NURS 223 EXAM 2-COMPLETED A with Elaborate Answers and responses
Document Content and Description Below
NURS 223 EXAM 2 1. The student nurse learning about cellular regulation understands that which process occurs during the S phase of the cell cycle? a. Actual division (mitosis) b. Doubling of DNA ... c. Growing extra membrane d. No reproductive activity During the S phase, the cell must double its DNA content through DNA synthesis. Actual division, or mitosis, occurs during the M phase. Growing extra membrane occurs in the G1 phase. During the G0 phase, the cell is working but is not involved in any reproductive activity. 2. A student nurse asks the nursing instructor what “apoptosis” means. What response by the instructor is best? a. Growth by cells enlarging b. Having the normal number of chromosomes c. Inhibition of cell growth d. Programmed cell death ANS: D Apoptosis is programmed cell death. With this characteristic, organs and tissues function with cells that are at their peak of performance. Growth by cells enlarging is hyperplasia. Having the normal number of chromosomes is euploidy. Inhibition of cell growth is contact inhibition. 3. The nursing instructor explains the difference between normal cells and benign tumor cells. What information does the instructor provide about these cells? a. Benign tumors grow through invasion of other tissue. b. Benign tumors have lost their cellular regulation from contact inhibition. c. Growing in the wrong place or time is typical of benign tumors. d. The loss of characteristics of the parent cells is called anaplasia. Benign tumors are basically normal cells growing in the wrong place or at the wrong time. Benign cells grow through hyperplasia, not invasion. Benign tumor cells retain contact inhibition. Anaplasia is a characteristic of cancer cells. 4. A group of nursing students has entered a futuristic science contest in which they have “developed” a cure for cancer. Which treatment would most likely be the winning entry? a. Artificial fibronectin infusion to maintain tight adhesion of cells b. Chromosome repair kit to halt rapid division of cancer cells c. Synthetic enzyme transfusion to allow rapid cellular migration d. Telomerase therapy to maintain chromosomal immortality ANS: A Cancer cells do not have sufficient fibronectin and so do not maintain tight adhesion with other cells. This is part of the mechanism of metastasis. Chromosome alterations in cancer cells (aneuploidy) consist of having too many, too few, or altered chromosome pairs. This does not necessarily lead to rapid cellular division. Rapid cellular migration is part of metastasis. Immortality is a characteristic of cancer cells due to too much telomerase. 5. Which statement about carcinogenesis is accurate? a. An initiated cell will always become clinical cancer. b. Cancer becomes a health problem once it is 1 cm in size. c. Normal hormones and proteins do not promote cancer growth. d. Tumor cells need to develop their own blood supply. Tumors need to develop their own blood supply through a process called angiogenesis. An initiated cell needs a promoter to continue its malignant path. Normal hormones and proteins in the body can act as promoters. A 1-cm tumor is a detectable size, but other events have to occur for it to become a health problem. 6. The nurse caring for oncology clients knows that which form of metastasis is the most common? a. Bloodborne b. Direct invasion c. Lymphatic spread d. Via bone marrow Bloodborne metastasis is the most common way for cancer to metastasize. Direct invasion and lymphatic spread are other methods. Bone marrow is not a medium in which cancer spreads, although cancer can occur in the bone marrow. 7. A nurse is assessing a client with glioblastoma. What assessment is most important? a. Abdominal palpation b. Abdominal percussion c. Lung auscultation d. Neurologic examination A glioblastoma arises in the brain. The most important assessment for this client is the neurologic examination. 8. A nurse has taught a client about dietary changes that can reduce the chances of developing cancer. What statement by the client indicates the nurse needs to provide additional teaching? a. “Foods high in vitamin A and vitamin C are important.” b. “I’ll have to cut down on the amount of bacon I eat.” c. “I’m so glad I don’t have to give up my juicy steaks.” d. “Vegetables, fruit, and high-fiber grains are important.” ANS: C To decrease the risk of developing cancer, one should cut down on the consumption of red meats and animal fat. The other statements are correct. 9. A client is in the oncology clinic for a first visit since being diagnosed with cancer. The nurse reads in the client’s chart that the cancer classification is TISN0M0. What does the nurse conclude about this client’s cancer? a. The primary site of the cancer cannot be determined. b. Regional lymph nodes could not be assessed. c. There are multiple lymph nodes involved already. d. There are no distant metastases noted in the report. TIS stands for carcinoma in situ; N0 stands for no regional lymph node metastasis; and M0 stands for no distant metastasis. 10. A client asks the nurse if eating only preservative- and dye-free foods will decrease cancer risk. What response by the nurse is best? a. “Maybe; preservatives, dyes, and preparation methods may be risk factors.” b. “No; research studies have never shown those things to cause cancer.” c. “There are other things you can do that will more effectively lower your risk.” d. “Yes; preservatives and dyes are well known to be carcinogens.” Dietary factors related to cancer development are poorly understood, although dietary practices are suspected to alter cancer risk. Suspected dietary risk factors include low fiber intake and a high intake of red meat or animal fat. Preservatives, preparation methods, and additives (dyes, flavorings, sweeteners) may have cancer-promoting effects. It is correct to say that other things can lower risk more effectively, but this does not give the client concrete information about how to do so, and also does not answer the client’s question. 1. The nursing student learning about cancer development remembers characteristics of normal cells. Which characteristics does this include? (Select all that apply.) a. Differentiated function b. Large nucleus-to-cytoplasm ratio c. Loose adherence d. Nonmigratory e. Specific morphology ANS: A, D, E Normal cells have the characteristics of differentiated function, nonmigratory, specific morphology, a smaller nucleus-to-cytoplasm ratio, tight adherence, and orderly and well-regulated growth. 2. The nurse working with oncology clients understands that interacting factors affect cancer development. Which factors does this include? (Select all that apply.) a. Exposure to carcinogens b. Genetic predisposition c. Immune function d. Normal doubling time e. State of euploidy The three interacting factors needed for cancer development are exposure to carcinogens, genetic predisposition, and immune function. 3. A nurse is participating in primary prevention efforts directed against cancer. In which activities is this nurse most likely to engage? (Select all that apply.) a. Demonstrating breast self-examination methods to women b. Instructing people on the use of chemoprevention c. Providing vaccinations against certain cancers d. Screening teenage girls for cervical cancer e. Teaching teens the dangers of tanning booths ANS: B, C, E Primary prevention aims to prevent the occurrence of a disease or disorder, in this case cancer. Secondary prevention includes screening and early diagnosis. Primary prevention activities include teaching people about chemoprevention, providing approved vaccinations to prevent cancer, and teaching teens the dangers of tanning beds. Breast examinations and screening for cervical cancer are secondary prevention methods. 4. A nurse is providing community education on the seven warning signs of cancer. Which signs are included? (Select all that apply.) a. A sore that does not heal b. Changes in menstrual patterns c. Indigestion or trouble swallowing d. Near-daily abdominal pain e. Obvious change in a mole ANS: A, B, C, E The seven warning signs for cancer can be remembered with the acronym CAUTION: changes in bowel or bladder habits, a sore that does not heal, unusual bleeding or discharge, thickening or lump in the breast or elsewhere, indigestion or difficulty swallowing, obvious change in a wart or mole, and nagging cough or hoarseness. Abdominal pain is not a warning sign. Chapter 22: Care of Patients with Cancer 1. A nurse in the oncology clinic is providing preoperative education to a client just diagnosed with cancer. The client has been scheduled for surgery in 3 days. What action by the nurse is best? a. Call the client at home the next day to review teaching. b. Give the client information about a cancer support group. c. Provide all the preoperative instructions in writing. d. Reassure the client that surgery will be over soon. Clients are often overwhelmed at a sudden diagnosis of cancer and may be more overwhelmed at the idea of a major operation so soon. This stress significantly impacts the client’s ability to understand, retain, and recall information. The nurse should call the client at home the next day to review the teaching and to answer questions. The client may or may not be ready to investigate a support group, but this does not help with teaching. Giving information in writing is important (if the client can read it), but in itself will not be enough. Telling the client that surgery will be over soon is giving false reassurance and does nothing for teaching. 2. A nurse reads on a hospitalized client’s chart that the client is receiving teletherapy. What action by the nurse is best? a. Coordinate continuation of the therapy. b. Place the client on radiation precautions. c. No action by the nurse is needed at this time. d. Restrict visitors to only adults over age 18. ANS: A The client needs to continue with radiation therapy, and the nurse can coordinate this with the appropriate department. The client is not radioactive, so radiation precautions and limiting visitors are not necessary. 3. A new nurse has been assigned a client who is in the hospital to receive iodine-131 treatment. Which action by the nurse is best? a. Ensure the client is placed in protective isolation. b. Hand off a pregnant client to another nurse. c. No special action is necessary to care for this client. d. Read the policy on handling radioactive excreta. This type of radioisotope is excreted in body fluids and excreta (urine and feces) and should not be handled directly. The nurse should read the facility’s policy for handling and disposing of this type of waste. The other actions are not warranted. 4. A client in the oncology clinic reports her family is frustrated at her ongoing fatigue 4 months after radiation therapy for breast cancer. What response by the nurse is most appropriate? a. “Are you getting adequate rest and sleep each day?” b. “It is normal to be fatigued even for years afterward.” c. “This is not normal and I’ll let the provider know.” d. “Try adding more vitamins B and C to your diet.” ANS: B Regardless of the cause, radiation-induced fatigue can be debilitating and may last for months or years after treatment has ended. Rest and adequate nutrition can affect fatigue, but it is most important that the client understands this is normal. 5. A client tells the oncology nurse about an upcoming vacation to the beach to celebrate completing radiation treatments for cancer. What response by the nurse is most appropriate? a. “Avoid getting salt water on the radiation site.” b. “Do not expose the radiation area to direct sunlight.” c. “Have a wonderful time and enjoy your vacation!” d. “Remember you should not drink alcohol for a year.” The skin overlying the radiation site is extremely sensitive to sunlight after radiation therapy has been completed. The nurse should inform the client to avoid sun exposure to this area. This advice continues for 1 year after treatment has been completed. The other statements are not appropriate. 6. A client is receiving chemotherapy through a peripheral IV line. What action by the nurse is most important? a. Assessing the IV site every hour b. Educating the client on side effects c. Monitoring the client for nausea d. Providing warm packs for comfort ANS: A Intravenous chemotherapy can cause local tissue destruction if it extravasates into the surrounding tissues. Peripheral IV lines are more prone to this than centrally placed lines. The most important intervention is prevention, so the nurse should check hourly to ensure the IV site is patent, or frequently depending on facility policy. Education and monitoring for side effects such as nausea are important for all clients receiving chemotherapy. Warm packs may be helpful for comfort, but if the client reports that an IV site is painful, the nurse needs to assess further. 7. A client with cancer is admitted to a short-term rehabilitation facility. The nurse prepares to administer the client’s oral chemotherapy medications. What action by the nurse is most appropriate? a. Crush the medications if the client cannot swallow them. b. Give one medication at a time with a full glass of water. c. No special precautions are needed for these medications. d. Wear personal protective equipment when handling the medications. ANS: D During the administration of oral chemotherapy agents, nurses must take the same precautions that are used when administering IV chemotherapy. This includes using personal protective equipment. These medications cannot be crushed, split, or chewed. Giving one at a time is not needed. 8. The nurse working with oncology clients understands that which age-related change increases the older client’s susceptibility to infection during chemotherapy? a. Decreased immune function b. Diminished nutritional stores c. Existing cognitive deficits d. Poor physical reserves As people age, there is an age-related decrease in immune function, causing the older adult to be more susceptible to infection than other clients. Not all older adults have diminished nutritional stores, cognitive dysfunction, or poor physical reserves. 9. After receiving the hand-off report, which client should the oncology nurse see first? a. Client who is afebrile with a heart rate of 108 beats/min b. Older client on chemotherapy with mental status changes c. Client who is neutropenic and in protective isolation d. Client scheduled for radiation therapy today ANS: B Older clients often do not exhibit classic signs of infection, and often mental status changes are the first observation. Clients on chemotherapy who become neutropenic also often do not exhibit classic signs of infection. The nurse should assess the older client first. The other clients can be seen afterward. 10. A client has a platelet count of 9800/mm3. What action by the nurse is most appropriate? a. Assess the client for calf pain, warmth, and redness. b. Instruct the client to call for help to get out of bed. c. Obtain cultures as per the facility’s standing policy. d. Place the client on protective isolation precautions. A client with a platelet count this low is at high risk for serious bleeding episodes. To prevent injury, the client should be instructed to call for help prior to getting out of bed. Calf pain, warmth, and redness might indicate a deep vein thrombosis, not associated with low platelets. Cultures and isolation relate to low white cell counts. 11. A client hospitalized for chemotherapy has a hemoglobin of 6.1 mg/dL. What medication should the nurse prepare to administer? a. Epoetin alfa (Epogen) b. Filgrastim (Neupogen) c. Mesna (Mesnex) d. Oprelvekin (Neumega) ANS: A The client’s hemoglobin is low, so the nurse should prepare to administer epoetin alfa, a colony-stimulating factor that increases production of red blood cells. Filgrastim is for neutropenia. Mesna is used to decrease bladder toxicity from some chemotherapeutic agents. Oprelvekin is used to increase platelet count. 12. A nurse works with clients who have alopecia from chemotherapy. What action by the nurse takes priority? a. Helping clients adjust to their appearance b. Reassuring clients that this change is temporary c. Referring clients to a reputable wig shop d. Teaching measures to prevent scalp injury All of the actions are appropriate for clients with alopecia. However, the priority is client safety, so the nurse should first teach ways to prevent scalp injury. 13. A client is receiving interleukins along with chemotherapy. What assessment by the nurse takes priority? a. Blood pressure b. Lung assessment c. Oral mucous membranes d. Skin integrity ANS: A Interleukins can cause capillary leak syndrome and fluid shifting, leading to intravascular volume depletion. Although all assessments are important in caring for clients with cancer, blood pressure and other assessments of fluid status take priority. 14. A client is receiving rituximab (Rituxan) and asks how it works. What response by the nurse is best? a. “It causes rapid lysis of the cancer cell membranes.” b. “It destroys the enzymes needed to create cancer cells.” c. “It prevents the start of cell division in the cancer cells.” Rituxan prevents the initiation of cancer cell division. The other statements are not accurate. 15. Four clients are receiving tyrosine kinase inhibitors (TKIs). Which of these four clients should the nurse assess first? a. Client with dry, itchy, peeling skin b. Client with a serum calcium of 9.2 mg/dL c. Client with a serum potassium of 2.8 mEq/L d. Client with a weight gain of 0.5 pound (1.1 kg) in 1 day ANS: C TKIs can cause electrolyte imbalances. This potassium level is very low, so the nurse should assess this client first. Dry, itchy, peeling skin can be a problem in clients receiving biologic response modifiers, and the nurse should assess that client next because of the potential for discomfort and infection. This calcium level is normal. TKIs can also cause weight gain, but the client with the low potassium level is more critical. 16. A nurse is assessing a female client who is taking progestins. What assessment finding requires the nurse to notify the provider immediately? a. Irregular menses b. Edema in the lower extremities c. Ongoing breast tenderness d. Red, warm, swollen calf All clients receiving progestin therapy are at risk for thromboembolism. A red, warm, swollen calf is a manifestation of deep vein thrombosis and should be reported to the provider. Irregular menses, edema in the lower extremities, and breast tenderness are common side effects of the therapy. 17. A client with a history of prostate cancer is in the clinic and reports new onset of severe low back pain. What action by the nurse is most important? a. Assess the client’s gait and balance. b. Ask the client about the ease of urine flow. c. Document the report completely. d. Inquire about the client’s job risks. ANS: A This client has manifestations of spinal cord compression, which can be seen with prostate cancer. This may affect both gait and balance and urinary function. For client safety, assessing gait and balance is the priority. Documentation should be complete. The client may or may not have occupational risks for low back pain, but with his history of prostate cancer, this should not be where the nurse starts investigating. 18. The nurse has taught a client with cancer ways to prevent infection. What statement by the client indicates that more teaching is needed? a. “I should take my temperature daily and when I don’t feel well.” b. “I will wash my toothbrush in the dishwasher once a week.” c. “I won’t let anyone share any of my personal items or dishes.” d. “It’s alright for me to keep my pets and change the litter box.” ANS: Dd. Weigh the client daily before the client eats. ANS: B Ondansetron side effects include postural hypotension, vertigo, and bradycardia, all of which increase the client’s risk for injury. The nurse should assist the client when getting out of bed. Headache and fluid retention are not side effects of this drug. 20. A nurse working with clients who experience alopecia knows that which is the best method of helping clients manage the psychosocial impact of this problem? a. Assisting the client to pre-plan for this event b. Reassuring the client that alopecia is temporary c. Teaching the client ways to protect the scalp d. Telling the client that there are worse side effects ANS: A Alopecia does not occur for all clients who have cancer, but when it does, it can be devastating. The best action by the nurse is to teach the client about the possibility and to give the client multiple choices for preparing for this event. Not all clients will have the same reaction, but some possible actions the client can take are buying a wig ahead of time, buying attractive hats and scarves, and having a hairdresser modify a wig to look like the client’s own hair. Teaching about scalp protection is important but does not address the psychosocial impact. Reassuring the client that hair loss is temporary and telling him or her that there are worse side effects are both patronizing and do not give the client tools to manage this condition. 21. A client is admitted with superior vena cava syndrome. What action by the nurse is most appropriate? a. Administer a dose of allopurinol (Aloprim). b. Assess the client’s serum potassium level. c. Gently inquire about advance directives. d. Prepare the client for emergency surgery. Superior vena cava syndrome is often a late-stage manifestation. After the client is stabilized and comfortable, the nurse should initiate a conversation about advance directives. Allopurinol is used for tumor lysis syndrome. Potassium levels are important in tumor lysis syndrome, in which cell destruction leads to large quantities of potassium being released into the bloodstream. Surgery is rarely done for superior vena cava syndrome. 22. A client is having a catheter placed in the femoral artery to deliver yttrium-90 beads into a liver tumor. What action by the nurse is most important? a. Assessing the client’s abdomen beforehand b. Ensuring that informed consent is on the chart c. Marking the client’s bilateral pedal pulses d. Reviewing client teaching done previously ANS: B This is an invasive procedure requiring informed consent. The nurse should ensure that consent is on the chart. The other actions are also appropriate but not the priority. 23. A nurse works on an oncology unit and delegates personal hygiene to an unlicensed assistive personnel (UAP). What action by the UAP requires intervention from the nurse? a. Allowing a very tired client to skip oral hygiene and sleep b. Assisting clients with washing the perianal area every 12 hours c. Helping the client use a soft-bristled toothbrush for oral care d. Reminding the client to rinse the mouth with water or saline Even though=ian community center. The nurse plans to present information specifically on which types of cancer? a. Breast and colorectal b. Skin and lymphoma c. Liver and stomach d. Uterine and ovarian ANS: A Asians have higher rates of breast, colorectal, prostate, lung, and stomach cancers than are seen in the general population. 23. In preparing a cancer risk reduction pamphlet for African-American clients, it is most important that the nurse include information on prevention and early detection for which types of cancer? a. Lung and prostate b. Bone and leukemia c. Skin and lymphoma d. Stomach and esophageal ANS: A African Americans have higher incidences of lung, prostate, breast, colorectal, and uterine cancers than are seen in the general population. 24. The nurse is seeing clients in a clinic. Which client does the nurse assess further for the development of cancer? a. Client with a cough that has lasted for 4 months b. Client whose mother died of lung cancer c. Client with a 10-pound weight gain d. Woman whose last mammogram was 3 years ago ANS: A The seven warning signs of cancer include changes in bowel/bladder habits, a sore that does not heal, unusual bleeding or discharge, thickening or a lump in the breast or elsewhere, indigestion or difficulty swallowing, obvious change in a wart/mole, and nagging cough/hoarseness. The other clients do not have warning signs of cancer. 25. It is most important that the nurse include which activity for the young adult client with Down syndrome? a. Encouraging more fruit and leafy green vegetables in the diet b. Teaching him how to perform testicular self-examination c. Assessing the skin for unusual bruises and petechiae d. Testing the client’s stool for occult blood ANS: C All screening and prevention activities are appropriate. However, people with Down syndrome have an increased lifetime risk for the development of leukemia. 26. The nurse is interested in primary prevention for cancer. Which activity does the nurse most likely participate in? a. Distributing occult fecal blood test kits to people at the shopping mall b. Arranging transportation volunteers for clients undergoing radiation therapy c. Teaching high school students the dangers of using tobacco d. Educating adolescent girls about getting an annual Papanicolaou (PAP) smear ANS: C Primary prevention focuses on activities that occur before an illness, such as education and vaccinations. Occult fecal blood testing and PAP smears are secondary prevention activities designed for screening and early diagnosis. Arranging transportation for a client who is undergoing radiation therapy is tertiary prevention. 27. The nurse assesses which client most carefully for cancer development? a. Young man receiving radiation therapy for a brain tumor b. Young adult woman who recently had postpartum hemorrhage c. Adolescent male recently diagnosed with acquired immune deficiency syndrome (AIDS) d. Older woman undergoing chemotherapy for bowel cancer ANS: D Age and immune suppression are two of the greatest risk factors for cancer development. The young man with brain cancer and the adolescent are at increased risk, but their risk is not as great as that of the older woman undergoing chemotherapy for bowel cancer. Postpartum hemorrhage is not related to cancer development. 1. A client has colorectal cancer. Which activities are especially important for the nurse to conduct for this client? (Select all that apply.) a. Monitor liver function studies. b. Maintain accurate intake and output. c. Obtain daily weight using the same scale. d. Palpate lymph nodes at each clinic visit. e. Ask the client about changes in belly size. ANS: A, D, E Common sites of metastasis for colorectal cancer include the liver, lymph nodes, and adjacent structures such as the abdominal cavity. Intake and output and daily weights would not provide data related to possible metastases. Chapter 24: Care of Patients with Cancer 1. What statement indicates that the client understands teaching about neutropenia? a. “I need to use a soft toothbrush.” b. “I have to wear a mask at all times.” c. “My grandchildren may get an infection from me.” d. “I will call my doctor if I have an increase in temperature.” ANS: D Bone marrow suppression leads to neutropenia and increases the client’s risk for infection. Decreased numbers of neutrophils and other white blood cells can minimize the clinical manifestations of infection. For this reason, the client may not develop a high temperature, even with severe infection, and any elevation of temperature should be reported immediately to the health care provider. The client does not need to wear a mask or use a soft toothbrush (although if the client has low platelets, he or she should use a soft toothbrush to avoid causing trauma). The client is not contagious. 2. A client is undergoing radiation therapy and asks the nurse about skin care for the exposed area. Which statement by the nurse is most accurate? a. “No products work well to reduce the skin reactions you get from radiation.” b. “No one product works best, so you can choose what you would like to use.” c. “The only medication that works well for skin reactions is very expensive.” d. “No good studies on skin care with radiation have been conducted to date.” ANS: B A recent placebo-controlled study showed that none of three products used to manage radiation-related skin reactions was superior to the others. Researchers concluded that clients should use products that are easy to obtain and use and are within the client’s budget. Simply stating that no one product works well does not give the client enough information to make an informed choice. Prescription medications for skin reactions can be expensive, but again this response does not help the client make a decision. 3. A client who has just had a mastectomy is crying. When the nurse asks about her crying, the client responds, “I know I shouldn’t cry because this surgery may well save my life.” What is the nurse’s best response? a. “It is all right to cry. Mourning this loss will help make you stronger.” b. “I know this is hard, but your chances of survival are better now.” c. “I can arrange for someone who had a mastectomy to come visit if you like.” d. “How have you coped with difficult situations in the past?” ANS: C Often, cancer surgery involves the loss of a body part or a decrease in function. Mourning or grieving for a body image alteration is a healthy part of adapting or adjusting to a new image. Visiting with someone who has experienced the same situation as the client is very helpful in showing the client that many aspects of life can be the same afterward. If the opportunity to arrange this type of visit is available, this would be the nurse’s best response. The other options do not provide any assistance to the client in coping with her new body image and grieving for her loss. 4. In evaluating dietary teaching for a client with chemotherapy-induced neutropenia, the nurse becomes concerned when the client makes which food choice? a. Fruit salad b. Applesauce c. Steamed broccoli d. Baked potato ANS: A The client who is neutropenic should be taught to eat a low-bacteria diet. This includes avoiding raw fruits or vegetables and undercooked meat, eggs, or fish. 5. What teaching is essential for a client who has received an injection of iodine-131? a. “Do not share a toilet with anyone else or let anyone clean your toilet.” b. “You need to save all your urine for the next week.” c. “No special precautions are needed because this type of radiation is weak.” d. “Avoid all contact with other people until the radiation device is removed.” ANS: A The radiation source is an unsealed isotope that is eliminated from the body in waste products, especially urine and feces. This material is radioactive for about 48 hours after instillation of the isotope. Having the client not share a toilet with other people or allowing anyone to clean the client’s toilet for a specific period of time ensures that the isotope has been completely eliminated, and that the client’s wastes are no longer radioactive. 6. A client has bone cancer. What intervention does the nurse implement as a priority for this client? a. Using a lift sheet when repositioning the client b. Positioning the client’s heels to keep them from touching the mattress c. Providing small, frequent meals rich in calcium and phosphorus d. Applying pressure for 5 minutes after intramuscular injections ANS: A Bone metastasis of cancer can cause such bone destruction that grasping or pulling a client can result in a pathologic fracture. Using a lift sheet spreads the client’s weight more evenly, preventing excessive force on any one body area. Preventing pressure on the heels will help prevent pressure ulcers; this is a good intervention for all clients but does not take priority over preventing fractures. Adding calcium and phosphorus to meals will not prevent fractures. Applying pressure after IM injections is not related to this client’s condition. 7. A client is undergoing radiation therapy and says, “I will be so glad when this is over and I don’t have to worry about my skin.” What response by the nurse is most appropriate? a. “Unfortunately, your skin will be permanently damaged from the radiation.” b. “You need to protect your skin from the sun for at least a year afterward.” c. “You can get a prescription for special lotions that reduce the effects of radiation.” d. “You’re having skin problems? That is unusual; let me take a look at your skin.” ANS: B Skin that has been in the path of external radiation is more susceptible to sun damage and must be protected from the sun for at least a year after completion of radiation therapy. Skin changes due to radiation are common but may not be permanent, depending on the amount of radiation absorbed. No one skin care product has been shown to significantly help radiation-related skin problems. 8. A client scheduled to undergo radiation therapy for breast cancer asks why 6 weeks of daily treatment is necessary. What is the nurse’s best response? a. “Your cancer is widespread and requires more than the usual amount of radiation treatment.” b. “Giving larger doses of radiation for a shorter period of time does not produce better effects and has worse side effects.” c. “Research has shown that more cancer cells are killed if radiation is given in smaller doses over a longer time period.” d. “It is less likely that your hair will fall out or that you will become anemic if radiation is given in this manner.” ANS: C Because of varying responses of all cancer cells within a given tumor, small doses of radiation are given on a daily basis for a set period of time. This method allows multiple opportunities to destroy cancer cells while minimizing damage to normal tissues. 9. A client’s radiation implant has become dislodged overnight, and the nurse finds it in the client’s bed. What does the nurse do first? a. Assess the client’s skin for radiation burns. b. Use tongs to put the implant into the radiation container. c. Notify the safety officer and move the client to a different room. d. Don gloves and attempt to replace the implant. ANS: B The implant does emit radiation and should be placed into the secure, lead-lined container in the client’s room. The nurse does not directly touch this implant but uses long-handled tongs for this purpose. The nurse does not need to assess the client’s skin, nor should he or she attempt to replace the source. Moving the client is not necessary, although in keeping with facility policy, the radiation safety officer may need to be notified. 10. A client is receiving a chemotherapeutic agent intravenously through a peripheral line. What is the nurse’s first action when the client reports burning at the site? a. Check for a blood return. b. Slow the rate of infusion. c. Discontinue the infusion. d. Apply a cold compress. ANS: C Both irritants and vesicants can cause tissue damage. If the nurse suspects extravasation, he or she should immediately stop the infusion. Even if the IV has a good blood return, some of the chemotherapeutic agent can still be leaking into the tissues. Slowing the rate of infusion is not sufficient to prevent further leakage and damage. Applying a cold compress may or may not be the correct action, depending on the specific agent. However, the compress would be applied only after the infusion has been discontinued. 11. A client receiving intravenous chemotherapy asks the nurse the reason for wearing a mask, gloves, and gown while administering drugs to the client. What is the nurse’s best response? a. “These coverings protect you from getting an infection from me.” b. “I am preventing the spread of infection from you to me or any other client here.” c. “The policy is for any nurse giving these drugs to wear a gown, gloves, and mask.” d. “The clothing protects me from accidentally absorbing these drugs.” ANS: D Most chemotherapy drugs are absorbed through the skin and mucous membranes. As a result, health care workers who prepare or give these drugs, especially nurses and pharmacists, are at risk for absorbing them. Even at low doses, chronic exposure to chemotherapy drugs can affect health. The Oncology Nursing Society and the Occupational Safety and Health Administration (OSHA) have specific guidelines for using caution and wearing protective clothing whenever preparing, giving, or disposing of chemotherapy drugs. 12. A client’s spouse reports that the last time the client received lorazepam (Ativan) before receiving chemotherapy, the client was extremely drowsy and didn’t remember the trip home. Which is the nurse’s best action? a. Hold the dose of lorazepam for this round of chemotherapy. b. Explain that this is a normal response to the drug. c. Perform a Mini-Mental State Examination. d. Document the response in the client’s chart. ANS: B Lorazepam, a benzodiazepine, induces sedation and amnesia, in addition to having antiemetic effects. Many clients have little if any memory about events occurring within a few hours after receiving lorazepam. This is an expected side effect and does not denote any permanent reduced cognition in the client. Both the client and the spouse should be aware of this effect so that the client is not at risk for injury. Driving, cooking, or operating mechanical equipment should not be performed until the drug’s effects have worn off. 13. A client is on chemotherapy and has a platelet count of 25,000. Which intervention is most important to teach this client? a. “Eat a low-bacteria diet.” b. “Take your temperature daily.” c. “Use a soft-bristled toothbrush.” d. “Avoid alcohol-based mouthwashes.” ANS: C This client has thrombocytopenia, which is a common side effect of chemotherapy. This increases the client’s risk for prolonged bleeding in response to even minor injury, especially from highly vascular areas such as the gums. The client should be taught to use a soft toothbrush. A low-bacteria diet and daily temperature monitoring would be used in a client who is neutropenic. Alcohol-based mouthwashes will dry mucous membranes. 14. A client with chemotherapy-induced bone marrow suppression has received filgrastim (Neupogen). Which laboratory finding indicates that this therapy is effective for the client? a. Hematocrit is 28%. b. Hematocrit is 38%. c. Segmented neutrophil count is 2500/mm3. d. Segmented neutrophil count is 3500/mm3. ANS: D Filgrastim is a single-lineage growth factor that stimulates the maturation and release of only segmented neutrophils. This drug is not given unless the neutrophil count is dangerously low. The near-normal range of neutrophils indicates effective therapy. 15. What is the priority problem for a client experiencing chemotherapy-induced anemia? a. Risk for injury related to fatigue b. Fatigue related to decreased oxygenation c. Body image problems related to skin color changes d. Inadequate nutrition related to anorexia ANS: A Safety is always a client priority. The client who is anemic will be fatigued and may need assistance with activity to prevent injury. The other problems may apply; however, they do not take priority over safety. 16. A client is hospitalized for chemotherapy. The registered nurse intervenes when observing which action by the nursing assistant? a. Allowing the client to rest instead of making him or her perform oral hygiene b. Helping the client wash the groin and axillary areas every 12 hours c. Cutting food and opening food packages when the client’s meal tray arrives d. Reminding the client to use the incentive spirometer every hour while awake ANS: A The biggest dangers to clients on chemotherapy are neutropenia and the risk of serious infection or sepsis. Most infections arise from overgrowth of the client’s own normal flora, so personal hygiene is critical. The client must perform hygiene measures on a schedule, even if he or she is very tired. Instead of allowing the client to rest, the nursing assistant should help the client perform oral hygiene and other measures. The other actions would be acceptable. 17. The student nurse overhears several staff members referring to a client who is receiving chemotherapy as having “chemo brain.” The student asks the instructor what that means. Which response by the instructor is best? a. “That is an awful thing to say and the staff should not call a client by that name.” b. “It refers to the client’s brain as being irreversibly damaged by the chemotherapy.” c. “The client has reduced cognitive function that may last for several years.” d. “The client has delirium related to the toxic effects of the chemotherapy.” ANS: C “Chemo brain” refers to the changes in concentration, memory, and learning that sometimes accompany chemotherapy. It usually is not present at 3 years after chemotherapy has been completed, so clients should be reassured that this is a temporary condition. Although the staff should be more sensitive, simply criticizing them does not help the student understand the situation. 18. A client with prostate cancer is taking estrogen daily to control tumor growth. He reports that his left calf is swollen and painful. Which is the nurse’s best action? a. Instruct the client to keep the leg elevated. b. Measure and compare calf circumferences. c. Apply ice to the calf after massaging it. d. Document this expected response. ANS: B An adverse reaction to hormonal manipulation therapy is the development of thrombus formation. The nurse should measure both calf circumferences and compare them; the side with a thromboembolism will be larger. Elevation may be helpful, but first the nurse needs to assess the situation. Massaging a calf that is swollen and painful is never correct, because this action might break a clot to form an embolus, which could then travel to the lungs. 19. A client is receiving interleukin-2 (IL-2) for cancer. Which drug is the nurse prepared to administer if needed? a. Lorazepam (Ativan) b. Meperidine (Demerol) c. Furosemide (Lasix) d. Epoetin alfa (Epogen) ANS: B Clients receiving IL-2 therapy usually experience chills, fever, and rigors during the infusion, especially the first time that they receive the drug. These reactions are a normal response to the administration of biological response modifiers such as IL-2. Clients are treated symptomatically for the discomfort. Demerol is used to treat the chills and rigor. The other medications would not treat a side effect of IL-2 therapy. 20. A nurse manager on an oncology nursing unit notes an increased incidence of infection and serious consequences for clients on the unit. Which action by the nursing manager is most beneficial in this situation? a. Review asepsis policies at a mandatory in-service for staff. b. Spot-check all staff for good handwashing practices. c. Develop standard protocols to identify and treat clients with infection. d. Institute protective precautions for all clients receiving chemotherapy. ANS: C Treatment delays have a serious negative impact on neutropenic clients with infection. Nursing units should have standardized protocols to obtain cultures and diagnostic tests, and to start antibiotics as soon as a client is suspected of having an infection. In-services and spot-checking for good handwashing practice are good ideas as part of a comprehensive infection control practice but are not as important as standard protocols that ensure rapid diagnosis and treatment. Not all clients on chemotherapy will need protective precautions. 21. A client has small cell lung cancer. Which laboratory result requires immediate intervention by the nurse? a. Serum potassium of 5.1 mEq/L b. Serum sodium of 118 mEq/L c. Hematocrit of 45% d. Blood urea nitrogen (BUN) of 10 mg/dL ANS: B In the syndrome of inappropriate antidiuretic hormone hypersecretion (SIADH), secretion of antidiuretic hormone (ADH) from the posterior pituitary gland is increased, causing the client to reabsorb water from the distal convoluted tubule and collecting duct. As a result, weight increases, and serum sodium and hematocrit levels are diluted. Blood urea nitrogen (BUN) and hematocrit are normal. Potassium is slightly high, but very low sodium places the client at risk for seizures and even death. 22. A client with advanced cancer is being treated with intravenous mithramycin (Mithracin). Which clinical manifestation indicates that the treatment is effective? a. Bowel sounds are active in all four quadrants. b. The client’s serum sodium level is 138 mEq/L. c. The pulse rate is 68 beats/min and bounding. d. Urine output has increased to 30 mL/hr. ANS: A Mithramycin is used to treat hypercalcemia, which is seen most often in oncology clients who have bone metastases. Hypercalcemia reduces excitable membrane activity, causing decreased intestinal motility. Return of intestinal motility is an indication that serum calcium levels are decreasing. Mithramycin has no direct effect on serum sodium levels or urine output. The pulse rate most likely would be rapid and irregular with hypercalcemia and would normalize as calcium levels return to normal. 23. A nurse is reviewing the white blood cell count with differential for a client receiving chemotherapy for cancer. Which finding alerts the nurse to the possibility of sepsis? a. Total white blood cell count is 9000/mm3. b. Lymphocytes outnumber basophils. c. “Bands” outnumber “segs.” d. Monocyte count is 1800/mm3. ANS: C Normally, mature segmented neutrophils (“segs”) are the major population of circulating leukocytes, constituting 55% to 70% of the total white blood cell count. Less than 3% to 5% of circulating white blood cells should be the less mature band neutrophils. A left shift occurs when the bone marrow releases more immature neutrophils than mature neutrophils. This condition indicates severe infection with possible sepsis and must be explored further. 24. A client is receiving high-dose chemotherapy for multiple myeloma. Which intervention is most important for the nurse to implement to prevent complications during chemotherapy? a. Ensure that the client’s fluid intake is 3000 to 5000 mL/day. b. Monitor telemetry every hour during therapy. c. Apply pressure to all injection sites for 5 minutes. d. Assist the client in all ambulatory activities. ANS: A This client is at high risk for tumor lysis syndrome. Tumor lysis syndrome is the precipitation of intracellular products released when tumor cells are destroyed rapidly. These products, particularly purines, can increase uric acid crystal precipitation in the kidney tubules and may cause acute tubular necrosis. In addition, serum potassium levels can become high. Maintaining adequate hydration and urine output is essential in preventing complications. 25. The nurse teaches a client with superior vena cava syndrome that improvement is characterized by which clinical manifestation? a. The client’s hands are less swollen. b. Breath sounds are clear bilaterally. c. The client’s back pain is relieved. d. Pedal edema is present. ANS: A With superior vena cava syndrome, blood flow through the vena cava is compromised as a result of tumor growth. Blood backs up into the periphery, and the client experiences upper body swelling, including the hands and feet. Compression of the superior vena cava has no effect on breath sounds. This would occur when blood is impeded from leaving the lungs, and with disorders that affect the left side of the heart. Back pain is not associated with this disorder. 26. A client has late-stage colon cancer with metastasis to the spine and bones. Which nursing intervention does the nurse add to the care plan to address a priority problem? a. Provide six small meals and snacks daily. b. Offer the client prune juice twice a day. c. Ensure that the client gets adequate rest. d. Give the client pain medications around the clock. ANS: D Although all interventions might be appropriate, a client with late-stage cancer and bone metastases is at risk for severe pain. Giving the client pain medication around the clock is the best way to manage this type of pain. 27. After receiving change-of-shift report, which client does the nurse assess first? a. Client with leukemia who needs an antiemetic before chemotherapy b. Client with breast cancer scheduled for external beam radiation c. Client with xerostomia associated with laryngeal cancer d. Client with neutropenia who has just been admitted with a possible infection ANS: D The most complex, potentially unstable client is the one with neutropenia with suspected infection. Because the onset of infection is insidious in clients with neutropenia, this client is at risk for sepsis. All other clients are stable. 28. The nurse questions which activity for the client with thrombocytopenia? a. Application of warm compresses to bruises b. Cleaning teeth with a soft-bristled brush c. Taking acetaminophen (Tylenol) for pain d. Using stool softeners daily for constipation ANS: A Ice should be applied to areas of bruising or trauma to decrease bleeding. Warm compresses would lead to vasodilation and potentially to more bleeding. It is important to implement measures to decrease the risk of bleeding. A soft-bristled toothbrush decreases trauma to gums, which could cause bleeding. Straining at the stool could increase risk for rectal bleeding, so stool softeners may be prescribed. Acetaminophen does not affect platelet function and bleeding as do aspirin products. 29. The nurse prioritizes which intervention in a client with xerostomia secondary to radiation therapy to the neck area? a. Applying lotions and oils to affected areas b. Wearing a hat to decrease heat loss c. Providing oral care after meals and at bedtime d. Monitoring vital signs every 4 hours ANS: C Head and neck radiation may damage the salivary glands, may cause dry mouth (xerostomia), and may increase the client’s lifelong risk for tooth decay. Instruct clients to avoid using lotions or ointments in these areas unless the radiologist prescribes them. Xerostomia is not associated with hair loss, which might require a hat. Monitoring vital signs is important for any client receiving radiation therapy but is not a priority for the client with xerostomia. 30. Which statement indicates that the client needs more teaching about mucositis? a. “I will rinse my mouth with water after every meal.” b. “I will use a soft-bristled toothbrush to prevent trauma.” c. “I should use an alcohol-based mouth rinse to kill bacteria.” d. “I cannot use floss because it may irritate my gums.” ANS: C Mouthwashes that contain alcohol are drying and can exacerbate mucosal irritation, leading to painful mouth sores. Rinsing the mouth with water or normal saline is indicated. Interventions aimed at decreasing risk for trauma or irritation are matters of priority because of inflammation associated with mucositis. 1. In planning a teaching session for a client undergoing photodynamic therapy for lung cancer, the nurse includes which statements? (Select all that apply.) a. “This is a palliative treatment that should decrease your pain.” b. “Avoid exposure to the sun for 1 to 3 months after the treatment.” c. “Do not eat or drink anything before your treatments.” d. “Do not remove skin markings between treatments.” e. “You need to wear sunglasses to protect your eyes after treatments.” f. “Make sure you keep your curtains closed at home afterward.” ANS: B, E, F Phototherapy causes general sensitivity to light for up to 12 weeks. During this time, the client is at high risk for light sensitivity and eye pain. After the procedure, the client is taught to decrease exposure to sunlight (to the point of being homebound). 2. The nurse is planning care for a client with hypercalcemia secondary to bone metastasis. Which interventions are included in the plan? (Select all that apply.) a. Increase oral fluids. b. Place an oral airway at the bedside. c. Monitor for Chvostek’s sign. d. Implement seizure precautions. e. Assess for hyperactive reflexes. f. Observe for muscle weakness. ANS: A, F Early manifestations of hypercalcemia include fatigue, loss of appetite, nausea, vomiting, constipation, and polyuria (increased urine output). More serious problems include severe muscle weakness, loss of deep tendon reflexes, paralytic ileus, dehydration, and electrocardiographic changes. An oral airway is not needed. Chvostek’s sign is an assessment for hypocalcemia. Seizures and hyperactive reflexes do not occur with hypercalcemia. 3. The nurse is caring for a client who has a sealed radiation implant for cervical cancer. Which activities by the nurse are appropriate? (Select all that apply.) a. Inform the supervisor of the nurse’s positive pregnancy test. b. Obtain the dosimeter badge from the nurse going off shift. c. Keep the client’s door open for frequent observation. d. Dispose of dirty linen in a red “biohazard” bag. e. Wear a lead apron while providing client care. ANS: A, E Pregnant nurses should never care for clients with sealed implants of radioactive material, so if the nurse suspects she is pregnant, she should inform her supervisor and request a different assignment. Nurses should wear lead aprons while providing care, ensuring that the apron always faces the client. Each nurse should have his or her own dosimeter film badge. The client’s door should be kept closed whenever possible and dirty linens kept in the client’s room until the radiation source is removed. Chapter 9: End-of-Life Care MULTIPLE CHOICE 1. The client tells the nurse that even though it has been 4 months since her sister’s death, she frequently finds herself crying uncontrollably. The client is afraid that she is “losing her mind.” What is the nurse’s best response? a. “Most people move on within a few months. You should see a grief counselor.” b. “Whenever you start to cry, distract yourself from thoughts of your sister.” c. “You should try not to cry. I’m sure your sister is in a better place now.” d. “Your feelings are completely normal and may continue for a long time.” ANS: D Frequent crying is not an abnormal response. The nurse should let the client know that this is normal and okay. Although the client may benefit from talking with a grief counselor, it is not unusual for her to still be grieving after a few months. The other responses are not as therapeutic because they justify or minimize the client’s response. 2. The nurse is discussing advance directives with a client. Which statement by the client indicates good understanding of the purpose of an advance directive? a. “An advance directive will keep my children from selling my home when I’m old.” b. “An advance directive will be completed as soon as I’m incapacitated and can’t think for myself.” c. “An advance directive will specify what I want done when I can no longer make decisions about health care.” d. “An advance directive will allow me to keep my money out of the reach of my family.” ANS: C An advance directive is a written document prepared by a competent individual that specifies what, if any, extraordinary actions a person would want taken when he or she can no longer make decisions about personal health care. It does not address issues such as the client’s residence in his or her own home. 3. The nurse is caring for a client who is considering being admitted to hospice. What is the nurse’s best response? a. “Hospice admission has specific criteria. You may not be a viable candidate, so we will look at alternative plans for your discharge.” b. “Hospice care focuses on a holistic approach to health care. It is designed not to hasten death, but rather to relieve symptoms.” c. “Hospice care will not help with your symptoms of depression. I will refer you to the facility’s counseling services instead.” d. “You seem to be experiencing some difficulty with this stage of the grieving process. Let’s talk about your feelings.” ANS: B As both a philosophy and a system of care, hospice care uses an interdisciplinary approach to assess and address the holistic needs of clients and families to facilitate quality of life and a peaceful death. This holistic approach neither hastens nor postpones death but provides relief of symptoms experienced by the dying client. 4. A hospitalized American Indian client is approaching death. Family members who are standing vigil in the client’s room begin to divide up his possessions among themselves as his symptoms progress. What is the nurse’s most important intervention? a. Ask the family members to step outside the room so the client cannot hear them. b. Tell the family that they are being insensitive and their behavior is inappropriate. c. Recognize that this is a culturally appropriate activity and document it in the chart. d. Report these activities to the client’s physician and the nursing supervisor. ANS: C American Indians often disperse material possessions before or after death to friends and family members. Recognizing this culturally appropriate activity would not be consistent with removing the family, stopping the activity, or reporting the client’s family’s behaviors. 5. The spouse of a dying client states that she is concerned that her husband is choking to death. What is the nurse’s best response? a. “Do not worry. The choking sound is normal during the dying process.” b. “I will administer more morphine to keep your husband comfortable.” c. “I can ask the respiratory therapist to suction secretions out through his nose.” d. “I will have another nurse assist me to turn your husband on his side.” ANS: D The choking sound or “death rattle” is common in dying clients. The nurse should acknowledge the spouse’s concerns and provide interventions that will reduce the choking sounds. Repositioning the client onto one side with a towel under the mouth to collect secretions is the best intervention. Morphine will assist with comfort but will not decrease the choking sounds. Nasal tracheal suctioning is not appropriate in a dying client. The nurse should not minimize the spouse’s concerns. 6. The terminally ill client is prescribed morphine to help cope with increasing discomfort. A family member expresses concern that the client is on “too much morphine.” What is the nurse’s best response? a. “What has the physician told you about your family member’s illness?” b. “Don’t worry about that. We’re following the physician’s plan of care.” c. “Tell me more about what you mean by too much morphine.” d. “You should talk with your physician about this when he makes rounds.” ANS: C Asking family members to explain what they mean by “too much morphine” serves to gain more information for the nurse. The other questions will not help the nurse obtain more information about the client’s care or the family’s concerns. 7. The nurse is teaching a family member about various types of complementary therapies that might be effective for relieving the dying client’s anxiety and restlessness. Which statement by the family member indicates understanding of the nurse’s teaching? a. “Maybe we should just hire a round-the-clock sitter to stay with Grandmother.” b. “I have some of her favorite hymns on a CD that I could bring for music therapy.” c. “I don’t think that she’ll need pain medication along with her herbal treatments.” d. “I will burn therapeutic incense in the room so we can stop the anxiety pills.” ANS: B Music therapy is a complementary therapy that may produce relaxation by quieting the mind and removing a client’s inner restlessness. Complementary therapies are used in conjunction with traditional therapy. The complementary therapy would not replace pain or anxiety medication but may help decrease the need for these medications. Hiring an around-the-clock sitter does not demonstrate that the client’s family understands complementary therapies. 8. A terminally ill client has just died in a hospital setting with family members at the bedside. The health care provider is also present. What should be the nurse’s priority intervention as postmortem care begins? a. Call for emergency assistance so that resuscitation procedures can begin. b. Ask the family members if they would like to spend time alone with the client. c. Ensure that a death certificate has been completed by the physician. d. Request family members to prepare the client’s body for the funeral home. ANS: B Before moving the client’s body to the funeral home, the nurse should ask family members if they would like to be alone with the client. Emergency assistance will not be necessary. Although it is important to ensure that a death certificate has been completed before the client is moved to the mortuary, the nurse first should ask family members if they would like to be alone with the client. The client’s family should not be expected to prepare the body for the funeral home. 9. The nurse is providing care for a hospice client who is in the last stages of the dying process. The client develops a pressure ulcer on her sacrum, and family members tell the nurse that they would like a specialist consulted to treat the ulcer. When the nurse discusses this with the client, the client states that the ulcer does not bother her, that it is not causing her pain, and that she’d rather not have additional caregivers at this time. What should the hospice nurse do next? a. Tell the family the wound care specialist will be consulted and treatment will begin. b. Ask the social worker and the chaplain to talk with family members about the dying process. c. Explain the client’s desires to the family, emphasizing that the client will be made as comfortable as possible. d. Ask the agency mental health nurse to speak with the client about refusing treatment. ANS: C When palliative care is provided to the dying client, symptoms will be actively treated only if they are causing the client distress. In this case, the client has stated that the pressure ulcer is not causing her distress, and she does not want further intervention. 10. The nurse is being trained in hospice care. Which intervention by the nurse is most compatible with the goals of end-of-life care for the client? a. Administer influenza and pneumococcal vaccinations. b. Prevent the client with chronic obstructive pulmonary disease from smoking. c. Perform passive range-of-motion exercises to prevent contractures. d. Permit the client with diabetes mellitus to have a serving of ice cream. ANS: D When a client is near the end of life, nursing interventions should be focused toward facilitating peaceful death by granting the client’s wishes and identifying his or her needs. Allowing a client who wishes to have something that is not permitted in the diet can be comforting if he or she has a craving or a desire for that food. There is no reason to withhold it at this time. 11. The nurse is assessing the dying client. Which manifestations of a dying client should the nurse assess to determine whether the client is near death? a. Level of consciousness b. Respiratory rate c. Bowel sounds d. Pain level on a 0 to 10 scale ANS: B All of these assessments should be performed during the dying process. As the peripheral circulation decreases, the client’s level of consciousness and bowel sounds decrease. The client is unable to provide a numeric number on a pain scale. The nurse should continue to assess respiratory rate throughout the dying process. As the rate drops significantly and breathing becomes agonal, death is near. 12. The wife is concerned because her terminally ill husband does not want to eat. What is the nurse’s best response? a. “Let him know that food is available if he wants it, but do not insist that he eat.” b. “A feeding tube can be placed in the nose to provide important nutrients.” c. “Force him to eat even if he does not feel hungry, or he will die sooner.” d. “He is getting all the nutrients he needs through his intravenous catheter.” ANS: A When family members understand that the client is not suffering from hunger and is not “starving to death,” they may allow the client to determine when, what, or if to eat. Often, as death approaches, metabolic needs decrease and clients do not feel the sensation of hunger. Forcing them to eat frustrates the client and the family. 13. The family members of a client with a terminal illness tell a nurse that the client keeps asking if she is dying. What is the nurse’s best response? a. “Whenever she asks about dying, change the subject.” b. “Tell her the truth in as gentle a way as possible.” c. “Tell her that she will get better eventually.” d. “Ask her if she is afraid to die.” ANS: B Being honest and truthful at such a time is important. It helps the client develop trust in those caring for her. Changing the subject will frustrate the client and may make her distrustful. Providing false hope is not a realistic intervention. Asking a pointed question often will not elicit the information that you want from the client. It is better to ask open-ended questions. 14. The client’s family members are concerned that the client should have a urinary catheter placed because of her decreasing urinary output. What is the hospice nurse’s best response? a. “A Foley catheter is inserted only if she is taking medications that affect output.” b. “I will insert a Foley catheter if her urinary output drops below 500 mL/day.” c. “A Foley catheter will be inserted if her bladder becomes distended.” d. “I will insert a Foley catheter if she becomes incontinent of urine.” ANS: C Insertion of an indwelling catheter is acceptable if the client is unable to void, has a distended bladder, and would be more comfortable not moving. The other statements are not appropriate uses for an indwelling catheter in a hospice setting. 15. The health care provider suggests inpatient hospice for a client. The family members are concerned that their loved one will receive only custodial care. What is the nurse’s best response? a. “The goal of palliative care is to provide the greatest degree of comfort possible and help the dying person enjoy whatever time is left.” b. “Palliative care will release you from the burden of having to care for someone in the home. It does not mean that curative treatment will stop.” c. “A palliative care facility is like a nursing home and costs less than a hospital because only pain medications are given.” d. “Your relative is unaware of her surroundings and will not notice the difference between her home and a palliative care facility.” ANS: A Palliative care provides an increased level of personal care designed to manage symptom distress. The focus is on pain control and helping the relative die with dignity. 16. A dying client’s family members are spending time with the client. What instruction is best to give to family members regarding noise in the client’s room? a. “Remember that she cannot hear you.” b. “Try to get her to talk or respond to you.” c. “Avoid making any noise when you are with her.” d. “Talk in your normal speaking voice.” ANS: D The sense of hearing may remain intact, even when it appears that the client is totally unresponsive to any sort of stimuli. The family member should speak to the client as if she were fully aware. 17. A client who is near death appears to be having difficulty breathing. What is the nurse’s highest-priority intervention? a. Teach the family how to perform nasotracheal suctioning. b. Request that the physician order morphine sulfate. c. Document the finding in the client’s chart. d. Call a respiratory therapist to intubate the client. ANS: B Morphine sulfate is the standard treatment for dyspnea near death; it relieves the psychological and physiologic distress that accompanies breathlessness. Suctioning or intubation may cause the client discomfort. Documentation is important, but it is not the priority intervention because it does nothing to relieve the client’s distress. 18. The nurse is caring for a dying client who becomes very agitated. What is the nurse’s best response? a. Use music therapy to promote relaxation. b. Increase the dose of intravenous opioids. c. Provide a second antipsychotic medication. d. Assess the client for urinary retention. ANS: D Dying clients become agitated when they are in pain or have some discomfort. Before administering medications or other therapies to decrease discomfort, the nurse should assess for potential causes of discomfort including urinary retention. 19. An experienced hospice nurse is training a new nurse in the practices of palliative care. What statement by the new nurse indicates understanding about drug therapy for end-of-life care? a. “I can administer as much pain medication as I want because the client is dying.” b. “The administration of these medications will hasten the client’s death.” c. “I can administer medication per the protocol to relieve the client’s symptoms.” d. “The purpose of palliative sedation is to relieve family members’ distress.” ANS: C Palliative care nurses follow protocols when administering medications. These protocols are standing prescriptions from the provider that identify the appropriate medication, dose, and situation for administration. The nurse cannot administer more than is prescribed. The medications are given to promote comfort and if administered per protocol will not hasten death. 20. An older client was admitted to hospice owing to impending death in approximately 6 weeks. After 2 months, the family remains at the bedside but is becoming increasingly impatient and irritable. What is the best nursing intervention? a. Ask the family to leave and not return until they are calmer. b. Sit with the family and listen to their concerns and fears. c. Tell the family members not to worry, the client will die soon. d. Consult the chaplain to come and pray with the client’s family. ANS: B Death cannot be accurately predicted. The nurse should sit with the family and listen to their concerns. The nurse should not provide false hope or reassurance. Family members should remain with the client as long as they would like. The chaplain should be consulted if the family requests. 21. An intensive care nurse is discussing withdrawal of care with a client’s family. The family expresses concerns related to discontinuation of therapy. What is the nurse’s best response? a. “I understand your concerns, but in this state, discontinuation of care is not a form of active euthanasia.” b. “You will need to talk to the provider because I am not legally allowed to participate in the withdrawal of life support.” c. “I realize this is a difficult decision. Discontinuation of therapy will allow the client to die a natural death.” d. “There is no need to worry. Most religious organizations support the client’s decision to stop medical treatment.” ANS: C The nurse should validate the family’s concerns and provide accurate information about the discontinuation of therapy. The other statements address specific issues related to the withdrawal of care but do not provide appropriate information about its purpose. If the client’s family asks for specific information about euthanasia, legal, or religious issues, the nurse should provide unbiased information about these topics. MULTIPLE RESPONSE 1. The hospice nurse is caring for a dying client and her family members. What nursing interventions are appropriate to use? (Select all that apply.) a. Teach family members about physical signs of impending death. b. Encourage the management of adverse symptoms. c. Assist family members by offering an explanation for their loss. d. Encourage reminiscence by both client and family members. e. Avoid spirituality because the client’s and the nurse’s beliefs may not be congruent. f. Do not encourage hope for the terminally ill client. ANS: A, B, D The nurse should teach family members about the physical signs of death, because family members often become upset when they see physiologic changes in their loved one. Palliative care includes management of symptoms so that the peaceful death of the client is facilitated. Reminiscence will help both the client and family members cope with the dying process. The nurse is not expected to explain why this is happening to the family’s loved one. The nurse can encourage spirituality if the client is agreeable, regardless of whether her religion is the same. 2. The nurse is providing care for a dying client. The nurse would place highest priority on treating which symptoms? (Select all that apply.) a. Anorexia b. Weight loss c. Pain d. Agitation e. Nausea f. Hair loss g. Dyspnea ANS: C, D, E, G Only symptoms that cause distress for a dying client should be treated. Such symptoms include pain, nausea and vomiting, dyspnea, and agitation. These problems interfere with the client’s comfort. Even when symptoms, such as anorexia or weight loss, disturb the family, they should be treated only if the client is distressed by their presence. The nurse should provide education to the family and the client related to normal symptoms of dying. 3. The nurse is admitting a new client to the hospital and needs to determine the plan of care. What criterion is required for the client to make his own medical decisions? (Select all that apply.) a. Can communicate his treatment preferences b. Is able to read and write at an 8th grade level c. Is oriented enough to received information d. Can evaluate and deliberate information e. Has completed an advance directive ANS: A, C, D To have decision-making ability, a person must be able to perform three tasks: receive information (but not necessarily oriented 4); evaluate, deliberate, and mentally manipulate information; and communicate a treatment preference. The client does not have to read or write at a specific level. Education can be provided at the client’s level, so that he can make the necessary decisions. The client does not need to complete an advance directive to make his own medical decisions. An advance directive will be necessary if he wants to designate someone to make medical decisions when he is unable to. Black & Hawks: Medical-Surgical Nursing, 8th Edition Chapter 16: Perspectives in Oncology MULTIPLE CHOICE 1. In planning programs for cancer prevention, the nurse should provide information about cancer as the _____ leading cause of death a. major b. second c. third d. fourth ANS: B Each year, approximately 564,000 Americans die of cancer. Cancer remains the second leading cause of death in the United States. 2. After discussing the difference between benign and malignant tumors with a client, the nurse would know that the client understood the discussion when the client says a. “A benign tumor does not invade other tissue.” b. “Malignant tissue is not found far from the original site of the tumor.” c. “Malignant tumors do not respond well to chemotherapy.” d. “The control of growth is impaired only in malignant tissue.” ANS: A A benign neoplasm is a usually harmless growth that does not spread or invade other tissue. A malignant neoplasm is a harmful mass capable of invasion of other tissues and metastasis to distant organs. 3. The number of new cancer cases diagnosed has increased steadily since 1900. The nurse explains to a client that one of the reasons for this increase is that a. cancer is related to most birth defects. b. many false-positive cancer results are reported. c. people who live longer are less prone to cancer. d. statistical analysis and reporting are more accurate. ANS: D The apparent increase in the incidence of cancer may be somewhat misleading. It may simply reflect more precise diagnostic and statistical methods combined with the trend toward a longer life span. 4. A nurse is conducting a smoking cessation clinic. What information about smoking does the nurse include in the teaching component of the program? a. A pack-year history is the length of time, in years, a person has smoked. b. Smokeless tobacco is harmless because the carcinogens have been removed. c. Smoking causes more cancer in the United States than do all other causes combined. d. The risk of cancer for someone who stops smoking does not improve. ANS: C There is a direct linear relationship between the amount and number of years a person has smoked and cancer risk. Tobacco is the most important known cause of cancer in the United States. A pack-year history is the number of cartons smoked a day multiplied by the number of years a person has smoked. While some carcinogens have been removed from smokeless tobacco, “chew” remains a leading cause of oral cancer. After a person quits smoking, the chances of getting lung cancer actually diminish. 5. A client is considering having genetic testing for cancer that “runs in the family.” Vital information for the nurse to include in the teaching plan before the client has the testing includes telling the client that a. Genetic testing is simple and inexpensive and the client does not need to seek out a specialist to interpret the results. b. If a genetic test comes back positive for a gene related to cancer, the client will develop the cancer. c. There are so many genetically-based cancers that even genetic testing cannot possibly cover them all. d. There are specific state and federal laws to protect people who undergo genetic testing from insurance and job discrimination. ANS: D Only about 5-10% of cancers are hereditary, but many more seem to be “familial.” Inherited cancers arise from a single gene mutation. This is a specialized area of oncology and the testing is quite expensive. There are specific, but limited, laws protecting those who undergo genetic testing against job and insurance discrimination and clients should understand these laws before having genetic testing done. 6. The nurse reviewing a research report recognizes that a discussion of oncogenes will address a. a chemotherapeutic agent that eradicates viruses that cause cancer. b. factors in the immune system protecting the client from malignant growths. c. risk factors in cancer development. d. segments of DNA that transform normal cells into malignant cells. ANS: D Oncogenes are small segments of cellular deoxyribonucleic acid (DNA) that can transform normal cells into malignant cells when appropriately activated. 7. A nurse is conducting a wellness seminar in which the cancer-fighting actions of diet and physical activity are presented. A woman in the audience says, “I thought diet and exercise were related to heart disease.” The best response by the nurse is a. “In people who don’t smoke, diet and activity are the most important risk factors.” b. “They are important for both, but the diet to prevent cancer is totally different.” c. “They are important for heart disease too, but cancer is a bigger killer.” d. “You’re right; diet and activity are more important to prevent heart disease.” ANS: A For people who do not smoke, diet and exercise are the two most important modifiable cancer risks. The diets for both cancer and heart disease prevention are similar: low fat and high fiber. Heart disease is the number one killer in this country. 8. A client has worked for 2 years installing insulation containing asbestos. The nurse will determine further assessment questions based on the understanding that occupational exposure to carcinogens represents _____% of all human cancers. a. <2 b. 2-8 c. 10-12 d. >12 ANS: B Occupational exposure to carcinogens causes about 2-8% of all known human cancers. 9. A nurse is administering IV chemotherapy. What personal protective equipment (PPE) should the nurse use when doing this task? a. A gown and gloves b. Gloves and a mask c. No special PPE is needed d. Only gloves ANS: A Because chemotherapy presents a hazard to health care staff, the nurse should wear a gown and gloves when administering it. 10. After explaining how malignant cells differ from normal cells to a client with breast cancer, the nurse knows the client understands the characteristics of malignant cells when the client says “Malignant cells a. are larger than normal cells and have designated purposes.” b. cannot grow if inflammation is present.” c. develop chromosomal abnormalities as they mature.” d. develop the same antigens as normal cells do.” ANS: C Malignant cells may have an abnormal number of chromosomes or an abnormal arrangement. They also develop antigens that are completely different from those associated with normal cells. Malignant cells serve no useful purpose. 11. A client angrily tells the nurse that he cannot understand why he has liver cancer when he started out with bladder cancer. The nurse would recognize that the client misunderstands how a malignant tumor metastasizes when he states that cancer can spread by a. attaching to white blood cells. b. direct extension into the lymphatic system. c. invasion into the blood vessels. d. new growths into internal body cavities. ANS: A For the purposes of study, the metastatic cascade may be divided into three stages. Stage 1 involves invasion of neoplastic cells from the primary tumor into surrounding tissue and penetration of blood and lymph vessels. Metastatic spread to distant organs and tissues is almost always the result of cells moving through the bloodstream. Direct expansion of tumors in body cavities occurs as cells travel throughout the cavity to develop new growth on other serosal surfaces. 12. The nurse assessing a client’s risk of cancer from cigarette smoking notes that the client has smoked one-half pack per day for 10 years. The nurse calculates that this client has a history of a. 2 pack-years. b. 5 pack-years. c. 10 pack-years. d. 20 pack-years. ANS: B A “pack-year” refers to the number of packs of cigarettes smoked per day times the number of years the client has smoked . 13. A nurse preparing a teaching plan for a client recently diagnosed with cancer will include the fact about growth patterns of cancer that cancer cells a. exhibit contact inhibition. b. grow in adverse conditions, such as lack of nutrients. c. have a growth rate equal to or less than cell death rate. d. proliferate in response to specific stimuli. ANS: B Cancer cells grow in adverse conditions that contribute to a weakened immune system (e.g., lack of nutrients). The cells also proliferate in response to abnormal stimuli and do not exhibit contact inhibition, and the rate of cell formation exceeds that of cell death. 14. A client has a benign tumor that has originated in adipose tissue. The nurse explains that this type of tumor is classified as a a. fibroma. b. lipoma. c. leiomyoma. d. carcinoma. ANS: B A lipoma arises in adipose tissue. A fibroma can arise anywhere but is usually found in the uterus. A leiomyoma arises from smooth muscle. A carcinoma is a cancer of epithelial cell origin. Chapter 17: Clients with Cancer MULTIPLE CHOICE 1. The nurse is reviewing the American Cancer Society (ACS) recommendations for breast cancer screening with a 50-year-old female client. The nurse should emphasize the recommendation for a. breast examination by a health care professional semi-annually. b. breast self-examination (BSE) monthly. c. chest x-ray study yearly when the client is over age 40. d. mammography when a lump is detected. ANS: A ACS recommends annual mammography for women 40 years of age and older. ACS also recommends monthly BSE beginning at age 20. Chest x-ray has no value in screening women for breast cancer. 2. The recommendation the nurse should share with a 22-year-old sexually active client who is seeking information on the prevention of cervical cancer is that a Pap smear a. is needed annually by all women over age 18. b. should be done annually until two tests are negative, then once every 2-3 years, in women over 30. c. should be done biannually for clients who have been sexually active for 3 years but not later than age 21. d. should be performed twice a year for all sexually active women over age 18. ANS: B Sexually active women, regardless of age, and those 18 or older should have an annual Pap smear. Women over age 30 can be screened every 2 to 3 years after they have had 2 normal tests in a row. 3. After a client has a series of diagnostic tests, the studies confirm the presence of rectal cancer. The nurse’s primary intervention should be to a. assess the meaning and effect of cancer as perceived by the client. b. determine if the client is emotionally ready to deal with the diagnosis of cancer. c. reassure the client that many treatment modalities are available. d. support the physician when the client is informed of the diagnosis. ANS: A Client reactions to cancer vary greatly. The nurse should actively listen for remarks that describe the meaning and effect of cancer as experienced by the client. 4. The nurse caring for a client with cancer of the thyroid gland has a tumor classified as T2, N1, M0. The nurse explains that the “T” in this classification schema represents a. number of years the tumor has been present. b. site of the tumor. c. size of the tumor. d. virulence of malignancy. ANS: C The TMN system is the accepted system for cancer staging today; T refers to tumor, N to the regional lymph nodes, and M to metastasis. T1-T4 defines the increasing tumor size and involvement. 5. A 32-year-old client who has a history of familial polyposis but no manifestations still wants to explore the possibility of preventive surgery. The most appropriate response the nurse can make is a. “Cancer is not always hereditary, and you should change risk factors in your life.” b. “It is an overreaction to seek radical treatment before you develop symptoms.” c. “Monthly rectal smears may allay your anxiety without surgery.” d. “Subtotal colectomy is a procedure you might seek further information about.” ANS: D Clients with familial polyposis have a 50% risk of developing colon cancer by age 40. By age 70, all clients with this inherited trait have developed colon cancer. Clients with ulcerative colitis also have an increased risk for colon cancer. Prophylactic subtotal colectomies may be indicated for this group of clients. 6. Yesterday a 28-year-old client was diagnosed with rectal cancer. The nurse has made the nursing diagnosis of Anxiety Related to Fear of the Unknown, as manifested by anger. The best approach for the nurse to take in relation to the client’s need for information is to a. offer suggestions to modify the client’s expressions of anger. b. provide the client with a detailed plan for future interventions. c. provide the client with simple explanations of proposed treatments. d. specifically discuss the scientific facts related to rectal cancer. ANS: C Informational needs are very high during the diagnostic and treatment periods. Tests, procedures, and treatment, which are often very technical and complicated, need to be explained. During this time of anxiety and stress, the simplest explanation is usually the most appropriate and is all that the client can assimilate. But be sure to incorporate all the details the client and family wants. 7. The nurse is administering medication in phase III trials to a client with lung cancer. Assessments made in this phase of the drug investigation involve a. determination of the maximum tolerated dose. b. evaluation of the drug’s general effectiveness. c. explanation of how the drug compares with standard treatments. d. description of the type and severity of side effects. ANS: C 8. The client is receiving a drug in a phase I clinical trial. Regarding the type of malignancy for which the client is being treated, the nurse makes the assumption that the cancer a. and its treatment are not covered by the client’s insurance. b. is limited in size and virulence. c. is not following the expected disease course. d. will not respond to other known treatments for cancer. ANS: D Phase I trials may involve significant risks for the subject and only minimal, if any, benefit; they are offered only to those with advanced disease and for whom there are no other known treatment options. 9. The nurse caring for a client who has an implanted radiation source should reduce self-exposure by incorporating the strategy of a. limiting the time spent close to the client to 30 minutes per 8-hour shift. b. remaining 6 feet away from the client except for essential care. c. wearing a lead-shielded apron whenever entering the client’s room. d. wearing a radiation meter or film badge to measure exposure. ANS: A Three key principles for working with radiation are distance, time, and shielding. Nurses should strive to minimize the amount of time they are exposed to a radiation source, although they must still meet the client’s care and needs. Exposure time generally should be limited to 30 minutes of direct care per 8-hour shift. Remaining 6 feet away from the client would reduce exposure as compared to standing 3 feet away, but is not the recommended course of action. A lead apron would also reduce exposure, but nurses have found them too cumbersome to use and they are not routinely worn. The radiation meter or film badge does nothing to reduce exposure, but does measure it. 10. The nursing action that has the highest priority for a 32-year-old client with an implanted radiation source should focus on a. assessing the client’s reaction to the diagnosis and treatment. b. preventing skin problems related to radiation. c. promoting regular activity while confined to the room. d. safeguarding the client and others from unnecessary radiation exposure. ANS: D Sealed-source radioactive implants require a private room and bath because of the risk of implant dislodgment and subsequent exposure of other people to the radiation. Rooms at the ends of halls or stairwells may be designated for use by such clients because their location provides a decreased chance of exposure to others. 11. A client is receiving interleukin-2 (IL-2) as part of the therapeutic plan to manage malignant melanoma. The nurse should emphasize the ability of this agent to a. increase oxygenation to cells that are not malignant. b. physically dissolve the tumor mass. c. replace damaged and diseased cells from bone marrow. d. strengthen the client’s immune response. ANS: D Interleukins are proteins that serve as regulators of the immune system. IL-2 is derived from T cells, augments various other T-cell activities, and enhances the function of natural killer cells. Interleukins have none of the other effects. 12. The nurse administering granulocyte colony-stimulating factor (G-CSF; Neupogen) to a client who is also receiving chemotherapy should assess the client for a. a rash. b. bone pain. c. fatigue. d. muscle aches. ANS: B Bone pain is the most commonly reported side effect of G-CSF, although the other options can also occur. 13. When there is extravasation of vincristine (Oncovin), the nurse should initially a. apply cold compresses to the site. b. apply manual pressure to delay further circulation. c. call the physician immediately. d. leave the cannula in place and aspirate. ANS: D In the case of an extravasation, the cannula should be left in place and an attempt made to aspirate the drug from the cannula and site. The nurse should then remove the needle and apply warm compresses. Direct pressure should not be applied to the site. The site is observed for enduration, erythema, necrosis, and pain. The physician should be notified after the nurse has treated the client. 14. When the client questions why the chemotherapeutic drug is being administered by intracavitary instillation, the nurse could best answer by explaining that this approach is a a. cost-effective and more rapidly-acting method of treatment. b. diffuse method of systemic administration that avoids side effects. c. means to allow high concentrations of drugs to be directed at the tumor. d. non-invasive method of administration. ANS: C With the intracavitary method, a high concentration of a chemotherapeutic agent is delivered to the local tumor site. 15. When a client undergoing systemic chemotherapy reaches the nadir of treatment, priority care by the nurse should be directed toward a. assisting the client to eat an adequate amount of food to maintain nutrition. b. enhancing the effects of chemotherapy by encouraging mild activity. c. improving the mental state of the client by using mental imagery. d. protecting the client from infection and bleeding. ANS: B The time after chemotherapy administration when the white blood cell or platelet count is at the lowest point is referred to as the nadir. For most myelosuppressive agents, the nadir occurs within 7 days after drug administration. Knowledge of blood count nadirs helps to predict when the client is at greatest risk for infection and bleeding. 16. Before the specially trained nurse gives the prescribed dose of a chemotherapeutic agent, the nurse should a. collect an extra syringe and needle in case of contamination. b. cover the client with a water-resistant shield. c. explain the expected side effects of the drug to the client. d. verify dose, drug, and schedule with another nurse. ANS: D As a precaution against medication error, the chemotherapeutic drug should be verified by another licensed professional. Chemotherapy should be administered only by adequately prepared registered professional nurses who have taken special courses in administering chemotherapy and who are highly skilled. 17. The nurse can best avoid catheter occlusion in a client with a recently inserted venous access device (VAD) by a. administering medications in small volumes. b. flushing the catheter per agency protocol. c. instructing the client to keep the arm extended during administration. d. using the catheter only for vesicant drugs. ANS: B Intraluminal occlusion may occur secondary to a blood clot or precipitate. Prevention strategies include proper flushing, vigilance for drug incompatibilities, and adherence to proper drug dilutions. Procedures for the care and maintenance of VADs vary with each clinical setting and type of device. 18. The specially prepared nurse administering chemotherapeutic drugs should a. administer intravenous medications only through VADs. b. apply ice to the area after an intramuscular injection of chemotherapy. c. wear a mask during administration of the agent. d. wear gloves and a gown during preparation and administration of the drugs. ANS: D Several organizations, including the Occupational Safety and Health Administration, National Study Commission on Cytotoxic Exposure, and Oncology Nursing Society, have prepared guidelines for the safe preparation, handling, and disposal of antineoplastics. These guidelines call for the use of gloves and gowns during preparation and administration and the use of a biologic safety cabinet for drug preparation. VADs are not required for chemotherapy, although they are in widespread use. Chemotherapy is not given via the IM route. A mask is not required for administration of chemotherapy. 19. The nurse should closely assess a client undergoing chemotherapy for a tumor that is responding to the therapy for any indication of tumor lysis syndrome, which is marked by a. hypercalcemia. b. hyperkalemia. c. increase in antidiuretic hormone (ADH). d. platelet count below 20,000/mm3. ANS: B Cellular death of the tumor caused by the chemotherapy releases potassium, causing hyperkalemia.Cellular death of the tumor caused by the chemotherapy releases potassium, causing hyperkalemia. 20. The nurse has assigned the nursing diagnosis Imbalanced Nutrition: Less than Body Requirements, Related to Anorexia for a client with colon cancer. Nursing goals include the maintenance of present body weight. To achieve this goal, the nurse should suggest a diet that is high in a. calories and low in cholesterol. b. fat and calories. c. fat and low in bulk. d. protein and calories. ANS: D Adequate hydration and a high-protein, high-calorie diet are vital to the recovery of normal cells from the adverse effects of chemotherapy. 21. The nurse caring for a neutropenic, 75-year-old man undergoing treatment for prostate cancer assesses an oral temperature of 100.4° F. The most appropriate interpretation of this finding is that the client a. is experiencing an expected, systemic chemotherapeutic effect. b. is experiencing the expected increase in metabolism that accompanies malignancy. c. may have a medical emergency and needs prompt further assessment. d. may have a urinary tract infection causing a low-grade fever. ANS: C Fever is the cardinal, and often the only, manifestation of infection in the neutropenic client. The development of fever in a neutropenic client should be treated as a medical emergency and mandates prompt assessment, diagnosis, and intervention. The source could be a urinary tract infection, but the client needs a work-up to determine the source of any infection (e.g., blood cultures, a chest x-ray, and a urinalysis). 22. The nurse caring for a client receiving chemotherapy assesses for indication of thrombocytopenia. Based on laboratory values, the client becomes at high risk for hemorrhage at the point when the platelet count is less than a. 60,000/mm3. b Teaching about the risks associated with cigarette smoking is recommended at every patient encounter because cigarette smoking is associated with multiple health problems. A tumor must be at least 0.5 cm large before it is detectable by current screening methods and may already have metastasized by that time. Oncofetal antigens such as CEA may be used to monitor therapy or detect tumor reoccurrence, but are not helpful in screening for cancer. The seven warning signs of cancer are actually associated with fairly advanced disease. 4. The nurse should include which food choice when providing dietary teaching for a patient scheduled to receive external beam radiation for abdominal cancer? a. Fresh fruit salad b. Roasted chicken c. Whole wheat toast d. Cream of potato soup ANS: B To minimize the diarrhea that is commonly associated with bowel radiation, the patient should avoid foods high in roughage, such as fruits and whole grains. Lactose intolerance may develop secondary to radiation, so dairy products should also be avoided. 5. During a routine health examination, a 40-year-old patient tells the nurse about a family history of colon cancer. Which action should the nurse take next? a. Teach the patient about the need for a colonoscopy at age 50. b. Teach the patient how to do home testing for fecal occult blood. c. Obtain more information from the patient about the family history. d. Schedule a sigmoidoscopy to provide baseline data about the patient. ANS: C The patient may be at increased risk for colon cancer, but the nurse’s first action should be further assessment. The other actions may be appropriate, depending on the information that is obtained from the patient with further questioning. 6. A patient who is diagnosed with cervical cancer that is classified as Tis, N0, M0 asks the nurse what the letters and numbers mean. Which response by the nurse is most appropriate? a. “The cancer involves only the cervix.” b. “The cancer cells look almost like normal cells.” c. “Further testing is needed to determine the spread of the cancer.” d. “It is difficult to determine the original site of the cervical cancer.” ANS: A Cancer in situ indicates that the cancer is localized to the cervix and is not invasive at this time. Cell differentiation is not indicated by clinical staging. Because the cancer is in situ, the origin is the cervix. Further testing is not indicated given that the cancer has not spread. 7. The nurse teaches a patient who is scheduled for a prostate needle biopsy about the procedure. Which statement, if made by the patient, indicates that teaching was effective? a. “The biopsy will remove the cancer in my prostate gland.” b. “The biopsy will determine how much longer I have to live.” c. “The biopsy will help decide the treatment for my enlarged prostate.” d. “The biopsy will indicate whether the cancer has spread to other organs.” ANS: C A biopsy is used to determine whether the prostate enlargement is benign or malignant, and determines the type of treatment that will be needed. A biopsy does not give information about metastasis, life expectancy, or the impact of cancer on the patient’s life. 8. The nurse teaches a postmenopausal patient with stage III breast cancer about the expected outcomes of cancer treatment. Which patient statement indicates that the teaching has been effective? a. “After cancer has not recurred for 5 years, it is considered cured.” b. “The cancer will be cured if the entire tumor is surgically removed.” c. “Cancer is never considered cured, but the tumor can be controlled with surgery, chemotherapy, and radiation.” d. “I will need to have follow-up examinations for many years after I have treatment before I can be considered cured.” ANS: D The risk of recurrence varies by the type of cancer. Some cancers are considered cured after a shorter time span or after surgery, but stage III breast cancer will require additional therapies and ongoing follow-up. 9. A patient with a large stomach tumor that is attached to the liver is scheduled to have a debulking procedure. Which information should the nurse teach the patient about the outcome of this procedure? a. Pain will be relieved by cutting sensory nerves in the stomach. b. Relief of pressure in the stomach will promote better nutrition. c. Tumor growth will be controlled by the removal of malignant tissue. d. Tumor size will decrease and this will improve the effects of other therapy. ANS: D A debulking surgery reduces the size of the tumor and makes radiation and chemotherapy more effective. Debulking surgeries do not control tumor growth. The tumor is debulked because it is attached to the liver, a vital organ (not to relieve pressure on the stomach). Debulking does not sever the sensory nerves, although pain may be lessened by the reduction in pressure on the abdominal organs. 10. External-beam radiation is planned for a patient with cervical cancer. What instructions should the nurse give to the patient to prevent complications from the effects of the radiation? a. Test all stools for the presence of blood. b. Maintain a high-residue, high-fiber diet. c. Clean the perianal area carefully after every bowel movement. d. Inspect the mouth and throat daily for the appearance of thrush. ANS: C Radiation to the abdomen will affect organs in the radiation path, such as the bowel, and cause frequent diarrhea. Careful cleaning of this area will help decrease the risk for skin breakdown and infection. Stools are likely to have occult blood from the inflammation associated with radiation, so routine testing of stools for blood is not indicated. Radiation to the abdomen will not cause stomatitis. A low-residue diet is recommended to avoid irritation of the bowel when patients receive abdominal radiation. 11. A patient with Hodgkin’s lymphoma who is undergoing external radiation therapy tells the nurse, “I am so tired I can hardly get out of bed in the morning.” Which intervention should the nurse add to the plan of care? a. Minimize activity until the treatment is completed. b. Establish time to take a short walk almost every day. c. Consult with a psychiatrist for treatment of depression. d. Arrange for delivery of a hospital bed to the patient’s home. ANS: B Walking programs are used to keep the patient active without excessive fatigue. Having a hospital bed does not necessarily address the fatigue. The better option is to stay as active as possible while combating fatigue. Fatigue is expected during treatment and is not an indication of depression. Minimizing activity may lead to weakness and other complications of immobility. 12. The nurse is caring for a patient with colon cancer who is scheduled for external radiation therapy to the abdomen. Which information obtained by the nurse would indicate a need for patient teaching? a. The patient swims a mile 3 days a week. b. The patient snacks frequently during the day. c. The patient showers everyday with a mild soap. d. The patient has a history of dental caries with amalgam fillings. ANS: A The patient is instructed to avoid swimming in salt water or chlorinated pools during the treatment period. The patient does not need to change habits of eating frequently or showering with a mild soap. A history of dental caries will not impact the patient who is scheduled for abdominal radiation. 13. A patient undergoing external radiation has developed a dry desquamation of the skin in the treatment area. The nurse teaches the patient about management of the skin reaction. Which statement, if made by the patient, indicates the teaching was effective? a. “I can buy some aloe vera gel to use on the area.” b. “I will expose the treatment area to a sun lamp daily.” c. “I can use ice packs to relieve itching in the treatment area.” d. “I will scrub the area with warm water to remove the scales.” ANS: A Aloe vera gel and cream may be used on the radiated skin area. Ice and sunlamps may injure the skin. Treatment areas should be cleaned gently to avoid further injury. 14. A patient with metastatic cancer of the colon experiences severe vomiting following each administration of chemotherapy. Which action, if taken by the nurse, is most appropriate? a. Have the patient eat large meals when nausea is not present. b. Offer dry crackers and carbonated fluids during chemotherapy. c. Administer prescribed antiemetics 1 hour before the treatments. d. Give the patient two ounces of a citrus fruit beverage during treatments. ANS: C Treatment with antiemetics before chemotherapy may help prevent nausea. The patient should eat small, frequent meals. Offering food and beverages during chemotherapy is likely to cause nausea. The acidity of citrus fruits may be further irritating to the stomach. 15. The nurse administers an IV vesicant chemotherapeutic agent to a patient. Which action is most important for the nurse to take? a. Infuse the medication over a short period of time. b. Stop the infusion if swelling is observed at the site. c. Administer the chemotherapy through a small-bore catheter. d. Hold the medication unless a central venous line is available. ANS: B Swelling at the site may indicate extravasation, and the IV should be stopped immediately. The medication generally should be given slowly to avoid irritation of the vein. The size of the catheter is not as important as administration of vesicants into a running IV line to allow dilution of the chemotherapeutic drug. These medications can be given through peripheral lines, although central vascular access devices (CVADs) are preferred. 16. A chemotherapy drug that causes alopecia is prescribed for a patient. Which action should the nurse take to maintain the patient’s self-esteem? a. Tell the patient to limit social contacts until regrowth of the hair occurs. b. Encourage the patient to purchase a wig or hat and wear it once hair loss begins. c. Teach the patient to gently wash hair with a mild shampoo to minimize hair loss. d. Inform the patient that hair usually grows back once the chemotherapy is complete. ANS: B The patient is taught to anticipate hair loss and to be prepared with wigs, scarves, or hats. Limiting social contacts is not appropriate at a time when the patient is likely to need a good social support system. The damage occurs at the hair follicle and will occur regardless of gentle washing or use of a mild shampoo. The information that the hair will grow back is not immediately helpful in maintaining the patient’s self-esteem. 17. A patient who has ovarian cancer is crying and tells the nurse, “My husband rarely visits. He just doesn’t care.” The husband indicates to the nurse that he never knows what to say to help his wife. Which nursing diagnosis is most appropriate for the nurse to add to the plan of care? a. Compromised family coping related to disruption in lifestyle b. Impaired home maintenance related to perceived role changes c. Risk for caregiver role strain related to burdens of caregiving responsibilities d. Dysfunctional family processes related to effect of illness on family members ANS: D The data indicate that this diagnosis is most appropriate because poor communication among the family members is affecting family processes. No data suggest a change in lifestyle or its role as an etiology. The data do not support impairment in home maintenance or a burden caused by caregiving responsibilities. 18. A patient receiving head and neck radiation for larynx cancer has ulcerations over the oral mucosa and tongue and thick, ropey saliva. Which instructions should the nurse give to this patient? a. Remove food debris from the teeth and oral mucosa with a stiff toothbrush. b. Use cotton-tipped applicators dipped in hydrogen peroxide to clean the teeth. c. Gargle and rinse the mouth several times a day with an antiseptic mouthwash. d. Rinse the mouth before and after each meal and at bedtime with a saline solution. ANS: D The patient should rinse the mouth with a saline solution frequently. A soft toothbrush is used for oral care. Hydrogen peroxide may damage tissues. Antiseptic mouthwashes may irritate the oral mucosa and are not recommended. 19. A patient has been assigned the nursing diagnosis of imbalanced nutrition: less than body requirements related to painful oral ulcers. Which nursing action will be most effective in improving oral intake? a. Offer the patient frequent small snacks between meals. b. Assist the patient to choose favorite foods from the menu. c. Provide teaching about the importance of nutritional intake. d. Apply the ordered anesthetic gel to oral lesions before meals. ANS: D Because the etiology of the patient’s poor nutrition is the painful oral ulcers, the best intervention is to apply anesthetic gel to the lesions before the patient eats. The other actions might be helpful for other patients with impaired nutrition, but would not be as helpful for this patient. 20. A widowed mother of four school-age children is hospitalized with metastatic ovarian cancer. The patient is crying and tells the nurse that she does not know what will happen to her children when she dies. Which response by the nurse is most appropriate? a. “Why don’t we talk about the options you have for the care of your children?” b. “I’m sure you have friends that will take the children when you can’t care for them.” c. “For now you need to concentrate on getting well and not worrying about your children.” d. “Many patients with cancer live for a long time, so there is still time to plan for your children.” ANS: A This response expresses the nurse’s willingness to listen and recognizes the patient’s concern. The responses beginning “Many patients with cancer live for a long time” and “For now you need to concentrate on getting well” close off discussion of the topic and indicate that the nurse is uncomfortable with the topic. In addition, the patient with metastatic ovarian cancer may not have a long time to plan. Although it is possible that the patient’s friends will take the children, more assessment information is needed before making plans. 21. A patient who has severe pain associated with terminal pancreatic cancer is being cared for at home by family members. Which finding by the nurse indicates that teaching regarding pain management has been effective? a. The patient uses the ordered opioid pain medication whenever the pain is greater than 5 (0 to 10 scale). b. The patient agrees to take the medications by the IV route in order to improve analgesic effectiveness. c. The patient takes opioids around the clock on a regular schedule and uses additional doses when breakthrough pain occurs. d. The patient states that nonopioid analgesics may be used when the maximal dose of the opioid is reached without adequate pain relief. ANS: C For chronic cancer pain, analgesics should be taken on a scheduled basis, with additional doses as needed for breakthrough pain. Taking the medications only when pain reaches a certain level does not provide effective pain control. Although nonopioid analgesics also may be used, there is no maximum dose of opioid. Opioids are given until pain control is achieved. The IV route is not more effective than the oral route, and usually the oral route is preferred. 22. Interleukin-2 (IL-2) is used as adjuvant therapy for a patient with metastatic renal cell carcinoma. Which information should the nurse include when explaining the purpose of this therapy to the patient? a. IL-2 enhances the immunologic response to tumor cells. b. IL-2 stimulates malignant cells in the resting phase to enter mitosis. c. IL-2 prevents the bone marrow depression caused by chemotherapy. d. IL-2 protects normal cells from the harmful effects of chemotherapy. ANS: A IL-2 enhances the ability of the patient’s own immune response to suppress tumor cells. IL-2 does not protect normal cells from damage caused by chemotherapy, stimulate malignant cells to enter mitosis, or prevent bone marrow depression. 23. The home health nurse cares for a patient who has been receiving interferon therapy for treatment of cancer. Which statement by the patient indicates a need for further assessment? a. “I have frequent muscle aches and pains.” b. “I rarely have the energy to get out of bed.” c. “I experience chills after I inject the interferon.” d. “I take acetaminophen (Tylenol) every 4 hours.” ANS: B Fatigue can be a dose-limiting toxicity for use of biologic therapies. Flulike symptoms, such as muscle aches and chills, are common side effects with interferon use. Patients are advised to use acetaminophen every 4 hours. 24. A patient with leukemia is considering whether to have hematopoietic stem cell transplantation (HSCT). The nurse will include which information in the patient’s teaching plan? a. Transplant of the donated cells is painful because of the nerves in the tissue lining the bone. b. Donor bone marrow cells are transplanted through an incision into the sternum or hip bone. c. The transplant procedure takes place in a sterile operating room to minimize the risk for infection. d. Hospitalization will be required for several weeks after the stem cell transplant procedure is performed. ANS: D The patient requires strict protective isolation to prevent infection for 2 to 4 weeks after HSCT while waiting for the transplanted marrow to start producing cells. The transplanted cells are infused through an IV line, so the transplant is not painful, nor is an operating room or incision required. 25. The nurse teaches a patient with cancer of the liver about high-protein, high-calorie diet choices. Which snack choice by the patient indicates that the teaching has been effective? a. Lime sherbet b. Blueberry yogurt c. Cream cheese bagel d. Fresh strawberries and bananas ANS: B Yogurt has high biologic value because of the protein and fat content. Fruit salad does not have high amounts of protein or fat. Lime sherbet is lower in fat and protein than yogurt. Cream cheese is low in protein. 26. A patient with cancer has a nursing diagnosis of imbalanced nutrition: less than body requirements related to altered taste sensation. Which nursing action is most appropriate? a. Add strained baby meats to foods such as casseroles. b. Teach the patient about foods that are high in nutrition. c. Avoid giving the patient foods that are strongly disliked. d. Add extra spice to enhance the flavor of foods that are served. ANS: C The patient will eat more if disliked foods are avoided and foods that the patient likes are included instead. Additional spice is not usually an effective way to enhance taste. Adding baby meats to foods will increase calorie and protein levels, but does not address the issue of taste. The patient’s poor intake is not caused by a lack of information about nutrition. 27. During the teaching session for a patient who has a new diagnosis of acute leukemia the patient is restless and is looking away, never making eye contact. After teaching about the complications associated with chemotherapy, the patient asks the nurse to repeat all of the information. Based on this assessment, which nursing diagnosis is most appropriate for the patient? a. Risk for ineffective adherence to treatment related to denial of need for chemotherapy b. Acute confusion related to infiltration of leukemia cells into the central nervous system c. Risk for ineffective health maintenance related to anxiety about new leukemia diagnosis d. Deficient knowledge: chemotherapy related to a lack of interest in learning about treatment ANS: C The patient who has a new cancer diagnosis is likely to have high anxiety, which may impact learning and require that the nurse repeat and reinforce information. The patient’s history of a recent diagnosis suggests that infiltration of the leukemia is not a likely cause of the confusion. The patient asks for the information to be repeated, indicating that lack of interest in learning and denial are not etiologic factors. 28. A hospitalized patient who has received chemotherapy for leukemia develops neutropenia. Which observation by the nurse would indicate a need for further teaching? a. The patient ambulates several times a day in the room. b. The patient’s visitors bring in some fresh peaches from home. c. The patient cleans with a warm washcloth after having a stool. d. The patient uses soap and shampoo to shower every other day. ANS: B Fresh, thinned-skin fruits are not permitted in a neutropenic diet because of the risk of bacteria being present. The patient should ambulate in the room rather than the hospital hallway to avoid exposure to other patients or visitors. Because overuse of soap can dry the skin and increase infection risk, showering every other day is acceptable. Careful cleaning after having a bowel movement will help prevent skin breakdown and infection. 29. The nurse is caring for a patient who has been diagnosed with stage I cancer of the colon. When assessing the need for psychologic support, which question by the nurse will provide the most information? a. “How long ago were you diagnosed with this cancer?” b. “Do you have any concerns about body image changes?” c. “Can you tell me what has been helpful to you in the past when coping with stressful events?” d. “Are you familiar with the stages of emotional adjustment to a diagnosis like cancer of the colon?” ANS: C Information about how the patient has coped with past stressful situations helps the nurse determine usual coping mechanisms and their effectiveness. The length of time since the diagnosis will not provide much information about the patient’s need for support. The patient’s knowledge of typical stages in adjustment to a critical diagnosis does not provide insight into patient needs for assistance. Because surgical interventions for stage I cancer of the colon may not cause any body image changes, this question is not appropriate at this time. 30. The nurse assesses a patient who is receiving interleukin-2. Which finding should the nurse report immediately to the health care provider? a. Generalized muscle aches b. Complaints of nausea and anorexia c. Oral temperature of 100.6° F (38.1° C) d. Crackles heard at the lower scapular border ANS: D Capillary leak syndrome and acute pulmonary edema are possible toxic effects of interleukin-2. The patient may need oxygen and the nurse should rapidly notify the health care provider. The other findings are common side effects of interleukin-2. 31. The nurse obtains information about a hospitalized patient who is receiving chemotherapy for colorectal cancer. Which information about the patient alerts the nurse to discuss a possible change in therapy with the health care provider? a. Poor oral intake b. Frequent loose stools c. Complaints of nausea and vomiting d. Increase in carcinoembryonic antigen (CEA) ANS: D An increase in CEA indicates that the chemotherapy is not effective for the patient’s cancer and may need to be modified. The other patient findings are common adverse effects of chemotherapy. The nurse may need to address these, but they would not necessarily indicate a need for a change in therapy. 32. The nurse reviews the laboratory results of a patient who is receiving chemotherapy. Which laboratory result is most important to report to the health care provider? a. Hematocrit of 30% b. Platelets of 95,000/µL c. Hemoglobin of 10 g/L d. White blood cell (WBC) count of 2700/µL ANS: D The low WBC count places the patient at risk for severe infection and is an indication that the chemotherapy dose may need to be lower or that WBC growth factors such as filgrastim (Neupogen) are needed. Although the other laboratory data indicate decreased levels, they do not indicate any immediate life-threatening adverse effects of the chemotherapy. 33. When caring for a patient who is pancytopenic, which action by unlicensed assistive personnel (UAP) indicates a need for the nurse to intervene? a. The UAP assists the patient to use dental floss after eating. b. The UAP adds baking soda to the patient’s saline oral rinses. c. The UAP puts fluoride toothpaste on the patient’s toothbrush. d. The UAP has the patient rinse after meals with a saline solution. ANS: A Use of dental floss is avoided in patients with pancytopenia because of the risk for infection and bleeding. The other actions are appropriate for oral care of a pancytopenic patient. 34. The nurse supervises the care of a patient with a temporary radioactive cervical implant. Which action by unlicensed assistive personnel (UAP), if observed by the nurse, would require an intervention? a. The UAP flushes the toilet once after emptying the patient’s bedpan. b. The UAP stands by the patient’s bed for 30 minutes talking with the patient. c. The UAP places the patient’s bedding in the laundry container in the hallway. d. The UAP gives the patient an alcohol-containing mouthwash to use for oral care. ANS: B Because patients with temporary implants emit radioactivity while the implants are in place, exposure to the patient is limited. Laundry and urine/feces do not have any radioactivity and do not require special precautions. Cervical radiation will not affect the oral mucosa, and alcohol-based mouthwash is not contraindicated. 35. The nurse receives change-of-shift report on the oncology unit. Which patient should the nurse assess first? a. 35-year-old patient who has wet desquamation associated with abdominal radiation b. 42-year-old patient who is sobbing after receiving a new diagnosis of ovarian cancer c. 24-year-old patient who received neck radiation and has blood oozing from the neck d. 56-year-old patient who developed a new pericardial friction rub after chest radiation ANS: C Because neck bleeding may indicate possible carotid artery rupture in a patient who is receiving radiation to the neck, this patient should be seen first. The diagnoses and clinical manifestations for the other patients are not immediately life threatening. 36. Which action should the nurse take when caring for a patient who is receiving chemotherapy and complains of problems with concentration? a. Teach the patient to rest the brain by avoiding new activities. b. Teach that “chemo-brain” is a short-term effect of chemotherapy. c. Report patient symptoms immediately to the health care provider. d. Suggest use of a daily planner and encourage adequate rest and sleep. ANS: D Use of tools to enhance memory and concentration such as a daily planner and adequate rest are helpful for patients who develop “chemo-brain” while receiving chemotherapy. Patients should be encouraged to exercise the brain through new activities. Chemo-brain may be short- or long-term. There is no urgent need to report common chemotherapy side effects to the provider. 37. The nurse assesses a patient with non-Hodgkin’s lymphoma who is receiving an infusion of rituximab (Rituxan). Which assessment finding would require the most rapid action by the nurse? a. Shortness of breath b. Temperature 100.2° F (37.9° C) c. Shivering and complaint of chills d. Generalized muscle aches and pains ANS: A Rituximab (Rituxan) is a monoclonal antibody. Shortness of breath should be investigated rapidly because anaphylaxis is a possible reaction to monoclonal antibody administration. The nurse will need to rapidly take actions such as stopping the infusion, assessing the patient further, and notifying the health care provider. The other findings will also require action by the nurse, but are not indicative of life-threatening complications. 38. A patient who is being treated for stage IV lung cancer tells the nurse about new-onset back pain. Which action should the nurse take first? a. Give the patient the prescribed PRN opioid. b. Assess for sensation and strength in the legs. c. Notify the health care provider about the symptoms. d. Teach the patient how to use relaxation to reduce pain. ANS: B Spinal cord compression, an oncologic emergency, can occur with invasion of tumor into the epidural space. The nurse will need to assess the patient further for symptoms such as decreased leg sensation and strength and then notify the health care provider. Administration of opioids or use of relaxation may be appropriate but only after the nurse has assessed for possible spinal cord compression. DIF: Cognitive Level: Apply (application) REF: 277 OBJ: Special Questions: Prioritization TOP: Nursing Process: Implementation MSC: NCLEX: Physiological Integrity 39. The nurse is caring for a patient with left-sided lung cancer. Which finding would be most important for the nurse to report to the health care provider? a. Hematocrit 32% b. Pain with deep inspiration c. Serum sodium 126 mEq/L d. Decreased breath sounds on left side ANS: C Syndrome of inappropriate antidiuretic hormone (and the resulting hyponatremia) is an oncologic metabolic emergency and will require rapid treatment in order to prevent complications such as seizures and coma. The other findings also require intervention, but are common in patients with lung cancer and not immediately life threatening. DIF: Cognitive Level: Apply (application) REF: 278 OBJ: Special Questions: Prioritization TOP: Nursing Process: Assessment MSC: NCLEX: Physiological Integrity 40. An older adult patient who has colorectal cancer is receiving IV fluids at 175 mL/hour in conjunction with the prescribed chemotherapy. Which finding by the nurse is most important to report to the health care provider? a. Patient complains of severe fatigue. b. Patient needs to void every hour during the day. c. Patient takes only 50% of meals and refuses snacks. d. Patient has audible crackles to the midline posterior chest. ANS: D Rapid fluid infusions may cause heart failure, especially in older patients. The other findings are common in patients who have cancer and/or are receiving chemotherapy. DIF: Cognitive Level: Apply (application) REF: 278 OBJ: Special Questions: Prioritization TOP: Nursing Process: Assessment MSC: NCLEX: Physiological Integrity 41. After change-of-shift report on the oncology unit, which patient should the nurse assess first? a. Patient who has a platelet count of 82,000/µL after chemotherapy b. Patient who has xerostomia after receiving head and neck radiation c. Patient who is neutropenic and has a temperature of 100.5° F (38.1° C) d. Patient who is worried about getting the prescribed long-acting opioid on time ANS: C Temperature elevation is an emergency in neutropenic patients because of the risk for rapid progression to severe infections and sepsis. The other patients also require assessments or interventions, but do not need to be assessed as urgently. Patients with thrombocytopenia do not have spontaneous bleeding until the platelets are 20,000/µL. Xerostomia does not require immediate intervention. Although breakthrough pain needs to be addressed rapidly, the patient does not appear to have breakthrough pain. DIF: Cognitive Level: Analyze (analysis) REF: 277 OBJ: Special Questions: Prioritization; Multiple Patients TOP: Nursing Process: Assessment MSC: NCLEX: Safe and Effective Care Environment MULTIPLE RESPONSE 1. The nurse at the clinic is interviewing a 64-year-old woman who is 5 feet, 3 inches tall and weighs 125 pounds (57 kg). The patient has not seen a health care provider for 20 years. She walks 5 miles most days and has a glass of wine 2 or 3 times a week. Which topics will the nurse plan to include in patient teaching about cancer screening and decreasing cancer risk (select all that apply)? a. Pap testing b. Tobacco use c. Sunscreen use d. Mammography e. Colorectal screening ANS: A, C, D, E The patient’s age, gender, and history indicate a need for screening and/or teaching about colorectal cancer, mammography, Pap smears, and sunscreen. The patient does not use excessive alcohol or tobacco, she is physically active, and her body weight is healthy. 2. A patient develops neutropenia after receiving chemotherapy. Which information about ways to prevent infection will the nurse include in the teaching plan (select all that apply)? a. Cook food thoroughly before eating. b. Choose low fiber, low residue foods. c. Avoid public transportation such as buses. d. Use rectal suppositories if needed for constipation. e. Talk to the oncologist before having any dental work done. ANS: A, C, E Eating only cooked food and avoiding public transportation will decrease infection risk. A high-fiber diet is recommended for neutropenic patients to decrease constipation. Because bacteria may enter the circulation during dental work or oral surgery, the patient may need to postpone dental work or take antibiotics. Chapter 52: Nursing Management: Breast Disorders 1. The nurse teaching a young women’s community service group about breast self-examination (BSE) will include that a. BSE will reduce the risk of dying from breast cancer. b. BSE should be done daily while taking a bath or shower. c. annual mammograms should be scheduled in addition to BSE. d. performing BSE after the menstrual period is more comfortable. ANS: D Performing BSE at the end of the menstrual period will reduce the breast tenderness associated with the procedure. The evidence is not clear that BSE reduces mortality from breast cancer. BSE should be done monthly. Annual mammograms are not routinely scheduled for women under age 40, and newer guidelines suggest delaying them until age 50. 2. During a well woman physical exam, a 43-year-old patient asks about her risk for breast cancer. Which question is most pertinent for the nurse to ask? a. “Do you currently smoke tobacco?” b. “Have you ever had a breast injury?” c. “At what age did you start having menstrual periods?” d. “Is there a family history of fibrocystic breast changes?” ANS: C Early menarche and late menopause are risk factors for breast cancer because of the prolonged exposure to estrogen that occurs. Cigarette smoking, breast trauma, and fibrocystic breast changes are not associated with increased breast cancer risk. 3. A 51-year-old patient with a small immobile breast lump is considering having a fine-needle aspiration (FNA) biopsy. The nurse explains that an advantage to this procedure is that a. FNA is done in the outpatient clinic and results are available in 1 to 2 days. b. only a small incision is needed, resulting in minimal breast pain and scarring. c. if the biopsy results are negative, no further diagnostic testing will be needed. d. FNA is guided by a mammogram, ensuring that cells are taken from the lesion. ANS: A FNA is done in outpatient settings and results are available in 24 to 48 hours. No incision is needed. FNA may be guided by ultrasound, but not by mammogram. Because the immobility of the breast lump suggests cancer, further testing will be done if the FNA is negative. 4. Which assessment finding in a 36-year-old patient is most indicative of a need for further evaluation? a. Bilateral breast nodules that are tender with palpation b. A breast nodule that is 1 cm in size, nontender, and fixed c. A breast lump that increases in size before the menstrual period d. A breast lump that is small, mobile, with a rubbery consistency ANS: B Painless and fixed lumps suggest breast cancer. The other findings are more suggestive of benign processes such as fibrocystic breasts and fibroadenoma. 5. A 53-year-old woman at menopause is discussing the use of hormone therapy (HT) with the nurse. Which information about the risk of breast cancer will the nurse provide? a. HT is a safe therapy for menopausal symptoms if there is no family history of BRCA genes. b. HT does not appear to increase the risk for breast cancer unless there are other risk factors. c. The patient and her health care provider must weigh the benefits of HT against the risks of breast cancer. d. Natural herbs are as effective as estrogen in relieving symptoms without increasing the risk of breast cancer. ANS: C Because HT has been linked to increased risk for breast cancer, the patient and provider must determine whether or not to use HT. Breast cancer incidence is increased in women using HT, independent of other risk factors. HT increases the risk for both non–BRCA-associated cancer and BRCA-related cancers. Alternative therapies can be used but are not consistent in relieving menopausal symptoms. 6. A 58-year-old woman tells the nurse, “I understand that I have stage II breast cancer and I need to decide on a surgery, but I feel overwhelmed. What do you think I should do?” Which response by the nurse is best? a. “I would have a lumpectomy, but you need to decide what is best for you.” b. “Tell me what you understand about the surgical options that are available.” c. “It would not be appropriate for me to make a decision about your health.” d. “There is no need to make a decision rapidly; you have time to think about this.” ANS: B Inquiring about the patient’s understanding shows the nurse’s willingness to assist the patient with the decision-making process without imposing the nurse’s values or opinions. Treatment decisions for breast cancer do need to be made relatively quickly. Imposing the nurse’s opinions or showing an unwillingness to discuss the topic could cut off communication. 7. The nurse will teach a patient with metastatic breast cancer who has a new prescription for trastuzumab (Herceptin) that a. hot flashes may occur with the medication. b. serum electrolyte levels will be drawn monthly. c. the patient will need frequent eye examinations. d. the patient should call if she notices ankle swelling. ANS: D Trastuzumab can lead to ventricular dysfunction, so the patient is taught to self-monitor for symptoms of heart failure. There is no need to monitor serum electrolyte levels. Hot flashes or changes in visual acuity may occur with tamoxifen, but not with trastuzumab. 8. After a 48-year-old patient has had a modified radical mastectomy, the pathology report identifies the tumor as an estrogen-receptor positive adenocarcinoma. The nurse will plan to teach the patient about a. estradiol (Estrace). b. raloxifene (Evista). c. tamoxifen (Nolvadex). d. trastuzumab (Herceptin). ANS: C Tamoxifen is used for estrogen-dependent breast tumors in premenopausal women. Raloxifene is used to prevent breast cancer, but it is not used postmastectomy to treat breast cancer. Estradiol will increase the growth of estrogen-dependent tumors. Trastuzumab is used to treat tumors that have the HER-2 receptor. 9. Which nursing action should be included in the plan of care for a patient returning to the surgical unit following a left modified radical mastectomy with dissection of axillary lymph nodes? a. Obtain a permanent breast prosthesis before the patient is discharged from the hospital. b. Teach the patient to use the ordered patient-controlled analgesia (PCA) every 10 minutes. c. Post a sign at the bedside warning against venipunctures or blood pressures in the left arm. d. Insist that the patient examine the surgical incision when the initial dressings are removed. ANS: C The patient is at risk for lymphedema and infection if blood pressures or venipuncture are done on the right arm. The patient is taught to use the PCA as needed for pain control rather than at a set time. The nurse allows the patient to examine the incision and participate in care when the patient feels ready. Permanent breast prostheses are usually obtained about 6 weeks after surgery. 10. The nurse provides discharge teaching for a 61-year-old patient who has had a left modified radical mastectomy and lymph node dissection. Which statement by the patient indicates that teaching has been successful? a. “I will need to use my right arm and to rest the left one.” b. “I will avoid reaching over the stove with my left hand.” c. “I will keep my left arm in a sling until the incision is healed.” d. “I will stop the left arm exercises if moving the arm is painful.” ANS: B The patient should avoid any activity that might injure the left arm, such as reaching over a burner. If the left arm exercises are painful, analgesics should be used and the exercises continued in order to restore strength and range of motion. The left arm should be elevated at or above heart level and should be used to improve range of motion and function. 11. A 33-year-old patient has a saline breast implant inserted in the outpatient surgery area. Which instruction will the nurse include in the discharge teaching? a. Take aspirin every 4 hours to reduce inflammation. b. Check wound drains for excessive blood or a foul odor. c. Wear a loose-fitting bra to decrease irritation of the sutures. d. Resume normal activities 2 to 3 days after the mammoplasty. ANS: B The patient should be taught drain care because the drains will be in place for 2 or 3 days after surgery. Normal activities can be resumed after 2 to 3 weeks. A bra that provides good support is typically ordered. Aspirin will decrease coagulation and is typically not given after surgery. 12. The nurse is providing preoperative teaching about the transverse rectus abdominis musculocutaneous (TRAM) procedure to a patient. Which information will the nurse include? a. Saline-filled implants are placed under the pectoral muscles. b. Recovery from the TRAM surgery takes at least 6 to 8 weeks. c. Muscle tissue removed from the back is used to form a breast. d. TRAM flap procedures may be done in outpatient surgery centers. ANS: B Patients take at least 6 to 8 weeks to recover from the TRAM surgery. Tissue from the abdomen is used to reconstruct the breast. The TRAM procedure can take up to 8 hours and requires postoperative hospitalization. Saline implants are used in mammoplasty. 13. A patient newly diagnosed with stage I breast cancer is discussing treatment options with the nurse. Which statement by the patient indicates that additional teaching may be needed? a. “There are several options that I can consider for treating the cancer.” b. “I will probably need radiation to the breast after having the surgery.” c. “Mastectomy is the best choice to decrease the chance of cancer recurrence.” d. “I can probably have reconstructive surgery at the same time as a mastectomy.” ANS: C The survival rates with lumpectomy and radiation or modified radical mastectomy are comparable. The other patient statements indicate a good understanding of stage I breast cancer treatment. 14. Which information will the nurse include in patient teaching for a 36-year-old patient who is scheduled for stereotactic core biopsy of the breast? a. A local anesthetic will be given before the biopsy specimen is obtained. b. You will need to lie flat on your back and lie very still during the biopsy. c. A thin needle will be inserted into the lump and aspirated to remove tissue. d. You should not have anything to eat or drink for 6 hours before the procedure. ANS: A A local anesthetic is given before stereotactic biopsy. NPO status is not needed because no sedative drugs are given. The patient is placed in the prone position. A biopsy gun is used to obtain the specimens. 15. A student nurse prepares a list of teaching topics for a patient with a new diagnosis of breast cancer. Which item should the charge nurse suggest that the student nurse omit from the teaching topic list about breast cancer diagnostic testing? a. CA 15-3 level testing b. HER-2 receptor testing c. Estrogen receptor testing d. Oncotype DX assay testing ANS: A Tumor markers such as CA 15-3 are used to monitor response to treatment for breast cancer, not to detect or diagnose breast cancer. The other tests are likely to be used for additional diagnostic testing in a patient with breast cancer. 16. The nurse will anticipate teaching a 56-year-old patient who is diagnosed with lobular carcinoma in situ (LCIS) about a. lumpectomy. b. lymphatic mapping. c. MammaPrint testing. d. tamoxifen (Nolvadex). ANS: D Tamoxifen is used as a chemopreventive therapy in some patients with LCIS. The other diagnostic tests and therapies are not needed because LCIS does not usually require treatment. 17. Which information should the nurse include in teaching a patient who is scheduled for external beam radiation to the breast? a. The radiation therapy will take a week to complete. b. Careful skin care in the radiated area will be necessary. c. Visitors are restricted until the radiation therapy is completed. d. Wigs may be used until the hair regrows after radiation therapy. ANS: B Skin care will be needed because of the damage caused to the skin by the radiation. External beam radiation is done over a 5- to 6-week period. Scalp hair loss does not occur with breast radiation therapy. Because the patient does not have radioactive implants, no visitor restrictions are necessary. 18. Which patient statement indicates that the nurse’s teaching about tamoxifen (Nolvadex) has been effective? a. “I can expect to have leg cramps.” b. “I will call if I have any eye problems.” c. “I should contact you if I have hot flashes.” d. “I will be taking the medication for 6 to 12 months.” ANS: B Retinopathy, cataracts, and decreased visual acuity should be immediately reported because it is likely that the tamoxifen will be discontinued or decreased. Tamoxifen treatment generally lasts 5 years. Hot flashes are an expected side effect of tamoxifen. Leg cramps may be a sign of deep vein thrombosis, and the patient should immediately notify the health care provider if pain occurs. 19. The nurse is admitting a patient scheduled this morning for lumpectomy and axillary lymph node dissection. Which action should the nurse take first? a. Teach the patient how to deep breathe and cough. b. Discuss options for postoperative pain management. c. Explain the postdischarge care of the axillary drains. d. Ask the patient to describe what she knows about the surgery. ANS: D Before teaching, the nurse should assess the patient’s current knowledge level. The other teaching also may be appropriate, depending on the assessment findings. 20. When the nurse is working in the women’s health care clinic, which action is appropriate to take? a. Teach a healthy 30-year-old about the need for an annual mammogram. b. Discuss scheduling an annual clinical breast examination with a 22-year-old. c. Explain to a 60-year-old that mammography frequency can be reduced to every 3 years. d. Teach a 28-year-old with a BRCA-1 mutation about magnetic resonance imaging (MRI). ANS: D MRI (in addition to mammography) is recommended for women who are at high risk for breast cancer. A young woman should have a clinical breast exam every 3 years. Annual mammograms are recommended for women over 50. 21. Which action will the nurse include in the plan of care for a patient with right arm lymphedema? a. Check blood pressure (BP) on both right and left arms. b. Avoid isometric exercise on the right arm. c. Assist with application of a compression sleeve. d. Keep the right arm at or below the level of the heart. ANS: C Compression of the arm assists in improving lymphatic flow toward the heart. Isometric exercises may be prescribed for lymphedema. BPs should only be done on the patient’s right arm. The arm should not be placed in a dependent position. 22. A 36-year-old who has a diagnosis of fibrocystic breast changes calls the nurse in the clinic with symptoms. Which is most important to report to the health care provider? a. There is yellow-green discharge from the patient’s right nipple. b. There is an area on the breast that is hot, pink, and tender to touch. c. The lumps are firm and most are in the upper outer breast quadrants. d. The lumps are larger and painful before the patient’s menstrual period. ANS: B An area that is hot or pink suggests an infectious process such as mastitis, which would require further assessment and treatment. The other information also will be reported, but these findings are typical in fibrocystic breasts. 23. The nurse notes bilateral enlargement of the breasts during examination of a 62-year-old man. Which action should the nurse take first? a. Teach the patient how to palpate the breast tissue for lumps. b. Question the patient about medications being currently used. c. Refer the patient for mammography and biopsy of the breast tissue. d. Explain that this is a temporary condition due to hormonal changes. ANS: B The first action should be further assessment. Because gynecomastia is a possible side effect of drug therapy, asking about the current drug regimen is appropriate. The other actions may be needed, depending on the data that are obtained with further assessment. 24. A patient has had left-sided lumpectomy (breast-conservation surgery) and an axillary lymph node dissection. Which nursing intervention is appropriate to delegate to a licensed practical/vocational nurse (LPN/LVN)? a. Teaching the patient how to avoid injury to the left arm b. Assessing the patient’s range of motion for the left arm \g in hospice is desirable because patient losses are common. ANS: B It is appropriate for the nurse to cry and express sadness in other ways when a patient dies, and the family is likely to feel that this is therapeutic. Contacting a grief counselor, leaving the family to grieve privately, and considering whether hospice continues to be a satisfying place to work are all appropriate actions as well, but the nurse’s initial action at this time should be to share the grieving process with the family. 11. A middle-aged patient tells the nurse, “My mother died 4 months ago, and I just can’t seem to get over it. I’m not sure it is normal to still think about her every day.” Which nursing diagnosis is most appropriate? a. Hopelessness related to inability to resolve grief b. Complicated grieving related to unresolved issues c. Anxiety related to lack of knowledge about normal grieving d. Chronic sorrow related to ongoing distress about loss of mother ANS: C The patient should be reassured that grieving activities such as frequent thoughts about the deceased are considered normal for months or years after a death. The other nursing diagnoses imply that the patient’s grief is unusual or pathologic, which is not the case. 12. The son of a dying patient tells the nurse, “Mother doesn’t really respond any more when I visit. I don’t think she knows that I am here.” Which response by the nurse is appropriate? a. “You may need to cut back your visits for now to avoid overtiring your mother.” b. “Withdrawal may sometimes be a normal response when preparing to leave life.” c. “It will be important for you to stimulate your mother as she gets closer to dying.” d. “Many patients don’t really know what is going on around them at the end of life.” ANS: B Withdrawal is a normal psychosocial response to approaching death. Dying patients may maintain the ability to hear while not being able to respond. Stimulation will tire the patient and is not an appropriate response to withdrawal in this circumstance. Visitors are encouraged to be “present” with the patient, talking softly and making physical contact in a way that does not demand a response from the patient. 13. Which patient should the nurse refer for hospice care? a. 60-year-old with lymphoma whose children are unable to discuss issues related to dying b. 72-year-old with chronic severe pain as a result of spinal arthritis and vertebral collapse c. 28-year-old with AIDS-related dementia who needs palliative care and pain management d. 56-year-old with advanced liver failure whose family members can no longer provide care in the home ANS: C Hospice is designed to provide palliative care such as symptom management and pain control for patients at the end of life. Patients who require more care than the family can provide, whose families are unable to discuss important issues related to dying, or who have severe pain are candidates for other nursing services but are not appropriate hospice patients. 14. The nurse admits a terminally ill patient to the hospital. What is the first action that the nurse should complete when planning this patient’s care? a. Determine the patient’s wishes regarding end-of-life care. b. Emphasize the importance of addressing any family issues. c. Discuss the normal grief process with the patient and family. d. Encourage the patient to talk about any fears or unresolved issues. ANS: A The nurse’s initial action should be to assess the patient’s wishes at this time. The other actions may be implemented if the patient or the family express a desire to discuss fears, understand the grief process, or address family issues, but they should not be implemented until the assessment indicates that they are appropriate. 15. Which action is best for the nurse to take to ensure culturally competent care for an alert, terminally ill Filipino patient? a. Ask the patient and family about their preferences for care during this time. b. Let the family decide whether to tell the patient about the terminal diagnosis. c. Obtain information from Filipino staff members about possible cultural needs. d. Remind family members that dying patients prefer to have someone at the bedside. ANS: A Because cultural beliefs may vary among people of the same ethnicity, the nurse’s best action is to assess the expectations of both the patient and family. The other actions may be appropriate, but the nurse can only plan for individualized culturally competent care after assessment of this patient and family. 1. Which nursing actions for the care of a dying patient can the nurse delegate to a licensed practical/vocational nurse (LPN/LVN) (select all that apply)? a. Provide postmortem care to the patient. b. Encourage the family members to talk with and reassure the patient. c. Determine how frequently physical assessments are needed for the patient. d. Teach family members about commonly occurring signs of approaching death. e. Administer the prescribed morphine sulfate sublingual as necessary for pain control. ANS: A, B, E Medication administration, psychosocial care, and postmortem care are included in LPN/LVN education and scope of practice. Patient and family teaching and assessment and planning of frequency for assessments are skills that require registered nurse level education and scope of practice. [Show More]
Last updated: 1 year ago
Preview 1 out of 88 pages
Instant download
Buy this document to get the full access instantly
Instant Download Access after purchase
Add to cartInstant download
Reviews( 0 )
Document information
Connected school, study & course
About the document
Uploaded On
Mar 18, 2021
Number of pages
88
Written in
Additional information
This document has been written for:
Uploaded
Mar 18, 2021
Downloads
5
Views
58

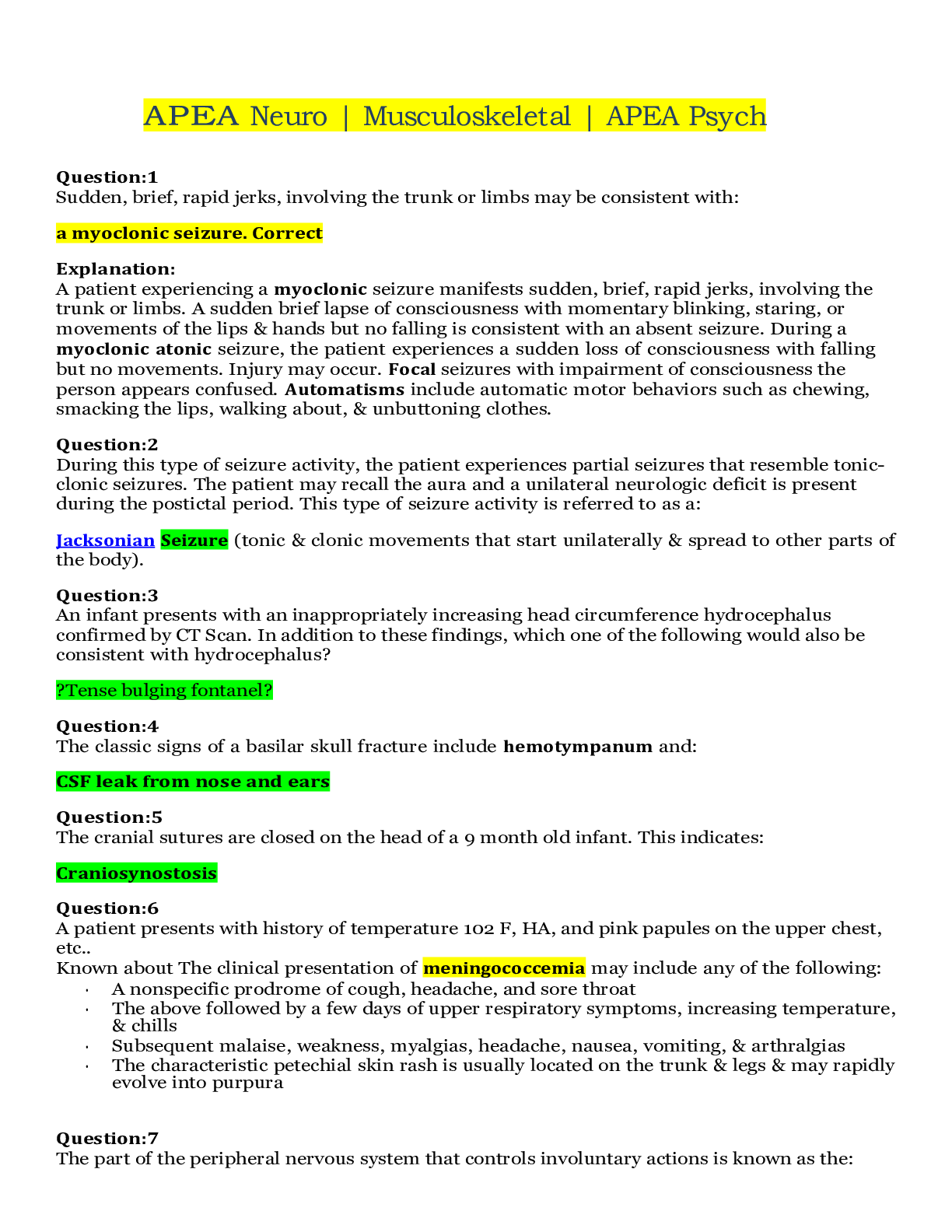
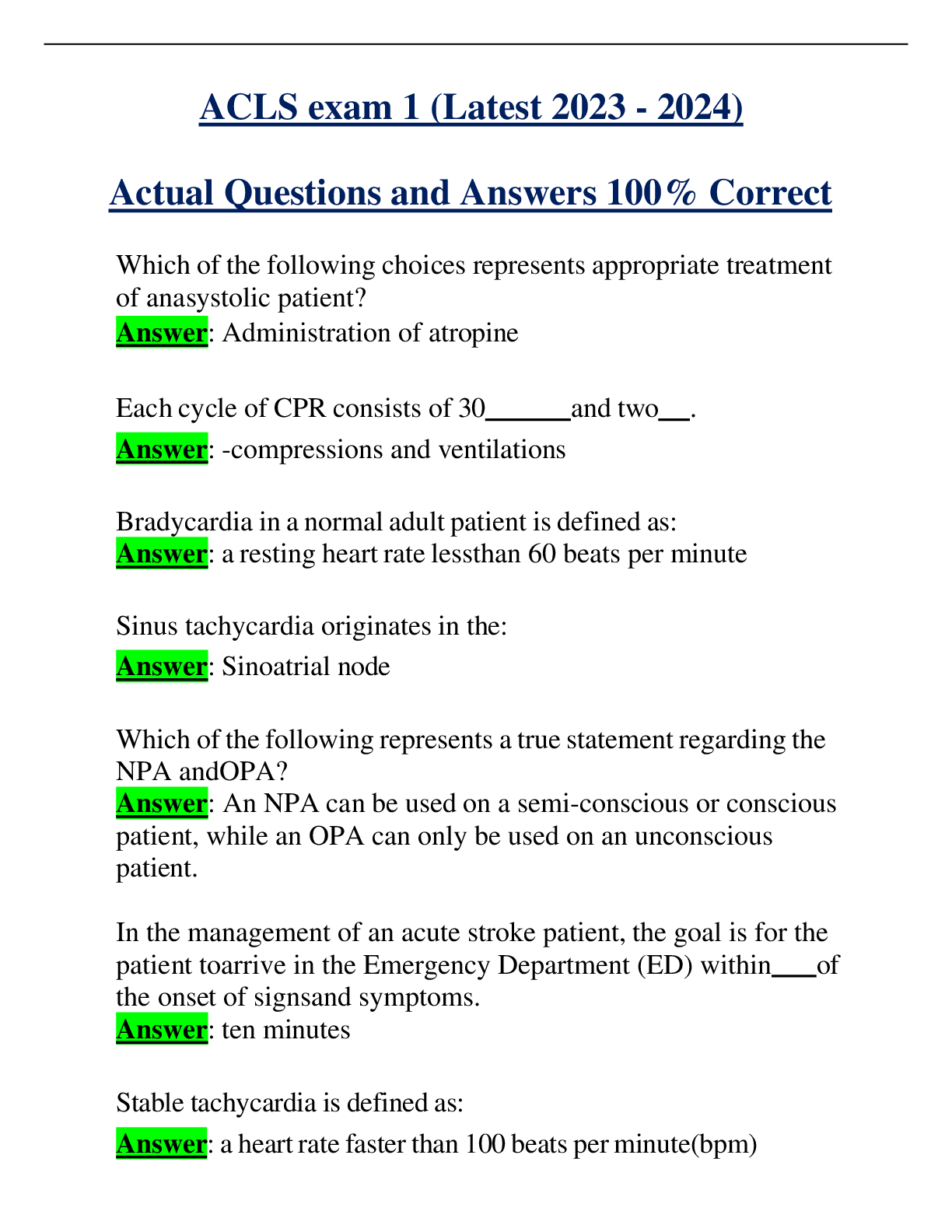
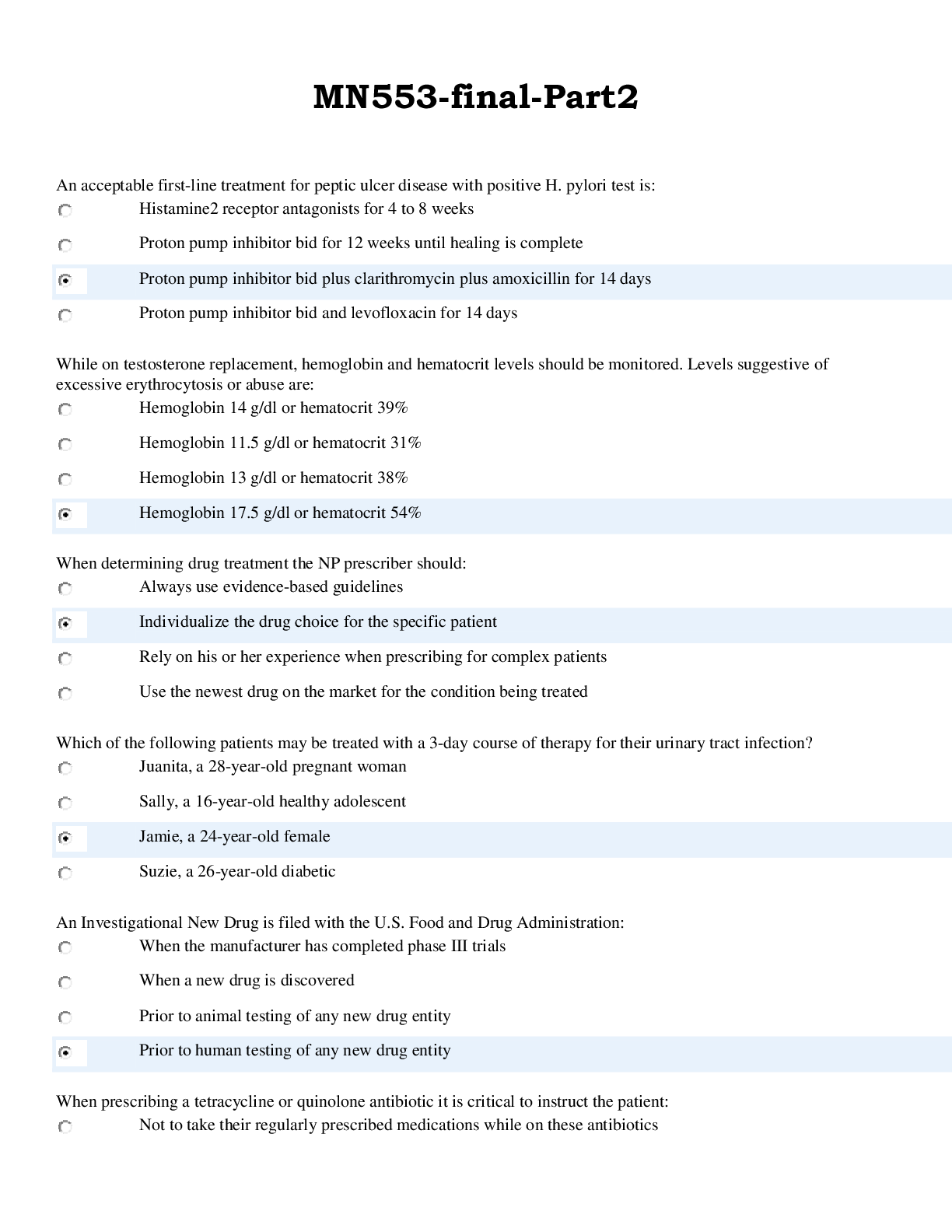
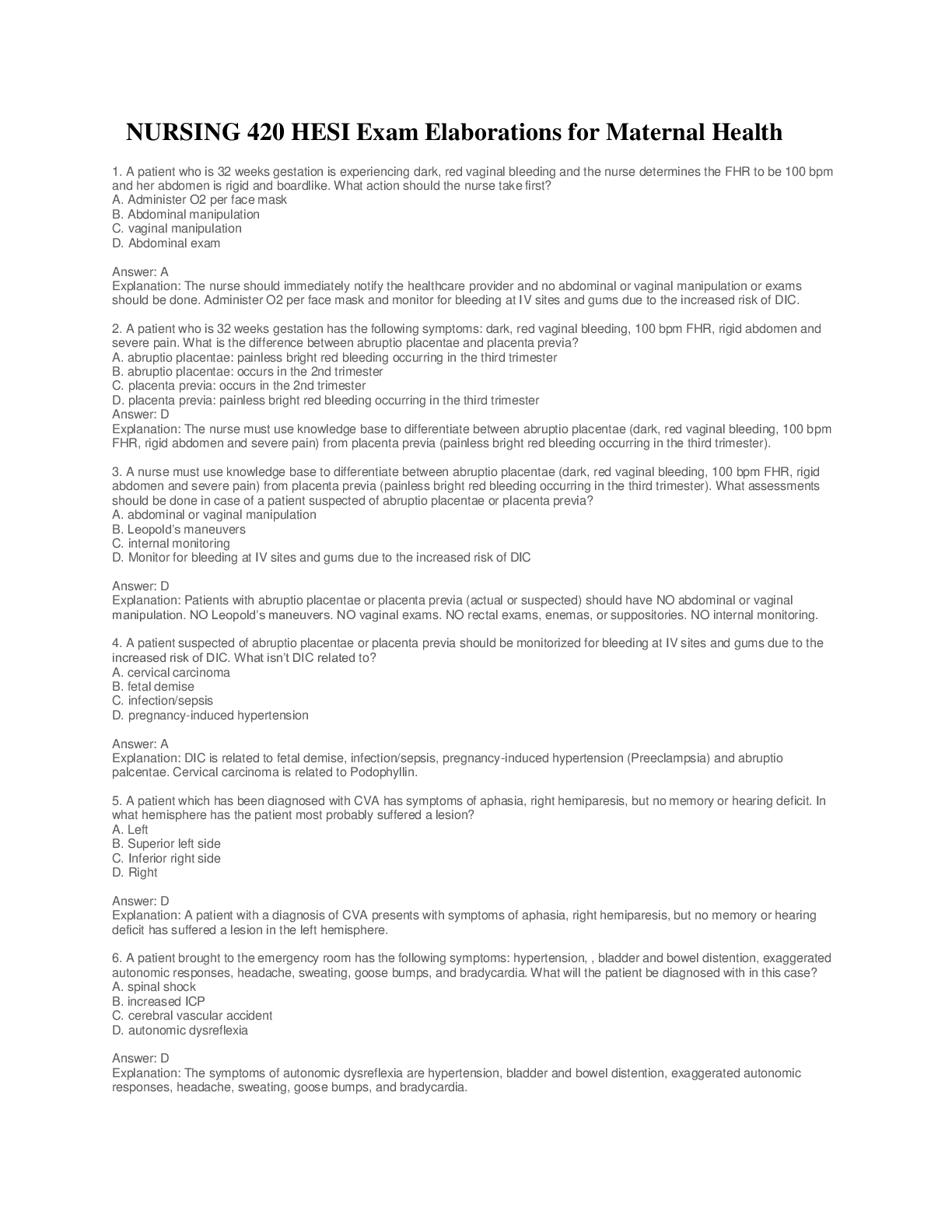

.png)