*NURSING > Study Notes > Eye, Ear, Skin, and Allergies (All)
Eye, Ear, Skin, and Allergies
Document Content and Description Below
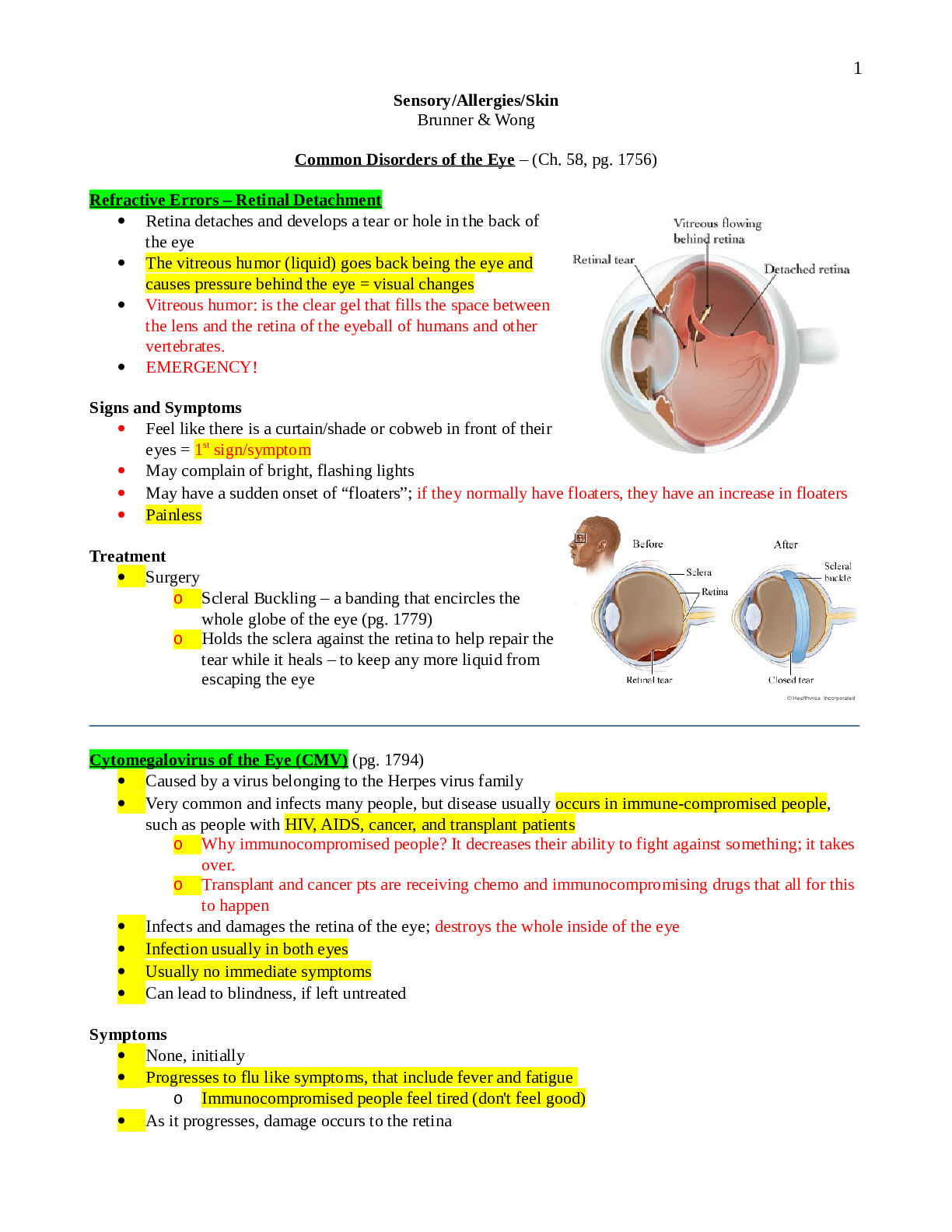
Sensory/Allergies/Skin Brunner & Wong Common Disorders of the Eye – (Ch. 58, pg. 1756) Refractive Errors – Retinal Detachment Retina detaches and develops a tear or hole in the back of th... e eye The vitreous humor (liquid) goes back being the eye and causes pressure behind the eye = visual changes Vitreous humor: is the clear gel that fills the space between the lens and the retina of the eyeball of humans and other vertebrates. EMERGENCY! Signs and Symptoms Feel like there is a curtain/shade or cobweb in front of their eyes = 1st sign/symptom May complain of bright, flashing lights May have a sudden onset of “floaters”; if they normally have floaters, they have an increase in floaters Painless Treatment Surgery o Scleral Buckling – a banding that encircles the whole globe of the eye (pg. 1779) o Holds the sclera against the retina to help repair the tear while it heals – to keep any more liquid from escaping the eye __________________________________________________________________________________________ Cytomegalovirus of the Eye (CMV) (pg. 1794) Caused by a virus belonging to the Herpes virus family Very common and infects many people, but disease usually occurs in immune-compromised people, such as people with HIV, AIDS, cancer, and transplant patients o Why immunocompromised people? It decreases their ability to fight against something; it takes over. o Transplant and cancer pts are receiving chemo and immunocompromising drugs that all for this to happen Infects and damages the retina of the eye; destroys the whole inside of the eye Infection usually in both eyes Usually no immediate symptoms Can lead to blindness, if left untreated Symptoms None, initially Progresses to flu like symptoms, that include fever and fatigue o Immunocompromised people feel tired (don't feel good) As it progresses, damage occurs to the retina 1 Painless May have blind spots, floating specks, light sensitivity, eye redness, blurred vision As time goes by, sudden vision loss and flashes of light may occur Spreads to both eyes More serious complication - retinal detachment (if not treated) Diagnosis By ophthalmology exam o Pupil is dilated with medication, which makes it easier for the doctor to observe the inner portion – can then see the damage caused by virus Blood and urine tests may be done to detect the presence of the virus Treatment Antiviral Drugs – they slow down the virus, but can’t cure it o End in -vir o Administered IV or through a catheter Drugs o Acyclovir o Cytovir o Ganciclovir – IV, PO, or intravitreously (4mm intraocular implant or insert containing the medication. The drug is released during a 5 to 8 month period.) o Cidofovir – delays the replication of CMV and is administered by IV. Nephrotoxicity, proteinuria and increased serum creatinine levels are side effects. o Foscarnet – inhibits viral DNA replication. May be the med of choice when ganciclovir is ineffective. Can be administered by IV or intravitreal injection. Vitrasert: implant that is inserted directly in eye (ganciclovir); implant gradually secretes medication; releases the antiviral overtime; lasts 5 – 8 months; done on an outpatient basis Complications Blindness Most serious is retinal detachment – leads to seriously limited vision and blindness Because it’s a virus, it can lead to kidney impairment and low WBC count. (The treatment drugs are VERY nephrotoxic, BUN and Creatinine labs, Creatinine clearance (24 hr urine) drawn, hard on the kidneys – some complications could be due to drugs) Antivirals cause damage to the kidneys o Kidney damage (medications) – antivirals cause kidney damage; monitor BUN, Createnine, Createnine clearance (24 hr. urine) Very low WBC Prevention Prevented by regular eye exams, even if no symptoms present Immunocompromised people should have eye exam every 6 months – b/c there are no s/s; if they have the eye exam, maybe that can catch it early before it causes damage __________________________________________________________________________________________ Orbital Fracture Trauma (pg. 1782-1784) Soft tissue injury is usually associated with head injury If there is soft tissue injury, check for underlying fracture, especially with blunt trauma Orbital trauma = under the eye 2 Causes: sports (baseball/baseball bat slipped out of their hand), fighting, falls Simple facial x-ray shows that they have a fracture, then they will perform a CT o CT should be done to determine what structures were affected o They can get a cranial abscess b/c everything in the sinus cavity has gained access to the orbit; can be fatal Associated with head trauma Check Visual Acuity ASAP o If their vision is not affected yet, keep checking to prevent irreversible damage; Signs & Symptoms Will have tenderness, ecchymosis, swelling, proptosis (downward displacement of eyeball), hemorrhage If there is an immediate loss of vision, it is usually irreversible damage = damaged the optic nerve (Proptosis) Ocular Trauma Eye injury Leading cause of blindness in children and young adults due to sports injuries, occupational injuries, weapons, MVA, assault, explosives, fireworks Two Types need critical attention o Chemical Burn – IRRIGATE with normal saline or tap water - flush it, flush it, flush it, if they are not in the ER where you can flush it with normal saline, if they are at home use simple tap water, keep flushing until Medical care gets there Flush for at least 20 minutes Phone call from a parent who says “my kid splashed bleach in their eye”. Tell them to keep flushing it until help arrives. o Foreign Body - never ever mess with it, leave it alone, don't let the patient take it out, the MD should be the one to take it out, put a metal shield over it to keep them from messing with that eye; If it is sticking out of the eye, stabilize it and send them to an eye doctor. Put eye-numbing medication in it, patch it up, and send to ophthalmologist! Infections and Inflammatory Conditions of the Eye (pg. 1787-1790) Conjunctivitis – “pink eye”; pink appearance of subconjunctival blood vessels and congestion (outside part of the eye) Three Types of Conjunctivitis Bacterial o Caused by staph, strep, haemophilus (H Influenza) o Exudate in the eye in the morning, self-limiting o Treat with antibiotic eye drops - takes two weeks to go away o Steroid eye drops to help with the redness 3 Viral – the worst o VERY contagious o Usually caused by adenovirus and herpes simplex o Does not respond to antibiotics o Lasts longer than bacterial o Seldom responds to antibiotic treatment o No work or school for three to seven days, because it is so highly contagious o Usually seen in preschool, first or second grade, keep them away long enough to eradicate it o Treat with compresses (to make it feel nice) They have exudate problem – their eyes stick together = apply warm compress If they have eye pain, cold compress Bacterial or Viral Conjunctivitis: o Clean their toys with bleach and hot, soapy water o If you add bleach, rinse it extremely well; they put toys in their mouth Allergic o Caused by allergic rhinitis o Usually have a hx of pollen allergy o Biggest complaint: feel like they have sand in their eye o Treatment is antihistamine eye drops and/or steroid drops Teach pts proper hand hygiene – before and after eye drop treatment, or preferably to use gloves to clean the eye If the dropper gets into the eye = contaminated o Throw away, call MD No eye makeup Light sensitivity - wear dark glasses outside and inside Uveitis (Brunner, pg. 1790) Inflammatory process of the middle layer of the eye, the uveal tract o Lower middle portion of the eye This part contains veins and arteries that transports blood to the parts of the eye responsible for vision This is more serious Just like conjunctivitis, but it affects a different part of the eye Symptoms Eye redness Irritation Eye pain Blurred vision Increased sensitivity to light Floating spots Cause Usually an infection – viral, bacterial, parasite, fungus Can affect other parts of the body (because it affects blood supply) 4Treatment Needs to be done right away Have light sensitivity - wear dark glasses outside and inside Steroid eye drops to reduce swelling Antibiotic eye drops for pts with infectious uveitis Steroid and abx eye drops should be used opposite – don't use them at the same time Drugs to relieve pain Teaching The eye drops will probably sting/burn when administered Should be temporary, no more than 15-20 seconds If it lasts longer = stop using the meds and call MD __________________________________________________________________________________________ Orbital Cellulitis (pg. 1790) Inflammation of tissues surrounding the eye due to bacteria, virus, or fungus Common in pediatrics Cause Number one is a sinus infection Children usually H influenza Adults usually staph or strep Treatment If untreated, can lead to optic nerve damage, intracranial abscess, and death (Intracranial abscess…. inflammation is tissue around the eye. If untreated, an abscess is formed and the eye is close to the brain, so it can move into the brain) Treated with high dose, broad spectrum, systemic antibiotics (IV, not by mouth) Orbital and Ocular Neoplasms (Brunner, pg. 1790) Non-cancerous Benign lesions of Orbit Masses characterized by lack of infiltration to other tissues Develops from infancy, grows and presents later in life Diagnosed with exam, palpation, XR, and/or a CT Pt will complain of visual function disturbances The lesion is pushing the eyeball outward o Will have proptosis – downward displacement of eye Treated by excision Benign lesions of Eyelids Usually size increases with age Starts out as a mole or extra epithelials If its tiny, they will not remove it until it starts affecting their vision Treated by excision Benign lesions of Conjunctiva 5 Starts in late childhood, early adolescence If its tiny, they will not remove it until it starts affecting their vision Treated by excision Malignant Orbital and Ocular Neoplasms of….. (pg. 1792) Cancerous Can infiltrate other areas Treatment Excision, Radiation and/or Chemo Some require reconstructive surgery (some treatments require removal of the eye) Malignant Tumors of the Orbit: Rhabdomyosarcoma -- the most common neoplasm in childhood Manifestations Proptosis Lid swelling Impaired ocular motility Usually metastasizes to lung Requires a removal of the eye = enucleation Malignant Tumors of the Globe: Retinoblastoma, most of the time – it’s hereditary Occurs in childhood Manifestations Cellulitis White pupil o When you take a photo with a camera, the pupil usually appears red. If the pupil appears white on one side, it should be evaluated o Usually occurs in children; the mothers notice it when they take pictures Requires a removal of the eye = enucleation Malignant Tumors of the Eyelid: Basal cell carcinoma most common; like a skin cancer = eyelid is apart of the skin Very common in people with fair skin with a Hx of chronic sun exposure, Invasive, but slow growing Doesn’t usually metastasize Usually occurs on lower eyelid near the inner canthus area Malignant Tumors of the Conjunctiva: Metastasis is rare, they just take it out Types of Eye Surgery (Brunner, pg. 1792) Enucleation – removal of the entire eye and part of the optic nerve Because of: Trauma, glaucoma, retinal detachment, blindness (if there is pain w/the blindness), retinoblastoma Pts will get a prosthesis after surgery, but must wait until the entire structure heals before they can get a prosthesis; they do not go ahead and fit for ocular prosthesis until it is healed Evisceration – remove intra-ocular contents by incision thru cornea 6 Because of: Trauma with ruptured globe, infection Prosthetic implant will usually have a better fit, because sclera, optic nerve, and muscles are all left intact Still have sclera, optic nerve = better prosthesis fit (vs enucleation = removal of the eye and part of the optic nerve) Exenteration – removal of the eyelids, eye, and all of the orbital contents (Picture >>>>>) Usually due to a malignancy A prosthesis will follow surgery Before prosthesis, pt will usually have to have a lot of plastic surgery to have eye lids and all of that recreated Will have to have an ocular prosthesis plus reconstructive surgery to it’ll fit; have to have eyelids made Ocular Prosthesis - implant or conformer – helps prevent a contracted, sunken appearance, made to be placed in socket, fitting process starts 6-8 weeks after surgery; matches exactly to the other eye; prosthesis usually last about six years; “glass eye”; not made of silicon Nursing Care includes: physical, social, psychological considerations Not only have they lost an eye, they have also lost their vision. Need emotional support Teaching should include: o Hand hygiene – due to insertion and removal of prosthesis for cleaning and put back in They get very comfortable with their prosthesis; can sleep in it, etc. Have to have frequent eye exams to make sure it still fits Nursing Interventions for Ocular Surgery Patients Goals Preserve visual function Maintain the anatomical relation of the ocular structures Always be aware of the developmental stage of your patient, also age and culture Complications Blindness, if the optic nerve is damaged or blood supply is compromised during surgery May lead to optic nerve damage May get ptosis, lazy or droopy eye = can be temporary o Sometimes resolves itself after surgery (depends on what caused it) Hemorrhage o Bleeding of serous blood is to be expected. o Bright red blood could mean hemorrhage and the HCP needs to be notified ASAP. Treatments Prophylactic IV antibiotics – before surgery Corticosteroids for optic nerve swelling = Temporary Topical ocular antibiotics Ice compresses 24 to 48 hours post-op (decreases periorbital swelling) Elevate the HOB 30 to 45 degrees – to decrease swelling and intraocular pressure o Other ways to increase intraocular pressure: Bending over at the waist Ex: to tie shoes, cleaning o Do not want them doing this ^^ 7Discharge teaching Teaching on meds – how to administer – (PO or drops) – explain hygiene with drop meds o Teach about abx that they might have to take by mouth o Eye drops Teach not to contaminate the dropper Teach that any type of eye drops can affect the systemic system Beta blocker for glaucoma = affect BP and HR Steroid = affect blood sugar Teaching on compresses __________________________________________________________________________________________ Ocular Medications (pg. 1795) Drop meds - once the dropper has touched they eye, they are considered infected Topical Anesthetic – usually used prior to a procedure – for severe eye pain Numbs the eye Lasts 10 to 20 minutes Tell patients not to rub eye (since it’s numb, they can scratch eye and not know it) = can cause more damage that is already present Pontocaine Proparacaine hydrochloride, tetracaine hydrochloride are commonly used drops Makes it numb, one drop of tetracaine hydrochloride will numb the eye for 10-15 minutes at a time Anti-infective - will still have same side effects as taking PO or IV antibiotics Anti-fungal Antiviral Antibiotics Will get the same systemic effect in eye drops Anti-Allergy – used to treat allergic reactions and/or symptoms = temporary o If used on a daily basis, overtime, the redness in the eyes will come back sooner and sooner o Should not use the one w/ Astrigen in it o Just use a lubricant eye drop Corticosteroids and NSAIDs Corticosteroids – affect glucose Short term eye drops Used to treat inflammatory conditions Need to teach them they have to shake the meds well before use NSAIDs have fewer side effects Corticosteroids (usually long term treatment) – side effects: glaucoma, cataracts, infection, impaired wound healing, and increased intraocular pressure. Ocular irrigants and lubricants 8 Irrigants: used to irrigate, flush, cleanse, or lubricate eye Wet the eye (artificial tears) Lubricants be used every hour if used for corneal lubrication Nursing Management regarding ocular medications Hand hygiene before and after Don't contaminate eye drop dropper Stinging, burning, blurred vision is temporary, but if it continues to for a long period of time, call your doctor Blurred vision occurs after application: If you have an elderly client at r/f falls taking eye drops, tell them not to get up at least 10-15mins after using eye drops Tell pt to be careful with ambulation (meds might cause blurred vision) Tell pt how to perform proper administration of drops (explain why they need to hold pressure at the corner at the eye Chart 58-13 ________________________________________________________________________________________ Common Disorders of the Ear (Ch. 59, pg. 1802) Ear Function – hearing and balance Assessment Otoscope Exam Weber – bone conduction Rinne – air conduction Whisper Audiometry Exam – testing hearing Tympanogram – checks middle ear; muscle function A&P Section on ear – pg. 1802-1804 Test hearing Conditions of the External Ear Otitis Media Kids get OM a lot, versus adults, b/c of short eustachian tubes, they are in school and pass the infection among the other children External Otitis – Otitis External; "swimmers ear" Severe ear canal swelling Can be bacterial, viral, and/or fungal o There can be fungus in pool water S/s – pain; fullness; hearing loss; canal edema and erythema Tx – antibiotic/steroid ear drops combo If untreated will lead to malignant otitis media (mastoiditis); it infects the mastoid bone behind the ear NO SWIMMING until all the abx are gone Can go swimming if they wear ear plugs that are fitted Shower: to alleviate water in the ear, ear plugs or rub Vaseline on a cotton ball and stick in ear (Vaseline does not allow water to get by it) 9Causes Water in the ear (swimmer’s ear) Trauma, systemic conditions (vitamin deficiency, endocrine disorders), dermatosis such as psoriasis Can be bacterial from staph or pseudomonas or fungus from aspergillus Acute Otitis – usually bacterial Happens all of a sudden S/s – fever; unilateral otalgia (ear pain); purulent exudate; tympanic membrane erythematous and bulging (typically the TM is concave, not bulging) Tx: antibiotic ear drops, if tympanic membrane is not perforated (a hole in it); if it is perforated you can no longer use the ear drops o How to tell if TM is perforated? Immediate relief of pain after pain is present (CALL MD) Chronic Otitis – irreversible damage to TM Continual otitis media S/s – foul smelling otorrhea and pain Tx – antibiotic drops or abx powder o Abx to dry up the infection Serous Otitis Media (SOM) (pg. 1814) - fluid in the inner ear, but no evidence of infection Causes Eustachian tube dysfunction Upper respiratory infection Allergies Manifestations Conductive hearing loss Feeling of fullness in ear Congestion Popping or cracking sensation in the ear Treatment Myrongotomy – tubes for an opening of the TM Antibiotics (if infection present) Steroids Tympanic Membrane Perforation – usually infection, trauma, or foreign body (kids take stuff and stuck in their ear = qtip); ear drum has a hole in it Causes Usually due to infection, trauma, foreign objects Usually heals spontaneously If not, they have to do a tympanoplasty type 1 (pg. 1815) Observe for otorrhea and rhinorrhea (ear and nose drainage) (pg. 1813) No ear drops or water in ear canal Manifestations Otorrhea and rhinorrhea and sudden relief of pain Treatment – no ear drops; no water in canal: myringoplasty (suturing or fixing of the perforated TM) if does not heal spontaneously 10Nursing Care No q-tips or scratching the canal No water in canal until healed No swimming until healed When showering – use cotton balls covered in petroleum jelly; place in ear to seal off the ear canal (pg. 1812) Reminder on eardrops: Child (until 6 or 7) – pull down and back (remember chilD – D for down) Adult – pull up and back (adUlt – U for up) Conditions of the Inner Ear Labyrinthitis – inflammation of inner ear (affects hearing and balance) Causes Bacterial or viral infection Can be a complication of otitis media Affects hearing and balance Treatment IV antibiotics Fluid replacement Antihistamines Anti-emetics __________________________________________________________________________________________ Cholesteatoma (pg. 1814) – Benign tumor of ear drum Ingrowth of skin of the eardrum into the middle ear If treatment is delayed, the tumor may destroy structures of the temporal bone Tumor is fast growing Manifestations Hearing loss Neurological deficits Treatment Surgery – mastoidectomy (removal of the mastoid bone) __________________________________________________________________________________________ Glomus Tympanicum (pg. 1817) Rare malignant tumor of the middle ear Treatment Surgical excision and/or radiation therapy, if surgery is not an option 11__________________________________________________________________________________________ Facial Nerve Neuroma (pg. 1823) – benign tumor of cranial nerve number 7 = the facial nerve Manifestation Facial nerve paralysis – first manifestation Usually complain that their face in numb, (Stroke) a lot of times it is overlooked, but they need to remove tumor because if not, the paralysis will be permanent Will display facial drooping Treatment Surgical removal = excision __________________________________________________________________________________________ Acoustic Neuroma (pg. 1823) - benign tumor Manifestations Vertigo Hearing loss Tinnitus – ringing in the ears Treatment Surgery – Craniotomy to remove tumor Complication during the craniotomy – Facial nerve can be damaged = if present they will display facial drooping (cranial nerve 7) = call the MD ______________________________________________________________________________ Types of Ear Surgery Tympanoplasty (pg. 1815) - reconstructive surgery of tympanic membrane 5 Types o Type I – Myringoplasty – closure of the perforated tympanic membrane o Types II-V – extensive repair of the middle ear structures (of the bones) Ossiculoplasty – reconstruction of middle ear bones to restore hearing Mastoidectomy – remove part or all of mastoid bone, because they want to create a dry, healthy ear. Always check facial nerve number 7, may be damaged during surgery – will show facial drooping if damaged Nursing Interventions for Patients having Ear Surgery (pg. 1816) Reduce anxiety Relieve pain - after surgery, intermittent, sharp pain is ok, but if they are having throbbing, constant pain it is NOT ok and should be reported ASAP Prevent complications – check CBC, chemistries, bleeding tendencies (PT, PTT, INR) Prevent infection - antibiotics prophylactically, prevent water getting into the ear canal for six weeks after surgery (cotton ball/Vaseline) Improve hearing and communication – decrease noise, face pt when speaking to them, speak clearly, have good lighting; might not be able to hear immediately after surgery; establish other ways of communication; do not scream 12 Prevent injury – inner ear – place for balance and hearing, so surgery can affect their balance; vertigo; assist them when they first get up or tell them to get up slowly and sit on the side of the bed before going anywhere Prevent altered sensory perception – hearing will be affected Promote home care – teach them to sneeze with their mouth open, cannot blow their nose for three weeks, no heavy lifting = prevents pressure on the ears, no water in the ear canal for 6 weeks __________________________________________________________________________________________ Allergic Disorders (Ch. 53, pg. 1606) Allergy is an inappropriate, often harmful, response of the body’s immune system to a normally harmless substance(s); substances = allergens Allergens - dust, weeds, pollen, dander, medication, etc. Chemical Mediators are released in allergic reactions, which is what causes the allergic reaction. May produce mild to life threatening symptoms. **The allergen causes you to do that; th chemical mediators is what is released that may cause the problem; it’s not the allergen itself, it’s the chemical mediators that cause the reaction. Allergy Pathophysiology - allergens encounter antigens, which cause a series of events to render the foreign invaders harmless, when lymphocytes respond, antibodies are formed Antibodies - combine with antigens like a lock and key, with only one key that fits a certain lock. Once antibodies are formed, they initiate immunoglobulins Immunoglobulins (pg. 1607) •IgE – these are the ones involved in allergic disorders; found in lymph nodes, tonsils, appendix, blood, and intestinal tract •IgD, IgG, IgM, IgA Types of Allergens Airborne - pollen, dust, smokes, fumes, perfumes, dander Ingested - food, medications Contact - stings, latex, allergy testing or shots, dyes, oils, poison ivy, poison oak Allergic Reactions Hypersensitivity – excessive immune response to any stimulus; Doesn’t usually react at the first exposure – it follows after a buildup of antibodies. 4 Types of Reactions (pg. 1609) Type I – Anaphylactic – very common o Most severe, explosive onset; you’re fine one minute…the next minute you’re not o Usually have edema in the larynx = breathing trouble > respiratory collapse > cardiovascular collapse > death o Hypotension, bronchospasms, and cardiovascular collapse o Increased heart rate, decreased BP o Immediate reaction, beginning within minutes of exposure o Treated with EPINEPHRINE; given injection (if they come in ER w/o IV access), then IV Antihistamine (diphenhydramine) Steroids 13o Ex: allergic rhinitis, asthma, severe allergic response to latex or penicillin; food; medications o Ex: pt comes into ER having an anaphylactic reaction, you give Epi, put them on O2, given them a steroid, given an antihistamine, given fluids, observe for a couple of hrs…let them go home? NO! About 6 hrs later, they have rebouce (they have it all over again); they are admitted for observation for at least 24hrs o Most common cause of anaphylactic reaction = medications Penicillin allergy – give ciprofloxacin, floroquinolones, erythromycin No –cillin medications (Ex: amoxicillin) No cephalosporins – b/c of cross contamination Type II – Cytotoxic – attack on the normal body as foreign, leading to cell and tissue death. o Ex: myasthenia gravis, blood transfusion reaction, hemolytic anemia, immune complex Type III – Immune Complex – phagocytic action depositing immune complexes in joints and kidneys resulting in tissue injury o Ex: Lupus, RA, nephritis, and bacterial endocarditis Type IV – Delayed – most common, mostly delayed response it to medication and food, hypersensitivity usually 24-72 hrs after exposure o Ex: contact dermatitis (poison oak/ivy), tape, latex, poison ivy Assessment and Diagnostics History and Physical History - what kind of reaction? Symptoms? Physical - Rashes and lesions? Redness? Edema? Ecchymosis? Diagnostics CBC – WBC will be elevated if they are allergic, but we want to look at the eosinophils (if there is an esophonophil count on CBC = allergic reaction); WBC count between 5 and 15 Total serum IgE, not as sensitive as other tests, but can be helpful in diagnosing. Skin Tests – (pg. 1609) – allergy skin test; most definitive test, they inject the medication = the pt gets a wheal and a flare = normal reaction of the body; positive wheal and flare is clinically significant usually intra-dermal or superficial application; o If in doubt may require a RAST test – usually done on the back to reduce sensitivity; inject medications; must have a crash cart available = if they have an anaphylactic reaction, you have to medicate them; testing in not done during bronchospasms; need to stop antihistamine and steroids 48-96 hrs prior to testing. A positive test is a 3+ wheal or 1.5 localized erythema. Best time to do RAST testing is in the winter time b/c they can go longer periods of time w/o their steroids and antihistamines Anaphylaxis - substances that usually cause it are foods, medications, stings, and latex – avoid it, stay away from it Causes: o Food –nuts, shellfish, eggs, and milk o Meds - penicillin, contrast dye, Aspirin, NSAIDs, antibiotics, blood transfusions Need to keep an epi pen with them at all times Primary prevention is AVOIDANCE 14 Give EPI FIRST Their airway will be compromised, so secure a patent airway – before CPR or anything like that. Treated with EPI and IV fluids and antihistamines If the allergen is something that you are infusing (Blood, IV Antibiotics) - STOP it, start NS, flush it and have someone call the MD, don't keep giving it to them the allergen These people need to be monitored closely for 12-14 hrs after you have treated them because they may develop rebound anaphylaxis o Latex Prevention: avoid the food Education: carry an Epi pen Blood transfusion reaction: stop the transfusion, disconnect the line, start new like w/NS, send the tubing to the lab to be tested __________________________________________________________________________________________ Allergic Rhinitis - Aka “hay fever” or seasonal allergies Symptoms are benign Happens at the same time every year, spring-tree pollen, summer-grass pollen, and fall-rag weed Most common respiratory allergy Increases with age Allergen gains access to the nasal passages, causes edema, histamine is released, you start coughing/sneezing/itchy throat You get a sensitization, nasal edema, and then the histamine is released when exposed to Manifestations Cough and sneeze, nasal congestion, and an itchy throat Treatment (pg. 1617 – 1620) Avoid it, use air purifiers, removal of dust, don’t use down pillows, avoid smoke or whatever the trigger is, take a shower at night before you go to bed because the pollen is on your hair/clothes, lay on pillow, every time you roll over you are breathing in the pollen Antihistamines – major side effect is sedation - make you sleepy and drowsy o Antihistamines – Contraindicated in third trimester of pregnancy and nursing mothers, newborns and children, elderly, people with asthma, open angle glaucoma, and hypertension o Teach to use a humidifier because they dry nasal passages up No humidifier? = Water in a little bowel (place it beside bed or under bed when sleep at night; after 3-4 days the water will start evaporating; refill it) Antihistamines w/ decongestants o Contraindicated in pts w/ HTN Nasal sprays may take up to a week for you to get any benefit – recommended prior to seasonal allergies starting; start it a week before allergy fare ups Corticosteroids o Cause major nose bleeds o Will cause dry nasal mucosa o Itching and burning of nasal passages o May use oral steroids short term, in tapered doses. Do not stop abruptly. o Side effects - weight gain, fluid retention, elevated blood sugars or blood sugar swings Inhalers – for daily use; after using the inhaler, ask pt to rinse their mouth o Inhalers w/steroids can cause thrust Immunotherapy are allergy shots, 15o Most effective with ragweed pollen o Also good with grass or tree pollen, cat dander, dust o Should be done in doctor’s office or clinic b/c they can have an anaphylaxis reaction (no one has epi at home) __________________________________________________________________________________________ Contact Dermatitis (Wong, ch. 30, pg. 1074, Brunner pg. 1623) Can be acute or chronic Poison ivy, poison oak Inflammation due to exposure or contact with chemicals or allergens Manifestations Itching, burning, fluid filled lesions, vesicles, erythema, edema Treatment Removal of what caused the exposure Treatment: topical antihistamines and steroids If severe – treat with topical antihistamines and steroids (PO, short term) for seven days __________________________________________________________________________________________ Atopic Dermatitis (Wong pg. 1086, pg. 1623 Brunner) Very common in children Dry, itchy skin AKA: eczema Teach parents to use mild detergent, cotton fabrics, humidify the air, keep temp between 68-72 degrees (as cool as possible), may give a little antihistamines, use daily moisturizers, and topical steroids If they have open lesions (from scratching during exacerbations), the patient cannot have any flu shots or immunizations __________________________________________________________________________________________ Dermatitis Medicamentosa (pg. 1624-1625) Drug reaction with sudden skin rash Sudden onset of skin rash that is caused by medications (that they have taken for a long time) Treatment Discontinue medication and inform all HCP of the reaction It’s usually due to an ABX ________________________________________________________________________________ Urticaria and Angioneurotic Edema Urticaria - hives that itch Angioneurotic edema Lesions over the entire back, they do not pit (pit: touch it and turns white); these stay red, diffuse swelling of face, lips, hands, and tongue Usually due to penicillin and ace inhibitors Treatment: o If they don't get there early enough to be tubed, have to trach them o Epinephrine, antihistamines, and corticosteroids 16 In ICU for several days ________________________________________________________________________________ Food Allergy Common Causes Tree nuts, peanuts, shell fish, legumes, peas, beans, licorice, eggs, wheat, chocolate, milk, berries Tree nuts and peanuts – children have the most severe reaction Can be mild or severe allergy Can start off mild, but continued exposure or eating the food will make the reaction worse Signs and Symptoms Uticaria (hives) Wheezing, coughing Itching of the tongue, pallet, mouth Treatment Avoid that food Corticosteroids, antihistamines, Epi __________________________________________________________________________________________ Latex Allergy Latex is made from a natural rubber protein allergy from the sap of a rubber tree Number one group at risk – health care workers, kids w/myelomingeocele Cross reactions - kiwi, bananas, papaya, pineapple, mango, avocado, passion fruit, and chestnuts o Pt may think they’re allergic to the fruit b/c when they eat it, they have s/s o If a person is allergic to latex, they may be allergic to the foods as well (but not necessarily) Signs and symptoms Erythema Puritus Urticaria Wheezing, dyspnea Laryngeal edema, bronchospasm Tachycardia, hypotension, cardiac arrest Treatment EPI pen Patients should wear medical ID that states that they are allergic to latex If having surgery, inform the physician; they have to go FIRST, because the room has to be prepped/decontaminated latex-free __________________________________________________________________________________________ Dermatologic (skin) Disorders (Brunner, ch. 56, pg. 1676) Primary Goals o Prevent additional damage o Prevent secondary infection 17o Reverse the inflammatory process o Relieve the symptoms Nursing Care o Administration of topical and systemic medications o Wound care and dressing o Proper hygiene o Address emotional and psychological needs of the pt __________________________________________________________________________________________ Infectious Diseases of the Skin (Brunner, pg. 1687 / Wong, ch. 30, pg. 1069-1070) Bacterial Impetigo – superficial infection of the skin and is highly contagious Usually caused by strep, staph, or multiple bacteria Towels and utensils are #1 cause of contamination, causing the spread of the infection o Wash in extremely hot water w/bleach Common in children; going to daycare Excess use of antibacterial soap may be a questionable cause or may contribute to the problem Has nothing to do w/hygiene nor socioeconomic status Manifestations Start as small red macules that turn into vesicles that rupture and have a honey yellow crust Treatment Systemic antibiotics usually penicillin = best treatment If area is small, treat with mupirocin – topical antibiotic. Apply 7 times a day for 7 days; wash the old off and put the new on = usually not adhered to Contact precautions = gloves Wash utensils and towels, with hot water, and toys in hot water but with no bleach __________________________________________________________________________________________ Folliculitis (pimple) – an infection originating in the hair follicle Cause is usually staph Usually on face, legs, axillae, trunk, and buttocks Usually due to staph No picking or squeezing o When you pop it, half of the infection comes out and the other half is pushed further down into the tissue Treatment: antibiotic = Keflex (allergic to cephalosporine? > V-pack) __________________________________________________________________________________________ 18Furuncle (aka “boil”) (Brunner, pg. 1688, Wong, pg. 1070) – an infection deep in the hair follicle and surrounding tissue Prevalent in areas of irritation, pressure, friction, and excessive perspiration Cause is usually staph Appears as a painful nodule Has a yellow or black center several days after nodule appears Develops from pick and popping the folliculitis; when a pimple is popped, half of the infection comes out and the other half is pushed further down into the tissue Folliculitis leads to a boil (if it is popped); when the furuncle comes to a head…you squeeze it and it turns into a carbuncle. __________________________________________________________________________________________ Carbuncle (“multiple boils”) is an abscess of the skin and subcutaneous tissue Cause - staph Prevalent in hot climates It can start as folliculitis, but we create a carbuncle! Manifestations Pt appears ill and has a fever, pain, leukocytosis, and an infection may enter the bloodstream; b/c we have pushed all the infection further in the skin Wherever the carbuncle is, it can cause symptoms o Ex: on the jaw: may have pain talking or eating; on your butt: may hurt to sit o Wherever it is, assess and see if it is causing any other problems Treatment for Folliculitis, Furuncle, and Carbuncle: Systemic antibiotics Warm moist compresses May require surgical intervention, I &D-incision and drainage Educate patient not to rupture the abscess Pts that are immunocompromised are at greater risk for developing these conditions Teaching: Don’t pop it, squeeze it, or scratch it Use compress to bring it to a head by itself and it’ll rupture by itself __________________________________________________________________________________________ Herpes Zoster (aka “shingles”) (Brunner, pg. 1689, also Wong, pg. 1072) An infection caused by the varicella-zoster virus Dormant chicken pox virus inside the nerve cells near the brain and spinal cord Prevalent in Caucasian population and in immunocompromised patients (AIDS, cancer) Manifestations Pain first, then a rash along a nerve route; burning, stabbing, aching, with tenderness and itching o If its around the eye = medical emergency = need to be referred to an ophthalmologist ASAP 19o They can go blind Eruption of grouped, red vesicles that rupture and crust Vesicles are usually unilateral in the thoracic, cervical, or cranial nerve areas in a band-like configuration (they follow the path of nerves) Course of illness - one to three weeks Healing – can take from 7 days to a month Complication Post-herpetic neuralgia with pain and numbness that lasts up to 6 months Gabapentin used for ^^ for neuropathy Treatment Goal is to relieve pain and to reduce or avoid complications Oral antivirals: (pg. 1689) o Acyclovir o Valacyclovir o Famciclovir Antivirals should be started within 24 hours after the rash has occurred to decrease the number of lesions, but it does not decrease the severity 50/50/50 rule – within 50 hours, 50 years of age or greater, 50 lesions or more Side effects are headache, N/V, diarrhea, joint pain, malaise, fatigue Corticosteroids Analgesics Vaccine for 55 years old and older, few side effects, good results Ophthalmic herpes is a medical emergency and need referral to ophthalmologist immediately because they can lose their vision __________________________________________________________________________________________ Infectious Diseases of the Skin Herpes Simplex has 2 types: (pg. 1690) Herpes Simplex I – mouth (orolabial) Herpes Simplex 2 – genital Both types can be found in either area Herpes Simplex 1 Orolabial – aka “fever blisters” or “cold sores” Erythematous clusters of grouped vesicles found on the lips May feel some burning or itching 24 hours before the vesicles appear Triggers – increased stress and sunlight. Teach people not to share lipstick, drinks or utensils. Use proper hand hygiene. Treatment Usually topical If severe, will be given an oral antiviral (to be taken 5 x a day) Herpes Simplex 2 (Brunner, pg.1690, Ch. 47, Wong, pg. 548) 20 Genital Grouped vesicles on the vagina, rectum or penis Classified as an STD Recurrent and lifelong No cure – you may not have signs and symptoms but you always have Herpes Simplex 2. Treatment (pg. 1691) Antivirals – helps to suppress the development of reoccurrence by 85% Teach: Must take Rx antivirals to prevent spread, use of condoms If a mother has it and is pregnant she has to have a C-Section to prevent spreading to the newborn __________________________________________________________________________________________ Non-Infectious Inflammatory Dermatoses (Brunner, pg. 1694/Wong pg. 1085) Psoriasis One of the most common skin diseases Hereditary More common between ages 15 to 35 Immunologic disease that comes and goes; worse in the winter time Triggers – stress, anxiety, trauma, infection, seasonal or hormonal changes Patho - basal layer cells replicate quickly and they surface to become red, scaly plaques Red patches of skin covered in silvery/white scales, if the scales are removed, it reveals a dark red base with bleeding Usually manifests bilaterally Seen on scalp, elbows, knees and lower back There is no cure It can be a complication of Rheumatoid arthritis of multiple joints Treatment (pg. 1695) Biological modifiers (etanercept, infliximab): make you immunocompromised; suppresses the immune system; risk for infection Topical steroids Methotrexate – can be toxic to liver, kidneys, and bone marrow o Must have CBC, liver function tests, BUN, creatinine o Teach that it’s a chemotherapy agent and no alcohol can be consumed while on this o Can be harmful to fetus __________________________________________________________________________________________ Stevens – Johnson Syndrome and Toxic Epidermal Necrolysis (TEN) (Brunner, pg. 1702/Wong pg. 1085) Both are potentially fatal skin disorders Mortality rate up to 35% Triggered by medication reactions antibiotics, Sulfonamides, NSAIDS, or anti-seizure medications Manifestations 21 Fever, headache, malaise, flu-like symptoms Rapid onset of large flaccid-looking boil (like little water balloons) that rupture, sheets of skin start shedding off They may lose so many sheets of skin that they can lose their finger nails and toe nails and eye lashes (looks like scalded skin – it’s called “scalded skin syndrome”) o May lead to infection and electrolyte disorders – due to the shedding of large sheets of skin o The skin is a barrier that helps you keep electrolytes and fluids Treatment IV fluids IV immunoglobulins, Topical antibiotic agents Pain management Systemic antibiotics __________________________________________________________________________________________ Skin Cancer (Brunner pg. 1706) Most common cancer in US Leading Cause – sun exposure, tanning beds Diagnosis by biopsy and histologic evaluation Population at risk – fair hair, fair skinned, blue eyed people; they don't tan = they burn Pg. 1706, chart 56-5 Basal Cell Carcinoma Most common Appearance – small waxy nodule with rolled, translucent borders (can’t see the border) Raised lesions May have vessels that come out from it Face is most common site Recurrence is common, but rarely metastasizes Squamous Cell Carcinoma Most common Appearance - rough looking, kind of thick, scaly, blackish center Raised lesions Common Sites – upper extremities, face, lip, ears, nose, forehead = most exposed areas o Wear hats and SPF on the face and ears daily Invasive cancer Malignant Melanoma Most lethal Incidence more common in men, 24-45 years in age Incidents and mortality (death) is increasing 22 Population at risk – fair haired, fair skinned, blue eyes, freckles, burn and don't tan, have had a history of at least one incident of sun burn or sun poisoning, or tanning bed exposure at least 10 times a year Appearance - flat irregular borders, brown and black in color Treatment is wide surgical excision and may need skin grafting – b/c it is so invading; plus radiation and chemo Surgery has to remove skin from a wide border around the area and makes recovery painful = take muscle tissue? Even more painful! Skin Cancer Treatment Surgical Excision – they go in excise the lesion and look to see if it has invaded any other tissue Electrosurgery –burning it off Cryosurgery – freezing it Radiation Therapy – after skin cancer, especially after malignant melanoma Prevention of Skin Cancer (Brunner, pg. 1711) SPF – 15 or higher everyday Avoid sun exposure between 10-3 Lip Balm - SPF of 15 or higher Avoid tanning beds Educate using “ABCDE” o A=asymmetry (doesn't match if folded over itself) o B=borders irregular o C=color changes (Ex: that mole has changed colors) o D=diameter (greater than 6mm or the size of a pencil eraser) o E=evolving over time (Ex: I’ve had this for a long time, but it keeps changing; “it’s getting bigger”) [Show More]
Last updated: 1 year ago
Preview 1 out of 23 pages
Reviews( 0 )
Document information
Connected school, study & course
About the document
Uploaded On
Mar 11, 2021
Number of pages
23
Written in
Additional information
This document has been written for:
Uploaded
Mar 11, 2021
Downloads
0
Views
77

.png)
.png)
How Do Geographically Dispersed Teams Collaborate Effectively Paper.png)