*NURSING > HESI MED SURG > 2020 HESI Medical surgical LPNPN (nursing v1) | Keiser University - NURSING 112023 | DETAILED SOLUTI (All)
2020 HESI Medical surgical LPNPN (nursing v1) | Keiser University - NURSING 112023 | DETAILED SOLUTION
Document Content and Description Below
2020 HESI Medical-Surgical LPN/PN Nursing V1 Question 1 The nurse is providing care for a patient who is unhappy with the health care provider’s care. The patient signs the Against Medical Advic... e (AMA) form and leaves the hospital against medical advice. What should the nurse include in the documentation of this event in the patient’s medical record or on the AMA form? 1. Documentation that the patient was informed that he or she cannot come back to the hospital 2. Documentation that the patient was informed that he or she was leaving against medical advice 3. Documentation that the risks of leaving against medical advice were explained to the patient 4. Documentation of any discharge instructions given to the patient 5. Documentation indicating an incident report has been completed Rationale 1: It should be clearly documented that the patient was advised and understands that he or she can come back. Rationale 2: It should be clearly documented in the patient’s record and on the AMA form that the patient was advised that he or she was leaving against medical advice. Rationale 3: It should be clearly documented that the patient understands the risks of leaving against medical advice. Rationale 4: The AMA form includes the name of the person accompanying the patient and any discharge instructions given. Rationale 5: Facility policy may require that an incident report be completed, but it must not be referenced in the chart. The patient’s record is a legal document, so the nurse should never document that he or she filed an incident report. Question 2 A nurse documents this statement in a patient’s medical record: “2/25/–, 2235. At 2015 patient awoke suddenly and complained of shortness of air. Pulse oximetry reading was 82% on room air and audible wheezes could be heard.” This documentation meets which documentation guidelines? 1. Documentation is timely 2. Documentation is concise 3. Documentation is objective 4. Documentation includes date and time of entry 5. Documentation is complete and accurate Rationale 1: The nurse should document as soon as possible after an observation is made or care is provided. The entry was made in the patient’s medical record at least 2 hours after the patient complaint and should be labeled late entry. Rationale 2: This entry describes the situation fully but is concise. Rationale 3: The nurse describes factual events that can be seen, heard, smelled, or touched. It is important to be objective and avoid vague statements that are subjective. Rationale 4: Both the date and the time of the entry are documented. Rationale 5: The nurse should document only facts: what he or she can see, hear, and do. Question 3 A nurse documents the following in a patient’s medical record: “2/1/ , 1500. Patient appears weak and faint. Patient’s skin is moist and cool, vomited bright red blood with clots. Health care provider notified and order received to give 2 u of packed red blood cells if stat Hgb is < 8.0. Pain medication will be given.” This documentation meets which documentation principle? 1. Document objectively. 2. Do not document procedures in advance. 3. Use approved abbreviations. 4. Document changes in patient condition. Rationale 1: Documentation should be objective and avoid vague statements that are subjective. Only factual occurrences that can be seen, heard, smelled, or touched should be described. The use of the word “appears” is subjective and could be manipulated later should the treatment or judgment be challenged. Rationale 2: The nurse has documented that pain medication will be given. This is documenting in advance. Rationale 3: The Joint Commission has designated the inappropriateness of “u” as an abbreviation. “U” should be written out as “unit(s).” If unsure whether the abbreviation is correct, the nurse should spell out the word; “<” can be misinterpreted, so it should be spelled out as “less than.” Rationale 4: In general, employers as well as state, federal, and professional standards require documentation to include initial and ongoing assessments, any change in the patient’s condition, therapies given and patient response, patient teaching, and relevant statements by the patient. Question 4 A nursing unit has changed its documentation system to documenting by exception. How will this system save time? 1. It eliminates lengthy or repetitive documentation. 2. It allows flexibility and description in the documentation. 3. It allows the reader to easily locate information about a specific problem. 4. It allows for quick and easy retrieval of information. Rationale 1: Documenting by exception eliminates lengthy or repetitive documentation. Rationale 2: Flexible and descriptive documentation is an advantage of the narrative system. Rationale 3: PIE charting allows easy location of information about a specific problem. Rationale 4: The electronic health record allows for quick and easy retrieval of information. Question 5 A hospital is considering changing its documentation system to reduce the number of medication errors. Which system should the hospital investigate? 1. Problem, intervention, evaluation (PIE) system 2. Electronic medical record 3. Problem-oriented medical record 4. Narrative system Rationale 1: The PIE system consists of a list of the patient’s problems, interventions taken to alleviate the problems, and evaluation of the patient’s response to the interventions. This system does not have the specific benefit of reducing medication errors. Rationale 2: The electronic medical record decreases errors and allows for the reconciliation of the patient’s medications on admission, daily, and on discharge. Rationale 3: The five components of the problem-oriented medical record are baseline data, a problem list, a plan of care for each problem, multidisciplinary progress notes, and a discharge summary. This system does not have the specific benefit of reducing medication errors. Rationale 4: Narrative documentation does not have the specific benefit of reducing medication errors. Question 6 Which nursing activities are examples of independent functions of the nursing role? 1. Teaching a soon-to-be-discharged patient about the medication regimen that the health care provider has prescribed 2. Talking with the patient about his or her abilities to manage personal hygiene activities while in the usual state of health at home 3. Incorporating adaptive techniques into nursing care as recommended by occupational therapy 4. Administering analgesic medication ordered by the health care provider 5. Introducing oneself to, and interviewing, the patient to collect data about physical health status Rationale 1: Teaching the patient about medications prescribed by the health care provider is an interdependent activity. Rationale 2: This activity is part of the assessment process, which is an independent activity that nurses may perform, based on their education and skills. Rationale 3: Working in coordination with another health team member is an interdependent activity. Rationale 4: Administering medication prescribed by the health care provider is an example of a dependent activity. Rationale 5: These activities are included in assessment, which is an independent activity that nurses may perform, based on their education and skills. Question 7 The nurse is caring for a 70-year-old patient who was just admitted to an inpatient rehabilitation center. The patient had required total parenteral nutrition for several days, but recently resumed and is tolerating a regular diet. She has another 4 days left in a course of intravenous antibiotics to complete treatment of a positive central line culture. Which nursing action, required in the care of this patient, is considered a dependent role function? 1. Requesting that the health care provider order a consult because the patient states that her dentures no longer fit properly and she has trouble chewing 2. Asking the nursing assistant to demonstrate to the patient how to operate the call system 3. Interviewing the patient to assess whether she needs assistance with getting out of bed 4. Administering the antibiotics prescribed by the health care provider Rationale 1: Assessing that the patient has a need that requires further assessment by other team members and communicating that need to the appropriate team member is an example of an interdependent activity. Rationale 2: This is an independent activity that nurses may perform or delegate, based on their and the delegate’s education and skills. Rationale 3: Assessment is an independent activity that nurses may perform, based on their education and skills. Rationale 4: Dependent activities are those prescribed by the health care provider and carried out by the nurse. Question 8 When asking a patient if a pain medication provided a few hours ago has been effective, the nurse is performing which step of the nursing process? 1. Planning 2. Implementation 3. Evaluation 4. Assessment Rationale 1: Planning consists of prioritizing among the chosen nursing diagnoses and determining interventions to move the patient to optimal health. Rationale 2: Implementation is the actual “doing” step of the nursing process. In this case, implementation occurred when the medication was administered. Rationale 3: Evaluation focuses on a patient’s behavioral changes and compares them with the criteria stated in the objectives. It consists of both the patient’s status and the effectiveness of the nursing care. Both must be evaluated continuously, with the care plan modified as needed. Rationale 4: Assessment comprises examining the patient and identifying cues, collecting and analyzing data, and reaching conclusions. In this situation, assessment occurred when the nurse identified that the patient was in pain. Question 9 The nursing instructor knows that further education is needed when a student makes which statement? 1. “Assessment precedes nursing diagnosis and outcome identification.” 2. “Planning follows nursing diagnosis and outcome identification and precedes implementation.” 3. “Evaluation follows implementation and precedes planning.” 4. “Planning follows assessment and precedes evaluation.” Rationale 1: The correct order is assessment, diagnosis, planning, implementation, and evaluation. Rationale 2: The correct order is assessment, diagnosis, planning, implementation, and evaluation. Rationale 3: The correct order is assessment, diagnosis, planning, implementation, and evaluation. Rationale 4: The correct order is assessment, diagnosis, planning, implementation, and evaluation. Question 10 A 16-year-old patient has been admitted for treatment of presumptive pelvic inflammatory disease. The patient’s hygiene is poor and she reports living “on the street” for a year. She is febrile and tachycardic and reports pain as 10 on the 1-to-10 scale. The nurse identifies Acute Pain as the priority nursing diagnosis. Which outcome statement is appropriate? 1. The patient’s comfort will be achieved and maintained. 2. The patient will be discharged to a safe living environment. 3. The patient will be reunited with her parents. 4. The patient’s infection will be eradicated. Rationale 1: Achieving and maintaining comfort addresses the nursing diagnosis of acute pain related to possible pelvic inflammatory disease identified by the nurse. Rationale 2: The patient’s living environment is of concern but is not the correct outcome for the priority nursing diagnosis. Rationale 3: Reuniting the patient with her parents may not be a desired goal for this patient. It also does not match the nursing diagnosis chosen. Rationale 4: Eradication of the infection is a desired outcome but does not match the chosen nursing diagnosis. Question 11 While assessing a female patient from the Middle East, the nurse observes that the patient makes no eye contact and answers questions by nodding or with only a few words. The nurse’s entry in the patient’s record states that the patient “appears to be frightened.” This isan example of which factor associated with assessment? 1. Personal interpretation 2. Subjective data 3. Nursing diagnosis 4. Objective data Rationale 1: This is the nurse’s personal interpretation of the patient’s behavior. It has not been validated with the patient. These behaviors may indicate a number of possibilities such as physical, mental, and emotional status or cultural and social norms. Rationale 2: A direct quote from the patient would be subjective data. Rationale 3: This statement does not meet the criteria for a nursing diagnosis. Rationale 4: A description of the patient’s behavior such as “makes no eye contact” would be objective data. Question 12 The patient tells the nurse that everything “tastes funny” since starting a new medication, making eating unpleasant. The nurse has given this medication to other patients and has not heard this complaint from any of them. The nurse checks the drug reference again to learn whether this is a known side effect of the medication and reads that it is. This information may be helpful in making a nursing diagnosis and determining how best to address this problem. Which data from this scenario is considered subjective? 1. The nurse rechecks the drug reference about known side effects of the medication. 2. The patient tells the nurse that everything “tastes funny.” 3. The nurse reads that this medication can cause a metallic taste in some patients. 4. Other patients who have taken this medication have never reported this side effect to the nurse. Rationale 1: Rechecking the drug reference is an example of obtaining factual information about the medication, not data about the patient. Rationale 2: The statement by the patient is subjective data because it reflects something that only the patient, not the nurse, can perceive. Rationale 3: That this medication can cause a metallic taste is factual information about the medication, not data about the patient. Rationale 4: The nurse’s prior experience with this medication is not data about the patient. Question 13 Which statement represents a nursing diagnosis? 1. High risk for delayed maternal-infant bonding due to maternal-infant separation 2. Crohn’s disease 3. Hypertension 4. Appendicitis Rationale 1: This is an example of a nursing diagnosis. The statement indicates a clinical judgment that this new mother-baby couplet is at greater risk of experiencing a delay in bonding than other mother-baby couplets. Rationale 2: Crohn’s disease is a medical diagnosis. Rationale 3: Hypertension is a collaborative problem. Rationale 4: Appendicitis is a medical diagnosis. Question 14 Which statements reflect collaborative problems? 1. Knowledge deficit related to infant safety as evidenced by mother leaving crib rail down 2. Sleep apnea 3. Neonatal abstinence syndrome 4. Gestational diabetes 5. Sleep pattern disturbance related to hospital environment and routines Rationale 1: The nurse can diagnose this knowledge deficit and use independent nursing interventions to address the problem. This is a nursing diagnosis. Rationale 2: Sleep apnea is a medical diagnosis and therefore a collaborative problem. Rationale 3: Neonatal abstinence syndrome is a medical diagnosis and therefore a collaborative problem. Rationale 4: Gestational diabetes is a medical diagnosis and therefore a collaborative problem. Rationale 5: The nurse can diagnose that a patient has disturbed sleep and can intervene to reduce noise and other disturbances in the environment. This is a nursing diagnosis. Question 15 The nurse is using critical thinking to better understand a patient. The nurse is working in which part of the nursing process? 1. Implementation 2. Nursing diagnosis and outcome identification 3. Assessment 4. Planning Rationale 1: Using critical thinking to reduce the risk of undesirable results is part of implementation. Rationale 2: Using critical thinking to identify actual and potential problems is associated with the diagnostic step of the nursing process. Rationale 3: The goal of assessment is to learn as much as possible about the patient within the context of the nurse-patient relationship. One characteristic of the nurse-patient relationship is the nurse’s continuous focus on better understanding of the patient. Rationale 4: Using critical thinking to make decisions about an action is associated with planning. Question 16 Which aspect of critical thinking would the nurse use when making a nursing diagnosis? 1. Making decisions about an action 2. Identifying potential and actual problems 3. Increasing the likelihood of obtaining good results 4. Getting a better understanding of someone else Rationale 1: Making decisions about an action is associated with planning. Rationale 2: Identifying potential and actual problems is analogous to identifying nursing diagnoses, potential and actual. Rationale 3: Increasing the likelihood of obtaining good results is related to evaluation. Rationale 4: Getting a better understanding of someone else is related to assessment. Question 17 Critical thinking empowers the nurse to recognize important situational cues and respond quickly to adapt interventions, optimizing their effectiveness and the likelihood of a good outcome. What is true about this aspect of critical thinking? 1. This method of thinking is similar to the way that a skilled nurse uses continued assessment and evaluation to adapt the patient’s care plan. 2. Using this method of critical thinking produces only one correct solution to a problem. 3. The need to change the plan of care indicates that critical thinking and the nursing process are not compatible. 4. The statement proves that critical thinking is another term for the nursing process. Rationale 1: The nurse uses critical thinking to continually assess the patient and evaluate response to interventions, then making changes to the plan of care to improve outcomes. Rationale 2: Critical thinking does not imply that there is only one correct answer to a problem; rather it demands that the nurse looks at information related to the question from many different viewpoints to identify the next step. Rationale 3: Thinking critically about patient response to interventions encourages the nurse to change portions of the care plan that are not effective. Rationale 4: Critical thinking and the nursing process are not synonymous; critical thinking enhances and complements the nursing process but is not identical to it. Question 18 The nurse is using the Kardex to plan a patient’s care. What information would the nurse expect to find in this document? 1. Nursing notes from the previous shift 2. Schedule of diagnostic tests 3. Level of activity 4. Diet 5. IV therapy Rationale 1: Nursing notes are not found on the Kardex. Rationale 2: The patient’s schedule for diagnostic testing is recorded on the Kardex. Rationale 3: The patient’s level of activity is recorded on the Kardex. Rationale 4: The diet prescribed for the patient is recorded on the Kardex. Rationale 5: The fluid, additives, and rate of IV therapy are recorded on the Kardex. Question 19 According to the Health Insurance Portability and Accountability Act (HIPAA), which persons have legal access to the patient’s health record? 1. The patient 2. Any nurses working on the unit where the patient is hospitalized 3. Any physician who has credentials to admit patients to the hospital 4. The respiratory therapist who is providing inhalation therapy for the patient 5. The nuclear medicine technician who provided care during the patient’s last hospitalization Correct Answer: 1,4 Rationale 1: The information in the record belongs to the patient, who has the legal right to review it at any time. Rationale 2: The only nurses who have the legal right to review the record are the nurses involved with the patient’s care. Rationale 3: The only physicians who have the legal right to review the record are the physicians involved in the patient’s care. Rationale 4: The respiratory therapist who is involved in the patient’s care has the legal right to review the patient’s chart. Rationale 5: If the technician is not involved in caring for the patient on this admission, he or she has no legal right to review the chart. Question 20 During a routine breast examination of a patient, the nurse notes a small amount of nipple discharge. What nursing actions are indicated? 1. Tell the patient she may have cancer. 2. Send the specimen to the lab. 3. Ask the patient if she has noticed discharge before. 4. Collect a specimen on a slide. 5. Document the finding. Rationale 1: Telling the patient she has cancer is inappropriate; discharge is not always a sign of cancer. Rationale 2: The nipple drainage would be sent to the lab for analysis. Rationale 3: The nurse would question if this discharge has occurred before and when it began. Rationale 4: The drainage should be collected on a specimen slide. Rationale 5: The nurse would document the finding so that future comparisons can be made if the drainage continues. Question 21 During a routine pelvic examination, the nurse instructs the patient to bear down. The nurse explains that this motion makes it easier to assess for which conditions? 1. Rectoceles 2. Prolapsed uterus 3. Vaginal tumors 4. Ovarian cysts 5. Cystoceles Rationale 1: Rectocele, or relaxation of the posterior vaginal wall over the rectum, is assessed by asking the patient to bear down so that the health care provider can determine the presence of the structures through the vagina. Rationale 2: Prolapsed uterus, or the protrusion of the uterus into the vaginal wall, is assessed by asking the patient to bear down so that the health care provider can determine the presence of the structures through the vagina. Rationale 3: Vaginal tumors may be detected by visual inspection of the pelvis through a speculum device. Rationale 4: Ovarian cysts are palpated manually, and the patient does not have to bear down to determine their presence. Rationale 5: Cystocele, or relaxation of the anterior vaginal wall under the urinary bladder, is assessed by asking the patient to bear down so that the health care provider can determine the presence of the structures through the vagina. Question 22 The nurse is instructing a female patient about changes in sexual functioning that may result from the aging process. Which nursing diagnoses would the nurse incorporate into the plan of care for this patient regarding sexual intercourse? 1. Risk for Injury 2. Risk for Infection 3. Impaired Skin Integrity 4. Altered Tissue Perfusion 5. Alteration in Comfort Rationale 1: The patient could be at risk of injury due to thinning vaginal tissues. Rationale 2: With intercourse, the vaginal tissue may tear, and infection of the disrupted tissue could result. Rationale 3: Impaired Skin Integrity may result because of the thinning of the vaginal mucosa and loss of adipose tissue. Rationale 4: The aging process does not reduce the perfusion of the vaginal mucosa. Rationale 5: Intercourse may be painful because of the estrogen loss and drying of the vaginal mucosa. Question 23 A female patient who is experiencing hot flashes during menopause asks the nurse how long they will last. Which information should the nurse provide? 1. Hot flashes do not occur after the first year of menopause. 2. Hot flashes usually occur once a month. 3. The patient may have hot flashes for up to 5 years. 4. Hot flashes generally disappear after the first 2 years of menopause. Correct Answer: 3 Rationale 1: Hot flashes are unpredictable and may last longer than 1 year. Rationale 2: There is no indication that hot flashes occur only once a month. Rationale 3: Hot flashes are unpredictable and may last up to 5 years, especially if the patient is not taking hormone replacement therapy. Rationale 4: Hot flashes may last longer than 2 years. Question 24 A young adult male asks the nurse about the recommended frequency of testicular self- exams. How should the nurse respond? 1. “The more frequently exams are performed, the more beneficial they are.” 2. “You should have been taught to self-examine starting at age 12.” 3. “Not all experts believe that testicular self-examination is necessary or beneficial for young men.” 4. “It is essential that you perform this exam each month.” Correct Answer: 3 Rationale 1: Guidelines do not indicate that testicular self-exams are beneficial the more they are performed. Rationale 2: There is no indication that a 12-year-old should be taught testicular self- examination. Rationale 3: Testicular self-exams for adolescents and young men have been shown to cause more harm than benefit, according to the United States Preventive Service Task Force (USPSTF). USPSTF guidelines state that routine exams should not be performed. Rationale 4: Not all experts believe that testicular exams are necessary for adolescents and young men. Question 25 A 20-year-old female asks the nurse when she should begin having pelvic examinations. Which question should the nurse ask before responding? 1. “Are you on any medications?” 2. “Do you have a boyfriend?” 3. “Are you sexually active?” 4. “Are you asking because you think you are pregnant?” Correct Answer: 3 Rationale 1: Asking about medications is too broad a question and does not give the nurse information about the patient’s sexual practices. Rationale 2: Having a boyfriend does not always indicate sexual activity. Rationale 3: The United States Preventive Services Task Force (USPSTF) recommends that pelvic examinations begin about 3 years after the initiation of sexual intercourse but no later than 21 years of age. Rationale 4: Pregnancy is a reason for a pelvic examination, but it is not the only reason. The nurse should also not assume that the patient may be pregnant. Question 26 The patient asks why the nurse is asking questions about her mother’s obstetrical history. Which rationale for this questioning should the nurse provide? 1. “If your mother smoked while she was pregnant with you, your risk of lung cancer is higher.” 2. “Use of medications to prevent miscarriage may have an impact on your health.” 3. “The government wants to know for a genetic study.” 4. “If your mother had bleeding after delivery, you should avoid aspirin if you become pregnant.” Correct Answer: 2 Rationale 1: There is no correlation between smoking during pregnancy and the development of lung cancer in the child. Rationale 2: Daughters of women who took diethylstilbesterol (DES) are at higher risk of developing cancer of the vagina and cervix. Rationale 3: This is not a reason to collect this information. Rationale 4: All pregnant women should avoid aspirin. There is no correlation between their mothers’ obstetric history and the need to avoid aspirin. Question 27 Which statement by a patient offers the nurse information about moliminal symptoms? 1. “I have headaches if I don’t eat regularly.” 2. “When I was pregnant, my feet and ankles were swollen every day.” 3. “My last boyfriend gave me hepatitis.” 4. “I get terrible cramps with my periods.” Correct Answer: 4 Rationale 1: Headaches that occur when meals are missed may be due to hypoglycemia. This is not a moliminal symptom. Rationale 2: Swelling of the feet and ankles during pregnancy is not a moliminal symptom. Rationale 3: Hepatitis is not associated with moliminal symptoms. Rationale 4: Symptoms associated with menses are moliminal symptoms. Question 28 On assessment the nurse notes that a patient’s urinary opening is on the ventral side of the penis. How should the nurse document this finding? 1. Hypospadias 2. Hydrocele 3. Cryptorchidism 4. Varicocele Correct Answer: 1 Rationale 1: In hypospadias, the urinary opening is on the ventral or bottom side of the penis. Rationale 2: A hydrocele is swelling due to fluid accumulation in the scrotum. Rationale 3: Cryptorchidism is the presence of an undescended testicle. Rationale 4: Varicocele is varicosities of the veins of the scrotum. Question 29 Which precautions should the nurse conducting an assessment of the reproductive system take to avoid the cremasteric reflex? 1. Ask the patient to cough during the exam for inguinal hernia. 2. Ask the patient to breathe in slowly through the nose and out through the mouth. 3. Conduct the examination in a warm room. 4. Lubricate the finger used for the prostate exam. Correct Answer: 3 Rationale 1: Coughing during the exam for inguinal hernia intensifies the bulging. This is not the cremasteric reflex. Rationale 2: Slow breathing does not eliminate the cremasteric reflex. Rationale 3: The cremasteric reflex, in which the testicles rise in the scrotum to the abdominal cavity, can be reduced by conducting the exam in a warm room. Rationale 4: The cremasteric reflex is not related to the prostate exam. Question 30 During assessment, the nurse notes a third nipple about 4 inches below the patient’s costal margin. What nursing action is indicated? 1. Ask the patient when this nipple appeared. 2. Document this normal variant. 3. Discuss the finding with the health care provider because these nipples are commonly malignant. 4. Look for additional nipples on the patient’s back. Correct Answer: 2 Rationale 1: Patients are born with this condition. Rationale 2: Supernumerary nipples are normal variants but should be documented in the medical record. Rationale 3: This is a benign condition. Rationale 4: These extra nipples appear down the “milk lines” that run from the axilla across the nipple and down the abdomen to the groin. They are not found on the back. Question 31 The patient has respiratory difficulty due to changes in anatomic dead space. The nurse plans interventions based on changes in which physiological process? 1. Beginning of the gas exchange process 2. Neutralizing the air 3. Filtering the air 4. Separating the air Correct Answer: 3 Rationale 1: The anatomical dead space includes the structures from the nose to the terminal bronchioles. Air flows through the anatomical dead space, but these structures do not participate in gas exchange. Rationale 2: The anatomical dead space includes the structures from the nose to the terminal bronchioles. Air flows through this space, but it is not neutralized. Rationale 3: The trachea is part of the anatomical dead space. It traps particulate matter to keep it from entering the lungs. Rationale 4: The anatomical dead space includes the structures from the nose to the terminal bronchioles. The air is not separated in these structures. Question 32 During an assessment, a patient begins to cough. How would the nurse evaluate this finding? 1. The patient has a cold. 2. The patient is nervous. 3. Something other than air was entering the larynx. 4. The patient is not fully conscious. Correct Answer: 3 Rationale 1: A cough does not indicate the presence of a cold. Additional assessment would be necessary. Rationale 2: A cough is not sufficient assessment data to determine that a patient is nervous. Rationale 3: If anything other than air enters the larynx, a cough reflex expels the foreign substance before it can enter the lungs. Rationale 4: The protective reflex of coughing may not be present if the person is unconscious. A cough is not enough data to determine level of consciousness. Question 33 A patient is diagnosed with a low iron count. The nurse would be alert for which finding associated with this condition? 1. Increased carbon dioxide in the blood 2. Nausea 3. Anxiety 4. Poor tissue oxygenation Correct Answer: 4 Rationale 1: Low iron would not increase carbon dioxide levels in the blood. Rationale 2: Nausea is not generally associated with low iron count. Rationale 3: Anxiety is not generally associated with low iron count. Rationale 4: Oxygen is carried in the blood either bound to hemoglobin or dissolved in the plasma. Oxygen is not very soluble in water, so almost all oxygen that enters the blood from the respiratory system is carried to the cells of the body by hemoglobin. Question 34 During the palpation of a patient’s chest for expansion, the nurse notices a decrease in expansion of the right side. This finding is consistent with which condition? 1. Emphysema 2. Pneumothorax 3. Flail chest 4. Heart failure 5. Influenza Correct Answer: 2,3 Rationale 1: Bilateral chest expansion is decreased in emphysema. Rationale 2: Thoracic expansion is altered on the affected side in patients with pneumothorax. Rationale 3: One side of the chest would not expand at the correct time if the patient has a flail chest. Rationale 4: Heart failure does not result in a change in chest expansion. Rationale 5: Thoracic expansion is not affected by influenza. Question 35 The nurse is preparing to auscultate a patient’s lungs. Which breath sounds would the nurse consider abnormal? 1. Crackles 2. Vesicular breath sounds 3. Bronchovesicular breath sounds 4. Wheezes 5. Bronchial breath sounds Correct Answer: 1,4 Rationale 1: Crackles are caused by airways that collapse during expiration and “pop” open during inspiration or by air bubbles passing through fluid. They are not normal breath sounds. Rationale 2: Vesicular breath sounds are the soft, low-pitched sounds heard over the majority of lung fields. They are normal. Rationale 3: Bronchovesicular breath sounds represent air movement in the moderate airways between the main bronchi and smaller airways. They are normal breath sounds. Rationale 4: Wheezes are continuous musical sounds caused by air flowing across airways that are narrowed or obstructed. They are abnormal breath sounds. Rationale 5: Bronchial breath sounds are heard over the major airways and are normal. Question 36 During a bronchoscopy, the nurse is to initially give 1.5 mg of midazolam hydrochloride (Versed) and another 1.5 mg of Versed in 2 minutes. Based on a concentration of 5 mg/mL, the nurse will draw up a total of mL for the two doses. Correct Answer: 0.6 Rationale : 0.3 mL is to be given for the initial dose and another 0.3 mL in 2 minutes. 0.3 x 2 = 0.6 mL Question 37 A patient has these arterial blood gas (ABG) results. In analyzing the data, the nurse recognizes the patient has which condition? 1. Metabolic acidosis 2. Metabolic alkalosis 3. Respiratory acidosis 4. Respiratory alkalosis Correct Answer: 3 Rationale 1: The PaO2 is 75–100 mmHg, HCO3 is 24–28 mEq/L, and the base excess (BE) is + 2 mEq/L, which would not indicate metabolic acidosis. Rationale 2: The PaO2 is 75–100 mmHg, HCO3 is 24–28 mEq/L, and the base excess (BE) is + 2 mEq/L, which would not indicate metabolic alkalosis. Rationale 3: The patient is in respiratory acidosis, as the pH is decreased below normal (7.35– 7.45) and the PaCO2 is increased from normal (35–45 mmHg). Rationale 4: The PaO2 is 75–100 mmHg, HCO3 is 24–28 mEq/L, and the base excess (BE) is + 2 mEq/L, which would not indicate respiratory alkalosis. Question 38 The nurse is conducting a health history on a patient with dyspnea. Place the questions in correct sequence. Choice 1. How would you describe the dyspnea? Choice 2. What severity rating would you assign the dyspnea? Choice 3. Does the dyspnea seem to affect both lungs? Choice 4. How long does the dyspnea last? Choice 5. What makes the dyspnea better or worse? Choice 6. When did the dyspnea start? Correct Answer: 6,5,1,3,2,4 Rationale 1: This question addresses the quality (Q) component of OPQRST. Rationale 2: This question addresses the severity (S) component of OPQRST. Rationale 3: This question addresses the radiation (R) component of OPQRST. Rationale 4: This question addresses the timing (T) component of OPQRST. Rationale 5: This question addresses palliating or provoking factors (P) component of OPQRST. Rationale 6: This question addresses the onset (O) component of OPQRST. Question 39 The nurse administers oxygen to a patient who has lost a moderate amount of blood following a motor vehicle accident. What is the primary rationale for this nursing action? 1. To ease the work of breathing 2. To compensate for the reduction in circulating oxygen 3. To provide comfort 4. To prevent shock Correct Answer: 2 Rationale 1: Breathing might be easier, but this is an additional benefit, not the primary reason. Rationale 2: As blood volume is lost, hemoglobin is lost. Oxygen is carried from the respiratory system to the cells by hemoglobin in the blood. Rationale 3: The patient might be more comfortable, but this is an additional benefit not the primary reason. Rationale 4: The risk of shock might be decreased through oxygen administration, but this is an additional benefit not the primary reason. Question 40 The nurse anticipates that a patient with multiple fractured ribs is at risk for which condition? 1. Decreased lung expansion 2. Increased respiratory rate 3. Prolonged expiratory phase 4. Low arterial carbon dioxide level Correct Answer: 1 Rationale 1: Due to the rib fractures, it might be difficult for the patient to have full rib cage expansion because of the pain. Rationale 2: The respiratory rate might tend to be slower and more shallow than usual. Rationale 3: The expiratory phase might be shortened due to the pain. Rationale 4: The carbon dioxide would be high rather than low. Question 41 A patient admitted with probable emphysema is scheduled for diagnostic tests. Which test would assess the patient’s acid-base balance? 1. Bronchoscopy 2. Sputum studies 3. Pulse oximetry 4. Arterial blood gases (ABGs) Correct Answer: 4 Rationale 1: A bronchoscopy provides visualization of internal respiratory structures. Rationale 2: Sputum studies can provide specific information about bacterial organisms. Rationale 3: Pulse oximetry is a noninvasive test that evaluates the oxygen saturation level of blood. Rationale 4: ABGs are done to assess alterations in acid-base balance caused by respiratory disorders, metabolic disorders, or both. Question 42 After auscultating a patient’s chest, the nurse reports the findings to the preceptor. Which statement would indicate the need for immediate reassessment by the preceptor? 1. “I heard coarse crackles earlier, but now they sound finer.” 2. “I heard wheezing earlier, but now I don’t hear it.” 3. “There are coarse crackles that clear with coughing.” 4. “The patient was clear, but now there are scattered wheezes bilaterally.” Correct Answer: 2 Rationale 1: Coarse and fine are descriptors for crackles. Rationale 2: The absence of wheezing in a patient who had wheezing before may indicate impending respiratory arrest. The preceptor should reassess the patient immediately. There is also a possibility that therapy has reduced the wheezes and that no emergency exists. Rationale 3: This finding is not indicative of the need for immediate action. Rationale 4: This finding is not indicative of the need for immediate action. Question 43 The nurse is planning a class for unlicensed assistive personnel. Which factors should the nurse describe as causing interference with accurate pulse oximeter readings? 1. Ambient light 2. Nail polish 3. Inhalation injuries 4. Arterial pulse deficit 5. Sensor placement on the ear Correct Answer: 1,2,3,4 Rationale 1: Ambient light can cause inaccurate readings. Rationale 2: Nail polish on finger- or toenails can cause inaccurate readings. Rationale 3: Inhalation injuries can cause inaccurate readings. Rationale 4: Inadequate arterial pulses can cause inaccurate readings. Rationale 5: As long as the sensor is not placed on cartilage, the reading should be accurate. Question 44 The nurse wants to assess the apex of a patient’s right lung. In which location should the nurse place the stethoscope? 1. Intercostal space, sixth rib near the sternum 2. Intercostal space, fourth rib near the axillary line 3. Below the scapula 4. Near the right clavicle Correct Answer: 4 Rationale 1: This placement is too low. Rationale 2: This placement is too low. Rationale 3: The scapulae are located posterior to the lungs. Rationale 4: The apex of each lung lies just below the clavicle, whereas the base of each lung rests on the diaphragm. Question 45 The nurse knows that the caregiver of a patient with a respiratory illness understands discharge teaching when the caregiver makes which statement? 1. “I can expect to hear adventitious sounds only in the mornings; the rest of the day, breath sounds should be normal.” 2. “If I hear extra sounds during a deep breath, I know I am hearing adventitious sounds.” 3. “Adventitious sounds may be heard during inspiration or expiration because of secretions or inflammation.” 4. “I will know I am hearing adventitious breath sounds if I hear any sounds when I listen over the lower chest.” Correct Answer: 3 Rationale 1: Adventitious or abnormal breath sounds may be heard at any time of day or night. Rationale 2: The patient does not need to take a deep breath for adventitious or abnormal sounds to be heard. Rationale 3: Adventitious or abnormal breath sounds may be heard during inspiration and expiration. Rationale 4: Adventitious or abnormal breath sounds may be heard over any portion of the chest or back. Question 46 A review of a patient’s medical record reveals that the patient is using accessory muscles to aid breathing. Which muscle groups would the nurse expect to see in use? 1. Abdominals 2. Scalene 3. Brachialis 4. Trapezius 5. Sternocleidomastoid Correct Answer: 1,2,4,5 Rationale 1: Abdominal muscles are used to augment respiratory effort. Rationale 2: Scalene muscles are the muscles of the lateral neck. These muscles can be used to augment respiratory effort. Rationale 3: The brachialis muscles are in the arm and are not useful in augmenting respiratory effort. Rationale 4: The trapezius muscles of the upper back can augment respiratory effort. Rationale 5: The sternocleidomastoid muscles are in the anterior neck and are often used to augment respiratory effort. Question 47 A patient with pneumonia is experiencing shunt ventilation. The nurse plans care for the patient based on which considerations? 1. Shunt ventilation is the normal state for a patient who has pneumonia. 2. Blood flow to the alveoli is compromised. 3. Blood is flowing past the alveoli but is not being oxygenated. 4. Ventilation is inadequate at the alveolar level. 5. Hypoxia may occur if the unaffected lung cannot compensate. Correct Answer: 3,4,5 Rationale 1: Shunt ventilation is not normal and the patient may decompensate quickly. Rationale 2: In shunt ventilation, blood flow to the alveoli is normal. Rationale 3: Blood is “shunting” past the alveoli, but oxygenation is not taking place. Rationale 4: Not enough oxygen is being delivered to the alveoli, and blood is not being oxygenated. Rationale 5: As long as the unaffected lung can supply sufficient oxygen, the patient may show few ill effects from shunt ventilation. However, should the unaffected lung fail to compensate, hypoxia will occur. Question 48 The nurse had planned to conduct a patient interview regarding pulmonary history. Which patient behaviors would indicate to the nurse that this interview should be delayed? 1. The patient cannot speak in complete sentences. 2. The patient is sitting up at the bedside. 3. The patient’s respiratory rate has increased from 14 to 20. 4. The patient has assumed a forward leaning posture, braced on the hands. 5. The patient’s arterial blood gases reveal a pH of 7.38. Correct Answer: 1,3,4 Rationale 1: The patient who cannot speak in complete sentences may be suffering from respiratory distress. The nurse should delay the interview and should conduct further physical assessment. Rationale 2: Finding the patient sitting up at the bedside is not a reason to delay the interview unless other, more specific, assessments are also made. Rationale 3: An increase in respiratory rate may indicate respiratory distress. The nurse should delay the interview and conduct additional physical assessment. Rationale 4: This position is called the “tripod” position and is a classic maneuver to expand lung fields. The patient may be in acute respiratory distress, so the interview should be delayed. Rationale 5: This is a normal arterial blood gas reading and does not indicate respiratory compromise. Question 49 A patient from Southeast Asia presents to the clinic with complaints of shortness of breath. The patient says, “I tried to coin my wind illness, but it did not work.” Which assessment finding would the nurse expect? 1. The patient is wearing an amulet shaped like a dragon. 2. The patient has burns on the inside of the nose and mouth. 3. The patient is pale from blood loss. 4. The patient has small scrapes across the back and chest. Correct Answer: 4 Rationale 1: The patient may be wearing an amulet, but probably not to treat the illness. Rationale 2: Treating “wind illness” does not include burning the inside of the nose and mouth. Rationale 3: There is no indication that cultural treatment for “wind illness” would cause large amounts of blood loss. Rationale 4: Coining is a cultural practice that involves scraping the skin of the thorax with a coin or spoon. The scraping may leave lesions. Question 50 The patient says, “I think I am allergic to something in my house. I feel better when I am away for a few days.” What should the nurse suggest? 1. “You might want to keep your dog outside.” 2. “You might want to consider having allergy testing done.” 3. “You should remove dust by vacuuming your house every day and getting rid of your drapes and decorative pillows.” 4. “You should consider having your home professionally cleaned.” Correct Answer: 2 Rationale 1: The nurse has no reason to suspect that the patient is allergic to the dog. Rationale 2: Before efforts to rid a home of allergens begin, the patient should be aware of which substances are causing symptoms. Rationale 3: The nurse does not know if the patient is allergic to dust. Rationale 4: The nurse is not aware of what or if the patient is allergic to anything in the house. Chemical cleaners can also cause allergies. Question 51 The nurse is conducting a health history interview with a patient who has severe respiratory disease. The nurse asks specific questions about how the patient performs oral hygiene. What is the rationale for this questioning? 1. Oral infections can result in pulmonary infections. 2. The ability to perform good oral hygiene reflects an ability to hold one’s breath for several seconds. 3. Respiratory illness is associated with an increased risk for dental caries. 4. People who perform good oral hygiene typically also perform good hand hygiene. Correct Answer: 1 Rationale 1: This patient is at risk for pulmonary infection. Oral infections can travel down the pulmonary tree and cause pulmonary access formation. Rationale 2: This may be accurate, but it is not the rationale for this questioning. Rationale 3: There is no indication that respiratory illness causes tooth decay. Rationale 4: There is no association between these two hygiene practices that would serve as a rationale for these questions. Question 52 A patient with a preexisting pulmonary illness is being seen in the clinic for a routine assessment. The patient says, “My family and I are going skiing for our next vacation.” What information should the nurse provide? 1. “Going to high altitudes is not a good idea for your health.” 2. “You should be watchful for any respiratory problems while you are there.” 3. “You should go to the seashore instead.” 4. “Be certain to fly directly to the resort if possible.” Correct Answer: 2 Rationale 1: High altitudes may or may not affect the patient’s health. Rationale 2: High altitudes may cause decompensation of respiratory status for any person, but persons with preexisting pulmonary illness are at greater risk. Rationale 3: The nurse should not tell the patient where to go on vacation. Rationale 4: There is no indication that flying directly to the resort should be recommended. Question 53 A nurse researcher is planning a study regarding occupational exposure to asbestos and the development of asbestos-related pulmonary disease. The researcher should look to workers from which occupations as commonly having this exposure? 1. Firefighters 2. Auto mechanics 3. Those involved in new home construction 4. Teachers 5. Cooks Correct Answer: 1,2 Rationale 1: Older buildings may contain significant amounts of asbestos. Firefighters may be exposed during fire events. Rationale 2: Auto mechanics may be exposed to the asbestos in vehicle brake linings. Rationale 3: Asbestos has been removed from modern construction materials. Construction workers in new home construction would not be likely to have high exposure rates. Rationale 4: There is no reason to believe that teachers are at risk for exposure to asbestos. Rationale 5: There is no reason to believe that cooks are at high risk for exposure to asbestos. Question 54 A review of a patient’s medical record reveals a 70-pack-year smoking history. The patient says he smokes two packs of cigarettes every day. The nurse calculates that this patient has been smoking for years. Correct Answer: 35 Rationale : Pack years are figured by the number of packs a day times the years smoked. This patient has a 70-pack-year history and smokes two packs per day. He has been smoking for approximately 35 years. Question 55 A patient has been admitted for exacerbation of a chronic pulmonary disease. The nurse would assign the nursing diagnosis Activity Intolerance when which assessment is made? 1. The patient’s heart rate increases by 20 beats per minute when she ambulates to the bathroom in her hospital room. 2. The patient’s husband reports that she sits in a recliner chair most of the day. 3. The patient complains of cramping in her legs at night. 4. The patient’s ankles demonstrate 3+ edema bilaterally. Correct Answer: 1 Rationale 1: Increasing heart rate on exertion is a finding associated with intolerance of activity. Rationale 2: This is not enough evidence to support activity intolerance as a nursing diagnosis. The patient may be depressed or simply desire to stay in the chair. Rationale 3: Night leg cramps may or may not be associated with activity intolerance. Rationale 4: Ankle edema may or may not be associated with activity intolerance. Question 56 A patient is admitted after falling down a flight of stairs. The nurse notes that the patient’s larynx is slightly left of center. The nurse should assess for which conditions? 1. Right heart failure 2. Left hemothorax 3. Right pneumothorax 4. Right hemothorax 5. Central pneumothorax Correct Answer: 3,4 Rationale 1: Tracheal deviation does not indicate right heart failure. Rationale 2: Left hemothorax is not occurring in this case. Rationale 3: Collection of fluid or air in the right chest cavity results in tracheal deviation to the left. Rationale 4: Collection of fluid or air in the right chest cavity results in tracheal deviation to the left. Rationale 5: Pneumothorax is classified as right or left, not central. Question 57 The nurse is assessing a patient for pedal edema. If using the correct technique, the nurse will depress the tissue for seconds. Correct Answer: 5 Rationale : To assess edema and to elicit pitting edema, the nurse would depress the tissue of the ankle for 5 seconds. Question 58 To establish the location of a respiratory sound, the nurse uses standard landmarks. The nurse locates the second rib as adjacent to which structure? 1. Supersternal notch 2. Sternal angle 3. Costal margin 4. Xiphoid process Correct Answer: 2 Rationale 1: The second rib is below this area. Rationale 2: The rib that is adjacent to the sternal angle is the second rib. Rationale 3: The costal margin is the bottom of the rib cage. Rationale 4: The xiphoid process is the distal end of the sternum and is closest to the seventh rib. Question 59 During auscultation of the thorax, the nurse hears a low-pitched creaking sound. What should be the nurse’s next action? 1. Have the patient cough to attempt to clear the sound. 2. Have the patient turn to the left side. 3. Collaborate with the physician regarding a chest X-ray. 4. Ask the patient to hold her breath. Correct Answer: 4 Rationale 1: Crackles may clear with coughing, but this description does not match that of crackles. Rationale 2: Positioning the patient will not change this assessment finding. Rationale 3: An X-ray will likely be ordered, but this is not the first action indicated. Rationale 4: This assessment represents a rub. The next assessment step is to differentiate pleural rub from cardiac rub by asking the patient to hold the breath. If the sound disappears, it is a cardiac rub. Question 60 A parent has just started using a “red, yellow, green” peak flow meter to monitor his young son’s pulmonary disease at home. The parent calls the clinic and reports that the last two results have been in the red zone. What advice should the nurse offer this parent? 1. “Rinse the meter out with warm salt water and repeat the test.” 2. “Bring your son and the meter to the clinic for evaluation.” 3. “Don’t bother using the meter until I can check your technique at next week’s appointment.” 4. “These are the results we hope to see, so it sounds like you are doing a good job managing your son’s illness.” Correct Answer: 2 Rationale 1: There is no indication that the meter needs any type of maintenance. Rationale 2: Two red readings may indicate respiratory complications. The patient should be evaluated. The nurse should also have the parent bring in the meter so his or her technique can be evaluated. Rationale 3: The parent’s technique may be wrong, but the patient may be experiencing significant respiratory changes. Assessment cannot wait until next week. Rationale 4: Red readings indicate potential respiratory complications. Question 61 A 40-year-old male has reported to the clinic with complaints of impotence. The nurse is reviewing the patient’s health history. Which statements by the patient warrant further investigation? 1. “I take medications to control my blood pressure.” 2. “I had the mumps when I was a boy.” 3. “I had a vasectomy 4 years ago.” 4. “I have had diabetes for several years.” 5. “My wife has a history of cervical cancer.” Correct Answer: 1,4 Rationale 1: Certain antihypertensive drugs may cause impotence. Rationale 2: The mumps are a risk factor for male infertility, not impotence. Rationale 3: A vasectomy results in sterility, not impotence. Rationale 4: Diabetes mellitus over time may result in vascular damage, leading to impotence. Rationale 5: The presence of cervical cancer in a partner is not linked to impotence. Question 62 The nurse is preparing to obtain a sexual history from a male patient. Which question is of the highest importance in this assessment? 1. “Do you engage in same-sex activity?” 2. “Do you have sex frequently?” 3. “Do you enjoy sexual intercourse?” 4. “Do you engage in masturbation?” Correct Answer: 1 Rationale 1: Assessing for the risk of sexually transmitted infections and preventing sexually transmitted infections are a priority for this patient. Sexual intercourse with same-sex partners further increases the risk for HIV infection. Determination of same-sex activity by a man is key in assessing risk factors. Rationale 2: The frequency of sexual intercourse is part of the data collection but does not have the same importance as the determination of risk factors. Rationale 3: The enjoyment of sexual intercourse is part of the data collection but does not have the same importance as the determination of risk factors. Rationale 4: Masturbation may be included in the data collection, but it is not as important as the assessment of risk factors. Question 63 The nurse is providing instruction to a patient who has been diagnosed with prostate cancer. Which statement by the patient would indicate understanding of the nurse’s instruction? 1. “The prostate gland is where sperm are formed.” 2. “The prostate gland is located at the neck of my bladder.” 3. “The prostate gland produces semen.” 4. “The prostate gland is normally very small, only about a quarter of an inch long.” Correct Answer: 2 Rationale 1: Sperm are formed in the testes. Rationale 2: The prostate gland is located at the bladder neck. Rationale 3: Semen is produced by seminal vesicles. Rationale 4: The normal size of the prostate gland is about 2.5 cm or about 1 inch. Question 64 A patient presents to the emergency department with swelling and pain in his scrotum. The nurse anticipates dysfunction in which structures? 1. Testes 2. Vas deferens 3. Epididymis 4. Seminal vesicle 5. Prostate Correct Answer: 1,3 Rationale 1: The testes are contained in the scrotum. Rationale 2: The vas deferens is located in the abdomen. Rationale 3: The epididymis is located in the scrotum. Rationale 4: The seminal vesicle is located behind the prostate. Rationale 5: The prostate is located at the bladder neck. Question 65 The nurse is performing an assessment of a female patient’s breasts. Which findings indicate the need for further assessment? 1. One breast is shaped differently from the other. 2. The breasts do not display prominent veins. 3. The nipples are a light tan in color. 4. There is clear discharge from one nipple. 5. There is an area of dimpled skin on one breast. Correct Answer: 1,4,5 Rationale 1: Changes in contour may be revealed as a shape difference and should be further evaluated. Rationale 2: The absence of prominent veining is normal. Rationale 3: The nipple color may range from pink to brown. Rationale 4: Nipple discharge should be further evaluated. Rationale 5: Dimpling and abnormal contours should be further evaluated. Question 66 The nurse is conducting a presentation to a group of women concerning menopause. Which statements by a participant indicate good understanding of the process? 1. “Lubrication for intercourse will not be as necessary after menopause.” 2. “My risk for vaginal infections is reduced once my estrogen levels decrease during menopause.” 3. “My ovaries will shrink in size after menopause.” 4. “The hair under my arms will thicken.” 5. “I can expect my pubic hair to turn gray.” Correct Answer: 3,5 Rationale 1: The loss of estrogen as a woman ages is responsible for the reduction in vaginal lubrication. Patients experiencing this loss may require lubricants to promote comfort. Rationale 2: The vaginal dryness associated with menopause places the woman at an increased risk for the development of vaginal infections. Rationale 3: The ovaries shrink in size as a result of menopause. A palpable ovary should be considered enlarged. Rationale 4: Axillary hair becomes sparser. Rationale 5: Pubic hair turns gray and becomes sparser. Question 67 During a vaginal examination of a 33-year-old patient, a nontender mass at the posterolateral portion of the labia majora is noted. The nurse anticipates which diagnosis? 1. Rectocele 2. Fistula 3. Bartholin cyst 4. Cyst of the Skene’s gland Correct Answer: 3 Rationale 1: A rectocele results when the walls between the rectum and the vagina become weakened. Rationale 2: A fistula results when there is an opening between two separate organs. Rationale 3: The Bartholin glands are located at the posterolateral labia majora. These glands are responsible for providing lubrication to the female genitalia. A swelling in this area is consistent with the diagnosis of a Bartholin cyst. Rationale 4: The Skene’s glands are located on either side of the urethral meatus. Question 68 The nurse is preparing to examine a male patient’s reproductive organs. What nursing actions are part of preparing for this examination? 1. Secure a private examination room. 2. Use clean hands for the examination. 3. Ask the patient to lie down on the exam table. 4. Ask the patient put on a gown. 5. Make sure the room temperature is cool. Correct Answer: 1,4 Rationale 1: The nurse ensures that the examining room is warm and private. Rationale 2: The nurse puts on gloves before beginning and wears them throughout the examination. Rationale 3: The assessment may be done with the patient sitting or standing. Rationale 4: The nurse has the patient remove his clothing and put on a gown or drape. Rationale 5: A cool temperature may be uncomfortable to the patient who is undressed. Question 69 During an assessment, a female patient asks why the nurse is “feeling her armpit.” Which responses are appropriate? 1. “I’m counting your ribs.” 2. “Don’t you feel your own armpits?” 3. “Breast tissue extends into this area.” 4. “I’m assessing hair distribution in this area.” 5. “The armpits should be part of your breast self-exam.” Correct Answer: 3,5 Rationale 1: Counting the ribs is unnecessary. Rationale 2: This response does not address the patient’s question. Rationale 3: Various palpation patterns may be used as long as every part of each breast is palpated, including the axillary tail, or the tail of Spence, which is the breast tissue that extends from the upper outer quadrant toward and into the axillae. Rationale 4: Hair distribution would be assessed with visualization, not palpation. Rationale 5: The nurse will explain breast self-exam (BSE) to the patient. Question 70 The nurse is assessing for a left inguinal hernia in a male patient. Which technique should the nurse use? 1. Palpate for a structure that feels like a “bag of worms.” 2. Use the left forefinger to examine the inguinal ring. 3. Ask the patient to cough during the assessment. 4. Have the patient face a table and lean over it. Correct Answer: 3 Rationale 1: The structure that feels like a “bag of worms” is a varicocele. Rationale 2: The right forefinger is used to examine the left inguinal ring. Rationale 3: The nurse asks the patient to cough which brings the bulging hernia down against the nurse’s finger. Rationale 4: This position is used for palpation of the prostate. Question 71 A female patient is admitted with a painful swelling in the perineal body. Where would the nurse look to assess this lesion? 1. Between the anus and the fourchette 2. Just lateral to the urethral meatus 3. Just anterior to the clitoris 4. Just anterior to the opening to the vagina Correct Answer: 1 Rationale 1: The perineal body is located between the fourchette in the front and the anus in the back. Rationale 2: The structure just lateral to the urethral meatus is the labium minus. Rationale 3: The structure just anterior to the clitoris is the prepuce. Rationale 4: The structure just anterior to the vagina orifice is the urethral meatus. Question 72 The nurse is reviewing the laboratory analysis of a female patient’s hormones. Increases in which hormone levels would indicate ovulation is occurring? 1. Estrogen 2. Luteinizing hormone 3. Progesterone 4. Gonadotropin-releasing hormone Correct Answer: 2 Rationale 1: Estrogen levels peak prior to the release of the hormone necessary for ovulation. Rationale 2: When the luteinizing hormone peaks, ovulation occurs. Rationale 3: Increases in the progesterone level occur after ovulation. Rationale 4: The gonadotropin-releasing hormone stimulates the anterior pituitary to release the follicle-stimulating hormone, which occurs prior to ovulation. Question 73 A patient with a menstrual cycle of 28 days asks about the timing of ovulation. The nurse would respond that ovulation would most likely occur on which days? 1. 14 to 16 2. 20 to 22 3. 10 to 12. 4. 1 to 2 Correct Answer: 1 Rationale 1: Ovulation occurs at mid-cycle. Because there are 28 days in the patient’s menstrual cycle, ovulation would occur on day 14 to 16. Rationale 2: Days 20 to 22 follow the time of ovulation for this patient. Rationale 3: Days 10 to 12 precede the likely ovulation time for this patient. Rationale 4: Days 1 to 2 are the first days of menstruation, at the beginning of the cycle. Ovulation will not occur for several more days. Question 74 A patient is having a routine prostate examination. Which question is an important part of this examination? 1. “Do you have polyuria in the morning?” 2. “Do you take laxatives or stool softeners?” 3. “Do you have difficulty with urination?” 4. “Do you experience constipation?” Correct Answer: 3 Rationale 1: Polyuria in the morning is not a sign of prostate disease. Rationale 2: Taking laxatives or stool softeners does not affect the function of the prostate. Rationale 3: When the prostate is enlarged, it disrupts urinary flow and causes several urinary symptoms. Rationale 4: Experiencing constipation is not associated with the prostate gland. Question 75 The nurse is assessing the medication history of a patient with an enlarged prostate. The nurse would inquire about the use of which herbal supplement? 1. Ginkgo 2. Saw palmetto 3. Green tea 4. Fish oil Correct Answer: 2 Rationale 1: Ginkgo is not used to improve prostate health. Rationale 2: Saw palmetto is an herbal supplement sometimes suggested for use by patients with an enlarged prostate gland. Rationale 3: Green tea is not associated with prostate health. Rationale 4: Fish oil is not associated with prostate health. Question 76 During a physical examination, a male patient reports discharge from the urinary meatus. The discharge is not visible to the nurse. What is the first action the nurse would ask the patient to take? 1. Continue to watch for other signs of a sexually transmitted infection (STI). 2. Return to the clinic when the discharge occurs. 3. Strip the penis to bring discharge to the meatus for culture. 4. Go to the emergency department for further testing. Correct Answer: 3 Rationale 1: Watching for other signs of an STI is premature because the nurse does not know if the discharge is related to an STI. Rationale 2: Returning to the clinic when the discharge occurs is appropriate, but the initial action would be to attempt to obtain a culture of the fluid. Rationale 3: The patient should strip (compress or milk) the penis to bring discharge to the meatus so that testing can be performed. Rationale 4: Going to the emergency department is unnecessary because the patient can be further tested and treated during the examination. Question 77 The nurse is assisting the health care provider with a routine prostate examination. The nurse could assist the patient to which positions for this examination? 1. On the left side with right knee drawn up 2. Leaning over the examination table 3. Standing in the most comfortable position 4. On the right side with both knees flexed 5. In the lithotomy position Correct Answer: 1,2 Rationale 1: This is a correct anatomical position for a routine prostate examination. Rationale 2: This is a correct anatomical position for a routine prostate examination. Rationale 3: Standing does not allow access to the prostate. Rationale 4: There is no reason for both knees to be drawn up, and this may make the patient more uncomfortable. Rationale 5: The lithotomy position is used to examine the internal female reproductive organs. It is not recommended for prostate examination. Question 78 While obtaining a social history on a male patient regarding patterns of alcohol use, the nurse becomes aware that the patient may have a drinking problem. The nurse continues assessing the patient using the CAGE questionnaire. Which questions would the nurse ask? 1. “Have you ever felt annoyed by criticism of your drinking?” 2. “Have you ever felt the desire to stop drinking?” 3. “Have you ever taken a drink first thing in the morning?” 4. “Have you ever felt the need to cut down on drinking?” 5. “Have you ever felt guilty about drinking?” Correct Answer: 1,3,4,5 Rationale 1: Annoyance at being criticized for drinking is one of the areas assessed by the CAGE questionnaire. Rationale 2: This question is not part of the CAGE questionnaire. Rationale 3: Asking about drinking first thing in the morning is part of the CAGE questionnaire. Rationale 4: Asking about feeling the need to cut down on drinking is part of the CAGE questionnaire. Rationale 5: Guilt about drinking is assessed by the CAGE questionnaire. Question 79 A patient is having a breast examination and is asked by the nurse to position her arms at her sides, then to press her hands to her hips. The patient asks why she has to perform so many different positions for the examination. What rationale would the nurse provide for this request? 1. Several positions pull ligaments, causing dimpling if a tumor is present. 2. Having the patient move facilitates a neurological assessment along with the breast examination. 3. These movements help to determine the patient’s state of balance. 4. These movements help test motor strength. Correct Answer: 1 Rationale 1: Several maneuvers move the breast and pull the suspensory ligaments in such a way that a tumor would cause dimpling or a bulge. Rationale 2: Neurological assessment is not the rationale for maneuvering the extremities during a breast examination. Rationale 3: Testing the state of balance is not the rationale for these movements. Rationale 4: Testing motor strength is not the rationale for these movements. Question 80 A patient’s laboratory results reveal a low platelet count. The nurse would assess the patient for which skin finding? 1. Jaundice 2. Petechiae 3. A brown or dark tinge to the skin 4. A flushed appearance Correct Answer: 2 Rationale 1: Jaundice is generally related to liver failure. Rationale 2: Petechiae are small capillary bleeds that manifest as red dots on the skin. Petechiae can result from bleeding disorders caused by reduced platelets. Rationale 3: Brown or darker skin than normal may indicate a breakdown of erythrocytes. This is not associated with platelet dysfunction. Rationale 4: Pink or flushed skin may be caused by polycythemia vera. Question 81 A patient’s mean corpuscular volume (MCV) is low. How would the nurse explain this finding to the patient? 1. “Your red blood cells do not have enough hemoglobin.” 2. “Your red blood cells are not consistent in size.” 3. “Your hematocrit is low.” 4. “Your red blood cells are small.” Correct Answer: 4 Rationale 1: Mean corpuscular hemoglobin (MCH) and mean corpuscular hemoglobin concentration (MCHC) are tests for the amount of hemoglobin in a red blood cell. Rationale 2: The red blood cell distribution width (RDW) is a direct measure of the consistency of red blood cell size. Rationale 3: MCV is not a measure of hematocrit. Hematocrit changes with hydration status, so it is not possible to correlate hematocrit level and MCV. Rationale 4: MCV is a measure of t size of red blood cells. Question 82 The patient is scheduled to have a mean corpuscular volume (MCV), mean corpuscular hemoglobin (MCH), and mean corpuscular hemoglobin concentration (MCHC) drawn. How would the nurse explain the purpose of these tests? 1. “These tests will help us determine if you have cancer in your blood.” 2. “We are testing to see if you have an infection.” 3. “These tests will help us determine what kind of anemia you have.” 4. “We are testing to see if you have anemia.” Correct Answer: 3 Rationale 1: These tests are not used to detect cancer in the blood. Rationale 2: These tests are not used to detect infection. Rationale 3: MCV, MCH, and MCHC are used to help determine type of anemia. Rationale 4: The total red blood cell count would indicate if anemia is present. Question 83 A patient has just had a bone marrow biopsy taken from the iliac crest. What is the nurse’s next action? 1. Apply a fluid collection device around the drain. 2. Cover the biopsy site with a bulky pressure dressing. 3. Plan to assess the patient regularly for pain and bleeding. 4. Have the patient ambulate to mobilize marrow replacement. Correct Answer: 3 Rationale 1: A drain is not inserted in this procedure. Rationale 2: There is no need to use a bulky dressing over this site. A small gauze square is applied with mild pressure. Rationale 3: The nurse should assess this patient regularly for pain and bleeding. Rationale 4: There is no specific need to have the patient ambulate. Question 84 A patient diagnosed with sickle cell anemia is in severe pain. How would the nurse explain the etiology of this pain? 1. “You don’t have enough red blood cells to carry oxygen to your tissues.” 2. “You have infection in your blood because your white blood cells are not working correctly.” 3. “Your red blood cells clog up the vessels and the tissues don’t get oxygen.” 4. “You have too many red cells, so your blood is too thick.” Correct Answer: 3 Rationale 1: The major etiology of pain in sickle cell anemia is not related to a decreased number of red blood cells. Rationale 2: Sickle cell anemia is not related to changes in the white blood cells. Rationale 3: Because of their sickled shape, the RBCs occlude vessels, causing ischemia to the tissues being supplied by the vessels. Ischemia results in pain. Rationale 4: The pathology of sickle cell anemia does not include excess of red blood cells. Question 85 Which chief complaint would the nurse evaluate as indicating the patient may have problems with erythrocyte levels? 1. “I have been running a low-grade fever for a week.” 2. “I have bruises all over my body.” 3. “I am sick all the time.” 4. “I am so tired all the time.” Correct Answer: 4 Rationale 1: Fever is more closely associated with leukocytes. Rationale 2: Bruising is associated with a dysfunction of platelets. Rationale 3: Frequent illnesses may reflect a dysfunction of leukocytes. Rationale 4: Fatigue is often associated with changes in erythrocyte level. Question 86 A patient reports that she has decided to follow a vegetarian diet. The nurse would discuss methods of obtaining enough of which important element in the diet? 1. Calories 2. Iron 3. Fat 4. Protein Correct Answer: 2 Rationale 1: Vegetarian diets have sufficient calories. Rationale 2: Many of the sources of iron in the diet are meat-based. A person following a vegetarian diet must be certain to obtain sufficient iron. Rationale 3: Vegetarian sources of fat include vegetable oils and nuts. Rationale 4: Vegetarian diets make use of plant-based proteins, eggs, and dairy products. Question 87 A patient with a lung disease takes prophylactic antibiotics and tries to stay indoors during the winter. Today the patient reports bleeding more than normal after a minor injury. How would the nurse evaluate this report? 1. The antibiotic may be interfering with clotting times. 2. The patient is not getting enough vitamin D from sunlight. 3. The patient may be ingesting more vitamin K–containing food. 4. The patient’s lung disease has affected the production of platelets. Correct Answer: 1 Rationale 1: Some people develop prolonged bleeding times while taking antibiotics. Rationale 2: Insufficient vitamin D is not the likely reason for this bleeding. Rationale 3: Vitamin K is an antidote for warfarin and can cause increased clotting, not increased bleeding. Rationale 4: There is no indication that lung disease reduces platelet production. It may, however, increase erythrocyte production. Question 88 A patient is suspected of having pernicious anemia. Which area of the body would the nurse pay particular attention to during assessment? 1. Nose 2. Tongue 3. Hands 4. Feet Correct Answer: 2 Rationale 1: The nose does not change when pernicious anemia is present. Rationale 2: The tongue takes on a characteristic smooth texture when pernicious anemia is present. Rationale 3: There is no particular change in the hands associated with pernicious anemia. Rationale 4: There is no particular change in the feet associated with pernicious anemia. Question 89 The nurse is reviewing laboratory results for a 45-year-old woman. Which result would the nurse immediately discuss with the health care provider? 1. Hemoglobin 10.8 g/dL 2. Mean corpuscular volume 89µm3 3. Mean corpuscular hemoglobin 30 pg 4. Total RBC 4,500,000 cells per cubic millimeter Correct Answer: 1 Rationale 1: Normal hemoglobin for an adult woman is 12–15 g/dL. The nurse should immediately discuss this low result with the health care provider. Rationale 2: This is a normal MCV level. Rationale 3: This is a normal MCH. Rationale 4: This is a normal total RBC for an adult woman. Question 90 A patient is scheduled for a bone marrow aspiration. The nurse would reinforce which teaching about this procedure? 1. Bone marrow fluid will be drawn into a needle. 2. The sample will be taken from a vertebra in the neck. 3. Bone marrow fluid and a piece of bone will be collected. 4. The patient will receive general anesthesia for this procedure. Correct Answer: 1 Rationale 1: Bone marrow aspiration includes collection of fluid through a needle. Rationale 2: The sample is generally taken from the iliac crest. Rationale 3: If bone is collected, the procedure is a bone marrow biopsy. Rationale 4: This procedure is performed under local anesthesia. Question 91 The nurse is aware that which occupations could put a patient at risk for carpal tunnel syndrome? 1. Wheat farmer 2. Store cashier 3. Barber 4. Computer data input specialist 5. Carpenter Correct Answer: 2,3,4,5 Rationale 1: The normal activities of wheat farming would be unlikely to put the farmer at risk for carpal tunnel syndrome. Rationale 2: Repetitive hand motions are required for this profession, which increases the risk for carpal tunnel syndrome. Rationale 3: Repetitive hand motions are required for this profession, which increases the risk for carpal tunnel syndrome. Rationale 4: Repetitive hand motions are required for this profession, which increases the risk for carpal tunnel syndrome. Rationale 5: Repetitive hand motions are required for this profession, which increases the risk for carpal tunnel syndrome. Question 92 A patient is diagnosed with a compound fracture and is scheduled for immediate surgery. Which nursing diagnosis would have the highest priority in the immediate postoperative period? 1. Impaired Transfer Ability 2. Risk for Post-Trauma Syndrome 3. Risk for Infection 4. Risk for Falls Correct Answer: 3 Rationale 1: The patient may have difficulty with transfers, but this is not the greatest priority. Rationale 2: Depending on the reason for the injury and the patient’s response, post-trauma syndrome may be applicable. This is not the greatest priority. Rationale 3: The patient with an open, compound fracture has multiple bone breaks penetrating through the skin and must be assessed and cared for vigilantly for signs of infection. Rationale 4: The patient is at risk for a fall due to fracture, but this is not the highest priority. Question 93 The nurse should assess a patient with a long leg cast for which signs that would indicate compromised circulation? 1. Swelling of the toes 2. Drainage on the cast 3. Elevated temperature 4. Foul odor 5. A tight cast Correct Answer: 1,5 Rationale 1: Swelling of the toes is likely due to decreased venous return caused by the cast being too tight. Rationale 2: Drainage may indicate bleeding or infection. Rationale 3: An elevated temperature indicates infection. Rationale 4: Foul odor indicates an infective process. Rationale 5: Edema can cause the cast to become tight. A tight-fitting cast can lead to compartment syndrome. Question 94 A patient is diagnosed with a sprained right ankle. The nurse instructs the patient on which common treatment of sprains? 1. Application of a long leg cast 2. Opioid pain medication 3. Heat, rest, compression, and elevation 4. Rest, ice, compression, and elevation Correct Answer: 4 Rationale 1: Sprains are not treated with casts. Rationale 2: Anti-inflammatory medications are best for sprains. Opioids are generally not required. Rationale 3: Heat is contraindicated for treatment of sprains as it may increase swelling and pain. Rationale 4: The interventions included in RICE therapy allow the injured muscle, ligament, or tendon to heal (rest), cause vasoconstriction and reduce pain (ice), decrease edema formation and pain (compression), and promote venous return to decrease edema and pain (elevation). Question 95 The patient is diagnosed with an oblique fracture of the left femur. The nurse understands that the process of bone healing occurs in phases. Place in order the phases of the bone healing process. Click and drag the options below to move them up or down. Choice 1. Reparative phase Choice 2. Initial injury (fracture) Choice 3. Inflammatory phase Choice 4. Remodeling phase Correct Answer: 2,3,1,4 Rationale 1: Calcium is deposited during the inflammatory phase and a callus forms in the reparative phase. Collagen forms and calcium deposition continues. Rationale 2: The bone healing process begins after the initial injury or fracture. Rationale 3: The bleeding and inflammation that develop at the site of the fracture initiate the inflammatory phase. Rationale 4: During the remodeling phase, excess callus is removed and new bone is laid down along the fracture line. The fracture site calcifies and the bone reunites. Question 96 Which assessment data would the nurse interpret as indicating a patient could be experiencing a fat embolus? 1. Pulse oximetry 86% 2. Petechiae on the chest and upper arms 3. Shortness of breath and chest pain 4. Respiratory rate 32 5. Skin hot, dry, and flushed Correct Answer: 1,2,3,4 Rationale 1: Hypoxemia is one of the classic findings associated with fat embolism syndrome. Rationale 2: Petechial rash is a late manifestation of fat embolism syndrome. Rationale 3: Dyspnea is an early finding of fat embolism syndrome. Rationale 4: Tachypnea is an early finding of fat embolism syndrome. Rationale 5: Hot, dry, and flushed skin may indicate other pathology but is not associated with fat embolism syndrome. Question 97 A patient recovering from a fractured hip is at risk for developing deep vein thrombosis (DVT). The nurse monitors for which findings that would indicate DVT is occurring? 1. Positive Homans’ sign 2. Decreased urine output 3. Confusion 4. Tachypnea Correct Answer: 1 Rationale 1: Homans’ sign is considered positive when plantar and dorsiflexion on the affected side cause calf pain. A positive Homans’ is considered a sign of possible DVT. Rationale 2: Dehydration may cause DVT, but decreased urine output alone would not be a reason to suspect DVT. Rationale 3: Confusion is not a sign of DVT, but it may indicate that venous thromboembolism has occurred from a DVT. Rationale 4: Tachypnea is not a sign of DVT, but it may indicate that venous thromboembolism has occurred from a DVT. Question 98 The nurse is changing a patient’s stump dressing. How would the nurse document this dressing technique? 1. Figure-of-eight bandage 2. Binder wrapping 3. Splinting 4. Bivalving Correct Answer: 1 Rationale 1: Compression wrapping of the extremity helps to prevent edema. Figure-of-eight bandaging starts at the distal stump (after the bandage is anchored around the waist) and is wrapped back toward the waist. Rationale 2: This bandage is not applied like a binder. Rationale 3: No splint is used in this technique. Rationale 4: Bivalving of a cast is used to reduce the risk of compartment syndrome. Question 99 The patient has a fracture of the right tibia and fibula. The orthopedic surgeon decides to surgically correct the fractures with the type of device pictured in the figure. What type of device is being used? 1. External fixation device 2. Internal fixation device 3. Buck’s traction 4. External wiring Correct Answer: 1 Rationale 1: In external fixation, pins are placed through the bone above and below the fracture site to attach the bone to an external frame. Rationale 2: Internal fixation devices involve a surgical incision with the placement of plates and screws. The incision is then closed and the devices are not visible externally. Rationale 3: Buck’s traction is a traction device used for fractured hips. Rationale 4: This is not a wiring device. Question 100 The nurse has identified the diagnosis Acute Pain for a patient recovering from an above-the- knee amputation. Which nursing interventions would be beneficial for this patient? 1. Administer analgesics before pain reaches a higher level. 2. Support the injured area when moving the patient. 3. Elevate the stump on three pillows. 4. Encourage deep breathing and relaxation exercise. 5. Reposition the patient every 8 hours. Correct Answer: 1,2,4 Rationale 1: Analgesics alleviate pain by stimulating opiate receptor sites. If pain medication is given when pain is rated at a lower level, the pain will be managed more effectively. Rationale 2: Supporting the injured area reduces pain when the patient is moving. Rationale 3: Elevating the stump can increase the risk of hip contractures. Rationale 4: Encouraging deep breathing and relaxation will increase the effectiveness of analgesics and modify the pain. Rationale 5: The patient should be repositioned every 2 hours to prevent muscle cramping and prolonged pressure on any area. BONUS Question 101 A patient who sustained massive trauma has just lost consciousness. A cardiac monitor is initiated, and it reveals pulseless electrical activity. The team working on this patient would quickly assess for which conditions? Note: Credit will be given only if all correct choices and no incorrect choices are selected. Select all that apply. 1. Loose electrical leads to the monitor 2. Cardiac tamponade 3. Tension pneumothorax 4. Profound hypovolemia 5. Spinal cord injury Correct Answer: 2,3,4 Rationale 1: The patient has a rhythm but no pulse. The monitor is working correctly. Rationale 2: Cardiac tamponade would cause standstill of the heart so no pulse would be generated, but electrical activity would still be present for a period of time. Rationale 3: Tension pneumothorax can result in mediastinal shift, which would reduce or stop the flow of blood from the heart. This can make pulses very weak or absent. Electrical activity would be present for a period of time. Rationale 4: If hypovolemia is profound, there is little venous return to the heart, resulting in very diminished cardiac output. Pulses would be very weak or absent. Electrical activity would be present for a period of time. Rationale 5: Spinal cord injury would result in paralysis and might affect cardiac status but would not be characterized by pulseless electrical activity. Question 102 A patient is admitted to the ED with massive trauma. What nursing intervention will help protect this patient from coagulopathy? 1. Start oxygen immediately. 2. Cover the patient with a blanket. 3. Place a pillow under the patient’s feet. 4. Use sterile technique for all invasive procedures. Correct Answer: 2 Rationale 1: The patient does need immediate supplementary oxygen, but this will not protect against coagulopathy. Rationale 2: Hypothermia increases the risk for coagulopathy and mortality. Rationale 3: Elevating the patient’s feet is not significant to the prevention of coagulopathy. Rationale 4: The nurse should use sterile technique for invasive procedures, but this will not protect against coagulopathy. [Show More]
Last updated: 1 year ago
Preview 1 out of 52 pages
Reviews( 0 )
Document information
Connected school, study & course
About the document
Uploaded On
Mar 21, 2021
Number of pages
52
Written in
Additional information
This document has been written for:
Uploaded
Mar 21, 2021
Downloads
0
Views
68


.png)

 (1).png)
 (1).png)
 (1).png)
 (1).png)

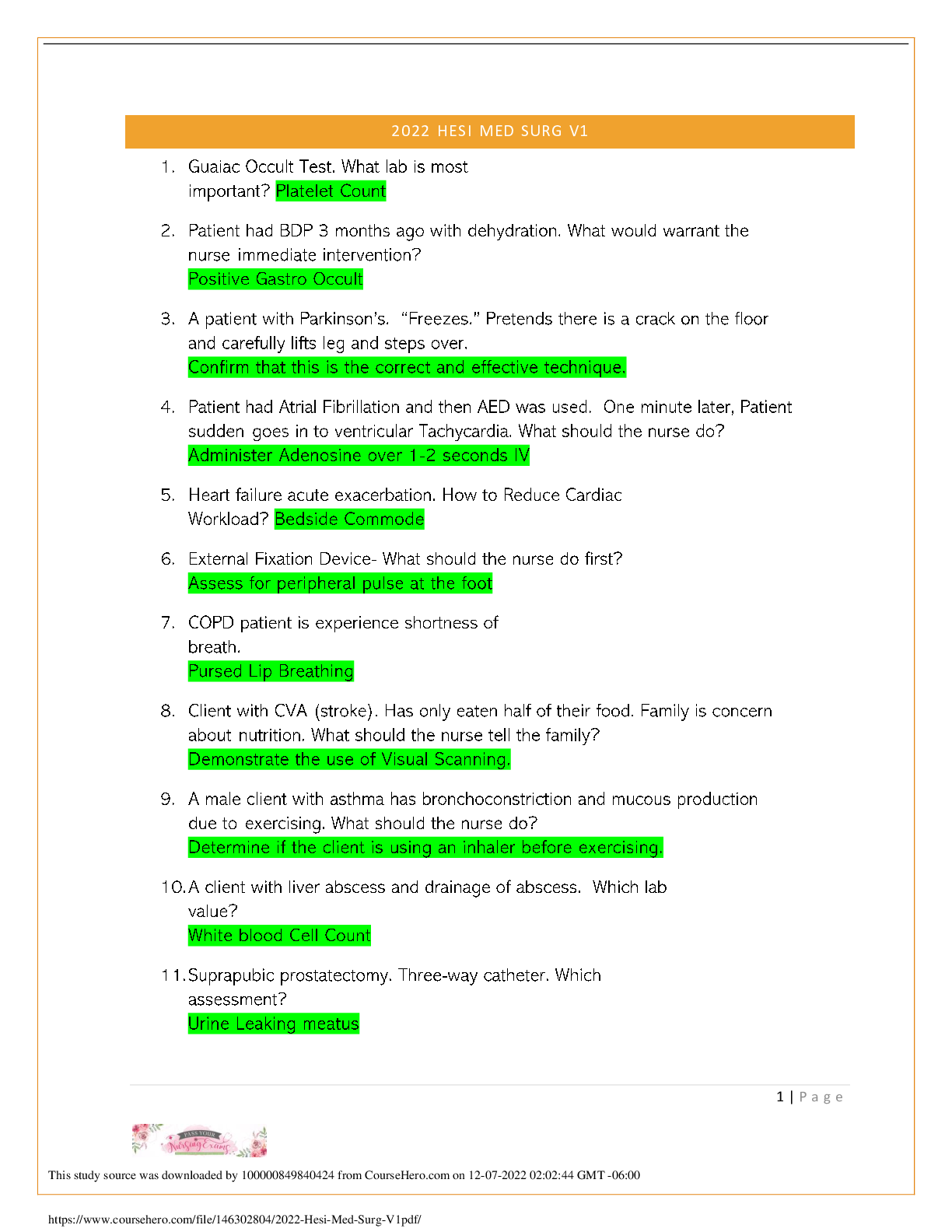
 (1).png)

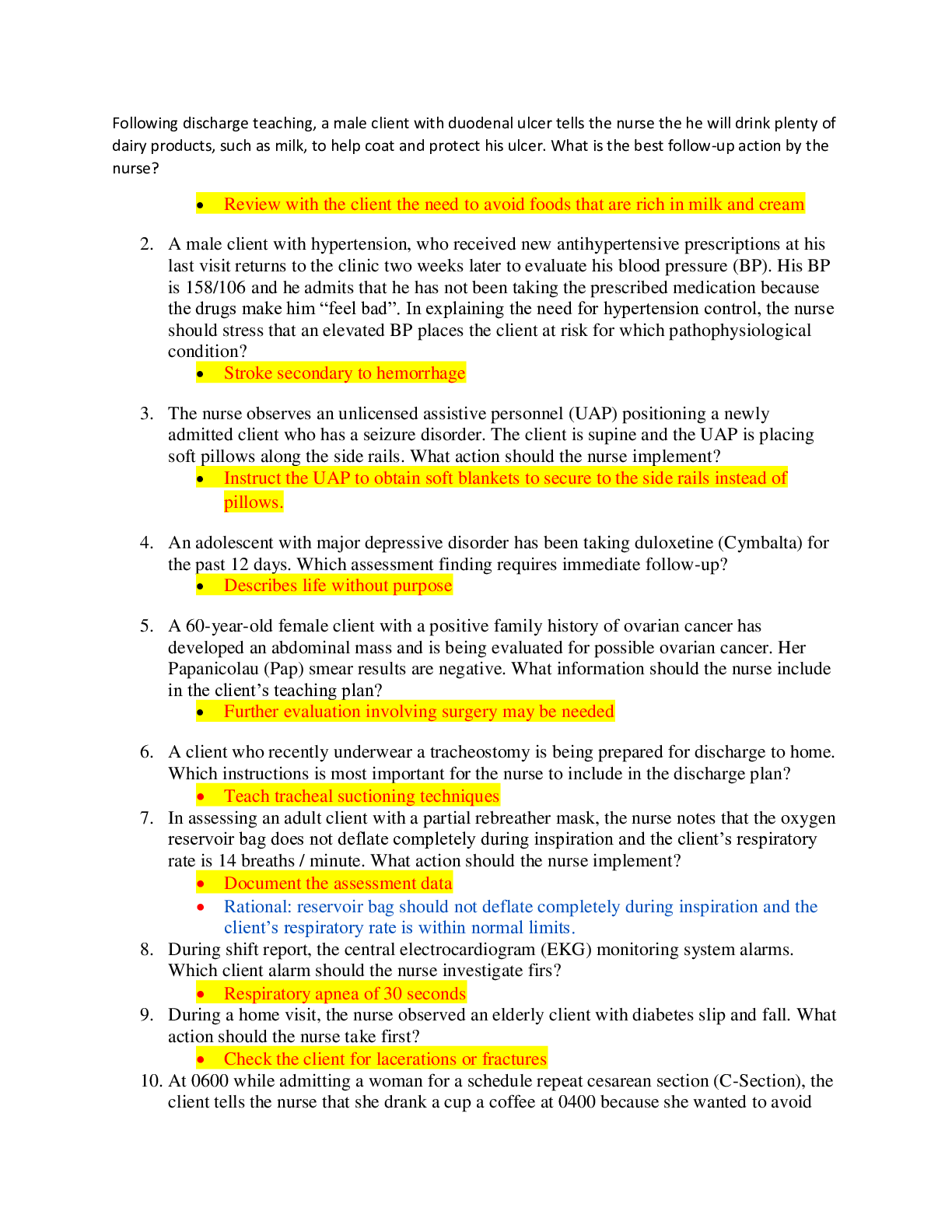
 Test Bank.png)
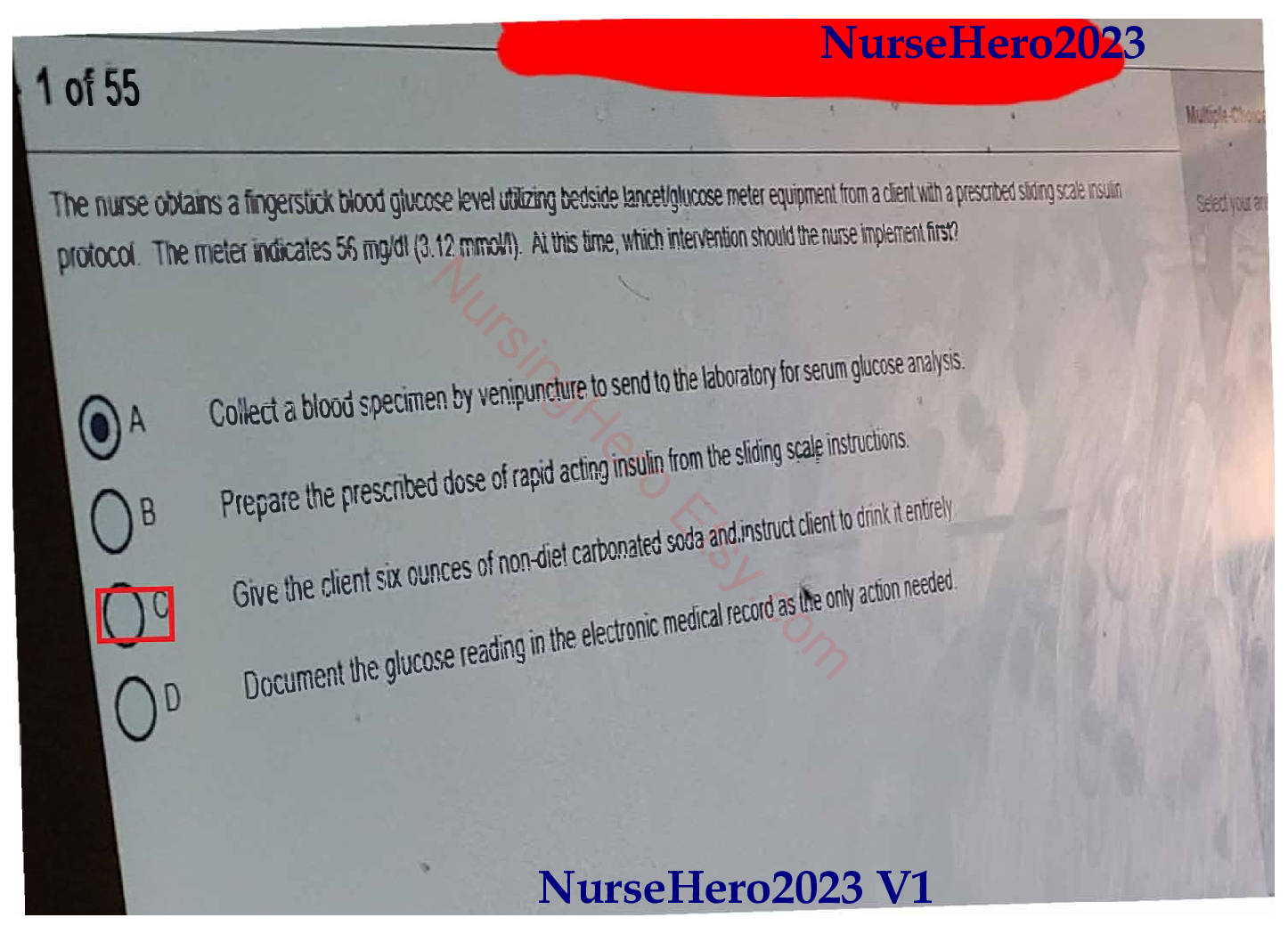
.png)

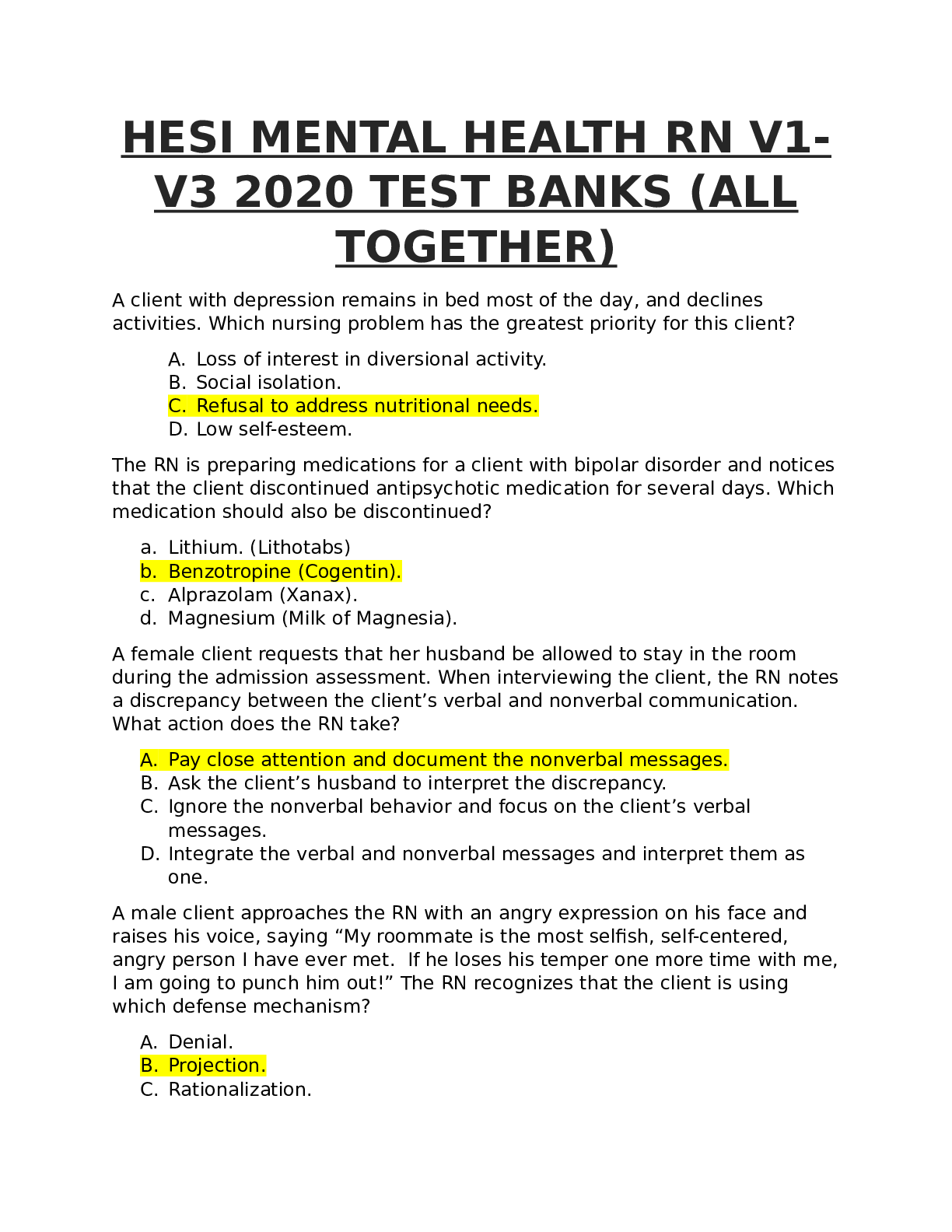
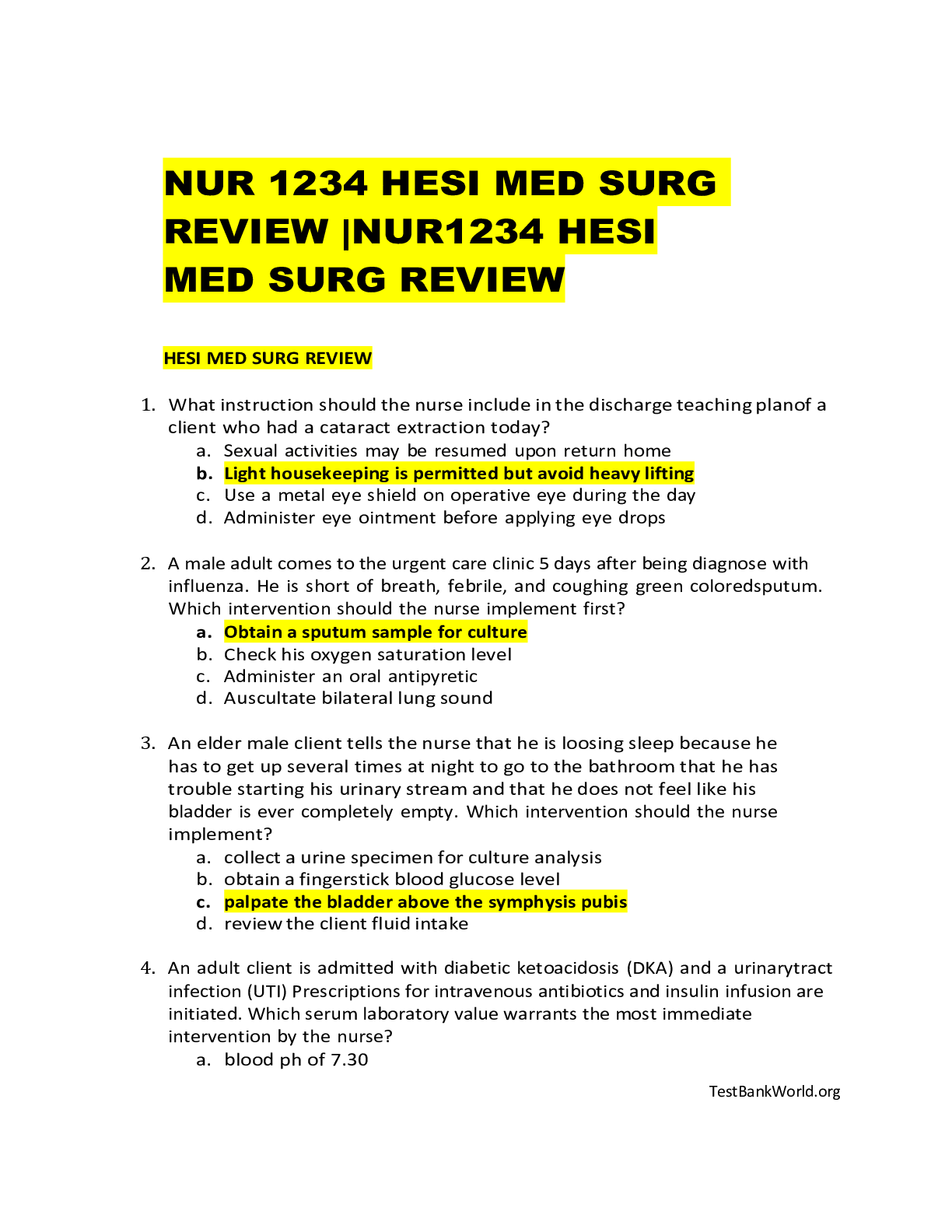
.png)
 Correct Study Guide, Download to Score A.png)