Hesi Fundamentals 2019 Exam (Questions and Answers)
Document Content and Description Below
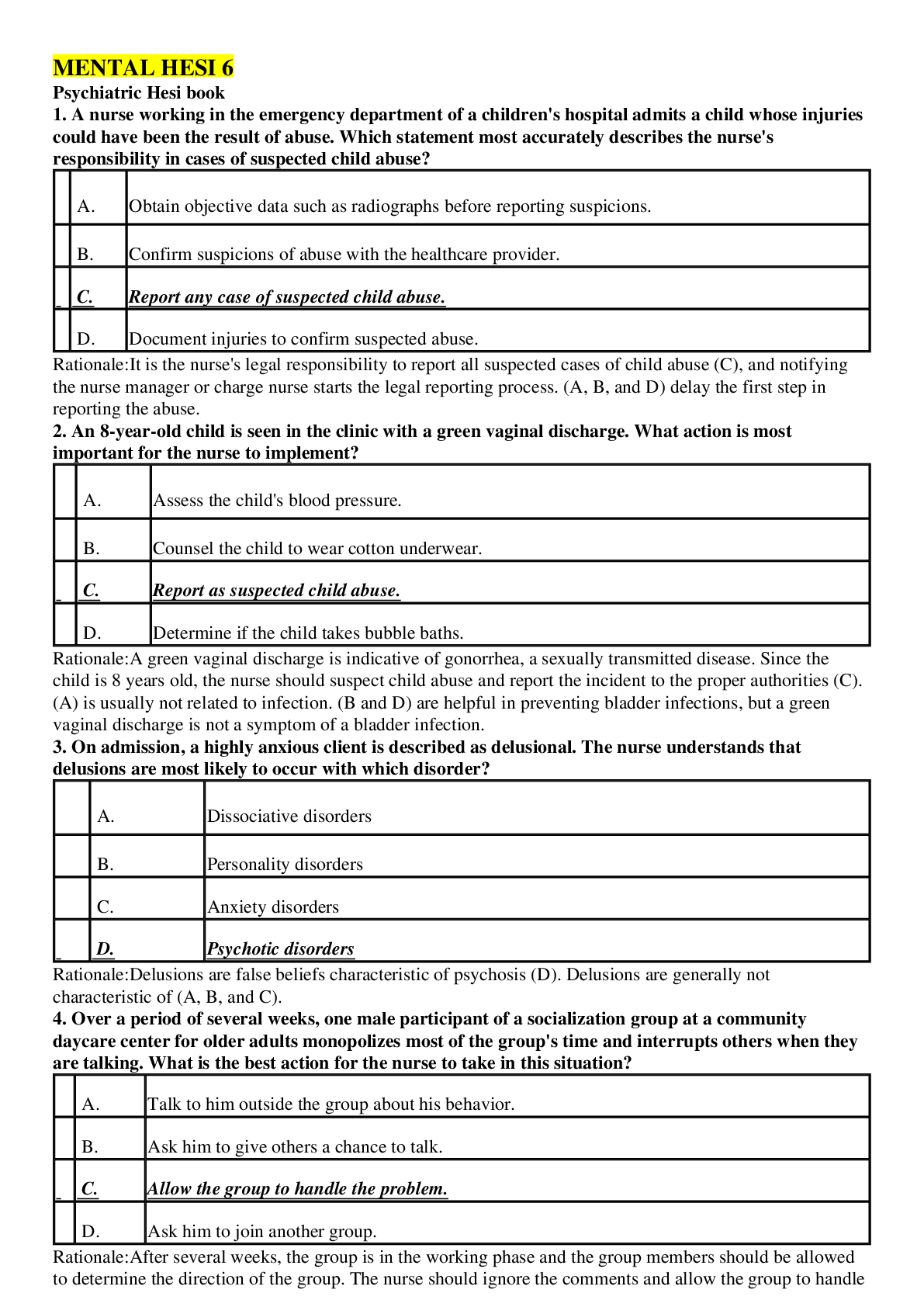
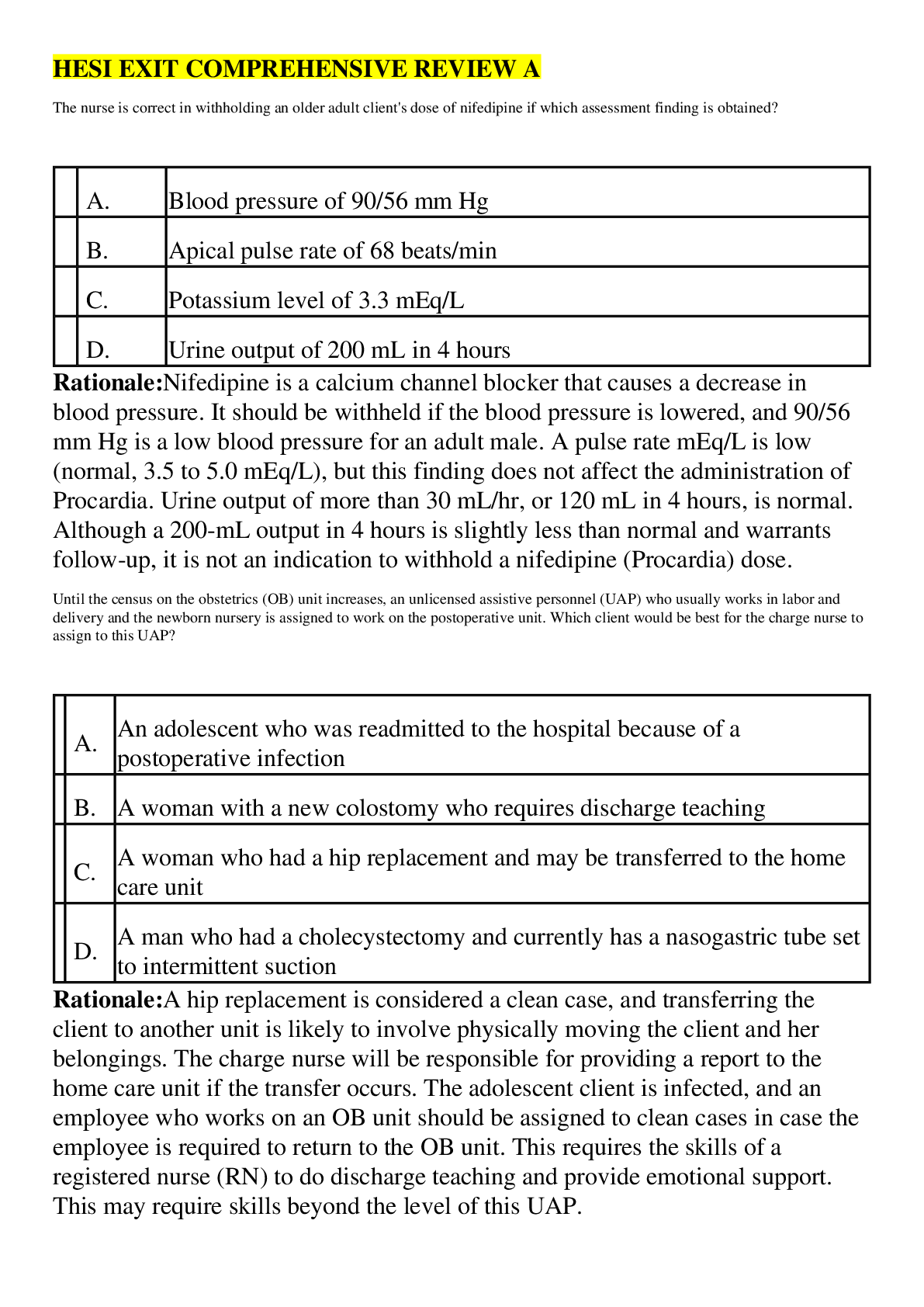
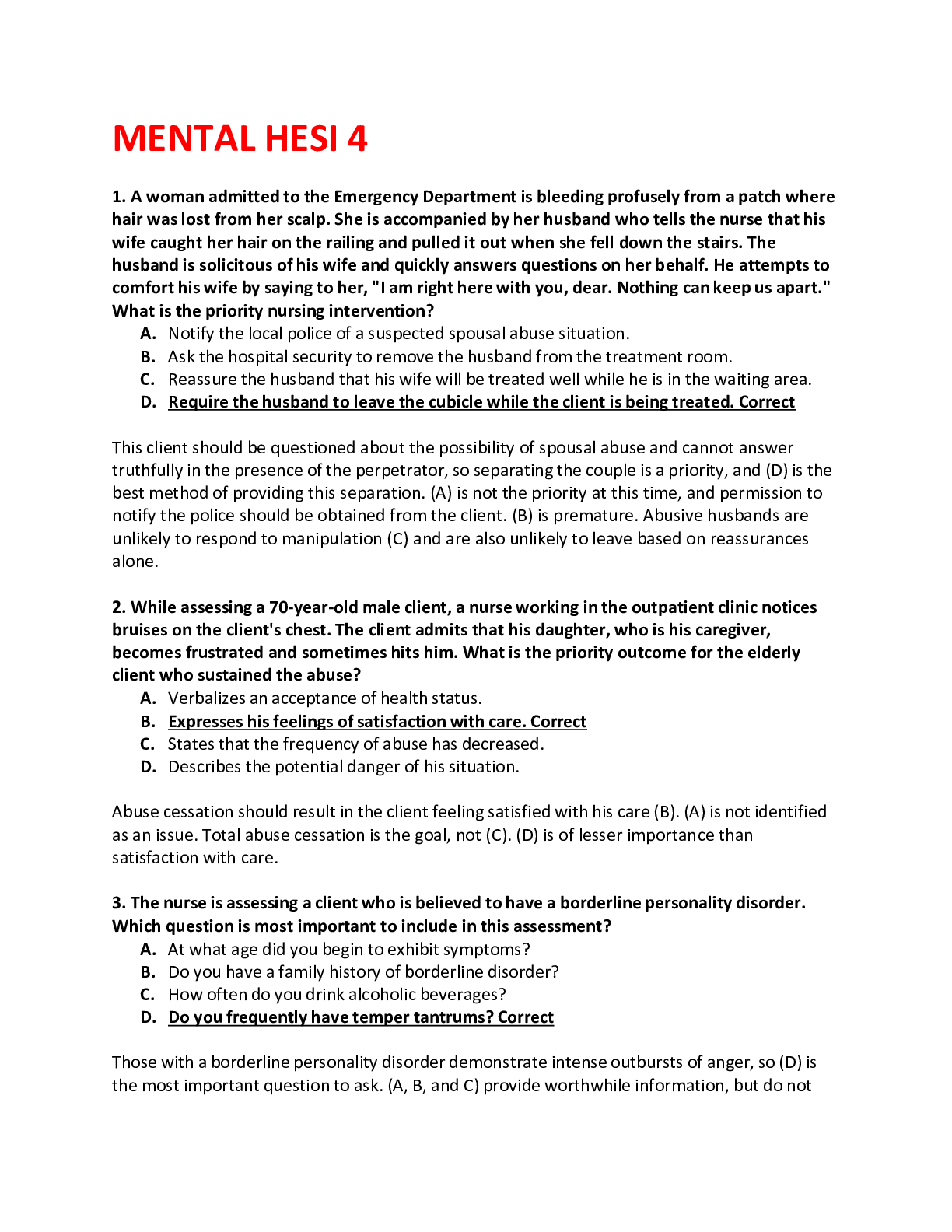
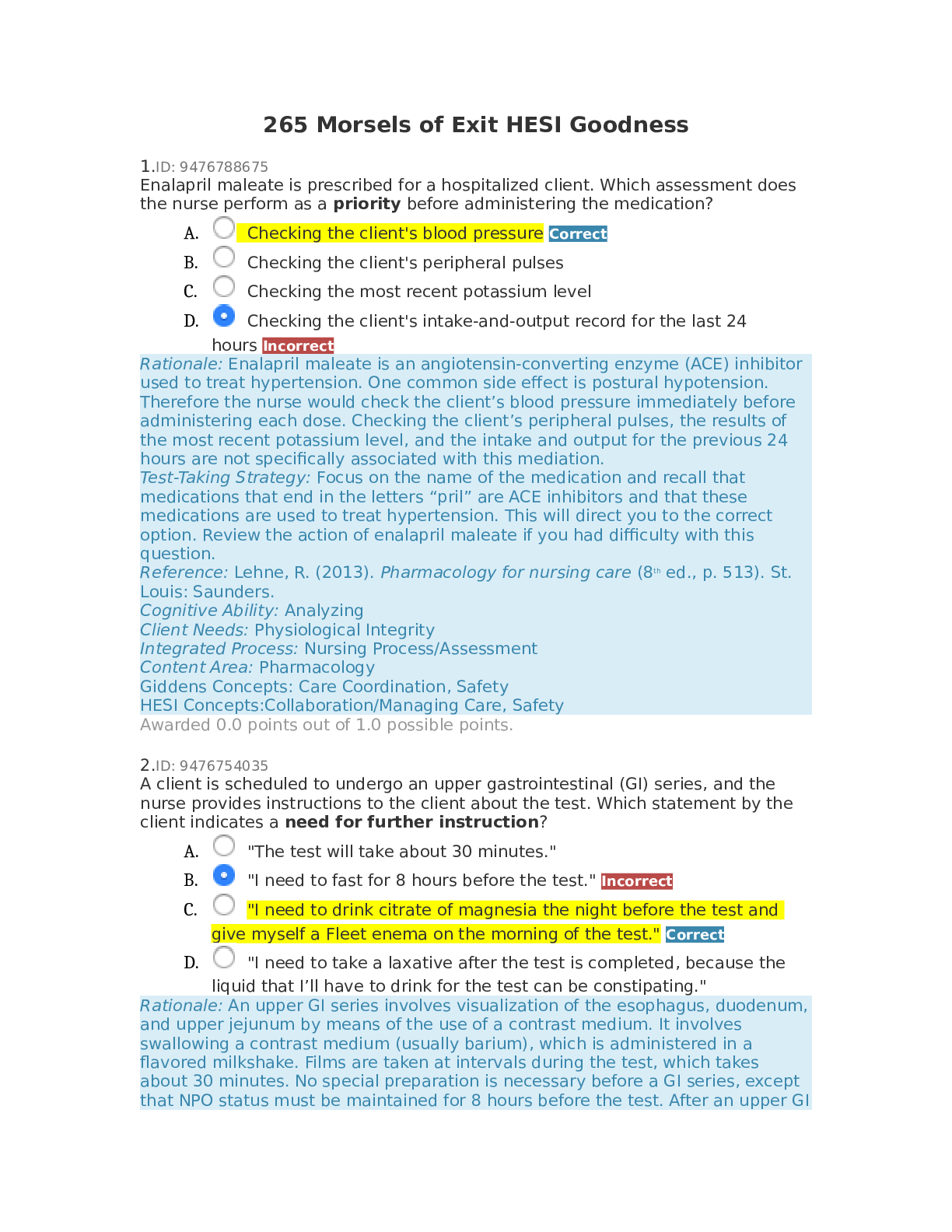
Hesi Fundamentals 2019 Exam (Questions and Answers) 1. The home health nurse visits an elderly female client who had a brain attack three months ago and is now able to ambulate with the assistance of... a quad cane. Which assessment finding has the greatest implications for this client's care? • The husband, who is the caregiver, begins to weep when the nurse asks how he is doing. • The client tells the nurse that she does not have much of an appetite today. • The nurse notes that there are numerous scatter rugs throughout the house. Correct • The client's pulse rate is 10 beats higher than it was at the last visit one week ago. Scatter rugs (C) pose a safety hazard because the client can trip on them when ambulating, so this finding has the greatest significance in planning this client's care. Psychological support of the caregiver (A) is a less acute need than that of client safety. The nurse needs to obtain more information about (B), but this is not a safety issue. (D) is not a significant increase, and additional assessment might provide information about the reason for the increase (anxiety, exercise, etc.). 2. The nurse is digitally removing a fecal impaction for a client. The nurse should stop the procedure and take corrective action if which client reaction is noted? • Temperature increases from 98.8° to 99.0° F. • Pulse rate decreases from 78 to 52 beats/min. Correct • Respiratory rate increases from 16 to 24 breaths/min. • Blood pressure increases from 110/84 to 118/88 mm/Hg. Parasympathetic reaction can occur as a result of digital stimulation of the anal sphincter, which should be stopped if the client experiences a vagal response, such as bradycardia (B). (A, C, and D) do not warrant stopping the procedure. 3. The nurse is providing passive range of motion (ROM) exercises to the hip and knee for a client who is unconscious. After supporting the client's knee with one hand, what action should the nurse take next? • Raise the bed to a comfortable working level. • Bend the client's knee. • Move the knee toward the chest as far as it will go. • Cradle the client's heel. Correct Passive ROM exercise for the hip and knee is provided by supporting the joints of the knee and ankle (D) and gently moving the limb in a slow, smooth, firm but gentle manner. (A) should be done before the exercises are begun to prevent injury to the nurse and client. (B) is carried out after both joints are supported. After the knee is bent, then the knee is moved toward the chest to the point of resistance (C) two or three times. 4. A client who has moderate, persistent, chronic neuropathic pain due to diabetic neuropathy takes gabapentin (Neurontin) and ibuprofen (Motrin, Advil) daily. If Step 2 of the World Health Organization (WHO) pain relief ladder is prescribed, which drug protocol should be implemented? • Continue gabapentin. Correct • Discontinue ibuprofen. • Add aspirin to the protocol. • Add oral methadone to the protocol. Based on the WHO pain relief ladder, adjunct medications, such as gabapentin (Neurontin), an antiseizure medication, may be used at any step for anxiety and pain management, so (A) should be implemented. Nonopiod analgesics, such as ibuprofen (A) and aspirin (C) are Step 1 drugs. Step 2 and 3 include opioid narcotics (D), and to maintain freedom from pain, drugs should be given around the clock rather than by the client s PRN requests. 5. The nurse is preparing to irrigate a client's indwelling urinary catheter using an open technique. What action should the nurse take after applying gloves? • Empty the client's urinary drainage bag. • Draw up the irrigating solution into the syringe. Correct • Secure the client's catheter to the drainage tubing. • Use aseptic technique to instill the irrigating solution. To irrigate an indwelling urinary catheter, the nurse should first apply gloves, then draw up the irrigating solution into the syringe (B). The syringe is then attached to the catheter and the fluid instilled, using aseptic technique (D). Once the irrigating solution is instilled, the client's catheter should be secured to the drainage tubing (C). The urinary drainage bag can be emptied (A) whenever intake and output measurement is indicated, and the instilled irrigating fluid can be subtracted from the output at that time. 6. Which client care requires the nurse to wear barrier gloves as required by the protocol for Standard Precautions? • Removing the empty food tray from a client with a urinary catheter. • Washing and combing the hair of a client with a fractured leg in traction. • Administering oral medications to a cooperative client with a wound infection. • Emptying the urinary catheter drainage bag for a client with Alzheimer's disease. Correct Possible contact with body secretions, excretions, or broken skin is an indication for wearing barrier (nonsterile) gloves. Emptying a urine drainage bag requires the use of gloves (D). (A, B, and C) do not require gloves. 7. What action should the nurse implement to prevent the formation of a sacral ulcer for a client who is immobile? • Maintain in a lateral position using protective wrist and vest devices. • Position prone with a small pillow below the diaphragm. Correct • Raise the head and knee gatch when lying in a supine position. • Transfer into a wheelchair close to the nurse's station for observation. The prone position (B) using a small pillow below the diaphragm maintains alignment and provides the best pressure relief over the sacral bony prominence. Using protective (restraining) devices (A) is not indicated. Raising the head and bed gatch (C) may reduce shearing forces due to sliding down in bed, but it interferes with venous return from the legs and places pressure on the sacrum, predisposing to ulcer formation. Sitting in a wheelchair (D) places the body weight over the ischial tuberosities and predisposes to a potential pressure point. 8. What intervention should the nurse include in the plan of care for a client who is being treated with an Unna's paste boot for leg ulcers due to chronic venous insufficiency? • Check capillary refill of toes on lower extremity with Unna's paste boot. Correct • Apply dressing to wound area before applying the Unna's paste boot. • Wrap the leg from the knee down towards the foot. • Remove the Unna's paste boot q8h to assess wound healing. The Unna's paste boot becomes rigid after it dries, so it is important to check distally for adequate circulation (A). Kerlix is often wrapped around the outside of the boot and an ace bandage may be used to cover both, but no bandage should be put under it (B). The Unna's paste boot should be applied from the foot and wrapped towards the knee (C). The Unna's paste boot acts as a sterile dressing, and should not be removed q8h. Weekly removal is reasonable (D). 9. The nurse is administering an intermittent infusion of an antibiotic to a client whose intravenous (IV) access is an antecubital saline lock. After the nurse opens the roller clamp on the IV tubing, the alarm on the infusion pump indicates an obstruction. What action should the nurse take first? • Check for a blood return. • Reposition the client's arm. Correct • Remove the IV site dressing. • Flush the lock with saline. If the client's elbow is bent, the IV may be unable to infuse, resulting in an obstruction alarm, so the nurse should first attempt to reposition the client's arm to alleviate any obstruction (B). After other sources of occlusion are eliminated, the nurse may need to check for a blood return (A), remove the dressing (C), or flush the saline lock (D) and then resume the intermittent infusion. 10. A female client who has breast cancer with metastasis to the liver and spine is admitted with constant, severe pain despite around-the-clock use of oxycodone (Percodan) and amitriptyline (Elavil) for pain control at home. During the admission assessment, which information is most important for the nurse to obtain? • Sensory pattern, area, intensity, and nature of the pain. Correct • Trigger points identified by palpation and manual pressure of painful areas. • Schedule and total dosages of drugs currently used for breakthrough pain. • Sympathetic responses consistent with onset of acute pain. The components of every pain assessment should include sensory patterns, area, intensity, and nature (PAIN) of the pain (A) and are essential in identifying appropriate therapy for the client's specific type and severity of pain, which may indicate the onset of disease progression or complications. Triggers (B), current drug usage (C), and sympathetic responses (D), such as tachycardia, diaphoresis, and elevated blood pressure, are important, but should be obtained after focusing on (A). ............CONTINUED [Show More]
Last updated: 1 year ago
Preview 1 out of 16 pages
Reviews( 0 )
Document information
Connected school, study & course
About the document
Uploaded On
Jan 27, 2021
Number of pages
16
Written in
Additional information
This document has been written for:
Uploaded
Jan 27, 2021
Downloads
0
Views
49


 (1).png)