NCLEX-RN Practice Quiz Test Bank #11 (75 Questions)
Document Content and Description Below
NCLEX-RN Practice Quiz Test Bank #11 (75 Questions) 1. 1. Question A patient is admitted to the hospital with a diagnosis of primary hyperparathyroidism. A nurse checking the patient’s lab results w... ould expect which of the following changes in laboratory findings? o A. Elevated serum calcium o B. Low serum parathyroid hormone (PTH) o C. Elevated serum vitamin D o D. Low urine calcium Incorrect Correct Answer: A. Elevated serum calcium The parathyroid glands regulate the calcium level in the blood. In hyperparathyroidism, the serum calcium level will be elevated. A normal PTH in the presence of hypercalcemia is considered inappropriate and still consistent with PTH-dependent hypercalcemia. PTH levels should be very low in those patients with PTH-independent hypercalcemia. A comprehensive clinical evaluation complemented by routine laboratory and radiologic studies should be sufficient to establish a diagnosis of primary hyperparathyroidism in a patient with persistent hypercalcemia and an elevated serum level of parathyroid hormone. • Option B: Parathyroid hormone levels may be high or normal but not low. Patients with primary hyperparathyroidism and other causes of PTH-dependent hypercalcemia often have frankly elevated levels of PTH, while some will have values that fall within the reference range for the general population. It is uncommon for clinically occult malignancies to cause hypercalcemia. Most patients with malignancy-associated hypercalcemia are known to have cancer, or cancer is readily detectable on initial evaluation, and PTH levels will be suppressed. • Option C: Parathyroid hormone levels may be high or normal but not low. The body will lower the level of vitamin D in an attempt to lower calcium. • Option D: Urine calcium may be elevated, with calcium spilling over from elevated serum levels. This may cause renal stones. A review of previous medical records can often be of significant value in establishing the cause of hypercalcemia. Most patients with hyperparathyroidism have persistent or intermittent hypercalcemia for many years before a definitive diagnosis is established. 2. 2. Question A patient with Addison’s disease asks a nurse for nutrition and diet advice. Which of the following diet modifications is not recommended? • A. A diet high in grains. • B. A diet with adequate caloric intake. • C. A high protein diet. • D. A restricted sodium diet. Incorrect Correct Answer: D. A restricted sodium diet. A patient with Addison’s disease requires normal dietary sodium to prevent excess fluid loss. Do not reduce salt in the diet. The client may need to add extra salt to his food during hot and humid weather or after exercise to replace salt lost through sweating. Do not use salt substitutes. • Option A: Addison’s disease is a rare condition. It develops when the adrenal glands, which are located above the kidneys, do not make enough of certain hormones. These hormones are important for normal body function. They help the body cope with stress, hold salt and water, and maintain blood pressure. The client should include complex carbohydrates in his diet, including grains. • Option B: A high protein diet is recommended for the client with Addison’s disease. The adrenal fatigue diet aims to stabilize blood sugar and balance cortisol levels by limiting sugar while increasing the intake of protein, healthy fats, veggies, and whole grains. Healthy fats and high-quality proteins slow the blood sugar rollercoaster and promote stable blood sugar levels throughout the day. • Option C: Adequate caloric intake is recommended. Refined carbohydrates quickly break down into sugar after you ingest them, which causes a spike in blood sugar followed by a steep decline. The diet discourages foods that are inflammatory or hard to digest and may contribute to gut health issues. The adrenal fatigue diet is more about eating more foods that make the client feel good and nourish the body versus restricting. 3. 3. Question A patient with a history of diabetes mellitus is in the second postoperative day following cholecystectomy. She has complained of nausea and isn’t able to eat solid foods. The nurse enters the room to find the patient confused and shaky. Which of the following is the most likely explanation for the patient’s symptoms? • A. Anesthesia reaction • B. Hyperglycemia • C. Hypoglycemia • D. Diabetic ketoacidosis Incorrect Correct Answer: C. Hypoglycemia A postoperative diabetic patient who is unable to eat is likely to be suffering from hypoglycemia. The actual treatment recommendations for a given patient should be individualized, based on diabetes classification, usual diabetes regimen, state of glycemic control, nature and extent of surgical procedure, and available expertise. • Option A: An anesthesia reaction would not occur on the second postoperative day. Anesthesia and surgery cause a stereotypical metabolic stress response that could overwhelm homeostatic mechanisms in patients with pre-existing abnormalities of glucose metabolism. The invariant features of the metabolic stress response include release of the catabolic hormones epinephrine, norepinephrine, cortisol, glucagons, and growth hormone and inhibition of insulin secretion and action. • Option B: Confusion is a late sign of hyperglycemia. Shakiness is not one of its symptoms. The management approach in these categories of patients always includes insulin therapy in combination with dextrose and potassium infusion. Major surgery is defined as one requiring general anesthesia of ?1 h. At a minimum, blood glucose should be monitored before and immediately after surgery in all patients. Those undergoing extensive procedures should have hourly glucose monitoring during and immediately following surgery. • Option D: Symptoms of DKA include excessive thirst, frequent urination, abdominal pain, fruity-scented breath, confusion, and shortness of breath. However, shakiness is not a sign of DKA. The stress of surgery itself results in metabolic perturbations that alter glucose homeostasis, and persistent hyperglycemia is a risk factor for endothelial dysfunction, postoperative sepsis, impaired wound healing, and cerebral ischemia. The stress response itself may precipitate diabetic crises (diabetic ketoacidosis [DKA]. 4. 4. Question A nurse assigned to the emergency department evaluates a patient who underwent fiberoptic colonoscopy 18 hours previously. The patient reports increasing abdominal pain, fever, and chills. Which of the following conditions poses the most immediate concern? • A. Bowel perforation • B. Viral gastroenteritis • C. Colon cancer • D. Diverticulitis Incorrect Correct Answer: A. Bowel perforation Bowel perforation is the most serious complication of fiberoptic colonoscopy. Important signs include progressive abdominal pain, fever, chills, and tachycardia, which indicate advancing peritonitis. Bowel perforation results from insult or injury to the mucosa of the bowel wall resulting from a violation of the closed system. This exposes the structures within the peritoneal cavity to gastrointestinal contents. Patients presenting with abdominal pain and distension, especially in the appropriate historical setting, must be evaluated for this entity as delayed diagnosis can be life-threatening due to the risk of developing infections such as peritonitis. • Option B: Several different viruses including rotavirus, norovirus, adenovirus, and astroviruses account for most cases of acute viral gastroenteritis. Most are transmitted via the fecal-oral route, including contaminated food and water. Transmission has also been shown to occur via fomites, vomitus, and possibly airborne methods. Norovirus is more resistant to chlorine and ethanol inactivation than other viruses. Acute gastroenteritis is defined by loose or watery diarrhea that consists of 3 or more bowel movements in a day. Other symptoms may include nausea, vomiting, fever, or abdominal pain • Option C: Colon cancer does not cause these symptoms. Tumor location on clinical presentation can be separated on left-sided with more changes in bowel habits and hematochezia, and right-sided with obscured anemia impacting on late stage at diagnosis. The provider should perform a thorough physical examination for signs of ascites, hepatomegaly, and lymphadenopathy. • Option D: Diverticulitis may cause pain, fever, and chills, but is far less serious than perforation and peritonitis. Acute diverticulitis is inflammation due to micro-perforation of a diverticulum. The diverticulum is a sac-like protrusion of the colon wall. Diverticulitis can present in about 10% to 25% of patients with diverticulosis. Diet appears to play a significant role. Low fiber, high fat, and red meat diets may increase the risk for development of diverticulosis and possible diverticulitis. Obesity and smoking are known to increase the potential for both diverticulitis and diverticular bleeding. 5. 5. Question A patient is admitted to the same day surgery unit for liver biopsy. Which of the following laboratory tests assesses coagulation? Select all that apply. • A. Partial thromboplastin time • B. Prothrombin time • C. Platelet count • D. Hemoglobin • E. Complete Blood Count • F. White Blood Cell Count Incorrect Correct Answer: A, B, & C Prothrombin time, partial thromboplastin time, and platelet count are all included in coagulation studies. • Option A: PTT tests the function of all clotting factors except factor VII (tissue factor) and factor XIII (fibrin stabilizing factor). PTT is commonly used in clinical practice to monitor patient response to unfractionated heparin infusion, to target therapeutic anticoagulation, and as part of a “coagulation panel” to help elucidate causes of bleeding or clotting disorders. • Option B: Prothrombin time (PT) is one of several blood tests routinely used in clinical practice to evaluate the coagulation status of patients. More specifically, PT is used to evaluate the extrinsic and common pathways of coagulation, which would detect deficiencies of factors II, V, VII, and X, and low fibrinogen concentrations. • Option C: Clinicians can monitor the function of platelets by evaluating the bleeding time, which evaluates the time between breaking the vasculature and formation of an effective platelet plug. This time may be elevated in conditions like uremia, in which platelet count is normal but demonstrates impaired function. • Option D: A hemoglobin test measures the levels of hemoglobin in the blood. Hemoglobin is a protein in the red blood cells that carries oxygen from the lungs to the rest of the body. Hemoglobin variant testing measures by percentage, the relative hemoglobin types present in erythrocytes. This testing allows for the detection of hemoglobin variants and thalassemic disorders. • Option E: A complete blood count (CBC) is a blood test used to evaluate the overall health and detect a wide range of disorders, including anemia, infection and leukemia. A complete blood count test measures several components and features of the blood, including red blood cells, white blood cells, hemoglobin, hematocrit, and platelets. • Option F: A white blood cell (WBC) count is a test that measures the number of white blood cells in the body. Of note, if a subtype of white blood cells seems to be elevated based on the differential, the actual value of the type of white blood cells should be calculated by multiplying the percentage listed on the differential by the total number of white blood cells. 6. 6. Question A patient on the cardiac telemetry unit unexpectedly goes into ventricular fibrillation. The advanced cardiac life support team prepares to defibrillate. Which of the following choices indicates the correct placement of the conductive gel pads? • A. The left clavicle and right lower sternum. • B. Right of midline below the bottom rib and the left shoulder. • C. The upper and lower halves of the sternum. • D. The right side of the sternum just below the clavicle and left of the precordium. Incorrect Correct Answer: D. The right side of the sternum just below the clavicle and left of the precordium. One gel pad should be placed to the right of the sternum, just below the clavicle and the other just left of the precordium, as indicated by the anatomic location of the heart. To defibrillate, the paddles are placed over the pads. According to the ILCOR guidelines, the sternal paddle should be placed ‘just to the right of the upper sternal border below the clavicle’ and the apical paddle ‘to the left of the nipple with the centre of the electrode in the mid-axillary line’. • Option A: During the gel pad placement study it was noticed that about 50% of doctors placed the rectangular apical paddle vertically upwards, pointing towards the left armpit. The other 50% placed it in a horizontal position across the chest. The present ILCOR guidelines do not specify which orientation should be used for defibrillation. It was hypothesized that, with the paddle method for defibrillation, it would be more difficult to get good skin contact across the curved chest wall with the horizontal orientation, and in a small study this proved to be the case. • Option B: In theory, a paddle position that is too superomedial means that less current will traverse the myocardium. When 60 N (the median force used by defibrillator operators in clinical practice) is applied to both paddles, the resulting TTI is 5% greater with the horizontal orientation. Thus, if paddles are used, it is recommended to use a vertical orientation. It is expected that their flexibility will allow better electrode/skin contact across the curved chest wall; however, in the absence of any evidence to the contrary, it is advised to use vertical orientation for this method as well. • Option C: Most healthcare workers are not [Show More]
Last updated: 7 months ago
Preview 1 out of 92 pages
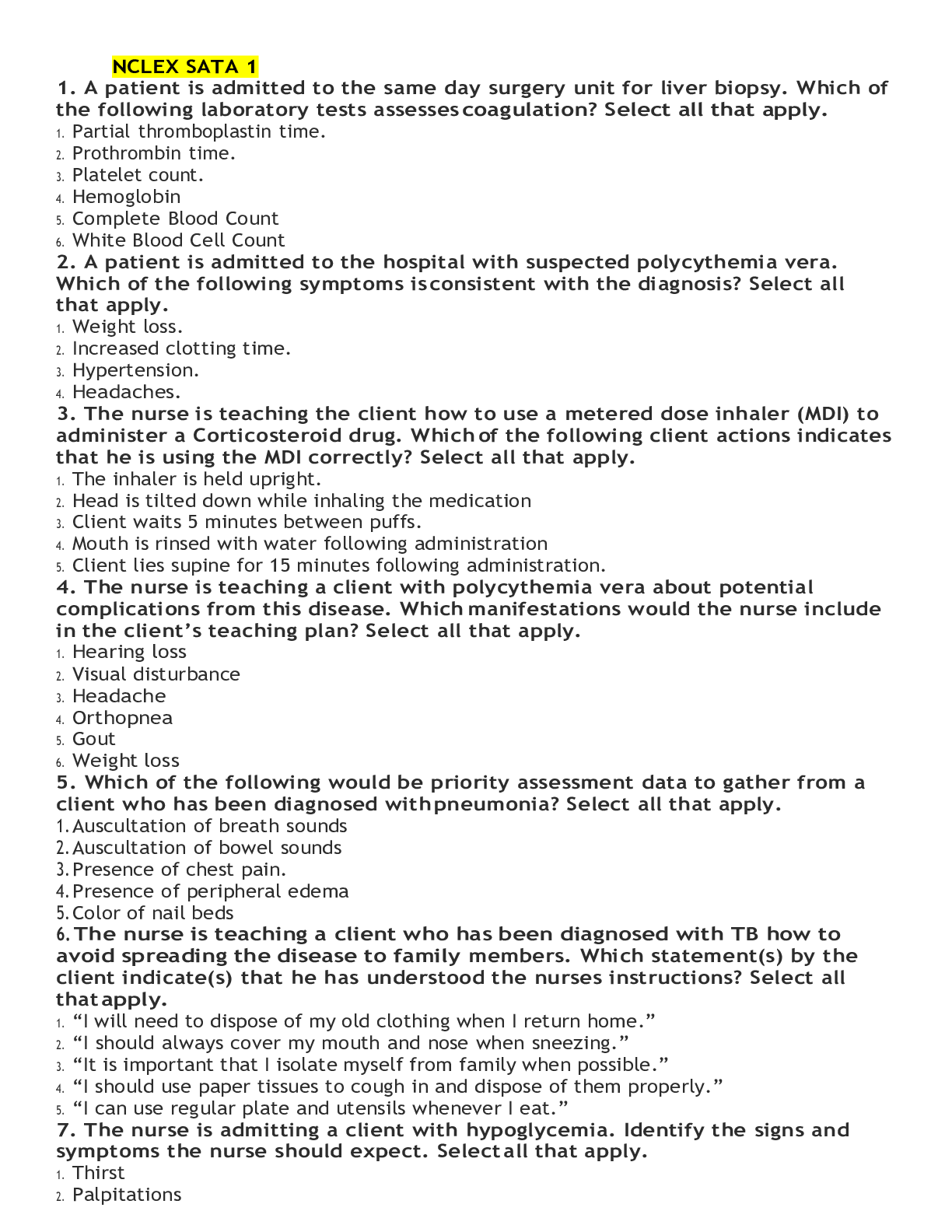
Instant download
Buy this document to get the full access instantly
Instant Download Access after purchase
Add to cartInstant download
Also available in bundle (1)

NCLEX-RN Practice Quiz Test Bank SET 1-12 BUNDLE | (900 Questions in Total)
NCLEX-RN Practice Quiz Test Bank SET 1-12 BUNDLE | (900 Questions in Total)
By Ajay25 7 months ago
$50
12
Reviews( 0 )
Document information
Connected school, study & course
About the document
Uploaded On
Oct 13, 2023
Number of pages
92
Written in
Additional information
This document has been written for:
Uploaded
Oct 13, 2023
Downloads
0
Views
65

 NCLEX Study Guide.png)