*NURSING > Study Notes > NUR 2790 Exam III Nursing III Content Study Guide-Rasmussen College: 100% Correct. (All)
NUR 2790 Exam III Nursing III Content Study Guide-Rasmussen College: 100% Correct.
Document Content and Description Below
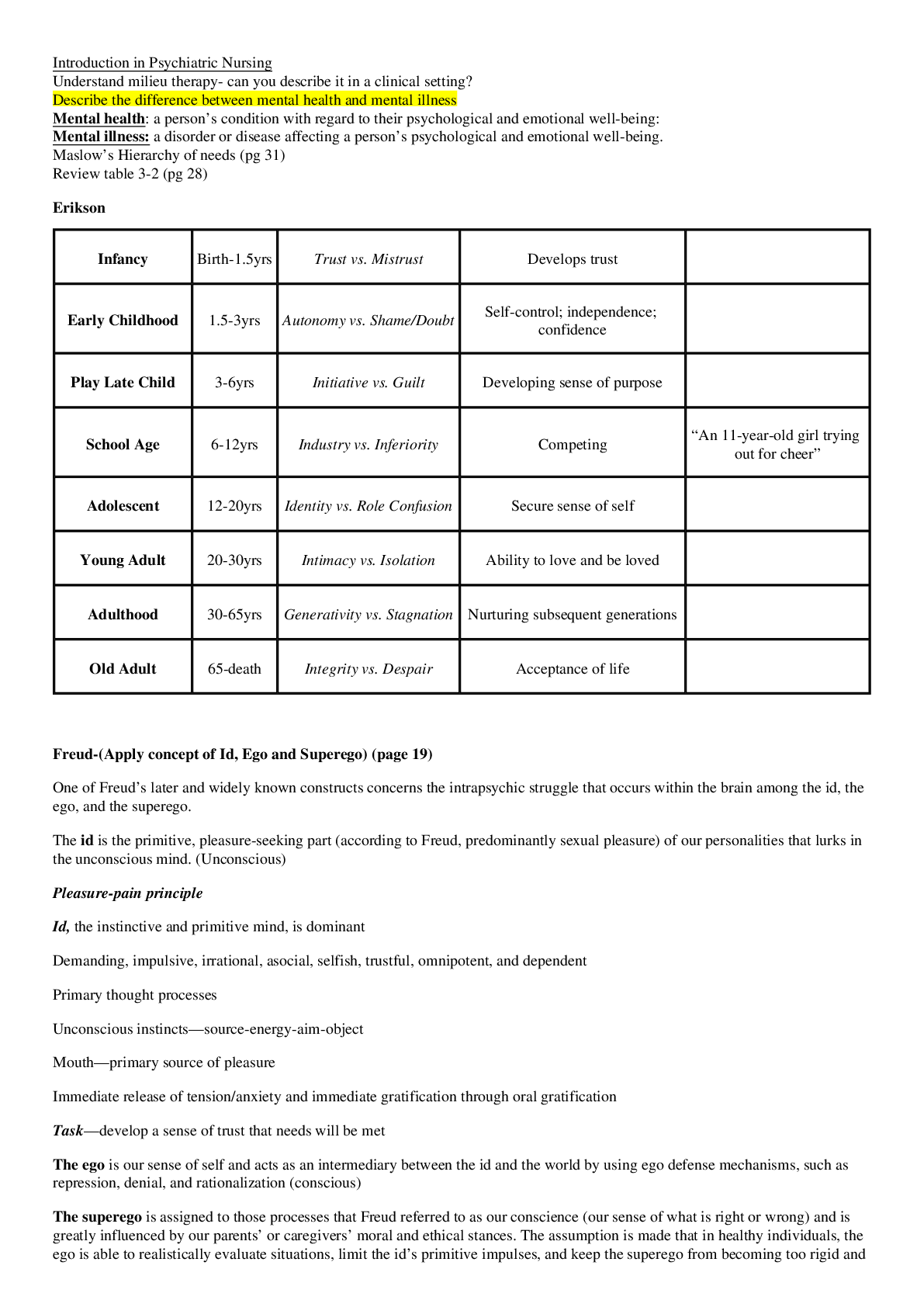
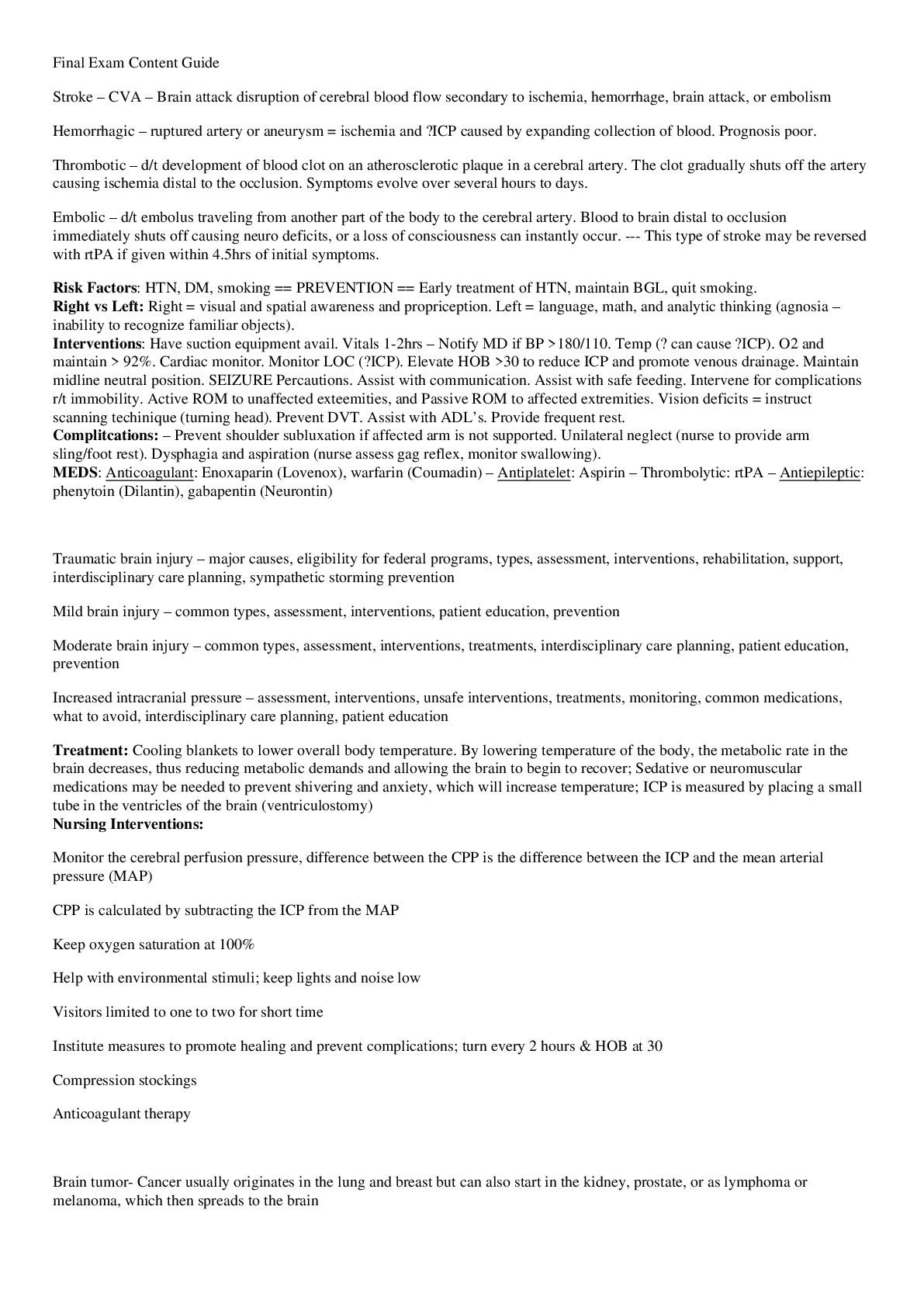
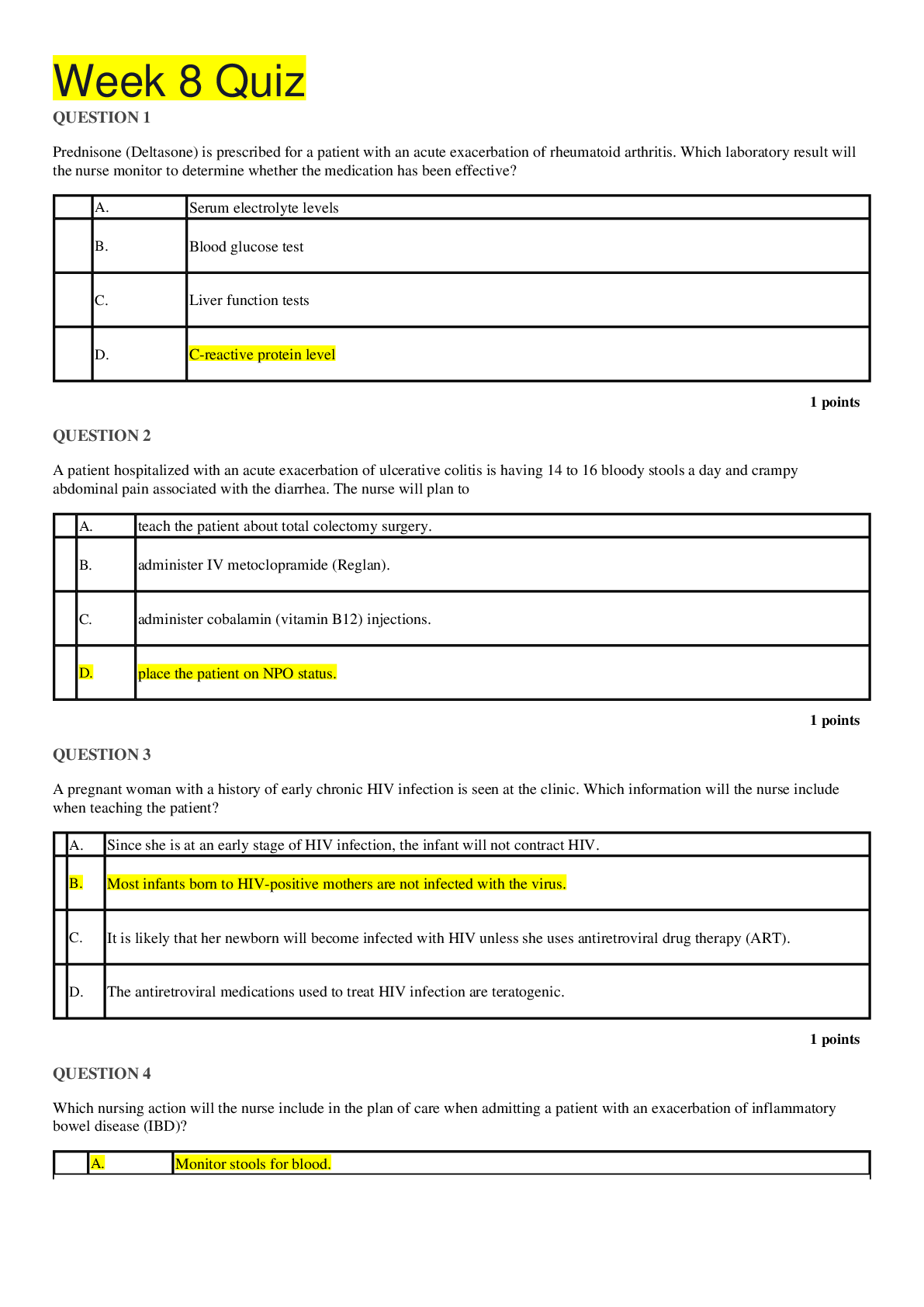
NUR 2790 Exam III Nursing III Content Study Guide-Rasmussen College: 100% Correct. Nursing III Exam 3 Content Guide 1. Acromegaly – gigantism; caused by hypersecretion of pituitary GH over a lon... g period of time (or childhood). Hyperprolactinemia is a prolactin secreting pituitary tumor (most commonly d/t ingestion of dopamine antagonist dugs; haloperidol, risperidone). In some incidences, pituitary prolactinomas secrete GH simultaneously and cause acromegaly. This condition is associated with a decrease in estrogen – so s/s in women: vaginal dryness, hot flashes, galactorrhea, amenorrhea, oligomenorrhea, anovulation (infertility). In men: causes ↓testosterone s/s: ↓facial and body hair, ED, ↓libido, small testis, and infertility. Tx: cabergoline (Dostinex) Diagnosis often missed or delayed (~ 42yrs). Undertreated ↑morbidity and mortality d/t the chronic effect of GH on body organs = ↑ cardiovascular, cerebrovascular, and respiratory disease; malignancies; and diabetes. In children and adolescents: GH stimulates growth in all body tissues prior to fusion of the growth plate. In adults: GH causes continued growth of soft tissues and small bones of the hands/feet & the membranous bones of the skull and face. Signs and symptoms of: Child 7ft tall. Changes in facial features. Obesity, carpal tunnel, enlarged tongue, glucose intolerance. 30% will have some form of cardiac disease, (CAD, cardiac dysrhythmias, left ventricular hypertrophy (LVH), or cardiomyopathy) also associated with colon polyps. Treatment: Surgical removal of the tumor, radiotherapy, or medical therapy. Common medications: Octreotide (Sandostatin) – usually for residual GH after surgery. SQ 3x/day or IM in long acting Q4weeks. ORAL med: bromocriptine (Parlodel) – less effective but cheaper and can be taken PO. Assessment of: Labs: hGH, prior to the hGH test the patient should fast, and the test should be drawn at 8.00 a.m. b/c of circadian cycle. Normally (hGH ) MEN: < 5 ng/mL WOMEN: <10 ng/mL Acromegaly = hGH > 10 ng/mL . The glucose suppression test: measuring GH following the admin of 100 g of glucose. Normally, GH secretion is lowered to less than 2 ng/mL. A result greater than 2 ng/mL is considered conclusive of a diagnosis of acromegaly. - Plain films will often show sella turcica enlargement due to a pituitary tumor. Thickening of the calvarium, and enlargement of the sinuses, jaw, and heel pads can also be seen on X-ray. MRI = show tumor location and size. Patient education: If Pt is hyperglycemic d/t hypersecretion of GH = diabetic management. Cardio (↑cholest, or HTN) tx needed. Teaching in prevention of complications of disease. 2. Cushing’s syndrome – Hypercortisolism is most often caused by excessive production and release of ACTH by a pituitary secreting adenoma. Commonly occurs in women 20-40 and are approximately 20% of the pituitary tumors. Signs and symptoms of: Many of the clinical manifestations of hypercortisolism = exaggerated action of cortisol, which affects glucose, protein, and fat metabolism. Bruising, poor wound healing, excess hair growth in females, HTN, edema of extremities, accumulation of fat in the face (moon face), voice changes, hyperlipidemia, dysrhythmias, emotional liability, irritability, depression, poor memory, euphoria, psychosis, suicidal tendencies, protein breakdown and muscle wasting, osteopenia, osteoporosis, renal calculi, polyuria, amenorrhea in females, decrease in libido, impotence, decrease in body hair (males), protruding abdomen, subclavicular fat pads (buffalo hump), hyperinsulinemia, Potassium and Sodium imbalances, and abnormal glucose tolerance test. Assessment: Fluid and electrolyte imbalances, sx of heart failure (diuretics, BP meds, cardiotonic meds). SOB, weakness (hypokalemia) – assist with ADL’s. Prevent infection (compromised immune sys) – watch for low grade temp. – Poor wound healing, opportunistic infections. Common treatment: No drugs are avail to successfully suppress pituitary ACTH secretion. Ketoconazole, metyrapone, and aminoglutethimide are expensive drugs, with limited success in treating Cushing’s. Treatment of choice is selective transsphenoidal resection with tumor removal to correct the hypercortisolism. Radiotherapy may be prescribed. In extreme cases, bilateral adrenalectomy has been done when all other therapies have failed with lifelong hormone replacement therapy. - For surgery: Packing of nasal passage for 24-48hrs – instruct deep breathing exercises thru mouth. Liquid diet, use toothettes for cleaning teeth. Neuro assessment Qhr. Monitor for ↑ICP, avoid straining. Risk for CSF leak – look for clear drainage/halo ring on drip pad under nose, will test + for glucose if CSF. If + = bedrest with HOB elevated. Normally leak will cease spontaneously. ↑Risk infection. Therefore, antibiotics are usually ordered. Monitor fluid status. Risk for SIADH, or diabetes insipidus. Patient education and support: Wt gain 25 -100 pounds, acne, excess body hair, redistribution of fat, and striae on the abdomen and breasts=Encourage the Pt to explore feelings. Prevent infection. Prevent fracture. 3. Hypothyroidism – Insufficient secretion of TH by thyroid gland, causing decreased metabolic rate and heat production, and various effects on body system Assessment, Common medications: thyroid hormone replacement: dessicated thyroid, thyroxine (Synthroid), or triiodothyronine (Cytomel). Give med in AM 1 hour b4 meal or 2 hrs after meal to facilitate absorption Pregnant and non-pregnant treatment Myxedema (a life-threatening crisis state of hypothyroidism): non-pitting edema in connective tissues throughout body, puffy face and tongue, severe metabolic disorders, hypothermia, cardiovascular collapse, and coma 4. Thyroid crisis (Hyperthyroidism) – A pt with hyperthyroidism is susceptible to a thyroid crisis. Often caused by increased medications, a thyroid crisis (thyroid storm) is a rare but often life-threatening emergency. Early identification is essential. Assessment: Infection, stress or emotional trauma, pregnancy, a comorbidity, or medications may precipitate it. Clinical manifestations: extremely high fever (>102), abdominal pain, nausea, vomiting, diarrhea, tremors, severe neurological signs and symptoms (e.g., restlessness, delirium/confusion, agitation, psychosis, and coma), and cardiovascular problems (Tachycardia, atrial fibrillation, heart failure, and angina). Most patients will have high systolic blood pressure with a wide pulse pressure. One of the earliest clues to the onset of a thyroid storm is high fever and diaphoresis that are out of proportion to an infection. possible seizure Interventions: Respiratory support should be provided immediately. Hemodynamic instability is a major priority. IV access is a priority to correct volume and electrolyte depletion and administer nutrition as indicated. Vasopressors to restore or maintain BP. May implement measures to treat heart failure (digoxin, and diuretics). Reduce fever immediately. A cooling blanket and the administration of acetaminophen as ordered is standard care. Adrenal insufficiency with the stress related to the thyroid storm = glucocorticoids such as hydrocortisone. Patient education: NO ASPIRIN. 5. Grave’s Disease – pronounced hyperthyroidism often associated with enlarged thyroid gland and exophthalmos; also called thyrotoxicosis. Signs of: . Neck goiter and exophthalmos (bulging eyes) are characteristic. Tachycardia, nervousness, insomnia, increased heat production, and weight loss. Cardiac problems: increased systolic blood pressure, a widened pulse pressure, and other dysrhythmias. Treatment: Antithyroid medications: Methimazole (Tapazole), Propylthiouracil 6. Inflammatory Immune Response – is a response that is composed of several body systems, which are constantly on alert to detect nonself and harmful intruders from the normal cells and proteins in the body. The immune system can remember a foreign agent and develop a heightened response during a subsequent exposure. When regulation of the immune response is controlled, the response is protective; however, when the immune response is exaggerated, the consequences can be dangerous. The purposes of this innate protective response are to control bleeding, remove waste products, limit infection, and promote healing. IIR responses cause local vasodilation to aid in delivering an increased bloodflow and to bring neutrophils, macro- phages (the major phagocytic cells of the immune system), and clotting factors to the damaged area. Cardinal signs of local reaction to an injury or infection as first described by Celsus, an early Roman physician: • Rubor (redness) due to vasodilation • Calor (heat) due to increased bloodflow to area • Tumor (swelling) due to release of fluids containing white blood cells and proteins to the insult site • Dolor (pain) due to swelling that stretches the surrounding tissues; pain alerts the patient to rest the affected area to assist prevention of further damage 7. Shock – Review all the material on different types of shock and clinical manifestations of each. Different types: The shock syndrome, or acute circulatory failure, can be classified according to etiology into three basic categories: hypovolemic, cardiogenic, and distributive. Sub-categories of distributive shock include neurogenic, anaphylactic, and septic. Causes of the different types: Progression from one stage to the other is dependent on the patient’s health status, duration of the insult, response to therapy, and the correction of the underlying cause. The end result is always the same; tissues fail to receive oxygen and nutrients, and are unable to eliminate waste products - Hypovolemic shock: an insufficient intravascular volume and low cardiac output; is initiated by various causes. Blood loss due to internal or external bleeding, fluid loss, injury or vomiting, diarrhea, severe dehydration, burns, surgery, ascites, or peritonitis. MANIFESTATIONS OF HYPOVOLEMIC SHOCK Tachycardia is a compensatory helps remove accumulating lactic acid. May result in cardiac arrhythmias and chest pain (inadequate filling of the cardiac arteries during diastole). Due to lack of tissue perfusion, the patient’s level of consciousness is altered. Pulse pressure narrows as the diastolic increases. Tachypnea and increase in depth of respirations (may gasp for breath). Decline in urine output. Skin pale, cool, delayed capillary refill. Jugular veins appear flat. Decreased cerebral perfusion and a change in LOC. Disoriented, confused, restless, anxious. Nursing Interventions: Minimize fluid loss. Large diameter catheter – Give Fluids (monitor FV overload), Oxygen, Meds. Observe for changes in Respirations, heart sounds, assess lung sounds, chest pain. (Risk of Secondary shock if given blood products = anaphylactic shock) Monitor lab results, I&O. Give pain meds. Position, the patient with legs elevated, trunk flat, and head and shoulders above the chest (modified Trendelenburg position). Monitor s/s infection (IV). - Cardiogenic: a diminished cardiac output is due to loss of left ventricular pump function. It results in tissue hypoxia even when fluid volume is adequate. MANIFESTATIONS OF CARDIOGENIC SHOCK Hypotension SBP < 90 mm Hg. Heart rate > 100 beats per minute. Weak thready pulse, Diminished heart sounds. Change in level of consciousness (LOC). Cool, pale, moist skin Urine output less than 30 mL/hour Chest pain. Dysrhythmias. Tachypnea. Crackle breath sounds. ↓cardiac output. Nursing Interventions: Fluids, Oxygen, Meds. Observe for changes in Respirations, heart sounds, assess lung sounds, chest pain. Monitor lab results, I&O. Give pain meds to diminish myocardial O2 consumption). Calm environment, education to reduce anxiety. Limit activities to preserve O2. Give pain meds - Distributive shock: • Anaphylactic shock: due to hypersensitivity to a foreign substance (antigen/antibody reaction). • Neurogenic shock: due to disruption of outflow of sympathetic nervous system response—often due to tissue damage in the spinal cord pathway. • Septic shock: result of overwhelming infection. Phases of shock: Initial - -Decreased CO, impaired tissue perfusion, elevated lactic acid. No clinical s/sx except for elevated lactic acid. Compensatory - - Body is trying to bring us back to homeostasis. - Neural changes: SNS activated (epi/norepi activated) - Hormonal changes: (ACTH is released, kidneys affected, K+/Na+ affected) - Chemical compensation (leads to respiratory alkalosis!) Progressive - Unable to continue compensatory phase. Multi organ dysfunction syndrome (MODS). Organ hypoperfusion Refractory - - Death is inevitable ASSESSMENT AND CARE OF SHOCK SYNDROME Clinical findings correlated with organs compromised by inadequate oxygen. Regardless of the type of shock, it leads to a SBP of less than 90 mm Hg and the narrowing of pulse pressure that is inadequate to meet the tissue needs. (SBP may be elevated initially.) First: Position pt. to maximize o2 return to the brain (admin O2), monitor pulse & resp rates, keep normothermic. Initial Compensatory Stage: Body mechanisms are triggered to maintain adequate BP and tissue perfusion. Subtle changes in baseline may be observed. Monitor heart rate and pulse, blood pressure, central venous pressure (CVP), respiratory rate, core, and peripheral temperature, and urinary output. Pulse oximetry may also be performed. Arterial gases are monitored for accurate assessment. Blood sampling for urea and electrolyte levels, full blood count, and glucose levels may also be performed. Elevated glucose levels are present with release of stress hormones such as cortisol. Progressive Stage: Compensating mechanisms begin to fail. Symptoms are evident of inadequate organ perfusion. A full assessment should be done to identify any signs of blood or fluid loss, fluid shift as in ascites, infection, vomiting, or inadequate fluid intake. Decompensated Stage: Failure of compensating mechanisms. No response to treatment. There is a great risk of cardiac arrest. A rising serum lactate is an indicator of inadequate tissue perfusion due to metabolic acidosis. Low arterial oxygen con- tent, chest pain, cardiac dysrhythmias, altered level of consciousness (LOC), or low urinary output. MAPB cannot be maintained without assistance. 8. Angina – Assessment, Different types, Treatment, Patient education, Causes 9. Myocardial Infarction – Assessment, Clinical manifestations, Common medications, Side effects of common medications, Patient education, Phases of rehabilitation 10. Coronary Artery Disease – Modifiable risk factors, Assessment, Common treatment, Prevention 11. Cardiac Angiograms- Coronary angiogram, or heart catheterization, is an invasive procedure that is considered the gold standard for diagnosis of CAD. How is it used: A right-sided heart catheterization involves a catheter placed through a vein and advanced to the heart. Hemodynamic pressures measured and the tricuspid and pulmonary valve function are evaluated. A left-sided heart catheterization involves a catheter placed through an artery and advanced to coronary arteries to visualize the anatomy. The bloodflow of the coronary arteries and the function of the mitral and aortic valves and the left ventricle are evaluated. Why is it used: This procedure directly visualizes the coronary artery anatomy and assesses hemodynamic parameters and ventricular function. Fluoroscopic visualization of the coronary arteries defines the location and severity of blockages. The ventriculogram identifies areas of wall motion and contractility abnormalities. Coronary angiogram is the only definitive test to diagnose coronary spasm or variant angina. Results of this study are used to determine treatment options and prognosis. 12. Arteriovenous shunt – Ateriovenous Fistula (AVF) • Confirm patency and the presence of thrill (palpated pulsation) and bruit (whooshing sound heard with a stethoscope) along the course of the AVF. • Practice nephrology precautions to prevent thrombosis and infection. This includes no blood pressure measurement, IV accesses, or laboratory blood draws on the affected extremity. • Teach the patient to avoid constrictive clothing and to check fistula patency daily. The patient should report absence of thrill or bruit promptly. • Teach the patient to handle posttreatment bleeding at the cannula site: apply direct pressure for several minutes to the control bleeding, apply a dry dressing, and call the health care provider as appropriate. 13. Disseminated intravascular coagulation – This condition is a disorder of the clotting cascade. It results in depletion of clotting factors in the blood and occurs when the body’s blood clotting mechanisms are activated through- out the body instead of being localized to an area of injury. Small blood clots form throughout the body, and eventually the blood clotting factors are used up and not available to form clots at sites of real tissue injury. Clot dissolving mechanisms are also increased. Some causes of DIC: (a) complications of obstetrics in which uterine material with tissue factor activity gains access to the mater- nal circulation such as in abruptio placenta; (b) infection with gram-negative bacteria, which secrete an endotoxin that induces the generation of tissue factor; (c) malignan- cies, particularly adenocarcinoma of the pancreas or prostate as well as promyelocytic leukemia; and (d) head trauma Tests to identify DIC: fibrinogen, serum fibrinogen, prothrombin time (PT), partial thromboplastin time (PTT), platelet count, and thrombin time test The goal is to determine the underlying cause of DIC and provide treatment for that identified cause. Replacement therapy of the coagulation factors is achieved by transfusion of fresh frozen plasma. Cryoprecipitates may also be used if fibrinogen is significantly low. Heparin, a medication used to prevent thrombosis, is sometimes used in combination with replacement therapy. The underlying disease that causes the disorder will usually predict the probable outcome. Complications of DIC include severe bleeding, stroke, and lack of blood flow to arms, legs, or organ 14. Fibrinolytic Therapy –Stops infarction process. Fibrinolytic therapy must be given as soon as possible, ideally within the first hour of onset of symptoms and preferably within the first six hours of onset of symptoms. Common medications: alteplase (Activase), reteplase (Retavase), and tenecteplase (TNKase). Patient monitoring: may have a minor or major bleeding episode as a consequence of therapy. Prior to administration of fibrinolytics, the nurse screens patients for bleeding risks, obtains baseline vital signs and physical assessment. Monitor patient for resolu- tion or recurrence of chest pain, resolution or return of ST abnormalities, and early peak of cardiac biomarkers signifying successful reperfusion. Assess for evidence of bleeding. Patient education: Provide simple explanations for the patient and family and offer realistic reassurances. 15. Pheochromocytoma –is a tumor of the adrenal gland that secretes catecholamines. The catecholamines (epinephrine and norepinephrine) are often secreted in large amounts and produce severe effects on the heart and vascular system including hypertension, myocardial infarction, and cerebrovascular hemorrhage. Assessment: Monitoring the patient’s vital signs along with neurovascular, cardiac, and respiratory assessment is a priority. Pt’s may experience orthostatic hypotension, instruct to rise slowly and recognize symptoms to avoid falls. **Consider pheochromocytoma when the pt has severe HTN and suspicious symptoms such as palpitations, diaphoresis, headache lasting minutes to hours, and chest or abdominal pain that is not explainable. More than one third of patients who have them die from a stroke or cardiac arrhythmia prior to diagnosis. Symptoms of: Severe headache, palpitations, and profuse sweating are the most common symptoms. In addition, patients can have chest discomfort, anxiety, visual disturbances, constipation, weight loss, and cold hands or feet. Treatment 16. Pyelonephritis – infection of upper urinary tract. If untreated it can extend to tubules of nephron creating potential for renal failure. Common risk factors: Urinary retention, Lower UTI, abx resistance, some drugs that may cause necrosis of renal papillae leading to sloughed papillae = blockage = pyelonephritis. Pregnancy, urinary tract obstruction, congenital malformation, urinary tract trauma, calculi, and diabetes Assessment of: Flank pain (costovertebral angle), fever, chills, painful urination, frequency, nocturia, muscle tenderness, malaise. Obtain UA/UC. Urine culture: hematuria, pyuria, bacteriuria, leukocyte casts, leukocytosis. CT for obstructive etiology (unresponsive to abx for 72hrs). US when CT contraindicated (such as pregnancy). Common treatment: Treat UTI. Antimicrobials, urinary antiseptics, and analgesics for pain Interventions: Hand washing (prevent nosocomial infection). Avoid catheterization, and promote early removal of caths. Strict aseptic tech when inserting cath. Monitor VS and Fluid balance. Ensure hydration (I&O) – Encourage 2L a day. Labs: Electrolytes, WBC, BUN, and creatinine. Patient education: Prevent further infection – complete full course of abx (prevent drug resistance, and maintain therapeutic drug level) Monitor UO and notify care provider if less than 1500 mL/day. Methods to prevent chronic renal insufficiency. Take high-calorie, low-protein diet if oliguria is present Hygiene to prevent further infections. Encourage bedrest during acute stage 17. Kidney transplant – Medications: immunosuppressant drugs, analgesics Interventions: Wear surgical mask when in Pt’s room. Perform baseline and ongoing postoperative assessments (VS, LOC, status of dressing). Encourage freq position changes, coughing and deep breathing, and early ambulation. Patient monitoring: signs of tissue rejection: fever; redness, tenderness, and swelling at surgical site; elevated WBC count; decreased UO with increased proteinuria, sudden wt gain; HTN; ↑BUN/ creatinine Monitor UO closely; report output less than 100mL/hour (↓ UO may =thrombus formation at renal artery anastomosis site) Expect blood-tinged urine for several days; irrigate catheter as ordered (strict aseptic tech) - With a living donor transplant, urine flow should begin immediately after revascularization and connection of ureter to client’s bladder; with a cadaver transplant, expect anuria (urine output less than 100 mL in 24 hrs) for 2 days to 2 weeks, client will need dialysis during this period Education: Home care for client: I&O; notify physician if UO < 600 mL/24-hour period. weigh self at least twice weekly. Drink at least 1–2 liters of fluid daily. Report signs of rejection: redness, warmth, tenderness, or swelling over kidney; fever; decreased UO; elevated BP (obtain and use home BP measuring device) Avoid crowds and persons with known infections for 3 months after surgery Practice regular, moderate exercise, but avoid heavy lifting or contact sports for at least 3 months; use shoulder but not lap-style seat belts. Wait 6 weeks b4 sex 18. Rhabdomyolysis – Muscle destruction (cell death – bkd of striated muscle) release of cellular o=phosphorus & release of myoglobin to urine. This is a MAJOR cause of acute renal failure! Causes: Direct muscle injury, drugs, toxins, infection, excessive exercise, DKA, hypothermia, severe burns, ischemia, electrolyte imbalances, immune disorders Assessment of: What Pt was doing prior to onset of Sx. (Running long distance without hydration). ↑ creatinine kinase (CK-MM), which confirm muscle injury. CK-MM = specific diagnostic serum marker for rhabdomyolysis. Urine = myoglobin, acidic pH, and have RBC’s. ↑BUN & creatinine ratio; and ↑uric acid levels. Complications of: hyperkalemia, which is the most life-threatening consequence of muscle necrosis. Hyperphosphatemia and hypocalcemia. Compartment syndrome (fasciotomy – keep from infection) Hyperphosphatemia: serum phosphorus level of greater than 4.5 mg/dL (normal range 2.5–4.5 mg/dL – Monitor for ECG changes and conduction disturbance, tachycardia. Paresthesias (especially lips and fingertips), muscle spasms, and tetany (positive Chvostek and Trousseau signs) from decreased Ca++ that accompanies increased phosphorus Compartment syndrome may develop with extensive muscle damage. The mechanism of injury is acute swelling in a muscular compartment. Rigid, nonexpanding fascia surrounds each muscle group, forming a compartment for the muscle. Fascia is rigid and unable to accommodate swelling. Increased pressure within the constrictive compartment causes further muscle necrosis, vascular constriction, and nerve damage. This can occur immediately or may be delayed for up to three days. The health care team must monitor for development of or increase in neurovascular deficit. This presents a surgical emergency to relieve the compartment pressure before permanent damage occurs. The treatment of choice is fasciotomy (incision through a fibrous layer that separates muscles) with closure following resolution of swelling. Treatment of: minimize complications & intervene effectively as complications of muscle necrosis occur. Monitoring and patient education 19. Renal issues – Renal failure (acute and chronic) - Common causes: Acute: Prerenal (↓Blood flow to kidney – dehydration), Intrarenal (tubular necrosis from nephrotoxic drugs), Postrenal (obstruction to urine flow). Chronic: progressive and irreversible decline in renal fx. Diabetes and HTN main causes. - Common issues: Acute: Fluid overload & pulmonary edema in a few hours. Hypokalemia. HTN - Common treatments: Acute: Potassium: replacement in high output failure and restriction in low output failure. Maintain BP/admin BP meds. (renin secreted activating angiotensin system = ↑BP) - Assessment: Acute - Common lab values: Acute: diagnostic tests for ARF/ AKI: plain abdominal X-ray of the kidneys, ureters and bladder (KUB) to determine calculi or renal vascular calcification; a renal ultrasound to identify renal vascular blood flow and to rule out obstruction; and a bladder scan to detect urinary retention. In addition, laboratory studies may include several blood chemistry tests (e.g., BUN, serum creatinine), a basic metabolic panel (BMP), and a CBC 20. Acute Respiratory Distress Syndrome (ARDS) – The alveoli fill with fluid, thus minimizing or prohibiting gas exchange. It is a sudden progressive pulmonary disorder that is manifested by severe dyspnea, hypoxemia, and diffuse bilateral infiltrates. Assessment Causes: Risk factors include direct injury from aspiration, near-drowning, inhalation of smoke and other toxic gases, pneumonia, radiation, drug toxicity, and severe chest trauma. Indirect injuries include sepsis, pneumonia, cardiopulmonary bypass (CPB), embolism, severe pancreatitis, SIRS, DIC, and shock states. Treatment: Treat underlying cause, promote gas exchange and O2 therapy, prevent complications. Intubation and mechanical vent. PEEP oxygenation. [Show More]
Last updated: 1 year ago
Preview 1 out of 7 pages
Reviews( 0 )
Document information
Connected school, study & course
About the document
Uploaded On
May 13, 2020
Number of pages
7
Written in
Additional information
This document has been written for:
Uploaded
May 13, 2020
Downloads
0
Views
60



.png)
.png)
How Do Geographically Dispersed Teams Collaborate Effectively Paper.png)