*NURSING > HESI MED SURG > NURSING MED SURG Exam 2 required to ace your tests (All)
NURSING MED SURG Exam 2 required to ace your tests
Document Content and Description Below
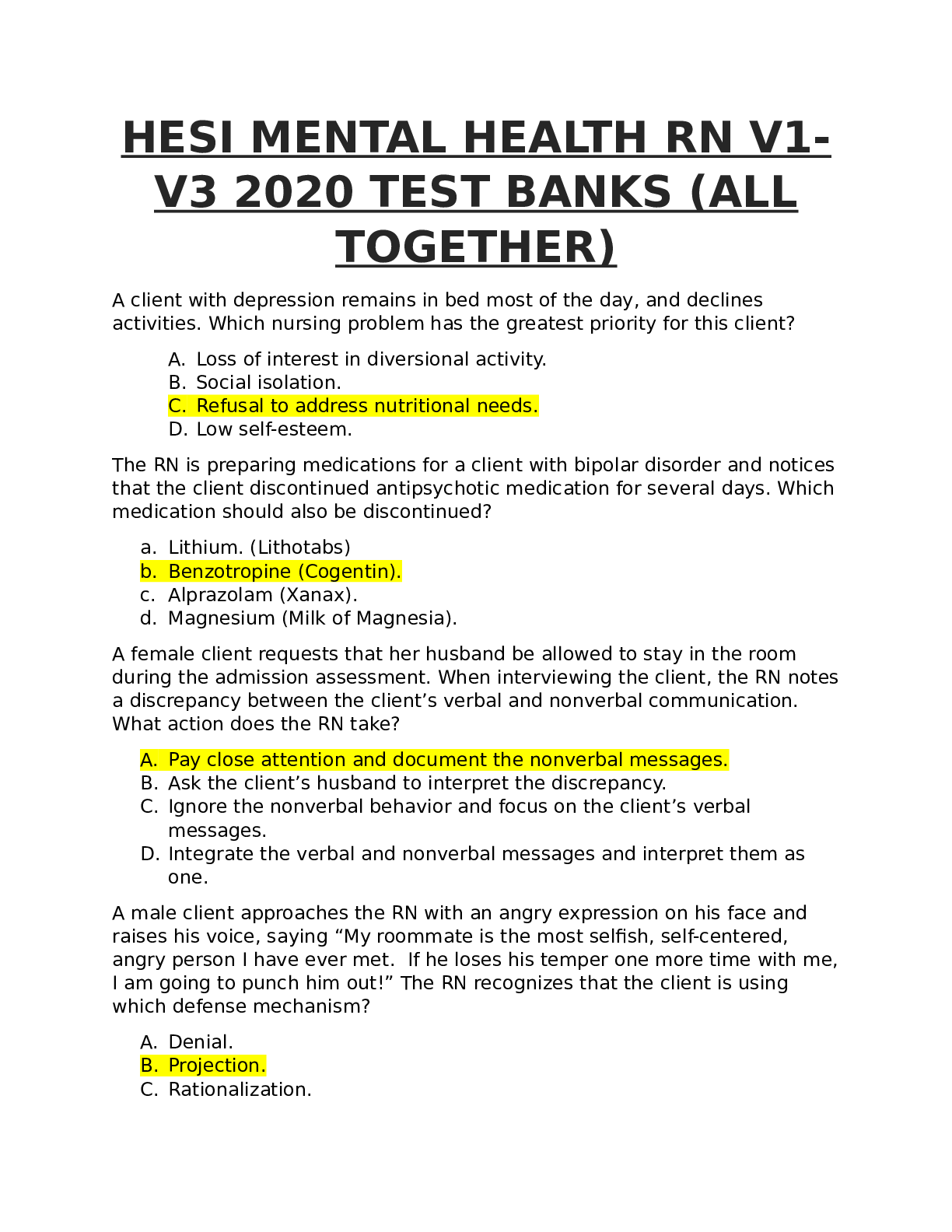
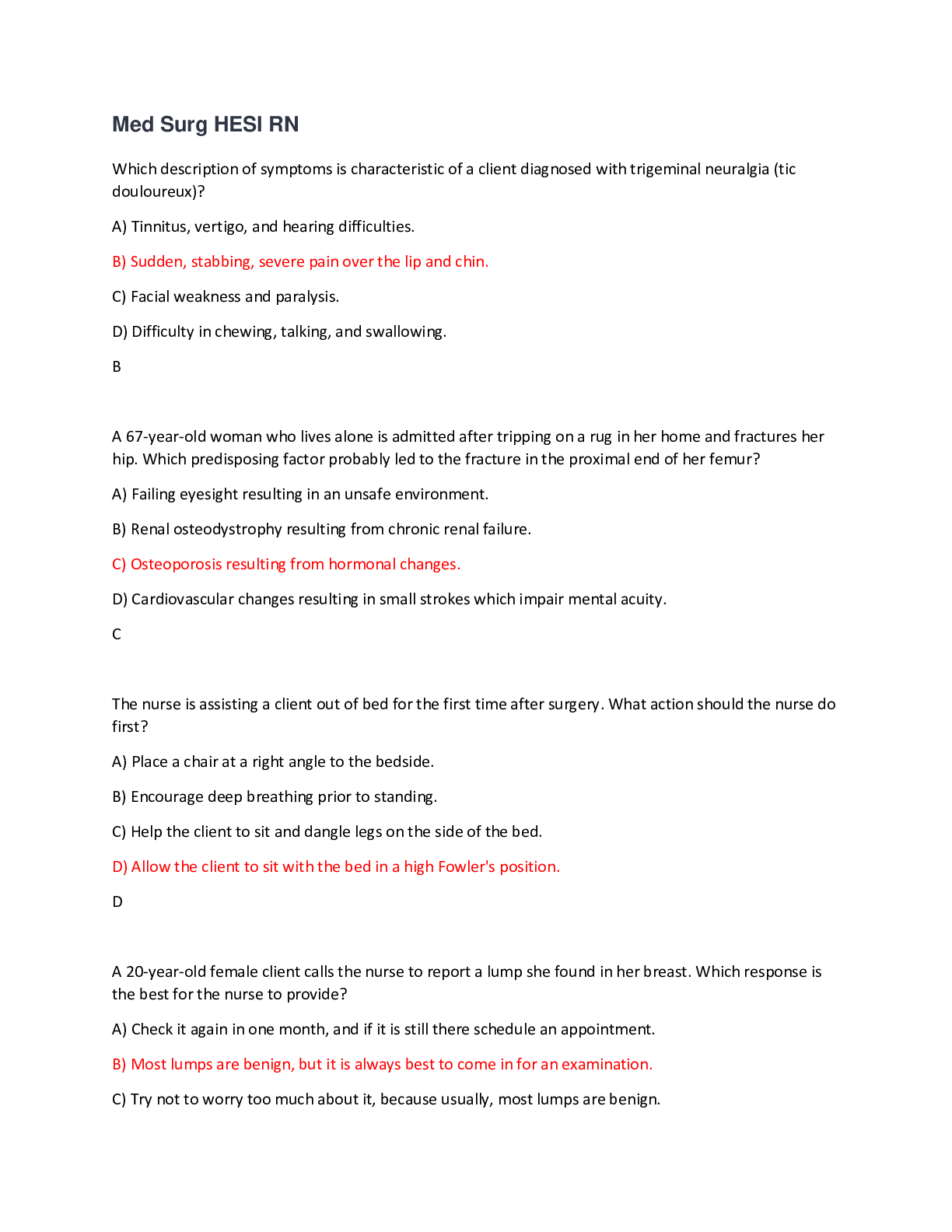
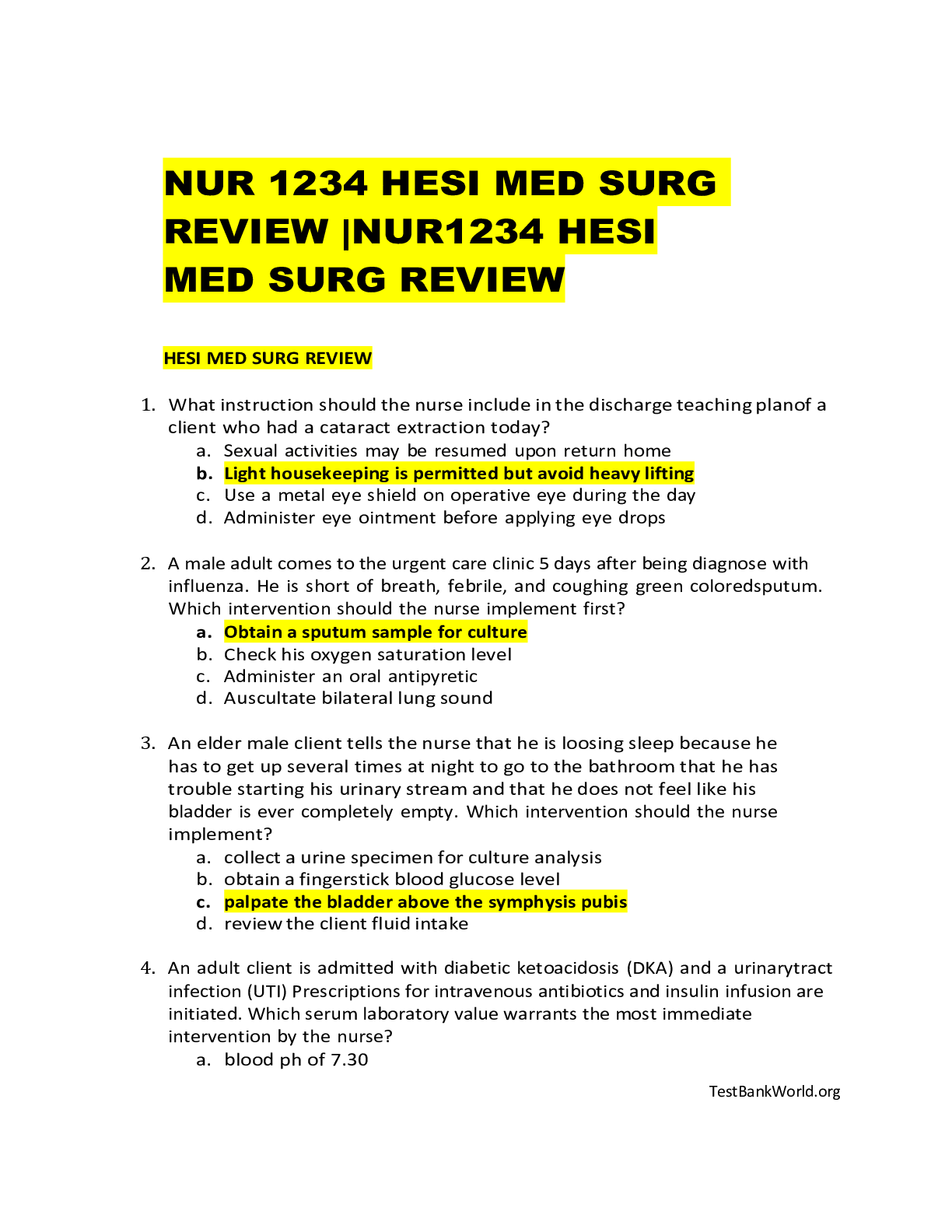
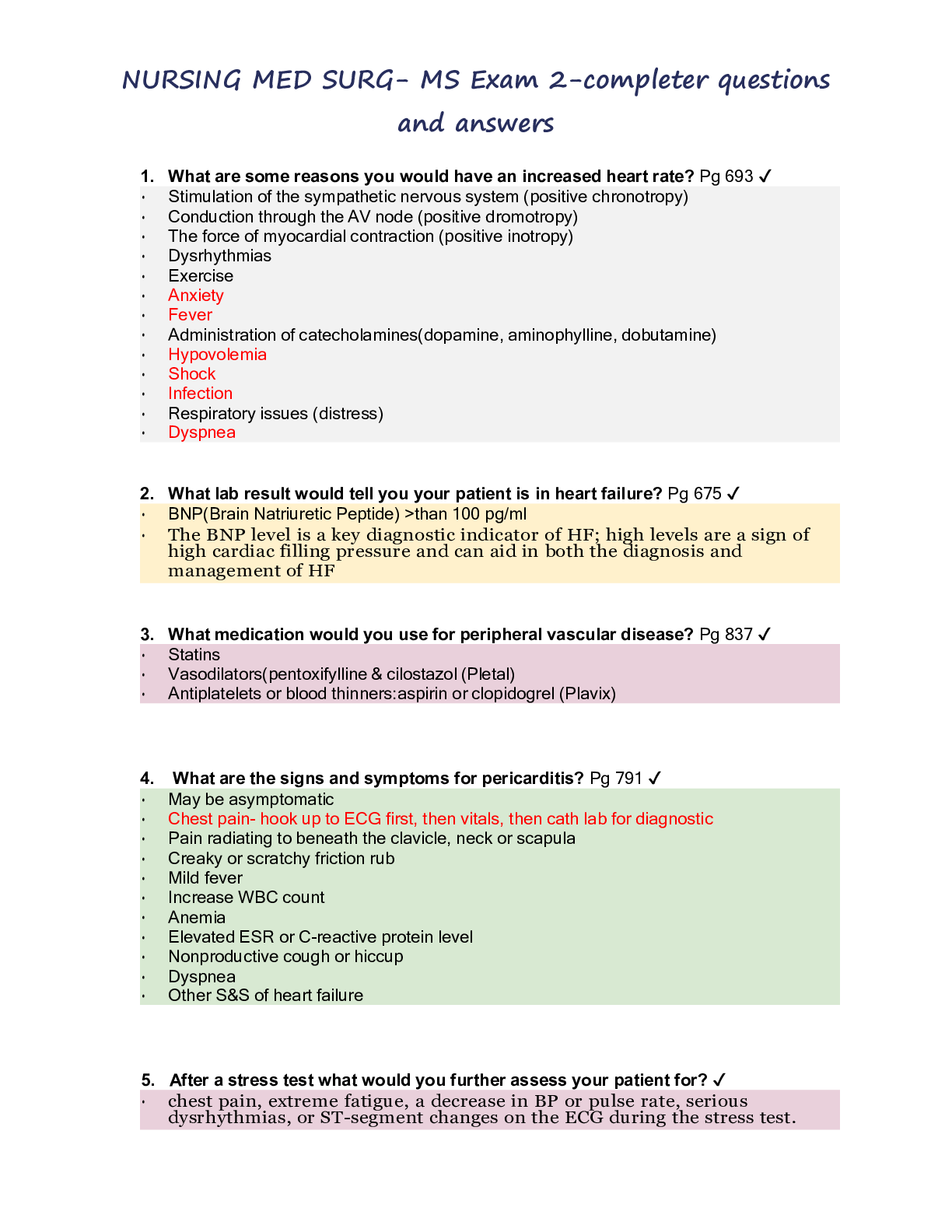
1. What are some reasons you would have an increased heart rate? Pg 693 ✔ Stimulation of the sympathetic nervous system (positive chronotropy) Conduction through the AV node (positive drom... otropy) The force of myocardial contraction (positive inotropy) Dysrhythmias Exercise Anxiety Fever Administration of catecholamines(dopamine, aminophylline, dobutamine) Hypovolemia Shock Infection Respiratory issues (distress) Dyspnea 2. What lab result would tell you your patient is in heart failure? Pg 675 ✔ BNP(Brain Natriuretic Peptide) >than 100 pg/ml The BNP level is a key diagnostic indicator of HF; high levels are a sign of high cardiac filling pressure and can aid in both the diagnosis and management of HF 3. What medication would you use for peripheral vascular disease? Pg 837 ✔ Statins Vasodilators(pentoxifylline & cilostazol (Pletal) Antiplatelets or blood thinners:aspirin or clopidogrel (Plavix) 4. What are the signs and symptoms for pericarditis? Pg 791 ✔ May be asymptomatic Chest pain- hook up to ECG first, then vitals, then cath lab for diagnostic Pain radiating to beneath the clavicle, neck or scapula Creaky or scratchy friction rub Mild fever Increase WBC count Anemia Elevated ESR or C-reactive protein level Nonproductive cough or hiccup Dyspnea Other S&S of heart failure 5. After a stress test what would you further assess your patient for? ✔ chest pain, extreme fatigue, a decrease in BP or pulse rate, serious dysrhythmias, or ST-segment changes on the ECG during the stress test. Facial flushing, chest discomfort, anxiety, ischemia, ↑HR(vitals, ECG), rest, atropine-dilates. ASSESS-ASSESS If chest discomfort persist during stress test: stop test, ECG, vitals 5. Define murmur ✔ Sounds created by abnormal, turbulent flow of blood in heart Intensity A grading system is used to describe the intensity or loudness of a murmur. Grade 1: Very faint and difficult for the inexperienced clinician to hear Grade 2: Quiet but readily perceived by the experienced clinician Grade 3: Moderately loud Grade 4: Loud and may be associated with a thrill Grade 5: Very loud; heard when stethoscope is partially off the chest; associated with a thrill Grade 6: Extremely loud; detected with the stethoscope off the chest; associated with a thrill 6. Patient teaching before, during, and after, cardiac catheterization. ✔ Nursing responsibilities before cardiac catheterization include: • Instructing the patient to fast, usually for 8 to 12 hours, before the procedure • Informing patient that if catheterization is to be performed as an outpatient procedure, a friend, family member, or other responsible person must transport the patient home • Informing the patient about the expected duration of the procedure and advising that it will involve lying on a hard table for less than 2 hours • Reassuring the patient that IV medications are given to maintain comfort • Informing the patient about sensations that will be experienced during the catheterization. Knowing what to expect can help the patient cope with the experience. The nurse explains that an occasional pounding sensation (palpitation) may be felt in the chest because of extra heartbeats that almost always occur, particularly when the catheter tip touches the endocardium. The patient may be asked to cough and to breathe deeply, especially after the injection of contrast agent. Coughing may help disrupt a dysrhythmia and clear the contrast agent from the arteries. Breathing deeply and holding the breath help lower the diaphragm for better visualization of heart structures. The injection of a contrast agent into either side of the heart may produce a flushed feeling throughout the body and a sensation similar to the need to void, which subsides in 1 minute or less. • Encouraging the patient to express fears and anxieties. The nurse provides education and reassurance to reduce apprehension. Nursing responsibilities after cardiac catheterization are dictated by hospital policy and primary provider preferences and may include: • Observing the catheter access site for bleeding or hematoma formation and assessing peripheral pulses in the affected extremity (dorsalis pedis and posterior tibial pulses in the lower extremity, radial pulse in the upper extremity) every 15 minutes for 1 hour, every 30 minutes for 1 hour, and hourly for 4 hours or until discharge. BP and heart rate are also assessed during these same time intervals. However, a recent study did not find an association between changes in these vital signs and bleeding complications (Mert, Intepeler, Bengu, et al., 2012). These results suggest that the best method for discovering bleeding is through frequent nursing assessments of the catheter access site (Chart 25-5). • Evaluating temperature, color, and capillary refill of the affected extremity during these same time intervals. The patient is assessed for affected extremity pain, numbness, or tingling sensations that may indicate arterial insufficiency. The best technique to use is to compare the examination findings between the affected and unaffected extremities. Any changes are reported promptly. • Screening carefully for dysrhythmias by observing the cardiac monitor or by assessing the apical and peripheral pulses for changes in rate and rhythm. A vasovagal reaction, consisting of bradycardia, hypotension, and nausea, can be precipitated by a distended bladder or by discomfort from manual pressure that is applied during removal of an arterial or venous catheter. The vasovagal response is reversed by promptly elevating the lower extremities above the level of the heart, infusing a bolus of IV fluid, and administering IV atropine to treat the bradycardia. • Maintaining bed rest for 2 to 6 hours after the procedure. If manual pressure or a mechanical device was used during a femoral artery approach, the patient remains on bed rest for up to 6 hours with the affected leg straight and the head of the bed elevated no greater than 30 degrees (Weigand, 2011). For comfort, the patient may be turned from side to side with the affected extremity straight. If a percutaneous vascular closure device or patch was deployed, the nurse checks local nursing care standards and anticipates that the patient will have fewer activity restrictions. The patient may be permitted to ambulate within 2 hours (Hammel, 2009). If the radial artery was accessed, the patient remains on bed rest for 2 to 3 hours or until the effects of sedation have dissipated. The patient may sit up in bed. A hemostasis band or pressure dressing may be applied over the catheter access site. Analgesic medication is administered as prescribed for discomfort. Patients are instructed to avoid repetitive movement of the affected extremity for 24 to 48 hours (Durham, 2012). Patients are instructed to avoid sleeping on the affected arm for 24 hours. • Instructing the patient to report chest pain and bleeding or sudden discomfort from the catheter insertion sites promptly • Monitoring the patient for contrast agent–induced nephropathy by observing for elevations in serum creatinine levels. Oral and IV hydration is used to increase urinary output and flush the contrast agent from the urinary tract; accurate oral and IV intake and urinary output are recorded. • Ensuring patient safety by instructing the patient to ask for help when getting out of bed the first time after the procedure. The patient is monitored for bleeding from the catheter access site and for orthostatic hypotension, indicated by complaints of dizziness or lightheadedness (Wiegand, 2011;Woods et al., 200 7. Know about the electric conductivity of the heart. (pg.691) ✔ Electrical impulses initiated at the SA node (pacemaker) 60-100 causes atrial contraction AV nodes (40-60) coordinates the incoming electrical impulses and after a slight delay relays the impulse to the ventricles The impulse is conducted through the Bundle of His (30-40) , then divides into the right and left bundle branch Impulses reach the Purkinje fibers (30-40) which rapidly conduct the impulses through the thick walls of the ventricles 8. Patient teaching about coagulotherapy. Pg 851 ✔ Avoid procedures/activities that can increase intracranial pressure (coughing, straining) Avoid meds that interfere with coagulation therapy (aspirin, NSAIDs, beta-lactam antibiotics) Avoid rectal probes, rectal meds Avoid IM injections Monitor amount of external bleeding Oral hygiene carefully (soft toothbrush) Take the anticoagulant at the same time every day and notify doctor if any signs of bleeding ( reddish or brownish urine, epistaxis, tarry stools) Ambulation, sequential com [Show More]
Last updated: 1 year ago
Preview 1 out of 27 pages
Reviews( 0 )
Document information
Connected school, study & course
About the document
Uploaded On
Mar 26, 2021
Number of pages
27
Written in
Additional information
This document has been written for:
Uploaded
Mar 26, 2021
Downloads
0
Views
39


 Test Bank.png)
.png)