*NURSING > EXAM > West Coast University: NURS 100 Midterm Study Guide Latest updated 2022/2023,100%CORRECT (All)
West Coast University: NURS 100 Midterm Study Guide Latest updated 2022/2023,100%CORRECT
Document Content and Description Below
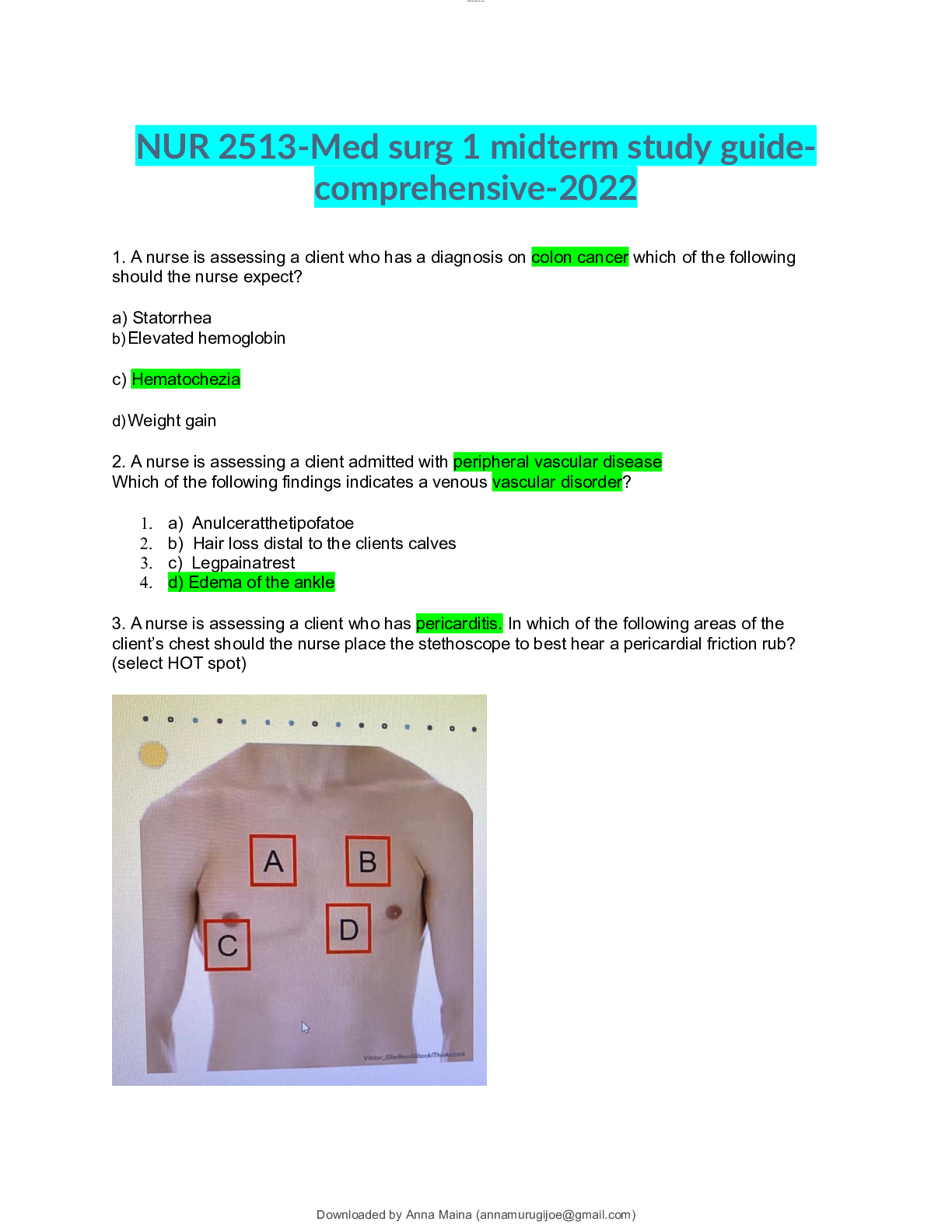
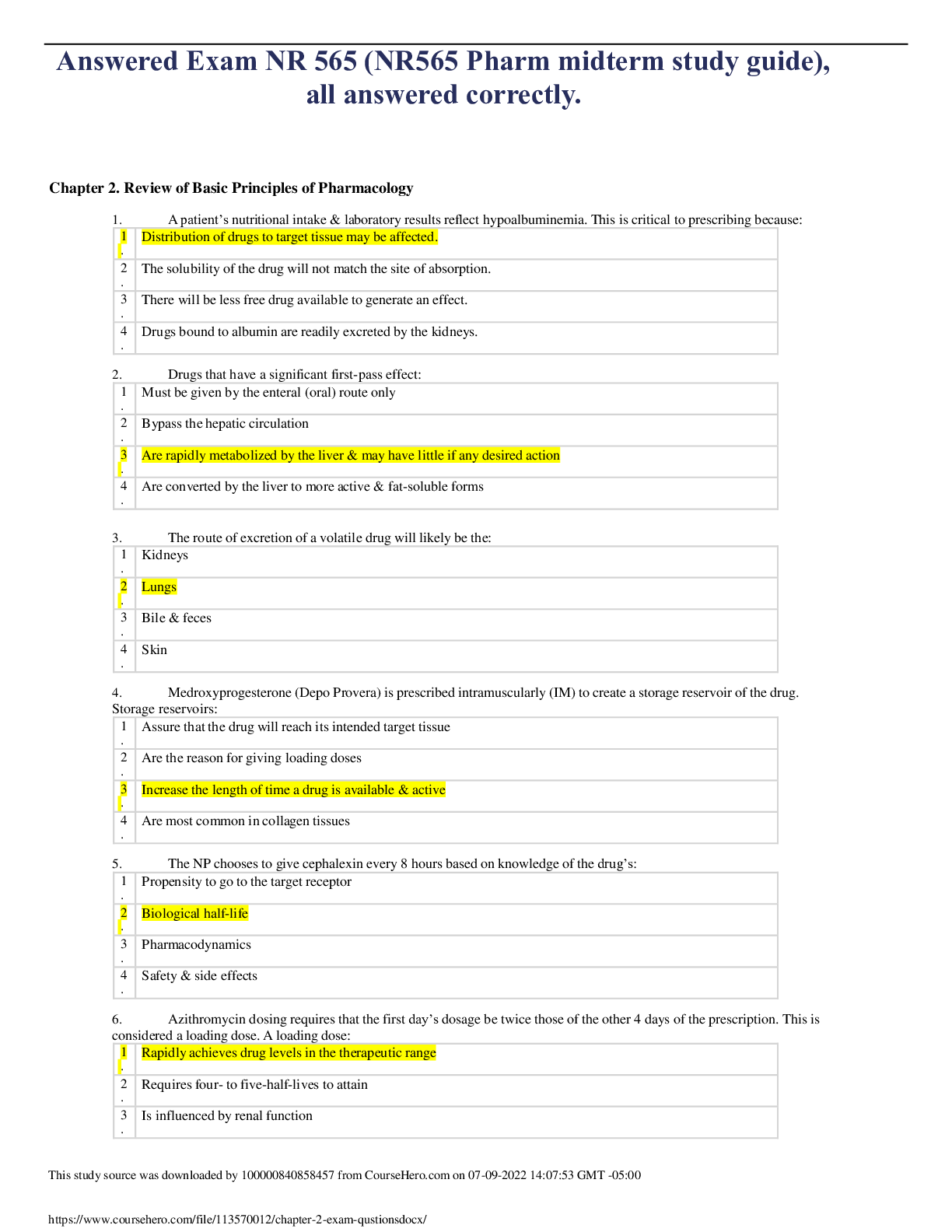
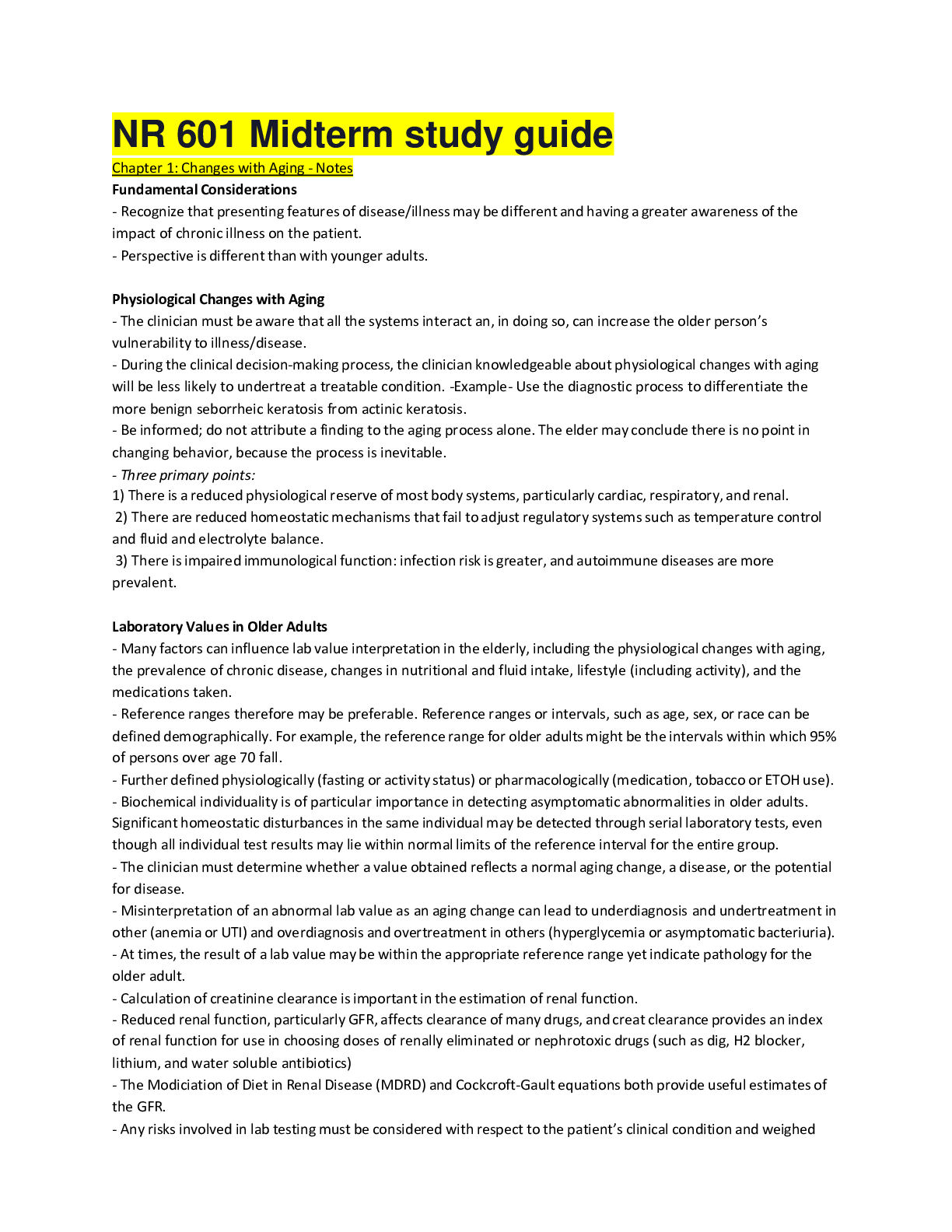
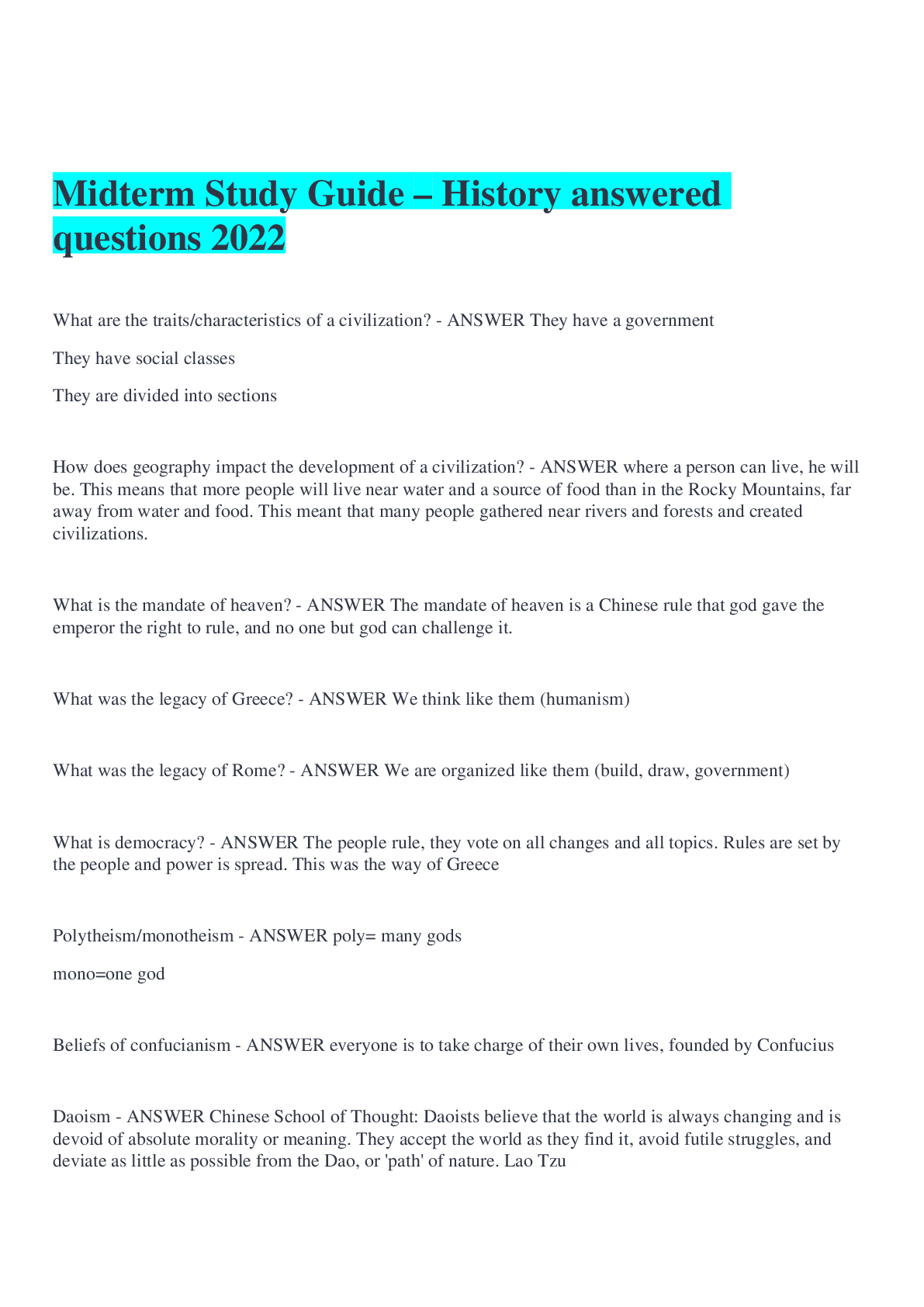
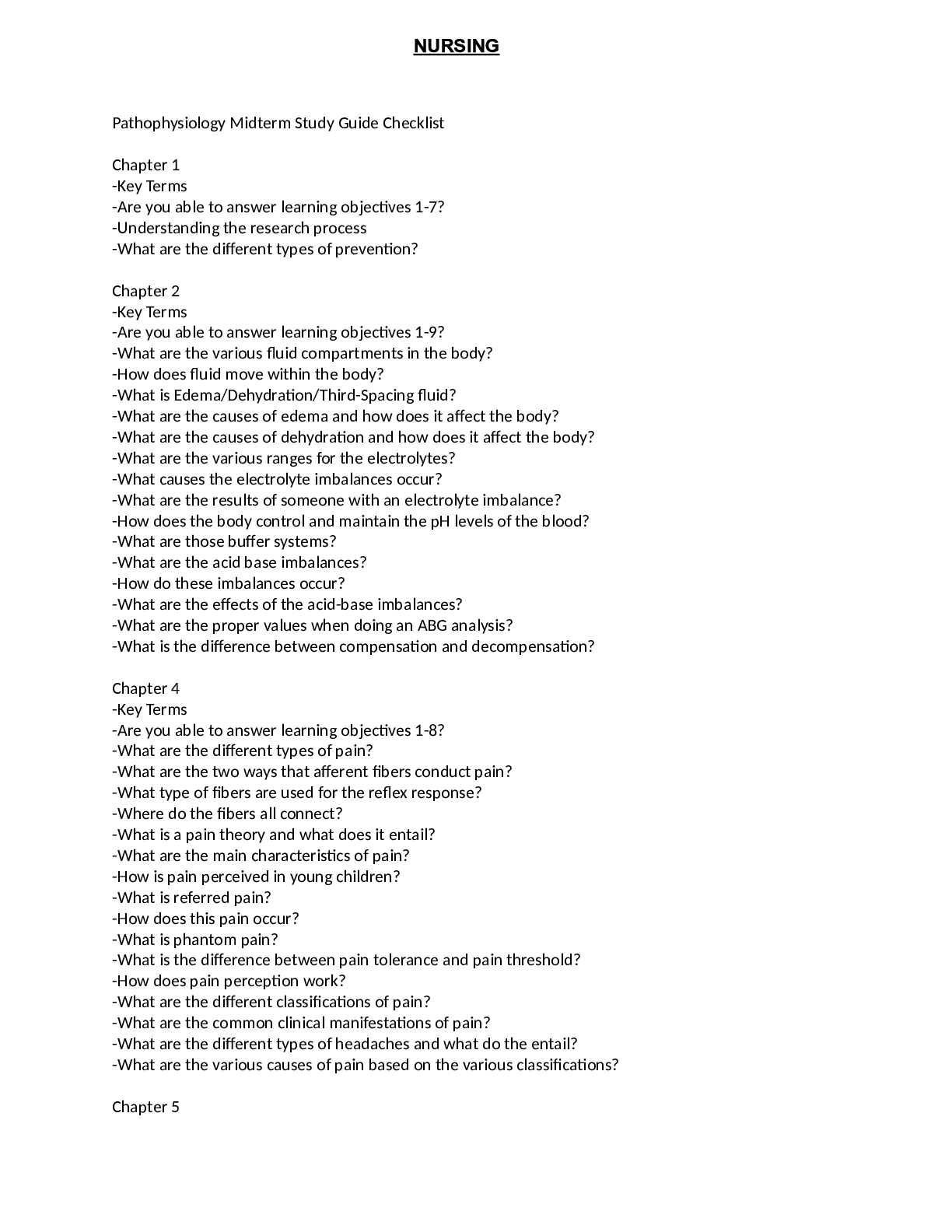
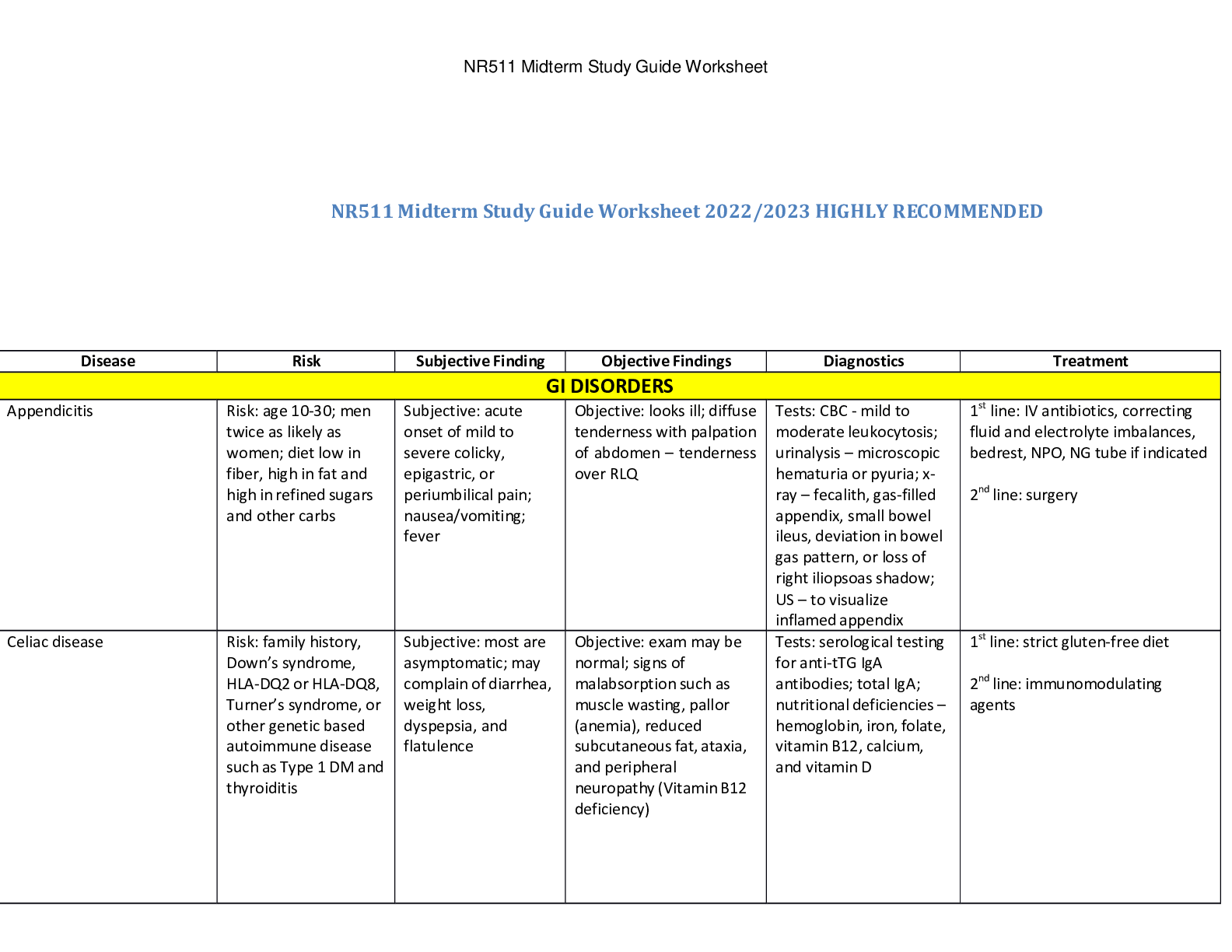
West Coast University: NURS 100 Midterm Study Guide Latest updated 2022/2023 1. Fall prevention: - Patients are at risk for falls (dementia, Alzheimer’s, confusion, vision, HISTORY OF FALLS) Indic... ations for risk for falls: yellow nametag, yellow signs. Patient safety #1 - When patient starts to fall, SLOWLY let them slide on the floor, close to you. 2. Occult blood: test to see hidden blood in the stool (can send specimen stool to lab to see if there is blood in the stool) - Black stool indicates: iron consumption or food/medication 3. Nursing DX for sleep disorders or lack of sleep: - Insomnia (inability to sleep) - Sleep apnea (when sleeping, there is absence of breath. Use specific CPAP machine to help you breath while asleep) - Narcolepsy (can fall asleep anywhere) - Sleep deprivation (lack of sleep) 4. Physical assessment: (Why: to create plan of care) *DOCUMENT EVERYTHING* - Neurological system: Visual assessment (look @ patients color, breathing pattern, face, posture (brain stem abnormalities)) Introduce yourself Determine LOC (x4= patient is alert/oriented (0-4)) - person (aware who they are?) - event (where they are?) - situation (who is the president of the USA?) - time frame (what day is today? Or what time is it?) Asking for patient’s identification, check for level of consciousness Pupils: Cranial nerve III (Oculomotor) responsible for pupil size and certain movement of the eye (Brisk= rapid response where the pupils constricts/dilates fast) Cranial nerves Masses on the head (Ex: bumps/ lumps) Speech: Check for verbal communication, clear speech, and how they respond (Ex. Stoke (slurred)) Vital signs & medical histories - Eyes: First assessment PERRLA (Pupils, Equal, Round, Reactive, to Light, Accommodation) - Penlight (pupils will constrict and dilating) - alter pupils: drugs, alcohol, stroke, brain damage Cranial nerve: III (Oculomotor) responsible for pupil size and certain movement of the eye - Mouth & Tongue & Neck & Ears & Nose: “AAHHH” checking if the Uvula wiggles (one of the cranial nerves) moisture, don’t want it to be too dry Teeth, missing tooth tongue for any open sores PINK tongue= normal NORSE & EARS: Check for any abnormal drainage, objects NECK: check Lymph nodes - Lungs: Check for patients color, chest raising, respiration, O2 saturation, ask for shortness of breathe Listen to 6 anterior and 8 posterior (last 2 will be in the last two lower lobes) Abnormal sounds= adventitious Crackles = high pitched, sound like rice crispy (snap crackle pop) can be heard with patients with pneumonia Rhonchi = low pitched, sounds like SNORING; can be heard with patients with COPD Wheezing = musical; asthma patients Stridor = see it more on children (choking) - Heart: Aortic, Pulmonic, ERB’s point, Tricuspid, Mitral (All People Enjoy Time Magazine) Listening for LUB-DUB S1 = Tricuspid & Mitral valves closing (LUB) S2 = Aortic & Pulmonic valves closing (DUB) Aortic: 2nd Right ICS Pulmonic: 2nd Left ICS ERB’s: 3rd Left ICS Tricuspid: 4th Left ICS Mitral: 5th ICS Left mid-clavicular line - Abdomen: First thing you do is Inspection (look), then Auscultation (listen) to the different quadrants and or bowl movements, finally Palpation (feel) asking if there is any tenderness, pain, masses. Ask when was the patients bowl movement? Belly button as middle/center Right upper/lower quadrant, left upper/low quadrant - Right LQ: appendix - Left LQ: most likely won’t hear anything - Skin: Looking at the color, edema, texture, rashes: Cyanosis: blue Jaundice: yellow Pale: white Dusky: grey Diaphoretic: sweaty Ecchymosis: black and blue (bruise) Edema (water swelling): the depth, indentation (2mm = 1+ mild edema 8mm = 4+) - Elevate the leg - Ted stocking (venous return) for Deep vein Thrombosis (at risk = immobility) - Do not massage b/c can dislodge blood clot and cause embolism - Pressure ulcers: Stage 1: redness (no circulation) sores are not open Stage 2: skin is broken-down Stage 3: subcutaneous (deep) Stage 4: sore is very deep reaching into muscle/bones causing extensive damage Braden scale: determine if the patient is at risk for pressure ulcers (sensory perception, moisture, activity, mobility, nutrition, and friction/sheer) Re-Positioning/Positioning patient every 2 hours to prevent pressure sore/ulcers - Skin tenting/turgor: Best places to check are around the neck area and sternum. Skin is tenting which means patient is suffering from dehydration. The skin is very slow to return to normal, or the skin "tents" up during a check. This can indicate severe dehydration that needs quick treatment. To check for skin turgor, the health care provider grasps the skin between 2 fingers so that it is tented up. Commonly on the lower arm or abdomen is checked. The skin is held for a few seconds then released. Skin with normal turgor snaps rapidly back to its normal position. Capillary refill: pushing down on the nail beds and should come back to a pink color within 2-3 seconds after pressure is remove (used to monitor dehydration and blood flow to tissues) 5. Vital Signs: - BP: 120/80 normal Alter BP: medication, anxiety, caffeine, smoking, exercise. * double check, if come out with abnormal BP, CHECK AGAIN* Ex: if CNA says patient’s BP is 80/60 nurse must recheck BP. DON’T give medication right away!! #35. Prehypertension: 120-139/80-89 - Pulse: Adults 60-100 beats (normal) less than 60= bradycardia more than 100= tachycardia - where to take a pulse: radial, corroded, brachial, femoral, petal, popliteal, apical CPR: if patient is not breathing, check patients corroded for pulse (#6) If pulse still irregular after 1 min. on radial/brachial pulse go to apical pulse for 1 minute listen to the 4th and 5th intercostal space. Altered pulse: coffee, exercise, anxiety, postop patient (Ex: patient has 120 heart rate). Assess and ask if patent is alert and oriented and how their feeling. - Temperature: where to take temperature: oral, axillary (armpit), tympanic (ear), temporal (forehead), rectal. - Ex: a lady’s temp shows 101.7, she has a fever but patient looks fine. There is alteration of temperature such as: drinking something hot. Each route will have different readings rectal higher than oral, oral higher than axillary, different readings depending on route. - Respiration: Normal 12-20 breathes/min. Oxygen: Pulsox (clips on finger to see oxygenation of blood) Normal 95-100 (but if patient has O2 of 92 and patient looks good, color good, no cyanosis then 92 is fine. Anything less than 90 = concern, desaturation begins meaning O2 level is going down and their having difficulty breathing. Shortness of breath first thing to do it put the head of the bed @ Fowler’s (sitting UP) As nurses, we can put oxygenation @ 2L if patient has shortness of breath. CANNOT put it up unless doctor’s orders. (Color, lips blue, wheezing, sweating 7 & 30. Pain management/ pain medication: - Pain: P: Provoke- what were you doing when the pain started? Q: Quality- what does it feel like? Ex: dull, shooting, stabling, sharp R: Radiating- where is the pain located? S: Severity- level of pain 0-10 scale T: Time- when did it start? How long does it occur? - Give pain medication before pain gets severe 10. Give medication 30 before a procedure like ambulating. (administer pain medication) - Pain medications: - Opioids (side effect: constipation (make sure patient is moving their bowls appropriately) Ex: Anesthesia (slows down organs, make sure that patient is moving their bowls appropriately) - NSAIDS, Aspirins (side effects: GI bleeds) #32 - Managing client’s pain, best time to teach patient on other treatments: before medicating patient 8 & 36. Communication: SBAR (SBAR is what you want to communicate to doctors, other nurses) S: situation - something that is happening NOW (present). Nurses communicate with EVERYONE. Give solid information. B: background- what happened in the PAST, the history of the patient (Ex: history of hypertension, diabetes) you want to give the provider or whoever you’re communicating with the background. A: assessment- how you’re assessing the client (vital signs, skin color, what the heart sounds like, what the lungs might sound like, bowl; head-to-toe assessment) R: recommendation- what you recommend for the FUTURE (Ex: lab values that patient may need to determine what’s going on with the patient, diagnostic test, discharge if the patient is ready to go home vitals look stable and lab values look good and no more complaints) - Nurses are with patients day after day, nurses know the patients more than the physicians. Nurses can recommend things to the doctor for the patient. Ex: of SBAR - When calling a doctor, first thing you do is introduce yourself “I am a RN Janelle, I am taking care of patient on the 5th floor Mr. Jones in room 101 he came in complaining about chest pain, today he is complaining for chest pain again of the scale of 0-10 he is saying it is a 7 we’ve given him 3 nitroglycerin and he’s still complaining of pain his background is no problems in the past, history of hypertension, right now his color is pale, diaphoretic, very anxious, vitals are , can we do some lab work on him, and we have an EKG on him. Certified interpreter or gestures or AT&T interpreter (phone) or picture boards -if client does not speak English and if client speaks another language. CANNOT ask a family member, or anyone to translate to client. MUST have a certified interpreter. Ex: stroke patients; their speech is slurred so nurse cannot understand them and they may understand the nurse but their communication on their end is not appropriate so nurse can use a picture board or ways to communicate with them. - Documentation is very important, NOT documented = NOT done *Cover your butt and make sure everything is documented* *Document everything done to patient at all times* - Doctor’s orders * Whenever in DOUBT about a Doctor’s order, it is BEST to call the Doctor directly to verify the order* 9. Administering Enema: STOP when patient feels pain or bleeding 10. S&S of infection: swelling, redness, warm to touch, elevated temperature, elevated WBCs, & fatigue 11. Bedpan: 2 types: regular bedpan & fracture bedpan Position bed: Elevate the head of the bed Positioning immobilized patient on bedpan: - Place bedpan firmly against buttocks - Push buttocks down into mattress with open rim toward feet - Place one hand against bedpan; place other hand around patient’s fore hip 12. Physical assessment findings for a patient with heart/lung disease: - Normal nail: 160-degree angle between nail plate & nail - Nail clubbing: larger than 180-degrees - Clubbing means lack of oxygen, affecting the heart - Causes: Chronic lack of oxygen; HEART or PULMONARY disease - Respiratory & cardiac diseases can be assessed through the fingers and nails 13. Subjective & Objective Data: -Subjective: Symptoms (what the patient says) - Objective: Signs (vitals, lab value, etc.) 15. Personal Hygiene: CLEAN to DIRTY 16. PPE: Universal precaution: GLOVES Contact precaution/isolation: Bacteria (C. Diff, Pneumonia, MRSA, E. Coli, Varicella) Gloves and gown (Ex. E. Coli: urine) wherever you come in contact *most common* Airborne Droplet 17. Purpose of physical assessment: to create a plan of care 18. Sterile Techniques: 1in. boarder around sterile field = non-sterile 19.Dietary meal plan to promote healthy bowel elimination: HIGH FIBER 20: Sensory deficit: speech, vision, and hearing loss - The older you get, your sense decrease - Stroke patients have slurred speech and cannot communicate appropriately 21. HAND WASHING & INFECTION CONTROL = to prevent infection *Wash with warm water and soap if patient has C. Diff (infection transmitted through fecal; patient would have diarrhea LOTS) 22 & 23. Patient teaching when client on narcotic pain killers: Constipation (give patient fiber and fluids) 24. ADL’s: Bathing Dressing Feeding Brushing teeth 25 & 26.Nursing DX for patient with communication problems: aphasia - Communication = gestures, pictures, body language 27. Acrylic nails why are they discouraged? - Capillary refills - Bacteria/infection - O2 saturation 28. Atelectasis: collapsed lung, breath sounds = no breathe sounds at all or diminished 29. 2 types of aphasia: - Receptive aphasia: difficulty understanding spoken or written language - Expressive aphasia: inability to convey information/thought verbally or writing. 31. Know abnormal/adventitious breath sounds: Abnormal sounds= adventitious Crackles = high pitched, sound like rice crispy (snap crackle pop) can be heard with patients with pneumonia Rhonchi = low pitched, sounds like SNORING; can be heard with patients with COPD Wheezing = musical; asthma patients Stridor = see it more on children (choking) 34 & 37. Orthostatic HP & Intervention when ambulating client who has been in bed rest for a long period of time: - Orthostatic hypotension: dizzy when getting up. Blood Pressure DROPS. - Sit patient up on the bed, let feet dangle and take few breathes before standing up - Stand patient slowly 38. Wound Dehiscence & Evisceration: - Dehiscence: the layers of the skin open up, so incision site will open separation of the wound layers - Evisceration: opening of the incision, protrusion of the internal organs 39. Negative effects of immobility on all systems: - Neurological: depression - Lungs: pneumonia or atelectasis - Muscles: weak or atrophy - GI: constipation 40. Restraints: - When to apply: history of violence or previous falls - Need Doctors order, if by phone Dr. has 24 hr. to sign - Make sure restraints are not too tight = 2 fingers - Tie to bed not side rails 41. Stages of pressure sores, nursing interventions on how to prevent, Braden scale: - Pressure ulcers: Stage 1: redness (no circulation) sores are not open Stage 2: skin is broken-down Stage 3: subcutaneous (deep) Stage 4: sore is very deep reaching into muscle/bones causing extensive damage Braden scale: determine if the patient is at risk for pressure ulcers (sensory perception, moisture, activity, mobility, nutrition, and friction/sheer) Re-Positioning/Positioning patient every 2 hours to prevent pressure sore/ulcers [Show More]
Last updated: 1 year ago
Preview 1 out of 9 pages
Reviews( 0 )
Document information
Connected school, study & course
About the document
Uploaded On
Mar 26, 2023
Number of pages
9
Written in
Additional information
This document has been written for:
Uploaded
Mar 26, 2023
Downloads
0
Views
15