*NURSING > Final Exam Review > NR509 Group Final Exam/NR 509 Final Exam Study Guide. (All)
NR509 Group Final Exam/NR 509 Final Exam Study Guide.
Document Content and Description Below
NR509 Group Final Exam/NR 509 Final Exam Study Guide.Chamberlain College of Nursing - NR 509 NR509 Group Final Exam/NR 509 Final Exam Study Guide. Chapter 5 Ashley (1-6)/ Catlin (7-9) Behavior/Me... ntal Health Assessment and Modification for Age -Unexplained conditions lasting >6weeks should prompt screening for depression, anxiety, or both -PRIME-MD (Primary Care Evaluation of Mental Disorders). 26 questions and take 10 minutes to complete. Used for the 5 most common=anxiety, depression, alcohol, somatoform, and eating disorders. -Patient indications for Mental Health Screening: 1.Medically unexplained physical symptoms-more than half have depression and anxiety disorders 2. Multiple physical or somatic symptoms or high symptom count 3.High severity of the presenting somatic symptoms, chronic pain 4.Symptoms for more than 6 weeks 5. Physician rating as a ―difficult encounter‖ 6. Recent stress 7.Low-self rating of overall health 8.Frequent use of health care services 9.Substance abuse. -CAGE=substance-related and addictive disorders Modification for Age Elderly: -Complain of memory problems but usually is due to benign forgetfulness -Retrieve and process data more slowly and take longer to learn new information -Slower motor responses and their ability to perform complex task may diminish -Important to distinguish age-related changes from manifestations of mental disorders -More susceptible to delirium which can be the first sign of infection, problems with medications, or impending dementia Infant: Assess mental status of a newborn=observing newborn activities 1.Look at human faces and turn to parents voice 2.Ability to shout out repetitive stimuli 3. Bond with caregiver 4.Self-soothe Normal VS. Abnormal Findings and Interpretation -Mood disorders: compulsions, obsessions, phobias, and anxieties -Lethargic: drowsy, but open their eyes and look at you, respond to questions, and then fall asleep. -Obtunded: open their eyes and look at you, but respond slowly and are somewhat confused. -Agitated depression: crying, pacing, and hand-wringing -Depression: the hopeless slumped posture and slowed movements.-Grooming and personal hygiene may deteriorate: Depression, schizophrenia, and dementia -Manic Episode: the agitated and expansive movement of a manic episode -Obsessive-Compulsive Disorder: Excessive fastidiousness -Lesion parietal cortex: one side neglect in the opposite parietal cortex, usually in the nondominant side -Parkinsonism: facial immobility -Paranoia: anger, hostility, suspiciousness, or evasiveness -Mania: Elation and euphoria -Schizophrenia: flat affect and remoteness -Apathy (dull affect with detachment and indifference): dementia, anxiety, and depression -Hallucination: schizophrenia, alcohol withdrawal, and systemic toxicity -Amnestic Disorders: impaired memory or new learning ability and reduce social or occupational functioning, but lack the global features of delirium and or dementia. Anxiety and depression, and intellectual disability may also cause recent memory impairment. -Calculating ability: poor performance = dementia or aphasia -Variations and abnormalities in thought processes: 1.Circumstantiality: The mildest thought disorder, consisting of speech with unnecessary detail, indirections, and delay in reaching the point. Some topics may have a meaningful connection -Occurs in people with obsessions 2. Derailment: Tangential, speech with shifting from topics that are loosely connected or unrelated. The patient is unaware of the lack of association -Schizophrenia, manic episodes, and other psychotic disorders 3.Flight of ideas, an almost continuous flow of accelerated speech with abrupt changes from one topic to the next. Changes are based on understandable associations, play on words, or distracting stimuli, but ideas are not well connected. -Manic episodes 4.Neologisms: invented or distorted words, or words with new and highly idiosyncratic meanings -Schizophrenia, psychotic disorders, and aphasia 5.Incoherence: Speech that is incomprehensible and illogical, with lack of meaningful connections, abrupt changes in topic, or disordered grammar or word use. Flight of ideas, when severe, may produce incoherence -Schizophrenia 6.Blocking: Sudden interruption of speech in mid sentence or before the idea is completed ―losing the thought‖ -Schizophrenia 7.Confabulation: Fabrication of facts or events, to fill in the gaps from impaired memory -Korsakoff syndrome from alcoholism 8.Perseveration: persistent repetition of words or ideas -Schizophrenia or other psychotic disorders 9. Echolalia: Repetition of the words and phrases of others -Manic episodes or Schizo 10.Clanging: Speech with choice of words based on sound, rather than meaning, as in rhyming and punning. Example: ―look at my eyes and nose, wise eyes and rosy nose. To to one, the ayes have it!‖ -Schizo and manic episodes Abnormalities of Perception1. Illusions: misinterpretations of real external stimuli, such as mistaking rustling leaves for the sounds of voices -Grief, delirium, PTSD, Schizo 2.Hallucinations: Perception-like experiences that seem real but, unlike illusions, lack actual external stimulation. The person may or may not recognize the experiences as false. May be auditory, visual, olfactory, gustatory, tactile, or somatic. -PTSD, Schizo, delirium, dementia, alcoholism Abnormalities of Thought Content 1.Compulsions -repetitive behaviors feel driven to perform in response to an obsession (anxiety disorders) 2.Obessions -Recurrent persistent thoughts, images, or urges 3.Phobias -Persistent irrational thoughts, compelling desire to avoid provoking stimulus 4.Anxieties 5.Feelings of unreality 6.Feelings of Depersonalization 7.Delusions Erotomanic: the belief that another person is in love with the individual Somatic: involves body functions Unspecified: includes delusions of reference without a prominent persecutory or grandiose component Speech Patterns -Slow speech: depression -Accelerated speech: mania -Articulation: are the words clear and distinct: does the speech have a nasal quality -Dysarthria: defective articulation ―slurred speech‖ -Dysphonia: results from impaired volume, quality, or pitch of voice. Difficulty speaking due to a physical disorder of the mouth, tongue, throat, or vocal cords. -Aphasia: the loss of ability to understand (receptive/Wernicke) or express speech (expressive/Broco aphasia) -Brocas aphasia: patients articulate very slowly and with a great deal of effort. Nouns, verbs, important adjectives are usually present and only small grammatical words are dropped from speech "Well…..cat and…..up……..um, well, um…forget it" -Wernicke's aphasia the patient can speak effortlessly and fluently, but his words often make no sense ―the coffee cat looks crazy still‖ -Cerebrovascular infarction -Fluency: fluency reflects the rate, flow, and melody of speech and the content and use of words. Abnormalities -Hesitancies and gaps in the flow and rhythm of words -Disturbed inflections, such as monotone -Circumlocutions: phrases or sentences are substituted for a word the person cannot think of. Example ―what you write with for ―pen‖ -Paraphasia: malformed, wrong, or invented -Testing for Aphasia -Word comprehension: ask the patient to follow one-stage commands such as ―Point to your nose‖-Repetition -Naming -Reading comprehension -Writing Mental Status Examination Brief test used to screen for cognitive dysfunction or dementia, and follow the patients course over time. 1. Orientation 2.Short-term memory-retention/recall 3.Language 4.Attention 5.Calculation 6.Constructive Praxis Example of findings that suggest dementia: ―The patient appears sad and fatigued; clothes are wrinkled. Speech is slow and words are mumbled. Thought processes are coherent, but insight into current life reverses is limited. The patient is oriented to person, place, and time. Digit span, serial 7s, and calculations accurate, but responses delayed. Clock drawing is good. Screening for Depression High Yield Screening Questions for office practice: 1. over the past 2 weeks, have you felt down, depressed, or hopeless? 2. Over the past 2 weeks, have you felt little interest or pleasure in doing things (anhedonia)? Symptoms of depression: low self-esteem, loss of pleasure (anhedonia), sleep disorder, difficulty concentrating. Depression tends to be long-lasting and can recur. Suicide is the second leading cause of death among 15-24 year old. Suicide rate are the highest among those ages 45 to 54, followed by elderly adults 85 years old or older. 90 % of suicide is non-hispanic whites. Other symptoms of depression: headaches, muscle aches, fatigue Generalized Anxiety Disorder -Most common mental disorder in primary care - High Yield Screening Questions for office practice: 1. Over the past 2 weeks, have you been feeling nervous, anxious, on edge, unable to stop or control worrying? 2. Over the past 4 weeks, have you had an anxiety attack-suddenly feeling fear or panic? You can screen for core anxiety symptoms by asking the first two questions from the 7- item generalized anxiety disorder (GAD) scale. Scores on this GAD subscale range from 0 to 6; a score of 0 suggests that no anxiety disorder is present. A score of 10 on the GAD-7 identifies GAD; scores of 5, 10, and 15 represent mild, moderate, and severe levels of anxiety. Depressive DisordersDepression and anxiety disorders are a common cause of hospitalization in the United States, and mental illness is associated with increased risks for chronic medical conditions, decreased life expectancy, disability, substance abuse, and suicide. About 19million adult American or almost 7% have major depression with other coexisting anxiety disorder or substance abuse. Depression is as common in women as men, and the prevalence of postpartum depression is about 7% to 13%. Most patients with chronic medical conditions have depression. Symptoms of depression in high-risk patients may be subtle and may include; 1. Low self-esteem 2. Loss of pleasure in daily activities (Anhedonia) 3. Sleep disorder, 4. Difficulty concentrating or making decisions. Look carefully for symptoms of depression in vulnerable patients, especially those who are young, female, single, divorced or separated, seriously or chronically ill, bereaved, or have other psychiatric disorders, including substance abuse. A personal or family history of depression also places patients at risk. Asking two simple questions about mood and anhedonia appears to be as effective as using more detailed instruments. All positive screening tests warrant full diagnostic interviews. Failure to diagnose depression can have fatal consequences—the presence of an affective disorder is associated with an 11-fold increased risk for suicide. Depression screening 1. Over the past 2 weeks, have you felt down, depressed, or hopeless? 2. Over the past 2 weeks, have you felt little interest or pleasure in doing things (anhedonia)? Depression tends to be long-lasting and can recur. Because of these two factors, a waitand-see approach to treatment is not desirable and timely treatment is necessary. Schizophrenia 1. Grooming and personal hygiene may deteriorate 2. flat affect and remoteness 3. Hallucinations: lack actual external stimulation 4. Derailment: Tangential, speech with shifting from topics that are loosely connected or unrelated. The patient is unaware of the lack of association. 5. Neologisms: invented or distorted words, or words with new and highly idiosyncratic meaning 6. Incoherence: Speech that is incomprehensible and illogical, with lack of meaningful connections, abrupt changes in topic, or disordered grammar or word use. 7. Flight of ideas, when severe, may produce incoherence 8. Blocking: Sudden interruption of speech in mid sentence or before the idea is completed ―losing the thought‖ 9. Clanging :speech with choice of words based on sound, not meaning 10. Echolalia: repetition of the words and phrases 11. Illusions: mistinterpretations of real external stimuli (mistaking rustling leaves for the sound of voices) 12. Usually occurs in late teens, early 20s (college students, common psych break) 13. Commonly seen in other family membersSuicide Risk and Prevention Protective factors buffer individuals from suicidal thoughts and behavior. To date, protective factors have not been studied as extensively or rigorously as risk factors. Identifying and understanding protective factors are, however, equally as important as researching risk factors. Protective Factors ● Effective clinical care for mental, physical, and substance abuse disorders ● Easy access to a variety of clinical interventions and support for help seeking ● Family and community support (connectedness) ● Support from ongoing medical and mental health care relationships ● Skills in problem solving, conflict resolution, and nonviolent ways of handling disputes Cultural and religious beliefs that discourage suicide and support instincts for selfpreservation Suicide is the second leading cause of death among 15- to 24-year olds. Suicide rates are highest among those ages 45 to 54 years, followed by elderly adults ≥age 85 years. Men have suicide rates nearly four times higher than women, though women are three times more likely to attempt suicide. Men are most likely to use firearms to commit suicide, while women are most likely to use poison. Overall, suicides in non-Hispanic whites account for about 90% of all suicides. American Indian/Alaska Native women ages 15 to 24 years have the highest suicide rates of any racial/ethnic group. Substance Use Disorders, Including Alcohol and Prescription Drugs. The harmful interactions between mental disorders and substance use disorders also present a major public health problem. Rates of drug-induced deaths continue to increase and are highest among whites and American Indian/Alaska Natives. The Centers for Disease Control and Prevention reports that prescription drugs have replaced illicit drugs as a leading cause of drug-induced deaths. Every patient should be asked about alcohol use, substance abuse, and misuse of prescription drugs Suicide Risk and Prevention Risk Factors ● Family history of suicide ● Family history of child maltreatment ● Previous suicide attempt(s) ● History of mental disorders, particularly clinical depression ● History of alcohol and substance abuse ● Feelings of hopelessness ● Impulsive or aggressive tendencies ● Cultural and religious beliefs (e.g., belief that suicide is noble resolution of a personal dilemma) ● Local epidemics of suicide ● Isolation, a feeling of being cut off from other people ● Barriers to accessing mental health treatment ● Loss (relational, social, work, or financial) ● Physical illness● Easy access to lethal methods ● Unwillingness to seek help because of the stigma attached to mental health and substance abuse disorders or to suicidal thoughts Chapter 9 & 12 Kailey/Jenna Cardiac/Vascular Assessment and Modification for Age Normal VS. Abnormal Findings and Interpretation -Acute aortic dissection: anterior chest pain, often tearing or ripping and radiating into the back or neck. -Sudden dyspnea: PE, PNEUMO, and anxiety -PMI (point of maximal impulse) APEX OF THE LEFT VENTRICLE identified during palpation of the precordium, locates the left border of the heart and is normally found in the 5th intercostal space at or just medial to the left midclavicular line (or 7 to 9 cm lateral to the midsternal line). Normal diameter 1 to 2.5 cm. The left ventricle, behind the RV and to the left, forms the left margin of the heart, its tapered inferior tip is often termed the cardiac apex which produces the apical impulse, identified during palpation of the precordium as the PMI. Abnormal PMI 1. Situs inversus and dextrocardia->PMI located at the right side of chest 2. PMI>2.5cm-> left ventricular hypertrophy from HTN or aortic stenosis causing pressure overload in the left ventricle 3. Displacement of the PMI lateral to the midclavicular line or > 10 cm lateral to the midsternal line-> LVH and Ventricular dilatation from a MI or heart failure 4. COPD patients-> the PMI may be in the xiphoid or epigastric area due to right ventricular hypertrophy 5. Hyperkinetic high-amplitude=hyperthyroidism severe anemia, HTN, aortic stenosis, and aortic regurgitation 6. Sustained high amplitude- increased LVH from HTN Cardiac chambers, valves, and circulation 1. AV valves= Mitral and Tricuspid (based on location) 2. Semilunar valves= Aortic and Pulmonic (based on half-moon shape) 3. S1 & S2=vibrations emanating from the leaflets, the adjacent cardiac structures, and the flow of blood. 4. S1=Closure of the mitral valve 5. s2=Aortic valve closure 6. S2 split= Closure of aortic valve and then pulmonic valves, best heard over the pulmonic area with the bell of the stethoscope 7. S3 & S4= Heart failure or acute myocardial ischemia 8. S3=caused by rapid deceleration of blood against the ventricular wall 9. S4= increased left ventricular end diastolic stiffness which decreases compliance 10. Systolic blood pressure=maximal left ventricular pressure 11. Diastole= left ventricular pressure continues to drop and falls below left atrial pressure. The mitral valve opens, event usually silent but may be audible if valve leaflet motion to restricted (mitral stenosis)12. Right ventricle is the chamber that you can assess by palpation since it occupies most of the anterior surface of the heart. Events in the Cardiac Cycle 1. Systole= Ventricular contraction 5mm HG to 120 mm HG. Blood ejected into Aorta. Aorta valve open and mitral closed. 2. Diastole= Ventricular relaxation blood flows from atrium to ventricular. Aorta valve closed, and mitral valve open. Normal JVP: 3 cm above the sternal angle, in patients with obstructive lung disease, JVP can appear elevated on expiration but veins collapse on inspiration. 1. Jugular venous pressure-reflect right atrial pressure which in turn equals central venous pressure and right ventricular end-diastolic pressure.Lies deep in SCM muscles. Abnormal JVP: falls with loss of blood or decreased venous vascular tone and increases with right or left heart failure, HTN, tricuspid stenosis, AV dissociation, increased vascular tone, and pericardial compression or tamponade. Jugular Venous Pulsations 1. A-atrial contraction, C-carotid transmission, V-venous filling 2. Abnormally prominent waves occur: increased resistance to right atrial contraction, tricuspid stenosis, 1st/2nd/3rd degree AVB, SVT, junctional tachycardia, pulmonary HTN, pulmonic stenosis. 3. Absent a waves=A FIB 4. Systolic phenomenon is the X descent 5. Increased V waves=occur in tricuspid regurgitation, atrial defects, and constrictive pericarditis. 6. Abnormal: >3 cm above sternal angle (NOT NOTCH) or > 8 cm above right atrium, best measured at the end of expiration 7. The vertical height of the blood column in centimeters, plus 5 cm, is the JVP Carotids Characteristics: amplitude, contour, timing of upstroke in relation to S1 and S2 Normal: 2+, no bruits or thrills Abnormal: small, thready or weak in cardiogenic shock, and bounding in aortic regurgitation 1. Carotid upstroke is delayed in aortic stenosis 2. Carotid pulse mall, thready, or weak= cardiogenic shock 3. The pulse pounding= aortic regurgitation 4. Bruit-murmur like sound arising from turbulent arterial blood flow. Caused byatherosclerotic luminal stenosis 5. Carotid vs. Jugular: carotid is palpable Dextrocardia-a rare congenital transposition of the heart, the heart is situated in the right chest cavity and generates a right-sided apical impulse.Pulsus alternans: a bigeminal pulse that varies from beat to beat, almost always indicates LV dysfunctions Paradoxical pulse: varies with respiration, greater than normal drop in BP during inspiration, suspected with cardiac tamponadeCardiovascular Risk Factors Screening - Heart Disease: long asymptomatic latent period. Assess lifetime risk in asymptomatic patients starting at age 20 since many deaths occurs from lack of prior warning signs or cardiac diagnosis. -AHA guidelines recommend screening every 2 years in patients over 20 for blood pressure, body mass index, waist circumference, and pulse -The physical examination criteria for identifying metabolic syndrome include a waist of 40 inches or greater for males, a waist of 35 inches or greater for females, and a blood pressure of 130/85 or greater (in both males and females). - Women: o CVD and CHD higher in black women then white women. o Women> 65: higher prevalence of HTN than men. o Stroke 60% deaths o Unique risk factors: pregnancy, hormone therapy, early menopause, preeclampsia. More likely to have a-fib, migraine with aura, obesity, and metabolic syndrome. - Major cardiovascular risk factors and screening frequency o Family hx of CVD o Cigarette smoking o Poor diet o Physical inactivity o Obesity (especially central) o Hypertension o Dyslipidemias: screen for men >35 and women >45 with increase risk of CHD; screen by age 20 in those who have DM, HTN, obesity, tobacco use, noncoronary atherosclerosis, or family hx of early CVD. o Diabetes: Screen at age 45 and repeat every 3 years; screen at any age when BMI >25 with additional risk factors. o Pulse o Metabolic syndrome: cluster of risk factors that increase both CVD and DM. Presence of 3 of the 5 risk factors: § Waist circumference men>102cm; women >88cm § Fasting plasma glucose: >100; or being treated for high BS § HDL cholesterol: men <40 women ;<50; or being treated § Triglycerides: >150; or being treated § BP: >130/85; or being treated Heart Disease Heart Sounds (jen) Heart Sounds - Closure of the heart valves creates a pair of audible heart sounds. - The first sound, S1, arises from closure of the mitral valve. - Tricuspid valve closure may also contribute to S1. - The second sound, S2, arises from closure of the aortic valve. - Pulmonic valve closure may also contribute to S2. - Ventricular diastole occurs between S2 and the next S1. - After the mitral valve opens, there is a period of rapid ventricular filling as blood flows early in diastole from left atrium to left ventricle. - Third heart sound: S3o In children and young adults (35-40 and last trimester of pregnancy), may arise from rapid deceleration of the column of blood against the ventricular wall. o An S3 in adults over age 40 years (an S3 gallop) is usually pathologic, arising from high left ventricular filling pressures and abrupt deceleration of inflow across the mitral valve at the end of the rapid filling phase of diastole. Causes include decreased myocardial contractility, heart failure, and ventricular volume overload from aortic or mitral regurgitation, and left-to-right shunts. o Left-side S3; heard at apex with pt on left lateral position o Right-sided S3: heard at lower left sternal border or below xiphoid with pt supine; louder on inspiration - Fourth heart sound, S4, o not often heard in normal adults, and marks atrial contraction. o It immediately precedes S1 of the next beat and can also reflect a pathologic change in ventricular compliance. o Causes of a left-sided S4 include hypertensive heart disease, aortic stenosis, and ischemic and hypertrophic cardiomyopathy. o Left-sided S4 best heard at apex in left lateral decubitus position. o Right-sided S4 heard along lower left sternal border or below xiphoid. Louder with inspiration. - The fact that diastole usually lasts longer than systole is helpful in distinguishing the two sounds. o The aortic and pulmonic valves are closed, and the mitral and tricuspid valves are open, as seen in diastole o Systole: period of ventricular contraction o Diastole: period of ventricular relaxation. o Cardiac cycle: § During systole · Aortic valve is open, allowing ejection of blood from the left ventricle into the aorta. · The mitral valve is closed, preventing blood from regurgitating back into the left atrium. · During systole the pulmonic valve opens and the tricuspid valve closes as blood is ejected from the RV into the pulmonary artery § During diastole · The aortic valve is closed, preventing regurgitation of blood from the aorta back into the left ventricle. · The mitral valve is open, allowing blood to flow from the left atrium into the relaxed left ventricle. · During diastole, the pulmonic valve closes and the tricuspid valve opens as blood flows into the right atrium A second-degree A-V block can result in a pulse rate less than 60 Auscultation of Heart Sounds - Diaphragm is better for detecting higher pitched sounds such as S1 or S2, the murmurs of aortic and mitral regurgitation, and pericardial friction rubs. - The bell is more sensitive to low-pitched sounds such as S3 or S4 and the murmur of mitral stenosis. - Correlate heart sounds with the patient‘s jugular venous pressure and carotid pulse. For example, if there is a diffuse PMI and an S3 suggesting congestive heart failure, look for an elevated JVP. - You will listen for S1 and S2 in each of the six listening areas: in the aortic area in the right 2nd interspace close to the sternum, in the pulmonic area in the left 2nd interspace close to the sternum, in the left 3rd interspace, in the tricuspid area in the left 4th and left 5th interspaces, and in the mitral area at the apex. - Note the cardiac rate and rhythm. Normally the rate is 60–100 beats per minute, and the rhythm is regular. - Identify S1 and S2, in the aortic area, S2 is usually louder than S1. - S2 is also usually louder than S1 in the pulmonic area. - Listening in the pulmonic area, identify the inspiratory splitting of S2 into its two components. o Its first component, A2, is from aortic valve closure. § A2 louder than P2 § A2 heard over precordium § P2 heard over 2nd and 3rd left interspace close to sternum. Here you search for splitting of S2.o Its second component, P2, comes from pulmonic valve closure. o This ―physiologic split‖ of S2A (aortic) and S2P (pulnomic) normally occurs during inspiration. Use the bell with light pressure over the 2nd left intercostal space to hear the s2 split best. o During expiration, however, these two components are fused into a single sound, S2. - S2 usually diminishes in intensity while S1 becomes louder as you proceed down through the 3rd interspace and into the tricuspid and mitral areas. - If patient has emphysema, listen to heart sounds in the epigastrium area. - Use bell of the stethoscope and listen along the lower left sternal border in the left 4th and 5th interspaces. Then listen at the apex. - To hear S3, S4, and the murmur of mitral stenosis, place patient in left lateral decubitus position. o This brings the left ventricle closer to the chest wall and makes low pitched sounds more audible. Then, recheck the position of the apical impulse and place the bell lightly over that location. Is there an audible S3. Now, notice how the third heart sound disappears when the bell is placed more firmly on the chest wall. Listen again with light pressure o In most adults over age 40 years, the diastolic sounds of S3 and S4 are pathologic, and are correlated with heart failure and acute myocardial ischemia. o an S3 corresponds to an abrupt deceleration of inflow across the mitral valve, and an S4 to increased left ventricular end diastolic stiffness which decreases compliance. Murmurs Heart murmurs: distinct heart sounds distinguished by their pitch and their longer duration. They are attributed to turbulent blood flow and are usually diagnostic of VALVULAR DISEASE. Identify when the murmur occurs (systolic or diastolic) by palpating the carotid artery at the same time Chest Wall Location and Origin of Valve Sounds and Murmurs R 2nd Interspace to the apex Aortic Valve Left 2nd and 3rd interspaces close to the sternum, but also at higher or lower levels Pulmonic Valve At or near the lower left sternal border Tricuspid At and around the cardiac apex Mitral Valve Midsystolic Murmurs 1. Innocent Murmur: Left 2nd to 4th interspace between the left sternal border and the apex. Minimal radiation. Grade 1 to 2, possibly 3. Soft to medium pitch. Variable quality. Usually decreases or disappears on sitting. Turbulent blood flow, probably generated by Ventricular ejection of blood into the aorta from the left and occasionally right ventricle. VERY COMMON IN CHILDREN AND YOUNGER ADULTS. Older adults= CVD 2. Physiologic Murmurs: Similar to innocent murmur. Turbulence due to temporary increase in blood flow in predisposing conditions such as anemia, pregnancy, fever, and hyperthroid Pathologic Murmurs/Midsystolic1. Aortic Stenosis: Right 2nd and 3rd interspaces. Radiation, often to the carotids, down the left sternal border, even to the apex. Sometimes soft but often loud with a thrill intensity. Medium, harash; crescendo-decrescendo may be higher at the apex for pitch. Often harsh, may be more musical at apex for quality. Heard best with patient sitting and leaning forward.Significant stenosis causes turbulent blood flow across the valve, and increased LV afterload. CAUSE: VALVE CALCIFICATION in older adults. Second most common cause: CONGENITAL BICUSPID AORTIC VALVE. 2. Hypertrophic Cardiomyopathy: 3rd and 4th IS. Medium pitch. Harsha quality. Intensity decreases with squatting and Valsalva release phase (increased venous return), increases with standing and valsalva strain phase. The carotid upstroke rises quickly, unlike aortic stenosis.The apical pulse is sustained. S2 may be single. S4 is usually present at the apex, unlike mitral stenosis. Usually benign, but can progress to syncope, ischemia, AFIB, dilated cardiomyopathy and heart failure, and increase stroke, and sudden death. Unexplained diffuse or focal ventricular hypertrophy with myocyte disarray and fibrosis associated with unusually rapid ejection of blood from the left ventricle during systole. lus and from leaflet, papillary muscle, or chordae tendineae dysfunction. 3. Tricuspid Regurgitation: Lower left sternal border, if RV pressure is high=murmur is loud a the apex and confused for mitral regurgitation. Blowing, holosystolic quality. Precordial Rock. JVP elevated. Pulsatile liver, ascites, edema. When the tricuspid valve fails to close fully in systole, blood regurgitates from RV to right atrium, producing a murmur. Common causes: RV failure and dilatation, with resulting enlargement of the tricuspid orifice, often induced by pulmonary HTN or LV failure; and endocarditis. 4. Ventricular Septal Defect: 3rd, 4th, 5th. Radiation often wide. Very loud with thrill. S2 obscured by loud sound. Larger defects cause, left to right shunts, pulmonary HTN, RV overload. Congenital abnormality. 5. Mitral valve prolapse: short, high-pitched sound in systole, followed by a murmur which increases in intensity until S2, best heard over the apex. A great test would be having pt squat, the noise will move later in systole along with the murmur Diastolic Murmurs 1. Aortic Regurgitation: use diaphragm for high pitch. Heard better when patient is upright leaning forward. Blowing decrescendo quality. Diastolic pressure drops to as low as 50 mm Hg; pulse pressure can widen to > 80.Apical pulse becomes diffuse.Corrigan pulse. Duroziez sign. Quincke pulses. The aortic valve leaflets fail to close completely during diastole, causing regurgitation from the aorta back into the left ventricle and left ventricle overload. Austin Flint. Causes: leaflet abnormalities, marfan syndrome, subvalvular abnormalities such as subaortic stenosis or an atrial septal defect 2. Aortic insufficiency: usually associated with a bounding carotid pulse 3. Mitral insufficiency: produces a murmur of equal intensity throughout systole 4. Mitral Stenosis : Apex. Little to no vibration. Low pitched rumble with presystolic accentuation. USE BELL. A FIB occurs in about a third of symptomatic patients, increasing the risk of blood clots. The stiffened mitral valve leaflets move into the left atrium in mid systole and narrow the valve openings, causing turbulence. Common causes: Rheumatic fever, which causes fibrosis, calcification, and thickening of the leaflets and commissures, and chordal fusion.6. Pulmonic Stenosis: Left 2 & 3 IS. If radiation loud, toward the left shoulder and neck. Intensity is soft to loud, if loud associated with thrill. JVP prominent a wave. The RV is often sustained. An early pulmonic ejection sound is present in mild to moderate. Severe, s2 is widely split and P2 softens. May hear a right-sided s4 over the left sternal border. Congenital disorder with valvular, supravalvular, or subvalvular stenosis. Pansystolic (Holosystolic) Murmurs 1. Mitral regurgitation: apex. Radiation to the left axilla. Intensity does not change with inspiration. Occurs when the mitral valve fails to close in systole, blood regurgitates from left ventricle to the left atrium causing the murmur and increasing LV preload=LV dilation. Causes: structural, from mitral valve prolapse, infectious endocarditis, rheumatic heart disease, collagen vascular disease. Stenotic Valve (aortic stenosis)- abnormally narrowed valvular orifice that obstructs blood flow Regurgitant Murmur-a valve allows blood to leak backward into a retrograde directionCongestive Heart Failure Orthopnea: dyspnea that occurs when lying down and improves when the patient sits up, is part of the cardiovascular review of systems and, if positive, may indicate congestive heart failure. Maneuvers to identify Murmurs and Heart Failure (jen) - Standing position: venous return to the heart decreases, as does peripheral vascular resistance. Arterial blood pressure, stroke volume, and the volume of blood in the left ventricle all decline. Squatting position: vascular and volume changes occur in the opposite direction. o These maneuvers help (1) to identify a prolapsed mitral valve and (2) to distinguish hypertrophic cardiomyopathy from aortic stenosis. - Valsalva maneuver: Used to identify hypertrophic cardiomyopathy, heart failure, and pulmonary hypertension. o The murmur of hypertrophic cardiomyopathy is the only systolic murmur that increases during the ―strain phase‖ of the Valsalva maneuver due to increased outflow tract obstruction. o Identify HF and Pulmonary HTN by using blood pressure cuff kept at 15 mmHg above SBP during Valsalva Maneuver. In patients with severe heart failure, blood pressure remains elevated and there are Korotkoff sounds during the phase 2 strain phase, but not during phase 4 release, termed ―the square wave‖ response. This response is highly correlated with volume overload and elevated left ventricular end-diastolic pressure and pulmonary capillary wedge pressure, in some studies outperforming brain natriuretic peptide o In healthy patients, phase 2, the “strain” phase, is silent; Korotkoff sounds are heard after straining is released during phase 4. - Isometric handgrip: increases systolic murmurs of mitral regurgitation, pulmonic stenosis, and ventricular septal defect; also diastolic murmurs of aortic regurgitation and mitral stenosis.- Transient Arterial Occlusion: Transient compression of both arms by bilateral blood pressure cuff inflation to 20 mm Hg greater than peak SBP augments the murmurs of mitral regurgitation, aortic regurgitation, and ventricular septal defect. Signs of heart failure on assessment: (jen) - An elevated JVP is highly correlated with both acute and chronic heart failure. It is also seen in tricuspid stenosis, chronic pulmonary hypertension, superior vena cava obstruction, cardiac tamponade, and constrictive pericarditis - In patients with obstructive lung disease, the JVP can appear elevated on expiration, but the veins collapse on inspiration. This finding does not indicate heart failure. - An elevated JVP is >95% specific for an increased left ventricular end diastolic pressure and low left ventricular EF, although its role as a predictor of hospitalization and death from heart failure is less clear. - Displacement of the PMI lateral to the midclavicular line or >10 cm lateral to the midsternal line occurs in LVH and also in ventricular dilatation from myocardial infarction (MI) or heart failure. - Pulsus alternans: Patient will have a strong pulse, then weak pulse, indicative of severe left sided HF - A diffuse apical impulse suggests left ventricular dilatation often found in congestive heart failure. - An S3 in adults over age 40 years (an S3 gallop) is usually pathologic, arising from high left ventricular filling pressures and abrupt deceleration of inflow across the mitral valve at the end of the rapid filling phase of diastole. Causes include decreased myocardial contractility, heart failure, and ventricular volume overload from aortic or mitral regurgitation, and left-to-right shunts. - In most adults over age 40 years, the diastolic sounds of S3 and S4 are pathologic, and are correlated with heart failure and acute myocardial ischemia. - Orthopnea and PND occur in left ventricular heart failure and mitral stenosis and also in obstructive lung diseasePeripheral Artery Disease PAD-refers to stenotic, occlusive, and aneurysmal disease of the abdomen aorta, its mesenteric and renal branches, and the arteries of the lower extremities, exclusive of the coronary arteries. Atherosclerotic disease leading to obstruction of peripheral arteries causing exertional claudication (muscle pain relieved by rest) and atypical leg pain; may progress to ischemic pain at rest. Usually in calf but also in the buttock, hip, thigh, or foot depending on the level of obstruction; rest pain may be distal in the toes or forefoot.PAD timing: may be brief if relieved by rest; if there is rest pain, may be persistent and worse at night. PAD aggravating factors: Exercise such as walking; if rest pain, leg elevation and bedrest. Coronary heart disease risk equivalent: peripheral arterial disease, abdominal aortic aneurysm, carotid atherosclerotic disease, and diabetes mellitus. Relief factors: Rest usually stops the pain in 1-3 min; rest pain may be relieved by walking (increases perfusion), sitting with legs dependent. Associated manifestations: local fatigue, numbness, progressing to cool dry hairless skin, trophic nails, diminished to absent pulses, pallor with elevation, ulceration, gangrene. Asymmetric BPs can be sign of: aortic dissection or coarctation/congenital narrowing of the aorta PAD risk factors: 1. > 50 2. Smoking, dm, htn, elevated cholesterol, african american, or CAD Symptom location suggests the site of arterial ischemia: 1. Buttock, hip-aortoiliac 2. Erectile dysfunction- iliac-pudendal 3. Thigh- common femoral or aortoiliac 4. Upper calf- superficial femoral 5. Lower calf- popliteal 6. Foot- tibial or peroneal Peripheral arterial disease warning signs: these symptoms suggest= intestinal ischemia of the celiac or superior or inferior mesenteric arteries 1. Fatigue, aching, numbness, or pain that limits walking or exertion in the legs; if present, identify the location. Ask also about erectile dysfunction. 2. Any poorly healing or non-healing wounds on the legs or feet 3. Any pain present when at rest in the lower leg or foot and changes when standing or supine. 4. Abdominal pain after meals and associated ―food fear‖ and weight loss 5. Any 1st degree relatives with AAA (15 %-28%) PAIN IN CALVES great indicator of PVD!!!! Upper extremity DVT- central venous catheters. Ask about arm discomfort, pain, paresthesias, and weaknesses. Most patients are asymptomatic with thrombosis detected on routine screening. Screening tool/diagnostic for all patients with suspected DVT: WELLS CLINICAL SCORE AND THE PRIMARY CARE RULERisk factors for lower-extremity peripheral arterial disease 1. > 65 year or > 50 years with a hx of dm or smoking 2. Leg symptoms with exertion 3. Non-healing wounds The ankle-brachial index: noninvasively diagnose PAD. The ABI is the ratio of blood pressure measurements in the foot an arm; values <0.9 are abnormal. Mild disease: ABI of 0.71 to 0.9. Moderate disease: ABI 0.7 and 0.41. Severe disease is ABI 0.4 or less. As the internal diameter of a blood vessel changes, the resistance changes as well...Resistance varies proportionally to the fourth power of the diameter Treatment for PAD: supervised exercise program, tobacco cessation, treatment of hyperlipidemia, optimal control of diabetes and htn, use of antiplatelet agents, meticulous foot care and well fitting shoes, revascularization. -expanding hematoma from triple A= may cause symptoms by compressing the bowel, aortic branch arteries, or ureters. -Mesenteric ischemia: food fear, weight loss, or dark stool. These symptoms suggest mesenteric ischemia from arterial embolism, arterial venous thrombosis, bowel volvulus or strangulation, or hypoperfusion. Failure to detect acute symptoms can cause bowel necrosis or death. -Atherosclerotic PAD: symptomatic limb ischemia with exertion. Ask about any pain or cramping in the legs during exertion that is relieved by rest within 10 minutes, called intermittent claudication, pain in calves. -Neurogenic claudication: Pain with walking or prolonged standing, radiating from the spinal area into the buttocks, thighs, lower legs, or feet. -Spinal stenosis: the positive likelihood ratio LR of spinal stenosis is>6 if the pain is relieved by sitting and bending forward, or if there is bilateral buttock or leg pain. Decreased arterial perfusion: hair loss over the anterior tibiae. Ask about coldness, numbness, or pallor in the legs or feet or loss of hair over the anterior tibial surfaces, and thin, shiny, atrophic skin Venous insufficiency: scaling, redness, varicosities, hyperpigmentation, and painful ulcerative lesion near the medial malleolus. Lymphatics from the ulnar surface of the forearm and hand, the little and ring fingers, and the adjacent surface of the middle finger, drain first into the epitrochlear nodes. Patients with spinal stenosis, have a relief of leg pain when they bend over. Sometimes leg pain can look like claudication, but if the pain is relieved by the patient bending over, it is likely that spinal stenosis, not PVD. Valve StenosisArterial/Venous InsufficiencyArterial/Venous Insufficiency Venous Insufficiency (brown) -Venous insufficiency: Often painful. Mechanism is venous stasis and HTN. Pulses are normal, although may be difficult to palpate through the edema. Normal, or cyanotic on dependency petechiae and then brown pigmentation appear with chronicity. Normal temperature. Edema often present. Often brown pigmentation around the ankles, stasis dermatitis, and possible thickening of the skin and narrowing of the leg as scarring develops. If ulceration occurs; develops at sides of ankle, especially medially. NO GANGRENE. Arterial insufficiency (Rubor and ischemic ulcer)Arterial insufficiency: Intermittent claudication, progressive to pain at rest. Tissue ischemia. Decreased or absent pulses. Pale, especially on elevation; dusk and red on dependency. Cool temperature. Absent or mild edema; may develop as the patient tried to relieve rest pain by lowering the leg. Trophic skin changes; thin, shiny, atrophic skin; loss of hair over the foot or toes; nails thickened and rigid. Ulceration involves the toes or points of trauma on feet. Gangrene may develop. Buerger Test: raise both legs to about 90 % for up to 2 minutes until there is maximal pallor of the feet. Light skinned-expect to see normal color or slight pallor. Dark skininspect soles of feet. 1. normal=return to pinkness about 10 sec or less. Filling of the veins in the feet and ankles, normally take 15sec. 2. Abnormal= Foot still pale and the veins are just starting to fill The Allen Test: compares the patency of the ulnar artery and radial arteries 1. Ask patient to make a tight fist then compress the radial and ulnar arteries w 2. Ask the patient to open the hand into a relaxed, slightly flexed position, the palm is pale 3. Release your pressure over the ulnar artery, if the ulnar artery is patent, the palm flushes within 3 to 5 sec. When drawing an arterial blood gas in the radial artery, perform the allen test to be sure that the ulnar artery is patent. Results : negative= palmar flushing positive= palmar pallor MARKED PALLOR SUGGESTS ARTERIAL INSUFFICIENCY Chapter 10 Kelly Breast/Axillae Assessment The Breast pg. 434 The most significant risk factors for breast cancer: age (65 years old), BRCA status 1 and/or BRCA 2, breast density on mammogram, personal history of breast cancer, family hx of breast cancer, and reproductive factors affecting duration of uninterrupted estrogen exposure. At the age of 50, the risk of breast cancer for someone with the BRCA1 gene is 50%. A thorough examination of the breasts includes careful inspection for skin changes, symmetry, contours, and retraction in four views. The risk of a breast mass being cancerous is 10% Breast tend to swell and become more nodular before menses from increasing estrogen. Best time for exam= 5-7 days after menstruation Inspect: Arms at side: note the appearance of the skin, color, thickening of the skin, pores.1. Redness suggests local infection or inflammatory carcinoma 2. Thickening and prominent pores suggests breast cancer Inspect size and symmetry of the breasts. Some differences in the size of the breasts and areolas are common and usually normal.Contour of the breasts. Look for changes such as masses, dimpling, or flattening. Compare one side with the other.The characteristics of the nipples, including size and shape, direction in which they point, any rashes or ulceration, or any discharge. 1. Flattening of the normally convex breasts suggest cancer 2. Asymmetry 3. Eczematous changes with rash, scaling, or ulceration on the nipple extending to the areola occurs in Paget disease of the breast, associated with underlying ductal or lobular carcinoma 4. A nipple pulled inward, tethered by underlying ducts signal retraction from a possible underlying cancer. The retracted nipple may be depressed, flat, broad, or thickened. 5. Clear or bloody nipple discharge (esp if unilateral) is suspicious of breast cancer. Arms Over Head: Hands Pressed Against Hips; Leaning Forward. To bring out dimpling or retraction that may otherwise be invisible, ask the patient to raise her arms over her head, then press her hands against her hips to contract the pectoral muscles. Inspect the breast contours care- fully in each position. If the breasts are large or pendulous, it may be useful to have the patient stand and lean forward, ), supported by the back of the chair or the examiner‘s hands. Palpate: Palpation is best performed when the breast tissue is flattened. The patient should be supine. Palpate the rectangular area extending from the clavicle to the inframammary fold or bra line, and from the midsternal line to the posterior axillary line and well into the axilla to ensure that you examine the tail of the breast. A thorough examination takes at least 3 minutes for each breast. Palpate in small, concentric circles applying light, medium, and deep pressure at each examining point. Press more firmly to reach the deeper tissues of a large breast. Examine the entire breast, including the periphery, tail, and axilla.Examining the lateral portion of the breast. To examine the lateral portion of the breast, ask the patient to roll onto the opposite hip, placing her hand on her forehead but keeping the shoulders pressed against the bed or examining table. This flattens the lateral breast tissue. Begin palpation in the axilla, moving in a straight line down to the bra line, then move the fingers medially and palpate in a vertical strip up the chest to the clavicle. Continue in verti- cal overlapping strips until you reach the nipple, then reposition the patient to flatten the medial portion of the breast. Examining the medial portion of the breast. To examine the medial portion of the breast, ask the patient to lie with her shoulders flat against the bed or examining table, placing her hand at her neck and lifting up her elbow until it is even with her shoulder (Fig. 10-13). Palpate in a straight line down from the nipple to the bra line, then back to the clavicle, continuing in vertical over- lapping strips to the mid-sternum, like mowing the lawn. Examine the breast tissue carefully for: Consistency of the tissues. Normal consistency varies widely, depending on the proportions of firmer glandular tissue and soft fat. Physiologic nodularity may be present, increasing before menses. Note the firm inframammary ridge, which is the transverse ridge of compressed tissue along the lower margin of the breast, especially in large breasts. This ridge is sometimes mistaken for a tumor. Tenderness that may occur prior to menses. Nodules. Palpate carefully for any lump or mass that is qualitatively different from or larger than the rest of the breast tissue. This is sometimes called a dominant mass that may be pathologic when evaluated by mammogram, aspiration, or biopsy. Assess and describe the characteristics of any nodule Location—by quadrant or clock, with centimeters from the nipple Size—in centimeters Shape—round or cystic, disc-like, or irregular in contour Consistency—soft, firm, or hard Delimitation—well circumscribed or not Tenderness Mobility—in relation to the skin, pectoral fascia, and chest wall. Gently move the breast near the mass and watch for dimpling. The AxillaeAlthough the axillae may be examined with the patient lying down, a sitting position is preferable. Inspect: Inspect-skin, rash, infection, unusual pigment. Palpate: Palpate- To examine the axilla, ask the patient to relax with the arm down and warn the patient that the examination may be uncomfortable. Support the patient‘s wrist or hand with your hand. Cup together the fingers of your hand and reach as high as you can toward the apex of the axilla. Place your fingers directly behind the pectoral muscles, pointing toward the midclavicle. Now press your fingers in toward the chest wall and slide them downward, trying to palpate the central nodes against the chest wall. Of the axillary nodes, the central nodes are most likely to be palpable. The central nodes at the apex of the axilla are most commonly involved in breast cancer If the central nodes feel large, hard, or tender, or if there is a suspicious lesion in the drainage areas for the axillary nodes, palpate for the other groups of axillary lymph nodes: ■ Pectoral nodes—grasp the anterior axillary fold between your thumb and fingers, and with your fingers, palpate inside the border of the pectoral muscle. ■ Lateral nodes—from high in the axilla, feel along the upper humerus. ■ Subscapular nodes—step behind the patient and, with your fingers, feel inside the muscle of the posterior axillary fold. ■ Infraclavicular and supraclavicular nodes—Also re-examine the infraclavicular and supraclavicular nodesNormal VS. Abnormal Findings and Interpretation Palpable Masses of the Breast. Breast masses show marked variation in etiology, from fibroadenomas and cysts seen in younger women, to abscess or mastitis, to primary breast cancer. All breast masses warrant careful evaluation, and definitive diagnostic measures should be pursued. Age Common Lesion Characteristics Age 15–25: Fibroadenoma Usually smooth, rubbery, round, mobile, nontender Age 25–50: Cysts Usually soft to firm, round, mobile; often tender Fibrocystic changes: Nodular, ropelike Cancer Irregular, firm, may be mobile or fixed to surrounding tissue Over 50: Cancer until proven otherwise As above Pregnancy/ lactation Lactating adenomas, cysts, mastitis, and cancer As above Paget‘s disease of the nipple, galactorrhea Tenderness-infection/premenstrual tenderness Nodules-cyst, fibroadenoma, cancer The Male Breast Gynecomastia-mass suspicious for cancer, fat Lymphadenopathy One third of men have breast tissue underlying their nipple Visible Signs of Breast CancerSkin dimpling Abnormal Contours Nipple Retraction and deviation Edema of the skin (breast) Paget Disease of the Nipple (scaly eczema-like crust around the nipple) Breast Cancer Self-Breast Examination Breast Cancer Self-Breast Examination Yearly mammography for women 40 years of age and older. For women at increased risk, many clinicians advise initiating screening mammography between ages 30 and 40, then every 2 to 3 years until 50 years of age. Although self-examination has not been shown to reduce mortality and is not recommended by all groups making screening recommendations, many choose to teach women a systematic method in which to examine their breasts. A high proportion of breast masses are detected by breast self-examination. Clinical breast examination (CBE) by a health care professional every 3 years for women between 20 and 39 years of age, and annually after 40 years of age ● Regular breast self-examination (BSE), in conjunction with mammography and CBE, to help promote health awareness ● The BSE is best timed 5 to 7 days after menses, when hormonal stimulation of breast tissue is low. ● Masses, nodularity, and change in color or inflammation, especially in the incision line (mastectomy), suggest recurrence of breast cancer. Patient Instructions for the Breast Self-Examination— American Cancer Society Lying supine- ● Lie down with a pillow under your right shoulder. Place your right arm behind your head. ● Use the finger pads of the three middle fingers on your left hand to feel for lumps in the right breast. The finger pads are the top third of each finger. Make overlapping, dime-sized circular motions to feel the breast tissue. ● Apply three levels of pressure in each spot: light, medium, and firm, using firmer pressure for tissue closest to the chest and ribs. A firm ridge in the lower curve of each breast is normal.Standing- ● While standing in front of a mirror with your hands pressing firmly down on your hips, look at your breasts for any changes of size, shape, contour, or dimpling, or redness or scaliness of the nipple or breast skin. (The pressing down on the hips position contracts the chest wall muscles and enhances any breast changes.) ● Examine the breast in an up-and-down or ―strip‖ pattern. Start at an imaginary straight line under the arm, moving up and down across the entire breast, from the ribs to the collarbone, until you reach the middle of the chest bone (the sternum). Remember how your breast feels from month to month. ● Repeat the examination on your left breast, using the finger pads of the right hand. ● If you find any masses, lumps, or skin changes, see your clinician right away. ● Examine each underarm while sitting up or standing and with your arm only slightly raised so you can easily feel in this area. Raising your arm straight up tightens the tissue in this area and makes it harder. Chapter 11 & 12 Tripti (1-6) / Joysline (7-11); Jenna Abdominal/Peritoneal/Rectal Assessment and Modification for Age Abdominal assessment: Sequence: Inspection, auscultation, percussion, palpation Auscultation: for bowel sounds, bruit, and friction rub. Possible abnormal sounds: increased or decreased motility, bruit of renal artery stenosis, liver tumor, splenic infarct. . Percuss the abdomen for patterns of tympany and dullness. Possible abnormalities: Ascites, GI obstruction, pregnant uterus, ovarian tumor Palpate all quadrants of the abdomen for abdominal tenderness. Light palpation for guarding, rebound, and tenderness. Possible abnormalities: Firm, board like abdominal wall—suggests peritoneal inflammation. Guarding if the patient flinches, grimaces, or reports pain during palpation. Rebound tenderness from peritoneal inflammation; pain is greater when you withdraw your hand than when you press down. Press slowly on a tender area, then quickly ―let go. If you feel a mass, examine with the abdominal muscles tensed, usually, abdominal wall masses can be observed, whereas intra-abdominal masses are more concerning.A left upper quadrant mass is more likely to be a kidney if there is no palpable ―notch,‖ you can push your fingers between the mass and the costal margin, there is normal tympany over this area, and you cannot push your fingers medial and deep to the mass Rectal assessment: Rectal assessment is a part of regular GI assessment over age of 40. Inspection: Check for fissures, lesions, scars, inflammation, discharge, rectal prolapse, skin tags, and external hemorrhoids. Palpation: The rectal walls should feel soft and smooth, without masses, fecal impaction, or tenderness. Peritoneal assessment: Check for ascites, a large accumulation of fluid in the peritoneal cavity caused by advanced liver disease, heart failure, pancreatitis, or cancer. Do not palpate a rigid abdomen. Peritoneal inflammation may be present, in which case palpation could cause pain or rupture an inflamed organPancreatitis- In acute pancreatitis, epigastric tenderness and rebound tenderness are usually present, but the abdominal wall may be soft. Intrapancreatic trypsinogen activation to trypsin and other enzymes, resulting in autodigestion and inflammation of the pancreas. Epigastric, may radiate straight to the back or other areas of the abdomen; 20% with severe sequelae of organ failure Chronic pancreatitis: Usually steady. Irreversible destruction of the pancreatic parenchyma from recurrent inflammation of either large ducts or small ducts. Epigastric, radiating to the back Severe, persistent, deep. Peptic Ulcer Disease Mucosal ulcer in stomach or duodenum >5mm, covered with fibrin, extending through the muscularis mucosa; H.pylori infection in 90 % of peptic ulcers Location-epigastric, may radiate straight to the back Quality-Variable, epigastric gnawing or burning(dyspepsia) may also be boring or aching, or hunger like Timing- wakes patient up at night. Occurs immediately over a few weeks, disappears for months, then recurs Aggravating factors- variable Relieving factors-food and antacid may bring reliefAssociated symptoms- n/v, belching, bloating, heartburn, weight loss Gastric ulcers: over 50 yrs old Duodenal ulcer: 30-60 years old GERDEpigastric pain. If patient reports heartburn and regurgitation together or more than once a week, the accuracy of diagnosis of GERD is 90 %. H.pyloria may be present. Usually occurs after meals, especially spicy foods. Aggravated by- lying down, bending over, physical activity, diseases such as scleroderma, gastroparesis, drugs like nicotine that relaxes the lower esophageal sphincter. Relieved by-Antacids, PPI, avoiding alcohol, smoking, fatty meals, chocolate, theophylline, CCB Associated symptoms- Wheezing, chronic cough, SOA, hoariness, choking sensation, dysphagia, regurgitation, halitosis, sore throat, increases risk for Barrett esophagus and esophageal cancer Risk factors- salivary flow which prolongs acid clearance by damping action of the bicarbonate buffer; obesity; delayed gastric emptying; selected medications; hiatal hernia. Appendicitis: Joysline Appendicitis - The appendix is a small, finger-like appendage attached to the cecum just below the ileocecal valve. Because it empties into the colon inefficiently and its lumen is small, it is prone to becoming obstructed and is vulnerable to infection (appendicitis). The obstructed appendix becomes inflamed and edematous and eventually fills with pus. It is the most common cause of acute inflammation in the right lower quadrant of the abdominal cavity and the most common cause of emergency abdominal surgery. Males are affected more than females, teenagers more frequently than adults. - Visceral periumbilical pain suggests early acute appendicitis from distention of an inflamed appendix. It gradually changes to parietal pain in the RLQ from inflammation of the adjacent parietal peritoneum. In the elderly, signs and symptoms of appendicitis may vary greatly. Signs may be very vague and suggestive of bowel obstruction or another process; some patients may experience no symptoms until the appendix ruptures. The incidence of perforated. Appendix is higher in the elderly because many of these people do not seek health care as quickly as younger people.- In women, consider pelvic inflammatory disease, ruptured ovarian follicle, and ectopic pregnancy. Combining signs with laboratory inflammatory markers and CT scans markedly reduces misdiagnosis and unnecessary surgery. -Obturator sign: right hypogastric pain with the right hip and knee flexed and the hip internally rotated CLINICAL MANIFESTATIONS - Lower right quadrant pain usually accompanied by low-grade fever, nausea, and sometimes vomiting. -At McBurney’s point (located halfway between the umbilicus and the anterior spine of the ilium), local tenderness with pressure and some rigidity of the lower portion of the right rectus muscle. - Rebound tenderness may be present; location of appendix dictates amounts of tenderness, muscle spasm, and occurrence of constipation or diarrhea. -Rovsing’s sign (elicited by palpating left lower quadrant, which paradoxically causes pain in right lower quadrant). - If appendix ruptures, pain becomes more diffuse; abdominal distention develops from paralytic ileus, and condition worsens. ASSESSMENT AND DIAGNOSTIC METHOD - Diagnosis is based on a complete physical examination and laboratory and radiologic tests. -Leukocyte count greater than 10,000/m -Neutrophil count greater than 75%; -Abdominal radiographs, ultrasound studies, and CT scans may reveal right lower quadrant density or localized distention of the bowel.Surgery is indicated if appendicitis is diagnosed and should be performed as soon as possible to decrease risk of perforation. -Administer antibiotics and intravenous fluids until surgery is performed. -Analgesic agents can be given after diagnosis is made. - The major complication is perforation of the appendix, which can lead to peritonitis Visceral periumbilical pain early signs of appendicitis. It gradually changes to parietal pain in the RLQ from inflammation of the adjacent parietal peritoneum. Acute inflammation of the appendix with distention or obstruction. Quality- mild but increasing, possibly cramping, steady and more severe Timing- last 4-6 hrs., depending on intervention Aggravating factors- movement or cough Relieving factors- it if subsides temporarily suspect perforation of the appendix Associated factors- anorexia, nausea and possibly vomiting following onset of pain, low fever Twice as likely in the presence of RLQ tenderness, Rovising sign, and the psoas sign; it is three times more likely if there is McBurney point tenderness. Localized tenderness anywhere in the RLQ, even in the right flank suggests appendicitis. Rovsing sign: pain in the RLQ during left sided pressure Psoas Sign Positive : increased abdominal pain while placing your hands just above the patient’s knee and ask to raise thigh against hand. Then asking patient to turn onto left side. Then extend the right leg at the hip. Flexion of the leg at the hip makes the psoas muscle contract; extension stretches it. Classic Sign= Begins near the umbilicus, then migrates to the RLQ. Diverticulitis: Joysline Diverticulitis- Inflammation of the diverticula. Left lower quadrant pain, especially with a palpable mass. Deep palpation is usually required to delineate the liver edge, the kidneys, and abdominal masses. The pain may be cramping at first, then steady. - Diverticulosis is necessary for the development of diverticulitis. Diverticulosis is a condition in which outpouchings, or diverticula, develop in the colon. The majority ofpatients with diverticulosis are asymptomatic. However, 1–4% of patients with diverticulosis will develop diverticulitis. Low dietary fiber intake, high red meat intake, obesity, physical inactivity and smoking are all associated with an increased risk of diverticulitis. - The diverticula of the colon often have no symptoms unless inflammation causes diverticulitis. The pain is constant in nature and tends to be worse with movement. The left-sided predominance of pain is due to the fact that most diverticulitis occurs in the sigmoid or descending colon. If the sigmoid colon is redundant there may be suprapubic or right-sided pain. Look for localized peritoneal signs and a tender underlying mass. - The clinical presentation of acute diverticulitis ranges from mild abdominal pain to peritonitis with sepsis. The diagnosis can often be made based on clinical features alone, but imaging is necessary in more severe presentations to rule out complications such as abscess and perforation. - Assess for guarding, rebound, and distention of the left lower quadrant. The treatment of diverticulitis depends on the severity of the presentation, presence of complications and underlying comorbid conditions. - Foods that can get stuck in a diverticula (such as popcorn, nuts, and corn) should be avoided. Hepatitis: Joysline Visceral pain in the RUQ. Liver span decreases. Jaundice- is a striking yellowish discoloration of the skin and sclera from increased levels of bilirubin, Hepatitis -Hepatitis, or inflammation of the liver, can be caused by several different viruses. Symptoms of hepatitis are universal, regardless if caused by an infectious agent or chronic condition, and can include fatigue, anorexia, abdominal pain, fever, diarrhea, vomiting, jaundice, dark urine, and pale clay-colored stools. The mode of transmission, communicability, and incubation period differ greatly with the type of virus. In the United States, hepatitis A, B, and C are the most common viruses that cause hepatitis and are of great public health significance. The best strategy for preventing infection and transmission of hepatitis A and B is vaccination. Also, educate patients about how the hepatitis viruses spread and behavioral strategies to reduce the risk of infection. Screen high-risk groups for hepatitis B. Hepatitis A. - Transmission of hepatitis A virus (HAV) is through a fecal– oral route. Fecal shedding followed by poor hand washing contaminates water and foods, leading to infection of household andsexual contacts. Infected children are often asymptomatic, contributing to spread of infection. To reduce transmission, advise hand washing with soap and water after bathroom use or changing diapers (daycare workers), and before preparing or eating food. Diluted bleach can be used to clean environmental surfaces. HAV infection is rarely fatal—fewer than 100 deaths occur each year— and usually only in people with other liver diseases; it does not cause chronic hepatitis. - The vaccine alone may be administered at any time before traveling to endemic areas. Healthy unvaccinated individuals should receive either a hepatitis A vaccine or a single dose of immune globulin (preferred for those ≥age 40 years) within 2 weeks of being exposed to HAV. These recommendations apply to close personal contacts of persons with confirmed HAV, coworkers of infected food handlers, and staff and attendees (and their household members) of childcare centers where HAV has been diagnosed in children, staff, or households of attendees. Hepatitis B. - Hepatitis B virus (HBV) infection is a more serious threat than infection with hepatitis A. The fatality rate for acute infection can be up to 1% and HBV infection can become chronic. Approximately 95% of infections in healthy adults are self-limited, with elimination of the virus and development of immunity. Risk of chronic HBV infection is highest when the immune system is immature—chronic infection occurs in 90% of infected infants and 30% of children infected before age 5 years. About 15% to 25% of those with chronic HBV infection die from cirrhosis or liver cancer, accounting for nearly 3,000 deaths each year in the United States. - Most persons with chronic infection are asymptomatic until the onset of advanced liver disease. Screening. The USPSTF recommends screening for HBV in persons at high risk for infection (grade B), including those born in countries with a high endemic prevalence of HBV infection, persons with HIV, injection drug users, men who have sex with men, and household contacts or sexual partners of HBV-infected persons. The CDC recommends screening all pregnantwomen, ideally in the first trimester, and universal vaccination for all infants beginning at birth. For adults, vaccine recommendations also target high-risk groups, including those in high-risk settings. Hepatitis C. - There is no vaccination for hepatitis C, so prevention targets counseling to avoid risk factors. Screening should be recommended for high-risk groups. - Hepatitis C virus (HCV), transmitted mainly by percutaneous exposures, it is the most prevalent chronic bloodborne pathogen in the United States. Anti-HCV antibody is detectable in just under 2% of the population, though prevalence is markedly increased in high-risk groups, particularly injection drug users. - Additional risk factors for HCV infection include blood transfusion or organ transplantation before 1992, transfusion with clotting factors before 1987, hemodialysis, health care workers with needle stick injury or mucosal exposure to HCV-positive blood, HIV infection, and birth from an HCV-positive mother. Sexual transmission is rare. - Hepatitis C becomes a chronic illness in over 75% of those infected and is a major risk factor for subsequent cirrhosis, hepatocellular carcinoma, and need for liver transplant for endstage liver disease. - However, the majority of persons with chronic HCV are unaware of being infected. Response to antiviral therapy (undetectable HCV RNA 24 weeks after completing treatment) ranges from 40% to over 90% depending on the viral genotype and the combination of drugs usedfor treatment. Consequently, the USPSTF has concluded that screening for hepatitis C infection is of moderate benefit for persons at high risk for infection as well as those born between 1945 and 1965 (grade B). a bile pigment derived chiefly from the breakdown of hemoglobin. Acholic stools-occur in viral hepatitis briefly A-Travel or meals in areas of poor sanitation, ingestion of contaminated water or foodstuffs. FECAL or ORAL route. Fecal shedding by poor hand washing contaminates water and foods, leading to infection of household and sexual contact. Infected children are asymptomatic. Vaccine: all children under 1y; chronic liver disease; traveling to areas with high endemic rates; men who have sex with men; injection and illicit drug users; person who have clotting disorders If exposed: healthy unvaccinated shoulder with get a hepatitis A vaccine or a single dose of immune globulin within 2 weeks of exposure B-Parenteral or mucous membrane exposure to infectious body fluids: blood, serum, semen, saliva through sexually contact or injection of needle. C- illicit injection drug use or blood transfusion . No vaccine. Becomes a chronic illness of those infected and is a major risk factor for subsequent cirrhosis, hepatocellular carcinoma, and need for liver transplant.Cirrhosis: varices such as esophageal varices are common with cirrhosis and can cause black tarry stools and positive occult blood. Other symptoms such as jaundice, ascites, spider hemangiomas, and dilated veins on the abdomen can signal cirrhosis. IBS: JoyslineIrritable bowel syndrome A chronic functional disorder of the colon (normal colonic tissue marked by exacerbations and remissions (spontaneous). Commonly exacerbated by excess stress. It may be classified as diarrhea predominant or constipation predominant. In some cases, it may alternate between the two. - Irritable bowel syndrome (IBS) is a chronic functional bowel disorder associated with abdominal pain or discomfort, bloating, and altered bowel habits that continue for 3 months with onset 6 months before diagnosis and occurs in the absence of any structural or biochemical abnormalities. IBS is a common disorder, although prevalence rates vary, in part because IBS remains undiagnosed in at least threequarters of patients. IBS is more common among women and more often diagnosed in younger individuals. - Change in bowel habits with a mass lesion warns of colon cancer. Intermittent pain for 12 weeks of the preceding 12 months with relief from defecation, change in frequency of bowel movements, or change in the form of stool (loose, watery, pelletlike), linked to luminal and mucosal irritants that alter motility, secretion, and pain sensitivity suggests irritable bowel syndrome. - Worse in the morning; rarely at night. Crampy lower abdominal pain, abdominal distention, flatulence, nausea; urgency, pain relieved with defecation. - Altered motility or secretion from luminal and mucosal irritants that change mucosal permeability, immune activation, and colonic transit, including mal-digested carbohydrates, fats, excess bile acids, gluten intolerance, enteroendocrine signaling, and changes in microbiomes. - Currently, there is no gold standard for the diagnosis of IBS. Diagnosis is complicated by the lack of reliable, standardized biomarkers and because abnormalities cannot be detected by radiologic or endoscopic tests. - Irritable bowel syndrome will cause loose bowel movements with cramps but no systemic symptoms of fever, weight loss, or malaise. This syndrome is more likely in young women with alternating symptoms of loose stools and constipation. Stress usually makes the symptoms worse, as do certain foods. - IBS diagnose guidelines recommend that providers use a symptom-based strategy based on routine physical examination and standardized criteria, such as the Rome III. The validated Bristol Stool Scale, developed in the late 1990s, is typically used to subtype IBS according to bowel habit.- Hypothyroidism can cause constipation Treatment Plan. -Increase dietary fiber. Supplement fiber with psyllium (Metamucil or Konsyl), methylcellulose (Citrucel), wheat dextrin (Benefiber). Start at a low dose (causes gas). -Avoid gas-producing foods: Beans, onions, cabbage, high-fructose corn syrup. If poor response, use a trial diet of lactose avoidance or gluten avoidance. -Antispasmodics for abdominal pain: Administer dicyclomine (Bentyl) or hyoscyamine as needed. - IBS with constipation: Begin a trial of fiber supplements, polyethylene glycol (osmotic laxative). If severe constipation: Prescribe lubiprostone or linaclotide (contraindicated in pediatric patients younger than 6 years, has caused death from dehydration). -IBS with diarrhea: Take loperamide (Imodium) before regularly scheduled meals. • Severe diarrhea–predominant IBS: Administer alosetron (warning: ischemic colitis, which can be fatal). Decrease life stress. Address anxiety/stress with patient and offer treatment strategies. Rule out: Amoebic, parasitic, or bacterial infections; inflammatory disease of the GI tract; and so forth. Check stool for ova and parasites (especially diarrheal stools) with culture -Osmotic diarrhea: usually related to lactose intolerance, watery diarrhea often follows meal ingestion. Crampy abdominal pain, distension, and gas often accompany symptoms. Diarrhea is often provoked by pizza, milkshakes, yogurt, and other lactose-containing foods Incontinence (jenna) - Urinary incontinence see p. 463 & 497 o If the patient reports incontinence, ask if the patient is leaking small amounts of urine due to increased intra-abdominal pressure from coughing, sneezing, laughing, or lifting. *Stress incontinence o Or following an urge to void, is there an involuntary loss of large amounts of urine? Is there a sensation of bladder fullness, frequent leakage, or voiding of small amounts but difficulty emptying the bladder? § In stress incontinence, increased abdominal pressure causes bladder pressure to exceed urethral resistance—there is poor urethral sphincter tone or poor support of bladder neck. Arises from decrease intraurethral pressure. · Causes: childbirth and surgery. Local conditions affecting urethral sphincter such as postmenopausal atrophy of mucosa and urethral infection; in men, stress incontinence may follow prostate surgery. · Symptoms: Occurs with coughing, laughing, and sneezing while in upright position. Urine loss if unrelated to conscious urge to urinate.· Physical signs: Atrophic vaginitis may be evident. Bladder distention absent. § In urge incontinence, urgency is followed by involuntary leakage due to uncontrolled detrusor contractions that overcome urethral resistance. · Bladder typically small. · Occur from decreased cortical inhibition of detrusor contractions from stroke, brain tumor, dementia, and lesions of the spinal cord above sacral level. o Symptoms: Involuntary urine loss followed by urge to urinate. Volume moderate. o Physical signs: small bladder not detectable on examination. · Also from Hyperexcitability of sensory pathways as in bladder infections, tumors, and fecal impactions. o Symptoms: urgency, frequency, nocturia with small-mod amounts. If acute inflammation is present, pain on urination. o Physical signs: decreased cortical inhibition will shows mental deficits or motor signs of central nervous system disease · Also from deconditioning of voiding reflexes such as frequent voluntary voiding at low bladder volumes. o Symptoms: possibly pseudo-stress incontinence – voiding 10- 20sec after stresses such as change in position, going up and down stairs, possibly laughing, coughing, sneezing. o Physical sign: signs of local pelvic problems or fecal impaction may be present. § In overflow incontinence, neurologic disorders or anatomic obstruction from pelvic organs or the prostate limit bladder emptying until the bladder becomes overdistended. Detrusor contractions are insufficient to overcome urethral resistance, causing urinary retention. · Mechanisms: Obstruction of the bladder outlet, as in benign prostatic hyperplasia or tumor. Weakness of the detrusor muscle associated with peripheral nerve disease at S2–4 level. Impaired bladder sensation that interrupts the reflex arc, as in diabetic neuropathy. · Symptoms: When intravesicular pressure overcomes urethral resistance, continuous dripping or dribbling incontinence ensues. Decreased force of the urinary stream. Prior symptoms of partial urinary obstruction or other symptoms of peripheral nerve disease may be present. · Physical signs: Examination often reveals an enlarged, sometimes tender, bladder. Other signs include prostatic enlargement, motor signs of peripheral nerve disease, a decrease in sensation (including perineal sensation), and diminished to absent reflexes. o Bladder control involved neuroregulatory and motor mechanism. Central and peripheral severe lesions affect S2 to S4 can affect normal voiding. Ask: does patient feel when bladder is full, when voiding: functional and mixed incontinence. § Functional incontinence arises from impaired cognition, musculoskeletal problems, or immobility. Patient functionally unable to reach the toilet in time because of impaired health or environmental conditions. · Mechanism: problems in mobility resulting from weakness, arthritis, poor vision, or other conditions. Environmental factors such as unfamiliar setting, distant bathroom, bed rails, or physical restraints.· Symptoms: Incontinence on way to toilet or only early morning. · Physical signs: Bladder not detectable on exam; look for physical or environmental clues as the cause. § Mixed incontinence is combined stress and urge incontinence is o Pt‘s functional status can affect voiding behaviors: mobile? Immobile? Alert? Medications? § Incontinence secondary to medications: Sedatives, tranquilizers, anticholinergics, sympathetic blockers, and potent diuretics The pain from a kidney stone causes dramatic, severe, colicky pain at the CVA that radiates down into the groin. Colon/Anorectal Cancer: Joysline Colorectal cancer - Very gradual (years) with vague GI symptoms. Tumor may bleed intermittently, and patient may have iron-deficiency anemia. Changes in bowel habits, stool, or bloody stool. Heme positive stool, dark tarry stools, mass on abdominal palpation. Older patients (older than 50 years of age), especially with history of multiple polyps or inflammatory bowel disease such as Crohn’s disease (CD) or ulcerative colitis (UC). - Screening for Colorectal Cancer: Screening tests include stool tests that detect occult fecal blood, such as fecal immunochemical tests, high-sensitivity guaiac-based tests, and tests that detect abnormal DNA. Endoscopic tests are also used for screening, including colonoscopy, which visualizes the entire colon and can remove polyps, and flexible sigmoidoscopy, which visualizes the distal 60 cm of the bowel. Imaging tests include double-contrast barium enema and CT colonography. Any abnormal finding on a stool test, imaging study, or flexible sigmoidoscopy warrants further evaluation with colonoscopy. - Colorectal cancer is the third most frequently diagnosed cancer among both men and women (over 140,000 new cases) and the third leading cause of cancer death (nearly 50,000 deaths) each year in the United States. The lifetime risk of diagnosis with colorectal cancer is about 5%, while the lifetime risk for dying from colorectal cancer is about 2%.50 The good news is that U.S. incidence and mortality rates have been gradually but steadily declining over the past three decades. These trends are attributed to changes in risk factor prevalence, such as decreased tobacco use; increased screening, which both prevents cancers and increases detection of early-stage curable cancers; and improved treatment.- The strongest risk factors for colorectal cancer are: increasing age; personal history of colorectal cancer, adenomatous polyps, or longstanding inflammatory bowel disease; and family history of colorectal neoplasia—particularly those with affected multiple first-degree relatives, a single first-degree relative diagnosed before age 60 years, or a hereditary colorectal cancer syndrome. - Prevention. The most effective prevention strategy is to screen for and remove precancerous adenomatous polyps. Screening programs using fecal blood testing or flexible sigmoidoscopy have been shown in randomized trials to reduce the risk of developing colorectal cancer. - Physical activity, aspirin and nonsteroidal anti-inflammatory drugs (NSAIDs), and postmenopausal combined hormone replacement therapy (estrogen and progestin) are also associated with decreased risk of colorectal cancer. - However, the USPSTF recommends against routinely using aspirin and NSAIDs for prevention in average-risk persons because the potential harms, including GI bleeding, hemorrhagic stroke, and renal impairment, outweigh the benefits (grade D). - Hormone therapy for cancer chemoprevention is not advised; women receiving combined therapy were actually more likely to present with advanced-staged colorectal cancers and appear to have a higher risk for colorectal cancer mortality. Hormone therapy is associated with increased risk of breast cancer, cardiovascular events, and venous thromboembolism. There has been no convincing evidence that dietary changes or taking supplements can prevent colorectal cancer. - With a past history of colon cancer and recent weight loss and fatigue, a relapse of colon cancer would be expected. Colon cancer usually metastasizes to the liver, creating hard, irregular nodules, usually non-tender, which can sometimes be palpated on examination Screening Tests. Screening tests include stool tests that detect occult fecal blood, such as fecal immunochemical tests, high-sensitivity guaiac-based tests, and tests that detect abnormal DNA. Endoscopic tests are also used for screening, including colonoscopy, which visualizes the entire colon and can remove polyps, and flexible sigmoidoscopy, which visualizes the distal 60 cm of the bowel. Imaging tests include double-contrast barium enema and CT colonography.Ischemia pain (abdominal) does not increase with palpation. ***Chapter 13 David Male Genitalia Assessment and Modification for Age Undescending testes: In infant, testis must often be ―milked‖ into the scrotum from the inguinal canal Surrounding or appended to the testes are several structures. The scrotum is a loose, wrinkled pouch of skin and underlying dartos muscle. The scrotum is divided into two compartments, each containing a testis or testicle. Covering the testis, except posteriorly, is the serous membrane of the tunica vaginalis, derived from the peritoneum of the abdomen and brought down into the scrotum during testicular descent through the deep internal inguinal ring. The parietal layer of the tunica vaginalis cloaks the anterior two thirds of the testis, and the visceral layer lines the adjacent scrotum. On the posterolateral surface of each testis is the softer, comma-shaped epididymis, consisting of tightly coiled tubules emanating from the testis that become the vas deferens. The epididymis is normally separated from the testis by a palpable sulcus, and provides a reservoir for storage, maturation, and transport of sperm. The inguinal canal, which lies medial to and roughly parallel to the inguinal ligament, forms a tunnel for the vas deferens as it passes through the abdominal muscles. The internal opening of the canal, the internal inguinal ring, is approximately 1 cm above the midpoint of the inguinal ligament. Neither the canal nor the internal ring is palpable through the abdominal wall. The exterior opening of the tunnel, the external inguinal ring, is atriangular slit-like structure palpable just above and lateral to the pubic tubercle. When loops of bowel force their way through the inguinal canal, they produce inguinal hernias. Another route for a herniating mass is the femoral canal, below the inguinal ligament. Although this canal is not visible, you can estimate its location by placing your right index finger, from below, on the right femoral artery. Your middle finger will then overlie the femoral vein; your ring finger, the femoral canal. Femoral hernias protrude at this location. Ask about any discharge from the penis, dripping, or staining of underwear. If penile discharge is present, clarify the amount, color, and any fever, chills, rash, or associated symptoms. Note that for men born between 1940 and 1989, the median age of sexual initiation is 16.1 years and the median number of lifetime partners is 8.8, underscoring the importance of screening for STIs. Inquire about sores or growths on the penis. Ask about swelling or pain in the scrotum. Inspection. Inspect the penis, including: The skin. Inspect the skin on the ventral and dorsal surfaces and the base of the penis for excoriations or inflammation, lifting the penis when necessary. The prepuce (foreskin). If present, retract the prepuce or ask the patient to retract it. This step is essential for the detection of chancres and carcinomas. Smegma, a cheesy, whitish material, may accumulate normally under the foreskin. The glans. Look for any ulcers, scars, nodules, or signs of inflammation. The urethral meatus. Inspect the location of the urethral meatus. Compress the glans gently between your index finger above and your thumb below. This maneuver should open the urethral meatus and allow you to inspect it for discharge. Normally, there is none. If the patient has reported a discharge that you are unable to see, ask him to strip, or milk, the shaft of the penis from its base to the glans. Alternatively, do this yourself. This maneuver may expel some discharge from the urethral meatus for appropriate examination. Have a glass slide and culture materials ready. Palpation. Palpate the shaft of the penis between your thumb and first two fingers, noting any induration. (This may be omitted in a young asymptomatic male patient.) Palpate any abnormality of the penis, noting any induration or tenderness. If you retract the foreskin, replace it before proceeding on to examine the scrotum. Inspection. Inspect the scrotum, including: The skin. Lift up the scrotum so that you can inspect its posterior surface. Note any lesions or scars. Inspect the pubic hair distribution. The scrotal contours. Inspect for swelling, lumps, veins, bulging masses, or asymmetry of the left and right hemiscrotum. The inguinal areas. Note any erythema, excoriation, or visible adenopathy. There may be dome-shaped white or yellow papules or nodules formed by occluded follicles filled with keratin debris of desquamated follicular epithelium. Such epidermoid cysts are common, frequently multiple, and benign. Palpation. If using a one-handed technique, palpate each testis and epididymisbetween your thumb and first two fingers. If using two hands, cradle the testis at both poles in the thumb and fingertips of both hands. Palpate the scrotal contents as you gently slide them back and forth from the fingertips of one hand to the other, without changing the position of your hands as they cup the scrotum. This technique is comfortable for the patient and allows a subtle controlled and accurate examination. The testes should be firm but not hard, descended, symmetric, nontender, and without masses. For each testis, assess size, shape, consistency, and tenderness; feel for any nodules. Pressure on the testis normally produces a deep visceral pain. Palpate the epididymis on the posterior surface of each testicle without applying excess pressure, which can cause discomfort. The epididymis feels nodular and cord-like and should not be confused with an abnormal lump. Normally, it should not be tender. Palpate each spermatic cord, including the vas deferens, between your thumb and fingers, from the epididymis to the external inguinal ring (Fig. 13-6). The vas feels slightly stiff and tubular and is distinct from the accompanying vessels of the spermatic cord. Palpate any nodules or swellings. Swelling in the scrotum apart from the testicles can be evaluated by transillumination. After darkening the room, shine the beam of a strong flashlight from behind the scrotum through the mass. Look for transmission of the light as a red glow Normal VS. Abnormal Findings and Interpretation Prostate Issues and Cancer Prostate Cancer: 2nd leading cause of cancer of cancer in the US. Risk Factors:<40, African American men, genetics, (potentially exposure to agent orange, diets high in animal fats, smoking, obesity. Prevention: PSA TESTING (normal levels are >4.0). False positives are caused by BPH, prostate infections, and ejaculation. Digital Rectal Exam: finds palpable nodules in the posterior and lateral areas of the prostate gland. It is unable to detect cancer in the anterior and central areas of the gland. The exam is performed by having the pt bear down and note any irregularities or nodules. Sweep your finger carefully over the prostate gland, identifying it‘s lateral lobes and the groove of the median sulcus. Note shape, mobility, and consistency of the prostate. Screening: Patients with average risk should begin screening between 50-55 years of age. PSA screening should continue every 1-2 years. High risk screening: should start at 40-45 years of age STIGonorrhea-yellow penile discharge Chlamydia-white discharge MOST COMMON STI Disseminated gonorrhea- rash, tenosynovitis, monoarticular arthritis, even meningitis,not always urogenital symptoms Genital warts (condylomata Acuminata)- single or multiple papules or plaques of carriable shapes. Caused by HPV. Incubation-weeks to months; inf ected person may not have visible warts Herpes: BURNING pain, vesicles Genital warts (condylomata Acuminata)- single or multiple papules or plaques of carriable shapes. Caused by HPV. Incubation-weeks to months; infected person may not have visible wartsSyphilis- small red papule that becomes chancre, a painless erosion up to 2 cm in diameter. Syphilis is fairly uncommon but does occur in the highly promiscuous population, especially when coupled with illegal drug use. Base of chancre is clean, red, smooth, and glistening; borders are raised and indurated. Chancre heals within 3 to 8 weeks. Cause-treponema pallidum, a spirochete. Incubation 9-90 days after exposure. May develop inguinal lymphadenopathy within 7 days, lymph nodes are rubbery, non-tender, mobile. Patients develop secondary syphilis while chancre still present (suggests coinfection of HIV) Chancroid- red papule or pustule initially, then forms a painful deep ulcer with ragged nonindurated margins; contains necrotic exudate, has a friable base. Cause- Haemophilus ducreyi, an anaerobic bacillus. Incubation- 3 to 7 days after exposure. Painful inguinal adenopathy Testicular Disorders and Cancer Acute orchitis: The scrotum will be red and tense. Orchitis is usually unilateral and often associated with viral infections such as mumps. Varicocele: Varicoceles are varicose veins surrounding the spermatic cord, coming through the inguinal ring. These veins feel like spaghetti and are often referred to as a ―bag of worms.‖ The increased number of veins affects the temperature of the testes, often causing infertility problems. Like most varicose veins in any area, varicoceles can cause a nonspecific aching. Although usually benign, a unilateral varicocele on the right or a varicocele which does not resolve in the supine position deserves further workup Hydrocele: Fluid-filled cyst originating within the tunica vaginalis. An examining finger can be placed over the mass into the inguinal ring. An outside light source can be placed beneath the scrotum. Hydroceles often transilluminate light, whereas solid tumors do not. Erectile Dysfunction May be a from psychogenic causes, especially if early morning erection is preserved; it may also reflect decreased testosterone, decreased blood flow in the hypogastric arterial system, impaired neural innervation, and diabetes.Erectile dysfunction, or the inability to maintain an erection, affects approximately 50% of older men. Vascular causes are the most common, from both atherosclerotic arterial occlusive disease and corpora cavernosa venous leak. Chronic diseases such as diabetes, hypertension, dyslipidemia, and smoking, as well as medication side effects, all contribute to the prevalence of erectile dysfunction Men with screen-detected cancers who undergo aggressive treatment with surgery or radiation frequently leads to complications such as erectile dysfunction, urinary incontinence, and bowel problems that adversely affect the quality of life Arterial ischemia in iliac–pudendal leads to erectile dysfunction Erectile dysfunction can be due to psychogenic causes, especially if early morning erection is preserved. Decreased testosterone, decreased blood flow in hypogastric arterial system, impaired neural innervation, and diabetes can also cause Erectile Dysfunction. Chapter 14- Becky 1-3/Kristin 4-6 Female Genitalia and Modification for Age External Genitalia (Vulva) includes mons pubis overlying the symphysis pubis; labia majora; labia minora; prepuce and clitoris. The opening into the vagina is the introitus (in virgins may be hidden by the hyman). The perineum refers to tissue between introitus and anus. The urethral meatus opening is between the clitoris and vagina. Paraurethral (Skene) glands are just posterior and adjacent to the meatus on either side. The Bartholin glands are posteriorly on both sides but not always visible. Internal Genitalia: Locate the cervix with a gloved and water-lubricated index finger.Assess support of vaginal outlet by asking patient to strain down. Enlarge the introitus by pressing its posterior margin downward. Insert a water-lubricated speculum of suitable size. Start with speculum held obliquely, then rotate to horizontal position for full insertion. Open the speculum and inspect cervix. Observe: ● Position ● Color ● Epithelial surface Any discharge or bleeding ● Any ulcers, nodules, or masses Obtain specimens for cytology (Pap smears) with: An endocervical broom or brush with scraper (except in pregnant women), to collect both squamous and columnar cells ● Or, if the woman is pregnant, use a cotton-tipped applicator moistened with water Inspect the vaginal mucosa as you withdraw the speculum. Palpate, by means of a bimanual examination: ● The cervix and fornices ● The uterus ● Right and left adnexa (ovaries) Assess strength of pelvic muscles. With your vaginal fingers clear of the cervix, ask patient to tighten her muscles around your fingers as hard and long as she can. Perform a rectovaginal examination to palpate a retroverted uterus, uterosacral ligaments, cul-de-sac, and adnexa or screen for colorectal cancer in women 50 years or older.ADOLESCENT GIRLS: Assessing sexual maturity is done by rating pubic hair Stage 1- Preadolescent girls have no pubic hair but may have fine, vellus hair Stage 2- Sparse growth of long, slightly pigmented, curly or straight hair along labia Stage 3- Darker coarser hair spreading to pubic symphysis Stage 4- Coarse and curly hair as in adults; but not as much and not including thighs Stage 5- Adult hair quantity and quality- spreads to medial surface of the thighs not on abdomen Considerations for Adolescent girls: first examination should be done by experienced provider. Adolescent Initial sign of puberty: hyman thickening and redundancy secondary to estrogen, widening of the hips, beginning of height spurt - these changes may be difficult to detect. The first easily detectable sign of puberty is the appearance of breast buds although pubic hair may be seen earlier. Normal VS. Abnormal Findings and Interpretation Normal: No inguinal adenopathy. External genitalia without erythema, lesions, or masses. Vaginal mucosa pink. Cervix parous, pink, and without discharge. Uterus anterior, midline,smooth, and not enlarged. No adnexal tenderness. Pap smear obtained. Rectovaginal wall intact. Rectal vault without masses. Stool brown and Hemoccult negative. Abnormal: Weakness of the pelvic floor muscles may cause pain; urinary incontinence; fecal incontinence; and prolapse of the pelvic organs that can produce a cystocele, rectocele, or enterocele. Risk factors are advancing age; prior pelvic surgery or trauma; parity and child-birth; clinical conditions (obesity, diabetes, multiple sclerosis, Parkinson disease); medications (anticholinergics, a-adrenergic blockers); and chronically increased intraabdominal pressure from chronic obstructive pulmonary disease (COPD), chronic constipation, or obesity.1 Loss of urethral support contributes to stress incontinence. Weakness of the perineal body from childbirth predisposes to rectoceles and enteroceles. Epidermoid Cyst A small, firm, round cystic nodule in the labia suggests an epidermoid cyst. They are yellowish in color. Look for the dark punctum marking the blocked opening of the gland Venereal Wart (Condyloma Acuminatum) Warty lesions on the labia and within the vestibule suggest condylomata acuminata from infection with human papillomavirus. Genital Herpes Shallow, small, painful ulcers on red bases suggest a herpes infection. Initial infection may be extensive, as illustrated here. Recurrent infections are usually confined to a small local patch. Syphilitic Chancre A firm, painless ulcer suggests the chancre of primary syphilis. Because most chancres in women develop internally, they often go undetected Secondary Syphilis (Condyloma Latum) Slightly raised, round or oval flattopped papules covered by a gray exudate suggest condylomata lata, a manifestation of secondary syphilis. They are contagious. Carcinoma of the Vulva An ulcerated or raised red vulvar lesion in an elderly woman may indicate vulvar carcinoma. Trichomonas vaginitis Discharge: Yellowish green, often profuse, may be malodorous Other Symptoms: Itching, vaginal soreness, dyspareuniaVulva: May be red Vagina: May be normal or red, with red spots, petechiae Laboratory Assessment: Saline wet mount for trichomonads Candida vaginitis Discharge White, curdy, often thick, not malodorous Other Symptoms: Itching, vaginal soreness, external dysuria, dyspareunia Vulva: Often red and swollen Vagina: Often red with white patches of discharge Laboratory Assessment: KOH preparation for branching hyphae Abnormalities of the Cervix Endocervical polyp A bright red, smooth mass that protrudes from the os suggests a polyp. It bleeds easily. Mucopurulent cervicitis A yellowish exudate emerging from the cervical os suggests infection from Chlamydia, gonorrhea (often asymptomatic), or herpes. Carcinoma of the cervix An irregular, hard mass suggests cancer. Early lesions are best detected by colposcopy following abnormal Pap smear from of high risk of HPV. Fetal exposure to diethylstilbestrol (DES) Several changes may occur: a collar of tissue around the cervix, columnar epithelium that covers the cervix or extends to the vaginal wall (then termed vaginal adenosis), and, rarely, carcinoma of the vagina. Relaxations of the Pelvic Floor A cystocele is a bulge of the anterior wall of the upper part of the vagina, together with the urinary bladder above it. A cystourethrocele involves both the bladder and the urethra as they bulge into the anterior vaginal wall throughout most of its extent. A rectocele is a bulge of the posterior vaginal wall, together with a portion of the rectum.A prolapsed uterus has descended down the vaginal canal. There are three degrees of severity: first, still within the vagina (as illustrated); second, with the cervix at the introitus; and third, with the cervix outside the introitus. Positions of the Uterus and Uterine Myomas An anteverted uterus lies in a forward position at roughly a right angle to the vagina. This is the most common position. Anteflexion—a forward flexion of the uterine body in relation to the cervix— often coexists. A retroverted uterus is tilted posteriorly with its cervix facing anteriorly. A retroflexed uterus has a posterior tilt that involves the uterine body but not the cervix. A uterus that is retroflexed or retroverted may be felt only through the rectal wall; some cannot be felt at all. A myoma of the uterus is a very common benign tumor that feels firm and often irregular. There may be more than one. A myoma on the posterior surface of the uterus may be mistaken for a retrodisplaced uterus; one on the anterior surface may be mistaken for an anteverted uterus. STI For STIs and HIV, assess risk factors by taking a careful sexual history and counseling patients about spread of disease and ways to reduce high-risk practices. Test women younger than 26 years and pregnant women for Chlamydia; in women at increased risk and pregnant women, test for gonorrhea, syphilis, and HIV. In 2006, the CDC recommended universal screening for HIV for those ages 13 to 64 because infection occurs in many without known risk factors. For sexually transmitted infections (STIs) and diseases, identify sexual preference (male, female, or both) and the number of sexual partners in the previous month. Ask if the patient has concerns about HIV infection, desires HIV testing, or has current or past partners at risk. In women, some STIs do not produce symptoms, but do increase the risk of infertility. Chlamydial infection is a cause of urethritis, cervicitis, PID, ectopic pregnancy, infertility, and chronic pelvic pain. Risk factors include age younger than 26 years, multiple partners, and prior history of STIs. To improve detection and treatment, the CDC and the USPSTF57 strongly recommend screening for STIs, summarized below. CDC STI and HIV Screening Recommendations 2014 ● Chlamydia and gonorrhea screening annually for all sexually active women ages <25 years and older women with risk factors such as new or multiple sex partners, or a sex partner infected with an STI.● Chlamydia, syphilis, hepatitis B, and HIV screening for all pregnant women and gonorrhea screening for at-risk pregnant women starting early in pregnancy, with repeat testing as needed to protect the health of mothers and their infants. Chlamydia, gonorrhea, and syphilis screening at least once a year for all sexually active gay, bisexual, and other MSM. MSM who have multiple or anonymous partners should be screened more frequently for STIs (i.e., at 3-to 6-month intervals). ● HIV testing at least once for all adults and adolescents from ages 13 to 64 years. ● ● HIV testing at least once a year for anyone having unsafe sex or using injection drug equipment. Sexually active gay and bisexual men may benefit from testing every 3 to 6 months. Bacterial VaginosisDischarge: Gray or white, thin, homogeneous, scant, malodorous Other Symptoms: Fishy genital odor Vulva: Usually normal Vagina: Usually normal Laboratory Assessment: Saline wet mount for ―clue cells,‖ ―whiff test‖ with KOH for fishy odor Example of physical exam findings: Bilateral shotty inguinal adenopathy. External genitalia without erythema or lesions. Vaginal mucosa and cervix coated with thin white homogeneous discharge with mild fishy odor. After swabbing the cervix, no discharge visible in the cervical os. Uterus midline; no adnexal masses. Rectal vault without masses. Stool brown and negative for fecal blood. pH of vaginal discharge >4.5‖ These findings are consistent with bacterial vaginosis. **Menstruation Cervical Disorders and Cancer As estrogen stimulation increases during adolescence, all or part of this columnar epithelium is transformed into squamous epithelium by a process termed metaplasia. This change may block the secretions of columnar epithelium and cause retention cysts, also called nabothian cysts. This appear as translucent nodules on the cervical surface and have no pathologic significance. A cervical polyp usually arises from the endocervical canal, becoming visible when it protrudes through the cervical os. It is bright red, soft, and rather fragile. When only the tip is seen, it cannot be differentiated clinically from a polyp originating in the endometrium. Polyps are benign but may bleedMucopurulent cervicitis - produces purulent yellow drainage from the cervical os, usually from the Chlamydia trachomatis, Neisseria gonorrhoeae, or herpes infection. These infections are sexually transmitted and may occur without signs and symptoms Carcinoma of the cervix - begins in an area of metaplasia. In its earliest stages, it cannot be distinguished from a normal cervix. In later stages, an extensive, irregular, cauliflower-like growth may develop. Early frequent intercourse, multiple partners, smoking, and infection with HPV increase the risk for cervical cancer Fetal exposure to diethylstilbestrol (DES) - daughters of women who took DES during pregnancy are greatly increased risk for several abnormalities, including 1.) columnar epithelium that covers most or all of the cervix, 2.) vaginal adenosis, i.e. extension of the epithelium to the vaginal wall, and 3.) a circular collar or ridge of tissue, of varying shapes, between the cervix and vagina. Much less common is an otherwise rare carcinoma of the upper vagina ***Chapter 18 Amie, (Shawna->childhood vaccines through tanner staging-completed 10/5) **Newborn/Infant/Pediatric Assessment and Modification for Age **Normal VS. Abnormal Findings and Interpretation Newborn Skin Disorders (Hye) Ruddy (reddish purple color):newborn with polycythemiaCutis marmorata-prominent in premature infants or infants with congenital hypothyroidism and Down syndrome. If acrocyanosis does not disappear within 8 hours or with warming, cyanotic congenital heart disease should be considered. Central cyanosis in a baby or child of any age should raise suspicion of congenital heart disease. The best area to look for central cyanosis is the tongue and oral mucosa, not the nail beds, lips, or the extremities.café-au-lait spots (See below) -Pigmented light-brown lesions (<1 to 2 cm at birth) Isolated lesions have no significance,but multiple lesions with sharp borders may suggest neurofibromatosisSkin desquamation -normal in fullterm newborns but may rarely be a sign of placental circulatory insufficiency or congenital ichthyosis. Both erythema toxicum (see above pic 18-2) and pustular melanosis may appear similar to the pathologic vesiculopustular rash of herpes simplex or Staphylococcus aureus skin infection. Midline hair tufts over the lumbosacral spine region - a possible spinal cord defect.Jaundice within the first 24 hours of birth may be from hemolytic disease of the newborn. Late-appearing jaundice or jaundice that persists beyond 2 to 3 weeks should raise suspicions of biliary obstruction or liver disease. A common source of jaundice during the first couple of weeks is breastfeeding jaundice, which resolves around 10 to 14 days of life. Persistent jaundice requires evaluation. A unilateral dark, purplish lesion, or ―port wine stain‖ over the distribution of the ophthalmic branch of the trigeminal nerve may be a sign of Sturge–Weber syndrome, which is associated with seizures, hemiparesis, glaucoma, and mental retardation. Significant edema of the hands and feet of a newborn girl may be suggestive of Turner syndrome. Other features such as a webbed neck would reinforce this diagnosis.Webbed neck: Dehydration is a common problem in infants. Usual causes are insufficient intake or excess loss of fluids from diarrhea. Birthmarks (Hye) Eyelid Patch: This birthmark fades, usually within the first year of life. Salmon Patch: called ―stork bite,‖ or ―angel kiss,‖splotchy pink mark fades with age. Café-au-lait Spots: These light-brown pigmented lesions usually have borders and are uniform. Noted in more than 10% of black infants. If > 5 café-au-lait spots exist, consider the diagnosis of neurofibromatosisSlate Blue Patches :more common among dark-skinned babies. to note that are not mistaken for bruises. Childhood VaccinationsPediatric Immunizations: https://www.cdc.gov/vaccines/schedules/downloads/child/0-18yrs-child-combined-schedule.pdfDevelopmental Milestones p. 853-890 Early childhood (1-4 years): after infancy, physical growth slows by ½; after 2 years, toddlers gain 2-3 kg and grow 5 cm/year. Gross motor skills: Walk by 15 months, run by 2 years, tricycle/jump by 4 years. Drawing/Fine motor: 18-month old scribbles, 2-year old draws lines, 4- year old makes circles; Cognitive: toddlers move from sensorimotor to symbolic thinking. 18- month old: 10-20 words, 2-year old: three-word sentences; 4-year old: complex sentences. Toddlers are impulsive with poor self-regulation= common temper tantrums. Middle Childhood (5-10 years): Physical growth: steadily and slowly, strength and coordination improve. More awareness of physical disability limitations. Cognitive: “concrete operational,” meaning capable of limited logic and more complex learning. Limited ability to understand consequences and are greatly influenced by school, family, and environment. + language complexity. Social: more independent, start activities, enjoy accomplishments (this helps with self-esteem), + self-identity evolves. + Guilt and poor self-esteem may emerge. Clear sense of “right” and “wrong.” Adolescents (11-20 years): Physical growth: pubertal transformation over several years (age 10- 14 years in girls, 11-16 years in boys); Cognitive: progression from concrete to formal operational thinking, ability to reason w/ abstract thinking; Social: family-influence versus autotomy and peer influence. + struggle for identity, independence, intimacy, stress, healthrelated problems, and high-risk behaviors. Tanner Staging Females: p. 897 Stage 1: preadolescent (elevation of nipple only)Stage 2: breast bud stage (elevation of breast and nipple as a small mound; enlargement of areolar diameter Stage 3: further enlargement of elevation of breast and areola; no contour separation Stage 4: projection of areola and nipple to form a second mound above the level of the breast Stage 5: mature stage (projection of nipple only; areola has receded to general contour of the breast) Males: p. 899 Stage 1: no pubic hair, penis is the same size as in childhood, testes and scrotum the same size as childhood Stage 2: sparse hair growth at base of penis, penis has slight to no enlargement, testes and scrotum are larger Stage 3: darker, courser, spreading pubic hair, increase in penis size (primarily length); further enlargement of testes and scrotum Stage 4: adult-type pubic hair except not involving thighs, further width and length growth of penis, development of the glans, further enlargement of testes and scrotal skin darkens Stage 5: adult hair quality and quantity, adult size and shape of penis, adult size and shape of testes and scrotumChapter 19 Kasie Pregnancy and Assessment- Prenatal care focuses on optimizing health and minimizing risk for the mother and fetus. The goals of the initial prenatal visit are to define the health status of the mother and fetus, confirm the pregnancy and estimate gestational age, develop a plan for continuing care, and counsel the mother about her expectations and concerns. During subsequent visits, you should assess any interim changes in the health status of the mother and fetus, review specific physical examination findings related to the pregnancy, and provide counseling and timely preventive screenings. Initial prenatal history ● Confirmation of pregnancy ● Symptoms of pregnancy ● Concerns and attitudes toward the pregnancy ● Current health and past clinical history ● Past obstetric history ● Risk factors for maternal and fetal health ● Family history of patient and father of the newborn ● Plans for breastfeeding ● Plans for postpartum contraception ● Determining gestational age and expected date of deliveryWeight loss due to nausea and vomiting that exceeds 5% of prepregnancy weight is considered excessive, representing hyperemesis gravidarum, and can lead to adverse pregnancy outcomes. Measure the blood pressure at every visit. Blood pressure parameters in pregnancy follow the recommendations of the Eighth Joint National Committee (JNC8) (see p. 130).34 Baseline prepregnancy readings are important for determining the patient’s usual range. In the second trimester, blood pressure normally drops below the no pregnant state. Hypertensive disorders affect 5% to 10% of all pregnancies, so all elevations in blood pressure must be closely monitored. Hypertension can be both an independent diagnosis and a marker of preeclampsia syndrome. This syndrome is “a pregnancy-specific syndrome that can affect virtually every organ system.”35 ACOG issued new recommendations on hypertension in pregnancy in 2013 that no longer depend on proteinuria, recognizing that preeclampsia cannot only be lethal for the mother and fetus, but doubles the risk of later-life cardiovascular disease. Preeclampsia increases cardiovascular disease risk eight-to nine fold in women with preeclampsia giving birth before 34 weeks’ gestation.34 Definition of Preeclampsia is SBP ≥140 or DBP ≥90 after 20 weeks on two occasions at least 4 hours apart in a woman with previously normal BP or BP ≥160/110 confirmed within minutes and proteinuria ≥300 mg/24 hours, protein: creatinine ≥0.3, or dipstick 1+; OR new onset hypertension without proteinuria and any of the following: thrombocytopenia (platelets <100,000/μL), impaired liver function (liver transaminase levels more than twice normal), new renal insufficiency (creatinine >1.1 mg/dL or doubles in the absence of renal disease), pulmonary edema, or new onset cerebral or visual symptoms.34 Head and Neck Face: With the patient seated, inspect the head and neck, paying particular attention to the following features: ■ Face. Irregular brownish patches around the forehead, cheeks, nose, and jaw are known as chloasma or melasma, the ―mask of pregnancy,‖ a normal skin finding during pregnancy. ■ Hair. Hair may become dry, oily, or sparse during pregnancy; mild hirsutism on the face, abdomen, and extremities is also common. 942 Facial edema after 20gestational weeks is suspicious for preeclampsia and should be investigated. Localized patches of hair loss should not be attributed to pregnancy (though postpartum hair loss is common). ● Gestational hypertension is systolic blood pressure (SBP) >140 mm Hg or diastolic blood pressure (DBP) >90 mm Hg first documented after 20 weeks, without proteinuria or preeclampsia, that resolves by 12 weeks postpartum. ● Chronic hypertension is SBP >140 or DBP >90 that predates pregnancy. Chronic hypertension affects almost 2% of U.S. births. Facial edema after 20 gestational weeks is suspicious for preeclampsia and should be investigated. Localized patches of hair loss should not be attributed to pregnancy (though postpartum hair loss is common). Anemia may cause conjunctival pallor. Erosions and perforations of the nasal septum may represent use of intranasal cocaine. Dental problems are associated with poor pregnancy outcomes, so initiate prompt dental referrals for tooth and gum pain or infections. Thyroid enlargement, goiters, and nodules are abnormal and require investigation. Dyspnea accompanied by increased respiratory rate, coughing, rales, or respiratory distress point to possible infection, asthma, pulmonary embolism, or per- partum cardiomyopathy Assess dyspnea and signs of heart failure for possible peripartum cardiomyopathy, particularly in the late stages of pregnancy. Murmurs may signal anemia. Investigate any diastolic murmur. Prenatal Laboratory Screenings. The standard prenatal screening panel includes blood type and Rh, antibody screen, complete blood count—especially hematocrit and platelet count, rubella titer, syphilis test, hepatitis B surface antigen, HIV test, STI screen for gonorrhea and chlamydia, and urinalysis with culture. Scheduled screenings include an oral glucose tolerance test for gestational diabetes around 24 to 28 weeks and a rectovaginal swab for group B streptococcus between 35 and 37 weeks. Because obesity is associated with insulin resistance, the obese pregnant patient is at increased risk of both gestational diabetes and type 2 diabetes mellitus. Both ACOG and the American Diabetes Association recommend testing for glucose tolerance in the first trimester for obese pregnant patients.33 if indicated, pursue additional tests related to the mother‘s risk factors, such as screening for aneuploidy, Tay–Sachs disease, or other genetic diseases, and amniocentesis Immunizations. Given the persistent increase in pertussis infection in the United States, the Centers for Disease Control and Prevention (CDC) Advisory Committee on Immunization Practices and ACOG recommend that T-dap be administered during each pregnancy, ideally at 27 to 36 weeks of gestation, regardless of the prior immunization history.21 Caretakers in direct contact with the infant should also receive T-dap. Inactivated influenza vaccination is indicated in any trimester during the influenza season.22 The following vaccinesare safe during pregnancy: pneumococcal, meningococcal, and hepatitis B. Hepatitis A and B, meningococcal polysaccharide and conjugate, and pneumococcal polysaccharide vaccines can be given, if indicated.23 The following vaccines are not safe during pregnancy: measles/mumps/rubella, polio, and varicella. All women should have rubella titers drawn during pregnancy and be immunized after birth if found to be nonimmune. Check Rh (D) and antibody typing at the first prenatal visit, at 28 weeks, and at delivery. Anti-D immunoglobulin should be given to all Rh-negative women at 28 weeks‘ gestation and again within 3 days of delivery to prevent sensitization if the infant is Rh-D positive. Chapter 20 Maria M. Geriatric Assessment General Survey. As the patient enters the room, how does the patient walk to the chair? Move onto the examining table? Are there changes in posture or involuntary movements? Note the patient‘s hygiene and dress. Assess the patient‘s apparent state of health, degree of vitality, and mood and affect Assess the patient for orthostatic hypotension, defined as a drop in SBP of ≥20 mm Hg or DBP of ≥10 mm Hg within 3 minutes of standing. -UNDERNUTRITION, WEAKNESS→FRAILTY -Kyphosis →increase risk falls -Flat affect→depression, alzheimer, Parkinson’s disease **VITAL SIGNS- .Normal VS. Abnormal Findings and Interpretation VITAL SIGNS *Abnormal if SBP drops > 20 mmHg or DBP of >10 mm hg within 3 min of standing *RR > OR EQUAL TO 25 BPM = lower respiratory infection, heart failure, COPD exacerbation *low weight→ poor nutrition /alcoholism , cognitive impairment , malignancy, chronic organ failure, (cardiac,renal, pulmonary) medication use, social isolation and poverty-Rapidly increase weights occurs in fluid overload SKIN Normal:skin thinning, loss elastic tissue and turgor and wrinkling. Benign lesions:comedones, blackheads on cheeks and around eyes, cherry angiomas, seborrheic keratoses seborrheic keratoses . comedones -watch for lesions indicative of basal cell carcinoma, a translucent nodule that spreads and leaves a depressed center wotja a form elevated border -squamous cell carcinoma , a firm reddish appearing lesion often emerging in a sun exposed area. HEAD AND NECK -Observe for senile ptosis , cjecl lower lids for ectropion(lower lid turns outward) or entropion (inward turning or lid) *also see pg 274-275 for more picsHearing-removal cerum improves hearing -oral cavity= ask pt to remove dentures to see gums. malodor=poor hygiene, periodontitis and caries -thyroid :older adults common cause of hyperthyroidism are graves disease and toxic multinodular goiter -thorax/lungs=increase AP diameter, purs-lipped breathing, dyspnea while talking →COPD -CARDIOVASCULAR:Isolated systolic hypertension and a widened PP are cardiac risk factors, prompting search left ventricular hypertrophy , extra heart sounds such as S3 and S4 abnormal. -breast and axilla :any lump or mass is abnormal -abdomen:bruit then suspect atherosclerotic vascular disease -Periph,vasc. Sytm: diminished or absent pulse present in PAD FEMALE GENITALIA/PELVIC:Erythema with satellite lesions results from Candida Infections -tortuous atheresclerotic aorta can raise pressure in left jugular veings Elder Abuse pg(984) Elder Mistreatment and Abuse. Screen vulnerable older adults for possible elder mistreatment, which includes abuse, neglect, exploitation, and abandonment. - higher among older adults with depression and dementia. -undetected due to the patient‘s fear of reprisal, physical or cognitive inability to report, and unwillingness to expose the abuser, of whom 90% are family members. Self-neglect, or ―the behavior of an elderly person that threatens his/her own health and safety,‖ is also a growing national concern and represents more the 50% of adult protective service referrals. -a careful history and high index of suspicion are important. Functional AssessmentsTechniques of Examination begins with ―Assessing Functional Status: the ‗Sixth Vital Sign,‘‖ which includes steps for evaluating the pt‘s risk for FALLS, one of the primary threats to older adult well-being. Establishing functional status provides a baseline for making interventions that optimize the pT‘s level of function and for identifying geriatric syndromes that can be treated or delayed, such as cognitive impairment, falls, incontinence, low BMI, dizziness, and impaired vision and hearing. Your assessment of functional status begins as the patient enters the room. *The 10-Minute Geriatric Screener is one of several validated and time-efficient performancebased assessment tools. T *he Screener is brief, has high interrater agreement, and can be easily used by office staff. It covers 3 ImporRTANT. Areas:: cognitive, psychosocial, and physical function. It includes vision, hearing, and questions about urinary incontinence, ] Adult Vaccinations Immunizations. Recommend vaccination for: - influenza; pneumonia, both PPSV23 and PCV13; - herpes zoster (shingles); -and tetanus/diphtheria and pertussis (Tdap and Td). *-*-*-*-For the most up-to-date recommendations, consult the updated annual guidelines and contraindications provided by the CDC at http://www.cdc.gov/vaccines. ****CDC information bellow from: https://www.cdc.gov/vaccines/adults/rec-vac/index.htmlAs we get older, our immune systems tend to weaken over time, putting us at higher risk for certain diseases. This is why, in addition to seasonal flu (influenza) vaccine and Td or Tdap vaccine (tetanus, diphtheria, and pertussis), you should also get: ● Shingles vaccine, which protects against shingles and the complications from the disease (recommended for healthy adults 50 years and older) ● Pneumococcal vaccines, which protect against pneumococcal disease, including infections in the lungs and bloodstream (recommended for all adults over 65 years old, and for adults younger than 65 years who have certain chronic health conditions) Older Adult Immunizations 2015 Influenza Vaccine The influenza vaccine protects against up to two strains of influenza A and influenza B in both trivalent and quadrivalent formulations. The following groups should receive the influenza vaccine each year: ● *All adults ≥50 years*Adults with chronic pulmonary and cardiovascular disorders including asthma (but excluding hypertension), and renal, hepatic, neurologic, hematologic, or metabolic disorders including diabetes Adults who are immunosuppressed from medication or HIV ● Residents of nursing homes and other long-term care facilities; adults with morbid obesity (BMI ≥40) *pneumococcal vaccine *zoster vaccine Tetanus/diphtheria (Td) and Tetanus/diphtheria/pertussis (Tdap) Vaccine [Show More]
Last updated: 1 year ago
Preview 1 out of 76 pages
Instant download
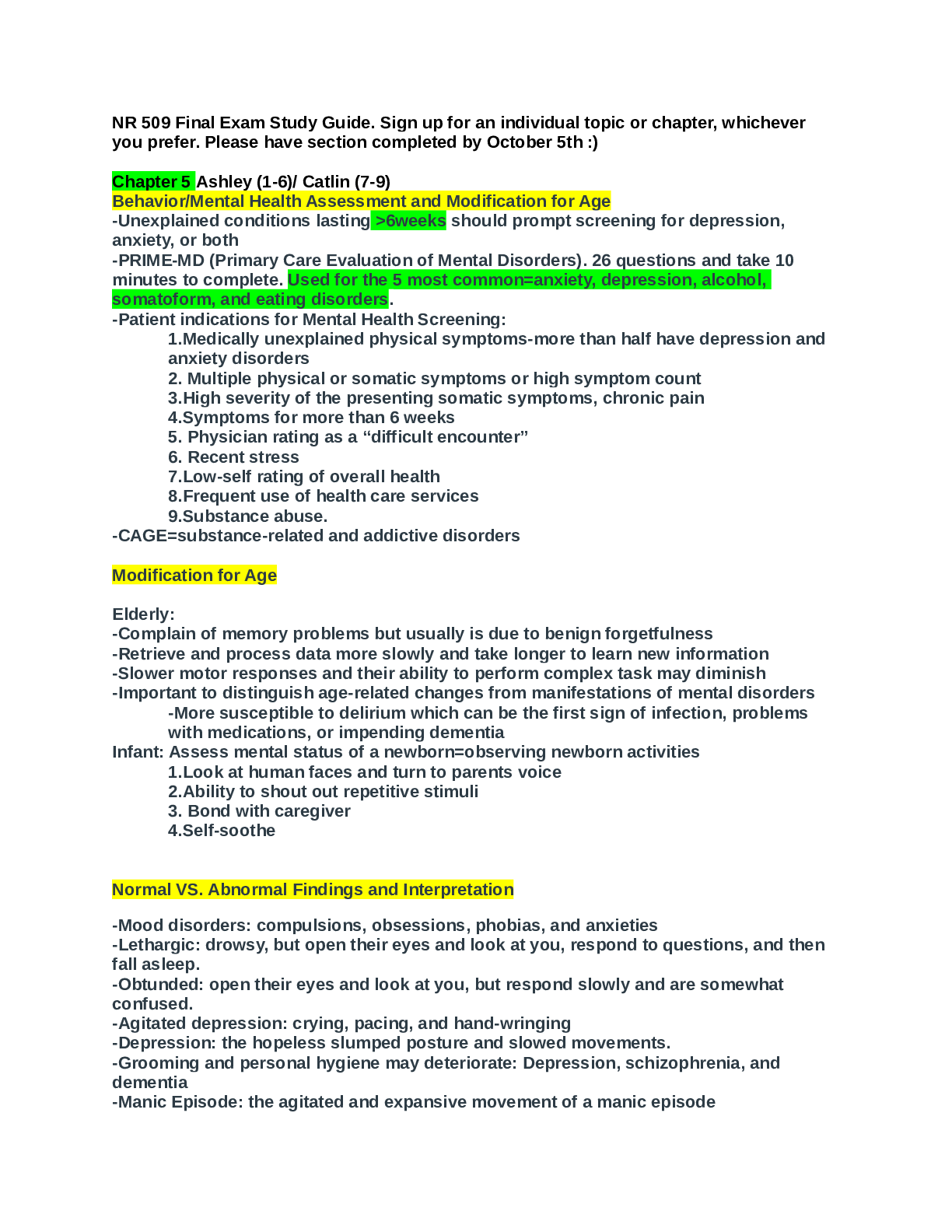
Buy this document to get the full access instantly
Instant Download Access after purchase
Add to cartInstant download
Reviews( 0 )
Document information
Connected school, study & course
About the document
Uploaded On
Mar 16, 2021
Number of pages
76
Written in
Additional information
This document has been written for:
Uploaded
Mar 16, 2021
Downloads
0
Views
44

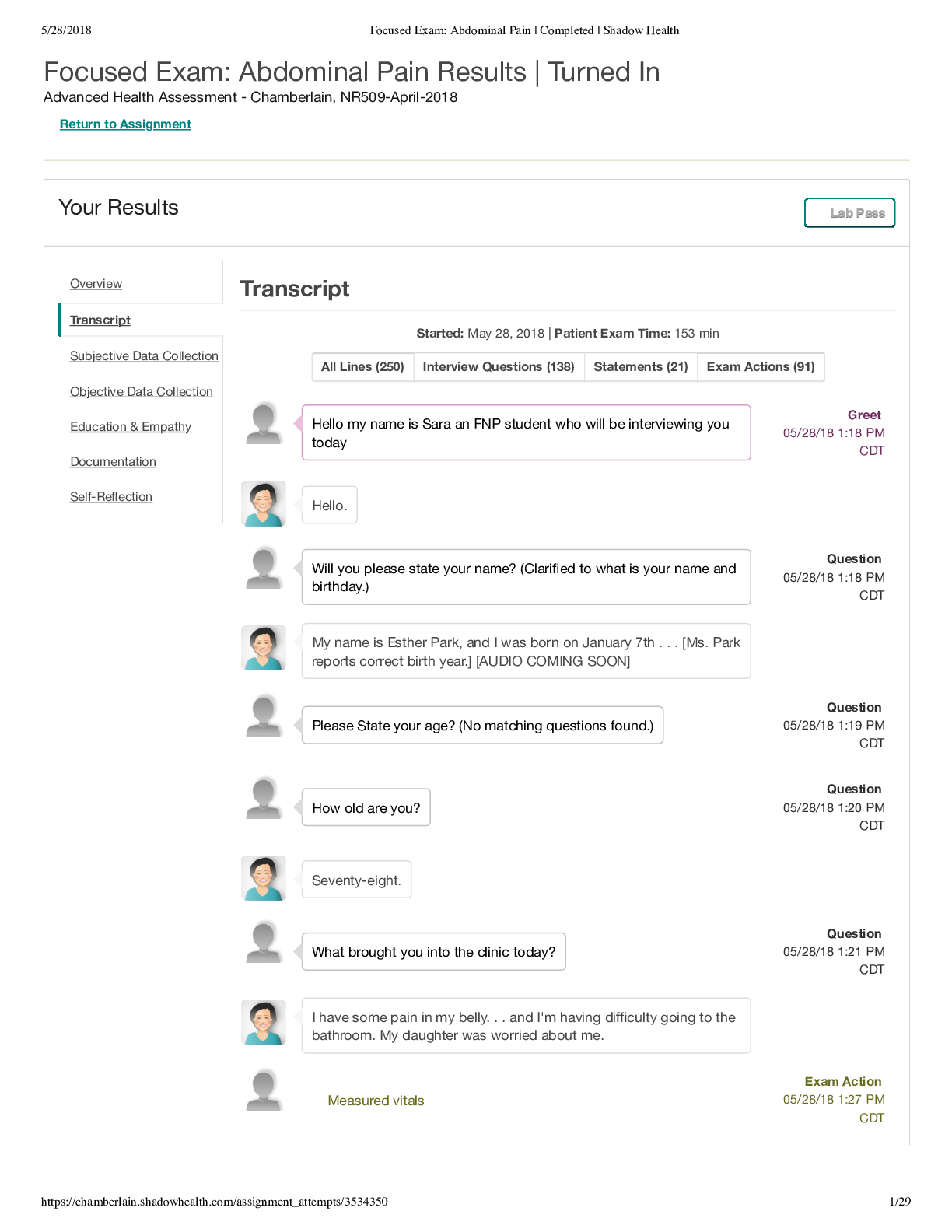
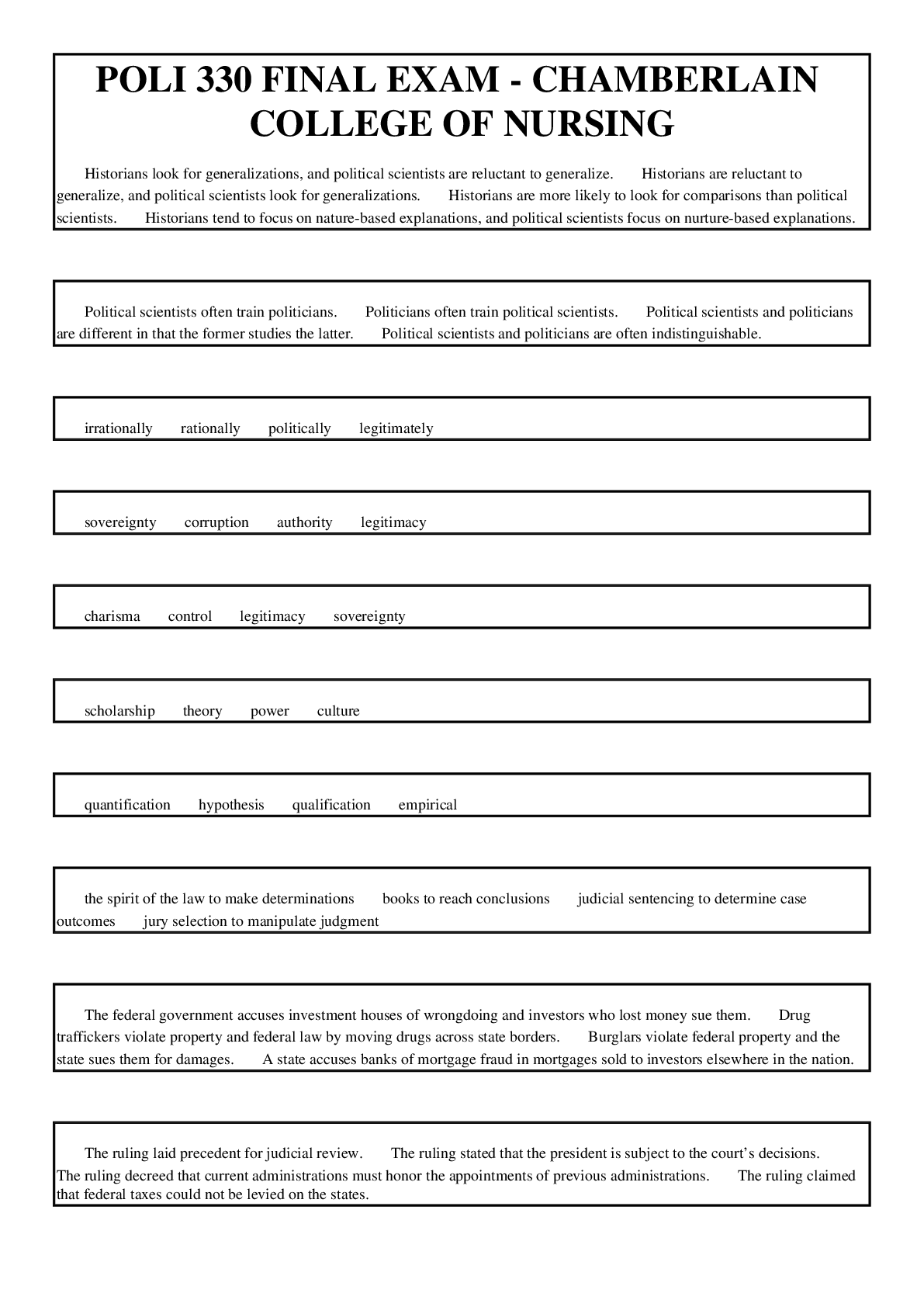
.png)