*NURSING > STUDY GUIDE > NURSING 306 / N306 Exam 1 Final Study Guide, Complete solution Guide(2019/2020), West Coast Universi (All)
NURSING 306 / N306 Exam 1 Final Study Guide, Complete solution Guide(2019/2020), West Coast University.
Document Content and Description Below
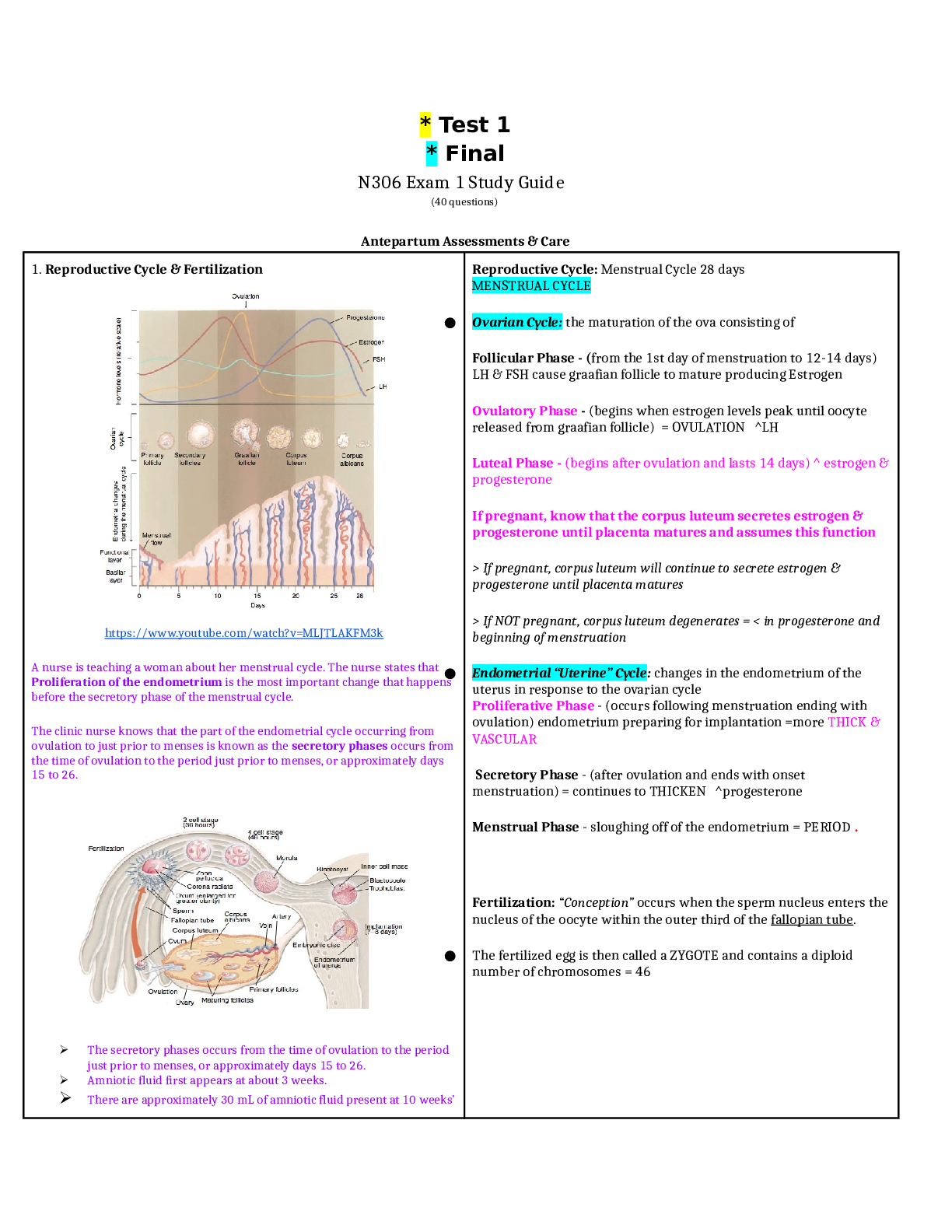
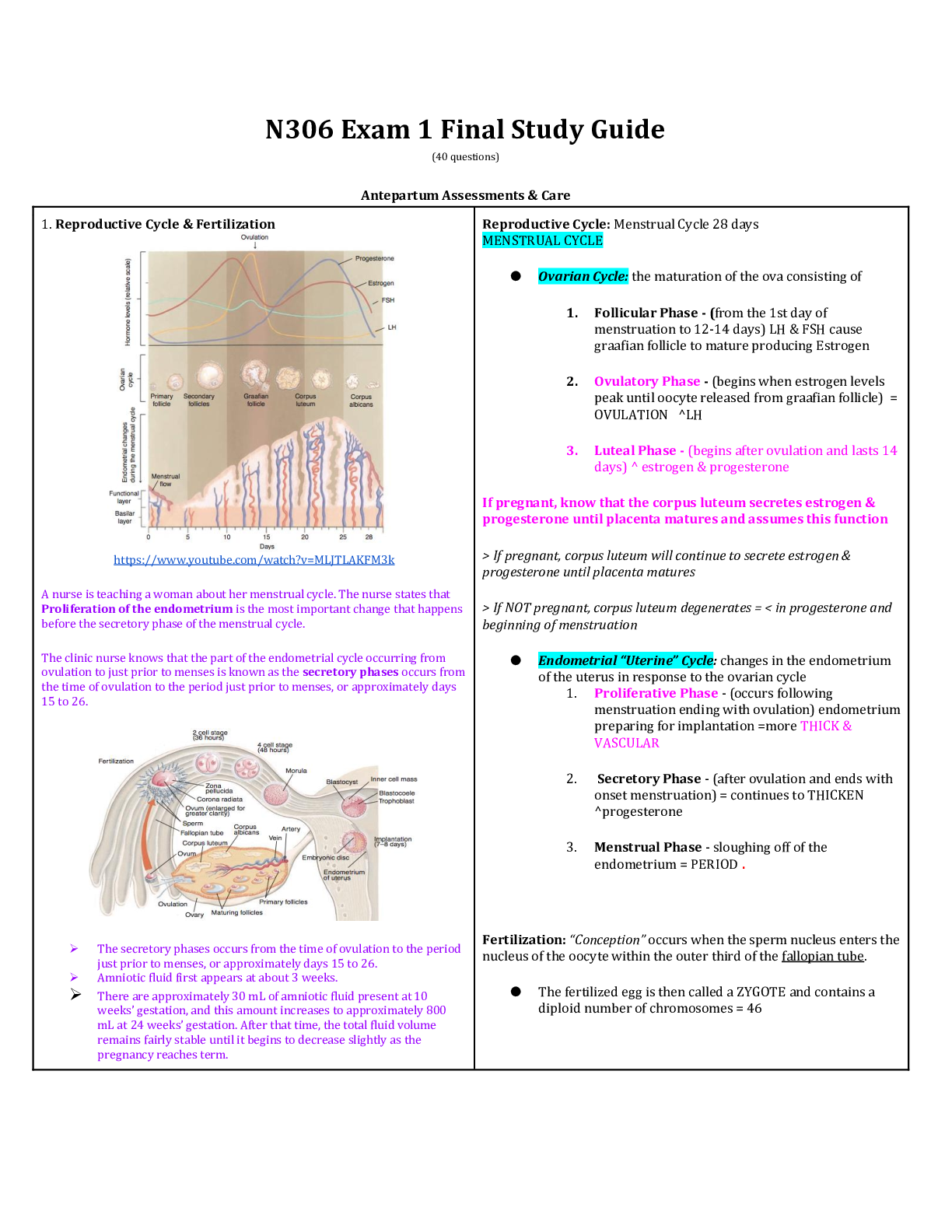
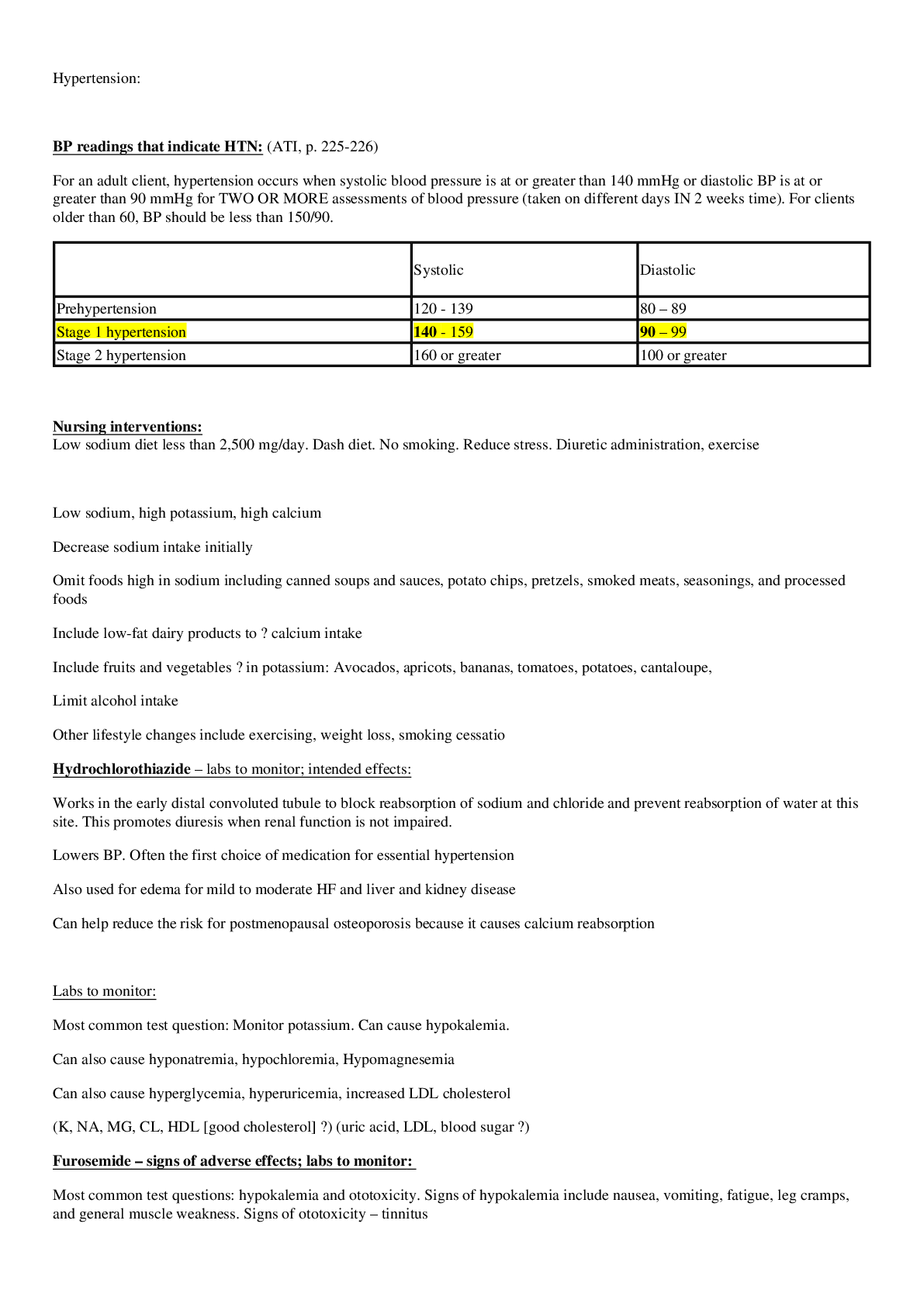
• Reproductive Cycle: Menstrual Cycle 28 days • MENSTRUAL CYCLE • ● Ovarian Cycle: the maturation of the ova consisting of • Follicular Phase - (from the 1st day of menstruation to ... 12-14 days) LH & FSH cause graafian follicle to mature producing Estrogen • 2. Ovulatory Phase - (begins when estrogen levels peak until oocyte released from graafian follicle) = OVULATION ^LH • Luteal Phase - (begins after ovulation and lasts 14 days) ^ estrogen & progesterone • If pregnant, know that the corpus luteum secretes estrogen & progesterone until placenta matures and assumes this function • If pregnant, corpus luteum will continue to secrete estrogen & progesterone until placenta matures • If NOT pregnant, corpus luteum degenerates = < in progesterone and beginning of menstruation • ● Endometrial “Uterine” Cycle: changes in the endometrium of the uterus in response to the ovarian cycle • Proliferative Phase - (occurs following menstruation ending with ovulation) endometrium preparing for implantation =more THICK & VASCULAR • Secretory Phase - (after ovulation and ends with onset menstruation) = continues to THICKEN ^progesterone • Menstrual Phase - sloughing off of the endometrium = PERIOD . • Fertilization: “Conception” occurs when the sperm nucleus enters the nucleus of the oocyte within the outer third of the fallopian tube. • ● The fertilized egg is then called a ZYGOTE and contains a diploid number of chromosomes = 46 • Infertility: the inability to conceive or maintain a pregnancy after 12 months of unprotected sexual intercourse • ● 6 months for women older than 35 y.o • Causes • ● 1/3 Male Factor • ○ Endocrine - < in LH, FSH, Testosterone • ○ Spermatogenesis - effects of gonadotoxins • Gonadotoxins include: drugs, infections, systemic illness, heat exposure, pesticides and radiation to the pelvic region. • ○ Sperm Antibodies - < in sperm motility • ○ Sperm Transport - blocked transport • ■ Vasectomy • ■ Prostatectomy • ■ Inguinal hernia • ■ Absence of Vas Deferens • ○ Disorders of Intercourse • ■ Erectile Dysfunction • ● 1/3 Female Factor • ○ Ovulatory Dysfunction • ■ Anovulation • ■ Inconsistent Ovulation • ○ Tubal & Pelvic Pathology • ■ Damage to the Fallopian tubes • ● ENDOMETRIOSIS • ■ Uterine Fibroids: benign growth of uterine wall • ○ Cervical Mucus Factor • ■ Surgical surgeries: cryotherapy (TX cervical dysplasia) • ■ Infection not allowing sperm to enter • ● 1/3 Both Male and Female Factors • DX Testing: • ● Screening for STI’s and STD’s • ● Labs assessing levels of LH, FSH, TSH, testosterone • ● Semen Analysis • ● Assessment of Ovulatory Dysfunction • ○ Daily Morning Body Basal Temp • ○ Day 3 of menstrual cycle = FSH & estradiol test taken • ○ Detecting LH surge 36hrs before ovulation • ● Endometrial Biopsy at end of menstrual cycle • ● Hysterosalpingogram radiological exam testing tubal problems • ● Laparoscopy -visualize/inspect ovaries • ● • TX: • ● Females: • ○ Same lifestyle changes as men • ○ Surgery to open tubes if abnormal • ○ Myomectomy - removal of uterine fibroids • ○ Antibiotics to TX infection • ○ Medication stimulating egg production • ■ CLOMIPHENE CITRATE: stimulates release of FSH & LH • ● PO cycle Day 3-7 • S/E: hot flashes, breast discomfort, headaches, insomnia • Pregnant woman’s blood volume increases by: 40% to 45% • Blood volume expansion during pregnancy leads to Physiological anemia of pregnancy, also referred to as pseudo-anemia of pregnancy, is due to Hemodilution. The increase in plasma volume is relatively larger than the increase in RBCs that results in decreased hemoglobin and hematocrit values. • A 26-year-old woman at 29 weeks’ gestation experienced epigastric pain following the consumption of a large meal of fried fish and onion rings. The pain resolved a few hours later. The most likely diagnosis for this symptom is cholelithiasis • The clinic nurse reviews the complete blood count results for a 30-year-old woman who is now 33 weeks’ gestation. Tamara’s hemoglobin value is 11.2 g/dL, and her hematocrit is 38%. The clinic nurse interprets these findings as: Normal pregnancy values for the third trimester • Iron deficiency anemia: hemoglobin <11g/dL and hematocrit ,33% • Know the Integumentary changes: chloasma “melasma”, linea negra, striae gravidarum SATA • 15,000 RBC in pregnancy is a normal finding • Increase HR of 15-20 bpm is physiologically okay • Psychological: • Developmental Tasks • The events of pregnancy and childbirth are considered a developmental “maturational” crisis is the life of a family • ● All family members are affected • ■ Acquiring knowledge and plans for the specific needs of pregnancy, childbirth, and early parenthood • ■ Preparing to provide for the physical care of the newborn • ■ Adapting financial patterns to meet increasing needs • ■ Realignment of tasks and responsibilities • ■ Adjusting patterns of sexual expression to accommodate pregnancy • ■ Expanding communication to meet emotional needs • ■ Reorienting of relationships with relatives • ■ Adapting relationships with friends and community to take account of the realities of pregnancy and the anticipated newborn • Nursing Tasks • ■ Assess knowledge related to pregnancy, childbirth, and early parenting. • ■ Assess progress in developmental tasks of pregnancy. • ■ Explore patterns of communication related to emotional needs, responsibilities, and new roles. • ■ Include the entire family; assessments and interventions must be considered in a family-centered perspective. • ■ Provide education and guidance related to pregnancy, childbirth, and early parenting • Embryo and Fetal Development: first 8 wks= Organogenesis • ➢ Ectoderm • ➢ Mesoderm • ➢ Endoderm • After 9th wk = Fetus • ● Fetus Circulation: ^ levels of oxygenated blood enter the fetal circulatory system from the • Placenta -> Umbilical Vein • ● Ductus Venosus connects Umbilical Vein to Inferior Vena Cava • ● Foramen Ovale (opening between L & R atrium) • ○ after delivery shunt closes within 3 months from blood returning to the L atrium • ● Ductus Arteriosus (connects Pulm Artery to Descending Aorta) • ○ after delivery it constricts in response to ^ blood oxygen levels and prostaglandins • Placenta Development: formed from both fetal and mother tissue • ● Chorionic Membrane (trophoblast & chorionic villi) • ○ Form fetal blood vessels of the placenta • ● Endometrium (decidua) = 3 layers • ○ Decidua Basalis: forms maternal side of the placenta • Placenta is divided into lobes “cotyledons” • Placental membrane separates maternal/fetal blood from • mixing but allows for exchange of nutrients, gases and • electrolytes through diffusion and active transport • Major Hormones of the Placenta • ● Progesterone: < in uterine contractility & facilitates implantation • ● Estrogen: “enlargement” breasts and uterus • ● hCG: + preg test, ^ in 1st trimester as it stimulates corpus luteum to keep secreting estrogen and progesterone until placenta is able to secrete it (6-7wks) • ● hPL: promotes fetal growth by regulating glucose and stimulates breasts to lactate • Umbilical Cord = 1 vein (oxygenated blood) and 2 arteries (deoxygenated blood) A.V.A • Any drugs, viruses, infections or other exposures that can cause embryonic/fetal development abnormality • The developing human is most vulnerable to the effects of teratogens during the period of organogenesis, THE FIRST 8 WEEKS OF GESTATION • Common Discomforts of Pregnancy • ● N/V • ○ Eat crackers or dry toast 30min to 1 hr before rising in the morning to relieve discomfort • ○ Avoid having an empty stomach • ○ Avoid spicy, greasy, or gas-forming foods • ○ Drink fluids between meals • ● Breast Tenderness • ○ Wear a bra with adequate support • ● Urinary Frequency • ○ Empty bladder frequently • ○ Decrease fluid intake before bedtime and use perineal pads • ○ Perform Kegel exercises • ● UTI’s • ○ Wipe from front to back • ○ Avoid bubble baths • ○ Wear cotton underpants • ○ Avoid tight fitting pants • ○ Consume 8 glasses of water per day • ○ Urinate ASAP • ○ Notify HCP if urine is foul-smelling, contains blood or appears cloudy • ● Fatigue • ○ Engage in frequent rest periods • ● Heartburn • ○ Eat small frequent meals • ○ Do not allow stomach to get too empty/full • ○ Sit up for 30min after meals • ○ Check with HCP before using OTC antacids • ● Constipation • ○ Drink plenty of fluids • ○ Eat a diet High in FIBER • ○ Exercise Regularly • ● Hemorrhoids • ○ Take warm sitz bath • ○ Use witch hazel pads • ○ Apply topical ointments to relieve discomfort • ● Backaches • ○ Exercise regularly • ○ Perform pelvic tilt exercises • ■ Arching & straightening back • ○ Use proper body mechanics -use legs to lift • ○ Use side-lying position • ● SOB or Dyspnea • ○ Maintain good posture • ○ Sleep with extra pillows • ○ Contact HCP if symptoms worsen • ● Leg Cramps • ○ Extend the affected leg • ○ Keep knee straight • ○ Dorsiflex the foot (toes towards head) • ○ Apply heat while extended • ○ Contact HCP if persists • ● Varicose Veins & Lower Extremity Edema • ○ Rest with legs elevated • ○ Avoid tight/constricting clothing • ○ Wear support hose • ○ Avoid sitting & standing in one position for long periods of time • ○ Do not sit with legs crossed at the knees • ○ Sleep in the left-lateral position • ○ Exercise moderately with frequent walking to stimulate venous return • ● Gingivitis, Nasal Stuffiness, Epistaxis • ○ Gently brush teeth/Good dental hygiene • ○ Use a humidifier • ○ Use normal saline drops or Spray • ● Braxton Hicks contractions • ○ Instruct client to change position & walking should cause contractions to subside • ○ If contractions increase in intensity and become frequent with regularity - Notify HCP • ● Supine Hypotension • ○ Lie in a side-lying or semi-sitting position with her knees slightly flexed • Warning/Danger Signs • ● First Trimester • ○ Abd Cramping/Pain: poss threatened abortion, UTI, appendicitis • ○ Vaginal Spotting/Bleeding: “ “ • ○ Absent Fetal Heart Sound: poss missed abortion • ○ Dysuria, Freq, Urgency: poss UTI • ○ Fever/Chills: poss infection • ○ Prolonged N/V: hyperemesis gravidarum, ^ risk for dehydration • ● Second Trimester • ○ Abd/Pelvic Pain: poss appendicitis, UTI, PTL or pyelonephritis • ○ Vaginal Bleeding: poss infection, friable cervix from preg changes, placenta previa, abruption placenta or PTL • ○ Absent Fetal Heart Sound: poss missed abortion • ○ Dysuria, Freq, Urgency: poss UTI • ○ Fever/Chills: poss infection • ○ Prolonged N/V: hyperemesis gravidarum, ^ risk for dehydration • ● Third Trimester • ○ S/S of PTL (abruptio placenta: placenta detaches from womb) • ■ rhythmic lower abd cramping, lower backache, pelvic pressure, leaking of amniotic fluid, ^ vaginal dc • ○ S/S of HTN disorder • ■ severe headache (not relieved), visual changes, facial or generalized edema • ○ “ “Maternal Screening • ● Risk Factors • ○ Biophysical Factors: genetic, nutritional, medical or obstetric issues • ○ Psychosocial Factors: negative maternal behaviors affecting fetus • ■ Smoking • ■ Caffeine use • ■ Alcohol/drug use • ■ Psychological status • ○ Sociodemographic Factors • ■ Age, prenatal care, parity, marital status, income and ethnicity • ○ Environmental Factors: hazards in workplace or home • Parasympathetic Nervous System (rest and digest/ homeostasis) • ● Stimulation < HR • ● Mediated by the vagus nerve innervating sinoatrial (SA) & atrioventricular (AV) • ★ Vagus Nerve stimulations SLOWS FHR & helps maintain variability (variability develops 28-30wks) • Sympathetic Nervous System (fight or flight) • ● Stimulation ^ FHR • ● Responsible for FHR variability • ● Occurring through the release of norepinephrine • ● May be stimulated during Hypoxemia • Central Nervous System (CNS) (controls activities of the body) • ● Responsible for variations in FHR • ● Responsible for baseline variability RT fetal activity • ● Regulates & coordinates autonomic activities • ● Responds to fetal movement • ● Mediates cardiac & vasomotor reflexes • Chemoreceptors: located in the aortic arch & CNS • ● Respond to changes in fetal O2/CO2 & pH levels • ★ Decreased O2 & Increased CO2 cause the peripheral chemoreceptors to stimulate the Vagal Nerve & SLOW HR • ★ Central Chemoreceptors respond to Increased HR and Increased BP • Fetal Hypoxia causes release of • → epinephrine and norepinephrine increases FHR and BP • → vasopressin increases HR in response to hypoxia • Hypovolemia • → Renin-angiotensin (secreted by the kidneys) produces vasoconstriction • Fetal Reserves: the reserve of O2 available to the fetus to withstand the transient changes in blood flow and O2 during labor • ● When O2 is decreased, blood flow is deferred to fetal vital organs to compensate BUT when the placental reserves of O2 are decrease or depleting, the fetus may not be able to compensate or adapt to the decreased O2 during contractions • ● Homeostatic Mechanism • ★ 3 Types of Fetal Responses - FHR Data • NON Hypoxic Reflex • ○ FRH Accelerations • Compensatory to Hypoxemia • ○ Variable Decelerations • Impending Decompensation • ○ Late Decelerations • Clinical conditions that impact FHR include • ● Gestational age • ● Prior results of fetal assessment • ● Medications • ● Maternal medical conditions • ● Fetal conditions • Assessing FRH Pattern: • Baseline FHR (rate/variability) • ○ Mean FRH rounded to increments of 5 BPM during a 10 min window • ○ There MUST be 2 min of identifiable baseline segments • ○ NORMAL 110-160bpm • Periodic/Episodic Changes (accelerations/decelerations) • Uterine Activity • ○ Frequency • ○ Duration • ○ Intensity • ○ Resting tone • ○ Relaxation time between UC’s • ★ Baseline Variability: the fluctuations in the baseline of the FHR • ○ Irregular in amplitude & frequency • ○ Most Important predictor to adequate fetal oxygenation • cerebral cortex > midbrain (medulla oblongata) > vagus nerve > heart • ● accels/decels not included • ABSENT: amplitude range is undetectable • = Can occur if the baby is sleeping, meds S/E • Maternal: supine hypo, cord compression, uterine tachysystole, drugs • = May also be a sign of hypoxia/acidosis if persistent for 60min with interventions • MINIMAL: amplitude range is undetectable < 5 bpm • = Can occur if the baby is sleeping, meds S/E • Maternal: supine hypo, cord compression, uterine tachysystole, drugs • = May also be a sign of hypoxia/acidosis if persistent for 60min with interventions • - • MODERATE: amplitude 6 -25 bpm • = Well oxygenated fetus with normal acid-base balance • Know this is NORMAL -keep monitoring • MARKED: amplitude range > 25 bpm • ★ Fetal Bradycardia: FHR <110 bpm for at least 10 min • ○ <FRH may lead to <CO = < umbilical cord blood flow leading to fetal hypoxia (needs immediate intervention) • ○ < 80 bpm = obstetric emergency • ○ Brady with normal variability is Benign • ○ Brady with loss of variability/late decelerations is a sign of current/impending fetal hypoxia • ○ Causes: • ■ Maternal related • ● Supine position • ● Hypotension • ● Dehydration • ● Meds: (ANAESTHETICS/ADRENERGIC RECEPTORS) • ● Rupture of the uterus/vasa previa or placental abruption • ■ Fetal related • ● Fetal response to hypoxia • ● Cord occlusion • ● Acute/late/profound hypoxemia • ● Hypothermia • ● Hypokalemia • ● Chorionic head compression • ● Fetal bradyarrhythmia • ○ TX: treat underlying cause/consider delivery • ○ Nursing Actions: • ■ Confirm EFM • ■ Assess fetal movement • ■ Fetal scalp stimulation • ■ Perform vaginal exam -assess for prolapsed cord • ■ Maternal VS • ■ Have mother change in position • ■ Discontinue oxytocin to < UC’s • ■ Give O2 10L/min via non-breather mask • ■ Stop < pushing • ■ support family • ■ contact HCP • ★ Fetal Tachycardia: FHR >160 bpm for at least 10 min • ○ May be a sign of fetal hypoxemia, especially with decreased variability and decelerations • ○ If tachy = 200-220 bpm, fetal demise • ○ Causes: • ■ Maternal fever/related causes • ● Infection • ■ Exposure to meds (Terbutaline) • ○ TX: treat underlying cause & consider delivery • ○ Nursing Actions: • ■ Assess maternal VS • ■ Give meds as ordered • ■ Use ice packs, if fever • ■ Assess for dehydration - IV fluids • ■ Change the mother’s position • ■ Decrease/Stop Pitocin (Oxytocin) • ■ Notify HCP • ★ Periodic v. Episodic Changes • ○ Periodic = accelerations/decelerations in FHR due to UC & persist • ○ Episodic = accelerations/decelerations in FRH not associated with UC (accelerations common) • ★ FHR Accelerations = predictive of adequate central fetal oxygenation and absence of fetal acidemia • ○ Visually abrupt transient increases above the FHR baseline • ○ 15 beats above the baseline (15 sec-2 min) • ○ Prolonged accelerations >2 min but < 10 min • ★ FHR Decelerations = transitory decreases in the FHR baseline • ○ Classified according to shape, timing & duration in relationship with the contraction • ○ RECURRENT if occur in at least 50% of UC’s within 20 min • ○ INTERMITTENT if occur fewer that 50% of UC’s within 20 min • ○ Nadir: lowest point of the deceleration (occurs at the peak of the contraction) • EARLY Decelerations: visibly apparent & symmetrical • ● Mirrors the UC’s • ● Normal • VARIABLE Decelerations: visibly apparent, abrupt decrease in FHR • ● Most common during labor • ● Decrease FHR is > 15 bpm for > 15 sec and <2min in duration • ● Can be a V, W or U shaped • ● May be due to umbilical cord occlusion/ cord compression • REPOSITION THE PATIENT • Consider Amnioinfusion, tocolytics, delivery • LATE Decelerations: visibly apparent, symmetrical gradual decrease of FHR due to UC’s • ● May be a sign of fetal intolerance to labor • ● Nadir occurs after peak of contraction • ● RT decreased availability of O2 because of uteroplacental insufficiency • ● Consider tocolytics, delivery • Interventions: Initiate Iv bolus, change maternal position, initiate oxygen therapy • PROLONGED Decelerations: • ● More than 15 bpm lasting >2 min but < 10 min • ● Caused by any mechanism that causes drastic < in O2 • ● Consider Amnioinfusion, tocolytics, delivery • The goal for maternal position change for prolonged deceleration is maximizing uterine blood flow. • These interventions maximize uterine blood flow, umbilical circulation and maternal fetal oxygenation by • ● Shifting maternal position to the L or R • ● Administer 500 mL of lactic ringers IV Bolus -maximize intravascular volume =improved uteroplacental perfusion • ● Correct hypotension by change in position, Ephedrine and proper hydration • ● Adm O2 10L/min on non-rebreather face mask • ● Reduce UC’s by • ○ Stopping Oxytocin • ○ Removing the cervical ripening agent • ○ Use Terbutaline to Relax the uterus • ○ Amnioinfusion - resolving variable decelerations • ○ Encourage pushing techniques • ○ Obtain fetal acid-base status if possible by fetus scalp sample • ○ Be supportive to mother & fam bam • ● If fetus has fetal acidemia = • ○ Notify HCP to initiate bedside eval for cesarean • ○ Notify anesthesia & peds team • ○ Move pt to OR • Amnioinfusion: room temp normal saline is infused into the uterus transcervically via an intrauterine pressure catheter to increase intra amniotic fluid cushioning the umbilical cord and reducing cord compression. • Used when there are Variable Decelerations in the first stage of labor due to a decrease in amniotic fluid • Also know the functions of the amniotic fluid: provides cushion for the fetus and prevents the fetus from getting contractures when bending arms and legs > mother is able to exercise, encouraged to walk daily • ● Ultrasonography: high frequency sound waves producing an image or an organ or tissue • ○ Gestational Age • ○ Fetal Growth • ○ Fetal Anatomy • ○ Placental Abnormalities & location • ○ Fetal Activity • ○ Amount of Amniotic Fluid • ○ Visual Assistance for invasive procedures ->amniocentesis • Standard Ultrasounds are typically done in 1st trimester to confirm preggo & calculate gestational age • ● Transvaginal Ultrasound - done at 1st trimester • ● Abdominal Ultrasound - supine position • ★ To calculate gestational age = measurements of • ○ Fetal-crown rump length • ○ Biparietal Diameter • ○ Femur Length • ○ Most accurate <20 wks • Chorionic Villus Sampling (CVS): the aspiration of a small amount of placental tissue for chromosomal, DNA and metabolic testing • ● Done within 10-12 weeks for chromosomal analysis to detect fetal abnormalities caused by genetic disorders • ● It tests for Cystic Fibrosis but NOT for Neural Tube Defects • ● Performed ideally at 10-13 wks - NOT recommended before 10 weeks • ● Procedure • ○ Supine/Lithotomy position • ○ A catheter/needle is inserted transvaginally with ultrasound guiding it (teaching) • ○ Sample of chorionic “placental” tissue is removed • ● Risks • ○ 10% of women experience bleeding • ○ 7% fetal loss rate due to bleeding or infection • ● Nursing Actions • ○ Review procedure with mother & fam • ○ Instruct breathing exercises • ○ Assist into position • ○ Label specimens • ○ Auscultate FHR after procedure twice in 30 min • ○ Assess mother’s well being • ○ Instruct mother to notify HCP if there is any abd cramping, fever, chills, bleeding • ○ Adm RhoGam to RH-negative women post procedure as indicated • Amniocentesis: a diagnostic procedure in which a needle is inserted through the maternal abdomen wall into the uterine cavity to obtain amniotic fluid Not part of a normal prenatal visit • ● Genetic testing (mother older than 35) • ● Hemolytic disease • ● Fetal lung maturity testing: • ○ Lecithin/sphingomyelin (L/S) ratio • ■ L:S ratio >2:1 indicates fetal lung maturity • ■ L:S ratio <2:1 indicates fetal lung immaturity in increased risk of respiratory distress syndrome. • ○ Phosphatidyl glycerol (PG) • ■ + PG indicates fetal lung maturity. • ■ - PG indicates immature fetal lungs. • ○ Lamellar body count (LBC) • ■ LBC of ≥50,000/μL is highly indicative of fetal lung maturity. • ■ LBC of ≤15,000/μL highly indicative of fetal lung immaturity. • ■ LBC results can be hindered by the presence of meconium, vaginal bleeding, vaginal mucous, or hydramnios. • ● Hemolytic disease in the fetus • ● Intrauterine infection • ● Performed at 14-20 weeks (Hartman said 16-20wks) • ● Results are in 2 weeks • ● Risks • ○ Trauma to the fetus/placenta • ○ RH sensitization from fetal blood in mother’s circulation • ○ Bleeding • ○ Preterm labor • ○ Infection • ● Nursing Actions • ○ Review the procedure with the mother • ○ If < 20 wks, a full bladder may be required for full visualization • ○ Breathing & Relaxation techniques • ○ Explain a local anaesthetic will be used • ○ Prep abd with antiseptic (Betadine) • ○ Label specimens • ○ Instruct woman not to lift anything heavy for 2 days • ○ Auscultate FHR after procedure twice in 30 min • ○ Assess mother’s well being • ○ Instruct mother to notify HCP if there is any abd cramping, fever, chills, bleeding • ○ Adm RhoGam to RH-negative women post procedure as indicated • Ultrasonography to guide placement • LESS THAN 1%FETAL LOSS RATE AFTER 15 WEEKS GESTATION! • Alpha-fetoprotein (AFP): a glycoprotein produced in the fetal liver, gastrointestinal tract, and yolk sac in early gestation. • ● Used to screen for NTD (spinal defects) & Ventral Abd Wall defects • ● 95% of NTD are occur in the absence of risk factors, it is done routinely • ● Procedure: blood sample is taken and sent to the lab • ○ < Levels may be Chromosome 21 defect (Trisomy 21/ Down Syndrome) (follow up with amniocentesis then administer RhoGAM if indicated by physician • ○ > Levels may be NTD, anencephaly, omphalocele, and gastroschisis (follow up with ultrasound) • ○ Further tests are done • ● Risks for high false-positives & negatives may also occur causing stress to the mother & family • ● Nursing Actions • ○ Educate mother about the screening • ○ Support mother & assist in scheduling • ○ Provide support group information • Multiple Marker Screen • ● Triple Marker Screening: combines all three chemical markers • AFP • Human chorionic gonadotropin (hCG) • Estriol levels • —With maternal age to detect some trisomies and NTDs. • ○ Used as an alternative to amniocentesis • ● Quad screen: adds inhibin-A to the triple marker screen to increase detection of trisomy 21 to 80% • ○ Done at 15-16 weeks • ○ Maternal blood is drawn & sent to lab • ■ Low levels of maternal serum alpha-fetoprotein (MSAFP) and unconjugated estriol levels suggest an abnormality. • ■ hCG and inhibin-A levels are twice as high in pregnancies with trisomy 21. • ■ Decreased estriol levels are an indicator of NTDs. • ○ No risks • ○ Nursing Actions “ ” • Daily fetal movement count (kick counts): • Surveillance after 28 wks (may feel them at 16-20 wks) • ➔ Palpate abd & track fetal movements daily for 1–2 hours • ◆ 10 kicks in 2 hrs = normal • ◆ 4 kicks in 1 hr = normal • ◆ < 4 kicks in 2 hrs should be reported • ◆ Teach mom to drink juice or eat something if baby is not moving, they may be asleep • Non-stress test (NST): screening tool that uses electronic fetal monitoring (EFM) to assess fetal condition or well- being • Know how the procedure is done • ➔ Healthy baby’s FHR accelerates with movement • ◆ FHR monitored with the external FHR transducer until reactive (up to 40 minutes), while running a FHR contraction strip for interpretation. • ◆ Monitor FHR and fetal activity for 20–30 minutes • ! The NST is considered reactive when the FHR increases • 15 beats above baseline for 15 seconds twice or more in • 20 minutes. • ! In fetuses less than 32 weeks’ gestation two accelerations • peaking at least 10 bpm above baseline and • lasting 10 seconds in a 20-minute period is reactive • ! Nonreactive NST is one without sufficient FHR accelerations • in 40 minutes and should be followed up with further testing such as BPP • Vibroacoustic stimulation (VAS): uses auditory stimulation (using an artificial larynx) to assess fetal well-being with EFM when NST is nonreactive. • ➔ VAS is only used when the baseline rate is determined to be within normal limits. • ➔ When deceleration or bradycardia is present, VAS is not an appropriate intervention • ➔ Procedure • ◆ Activating an artificial larynx on the maternal abdomen near the fetal head for 1 second in conjunction with the NST • ➔ Reactive when the FHR increases 15 beats above baseline for 15 seconds twice in 20 minutes. • Contraction stress test (CST): assess fetal well-being and uteroplacental function with EFM in women with nonreactive NST at term gestation. • ➔ Identifies a fetus that is at risk for compromise through observation of the fetal response to intermittent reduction in uteroplacental blood flow with stimulated uterine contractions • ➔ Monitor FHR and fetal activity for 20 minutes. • ➔ If no spontaneous UCs, contractions can be initiated in some women by having them brush the nipples for 10 minutes. • ➔ If nipple stimulation is unsuccessful, UCs can be stimulated with oxytocin via IV until 3 UCs in 10–20 minutes lasting 40 seconds occur • ◆ - or normal = no significant variable decelerations or no late decelerations in a 10-minute strip with 3 UCs > 40 seconds assessed with moderate variability. • ◆ + = late decelerations of FHR with 50% of UCs usually assessed with minimal or absent variability. • ◆ + result has been associated with an increased rate of fetal death, fetal growth restriction, lower 5-minute Apgar scores, cesarean section, and the need for neonatal resuscitation due to neonatal depression. > requires further testing such as BPP. • ◆ CST is equivocal or suspicious when there are intermittent late or variable decelerations, and further testing may be done or the test repeated in 24 hours. • ➔ Nursing Actions • ◆ Explain the procedure to the woman and her family. The CST stimulates contractions to evaluate fetal reaction to the stress of contractions • ◆ Have patient void before testing. • ◆ Position patient in a semi-Fowler’s position • ◆ Monitor vitals before and every 15 minutes during the test. I Provide comfort measures. • ◆ Provide emotional support. • ◆ Correctly interpret FHR and contractions. • ◆ Safely administer oxytocin • ● avoid uterine tachysystole: more than five uterine contractions in 10 minutes, fewer than 60 seconds between contractions, or a contraction greater than 90 seconds with a late deceleration occurring • ◆ Recognize adverse effects of oxytocin. • ◆ Schedule appropriate follow-up. • ◆ Risks are false positive with no needed interventions • Amniotic fluid index (AFI): measures the volume of amniotic fluid with ultrasound to assess fetal well-being and placental function. • ● Ultrasound measurement of pockets of amniotic fluid in four quadrants of the uterine cavity via ultrasound • ● Amniotic fluid level is based on fetal urine production, which is the predominate source of amniotic fluid and is directly dependent on renal perfusion • ● Average is 8-24 cm • ○ AFI ≤ 5 cm is indicative of oligohydramnios. Oligohydramnios is associated with increased prenatal mortality and a need for close maternal and fetal monitoring. • ○ An AFI above 24 cm is polyhydramnios, which may indicate fetal malformation such as NTDs, obstruction of fetal gastrointestinal tract, or fetal hydrops. • <uteroplacental perfusion→< fetal renal blood flow →<urine production → oligohydramnios • Nursing Actions: • ● Explain the procedure to the woman and her family. This test measures the amount of amniotic fluid with ultrasound to assess fetal well-being and how well the placenta is working. • ● Provide comfort measures. • ● Provide emotional support. • ● Schedule appropriate follow-up. • ● Special training in obstetric ultrasound is required for evaluation of amniotic fluid volume • Biophysical profile (BPP): ultrasound assessment of fetal status along with an NST. • ➔ Assessment of fetal breathing movement, gross body movement, fetal tone, amniotic fluid volume, and heart rate reactivity. • ➔ Indicated in pregnancies involving increased risk of fetal hypoxia and placental insufficiency such as maternal diabetes and hypertension. • ➔ An NST with the addition of 30 minutes of ultrasound observation for four indicators: fetal breathing movements, fetal movement, fetal tone, and measurement of amniotic fluid. • ◆ Assess fetal breathing movements: One or more episodes of rhythmic breathing movements of 30 seconds or movement within 30 minutes is expected. • ◆ Assess fetal movement: Three or more discrete body or limb movements in 30 minutes are expected. • ◆ Assess fetal tone: One or more fetal extremity extension with return to fetal flexion or opening and closing of the hand is expected. • ◆ Assess amniotic fluid volume: A pocket of amniotic fluid that measures at least 2 cm in two planes perpendicular to each other is expected. • ➔ A score of 2 (present) or 0 (absent) is assigned to each of the five components. • ➔ A total score of 8/10 is reassuring. • ➔ A score of 6/10 is equivocal and may indicate the need for delivery depending on gestational age. • ➔ A score of 4/10 means delivery is recommended because of a strong correlation with chronic asphyxia • ➔ A score of 2/10 or less prompts immediate delivery. • ➔ Fetal activity decreases or stops to reduce energy and oxygen consumption as fetal hypoxemia worsens. Decreased activity occurs in reverse order of normal development. • 26. Factors affecting labor (5 Ps) pg. 186 • Powers • Passage • Passenger • Psyche • 5. Position Intrapartum Period = with onset of reg uterine contractions lasting until placental expulsion • Labor is triggered by Both Maternal & Fetal factors • Powers “Contractions” - involuntary uterine contractions (UC) of labor and voluntary pushing or bearing down process • ● Frequency (mins): time from beginning of one contraction to the beginning of another • ● Duration (sec): time from beginning of one contraction to the end. • ● Intensity: strength (mild, moderate, or strong) • ● Bearing-down: occurs once the cervix is fully dilated (10 cm) and the woman feels the urge to push • Passage “Pelvis & Birth Canal”- the bony pelvis and the soft tissues of the cervix, pelvic floor, vagina, and introitus (external opening to the vagina) • ● Station: refers to the relationship of the ischial spines to the presenting part of the fetus and assists in assessing for fetal descent during labor • ● Soft tissue- effaces and dilates, allowing the descending fetus into the vagina • Passenger “Fetus” - fetal skull, fetal attitude, fetal life, fetal presentation, fetal size • ● Fetal skull- molding (the ability of the fetal head to change shape to accommodate/fit through the maternal pelvis) • ○ two parietal bones, two temporal bones, the frontal bone and occipital bone • ● fetal attitude or posture- proper attitude → head is in complete flexion in a vertex presentation • ● fetal presentation: cephalic (head first), breech (pelvis first), and shoulder (shoulder first) • Psyche “Woman’s Response” factors that influence the woman’s coping mechanism include: • ● culture- important to have a general understanding of birth practices of the groups with which they work • ● expectations- how childbirth is viewed by the woman/past experiences • ● support system- gives the mother a good sense of control • ● labor support- helps with anxiety and fear • Position • ● first stage of labor- an upright position • ● second stage- fetus aligns with pelvic inlet • ● births- lithotomy position • 27. Onset of labor True vs False labor pg. 195 True Labor Contractions occur at REGULAR intervals and Increase in Frequency, Duration and Intensity • ● TRUE Labor: contractions bring about changes in cervical effacement and dilation • ● FALSE Labor: irregular contractions with little or No cervical changes • 28. Stages of Labor & Childbirth pg. 198 • While performing Leopold’s maneuvers on a woman in early labor, the nurse palpates a flat area in the fundal region, a hard round mass on the left side, a soft round mass on the right side, and small parts just above the symphysis. The nurse concludes which of the following? The fetal presentation is scapular – shoulder • Labor or “Parturition” is the process in which the fetus, placenta, and membranes are expelled through the uterus • ● First Stage: Onset of Labor -> Complete Cervical Dilation • ○ Latent Phase (0-3 cm) • Woman feels a surge of energy • ○ Active Phase (4-7 cm) • ○ Transition Phase (8-10 cm) • Woman feels irritable, tells people to get out of the room • ● Second Stage: 10 cm -> Birth • ● Third Stage: Delivery of the Placenta • ● Fourth Stage: Postpartum • 29. Episiotomy & Lacerations pg. 212 • Episiotomy: an incision in the perineum to provide more space for the presenting part at delivery • no longer typical • ➢ Median/Midline = at the midline • ○ Heals More Quickly with less discomfort • ➢ Mediolateral = cut at a 45 degree angle to the L or R and may by used for a large infant. • ○ Heals Slowly • ○ Causes greater blood loss • ○ More painful • Lacerations: tears in the perineum that may occur at delivery • They may occur in the • ➢ Cervix • ➢ Vagina • ➢ and/or Perineum • Degrees • ● 1st Degree - perineal skin & vaginal mucous membrane • ● 2nd Degree - skin, mucous membrane & fascia of the perineal body • ● 3rd Degree - skin, mucous membrane & fascia of the perineal body & extends to the rectal sphincter • ● 4th Degree - extends into the rectal mucosa and exposes the lumen of the rectum • 30. Newborn transition & Apgar scoring pg. 216 • Newborn transition & initial care occur in labor & delivery room. • APGAR Scores should be obtained at 1 Minute and 5 Minutes after Birth. • APGAR Score is a rapid assessment of 5 physiological signs that indicate the physiological status of the newborn including • ➔ Activity (Muscle Tone) • ◆ Muscle Tone on degree of flexion & movement of extremities • ➔ Pulse • ◆ HR based on auscultation • ➔ Grimace • ◆ Reflex Irritability on response to tactile stimulation • ➔ Appearance • ◆ Color on observation • ➔ Respirations • ◆ RR based on observed movement of the chest • ❖ SEVERE Distress = 0-3 • ❖ MODERATE Difficulty with transition to extrauterine life = 4-6 • ❖ STABLE Status = 7-10 • Apgar Score is not used to determine need of resuscitation but it’s a rapid, objective, convenient shorthand for reporting the status of the newborn and the response of resuscitation after birth • 31. Management of discomforts labor pg. 218 • Gate Control Theory: • Labor pain is Acute & is transmitted from the periphery of the body along nerve pathways to the brain. • ➢ Uterine contractions from < in O2 supply to the uterus • ➢ ^ pressure & stretching of pelvic structures • ➢ Cervical Dilation/Stretching -> stimulation of the nerve ganglia • 1st Stage of Labor - Pain is caused by • ● Uterine muscle hypoxia • ● Accumulation of lactic acid in the muscles • ● Lower uterine and cervical stretching • ● Traction on pelvic organs • ● Pressure on the bony pelvis • 2nd Stage of Labor - Pain is due to • ● Pelvic muscle distension • ● Pressure on the perineum, cervix, urethra and rectum • Back pain is thought to be caused by pressure of the fetal occiput on the maternal spine & pelvis • Pain is influenced by both physical & psychosocial factors • 32. Pharmacologic & Nonpharmacologic pain relief pg. 219 • Non-pharmacological Management of Labor discomfort includes: • ● Preparation by the woman for childbirth • ○ Childbirth preparation classes • ○ Relaxation & Breathing Techniques: Deep breath at beginning of contraction -> breath slowly through contraction • ● Cutaneous Stimulation • ○ Effleurage: lightly stroking the abd in rhythm with breathing during contractions • ○ Back massage “Counter Pressure” to sacral area of mother • ● Thermal Stimulation • ○ Application of Warm/Cold: < catecholamine production which interferes with uterine contractility & Cold may < sensation of pain • ● Mental Stimulation • ○ Focal points, Imagery, Music - focusing mother’s attention away from the pain • ● Presence of support person • ○ Provide emotional support, comfort • ○ Doulas • Pharmacological Management of Labor Discomfort • Requires nurse to assess the woman’s preference for pain management throughout labor • ➔ A Pain Assessment needs to be completed • ★ 2 Med Categories • ○ Analgesics: labor should be established • ■ Meperidine (Demerol) : opioid • ■ Butorphanol (Stadol): opioid agonist-antagonist • ■ Sublimaze (Fentanyl): short acting opioid antagonist • ○ Anesthesia: • ■ Local: analgesic injected into perineum at episiotomy site • ■ Regional: • ● Pudendal Block • ● Epidural Block • COMPLICATIONS W/ EPIDURAL: DECREASE BP & HYPOTENSION • ● Spinal Block • ○ General Anesthesia: used in emergency c-section • Rubella titer is negative: must give immunization after delivery • NAEGELES RULE • GRAAFIAN FOLLICLE: LH & FSH HORMONES • CORPUS LUTEUM: PROGESTERONE AND ESTROGEN • GTPAL • Infertility: combination of women and male factors ( man blames his wife that she is the cause of them not being able to conceive. The nurse intervenes and tells them that it can be cause by both male and female causative factors. 1/3 • True/ false labor • Woman calls the hospital and says that she has been laying down watching TV and she has sudden dizziness : nurse ask if she has been laying on her back for a long time ( woman is 28weeks pregnant) • Woman has been in labor for 12 hours: her baseline is 140 150 and rises to 170-> causes fetal stress • Ambivalence is normal • Amniotic fluid -> cushions the baby • First 8 weeks if pregnancy is most crucial • Woman feels the baby moving -> this is a Presumptive sign (Quickening) • Stage 2 labor • What is the most important thing about FHR monitoring? • Non stress test: do not give oxytocin to stimulate contractions • A woman you are caring for in labor requests an epidural for pain relief in labor. Included in your preparation for epidural placement is a baseline set of vital signs. The most common vital sign to change after epidural placement: • Blood pressure, hypotension • Blood pressure, hypertension • Pulse, tachycardia • Pulse, bradycardia • 14. During preconception counseling, the clinic nurse explains that the time period when the fetus is most vulnerable to the effects of teratogens occurs from: • 2 to 8 weeks • 4 to12 weeks • 5 to 10 weeks • 6 to 15 weeks • 13. Information provided by the nurse that addresses the function of the amniotic fluid is that the amniotic fluid helps the fetus to maintain a normal body temperature and also: • Facilitates asymmetrical growth of the fetal limbs • Cushions the fetus from mechanical injury • Promotes development of muscle tone • Promotes adherence of fetal lung tissue • During a routine prenatal visit in the third trimester, a woman reports she is dizzy and lightheaded when she is lying on her back. The most appropriate nursing action would be to: • Order an EKG. • Report this abnormal finding immediately to her care provider. • Teach the woman to avoid lying on her back and to rise slowly because of supine hypotension. • Order a nonstress test to assess fetal well-being. • 2 questions on GTPAL (complicated like 2 sets of twin, 2 abortions, 2 miscarriage, 1 stillborn-which is considered preterm labor) • 2 questions on apgar (fill in the blank, give score based on the given data on the baby) • Present trends- select all • Food high in folic acid-select all; strawberry, green leafy, lentils, milk, or beans • Menstrual cycle-when is the best time to have sex? • Which one is NOT! correct about implantation? That it occurs 2-3 weeks after conception • BMI is 26.5, how much weight can the women gain? 15-25 • Nursing intervention on a variable deceleration? I think reposition the women • Substance abuse-select all-> abortion, low birth weight • Smoking- what is wrong- “I can smoke during pregnancy because I will have an easier delivery with a smaller baby • Teratogens-correct statement- first 8 weeks • August 1st is the LMP- what is the EDD? • Progesterone questions- increases vascularity of uterus • Expected cardiovascular change? I put increased heart rate by 15-20bpm • What do you check after 1 hours of epidural? Hypotension or headache? • Nursing teaching about amnionic villi sampling? Catheter is inserted • What is not part of the routine exam? Amniocentesis • Nausea and vomiting in the morning- select all- small meals, dry crackers • Normal skin changes-select all- chloasma, strae gravidarum, lenia nigra • When do you listen for the baby’s heart rate when based on the leopold maneuver you feel something round and firm in the fundus and something long and smooth on the right side? I put right upper quadrant • Women is having long labor with sever back pain, why? I don’t know the answer… options were Longitudinal fetal lie, womens pelvic structure and 2 more • What needs to be reported to HCP? Late deceleration • FHR has decelerations with each contractions and goes back to normal before contraction ends- what do you do? I put document and keep monitoring • Women’s membrane has ruptured-what is she at risk at? I put Intrauterine infection • Function of amniotic fluid- I put provides nutrition (cushions and temperate was already in the questions) • True labor- contractions are getting closer and stringer • 2-3 questions on genetics like the mom and dad are careers, what do you teach the patient • The women’s blood test shows negative rubella titer-what does this mean? I put it means that the mom is not immune and needs to get a vaccine after delivery • Questions on RhoGAM. Who do you give it to and why-options were weird [Show More]
Last updated: 1 year ago
Preview 1 out of 33 pages
Instant download
Buy this document to get the full access instantly
Instant Download Access after purchase
Add to cartInstant download
Reviews( 0 )
Document information
Connected school, study & course
About the document
Uploaded On
Apr 07, 2020
Number of pages
33
Written in
Additional information
This document has been written for:
Uploaded
Apr 07, 2020
Downloads
0
Views
39





 Correct Study Guide, Download to Score A.png)