*NURSING > SOAP NOTE > NR509 Week 2 SOAP Note – Chamberlain College of Nursing | NR 509 Week 2 SOAP Note – Grade A (All)
NR509 Week 2 SOAP Note – Chamberlain College of Nursing | NR 509 Week 2 SOAP Note – Grade A
Document Content and Description Below
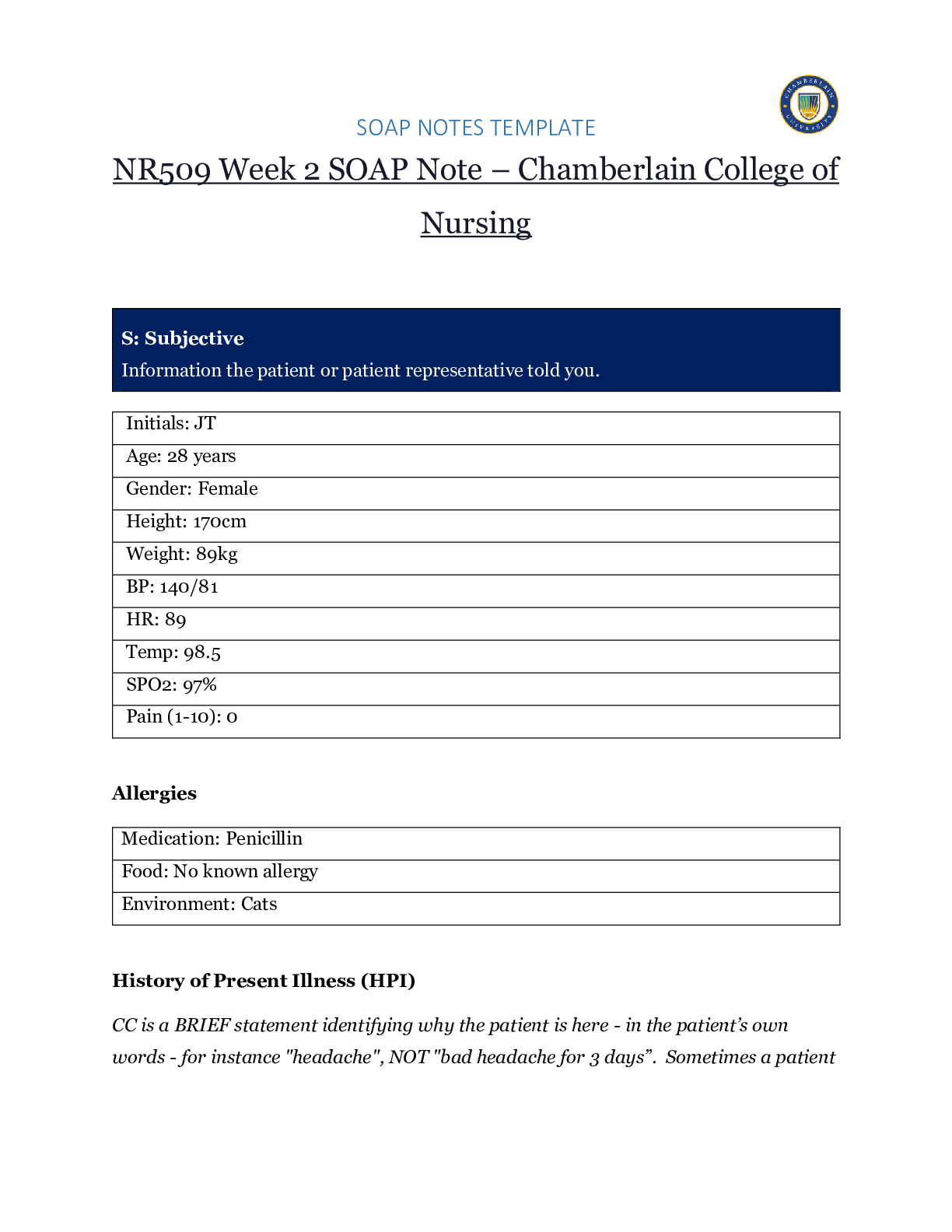
NR509 Week 2 SOAP Note – Chamberlain College of Nursing S: Subjective Information the patient or patient representative told you. Initials: JT Age: 28 years Gender: Female Height: 170cm ... Weight: 89kg BP: 140/81 HR: 89 Temp: 98.5 SPO2: 97% Pain (1-10): 0 Allergies Medication: Penicillin Food: No known allergy Environment: Cats History of Present Illness (HPI) CC is a BRIEF statement identifying why the patient is here - in the patient’s own words - for instance "headache", NOT "bad headache for 3 days”. Sometimes a patient has more than one complaint. For example: If the patient presents with cough and sore throat, identify which is the CC and which may be an associated symptom Chief Complaint (CC): Recent asthma attack which is not fully resolved Onset: 2 days ago, while visiting cousin with cats Location: N/A Duration: 2 days Characteristics: Chest tightness, worse when laying down & at night. Persistent cough x2 days Aggravating Factors: Physical activity, laying down Relieving Factors: Proventil inhaler, less effective than usual Treatment: Proventil inhaler Current Medications Medication Dosage Frequency Length of Time Used Reason for Use Proventil inhaler Albuterol 90mcg/spray PRN Long term Asthma Tylenol 500mg PRN Unknown Headaches Advil 600mg TID PRN Unknown Menstrual cramps Metformin 500mg PO Daily 1 month Diabetes Lisinopril 10mg PO Daily 1 month Hypertension Past Medical History (PMHx) – Includes but not limited to immunization status (note date of last tetanus for all adults), past major illnesses, hospitalizations, and surgeries. Depending on the CC, more info may be needed. Ms. Jones reports experiencing an asthma attack 2 days ago with ongoing shortness of breath, sleep disturbances and decreased appetite. She reports that her last hospitalization for asthma when she was in high school. She has been utilizing her Proventil inhaler more frequently. Tina reports having to use 3 puffs every 4 hours in the past couple of days and that it has not been effective. Social History (Soc Hx) - Includes but not limited to occupation and major hobbies, family status, tobacco and alcohol use, and any other pertinent data. Include health promotion such as use seat belts all the time or working smoke detectors in the house Ms. Jones is very active in church and with family, goes out occasionally with friends dancing, and enjoys bible study and volunteering with her church. She previously lived alone but moved back in with her mom and younger sister to help with finances after the death of her father. She is working on her bachelor’s degree in accounting. She does not use tobacco products or illicit drugs but reports that she tried both when younger. Ms. Jones drinks diet coke soda and drinks alcohol socially a couple times per month. She is currently single, not sexually active and not taking contraceptives but used birth control while sexually active with previous partner. She has never been married and has never been pregnant. She reports a total of three (guy) partners and denies any history of STI’s. Family History (Fam Hx) - Includes but not limited to illnesses with possible genetic predisposition, contagious or chronic illnesses. Reason for death of any deceased first-degree relatives should be included. Include parents, grandparents, siblings, and children. Include grandchildren if pertinent. Ms. Jones’ mom is fifty years old and has hyperlipidemia and hypertension. Her dad is deceased at fifty-eight years in age from a motor vehicle accident that occurred last year but had a history of hypertension, hyperlipidemia, and type II diabetes. Her paternal grandmother has hypertension. Her paternal grandfather (Grandpa Jones) died in his early sixties from colon cancer and had a history of type II diabetes. Ms. Jones’ maternal grandmother (Nana) died at age seventy-three from a stroke and had a history of hypertension and hyperlipidemia. Her maternal grandfather (Poppa) died at age seventy-eight from a heart attack and had a history of hypertension and hyperlipidemia. Ms. Jones has a younger sister and also has asthma. Her brother has no known medical problems, but Ms. Jones reports that he is overweight as well as most of her family. Her paternal uncle is an alcoholic. Review of Systems (ROS): Address all body systems that may help rule in or out a differential diagnosis Constitutional If patient denies all symptoms for this system, check here: Check the box next to each reported symptom and provide additional details. Check if Positive Symptom Details x Fatigue “I have been tired and cranky recently” Weakness Fever/Chills x Weight Changes Reports unexpected weight loss >10 pounds Trouble Sleeping Night Sweats Other Skin If patient denies all symptoms for this system, check here: Check the box next to each reported symptom and provide additional details. - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - -- Education Rationale/Citation Nonpharmacologic management of asthma—peak flow monitoring, avoidance of triggers, ongoing education related to disease process, utilization of asthma action plan (Hollier, 2018) Lifestyle alterations (eating, exercise, weight loss, heart disease, travel, work stress, etcetera) Better understanding leads to increased compliance (Johns Hopkins Medicine, n.d.) Diabetic diet options Better understanding leads to increased compliance (Johns Hopkins Medicine, n.d.) DASH diet for hypertension Better understanding leads to increased compliance (Johns Hopkins Medicine, n.d.) Compliance with treatment regimen (compliance with inhalers & oral asthma regimen, logging asthma symptoms daily, glucose & blood pressure monitoring, nutrition & hydration, meal planning, food log, alcohol, effects of illness, benefits of completing medication regimens, etcetera) Better understanding leads to increased compliance (Johns Hopkins Medicine, n.d.) Ongoing education related to the effects of diabetes & hypertension (increased risk of severe infection, heart disease, vascular disease, neuropathy, renal disease, eye disease, sleep apnea, etcetera) Better understanding leads to increased compliance (Johns Hopkins Medicine, n.d.) Education for all medications prescribed Better understanding leads to increased compliance (Johns Hopkins Medicine, n.d.) Follow-Up: Indicate when patient should return to clinic and provide detailed instructions indicating if the patient should return sooner than scheduled or seek attention elsewhere. None at this time: Follow-Up Rationale/Citation Follow up 3-6 months Ensure appropriate treatment results and patient compliance for disease stability References (Include at least one evidence-based peer-reviewed journal article which relates to this case. Use the correct APA 6th edition formatting.) List references below: Acetaminophen-Hydrocodone. (2018). Acetaminophen-hydrocodone, oral tablet. Retrieved from https://www.healthline.com/health/acetaminophen-hydocodone-oral-tablet Hollier, A. (2018). Clinical guidelines in primary care, 3rd Edition. Advanced Practice Education Association, Inc. Lafayette, LA. Lisinopril. (2019). Lisinopril dosage. Retrieved from https://www.drugs.com/dosage/lisinopril.html Johns Hopkins Medicine. (n.d.). Diabetes self management patient education materials. Retrieved from https://www.hokinsmedicine.org/gim/core_resources/patient%20handouts/index.html Metformin. (2019). Metformin (oral route). Retrieved from https://www.mayoclinic.org/drugs-supplements/metformin-oral-route/proper-use/drg-20067074 [Show More]
Last updated: 1 year ago
Preview 1 out of 20 pages
Reviews( 0 )
Recommended For You
*NURSING> SOAP NOTE > NURS 112 SOAP Note Chest Pain Pennsylvania State University -Download To Score An A (All)
NURS 112 SOAP Note Chest Pain Pennsylvania State University -Download To Score An A
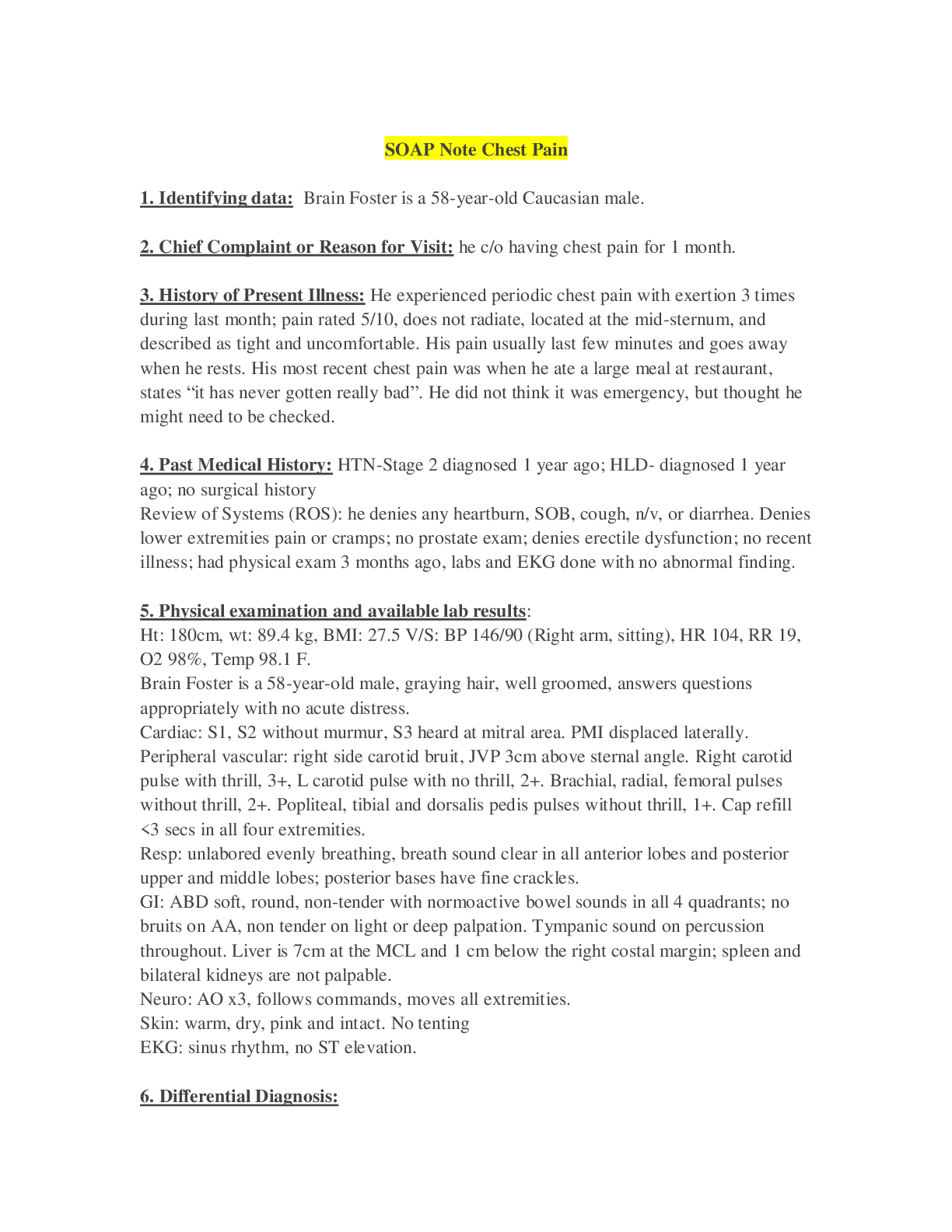
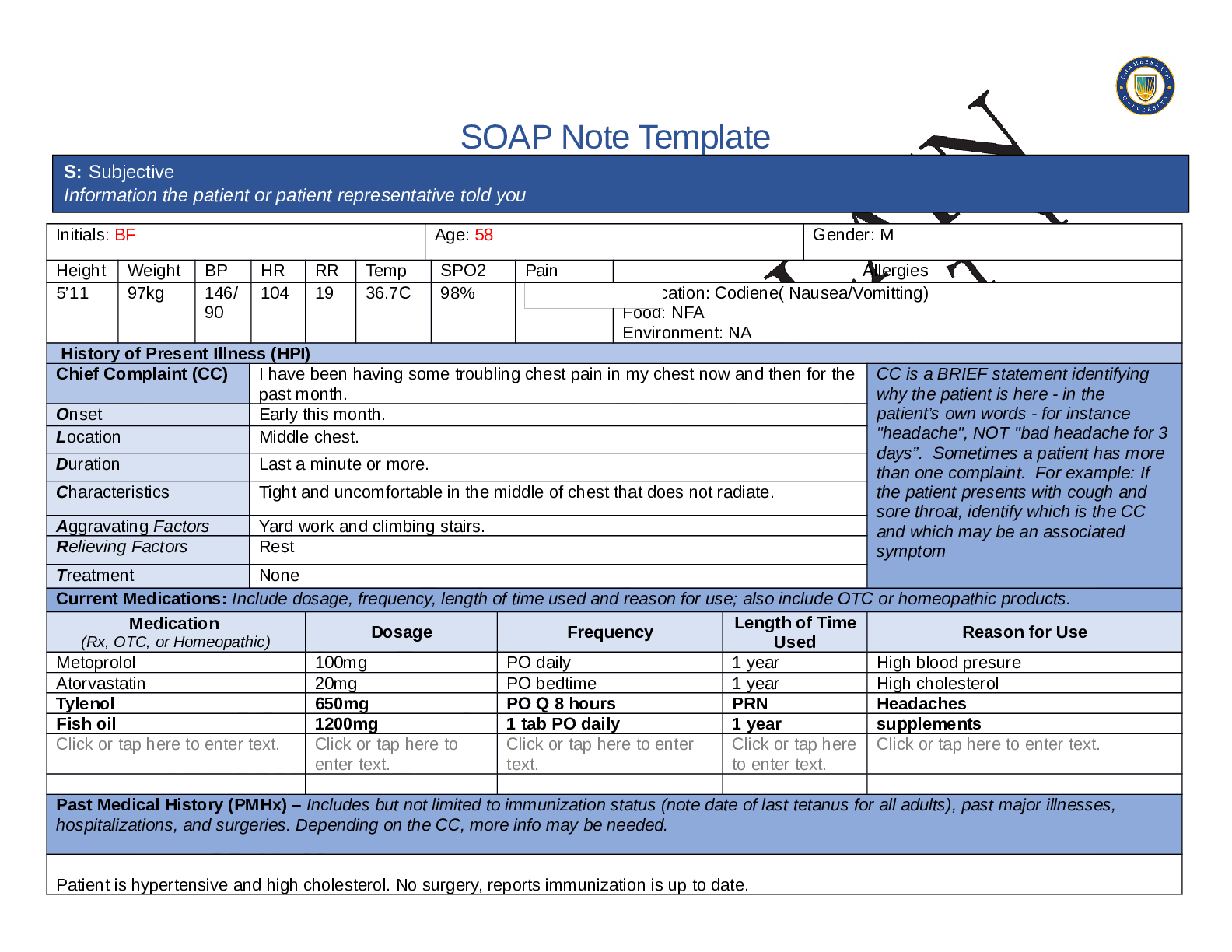
SOAP Note Chest Pain 1. Identifying data: Brain Foster is a 58-year-old Caucasian male. 2. Chief Complaint or Reason for Visit: he c/o having chest pain for 1 month. 3. History...
By Succeed , Uploaded: Aug 03, 2020
$9.5
*NURSING> SOAP NOTE > NR 509 Week 4 Soap Note (All)
NR 509 Week 4 Soap Note
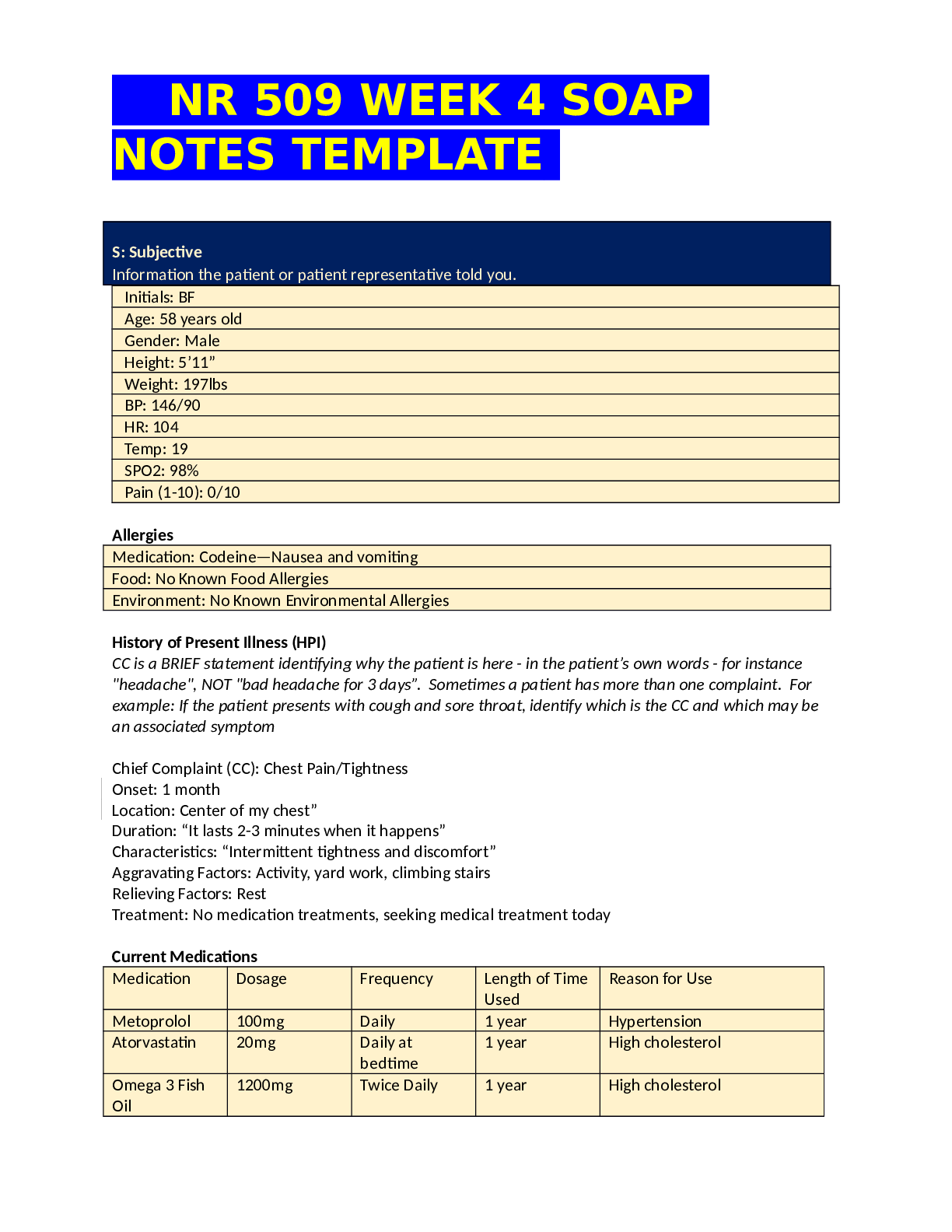
NR 509 WEEK 4 SOAP NOTES TEMPLATE S: Subjective Information the patient or patient representative told you. Initials: BF Age: 58 years old Gender: Male Height: 5’11” Weight: 197lbs BP:...
By Victor , Uploaded: Jun 03, 2022
$15.5
*NURSING> SOAP NOTE > Summary NR 509 Week 3 Neurology SOAP Note (All)
Summary NR 509 Week 3 Neurology SOAP Note
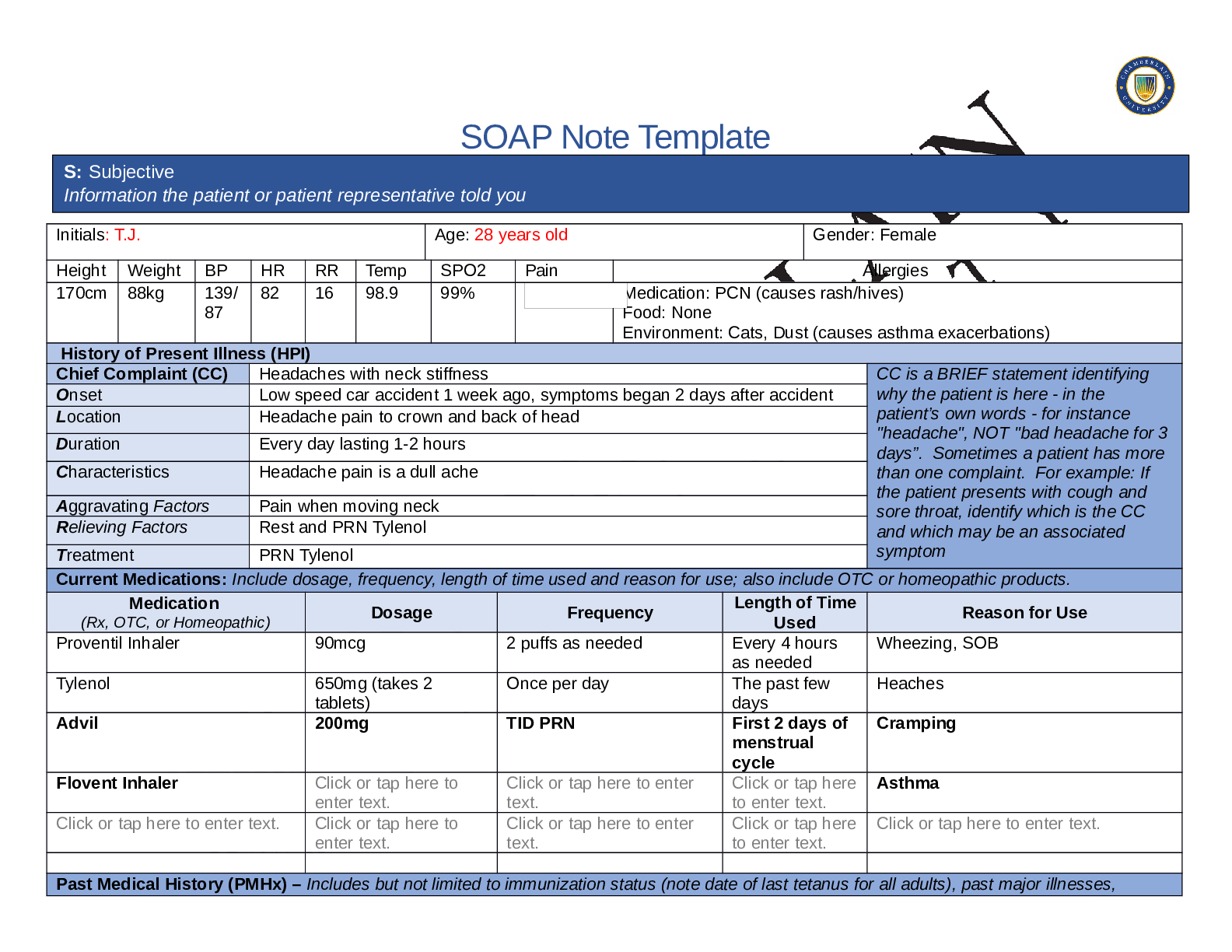
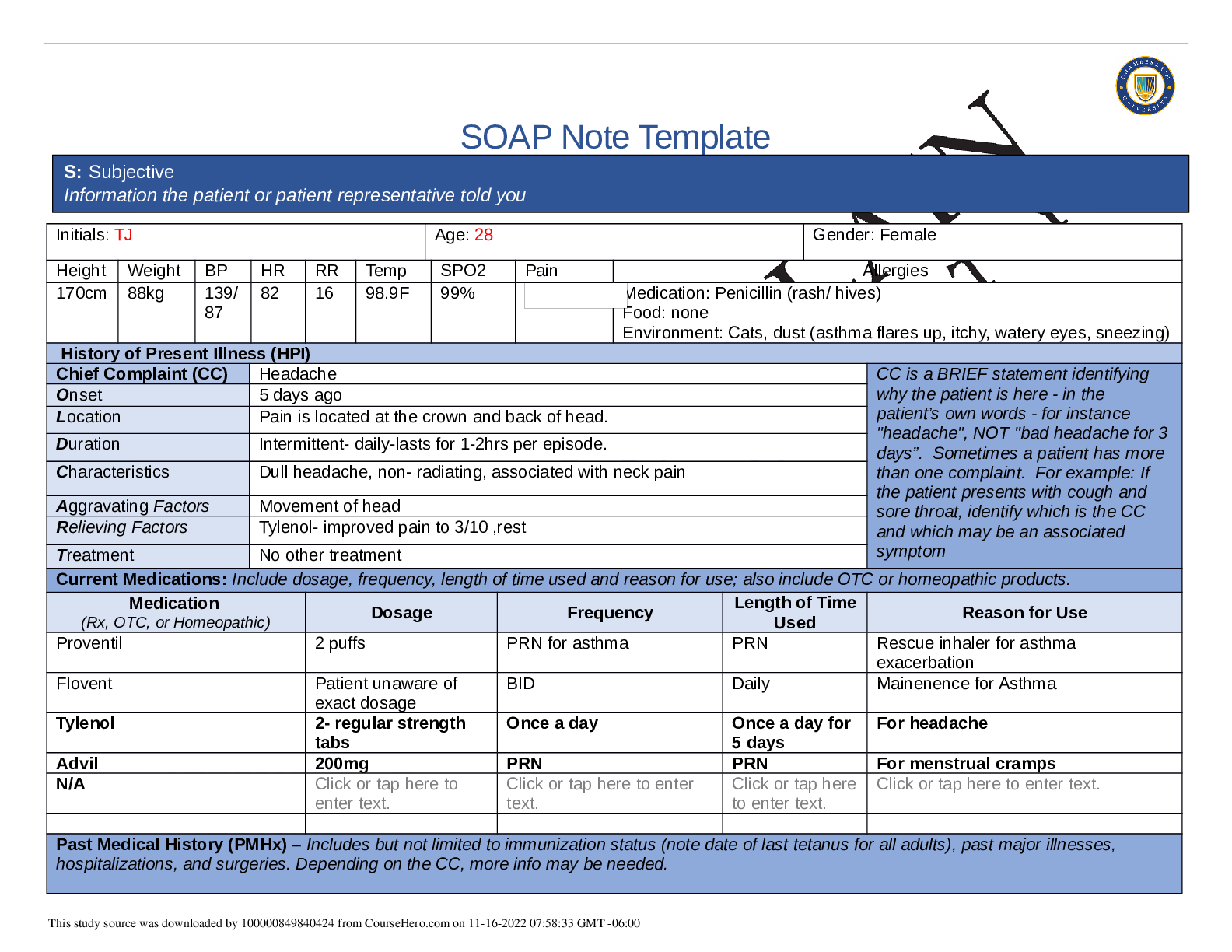
SOAP Note Template Initials: T.J. Age: 28 years old Gender: Female Height Weight BP HR RR Temp SPO2 Pain Allergies 170cm 88kg 139/ 87 82 16 98.9 99% Medication: PCN (causes rash/hives) Food: Non...
By Nutmegs , Uploaded: May 07, 2022
$11
*NURSING> SOAP NOTE > Summary NR 509 Week 1 Health History SOAP Note (All)
Summary NR 509 Week 1 Health History SOAP Note
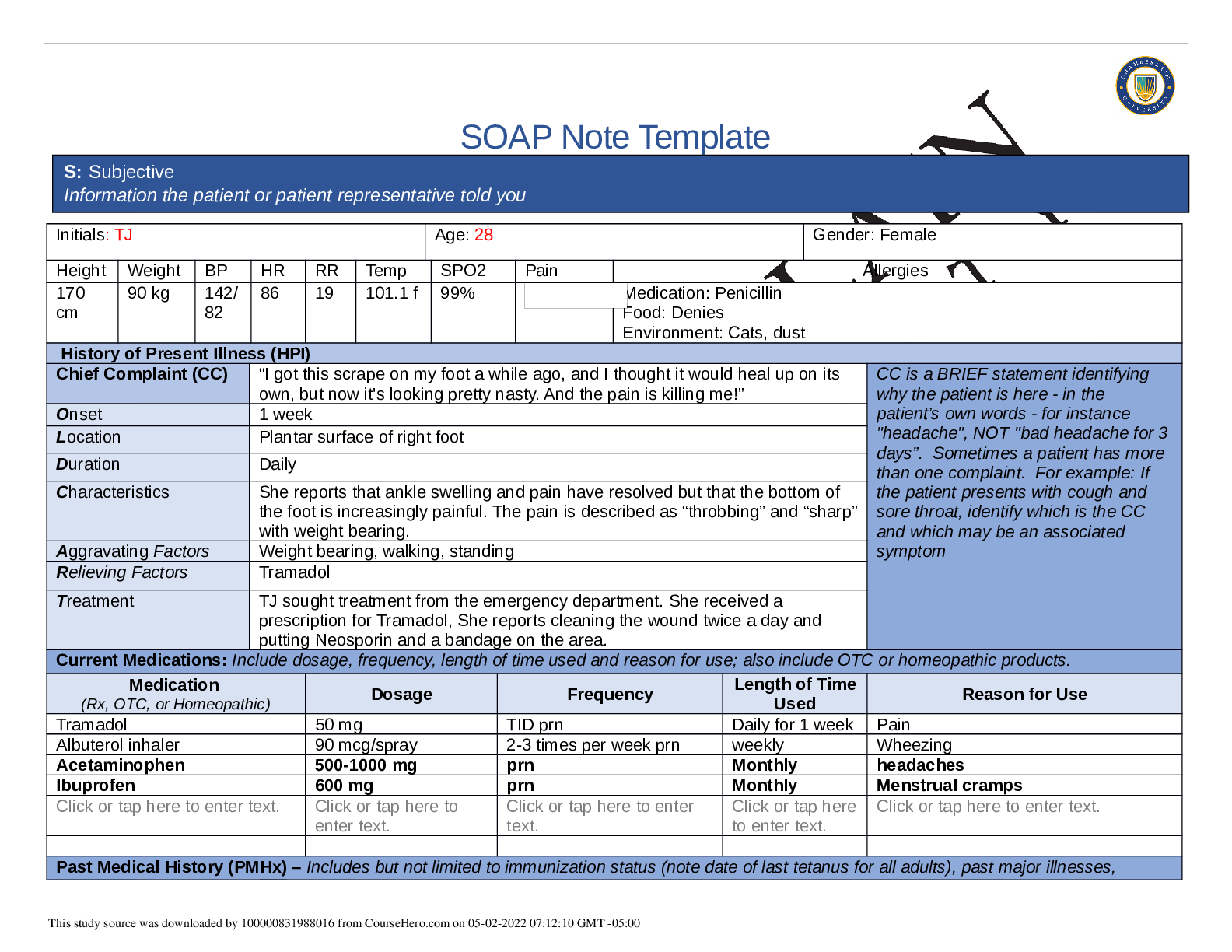
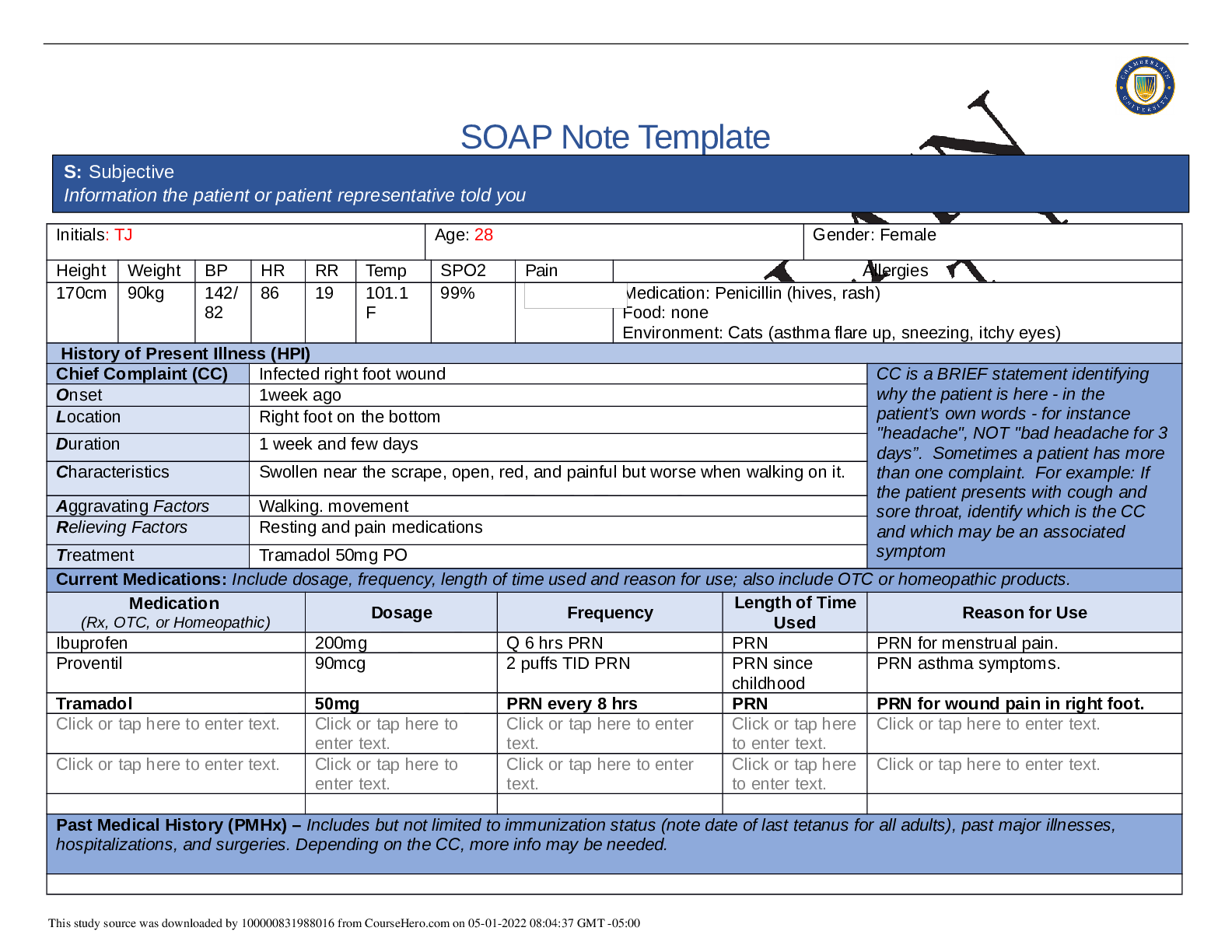
SOAP Note Template Initials: TJ Age: 28 Gender: Female Height Weight BP HR RR Temp SPO2 Pain Allergies 170 cm 90 kg 142/ 82 86 19 101.1 f 99% Medication: Penicillin Food: Denies Environment:...
By Nutmegs , Uploaded: May 02, 2022
$9
*NURSING> SOAP NOTE > Summary NR 509 Week 5 Abdominal Pain SOAP Note (All)
Summary NR 509 Week 5 Abdominal Pain SOAP Note
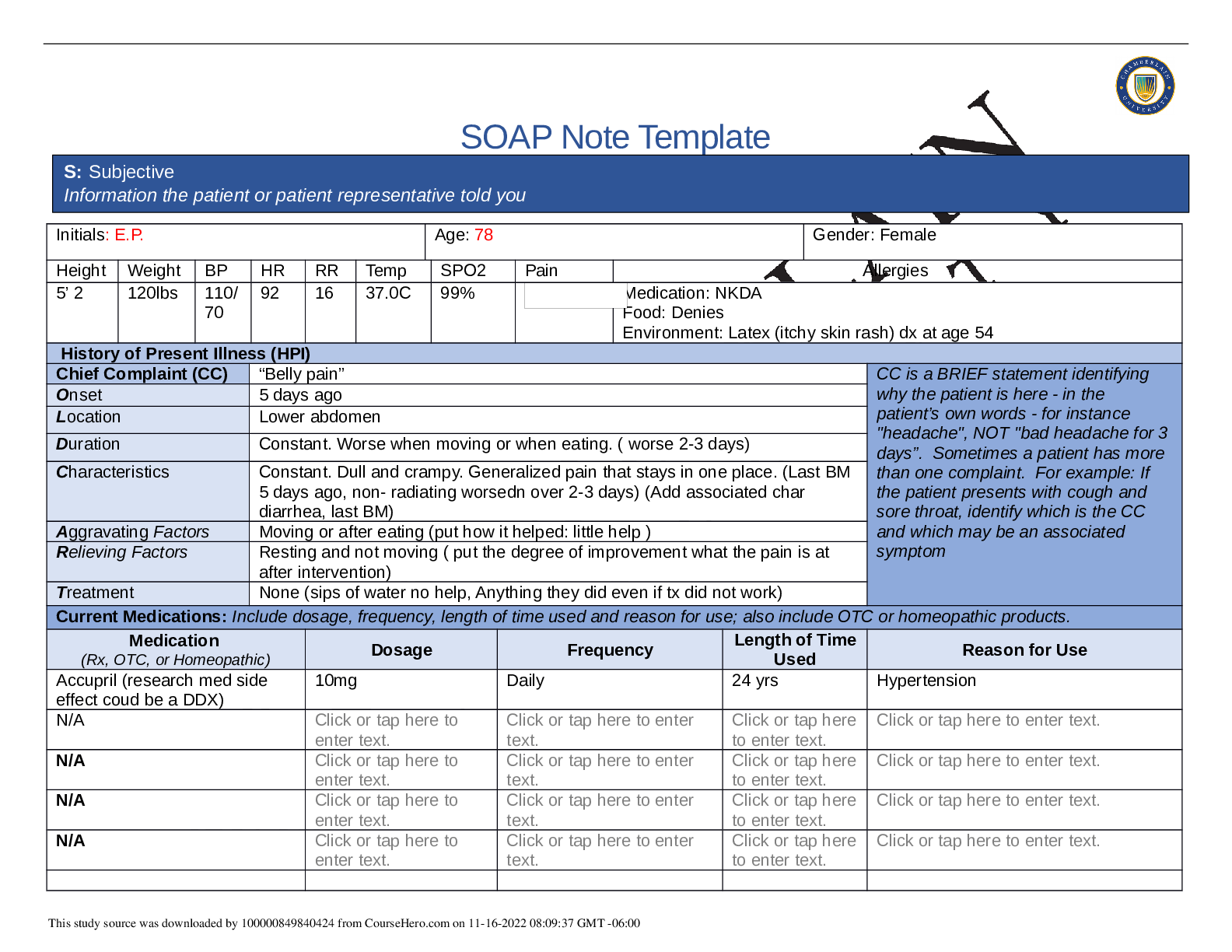
SOAP Note Template Initials: E.P. Age: 78 Gender: Female Height Weight BP HR RR Temp SPO2 Pain Allergies 5’ 2 120lbs 110/ 70 92 16 37.0C 99% Medication: NKDA Food: Denies Environment: Latex (it...
By Nutmegs , Uploaded: May 02, 2022
$11
*NURSING> SOAP NOTE > NR 509 Week 7, Danny Rivera, SOAP Note, February 2020 (All)
NR 509 Week 7, Danny Rivera, SOAP Note, February 2020
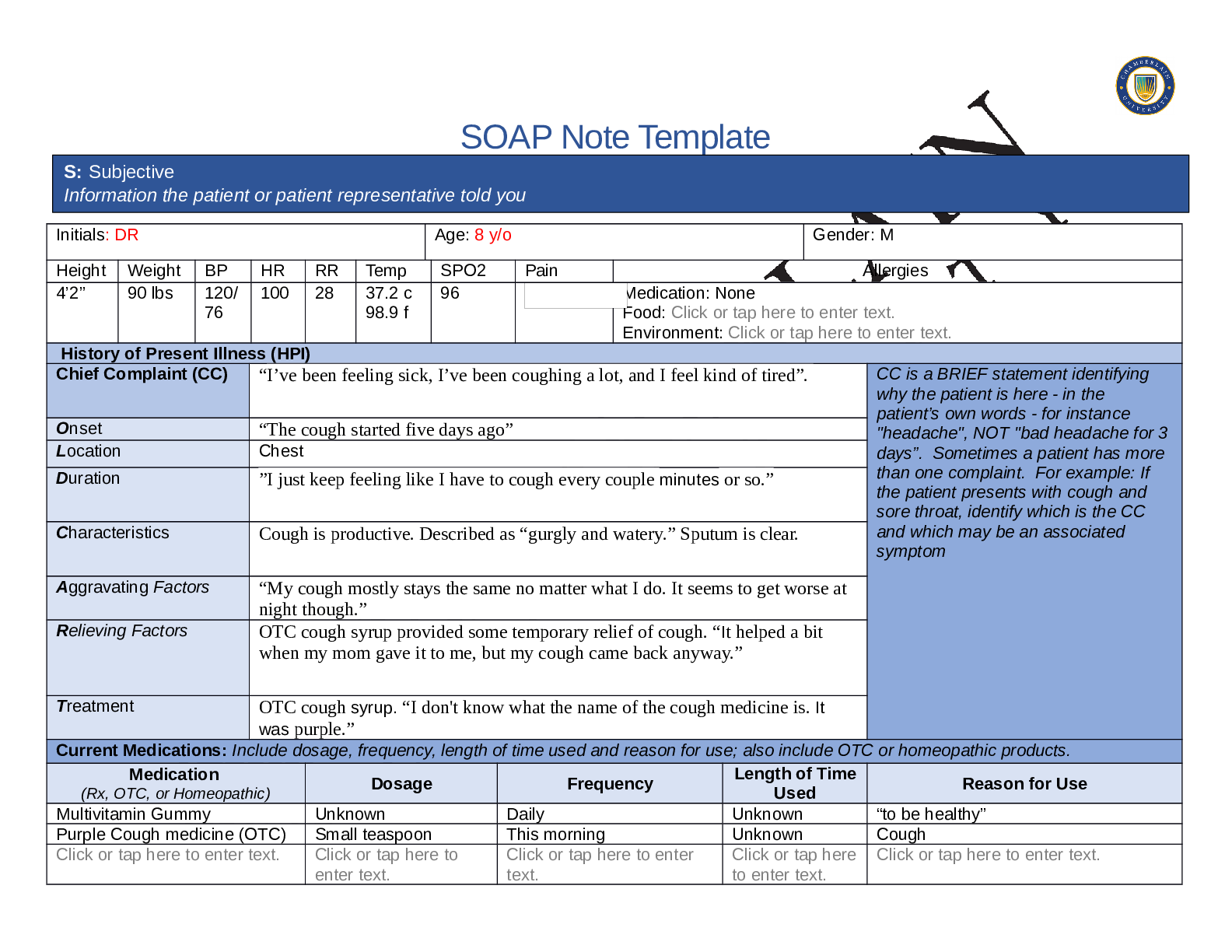
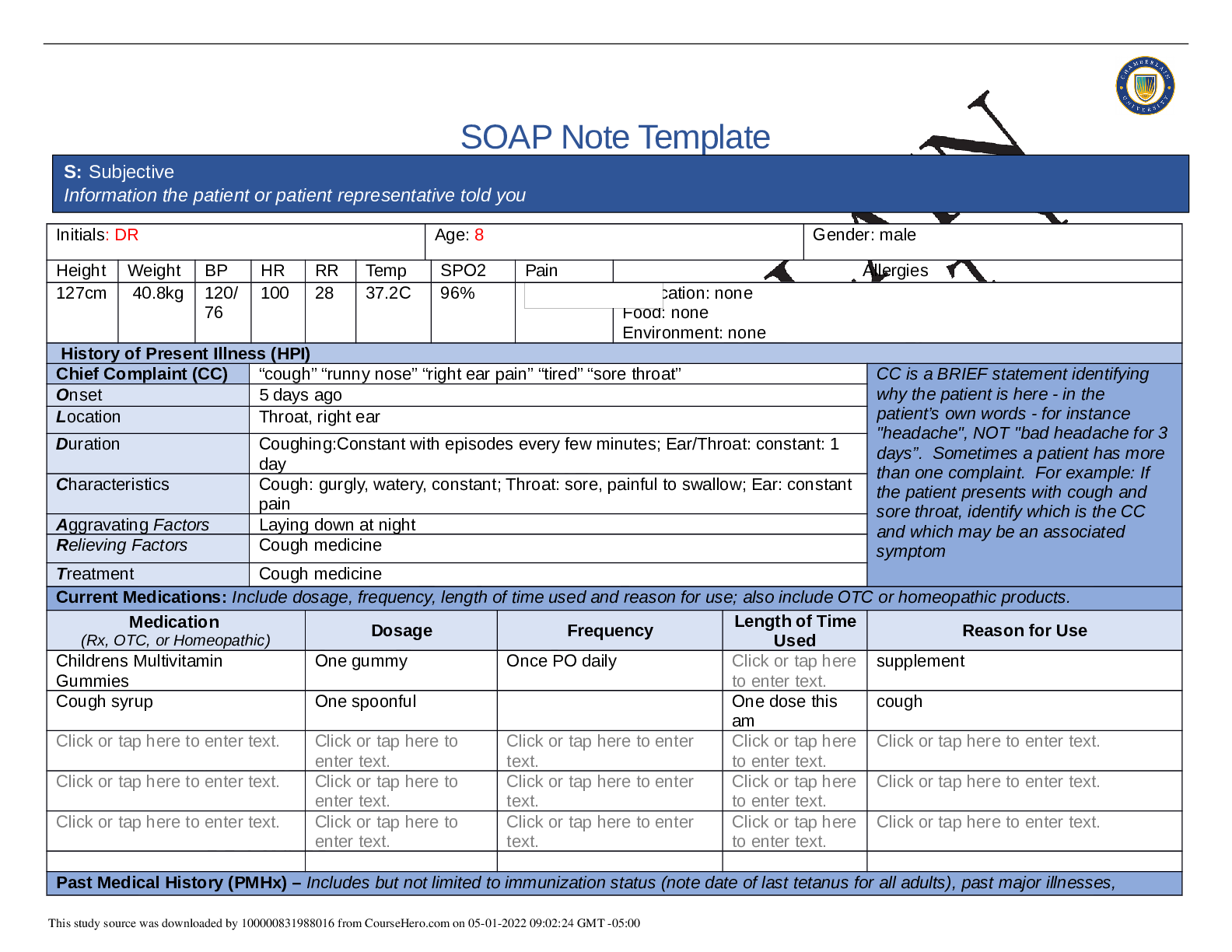
SOAP Note Template Initials: DR Age: 8 y/o Gender: M Height Weight BP HR RR Temp SPO2 Pain Allergies 4’2” 90 lbs 120/ 76 100 28 37.2 c 98.9 f 96 Medication: None Food: Click or tap here to ent...
By Nutmegs , Uploaded: May 01, 2022
$9
*NURSING> SOAP NOTE > NR 509 Week 4 Chest Pain SOAP Note (All)
NR 509 Week 4 Chest Pain SOAP Note
SOAP Note Template Initials: BF Age: 58 Gender: M Height Weight BP HR RR Temp SPO2 Pain Allergies 5’11 97kg 146/ 90 104 19 36.7C 98% Medication: Codiene( Nausea/Vomitting) Food: NFA Environment...
By Nutmegs , Uploaded: May 01, 2022
$9
*NURSING> SOAP NOTE > NR 509 Week 1 Health History SOAP Note (All)
NR 509 Week 1 Health History SOAP Note
SOAP Note Template Initials: TJ Age: 28 Gender: Female Height Weight BP HR RR Temp SPO2 Pain Allergies 170cm 90kg 142/ 82 86 19 101.1 F 99% Medication: Penicillin (hives, rash) Food: none Env...
By Nutmegs , Uploaded: May 01, 2022
$9
*NURSING> SOAP NOTE > NR 509 Week 3 Neurology SOAP Note (All)
NR 509 Week 3 Neurology SOAP Note
SOAP Note Template Initials: TJ Age: 28 Gender: Female Height Weight BP HR RR Temp SPO2 Pain Allergies 170cm 88kg 139/ 87 82 16 98.9F 99% Medication: Penicillin (rash/ hives) Food: none Environ...
By Nutmegs , Uploaded: May 01, 2022
$9
*NURSING> SOAP NOTE > NR 509 Week 6 Pediatric SOAP Note (All)
NR 509 Week 6 Pediatric SOAP Note
SOAP Note Template Initials: DR Age: 8 Gender: male Height Weight BP HR RR Temp SPO2 Pain Allergies 127cm 40.8kg 120/ 76 100 28 37.2C 96% Medication: none Food: none Environment: none History...
By Nutmegs , Uploaded: May 01, 2022
$9
Document information
Connected school, study & course
About the document
Uploaded On
Jan 26, 2021
Number of pages
20
Written in
Additional information
This document has been written for:
Uploaded
Jan 26, 2021
Downloads
0
Views
80






