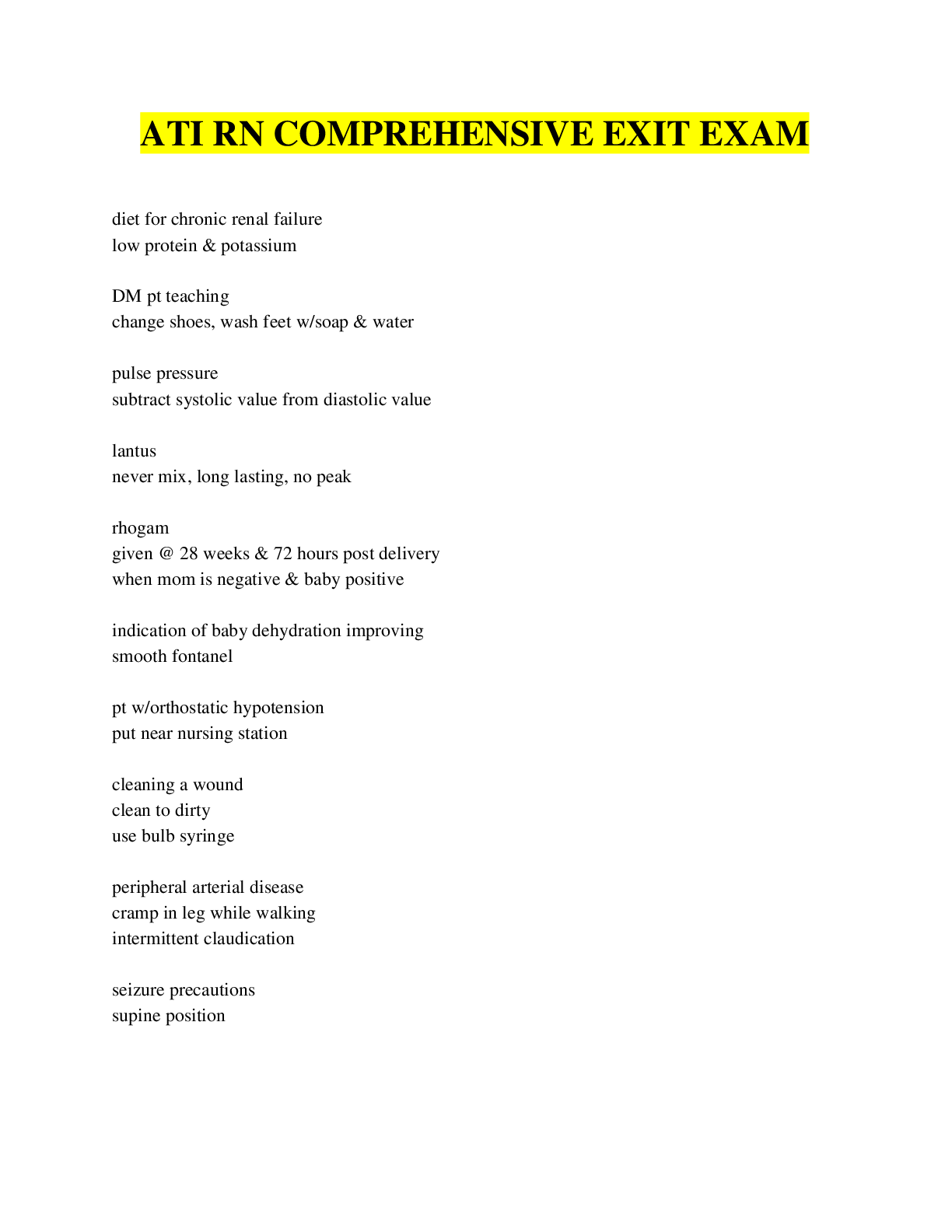
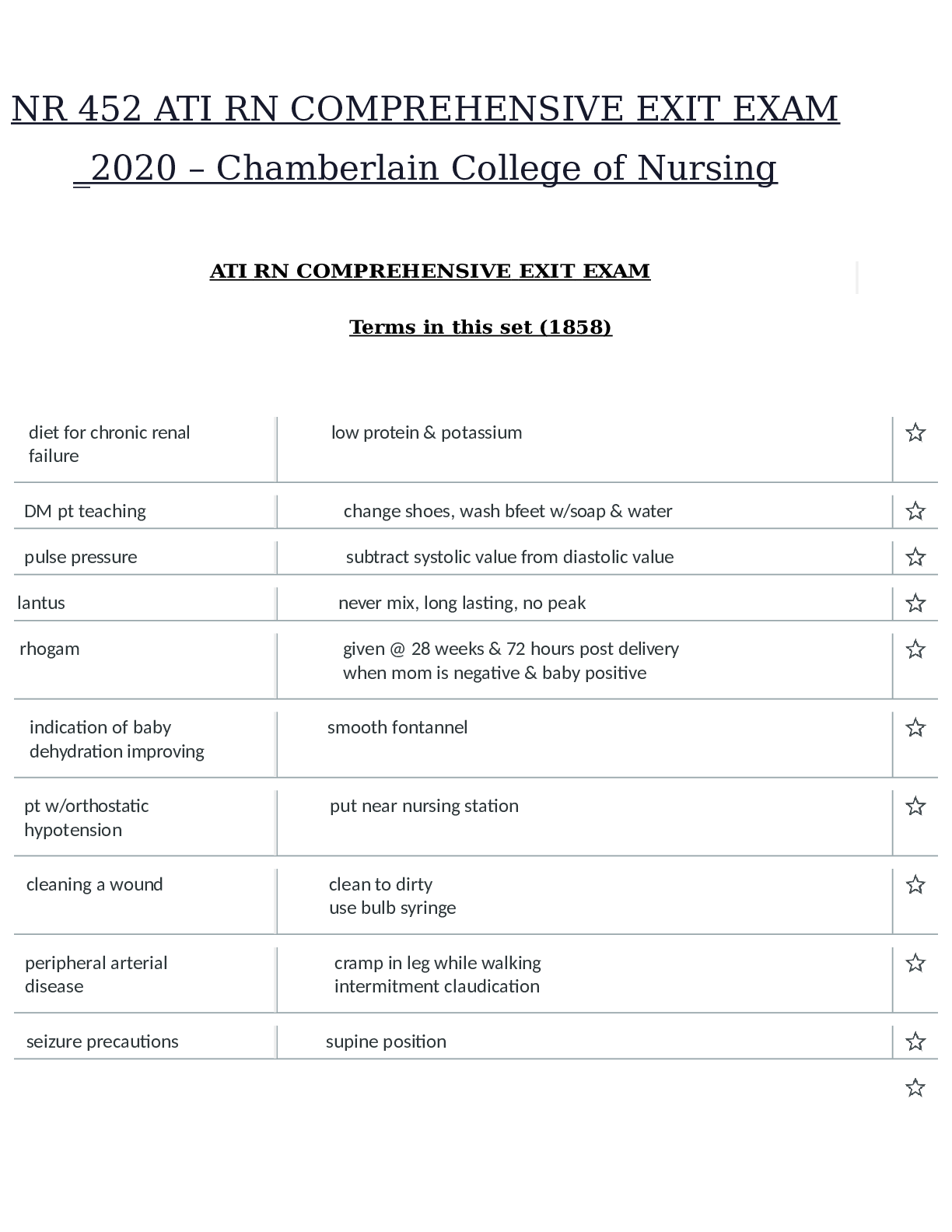
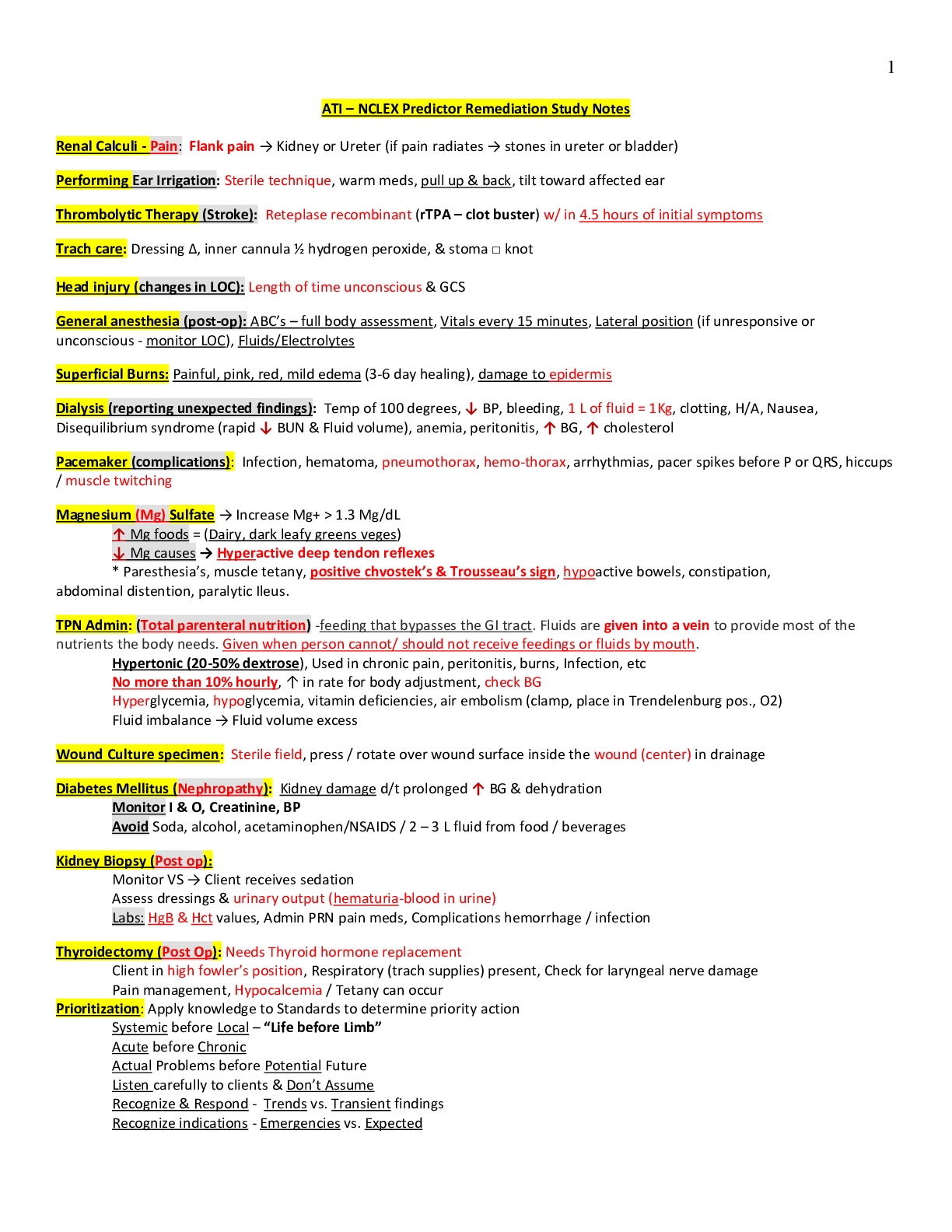
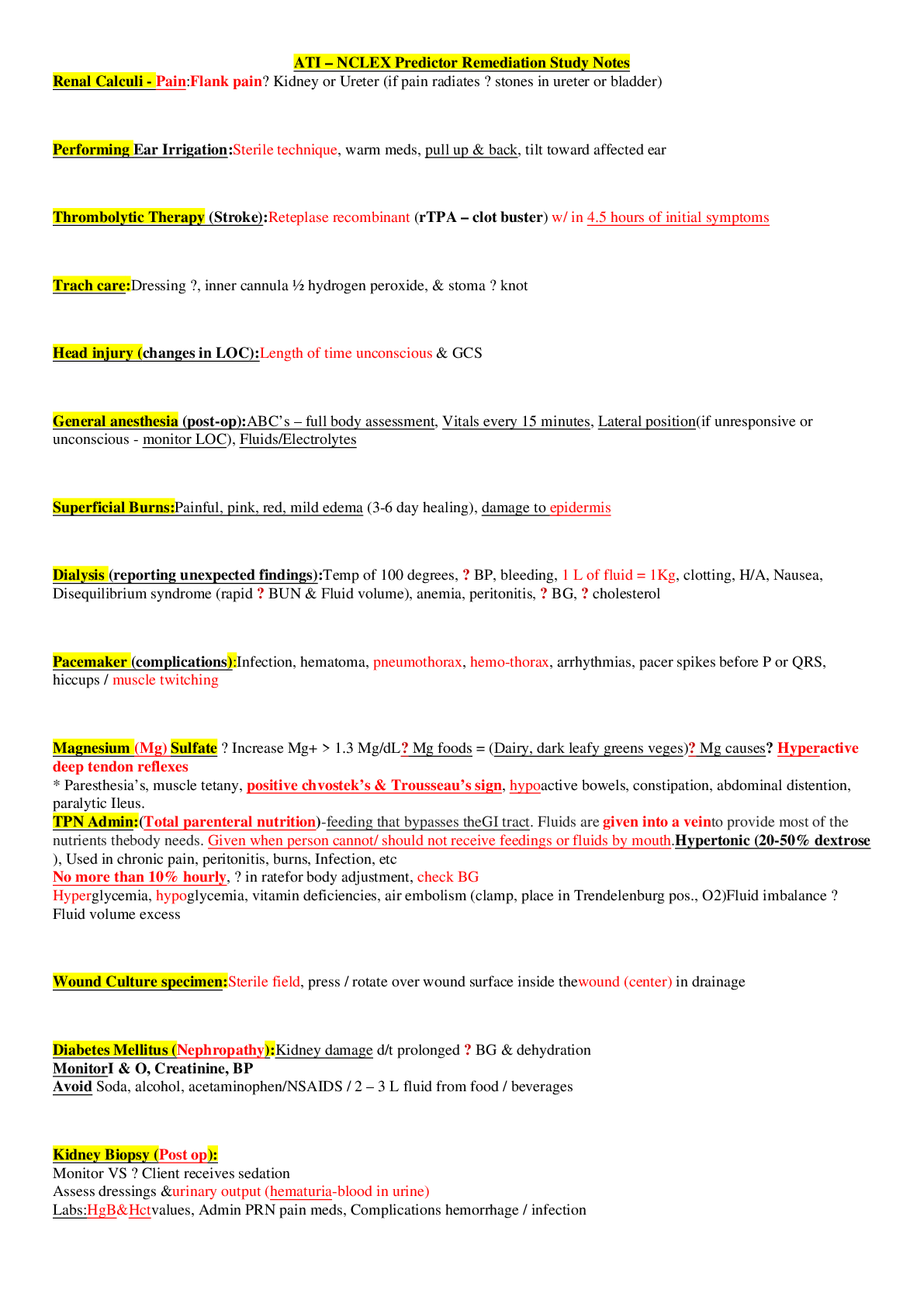
*NURSING > QUESTIONS and ANSWERS > ATI – NCLEX Predictor Remediation Study Notes understandable notes new docs 2021 (All)
ATI – NCLEX Predictor Remediation Study Notes understandable notes new docs 2021
Document Content and Description Below
ATI – NCLEX Predictor Remediation Study Notes Renal Calculi - Pain: Flank pain → Kidney or Ureter (if pain radiates → stones in ureter or bladder) Performing Ear Irrigation: Sterile techniq... ue, warm meds, pull up & back, tilt toward affected ear Thrombolytic Therapy (Stroke): Reteplase recombinant (rTPA – clot buster) w/ in 4.5 hours of initial symptoms Trach care: Dressing ∆, inner cannula ½ hydrogen peroxide, & stoma □ knot Head injury (changes in LOC): Length of time unconscious & GCS General anesthesia (post-op): ABC’s – full body assessment, Vitals every 15 minutes, Lateral position (if unresponsive or unconscious - monitor LOC), Fluids/Electrolytes Superficial Burns: Painful, pink, red, mild edema (3-6 day healing), damage to epidermis Dialysis (reporting unexpected findings): Temp of 100 degrees, ↓ BP, bleeding, 1 L of fluid = 1Kg, clotting, H/A, Nausea, Disequilibrium syndrome (rapid ↓ BUN & Fluid volume), anemia, peritonitis, ↑ BG, ↑ cholesterol Pacemaker (complications): Infection, hematoma, pneumothorax, hemo-thorax, arrhythmias, pacer spikes before P or QRS, hiccups / muscle twitching Magnesium (Mg) Sulfate → Increase Mg+ > 1.3 Mg/dL ↑ Mg foods = (Dairy, dark leafy greens veges) ↓ Mg causes → Hyperactive deep tendon reflexes * Paresthesia’s, muscle tetany, positive chvostek’s & Trousseau’s sign, hypoactive bowels, constipation, abdominal distention, paralytic Ileus. TPN Admin: (Total parenteral nutrition) -feeding that bypasses the GI tract. Fluids are given into a vein to provide most of the nutrients the body needs. Given when person cannot/ should not receive feedings or fluids by mouth. Hypertonic (20-50% dextrose), Used in chronic pain, peritonitis, burns, Infection, etc No more than 10% hourly, ↑ in rate for body adjustment, check BG Hyperglycemia, hypoglycemia, vitamin deficiencies, air embolism (clamp, place in Trendelenburg pos., O2) Fluid imbalance → Fluid volume excess Wound Culture specimen: Sterile field, press / rotate over wound surface inside the wound (center) in drainage Diabetes Mellitus (Nephropathy): Kidney damage d/t prolonged ↑ BG & dehydration Monitor I & O, Creatinine, BP Avoid Soda, alcohol, acetaminophen/NSAIDS / 2 – 3 L fluid from food / beverages Kidney Biopsy (Post op): Monitor VS → Client receives sedation Assess dressings & urinary output (hematuria-blood in urine) Labs: HgB & Hct values, Admin PRN pain meds, Complications hemorrhage / infection Thyroidectomy (Post Op): Needs Thyroid hormone replacement Client in high fowler’s position, Respiratory (trach supplies) present, Check for laryngeal nerve damage Pain management, Hypocalcemia / Tetany can occur Prioritization: Apply knowledge to Standards to determine priority action Systemic before Local – “Life before Limb” Acute before Chronic Actual Problems before Potential Future Listen carefully to clients & Don’t Assume Recognize & Respond - Trends vs. Transient findings Recognize indications - Emergencies vs. Expected Delegate to LPN: Monitoring Findings, Reinforcing teaching, performing trach care, suctioning, checking NG tube patency, administer tube feedings, inserting urinary catheter, administering meds (No IV) Delegate to AP: ADLs, Bathing, Grooming, Dressing, toileting, Ambulating, feeding w/out swallowing precautions, positioning, routine tasks, bed making, specimen collection, I & O, VS for stable clients, monitoring clinical manifestations after initial RN assess/eval. Paracentesis (prep) - take out fluid from belly (peritoneal fluid) Have client VOID Bariatric Surgery: (weight loss surgery) – Semi fowlers, 6 small meals/day, liquid/pureed food for first 6 weeks (not to exceed 1cup), Vitamin / mineral supplements, & 2 servings of protein daily. Ostomy (in small intestine) Avoid odorous & gas foods (dark green veges, dairy, fish, eggs, beans, corn), yogurt ↓ gas Avoid ↑ fiber foods for first 2 months, ↑ fluid intake Dumping Syndrome: Happens within 15mins of eating. Sx: cramps, diarrhea, tachycardia, dizziness, fatigue, hypoglycemia Interventions: small frequent meals, drink liquids 1hr b4/after Parkinson’s disease: Tremor, muscle rigidity, bradykinesia (slowness in movement), postural instability Stages: 1. Unilateral shaking / tremor of one limb 2. Bilateral limb involvement, difficulty walking/balance 3. Slowed physical movements 4. Akinesia & Rigidity make ADL’s difficult 5. Unable to stand/walk, dependent of cares, dementia Assault: threat Battery: touching Hypoglycemia Sx: Shakiness, confusion, sweating, tachycardia, diaphoresis, palpitations, H/A, lack of coordination, blurred vision, seizures, coma Oral Hypoglycemic Agents: promote insulin release from pancreas (Type2 DM) Glipizide (Glucotrol), Chlorpropamide (Diabines), Glyburide (Diabinese), Metformin (Glucophage). * Med for insulin overdose = Glucagon Radiation Adverse Effects: Skin changes, hair loss, debilitating fatigue, 30 minute visits / stays 6ft away / private room Infection control in clients home: good hygiene, avoid crowded areas, avoid raw foods (veges/meats), avoid cleaning litter boxes, clean home and avoid sick family. Client evacuation in response to fire: greatest good for the greatest amount of people Client in seclusion: 18 yo+ → 4 hours, 9 – 17 yo →2 hours, 8 yo & younger →1 hour Conduct Disorders: lack of remorse, bullies, threatens, low self-esteem, tempers, physical cruelty, destroys property, truant, and shoplifts Manic Phase: ↑ mood, irritable, lasts at least a week, euphoria, agitation, restless, ↑ in talking, flight of ideas, grandiose view of self, impulsive, manipulative, poor judgement, attention seeking. Paranoid: distrust / suspiciousness Schizoid: emotional detachment, disinterest in relationships, indifferent to praise/criticism, uncooperative Schizotypal: odd beliefs, eccentric appearance, magical thinking, perceptual distortions Antisocial: disregard for others, lack of empathy, unlawful, failure to accept responsibility, manipulative, impulsive, seductive Borderline: instability of affect, identity & relationships, splitting behaviors, fear of abandonment, self-injurious, impulsive Histrionic: attention seeking, seductive, flirtatious Narcissist: arrogant, constant admiration, lack of empathy Avoidant: anxious, wants close relationships, fear of rejection Dependent: dependency on another individual OCD: perfectionist, orderly, and control Clozapine (Anti-psychotic Atypical ) Adverse effects: metabolic syndrome, orthostatic hypotension, anti-cholinergic effects, agitation, dizziness, sedation, mild EPS, ↑ prolactin levels(galactorrhea, amenorrhea, gynecomastia), & sexual dysfunction Anti-lipemic Agents: (Statins) – treats high levels of fats/cholesterol in blood -called lipid-lowering drugs Monitor liver enzyme levels (hepatotoxicity) and muscles – monitor CK levels (myopathy & peripheral neuropathy) Med interactions: Fibrates (Genfibrozil) - ↑ myopathy risk, Erythroycin & Ketoconazole, Amiodarone, & Cyclosprine = Grapefruit juice can ↑ statin levels Gentamicin (effects urine output) -causes ototoxicity w/ diuretics, digoxin, lithium, ototoxic meds, NSAIDs, & anti-hypertensives Long term therapy for RA: DMARDs (methotrexate, etanercept, infliximab, adalimubrab, Azathioprine, Cyclosporine) ** Slow joint degradation Glucocorticoids (Prednisone) & NSAIDs provide symptom relief from inflammation & pain Bulb Syringe (for babies): Mouth first, then nose, depress. Then insert into mouth, avoid center of mouth- may stim. gag reflex. Priority action to an allergic response: Mild rashes/hives – Benadryl Anaphylaxis - treat with epi, bronchodilators, and anti-histamines Provide respiratory support & notify HCP Losartan (ARBs -Anti-Hypertensive (HTN) & kidney disease) - Cough & hyperkalemia are for ace inhibitors. Side Effects: Angioedema, hypotension, dizziness Tracheostomy Care: 2 xtra tubes, adequate humidification, oral care every 2 hours, trach care every 8 hours, sterile suctioning, surgical asepsis to remove / clean inner cannula, secure trach ties before removing old, square knot, clean from stoma outward Appropriate Doc.: Subjective/objective data, Accurate/concise, Complete/current, Organized/ date/ time/ blk ink Crutch safety: Support bodyweight at hand grips with elbows at 30 degrees, Position crutches on unaffected side when sitting or rising from a chair Varicella (chicken pox) Transmission: Direct contact, droplet, from person with shingles, 10-21 days, 1-2 days before lesions appear and all lesions have sabs Scoliosis: Lateral curvature of spine & spinal/truncal rotation that causes ribs asymmetry. Curve needs to be at least 10 degrees One leg shorter than the other. Asymmetry in scapula, ribs, flanks, shoulders, hips. Screening for Idiopathic Scoliosis: During pre-adolescence - Observe child from back Bend at waist with arms handing down & observe for asymmetry of ribs and flank Measure truncal rotation with a scolio-meter Use Cobb technique to determine degree of curvature Use riser scale to determine skeletal maturity ↓ Cardiac output (interventions): Maintain bedrest, Semi fowler’s/ fowler’s position while awake, Sleep w/ pillows Cardiac output positioning for optimal output: Left lateral side, Semi fowlers, Supine with wedge under one hip Infant car seat: Position infant in car seat at 45 degree angle, Safety restraints loose and low on abdomen Correct use of Condoms: On erect penis, empty space at tip for sperm reservoir (May be used with spermicidal gel to ↑ effectiveness), Protects against STI’s, only water soluble lube with latex condoms Amnio-infusion for Oligohydramnios: (not enough amniotic fluid around fetus) Infusion or NS or LR into amniotic cavity to reduce severity of variable decelerations caused by cord compression Scant amount or absence of amniotic fluid, Membranes must have ruptured to perform - Warm fluid Rhogam for Clients who are RH-Negative: (Antibodies from human plasma injected into RH+ mother to protect fetus) Chadwick’s sign – violet/blue color or cervix & vaginal mucosa Goodell’s sign – softening of cervical tip HSV (Herpes simplex virus): direct contact transmission to fetus is greatest during vaginal birth if woman has active lesions, Lesions & tender lymph nodes, Obtain cultures from women who have HSV or are at or near term Urinary frequency Interventions: ↓ fluid intake b-4 bed, Use perineal pads, and Kegel exercises ↓ stress incontinence Buddhist Dietary practices: vegetarian, nuts, legumes (dried peas/cooked beans), No eggs, no milk products Notifiable Communicable diseases: anthrax, botulism, cholera, diphtheria, gonorrhea, hep A/B/C, HIV, legionaries, lymes, malaria, mumps, pertussis, polio, syphilis, tetanus, TSS, TB, Typhoid fever, VRSA, At risk populations, transmissions routes Anterior Pituitary Hormones: Stimulate growth - Caution in DM patients – can cause hyperglycemia (Somatropin) Anti-Convulsants: Tx- seizures (caphe) Petit Mal (Valet) Carbamazepine, valproic acid, ethosuximide, Phenytoin/phenobarbital – adverse effects = yellowing of skin, nystagmus, teratogenicity, osteomalacia, H/A, vertigo, ataxia Ophthalmic Agents: Beta Blockers: ↓ aqueous humor production (betotopic, betaxon, betagan, betimol) Prostaglandin Analogs: ↑ aqueous humor outflow (xalantan, travatan) Alpha Adrenergic Agonists: ↓ aqueous humor & ↑ outflow (Alphagan) Direct Acting Cholinergic Agonist: ↓IOP & ↑ outflow of AH (Pilocarpine) Side effects for Ophthalmic Agents: Blurred vision, angle closure glaucoma, dry eyes, photophobia, ocular pressure, can cause systemic effects, ciliary muscle constriction Mixing Insulin: (Clear before Cloudy) Air into NPH (Cloudy), Air into Regular (Clear), Draw up Regular (Clear), Draw up NPH (Cloudy) * Hypoglycemia is most likely to occur during peak. Obstetric History: (GTPAL) Gravida, Term, Preterm, Abortions, Living Children Pre-Term Infant: Anticipated Problems (TRIES) Temperature regulation (poor), Resistance to infections (poor), Immature Liver, Elimination problems (Necrotizing Enterocolitis), Sensory-Perceptual Functions (Retinopathy) Fetal Heart Rate: (VEAL CHOP) Variable Decels Cord Compression Early Decels Head Compression Accelerations O2 (Baby is well-oxygenated) Late Decels Placental Utero Insufficiency Pregnant Client - Med. Surg Floor: (FETUS) Fetal heart tones (document every shift) Emotional Support Temperature (Measure maternal) Uterine Activity/Contractions (early-low back pain) Sensations of fetal movement Placenta Previa: low implantation of the placenta / Bright red bleeding present that is painless. Place mother on bedrest in side lying position / Weigh perineal pads Abuptio Placenta: Premature separation of the placenta - Dark red bleeding may or may not be present with sharp stabbing pain Start fluid replacement, oxygen by mask, monitor FHR, keep in lateral position, pregnancy must be terminated - birth or C-Section Endocrine Agents: Thyroid Hormones (Hypothyroidism) Synthetic form of thyroxine (T4), ↑ metabolic rate, body temp, oxygen use, renal perfusion, blood volume, & growth processes. (Levothyroxine, Thyroid, Liothronien, Anti-thyroid meds (hyperthyroidism), graves, thyrotoxicosis, propythiouracil (PTU) Cholecystitis: (Inflammation of Gall Bladder) ↓ fat intake, NO - coffee, broccoli, cauliflower, cabbage, onions/ legumes Compartment Syndrome: Sx: (5 Ps) Pain, Pallor, Pulse ↓ or absent, ↑ BP, Paresthesia (tingling hands, feet) Acute Renal Failure: Can cause HypoNatremia, HyperKalemia, HypoCalcemia, & HyperPhosphatemia Shock Sx: (Chord Item) Anti-Platelets: Aspirin, Plavix (clopidogrel) Cold, clammy skin, Hypotension, Oliguria, Drowsiness, ↑bleeding risk, prevent MI/stroke, taken PO Rapid/shallow breathing, Irritability, Tachycardia Watch for hemorrhagic stroke (weakness, Dizziness, H/A) Elevated or reduced CVP, Multi-Organ damage Avoid NSAIDs, Heparin, warfarin, corticosteroids Anti-Platelets: Aspirin, Plavix (clopidogrel) ↑bleeding risk, prevent MI/stroke, taken PO Herb/Botanical Therapy Watch for hemorrhagic stroke (weakness, Dizziness, H/A) Echinacea (common cold), Ginger root (↓ nausea, RA) Avoid NSAIDs, Heparin, warfarin, corticosteroids Ginko Biloba (↑ vasodialation, dementia, alzheimers) HypoCalcemia Sx: (CATS) Valarian (↑ GABA to prevent insomnia) – don’t use in MH, Convulsions, Arrhythmias, Tetany, Stridor / Spasms Or pregnancy. Black cohosh (estrogen sub)-↑ anti HTN Nephrotic Syndrome meds& hypoglycemia Serum Proteins in urine, Diet with sufficient protein Peptic Ulcer Disease Diet low in sodium Avoid frequent meals/snacks, alcohol, smoking, NSAIDs, Nephrolithiasis (kidney stones) Coffee, spicy foods, & caffeine ↑ Fluid Consumption is primary intervention Lactose Intolerance HypoKalemia Sx: (6 L’s) Distention, Cramps, Flatus, Diarrhea Lethargy, Leg Cramps, Limp Muscles HypoGlycemia Sx: (TIRED) Low Shallow Respirations Tachycardia, Irritability, Restlessness, Excessive Hunger Lethal Cardiac Dysrhythmias Depression / Diaphoresis Lots of urine (polyuria) End Stage Renal Disease: GFR <25mL/min Pre-End Stage Renal Disease Serum creatinine rises, dialysis or transplant required ↑ in serum creatinine ↑ protein, ↓phosphorus, ↓potassium, ↓sodium Limit protein & phosphorous (meat, dairy, pb, dried peas, Fluid restricted diet Beans, cola, chocolate beer) Protein needs ↑ once dialysis begins Restrict sodium to maintain BP Vitamin D deficiency occurs Arterial occlusion (4 P’s) HTN Care: (Diuretic) Pain, Pulselessness, Pallor, Paresthesia Daily weight, I&O’s, urine output, response of BP, CHF Treatment: (MADD DOG) Electrolytes, take pulse, Ischemic Episodes (TIA’s) Morphine, Aminophylline, Digoxin, Diuretics, Oxygen Complications (CVA, CAD, CHR, CRF) Gases (ABG’s) Labs: Normal Values: Normal Values: Creatinine 0.6-1.2 Males 0.5-1.1 Females RBC 4.7-6.1 Males 4.2-5.4 Females Hematocrit 42-52 Males 37-47 Females Urine Specific Gravity 1.0-1.030 APTT 40 Sec. Digoxin 0.5-2.0 Lithium 0.8-1.4 Anti-Emetics (-tron, -zine): Can cause sedation. Metoclopramide (Reglan)- monitor for EPS PPI’s (-zole): can cause Vit. B12 deficiency Erectile Dysfunction agents (-fil): Can cause H/A, flushing, back pain, muscle aches, & temporary vision changes. * Don’t take if have heart problems, BP issues, or stroke. Anti-Enemics: Liquid iron can cause teeth staining, dilute w/ water or juice. Iron – given IM (Z-track method) Oral Iron – avoid Vit. C. (antacids by 2 hours, empty stomach 1 hr before meals) * Black stools are common. Encourage intake of high iron foods. Anti-Coagulants: prevents of blood coagulation/clotting Heparin Sodium – admin = IV or SQ (Antidote=Protamine Sulfate) - Normal APTT = 60-80 seconds Enoxaparin (Lovenox) – admin = SQ, longer ½ life * Administer with MI or DVT * ↑ bleeding risk Avoid: Corticosteriods, NSAIDs, Vit. K, PO Hypoglycemics. Coumadin – admin = PO (Antidote = Vit. K) Avoid: using with low platelets, foods high in Vit. K, Tylenol, glucocorticoids, aspirin, use while pregnant Monitor: INR & patient HypoNatremia: ↓ Sodium - Sx: confusion, restlessness, lethargy, seizures, coma - Treat: fluid restriction HypoKalemia: ↓ Potassium - Sx: poor muscle strength, slow reflexes, flat T waves (cardiac dysrhythmias) - Treat: PO or IV Potassium supplement HyperNatremia: ↑ Sodium - Sx: Postural hypotension - Treat: Fluids (drink/IV) HyperKalemia: ↑Potassium - Sx: Twitching, contraction, paralysis, peaked T waves (cardiac dysrhythmias) - Treat: Kayexalate, Loop diuretic, Insulin HypoCalcemia: ↓ Calcium - Sx: twitching, muscle cramps, Trousseau/Chvostaks - Treat: dietary supplement, antacids, and vitamins HyperCalcemia: ↑ Calcium - Sx: muscle weakness, fatigue, slow GI - Treat: diuretic, 3-4L fluid daily, weight bearing, and calcitonin Antidotes: Bethanechol/Neostigmine = Atropine Atropine = Phyosostigmine Digoxin = Digibind Warfarin = Vitamin K Heparin = Protamine Sulfate Insulin Induced Hypoglycemia = Glucagon Acetaminophen = Acetylcysteine (mucomyst) Ace Inhibitors (-pril): HF, HTN, MI, and Diabetic Neuropathy Side effects: orthostatic hypotension, dry cough, hyperkalemia, NSAIDs ↓ therapeutic effects Alpha Adrenergic Blockers (-zosin): Dilate Veins/Arteries (Prazosin, Doxazosin) ARBS (-sartan): Produce vasodilation by blocking Angiotensin II. (Losartan) CCB’s (-dipine): Vasodilation by blocking calcium channels. (Nifedipine, Amlodipine, verapamil, Diltiazem) Avoid: drinking grapefruit juice – can lead to toxicity Electrolytes: Sodium: Administer Isotonic IV therapy (NS/LR) Potassium: Maintains electrical excitability of muscle conduction of nerve impulses (NEVER given IV PUSH) Calcium: Muscoskeletal, neuro / cardio function, implement seizure precautions Magnesium: Skeletal muscle contraction & blood coagulation. Monitor: BP, Pulse, Respirations Anti-Gout Meds: Gout is a type of arthritis. Buildup of Uric Acid. First line: NSAIDs / Prednisone, Colchicine (GI distress potential – take with food) Allopurinol: prevents uric acid production Drug interactions: salicylates, loop diuretics, alcohol, warfarin Food interactions: anchovies, yeast, organ meat, legumes, mushroom, spinach, asparagus, cauliflower Anti-Reabsorptives : slow bone removal or improve bone mass. (Menopausal women) Bisphosphonates (Alendronate – Fosamax). Can cause severe esophagitis. Take on empty stomach w/8oz of water & sit upright for 30 minutes. Anti-Neoplastics: Cancer meds Side effects: soreness, difficulty swallowing, diarrhea, stomach pain, low platelets, anemia, sensitive skin, excess tear formation Mental Status Exam: LOC, physical appearance, behavior, & cognitive/intellectual abilities Anxious / depressed: open ended supportive statements Suicidal: direct yes/no questions to assess risk Panicked: use gentle reality orientation Confused: Provide reality orientation Delusions/Hallucinations/Paranoia: Acknowledge, don’t reinforce Obsessive Compulsive Behavior: Communicate after behavior Personality/Cognitive Disorder: Be calm and matter of fact Aggressive/Violent: set boundaries, limits, short simple sentences Psychiatric Meds: SSRI’s: Citalopram, Fluoxetine, Sertraline (avoid St John’s Wort) TCA’s: Amitriptyline (anticholinergic effects “cant’s” – orthostatic Hypotension MAOI’s: Phenelzine, Hypertensive Crisis Atypical: bupropion (appetite suppression, H/A, Dry mouth) SNRI’s: Venlafaxine / Duloxetine (nausea, weight gain, sexual dysfunction) RN delegate surgical asepsis responsibilities to UAP's? Only under RN supervision When should traditional hand washing be used instead of using alcohol-based sanitizer? Hands are visibly soiled, touching bodily fluids, Before/after applying sterile gloves, After using sanitizer 10+ times Contradictions of good hand hygiene Nail polish, Long nails, using lotions, Wearing jewelry Potential routes of entry into the body for blood borne pathogens? Mucous membranes, Puncture wounds, Burns on hands, Blood Personal Protective Equipment (PPE) is the single most effective way to prevent the transmission of infection Two potential sites for nosocomial infections: hospital & Homecare Causes of nosocomial infections: suppressed immune system, Failure to follow isolation precautions or aseptic technique, Hospital error A physician is preparing to perform a lumbar puncture. The suspected diagnosis is bacterial meningitis. What type of precaution is needed? Standard precautions A 70 y. male develops new diarrhea and a high WBC while in the hospital recovering from MV Replacement surgery which was complicated by a CVA. He is bed bound and incontinent of stool. What do you suspect is the cause for his diarrhea? A bacterial, nosocomial infection Medical abbreviation: CBR, BR complete bedrest, bedrest Frequent bathing for the older client is necessary to prevent skin breakdown. False A bath can be helpful in soaking a client's pelvic area in warm water to decrease inflammation. sitz 3 guidelines for providing patient-centered care when addressing a client's hygiene needs Be respectful to cultural values, Ask the pt in what order they would like to complete their hygiene routine. Provide hygienic care as often as necessary (but not too often) and as gently as necessary. What should be included in documentation of a bath? Date and time, Type of bath, Abnormal findings/pt reaction When might the RN need to collaborate a colleague for personal care? If a patient is not ambulatory and is too heavy to be moved alone What are the components of the Braden scale? Sensory perception, moisture, activity, mobility, nutrition, friction & shear - High score indicates low risk. Trochanter roll -Keeps hips in a neutral position Hemiparesis Weakness on one sign of the body Hemiplegia - Paralysis on one side of the body Prone position - Lying on the abdomen Sim's position - Lying on left side w/ left leg straight and right knee bent Foot drop - Gait w/ drop of the forefoot Fracture pan - A bedpan used for someone w/ a hip fracture Fecal impaction - Dry, hard stool stuck in the rectum Hand roll - Hand placed in the palm to prevent fractures WNL - Within normal limits BRP - bathroom privileges BUS - Bladder ultrasonic scanner Factors to consider when delegating to UAP - Scope of practice, Facility, state regulations, Level of experience, Pt safety Hazards of immobility on CV system & interventions DVT: elastic stockings, SCD's, Orthostatic BP: give pt time between position changes Hazards of immobility on pulmonary system & interventions PE: TED host, Inadequate expansion of the chest: place pt in orthopneic position Pneumonia: clean/sterile technique, pneumovax Intervention for each: early and frequent ambulation Hazards of immobility on renal system & interventions-UTI, problems with continence, altered BP: monitor I/O's, assist w/ voiding as needed Hazards of immobility on integumentary system & interventions Skin breakdown: repositioning, monitor nutrition status, reduce moisture, and provide hygiene care Hazards of immobility on musculoskeletal system & interventions Stiff joints: ROMs/ambulation Muscle atrophy: ROMs/ambulation Ca2+ imbalance: nutrition measures Risk factors for skin breakdown Poor nutrition, bedrest, obesity, using an SPM machine, increased friction and shear 4 areas prone to skin breakdown-Tailbone, Heels, Elbows, Hips Intervention most effective in preventing flaccidity in a hospitalized patient? Early ambulation after surgery After application of sequential compression devices (SCDs) on a patient, what assessment finding is essential for the nurse to include in documentation? Lower extremity circulatory status Components of Morse Fall Scale- History of falls, secondary diagnosis, ambulatory aid, IV/hep lock, gait/transferring, mental status Scores: 45+ = high risk 25-44 = moderate risk 0-24 = low risk TB Injection - Max amt: 0.1 cc, site: forearm, Angle: 15-20 degrees, Length: 1/4 - 1/2 in, Aspiration? No SQ injections - Max amt: 2 cc, Usual site: Upper arm, stomach, Angle: 45 degrees, Length: 1/2 - 1 in, Aspiration? Yes IM injections - Max amt: 5 cc Usual site: deltoid (1 cc), gluteus med/max or vastus lateralis (5 cc), Angle: 90 degrees, Length: 1 - 1.5 in, Aspiration? Yes What factors affect a BG result? Having fasted or eaten, time of day, level of activity, stress, illness, menstruation client most at risk for hypoglycemia? In the morning before breakfast Considerations for pt's on blood thinners such as warfarin, asprin, heparin, coumadin, etc? Monitor platelet levels (labs) Watch for bleeding/reduce risks of bleeding Monitor vitals (esp. BP) Assess skin Monitor mobility status benzodiazepines to older adults? No, benzo's increase the risk of accidents and mental deficits FUO - fever of unknown origin qhs - at bedtime ac - before meals Contraindications for opening capsules and mixing with food? EC: enteric coated & ER: extended release Rapid acting insulin Generic & brand names: Inslin aspart (NovoLog), insulin glulisine (Apidra), insulin lispro (Humalog) Onset: 15 min Peak: 30 - 90 min Duration: 3-5 hr Short acting insulin - Insulin regular (Humulin R, Novolin R) Onset: 30 - 60 min Peak: 2 - 4 hr Duration: 5 - 8 hr Intermediate-acting insulin- Insulin NPH (Humulin/Novolin N) Onset: 1 - 3 hr Peak: 8 hr Duration: 12 - 16 hr Long-acting insulin- insulin glargine (lantus), insulin detemir (levemir) Onset: 1 hr Peak: no clear peak Duration: 20 - 26 hr Signs of infiltration -Edema, pallor, decreased skin temperature around the site, and pain Signs of phlebitis - Pain, increased skin temperature, and redness along the vein Signs of extravasation (infiltration w/ dislodged IV catheter) - Pain, stinging or burning at the site, swelling, and redness Nursing interventions for infiltration, phlebitis, and extravasation Infiltration: D/C IV, elevate extremity, apply warm compress Phlebitis: D/C IV, apply warm/moist compress Extravasation: D/C IV, apply cool compress, administer antidote if needed, document degree of extravasation INT -intermittent (catheter) The 6 rights of medication administration 1. Right drug 2. Right dose 3. Right route 4. Right pt 5. Right time 6. Right documentation 3 nursing interventions r/t routine care of peripheral IV 1. Check insertion site frequently 2. Change tubing every 96 hr 3. Use good hand hygiene + standard precautions Factors to consider when choosing the best IV location Age, condition of veins, circulation status, length of IV therapy What is the smallest gauge IV catheter used to infuse blood? 20-22: RBS' might get crushed when using a smaller cath. 4 techniques to improve the chances of good IV access 1. Trim hair around the area 2. Gently stroke the area from the distal to proximal end 3. Place a warm blanket over the extremity 4. Palpate gently At what range of rate should you administer maintenance fluids? 75-150 Does the secondary/piggyback IV bag hang above or below the primary bag? Below What gauge catheters should you use for IV access? (smaller the gauge, larger the hole) 24: children 22: older adults (esp women) 20: healthy adult 16-18: trauma pt's What is included in an IV start kit? Tourniquet, alcohol wipes, gauze, tape Will also need: IV catheter, saline flushes, extension tubing Cardiac tamponade - Fluid in the pericardial sac Tunneled catheter - A catheter surgically inserted into a trench Delegation: central lines - Care/dressing changes cannot be delegated to UAP. UAP may observe central lines and report concerns. What are PICC lines (ARM) used for? Used for long-term IV access What are multi lumen central catheters used for? Monitoring central venous pressure, sampling blood, and simultaneous administration of multiple IV solutions/drugs Hickman catheter - Used for chemotherapy or blood withdrawal Nursing interventions associated w/ routine care of a central IV 1. Clamp the central line when not in use 2. Maintain patency by flushing 3. Avoid excessive force w/ small syringes 4. Never use a syringe smaller than 10 mL List potential central IV complications and nursing interventions associated w/ each 1. Infection: hand hygiene, scrub the hub, and use aseptic technique 2. Pneumothorax: monitor vitals, admin O2 if needed, notify the provider of warning signs 3. Air embolism: check the line frequently, keep catheters clamped, don't inject air; if embolism occurs: clamp catheter, admin O2, and place pt of left side in Trendelenburg (supine w/ feet elevated) Which activity is important to include in the plan of care for a client with a PICC? Use sterile technique when changing the PICC dressing. UA - urinary analysis for culture & sensitivity What are two ways the nurse may obtain a C&S? Sterile collection from Foley - Sterile collection from straight cath Midstream urine collection Clean the peritoneal area Collect a midstream sample after urinating for several seconds What color does a fecal sample containing occult blood turn? Blue A UA that is positive for hemoglobin, WBCs, and nitrites indicates: UTI 3 strategies for preventing UTI in the client after insertion of an indwelling catheter. Provide peritoneal care every 6 hours Change out the catheter every 8 hours Drain the collection bag PRN (when full and before ambulation) Remove the Foley post-op day 2 Maintain adequate fluid intake A patient with an indwelling catheter reports a need to void. What is the priority intervention for the nurse to perform? a. Check to see if the catheter is patent. LIWS - Low intermittent wall suction Contraindications for an NG/OG tube - Obstruction, tube already inserted, recent facial surgery, bleeding contraindications Your pt has a PEG tube that was inserted 2 days ago. As you are preparing your pt's morning medications, you are unable to flush the tube with sterile water. Give 2 examples of nursing interventions to manage this problem. Check to see if the tubing is clamped. Check the tubing for clogs. Push in air. Try to unclog w/ warm water. Get order for enzyme. Your pt is receiving TPN. What are some potential complications related to administration of TPN? Give examples of nursing interventions necessary to prevent complications related to administration of TPN. Skin breakdown/irritation: assess frequently, provide adequate hygiene care Air embolism: be careful about administering solutions in the wrong line You are an RN who is inserting an NG tube for decompression. Your pt begins to gag. Give 3 examples of nursing interventions to manage your pt's response. Stop pushing and slow down insertion. Tilt pt's chin toward chest. Check the mouth for substances to prevent aspiration. Continue advancing the tube btwn breaths. laboratory values to monitor for patients requiring continuous enteral feeding? Electrolyte levels, glucose levels patient discharged home with a PEG tube. dietary education/nutritional planning is important once the pt goes home. Ability to clean the dressing and insert feedings properly, knowledge of what to do if complications arise Hydrocolloid dressing - Opaque, biodegradable, non-breathable, adherent dressing Penrose drain - A surgical fluid drain Calcium alginate - Gel used to entrap enzymes during wound healing Hydrogel dressing - Gel used to regulate fluid exchange and relieve pain during wound healing Bio-occlusive dressing - Transparent, air-tight, and impermeable to fluid Eschar - Slough produced by a burn, corrosion, or gangrene Serosanguinous fluid - Blood + serum - Yellow in color w/ some appearance of blood Debridement - Removing dead or contaminated tissue Purulent - pus-containing Undermining - Surgically separating the skin from the underlying stoma to be used to cover a wound Maceration - Softening of tissue after lengthy fluid exposure Granulation tissue - Red, moist tissue made up of new blood vessels Indicates healing Lavage - Washing out a body cavity w/ water or a medicated solution Primary intention - The process of healing in a surgically-closed, approximated wound Assessing surgical wounds Depth/width/height, Ulcer stage, Presence of undermining/tunneling, any change in wound appearance, Amt, characteristics of exudate, Color (note change) Secondary intention - The process by which chronic wounds heal- the wound's edges do not come together. The would heals by the formation of granulation tissue, wound contraction, and epithelialization. Describe variables included in assessing chronic wounds Shape, Size, Condition of wound bed, Color, Granulation status How does proper wound care promote wound healing? 1. Removes bacteria 2. Promotes or supplies fluids that promote healing 3. Provides conditions needed for epithelialization 4. Insulation protects the wound from further trauma 5. Filling dead space prevents exudate Factors that inhibit wound healing. 1. Low iron 2. Poor perfusion or lack of oxygen 3. Suppressed immune system 4. Certain medications (especially cancer treatments, steroids, and DM meds) The 75-year-old pt has undergone an open cholecystectomy 2 days ago and has a JP drain. Which interventions should the nurse delegate to the(UAP)? Select all that apply. 3. Take and record the client's vital signs. 4. Empty the client's indwelling catheter bag at the end of the shift. 5. Assist the client to ambulate in the hallway three to four times a day. Medical abbreviation: TCDB - turn, cough, & deep breath Can suction be performed by the UAP? No What respiratory care tasks can be delegated to the UAP? Turning a client and having them deep breathe or having client use incentive spirometer *Teaching and assessments for these tasks are responsibilities of the nurse. Young adult who sustained a severe traumatic brain injury, unconscious on a ventilator for several weeks and requires frequent tracheal suctioning of thick tenacious secretions to prevent aspiration. A cuffed tracheostomy tube - to prevent aspirations 3 hazards associated with suctioning and describe how the nurse can minimize the risks. Hypoxia - do not over-suction Injury to the airway - use proper technique Nosocomial infections - only aspirate with the sterile part of the tube Describe situations when the cuff of a tracheostomy tube would be deflated. When the client needs to speak, When the client has become more stable and no longer needs the cuff for ventilation Describe the purpose of a fenestrated tracheostomy tube and the purpose of the Passy Muir valve. Allows patient to breath normally, cough, speak, and swallow. The valve improves communication. Precautions necessary for O2 admin – Keep away from shades/curtains. No open flames, don't use razors or radios. Notify visitors. Handle tanks with caution. Check equipment before initiating use. No use of petroleum. Place "Oxygen in Use" sign by client. Your client has a history of pulmonary emphysema and CO2 retention, would an oxygen order for 4L/min be appropriate? No, the risk of rebreathing carbon dioxide is increased. Steps to teaching a pt how to use an incentive spirometer. 1. Exhale normally 2. Put the mouthpiece in your mouth and close your lips tightly around it. 3. Inhale slowly and deeply. Try to make the indicator rise up to the level of the goal marker. 4. When you cannot inhale any longer, remove the mouthpiece and hold your breath for at least 3 seconds. 5. Exhale normally. 6. Repeat these steps 10 to 12 times every hour when you are awake, or as often as directed. Clean the mouthpiece after use. Administering meds into the eyes Use medical aseptic technique. »»Have the client sit upright or lie supine with the head tilted slightly, looking up. »»Rest the dominant hand on the client's forehead, hold the dropper above the conjunctival sac about 1 to 2 cm, drop the medication into the center of the sac, and have the client close the eye gently. »»Apply gentle pressure with the finger and a clean tissue on the nasolacrimal duct for 30 to 60 seconds to prevent systemic absorption. Administering meds into the ears »»Use medical aseptic technique. »»Have the client sit upright or maintain a side-lying position. »»Straighten the ear canal by pulling the auricle upward and outward for adults or down and back for children. Hold the dropper 1 cm above the ear canal, instill medication, and then gently apply pressure with finger to tragus of ear unless contraindicated due to pain. »»Do not press a cotton ball deep into the ear canal. If needed, gently place it into the outermost part of the ear canal. »»Have the client remain in the side-lying position if possible for 2-3 min. Administering meds into the nose - Use medical aseptic technique. »»Have the client supine with the head positioned to allow the medication to enter the appropriate nasal passage. »»Use the dominant hand to instill drops, supporting the head with the non-dominant hand. »»Instruct the client to breathe through the mouth, stay in a supine position, and not to blow the nose for 5 min after drop insertion. How much fluid can the deltoid accommodate for IM injections? up to 1 mL Disadvantages of oral meds Oral medications have a highly variable absorption. Inactivation can occur by the GI tract or first-pass effect. The client must be cooperative and conscious. Contraindications include nausea and vomiting. IM injection disadvantages IM injections are associated with a higher cost. IM injections are inconvenient. There can be pain with the risk for local tissue and nerve damage. There is a risk for infection at the injection site. IV therapy disadvantages Even higher cost than IM's Inconvenient Immediate absorption, which can be dangerous if the wrong dosage or the wrong medication is given. There is an increased risk for infection or embolism with IV injections. Potential irritation to the vein. Precautions when initiating IVs on older clients, clients taking anticoagulants, or clients with fragile veins Avoid tourniquets. Use a blood pressure (BP) cuff instead. Do not slap the extremity to visualize veins. Avoid rigorous friction while cleaning the site. How to select veins for IV Choose: Distal veins first on the non-dominant hand. A site that is not painful or bruised and will not interfere with activity. A vein that is resilient with a soft, bouncy sensation when palpated. What should be documented after initiating IV therapy? Date & time, insertion site & appearance, catheter size, type of dressing, IV fluid & rate, number/locations/condition of failed attempts, client's response Factors affecting med dosage and response: Weight, Age, Gender, Genetics, Biorhythmic cycles, Tolerance, Accumulation, Psychological factors, Medical conditions (GI issues, vascular insufficiency, liver disease, renal disease) What is a Salem sump tube used for? Decompression or lavage What pH should gastric residuals be? Between 0 and 4 What should you use to flush the NG tube before administering formula? At least 30 mL of tap water What should you do when providing enteral feeding and residuals exceed 250 mL for two consecutive assessments? Withhold the feeding. Notify the provider. Maintain semi-Fowler's position. Recheck residual in 1 hr. What should you do when providing enteral feeding and your pt has diarrhea 3+ times w/in 24 hr? D/C the feeding. Notify the provider. Confer with the dietitian. Provide skin care and protection. What should you do when providing enteral feeding and your pt has N/V? Withhold the feeding. Turn the client to the side. Notify the provider. Check the tube's patency. Aspirate for residual. Auscultate for bowel sounds. Obtain a chest x-ray. Nursing interventions for O2 via nasal cannula Assess the patency of the nares. Ensure that the prongs fit in the nares properly. Use water-soluble gel to prevent dry nares. Provide humidification for flow rates of 4 L/min and above Expected Physiological Changes During Pregnancy: Positioning for Optimal Cardiac Output & contraception ⦁ Nurse should assess which methods will best fit a client’s lifestyle ⦁ Natural Family Planning ⦁ Abstinence: Client education focuses on refraining from sex (duh) and can focus on “affectionate touching, communication, holding hands,” etc ⦁ Benefits include it being the most effective birth control method that also cuts down on STD infection ⦁ Coitus Interruptus (withdrawal): Withdrawal of penis from vagina prior to ejaculation ⦁ Benefits: possible choice for monogamous couples who don’t have other methods of birth control ⦁ Disadvantages: Least effective method of contraception, no STD protection, high risk of pregnancy ⦁ Calendar Method: uses calendar to figure out when fertile time is and avoiding sex during this time, keeping in mind that sperm are viable 48-120 hours ⦁ Advantages: Most useful when combined with basal body temperature and cheap ⦁ Disadvantages: Not reliable, no STD protection, requires accurate record keeping and risk of pregnancy ⦁ Basal Body Temperature: Temp drops slightly before time of ovulation and can be used as natural contraception. Client measures temp in morning prior to getting out of bed. ⦁ Advantages: Cheap, convenient, and no adverse effects (except a baby) ⦁ Disadvantages: Temp can be influenced by other variables like stress, fatigue, alcohol, illness, etc and no STD protection ⦁ Symptom-Based Method (Cervical Mucus): Client notes that cervical mucus gets thin and flexible under influence of estrogen and progesterone to allow for sperm viability and motility (spinnbarkeit sign = mucus stretches between fingers is greatest during ovulation) ⦁ Pros: Helps woman become knowledgeable about her own fertile periods and the status of mucus ⦁ Cons: No STD protection and risk of pregnancy ⦁ Barrier Methods: ⦁ Male Condom: ⦁ Pros: STD protections, no adverse effects and readily accessible ⦁ Cons: High rate of noncompliance, reduce spontaneity, possible rupture, etc ⦁ Female Condom: Insert closed end of pouch is inserted into vagina by client prior to sex and anchored around cervix, ⦁ Pros: protects against babies and STDs ⦁ Diaphragm and Spermicide: Fits snugly over cervix with spermicide cream or gel, comes in different sizes (fitted by provider every 2 years or after change in client weight by 20%). Leave in 6-24 hours after sex an wash with mild soap/water after each use. ⦁ Pros: More client control ⦁ Cons: requires prescription and visit to HCP, no STD protection, must be inserted correctly or hello baby ⦁ Contraindications: Hx of TSS, frequent UTIs ⦁ Cervical Cap and Spermicide: Fits over cervix and comes in 3 sizes, insert prior to sex and leave in 6-24 hours after sex, wash after each use ⦁ Cons: Risk of TSS, allergic rxn, no STD protection ⦁ Contraceptive Sponge: Fits over cervix and is OSFA, leave in 6-24 hours post sex ⦁ Cons: No STD protection ⦁ Hormonal Methods: ⦁ Combined Oral Contraceptives: Contains estrogen and progestin and suppresses ovulation, thickening cervical mucus blocking semen, and altering uterine decidua (no implantation). Patient education – take missed dose ASAP, monitor for S/Sx of stroke or DVT ⦁ Pros: Effective, decreased menstrual blood and iron loss, improves acne ⦁ Cons: No STD protection, increased risk of DVT/stroke ⦁ Progestin- Only Pills (Minipill): Provides same action as combination pills ⦁ Client Education: Take at same time of day, you cannot miss a pill, use back up method during first month of use to prevent pregnancy ⦁ Pros: Fewer side effects (SE), safe to take while breastfeeding ⦁ Cons: No STD protection, less effective in suppressing ovulation than combined contraceptives, can’t use if had breast cancer ⦁ Emergency Oral Contraceptive: Morning after pill ⦁ Client education: taken within 72 hours of sex, take antiemetic one hour prior to taking, see HCP if no period in 21 days ⦁ Pros: No age restriction ⦁ Cons: Nausea, no long term contraception, no STD protection, risk of pregnancy ⦁ Transdermal Patch: Contains progesterone and ethinyl estradiol delivered at continuous levels ⦁ Education: Apply to dry skin over butt, abdomen, upper arm or torso (not over breast tissue) and apply new patch on same day of the week for 3 weeks ⦁ Pros: Avoids liver metabolism, decreased risk of forgetting pill ⦁ Cons: No STD protection, same adverse effects as oral contraceptives, possible skin reaction from patch, less effective for women over 198 lbs ⦁ Injectable Progestins: Medroxyprogesterone is IM or SQ injection every 11-13 weeks (3 months) ⦁ Education: Keep follow up appointments, maintain enough Ca and Vitamin D ⦁ Pros: Effective, only 4 injections a year, possible absence of periods, decreased risk of uterine cancer is used long term ⦁ Cons: Decrease bone mineral density, no STD protection, return to fertility can be delayed up to 18 months after stopping injection ⦁ Contraindications: Breast cancer, abnormal LFTs ⦁ Contraceptive Vaginal Ring: Delivers estonegestrel and ethinyl estradiol continuously ⦁ Education: Ring should be replaced every 3 weeks and inserted on same day of week monthly ⦁ Pros: Doesn’t have to be fitted, decr chance of forgetting to take pill, absorbed vaginally so lower doses can be used ⦁ Cons: No STD protection, same adverse effects as pill, some possible discomfort during sex ⦁ Implantable Proegestin: Rod containing estonegestrel is inserted on inner side of arm ⦁ Pros: Lasts for 3 years, reversible ⦁ Cons: Causes irregular menstrual bleeding, no STD protection, irregular and unpredictable menstrual bleeding, increased acne and weight gain ⦁ Contraindicated with breast cancer ⦁ IUD: ⦁ Pros: effective 1-10 years, have hormonal and non hormonal options ⦁ Cons: Increased risk of PID, no STD protection, possible infection for IUD ⦁ Contraindicated in women NOT in monogamous relationship, PID ⦁ Trans cervical sterilization: small flexible agents (like copper) are inserted in fallopian tubes causing scarring of tissue. Client must be examined after 3 months to check procedure ⦁ Pros: Quick procedure with no anesthesia, 99.8% effective and rapid return to normal ADLs ⦁ Cons: Not reversible, not effective for 3 months (use back up), no STD protection, changes in menstrual patterns, possible perforation can occur along with ectopic pregnancy ⦁ Surgical Methods: ⦁ Female Sterilization (bilateral tubal ligation): fallopian tubes are cut/burned ⦁ Pros: Permanent contraception, sex is unaffected ⦁ Cons: No STD protection, carries typical surgical risks of hemorrhage/infection/etc ⦁ Male Sterilization (vasectomy): Cut of vas deferens ⦁ Education: Go easy on activities for several days after surgery ⦁ Pros: Permanent, procedure is short and safe ⦁ Cons: Requires surgery, no STD protection, risk of infection ⦁ Body System Changes ⦁ Cardiac Output (CO) ⦁ Increases 30-50% and blood volume increase 30-45% at term ⦁ HR reaches a peak at 32 weeks’ gestation ⦁ Respiratory ⦁ Last trimester the chest enlarges to compensate for increased oxygen demands (as uterus pushes upward) ⦁ RR increases as total lung capacity decreases ⦁ Musculoskeletal ⦁ Body alterations and weight increase, making body adjust in posture and pelvic joints relax ⦁ GI ⦁ N/V occur to hormonal changes ⦁ Constipation may occur as slowing of transit time ⦁ Renal ⦁ Filtration rate increases secondary to the influence of pregnancy hormones and increase in blood volume ⦁ Endocrine ⦁ Placenta becomes endocrine organ that produces large amounts of hCG, estrogen, progesterone, etc ⦁ BP ⦁ Supine position makes BP appear lower because of pressure on vena cava from uterus (supine hypotension) ⦁ S/Sx include dizziness, pale/clammy skin, lightheadedness ⦁ Change position to left lateral side lying, semi-fowler’s position or if in supine then place wedge under hip to alleviate the pressure on the vena cava ⦁ Pulse ⦁ Increases 10-15 BPM around 32 weeks’ ⦁ Stays elevated throughout remainder of pregnancy ⦁ Respirations ⦁ Remain unchanged or slightly increased ⦁ SOB may be noted because of changes in pressure against the diaphragm ⦁ GTPAL ⦁ Gravidum ⦁ Term births (38 weeks or more) ⦁ Preterm births (viability up to 37 weeks) ⦁ Abortions/miscarriages ⦁ Living Children Prenatal Care: Interventions for Urinary Frequency During Pregnancy ⦁ Urinary Frequency: Typically occurs during 1st and 3rd trimesters ⦁ Patient should empty bladder entirely and decrease fluid intake before bedtime ⦁ Use perineal pads ⦁ Kegal exercises will help to reduce stress incontinence ⦁ N/V occurs during the first trimester ⦁ Should eat crackers or dry toast 30 min to 1 hour before getting out of bed ⦁ Avoid having an empty stomach ⦁ Don’t eat spicy foods, greasy foods, or gas forming foods ⦁ Drink fluid between meals ⦁ Breast Tenderness – first trimester ⦁ Wear a support bra ⦁ UTIs are more common because of renal changes and vaginal flora becoming more alkaline ⦁ Encourage proper wiping, avoid bubble baths, wear cotton underwear, avoid tight fitting pants, and drink tons of water, the usual suspects ⦁ Fatigue occurs a lot in 1t and 3rd trimester ⦁ Engage in frequent rest breaks ⦁ Constipation occurs a lot in 2-3 trimester ⦁ Drink lots of fluid ⦁ Eat high fiber diet ⦁ Exercise regularly ⦁ Hemorrhoids occur in 2-3 trimesters ⦁ Warm sitz bath ⦁ Witch hazelpads ⦁ Topical ointments ⦁ Supine Hypotension happens in supine position where the gravid uterus compresses vena cava ⦁ Side lying position or semi-sitting position with knees slightly flexed will help alleviate this feeling ⦁ Health Promotions ⦁ Avoid OTC Meds, alcohol and tobacco ⦁ Exercise throughout pregnancy can offer great benefits ⦁ Avoid hot tubs or saunas ⦁ Consume at least 2 L of water a day ⦁ Nurse should educate the client about: ⦁ Flu immunizations ⦁ Stop smoking ⦁ Treat current infections ⦁ Genetic counseling and testing ⦁ Exposure to hazardous materials Infections: ⦁ TORCH Infections are toxoplasmosis, other infections (like hepatitis), rubella virus, cytomegalovirus, and herpes simplex virus and can all negatively affect a pregnant woman (can cross placenta and be teratogenic) ⦁ Risk Factors: ⦁ Toxoplasmosis is caused by consumption of raw or undercooked meat or cleaning cat litter boxes ⦁ Other infections like syphilis are related to congenital defects ⦁ Rubella is spread to infants if the mother has it during preganancy ⦁ Cytomegalovirus is transmitted through droplets (vaginal secretions, breast milk, etc) ⦁ HSV is spread by direct contact with oral or genital lesions (risk is greatest if woman has active lesions with a vaginal birth) ⦁ Expected findings ⦁ Toxoplasmosis resembles flu like symptoms ⦁ Rubella symptoms include joint and muscle pain, rash, fever and possible fetal death ⦁ Cytomegalovirus can be asymptomatic or mono like symptoms ⦁ HSV has painful blisters, lesions and tender lymph nodes and can be fatal for fetuses ⦁ Nursing Care: Rubella immunizations are contraindicated for pregnant women because the pregnant women can develop an infection (avoid groups of children) ⦁ Medications: antibiotics and for toxoplasmosis treat with pyrimethamine and sulfadiazine (harmful to fetus but essential) ⦁ Education is focused on prevention and hand hygiene, safe cooking practices, safe sex and emotional support Therapeutic Procedures to Assist with Labor and Delivery ⦁ External Cephalic Version: Uses an ultrasound to externally manipulate the fetus into cephalic lie and is done around 36-37 weeks. High risk of placental abruption, umbilical cord compression and emergency C-section ⦁ Client Prep: Perform NST to evaluate fetus, ensure Rho(D) has was given at 28 weeks, admin IV fluid and tocolytics to relax uterus to permit easier manipulation ⦁ Ongoing Care: Monitor FHR, VS, watch for hypotension ⦁ Bishop Score: Determines maternal readiness for labor by assessing cervix ⦁ Five factors are assigned value 0-3, cervical dilation/effacement/consistency/position/station of presenting part ⦁ Client readiness should be 8+ for a multiparous client or 10+ for nulliparous client ⦁ Cervical Ripening: This increases cervical readiness for labor and can eliminate the need for oxytocin to induce labor ⦁ Used for clients who cervix fails to dilate and efface ⦁ Considerations: Assess for urinary retention, PROM, vaginal bleeding, fetal distress ⦁ Interventions: Side lying position, monitor VS and FHR ⦁ Complications: Hyperstimulation requires SQ of terbutaline, Fetal Distress requires O2/position client on left lateral side/increase IV fluid/Notify HCP ⦁ Induction of Labor: deliberately initiates uterine contractions chemically or mechanical means ⦁ Requirements: Bishop score of 8 for multiparous and 10 in nulliparous for 39 weeks gestation client ⦁ Considerations: Prep client for cervical ripening, possible use of oxytocin, anmiotomy or amniotic membrane stripping ⦁ Monitor VS and FHR/contraction pattern every 15 minutes and with every change in dose ⦁ Increase oxytocin until contraction frequency are more than 2 minutes or duration is longer than 90 seconds ⦁ Complications: Nonreassuring FHR (less than 110 or greater than 160 BPM) – must position into side lying, keep IV fluids open, notify HCP, monitor VS and FHR ⦁ Augmentation of Labor: Stimulation of hypotonic contractions once labor has started spontaneously but progress is inadequate ⦁ Amniotomy: HCP ruptures amniotic membranes using a hook, but increases client risk of cord prolapse or infection ⦁ Must make sure presenting part of fetus is engaged prior to procedure ⦁ Take temp every 2 hours and provide comfort measures ⦁ Amniofusion: Normal saline or LR are instilled into the amniotic cavity to help reduce the severity of variable decelerations caused by cord compression ⦁ Indications: Oligohydramnios or fetal cord compression ⦁ Interventions: warm fluid prior to administration, assess and monitor client/fetus frequently ⦁ Vacuum-Assisted Delivery: Used for maternal exhaustion and ineffective pushing, fetal distress during second stage of labor and only used for 34 week gestation and later ⦁ Position in lithotomy position, monitor VS and FHR ⦁ Can cause swelling of the scalp that disappears within 3-5 days (caput succedaneum) ⦁ Forceps Assisted Birth is used during prolonged labor and fetal distress labor ⦁ Position in lithotomy and ensure bladder is empty ⦁ Assess FHR during and after intervention, observe neonate for bruising and injuries from forceps as well as mother ⦁ Complications include lacerations of cervix/vagina/perineum, injury to bladder, facial bruising or injury to facial nerve on neonate ⦁ Episiotomy is an incision to the perineum made to enlarge the vagina (speeds up delivery and minimizes soft tissue damage) ⦁ Indicated to shorten second stage of labor, prevent cerebral hemorrhage of fragile preterm infant or help with a macrosomic infant ⦁ Two types of episiotomy: ⦁ Median (midline) episiotomy – most commonly used and is a cut from the vagina to the rectum ⦁ Mediolateral episiotomy – extends from the vaginal outlet posterolateral, either to left or right of the midline and is used when posterior extension is likely. ⦁ Greater blood loss, repair is more difficult, local anesthetic is administered ⦁ Alternate labor positions to reduce pressure on the perineum and promote stretching ⦁ Cesarean birth is a transabdominal incision made horizontally in the lower segment of the uterus and can be needed for many reasons: placenta previa, dystocia, multiple gestations, umbilical prolapse and more ⦁ Assess vitals, FHR, maintain IV fluids, ensure NPO prior to procedure ⦁ Monitor for infection and excessive bleeding post-op, tender uterus and foul smelling lochia can indicate endometritis, and encourage ambulation ⦁ Complications include aspiration, wound infection, hemorrhage, UTI, fetal injuries, etc ⦁ VBAC is a vaginal birth after c section previously ⦁ Mother must have no other uterine scars, 1-2 previous low transverse c-section births and adequate pelvis ⦁ Constantly asses vitals and FHR Nursing Care of Newborns ⦁ APGAR Scoring: Rules out abnormalities through an assessment done just after birth ⦁ HR: Absent 0 – Greater than 100 BPM 2 ⦁ RR: Absent 0 – Good Cry 2 ⦁ Muscle Tone: Flaccid 0 – 2 Well Flexed ⦁ Reflex Irritability: None 0 – 2 Cry ⦁ Color: Blue/Pale 0 – Completely Pink 2 ⦁ Expected Weight Ranges: ⦁ Weight: 2500 – 4000 g ⦁ Length: 45-55 cm ⦁ Head Circumference: 32 – 36.8 cm ⦁ Chest Circumference: 30 to 33 cm ⦁ Gestational Age Assessment: ⦁ New Ballard Scale: Newborn maturity rating scale that assesses neuromuscular and physical maturity ⦁ Vital Signs ⦁ RR: 30-60 breaths/min and short periods of apnea are normal (<15 seconds) ⦁ HR: 110-160 BPM ⦁ BP: 60-80 / 40-50 mm Hg ⦁ Temperature: 36.5 – 37.5 C (97.7-99.5 F) ⦁ Reflexes: ⦁ Sucking and Rooting: Expect to elicit by stroking the cheek or edge of the mouth, newborn will turn towards side that is touched (expected age: disappears around 3-4 months) ⦁ Palmar Grasp: Elicit by placing examiner’s finger in palm of newborn’s hand and fingers will curl around examiners fingers (expected age: lessens by 3-4 months) ⦁ Plantar Grasp: Elicit by placing examiners finger at base of newborn’s toes and newborn will respond by curling toes (age: birth to 8 months) ⦁ Moro Reflex: Elicit by allowing head and trunk of newborn in semi sitting position to fall backwards and newborn will symmetrically extend and then abduct arms at the elbows and fingers spread to form a C (age: birth to 6 month) ⦁ Babinski Reflex: Elicit by stroking outer edge of sole of foot and toes will fan up and outward (Age: birth to 1 year) ⦁ Stepping: Elicit by holding newborn upright with feet touching flat surface and they will respond with stepping movements (Age: birth to 4 weeks) ⦁ Diagnostic and Therapeutic Procedures Following Birth: Blood tests are done to determine Rh factor, blood type and evaluate for infection. ⦁ Expected Lab Values: ⦁ Hgb: 14 to 24 ⦁ Platelets: 150,000 to 300,000 ⦁ Hct: 44-64% ⦁ Glucose: 40-60 ⦁ RBC Count: 4.8 ⦁ Bilirubin: ⦁ 24 hours: 2-6 ⦁ 48 hours: 6-7 ⦁ 3-5 days: 4-6 ⦁ Leukocytes: 9,000 to 30,000 ⦁ Complications ⦁ Airway obstruction R/T Mucus: Use bulb syringe or gentle chest percussion ⦁ Hypothermia: Monitor for temp changes and place in warmer if needed ⦁ Inadequate oxygen supply R/T obstructed airway, poor functioning cardiopulmonary system or hypothermia ⦁ Bulb Syringe ⦁ Mouth first, then nose ⦁ Depress, then insert into one side ⦁ Avoid center – may stimulate gag reflex ⦁ If unsuccessful, back blows, chest thrusts, or mechanical suctioning may be used CAM (Complementary & Alternative Medicine) ⦁ What is Complementary? ⦁ “In addition to…” modern medicine ⦁ What is Alternative? ⦁ “Instead of…” modern medicine ⦁ Define “Chi” ⦁ Chinese life force that provides warmth and protection from illness and injury. ⦁ Reiki ⦁ Use of hands to correct energy fields/chakras. Energy flows from universe into patient. Can help increase WBC and RBC production. Realignment of energy flow. ⦁ Ayurveda ⦁ Indian medicine. Preventive medicine that teaches health is balanced by nature, body, mind and spirit. Uses oils, diet, senses and behavior. ⦁ Guided Imagery ⦁ Focusing on an image either created by the therapist or by the patient’s mind. Uses all 5 senses. S/E are sleepiness and extreme relaxation. ⦁ Biofeedback ⦁ Uses thoughts to control physiological body responses. Electrodes are placed on patient to monitor body response to stress. Patient then relaxes those areas during times of pain, anxiety, temperature, HTN, TMJ, H/A, etc. Stroke ⦁ What test needs to be done right away when a stroke patient comes to an ER? ⦁ CT SCAN immediately! This will help determine what type of stroke has occurred. ⦁ CT doesn’t require NPO status or any contrast. Results are immediate. ⦁ A patient started having a headache at 4am and started slurring their speech around 0415. If they do, in fact, have an embolic stroke, how long is their window to be able to get TPA? Hint: First symptom was the headache. ⦁ “Golden 3-Hour window” from the “last time normal” to the time the TPA is administered. ICP ⦁ ICP is… ⦁ Intracranial Pressure (pressure within the skull) ⦁ A normal ICP is… ⦁ 7-15mmHg ⦁ What things increase ICP? ⦁ Anything that makes your face RED increases ICP ⦁ Blowing nose, sneezing, lowering HOB, swelling (tumors, stroke, meningitis, etc.). ⦁ Elevating the HOB improves venous drainage and decreases ICP ⦁ What do hypertonic saline and Mannitol do for ICP? ⦁ Mannitol: takes ICP fluid to kidneys for removal ⦁ Hypertonic Saline: pulls fluid from the tissues into the bloodstream, such as burns, ICP and post-op to reduce swelling. ⦁ Why is clustering a bunch of activities together for a patient with increased ICP a bad idea? ⦁ This can increase ICP. Therefore the nurse must decrease stimuli and maintain a calm, low noise, low light, and stress-free environment. ⦁ Why is giving a stool softener a good idea? ⦁ We don’t want these patients to STRAIN with their bowel movements, as it will increase ICP. ⦁ What are the early indicators of increased ICP? What are the late indicators? Early Indicators Late Indicators H/A (usually BAD and prolonged) N/V Blurry Vision Pupillary changes Cheyne Stokes (from lack of O2 to brain) Widening Pulse Pressure (sys-dys=pp) Bradycardia Bulging Fontanels (in infants) Irritability (in infants) ⦁ What is Cushing’s triad and what does it tell you? ⦁ Indicates LATE increase in ICP ⦁ BAD NEWS! ⦁ Symptoms Include: ⦁ Bradycardia ⦁ Widening Pulse Pressure ⦁ Cheyne Stokes (changes in respirations) ⦁ What are the bad posturing poses we talked about and what might they indicate? ⦁ Decerebrate Posturing ⦁ Pointed toes, arms down, wrists are flexed out ⦁ Decorticate Posturing ⦁ Everything is pulled towards the core These indicate severe brain swelling from ICP. Liver ⦁ Know your liver labs ⦁ ALT: 3-35 IU/L or 8-20 units/L ⦁ AST: 5-40 units/L ⦁ ALP: 30-120 units/L ⦁ Bilirubin: 0.1-1.0 mg/dL ⦁ PTT: 11-12.5 sec ⦁ INR: 0.7 – 1.8 ⦁ Hemoglobin: 12-18g/dL ⦁ Platelets: 100,000 – 400,000 ⦁ Ammonia: 15-45mcg/dL (or 11-32 umol/L) ⦁ Creatinine: 0.5-1.2 mg/dL ⦁ Albumin: 3.5 – 5.0 g/dL ⦁ Potassium (K+): 3.5-5.5 meq/L ⦁ What is going on with lab levels in Liver Dysfunction? Levels that are going UP Levels that are going DOWN ALT AST ALP Bilirubin Creatinine Ammonia PTT/INR (prolonged) Hemoglobin Platelets K+ (initially) Albumin ⦁ What do you give to reduce ammonia levels? ⦁ Lactulose ⦁ Initially, potassium can be very low in liver failure, but it gets tricky later on in the disease as kidneys are affected. ⦁ Why are liver failure patients at such great risk for bleeding? What labs reflect this problem? ⦁ Liver is highly vascularized ⦁ LOTS of blood vessels! ⦁ Hepatitis A, B, and C: What are the symptoms, and how are they spread (vowels versus consonants). Hep A Hep B Hep C Symptoms: Mild, flu-like sx Spread: Fecal – Oral Route Contaminated food/water, Shellfish Symptoms: anorexia, N/V, jaundice, fever, rashes, light colored stool, dark urine Spread: Blood – Body Fluids Sex, healthcare workers, needles, drug users, hemodialysis pts., babies Symptoms: Flu-like sx (can be severe) Spread: Blood – Body Fluids, IV drug users, Mobility ⦁ CMS, CMS, CMS: This is VERY IMPORTANT IN FRACTURES. What does it stand for and how do you measure it? ⦁ CMS stands for: Circulation, Motion, Sensation ⦁ Circulation: pulses, capillary refill ⦁ Motion: can they move? ⦁ Sensation: N/T, feeling ⦁ RICE: What is it? What do we use it for? (almost all injuries, right)? ⦁ RICE stands for: Rest, Ice, Compression, Elevation ⦁ Helps prevent swelling. Vasoconstriction. ⦁ Hip Surgery. Knee Surgery. What are the risks? What things do you assess for? Why? ⦁ Circulation, sensation and motion distal to the affected area. ⦁ PT is at risk for: DVT, wound infection, hematoma, hip dislocation, and neurovascular compromise. ⦁ What is the difference between an open or closed fracture? What do you place on an open fracture? ⦁ Open Fractures: skin is broken, bone is showing ⦁ Cover with a sterile saline soaked gauze dressing ⦁ Stop the bleeding. Analgesia, ABX, Tetanus shot ⦁ Immobilize & elevate ⦁ Closed Fractures: skin is still intact. Bone does NOT penetrate skin. ⦁ Do you use a cold pack (ice) and the rest of RICE with a fracture? ⦁ YES! Absolutely! ⦁ What is compartment syndrome and what would you assess if it was compartment syndrome? What are the risks to your kidneys (condition that starts with an “r”)? ⦁ Compartment Syndrome: ⦁ Swelling in tissues that compromises perfusion ⦁ Monitor for the 6P’s ⦁ Pain ⦁ Paresthesia ⦁ Paresis ⦁ Pressure ⦁ Pallor ⦁ Pulse ⦁ First sign is Extreme pain disproportionate to the injury, along with change in sensation distal to the affected compartment ⦁ Can be prevented by… ⦁ Reducing bleeding and inflammation to site of injury. For fractures this could be traction, early splinting, early immobilization, elevation of the limb TO THE LEVEL of the heart (NOT above it!). ⦁ Rhabdomyolysis can adversely impact the kidneys because of all the breakdown of the muscles and the myoglobin into the blood. Electrolytes & Fluid ⦁ K+ normal values? 3.5 – 5.5 meq/L Hyperkalemia Hypokalemia Twitches and contractions Cramping, irritable Hyperactive bowel Peaked T Wave Weak, slowing things down Fatigue, decreased respirations Flat T Wave ⦁ Na+ normal values: 135-145 mg/dL Hypernatremia Hyponatremia Dehydration Symptoms! Dry mucous membranes, poor skin turgor, hypotension Thirst Neurological Symptoms/BRAIN! Confusion, coma, changes in LOC JVD, bulging fontanels, H/A Excess water accumulation ⦁ Ca+ normal values: 8.5 – 10.5 mg/dL Hypercalcemia Hypocalcemia Weak, slowing things down Fatigue, hyporeflexia, coma Hypoactive bowel sounds Twitches and contractions Chvostek’s Sign Trousseau’s Sign Tetany, diarrhea, cramping ⦁ What is Chvostek’s sign and what does it indicate? ⦁ Cheek spasms when touched ⦁ Indicates: Low Ca+ (Hypocalcemia) ⦁ Easy Way to Remember Electrolytes & What they do Twitches & Contractions Slowing things down/Weakness HIGH K+ LOW Ca+ HIGH Phosphate- LOW K+ HIGH Ca+ LOW Phosphate- Oxygenation ⦁ Why does a person have poor oxygenation when their hemoglobin is low? ⦁ Hemoglobin is the O2 carrying molecule. Low Hgb = decreased 02 carrying capacity ⦁ What’s the difference between hypoxia and hypoxemia? ⦁ Hypoxia: lack of 02 to the brain/tissues. Measured by Pulse Oximetry. ⦁ Hypoxemia: Decreased level of oxygen in the arterial blood as measured by the PaO2. ⦁ What are the symptoms of hypoxia? Just remember, these symptoms could be implicated in an “ABC type” question. ⦁ Tachycardia, confusion, restless, irritable, anxiety, orthopnea, irregular breathing, use of accessory muscles to breathe. Acid/Base Balance ⦁ Normal Levels ⦁ pH: 7.35 – 7.45 ⦁ PaCO2: 45 - 35 ⦁ HC03: 22 - 26 ⦁ Interpret this ABG: pH 7.25 PaCo2 39 HCO3- 9 ⦁ Metabolic Acidosis, Uncompensated ⦁ Interpret this ABG: pH 7.39 PaCo2 39 HCO3- 26 ⦁ Normal ABG ⦁ What causes imbalances in the body ⦁ Respiratory (PaCO2) Acidosis Alkalosis “You cannot blow out your acid” Holding your breath Anesthesia/sedation Decreased respirations/COPD “Blowing out too much acid” Hyperventilation ⦁ Metabolic (HC03) Acidosis Alkalosis “Shitting out your base” Diarrhea Dehydration “Puking out your acid” Vomiting Suctioning Using too much Antacids Cancer ⦁ Primary, Secondary, and Tertiary Prevention ⦁ Primary: Reducing your risk of cancer. [Ex: vaccines, diet changes, exercise, quit smoking, decrease ETOH intake, using sunscreen, decreasing # of sexual partners.] ⦁ Secondary: Early Detection. [Ex: Blood Pressure monitoring, along with yearly screenings: Pap smear, self-breast/testicular exams, mammograms, colonoscopies, flex sig., etc.] ⦁ Tertiary: Prevention of Recurrence. [Ex: reducing disability from cancer, minimizing S/E, increasing maintenance, and preventing it from happening again.] ⦁ What’s normal after each of the chemotherapies? ⦁ Nausea, vomiting, pain, skin reactions, fatigue/malaise ⦁ Mucositis (inflammation/ulceration of the mouth & GI tract) ⦁ Cachexia (breakdown of muscle mass) and anorexia ⦁ Cognitive changes/memory impairment/hard time finding the right word (“chemo brain” for up to 2 years after treatment, caused by Tamoxifen), neuropathy (usually reversible if caught early) ⦁ For “chemo brain”, use post-its, calendars, reminders on your phone, write notes to yourself. Give the patient control/empower the patient over the situation when you can. ⦁ What are the cardinal signs of cancer? ⦁ What are normal values for… ⦁ ANC (Absolute Neutrophil Count): Over 2,000. Anything under 2,000 is considered Neutropenia. ⦁ If low, need to implement Neutropenic Precautions & Private Room (Positive Pressure) ⦁ WBC: 5,000 – 10,000 ⦁ If low, patient is at increased risk of illness and inability to fight that illness. For BMT patients, this could indicate Graft vs. Host disease. Also BMT patients may take a long period to regenerate blood cells and can put them at increased risk of infection. ⦁ Temp: Over 100.4 + indicates a “fever” ⦁ If high, tells us body is fighting an infection/illness and that the nurse needs to further investigate ⦁ Prostate Specific Antigen [PSA] ⦁ What does it mean as a marker? Given off by the tumor or by the normal tissues in response to the presence of the tumor. ⦁ What does it mean when it goes up or down? ⦁ PSA [goes up] means that cancer/tumor is not responding to treatment or it has metastasized. ⦁ PSA [goes down] means that the cancer/tumor is responding to treatment. ⦁ Nausea ⦁ Anticipatory: sx appear earlier than expected. Sx also appear in those receiving radiation therapy. ⦁ Acute: occur within 24 hours after chemotherapy has begun. ⦁ Delayed: occurs more than 24 hours after chemotherapy has begun. ⦁ What kind of medications can you give for nausea (#1 complaint)? ⦁ Zofran (ondansetron), Reglan (metoclopramide), Ativan (lorazepam), Benadryl (diphenhydramine) ⦁ Marinol (Cannabinoids, Cannabis) ⦁ Dexamethasone (helpful for anorexic patients) ⦁ Dronabinol (Marijuana) ⦁ Peppermint Oil ⦁ Acupressure at the wrists help with nausea (Sea Bands) ⦁ Define Cellular Regulation ⦁ Normal production/replication of cells (Mitosis/Meiosis is normal). ⦁ Cancer cells have uncontrolled replication. They lack contact inhibition (which means they outgrow their borders). They also lack fibronectin and do not stick together. They have unorganized DNA/chromosomes (aneuploidy) ⦁ Go over and understand/apply the TNM system ⦁ Brachytherapy (Internal Radiation): radioactive pieces placed in the patient near the site of cancer/tumor. ⦁ Nurse has to let patient know that they (nurse, family, friends, etc) will be limiting their time with the patient to decrease their own exposure to radiation. ⦁ Maintain 6ft distance from patient ⦁ Keep lead lined container within the room incase radioactive piece becomes dislodged. Thrombocytopenia ⦁ What is it? It is a PLATELET count less than 100,000 (normal levels are 150,000 – 300,000) ⦁ Watch for bleeding/hemorrhage and bruising Palliative Care ⦁ The goal of palliative care is to make the patient more comfortable and make their transition a better experience. Disaster Management ⦁ How is mass casualty triage different than regular triage? ⦁ Focus is on those most likely to survive (Reds & some Yellows) ⦁ Prioritize mass casualty victims ⦁ Green: patients need minimal healthcare ⦁ Yellow: patients who need care, but not immediately ⦁ Red: patients who need care immediately & are life threatened ⦁ Black: patients who will most likely die, even with interventions ⦁ ABC’s with assessments. ⦁ CAB’s with interventions. Cardiac Telemetry Normal Sinus Rhythm Sinus Bradycardia Sinus Tachycardia SVT HR 60-100 bpm “P” Wave present HR under 60bpm HR over 100bpm No “P” Wave, Narrow QRS. Electrical impulse occurs in tissue above the ventricles. No Tx Needed Tx: Atropine Tx: treat the cause Tx: Adenosine (have crash cart near) Atrial Fibrillation Atrial Tachycardia Ventricular Fibrillation Ventricular Tachycardia Irregular QRS complex. Caused by Coronary Heart Disease, HF, alcoholism, hyperthyroidism, etc. *MOST COMMON in older adults* Impulses originate in Atrial Tissue outside the SA node (“the focus”). Assess for Digoxin toxicity & K+ levels. Wobbly ventricle. Very close to death. Happens due to MI, K+ imbalances, drug toxicity, and electrocution. Wide QRS Complex. Happens when consecutive PVC’s occur. HR 100-250bpm. Tx: Pt on Coumadin to prevent clots Tx: Synchronized Cardioversion Tx: Immediate AED & CPR Tx: Cardioversion if non-responsive. If no HR, start CPR & AED. Amiodarone is drug of choice. ⦁ What is normal CVP? ⦁ Tells us how much blood is returning to the heart ⦁ Tells us the ability of the heart to pump blood into the arterial system ⦁ Normal Value: 4-10mmHg ⦁ What makes it high? ⦁ Right Ventricular Failure ⦁ Hypervolemia (volume overload) ⦁ What makes it low? ⦁ Sepsis (per Sarah Grace in class) ⦁ Hypovolemia (volume deficit) If my patient has something wrong on their monitor, I do the following steps: Assess Diagnose, Plan, Intervene, and Evaluate. MI/Heart Attack ⦁ What are the interventions for a patient with an MI? ⦁ 12-Lead EKG (quickly able to diagnoses damage or disease if patient presents with chest pain) ⦁ First 24 hours after MI is highest risk of death & cardiac tissue death ⦁ Emergency Management of Chest Pain (Mnemonic: MONAH) ⦁ Morphine IV ⦁ Oxygen ⦁ Nitro ⦁ Aspirin ⦁ Heparin ⦁ If you have a patient with all the signs and symptoms of an MI, can they still have an MI (a silent MI)? Why do these things happen? ⦁ Yes, especially in the elderly. Since they are missing that classic symptom of chest pain, they often delay coming to the Emergency Department. ⦁ What’s the most convenient screening tool to determine if the patient is having an MI or determine whether it is a STEMI or NON-STEMI? ⦁ 12-Lead EKG (quickly able to diagnoses damage or disease if patient presents with chest pain) ⦁ What is an ECG? Why is it the most important of screening tools? ⦁ Electrocardiogram ⦁ Assesses presence and location of tissue ischemia (tissue death) ⦁ Assesses the ability of the heart walls to contract or relax. ⦁ What is a troponin? ⦁ What is a normal value? ⦁ <0.01ng/mL ⦁ Why is this helpful in evaluating unstable angina? ⦁ Tells us if there is cardiac damage following a MI. It is a protein released into circulation with heart muscle injury. ⦁ Why is a stress echo important? ⦁ It is helpful to compare the heart at rest, versus in motion and detects any wall abnormalities due to motion. ⦁ What is the prep for a stress echo? ⦁ Do not eat immediately before the stress echo (risk of N/V) ⦁ Why is ongoing telemetry used with unstable angina? ⦁ To monitor the patients and detect significant arrhythmias or abnormalities. ⦁ Cardiac (continued) ⦁ Cardiac Output = SV x HR ⦁ Why does the HR go up in Hypovolemia? ⦁ Body is trying to compensate for lack of fluid (perfusion) to the rest of the body so it increases the HR to get better perfusion. ⦁ Know the flow of electricity through the heart: ⦁ SA Node AV Node Bundle of HIS Right and Left Bundle Branches Purkinje Fibers ⦁ What is conductivity? ⦁ The ability of the cardiac cells to transmit an impulse. ⦁ Renal ⦁ Define Chronic versus Acute Renal Failure ⦁ Acute: sudden loss of kidney function ⦁ Chronic: overtime, gradual loss of kidney function. ⦁ What is Creatinine? ⦁ Normal Value: 0.5 – 1.2 mg/dL ⦁ Tells us the rate at which the kidneys are able to clear Creatinine from the blood ⦁ What is BUN? ⦁ Normal Value: 5-20 mg/dL ⦁ Tells us the kidney’s ability to excrete ⦁ What is pyelonephritis ⦁ Kidney infection/inflammation from bacteria that traveled up from the ureters. Sometimes a complication of a bladder infection/UTI. ⦁ Burns ⦁ Remember that we need to rehydrate burns. Why? ⦁ We need to rehydrate burns to establish perfusion to burn site ⦁ Massive amounts of fluid are shifting and also evaporating from the burn, edema formation, ect. ⦁ Remember that we need good nutrition to heal burns. Why? What nutrients are important for this? ⦁ Protein (check albumin levels, should be 3.5 or above) ⦁ Calories ⦁ Carbohydrates ⦁ Fats ⦁ Small, frequent feedings ⦁ If there is a circumferential burn of the neck, what will need to happen to ensure that this person continues to ventilate? ⦁ INTUBATE!!! ⦁ What is the Parkland formula and what does it represent? ⦁ 2ml to 4ml x Kg x % burn = fluid replacement need ⦁ Applies to the first 24 hours after a burn ⦁ What is the best indicator of perfusion in patients who have sustained a burn? ⦁ URINE OUTPUT ⦁ What electrolytes may be “off-kilter” in a burn? ⦁ Metabolic Acidosis ⦁ Hematuria, Myoglobinuria (protein breakdown) Labs (Increasing Values) Labs (Decreasing Values) Potassium (K+) Hemoglobin (Hgb) Hematocrit (Hct) Creatinine clearance Fluid Volume/Hypovolemia Fibrinogen Platelets WBC NA+, Albumin, Immunoglobulin Nitrogen Balance ⦁ First Degree ⦁ Superficial-Partial Thickness ⦁ Epidermal Layer affected ⦁ Symptoms: erythema, minimal edema, pain & blanching. NO blisters. ⦁ Ex: Sunburns, UV light ⦁ Second Degree ⦁ Deep-Dermal/Partial Thickness ⦁ Epidermis & Dermis affected ⦁ Symptoms: erythema, oozing, blisters, pain, shiny Sub-Q tissue shows after blisters pop. ⦁ Ex: Touching Hot Solids/Liquids, direct flames ⦁ Third/Fourth Degree ⦁ Full-Thickness Burn ⦁ Epidermis, Dermis, Sub-Q, Nerves, Muscles & Bone are burned ⦁ Symptoms: Eschar, little or no pain, edema, deeply charred tissue and bone. ⦁ Rule of Nines: ⦁ Death & Dying ⦁ Review the cultural table: You will need to know Table 7-1, p 113-114 Living Will Advance Directive that allows a person to determine what medical treatment they want or do not want to have. (Ex: mechanical ventilation, tube feedings, hydration, etc.). Medicare Hospice Benefit Benefits paid for by the federal government for hospice services. Available to those with 6 months or less to live. Palliative care Pain relief and enhancement of quality of life when treatment options have been exhausted. Physical Dependence Can develop when a person receives several doses a day of an opioid medication for two weeks or more. The medication is gradually withdrawn to avoid withdrawal symptoms. Physician Assisted Suicide The enabling or assisting of death by a physician in consultation with a terminally ill patient. Power of Attorney for Health Care (POA) Person appointed to make decisions about healthcare for a person if they have lost the decisional capacity to do so on their own. Terminal Illness Is one in which there is no possibility for a cure, resulting in the decline of the patient’s physical condition and then death. Anticipatory Grief Emotional response and behaviors by those who will be affected by the patient’s death. Preparing for the ultimate loss of a loved one. Cheyne-Stokes Breathing Fast & deep breathing followed by apnea and then fast & deep breathing resume again. Agonal Breathing Gasping or labored breathing, which happens right before death. Advanced Directives Written documents that allow a person to state in advance specific decisions about how they want their healthcare managed if they are incapacitated or unable to communicate Bereaved The people/person who are mourning a loss Do Not Resuscitate (DNR) An order stating that the patient does not want CPR in the event that the patient’s heart stops beating. Tips: Providing a place close to a dying patient (even in a code) provides comfort for the family. They may need a chair next to the room. Better outcomes are seen in coping skills if people are able to see the event, say, from a chair you provide right outside the door for a grown-up or allowing a child to be held after death. Shock What is a normal lactic acid? ⦁ 4.5 to 19.8 mg/dL (0.5 to 2.2 mmol/L) Why does someone have a high lactic acid when they are hypovolemic? Or in any shock for that matter…. ⦁ Because lactic acid is produced during anaerobic (without 02) metabolism and during shock, there is a lack or decreased 02 level to cells. What is Shock? Decreased oxygenation to the tissues/decreased perfusion Cells go into “Panic Mode” Imbalance between O2 supply to the tissues/organs and the O2 demand of those items. Stages of Shock Initial Stage (decreased CO & impaired tissue perfusion R/T anaerobic metabolism & lactic acid production.) Compensatory (body starts to initiate compensatory mechanisms via the SNS – Sympathetic Nervous System) Multiple Organ Failure (every body system is affected and MOD happens) Refractory (body will no longer respond to therapy) Types of Shock, Causes & Interventions Distributive Anaphylaxis - Hypersensitivity response due to an antigen-antibody reaction. Symptoms ⦁ Vasodilation, broncho-constriction & inflammation ⦁ Stridor, wheezing, Rales & rhonchi ⦁ Hypotension ⦁ Tachycardia, decreased CO ⦁ N/V, diarrhea ⦁ Pruitis/uticaria ⦁ Complaints of feeling itchy, warm, abdominal cramping, pain & dyspneic Nursing Interventions ⦁ Epinephrine ⦁ Benadryl ⦁ Solu-Medrol ⦁ Watch airway (assess for hoarseness, stridor & dyspnea = laryngeal edema) ⦁ Assess swelling Neurogenic - Caused by suppression of SNS. Anything that disrupts the signal to the hypothalamus or that blocks outflow of the Sympathetic responses. Common following a spinal cord injury at T6 or above. Vessels end up getting bigger & less blood goes back to the heart. Symptoms Hypotension (CVP goes down) Bradycardia Temperature dysregulation (results in heat loss) Dry skin Poikilothermia (taking on the temperature of the environment) Nursing Interventions Dopamine (inotrpoin) Vasopressin (ADH hormone) Vasopressors (ephedrine, norepinephrine) Phenylephrine (for those who do not respond adequately to dopamine) “Rider” is NS just to keep the vein open and run meds in Septic - Caused by Gram Negative Bacteria, Systemic infection Iatrogenic (caused by healthcare interventions such as Central Lines) Nursing Interventions for Septic Shock Fluids & Vasopressors (vasoconstrictors help increase the BP) Norepinephrine is the drug of choice for Vasopressor Antibiotics (usually more than 1) TED Stockings for DVT prevention Semirecumbent positioning Monitor Labs Lactic Acid ⦁ HIGH – if perfusion is bad ⦁ LOW – if perfusion is getting better Monitor K+ and other electrolytes WBC (will be high in this type of shock) CRP (will be high) Temperature (will be high) Dialysis can help regulate BP on patients who are Septic Cardiogenic - Something is wrong with the pump (heart) Failure of the left, right or both of the ventricles which results in a failure to pump out blood Can be precipitated by a MI, irregular HR or cardiomyopathy. CHF exacerbations. Symptoms Hypotension (less than 90 systolic) Tachycardia (HR over 100bpm) Tachypnea Weak, thready pulse. Diminished heart sounds. Chest pain. Decreased CO. Dysrhythmias. Cool, pale, moist skin. Mottling. Poor capillary refill. Urine output less than 30ml/hr. Decreased kidney function. Crackle breath sounds Change in LOC Nursing Interventions Provide supplemental O2 PRN. Prepare to intubate & vent patient. Low-dose Morphine (helps open up blood vessels, also with pain & anxiety) Maintain bed rest, decrease anxiety, fear and pain levels Position the patient for maximum chest excursion & comfort Give Diuretics and/or vasodilators (nitro) to reduce circulating volume Give Dobutamine (will increase CO by making a more forceful contraction) Obstructive - Anything that causes a blockage of blood/oxygen Pulmonary embolism Cardiac Tamponade (increased pressure in the pericardial sac) Pneumothorax that presses on the heart Atrial tumor or clot Hypovolemic Absolute Hypovolemia Loss of large amount of blood or fluid (hemorrhage, severe dehydration, stab/gunshot wound) Body tries to compensate by increasing respirations, HR and depth of respirations. Vasoconstriction occurs to bump up the BP. The body can compensate for up to 750ml of blood. Symptoms Changes in LOC, confusion, disoriented, restless, anxious, irritable Tachypnea & Increased depth of respirations Tachycardia Chest pain Decreased urinary output Delayed capillary refill, cool/pale skin Flat jugular veins Nursing Interventions Control the bleeding Restore fluids (insert an IV) Vitals Assess fluid status Monitor Labs: Hemoglobin, Hematocrit, & WBC’s Comfort measures (calm environment, limit activities, reduce anxiety) Patient Positioning Modified Trendelenburg (patient’s legs should be elevated w/trunk flat & head and shoulders above the chest) ARDS (Acute Respiratory Distress Syndrome) What is it? The alveoli fill with fluid which minimizes/inhibits gas exchange Inflammation in Lungs & abnormal coagulation issues Inflammation & coagulation go hand in hand Nursing Interventions Treat the cause Treat the inflammation Promote Gas Exchange (mechanical ventilation management) Monitor ABG’s SIRS (Systemic Inflammatory Response Syndrome) - Similar to ARDS, but it happens within the entire body Can be initiated by Sepsis MODS (Multiple Organ Dysfunction Syndrome) - Can result from ARDS, SIRS or even Sepsis The organs are shutting down DIC (Disseminated Intravascular Coagulation) - Something happens where you use up all of your platelets and clotting factors and you have nothing left so you bleed out. Hard to revive these patients Nursing Interventions Do NOT give any medications via IM. Use another method! Do NOT place a Foley catheter if it is not already there NO razors or sharp objects. Change positions slowly Do not strain during BM’s. Avoid constipation. Metabolism What is pheochromocytoma? Pathophysiology Adrenal medullary tumor Leads to irregular secretions of epinephrine and norepinephrine Symptoms: Intermittent attacks of: H/A, palpitations, profuse sweating, and increased BP Nursing Considerations: Remove the tumor, chemotherapy to remove tumor cells Radiotherapy to destroy tumor cells Medications to control the sx of the disease What is SIADH? Symptoms: Confusion, H/A (not relieved by analgesics), and lethargy. Cerebral edema, Hyponatremia. Slow reflexes, weight gain, personality changes, muscle changes, N/V, and diarrhea. Pathophysiology: Hypersecretion of ADH (even when the patient is not hypovolemic) Nursing Considerations: Fluid restriction (600-1200ml/day) Monitor non-liquid fluid intake Administer NaCL 3% for Hyponatremia Neurological checks What is Diabetes Insipidus? Symptoms: Excessive thirst, increased urinary output (polyuria) can result in dehydration Treatment: Indomethacin (anti-inflammatory) HTZ & Amiloride (diuretics) ATI – RN Comprehensive Online Practice 2016 A A newborn receives Vit. K at birth to help prevent bleeding. Administering enteral feedings via an NG-tube, the nurse should keep the HOB elevated at 45degrees for an hour after feeding to reduce the risk of aspiration. Foods high in Vit. A = 1 medium raw carrot (2,025 mcg/dL) (spinach, squash, & cantelope have an avg of 600 which is much lower) Delegation: UAP (collection of stool specimen, bed preparation) LPN: can insert NG Tube (cannot admin. RBCs/blood) Pre-surgical signing of informed consent: only if the client can accurately describe the upcoming procedure (if the client has been explained the procedure by the doctor, a nurse cannot assume the client understands the information) A client is receiving TPN (Total Perenteral Nutrition) solution by IV Infusion at 60mL/hr. The Nurse notices the pump has stopped working. What should the nurse do? Provide Dextrose 10% in water solution using manual drip tubing at 60mL/hr until new pump is available (TPN can only be administered by Infusion Pump) ** Patients receiving TPN Tx should have frequent blood glucose checks to monitor for potential hyperglycemia d/t dextrose in TPN solution. A client with schizophrenia is taking chlorpromazine: The greatest risk for injury to this client is neuroleptic malignant syndrome which Sx include: high fever, dysrhythmia, & decreased level of consciousness) Administering ear drops to school age child: pull pinna UPWARD & BACK for children 4+ age. For children 3 & under, pull pinna DOWNWARD & BACK. Autonomic Dysreflexia Sx: Facial Flushing, Nasal Congestion, & H/A Cranial Nerve II (CNII) deficit: Visual Impairment Appendicitis Pain location: McBurney’s point – LRQ Thrombocytopenia: Low platelets = increased bleed risk. Avoid venipunctures. Newborn immediately after birth = Dry immediately to minimize cold stress. Newly admitted newborn into nursery has pink body/blue feet: coloring is normal. Normal temp. range is 97.7- 100F. Stage II Pressure Ulcer: Partial thickness skin loss/blister. Infectious Gastroenteritis precautions: top priority is to restore fluid volume deficit (dehydration). The nurse would initiate oral rehydration that contains: sodium, potassium, chloride, citrate or bicarbonate,& glucose. Client suffering from recent stroke needs to go to the bathroom: the nurse should assess for functional limitations so he/she can get necessary help for transfer/ambulation. Client with schizophrenia have speech alteration associating with clang association A couple suffering from unsuccessful pregnancies for over a year: nurse should offer support groups to couple. Toddler Snacks: steamed carrots bcuz they are soft and don’t present a choking hazard. Hep A education precautions to client: wash all kitchen counter tops with 1:100 concentration chlorine/bleach Tracheostomy care in order: Remove Inner Cannula, remove soiled dressing, clean stoma with sterile saline, change trach collar. Patient discharge teaching about Warfarin: report to HCP if patient has red, black or tarry stools (could indicate bleeding) Manic Phase of schizophrenia: client will exhibit grandiose thoughts/behavior. Fluoxetine adverse effects to report to HCP: Tremors – can indicate serotonin syndrome 2-72 hours after Tx begins. (Tremors, agitation, confusion, anxiety, & hallucinations) Cardiac Tamponade Sx: Pulsus paradoxus (having a systolic bp 10mmHg or greater on inspiration than expiration, along with JVT, bradycardia, hypotension) Decreased Lung Expansion = a physiological change with aging d/t decreased mobility of ribs. Life threatening complication of fractures = Upper Chest Petechiae (indicate client is at risk for Fat Embolism Syndrome) Nutritional Teaching for a client with myasthenia gravis: Small bites/eat slowly, choose snacks high in calories. Foodborne Botulism = reportable to the CDC Alprazolam = a nurse should initiate fall precautions bcuz med can cause hypotension, dizziness, fainting upon rise, & drowsiness. Hemolytic Blood Transfusion reaction = low back pain Kawasaki disease acute phase Sx: fever unresponsive to antipyretics Cystic Fibrosis concern: Hemoptysis greater than 250mL/24hr indicate hemorrhage risk. Fetus in the Left Occiput Anterior position(LOA) position: the nurse will assess heart sounds at the LLQ. Adult client in PACU after general anesthesia: a stridor indicates an obstruction and the MD should be notified asap. Care for immobile clients = Nurse should use trochanter rolls to prevent external rotation/abduction of the hips which will maintain correct body alignment. Oxygen toxicity Sx: Bradypnea Diabetic Insipidus: Nurse must monitor for Polyuria. Increased urine output more than 4L/day results from decrease in deficiency of anti-diuretic hormone. UAP delegation: UAPs can take BP before and after medication administration. When mixing Regular Insulin with NPG Insulin= Inject units of air needed for NPH(cloudy) insulin into the NPH vile WITHOUT touching the insulin. Then inject air into the Regular Insulin(clear) as needed and remove nec. Insulin amount. Orthostatic Hypotension: can happen from people with fluid volume deficit d/t low blood volume from dehydration. Black tags in ER settings d/t a disaster: used to identify those patients who aren’t likely to survive or will need significant costs to potentially save life. Slurred speech & extremity weakness following a cardiac catheter procedure could indicate: stroke, which is a potential complication of cardiac catheter. RA Tx for pain/swelling in multiple joints = allow for frequent rest periods throughout the day. Balance rest/exercise. Disaster management includes: prevention, preparedness, response, and recovery stages. Vaso-occlusive sickle anemia crisis Sx = Hematuria (ischemia of the kidneys) Trach. Care suctioning = only suction for 10 seconds to minimize oxygen loss Methadone = Sedation and drowsiness are common side effects of this medication. Medical equipment working incorrectly, the nurse should: complete an incident report and occurrences During pregnancy, a food to avoid over concerns of listeriosis would include: Salami and other lunch meats. Saw palmetto herbal supplements: can result in false low PSA levels (delaying cancer diagnosis) True Labor during pregnancy = the cervix transitions to an anterior position. Suicidal clients: social isolation is a concern. Clozapine (schizophrenia med): can cause agranulocytosis. Low WBC counts contraindicate taking this med. Delirium Sx: Rapid speech Digoxin Toxicity Sx: Nausea Misoprostol side effects include inducing of uterine contractions. Women should have pregnancy test prior to taking med. Tunneled central venous catheter = an adolescent should keep line clamped (d/t no valve on line) to prevent backflow. Post-Op c-section monitoring = LLQ unilateral pain could indicate a DVT Anti-Social personality = shows lack of remorse Client post-partum with boggy uterus and heavy loci, the nurse should: massage the uterus to expel clots Another nurse witnesses another nurse charting something that nurse didn’t do: Gather more information about the nurses actions is 1st action. A post op client refusing to ambulate: the nurses 1st action would be to assess pain status. Fire in patients room: “RACE” Remove client, Activate alarm, Call for help, alert others of danger. Acupressure bands on wrists = good alternative therapy for N/V Troponin T = Myocardial muscle protein released into the blood stream after a MI. Post op tonsillectomy: the nurse should position clients in the lateral or prone position w/ head lower than chest to avoid aspiration of saliva/blood from surgical site. Abruptio Placenta Sx: persistent uterine contractions, board like abdomen, and red vaginal bleeding. Lithium Carbonate for Tx of Bipolar Disorder: monitor patient for confusion. Head to toe assessment documentation: wrote brief notes while doing assessment, but not detailed. Save the details for documentation on chart. Celiac Disease= following a gluten-free diet. Infants rooting check: rub the baby’s cheek. Obstructive Sleep Apnea from Hypoxia = Hypertension MDMA medication Sx: Diaphoresis Uric-Acid acceptable foods = oranges (citrus fruits) Ovarian Cancer Sx: Abdominal Bloating Hypokalemia (low potassium) Sx: muscle weakness/deep tendon reflexes Raynaud’s Disease Sx: Blanching of fingers/toes 1st step in emergency preparedness = notifying the incident commander Discharge prep for client with intimate violence = helping client develop a safety plan Type I diabetics: should not use cold therapy d/t impaired extremity circulation Constipation during pregnancy: caused by growing uterus displacing compression on the intestines. DVT in lower legs: elevate extremity Opioid disposal of extra amounts: need 2nd nurse for verification Enoxaparin = anticoagulant used post op Hand rolls are used for: maintaining functional position RBC transfusions require: a 20 gauge needle or larger. Macular Degeneration = Decreased central vision Estradiol: Monitor for H/A Hot water in homes with young children: no higher than 120 degrees Anorexia: watch client eat before during and after. Amitriptyline: Common side effects = dry mouth & constipation Lorazepam antidote = Flumazenil Client with restraints: needs continuous supervision Stroke: “F.A.S.T.” Face: Smile….any drooping? Arms: Raise them…. Speech: Speak – any slurring? Time: Call 911 Alert & Oriented X4 = Questions to ask – 1. Name 2. Place 3. Time 4. Situation Remediation from Comprehensive Predictor #1 (12/09/2016) Safe Medication Administration and Error Reduction: Intervening for Unsafe Practice- ⦁ Avoid distractions during medication preparation; may increase the risk for error. ⦁ Check the labels for the medication name and concentration; double-check insulin and heparin with another nurse. ⦁ Question multiple tablets or vials for a single dose. ⦁ Only give medications that have been personally prepared. ⦁ Follow correct procedures for all routes of administration. ⦁ Communicate clearly both in writing and speaking; use verbal Rx only for emergencies. ⦁ Omit or delay doses as indicated by client’s condition. ⦁ Follow all laws and regulations regarding controlled substances when preparing and administering medications; keep controlled substances locked and discarding an excess should be witnessed by another nurse. Tertiary Prevention for Clients Who Have HIV- ⦁ Maximization of recovery after an injury or illness (rehabilitation); Nutrition counseling, exercise rehabilitation, case management, PT and OT, and support groups. PICC Therapy-Peripherally Inserted Central Catheter ⦁ Used up to 12 months; indicated for administration of blood, long-term administration of chemo, ABX, and TPN. ⦁ Care of a PICC includes: Assessing the site every 8 hours; changing tube and positive pressure cap every 3 days; using a 10 mL syringe or larger to flush the line; performing flush for intermittent medication administration; obtaining blood samples by (withdrawing 10 mL and discarding, taking a second syringe and withdrawing 10 mL for sample, and taking a third syringe and flushing with 10 mL of NS; using a transparent dressing (dressing changes every 7 days); advising client not to immerse arm in water; NOT to have BP taken in arm with PICC line. Prioritization of Client Care- ⦁ Prioritize systemic before local (“life before limb”). ⦁ Prioritize acute (less opportunity for physical adaptation) before chronic (greater opportunity for physical adaptation). ⦁ Prioritize actual problems before potential future problems. ⦁ Listen carefully to clients and don’t assume. ⦁ Recognize and respond to trends versus transient findings. ⦁ Recognize signs of medical emergencies and complications versus “expected client findings.” ⦁ Apply clinical knowledge to procedural standards to determine the priority action. ⦁ Maslow’s Hierarchy ⦁ ABCs ⦁ Safety/Risk Reduction ⦁ Assessment/Data Collection First ⦁ Survival Potential ⦁ Least Restrictive/Least Invasive ⦁ Acute vs. Chronic/Urgent vs. Nonurgent/Stable vs. Unstable Priority Action for a Client Who Has Manic Depressive Disorder (MDD)- ⦁ First line of therapy is medications; may take 2-3 weeks to become therapeutic. ⦁ Hospitalization may be necessary, close supervision, and suicide prevention. Medications for Psychotic Disorders: Prioritizing Client Care- ⦁ Schizophrenia is the primary reason for the administration of antipsychotic medications. ⦁ Atypical antipsychotic agents are now medications of choice for clients because they are more effective with fewer adverse effects; give relief of both positive and negative symptoms, decrease in affective symptoms (depression and anxiety), improvement of neurocognitive defects, fewer or no EPS, fewer anticholinergic effects, and less relapse. ⦁ Chlorpromazine (Thorazine): Chew sugarless gum, sip on water, and wear sunglasses when outdoors; constipation, blurred vision, photophobia, tachycardia. Right to Refuse Treatment- ⦁ If a client chooses to commit to a mental health facility, the client is considered competent; therefore, the client has the right to refuse treatment. ⦁ If a client enters the mental health facility against their will for an indefinite period of time, the client is still considered competent and has the right to refuse treatment unless they have been judged incompetent. Referral to Respite Care- ⦁ Continuing health care addresses long-term or chronic health care needs. ⦁ Examples include end-of-life care, palliative care, hospice, adult day care, and in-home respite care. Referral for Swallowing Difficulties (Dysphagia)- Speech Therapists Feeding a Client Who Has Dysphagia- ⦁ Modifying the texture of foods and the consistency of liquids to achieve proper nutrition. ⦁ These clients are at an increased risk for aspiration; place the client in an upright or high-Fowler’s position to facilitate swallowing. Allow adequate time for eating, utilize adaptive eating devices, and encourage small bites and thorough chewing. Avoid thin liquids and sticky foods. Latex Allergy- Bananas can predispose a client to be at risk for a Latex allergy. Priority Interventions for Initiation of Therapy- ⦁ Nurses should know the medication category/class, mechanism of action, therapeutic effect, side effects, adverse effects, toxic effects, medication interactions, precautions/contraindications, preparation, dosage, and administration of the medications they are administering to their patients. ⦁ Nurses should update the Health History of their patients and complete a physical examination of their patients. ⦁ Six Rights of Safe Medication Administration (Right Client, Medication, Dose, Time, Route, and Documentation). Home Oxygen Safety- ⦁ “No Smoking” sign at front door of the home/ door to the client’s bedroom, no smoking in the presence of oxygen. Smoke outside the home only. Keep O2 tanks away from curtains/drapes by windows(static electricity). Ensure electrical equipment is in good repair and well grounded. Replacing bedding to cotton. have fire extinguisher readily available Priority Action for an Electrical Hazard- ⦁ Medical Equipment - used by the nurse only after a safety inspection and adequate instruction. ⦁ Fire extinguisher, use the PASS sequence: P – Pull the pin. A – Aim at the base of the fire. S – Squeeze the levers. S – Sweep the extinguisher from side to side, covering the area of the fire. ⦁ Fire response (RACE): R – Rescue: Rescue and protect clients in close proximity to the fire by evacuating them to a safer location. Ambulatory clients can walk unattended to a safe location. A – Alarm: Activate the facility alarm system, and then report fire details and location per facility protocol. C – Contain: Contain the fire by closing doors and windows as well as turning off any sources of oxygen and electrical devices. Clients who are on life support are ventilated with a bag-valve mask. E – Extinguish: Extinguish the fire if possible using an appropriate fire extinguisher. Vital Signs: Hyperthermia- ⦁ Obtain blood cultures. Administer ABX after obtaining specimens. ⦁ Labs: WBC counts, sedimentation rates, and electrolytes. ⦁ Provide fluids and rest. Minimize activity. Use a cooling blanket. ⦁ Provide antipyretics. ⦁ Offer blankets during chills and remove them when the client feels warm. ⦁ Provide oral hygiene and dry clothes and linens. ⦁ Keep environmental temperature between (70-80◦F). Caring for a Client Who Has an Infection- ⦁ Use frequent and effective hand hygiene. ⦁ Inform clients about immunizations. ⦁ Educate clients about good oral hygiene. ⦁ For immobile clients, ensure that pulmonary hygiene (turning, coughing, deep breathing, incentive spirometry) is done every 2 hours. ⦁ Use of aseptic technique and proper PPE. ⦁ Following isolation guidelines (includes hand hygiene and the use of barrier precautions which intend to reduce the transmission of infectious organisms). ⦁ Standard Precautions and Transmission Precautions (Droplet, Airborne, and Contact). Infection Control: Standard Precautions for Nurses- implement for all clients. ⦁ Hand hygiene using an alcohol-based waterless product is recommended after contact with the client, body fluids, and contaminated equipment and articles, and after removal of gloves; alcohol-based waterless antiseptic is preferred. ⦁ Clean gloves are worn. ⦁ Masks, eye protection, and face shields are required when care may cause splashing or spraying of body fluids. Chronic Neuromusculoskeletal Disorders: Treatment of Positional Plagiocephaly- ⦁ Plagiocephaly, also known as flat head syndrome, is a condition characterized by an asymmetrical distortion (flattening of one side) of the skull. It is characterized by a flat spot on one side of the head caused by remaining in a supine position for too long. Tx=wearing a helmet – 23hrs/day Legal and Ethical Issues: Caring for a Client Who Is in Seclusion and Restraints- ⦁ Should be ordered for the shortest duration necessary; indicated for the physical protection of the client and/or the protection of other clients and staff. ⦁ Restraints can either be physical or chemical. ⦁ Treatment must be ordered by the PCP in writing. The order must specify the duration of the treatment. The provider must rewrite the order, specifying the type of restraint, every 24 hours or the frequency of time specified by facility policy. ⦁ Nursing responsibilities must be identified in the protocol, including how often the client should be assessed (including the client’s behavior), offered food and fluid, toileted, and monitored for vital signs. (All usually every 2 hours). Remove or replace restraints frequently to ensure good circulation to the area and allow for full ROM to the limb that has been restricted. Pad bony prominences. Use a quick-release knot to tie the restraint to the bed frame. ⦁ The prescription and renewal are limited to 4 hours for an adult, 2 hours for clients ages 9 to 17, and 1 hour for clients younger than 9 years of age. ⦁ In an emergency situation, the nurse must obtain the written order within a specified period of time (usually 15 to 30 mins). Chronic Neurological Disorders: Teaching about Phenytoin- ⦁ Monitor for symptoms (CNS effects: nystagmus, sedation, ataxia, double vision, cognitive impairment) and notify the provider if symptoms occur. ⦁ Advise clients to maintain good oral hygiene. ⦁ Stop medication if rash develops. ⦁ Avoid use in pregnancy. ⦁ Administer at slow IV rate and in dilute solution to prevent adverse CV effects. ⦁ Encourage clients to consume adequate amounts of calcium and vitamin D. ⦁ Dose of oral contraceptives may need to be adjusted or an alternative form of birth control used. ⦁ Monitor for therapeutic effects of warfarin and glucocorticoids; dosages may need to be adjusted. ⦁ Advise clients to avoid alcohol and other CNS depressants. Postpartum Physiological Adaptations: Expected Assessment Findings- ⦁ BUBBLE ⦁ (B) Breasts: Secretion of colostrum (during pregnancy and 2 to 3 days after birth); milk is produced 2 to 3 days after delivery. ⦁ (U) Uterus (Fundal height, Uterine placement, and Consistency): Involution of the uterus (back to its pre-pregnancy state); uterus decreases in size from 1000 grams to 50-60 grams over a 6 week period; immediately after delivery the fundus should be firm, midline with the umbilicus, and at the level of the umbilicus (every 24 hours the fundus should descend approximately 1-2 cm). ⦁ (B) Bowel and GI Function: Increased appetite post-delivery; constipation with bowel evacuation delayed until 2-3 days after birth; hemorrhoids. ⦁ (B) Bladder Function: Urinary retention; postpartal diuresis with increased urinary output within 12 hr of delivery. ⦁ (L) Lochia: Lochia rubra (1-3 days: bright red, bloody consistency, fleshy odor, may contain small clots); Lochia serosa (day 4-10 after delivery: pinkish brown color and serosanguinous consistency); Lochia alba (day 11-up to and beyond 6 weeks postpartum: yellowish, creamy white color, fleshy odor). Amount is assessed by the quantity of saturation on the perineal pad: Scant (less than 2.5 cm), Light (less than 10 cm), Moderate (more than 10 cm), Heavy (one pad saturated within 2 hr), and excessive blood loss (one pad saturated in 15 min or less, or pooling of blood under buttocks). ⦁ (E) Episiotomy (Edema, Ecchymosis, and Approximation): Cervix is soft after birth and may be edematous, bruised, and have small lacerations (within 2 to 3 days postpartum, it shortens and becomes firm). The soft tissues of the perineum may be erythematous and edematous (hematomas or hemorrhoids may be present and the pelvic floor muscles may be overstretched and weak). The vagina gradually returns to its pre-pregnancy size with the reappearance of rugae and a thickening of the vaginal mucosa. Prenatal Care: Fetal Heart Rate Monitoring- ⦁ Fetal HR can be heard by Doppler at 10-12 weeks gestation or heard with an ultrasound stethoscope at 16-20 weeks of gestation. Listen at the midline, right above the symphysis pubis, by holding the stethoscope firmly on the abdomen. Health Promotion of Infants (1 Month to 1 Year): Expected Growth and Development Findings- ⦁ The infant’s posterior fontanel closes by 2-3 months of age. The infant’s anterior fontanel closes by 12-18 months of age. ⦁ Weight: Infants gain 5-7 ounces per week for the first 6 months. Infants triple their birth weight by the end of year 1. ⦁ Height: Infants grow 1 inch per month for the first 6 months. Infants grow 0.5 inches per month for the next 6 months after. ⦁ Infants head circumference increases 0.6 inches the first 6 months of life and 0.2 inches between 6 and 12 months. ⦁ Infants should have 6-8 teeth by the end of the first year. ⦁ 1 month: Demonstrates head lag; has a grasp reflex. ⦁ 2 months: Lifts head off mattress; holds hands in an open position. ⦁ 3 months: Raises head and shoulders off mattress; no longer has a grasp reflex; keeps hands loosely open. ⦁ 4 months: Rolls from back to side; places objects in mouth. ⦁ 5 months: Rolls from front to back; uses palmar grasp dominantly. ⦁ 6 months: Rolls from back to front; holds bottle. ⦁ 7 months: Bears full weight on feet; moves objects from hand to hand. ⦁ 8 months: Sits unsupported; begins using pincer grasp. ⦁ 9 months: Pulls to a standing position; has a crude pincer grasp. ⦁ 10 months: Changes from a prone to a sitting position; grasps rattle by its handle. ⦁ 11 months: Walks while holding on to something; places objects into a container. ⦁ 12 months: Sits down from a standing position without assistance; tries to build a two-block tower without success. ⦁ Piaget: Sensorimotor stage (Birth to 24 months); separation, object permanence, and mental representation. ⦁ Language: Vocalizes with cooing noises, responds to noise, turns head to the sound of a rattle, laughs and squeals, pronounces single-syllable words, and begins speaking two-word phrases and progresses to speaking three-word phrases. ⦁ Erikson: Trust vs. Mistrust. ⦁ Age-Appropriate Activities: Rattles, mobiles, teething toys, nesting toys, playing pat-a-cake, playing with balls, and reading books. Health Promotion of Preschoolers (3 to 6 Years): Developmental Age- ⦁ Weight: Preschoolers should gain about 4.5-6.5 pounds per year. ⦁ Height: Preschoolers should grow about 2.5-3 inches per year. ⦁ 3 years: Rides a tricycle; jumps off bottom step; stands on one foot for a few seconds. ⦁ 4 years: Skips and hops on one foot; throws a ball overhead. ⦁ 5 years: Jumps rope; walks backward with heel to toe; moves up and down stairs easily. ⦁ Piaget: Preoperational phase: (Preconceptual thought: 2-4 years of age: artificialism, animism, imminent justice; Intuitive thought: 4-7 years of age: can classify information and are aware of cause and effect). ⦁ Time: Begin to understand concepts of past, present, and future. ⦁ Language: Can speak in sentences and identify colors, and they enjoy talking. ⦁ Erikson: Initiative vs. Guilt. ⦁ Age-Appropriate Activities: Playing ball, putting puzzles together, riding tricycles, playing pretend and dress-up activities, role playing, painting, sewing cards and beads, and reading books. Infections: Teaching About Immunizations During Pregnancy- ⦁ Vaccinations that should be encouraged are: Hepatitis B, pneumococcal infection, Hib, and viral influenza. ⦁ Vaccinations that are to be discouraged and are contraindicated include the Rubella vaccine. Stroke: Priority Findings to Assess- ⦁ Transient symptoms: Visual disturbances, dizziness, slurred speech, and a weak extremity; may indicate a TIA which can be a warning sign of an impending stroke. ⦁ Left-hemispheric Stroke: Expressive and receptive aphasia (inability to speak and understand language); agnosia (unable to recognize familiar objects); alexia (reading difficulty); agraphia (writing difficulty); right extremity hemiplegia (paralysis) or hemiparesis (weakness); slow, cautious behavior; depression, anger, and quick to become frustrated; visual changes (hemianopsia- loss of visual field in one or both eyes). ⦁ Right-hemispheric Stroke: Altered perception of deficits (overestimation of abilities); one-sided neglect (ignore the left side of the body- cannot see, feel, or move affected side, so client unaware of its existence); loss of depth perception; poor impulse control and judgment; left hemiplegia (paralysis) or hemiparesis (weakness); visual changes (hemianopsia-loss of visual field in one or both eyes). ⦁ Notify the provider immediately if the client’s BP exceeds a systolic greater than 180 mm Hg or a diastolic greater than 110 mm Hg. ⦁ Fever can cause an increase in ICP. ⦁ Monitor for changes in the client’s LOC (increased ICP sign). ⦁ Elevate the client’s HOB approximately 30◦ to reduce ICP and to promote venous drainage. ⦁ Institute seizure precautions. Contraception: Contraindications of Combination Oral Contraceptives- ⦁ Women with a history of blood clots, stroke, cardiac problems, breast or estrogen-related cancers, pregnancy, or smoking, are advised not to take oral contraceptive medications. ⦁ Oral contraceptive effectiveness decreases when taking medications that affect liver enzymes, such as anticonvulsants and ABX. Care of Special Populations: Recognizing Elder Abuse- ⦁ Abuse towards an older adult in the home (elder abuse), such as pushing an older adult parent and causing her to fall. ⦁ Recognizing potential or actual older adult abuse: unexplained or repeated physical injuries; physical neglect and unmet basic needs; rejection of assistance by caregiver; financial mismanagement; withdrawal and passivity; depression. Bipolar Disorders: Providing Nutrition for a Client Experiencing Acute Mania- ⦁ Providing portable, nutritious food, since the client may not be able to sit down to eat. Medications for Children and Adolescents with Mental Health Issues: Evaluating Client Teaching- ⦁ ADHD: improved ability to focus, complete tasks, interacts with peers, & manages impulsivity. ⦁ Monitor BP, chew sugarless gum, sip water, and watch for orthostatic hypotension, monitor weight. Psychotic Disorders: Communicating With a Client Who Is Hallucinating- ⦁ Provide a safe/structured environment to distract the client from thinking about hallucinations. ⦁ Promote therapeutic communication to lower anxiety, decrease defensive patterns, encourage structured participation socially, encourage friendships, and establish trust. ⦁ Ask client directly about hallucinations. Don’t agree or disagree with clients views, but respond with comments like, “I don’t hear anything, but you sound frightened.” ⦁ Do not argue, be genuine, be empathetic. Mobility and Immobility: Complications of Immobility- ⦁ Integumentary: Decreased circulation to tissue causing ischemia, which can lead to pressure ulcers. ⦁ Respiratory: Stasis of secretions and decreased and weakened respiratory muscles, resulting in atelectasis (complete or partial lung collapse) and hypostatic pneumonia; decreased cough response. ⦁ Cardiovascular: Decreased CO leading to poor cardiac effectiveness, which results in increased cardiac workload; increased oxygenation requirement; increased risk of thrombus development. ⦁ Metabolic: Decreased protein resulting in loss of muscle; loss of weight; alterations in calcium, fluid, and electrolytes; resorption of calcium from bones; decreased urinary elimination of calcium resulting in hypercalcemia. ⦁ Elimination: (GU) Urinary stasis; change in calcium metabolism with hypercalcemia resulting in renal calculi; decreased fluid intake, poor perineal care, and indwelling urinary catheters resulting in UTIs. (GI) Decreased peristalsis; decreased fluid intake; constipation, then fecal impaction, then diarrhea. Complementary and Alternative Therapies: Biofeedback for Migraines- ⦁ Migraine Complimentary care: Mind-body therapies (biofeedback, art therapy, meditation, yoga, psychotherapy, tai chi). Biofeedback › Using technology to increase awareness of various neurological body responses to minimize extremes. Complementary and Alternative Therapies: Contraindications for Acupuncture- ⦁ Contraindication for Acupuncture: Drugs/alcohol intoxication, pacemaker use, seizure disorder, bleeding disorders (hemophilia or use of blood thinners), infectious skin diseases, pregnant, herpes voster Acute and Chronic Glomerulonephritis: Dietary Choices- ⦁ Low in Sodium and restrict fluid intake. Antibiotics Affecting Protein Synthesis: Adverse Effects of Tobramycin- ⦁ Ototoxicity: Cochlear damage (hearing loss) and vestibular damage (loss of balance). ⦁ Nephrotoxicity related to high total cumulative dose resulting in acute tubular necrosis (proteinuria, casts in the urine, dilute urine, elevated BUN, creatinine levels). ⦁ Intensified neuromuscular blockade resulting in respiratory depression. ⦁ Hypersensitivity (rash, pruritus, paresthesia of hands and feet, and urticaria). Medications Affecting Coagulation: Contraindications for Thrombolytic Therapy- ⦁ Because of the additive risk for serious bleeding, use is contraindicated in clients who have: Any prior intracranial hemorrhage (hemorrhagic stroke), known structural cerebral vascular lesion (arteriovenous malformation), suspected aortic dissection, active internal bleeding, history of significant closed head or facial trauma in the past 3 months, acute pericarditis, and brain tumors. Medications for Depressive Disorders: Client Teaching About Phenelzine- ⦁ Phenelzine (Nardil): (MAOI) – increases dopamine, serotonin, and norepinephrine (CNS Stimulation). ⦁ Depression and Bulimia. ⦁ Don’t use if pregnant and avoid OTC decongestants. Blood and Blood Product Transfusions: Preparing to Administer Packed RBCs- ⦁ Anemia (Hgb 6-10 /dL) can receive packed RBCs; kidney failure clients as well. ⦁ Assess laboratory values, such as Hgb and Hct. ⦁ Verify the Rx for a specific blood product. ⦁ Obtain blood samples for compatibility determination, such as type and crossmatch. ⦁ Initiate large-bore IV access; a 20-gauge needle is standard for blood administration. ⦁ Assess the client for a history of blood-transfusion reactions. ⦁ Obtain blood products from the blood bank; inspect the blood and confirm the client’s identity, blood compatibility, and expiration time of the blood product with another nurse. ⦁ Prime the blood tubing with NS. Blood products are only infused with NS. ⦁ Obtain the client’s baseline VS. Cardiovascular Diagnostic and Therapeutic Procedures: Care for a Client Who Has an Implanted Venous Port- ⦁ Insertion location: Port is surgically implanted into chest wall pocket; the catheter is inserted into the subclavian vein with the tip in the superior vena cava. ⦁ Indications: Long-term (a year or more) need for vascular access; commonly used for chemotherapy. ⦁ To access a port: Apply local anesthetic to skin if indicated. Palpate skin to locate the port body septum to ensure proper insertion of the needle. Clean the skin with alcohol for at least 3 seconds and allow to dry prior to insertion of the needle. ⦁ Access with a noncoring (Huber) needle. ⦁ Flush with 10 mL NS after every use and at least once per month. Cardiovascular Diagnostic and Therapeutic Procedures: Peripherally Inserted Central Catheter- ⦁ Description: 40-65 cm in length with single or multiple lumens. ⦁ Insertion location: Basilic or cephalic vein with at least one finger’s breadth below or above the antecubital fossa; the catheter should be advanced until the tip is positioned in the lower one-third of the superior vena cava. ⦁ PICCs may be inserted by specially trained nurses. Apply local anesthetic at insertion site and insert the catheter using surgical aseptic technique. Dosage Calculation: Intermittent IV Bolus- ⦁ Volume to be Infused (mL) x Drop Factor (gtt/mL) = IV Flow Rate (gtts/min). Time (min) Diabetes Mellitus Management: Evaluating Understanding of Insulin Regimen- ⦁ Insulin regimens are established for clients who have Type I Diabetes Mellitus. ⦁ More than 1 type of insulin (rapid, short, intermediate, and long-acting); given 1 or more times a day based on BG results. ⦁ Continuous infusion of insulin may be accomplished using a small pump that is worn externally. The pump is programmed to deliver insulin through a needle in subcutaneous tissue. The needle should be changed at least every 2 to 3 days to prevent infection. ⦁ Provide information regarding self-administration of insulin. ⦁ Rotate injection sites to prevent lipohypertrophy (increased swelling of fat) or lipoatrophy (loss of fat tissue) within one anatomic site (prevents day-to-day changes in absorption rates). ⦁ Plan meals to achieve appropriate timing of food intake, activity, onset, and peak of insulin. Calories and food composition should be similar each day. Opioid Agonists and Antagonists: Priority Findings for Child Receiving Morphine- ⦁ Respiratory depression: Monitor VS, stop opioids if RR is less than 12, have Narcan and resuscitation equipment available. ⦁ Opioid Overdose: Triad of Coma, respiratory depression, and pinpoint pupils. Pain Management: Interventions After Epidural Administration- ⦁ Administer a bolus of IV fluids to help offset maternal hypotension. ⦁ Encourage client to remain in the side-lying position after insertion of the epidural catheter to avoid supine hypotension syndrome with compression of the vena cava. ⦁ Monitor maternal BP and pulse, observe for hypotension, respiratory depression, and decreased oxygen saturation. Assess FHR patterns continuously. ⦁ Monitor for the return of sensation and motor control in the client’s legs after delivery but prior to standing. Seizures: Client Education Regarding an Electroencephalogram (EEG)- ⦁ Abstain from caffeine for several hours prior to the procedure. ⦁ Wash hair before and after the procedure. ⦁ Inform the child that he may be asked to take deep breaths and/or exposed to flashes of light during the procedure. ⦁ If prescribed, instruct the parent to withhold sleep prior to the test. ⦁ Inform the child that the test will not be painful. Electrolyte Imbalances: Analyzing Preadmission Results and Preoperative Findings to Report- ⦁ Sodium: 136-145 mEq/L. ⦁ Potassium: 3.5-5.0 mEq/L. ⦁ Calcium:9.0-10.5 mg/dL. ⦁ Magnesium: 1.3-2.1 mEq/L. ⦁ Chloride: 98-106 mEq/L. ⦁ Phosphorus: 3.0-4.5 mg/dL. Angina and Myocardial Infarction: Plan of Care for Thrombolytic Therapy- ⦁ Streptokinase (Streptase) and alteplase (Activase) are used to break up clots. ⦁ Give within 6 hrs of infarction. ⦁ Assess for contraindications (active bleeding, PUD, history of CVA, recent trauma). ⦁ Monitor for effects of bleeding (mental status changes, hematuria). ⦁ Monitor bleeding times (PT, aPTT, INR, fibrinogen levels, and CBC). ⦁ Monitor for side effects (thrombocytopenia, anemia, hemorrhage). ⦁ Administer streptokinase slowly to prevent hypotension. ⦁ Remind client of the risk for bruising and bleeding while on this medication. Meningitis: Caring for a Newly Admitted Client- ⦁ Maintain isolation precautions (DROPLET precautions); these precautions continue until ABX have been administered for 24 hr and when oral and nasal secretions are no longer infectious. ⦁ Standard precautions are implemented for all clients who have meningitis. ⦁ Implement fever-reducing measures. ⦁ Report meningococcal infections to the public health department. ⦁ Provide a quiet environment; minimize exposure to bright light. ⦁ Maintain bedrest with the HOB elevated at 30◦. ⦁ Monitor the client for increased ICP; avoid coughing and sneezing. ⦁ Institute seizure precautions. ⦁ Replace fluid and electrolytes. Meningitis: Priority Action for Bacterial Meningitis- ⦁ ISOLATE the client as soon as meningitis is suspected. Hyperthyroidism: Assessing for Complications Following a Thyroidectomy- ⦁ Advise the client to notify the nurse of any tingling sensation of the mouth, tingling of the distal extremities, or muscle twitching (could indicate hypocalcemia and tetany). ⦁ Remind the client that talking at intervals will be expected to check for nerve damage with measurement of VS. ⦁ Instruct the client to notify the surgeon of incisional drainage, swelling, or redness that may indicate infection. ⦁ Advise the client and family to monitor for manifestations of hypothyroidism, such as hypothermia, lethargy, and weight gain. ⦁ Instruct patients who have had a total thyroidectomy that lifelong thyroid replacement medications will be required. ⦁ Advise the client to notify the surgeon of fever, increased restlessness, palpitations, or chest pain. ⦁ Inspect the surgical incision and dressing for drainage and bleeding, especially at the back of the neck. ⦁ Thyroid Storm/Crisis can occur following a thyroidectomy. Findings are hyperthermia, HTN, delirium, vomiting, abdominal pain, hyperglycemia, tachy-dysrhythmias, chest pain, dyspnea, and palpitations. Pressure Ulcers, Wounds, and Wound Management: Risks for Delayed Wound Healing- ⦁ Increased age, poor overall wellness, poor immune function, medications (anti-inflammatory and antineoplastic), poor tissue perfusion, poor nutrition, inadequate Hgb levels, obesity, chronic diseases, chronic stress, smoking, and wound stress. Postoperative Nursing Care: Client Care Following Mastectomy- ⦁ Teach the client how to care for her incision and drainage tubes. (Drains are usually left in for 1 to 3 weeks). ⦁ Advise the client to avoid placing her arm in a dependent arm position. This position will interfere with wound healing. Have the client wear a sling while ambulating (to support arm). ⦁ Encourage early arm and hand exercises (squeezing a rubber ball, elbow flexion and extension, and hand-wall climbing) to prevent lymphedema and to regain full range of motion. ⦁ Teach the client not to wear constrictive clothing and to avoid cuts and injuries to the affected arm. ⦁ Instruct the client to report numbness, pain, heaviness, or impaired motor function of the affected arm to the surgeon. ⦁ Have the client sit with the head of the bed elevated 30° when awake and support her arm on a pillow. Laying on the unaffected side can relieve pain. ⦁ Avoid administering injections, taking blood pressure, or obtaining blood from the client's affected arm. Place a sign above the client's bed regarding these precautions. ⦁ Emphasize the importance of a well-fitting breast prosthesis for a client who had a mastectomy. ⦁ Provide emotional support to the client and her family. Encourage the client to express feelings related to perception of sexuality and body image. Cardiovascular Diagnostic and Therapeutic Procedures: Action to Take Prior to Cardiac Catheterization- ⦁ Signed informed consent form is obtained. ⦁ Walking on a treadmill and comfortable shoes and clothing are recommended. ⦁ If a pharmacological stress test = a meds - adenosine (Adenocard) or dobutamine (Dobutrex) is given to stress the heart instead of walking on the treadmill. ⦁ Instruct the client to fast 2 to 4 hr before the procedure according to facility policy and to avoid tobacco, alcohol, and caffeine before the test. Chest Tube Inserting and Monitoring: Monitoring a Water Seal Drainage System- ⦁ Water seals are created by adding sterile fluid to a chamber up to the 2 cm line. The water seal allows air to exit from the pleural space on exhalation and stops air from entering with inhalation. ⦁ To maintain the water seal, the chamber must be kept upright and below the chest tube insertion site at all times. ⦁ The height of the sterile fluid in the suction control chamber determines the amount of suction transmitted to the pleural space. The application of suction results in continuous bubbling in the suction chamber. ⦁ Tidaling (movement of the fluid level with respiration) is expected in the water seal chamber. Monitor the water seal chamber for continuous bubbling (air leak finding). ⦁ If the chest tube drainage system is compromised, the nurse immerses the end of the tube in sterile water to restore the water seal. Hematologic Disorders: Preventing Sickle Cell Crisis- ⦁ Promote rest to decrease oxygen consumption. Administer oxygen as prescribed if hypoxia is present. ⦁ Maintain fluid and electrolyte balance. ⦁ Pain management: Treat mild to moderate pain with Tylenol or ibuprofen. Manage severe pain with opioid analgesics (codeine, morphine sulfate, oxycodone, Dilaudid, and methadone). ⦁ Administer blood products (packed RBCs). ⦁ Treat and prevent infection. ⦁ Monitor and report laboratory results. Renal Disorders: Risk Factors for Glomerular Disease- ⦁ Risk Factors - APSGN: streptococcal infection with a specific strain of group A ß-hemolytic streptococcus. ⦁ Subjective Data -Recent upper respiratory infection or streptococcal infection. ⦁ Objective Data -Cloudy, tea-colored urine , ↓urine output , Irritability, Ill appearance, Lethargy , Anorexia, discomfort (headache, abdominal pain, dysuria) ,Periorbital/facial edema , that is worse in the morning but then spreads to extremities and abdomen with progression of the day, mild to severe hypertension. Fluid Imbalances: Clinical Manifestations of Hypervolemia- ⦁ Tachycardia, bounding pulse, hypertension, tachypnea, increased central venous pressure. ⦁ Confusion, muscle weakness, H/A. ⦁ Weight gain, ascites. ⦁ Dyspnea, orthopnea, crackles, diminished breath sounds. ⦁ Edema, distended neck veins, pale and cool skin. Cardiovascular Disorders: Nursing Interventions to Decrease Cardiac Demands- ⦁ Remain calm when providing care. ⦁ Conserve the child’s energy by providing frequent rest periods, clustering cares, providing small, frequent meals, bathing PRN, and keeping crying to a minimum in cyanotic children. ⦁ Maintain bedrest. ⦁ Position the infant in a car seat or hold at a 45◦ angle. Keep safety restraints low and loose on the abdomen. ⦁ Allow the child to sleep with several pillows and encourage a semi-Fowler’s or Fowler’s position while awake. ⦁ Medications: Digoxin (improves myocardial contractility); Captopril and enalapril (reduce afterload by causing vasodilation, resulting in decreased pulmonary and systemic vascular resistance); Metoprolol or carvedilol (decrease HR and BP, and promote vasodilation). Furosemide or chlorothiazide (rid the body of excess fluid and sodium). Cystic Fibrosis: Illness Management at Home- ⦁ Chest Physiotherapy – 2x/day – not immediately before or after meals. ⦁ Drink fluids, exercise, vitamins A, D, E, K, eat 3 meals /day w/ snacks, eat high protein/calorie meals. ⦁ Pancreatic Enzymes – taken 30 min. within eating. ⦁ Clubbing fingers is a late manifestation of CF. Hyperthyroidism: Assessment Findings- ⦁ Nervousness, irritability, hyperactivity, emotional lability, decreased attention span. ⦁ Weakness, easy fatigability, exercise intolerance. ⦁ Heat intolerance, weight loss, increased appetite. ⦁ Insomnia and interrupted sleep. ⦁ Frequent stools and diarrhea. ⦁ Menstrual irregularities. ⦁ Warm, sweaty, flushed skin with velvety-smooth texture. ⦁ Tremor, hyperkinesia, hyperreflexia. ⦁ Vision changes, hair loss, goiter, bruit over the thyroid gland. ⦁ Elevated systolic BP and widened pulse pressure, tachycardia, and dysrhythmias. Cardiovascular Disorders: Laboratory Results Indicating Rheumatic Fever- ⦁ Throat culture for GABHS. ⦁ Serum antistreptolysin-O (ASO) titer – elevated or rising titer, most reliable diagnostic test. ⦁ C-reactive protein (CRP) – elevated in response to an inflammatory reaction. ⦁ Erythrocyte sedimentation rate – elevated in response to an inflammatory reaction. Disorders of the Eye: Manifestations of Acute Glaucoma- ⦁ H/A, mild eye pain, loss of peripheral vision, decreased accommodation, and elevated IOP; (Open-angle Glaucoma). ⦁ Rapid onset of elevated IOP, decreased or blurred vision, seeing halos around lights, pupils are nonreactive to light, severe pain and nausea, and photophobia; (Angle-closure Glaucoma). Heart Failure and Pulmonary Edema: Complications of Atrial Fibrillation- ⦁ Stroke and HF. Pulmonary Embolism: Expected Manifestations- ⦁ SOB, sudden/sharp chest pain, ↑HR, ↑breathing, sweating, anxiety, coughing up blood or pink/frothy mucous, fainting. Expected Findings for Retinoblastoma- ⦁ Cancer of the Retina. ⦁ Most common: White pupillary reflex. ⦁ Less Common: Lazy eye, vision problems, eye pain, redness of the white part of the eye, bleeding in the front part of the eye, bulging of the eye, a pupil that doesn’t get smaller when exposed to bright light, and a different color in each iris (the colored part of the eye). Allergies to medications * latex related to sensitivity to bananas and other fruits * betadine related to an allergen to shellfish * propofol related to an allergy to eggs or soybean oil. Diagnostic Procedures Summary: * Urinalysis – ruling out of infection * Blood type and cross match – transfusion readiness * CBC – infection/immune status * Hgb and Hct – fluid status, anemia * Pregnancy test – fetal risk of anesthesia * Clotting studies (PT, INR, aPTT, platelet count) * Electrolyte levels – electrolyte imbalances * Serum creatinine and BUN – renal status * ABGs – oxygenation status * Chest x-ray – heart and lung status * 12-lead ECG – baseline heart rhythm, dysrhythmias, history of cardiac disease, performed on all clients older than 40 years Rheumatic fever – Lab results: * Throat culture for GABHS * Serum antistreptolysin-O (ASO) titer – elevated or rising titer, most reliable diagnostic test * C-reactive protein (CRP) – elevated in response to an inflammatory reaction * Erythrocyte sedimentation rate – elevated in response to an inflammatory reaction Gross Motor Skills: * 3 year-olds: Rides a tricycle › Jumps off bottom step › Stands on one foot for a few seconds * 4 year-olds: Skips and hops on one foot › Throws ball overhead * 5 year-olds: Jumps rope › Walks backward with heel to toe › Throws and catches a ball with ease Signs of infiltration -Edema, pallor, decreased skin temperature around the site, and pain Signs of phlebitis - Pain, increased skin temperature, and redness along the vein Signs of extravasation (infiltration w/ dislodged IV catheter) - Pain, stinging or burning at the site, swelling, and redness Tunneled catheter - A catheter surgically inserted into a trench Cystic Fibrosis: * Chest Physiotherapy – 2x/day – not immediately before or after meals. * Drink fluids, exercise, vitamins A, D, E, K, eat 3 meals /day w/ snacks, eat high protein/calorie meals * Pancreatic Enzymes – taken 30 min. within eating. * Clubbing fingers is a late manifestation of CF Vision: Hardy-Rand-Rittler Test – person should be able to identify number in confusion of colors Glaucoma: Loss of peripheral vision Phenelzine (Nardil): (MAOI) –increases dopamine, serotonin, and norepinephrine (CNS Stimulation) * Depression & bulimia * don’t use if pregnant & avoid OTC decongestants AVOID – foods with Tyramine: aged cheese, peperoni, salami, avocados, figs, bananas, smoked fish, protein, beers, red wine, caffeine, chocolate, fava beans, ginseng. Schizophrenia: Med for Tx: Chlorpromazine (Thorazine): * chew sugarless gum, sip on water, and wear sunglasses when outdoors * Constipation, blurred vision, photophobia, tachycardia Depressive disorders: 1st line of therapy = Medications, but may take 2-3 weeks for therapeutic effects to be noticed * Hospitalization may be necessary, close supervision, suicide prevention * provide a safe/structured environment to distract the client from thinking about hallucinations * promote therapeutic communication to lower anxiety, decrease defensive patterns, encourage structured participation socially, encourage friendships, establish trust. * ask client directly about hallucinations. Don’t agree or disagree with clients views, but respond with comments like, “I don’t hear anything, but you sound frightened” * do not argue, be genuine, be empathetic Parkinson’s disease - EPS Sx: * Drooling, Involuntary arm movements (tardive dyskinesia), pacing (akathisia) Sustained Release Tabs: swallow whole (do not chew/crush), stay on regular schedule Transdermal Patches: place on one hip daily and alternate hips. Leave on for 9 hours. ADHD med evaluation of effectiveness: improved ability to focus, complete tasks, interacts with peers, & manages impulsivity. * Monitor BP, chew sugarless gum, sip water, and watch for orthostatic hypotension, monitor weight Nurses: responsible for understanding and protecting client rights. Pre-Procedure Nurse Responsibilities: * signed consent form (after demonstrating thorough understanding of procedure) * Client to FAST 2-4 hours prior to procedure [Show More]
Last updated: 1 year ago
Preview 1 out of 53 pages
Instant download
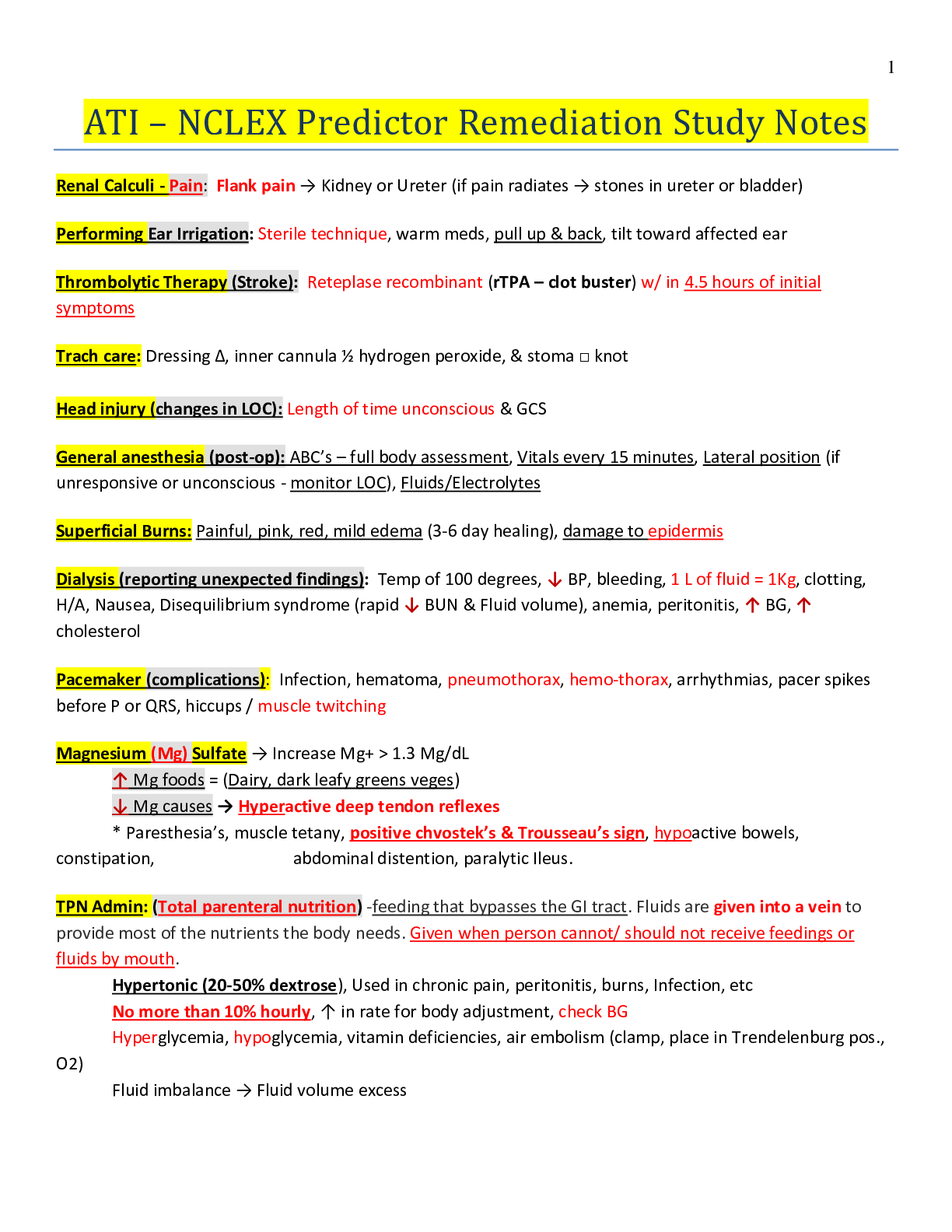
Buy this document to get the full access instantly
Instant Download Access after purchase
Add to cartInstant download
Reviews( 0 )
Document information
Connected school, study & course
About the document
Uploaded On
Feb 24, 2021
Number of pages
53
Written in
Additional information
This document has been written for:
Uploaded
Feb 24, 2021
Downloads
0
Views
51