*NURSING > EXAM > West Coast University: NURS 100 ATI Skills Modules Week 1 to 4 Latest Updated 2023,100% CORRECT (All)
West Coast University: NURS 100 ATI Skills Modules Week 1 to 4 Latest Updated 2023,100% CORRECT
Document Content and Description Below
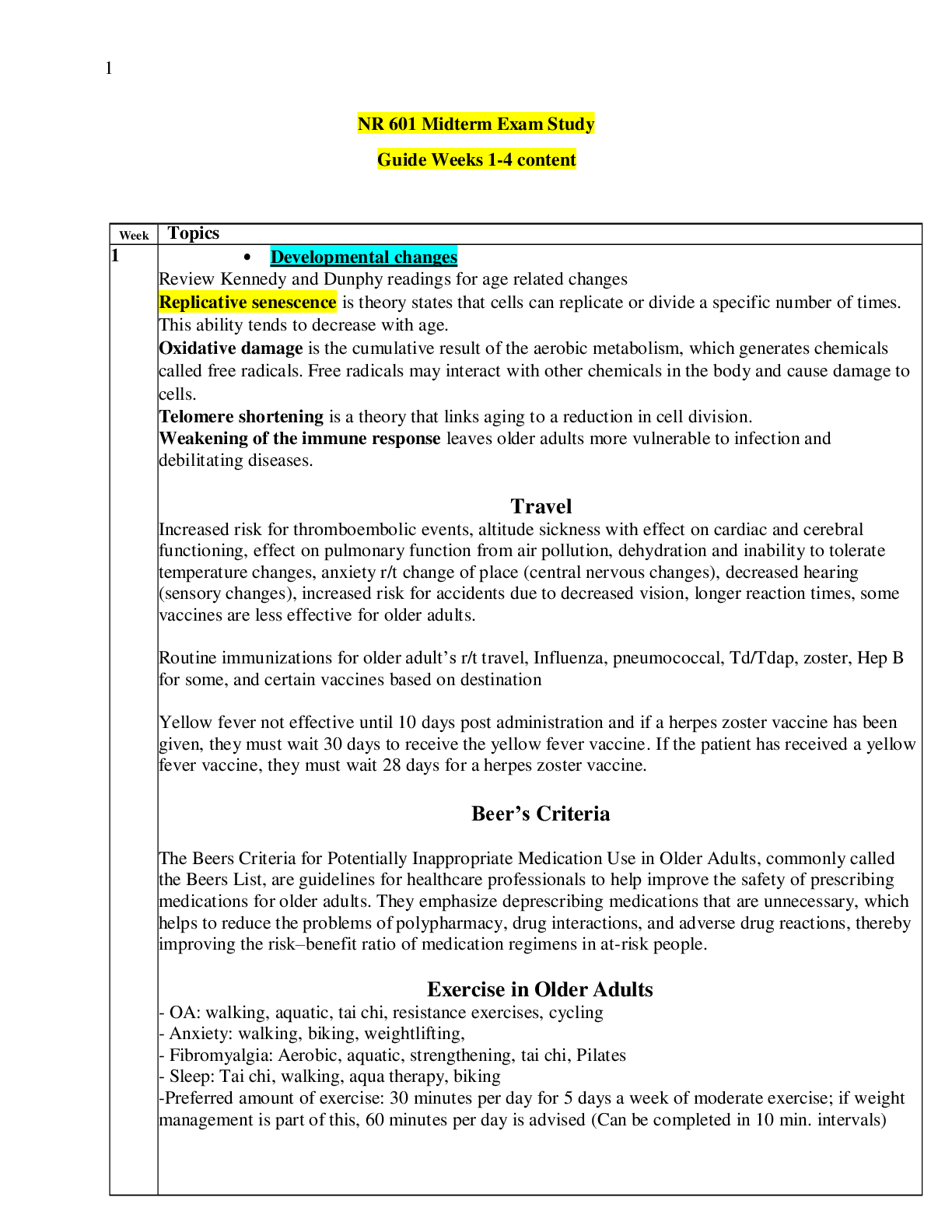
West Coast University: NURS 100 ATI Skills Modules Week 1 to 4 Latest Updated 2023 Week 1 Infection Control • Infection: invasion & proliferation of microorganisms in body tissue w/ potential... to affect nearly every body system • Standard precautions: reduce risk of transmission of micro-organisms (gloves & hand wash) • Transmission (isolation) precautions: for patients suspected to be infected w/ highly transmissible pathogens o Contact: VRE, MRSA, C. difficile, wound infections, herpes o Droplet: flu, Mycoplasma pneumonia, diptheria, mumps o Airborne • Terminology: o Antimicrobial- destroy or suppress the growth of pathogens o Antiseptic- reduces the number of pathogens on a surface o Asepsis- methods used to assure environment is pathogen-free as possible o Aseptic- as pathogen-free as possible o Bacteriostasis- inhibition of further bacterial growth o Chlorhexidine- antibacterial compound w/ substantial residual activity as liquid antiseptic & disinfectant o Disinfectant- any chemical agent to destroy or inhibit growth of harmful organisms o Endogenous- produced within an organism rather than externally o Exogenous- externally caused o Medical asepsis- infection control practices in healthcare (handwashing) (clean) o Surgical asepsis- destroy all pathogens (sterile) o Retrovirus- large group of RNA-based viruses infect immunocompromised individuals • Latex reactions o Irritant contact dermatitis: skin is dry, itchy, irritated o Chemical-sensitivity dermatitis: chemicals added to latex- rash like poison ivy o Latex allergy- most serious; protein in rubber become airborne (skin & respiratory) o Oil based creams breakdown latex gloves • Hand hygiene o Soap & water: warm water, wet, soap, 15 sec, dry from fingers to wrist o Alcohol-based: apply, rub until dry, gloves • PPE: Gloves, mask, respirators, goggles, face shield, gowns • Cough etiquette Vital Signs • T, P, R, BP • Terminology: o Antipyretic- substance or procedure that reduces fever o Apnea- temporary or transient cessation of breathing o Auscultatory gap- temporary disappearance of sounds over brachial artery, when cuff pressure is high o Bradycardia- slow P rate, less than 60/min o Bradypnea- slow R rate, less than 12 breaths/min o Diastolic pressure- lowest pressure against arterial walls o Dyspnea- difficult breathing o Febrile- feverish o Korotkoff sounds- 5 sounds heard during BP o Oximetry- oxygen saturation of arterial blood using oximeter o Oxygen saturation- % of hemoglobin bound w/ oxygen in blood o S1 - first heart sound, mitral & tricuspid (atrioventricular) valves close o S2 – second heart sound, aortic & pulmonary (semilunar) valves close o Systolic pressure- maximum pressure against arterial walls o Tachycardia- fast P rate, above 100 beats/min o Tachypnea- fast R rate, more than 20 breaths/min • T: oral (posterior sublingual pocket), rectal (1-1.5 in) • BP- Korotkoff sounds. Initial sound is systolic & last sound is diastolic 1. Tapping sound 2. Soft swishing sound 3. Crisp sound 4. Blowing sound 5. Silence • Oxygen sat (95%-100%)- finger • Apical pulse- if regular count for 30 sec & mult by 2. If irregular or taking cardiovascular meds, count for 1 min for accurate rate Pain Management • Terminology o Adjuvant analgesia- drug used to treat something other than pain but also enhances pain relief o Analgesia- absence of sensitivity to pain o Analgesic- substance used as pain reliever o Analgesic ceiling- dose of a particular drug beyond which additional mounts of the same drug do not increase the analgesic effect o Patient-controlled analgesia (PCA)- drug delivery system that uses a computerized pump with a button o Titration- the process of gradually adjusting the dose of a medication until desired effect is achieved • Nociception: pain processing o Transduction: sensory neurons detect tissue damage thru neurotransmitter sensitization of nociceptors o Transmission: pain impulse transmitted from peripheral nerves to spinal cord o Perception: conscious awareness of pain o Modulation: neurotransmitters inhibit pain signals • The gate-control theory- nociceptive info travels thru small nerve fibers. If large nerve fibers are more active than the small, then the “gate” is closed and little or no pain. • Pain by: o Duration- acute, chronic o Etiology- cancer, burn o Pathology- nociception, neuropathic o Characteristics- idiopathic, phantom, referred, radiating, intractable • Assessment (PQRST) o Provoked: what causes pain o Quality: what does it feel like (stabbing, dull, sharp) o Region/radiation: where? o Severity: intensity (pain scale) o Timing: when did it start? How often/long? • CRIES o Crying (infants) o Increase oxygen requirement o Increase in vital signs o Expression on face o Sleeping • FLACC ( 2mo – 7yrs) o Facial expression o Leg movement o Activity o Crying o Consolability Week 2 Child Physical Assessment • Terminology o Anosmia- absence of sense of smell o Auscultation- listening for sounds within the body (stethoscope, Doppler) o Bronchial breath sounds- loud, high-pitched, hollow over trachea & large bronchi o Bronchovesicular breath sounds- medium-pitched & quieter sounds over mainstem bronchi o Bruit- blowing or swishing sounds of turbulent blood flow o Conjunctiva- delicate membrane that lines eyelids & covers exposed sclera o Crackles (rales)- wet, popping sounds created by air moving through liquid or by collapsed alveoli snapping open on inspiration. They are most common at the end of inspiration. o Crepitus- dry, crackling sound by air in subcutaneous tissue, air moving thru fluid in lungs, or bone rubbing against bone o Direct percussion- technique of striking the part being assessed w/ a finger, without placing another finger between percussing finger and body part o Edema- accumulation of excess interstitial fluid o Erythema- redness of skin produced by capillary congestion o Kyphosis- “hunchback” excessive convex curvature of the thoracic spine view from side o Nasolabial fold- skin crevice between the nose and corner of mouth o Nystagmus- rapid, repetitive, involuntary, rhythmic movement of eyeball o Palpebral fissure- the longitudinal opening between eyelids o Precordium- anterior surface of the body covering the heart & stomach o Ptosis- drooping of upper eyelid o Ronchi- dry, low-pitched, snore-like noises produced in throat or bronchial tube due to partial obstruction o Stridor- harsh, high-pitched breath sound heard on inhalation w/ acute laryngeal obstruction o Vesicular breath sounds- soft, fine, breezy, low-pitched sounds over peripheral lung tissue • Pediatric perspective o Engage w/ parent & child o Organize: least invasive procedures first, uncomfortable procedures last o Involve child: play games, explain, concrete terms, teach o Steady pace o Be honest o Age: ▪ Infants: nonverbal activities (holding, rocking, patting), toy, blanket, quiet voice ▪ Toddler: repetitive, short, concrete instructions; dolls/puppets ▪ Preschooler: verbal, some knowledge ▪ School-age: sensitive to embarrassment, explain ever step ▪ Adolescents: verbal/nonverbals skills, ask parent to leave for sensitive issues • General patient survey: appearance, behavior, body posture, facial expression, parent & child interaction • Anthropometric measurements: growth o Weight: infants (platform scale, diaper removed), toddlers/adolescents (standing) o Height: infants (horizontal measuring board), toddlers/adolescents (stadiometer) • Vital signs o Temp ▪ Infants: rectal, axillary, tympanic 99.4- 99.7 (up to 1 yr) ▪ Toddlers/preschoolers: axillary 98.6- 99.7 (1- 5 yrs) ▪ School-age: tympanic 98- 98.6 (5- 11 yrs) ▪ Adolescents: orally 97.8- 98 (11 & up) o Pulse Adult Physical Assessment Level of Consciousness • Assess level of consciousness (Glosgow Coma Scale) • Evaluate level of orientation if patient is alert o Can they tell you their name, where they are, what day • Evaluate level of responsiveness if the patient is not alert o Respond to voice, touch, pain? Glosgow Coma Scale Integument • Inspect skin systematically for color, hair distribution, lesions • Palpate & inspect skin for temp, texture, & moisture • Palpate & inspect skin for turgor, edema, lesions • Assess any lesions for location, distribution, size, shape, color, texture, surface characteristics, exudate, and tenderness. • Inspect & palpate the hair for quantity, distribution, texture, color, and parasites. • Inspect & palpate the nails for color, shape, thickness, adhesion to the nailbed, lesions, clubbing, and capillary refill. Ear • Adults: pull ear upward & back • Children: downward & back • Cranial nerve I: sense of smell (mint or coffee) Scenario notes • Inspection of the extremities is completed before palpating the peripheral pulses in the physical assessment. • Auscultation, percussion, and palpation are the appropriate order of the techniques used in abdominal assessment. • Romberg test- Balance. Ask the patient to stand about 2 feet in front of you, with her feet together, toes pointed forward, and her hands at her sides. While you extend your hands so that one is on either side of the patient, ask her to close her eyes. Watch to see how well she can maintain balance in that position. A minimum of swaying is normal, but if the patient sways more than a couple of inches, stop the test and document that the patient demonstrated difficulty maintaining balance on Romberg testing. Ambulation, transferring, & ROM Terminology • Abduction- movement away from the midline of the body • Adduction- movement toward the midline of the body • Atrophy- decrease in size • Circumduction- circular movement of a limb or eye • Contracture- a deformity that results from the abnormal shortening of muscle tissue, highly resistant to stretching • Dorsiflexion- upward bending of the toes & the foot • Eversion- turning of a body part away from the midline • Gait- the pattern of how a person walks • Passive ROM- the process of putting a joint through its full extent of movement by someone other than the patient • Plantar flexion- bending the toes & foot downward Assisting with Ambulation • Maintains muscle tone, strength, joint flexibility & stimulates respiratory, circulatory, gastrointestinal systems • If patient becomes weak or dizzy during ambulation & begins to fall, place one leg forward to ease patient to the floor • When ambulation is not an option: o elastic stockings o sequential compression device- promote venous return & prevent DVT o venous foot pumps Positioning • supine • prone • lateral- relieve pressure on sacrum • sims’- receiving an enema • orthopneic (tripod)- breathing problems • fowler’s- increase comfort, improve ventilation • Trendelenburg- lowering head & raising foot Cane Length- • Cane on unaffected side (6-12 in of foot) • Move effected leg forward even w/ cane • Move unaffected leg ahead of can • Bring cane forward and effected leg even w/ cane Crutches • Both crutches on unaffected side, push up on effected side to stand • Move crutches forward • 4 point gait- left crutch right leg, R crutch L leg • 3 point gait (one leg)- crutch forward move unaffected leg forward • 2 point (partial weight baring) • Swing-to (weight on both legs) • Swing-through (weight on both legs & have upper body strength) Nurse assist • Introduce, Hand hygiene • Gait Belt if needed • Stand in front, rock 3 times to lift and stand Bed to stretcher • Raise bed slightly higher than stretcher • 2 nurse on side of rolling, 1 on opposite side • Transfer board under patient • 2 nurse pulling patient onto gurney, 1 opposite pulling out transfer board Mechanical lift • Sling under patient, arms over chest • Raise head of bed • Lift patient into chair Specimen collection Terminology • Clean-voided (midstream) specimen- sample of urine collected after beginning to urinate into the toilet, stopping the stream of urine, then urinating into a sterile collection cup • Culture & sensitivity (C&S)- laboratory cultivation of micro-organisms in a body fluid or substance placed in a special growth medium, followed by the identification of the antibiotic agents that can kill the pathogenic micro-organisms grown • Guaiac- a tree resin used as a reagent in the detection of occult (hidden) blood • Glucometer- device to determine concentration of glucose in blood • Melena- black, tarry feces created by action of intestinal secretions on blood • Occult blood- blood present in small amts to be detectable by specific tests • Vacutainer- trade name for evacuated blood collection tube system Blood specimens • Capillary blood samples- blood glucose, soap and water, edge of finger • Blood glucose testing- 70- 105 mg/dL, test strips stored in vial at room temp • Venipuncture- drawing blood from vein • Peripheral line phlebotomy- peripheral venous and arterial lines Specimens • Sputum • Stool: fecal occult blood testing (colorectal cancer), home testing w/ 3 samples o Smear stool on card, flip card over, open add drops of developer o Read 30-60 sec o Color change (blue) presence of blood • Urine: clean-catch (sterile cup) & catheter- surgical asepsis • Wound: collect from center of wound, drainage Personal hygiene Terminology • Activities of daily living (ADLs)- tasks performed routinely during course of a typical day • Canthus- the angular junction of eyelids at either corner of the eye • Cheilosis- manifestation of vitamin B complex deficiency; reddened lips w/ fissures • Dental caries- tooth decay • Excoriation- skin abrasion typically resulting from scratching • Expectorate- expel fluid or secretions from the mouth, throat, lungs by coughing/spitting • Fanfolding- applying the proximal half of a piece of linen in successive layers lengthwise for the purpose of tucking it under the patient and rolling the patient over it while stripping or making an occupied bed • Halitosis- bad breath • Hypoallergenic- unlikely to cause an allergic response • Incontinence- involuntary release of urine from bladder or feces via anus • Lunula- active area of nailbed growth at the base of fingernails & toenails • Maceration- softening or dissolution of tissue after lengthy exposure to fluid • NPO- nothing by mouth • Pediculosis- lice infestation • Perineum- (gooch) area between anus & genitalia • Sebum- fatty lubricant secreted by the skin’s sebaceous gland • Smegma- thick, cheesy secretion that accumulates under the labia minora or male foreskin • Stomatitis- inflammation of mouth • Thrush- fungal infection in mouth/throat by Candida albicans, white patches & ulcers Bathing • Wash from head down, constantly changing wash cloths (one for eyes, one for genitalia etc) o Maintain pt. dignity & privacy the whole time o Allow independence if able o Long strokes o Arms: wash from hands to armpits o Legs: thighs to feet o Perineal care LAST • Therapeutic, head-to-toe skin assessment • Complete bed bath: critical & long-term care • Partial bed bath • Therapeutic bath: skin disorders, burns use oatmeal or cornstarch • Shower/tub bath o Wash mitt Bed making • Wear gloves, be prepared • Change linens after bath or while patient is in shower/out of room • Bed rest patient: administer prescribed analgesic 30-60 min before • Change bottom, top sheet, and pillowcase. Leave same mattress, blanket, bedspread if not soiled Other care • Denture care • Hair & scalp • Nail, hand, foot • Oral: side-lying position • Perineal: part of complete bed bath • shaving Enemas Terminology • cathartic- an agent that causes emptying of the bowels, stronger than laxative • flatulence- excessive formation of gases in stomach or intestine • suppository- a solid, dissolvable cone-shaped medication inserted into rectum Bedpans • regular- patient able to lift hips • fracture- body or leg casts • beside- able to get out of bed but cannot walk Supplies • enema bag • lubricant • prepackaged enema solution • clamp, tube • bedpan Types of enemas • left side Sims’ position or left lateral position w/ right knew flexed • 15- 30 min or as long as you can • Why? Diagnostic, constipation. Only cleans sigmoid colon • cleansing: tap water, normal saline, soapsuds • Return-flow: 100-200 mL, lower container • Oil retention: oil absorbed by feces making it softer, retain as long as possible • Medicated: reduce bacteria/systemic effect • Carminative: relieve flatus & abdominal distention Wound Care Terminology • Approximated- closed, w/ wound’s edges touching each other • Arterial insufficiency- inadequate blood flow thru arteries • Bulla- blister, greater than 1 cm in diameter filled w/ clear fluid • Contusion- bruise • Debride- remove dead tissue from wound • Decubitus ulcer- pressure ulcer, impaired skin integrity due to prolonged pressure • Dehiscence- opening of edges of surgical wound w/ partial or total separation of wound layers • Ecchymosis- hemorrhagic spot/bruise • Erythema- reddening of skin by congestion of capillaries • Eschar- slough (hard crust) produced by thermal burn, corrosive application, gangrene Dressing change • Introduce, confirm client, verify allergies, gather supplies, assess pain • Raise bed for comfort, hand hygiene • Some require sterile field/gloves • Absorbent pad beneath client • Use saline (if stuck) for removal • Remove gloves, hand hygiene, new gloves • Clean wound, measure, change gloves • Label dressing w/ pen on piece of tape • Hand hygiene, client is comfortable, document dressing change Dressing change w/ irrigation & packing- acute injury • Same first steps as above • Sodium chloride 35 mL- pressurized irrigation • PPE • Absorbent pad, remove bandage/packing • Irrigate, flow downward until clear, pat dry w/ gauze, measure • Sterile gloves for packing, change clean gloves for wrapping Dressing change w/ irrigation & packing- pressure ulcer • Same first steps • Asses size, appearance, drainage, odor, depth • PPE • Irrigate until clear, measure • Packing- secondary healing, topical meds Anatomy & Physiology • Healing process: o Hemostasis- blood clotting o Inflammatory- skin color, heat, swelling, pain o Proliferative- restores skin integrity w/ new tissue, angiogenesis o Remodeling- scar tissue Basic wound care Drains Dressing & bandages • wet-to-dry: debridement; saline soaked gauze in wound, as it dries. It pulls exudate out of wound Negative pressure wound therapy Week 3 Nasogastric Tube Terminology • antireflux valve- device inserted into lumen of NG tubes to prevent seepage of gastric contents out of vented lumen • aspiration- inadvertent inhalation of fluid/other substances into lungs • flatus- gas or air generated in the stomach/intestines and expelled via anus • gastric aspirate- a substance/material obtained by withdrawal, via syringe, from stomach • ileus- mechanical/functional obstruction of intestines • lavage- therapeutic irrigation/washing out of a body part/cavity • lipid pneumonia- lung inflammation from fat particles entering bronchial tree • methemoglobinemia- presence of excessive methemoglobin (non-oxygen carrying pigment) in blood • parotid glands- 2 salivary secretory organs below & in front of ears • patency- state of being open/unobstructed • suction pressure- amount of negative force (mm Hg) to propel air/fluid out of body NG tube • purpose: o decompress the stomach & remove gas & fluid o lavage the stomach to remove ingested toxins other than poison o to diagnose problems w/ gastrointestinal motility o treat obstruction o compress a bleeding site when endoscopy is not immediately available o aspirate contents for analysis o administer radiographic contrast media to the gastrointestinal tract • types of tubes o double-lumen (two-channeled) gastric (Salem) sump tube: clear plastic, preferred for gastric decompression o single-lumen (Levin) tube: plastic or rubber, circular markings o Miller-Abbott: dual-purpose, simultaneous gastric suction & enteral feeding o Sengstaken-Blakemore tube: 3 lumen tube treat upper gastrointestinal bleeding; internal balloon to prevent hemorrhage Inserting a NG tube • high fowlers position- reduces risk of aspiration and promotes effective swallowing, raise bed level with hips • stethoscope, pen light, bath towel, water, emesis basin, pH strips, tongue blade • set up & then don gloves • steps o assess gag reflex- ability to swallow, risk of aspiration o measure tube: tip of nose to earlobe, to xiphoid process o lubricate first 4 in of tube o give patient water; towel, emesis basin, tissue in reach o insert tube: back & down o auscultate for breath sounds o test pH (1-5) to verify tube is in stomach o confirm tube placement w/ x-ray Gastric decompression • withdrawal fluid & check pH • connect NG tube to suction tube Care & maintenance of NG • check drainage • typical irrigation schedule- every 4 hrs • check pH • rinse tube w/ water & reconnect to suction tube • inspect skin around tube • water based lubricant in nose • frequent mouth care Removing NG tube • untape • some tubes have distal balloon, deflate balloon before removal • hold breath & remove Enteral Tube Feeding Terminology • carina- a projection of the lowest tracheal cartilage that forms a prominent semilunar ridge between orifices of the two bronchi • formula- mix of nutrients in liquid form, delivered to stomach or intestines • gastrostomy tube- hollow cylindrical device surgically into stomach • jejunostomy tube- tube surgically into jejunum • nasogastric tube- thru nose into stomach • nasoduodenal tube- thru nose & extending into duodenum • nasointestinal tube- thru nose into intestines (gastric ileus) • nasojejunal tube- thru nose into jejunum • percutaneous endoscopic gastrostomy (PEG) tube- endoscopically opening into stomach Inserting feeding tubes • medical history for nasal problems -> contraindicate tube insertion: nosebleeds, nasal polyps, chronic sinus infections, oral/facial/sinus surgery, aspiration, anticoagulant therapy • measure tube: nose-earlobe-xiphoid process; add 20-30 cm for duodenal or jejunal placement • inserting: o tip head back & breathe thru mouth o insert passed nasopharynx, then flex head toward chest & swallow o check position w/ penlight & tongue blade o observe for difficulty breathing, coughing, gagging o test gastric pH (1-5) grassy green, off-white & watery o confirm tube placement by x-ray • formulas: o warm to room temp, clean can w/ alcohol swab, check expiration, shake well o elemental- 1-3 kcal/mL; predigested nutrients that are easy for partially functional gastrointestinal tract to absorb o polymeric- 1-2 kcal/mL; whole nutrients (milk based blenderized foods), require functioning gastrointestinal tract o modular- 3.8-4 kcal/mL; single macronutrients (protein, glucose, polymers, lipids) not nutritionally complete; require functioning o specialty- 1-2 kcal/mL; meet specific nutritional needs for specific illnesses (liver failure, pulmonary disease, diabetes, HIV) Medication Administration 1 Terminology • adverse reaction- (adverse effect) noxious, unintended, undesired result of drug • allergic reaction- immune response to drug; mild itching to severe rash to anaphylaxis • anaphylaxis- immediate/life-threatening allergic response characterized by bronchospasm, laryngeal edema, rapid drop in BP • contraindication- pre-existing condition makes it unsafe/inappropriate to administer a drug • enteral- within or by way of the intestines • generic- (nonproprietary name) a noncommercial name of drug, less complex than chemical name & more complex than a brand/trade • idiosyncratic reaction- uncommon, unexpected, individual drug response result from genetic predisposition • instillation- administration of a liquid drop by drop • nebulizer- a device for creating & delivering an aerosol spray • ophthalmic- pertaining to the eye • paradoxical reaction- causing an effect opposite of intended effect • parenteral- via a route other than GI tract: subcutaneous, intramuscular, intrathecal, intravenous • polypharmacy- the concurrent use of multiple drugs • PRN- as needed • Synergistic effect- an increase in the effects of any drugs taken together • Toxic effect- seriously adverse drug reaction; excessive dosing • Unit-dose system- provision of drugs in single-dose packages Drug calculations/conversions (notes & examples in goodnotes) • Dimensional analysis • Ratio & proportion • Desired over have Drug tolerance & dependence • Tolerance: develops as a patient’s physiological response to the medication decreases after repeated administration • Dependence: o Psychological- intense feelings of craving for a substance (addiction) o Physical- needs a drug to function (withdrawal) Medication order • Patient name, date, name of drug, dose, route, frequency, signature of prescribing person Six Rights 1. Right medication- check medication label to medication administration record (MAR) 3 times before administering (as you remove med, as you prepare med, at patient’s bedside) 2. Right dose 3. Right route 4. Right time- 30 min before or after scheduled time is still the “right” time 5. Right patient- check ID band, name, & ID against MAR 6. Right documentation Routes • Parenteral: most direct & reliable; amuples, vials, syringes • Nonparenteral: oral- local & systemic effect, skin Medication Administration 2 Terminology • Canthus- angles formed by eye’s upper and lower eyelid • Cerumen- waxlike substance within ear • Conjunctival sac- space between eyelid and eyeball • Dorsal recumbent position- lying on back with knees flexed • Expectorate- expel secretions from throat or lungs by coughing & spittings • Instillation- administration of liquid drop by drop • Intraocular medication disk- small medication-delivery device resembling contact lens & inserted into conjunctival sac • Liniment- liquid or semiliquid preparation containing oil, alcohol, or water & applied to skin • Medication administration record (MAR)- a document completed per agency policy to verify that patients medications were administered as prescribed • Metered-does inhaler (MDI)- medication-delivery device that disperse medication as aerosol spray • Mydriatic- any drug that dilates the pupil • Ophthalmic- pertaining to the eye • Otic- pertaining to the ear • Pruritus- itching • Suppository- solid, dissolvable medication inserted into rectum, vagina, urethra • Suppurating- forming or discharging pus Administering meds • Inhaled • Nasal: have patient blow nose, supine position w/ head positioning • Nasogastric: crush solid meds and mix w/ sterile water • Ophthalmic: drops, ointments, intraocular disks • Oral, sublingual, buccal • Otic: room temp; pull pinna up & outward (adults), pull pinna down & back (children) • Rectal: bullet-shaped & refrigerated; rectum melts the meds • Topical: clean area then apply • Vaginal: oval-shaped & refrigerated Medication Administration 3 • Ampules- glass, single-use containers for liquid injectable meds o Flick top to remove medication, pull back top to snap off o Filter needle to withdrawal meds • Vials- plastic or glass containers for liquid or powder meds o Use sterile needle o Pressurize vial by drawing air into syringe, inject air and draw up solution • Syringes- packaged for single use (1mL-5mL) o 3 parts: barrel, tip, plunger o Luer-Lok tip: twist needle on o Non-Luer-Lok tip: push then twist on • 1 ½ in needle for intramuscular injection in ventrogluteal area o Heel of hand on greater trochanter, point index finger up toward the anterior superior iliac spine, extending the other fingers back along the iliac crest • Intradermal= tuberculin syringe 3/8 – 5/8 in, 25-27 gauge needle o Circle area w/ pen Week 4 Nutrition, Feeding, & Eating Terminology • Albumin- plasma protein formed in the liver and accounting for 2/3 of protein in plamsa • Amino acid- building blocks of protein • Anabolism- constructive phase of metabolism, synthesize protoplasm for growth & repair • Anthropometric measures- data for studying size, weight, proportions of body • Ascorbic acid- vitamin aids in tissue building & metabolic reactions (wound/fracture healing) • Bioelectric impedance analysis- estimating body composition that determines body tissues opposition to flow of electric current • Cachexia- physical wasting & malnutrition related to chronic disease\ Assisting w/ feeding • High fowlers • Help patient wash their hands • If necessary, refer to plate as a clock • Social: family time, engage in assistance Dietary modifications • Clear liquid: broth, fruit juices, gelatin, popsicles, coffee, tea • Full liquid: clear liquid & smooth textured dairy- custards, cooked cereals, vegetable juice, fruit juices • Pureed: full liquids & scrambled eggs, pureed meats, vegetables, fruits, mashed potatoes • Mechanical soft: ground meat, cottage cheese, rice, pancakes, bananas, peanut butter • Soft/low residue: low fiber, easily digested; pastas, tender meats, canned cooked fruits & vegies • High fiber: uncooked fruits, steamed vegies, corn meal, dried fruit • Modified fluid consistency: cream soups, honey, yogurt, pudding Fluid • Consume 2,000-3,000 mL of water daily • Avg output: 2,300-2,600 mL per day Airway Management Terminology • Atelectasis- airlessness or collapse of a lung; result of hypoventilation or obstruction • Endotracheal tube (ET)- a hollow tube inserted in trachea to establish & maintain a patent airway • Hypercapnia- an excess of CO2 in blood • Hypoxemia- diminishes amount of oxygen in arterial blood • Hypoxia- reduced supply of O2 to tissues • Obturator- device used to guide outer portion of tracheostomy tube during insertion • Postural drainage- mobilizing pulmonary secretions by positioning patients head downward to facilitate removal of secretions by gravity • Yankauer suction catheter- plastic or metal tube w/ curve at distal end to facilitate the removal of thick secretions during suctioning Suctioning • 100-120 mm Hg • Place water soluble lubricant on sterile surface • Don sterile gloves • Pour saline solution into basin • Connect suction catheter and tubing • Lubricate end and advance into nares o Nasopharyngeal: 16 cm o Nasotracheal: 14-20 cm • Suction 10-15 sec; wait 1 min between passes; no more than 2 at one time ET tube care • PPE, hand hygiene, don gloves • Suction mouth & airway • Remove securing device • Clean mouth: brush, suction • Reposition tube to other side of mouth every 12 hr • Tape to secure tube: have benzoin to apply to patients face Tracheostomy care • Suction • Remove dressing • Sterile glove on dominant hand • Non dominant hand- pour saline • Sterile glove on nondominant hand • Premoisten gauze • Remove inner cannula & clean w/ pipe cleaner • Clean outer cannula • New dressing- commercially prepared fenestrated dressing Oxygen Therapy Terminology • Apnea- cessation of respiration • Atelectasis- airlessness or collapse of lung; result of hypoventilation or obstruction • Bi-level positive airway pressure (BiPAP)- noninvasive, ventilation-assistance provides higher airway pressure during inspiration & lower pressure during expiration • Continuous positive airway pressure (CPAP)-noninvasive, ventilation-assistance provides positive airway pressure • Flow meter- controls rate of oxygen being delivered in liters/min • Fraction of inspired oxygen (FiO2)- oxygen level inhaled by or delivered to the patient • Hypercapnia- excess CO2 in blood • Nonrebreather mask- delivery high flow rates & high concentrations of O2 via a mask that fits snugly over mouth & nose • Positive-pressure ventilation- force air into lungs to provide breathing assistance • Venturi mask- holes on each side allow exhaled air to escape & color-coded entrainment ports that are adjustable to allow regulation of the concentration of oxygen delivered Care of patients receiving O2 • COPD o O2 too high flow rate -> CO2 narcosis (causes confusion, tremors, convulsions, coma) can lead to respiratory arrest • Semi- or high-fowlers position: helps facilitate lung expansion • Add padding to areas that irritate skin • Oxygen considered a medication (need order from provider) • Humidification of flow rate 4L/min or more Nasal cannula • Verify order, delivery device, & flow rate • Insert cannulas prongs in nares & loop tubing around ears Bed Position - 30 degree is common, prevent aspiration and help w/ ventilation - Suctioning & better ventilation High fowlers Severe dyspnea, during meals to prevent aspiration [Show More]
Last updated: 1 year ago
Preview 1 out of 23 pages
Reviews( 0 )
Document information
Connected school, study & course
About the document
Uploaded On
Mar 18, 2023
Number of pages
23
Written in
Additional information
This document has been written for:
Uploaded
Mar 18, 2023
Downloads
0
Views
16











.png)
.png)

 (1).png)