 1 cm in diameter. It may be coalesced papules. DIF: Cognitive Level: Understand REF: p. 178 TOP: Integrated Process: Nursing Process: Assessment MSC: Area of Client Needs: Physiologic Integrity: Reduction of Risk Potential 5. Which nursing consideration is important when caring for a child with impetigo contagiosa? a. Apply topical corticosteroids to decrease inflammation. b. Carefully remove dressings so as not to dislodge undermined skin, crusts, and debris. c. Carefully wash hands and maintain cleanliness when caring for an infected child. d. Examine child under a Wood lamp for possible spread of lesions. ANS: C A major nursing consideration related to bacterial skin infections, such as impetigo contagiosa, is to prevent the spread of the infection and complications. This is done by thorough hand washing before and after contact with the affected child. Corticosteroids are not indicated in bacterial infections. Dressings are usually not indicated. The undermined skin, crusts, and debris are carefully removed after softening with moist compresses. A Wood lamp is used to detect fluorescent materials in the skin and hair. It is used in certain disease states, such as tinea capitis. DIF: Cognitive Level: Understand REF: p. 177 TOP: Integrated Process: Nursing Process: Implementation MSC: Area of Client Needs: Physiologic Integrity: Reduction of Risk Potential 6. The nurse is caring for a 5-year-old child with impetigo contagiosa. The parents ask the nurse what will happen to their child’s skin after the infection has subsided and healed. Which answer should the nurse give? a. There will be no scarring. b. There may be some pigmented spots. c. It is likely there will be some slightly depressed scars. d. There will be some atrophic white scars. ANS: A Impetigo contagiosa tends to heal without scarring unless a secondary infection occurs. DIF: Cognitive Level: Apply REF: p. 177 TOP: Integrated Process: Teaching/Learning MSC: Area of Client Needs: Physiologic Integrity: Reduction of Risk Potential 7. What is cellulitis often caused by? a. Herpes zoster b. Candida albicans c. Human papillomavirus d. Streptococcus or Staphylococcus organisms ANS: D Streptococci, staphylococci, and Haemophilus influenzae are the organisms usually responsible for cellulitis. Herpes zoster is the virus associated with varicella and shingles. C. albicans is associated with candidiasis, or thrush. Human papillomavirus is associated with various types of human warts. NURSINGDOC.COM DIF: Cognitive Level: Remember REF: p. 176 TOP: Integrated Process: Nursing Process: Assessment MSC: Area of Client Needs: Physiologic Integrity: Reduction of Risk Potential 8. The nurse is conducting a staff in-service on appearance of childhood skin conditions. Lymphangitis (“streaking”) is frequently seen in which condition? a. Cellulitis b. Folliculitis c. Impetigo contagiosa d. Staphylococcal scalded skin ANS: A Lymphangitis is frequently seen in cellulitis. If it is present, hospitalization is usually required for parenteral antibiotics. Lymphangitis is not associated with folliculitis, impetigo, or staphylococcal scalded skin. DIF: Cognitive Level: Understand REF: p. 176 TOP: Integrated Process: Teaching/Learning MSC: Area of Client Needs: Physiologic Integrity: Reduction of Risk Potential 9. The nurse should expect to assess which causative agent in a child with warts? a. Bacteria b. Fungus c. Parasite d. Virus ANS: D Human warts are caused by the human papillomavirus. Infection with bacteria, fungus, and parasites does not result in warts. DIF: Cognitive Level: Understand REF: p. 177 TOP: Integrated Process: Nursing Process: Assessment MSC: Area of Client Needs: Physiologic Integrity: Reduction of Risk Potential 10. The nurse should implement which prescribed treatment for a child with warts? a. Vaccination b. Local destruction c. Corticosteroids d. Specific antibiotic therapy ANS: B Local destructive therapy individualized according to location, type, and number—including surgical removal, electrocautery, curettage, cryotherapy, caustic solutions, x-ray treatment, and laser therapies—is used. Vaccination is prophylaxis for warts and is not a treatment. Corticosteroids and specific antibiotic therapy are not effective in the treatment of warts. DIF: Cognitive Level: Apply REF: p. 178 TOP: Integrated Process: Nursing Process: Implementation MSC: Area of Client Needs: Physiologic Integrity: Reduction of Risk Potential 11. Herpes zoster is caused by the varNicUeRllSaINviGruTsB.aCnOdMhas an affinity for: a. sympathetic nerve fibers. b. parasympathetic nerve fibers. c. posterior root ganglia and posterior horn of the spinal cord. d. lateral and dorsal columns of the spinal cord. ANS: C The herpes zoster virus has an affinity for posterior root ganglia, the posterior horn of the spinal cord, and skin. The zoster virus does not involve sympathetic or parasympathetic nerve fibers and the lateral and dorsal columns of the spinal cord. DIF: Cognitive Level: Understand REF: p. 178 TOP: Integrated Process: Nursing Process: Assessment MSC: Area of Client Needs: Physiologic Integrity: Reduction of Risk Potential 12. The nurse is taking care of a 7-year-old child with herpes simplex virus (type 1 or 2). Which prescribed medication should the nurse expect to be included in the treatment plan? a. Corticosteroids b. Oral griseofulvin c. Oral antiviral agent d. Topical and/or systemic antibiotic ANS: C Oral antiviral agents are effective for viral infections such as herpes simplex. Corticosteroids are not effective for viral infections. Griseofulvin is an antifungal agent and not effective for viral infections. Antibiotics are not effective in viral diseases. DIF: Cognitive Level: Apply REF: p. 178 TOP: Integrated Process: Nursing Process: Planning MSC: Area of Client Needs: Physiologic Integrity: Pharmacologic and Parenteral Therapies 13. What causes tinea capitis (ringworm)? a. Virus b. Fungus c. Allergic reaction d. Bacterial infection ANS: B Ringworm is caused by a group of closely related filamentous fungi that invade primarily the stratum corneum, hair, and nails. They are superficial infections that live on, not in, the skin. Virus and bacterial infection are not the causative organisms for ringworm. Ringworm is not an allergic response. DIF: Cognitive Level: Understand REF: p. 179 TOP: Integrated Process: Nursing Process: Assessment MSC: Area of Client Needs: Physiologic Integrity: Reduction of Risk Potential 14. The nurse is caring for a school-age child with a tinea capitis (ringworm) infection. What should the nurse expect the therapeutic management of this child to include? a. Administering oral griseofulvin b. Administering topical or oral aNnUtiRbSioINtiGcsTB.COM c. Applying topical sulfonamides d. Applying Burow solution compresses to affected area ANS: A Treatment with the antifungal agent griseofulvin is part of the treatment for the fungal disease ringworm. Oral griseofulvin therapy frequently continues for weeks or months. Antibiotics, sulfonamides, and Burow solution are not effective in fungal infections. DIF: Cognitive Level: Understand REF: p. 179 TOP: Integrated Process: Nursing Process: Implementation MSC: Area of Client Needs: Physiologic Integrity: Pharmacologic and Parenteral Therapies 15. Parents tell the nurse that their child keeps scratching the areas where he has poison ivy. The nurse’s response should be based on which knowledge? a. Poison ivy does not itch and needs further investigation. b. Scratching the lesions will not cause a problem. c. Scratching the lesions will cause the poison ivy to spread. d. Scratching the lesions may cause them to become secondarily infected. ANS: D Poison ivy is a contact dermatitis that results from exposure to the oil urushiol in the plant. Every effort is made to prevent the child from scratching because the lesions can become secondarily infected. The poison ivy produces localized, streaked or spotty, oozing, and painful impetiginous lesions. Itching is a common response. Scratching the lesions can result in secondary infections. The lesions do not spread by contact with the blister serum or by scratching. DIF: Cognitive Level: Apply REF: p. 185 TOP: Integrated Process: Teaching/Learning MSC: Area of Client Needs: Physiologic Integrity: Reduction of Risk Potential 16. The nurse is taking care of a child with scabies. Which primary clinical manifestation should the nurse expect to assess with this disease? a. Edema b. Redness c. Pruritus d. Maceration ANS: C Scabies is caused by the scabies mite. The inflammatory response and intense itching occur after the host has become sensitized to the mite. This occurs approximately 30 to 60 days after initial contact. Edema, redness, and maceration are not observed in scabies. DIF: Cognitive Level: Understand REF: p. 180 TOP: Integrated Process: Nursing Process: Assessment MSC: Area of Client Needs: Physiologic Integrity: Reduction of Risk Potential 17. Which is usually the only symptomNUoRfSpINedGiTcBul.CosOiMs capitis (head lice)? a. Itching b. Vesicles c. Scalp rash d. Localized inflammatory response ANS: A Itching is generally the only manifestation of pediculosis capitis (head lice). Diagnosis is made by observation of the white eggs (nits) on the hair shaft. Vesicles, scalp rash, and localized inflammatory response are not symptoms of head lice. DIF: Cognitive Level: Understand REF: p. 182 TOP: Integrated Process: Nursing Process: Assessment MSC: Area of Client Needs: Physiologic Integrity: Reduction of Risk Potential 18. The nurse is talking to the parents of a child with pediculosis capitis. Which should the nurse include when explaining how to manage pediculosis capitis? a. “You will need to cut the hair shorter if infestation and nits are severe.” b. “You can distinguish viable from nonviable nits, and remove all viable ones.” c. “You can wash all nits out of hair with a regular shampoo.” d. “You will need to remove nits with an extra-fine-tooth comb or tweezers.” ANS: D Treatment consists of the application of pediculicide and manual removal of nit cases. An extra-fine-tooth comb facilitates manual removal. Parents should be cautioned against cutting the child’s hair short; lice infest short hair as well as long. It increases the child’s distress and serves as a continual reminder to peers who are prone to tease children with a different appearance. It is not possible to differentiate between viable and nonviable eggs. Regular shampoo is not effective; a pediculicide is necessary. DIF: Cognitive Level: Apply REF: p. 182 TOP: Integrated Process: Teaching/Learning MSC: Area of Client Needs: Physiologic Integrity: Reduction of Risk Potential 19. Which bite causes Rocky Mountain spotted fever? a. Flea b. Tick c. Mosquito d. Mouse or rat ANS: B Rocky Mountain spotted fever is caused by a tick. The tick must attach and feed for at least 1 to 2 hours to transmit the disease. The usual habitat of the tick is in heavily wooded areas. Fleas, mosquitoes, and mice or rats do not transmit Rocky Mountain spotted fever. DIF: Cognitive Level: Understand REF: p. 186 TOP: Integrated Process: Nursing Process: Assessment MSC: Area of Client Needs: Physiologic Integrity: Reduction of Risk Potential 20. The school nurse is conducting a class for school-age children on Lyme disease. Which is characteristic of Lyme disease? NURSINGDOC.COM a. Difficult to prevent b. Treated with oral antibiotics in stages 1, 2, and 3 c. Caused by a spirochete that enters the skin through a tick bite d. Common in geographic areas where the soil contains the mycotic spores that cause the disease ANS: C Lyme disease is caused by Borrelia burgdorferi, a spirochete spread by ticks. The early characteristic rash is erythema migrans. Tick bites should be avoided by entering tick-infested areas with caution. Light-colored clothing should be worn to identify ticks easily. Long-sleeved shirts and long pants tucked into socks should be the attire. Early treatment of the erythema migrans (stage 1) can prevent the development of Lyme disease. Lyme disease is caused by a spirochete, not mycotic spores. DIF: Cognitive Level: Understand REF: p. 186 TOP: Integrated Process: Teaching/Learning MSC: Area of Client Needs: Physiologic Integrity: Reduction of Risk Potential 21. The nurse is examining 12-month-old Amy, who was brought to the clinic for persistent diaper rash. The nurse finds perianal inflammation with satellite lesions that cross the inguinal folds. What is most likely the cause of the diaper rash? a. Impetigo b. Candida albicans c. Urine and feces d. Infrequent diapering ANS: B C. albicans infection produces perianal inflammation and a maculopapular rash with satellite lesions that may cross the inguinal folds. Impetigo is a bacterial infection that spreads peripherally in sharply marginated, irregular outlines. Eruptions involving the skin in contact with the diaper, but sparing the folds, are likely to be caused by chemical irritation, especially urine and feces. DIF: Cognitive Level: Analyze REF: p. 179 TOP: Integrated Process: Nursing Process: Assessment MSC: Area of Client Needs: Physiologic Integrity: Reduction of Risk Potential 22. A school nurse assesses a case of tinea capitis (ringworm) on a 6-year-old child. Which figure depicts the characteristic lesion of tinea capitis? a. b. INGTB.COM c. d. ANS: C Tinea capitis is characterized by lesions in the scalp configured of scaly, circumscribed patches or patchy, scaling areas of alopecia. Generally the lesions are asymptomatic but a severe, deep inflammatory reaction may occur that manifests as boggy, encrusted lesions (kerions). Impetigo contagiosa is depicted in the figure showing the vesicular lesion around the nares area that has become vesicular. The lesions rupture easily, leaving superficial, moist erosions that tend to spread peripherally in sharply marginated irregular outlines. The exudate dries to form heavy, honey-colored crusts. The figure depicting inflammation on the cheek is cellulitis. Inflammation of skin and subcutaneous tissues is characterized by intense redness, swelling, and firm infiltration. Cellulitis may progress to abscess formation. The figure depicting “streaked blisters” surrounding one large blister is characteristic of contact dermatitis from poison ivy contact. DIF: Cognitive Level: Analyze REF: p. 180 TOP: Integrated Process: Nursing Process: Assessment MSC: Area of Client Needs: Physiologic Integrity: Reduction of Risk Potential 23. Airborne isolation is required for a child who is hospitalized with: a. mumps. NURSINGDOC.COMb. chickenpox.c. exanthema subitum (roseola). d. erythema infectiosum (fifth disease). ANS: B Chickenpox is communicable through direct contact, droplet spread, and contaminated objects. Mumps is transmitted from direct contact with saliva of infected person and is most communicable before onset of swelling. The transmission and source of the viral infection exanthema subitum (roseola) is unknown. Erythema infectiosum (fifth disease) is communicable before onset of symptoms. DIF: Cognitive Level: Understand REF: p. 163 TOP: Integrated Process: Nursing Process: Implementation MSC: Area of Client Needs: Safe and Effective Care Environment Acyclovir (Zovirax) is given to children with chickenpox to: 24. a. minimize scarring. b. decrease the number of lesions. c. prevent aplastic anemia. d. prevent spread of the disease. ANS: B Acyclovir decreases the number of lesions; shortens duration of fever; and decreases itching, lethargy, and anorexia. Treating pruritus and discouraging itching minimize scarring. Aplastic anemia is not a complication of chickenpox. Strict isolation until vesicles are dried prevents spread of disease. DIF: Cognitive Level: Understand REF: p. 163 TOP: Integrated Process: Nursing Process: Implementation MSC: Area of Client Needs: Physiologic Integrity 25. The single parent of a 3-year-old child who has just been diagnosed with chickenpox tells the nurse that she cannot afford to stay home with the child and miss work. The parent asks the nurse if some medication will shorten the course of the illness. Which is the most appropriate nursing intervention? a. Reassure the parent that it is not necessary to stay home with the child. b. Explain that no medication will shorten the course of the illness. c. Explain the advantages of the medication acyclovir (Zovirax) to treat chickenpox. d. Explain the advantages of the medication VCZ immune globulin (VariZIG) to treat chickenpox. ANS: C Acyclovir is effective in treating the number of lesions; shortening the duration of fever; and decreasing itching, lethargy, and anorexia. It is important the parent stay with the child to monitor fever. Acyclovir lessens the severity of chickenpox. VariZIG is given only to high-risk children. DIF: Cognitive Level: Apply REF: p. 163 TOP: Integrated Process: Teaching/Learning MSC: Area of Client Needs: PhysiolNoUgiRcSIInNteGgTriBty.COM 26. Which may be given to high-risk children after exposure to chickenpox to prevent varicella? a. Acyclovir (Zovirax) b. Varicella globulin c. Diphenhydramine hydrochloride (Benadryl) d. VCZ immune globulin (VariZIG) ANS: D VariZIG is given to high-risk children to prevent the development of chickenpox. Acyclovir decreases the severity, not the development, of chickenpox. Varicella globulin is not effective because it is not the immune globulin. Diphenhydramine may help pruritus but not the actual chickenpox. DIF: Cognitive Level: Understand REF: p. 163 TOP: Integrated Process: Nursing Process: Implementation MSC: Area of Client Needs: Physiologic Integrity 27. Vitamin A supplementation may be recommended for the young child who has which disease? a. Mumps b. Rubella c. Measles (rubeola) d. Erythema infectiosum ANS: C Evidence shows vitamin A decreases morbidity and mortality in measles. Mumps is treated with analgesics for pain and antipyretics for fever. Rubella is treated similarly to mumps. Erythema infectiosum is treated similarly to mumps and rubella. DIF: Cognitive Level: Understand REF: p. 166 TOP: Integrated Process: Nursing Process: Implementation MSC: Area of Client Needs: Physiologic Integrity 28. A nurse is teaching parents about caring for their child with chickenpox. The nurse should let the parents know that the child is considered to be no longer contagious when which occurs? a. When fever is absent b. When lesions are crusted c. 24 hours after lesions erupt d. 8 days after onset of illness ANS: B When the lesions are crusted, the chickenpox is no longer contagious. This may be a week after onset of disease. Chickenpox is still contagious when child has fever. Children are contagious after lesions erupt. If lesions are crusted at 8 days, the child is no longer contagious. DIF: Cognitive Level: Apply REF: p. 163 TOP: Integrated Process: Teaching/Learning MSC: Area of Client Needs: Physiologic Integrity 29. A nurse is assessing a child and notes Koplik spots. In which of these communicable diseases are Koplik spots present? NURSINGDOC.COMa. Rubellab. Measles (rubeola)c. Chickenpox (varicella)d. Exanthema subitum (roseola) ANS: B Koplik spots are small irregular red spots with a minute, bluish white center found on the buccal mucosa 2 days before systemic rash. Rubella occurs with rash on the face, which rapidly spreads downward. Varicella appears with highly pruritic macules, followed by papules and vesicles. Roseola is seen with rose-pink macules on the trunk, spreading to face and extremities. DIF: Cognitive Level: Apply REF: p. 166 TOP: Integrated Process: Nursing Process: Assessment MSC: Area of Client Needs: Physiologic Integrity Which is a common childhood communicable disease that may cause severe defects in the fetus when it occurs in its congenital form? a. Erythema infectiosum 30. b. Roseola c. Rubeola d. Rubella ANS: D Rubella causes teratogenic effects on the fetus. There is a low risk of fetal death to those in contact with children affected with fifth disease. Roseola and rubeola are not dangerous to the fetus. DIF: Cognitive Level: Understand REF: p. 168 TOP: Integrated Process: Nursing Process: Assessment MSC: Area of Client Needs: Physiologic Integrity 31. Which is the causative agent of scarlet fever? a. Enteroviruses b. Corynebacterium organisms c. Scarlet fever virus d. Group A -hemolytic streptococci (GABHS) ANS: D GABHS infection causes scarlet fever. Enteroviruses do not cause the same complications. Corynebacterium organisms cause diphtheria. Scarlet fever is not caused by a virus. DIF: Cognitive Level: Understand REF: p. 169 TOP: Integrated Process: Nursing Process: Assessment MSC: Area of Client Needs: Physiologic Integrity 32. A parent reports to the nurse that her child has inflamed conjunctivae of both eyes with purulent drainage and crusting of the eyelids, especially on awakening. These manifestations suggest: a. viral conjunctivitis. b. allergic conjunctivitis. c. bacterial conjunctivitis. NURSINGDOC.COM d. conjunctivitis caused by foreign body. ANS: C Bacterial conjunctivitis has these symptoms. Viral or allergic conjunctivitis has watery drainage. Foreign body causes tearing and pain, and usually only one eye is affected. DIF: Cognitive Level: Analyze REF: p. 171 TOP: Integrated Process: Nursing Process: Evaluation MSC: Area of Client Needs: Physiologic Integrity 33. Which is an important nursing consideration when caring for a child with herpetic gingivostomatitis (HGS)? a. Apply topical anesthetics before eating. b. Drink from a cup, not a straw. c. Wait to brush teeth until lesions are sufficiently healed. d. Explain to parents how this is sexually transmitted. ANS: A Treatment for HGS is aimed at relief of pain. Drinking bland fluids through a straw helps avoid painful lesions. Mouth care is encouraged with a soft toothbrush. HGS is usually caused by herpes simplex virus type 1, which is not associated with sexual transmission. DIF: Cognitive Level: Apply REF: p. 172 TOP: Integrated Process: Nursing Process: Implementation MSC: Area of Client Needs: Physiologic Integrity 34. A parent has asked the nurse about how her child can be tested for pinworms. The nurse responds by stating that which is the most common test for diagnosing pinworms in a child? a. Lower gastrointestinal (GI) series b. Three stool specimens, at intervals of 4 days c. Observation for presence of worms after child defecates d. Laboratory examination of a fecal smear ANS: D Laboratory examination of substances containing the worm, its larvae, or ova can identify the organism. Most are identified by examining fecal smears from the stools of persons suspected of harboring the parasite. Fresh specimens are best for revealing parasites or larvae. Lower GI series is not helpful for diagnosing enterobiasis. Stool specimens are not necessary to diagnose pinworms. Worms will not be visible after child defecates. DIF: Cognitive Level: Understand REF: p. 174 TOP: Integrated Process: Teaching/Learning MSC: Area of Client Needs: Physiologic Integrity 35. A clinic nurse is assessing a child with erythema infectiosum (fifth disease). Which figure depicts the rash the nurse should expect to assess? a. RSINGTB.COM b. c. d. ANS: A Erythema infectiosum rash appears in three stages: erythema on face, chiefly on cheeks (“slapped face” appearance); disappears by 1-4 days. Chicken pox rash begins as macule, rapidly progresses to papule and then vesicle (surrounded by erythematous base; becomes umbilicated and cloudy; breaks easily and forms crusts); all three stages (papule, vesicle, crust) present in varying degrees at one time. Roseola rash is discrete rose-pink macules or maculopapules appearing first on trunk and then spreading to neck, face, and extremities; nonpruritic; fades on pressure; lasNtsU1R-S2INdGayTsB. .RCOubMeola rash—appears 3-4 days after onset of prodromal stage; begins as erythematous maculopapular eruption on face and gradually spreads downward; more severe in earlier sites (appears confluent) and less intense in later sites (appears discrete); after 3-4 days, assumes brownish appearance, and fine desquamation occurs over area of extensive involvement. DIF: Cognitive Level: Apply REF: p. 164 TOP: Integrated Process: Nursing Process: Assessment MSC: Area of Client Needs: Physiologic Integrity 36. A nurse is admitting a child to the hospital with a diagnosis of giardiasis. Which medication should the nurse expect to be prescribed? a. Metronidazole (Flagyl) b. Amoxicillin clavulanate (Augmentin) c. Clarithromycin (Biaxin) d. Prednisone (Orapred) ANS: A The drugs of choice for treatment of giardiasis are metronidazole (Flagyl), tinidazole (Tindamax), and nitazoxanide (Alinia). These are classified as antifungals. Amoxicillin and clarithromycin are antibiotics that treat bacterial infections. Prednisone is a steroid and is used as an anti-inflammatory medication. DIF: Cognitive Level: Apply REF: p. 174 TOP: Integrated Process: Nursing Process: Planning MSC: Area of Client Needs: Physiologic Integrity 37. A mother tells the nurse that she does not want her infant immunized because of the discomfort associated with injections. What should the nurse explain? a. This cannot be prevented. b. Infants do not feel pain as adults do. c. This is not a good reason for refusing immunizations. d. A topical anesthetic, EMLA, can be applied before injections are given. ANS: D Several topical anesthetic agents can be used to minimize the discomfort associated with immunization injections. These include EMLA (eutectic mixture of local anesthetic) and vapor coolant sprays. Pain associated with many procedures can be prevented and minimized by using the principles of atraumatic care. With preparation, the injection site can be properly anesthetized to decrease the amount of pain felt by the infant. Infants have the neural pathways to feel pain. Numerous research studies have indicated that infants perceive and react to pain in the same manner as do children and adults. The mother should be allowed to discuss her concerns and the alternatives available. This is part of the informed consent process. DIF: Cognitive Level: Apply REF: p. 151 TOP: Integrated Process: Teaching/Learning MSC: Area of Client Needs: Health Promotion and Maintenance MULTIPLE RESPONSE NURSINGDOC.COM 1. The community health nurse is teaching parents about prevention of the spread and reoccurrence of pediculosis (head lice). Which should the nurse include in the teaching session? (Select all that apply.) a. Dryclean nonwashable items. b. Spray the environment with an insecticide. c. Seal nonwashable items in a plastic bag for 5 days. d. Boil combs and brushes for 10 minutes. e. Discourage sharing of personal items. ANS: A, D, E To prevent the spread and reoccurrence of pediculosis the nurse should teach the parents to: dryclean nonwashable items, boil combs and brushes for 10 minutes or soak for 1 hour in a pediculicide, and discourage the sharing of personal items, such as combs, hats, scarves and other headgear. Spraying with insecticide is not recommended because of the danger to children and animals. Nonwashable items should be sealed for 14 days in a plastic bag. DIF: Cognitive Level: Apply REF: p. 182 TOP: Integrated Process: Teaching/Learning MSC: Area of Client Needs: Physiologic Integrity: Reduction of Risk Potential 2. A nurse is preparing to administer routine immunizations to a 4-month-old infant. The infant is currently up to date on all previously recommended immunizations. Which immunizations will the nurse prepare to administer? (Select all that apply.) a. Measles, mumps, and rubella (MMR) b. Rotavirus (RV) c. Diphtheria, tetanus, pertussis (DTaP) d. Varicella e. Haemophilus influenzae type b (HIB) f. Inactivated poliovirus (IPV) ANS: B, C, E, F Recommended immunization schedule for a 4-month-old, up to date on immunizations, would be to administer the rotavirus (RV), diphtheria, tetanus, pertussis (DTaP), Haemophilus influenza type b (HIB), and inactivated poliovirus (IPV) vaccinations. The measles, mumps, and rubella (MMR) and varicella would not be administered until the child is at least 1 year of age. DIF: Cognitive Level: Apply REF: p. 151 TOP: Integrated Process: Nursing Process: Implementation MSC: Area of Client Needs: Health Promotion and Maintenance NURSINGDOC.COM Chapter 07: Health Promotion of the Newborn and Family Hockenberry: Wong’s Essentials of Pediatric Nursing, 10th Edition MULTIPLE CHOICE 1. Which is the most critical physiologic change required of the newborn? a. Closure of fetal shunts in the heart b. Stabilization of fluid and electrolytes c. Body-temperature maintenance d. Onset of breathing ANS: D The onset of breathing is the most immediate and critical physiologic change required for transition to extrauterine life. Factors that interfere with this normal transition increase fetal asphyxia, which is a condition of hypoxemia, hypercapnia, and acidosis. This affects the fetus’s adjustment to extrauterine life. Closure of fetal shunts in the heart, stabilization of fluid and electrolytes, and body-temperature maintenance are important changes that must occur in the transition to extrauterine life, but breathing and the exchange of oxygen for carbon dioxide must come first. DIF: Cognitive Level: Understand REF: p. 190 TOP: Integrated Process: Nursing Process: Assessment MSC: Area of Client Needs: Health Promotion and Maintenance 2. Which is a function of brown adipose tissue (BAT) in the newborn? a. Provides ready source of calorNieUsRiSnINthGeTnBe.CwObMorn period b. Insulates the body against lowered environmental temperature c. Protects the newborn from injury during the birth process d. Generates heat for distribution to other parts of body ANS: D Brown fat is a unique source of heat for the newborn. It has a larger content of mitochondrial cytochromes and a greater capacity for heat production through intensified metabolic activity than does ordinary adipose tissue. Heat generated in brown fat is distributed to other parts of the body by the blood. It is effective in heat production only. The newborn has a thin layer of subcutaneous fat, which does not provide for conservation of heat. Brown fat is located in superficial areas such as between the scapulae, around the neck, in the axillae, and behind the sternum. These areas would not protect the newborn from injury during the birth process. DIF: Cognitive Level: Understand REF: p. 191 TOP: Integrated Process: Nursing Process: Assessment MSC: Area of Client Needs: Health Promotion and Maintenance 3. Which characteristic is representative of the newborn’s gastrointestinal tract? a. Stomach capacity is approximately 90 ml. b. Peristaltic waves are relatively slow. c. Overproduction of pancreatic amylase occurs. d. Intestines are shorter in relation to body size. ANS: A Newborns require frequent small feedings because their stomach capacity is approximately 90 ml. Peristaltic waves are rapid. A deficiency of pancreatic lipase limits the absorption of fats. Newborn’s intestines are longer in relation to body size than those of an adult. DIF: Cognitive Level: Understand REF: p. 191 TOP: Integrated Process: Nursing Process: Planning MSC: Area of Client Needs: Health Promotion and Maintenance 4. The nurse notes the first stool of a newborn is black and tarry. Which term is used to describe this type of stool? a. Meconium b. Transitional c. Miliaria d. Milk stool ANS: A Meconium is composed of amniotic fluid and its constituents, intestinal secretions, shed mucosal cells, and possibly blood. It is the newborn’s first stool. Transitional stools usually appear by the third day after the beginning of feeding. They are usually greenish brown to yellowish brown, thin, and less sticky than meconium. Miliaria are distended sweat glands that appear as minute vesicles, primarily on the face. Milk stool usually occurs by the fourth day. The appearance varies, depending on whether the neonate is breastfed or formula-fed. DIF: Cognitive Level: Remember REF: p. 191 TOP: Integrated Process: Nursing Process: Assessment MSC: Area of Client Needs: Health Promotion and Maintenance 5. A nurse notes that a 12-hour-old nNeUwRbSoIrNnGhTaBs.CnOotMhad the first meconium stool. The nurse documents this finding and continues to monitor the newborn because, in term newborns, the first meconium stool occurs within how many hours of birth? a. 6 to 8 b. 8 to 12 c. 12 to 24 d. 24 to 48 ANS: D The first meconium stool should occur within the first 24 to 48 hours. It may be delayed up to 7 days in very low birth weight newborns. Although it may occur earlier, the expected range is the first 24 to 48 hours of life. DIF: Cognitive Level: Remember REF: p. 191 TOP: Integrated Process: Teaching/Learning MSC: Area of Client Needs: Health Promotion and Maintenance 6. A nurse is doing an assessment on a newborn. Which is characteristic of a newborn’s vision at birth and an expected finding during the assessment? a. Ciliary muscles are mature. b. Blink reflex is absent. c. Tear glands function. d. Pupils react to light. ANS: D Although at birth the eye is still structurally incomplete, the pupils do react to light. The ciliary muscles are immature, limiting the eyes’ ability to focus on an object for any length of time. The blink reflex is responsive to minimal stimulus. The tear glands do not begin to function until ages 2 to 4 weeks. DIF: Cognitive Level: Remember REF: p. 193 TOP: Integrated Process: Nursing Process: Assessment MSC: Area of Client Needs: Health Promotion and Maintenance 7. The Apgar score of a newborn 5 minutes after birth is 8. Which is the nurse’s best interpretation of this? a. Resuscitation is likely to be needed. b. Adjustment to extrauterine life is adequate. c. Additional scoring in 5 more minutes is needed. d. Maternal sedation or analgesia contributed to the low score. ANS: B The Apgar reflects the newborn’s status in five areas: heart rate, respiratory effort, muscle tone, reflex irritability, and color. Scores of 7 to 10 indicate an absence of difficulty adjusting to extrauterine life. Scores of 0 to 3 indicate severe distress, and scores of 4 to 6 indicate moderate difficulty. The Apgar score is not used to determine the newborn’s need for resuscitation at birth. All newborns are rescored at 5 minutes. The newborn does not have a low score. DIF: Cognitive Level: Understand REF: p. 193 TOP: Integrated Process: Nursing Process: Assessment MSC: Area of Client Needs: Health Promotion and Maintenance NURSINGDOC.COM 8. The nurse is presenting an in-service session on assessing gestational age in newborns. Which information should be included? a. The newborn’s length and weight are the most accurate indicators of gestational age. b. The newborn’s Apgar score and the mother’s estimated date of confinement (EDC) are combined to determine gestational age. c. The newborn’s posture at rest and arm recoil are two physical signs used to determine gestational age. d. The newborn’s chest circumference compared to the head circumference is the determinant for gestational age. ANS: C With the newborn quiet and in a supine position, the degree of flexion in the arms and legs and the arm recoil can be used to help determine gestational age. Length, weight, and the chest/head circumference reflect the newborn’s size and weight, which vary according to race and gender. Birth weight alone is a poor indicator of gestational age and fetal maturity. The Apgar score is an indication of the newborn’s adjustment to extrauterine life, and the mother’s EDC is of no importance in determining gestational age. DIF: Cognitive Level: Apply REF: p. 193 TOP: Integrated Process: Nursing Process: Planning MSC: Area of Client Needs: Health Promotion and Maintenance 9. The nurse is assessing a 3-day-old, breastfed newborn who weighed 7 pounds, 8 ounces at birth. The newborn’s mother is now concerned that the newborn weighs 6 pounds, 15 ounces. Which is the most appropriate nursing intervention? a. Recommend supplemental feedings of formula. b. Explain that this weight loss is within normal limits. c. Assess child further to determine cause of excessive weight loss. d. Encourage mother to express breast milk for bottle feeding the newborn. ANS: B The newborn normally loses about 10% of the birth weight by age 3 or 4 days. The birth weight is usually regained by the tenth day of life. Because this is an expected occurrence, no further action is needed. The mother should be taught about normal newborn feeding and growing patterns. DIF: Cognitive Level: Apply REF: p. 196 TOP: Integrated Process: Teaching/Learning MSC: Area of Client Needs: Health Promotion and Maintenance 10. Why are rectal temperatures not recommended in the newborn? a. They are inaccurate. b. They do not reflect core body temperature. c. They can cause perforation of rectal mucosa. d. They take too long to obtain an accurate reading. ANS: C Rectal temperatures are avoided in the newborn. If done incorrectly, the insertion of a thermometer into the rectum can perforate the mucosa. Rectal temperatures, if taken correctly, are considered an accurate reflectiNoUnRoSfINcoGrTeBb.CodOyMtemperature. The inherent risks and intrusive nature limit the use. The time it takes to determine body temperature is related to the equipment used, not the route only. DIF: Cognitive Level: Remember REF: p. 197 TOP: Integrated Process: Nursing Process: Assessment MSC: Area of Client Needs: Health Promotion and Maintenance 11. The nurse should expect the apical heart rate of a stabilized newborn to be in which range? a. 60 to 80 beats/min b. 80 to 100 beats/min c. 120 to 140 beats/min d. 160 to 180 beats/min ANS: C The pulse rate of the newborn varies with periods of reactivity. Usually the pulse rate is between 120 and 140 beats/min; 60 to 100 beats/min is too slow for a neonate and 160 to 180 beats/min is too fast for a neonate. DIF: Cognitive Level: Remember REF: p. 197 TOP: Integrated Process: Nursing Process: Assessment MSC: Area of Client Needs: Health Promotion and Maintenance 12. A nurse is palpating a newborn’s fontanels. The nurse documents the anterior fontanel is which shape? a. Circle b. Triangle c. Square d. Diamond ANS: D The anterior fontanel is diamond-shaped and measures from barely palpable to 4 to 5 cm. Neither of the fontanels is a circle or a square. The triangle is the shape of the posterior fontanel. DIF: Cognitive Level: Understand REF: p. 198 TOP: Integrated Process: Communication and Documentation MSC: Area of Client Needs: Health Promotion and Maintenance 13. Which is the name of the suture separating the parietal bones at the top center of a newborn’s head? a. Frontal b. Coronal c. Sagittal d. Occipital ANS: C The sagittal suture separates the parietal bones on top of the newborn’s head. The frontal suture separates the frontal bones. The coronal suture is said to “crown the head.” There is no occipital suture. The lambdoid suture is at the margin of the parietal and occipital bones. DIF: Cognitive Level: Remember REF: p. 198 TOP: Integrated Process: Nursing PNroUcResSsI:NAGsTsBes.CsmOeMnt MSC: Area of Client Needs: Health Promotion and Maintenance 14. In a newborn’s eyes, strabismus is a normal finding because of: a. congenital cataracts. b. lack of binocularity. c. absence of red reflex. d. inability of pupil to react to light. ANS: B Newborns are unable to focus their eyes on an object. Binocularity does not develop until ages 3 to 4 months. Congenital cataracts, absence of red reflex, and inability of pupil to react to light are not normal findings and need further evaluation. DIF: Cognitive Level: Understand REF: p. 199 TOP: Integrated Process: Nursing Process: Assessment MSC: Area of Client Needs: Health Promotion and Maintenance 15. A nurse has determined that a newborn’s respiratory breathing is within a normal range. How should the nurse document this finding? a. Irregular, abdominal, 30 to 60 breaths/min b. Regular, abdominal, 25 to 35 breaths/min c. Regular, noisy, 35 to 45 breaths/min d. Irregular, quiet, 45 to 55 breaths/min ANS: A The respirations of a normal newborn are irregular and abdominal, with a rate of 30 to 60 breaths/min. Newborn respirations are irregular. Pauses in respiration less than 20 seconds in duration are considered normal. The newborn is an abdominal breather with a wider range of respiratory rates. DIF: Cognitive Level: Understand REF: p. 197 TOP: Integrated Process: Communication and Documentation MSC: Area of Client Needs: Health Promotion and Maintenance 16. When doing the first assessment of a male newborn, the nurse notes that the scrotum is large, edematous, and pendulous. This should be interpreted as a(n): a. normal finding. b. hydrocele. c. absence of testes. d. inguinal hernia. ANS: A A large, edematous, and pendulous scrotum in a term newborn, especially in those born in a breech position, is a normal finding. A hydrocele is fluid in the scrotum, usually unilateral, which usually resolves within a few months. The presence or absence of testes would be determined on palpation of the scrotum and inguinal canal. Absence of testes may be an indication of ambiguous genitalia. An inguinal hernia may be present at birth. It is more easily detected when the child is crying. DIF: Cognitive Level: Apply REF: p. 201 TOP: Integrated Process: Nursing Process: Assessment MSC: Area of Client Needs: Health NPUroRmSoINtioGnTaBn.CdOMMaintenance 17. Stroking the newborn’s cheek along the side of the mouth causes the newborn to turn the head toward that side and begin to suck. This is which reflex? a. Perez b. Sucking c. Rooting d. Extrusion ANS: C Stroking the newborn’s cheek along the side of the mouth causes the newborn to turn the head toward that side and begin to suck is a description of the rooting reflex, which usually disappears by ages 3 to 4 months but may persist for up to 12 months. The Perez reflex involves stroking the newborn’s back when prone; the child flexes extremities, elevating head and pelvis. It disappears at ages 4 to 6 months. The newborn begins strong sucking movements in response to circumoral stimulation. The reflex persists throughout infancy, even without stimulation. Newborns force their tongues outward, when the tongue is touched or depressed. This reflex usually disappears by age 4 months. DIF: Cognitive Level: Understand REF: p. 203 TOP: Integrated Process: Nursing Process: Assessment MSC: Area of Client Needs: Health Promotion and Maintenance 18. Which statement best represents the first stage of the first period of reactivity in the newborn? a. It begins when the newborn awakes from a deep sleep. b. It ends when the amount of respiratory mucus has decreased. c. It is an excellent time to acquaint the parents with the newborn. d. It is an excellent time for mother to sleep and recover. ANS: C During the first period of reactivity, the newborn is alert, cries vigorously, may suck the fist greedily, and appears interested in the environment. The newborn’s eyes are usually wide open, suggesting that this is an excellent opportunity for mother, father, and child to see each other. The second period of reactivity begins when the newborn awakens from a deep sleep. The second period of reactivity ends when the amount of respiratory mucus has decreased. The mother should sleep and recover during the second stage, when the newborn is sleeping. DIF: Cognitive Level: Understand REF: p. 202 TOP: Integrated Process: Nursing Process: Implementation MSC: Area of Client Needs: Health Promotion and Maintenance 19. The nurse observes that a new mother avoids making eye contact with her newborn. The nurse should perform which action? a. Examine newborn’s eyes for ability to focus. b. Assess for other attachment behaviors. c. Recognize this as a common reaction in new mothers. d. Ask mother why she won’t look at newborn. ANS: B Attachment behaviors are thought to indicate the formation of emotional bonds between the newborn and the mother. The mother’s failure to make eye contact with her newborn may indicate difficulties with the formaNtUioRnSIoNfGeTmBo.CtiOonMal bonds. The nurse should perform a more thorough assessment. Newborns do not have binocularity and cannot focus. It is uncommon for a mother to avoid making eye contact with her newborn and it is confrontational to ask why; this would put the mother in a defensive position. DIF: Cognitive Level: Apply REF: p. 205 TOP: Integrated Process: Nursing Process: Implementation MSC: Area of Client Needs: Health Promotion and Maintenance 20. At the time of birth, what is the grayish white, cheeselike substance that normally covers the newborn’s skin called? a. Miliaria b. Meconium c. Amniotic fluid d. Vernix caseosa ANS: D The grayish white, cheeselike substance that normally covers the newborn’s skin is the vernix caseosa. Miliaria are distended sweat glands that appear as minute vesicles. Meconium is the newborn’s first stool. Amniotic fluid is produced in utero. DIF: Cognitive Level: Remember REF: p. 206 TOP: Integrated Process: Nursing Process: Assessment MSC: Area of Client Needs: Health Promotion and Maintenance 21. What are distended sebaceous glands that appear as tiny white papules on cheeks, chin, and nose in the newborn period called? a. Milia b. Lanugo c. Mongolian spots d. Cutis marmorata ANS: A Distended sebaceous glands that appear as tiny white papules on cheeks, chin, and nose in the newborn period are milia, which are common variations found in newborns. Lanugo is fine downy hair. Mongolian spots are irregular areas of deep blue pigmentation, usually in the sacral and gluteal areas. Cutis marmorata is transient mottling when the newborn is exposed to decreased body temperatures. DIF: Cognitive Level: Remember REF: p. 206 TOP: Integrated Process: Nursing Process: Assessment MSC: Area of Client Needs: Health Promotion and Maintenance 22. Where would nonpathologic cyanosis normally be present in the newborn shortly after birth? a. Feet and hands b. Bridge of nose c. Circumoral area d. Mucous membranes ANS: A Cyanosis of the feet and hands is termed acrocyanosis and is a usual finding in newborns. Cyanosis present at the bridge of the nose, the circumoral area, and the mucous membranes is a potential sign of distress or majoNrUaRbSnIoNrGmTaBli.tCyO. M DIF: Cognitive Level: Analyze REF: p. 206 TOP: Integrated Process: Nursing Process: Assessment MSC: Area of Client Needs: Health Promotion and Maintenance 23. What term describes irregular areas of deep blue pigmentation seen predominantly in newborns of African, Asian, Native American, or Hispanic descent? a. Acrocyanosis b. Erythema toxicum c. Mongolian spots d. Harlequin color changes ANS: C Irregular areas of deep blue pigmentation seen predominantly in newborns of African, Asian, Native American, or Hispanic descent are Mongolian spots, which are common variations found in newborns of African, Asian, Native American, or Hispanic descent. Acrocyanosis is cyanosis of the hands and feet that is a usual finding in newborns. Erythema toxicum consists of pink papular vesicles that may appear in 24 to 48 hours and resolve after several days. Harlequin color changes are clearly outlined areas of color change. As the newborn lies on one side, the lower half of the body becomes pink and the upper half is pale. DIF: Cognitive Level: Understand REF: p. 206 TOP: Integrated Process: Nursing Process: Assessment MSC: Area of Client Needs: Health Promotion and Maintenance 24. The nurse observes flaring of nares in a newborn. This should be interpreted as: a. nasal occlusion. b. sign of respiratory distress. c. common response to sneezing. d. snuffles of congenital syphilis. ANS: B Nasal flaring is an indication of respiratory distress. A nasal occlusion would prevent the child from breathing through the nose. Because newborns are obligatory nose breathers, this would require immediate referral. Sneezing and thin white mucus drainage are common in newborns and are not related to nasal flaring. Snuffles are indicated by a thick, bloody, nasal discharge without sneezing. DIF: Cognitive Level: Understand REF: p. 207 TOP: Integrated Process: Nursing Process: Assessment MSC: Area of Client Needs: Physiologic Integrity 25. A nurse has completed an assessment on a newborn. Which finding is considered abnormal? a. Nystagmus b. Profuse drooling c. Dark green or black stools d. Slight vaginal reddish discharge ANS: B Profuse drooling or salivation is a potential sign of a major abnormality. Newborns with esophageal atresia cannot swallow their oral secretions, resulting in excessive drooling. Nystagmus is an involuntary movNemURenStINoGf TthBe.CeOyMes. This is a common variation in newborns. Meconium, the first stool of newborns, is dark green or black. Pseudomenstruation may be present in normal newborns. This is a blood-tinged or mucoid vaginal discharge. DIF: Cognitive Level: Understand REF: p. 207 TOP: Integrated Process: Nursing Process: Assessment MSC: Area of Client Needs: Physiologic Integrity 26. Which is most important in the immediate care of the newborn? a. Maintain patent airway. b. Maintain stable body temperature. c. Administer prophylactic eye care. d. Establish identification of mother and baby. ANS: A Maintaining a patent airway is the primary objective in the care of the newborn. The nurse uses a bulb syringe to clear the pharynx, followed by the nasal passages. Conserving the newborn’s body heat and maintaining a stable body temperature are important, but a patent airway must be established first. These are important functions, but physiologic stability is the first priority in the immediate care of the newborn. DIF: Cognitive Level: Analyze REF: p. 210 TOP: Integrated Process: Nursing Process: Planning MSC: Area of Client Needs: Physiologic Integrity 27. The nurse is careful to place the incubator away from cold windows or air-conditioning units. This is to conserve the newborn’s body heat by preventing heat loss through: a. radiation. b. conduction. c. convection. d. evaporation. ANS: A Radiation is the loss of heat to a cooler solid object. The cold air from either the window or the air conditioner will cool the incubator walls and subsequently the newborn’s body. Conduction involves the loss of heat from the body because of direct contact of the skin with a cooler object. Convection is the loss of heat similar to conduction but aided by air currents. Evaporation is the loss of heat through moisture. The newborn should be quickly dried of the amniotic fluid. DIF: Cognitive Level: Apply REF: p. 210 TOP: Integrated Process: Nursing Process: Implementation MSC: Area of Client Needs: Health Promotion and Maintenance 28. Parents of a newborn ask the nurse why vitamin K is being administered. The nurse accurately responds by explaining phytonadione (vitamin K) is administered to the newborn to: a. prevent bleeding. b. enhance immune response. c. prevent bacterial infection. d. maintain nutritional status. ANS: A Vitamin K is administered to prevNeUntRhSeINmGoTrrBh.CagOiMc disease of the newborn. Vitamin K is synthesized by the intestinal flora. Because the newborn’s intestine is sterile and breast milk is low in vitamin K, a supplemental source must be supplied. The purpose is not to enhance the immune response, prevent bacterial infection, or maintain nutritional status. The major function of vitamin K is to catalyze the liver synthesis of prothrombin, which is needed for blood clotting and coagulation. DIF: Cognitive Level: Apply REF: p. 211 TOP: Integrated Process: Teaching/Learning MSC: Area of Client Needs: Physiologic Integrity 29. In the newborn, intramuscular phytonadione (vitamin K) is administered into which muscle? a. Deltoid b. Dorsogluteal c. Vastus medialis d. Vastus lateralis ANS: D The vastus lateralis is the traditionally recommended injection site. The deltoid and dorsogluteal sites are not recommended for the vitamin K administration. The ventrogluteal may be used as an alternative site to the vastus lateralis. The vastus medialis is not used for intramuscular injections. DIF: Cognitive Level: Apply REF: p. 211 TOP: Integrated Process: Nursing Process: Implementation 30. 30. 31. 31. MSC: Area of Client Needs: Physiologic Integrity Recommendations for hepatitis B (HBV) vaccine include which statement? a. First dose is given between birth and age 2 days. b. First dose is given between ages 12 and 15 months. c. It is not recommended for neonates who are at low risk for hepatitis B. d. It is not recommended for neonates whose mothers are positive for HBV surface antigen. ANS: A To reduce the incidence of HBV in children and its serious consequences in adulthood, the first of three doses is recommended soon after birth and before hospital discharge. Between 12 and 15 months is too late. The recommendation is for the first dose to be given soon after birth. It is recommended for all newborns. Newborns born to mothers who are HBV surface antigen positive should be given the vaccine within 12 hours of birth. They also should be given hepatitis B immune globulin. DIF: Cognitive Level: Understand REF: p. 211 TOP: Integrated Process: Nursing Process: Implementation MSC: Area of Client Needs: Health Promotion and Maintenance A newborn is being discharged at age 48 hours. The parents ask how the newborn should be bathed this first week home. How should the nurse recommend to bathe the newborn? a. Daily with mild soap b. Daily with an alkaline soap c. Two or three times this week with plain water d. Two or three times this week with mild soap NURSINGDOC.COM ANS: C The newborn newborn’s skin has a pH of approximately 5. This acidic pH has a bacteriostatic effect. The parents should be taught to use only plain warm water for the bath and to bathe the child no more than two or three times a week for the first 2 weeks. Soaps are alkaline. They will alter the acid mantle of the child’s skin, providing a medium for bacterial growth. DIF: Cognitive Level: Apply REF: p. 213 TOP: Integrated Process: Teaching/Learning | Integrated Process: Teaching/Learning MSC: Area of Client Needs: Health Promotion and Maintenance 32. The stump of the umbilical cord usually separates in how many days? a. 3 b. 10 to 14 c. 16 to 20 d. 28 ANS: B The average cord separates in 10 to 14 days; 3 days is too soon and 16 to 28 days is too late. The cord should be separated by these times. DIF: Cognitive Level: Remember REF: p. 213 TOP: Integrated Process: Nursing Process: Assessment MSC: Area of Client Needs: Health Promotion and Maintenance 33. The parents of a newborn plan to have him circumcised. They ask the nurse about pain associated with this procedure. What knowledge should the nurse’s response be based on? a. Experience pain with circumcision b. Do not experience pain with circumcision c. Quickly forget about the pain of circumcision d. Are too young for anesthesia or analgesia ANS: A Circumcision is a surgical procedure. The American Academy of Pediatrics has recommended that, when circumcision is performed, procedural analgesia be provided. Pain is associated with surgical procedures. The newborn experiences pain, which can be alleviated with analgesia. Topical and injected analgesia are available for this procedure. DIF: Cognitive Level: Apply REF: p. 214 TOP: Integrated Process: Teaching/Learning MSC: Area of Client Needs: Physiologic Integrity 34. Early this morning, a baby boy was circumcised by using the Plastibell method. When should the nurse tell the mother that the baby can be discharged? a. The newborn voids b. Receiving vitamin K c. Yellow exudate forms over glans d. The Plastibell rim falls off ANS: A The circumcision site is evaluated for excessive bleeding every 30 minutes for at least 2 hours. After these observations and voiding, the newborn can be discharged. The newborn should have received vitamin K soNoUnRaSfItNeGr TdBel.iCvOeMry. This normal yellow exudate will usually form on the second day after the circumcision. Discharge can occur earlier. The Plastibell rim will separate and fall off within 5 to 8 days. The newborn should be discharged before this. DIF: Cognitive Level: Apply REF: p. 215 TOP: Integrated Process: Teaching/Learning MSC: Area of Client Needs: Health Promotion and Maintenance 35. What does the American Academy of Pediatrics recommend as the best form of newborn nutrition? a. Exclusive breastfeeding until age 2 months. b. Exclusive breastfeeding until age 6 months. c. Commercially prepared newborn formula for 1 year. d. Commercially prepared newborn formula until age 4 to 6 months. ANS: B The American Academy of Pediatrics has reaffirmed its position that a newborn be breastfed exclusively for the first six months of life. This group also supports programs that enable women to return to work and continue breastfeeding. Two months is too short of a period. The recommendation is for breastfeeding, not commercial formula. If the mother has stopped breastfeeding, then commercial formula, rather than whole milk, should be used until age 1 year. DIF: Cognitive Level: Understand REF: p. 216 TOP: Integrated Process: Nursing Process: Planning 36. 36. 37. 37. 38. 38. MSC: Area of Client Needs: Health Promotion and Maintenance On what is successful breastfeeding most dependent? a. Mother’s socioeconomic level b. Size of mother’s breasts c. Mother’s desire to breastfeed d. Birth weight of newborn ANS: C The factors that contribute to successful breastfeeding are the mother’s desire to breastfeed, satisfaction with breastfeeding, and available support systems. The mother’s socioeconomic level may affect the mother’s need to return to work and available support systems, but with support, the mother can be successful. The size of the mother’s breasts does not affect the success of breastfeeding. Very low birth weight newborns may be unable to breastfeed. The mother can express milk, and it can be used for the child. DIF: Cognitive Level: Apply REF: p. 216 TOP: Integrated Process: Nursing Process: Planning MSC: Area of Client Needs: Health Promotion and Maintenance What should a nursing intervention to promote parent-newborn attachment include? a. Delaying parent-newborn interactions until the second period of reactivity b. Explaining individual differences among newborns to the parents c. Alleviating stress for parents by decreasing their participation in the newborn’s care d. Allowing a newborn to fuss for a period of time before soothing by holdingANS: B NURSINGDOC.COM Nurses can positively influence the attachment of parent and child by recognizing and explaining individual differences to the parents. The nurse should emphasize the normalcy of these variations and demonstrate the uniqueness of each newborn. The nurse should facilitate parent-newborn interaction during the first period of reactivity. Decreasing the parents’ participation in care will interfere with parent-newborn attachment. The parents should be encouraged to hold the newborn when he or she is fussy and learn how best to soothe their newborn. DIF: Cognitive Level: Apply REF: p. 221 TOP: Integrated Process: Nursing Process: Implementation MSC: Area of Client Needs: Health Promotion and Maintenance A new mother wants to be discharged with her newborn as soon as possible. What should be done prior to discharge? a. Newborn has voided at least once b. Newborn does not spit up after feeding c. Jaundice, if present, appeared before 24 hours d. Appointment is made for home care or a primary care practitioner office visit within next 2 or 3 days ANS: D The American Academy of Pediatrics recommends that newborns discharged early receive follow-up care within 48 hours of a short stay in either a primary practitioner’s office or the home. The child should void every 4 to 6 hours. Spitting up small amounts after feeding is a normal occurrence in newborns. It would not delay discharge. Jaundice within the first 24 hours of life must be evaluated. DIF: Cognitive Level: Apply REF: p. 224 TOP: Integrated Process: Nursing Process: Evaluation MSC: Area of Client Needs: Health Promotion and Maintenance 39. What should nursing interventions to maintain a patent airway in a newborn include? a. Sleeping in the prone (on abdomen) position b. Wrapping neonate as snugly as possible c. Positioning neonate supine while sleeping d. Using bulb syringe to suction as needed, suctioning nose first, and then pharynx ANS: C Supine is the position recommended by the American Academy of Pediatrics to prevent sudden infant death syndrome. Sleeping in the prone position is not advised because of the possible link between sleeping in the prone position and sudden infant death syndrome. The child can be wrapped snugly, but should be placed on side or back. A bulb syringe should be kept by the bedside if necessary, but the pharynx should be suctioned before the nose. DIF: Cognitive Level: Apply REF: p. 210 TOP: Integrated Process: Nursing Process: Implementation MSC: Area of Client Needs: Health Promotion and Maintenance 40. A nurse is assessing the presence NofUeRxSpINecGtTedB.rCeOflMexes in a newborn. Which figure depicts the elicitation of the tonic neck reflex? a. b. c. d. ANS: B The tonic neck reflex is elicited when the newborn’s head is turned to one side; the arm and leg extend on that side, and opposite arm and leg flex (fencing position). The Moro reflex is elicited by sudden jarring or change in equilibrium. The newborn has extension and abduction of extremities and fanning of fingers, with index finger and thumb forming a C shape followed by flexion and adduction of extremities; legs may weakly flex. The dancing reflex is elicited when the newborn is held so that the sole of the foot touches a hard surface; there is a reciprocal flexion and extension of the leg, simulating walking. The crawl reflex is elicited when the newborn is placed on the abdomen; the newborn makes crawling movements with arms and legs. NURSINGDOC.COM DIF: Cognitive Level: Analyze REF: p. 204 TOP: Integrated Process: Nursing Process: Assessment MSC: Area of Client Needs: Health Promotion and Maintenance MULTIPLE RESPONSE 1. A nurse is teaching a class on breastfeeding to expectant parents. Which are contraindications for breastfeeding? (Select all that apply.) a. Human immunodeficiency virus (HIV) in mother b. Mastitis c. Inverted nipples d. Maternal cancer therapy e. Twin births ANS: A, D HIV in the mother and maternal cancer therapy place the newborn at risk. HIV can be transmitted through breast milk, as can be the metabolites of chemotherapy. Mastitis, inverted nipples, and twin births are not contraindications. DIF: Cognitive Level: Apply REF: p. 216 TOP: Integrated Process: Teaching/Learning MSC: Area of Client Needs: Health Promotion and Maintenance 2. A nurse is conducting discharge teaching for parents of a newborn. The nurse instructs the parents on which method of care for the umbilical cord? (Select all that apply.) a. Covering the cord with the diaper b. Cleansing the cord with water daily c. Keeping the cord area free of urine and stool d. Monitoring for signs of infection e. Applying bacitracin ointment to the cord daily ANS: B, C, D Parents are taught to keep the cord area free of urine and stool, cleanse daily with water if needed, and observe for any signs of infection. The diaper should not cover the cord. The diaper is folded in front below the cord to avoid irritation and wetness on the site. Bacitracin ointment should not be applied because the cord area should be kept dry, not moist. DIF: Cognitive Level: Apply REF: p. 225 TOP: Integrated Process: Teaching/Learning MSC: Area of Client Needs: Health Promotion and Maintenance 3. A nurse is planning a teaching session for parents of a newborn who plan to bottle-feed. Which should the nurse include in the teaching session? (Select all that apply.) a. Limiting the feeding to 15 minutes b. Propping the bottle for night feedings is acceptable c. Proper technique for cleansing the bottles and nipples d. Feeding infant on alternate sides of the lap e. Use of bottled water without fluoride should be avoided to mix powdered formula. ANS: C, D, E Parents preparing infant formula mNUusRtSwINaGshTBth.CeiOrMhands well and then wash all of the equipment used to prepare the formula (including the cans of formula) with soap and water. Sterilizing bottles and nipples 5 minutes in boiling water may be required when a hot-water dishwasher is not available. Similar to breastfed infants, bottle-fed infants need to be held on alternate sides of the lap to expose them to different stimuli. Bottled water should not be considered sterile unless otherwise indicated; bottled water without fluoride should be avoided for mixing infant formula. Propping the bottle during infant feedings at nighttime could cause the infant to aspirate. The feeding should not be hurried. Even though they may suck vigorously for the first 5 minutes and seem to be satisfied, infants should be allowed to continue sucking. Infants need at least 2 hours of sucking a day. If there are six feedings per day, then about 20 minutes of sucking at each feeding provide for oral gratification. DIF: Cognitive Level: Apply REF: p. 218 TOP: Integrated Process: Teaching/Learning MSC: Area of Client Needs: Health Promotion and Maintenance 4. A nurse is performing a gestational age assessment on a newborn. The nurse determines that the newborn is “term” if which findings are assessed? (Select all that apply.) a. Posture with fully flexed arms and legs b. Arm recoil brisk c. Square window at 90 degrees d. Scarf sign of elbow crossing over the midline e. Popliteal angle less than 90 degrees ANS: A, B, E A term newborn will have a posture that is fully flexed (arms and legs) and a brisk arm recoil. The popliteal angle in a term infant is less than 90 degrees. The square window should show no angle, the hand should lie flat on the ventral surface of the arm in the term newborn. In a term newborn, the elbow should not cross the midline during assessment of the scarf sign. DIF: Cognitive Level: Analyze REF: p. 193 TOP: Integrated Process: Nursing Process: Evaluation MSC: Area of Client Needs: Health Promotion and Maintenance SHORT ANSWER 1. A nurse is performing a 1-minute Apgar on a newborn. The nurse assesses that the newborn has a heart rate over 100, a good strong cry, some flexion of extremities, sneezes, and has a pink body with blue extremities. The nurse records what number as the Apgar? Record your answer in a whole number. ANS: 8 Sign 0 1 2 Heart rate Absent Slow, <100 beats/min >100 beats/min Respiratory effort Absent Irregular, slow, weak cry Good, strong cry Muscle tone Limp Some flexion of extremities Well flexed Reflex irritability NUR No response Grimace Cry, sneeze Color Blue, pale Body pink, extremities blue Completely pink The newborn gets 2 for heart rate, 2 for respiratory effort, 1 for muscle tone, 2 for reflex irritability and 1 for color = 8 DIF: Cognitive Level: Apply REF: p. 193 TOP: Integrated Process: Nursing Process: Implementation MSC: Area of Client Needs: Physiologic Integrity 2. A nurse is preparing to administer a prescribed phytonadione (vitamin K) injection 0.5 mg intramuscularly to a newborn. The phytonadione (vitamin K) ampule is labeled 1 mg equals 0.5 ml. How many milliliters will the nurse administer? Record your answer using two decimal places. ANS: 0.25 Formula: Desired Available Volume = 0.5 mg 1 mg 0.5 mL = 0.25 mL DIF: Cognitive Level: Apply REF: p. 211 TOP: Integrated Process: Nursing Process: Implementation MSC: Area of Client Needs: Physiologic Integrity NURSINGDOC.COM Chapter 08: Health Problems of Newborns Hockenberry: Wong’s Essentials of Pediatric Nursing, 10th Edition MULTIPLE CHOICE 1. Which is defined as a vaguely outlined area of edematous tissue situated over the portion of the scalp that presents in a vertex delivery? a. Caput succedaneum b. Hydrocephalus c. Cephalhematoma d. Subdural hematoma ANS: A A vaguely outlined area of edematous tissue situated over the portion of the scalp that presents in a vertex delivery is the definition of a caput succedaneum. The swelling consists of serum and/or blood accumulated in the tissues above the bone, and it may extend beyond the bone margin. Hydrocephalus is caused by an imbalance in production and absorption of cerebrospinal fluid. When production exceeds absorption, fluid accumulates within the ventricular system, causing dilation of the ventricles. A cephalhematoma has sharply demarcated boundaries that do not extend beyond the limits of the (bone) suture line. A subdural hematoma is located between the dura and the cerebrum. It would not be visible on the scalp. DIF: Cognitive Level: Remember REF: p. 229 TOP: Integrated Process: Nursing Process: Assessment MSC: Area of Client Needs: Health NPrUoRmSoINtioGnTaBn.CdOMMaintenance 2. Which finding on a newborn assessment should the nurse recognize as suggestive of a clavicle fracture? a. Negative scarf sign b. Asymmetric Moro reflex c. Swelling of fingers on affected side d. Paralysis of affected extremity and muscles ANS: B A newborn with a broken clavicle may have no symptoms. The Moro reflex, which results in sudden extension and abduction of the extremities followed by flexion and adduction of the extremities, will most likely be asymmetric. The scarf sign that is used to determine gestational age should not be performed if a broken clavicle is suspected. Swelling of fingers on affected side and paralysis of affected extremity and muscles are not indicative of a fractured clavicle. DIF: Cognitive Level: Analyze REF: p. 231 TOP: Integrated Process: Nursing Process: Assessment MSC: Area of Client Needs: Health Promotion and Maintenance 3. The parents of a newborn ask the nurse what caused the baby’s facial nerve paralysis. What knowledge should the nurse’s response be based on? a. Genetic defect b. Birth injury c. Spinal cord injury d. Inborn error of metabolism ANS: B Pressure on the facial nerve during delivery may result in injury to cranial nerve VII, which can occur with birth injury. A genetic defect, spinal cord injury, or inborn error of metabolism would not cause facial paralysis. DIF: Cognitive Level: Understand REF: p. 229 TOP: Integrated Process: Teaching/Learning MSC: Area of Client Needs: Health Promotion and Maintenance 4. A mother is upset because her newborn has erythema toxicum neonatorum. What information should the nurse base the response to the mother? a. Easily treated b. Benign and transient c. Usually not contagious d. Usually not disfiguring ANS: B Erythema toxicum neonatorum, or newborn rash, is a benign, self-limiting eruption of unknown cause that usually appears within the first 2 days of life. The rash usually lasts about 5 to 7 days. No treatment is indicated. Erythema toxicum neonatorum is not contagious. Successive crops of lesions heal without pigmentation. DIF: Cognitive Level: Apply REF: p. 233 TOP: Integrated Process: Teaching/Learning MSC: Area of Client Needs: Health NPrUoRmSoINtioGnTaBn.CdOMMaintenance 5. What is oral candidiasis (thrush) in the newborn? a. Bacterial infection that is life threatening in the neonatal period b. Bacterial infection of mucous membranes that responds readily to treatment c. Yeastlike fungal infection of mucous membranes that is relatively common d. Benign disorder that is transmitted from mother to newborn during the birth process only ANS: C Oral candidiasis, characterized by white adherent patches on the tongue, palate, and inner aspects of the cheeks, is not uncommon in newborns. Candida albicans is the usual causative organism. Oral candidiasis is usually a benign disorder in the newborn, often confined to the oral and diaper regions. It is caused by a yeastlike organism and is treated with good hygiene, application of a fungicide, and correction of any underlying disorder. Thrush can be transmitted in several ways, including by maternal transmission during delivery; person-to-person transmission; and contaminated bottles, hands, or other objects. DIF: Cognitive Level: Understand REF: p. 233 TOP: Integrated Process: Nursing Process: Implementation MSC: Area of Client Needs: Health Promotion and Maintenance 6. What does nursing care of the newborn with oral candidiasis (thrush) include? a. Avoiding use of pacifier b. Removing characteristic white patches with a soft cloth c. Continuing medication for a prescribed number of days d. Applying medication to oral mucosa, being careful that none is ingested ANS: C The medication must be continued for the prescribed number of days. To prevent relapse, therapy should continue for at least 2 days after the lesions disappear. Pacifiers can be used. The pacifier should be replaced with a new one or boiled for 20 minutes once daily. One of the characteristics of thrush is that the white patches cannot be removed. The medication is applied to the oral mucosa and then swallowed to treat Candida organisms in the gastrointestinal tract. DIF: Cognitive Level: Apply REF: p. 233 TOP: Integrated Process: Nursing Process: Planning MSC: Area of Client Needs: Physiologic Integrity 7. Which is a bright red, rubbery nodule with a rough surface and a well-defined margin that may be present at birth? a. Port-wine stain b. Juvenile melanoma c. Cavernous hemangioma d. Strawberry hemangioma ANS: D Strawberry hemangiomas or capillary hemangiomas are benign cutaneous tumors that involve capillaries only. They are bright red, rubbery nodules with rough surfaces and well-defined margin. They may or may not be apparent at birth but enlarge during the first year of life and tend to resolve spontaneously by age 2 to 3 years. Port-wine stain is a vascular stain that is a permanent lesion and is present atNbUirRthSI.NInGiTtiBa.lClyOMit is a pink, red, or, rarely, purple stain of the skin that is flat at birth and thickens, darkens, and proportionately enlarges as the child grows. Melanoma is not differentiated into juvenile and adult forms. A cavernous hemangioma involves deeper vessels in the dermis and has a bluish red color and poorly defined margins. DIF: Cognitive Level: Understand REF: p. 235 TOP: Integrated Process: Nursing Process: Assessment MSC: Area of Client Needs: Health Promotion and Maintenance 8. The parents of a newborn with a strawberry hemangioma ask the nurse what the treatment will be. What information does the nurse need to include in the response? a. Excision of the lesion will be necessary. b. Injections of prednisone into the lesion will reduce it. c. No treatment is usually necessary because of the high rate of spontaneous involution. d. Pulsed dye laser treatments will be necessary immediately to prevent permanent disability. ANS: C There is a high rate of spontaneous resolution, so treatment is usually not indicated for hemangiomas. Surgical removal would not be indicated. If steroids are indicated, then systemic prednisone is administered for 2 to 3 weeks. The pulse dye laser is used in the uncommon situation of potential visual or respiratory impairment. DIF: Cognitive Level: Apply REF: p. 235 TOP: Integrated Process: Teaching/Learning MSC: Area of Client Needs: Health Promotion and Maintenance 9. Which term refers to a newborn born before completion of week 37 of gestation, regardless of birth weight? a. Postterm b. Preterm c. Low birth weight d. Small for gestational age ANS: B A preterm newborn is any child born before 37 weeks of gestation, regardless of birth weight. A postterm or postmature newborn is any child born after 42 weeks of gestational age, regardless of birth weight. A low birth weight newborn is a child whose birth weight is less than 2500 g, regardless of gestational age. A small-for-gestational-age (or small-for-date) newborn is any child whose rate of intrauterine growth was slowed and whose birth weight falls below the 10th percentile on intrauterine growth curves. DIF: Cognitive Level: Remember REF: p. 235 TOP: Integrated Process: Nursing Process: Assessment MSC: Area of Client Needs: Health Promotion and Maintenance 10. Which refers to a newborn whose rate of intrauterine growth was slowed and whose birth weight falls below the 10th percentile on intrauterine growth charts? a. Postterm b. Postmature c. Low birth weight d. Small for gestational age NURSINGDOC.COM ANS: D A small-for-gestational-age (or small-for-date) newborn is any child whose rate of intrauterine growth was slowed and whose birth weight falls below the 10th percentile on intrauterine growth curves. A postterm or postmature newborn is any child born after 42 weeks of gestational age, regardless of birth weight. A low birth weight newborn is a child whose birth weight is less than 2500 g, regardless of gestational age. DIF: Cognitive Level: Remember REF: p. 236 TOP: Integrated Process: Nursing Process: Assessment MSC: Area of Client Needs: Health Promotion and Maintenance 11. The nurse is caring for a very low birth weight (VLBW) newborn with a peripheral intravenous infusion. Which statement describes nursing considerations regarding infiltration? a. Infiltration occurs infrequently because VLBW newborns are inactive. b. Continuous infusion pumps stop automatically when infiltration occurs. c. Hypertonic solutions can cause severe tissue damage if infiltration occurs. d. Infusion site should be checked for infiltration at least once per 8-hour shift. ANS: C Hypertonic fluids can damage cells if the fluid leaks from the vein. Careful monitoring is required to prevent severe tissue damage. Infiltrations occur for many reasons, not only activity. The vein, catheter, and fluid used all contribute to the possibility of infiltration. The continuous infusion pump may alarm when the pressure increases, but this does not alert the nurse to all infiltrations. Infusion rates and sites should be checked hourly to prevent tissue damage from extravasations, fluid overload, and dehydration. DIF: Cognitive Level: Understand REF: p. 236 TOP: Integrated Process: Nursing Process: Planning MSC: Area of Client Needs: Physiologic Integrity 12. The nurse is caring for a high-risk newborn with an umbilical catheter in a radiant warmer. The nurse notes blanching of the feet. Which is the most appropriate nursing action? a. Elevate feet 15 degrees. b. Place socks on newborn. c. Wrap feet loosely in prewarmed blanket. d. Report findings immediately to the practitioner. ANS: D Blanching of the feet, in a newborn with an umbilical catheter, is an indication of vasospasm. Vasoconstriction of the peripheral vessels, triggered by the vasospasm, can seriously impair circulation. It is an emergency situation and must be reported immediately. DIF: Cognitive Level: Apply REF: p. 239 TOP: Integrated Process: Nursing Process: Implementation MSC: Area of Client Needs: Physiologic Integrity 13. The mother of a preterm newbornNaUskRsSItNheGTnBur.CseOMwhen she can start breastfeeding. The nurse should explain that breastfeeding can be initiated when her newborn: a. achieves a weight of at least 3 pounds. b. indicates an interest in breastfeeding. c. does not require supplemental oxygen. d. has adequate sucking and swallowing reflexes. ANS: D Research supports that human milk is the best source of nutrition for term and preterm newborns. Preterm newborns should be breastfed as soon as they have adequate sucking and swallowing reflexes and no other complications such as respiratory complications or concurrent illnesses. Weight is not an issue. Interest in breastfeeding can be evaluated by having nonnutritive sucking at the breast during skin-to-skin kangaroo care so the mother and child may become accustomed to each other. Supplemental oxygen can be provided during breastfeeding by using a nasal cannula. DIF: Cognitive Level: Analyze REF: p. 241 TOP: Integrated Process: Teaching/Learning MSC: Area of Client Needs: Health Promotion and Maintenance 14. Which is the most appropriate nursing action when intermittently gavage-feeding a preterm newborn? a. Allow formula to flow by gravity. b. Insert tube through nares rather than mouth. c. Avoid letting newborn suck on tube. d. Apply steady pressure to syringe to deliver formula to stomach in a timely manner. ANS: A The formula is allowed to flow by gravity. The length of time to complete the feeding will vary. Preferably, the tube is inserted through the mouth. Newborns are obligatory nose breathers, and the presence of the tube in the nose irritates the nasal mucosa. Passage of the tube through the mouth allows the nurse to observe and evaluate the sucking response. The feeding should not be done under pressure. This procedure is not used as a timesaver for the nurse. DIF: Cognitive Level: Apply REF: p. 242 TOP: Integrated Process: Nursing Process: Implementation MSC: Area of Client Needs: Physiologic Integrity 15. A healthy, stable, preterm newborn will soon be discharged. The nurse should recommend which position for sleep? a. Prone b. Supine c. Side lying d. Position of comfort ANS: B The American Academy of Pediatrics recommends that healthy newborns be placed to sleep in a supine position. Other positions are associated with sudden infant death syndrome. The prone position can be used for supervised play. DIF: Cognitive Level: Apply NURSINRGETFB:.CpO.M252 TOP: Integrated Process: Teaching/Learning MSC: Area of Client Needs: Health Promotion and Maintenance 16. Which intervention should the nurse implement to maintain the skin integrity of the preterm newborn? a. Cleanse skin with a gentle alkaline-based soap and water. b. Cleanse skin with a neutral pH solution only when necessary. c. Thoroughly rinse skin with plain water after bathing in a mild hexachlorophene solution. d. Avoid cleaning skin. ANS: B The preterm newborn should be given baths no more than two or three times per week with a neutral pH solution. The eyes, oral and diaper areas, and pressure points should be cleansed daily. Alkaline-based soaps might destroy the acid mantle of the skin. They should not be used. The increased permeability of the skin facilitates absorption of the chemical ingredients. The newborn’s skin must be cleaned to remove stool and urine, which are irritating to the skin. DIF: Cognitive Level: Apply REF: p. 245 TOP: Integrated Process: Nursing Process: Implementation MSC: Area of Client Needs: Physiologic Integrity 17. Which is an important nursing action related to the use of tape and/or adhesives on preterm newborns? a. Avoid using tape and adhesives until skin is more mature. b. Use solvents to remove tape and adhesives instead of pulling on skin. c. Remove adhesives with warm water or mineral oil. d. Use scissors carefully to remove tape instead of pulling tape off. ANS: C Warm water, mineral oil, or petrolatum can be used to facilitate the removal of adhesive. In the preterm newborn, often it is impossible to avoid using adhesives and tape. The smallest amount of adhesive necessary should be used. Solvents should be avoided because they tend to dry and burn the delicate skin. Scissors should not be used to remove dressings or tape from the extremities of very small and immature newborns because it is easy to snip off tiny extremities or nick loosely attached skin. DIF: Cognitive Level: Analyze REF: p. 245 TOP: Integrated Process: Nursing Process: Implementation MSC: Area of Client Needs: Physiologic Integrity 18. The nurse is caring for a 3-week-old preterm newborn born at 29 weeks of gestation. While taking vital signs and changing the newborn’s diaper, the nurse observes the newborn’s color is pink but slightly mottled, arms and legs are limp and extended, hiccups are present, and heart rate is regular and rapid. The nurse should recognize these behaviors as manifestations of: a. stress. b. subtle seizures. c. preterm behavior. d. onset of respiratory distress. ANS: A NURSINGDOC.COM Color pink but slightly mottled, arms and legs limp and extended, hiccups, respiratory pauses and gasping, and an irregular, rapid heart rate are signs of stress or fatigue in a newborn. Neonatal seizures usually have some type of repetitive movement from twitching to rhythmic jerking movements. The behavior of a preterm newborn may be inactive and listless. Respiratory distress is exhibited by retractions and nasal flaring. DIF: Cognitive Level: Understand REF: p. 247 TOP: Integrated Process: Nursing Process: Assessment MSC: Area of Client Needs: Physiologic Integrity 19. When is the best time for the neonatal intensive care unit (NICU) nurse to initiate an individualized stimulation program for the preterm newborn? a. As soon as possible after newborn is born b. As soon as parent is available to provide stimulation c. When newborn is over 38 weeks of gestation d. When developmental organization and stability are sufficient ANS: D Newborn stimulation is essential for growth and development. The appropriate time for the introduction of an individualized program is when developmental organization and stability are achieved at approximately 34 and 36 weeks of gestation. The newborn needs to be developmentally ready for a stimulation program. The newborn must be assessed to determine the readiness and appropriateness of the stimulation program. The program should be designed and implemented by the nursing staff. The family can be involved, as the nurses help teach the parents to be responsive to the child’s cues, but the stimulation should not depend on the family’s availability. An individualized stimulation program should be started when the child is developmentally ready. DIF: Cognitive Level: Analyze REF: p. 244 TOP: Integrated Process: Nursing Process: Planning MSC: Area of Client Needs: Health Promotion and Maintenance 20. A preterm newborn, after spending 8 weeks in the NICU, is being discharged. The parents of the newborn express apprehension and worry that the newborn may still be in danger. How should the nurse interpret these statements? a. Normal b. A reason to postpone discharge c. Suggestive of maladaptation d. Suggestive of inadequate bonding ANS: A Parents become apprehensive and excited as the time for discharge approaches. They have many concerns and insecurities regarding the care of their newborn. A major concern is that they may be unable to recognize signs of illness or distress in their newborn. Preparation for discharge should begin early and iNnUclRuSdIeNGheTlBp.iCnOgMthe parent acquire the skills necessary for care. Apprehension and worry are normal adaptive responses. The NICU nurses should facilitate discharge by involving parents in care as soon as possible. DIF: Cognitive Level: Understand REF: p. 248 TOP: Integrated Process: Nursing Process: Planning MSC: Area of Client Needs: Psychosocial Integrity 21. The nurse is planning care for a family expecting their newborn to die. The nurse’s interventions should be based on which statement? a. Tangible remembrances of the newborn (e.g., lock of hair, picture) prolong grief. b. Photographs of newborns should not be taken after the death has occurred. c. Funerals are not recommended because mother is still recovering from childbirth. d. Parents should be encouraged to name their newborn if they have not done so already. ANS: D Naming the deceased newborn is an important step in the grieving process. It gives the parents a tangible person for whom to grieve, which is a key component of the grieving process. Tangible remembrances and photographs can make the newborn seem more real to the parents. Many NICUs will make bereavement memory packets, which may include a lock of hair, handprint, footprints, bedside name card, and other individualized objects. Families need to be informed of their options. The ritual of a funeral provides an opportunity for the parents to be supported by relatives and friends. DIF: Cognitive Level: Analyze REF: p. 248 TOP: Integrated Process: Nursing Process: Planning MSC: Area of Client Needs: Psychosocial Integrity 22. The nurse has been caring for a newborn who just died. The parents are present but say they are “afraid” to hold the dead newborn. Which is the most appropriate nursing intervention? a. Tell them there is nothing to fear. b. Insist that they hold newborn “one last time.” c. Respect their wishes and release body to morgue. d. Keep newborn’s body available for a few hours in case they change their minds. ANS: D When the parents are hesitant about holding and touching their newborn, the nurse should keep the newborn’s body for a few hours. Many parents change their minds after the initial shock of the newborn’s death. This will provide the parents time to see and hold their newborn if they desire. Stating that there is nothing to fear minimizes the parents’ feelings. The nurse should allow the family to parent their child as they wish in death, as in life. Many parents change their minds; if possible, the nurse should wrap the newborn in blankets and keep the newborn’s body on the unit for a few hours. DIF: Cognitive Level: Apply REF: p. 236 TOP: Integrated Process: Nursing Process: Implementation MSC: Area of Client Needs: Psychosocial Integrity 23. The nurse is planning care for a low birth weight newborn. Which is an appropriate nursing intervention to promote adequate oxygenation? a. Place in Trendelenburg position periodically. b. Suction at least every 2 to 3 hoNuUrRs.SINGTB.COM c. Maintain neutral thermal environment. d. Hyperextend neck with nose pointing to ceiling. ANS: C A neutral thermal environment is one that permits the newborn to maintain a normal core temperature with minimal oxygen consumption and caloric expenditure. The Trendelenburg position should be avoided. This position can contribute to increased intracranial pressure (ICP) and reduced lung capacity from gravity pushing organs against diaphragm. Suctioning should be done only as necessary. Routine suctioning may cause bronchospasm, bradycardia due to vagal nerve stimulation, hypoxia, and increased ICP. Neck hyperextension is avoided because it reduces diameter of trachea. DIF: Cognitive Level: Apply REF: p. 239 TOP: Integrated Process: Nursing Process: Implementation MSC: Area of Client Needs: Physiologic Integrity 24. A preterm newborn has been receiving orogastric feedings of breast milk. The nurse initiates nipple feedings, but the newborn tires easily and has weak sucking and swallowing reflexes. What is the most appropriate nursing intervention? a. Encourage mother to breastfeed. b. Try nipple-feeding preterm newborn formula. c. Resume orogastric feedings of breast milk. d. Resume orogastric feedings of formula. ANS: C If a preterm newborn tires easily or has weak sucking when nipple feedings are initiated, the nurse should resume orogastric feedings with the milk of mother’s choice. When nipple feeding is unsuccessful, it is unlikely that the newborn will be able to breastfeed. Breast milk should be continued as long as the mother desires. DIF: Cognitive Level: Apply REF: p. 241 TOP: Integrated Process: Nursing Process: Implementation MSC: Area of Client Needs: Physiologic Integrity 25. The parents of a newborn who has just died decide they want to hold their deceased infant. What is the most appropriate nursing intervention? a. Explain gently that this is no longer possible. b. Encourage parents to accept the loss of their newborn. c. Offer to take a photograph of their newborn because they cannot hold newborn. d. Get the newborn, wrap in a blanket, and rewarm in a radiant warmer so parents can hold their deceased infant. ANS: D The parents should be allowed to hold their newborn in the hospital setting. The newborn’s body should be retrieved and rewarmed in a radiant warmer. The nurse should provide a private place where the parents can hold their child for a final time. A photograph is an excellent idea, but it does not replace the parents’ need to hold the child. DIF: Cognitive Level: Apply REF: p. 250 TOP: Integrated Process: Nursing Process: Implementation MSC: Area of Client Needs: Psychosocial Integrity NURSINGDOC.COM 26. Which statement best describes the clinical manifestations of the preterm newborn? a. Head is proportionately small in relation to the body. b. Sucking reflex is absent, weak, or ineffectual. c. Thermostability is well established. d. Extremities remain in attitude of flexion. ANS: B Reflex activity is only partially developed. Sucking is absent, weak, or ineffectual. The preterm newborn’s head is proportionately larger than the body. Thermoregulation is poorly developed, and the preterm newborn needs a neutral thermal environment to be provided. The preterm newborn may be listless and inactive compared with the overall attitude of flexion and activity of a full-term newborn. DIF: Cognitive Level: Understand REF: p. 250 TOP: Integrated Process: Nursing Process: Assessment MSC: Area of Client Needs: Health Promotion and Maintenance 27. Physiologic jaundice in a newborn can be caused by: a. fetal-maternal blood incompatibility. b. destruction of red blood cells as a result of antibody reaction. c. liver’s inability to bind bilirubin adequately for excretion. d. immature kidneys’ inability to hydrolyze and excrete bilirubin. ANS: C Physiologic jaundice is caused by the immature hepatic function of the newborn’s liver coupled with the increased load from red blood cell hemolysis. The excess bilirubin from the destroyed red blood cells cannot be excreted from the body. The fetal-maternal blood incompatibility and the associated red cell destruction by antibodies are the causes of hemolytic disease of the newborn. The kidneys are not involved in the excretion of bilirubin. 28. 28. 29. 29. 30. 30. DIF: Cognitive Level: Understand REF: p. 255 TOP: Integrated Process: Nursing Process: Assessment MSC: Area of Client Needs: Physiologic Integrity When should the nurse expect breastfeeding-associated jaundice to first appear in a normal newborn? a. 0 to 12 hours b. 12 to 24 hours c. 2 to 4 days d. 4 to 5 days ANS: C Breastfeeding-associated jaundice is caused by decreased milk intake related to decreased caloric and fluid intake by the newborn before the mother’s milk is well established. Fasting is associated with decreased hepatic clearance of bilirubin; 0 to 24 hours is too soon. Jaundice within the first 24 hours is associated with hemolytic disease of the newborn; 4 to 5 days is too late. Jaundice at this time may be due to breast milk jaundice. DIF: Cognitive Level: Understand REF: p. 255 TOP: Integrated Process: Nursing Process: Assessment MSC: Area of Client Needs: Physiologic Integrity NURSINGDOC.COM The newborn with severe jaundice is at risk for developing: a. encephalopathy. b. bullous impetigo. c. respiratory distress. d. blood incompatibility. ANS: A Unconjugated bilirubin, which can cross the blood-brain barrier, is highly toxic to neurons. A newborn with severe jaundice is at risk for developing kernicterus or bilirubin encephalopathy. Encephalopathy is a highly infectious bacterial infection of the skin. It has no relation to severe jaundice and is the most likely complication of severe jaundice. A blood incompatibility may be the causative factor for the severe jaundice. DIF: Cognitive Level: Understand REF: p. 259 TOP: Integrated Process: Nursing Process: Assessment MSC: Area of Client Needs: Physiologic Integrity What is an early clinical manifestation of bilirubin encephalopathy in the newborn? a. Cognitive impairment b. Absence of stooling c. Lethargy or irritability d. Increased or decreased temperature ANS: C Clinical manifestations of bilirubin encephalopathy are those of nervous system depression or excitation. Prodromal symptoms consist of decreased activity, lethargy, irritability, hypotonia, and seizures. Newborns who survive may have evidence of cognitive impairment. Absence of stooling and increased/decreased temperature are not manifestations of bilirubin encephalopathy. DIF: Cognitive Level: Understand REF: p. 259 TOP: Integrated Process: Nursing Process: Assessment MSC: Area of Client Needs: Physiologic Integrity 31. A nurse is assessing for jaundice in a dark-skinned newborn. Where is the best place to assess for jaundice in this newborn? a. Buttocks b. Tip of nose and sclera c. Sclera, conjunctiva, and oral mucosa d. Palms of hands and soles of feet ANS: C Assessing for jaundice is part of the routine physical assessment in newborns. In dark-skinned newborns, the sclera, conjunctiva, and oral mucosa are the best place to observe jaundice because of the lack of skin pigmentation in these areas. The skin pigmentation in the buttocks, tip of nose and sclera, and palms of hands and soles of feet can mask the appearance of jaundice. DIF: Cognitive Level: Apply REF: p. 258 TOP: Integrated Process: Nursing Process: Assessment MSC: Area of Client Needs: Health Promotion and Maintenance NURSINGDOC.COM 32. A blood sample for measurement of bilirubin is required from a newborn receiving phototherapy. In what environment should this blood sample be drawn? a. While phototherapy lights are turned off b. While newborn remains under phototherapy lights c. When newborn is covered with a blanket d. When newborn has been off phototherapy for 30 to 60 minutes ANS: A When blood is drawn, phototherapy lights are turned off, and the blood is transported in a covered tube to avoid a false reading as a result of bilirubin destruction in the test tube. The lights will cause a degradation of the bilirubin in the sample, resulting in a falsely lowered result. The newborn does not need to be covered with a blanket. The phototherapy lights must be off. There is no reason to delay obtaining the blood sample. It can be drawn as soon as the lights are turned off. DIF: Cognitive Level: Apply REF: p. 262 TOP: Integrated Process: Nursing Process: Implementation MSC: Area of Client Needs: Physiologic Integrity 33. The nurse is preparing a parent of a newborn for home phototherapy. Which statement made by the parent would indicate a need for further teaching? a. “I should change the baby’s position many times during the day.” b. “I can dress the baby in lightweight clothing while under phototherapy.” c. “I should be sure that the baby’s eyelids are closed before applying patches.” d. “I can take the patches off the baby during feedings and other caregiving activities.” ANS: B The baby should be placed nude under the lights. The newborn should be repositioned frequently to expose all body surfaces to the lights. The newborn’s eyelids must be closed before the patches are applied because the corneas may become excoriated if in contact with the dressing. The eye patches should be removed during feedings and other caregiving activities so the newborn can have visual and sensory stimulation. DIF: Cognitive Level: Analyze REF: p. 262 TOP: Integrated Process: Teaching/Learning MSC: Area of Client Needs: Physiologic Integrity 34. The nurse is caring for a newborn with hyperbilirubinemia who is receiving phototherapy. Which is an appropriate nursing intervention for this newborn? a. Apply lotion as prescribed to moisturize skin. b. Maintain nothing-by-mouth (NPO) status to prevent nausea and vomiting. c. Monitor temperature to prevent hypothermia or hyperthermia. d. Keep eye patches on for at least 8 to 12 of every 24 hours. ANS: C Newborns who are receiving phototherapy are at risk for thermoregulation issues. The nurse must monitor the newborn’s temperature closely to rapidly detect either hypothermia or hyperthermia. Lotions are not used. They may predispose the newborn to increased tanning or “frying” effect. Newborns receiving phototherapy require additional fluid to compensate for increased fluid losses caused by thNeUlRigShINtsG. TTBh.eCOeyMe patches must be in place whenever the child is under the phototherapy lights. DIF: Cognitive Level: Apply REF: p. 262 TOP: Integrated Process: Nursing Process: Implementation MSC: Area of Client Needs: Physiologic Integrity 35. Hemolytic disease is suspected in a mother’s second newborn. Which factor is important in understanding how this could develop? a. The mother’s first child was Rh positive. b. The mother is Rh positive. c. Both parents have type O blood. d. RhIG (RhoGAM) was given to the mother during her first pregnancy. ANS: A Hemolytic disease of the newborn results from an abnormally rapid rate of red blood cell (RBC) destruction. The major causes of this are Rh and maternal-fetal ABO incompatibility. If an Rh-negative mother has previously been exposed to Rh-positive blood through pregnancy or blood transfusion, antibodies to this blood group antigen may develop so that she is isoimmunized. With further exposure to Rh, the maternal antibodies will agglutinate with the red cells of the fetus who has the antigen and destroy the cells. Hemolytic disease is also caused by ABO incompatibilities. Blood type is the important consideration. If both parents are type O blood, ABO incompatibility would not be a possibility. The mother should have received Rho(D) immune globulin to prevent antibody development after the first pregnancy. DIF: Cognitive Level: Analyze REF: p. 264 TOP: Integrated Process: Nursing Process: Assessment MSC: Area of Client Needs: Physiologic Integrity 36. When should the nurse expect jaundice to be present in a newborn with hemolytic disease? a. At birth b. During first 24 hours after birth c. 24 to 48 hours after birth d. 48 to 72 hours after birth ANS: B In hemolytic disease of the newborn, jaundice is usually evident within the first 24 hours of life. Newborns with hemolytic disease are usually not jaundiced at birth, although some degree of hepatosplenomegaly, pallor, and hypovolemic shock may occur when the most severe form, hydrops fetalis, is present; 24 to 72 hours is too late for hemolytic disease of the newborn. Jaundice at these ages isNmURoSstINliGkTelBy.CdOuMe to physiologic or early-onset breastfeeding jaundice. DIF: Cognitive Level: Understand REF: p. 264 TOP: Integrated Process: Nursing Process: Assessment MSC: Area of Client Needs: Physiologic Integrity 37. To whom is RhIG (RhoGAM) administered to prevent Rh isoimmunization? a. Rh-negative women who deliver an Rh-positive newborn b. Rh-positive women who deliver an Rh-negative newborn c. Rh-negative newborns whose mothers are Rh positive d. Rh-positive fathers before conception of second newborn when first newborn was Rh positive ANS: A RhIG human gamma globulin concentrate of anti-D is administered to all unsensitized Rh-negative women after delivery or abortion of an Rh-positive newborn or fetus. Administering RhIG to an individual who is Rh positive will result in agglutination of red cells and hemolysis. It will not alter the person’s genetic makeup. The anti-D antibody contained in RhIG will have no effect on Rh-negative newborns because the D antibody is not present. DIF: Cognitive Level: Apply REF: p. 265 TOP: Integrated Process: Nursing Process: Planning MSC: Area of Client Needs: Physiologic Integrity 38. 38. 39. 39. 40. 40. The nurse is caring for a newborn receiving an exchange transfusion for hemolytic disease. Assessment of the newborn reveals slight respiratory distress and tachycardia. Which should the nurse’s first action be? a. Notify practitioner. b. Stop the transfusion. c. Administer calcium gluconate. d. Monitor vital signs electronically. ANS: B When signs of cardiac or respiratory problems occur, the procedure is stopped, and the newborn’s cardiorespiratory status is allowed to stabilize. The practitioner is usually performing the exchange transfusion with the nurse’s assistance. The procedure must be stopped so the newborn can stabilize. Respiratory distress and tachycardia are signs of cardiorespiratory problems, not hypocalcemia. Calcium gluconate is not indicated. The vital signs should be monitored electronically throughout the entire procedure. DIF: Cognitive Level: Apply REF: p. 265 TOP: Integrated Process: Nursing Process: Implementation MSC: Area of Client Needs: Physiologic Integrity Which is the primary treatment for hypoglycemia in newborns with feeding intolerance? a. Oral glucose feedings b. Intravenous (IV) infusion of glucose c. Short-term insulin therapy d. Feedings (formula or breast milk) at least every 2 hoursANS: B NURSINGDOC.COM IV infusions of glucose are indicated when the glucose level is very low and when feedings are not tolerated. Early feedings in the normoglycemic newborn are preventive. When the newborn is unable to tolerate feedings or the blood glucose level has become extremely low, then IV infusions are indicated. Insulin administration will further depress the blood glucose level. Feedings can be preventive. The child may not be able to tolerate this frequency. DIF: Cognitive Level: Apply REF: p. 241 TOP: Integrated Process: Nursing Process: Planning MSC: Area of Client Needs: Physiologic Integrity Which is the most appropriate nursing intervention for the newborn who is jittery and twitching and has a high-pitched cry? a. Monitor blood pressure closely. b. Obtain urine sample to detect glycosuria. c. Obtain serum glucose and serum calcium levels. d. Administer oral glucose or, if newborn refuses to suck, IV dextrose. ANS: C These are signs and symptoms of hypocalcemia and hypoglycemia. A blood test is useful to determine the treatment. Laboratory analysis for calcium and blood glucose should be the priority intervention. Monitoring vital signs is important, but recognition of the possible hypocalcemia and hypoglycemia is imperative. A finding of glycosuria would not facilitate the diagnosis of hypoglycemia. A determination must be made between the hypocalcemia and hypoglycemia before treatment can be initiated. DIF: Cognitive Level: Apply REF: p. 283 TOP: Integrated Process: Nursing Process: Implementation MSC: Area of Client Needs: Physiologic Integrity 41. The nurse is planning care for a newborn receiving IV calcium gluconate for treatment of hypocalcemia. Which intervention is the most appropriate during the acute phase? a. Allow newborn to sleep with pacifier to decrease stimuli. b. Keep newborn awake to monitor central nervous system changes. c. Encourage parents to hold and feed newborn to facilitate attachment during illness. d. Awaken newborn periodically to assess level of consciousness. ANS: A For newborns with hypocalcemia, the nurse should manipulate the environment to reduce stimuli that might precipitate a seizure or tremors. A quiet, nonstimulating environment should be maintained for the newborn until calcium levels are normalized. Care should be provided without sudden jarring. Parents can be involved in observations and care when the child is awake. DIF: Cognitive Level: Apply REF: p. 284 TOP: Integrated Process: Nursing Process: Planning MSC: Area of Client Needs: PhysiolNoUgiRcSIInNteGgTriBty.COM 42. Which is the central factor responsible for respiratory distress syndrome? a. Deficient surfactant production b. Overproduction of surfactant c. Overdeveloped alveoli d. Absence of alveoli ANS: A The successful adaptation to extrauterine breathing requires numerous factors, which most term newborns successfully accomplish. Preterm newborns with respiratory distress are not able to adjust. The most likely central cause is the abnormal development of the surfactant system. The deficient production of surfactant results in unequal inflation of alveoli on inspiration and the collapse of the alveoli on end expiration. The number and state of development of the alveoli are not a central factors in respiratory distress syndrome. The instability of the alveoli related to the lack of surfactant is the causative issue. DIF: Cognitive Level: Remember REF: p. 267 TOP: Integrated Process: Nursing Process: Assessment MSC: Area of Client Needs: Physiologic Integrity 43. A preterm newborn of 36 weeks of gestation is admitted to the NICU. Approximately 2 hours after birth, the newborn begins having difficulty breathing, with grunting, tachypnea, and nasal flaring. Which is important for the nurse to recognize? a. This is a normal finding. b. This is not significant unless cyanosis is present. c. Improvement should occur within 24 hours. d. Further evaluation is needed. ANS: D Difficulty breathing, with grunting, tachypnea, and nasal flaring are clinical manifestations of respiratory distress syndrome and require further evaluation. This is not a normal finding and requires further evaluation. Cyanosis may be present, but these are significant findings indicative of respiratory distress without cyanosis. The child’s condition will most likely worsen for approximately 48 hours without intervention. Improvement may begin at 72 hours. DIF: Cognitive Level: Analyze REF: p. 269 TOP: Integrated Process: Nursing Process: Assessment MSC: Area of Client Needs: Physiologic Integrity 44. The nurse is caring for a preterm newborn who requires mechanical ventilation for the treatment of respiratory distress syndrome. What is the preterm newborn at increased risk of due to the mechanical ventilation? a. Alveolar rupture b. Meconium aspiration c. Transient tachypnea d. Retractions and nasal flaring ANS: A Positive pressure introduced by mechanical apparatus has created an increase in the incidence of ruptured alveoli and subsequent pneumothorax and bronchopulmonary dysplasia. Meconium aspiration is not associNaUteRdSwINiGthTmB.eCcOhManical ventilation. Tachypnea may be an indication of a pneumothorax, but it would not be transient. Retractions and nasal flaring are indications of the use of accessory muscles when the newborn cannot obtain sufficient oxygen. The use of mechanical ventilation bypasses the newborn’s need to use these muscles. DIF: Cognitive Level: Understand REF: p. 273 TOP: Integrated Process: Nursing Process: Assessment MSC: Area of Client Needs: Physiologic Integrity 45. The nurse is caring for a newborn with respiratory distress syndrome. The newborn has an endotracheal tube. Which statement describes nursing considerations related to suctioning? a. Suctioning should not be carried out routinely. b. Newborn should be in Trendelenburg position for suctioning. c. Routine suctioning, usually every 15 minutes, is necessary. d. Frequent suctioning is necessary to maintain patency of bronchi. ANS: A Suctioning is not an innocuous procedure and can cause bronchospasm, bradycardia, hypoxia, and increased ICP. It should never be carried out routinely. The Trendelenburg position should be avoided. This position can contribute to increased ICP and reduced lung capacity from gravity pushing organs against diaphragm. Routine suctioning is avoided because of the potential complications of bronchospasm, bradycardia, hypoxia, and increased ICP. DIF: Cognitive Level: Apply REF: p. 267 TOP: Integrated Process: Nursing Process: Implementation MSC: Area of Client Needs: Physiologic Integrity 46. A preterm newborn requires oxygen and mechanical ventilation. Which complications should the nurse assess for? a. Bronchopulmonary dysplasia, pneumothorax b. Anemia, necrotizing enterocolitis c. Cerebral palsy, persistent patent ductus d. Congestive heart failure, cerebral edema ANS: A Oxygen therapy, although lifesaving, is not without hazards. The positive pressure created by mechanical ventilation creates an increase in the number of ruptured alveoli and subsequent pneumothorax and bronchopulmonary dysplasia. Anemia, necrotizing enterocolitis, cerebral palsy, persistent patent ductus, congestive heart failure, and cerebral edema are complications not primarily due to oxygen therapy and mechanical ventilation. DIF: Cognitive Level: Analyze REF: p. 271 TOP: Integrated Process: Nursing Process: Assessment MSC: Area of Client Needs: Physiologic Integrity 47. What causes meconium aspiration syndrome? a. Hypoglycemia b. Carbon dioxide retention c. Bowel obstruction with meconium d. Aspiration of meconium in utero or at birth ANS: D Meconium aspiration syndrome isNcUaRuSseINdGbTyBt.hCeOaMspiration of amniotic fluid containing meconium into the fetal or newborn trachea in utero or at first breath. Hypoglycemia and carbon dioxide retention are not related to meconium aspiration. Bowel obstruction with meconium may be an indication of cystic fibrosis or Hirschsprung disease, not meconium aspiration. DIF: Cognitive Level: Understand REF: p. 272 TOP: Integrated Process: Nursing Process: Assessment MSC: Area of Client Needs: Physiologic Integrity 48. Which is the most common cause of anemia in preterm newborns? a. Frequent blood sampling b. Respiratory distress syndrome c. Meconium aspiration syndrome d. Persistent pulmonary hypertension ANS: A The most common cause of anemia in preterm newborns is frequent blood-sample withdrawal and inadequate erythropoiesis in acutely ill newborns. Microsamples should be used for blood tests, and the amount of blood drawn should be monitored. Respiratory distress syndrome, meconium aspiration syndrome, and persistent pulmonary hypertension are not causes of anemia. They may require frequent blood sampling, which will contribute to the problem of decreased erythropoiesis and anemia. DIF: Cognitive Level: Understand REF: p. 277 TOP: Integrated Process: Nursing Process: Assessment MSC: Area of Client Needs: Physiologic Integrity 49. A newborn is diagnosed with retinopathy of prematurity. What should the nurse know about this diagnosis? a. Blindness cannot be prevented. b. No treatment is currently available. c. Cryotherapy and laser therapy are effective treatments. d. Long-term administration of oxygen will be necessary. ANS: C Cryotherapy and laser photocoagulation therapy can be used to minimize the vascular proliferation process that causes the retinal damage. Blindness can be prevented with early recognition and treatment. Cryotherapy and laser therapy can be used to stop the process. Surgical intervention can be used to repair a detached retina if necessary. Long-term administration of oxygen is one of the causes. Oxygen should be used judiciously. DIF: Cognitive Level: Understand REF: p. 272 TOP: Integrated Process: Nursing Process: Assessment MSC: Area of Client Needs: Physiologic Integrity 50. Several types of seizures can occur in the newborn. Which is characteristic of clonic seizures? a. Apnea b. Tremors c. Rhythmic jerking movements d. Extensions of all four limbs ANS: C NURSINGDOC.COM Clonic seizures are characterized by slow rhythmic jerking movements that occur approximately 1 to 3 per second. Apnea is a common manifestation of subtle seizures. Tremors are not characteristic of seizure activity. They may be indicative of hypoglycemia or hypocalcemia. A clonic seizure would have extension and contraction of the extremities, not just extension. DIF: Cognitive Level: Understand REF: p. 277 TOP: Integrated Process: Nursing Process: Assessment MSC: Area of Client Needs: Physiologic Integrity 51. Newborns are highly susceptible to infection as a result of: a. excessive levels of immunoglobulin A (IgA) and immunoglobulin M (IgM). b. diminished nonspecific and specific immunity. c. increased humoral immunity. d. overwhelming anti-inflammatory response. ANS: B Newborns have diminished inflammatory (nonspecific) and humoral (specific) immunity. They are unable to mount a local inflammatory reaction at the portal of entry to signal infection, and the resulting symptoms are vague and nonspecific, delaying diagnosis and treatment. Newborns have diminished or absent IgA and IgM. Humoral and anti-inflammatory immune responses are diminished in newborns. DIF: Cognitive Level: Understand REF: p. 282 TOP: Integrated Process: Nursing Process: Assessment MSC: Area of Client Needs: Physiologic Integrity 52. Which is most descriptive of the clinical manifestations observed in neonatal sepsis? a. Seizures and sunken fontanels b. Sudden hyperthermia and profuse sweating c. Decreased urinary output and frequent stools d. Nonspecific physical signs with hypothermia ANS: D The clinical manifestations of neonatal sepsis are usually characterized by the newborn generally “not doing well.” Poor temperature control, usually with hypothermia, lethargy, poor feeding, pallor, cyanosis or mottling, and jaundice, may be evident. Seizures and sunken fontanels are not manifestations of the sepsis. Severe neurologic sequelae may occur in low birth weight children with sepsis. Hyperthermia is rare in neonatal sepsis. Urinary output is not affected by sepsis. DIF: Cognitive Level: Understand REF: p. 279 TOP: Integrated Process: Nursing Process: Assessment MSC: Area of Client Needs: Physiologic Integrity 53. The nurse is caring for a newborn whose mother is diabetic. Which clinical manifestations should the nurse expect to see? a. Hypoglycemic, large for gestational age b. Hyperglycemic, large for gestational age c. Hypoglycemic, small for gestational age d. Hyperglycemic, small for gestational age NURSINGDOC.COM ANS: A The clinical manifestations of a newborn born to a mother with diabetes include being large for gestational age, being plump and full-faced, having abundant vernix caseosa, being listless and lethargic, and having hypoglycemia. These manifestations appear a short time after birth. The newborn is hypoglycemic from increased fetal production of insulin and large for gestational age. DIF: Cognitive Level: Understand REF: p. 282 TOP: Integrated Process: Nursing Process: Assessment MSC: Area of Client Needs: Physiologic Integrity 54. The nurse is caring for a newborn who was born 24 hours ago to a mother who received no prenatal care. The newborn is a poor feeder but sucks avidly on his hands. Clinical manifestations also include loose stools, tachycardia, fever, projectile vomiting, sneezing, and generalized sweating. Which should the nurse suspect? a. Seizure disorder b. Narcotic withdrawal c. Placental insufficiency d. Meconium aspiration syndrome ANS: B Newborns exposed to drugs in utero usually show no untoward effects until 12 to 24 hours for heroin or much longer for methadone. The newborn usually has nonspecific signs that may coexist with other conditions such as hypocalcemia and hypoglycemia. In addition, these newborns may have loose stools, tachycardia, fever, projectile vomiting, sneezing, and generalized sweating, which is uncommon in newborns. Loose stools, tachycardia, fever, projectile vomiting, sneezing, and generalized sweating are manifestations not descriptive of seizure activity. Placental insufficiency usually results in a child who is small for gestational age. Meconium aspiration syndrome usually has manifestations of respiratory distress. DIF: Cognitive Level: Apply REF: p. 278 TOP: Integrated Process: Nursing Process: Assessment MSC: Area of Client Needs: Physiologic Integrity 55. Which should the nurse anticipate in the newborn whose mother used cocaine during pregnancy? a. Seizures b. Hyperglycemia c. Cardiac and respiratory problems d. Neurobehavioral depression or excitability ANS: D The nurse should anticipate neurobehavioral depression or excitability and implement care directed at the newborn’s manifestations. Few or no neurologic sequelae appear in newborns born to mothers who use cocaine during pregnancy. The newborn is usually a poor feeder, so hypoglycemia would be a more likely occurrence. Cardiac and respiratory problems are usually not evident in these newborns. DIF: Cognitive Level: Understand NURSINGDOC.COM TOP: Integrated Process: Nursing Process: Assessment MSC: Area of Client Needs: Physiologic Integrity 56. Which is characteristic of newborns whose mothers smoked during pregnancy? a. Large for gestational age b. Preterm, but size appropriate for gestational age c. Growth retardation in weight only d. Growth retardation in weight, length, and head circumference ANS: D Newborns born to mothers who smoke had growth failure in weight, length, and chest circumference when compared with newborns of mothers who did not smoke. A dose-effect relation exists. Newborns have significant growth failure, which is related to the number of cigarettes smoked. DIF: Cognitive Level: Understand REF: p. 287 TOP: Integrated Process: Nursing Process: Planning MSC: Area of Client Needs: Physiologic Integrity 57. Which is an important nursing consideration in preventing the complications of congenital hypothyroidism (CH)? a. Assess for family history of CH. b. Assess mother for signs of hypothyroidism. c. Be certain appropriate screening is done prenatally. d. Be certain appropriate screening is done on newborn. ANS: D Early diagnosis and treatment are essential to prevent the complications of CH. Neonatal screening is mandatory in all 50 United States and territories and is usually obtained in the first 24 to 48 hours of birth. A number of different etiologies exist for CH; family history will identify a small percentage only. The screening can be done postnatally on blood obtained via heel stick. DIF: Cognitive Level: Understand REF: p. 291 TOP: Integrated Process: Nursing Process: Planning MSC: Area of Client Needs: Physiologic Integrity 58. Phenylketonuria (PKU) is a genetic disease that results in the body’s inability to correctly metabolize: a. glucose. b. phenylalanine. c. phenylketones. d. thyroxine. ANS: B PKU is an inborn error of metabolism caused by a deficiency or absence of the enzyme needed to metabolize the essential amino acid phenylalanine. Phenylalanine hydroxylase is missing in PKU. Individuals with this disorder can metabolize glucose. Phenylketones are metabolites of phenylalanine, excreted in the urine. Thyroxine is one of the principal hormones secreted by the thyroid gland. NURSINGDOC.COM DIF: Cognitive Level: Understand REF: p. 292 TOP: Integrated Process: Nursing Process: Assessment MSC: Area of Client Needs: Physiologic Integrity 59. What is the Guthrie blood test use to diagnose in the newborn? a. Down syndrome b. Isoimmunization c. PKU d. Congenital hypothyroidism (CH) ANS: C The Guthrie blood test is an assay commonly used to diagnosis PKU. The test should be performed after the newborn has received postnatal feedings. Down syndrome is diagnosed through chromosomal analysis. Isoimmunization is detected by analysis of blood for unexpected antibodies. CH is diagnosed by analysis of a filter paper blood spot for thyroxine (T4). DIF: Cognitive Level: Remember REF: p. 292 TOP: Integrated Process: Nursing Process: Planning MSC: Area of Client Needs: Physiologic Integrity 60. The screening test for PKU is most reliable if the blood sample is: a. from cord blood. b. taken 14 days after birth. c. taken before oral feedings are initiated. d. fresh blood from the heel. ANS: D Fresh heel-stick blood is the preferred source for the test. Fresh heel-stick blood, not cord blood, must be used. The test must be performed soon after birth so that a low-phenylalanine diet can be instituted if required. The newborn should ingest breast milk or formula before the test is performed. DIF: Cognitive Level: Understand REF: p. 292 TOP: Integrated Process: Nursing Process: Implementation MSC: Area of Client Needs: Physiologic Integrity 61. Which is an important nursing consideration in the care of the newborn with PKU? a. Suggest ways to make formula more palatable. b. Teach proper administration of phenylalanine hydroxylase. c. Encourage the breastfeeding mother to adhere to a low-phenylalanine diet. d. Give reassurance that dietary restrictions are a temporary inconvenience. ANS: A To achieve optimal metabolic control, a restricted phenylalanine diet will probably be required for virtually all individuals with classic PKU throughout life. The nurse and nutritionist should work with families to make the formula more palatable for the newborn. Phenylalanine hydroxylase is not effective because it cannot act within the cell where phenylalanine is metabolized. Partial breastfeeding may be possible, but only with extremely careful monitoring of the newborn’s blood levels. According to the latest research, lifelong dietary restriction may be necessary. NURSINGDOC.COM DIF: Cognitive Level: Apply REF: p. 292 TOP: Integrated Process: Nursing Process: Assessment MSC: Area of Client Needs: Physiologic Integrity MULTIPLE RESPONSE 1. The nurse needs to obtain blood for ongoing assessment of a high-risk newborn’s progress. Which tests should the nurse monitor? (Select all that apply.) a. Blood glucose b. Complete blood count (CBC) c. Calcium d. Serum electrolytes e. Neonatal prothrombin time (PTT) ANS: A, C, D The most common blood tests done on high-risk newborns are blood glucose, bilirubin, calcium, hematocrit, serum electrolytes, and blood gases. Hematocrits rather than CBCs are performed. This will monitor the red cell volume. Neonatal prothrombin time (PTT) is not a test. DIF: Cognitive Level: Understand REF: p. 238 TOP: Integrated Process: Nursing Process: Planning MSC: Area of Client Needs: Physiologic Integrity 2. Which are clinical manifestations of the postterm newborn? (Select all that apply.) a. Excessive lanugo b. Increased subcutaneous fat c. Absence of scalp hair d. Parchment-like skin e. Minimal vernix caseosa f. Long fingernails ANS: D, E, F In postterm newborns, the skin is often cracked, parchment-like, and desquamating; there is little to no vernix caseosa; and fingernails are long. Lanugo is usually absent in postterm newborns. Subcutaneous fat is usually depleted, giving the child a thin, elongated appearance. Scalp hair is usually abundant. DIF: Cognitive Level: Understand REF: p. 255 TOP: Integrated Process: Nursing Process: Assessment MSC: Area of Client Needs: Health Promotion and Maintenance 3. The nurse is preparing to care for a newborn receiving phototherapy. Which interventions are appropriate? (Select all that apply.) a. Avoid stimulation. b. Decrease fluid intake. c. Expose all the newborn’s skin. d. Monitor skin temperature closely. e. Reposition the newborn every 2 hours. f. Cover the newborn’s eyes withNUeyReSIsNhGieTlBds.CoOrMpatches. ANS: D, E, F Several nursing interventions are instituted to protect the newborn during phototherapy. Temperature is closely monitored to prevent hyperthermia or hypothermia. The newborn is repositioned every 2 hours to maximize exposure to the phototherapy and to prevent skin breakdown. The infant’s eyes are shielded by an opaque mask to prevent exposure to the light. The newborn is clothed in a diaper because a side effect of phototherapy includes loose, greenish stools. Other side effects include increased metabolic rate; dehydration; electrolyte disturbances, such as hypocalcemia; and priapism. Infants receiving phototherapy may require additional fluid volume to compensate for insensible and intestinal fluid loss. The infant should receive adequate stimulation, which includes feeding and touching. DIF: Cognitive Level: Apply REF: p. 258 TOP: Integrated Process: Nursing Process: Planning MSC: Area of Client Needs: Safe and Effective Care Environment 4. A nurse is planning care for a preterm newborn. Which interventions should the nurse implement for skin care? (Select all that apply.) a. Use cleaning agents with neutral pH. b. Rub skin during drying. c. Use adhesive remover solvent when removing tape. d. Avoid removing adhesives for at least 24 hours. e. Consider pectin barriers beneath adhesives. ANS: A, D, E The skin care for a preterm newborn should include use of pH-neutral cleanser or soaps no more than two or three times a week. Adhesives should not be removed for at least 24 hours after application. Pectin barriers should be used beneath adhesives to protect skin. Avoid rubbing skin during bathing or drying. Do not use adhesive remover, solvents, or bonding agents. Adhesive removal can be facilitated using water, mineral oil, or petrolatum. DIF: Cognitive Level: Apply REF: p. 259 TOP: Integrated Process: Nursing Process: Implementation MSC: Area of Client Needs: Physiologic Integrity 5. A nurse is assessing a preterm newborn for the possibility of necrotizing enterocolitis (NEC). Which assessment findings should the nurse expect to find if NEC is confirmed? (Select all that apply.) a. Minimal gastric residual b. Abdominal distention c. Apnea d. Urinary output at 2 ml/kg/hr e. Unstable temperature ANS: B, C, E The nurse should observe for indications of early development of NEC by checking the appearance of the abdomen for distention (measuring abdominal girth, measuring residual gastric contents before feedings, and listening for bowel sounds) and performing all routine assessments for high-risk neonates. The preterm newborn may have apnea and unstable temperature if NEC is developing. The urinary output will be decreased and will be below the expected 2 ml/kg/hr. NURSINGDOC.COM DIF: Cognitive Level: Apply REF: p. 281 TOP: Integrated Process: Nursing Process: Assessment MSC: Area of Client Needs: Physiologic Integrity 6. A nurse is admitting a preterm newborn to the NICU. Which interventions should the nurse implement to prevent retinopathy? (Select all that apply.) a. Place on pulse oximetry. b. Decrease exposure to bright, direct lighting. c. Place on a cardiac monitor. d. Cover eyes with an eye shield at night. e. Use supplemental oxygen only when needed. ANS: A, B, E To prevent retinopathy, the nurse should provide preventive care by closely monitoring blood oxygen levels, responding promptly to saturation alarms, and preventing fluctuations in blood oxygen levels. Pulse oximetry is recommended to monitor the infant’s oxygenation status during resuscitation and to prevent excessive use of oxygen in both term and preterm infants. Decrease exposure to bright, direct lighting; although exposure to bright light has not been proven to contribute to retinopathy of prematurity, such exposure is undesirable from a neurobehavioral developmental perspective. Use supplemental oxygen judiciously and monitor oxygen blood levels carefully; prevent wide fluctuations in oxygen blood levels (hyperoxia and hypoxia). Placing the newborn on a cardiac monitor will not prevent retinopathy. Covering the eyes with eye shields is not a preventive measure for retinopathy. DIF: Cognitive Level: Apply REF: p. 272 TOP: Integrated Process: Nursing Process: Implementation MSC: Area of Client Needs: Physiologic Integrity 7. A nurse is assessing a preterm newborn. Which assessment findings are consistent with prematurity? (Select all that apply.) a. Abundant lanugo over the body b. Ear cartilage soft and pliable c. Flexed body posture d. Deep creases on the sole of the foot e. Skin is bright pink, smooth, and shiny. ANS: A, B, E The preterm newborn has fine lanugo hair that is abundant over the body. The ear cartilage is soft and pliable, and the soles and palms have minimal creases, resulting in a smooth appearance. The preterm newborn’s skin is bright pink (often translucent, depending on the degree of immaturity), smooth, and shiny, with small blood vessels clearly visible underneath the thin epidermis. In contrast to full-term infants’ overall attitude of flexion and continuous activity, preterm infants may be inactive and listless. The extremities maintain an attitude of extension and remain in any position in which they are placed. DIF: Cognitive Level: Apply REF: p. 266 TOP: Integrated Process: Nursing Process: Assessment MSC: Area of Client Needs: Physiologic Integrity 8. A nurse is reviewing acid-base laboratory data on a newborn admitted to the NICU for meconium aspiration. Which laboNraUtoRrSyINvGalTuBe.sCsOhMould the nurse report to the physician? (Select all that apply.) a. pH: 7.35 b. PCO2: 49 c. HCO3-: 30 d. PaO2: 96 ANS: B, C Normal values of pH for a newborn are: Birth: 7.11–7.36 1 day: 7.29–7.45 Child: 7.35–7.45. Normal values of PCO2 are: Newborn: 27–40 mm Hg Infant: 27–41 mm Hg Girls: 32–45 mm Hg Boys: 35–48 mm Hg. Normal values for HCO3- are: Infant: 21–28 mEq/ml Thereafter: 22–26 mEq/ml. The PaO2 is within normal limits for a newborn. Therefore, the nurse should report the PCO2 of 49 and the HCO3- of 30. DIF: Cognitive Level: Analyze REF: p. 270 TOP: Integrated Process: Nursing Process: Evaluation MSC: Area of Client Needs: Physiologic Integrity NURSINGDOC.COM [Show More]
Last updated: 1 year ago
Preview 1 out of 232 pages
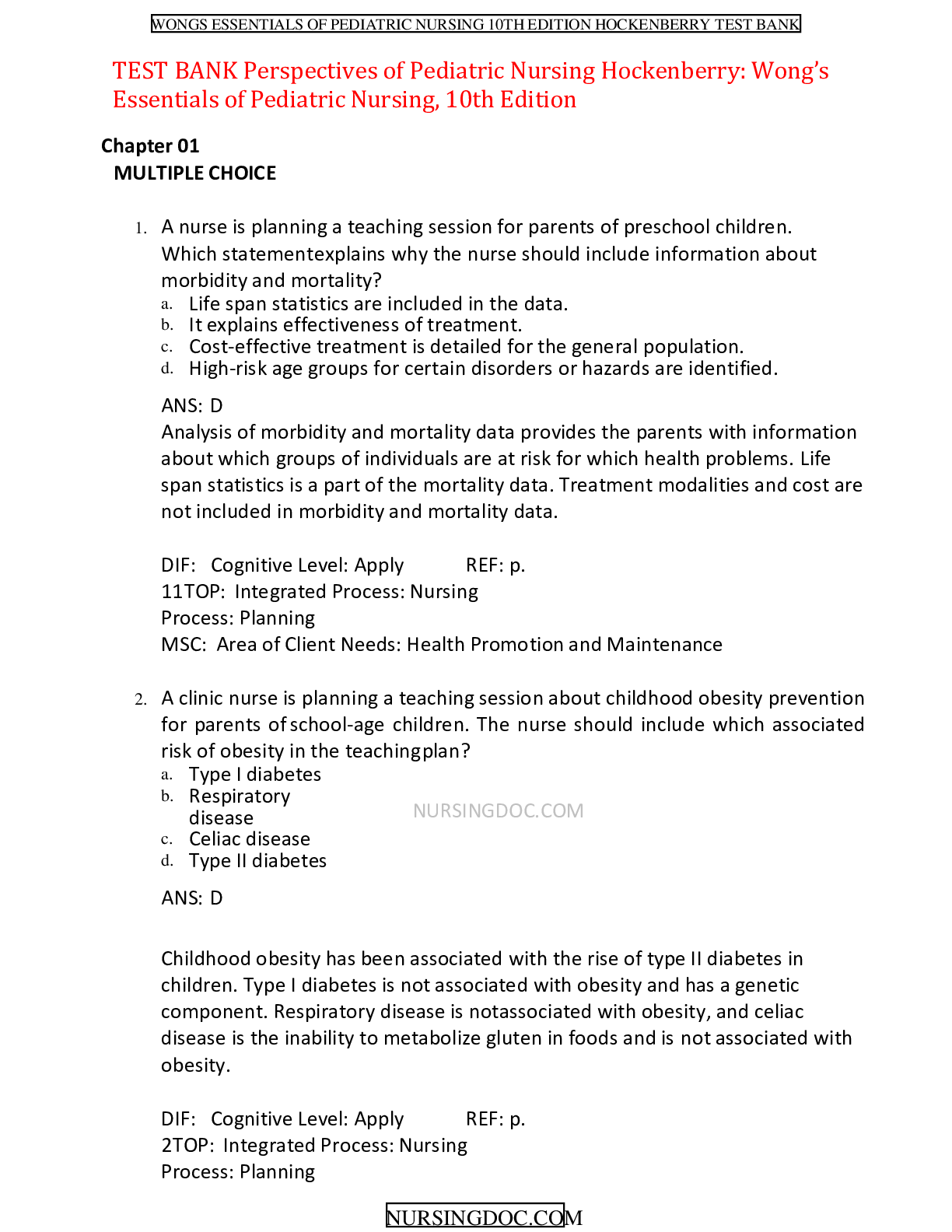
Reviews( 0 )
Document information
Connected school, study & course
About the document
Uploaded On
Dec 20, 2022
Number of pages
232
Written in
Additional information
This document has been written for:
Uploaded
Dec 20, 2022
Downloads
0
Views
44