*NURSING > SHADOW HEALTH > Week 9 - Comprehensive Assessment, Tina Jones - REQUIRED Results | Turned In Advanced Health Assessm (All)
Week 9 - Comprehensive Assessment, Tina Jones - REQUIRED Results | Turned In Advanced Health Assessment and Diagnostic Reasoning ,100% CORRECT
Document Content and Description Below
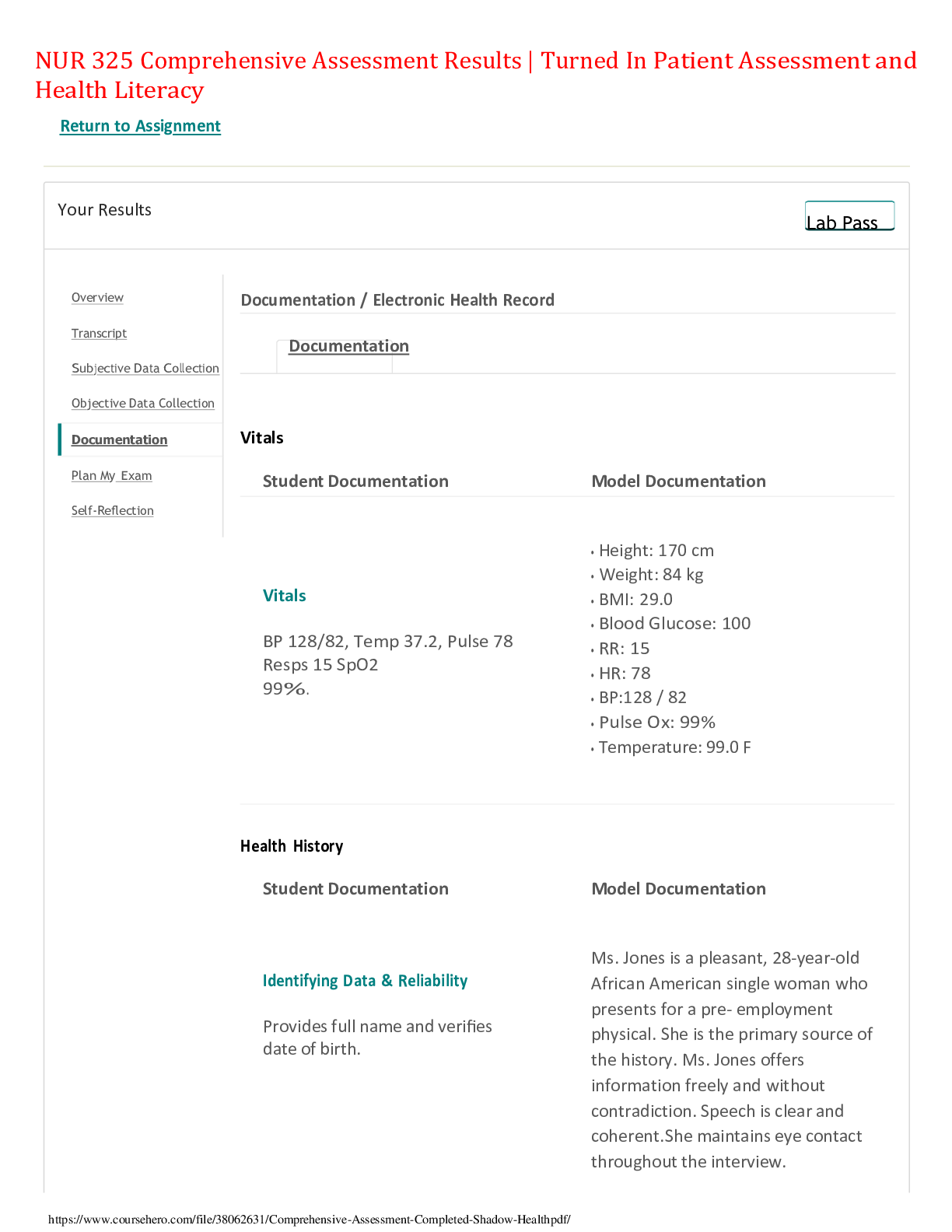
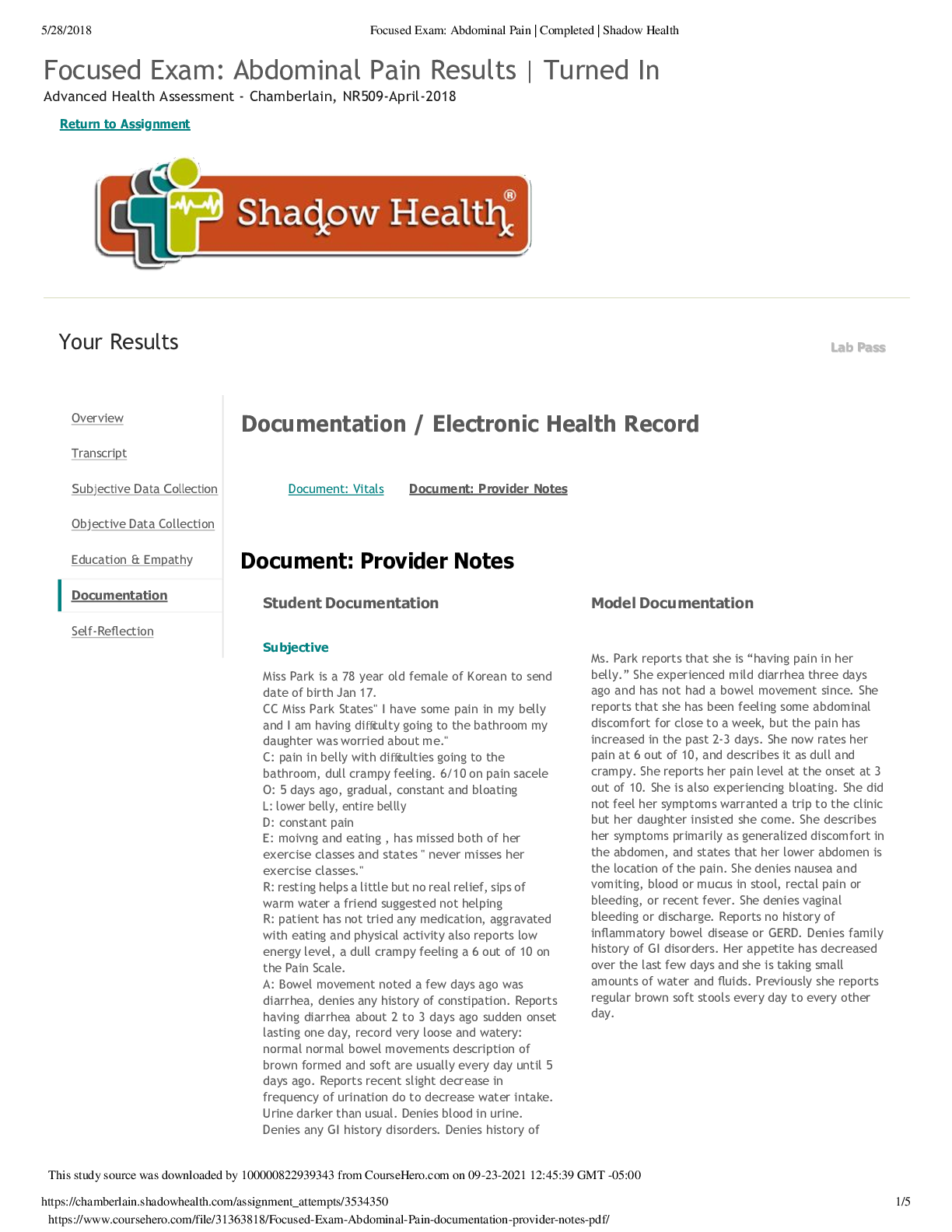
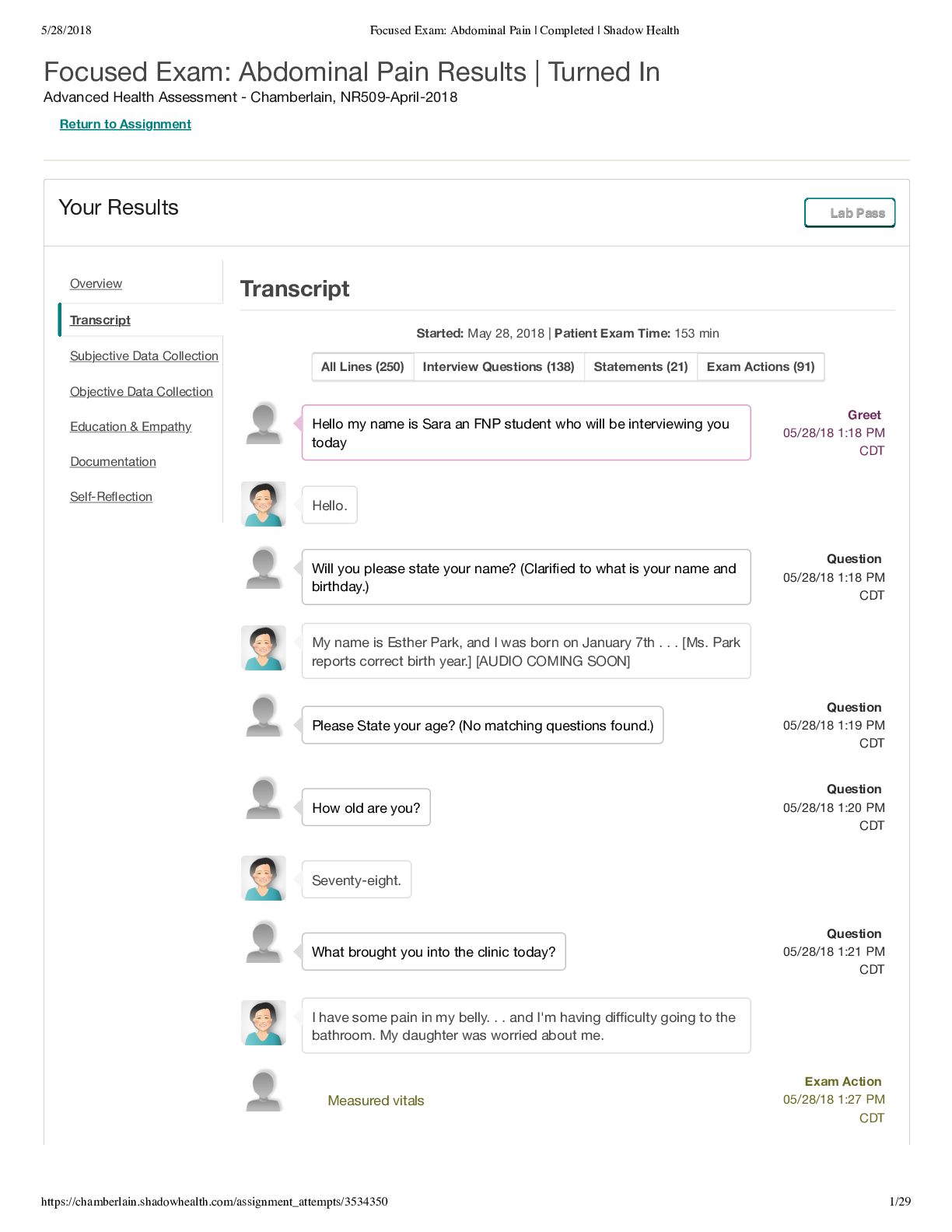
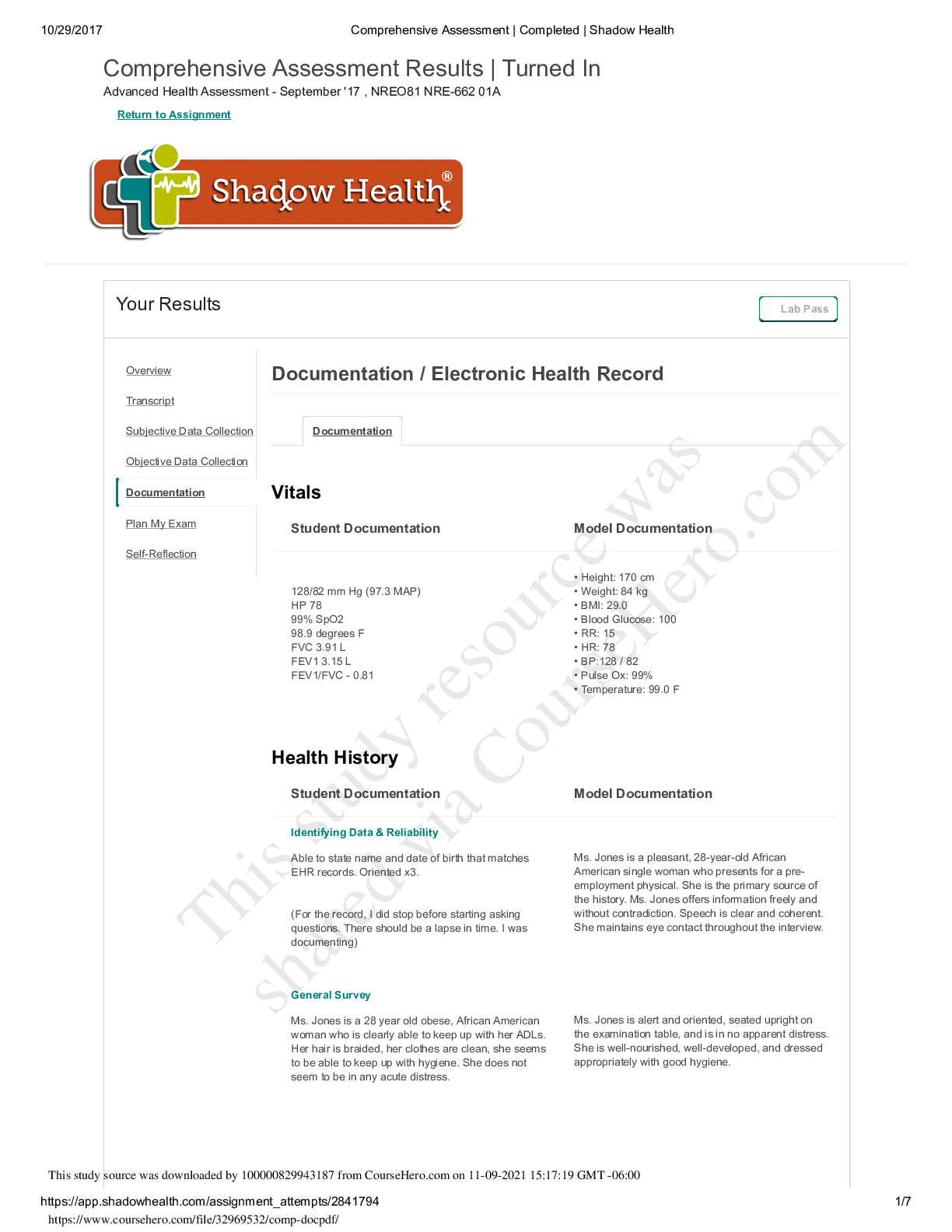
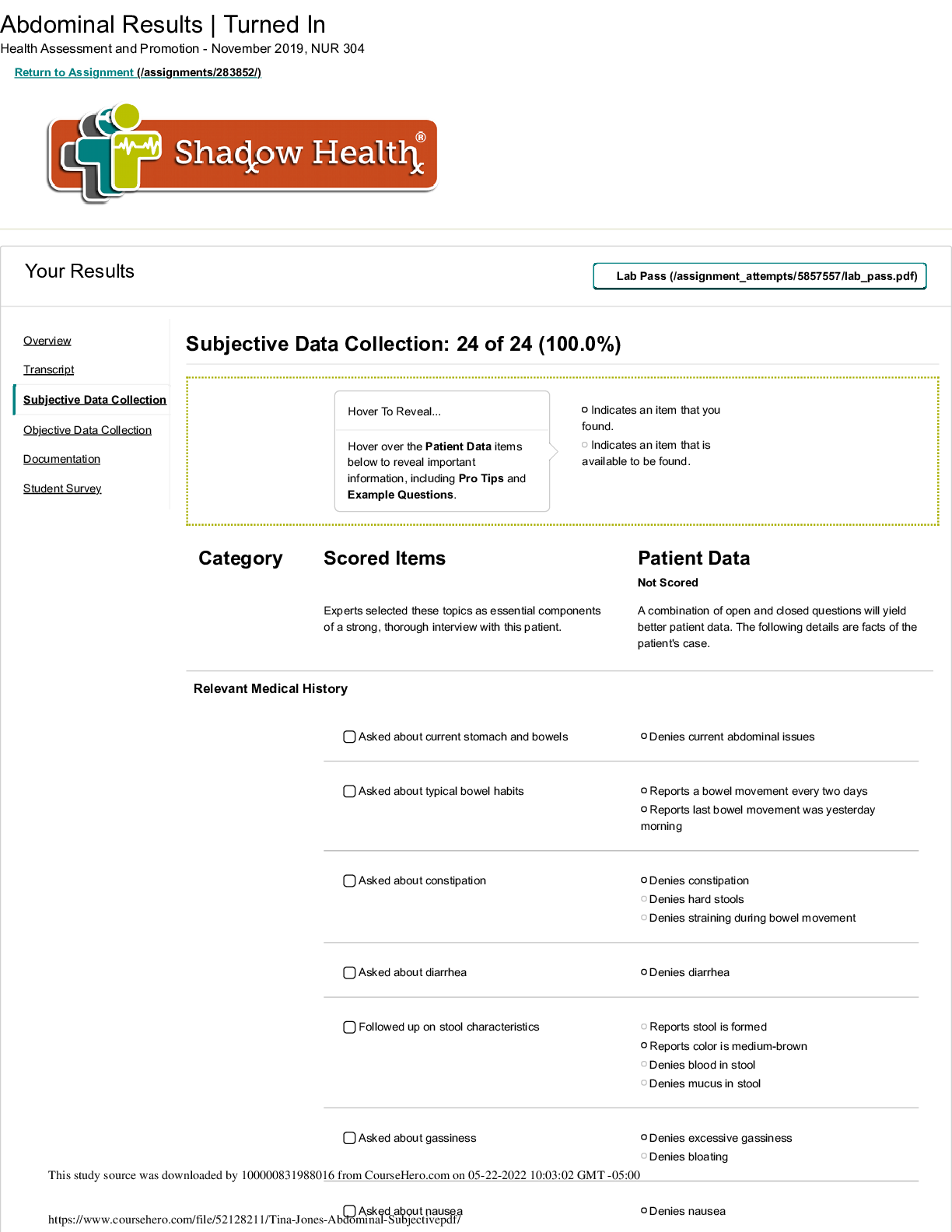
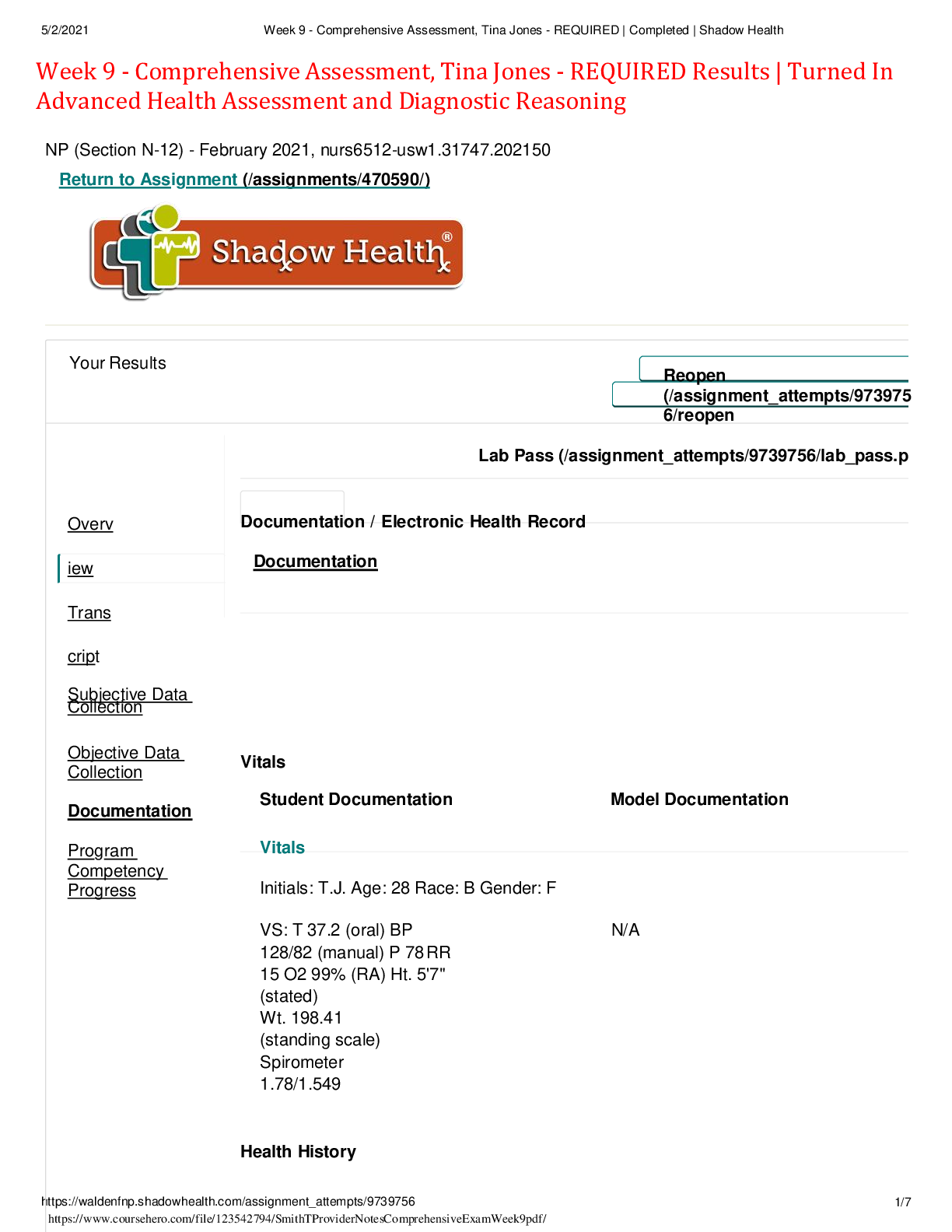
Week 9 - Comprehensive Assessment, Tina Jones - REQUIRED Results | Turned In Advanced Health Assessment and Diagnostic Reasoning NP (Section N-12) - February 2021, nurs6512-usw1.31747.202150 Ret... urn to Assignment (/assignments/470590/) Your Results Reopen (/assignment_attempts/9739756/reopen Lab Pass (/assignment_attempts/9739756/lab_pass.p Overview Transcript Subjective Data Collection Documentation / Electronic Health Record Documentation Objective Data Collection Documentation Program Competency Progress Vitals Student Documentation Model Documentation Vitals Initials: T.J. Age: 28 Race: B Gender: F VS: T 37.2 (oral) BP 128/82 (manual) P 78 RR 15 O2 99% (RA) Ht. 5'7" (stated) Wt. 198.41 (standing scale) Spirometer 1.78/1.549 N/A Health History Student Documentation Model Documentation Identifying Data & Reliability Miss Jones is a 28 y/o BF who presents to the clinic for a pre- employment physical. She is polite, cooperative, and speech is clear and appropriate to context. Makes appropriate eye contact. Miss Jones is unaccompanied for this visit. She is the primary source of data collection and is a reliable historian for this exam. N/A General Survey Miss Jones is a well-dressed, polite, moderately obese female. She is AAO x 3. She answers questions appropriately and appears to be in no acute distress or discomfort. Her VS are stable and she denies current pain or distress. N/A Reason for Visit The patient presents to the clinic for a pre-employment physical exam. N/A This study source was downloaded by 100000802531269 from CourseHero.com on 11-29-2022 21:38:18 GMT -06:00 Support History of Present Illness Patient presents to the clinic requesting physical exam for new job. She states she is in good health and was recently diagnosed with PCOS. N/A Medications Metformin 850 mg po one tab twice daily for DM Flovent two puffs twice daily for asthma Proventil two puffs prn for asthma Yaz (drosperenone/ethinyl estradiol) one tab by mouth daily for birth control. (Patient does not know dosage) Advil (OTC) prn for cramps (denies knowing dosage) N/A Allergies Penicillin-rash Cats-causes sneezing N/A Medical History Dibetes Mellitus (2016) Asthma (unknown date-childhood) PCOS (2020) No surgical history. Allergies: Penicillin (rash), Cats (nasal drainage and asthma occurrence). N/A Health Maintenance Follows a healthy diet with whole grains, fruits/vegetables, and moderate protein. Avoids sugar, tobacco, and drug use. Minimal alcohol consumption. Exercises daily. Takes medications as prescribed by physician. Maintains low-stress life-style. Practices good mental health. Wears seatbelt while in moving vehicle. She performs self-breast exams monthly and reports her last pap smear four months prior. Her last eye exam was three months ago and she was prescribed corrective lenses. Her last dental appointment was three months prior and she reports no negative findings. She received a flu vaccine in 2020 and received her first Covid vaccine in February of 2021. Monitors blood glucose daily. N/A Family History Father (deceased)-MVA. DM, HTN, Hyperlipidemia Mother-HTN, Hyperlipidemia. Paternal Grandfather (deceased)-Colon CA, HTN, DM. Paternal Grandmother-living. No significant health history. Maternal Grandmother (deceased)-CVA. HTN, Hyperlipidemia. Mother-Hyperlipidemia, HTN. Maternal Grandfather (deceased)-Heart disease. N/A Social History Miss Jones is a 28 y/o female who lives in a suburan area in a single story home with her mother and sister. She is a recent college graduate and is a full-time employee at a shipping company. She enjoys Bible study, reading, getting together with her friends, yoga, and cooking. She reports feeling secure and safe in her environment. She has both health and dental insurance and there are no financial issues within the household. She denies tobacco, illicit drug, and sexual activity. She drinks in moderation and defines herself as a "social drinker". The home is secured with CO2 monitors and smoke detectors. She wears a seatbelt while in a moving vehicle. She maintains a healthy diet of fruits, vegetables, and moderate protein. She avoids sugar and consumes carbohydrates in moderation. N/A Mental Health History She denies depression, suicidal ideations, or anxiety. She denies any diagnosis of mental illness. N/A Review of Systems - General General: Denies fever, chills, fatigue, or genralized weakness. She reports a weight loss of 5 lbs. but relates it to healthier eating/diet. She reports prior insomnia has abated. . N/A HEENT Student Documentation Model Documentation Subjective Head: Denies headaches, dizziness, LOC, or trauma. Wear corrective lenses. Denies hearing loss or changes in hearing, tinnitus, vertigo, or excess cerumen. Denies nasal discharge, congestion, or epistaxis. Denies dysphagia, sore throat, or hoarseness. Denies dry mouth, ulcerations, or bleeding gums. Neck: Denies stiffness, decreased ROM, masses, or nodules. N/A Objective Head: Normocephalic with even distribution of hair. Hair full, healthy, and shiny without evidence of thinning or breakage. No flaking to scalp noted. Atraumatic without lesions, masses, or bruising. Eyes: Visual acuity intact at 20/20 per Snellen chart (with corrective lenses). Visual acuity 20/35 without correction. Conjunctiva clear without exudate, crusting, or petechiae. PERRLA. 3+/brisk. EOM intact. Convergence normal at 7 cm. Sclera non-icteric. Fundi normal. Negative for nystagmus, strabismus, and ptosis. Ears: Equal placement bilaterally. Pinna, ear canals, and tragus without tenderness or swelling. Bilateral ear canals without discharge or drainage. Tympanic membrane normal in appearance without evidence of bulging or grayness. Minimal cerumen observed on inspection bilaterally. Hearing intact and normal as evidenced by the whisper test. Nose: Placement midline and centered of facial map. Straight with bulbous tip. Pink, moist nasa mucosa. Septum midline without deviation upon palpation. No tenderness to sinus space bilaterally upon palpation. Bilateral patency of nares. Nasal turbinates pink without bogginess. Throat: Oral mucosa pink and moist. Teeth intact without caries. No fetid breath. Tongue midline, pink, and moist without deviation. Symmetrical movement of tongue. No ulers or lesions observable. Gums pink without hemorrhagia. Negative for tonsillar swelling, pustules, or exudate. No adenopathy noted. Gag reflex intact. Negative for dysphagia. Pharynx normal in appearance. Neck: Supple and smooth without nodules or palpable masses. Non-tender without lymphadenopathy. ROM intact without deviation. Thyroid smooth without goiters. Jaw with full ROM and negative for clicks. No JVD. N/A Respiratory Student Documentation Model Documentation Subjective Respiratory: Denies SOB at rest or with exertion. Denies dyspnea, wheezing, or cough. Denies any exposure to person(s) with known TB and denies night sweats. N/A Objective Respiratory: Lungs clear to auscultation bilaterally without rales, rhonchi, or wheezing. Bilateral chest symmetrical. Anterior and posterior expansion symmetrical. Posterior and anterior tactile fremitus equal bilaterally. Resonance heard throughout all lung fields. No SOB/dyspnea upon exertion or at rest. Respirations even and unlabored. RR 15. N/A Cardiovascular Student Documentation Model Documentation Subjective CV: Denies chest pain, tightness, or pressure. Denies palpitations, arrhythmias, or increased BP. Denies edema or claudication. Denies varicose veins. N/A Objective CV: S1S2 auscultated. RRR without murmurs, bruits, gallops, or clicks. Capillary refill less than 3 seconds to upper and lower extremities. Well-perfused extremities without edema. PMI to anterior chest non-displaced wihtout heaves or clicks. All pulses (radial, brachial, femoral, popliteal, tibial, and dorsalis pedis) noted at 2+ (moderate). Carotid pulses 2+ bilaterally/negative for bruit. All arteries (femoral, iliac, renal, abdominal) negative for bruits. No cyanosis observed. No pursed lip breathing noted. All points of chest auscultated without positive abnormal findings. N/A Abdominal Student Documentation Model Documentation Subjective GI: Denies abdominal pain, tenderness, distention, or discomfort. Denies heartburn, indigestion, or n/v. Confirms daily BM's of normal texture and color. Denies constipation or diarrhea. N/A Objective Abdomen: Soft, rounded, moderately obese without tenderness or masses. Normoactive BS in all quadrants. Tympany heard in all quadrants. Negative for hepatosplenomegaly. Spleen is without dullness/non-palpable. No umbilical herniation palpated. Liver palpable 1 cm below RCM. Liver span 7 cm MCL on percussion. Negative BM presently. Positive upon inspection for multiple abdominal striae and hirsutism at linea nigra. N/A Musculoskeletal Student Documentation Model Documentation Subjective MS: Denies joint pain, swelling, or tenderness to joints. Denies redness at joints. Denies restricted or impaired ROM to upper or lower extremities. Reports no difficulty in performing ADL's. Denies gait imbalance, falls, fractures, or muscle pain. Reports no difficulty in performing ROM. N/A Objective MS; Posture appropriate without abnormal spinal curvature or kyphosis. Equal and full ROM to both upper and lower extremities. Bilateral hand/finger grips equal 5/5. Strength 5/5 thoughout musculature with positive and equal tone appropriate for age. MAE without difficulty or decreased ROM. Bilater hip strength 5/5 without audible clicks. Shoulder strength 5/5 with shrugging. Bilateral feet with decreased arch support. Negtive for pain associated with decrease. ROM to neck equal with both extension and flexion. Spinal extension and flexion poitive with full ROM.. No redness, swelling, or tenderness to joints or musculature. No trauma or fractures. Full ROM to all distal and proximal joints. Negative for limited Achilles flexion or extension. N/A Neurological Student Documentation Model Documentation Subjective Neurological: Denies numbness, tingling, or loss of sensation. Denies LOC, speech impediments or alterations in speech. Denies functional loss in extremities. Denies loss of memory or forgetfulness. N/A Objective Neurological: Patient is AAOx3. No LOC. Both short and long term memory intact. Cranial nerves I-XII intact without deviation to all sensations. Hand speed, rhythm, and smoothness appropriate and within normal expectations. Graphasthesia test poitive with "A" and "8" identified appropriately. Sterognosis positive with identification of key, coin, and paperclip. No unilateral impairment observed or noted. DTR 2+/positive to R/L triceps, biceps, patella, achilles, and brachioradial areas. No sensory loss or loss of sensation. Gait and balance steady and intact without alteration from normal functioning ability. Heel-to-shin test succesful. Full neurological exam within normal limits for patient/age. N/A Skin, Hair & Nails Student Documentation Model Documentation Subjective Integumentary: Denies rash, itching, blisters, or lesions. Reports mole on right upper shoulder but denies changes in size or color. Denies bruising easily. Reports excessive hair growth extending upward from pubic area onto abdomen. Reports striae on abdomen and hip area (anterior and posterior). Denies hair loss, thinning, or dryness of scalp. Denies ridges or changes to nail beds. N/A Objective Integumentary: Skin W/D/I with good turgor and color appropriate for race. No rashes, blisters, lesions, or bruising. Postive for striae to abdominal/hip areas. Striae purple in color/faded. No scaling, flaking, or vitiligo noted. Extension of pubic hair upwards along the linea nigra. Brown mole with established borders approximately .25 cm noted to posterior upper right scapula. N/A © Shadow Health® 2012 - 2021 (800) 860-3241 | Help Desk (https://support.shadowhealth.com/) | Terms of Service (/static/terms_of_service) | Privacy Policy (/static/privacy_policy) | Patents (https://www.shadowhealth.com/patents) [Show More]
Last updated: 1 year ago
Preview 1 out of 13 pages
Instant download
Buy this document to get the full access instantly
Instant Download Access after purchase
Add to cartInstant download
Reviews( 0 )
Document information
Connected school, study & course
About the document
Uploaded On
Jan 04, 2023
Number of pages
13
Written in
Additional information
This document has been written for:
Uploaded
Jan 04, 2023
Downloads
0
Views
23