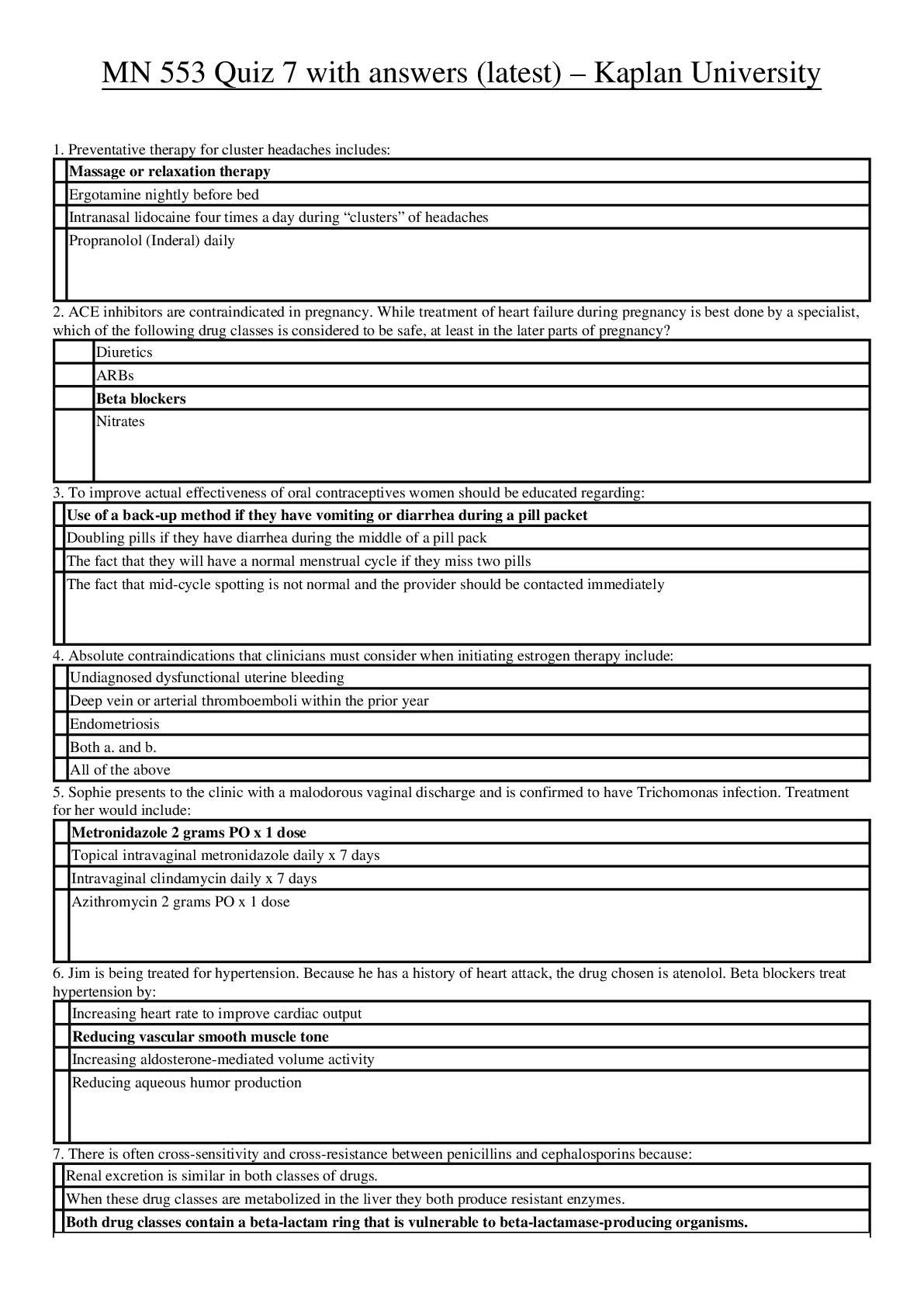
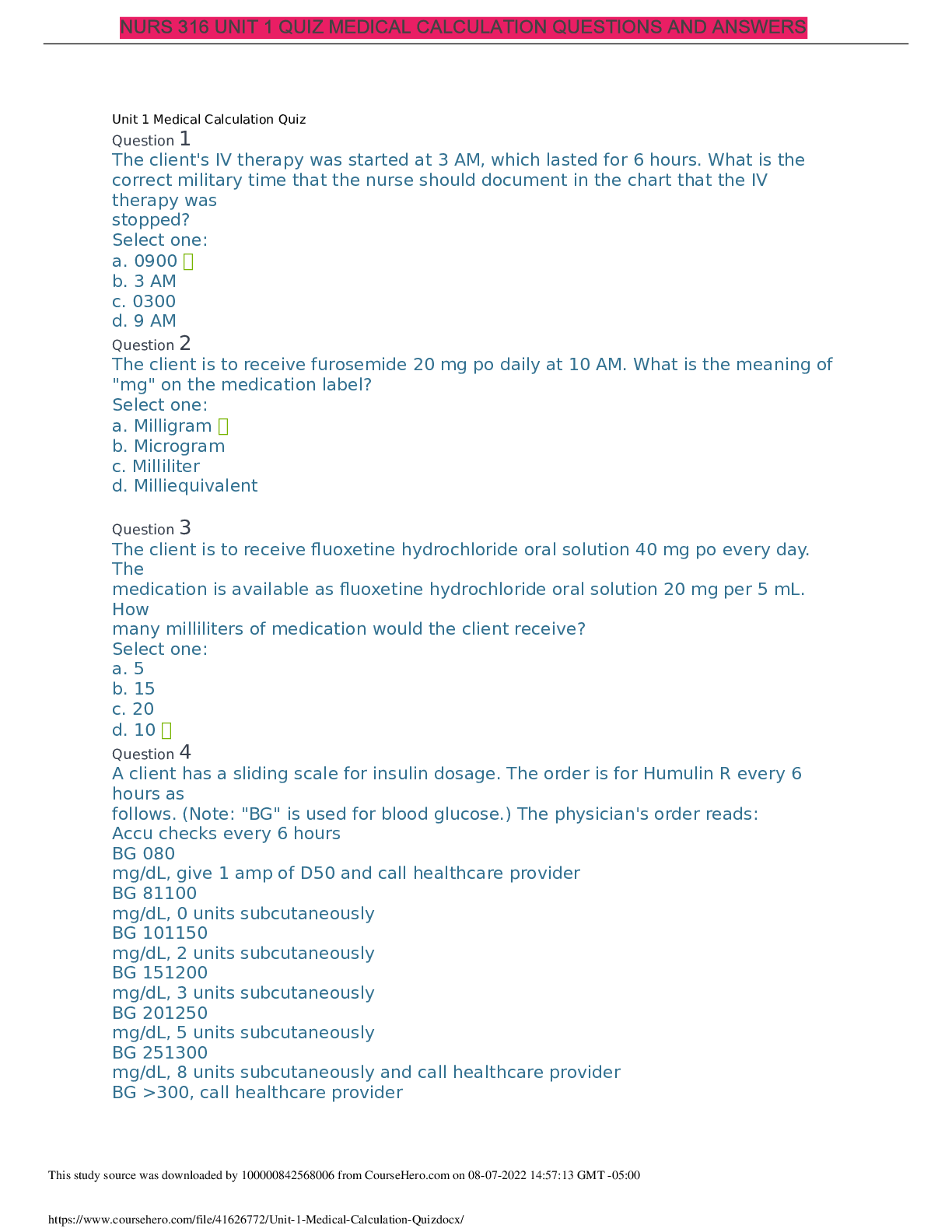
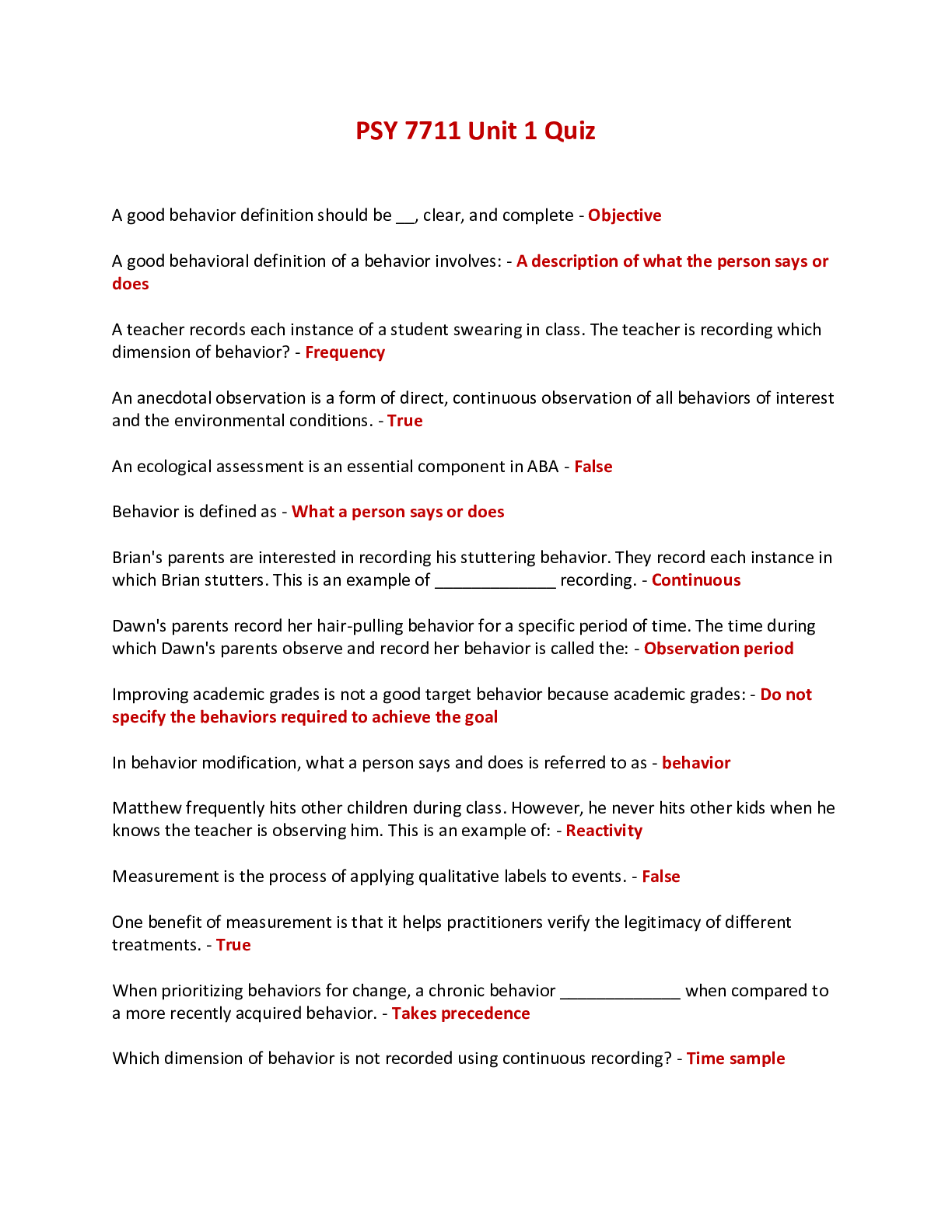
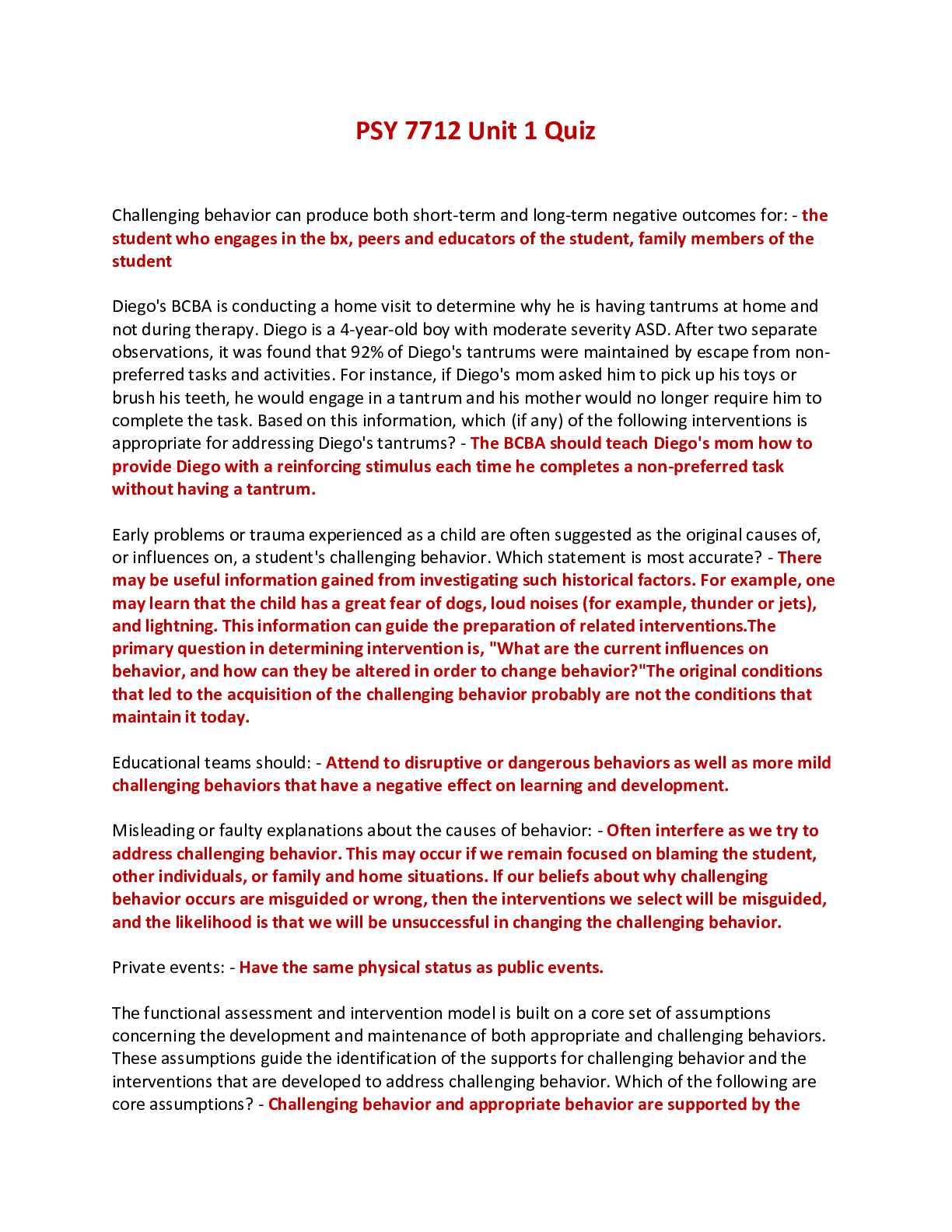
*NURSING > EXAM > MN 553 Unit 1 Quiz (Chapter 1 to 52) with answers (latest) – Kaplan University (All)
MN 553 Unit 1 Quiz (Chapter 1 to 52) with answers (latest) – Kaplan University
Document Content and Description Below
MN 553 Unit 1 Quiz (Chapter 1 to 52) with answers (latest) – Kaplan University Chapter 1. The Role of the Nurse Practitioner Multiple Choice Identify the choice that best completes the statem... ent or answers the question. ____ 1. Nurse practitioner prescriptive authority is regulated by: 1. The National Council of State Boards of Nursing 2. The U.S. Drug Enforcement Administration 3. The State Board of Nursing for each state 4. The State Board of Pharmacy ____ 2. The benefits to the patient of having an Advanced Practice Registered Nurse (APRN) prescriber include: 1. Nurses know more about Pharmacology than other prescribers because they take it both in their basic nursing program and in their APRN program. 2. Nurses care for the patient from a holistic approach and include the patient in decision making regarding their care. 3. APRNs are less likely to prescribe narcotics and other controlled substances. 4. APRNs are able to prescribe independently in all states, whereas a physician’s assistant needs to have a physician supervising their practice. ____ 3. Clinical judgment in prescribing includes: 1. Factoring in the cost to the patient of the medication prescribed 2. Always prescribing the newest medication available for the disease process 3. Handing out drug samples to poor patients 4. Prescribing all generic medications to cut costs ____ 4. Criteria for choosing an effective drug for a disorder include: 1. Asking the patient what drug they think would work best for them 2. Consulting nationally recognized guidelines for disease management 3. Prescribing medications that are available as samples before writing a prescription 4. Following U.S. Drug Enforcement Administration guidelines for prescribing ____ 5. Nurse practitioner practice may thrive under health-care reform because of: 1. The demonstrated ability of nurse practitioners to control costs and improve patient outcomes 2. The fact that nurse practitioners will be able to practice independently 3. The fact that nurse practitioners will have full reimbursement under health-care reform 4. The ability to shift accountability for Medicaid to the state level Chapter 2. Review of Basic Principles of Pharmacology Multiple Choice Identify the choice that best completes the statement or answers the question. ____ 1. A patient’s nutritional intake and laboratory results reflect hypoalbuminemia. This is critical to prescribing because: 1. Distribution of drugs to target tissue may be affected. 2. The solubility of the drug will not match the site of absorption. 3. There will be less free drug available to generate an effect. 4. Drugs bound to albumin are readily excreted by the kidneys. ____ 2. Drugs that have a significant first-pass effect: 1. Must be given by the enteral (oral) route only 2. Bypass the hepatic circulation 3. Are rapidly metabolized by the liver and may have little if any desired action 4. Are converted by the liver to more active and fat-soluble forms ____ 3. The route of excretion of a volatile drug will likely be the: 1. Kidneys 2. Lungs 3. Bile and feces 4. Skin ____ 4. Medroxyprogesterone (Depo Provera) is prescribed intramuscularly (IM) to create a storage reservoir of the drug. Storage reservoirs: 1. Assure that the drug will reach its intended target tissue 2. Are the reason for giving loading doses 3. Increase the length of time a drug is available and active 4. Are most common in collagen tissues ____ 5. The NP chooses to give cephalexin every 8 hours based on knowledge of the drug’s: 1. Propensity to go to the target receptor 2. Biological half-life 3. Pharmacodynamics 4. Safety and side effects ____ 6. Azithromycin dosing requires that the first day’s dosage be twice those of the other 4 days of the prescription. This is considered a loading dose. A loading dose: 1. Rapidly achieves drug levels in the therapeutic range 2. Requires four- to five-half-lives to attain 3. Is influenced by renal function 4. Is directly related to the drug circulating to the target tissues ____ 7. The point in time on the drug concentration curve that indicates the first sign of a therapeutic effect is the: 1. Minimum adverse effect level 2. Peak of action 3. Onset of action 4. Therapeutic range ____ 8. Phenytoin requires that a trough level be drawn. Peak and trough levels are done: 1. When the drug has a wide therapeutic range 2. When the drug will be administered for a short time only 3. When there is a high correlation between the dose and saturation of receptor sites 4. To determine if a drug is in the therapeutic range ____ 9. A laboratory result indicates that the peak level for a drug is above the minimum toxic concentration. This means that the: 1. Concentration will produce therapeutic effects 2. Concentration will produce an adverse response 3. Time between doses must be shortened 4. Duration of action of the drug is too long ____ 10. Drugs that are receptor agonists may demonstrate what property? 1. Irreversible binding to the drug receptor site 2. Upregulation with chronic use 3. Desensitization or downregulation with continuous use 4. Inverse relationship between drug concentration and drug action ____ 11. Drugs that are receptor antagonists, such as beta blockers, may cause: 1. Downregulation of the drug receptor 2. An exaggerated response if abruptly discontinued 3. Partial blockade of the effects of agonist drugs 4. An exaggerated response to competitive drug agonists ____ 12. Factors that affect gastric drug absorption include: 1. Liver enzyme activity 2. Protein-binding properties of the drug molecule 3. Lipid solubility of the drug 4. Ability to chew and swallow ____ 13. Drugs administered via IV: 1. Need to be lipid soluble in order to be easily absorbed 2. Begin distribution into the body immediately 3. Are easily absorbed if they are nonionized 4. May use pinocytosis to be absorbed ____ 14. When a medication is added to a regimen for a synergistic effect, the combined effect of the drugs is: 1. The sum of the effects of each drug individually 2. Greater than the sum of the effects of each drug individually 3. Less than the effect of each drug individually 4. Not predictable, as it varies with each individual ____ 15. Which of the following statements about bioavailability is true? 1. Bioavailability issues are especially important for drugs with narrow therapeutic ranges or sustained-release mechanisms. 2. All brands of a drug have the same bioavailability. 3. Drugs that are administered more than once a day have greater bioavailability than drugs given once daily. 4. Combining an active drug with an inert substance does not affect bioavailability. ____ 16. Which of the following statements about the major distribution barriers (blood-brain or fetal-placental) is true? 1. Water soluble and ionized drugs cross these barriers rapidly. 2. The blood-brain barrier slows the entry of many drugs into and from brain cells. 3. The fetal-placental barrier protects the fetus from drugs taken by the mother. 4. Lipid-soluble drugs do not pass these barriers and are safe for pregnant women. ____ 17. Drugs are metabolized mainly by the liver via phase I or phase II reactions. The purpose of both of these types of reactions is to: 1. Inactivate prodrugs before they can be activated by target tissues 2. Change the drugs so they can cross plasma membranes 3. Change drug molecules to a form that an excretory organ can excrete 4. Make these drugs more ionized and polar to facilitate excretion ____ 18. Once they have been metabolized by the liver, the metabolites may be: 1. More active than the parent drug 2. Less active than the parent drug 3. Totally “deactivated” so they are excreted without any effect 4. All of the above ____ 19. All drugs continue to act in the body until they are changed or excreted. The ability of the body to excrete drugs via the renal system would be increased by: 1. Reduced circulation and perfusion of the kidney 2. Chronic renal disease 3. Competition for a transport site by another drug 4. Unbinding a nonvolatile drug from plasma proteins ____ 20. Steady state is: 1. The point on the drug concentration curve when absorption exceeds excretion 2. When the amount of drug in the body remains constant 3. When the amount of drug in the body stays below the minimum toxic concentration 4. All of the above ____ 21. Two different pain medications are given together for pain relief. The drug—drug interaction is: 1. Synergistic 2. Antagonistic 3. Potentiative 4. Additive ____ 22. Actions taken to reduce drug—drug interaction problems include all of the following EXCEPT: 1. Reducing the dosage of one of the drugs 2. Scheduling their administration at different times 3. Prescribing a third drug to counteract the adverse reaction of the combination 4. Reducing the dosage of both drugs ____ 23. Phase I oxidative-reductive processes of drug metabolism require certain nutritional elements. Which of the following would reduce or inhibit this process? 1. Protein malnutrition 2. Iron-deficiency anemia 3. Both 1 and 2 4. Neither 1 nor 2 ____ 24. The time required for the amount of drug in the body to decrease by 50% is called: 1. Steady state 2. Half-life 3. Phase II metabolism 4. Reduced bioavailability time ____ 25. An agonist activates a receptor and stimulates a response. When given frequently over time, the body may: 1. Upregulate the total number of receptors 2. Block the receptor with a partial agonist 3. Alter the drug’s metabolism 4. Downregulate the numbers of that specific receptor ____ 26. Drug antagonism is best defined as an effect of a drug that: 1. Leads to major physiological and psychological dependence 2. Is modified by the concurrent administration of another drug 3. Cannot be metabolized before another dose is administered 4. Leads to a decreased physiological response when combined with another drug ____ 27. Instructions to a client regarding self-administration of oral enteric-coated tablets should include which of the following statements? 1. “Avoid any other oral medicines while taking this drug.” 2. “If swallowing this tablet is difficult, dissolve it in 3 ounces of orange juice.” 3. “The tablet may be crushed if you have any difficulty taking it.” 4. “To achieve best effect, take the tablet with at least 8 ounces of fluid.” ____ 28. The major reason for not crushing a sustained-release capsule is that, if crushed, the coated beads of the drugs could possibly result in: 1. Disintegration 2. Toxicity 3. Malabsorption 4. Deterioration ____ 29. Which of the following substances is the most likely to be absorbed in the intestines rather than in the stomach? 1. Sodium bicarbonate 2. Ascorbic acid 3. Salicylic acid 4. Glucose ____ 30. Which of the following variables is a factor in drug absorption? 1. The smaller the surface area for absorption, the more rapidly the drug is absorbed. 2. A rich blood supply to the area of absorption leads to better absorption. 3. The less soluble the drug, the more easily it is absorbed. 4. Ionized drugs are easily absorbed across the cell membrane. ____ 31. An advantage of prescribing a sublingual medication is that the medication is: 1. Absorbed rapidly 2. Excreted rapidly 3. Metabolized minimally 4. Distributed equally ____ 32. Drugs that use CYP 3A4 isoenzymes for metabolism may: 1. Induce the metabolism of another drug 2. Inhibit the metabolism of another drug 3. Both 1 and 2 4. Neither 1 nor 2 ____ 33. Therapeutic drug levels are drawn when a drug reaches steady state. Drugs reach steady state: 1. After the second dose 2. After four to five half-lives 3. When the patient feels the full effect of the drug 4. One hour after IV administration ____ 34. Upregulation or hypersensitization may lead to: 1. Increased response to a drug 2. Decreased response to a drug 3. An exaggerated response if the drug is withdrawn 4. Refractoriness or complete lack of response Chapter 3. Rational Drug Selection Multiple Choice Identify the choice that best completes the statement or answers the question. ____ 1. An NP would prescribe the liquid form of ibuprofen for a 6-year-old child because: 1. Drugs given in liquid form are less irritating to the stomach. 2. A 6-year-old child may have problems swallowing a pill. 3. Liquid forms of medication eliminate the concern for first-pass effect. 4. Liquid ibuprofen does not have to be dosed as often as the tablet form. ____ 2. In deciding which of multiple drugs used to use to treat a condition, the NP chooses Drug A because it: 1. Has serious side effects and it is not being used for a life-threatening condition 2. Will be taken twice daily and will be taken at home 3. Is expensive, but covered by health insurance 4. None of these are important in choosing a drug ____ 3. A client asks the NP about the differences in drug effects between men and women. What is known about the differences between the pharmacokinetics of men and women? 1. Body temperature varies between men and women. 2. Muscle mass is greater in women. 3. Percentage of fat differs between genders. 4. Proven subjective factors exist between the genders. ____ 4. The first step in the prescribing process according to the World Health Organization is: 1. Choosing the treatment 2. Educating the patient about the medication 3. Diagnosing the patient’s problem 4. Starting the treatment ____ 5. Treatment goals in prescribing should: 1. Always be curative 2. Be patient-centered 3. Be convenient for the provider 4. Focus on the cost of therapy ____ 6. The therapeutic goals when prescribing include(s): 1. Curative 2. Palliative 3. Preventive 4. All of the above ____ 7. When determining drug treatment the NP prescriber should: 1. Always use evidence-based guidelines 2. Individualize the drug choice for the specific patient 3. Rely on his or her experience when prescribing for complex patients 4. Use the newest drug on the market for the condition being treated ____ 8. Patient education regarding prescribed medication includes: 1. Instructions written at the high school reading level 2. Discussion of expected adverse drug reactions 3. How to store leftover medication such as antibiotics 4. Verbal instructions always in English ____ 9. Passive monitoring of drug effectiveness includes: 1. Therapeutic drug levels 2. Adding or subtracting medications from the treatment regimen 3. Ongoing provider visits 4. Instructing the patient to report if the drug is not effective ____ 10. Pharmacokinetic factors that affect prescribing include: 1. Therapeutic index 2. Minimum effective concentration 3. Bioavailability 4. Ease of titration ____ 11. Pharmaceutical promotion may affect prescribing. To address the impact of pharmaceutical promotion, the following recommendations have been made by the Institute of Medicine: 1. Conflicts of interest and financial relationships should be disclosed by those providing education. 2. Providers should ban all pharmaceutical representatives from their office setting. 3. Drug samples should be used for patients who have the insurance to pay for them, to ensure the patient can afford the medication. 4. Providers should only accept low-value gifts, such as pens and pads of paper, from the pharmaceutical representative. ____ 12. Under new U.S. Food and Drug Administration labeling, Pregnancy Categories will be: 1. Strengthened with a new coding such as C+ or C- to discern when a drug is more or less toxic to the fetus 2. Changed to incorporate a pregnancy risk summary and clinical considerations on the drug label 3. Eliminated, and replaced with a link to the National Library of Medicine TOXNET Web site for in-depth information regarding pregnancy concerns 4. Clarified to include information such as safe dosages in each trimester of pregnancy Chapter 4. Legal and Professional Issues in Prescribing Multiple Choice Identify the choice that best completes the statement or answers the question. ____ 1. The U.S. Food and Drug Administration regulates: 1. Prescribing of drugs by MDs and NPs 2. The official labeling for all prescription and over-the-counter drugs 3. Off-label recommendations for prescribing 4. Pharmaceutical educational offerings ____ 2. The U.S. Food and Drug Administration approval is required for: 1. Medical devices, including artificial joints 2. Over-the-counter vitamins 3. Herbal products, such as St John’s wort 4. Dietary supplements, such as Ensure ____ 3. An Investigational New Drug is filed with the U.S. Food and Drug Administration: 1. When the manufacturer has completed phase III trials 2. When a new drug is discovered 3. Prior to animal testing of any new drug entity 4. Prior to human testing of any new drug entity ____ 4. Phase IV clinical trials in the United States are also known as: 1. Human bioavailability trials 2. Postmarketing research 3. Human safety and efficacy studies 4. The last stage of animal trials before the human trials begin ____ 5. Off-label prescribing is: 1. Regulated by the U.S. Food and Drug Administration 2. Illegal by NPs in all states (provinces) 3. Legal if there is scientific evidence for the use 4. Regulated by the Drug Enforcement Administration ____ 6. The U.S. Drug Enforcement Administration: 1. Registers manufacturers and prescribers of controlled substances 2. Regulates NP prescribing at the state level 3. Sanctions providers who prescribe drugs off-label 4. Provides prescribers with a number they can use for insurance billing ____ 7. Drugs that are designated Schedule II by the U.S. Drug Enforcement Administration: 1. Are known teratogens during pregnancy 2. May not be refilled; a new prescription must be written 3. Have a low abuse potential 4. May be dispensed without a prescription unless regulated by the state ____ 8. Precautions that should be taken when prescribing controlled substances include: 1. Faxing the prescription for a Schedule II drug directly to the pharmacy 2. Using tamper-proof paper for all prescriptions written for controlled drugs 3. Keeping any pre-signed prescription pads in a locked drawer in the clinic 4. Using only numbers to indicate the amount of drug to be prescribed ____ 9. Strategies prescribers can use to prevent misuse of controlled prescription drugs include: 1. Use of chemical dependency screening tools 2. Firm limit-setting regarding prescribing controlled substances 3. Practicing “just say no” to deal with patients who are pushing the provider to prescribe controlled substances 4. All of the above ____ 10. Behaviors predictive of addiction to controlled substances include: 1. Stealing or borrowing another patient’s drugs 2. Requiring increasing doses of opiates for pain associated with malignancy 3. Receiving refills of a Schedule II prescription on a regular basis 4. Requesting that only their own primary care provider prescribe for them ____ 11. Medication agreements or “Pain Medication Contracts” are recommended to be used: 1. Universally for all prescribing for chronic pain 2. For patients who have repeated requests for pain medication 3. When you suspect a patient is exhibiting drug-seeking behavior 4. For patients with pain associated with malignancy ____ 12. A prescription needs to be written for: 1. Legend drugs 2. Most controlled drugs 3. Medical devices 4. All of the above Chapter 6. Factors That Foster Positive Outcomes Multiple Choice Identify the choice that best completes the statement or answers the question. ____ 1. A comprehensive assessment of a patient should be holistic when trying to determine competence in drug administration. Which of the following factors would the NP omit from this type of assessment? 1. Financial status 2. Mobility 3. Social support 4. Sexual practices ____ 2. Elena Vasquez’s primary language is Spanish, and she speaks very limited English. Which technique would be appropriate to use in teaching her about a new drug you have just prescribed? 1. Use correct medical terminology because Spanish has a Latin base. 2. Use a family member who speaks more English to act as an interpreter. 3. Use a professional interpreter or a reliable staff member who can act as an interpreter. 4. Use careful, detailed explanations. ____ 3. Rod, age 68, has hearing difficulty. Which of the following would NOT be helpful in assuring that he understands teaching about his drug? 1. Stand facing him and speak slowly and clearly. 2. Speak in low tones or find a provider who has a lower voice. 3. Write down the instructions as well as speaking them. 4. If he reads lips, exaggerate lips movements when pronouncing the vowel sounds. ____ 4. Which of the following factors may adversely affect a patient’s adherence to a therapeutic drug regimen? 1. Complexity of the drug regimen 2. Patient perception of the potential adverse effects of the drugs 3. Both 1 and 2 4. Neither 1 nor 2 ____ 5. The health-care delivery system itself can create barriers to adherence to a treatment regimen. Which of the following system variables creates such a barrier? 1. Increasing copayments for care 2. Unrestricted formularies for drugs, including brand names 3. Increasing the number of people who have access to care 4. Treating a wider range of disorders ____ 6. Ralph’s blood pressure remains elevated despite increased doses of his drug. The NP is concerned that he might not be adhering to his treatment regimen. Which of the following events would suggest that he might not be adherent? 1. Ralph states that he always takes the drug “when I feel my pressure is going up.” 2. Ralph contacts his NP to discuss the need to increase the dosage. 3. Ralph consistently keeps his follow-up appointments to check his blood pressure. 4. All of the above show that he is adherent to the drug regimen. ____ 7. Nonadherence is especially common in drugs that treat asymptomatic conditions, such as hypertension. One way to reduce the likelihood of nonadherence to these drugs is to prescribe a drug that: 1. Has a short half-life so that missing one dose has limited effect 2. Requires several dosage titrations so that missed doses can be replaced with lower doses to keep costs down 3. Has a tolerability profile with fewer of the adverse effects that are considered “irritating,” such as nausea and dizziness 4. Must be taken no more than twice a day ____ 8. Factors in chronic conditions that contribute to nonadherence include: 1. The complexity of the treatment regimen 2. The length of time over which it must be taken 3. Breaks in the usual daily routine, such as vacations and weekends 4. All of the above ____ 9. While patient education about their drugs is important, information alone does not necessarily lead to adherence to a drug regimen. Patients report greater adherence when: 1. The provider spent a lot of time discussing the drugs with them 2. Their concerns and specific area of knowledge deficit were addressed 3. They were given written material, such as pamphlets, about the drugs 4. The provider used appropriate medical and pharmacological terms ____ 10. Patients with psychiatric illnesses have adherence rates to their drug regimen between 35% and 60%. To improve adherence in this population, prescribe drugs: 1. With a longer half-life so that missed doses produce a longer taper on the drug curve 2. In oral formulations that are more easily taken 3. That do not require frequent monitoring 4. Combined with patient education about the need to adhere even when symptoms are absent ____ 11. Many disorders require multiple drugs to treat them. The more complex the drug regimen, the less likely the patient will adhere to it. Which of the following interventions will NOT improve adherence? 1. Have the patient purchase a pill container with compartments for daily or multiple times-per-day dosing. 2. Match the clinic appointment to the next time the drug is to be refilled. 3. Write prescriptions for new drugs with shorter times between refills. 4. Give the patient a clear drug schedule that the provider devises to fit the characteristic of the drug. ____ 12. Pharmacologic interventions are costly. Patients for whom the cost/benefit variable is especially important include: 1. Older adults and those on fixed incomes 2. Patients with chronic illnesses 3. Patients with copayments for drugs on their insurance 4. Patients on public assistance ____ 13. Providers have a responsibility for determining the best plan of care, but patients also have responsibilities. Patients the provider can be assured will carry through on these responsibilities include those who: 1. Are well-educated and affluent 2. Have chronic conditions 3. Self-monitor drug effects on their symptoms 4. None of the above guarantee adherence ____ 14. Monitoring adherence can take several forms, including: 1. Patient reports from data in a drug diary 2. Pill counts 3. Laboratory reports and other diagnostic markers 4. All of the above ____ 15. Factors that explain and predict medication adherence include: 1. Social 2. Financial 3. Health system 4. All of the above Chapter 7. Cultural and Ethnic Influences in Pharmacotherapeutics Multiple Choice Identify the choice that best completes the statement or answers the question. ____ 1. Cultural factors that must be taken into account when prescribing include(s): 1. Who the decision maker is in the family regarding health-care decisions 2. The patient’s view of health and illness 3. Attitudes regarding the use of drugs to treat illness 4. All of the above ____ 2. Ethnic differences have been found in drug: 1. Absorption 2. Hepatic metabolism 3. Filtration at the glomerulus 4. Passive tubular reabsorption ____ 3. The National Standards of Culturally and Linguistically Appropriate Services are required to be implemented in all: 1. Hospitals 2. Clinics that serve the poor 3. Organizations that receive federal funds 4. Clinics that serve ethnic minorities ____ 4. According to the National Standards of Culturally and Linguistically Appropriate Services, an interpreter for health care: 1. May be a bilingual family member 2. May be a bilingual nurse or other health-care provider 3. Must be a professionally trained medical interpreter 4. Must be an employee of the organization ____ 5. According to the U.S. Office of Minority Health, poor health outcomes among African Americans are attributed to: 1. The belief among African Americans that prayer is more powerful than drugs 2. Poor compliance on the part of the African American patient 3. The genetic predisposition for illness found among African Americans 4. Discrimination, cultural barriers, and lack of access to health care ____ 6. The racial difference in drug pharmacokinetics seen in American Indian or Alaskan Natives are: 1. Increased CYP 2D6 activity, leading to rapid metabolism of some drugs 2. Largely unknown due to lack of studies of this population 3. Rapid metabolism of alcohol, leading to increased tolerance 4. Decreased elimination of opioids, leading to increased risk for addiction ____ 7. Pharmacokinetics among Asians are universal to all the Asian ethnic groups. 1. True 2. False ____ 8. Alterations in drug metabolism among Asians may lead to: 1. Slower metabolism of antidepressants, requiring lower doses 2. Faster metabolism of neuroleptics, requiring higher doses 3. Altered metabolism of omeprazole, requiring higher doses 4. Slower metabolism of alcohol, requiring higher doses ____ 9. Asians from Eastern Asia are known to be fast acetylators. Fast acetylators: 1. Require acetylization in order to metabolize drugs 2. Are unable to tolerate higher doses of some drugs that require acetylization 3. May have a toxic reaction to drugs that require acetylization 4. Require higher doses of drugs metabolized by acetylization to achieve efficacy ____ 10. Hispanic native healers (curanderas): 1. Are not heavily utilized by Hispanics who immigrate to the United States 2. Use herbs and teas in their treatment of illness 3. Provide unsafe advice to Hispanics and should not be trusted 4. Need to be licensed in their home country in order to practice in the United States Chapter 8. An Introduction to Pharmacogenomics Multiple Choice Identify the choice that best completes the statement or answers the question. ____ 1. Genetic polymorphisms account for differences in metabolism, including: 1. Poor metabolizers, who lack a working enzyme 2. Intermediate metabolizers, who have one working, wild-type allele and one mutant allele 3. Extensive metabolizers, with two normally functioning alleles 4. All of the above ____ 2. Up to 21% of Asians are ultra-rapid 2D6 metabolizers, leading to: 1. A need to monitor drugs metabolized by 2D6 for toxicity 2. Increased dosages needed of drugs metabolized by 2D6, such as the selective serotonin reuptake inhibitors 3. Decreased conversion of codeine to morphine by CYP 2D6 4. The need for lowered dosages of drugs, such as beta blockers ____ 3. Rifampin is a nonspecific CYP450 inducer that may: 1. Lead to toxic levels of rifampin and must be monitored closely 2. Cause toxic levels of drugs, such as oral contraceptives, when coadministered 3. Induce the metabolism of drugs, such as oral contraceptives, leading to therapeutic failure 4. Cause nonspecific changes in drug metabolism ____ 4. Inhibition of P-glycoprotein by a drug such as quinidine may lead to: 1. Decreased therapeutic levels of quinidine 2. Increased therapeutic levels of quinidine 3. Decreased levels of a coadministered drug, such as digoxin, that requires P-glycoprotein for absorption and elimination 4. Increased levels of a coadministered drug, such as digoxin, that requires P-glycoprotein for absorption and elimination ____ 5. Warfarin resistance may be seen in patients with VCORC1 mutation, leading to: 1. Toxic levels of warfarin building up 2. Decreased response to warfarin 3. Increased risk for significant drug interactions with warfarin 4. Less risk of drug interactions with warfarin ____ 6. Genetic testing for VCORC1 mutation to assess potential warfarin resistance is required prior to prescribing warfarin. 1. True 2. False ____ 7. Pharmacogenetic testing is required by the U.S. Food and Drug Administration prior to prescribing: 1. Erythromycin 2. Digoxin 3. Cetuximab 4. Rifampin ____ 8. Carbamazepine has a Black Box Warning recommending testing for the HLA-B*1502 allele in patients with Asian ancestry prior to starting therapy due to: 1. Decreased effectiveness of carbamazepine in treating seizures in Asian patients with the HLA-B*1502 allele 2. Increased risk for drug interactions in Asian patients with the HLA-B*1502 allele 3. Increased risk for Stevens-Johnson syndrome in Asian patients with HLA-B*1502 allele 4. Patients who have the HLA-B*1502 allele being more likely to have a resistance to carbamazepine ____ 9. A genetic variation in how the metabolite of the cancer drug irinotecan SN-38 is inactivated by the body may lead to: 1. Decreased effectiveness of irinotecan in the treatment of cancer 2. Increased adverse drug reactions, such as neutropenia 3. Delayed metabolism of the prodrug irinotecan into the active metabolite SN-38 4. Increased concerns for irinotecan being carcinogenic ____ 10. Patients who have a poor metabolism phenotype will have: 1. Slowed metabolism of a prodrug into an active drug, leading to accumulation of prodrug 2. Accumulation of inactive metabolites of drugs 3. A need for increased dosages of medications 4. Increased elimination of an active drug ____ 11. Ultra-rapid metabolizers of drugs may have: 1. To have dosages of drugs adjusted downward to prevent drug accumulation 2. Active drug rapidly metabolized into inactive metabolites, leading to potential therapeutic failure 3. Increased elimination of active, nonmetabolized drug 4. Slowed metabolism of a prodrug into an active drug, leading to an accumulation of prodrug ____ 12. A provider may consider testing for CYP2D6 variants prior to starting tamoxifen for breast cancer to: 1. Ensure the patient will not have increased adverse drug reactions to the tamoxifen 2. Identify potential drug-drug interactions that may occur with tamoxifen 3. Reduce the likelihood of therapeutic failure with tamoxifen treatment 4. Identify poor metabolizers of tamoxifen Chapter 10. Herbal Therapy and Nutritional Supplements Multiple Choice Identify the choice that best completes the statement or answers the question. ____ 1. A good history of herb and supplement use is critical before prescribing because approximately ____ % of patients in the United States are using herbal products. 1. 10 2. 5 3. 38 4. 70 ____ 2. A potential harmful effect on patients who take some herbal medication is: 1. Constipation 2. Lead poisoning 3. Diarrhea 4. Life-threatening rash ____ 3. A thorough understanding of herbs is critical to patient safety. An example is the use of cinnamon to treat type II diabetes. It is important the patient uses Ceylon cinnamon, as the commercially available cassia cinnamon contains: 1. Coumadin, which may lead to bleeding problems 2. Coumarin, which can cause liver and kidney damage 3. Cinnamic aldehyde, which is toxic to the kidney 4. Cinnamate eugenol, which is toxic to the liver ____ 4. Traditional Chinese medicine utilizes yin (cooling) versus yang (warming) in assessing and treating disease. Menopause is considered a time of imbalance, therefore the Chinese herbalist would prescribe: 1. Herbs which are yang in nature 2. Herbs that are yin in nature 3. Ginger 4. Golden seal ____ 5. According to traditional Chinese medicine, if a person who has a fever is given a herb that is yang in nature, such as golden seal, the patient’s illness will: 1. Get worse 2. Get better 3. Not be adequately treated 4. Need additional herbs to treat the yang ____ 6. In Ayurvedic medicine, treatment is based on the patient’s dominant dosha, which is referred to as the person’s: 1. Vata 2. Pitta 3. Kapha 4. Prakriti ____ 7. Herbs and supplements are regulated by the U.S. Food and Drug Administration. 1. True 2. False ____ 8. When melatonin is used to induce sleep, the recommendation is that the patient: 1. Take 10 mg 30 minutes before bed nightly 2. Take 1 to 5 mg 30 minutes before bed nightly 3. Not take melatonin more than three nights a week 4. Combine melatonin with zolpidem (Ambien) for the greatest impact on sleep ____ 9. Valerian tea causes relaxation and can be used to help a patient fall asleep. Overdosage of valerian (more than 2.5 gm/dose) may lead to: 1. Cardiac disturbances 2. Central nervous system depression 3. Respiratory depression 4. Skin rashes ____ 10. The standard dosage of St John’s wort for the treatment of mild depression is: 1. 300 mg daily 2. 100 mg three times a day 3. 300 mg three times a day 4. 600 mg three times a day ____ 11. Patients need to be instructed regarding the drug interactions with St John’s wort, including: 1. MAO inhibitors 2. Serotonin reuptake inhibitors 3. Over-the-counter cough and cold medications 4. All of the above ____ 12. Ginseng, which is taken to assist with memory, may potentiate: 1. Aricept 2. Insulin 3. Digoxin 4. Propranolol ____ 13. Licorice root is a common treatment for dyspepsia. Drug interactions with licorice include: 1. Antihypertensives, diuretics, and digoxin 2. Antidiarrheals, antihistamines, and omeprazole 3. Penicillin antibiotic class and benzodiazepines 4. None of the above ____ 14. Patients should be warned about the overuse of topical wintergreen oil to treat muscle strains, as overapplication can lead to: 1. Respiratory depression 2. Cardiac disturbance 3. Salicylates poisoning 4. Life-threatening rashes ____ 15. The role of the NP in the use of herbal medication is to: 1. Maintain competence in the prescribing of common herbal remedies 2. Recommend common over-the-counter herbs to patients 3. Educate patients and guide them to appropriate sources of care 4. Encourage patients to not use herbal therapy due to the documented dangers Chapter 11. Information Technology and Pharmacotherapeutics Multiple Choice Identify the choice that best completes the statement or answers the question. ____ 1. Being competent in the use of information technology in clinical practice is expected in professional nurses. Advanced practice competence includes the ability to: 1. Search for information using the most common search engines 2. Serve as content experts in developing, implementing, and evaluating information systems 3. Write programs to assure the integrity of health information 4. Use information technology to prescribe drugs ____ 2. You are going to prescribe a drug and the electronic health record (EHR) alerts you that there is a potential drug–drug interaction. The alert is generated by: 1. The Food and Drug Administration MedWatch system 2. TOXNET, the National Institutes of Health alert system 3. The EHR clinical decision support system 4. Lexicomp, a commercial medication alert system ____ 3. Which of the following is a primary benefit of the use of computerized provider order entry for patient medications? 1. Reduces time that prescribing drugs takes 2. Eliminates the need to chart drugs prescribed 3. Decreases prescribing and transcription errors 4. Helps keep the number of drugs prescribed to a minimum ____ 4. A number of barriers and concerns exist before the goals of a safe and efficient information technology (IT) system can be realized. Which of the following is NOT a barrier to adoption and use of IT in prescribing drugs? 1. Cost of initial setup 2. Access to highly skilled experts 3. Compatibility between systems 4. Patient confidentiality risks ____ 5. EHRs: 1. Are being discouraged by the Centers for Medicare and Medicaid Services due to cost issues 2. Allow for all patient data to be centralized in one location for access by multiple providers 3. Use macros and templates to individualize care 4. Use standardized software to facilitate interoperability between systems ____ 6. Factors that facilitate keeping patient information confidential in an electronic health record (EHR) system include: 1. Designing software so that only those who need the information can gain access 2. Requiring providers to log off at the end of the clinical day 3. Keeping a file of the login and password information for each provider in a secure place 4. Having patients sign informed consent documents to have their data on an EHR ____ 7. Decision support systems often provide medication alerts that tell the prescriber: 1. Patient history data with a summary of their diagnoses 2. The usual dosage for the drug being prescribed 3. The patient’s latest laboratory values, such as potassium levels 4. Potential drug-to-drug interactions with other medications the patient is taking ____ 8. Prescribers have been shown to override a medication alert about a patient’s allergies when: 1. The history showed that the patient had tolerated the medication in the past 2. The benefit outweighed the risk 3. The medication was therapeutically appropriate and needed 4. All of the above ____ 9. The use of information technology for quality improvement in pharmacotherapeutics includes: 1. Incorporating the use of “apps” into all patient encounters 2. Tracking data trends within the practice via the electronic health record database 3. Informing patients that they have access to their medication list via the Internet 4. Using macros for individualizing patient care management ____ 10. The advantage of using information technology for patient education includes: 1. The ability to track the number of times you have given the patient the same instructions regarding their medication 2. Standardized and individualized patient education that is simultaneously recorded into the patient record 3. Easy access to private patient information specific to populations with a similar diagnosis 4. The ability to download and interpret patient information in multiple languages, easily and accurately ____ 11. One barrier to use of the Internet for both prescribing and for patient teaching is: 1. Lack of free public access to the Internet 2. Age, with older adults rarely understanding how to use a computer 3. Web pages and hyperlinks may change, be deleted, or be replaced 4. Few Web sites with information about drugs are free ____ 12. Information technology can be a time-saving device in a busy practice if it is used wisely. One way to make it a help rather than a hindrance is to: 1. Prioritize what is needed information and avoid spending time reading “interesting” information not central to the problem at hand 2. Integrate professional and personal searching so that the same browser does not need to be accessed repeatedly 3. Check e-mail frequently so that patient questions can be addressed promptly 4. Check for viruses, spyware, and malware ____ 13. Data in the electronic health record that the provider reviews prior to a patient encounter varies with the clinic setting. In an urgent care clinic, the provider should review: 1. The patient’s current diagnosis and history 2. Drugs the patient is currently taking 3. Any recent previous encounter for the same problem as this visit and what was done 4. All of the above ____ 14. Information technology (IT) can also be used to interact with a patient between encounters. Which of the following statements about such interactions is true? 1. Patients feel the provider does not care about them if they are not seen in a face-to-face encounter. 2. Data collected from patients between encounters via IT is less accurate and complete. 3. Collecting data between encounters via IT may mean a more efficient face-to-face encounter. 4. Between encounters is a good time to collect screening data. ____ 15. Discharge summaries using information technology have several advantages. They can: 1. Replace the need for oral instruction because the patient has printed material to read at home 2. Be filed with the patient’s chart to document patient teaching 3. Both 1 and 2 4. Neither 1 nor 2 ____ 16. Information technology can also be used for patient teaching during the encounter and after it. The provider can help patients and their families become savvy consumers of health-care information by: 1. Warning them about the questionable quality of health information online 2. Identifying easily used “apps” that patients can use to manage their medications 3. Teaching them how to identify high-quality Web sites and “red flags” signaling inaccurate content 4. All of the above ____ 17. Incorporating information technology (IT) into a patient encounter takes skill and tact. During the encounter, the provider can make the patient more comfortable with the IT the provider is using by: 1. Turning the screen around so the patient can see material being recorded 2. Not placing the computer screen between the provider and the patient 3. Both 1 and 2 4. Neither 1 nor 2 Chapter 12. Pharmacoeconomics Multiple Choice Identify the choice that best completes the statement or answers the question. ____ 1. Pharmacoeconomics is: 1. The study of the part of the U.S. economy devoted to drug use 2. The study of the impact of prescription drug costs on the overall economy 3. The analysis of the costs and consequences of any health-care-related treatment or service 4. The analysis of the clinical efficacy of the drug ____ 2. The direct costs of drug therapy include: 1. The actual cost of acquiring the medication 2. The loss of income due to illness 3. Pain and suffering due to inadequate drug therapy 4. The cost of a funeral associated with premature death ____ 3. Indirect costs associated with drug therapy include: 1. The cost of diagnostic tests to monitor therapeutic levels 2. Health-care provider time to prescribe and educate the patient 3. Child-care expenses incurred while receiving therapy 4. Loss of wages while undergoing drug therapy ____ 4. The intangible costs of drug therapy include: 1. Loss of wages while undergoing therapy 2. Inconvenience, pain, and suffering incurred with therapy 3. Cost of medical equipment in the laboratory used to monitor therapeutic drug levels 4. Cost of prescription drug coverage, such as Medicare Part D ____ 5. When a pharmacoeconomic analysis looks at two or more treatment alternatives that are considered equal in efficacy and compares the costs of each it is referred to as: 1. Cost-minimization analysis 2. Cost-of-illness analysis 3. Cost-effectiveness analysis 4. Cost-benefit analysis ____ 6. Cost-effectiveness analysis compares two or more treatments or programs that are: 1. Not necessarily therapeutically equivalent 2. Considered equal in efficacy 3. Compared with the dollar value of the benefit received 4. Expressed in terms of patient preference or quality-adjusted life years ____ 7. When the costs of a specific treatment or intervention are calculated and then compared with the dollar value of the benefit received it is referred to as: 1. Cost-minimization analysis 2. Cost-of-illness analysis 3. Cost-effectiveness analysis 4. Cost-benefit analysis ____ 8. Mary has a two-tiered prescription benefit plan, which means: 1. She can receive differing levels of care based on whether she chooses an “in-plan” provider or not. 2. She is eligible for the new Medicare Part D “donut hole” reduction of costs program. 3. She pays a higher copay for brand-name drugs than for generic drugs. 4. She must always choose to be treated with generic drugs first. ____ 9. Prescribing less-expensive generic drugs or drugs off the $4 retail pharmacy lists: 1. Increases the complexity of the pharmacoeconomics of prescribing for the individual patient 2. Increases compliance by reducing the financial burden of drug costs to the patient 3. Is not sound prescribing practice due to the inferiority of the generic products 4. Will increase the overall cost of drugs to the system due to the ease of overprescribing less-expensive drugs ____ 10. James tells you that he is confused by his Medicare Part D coverage plan. An appropriate intervention would be: 1. Order cognitive testing to determine the source of his confusion. 2. Sit down with him and explain the whole Medicare Part D process. 3. Refer him to the Medicare specialist in his insurance plan to explain the benefit to him. 4. Request his son come to the next appointment so you can explain the benefit to him. ____ 11. The “donut hole” in Medicare Part D: 1. Will be totally eliminated with the federal health-care reform enacted in 2010 2. Refers to the period of time when annual individual drug costs are between $250 and $2,250 per year and drug costs are covered 75% 3. Refers to the period between when the annual individual drug costs are $2,970 and $4,750 and the patient pays 52.5% of the costs of brand name drugs (2013) 4. Has no effect on whether patients continue to fill their prescriptions during the coverage gap ____ 12. Research has shown that when patients who are covered by Medicare Part D reach the “donut hole” in coverage they: 1. Ask for extra refills of medication to get them through the months of no coverage 2. Fill their prescriptions less frequently, including critical medications such as warfarin or a statin 3. Fill their critical medications, but hold off on filling less-critical medications 4. Demonstrate no change in their prescription filling pattern Chapter 13. Over-the-Counter Medications Multiple Choice Identify the choice that best completes the statement or answers the question. ____ 1. Michael asks you about why some drugs are over-the-counter and some are prescription. You explain that in order for a drug to be approved for over-the-counter use the drug must: 1. Be safe and labeled for appropriate use 2. Have a low potential for abuse or misuse 3. Be taken for a condition the patient can reliably self-diagnose 4. All of the above ____ 2. In the United States, over-the-counter drugs are regulated by: 1. No one. There is no oversight for over-the-counter medications. 2. The U.S. Food and Drug Administration Center for Drug Evaluation and Research 3. The U.S. Drug Enforcement Administration 4. MedWatch ____ 3. As drugs near the end of their patent, pharmaceutical companies may apply for the drug to change to over-the-counter status in order to: 1. Get a new patent for the over-the-counter form of the drug 2. Lower the costs because most prescription benefit plans do not cover generics 3. Market the drug to a whole new population, as they are able to market to patients instead of just providers 4. Continue to make large profits from their blockbuster brand-name drug ____ 4. New over-the-counter drug ingredients must undergo the U.S. Food and Drug Administration New Drug Application process, just as prescription drugs do. 1. True 2. False ____ 5. The ailment that generates the greatest over-the-counter annual drug sales is: 1. Constipation 2. Cough and colds 3. Heartburn 4. Acute and chronic pain ____ 6. Common over-the-counter pain relievers such as acetaminophen or ibuprofen: 1. Are always safer for the patient than prescription pain medication 2. Are harmful if taken in higher than recommended amounts 3. Have minimal interaction with prescription medications 4. Should never be given to children unless recommended by their provider ____ 7. When obtaining a drug history from Harold, he gives you a complete list of his prescription medications. He denies taking any other drugs, but you find that he occasionally takes aspirin for his arthritis flare ups. This is an example of: 1. His appropriately only telling you about his regularly prescribed medications 2. His hiding information regarding his inappropriate use of aspirin from you 3. A common misconception that intermittently taken over-the counter medications are not an important part of his drug history 4. A common misuse of over-the-counter aspirin ____ 8. The Combat Methamphetamine Epidemic Act, which is part of the 2006 U.S. Patriot Act: 1. Requires all providers to screen their patients for methamphetamine use 2. Restricts the prescribing of amphetamines to U.S. citizens 3. Requires a prescription be written for all methamphetamine precursors in all states 4. Restricts the sales of drugs that contain methamphetamine precursors, including a daily and 30-day limit on sales ____ 9. When prescribing a tetracycline or quinolone antibiotic it is critical to instruct the patient: 1. Not to take their regularly prescribed medications while on these antibiotics 2. Regarding the need for lots of acidic foods and juices, such as orange juice, to enhance absorption 3. Not to take antacids while on these medications, as the antacid decreases absorption 4. That there are no drug interactions with these antibiotics Chapter 14. Drugs Affecting the Autonomic Nervous System Multiple Choice Identify the choice that best completes the statement or answers the question. ____ 1. Charlie is a 65-year-old male who has been diagnosed with hypertension and benign prostatic hyperplasia. Doxazosin has been chosen to treat his hypertension because it: 1. Increases peripheral vasoconstriction 2. Decreases detrusor muscle contractility 3. Lowers supine blood pressure more than standing pressure 4. Relaxes smooth muscle in the bladder neck ____ 2. To reduce potential adverse effects, patients taking a peripherally acting alpha1 antagonist should do all of the following EXCEPT: 1. Take the dose at bedtime 2. Sit up slowly and dangle their feet before standing 3. Monitor their blood pressure and skip a dose if the pressure is less than 120/80 4. Weigh daily and report weight gain of greater than 2 pounds in one day ____ 3. John has clonidine, a centrally acting adrenergic blocker, prescribed for his hypertension. He should: 1. Not miss a dose or stop taking the drug because of potential rebound hypertension 2. Increase fiber in the diet to treat any diarrhea that may occur 3. Reduce fluid intake to less than 2 liters per day to prevent fluid retention 4. Avoid sitting for long periods, as this can lead to deep vein thrombosis ____ 4. Clonidine has several off-label uses, including: 1. Alcohol and nicotine withdrawal 2. Post-herpetic neuralgia 3. Both 1 and 2 4. Neither 1 nor 2 ____ 5. Jim is being treated for hypertension. Because he has a history of heart attack, the drug chosen is atenolol. Beta blockers treat hypertension by: 1. Increasing heart rate to improve cardiac output 2. Reducing vascular smooth muscle tone 3. Increasing aldosterone-mediated volume activity 4. Reducing aqueous humor production ____ 6. Which of the following adverse effects are less likely in a beta1-selective blocker? 1. Dysrhythmias 2. Impaired insulin release 3. Reflex orthostatic changes 4. Decreased triglycerides and cholesterol ____ 7. Richard is 70 years old and has a history of cardiac dysrhythmias. He has been prescribed nadolol. You do his annual laboratory work and find a CrCl of 25 ml/min. What action should you take related to his nadolol? 1. Extend the dosage interval. 2. Decrease the dose by 75%. 3. Take no action because this value is expected in the older adult. 4. Schedule a serum creatinine level to validate the CrCl value. ____ 8. Beta blockers are the drugs of choice for exertional angina because they: 1. Improve myocardial oxygen supply by vasodilating the coronary arteries 2. Decrease myocardial oxygen demand by decreasing heart rate and vascular resistance 3. Both 1 and 2 4. Neither 1 nor 2 ____ 9. Adherence to beta blocker therapy may be affected by their: 1. Short half-lives requiring twice daily dosing 2. Tendency to elevate lipid levels 3. Effects on the male genitalia, which may produce impotence 4. None of the above ____ 10. Beta blockers have favorable effects on survival and disease progression in heart failure. Treatment should be initiated when the: 1. Symptoms are severe 2. Patient has not responded to other therapies 3. Patient has concurrent hypertension 4. Left ventricular dysfunction is diagnosed ____ 11. Abrupt withdrawal of beta blockers can be life threatening. Patients at highest risk for serious consequences of rapid withdrawal are those with: 1. Angina 2. Coronary artery disease 3. Both 1 and 2 4. Neither 1 nor 2 ____ 12. To prevent life-threatening events from rapid withdrawal of a beta blocker: 1. The dosage interval should be increased by 1 hour each day. 2. An alpha blocker should be added to the treatment regimen before withdrawal. 3. The dosage should be tapered over a period of weeks. 4. The dosage should be decreased by one-half every 4 days. ____ 13. Beta blockers are prescribed for diabetics with caution because of their ability to produce hypoglycemia and block the common symptoms of it. Which of the following symptoms of hypoglycemia is not blocked by these drugs and so can be used to warn diabetics of possible decreased blood glucose? 1. Dizziness 2. Increased heart rate 3. Nervousness and shakiness 4. Diaphoresis ____ 14. Combined alpha-beta antagonists are used to reduce the progression of heart failure because they: 1. Vasodilate the peripheral vasculature 2. Decrease cardiac output 3. Increase renal vascular resistance 4. Reduce atherosclerosis secondary to elevated serum lipoproteins ____ 15. Carvedilol is heavily metabolized by CYP2D6 and 2C9, resulting in drug interactions with which of the following drug classes? 1. Histamine 2 blockers 2. Quinolones 3. Serotonin re-uptake inhibitors 4. All of the above ____ 16. Alpha-beta blockers are especially effective to treat hypertension for which ethnic group? 1. White 2. Asian 3. African American 4. Native American ____ 17. Bethanechol: 1. Increases detrusor muscle tone to empty the bladder 2. Decreases gastric acid secretion to treat peptic ulcer disease 3. Stimulates voluntary muscle tone to improve strength 4. Reduces bronchial airway constriction to treat asthma ____ 18. Clinical dosing of Bethanechol: 1. Begins at the highest effective dose to obtain a rapid response 2. Starts at 5 mg to 10 mg PO and is repeated every hour until a satisfactory clinical response is achieved 3. Requires dosing only once daily 4. Is the same for both the oral and parenteral route ____ 19. Patients who need to remain alert are taught to avoid which drug due to its antimuscarinic effects? 1. Levothyroxine 2. Prilosec 3. Dulcolax 4. Diphenhydramine ____ 20. Anticholinesterase inhibitors are used to treat: 1. Peptic ulcer disease 2. Myasthenia gravis 3. Both 1 and 2 4. Neither 1 nor 2 ____ 21. Which of the following drugs used to treat Alzheimer’s disease is not an anticholinergic? 1. Donepezil 2. Memantine 3. Rivastigmine 4. Galantamine ____ 22. Taking which drug with food maximizes it bioavailability? 1. Donepezil 2. Galantamine 3. Rivastigmine 4. Memantine ____ 23. Which of the following drugs should be used only when clearly needed in pregnant and breastfeeding women? 1. Memantine 2. Pyridostigmine 3. Galantamine 4. Rivastigmine ____ 24. There is a narrow margin between first appearance of adverse reaction to AChE inhibitors and serious toxic effects. Adverse reactions that require immediate action include: 1. Dizziness and headache 2. Nausea 3. Decreased salivation 4. Fasciculations of voluntary muscles ____ 25. Adherence is improved when a drug can be given once daily. Which of the following drugs can be given once daily? 1. Tacrine 2. Donepezil 3. Memantine 4. Pyridostigmine ____ 26. Nicotine has a variety of effects on nicotinic receptors throughout the body. Which of the following is NOT an effect of nicotine? 1. Vasodilation and decreased heart rate 2. Increased secretion of gastric acid and motility of the GI smooth muscle 3. Release of dopamine at the pleasure center 4. Stimulation of the locus coeruleus ____ 27. Nicotine gum products are: 1. Chewed to release the nicotine and then swallowed for a systemic effect 2. “Parked” in the buccal area of the mouth to produce a constant amount of nicotine release 3. Bound to exchange resins so the nicotine is only released during chewing 4. Approximately the same in nicotine content as smoking two cigarettes ____ 28. Nicotine replacement therapy (NRT): 1. Is widely distributed in the body only when the gum products are used 2. Does not cross the placenta and so is safe for pregnant women 3. Delays healing of esophagitis and peptic ulcers 4. Has no drug interactions when a transdermal patch is used ____ 29. Success rates for smoking cessation using NRT: 1. Are about the same regardless of the method chosen 2. Vary from 40% to 50% at 12 months 3. Both 1 and 2 4. Neither 1 nor 2 ____ 30. Cholinergic blockers are used to: 1. Counteract the extrapyramidal symptoms (EPS) effects of phenothiazines 2. Control tremors and relax smooth muscle in Parkinson’s disease 3. Inhibit the muscarinic action of ACh on bladder muscle 4. All of the above ____ 31. Several classes of drugs have interactions with cholinergic blockers. Which of the following is true about these interactions? 1. Drugs with a narrow therapeutic range given orally may not stay in the GI tract long enough to produce an action. 2. Additive antimuscarinic effects may occur with antihistamines. 3. Cholinergic blockers may decrease the sedative effects of hypnotics. 4. Cholinergic blockers are contraindicated with antipsychotics. ____ 32. Scopolamine can be used to prevent the nausea and vomiting associated with motion sickness. The patient is taught to: 1. Apply the transdermal disk at least 4 hours before the antiemetic effect is desired. 2. Swallow the tablet 1 hour before traveling where motion sickness is possible. 3. Place the tablet under the tongue and allow it to dissolve. 4. Change the transdermal disk daily for maximal effect. ____ 33. You are managing the care of a patient recently diagnosed with benign prostatic hyperplasia (BPH). He is taking tamsulosin but reports dizziness when standing abruptly. The best option for this patient is: 1. Continue the tamsulosin because the side effect will resolve with continued treatment. 2. Discontinue the tamsulosin and start doxazosin. 3. Have him double his fluid intake and stand more slowly. 4. Prescribe meclizine as needed for the dizziness. ____ 34. You are treating a patient with a diagnosis of Alzheimer’s disease. The patient’s wife mentions difficulty with transportation to the clinic. Which medication is the best choice? 1. Donepezil 2. Tacrine 3. Doxazosin 4. Verapamil ____ 35. A patient presents with a complaint of dark stools and epigastric pain described as gnawing and burning. Which of the medications is the most likely cause? 1. Acetaminophen 2. Estradiol 3. Donepezil 4. Bethanechol ____ 36. Your patient calls for an appointment before going on vacation. Which medication should you ensure he has an adequate supply of before leaving to avoid life-threatening complications? 1. Carvedilol 2. Donepezil 3. Bethanechol 4. Tacrine ____ 37. Activation of central alpha2 receptors results in inhibition of cardioacceleration and ______________ centers in the brain. 1. Vasodilation 2. Vasoconstriction 3. Cardiovascular 4. Respiratory Chapter 15. Drugs Affecting the Central Nervous System Multiple Choice Identify the choice that best completes the statement or answers the question. ____ 1. Sarah, a 42-year-old female, requests a prescription for an anorexiant to treat her obesity. A trial of phentermine is prescribed. Prescribing precautions include: 1. Understanding that obesity is a contraindication to prescribing phentermine 2. Anorexiants may cause tolerance and should only be prescribed for 6 months 3. Patients should be monitored for postural hypotension 4. Renal function should be monitored closely while on anorexiants ____ 2. Before prescribing phentermine to Sarah, a thorough drug history should be taken including assessing for the use of serotonergic agents such as selective serotonin reuptake inhibitors (SSRIs) and St John’s wort due to: 1. Additive respiratory depression risk 2. Additive effects affecting liver function 3. The risk of serotonin syndrome 4. The risk of altered cognitive functioning ____ 3. Antonia is a 3-year-old child who has a history of status epilepticus. Along with her routine antiseizure medication, she should also have a home prescription for_________ to be used for an episode of status epilepticus. 1. IV phenobarbital 2. Rectal diazepam (Diastat) 3. IV phenytoin (Dilantin) 4. Oral carbamazepine (Tegretol) ____ 4. Rabi is being prescribed phenytoin for seizures. Monitoring includes assessing: 1. For phenytoin hypersensitivity syndrome 3 to 8 weeks after starting treatment 2. For pedal edema throughout therapy 3. Heart rate at each visit and consider altering therapy if heart rate is less than 60 bpm 4. For vision changes, such as red-green blindness, at least annually ____ 5. Dwayne has recently started on carbamazepine to treat seizures. He comes to see you and you note that while his carbamazepine levels had been in the therapeutic range, they are now low. The possible cause for the low carbamazepine levels include: 1. Dwayne hasn’t been taking his carbamazepine because it causes insomnia. 2. Carbamazepine auto-induces metabolism, leading to lower levels in spite of good compliance. 3. Dwayne was not originally prescribed the correct amount of carbamazepine. 4. Carbamazepine is probably not the right antiseizure medication for Dwayne. ____ 6. Carbamazepine has a Black Box Warning due to life-threatening: 1. Renal toxicity, leading to renal failure 2. Hepatotoxicity, leading to liver failure 3. Dermatologic reaction, including Steven’s Johnson and toxic epidermal necrolysis 4. Cardiac effects, including supraventricular tachycardia ____ 7. Long-term monitoring of patients who are taking carbamazepine includes: 1. Routine troponin levels to assess for cardiac damage 2. Annual eye examinations to assess for cataract development 3. Monthly pregnancy tests for all women of childbearing age 4. Complete blood count every 3 to 4 months ____ 8. Six-year-old Lucy has recently been started on ethosuximide (Zarontin) for seizures. She should be monitored for: 1. Increased seizure activity, as this drug may auto-induce seizures 2. Altered renal function, including renal failure 3. Blood dyscrasias, which are uncommon but possible 4. Central nervous system excitement, leading to insomnia ____ 9. Sook has been prescribed gabapentin to treat neuropathic pain and is complaining of feeling depressed and having “strange” thoughts. The appropriate initial action would be: 1. Increase her dose 2. Assess for suicidal ideation 3. Discontinue the medication immediately 4. Decrease her dose to half then slowly titrate up the dose ____ 10. Selma, who is overweight, recently started taking topiramate for seizures and at her follow-up visit you note she has lost 3 kg. The appropriate action would be: 1. Tell her to increase her caloric intake to counter the effects of the topiramate. 2. Consult with a neurologist, as this is not a common adverse effect of topiramate. 3. Decrease her dose of topiramate. 4. Reassure her that this is a normal side effect of topiramate and continue to monitor her weight. ____ 11. Monitoring of a patient on gabapentin to treat seizures includes: 1. Routine therapeutic drug levels every 3 to 4 months 2. Assessing for dermatologic reactions, including Steven’s Johnson 3. Routine serum electrolytes, especially in hot weather 4. Recording seizure frequency, duration, and severity ____ 12. Scott’s seizures are well controlled on topiramate and he wants to start playing baseball. Education for Scott regarding his topiramate includes: 1. He should not play sports due to the risk of increased seizures 2. He should monitor his temperature and ability to sweat in the heat while playing 3. Reminding him that he may need higher dosages of topiramate when exercising 4. Encouraging him to use sunscreen due to photosensitivity from topiramate ____ 13. Cara is taking levetiracetam (Keppra) to treat seizures. Routine education for levetiracetam includes reminding her: 1. To not abruptly discontinue levetiracetam due to risk for withdrawal seizures 2. To wear sunscreen due to photosensitivity from levetiracetam 3. To get an annual eye exam while on levetiracetam 4. To report weight loss if it occurs ____ 14. Levetiracetam has known drug interactions with: 1. Combined oral contraceptives 2. Carbamazepine 3. Warfarin 4. Few, if any, drugs ____ 15. Zainab is taking lamotrigine (Lamictal) and presents to the clinic with fever and lymphadenopathy. Initial evaluation and treatment includes: 1. Reassuring her she has a viral infection and to call if she isn’t better in 4 or 5 days 2. Ruling out a hypersensitivity reaction that may lead to multi-organ failure 3. Rapid strep test and symptomatic care if strep test is negative 4. Observation only, with further assessment if she worsens ____ 16. Samantha is taking lamotrigine (Lamictal) for her seizures and requests a prescription for combined oral contraceptives (COCs), which interact with lamotrigine and may cause: 1. Contraceptive failure 2. Excessive weight gain 3. Reduced lamotrigine levels, requiring doubling the dose of lamotrigine 4. Induction of estrogen metabolism, requiring higher estrogen content OCs be prescribed ____ 17. The tricyclic antidepressants should be prescribed cautiously in patients with: 1. Eczema 2. Asthma 3. Diabetes 4. Heart disease ____ 18. A 66-year-old male was prescribed phenelzine (Nardil) while in an acute psychiatric unit for recalcitrant depression. The NP managing his primary health care needs to understand the following regarding phenelzine and other monoamine oxidase inhibitors (MAOIs): 1. He should not be prescribed any serotonergic drug such as sumatriptan (Imitrex) 2. MAOIs interact with many common foods, including yogurt, sour cream, and soy sauce 3. Symptoms of hypertensive crisis (headache, tachycardia, sweating) require immediate treatment 4. All of the above ____ 19. Taylor is a 10-year-old child diagnosed with major depression. The appropriate first-line antidepressant for children is: 1. Fluoxetine 2. Fluvoxamine 3. Sertraline 4. Escitalopram ____ 20. Suzanne is started on paroxetine (Paxil), a selective serotonin reuptake inhibitor (SSRI), for depression. Education regarding her antidepressant includes: 1. SSRIs may take 2 to 6 weeks before she will have maximum drug effects. 2. Red-green color blindness may occur and should be reported. 3. If she experiences dry mouth or heart rates greater than 80, she should stop taking the drug immediately. 4. She should eat lots of food high in fiber to prevent constipation. ____ 21. Cecilia presents with depression associated with complaints of fatigue, sleeping all the time, and lack of motivation. An appropriate initial antidepressant for her would be: 1. Fluoxetine (Prozac) 2. Paroxetine (Paxil) 3. Amitriptyline (Elavil) 4. Duloxetine (Cymbalta) ____ 22. Jake, a 45-year-old patient with schizophrenia, was recently hospitalized for acute psychosis due to medication noncompliance. He was treated with IM long-acting haloperidol. Besides monitoring his schizophrenia symptoms, the patient should be assessed by his primary care provider: 1. For excessive weight loss 2. With the Abnormal Involuntary Movement Scale (AIMS) for extrapyramidal symptoms (EPS) 3. Monthly for tolerance to the haloperidol 4. Only by the mental health provider, as most NPs in primary care do not care for mentally ill patients ____ 23. Anticholinergic agents, such as benztropine (Cogentin), may be given with a phenothiazine to: 1. Reduce the chance of tardive dyskinesia 2. Potentiate the effects of the drug 3. Reduce the tolerance that tends to occur 4. Increase central nervous system (CNS) depression ____ 24. Patients who are prescribed olanzapine (Zyprexa) should be monitored for: 1. Insomnia 2. Weight gain 3. Hypertension 4. Galactorrhea ____ 25. A 19-year-old male was started on risperidone. Monitoring for risperidone includes observing for common side effects, including: 1. Bradykinesia, akathisia, and agitation 2. Excessive weight gain 3. Hypertension 4. Potentially fatal agranulocytosis ____ 26. In choosing a benzodiazepam to treat anxiety the prescriber needs to be aware of the possibility of dependence. The benzodiazepam with the greatest likelihood of rapidly developing dependence is: 1. Chlordiazepoxide (Librium) 2. Clonazepam (Klonopin) 3. Alprazolam (Xanax) 4. Oxazepam (Serax) ____ 27. A patient with anxiety and depression may respond to: 1. Duloxetine (Cymbalta) 2. Fluoxetine (Prozac) 3. Oxazepam (Serax) 4. Buspirone (Buspar) and an SSRI combined ____ 28. When prescribing temazepam (Restoril) for insomnia, patient education includes: 1. Take temazepam nightly approximately 15 minutes before bedtime. 2. Temazepam should not be used more than three times a week for less than 3 months. 3. Drinking 1 ounce of alcohol will cause additive effects and the patient will sleep better. 4. Exercise for at least 30 minutes within 2 hours of bedtime to enhance the effects of temazepam. ____ 29. Patients should be instructed regarding the rapid onset of zolpidem (Ambien) because: 1. Zolpidem should be taken just before going to bed. 2. Zolpidem may cause dry mouth and constipation. 3. Patients may need to double the dose for effectiveness. 4. They should stop drinking alcohol at least 30 minutes before taking zolpidem. ____ 30. One major drug used to treat bipolar disease is lithium. Because lithium has a narrow therapeutic range, it is important to recognize symptoms of toxicity, such as: 1. Orthostatic hypotension 2. Agitation and irritability 3. Drowsiness and nausea 4. Painful urination and abdominal distention ____ 31. Tom is taking lithium for bipolar disorder. He should be taught to: 1. Take his lithium with food 2. Eat a diet with consistent levels of salt (sodium) 3. Drink at least 2 quarts of water if he is in a hot environment 4. Monitor blood glucose levels ____ 32. Cynthia is taking valproate (Depakote) for seizures and would like to get pregnant. What advice would you give her? 1. Valproate is safe during all trimesters of pregnancy. 2. She can get pregnant while taking valproate, but she should take adequate folic acid. 3. Valproate is not safe at any time during pregnancy. 4. Valproate is a known teratogen, but may be taken after the first trimester if necessary. ____ 33. When prescribing an opioid analgesic such as acetaminophen and codeine (Tylenol #3), instructions to the patient should include: 1. The medication may cause sedation and they should not drive. 2. Constipation is a common side effect and they should increase fluids and fiber. 3. Patients should not take any other acetaminophen-containing medications at the same time. 4. All of the above ____ 34. Kirk sprained his ankle and is asking for pain medication for his mild-to-moderate pain. The appropriate first-line medication would be: 1. Ibuprofen (Advil) 2. Acetaminophen with hydrocodone (Vicodin) 3. Oxycodone (Oxycontin) 4. Oral morphine (Roxanol) ____ 35. Kasey fractured his ankle in two places and is asking for medication for his pain. The appropriate first-line medication would be: 1. Ibuprofen (Advil) 2. Acetaminophen with hydrocodone (Vicodin) 3. Oxycodone (Oxycontin) 4. Oral morphine (Roxanol) ____ 36. Jack, age 8, has attention deficit disorder (ADD) and is prescribed methylphenidate (Ritalin). He and his parents should be educated about the side effects of methylphenidate, which are: 1. Slurred speech and insomnia 2. Bradycardia and confusion 3. Dizziness and orthostatic hypotension 4. Insomnia and decreased appetite ____ 37. Monitoring for a child on methylphenidate for attention deficit hyperactivity disorder (ADHD) includes: 1. ADHD symptoms 2. Routine height and weight checks 3. Amount of methylphenidate being used 4. All of the above ____ 38. When prescribing Adderall (amphetamine and dextroamphetamine) to adults with ADHD the nurse practitioner will need to monitor: 1. Blood pressure 2. Blood glucose levels 3. Urine ketone levels 4. Liver function Chapter 16. Drugs Affecting the Cardiovascular and Renal Systems Multiple Choice Identify the choice that best completes the statement or answers the question. ____ 1. Ray has been diagnosed with hypertension and an angiotensin-converting enzyme inhibitor is determined to be needed. Prior to prescribing this drug, the NP should assess for: 1. Hypokalemia 2. Impotence 3. Decreased renal function 4. Inability to concentrate ____ 2. Angiotensin-converting enzyme inhibitors are the drug of choice in treating hypertension in diabetic patients because they: 1. Improve insulin sensitivity 2. Improve renal hemodynamics 3. Reduce the production of angiotensin II 4. All of the above ____ 3. A potentially life-threatening adverse response to angiotensin-converting enzyme inhibitors is angioedema. Which of the following statements is true about this adverse response? 1. Swelling of the tongue or hoarseness are the most common symptoms. 2. It appears to be related to the decrease in aldosterone production. 3. Presence of a dry, hacky cough indicates a high risk for this adverse response. 4. Because it takes time to build up a blood level, it occurs after being on the drug for about 1 week. ____ 4. Angiotensin-converting enzyme inhibitors are useful in a variety of disorders. Which of the following statements are true about both its usefulness in the disorder and the reason for its use? 1. Stable angina because it decreases the thickening of vascular walls due to decreased modified release. 2. Heart failure because it reduces remodeling of injured myocardial tissues. 3. Both 1 and 2 are true and the reasons are correct. 4. Both 1 and 2 are true but the reasons are wrong. 5. Neither 1 nor 2 are true. ____ 5. Despite good blood pressure control, an NP might change a patient’s drug from an angiotensin-converting enzyme (ACE) inhibitor to an angiotensin II receptor blocker (ARB) because the ARB: 1. Is stronger than the ACE inhibitor 2. Does not produce a dry, hacky cough 3. Has no effect on the renal system 4. Reduces sodium and water retention ____ 6. While taking an angiotensin II receptor blocker (ARB), patients need to avoid certain over-the-counter drugs without first consulting the provider because: 1. Cimetidine is metabolized by the CYP 3A4 isoenzymes 2. Nonsteroidal anti-inflammatory drugs reduce prostaglandin levels 3. Both 1 and 2 4. Neither 1 nor 2 ____ 7. Laboratory monitoring for patients on angiotensin-converting enzyme inhibitors or angiotensin II receptor blockers should include: 1. White blood cell counts with the drug dosage increased for elevations above 10,000 feet 2. Liver function tests with the drug dosage stopped for alanine aminotransferase values twice that of normal 3. Serum creatinine levels with the drug dosage reduced for values greater than 2.5 mg/dL 4. Serum glucose levels with the drug dosage increased for levels greater than 120 mg/dL ____ 8. Jacob has hypertension, for which a calcium channel blocker has been prescribed. This drug helps control blood pressure because it: 1. Decreases the amount of calcium inside the cell 2. Reduces stroke volume 3. Increases the activity of the Na+/K+/ATPase pump indirectly 4. Decreases heart rate ____ 9. Which of the following adverse effects may occur due to a dihydropyridine-type calcium channel blocker? 1. Bradycardia 2. Hepatic impairment 3. Increased contractility 4. Edema of the hands and feet ____ 10. Patient teaching related to amlodipine includes: 1. Increase calcium intake to prevent osteoporosis from a calcium blockade. 2. Do not crush the tablet; it must be given in liquid form if the patient has trouble swallowing it. 3. Avoid grapefruit juice as it affects the metabolism of this drug. 4. Rise slowly from a supine position to reduce orthostatic hypotension. ____ 11. Vera, age 70, has isolated systolic hypertension. Calcium channel blocker dosages for her should be: 1. Started at about half the usual dosage 2. Not increased over the usual dosage for an adult 3. Given once daily because of memory issues in the older adult 4. Withheld if she experiences gastroesophageal reflux ____ 12. Larry has heart failure, which is being treated with digoxin because it exhibits: 1. Negative inotropism 2. Positive chronotropism 3. Both 1 and 2 4. Neither 1 nor 2 ____ 13. Furosemide is added to a treatment regimen for heart failure that includes digoxin. Monitoring for this combination includes: 1. Hemoglobin 2. Serum potassium 3. Blood urea nitrogen 4. Serum glucose ____ 14. Which of the following create a higher risk for digoxin toxicity? Both the cause and the reason for it must be correct. 1. Older adults because of reduced renal function 2. Administration of aldosterone antagonist diuretics because of decreased potassium levels 3. Taking an antacid for gastroesophageal reflux disease because it increases the absorption of digoxin 4. Doses between 0.25 and 0.5 mg/day ____ 15. Serum digoxin levels are monitored for potential toxicity. Monitoring should occur: 1. Within 6 hours of the last dose 2. Because a reference point is needed in adjusting a dose 3. After three half-lives from the starting of the drug 4. When a patient has stable renal function ____ 16. Rodrigo has been prescribed procainamide after a myocardial infarction. He is monitored for dyspnea, jugular venous distention, and peripheral edema because they may indicate: 1. Widening of the area of infarction 2. Onset of congestive heart failure 3. An electrolyte imbalance involving potassium 4. Renal dysfunction ____ 17. Which of the following is true about procainamide and its dosing schedule? 1. It produces bradycardia and should be used cautiously in patients with cardiac conditions that a slower heart rate might worsen. 2. Gastrointestinal adverse effects are common so the drug should be taken with food. 3. Adherence can be improved by using a sustained release formulation that can be given once daily. 4. Doses of this drug should be taken evenly spaced around the clock to keep an even blood level. ____ 18. Amiodarone has been prescribed in a patient with a supraventricular dysrhythmia. Patient teaching should include all of the following EXCEPT: 1. Notify your health-care provider immediately if you have visual change. 2. Monitor your own blood pressure and pulse daily. 3. Take a hot shower or bath if you feel dizzy. 4. Use a sunscreen on exposed body surfaces. ____ 19. The NP orders a thyroid panel for a patient on amiodarone. The patient tells the NP that he does not have thyroid disease and wants to know why the test is ordered. Which is a correct response? 1. Amiodarone inhibits an enzyme that is important in making thyroid hormone and can cause hypothyroidism. 2. Amiodarone damages the thyroid gland and can result in inflammation of that gland, causing hyperthyroidism. 3. Amiodarone is a broad spectrum drug with many adverse effects. Many different tests need to be done before it is given. 4. Amiodarone can cause corneal deposits in up to 25% of patients. ____ 20. Isosorbide dinitrate is prescribed for a patient with chronic stable angina. This drug is administered twice daily, but the schedule is 7 a.m. and 2 p.m. because: 1. It is a long-acting drug with potential for toxicity. 2. Nitrate tolerance can develop. 3. Orthostatic hypotension is a common adverse effect. 4. It must be taken with milk or food. ____ 21. Art is a 55-year-old smoker who has been diagnosed with angina and placed on nitrates. He complains of headaches after using his nitrate. An appropriate reply might be: 1. This is a parasympathetic response to the vasodilating effects of the drug. 2. Headaches are common side effects with these drugs. How severe are they? 3. This is associated with your smoking. Let’s work on having you stop smoking. 4. This is not related to your medication. Are you under a lot of stress? ____ 22. In teaching about the use of sublingual nitroglycerine, the patient should be instructed: 1. To swallow the tablet with a full glass of water 2. To place one tablet under the tongue if chest pain occurs and allow it to dissolve 3. To take one tablet every 5 minutes until the chest pain goes away 4. That it should “burn” when placed under the tongue or it is no longer effective ____ 23. Donald has been diagnosed with hyperlipidemia. Based on his lipid profile, atorvastatin is prescribed. Rhabdomyolysis is a rare but serious adverse response to this drug. Donald should be told to: 1. Become a vegetarian because this disorder is associated with eating red meat. 2. Stop taking the drug if abdominal cramps and diarrhea develop. 3. Report muscle weakness or tenderness and dark urine to his provider immediately. 4. Expect “hot flash” sensations during the first 2 weeks of therapy. ____ 24. Which of the following diagnostic studies would NOT indicate a problem related to a reductase inhibitor? 1. Elevated serum transaminase 2. Increased serum creatinine 3. Elevated creatinine kinase 4. Increased white blood cell counts ____ 25. Because of the pattern of cholesterol synthesis, reductase inhibitors are given: 1. In the evening in a single daily dose 2. Twice daily in the morning and the evening 3. With each meal and at bedtime 4. In the morning before eating ____ 26. Janice has elevated LDL, VLDL, and triglyceride levels. Niaspan, an extended-release form of niacin, is chosen to treat her hyperlipidemia. Due to its metabolism and excretion, which of the following laboratory results should be monitored? 1. Serum alanine aminotransferase 2. Serum amylase 3. Serum creatinine 4. Phenylketonuria ____ 27. Niaspan is less likely to cause which side effect that is common to niacin? 1. Gastrointestinal irritation 2. Cutaneous flushing 3. Dehydration 4. Headaches ____ 28. Dulcea has type 2 diabetes and a high triglyceride level. She has gemfibrozil prescribed to treat her hypertriglyceridemia. A history of which of the following might contraindicate the use of this drug? 1. Reactive airway disease/asthma 2. Inflammatory bowel disease 3. Allergy to aspirin 4. Gallbladder disease ____ 29. Many patients with hyperlipidemia are treated with more than one drug. Combining a fibric acid derivative such as gemfibrozil with which of the following is not recommended? The drug and the reason must both be correct for the answer to be correct. 1. Reductase inhibitors, due to an increased risk for rhabdomyolysis 2. Bile-acid sequestering resins, due to interference with folic acid absorption 3. Grapefruit juice, due to interference with metabolism 4. Niacin, due to decreased gemfibrozil activity ____ 30. Felicity has been prescribed colestipol to treat her hyperlipidemia. Unlike other anti-lipidemics, this drug: 1. Blocks synthesis of cholesterol in the liver 2. Exchanges chloride ions for negatively charged acids in the bowel 3. Increases HDL levels the most among the classes 4. Blocks the lipoprotein lipase pathway ____ 31. Because of their site of action, bile acid sequestering resins: 1. Should be administered separately from other drugs by at least 4 hours 2. May increase the risk for bleeding 3. Both 1 and 2 4. Neither 1 nor 2 ____ 32. Colestipol comes in a powdered form. The patient is taught to: 1. Take the powder dry and follow it with at least 8 ounces of water 2. Take it with a meal to enhance its action on fatty food 3. Mix the powder with 4 to 6 ounces of milk or fruit juice 4. Take after the evening meal to coincide with cholesterol synthesis ____ 33. The choice of diuretic to use in treating hypertension is based on: 1. Presence of diabetes with loop diuretics being used for these patients 2. Level of kidney function with a thiazide diuretic being used for an estimated glomerular filtration rate higher than the mid-40mL/min range 3. Ethnicity with aldosterone antagonists best for African Americans and older adults 4. Presence of hyperlipidemia with higher doses needed for patients with LDL above 130 mg/dL ____ 34. Direct renin inhibitors have the following properties. They: 1. Are primarily generic drugs 2. Are a renin-angiotensin-aldosterone system (RAAS) medication that is safe during pregnancy 3. Can be used with an angiotensin-converting enzyme and angiotensin II receptor blocker medications for stronger impact 4. “Shut down” the entire RAAS cycle ____ 35. When comparing angiotensin-converting enzyme (ACE) and angiotensin II receptor blocker (ARB) medications, which of the following holds true? 1. Both have major issues with a dry, irritating cough 2. Both contribute to some retention of potassium 3. ARBs have a stronger impact on hypertension control than ACE medications 4. ARBs have stronger diabetes mellitus renal protection properties than ACE medications ____ 36. What does the provider understand about the issue of “Diabetic Renal Protection” with angiotensin-converting enzyme (ACE) medications? Diabetes mellitus patients: 1. Have a reduced rate of renal progression, but still need to be discontinued when advanced renal issues present 2. Who start these medications never progress to renal nephropathy 3. With early renal dysfunction will see it reverse when on ACE medications 4. Without renal issues are the only ones who benefit from ACE protection ____ 37. What dermatological issue is linked to Amiodarone use? 1. Increased risk of basal cell carcinoma 2. Flare up of any prior psoriasis problems 3. Development of plantar warts 4. Progressive change of skin tone toward a blue spectrum ____ 38. Commercials on TV for erectile dysfunction (ED) medications warn about mixing them with nitrates. Why? 1. Increased risk of priapism 2. Profound hypotension 3. Development of blue discoloration to the visual field 4. Inactivation of the ED medication effect Chapter 17. Drugs Affecting the Respiratory System Multiple Choice Identify the choice that best completes the statement or answers the question. ____ 1. Digoxin levels need to be monitored closely when the following medication is started: 1. Loratadine 2. Diphenhydramine 3. Ipratropium 4. Albuterol ____ 2. Patients with pheochromocytoma should avoid which of the following classes of drugs because of the possibility of developing hypertensive crisis? 1. Expectorants 2. Beta-2-agonists 3. Antitussives 4. Antihistamines ____ 3. Harold, a 42-year-old African American, has moderate persistent asthma. Which of the following asthma medications should be used cautiously, if at all? 1. Betamethasone, an inhaled corticosteroid 2. Salmeterol, an inhaled long-acting beta-agonist 3. Albuterol, a short-acting beta-agonist 4. Montelukast, a leukotriene modifier ____ 4. Long-acting beta-agonists (LTBAs) received a Black Box Warning from the U.S. Food and Drug Administration due to the: 1. Risk of life-threatening dermatological reactions 2. Increased incidence of cardiac events when LTBAs are used 3. Increased risk of asthma-related deaths when LTBAs are used 4. Risk for life-threatening alterations in electrolytes ____ 5. The bronchodilator of choice for patients taking propranolol is: 1. Albuterol 2. Pirbuterol 3. Formoterol 4. Ipratropium ____ 6. James is a 52-year-old overweight smoker taking theophylline for his persistent asthma. He tells his provider he is going to start the Atkin’s diet for weight loss. The appropriate response would be: 1. Congratulate him on making a positive change in his life. 2. Recommend he try stopping smoking instead of the Atkin’s diet. 3. Schedule him for regular testing of serum theophylline levels during his diet due to increased excretion of theophylline. 4. Decrease his theophylline dose because a high-protein diet may lead to elevated theophylline levels. ____ 7. Li takes theophylline for his persistent asthma and calls the office with a complaint of nausea, vomiting, and headache. The best advice for him would be to: 1. Reassure him this is probably a viral infection and should be better soon 2. Have him seen the same day for an assessment and theophylline level 3. Schedule him for an appointment in 2 to 3 days, which he can cancel if he is better 4. Order a theophylline level at the laboratory for him ____ 8. Tiotropium bromide (Spiriva) is an inhaled anticholinergic: 1. Used for the treatment of chronic obstructive pulmonary disease (COPD) 2. Used in the treatment of asthma 3. Combined with albuterol for treatment of asthma exacerbations 4. Combined with fluticasone for the treatment of persistent asthma ____ 9. Christy has exercise-induced and mild persistent asthma and is prescribed two puffs of albuterol 15 minutes before exercise and as needed for wheezing. One puff per day of beclomethasone (QVAR) is also prescribed. Teaching regarding her inhalers includes: 1. Use one to two puffs of albuterol per day to prevent an attack with no more than eight puffs per day 2. Beclomethasone needs to be used every day to treat her asthma 3. Report any systemic side effects she is experiencing, such as weight gain 4. Use the albuterol metered-dose inhaler (MDI) immediately after her corticosteroid MDI to facilitate bronchodilation ____ 10. When prescribing montelukast (Singulair) for asthma, patients or parents of patients should be instructed: 1. Montelukast twice a day is started when there is an asthma exacerbation. 2. Patients may experience weight gain on montelukast. 3. Aggression, anxiety, depression, and/or suicidal thoughts may occur when taking montelukast. 4. Lethargy and hypersomnia may occur when taking montelukast. ____ 11. Montelukast (Singulair) may be prescribed for: 1. A 6-year-old child with exercise-induced asthma 2. A 2-year-old child with moderate persistent asthma 3. An 18-month-old child with seasonal allergic rhinitis 4. None of the above; montelukast is not approved for use in children ____ 12. The known drug interactions with the inhaled corticosteroid beclomethasone (QVAR) include: 1. Albuterol 2. MMR vaccine 3. Insulin 4. None of the above ____ 13. When educating patients who are starting on inhaled corticosteroids, the provider should tell them that: 1. They need to get any live vaccines before starting the medication. 2. Inhaled corticosteroids need to be used daily during asthma exacerbations to be effective. 3. Patients should rinse their mouths out after using the inhaled corticosteroid to prevent thrush. 4. They can triple the dose number of inhalations of medication during colds to prevent needing systemic steroids. ____ 14. Patients with allergic rhinitis may benefit from a prescription of: 1. Fluticasone (Flonase) 2. Cetirizine (Zyrtec) 3. OTC cromolyn nasal spray (Nasalcrom) 4. Any of the above ____ 15. Howard is a 72-year-old male who occasionally takes diphenhydramine for his seasonal allergies. Monitoring for this patient taking diphenhydramine would include assessing for: 1. Urinary retention 2. Cardiac output 3. Peripheral edema 4. Skin rash ____ 16. First-generation antihistamines such as loratadine (Claritin) are prescribed for seasonal allergies because they are: 1. More effective than first-generation antihistamines 2. Less sedating than the first-generation antihistamines 3. Prescription products, therefore are covered by insurance 4. Able to be taken with central nervous system (CNS) sedatives, such as alcohol ____ 17. When recommending dimenhydrinate (Dramamine) to treat motion sickness, patients should be instructed to: 1. Take the dimenhydrinate after they get nauseated 2. Drink lots of water while taking the dimenhydrinate 3. Take the dimenhydrinate 15 minutes before it is needed 4. Double the dose if one tablet is not effective ____ 18. Decongestants such as pseudoephedrine (Sudafed): 1. Are Schedule III drugs in all states 2. Should not be prescribed or recommended for children under 4 years of age 3. Are effective in treating the congestion children experience with the common cold 4. May cause drowsiness in patients of all ages ____ 19. Cough and cold medications that contain a sympathomimetic decongestant such as phenylephrine should be used cautiously in what population: 1. Older adults 2. Hypertensive patients 3. Infants 4. All of the above ____ 20. Martin is a 60-year-old patient with hypertension. The first-line decongestant to prescribe would be: 1. Oral pseudoephedrine 2. Oral phenylephrine 3. Nasal oxymetazoline 4. Nasal azelastine ____ 21. The first-line treatment for cough related to an upper respiratory tract infection (URI) in a 5-year-old child is: 1. Fluids and symptomatic care 2. Dextromethorphan and guaifenesin syrup (Robitussin DM for Kids) 3. Guaifenesin and codeine syrup (Tussin AC) 4. Chlorpheniramine and dextromethorphan syrup (Nyquil for Kids) Chapter 18. Drugs Affecting the Hematopoietic System Multiple Choice Identify the choice that best completes the statement or answers the question. ____ 1. Kenneth is taking warfarin and is asking about what he can take for minor aches and pains. The best recommendation is: 1. Ibuprofen 400 mg three times a day 2. Acetaminophen, not to exceed 4 grams per day 3. Prescribe acetaminophen with codeine 4. Aspirin 640 mg three times a day ____ 2. Juanita had a deep vein thrombosis (DVT) and was on heparin in the hospital and was discharged on warfarin. She asks her primary care provider NP why she was getting both medications while in the hospital. The best response is to: 1. Contact the hospitalist as this is not the normal guideline for prescribing these two medications and she may have had a more complicated case. 2. Explain that warfarin is often started while a patient is still on heparin because warfarin takes a few days to reach effectiveness. 3. Encourage the patient to contact the Customer Service department at the hospital as this was most likely a medication error during her admission. 4. Draw anticoagulation studies to make sure she does not have dangerously high bleeding times. ____ 3. The safest drug to use to treat pregnant women who require anticoagulant therapy is: 1. Low-molecular-weight heparin 2. Warfarin 3. Aspirin 4. Heparin ____ 4. The average starting dose of warfarin is 5 mg daily. Higher doses of 7.5 mg daily should be considered in which patients? 1. Pregnant women 2. Elderly men 3. Overweight or obese patients 4. Patients with multiple comorbidities ____ 5. Cecil and his wife are traveling to Southeast Asia on vacation and he has come into the clinic to review his medications. He is healthy with only mild hypertension that is well controlled. He asks about getting “a shot” to prevent blood clots like his friend Ralph did before international travel. The correct respond would be: 1. Administer one dose of low-molecular weight heparin 24 hours before travel. 2. Prescribe one dose of warfarin to be taken the day of travel. 3. Consult with a hematologist regarding a treatment plan for Cecil. 4. Explain that Cecil is not at high risk of a blood clot and provide education about how to prevent blood clots while traveling. ____ 6. Robert, age 51 years, has been told by his primary care provider (PCP) to take an aspirin a day. Why would this be recommended? 1. He has arthritis and this will help with the inflammation and pain. 2. Aspirin has anti-platelet activity and prevents clots that cause heart attacks. 3. Aspirin acidifies the urine and he needs this for prostrate health. 4. He has a history of GI bleed, and one aspirin a day is a safe dosage. ____ 7. Sally has been prescribed aspirin 320 mg per day for her atrial fibrillation. She also takes aspirin four or more times a day for arthritis pain. What are the symptoms of aspirin toxicity for which she would need to be evaluated? 1. Tinnitus 2. Diarrhea 3. Hearing loss 4. Photosensitivity ____ 8. Patient education when prescribing clopidogrel includes: 1. Do not take any herbal products without discussing it with the provider. 2. Monitor urine output closely and contact the provider if it decreases. 3. Clopidogrel can be constipating, use a stool softener if needed. 4. The patient will need regular anticoagulant studies while on clopidogrel. ____ 9. For patients taking warfarin, INRs are best drawn: 1. Monthly throughout therapy 2. Three times a week throughout therapy 3. Two hours after the last dose of warfarin to get an accurate peak level 4. In the morning if the patient takes their warfarin at night ____ 10. Patients receiving heparin therapy require monitoring of: 1. Platelets every 2 to 3 days for thrombocytopenia that may occur on day 4 of therapy 2. Electrolytes for elevated potassium levels in the first 24 hours of therapy 3. INR throughout therapy to stay within the range of 2.0 4. Blood pressure for hypertension that may occur in the first 2 days of treatment ____ 11. The routine monitoring recommended for low molecular weight heparin is: 1. INR every 2 days until stable, then weekly 2. aPTT every week while on therapy 3. Factor Xa levels if the patient is pregnant 4. White blood cell count every 2 weeks ____ 12. When writing a prescription for warfarin it is common to write _________ on the prescription. 1. OK to substitute for generic 2. The brand name of warfarin and Do Not Substitute 3. PRN refills 4. Refills for 1 year ____ 13. Education of patients who are taking warfarin includes discussing their diet. Instructions include: 1. Avoiding all vitamin K-containing foods 2. Avoiding high-vitamin K-containing foods 3. Increasing intake of iron-containing foods 4. Making sure they eat 35 grams of fiber daily ____ 14. Patients who are being treated with epoetin alfa need to be monitored for the development of: 1. Thrombocytopenia 2. Neutropenia 3. Hypertension 4. Gout ____ 15. The FDA issued a safety announcement regarding the use of erythropoiesis-stimulating agents (ESAs) in 2010 with the recommendation that: 1. ESAs no longer be prescribed to patients with chronic renal failure 2. The risk of tumor development be explained to cancer patients on ESA therapy 3. Patients should no longer receive ESA therapy to prepare for allogenic transfusions 4. ESAs be prescribed only to patients younger than age 60 years ____ 16. When patients are started on darbepoetin alfa (Aranesp) they need monitoring of their blood counts to determine a dosage adjustment in: 1. 6 weeks if they are a cancer patient 2. 1 week if they have chronic renal failure 3. 2 weeks if they are taking it for allogenic transfusion 4. Each week throughout therapy ____ 17. Jim is having a hip replacement surgery and would like to self-donate blood for the surgery. In addition to being prescribed epogen alpha he should also be prescribed: 1. Folic acid to prevent megaloblastic anemia 2. Iron, to start when the epogen starts 3. An antihypertensive to counter the adverse effects of epogen 4. Vitamin B12 to prevent pernicious anemia ____ 18. Monitoring for a patient being prescribed iron for iron deficiency anemia includes: 1. Reticulocyte count 1 week after therapy is started 2. Complete blood count every 2 weeks throughout therapy 3. Hemoglobin level at 1 week of therapy 4. INR weekly throughout therapy ____ 19. Patient education regarding taking iron replacements includes: 1. Doubling the dose if they miss a dose to maintain therapeutic levels 2. Taking the iron with milk or crackers if it upsets their stomach 3. Iron is best taken on an empty stomach with juice 4. Antacids such as Tums may help the upset stomach caused by iron therapy ____ 20. Patients with pernicious anemia require treatment with: 1. Iron 2. Folic acid 3. Epogen alpha 4. Vitamin B12 ____ 21. The first laboratory value indication that vitamin B12 therapy is adequately treating pernicious anemia is: 1. Hematocrit levels start to rise 2. Hemoglobin levels return to normal 3. Reticulocyte count begins to rise 4. Vitamin B12 levels return to normal ____ 22. Patients who are beginning therapy with vitamin B12 need to be monitored for: 1. Hypertensive crisis that may occur in the first 36 hours 2. Hypokalemia that occurs in the first 48 hours 3. Leukopenia that occurs at 1 to 3 weeks of therapy 4. Thrombocytopenia that may occur at any time in therapy Chapter 19. Drugs Affecting the Immune System Multiple Choice Identify the choice that best completes the statement or answers the question. ____ 1. Attenuated vaccines are also known as: 1. Killed vaccines 2. Booster vaccines 3. Inactivated vaccines 4. Live vaccines ____ 2. Live attenuated influenza vaccine (FluMist) may be administered to: 1. All patients over 6 months of age 2. Patients between ages 2 and 49 with no risk factors 3. Patients with an upper respiratory infection (URI) or asthma 4. Pregnant women ____ 3. The reason that two MMR vaccines at least a month apart are recommended is: 1. The second dose of MMR “boosts” the immunity built from the first dose. 2. Two vaccines 1 month apart is the standard dosing for all live virus vaccines. 3. If the two MMR vaccine doses are given too close together there is a greater likelihood of severe localized reaction to the vaccine. 4. Only 95% of patients are fully immunized for measles after the first vaccine, with 99% having immunity after two doses of MMR. ____ 4. The MMR vaccine is not recommended for pregnant women because: 1. Pregnant women do not build adequate immunity to the vaccine. 2. There is a risk of the pregnant women developing measles encephalopathy. 3. There is a risk of the fetus developing congenital rubella syndrome. 4. Pregnant women can receive the MMR vaccine. ____ 5. If the measles, mumps, rubella, and varicella (MMRV) combined vaccine is ordered to be given as the first MMR and varicella dose to a child the CDC recommends: 1. Parents be informed of the increased risk of fever and febrile seizures over the MMR plus varicella two-shot regimen. 2. Patients must also receive MMRV as the second dose of MMR and varicella in order to build adequate immunity. 3. Patients be premedicated with acetaminophen 15 minutes before the vaccine is given. 4. Patients should not be around pregnant women for the first 48 hours after the vaccine is given. ____ 6. The rotavirus vaccine (RotaTeq, Rotarix): 1. Is a live vaccine that replicates in the small intestine, providing active immunity against rotavirus 2. Should not be administered to infants who are or may be potentially immunocompromised 3. Is not given to an infant who has a febrile illness (temperature greater than 100.5oF) 4. All of the above ____ 7. Varicella vaccine is recommended to be given to patients who are: 1. HIV positive with a CD4+ T-lymphocyte percentage less than 15% 2. Taking corticosteroids (up to 2 mg/kg/day or less than 20 mg/day) 3. Pregnant 4. Immunocompromised ____ 8. Zoster vaccine (Zostavax) is: 1. A live varicella zoster vaccine from the same strain used to develop the varicella vaccine 2. Effective in preventing varicella zoster in patients of all ages 3. Recommended for patients age 40 to 80 who have had chickenpox 4. Administered at the same time as other live vaccines, as long as they are given the same day ____ 9. True contraindications to diphtheria, tetanus, and acellular pertussis (DTaP or Tdap) vaccine include: 1. Fever up to 104oF (40.5oC) after previous DTaP vaccine 2. Family history of seizures after DTaP vaccine 3. Adolescent pregnancy 4. Anaphylactic reaction with a previous dose ____ 10. Hepatitis B vaccine is contraindicated in patients who: 1. Were born after less than 32 weeks gestation (give first dose at age 6 months) 2. Are pregnant 3. Are on hemodialysis 4. Are allergic to yeast ____ 11. Human papillomavirus (HPV) vaccine (Gardasil, Cervarix): 1. Is a live virus vaccine that provides immunity to six strains of HPV virus 2. Has a common adverse effect of syncope within 15 minutes of giving the vaccine 3. Should not be given to males younger than age 12 years 4. May be given to pregnant women ____ 12. Influenza vaccine may be administered annually to: 1. Patients with an egg allergy 2. Pregnant patients 3. Patients age 6 weeks or older 4. Patients with acute febrile illness ____ 13. Immune globulin serums: 1. Provide active immunity against infectious diseases 2. Are contraindicated during pregnancy 3. Are heated to above body temperature to kill most hepatitis, HIV, and other viruses such as parvovirus 4. Are derived from pooled plasma of adults and contain specific antibodies in proportion to the donor population ____ 14. Hepatitis B immune globulin is administered to provide passive immunity to: 1. Infants born to HBsAg-positive mothers 2. Household contacts of hepatitis-B virus infected people 3. Persons exposed to blood containing hepatitis B virus 4. All of the above ____ 15. Rho(D) immune globulin (RhoGAM) is given to: 1. Infants born to women who are Rh positive 2. Sexual partners of Rh-positive women 3. Rh-negative women after a birth, miscarriage, or abortion 4. Rh-negative women at 36 weeks gestation ____ 16. Tuberculin purified protein derivative: 1. Is administered to patients who are known tuberculin-positive reactors 2. May be administered to patients who are on immunosuppressives 3. May be administered 2 to 3 weeks after an MMR or varicella vaccine 4. May be administered the same day as the MMR and/or varicella vaccine ____ 17. Diane may benefit from cyclosporine (Sandimmune). Cyclosporin may be prescribed to: 1. Treat rheumatoid arthritis 2. Treat patients with corn allergy 3. Pregnant patients 4. Treat patients with liver dysfunction ____ 18. Azathioprine has significant adverse drug effects, including: 1. Hypertension 2. Hirsutism 3. Risk of cancer 4. Gingival hyperplasia ____ 19. Pregnant women should receive the Tdap vaccine: 1. In the first trimester 2. Once every 10 years 3. In the third trimester of every pregnancy 4. Tdap is contraindicated in pregnancy ____ 20. Children who should receive meningococcal conjugate vaccine (Hib-MenCY, MenHibrix) include: 1. Children traveling to the Haj 2. Infants, routinely at 2, 4, 6, and 12 to 15 months 3. Infants with functional asplenia (including sickle cell disease) 4. Two year olds with complement deficiencies Chapter 20. Drugs Affecting the Gastrointestinal System Multiple Choice Identify the choice that best completes the statement or answers the question. ____ 1. Many patients self-medicate with antacids. Which patients should be counseled to not take calcium carbonate antacids without discussing it with their provider or a pharmacist first? 1. Patients with kidney stones 2. Pregnant patients 3. Patients with heartburn 4. Postmenopausal women ____ 2. Patients taking antacids should be educated regarding these drugs, including letting them know that: 1. They may cause constipation or diarrhea 2. Many are high in sodium 3. They should separate antacids from other medications by 1 hour 4. All of the above ____ 3. Kelly has diarrhea and is wondering if she can take loperamide (Imodium) for the diarrhea. Loperamide: 1. Can be given to patients of all ages, including infants and children, for viral gastroenteritis 2. Slows gastric motility and reduces fluid and electrolyte loss from diarrhea 3. Is the treatment of choice for the diarrhea associated with E. coli 0157 4. May be used in pregnancy and by lactating women ____ 4. Bismuth subsalicylate (Pepto Bismol) is a common OTC remedy for gastrointestinal complaints. Bismuth subsalicylate: 1. May lead to toxicity if taken with aspirin 2. Is contraindicated in children with flu-like illness 3. Has antimicrobial effects against bacterial and viral enteropathogens 4. All of the above ____ 5. Hannah will be traveling to Mexico with her church group over spring break to build houses. She is concerned she may develop traveler’s diarrhea. Advice includes following normal food and water precautions as well as taking: 1. Loperamide four times a day throughout the trip 2. Bismuth subsalicylate with each meal and at bedtime 3. A prescription for diphenoxylate with atropine to use if she gets diarrhea 4. None of the above ____ 6. Josie is a 5-year-old patient who presents to the clinic with a 48-hour history of nausea, vomiting, and some diarrhea. She is unable to keep fluids down and her weight is 4 pounds less than her last recorded weight. Besides IV fluids, her exam warrants the use of an antinausea medication. Which of the following would be the appropriate drug to order for Josie? 1. Prochlorperazine (Compazine) 2. Meclizine (Antivert) 3. Promethazine (Phenergan) 4. Ondansetron (Zofran) ____ 7. Jim presents with complaints of “heartburn” that is minimally relieved with Tums (calcium carbonate) and is diagnosed with gastroesophageal reflux disease (GERD). An appropriate first-step therapy would be: 1. Omeprazole (Prilosec) twice a day 2. Ranitidine (Zantac) twice a day 3. Famotidine (Pepcid) once a day 4. Metoclopramide (Reglan) four times a day ____ 8. Patients who are on chronic long-term proton pump inhibitor therapy require monitoring for: 1. Iron deficiency anemia, vitamin B12 and calcium deficiency 2. Folate and magnesium deficiency 3. Elevated uric acid levels leading to gout 4. Hypokalemia and hypocalcemia ____ 9. Sadie is a 72-year-old patient who takes omeprazole for her chronic GERD. Chronic long-term omeprazole use places her at increased risk for: 1. Megaloblastic anemia 2. Osteoporosis 3. Hypertension 4. Strokes ____ 10. Patrick is a 10-year-old patient who presents with uncomfortable constipation. Along with diet changes, a laxative is ordered to provide more rapid relief of constipation. An appropriate choice of medication for a 10-year-old child would be: 1. PEG 3350 (Miralax) 2. Bisacodyl (Dulcolax) suppository 3. Docusate (Colace) suppository 4. Polyethylene glycol electrolyte solution ____ 11. Methylnaltrexone is used to treat constipation in: 1. Patients with functional constipation 2. Patients with irritable bowel syndrome-associated constipation 3. Children with encopresis 4. Opioid-associated constipation ____ 12. An elderly person has been prescribed lactulose for treatment of chronic constipation. Monitoring with long-term treatment would include: 1. Electrolytes, including potassium and chloride 2. Bone mineral density for osteoporosis 3. Magnesium level 4. Liver function Chapter 21. Drugs Affecting the Endocrine System Multiple Choice Identify the choice that best completes the statement or answers the question. ____ 1. Both men and women experience bone loss with aging. The bones most likely to demonstrate significant loss are: 1. Cortical bones 2. Femoral neck bones 3. Cervical vertebrae 4. Pelvic bones ____ 2. Bisphosphonates treat or prevent osteoporosis by: 1. Inhibiting osteoclastic activity 2. Fostering bone resorption 3. Enhancing calcium uptake in the bone 4. Strengthening the osteoclastic proton pump ____ 3. Prophylactic use of bisphosphonates is recommended for patients with early osteopenia related to long-term use of which of the following drugs? 1. Selective estrogen receptor modulators 2. Aspirin 3. Glucocorticoids 4. Calcium supplements ____ 4. Patients with cystic fibrosis are often prescribed enzyme replacement for pancreatic secretions. Each replacement drug has lipase, protease, and amylase components, but the drug is prescribed in units of: 1. Lipase 2. Protease 3. Amylase 4. Pancreatin ____ 5. Brands of pancreatic enzyme replacement drugs are: 1. Bioequivalent 2. About the same in cost per unit of lipase across brands 3. Able to be interchanged between generic and brand-name products to reduce cost 4. None of the above ____ 6. When given subcutaneously, how long until neutral protamine Hagedorn insulin begins to take effect (onset of action) after administration? 1. 15 to 30 minutes 2. 60 to 90 minutes 3. 3 to 4 hours 4. 6 to 8 hours ____ 7. Hypoglycemia can result from the action of either insulin or an oral hypoglycemic. Signs and symptoms of hypoglycemia include: 1. “Fruity” breath odor and rapid respiration 2. Diarrhea, abdominal pain, weight loss, and hypertension 3. Dizziness, confusion, diaphoresis, and tachycardia 4. Easy bruising, palpitations, cardiac dysrhythmias, and coma ____ 8. Nonselective beta blockers and alcohol create serious drug interactions with insulin because they: 1. Increase blood glucose levels 2. Produce unexplained diaphoresis 3. Interfere with the ability of the body to metabolize glucose 4. Mask the signs and symptoms of altered glucose levels ____ 9. Lispro is an insulin analogue produced by recombinant DNA technology. Which of the following statements about this form of insulin is NOT true? 1. Optimal time of preprandial injection is 15 minutes. 2. Duration of action is increased when the dose is increased. 3. It is compatible with neutral protamine Hagedorn insulin. 4. It has no pronounced peak. ____ 10. The decision may be made to switch from twice daily neutral protamine Hagedorn (NPH) insulin to insulin glargine to improve glycemia control throughout the day. If this is done: 1. The initial dose of glargine is reduced by 20% to avoid hypoglycemia. 2. The initial dose of glargine is 2 to 10 units per day. 3. Patients who have been on high doses of NPH will need tests for insulin antibodies. 4. Obese patients may require more than 100 units per day. ____ 11. When blood glucose levels are difficult to control in type 2 diabetes some form of insulin may be added to the treatment regimen to control blood glucose and limit complication risks. Which of the following statements is accurate based on research? 1. Premixed insulin analogues are better at lowering HbA1C and have less risk for hypoglycemia. 2. Premixed insulin analogues and the newer premixed insulins are associated with more weight gain than the oral antidiabetic agents. 3. Newer premixed insulins are better at lowering HbA1C and postprandial glucose levels than long-acting insulins. 4. Patients who are not controlled on oral agents and have postprandial hyperglycemia can have neutral protamine Hagedorn insulin added at bedtime. ____ 12. Metformin is a primary choice of drug to treat hyperglycemia in type 2 diabetes because it: 1. Substitutes for insulin usually secreted by the pancreas 2. Decreases glycogenolysis by the liver 3. Increases the release of insulin from beta cells 4. Decreases peripheral glucose utilization ____ 13. Prior to prescribing metformin, the provider should: 1. Draw a serum creatinine to assess renal function 2. Try the patient on insulin 3. Tell the patient to increase iodine intake 4. Have the patient stop taking any sulfonylurea to avoid dangerous drug interactions ____ 14. The action of “gliptins” is different from other antidiabetic agents because they: 1. Have a low risk for hypoglycemia 2. Are not associated with weight gain 3. Close ATP-dependent potassium channels in the beta cell 4. Act on the incretin system to indirectly increase insulin production ____ 15. Sitagliptin has been approved for: 1. Monotherapy in once-daily doses 2. Combination therapy with metformin 3. Both 1 and 2 4. Neither 1 nor 2 ____ 16. GLP-1 agonists: 1. Directly bind to a receptor in the pancreatic beta cell 2. Have been approved for monotherapy 3. Speed gastric emptying to decrease appetite 4. Can be given orally once daily ____ 17. Avoid concurrent administration of exenatide with which of the following drugs? 1. Digoxin 2. Warfarin 3. Lovastatin 4. All of the above ____ 18. Administration of exenatide is by subcutaneous injection: 1. 30 minutes prior to the morning meal 2. 60 minutes prior to the morning and evening meal 3. 15 minutes after the evening meal 4. 60 minutes before each meal daily ____ 19. Potentially fatal granulocytopenia has been associated with treatment of hyperthyroidism with propylthiouracil. Patients should be taught to report: 1. Tinnitus and decreased salivation 2. Fever and sore throat 3. Hypocalcemia and osteoporosis 4. Laryngeal edema and difficulty swallowing ____ 20. Elderly patients who are started on levothyroxine for thyroid replacement should be monitored for: 1. Excessive sedation 2. Tachycardia and angina 3. Weight gain 4. Cold intolerance ____ 21. Which of the following is not an indication that growth hormone supplements should be discontinued? 1. Imaging indication of epiphyseal closure 2. Growth curve increases have plateaued 3. Complaints of mild bone pain 4. Achievement of anticipated height goals ____ 22. Besides osteoporosis, IV bisphosphonates are also indicated for: 1. Paget’s Disease 2. Early osteopenia 3. Renal cancer 4. Early closure of cranial sutures ____ 23. What is the role of calcium supplements when patients take bisphosphonates? 1. They must be restricted to allow the medication to work. 2. They must be taken in sufficient amounts to provide foundational elements for bone growth. 3. They must be taken at the same time as the bisphosphonates. 4. They only work with bisphosphonates if daily intake is restricted. ____ 24. Which of the following statements about pancreatic enzymes is true? 1. Dosing may be titrated according to the decrease of steatorrhea. 2. The amount of carbohydrates in the meal drives the amount of enzyme used. 3. The amount of medication used is increased with a cystic fibrosis pulmonary flare. 4. The FDA and Internet-available formulations are bioequivalent. ____ 25. Besides cystic fibrosis, which other medical state may trigger the need for pancreatic enzymes? 1. Paget’s disease 2. Pulmonary cancers 3. Gallbladder surgery 4. Some bariatric surgeries Chapter 22. Drugs Affecting the Reproductive System Multiple Choice Identify the choice that best completes the statement or answers the question. ____ 1. Men who use transdermal testosterone gel (AndroGel) should be advised to avoid: 1. Washing their hands after applying the gel 2. Wearing occlusive clothing while using the gel 3. Exposure to estrogens while using the gel 4. Skin-to-skin contact with pregnant women while using the gel ____ 2. Education when prescribing androgens to male patients includes advising that: 1. Short-term use places the patient at risk for hepatocellular carcinoma. 2. Cholestatic hepatitis and jaundice may occur with low doses of androgens. 3. Gynecomastia is a rare occurrence with the use of androgens. 4. Low sperm levels only occur with long-term use of androgens. ____ 3. Patients who are prescribed exogenous androgens need to be warned that decreased libido: 1. Is an unusual side effect of androgens and should be reported to the provider 2. Is treated with increased doses of androgens, so the patient should let the provider know if he is having problems 3. May be a sign of early prostate cancer and he should make an appointment for a prostate screening exam 4. May occur with androgen therapy ____ 4. The U.S. Food and Drug Administration warns that androgens may cause: 1. Peliosis hepatis 2. Orthostatic hypotension 3. Menstrual irregularities 4. Acne ____ 5. Monitoring for a patient who is using androgens includes evaluation of: 1. Complete blood count and C-reactive protein levels 2. Lipid levels and liver function tests 3. Serum potassium and magnesium levels 4. Urine protein and potassium levels ____ 6. Male patients require ______________________ before and during androgen therapy. 1. A digital prostate exam 2. A Doppler exam of testicular blood flow 3. Urine analysis for proteinuria 4. Serial orthostatic blood pressures ____ 7. Absolute contraindications to estrogen therapy include: 1. History of any type of cancer 2. Clotting disorders 3. History of tension headaches 4. Orthostatic hypotension ____ 8. Postmenopausal women with an intact uterus should not be prescribed: 1. Estrogen/progesterone combination 2. IM medroxyprogesterone (Depo Provera) 3. Estrogen alone 4. Androgens ____ 9. Women who have migraines with an aura should not be prescribed estrogen because of: 1. The interaction between triptans and estrogen, limiting migraine therapy choices 2. An increased incidence of migraines with the use of estrogen 3. An increased risk of stroke occurring with estrogen use 4. Patients with migraines may be prescribed estrogen without any concerns ____ 10. A 22-year-old woman receives a prescription for oral contraceptives. Education for this patient includes: 1. Counseling regarding decreasing or not smoking while taking oral contraceptives 2. Advising a monthly pregnancy test for the first 3 months she is taking the contraceptive 3. Advising that she may miss two pills in a row and not be concerned about pregnancy 4. Recommending that her next follow-up visit is in 1 year for a refill and annual exam ____ 11. A 19-year-old female is a nasal Staph aureus carrier and is placed on 5 days of rifampin for treatment. Her only other medication is combined oral contraceptives. What education should she receive regarding her medications? 1. Separate the oral ingestion of the rifampin and oral contraceptive by at least an hour. 2. Both medications are best tolerated if taken on an empty stomach. 3. She should use a back-up method of birth control such as condoms for the rest of the current pill pack. 4. If she gets nauseated with the medications she should call the office for an antiemetic prescription. ____ 12. A 56-year-old woman is complaining of vaginal dryness and dyspareunia. To treat her symptoms with the lowest adverse effects she should be prescribed: 1. Low-dose oral estrogen 2. A low-dose estrogen/progesterone combination 3. A vaginal estradiol ring 4. Vaginal progesterone cream ____ 13. Shana is receiving her first medroxyprogesterone (Depo Provera) injection. Shana will need to be monitored for: 1. Depression 2. Hypertension 3. Weight loss 4. Cataracts ____ 14. When prescribing medroxyprogesterone (Depo Provera) injections, essential education would include advising of the following potential adverse drug effects: 1. Hypertension and dysuria 2. Depression and weight gain 3. Abdominal pain and constipation 4. Orthostatic hypotension and dermatitis ____ 15. The medroxyprogesterone (Depo Provera) injection has a Black Box Warning due to: 1. The potential development of significant hypertension 2. Increased risk of strokes 3. Decreased bone density 4. The risk of a life-threatening rash such as Stevens-Johnson ____ 16. Shana received her first medroxyprogesterone (Depo Provera) injection 6 weeks ago and calls the clinic with a concern that she has been having a light “period” off and on since receiving her Depo shot. What would be the management of Shana? 1. Reassurance that some spotting is normal the first few months of Depo and it should improve. 2. Schedule an appointment for an exam as this is not normal. 3. Prescribe 4 weeks of estrogen to treat the abnormal vaginal bleeding. 4. Order a pregnancy test and suggest she use a back-up method of contraception until she has her next shot. ____ 17. William is a 62-year-old male who is requesting a prescription for sildenafil (Viagra). He should be screened for ________________ before prescribing sildenafil. 1. Renal dysfunction 2. Unstable coronary artery disease 3. Benign prostatic hypertrophy 4. History of priapism ____ 18. Men who are prescribed sildenafil (Viagra) need ongoing monitoring for: 1. Development of chest pain or dizziness 2. Weight gain 3. Priapism 4. Renal function ____ 19. Men who are prescribed an erectile dysfunction drug such as sildenafil (Viagra) should be warned about the risk for: 1. Impotence when combined with antihypertensives 2. Fatal hypotension if combined with nitrates 3. Weight gain if combined with antidepressants 4. All of the above ____ 20. Androgens are indicated for: 1. Symptomatic treatment for male deficiency 2. Female libido, endometriosis, and postmenopausal symptoms 3. Increased muscle mass 4. Symptomatic treatment in both sexes for cancer and HIV 5. 1, 2, and 4 6. All of the above ____ 21. Long-term use of androgens requires specific laboratory monitoring of: 1. Glucose, calcium, testosterone, and thyroid function 2. Calcium, testosterone, PSA, and liver function 3. Calcium, testosterone, PSA, liver function, glucose, and lipids 4. CBC, testosterone, PSA, and thyroid level ____ 22. Effects of estrogen include: 1. Regulation of the menstrual cycle 2. Maintenance of bone density by increasing bone reabsorption 3. Maintenance of the normal structure of the skin and blood vessels 4. A and C 5. All of the above ____ 23. Absolute contraindications that clinicians must consider when initiating estrogen therapy include: 1. Undiagnosed dysfunctional uterine bleeding 2. Deep vein or arterial thromboemboli within the prior year 3. Endometriosis 4. 1 and 2 5. All of the above ____ 24. Patients taking hormonal contraceptives and hormone replacement therapy need to take the drug daily at the same time to prevent: 1. Nausea 2. Breakthrough bleeding 3. Breast tenderness 4. Pregnancy Chapter 23. Drugs Affecting the Integumentary System Multiple Choice Identify the choice that best completes the statement or answers the question. ____ 1. Erik presents with one golden-crusted lesion at the site of an insect bite consistent with impetigo. His parents have limited finances and request the least expensive-treatment. Which medication would be the best choice for treatment? 1. Mupirocin (Bactroban) 2. Bacitracin and polymixin B (generic double antibiotic ointment) 3. Retapamulin (Altabax) 4. Oral cephalexin (Keflex) ____ 2. Juakeem is a nasal methicillin resistant staphylococcus aureus (MRSA) carrier. Treatment to eradicate nasal MRSA is mupirocin. Patient education regarding treating nasal MRSA includes: 1. Take the oral medication exactly as prescribed. 2. Insert one-half of the dose in each nostril twice a day. 3. Alternate treating one nare in the morning and the other in the evening. 4. Nasal MRSA eradication requires at least 4 weeks of therapy, with up to 8 weeks needed in some patients. ____ 3. Instructions for applying a topical antibiotic or antiviral ointment include: 1. Apply thickly to the infected area, spreading the medication well past the borders of the infection. 2. If the rash worsens, apply a thicker layer of medication to settle down the infection. 3. Wash hands before and after application of topical antimicrobials. 4. None of the above ____ 4. When Sam used clotrimazole (Lotrimin AF) for athlete’s foot he developed a red, itchy rash consistent with a hypersensitivity reaction. He now has athlete’s foot again. What would be a good choice of antifungal for Sam? 1. Miconazole (Micatin) powder 2. Ketoconazole (Nizoral) cream 3. Terbinafine (Lamisil) cream 4. Griseofulvin (Grifulvin V) suspension ____ 5. When prescribing griseofulvin (Grifulvin V) to treat tinea capitis it is critical to instruct the patient or parent to: 1. Mix the griseofulvin with ice cream before administering 2. Take the griseofulvin until the tinea clears, in approximately 4 to 5 weeks 3. Shampoo with baby shampoo daily while taking the griseofulvin 4. Griseofulvin is best absorbed if ingested with a high-fat food. ____ 6. First-line therapy for treating topical fungal infections such as tinea corporis (ringworm) or tinea pedis (athlete’s foot) would be: 1. OTC topical azole (clotrimazole, miconazole) 2. Oral terbinafine 3. Oral griseofulvin microsize 4. Nystatin cream or ointment ____ 7. When prescribing topical penciclovir (Denavir) for the treatment of herpes labialis (cold sores) patient education would include: 1. Spread penciclovir liberally all over lips and area surrounding lips. 2. Penciclovir therapy is started at the first sign of a cold sore outbreak. 3. Skin irritation is normal with penciclovir and it should resolve. 4. The penciclovir should be used a minimum of 2 weeks to prevent recurrence. ____ 8. Erika has been prescribed isotretinoin (Accutane) by her dermatologist and is presenting to her primary care provider with symptoms of sadness and depression. A Beck’s Depression Scale indicates she has mild to moderate depression. What would be the best care for her at this point? 1. Prescribe a select serotonin reuptake inhibitor (SSRI) antidepressant 2. Refer her to a mental health therapist 3. Contact her dermatologist about discontinuing the isotretinoin 4. Reassure her that mood swings are normal and schedule follow up in a week ____ 9. Drew is a 17-year-old competitive runner who presents with complaint of pain in his hip that occurred after he fell while running. His only medical problem is severe acne for which he takes isotretinoin (Accutane). With this history what would you be concerned for? 1. He may have pulled a muscle and needs to rest to recover. 2. He is at risk for bone injuries and needs to be evaluated for fracture. 3. Isotretinoin interacts with ibuprofen which is the pain medication of choice. 4. Teen athletes are at risk for repetitive stress injuries. ____ 10. Catherine calls the clinic with concerns that her acne is worse 1 week after starting topical tretinoin. What would be the appropriate care for her? 1. Change her to a different topical acne medication as she is having an adverse reaction to the tretinoin. 2. Switch her to an oral antibiotic to treat her acne. 3. Advise her to apply an oil-based lotion to her face to soothe the redness. 4. Reassure her that the worsening of acne is normal and it should improve with continued use. ____ 11. Li is a 6-month-old infant with severe eczema. She would benefit from topical corticosteroid therapy. Instructions for using topical corticosteroids in children include: 1. Apply liberally to all areas with eczema. 2. Double the frequency of application when the eczema is severe. 3. Apply sparingly to eczema areas. 4. Cover the eczema area with an occlusive dressing after applying a corticosteroid. ____ 12. Jose has had eczema for many years and reports that he thinks his corticosteroid cream is not working as well as it was previously. He may be experiencing tolerance to the corticosteroid. Treatment options include: 1. Increase the potency of the corticosteroid cream. 2. Recommend an interrupted or cyclic schedule of application. 3. Increase the frequency of dosing of the corticosteroid. 4. Discontinue the corticosteroid because it isn’t working any longer . ____ 13. When prescribing tacrolimus (Protopic) to treat atopic dermatitis patients should be informed that: 1. Tacrolimus is the most effective if it is used continuously for 4 to 6 months. 2. Tacrolimus should be spread generously over the affected area. 3. The FDA has issued a Black Box warning about the use of tacrolimus and the development of cancer in animals and humans. 4. The FDA recommends patients be screened for cancer before prescribing tacrolimus. ____ 14. Patients who are treated with greater than 100 grams per week of topical calcipotriene for psoriasis need to be monitored for: 1. High vitamin D levels 2. Hyperkalemia 3. Hypercalcemia 4. Hyperuricemia ____ 15. Jesse is prescribed tazarotene for his psoriasis. Patient education regarding topical tazarotene includes instructing them: 1. That tazarotene is applied in a thin film to the psoriasis plaque lesions 2. To apply it liberally to all psoriatic lesions 3. To apply tazarotene to nonaffected areas to prevent breakout 4. That tazarotene may cause hypercalcemia if it is overused ____ 16. Instructions for the use of selenium sulfide shampoo (Selsun) to treat scalp seborrhea include: 1. Shampoo daily and rinse well. 2. Worsening of seborrhea for the first week is normal. 3. Seborrhea usually clears up after a few weeks of treatment. 4. Shampoo twice a week for 2 weeks, then weekly. ____ 17. Topical diphenhydramine (Benadryl) is available OTC to treat itching. Patients or parents should be instructed regarding the use of topical diphenhydramine that: 1. For maximum effectiveness in treating itching, combine topical with oral diphenhydramine. 2. Topical diphenhydramine is the treatment of choice in treating poison ivy or poison oak. 3. Topical diphenhydramine should not be used in children younger than age 2 years. 4. When applying topical diphenhydramine, apply the cream liberally to all areas that itch. ____ 18. A patient has been prescribed silver sulfadiazine (Silvadene) cream to treat burns on his leg. Normal adverse effects of silver sulfadiazine cream include: 1. Transient leukopenia on days 2 to 4 that should resolve 2. Worsening of burn symptoms briefly before resolution 3. A red, scaly rash that will resolve with continued use 4. Hypercalcemia ____ 19. Instructions for the use of malathion (Ovide) for head lice include: 1. Use a blow dryer to dry the hair after applying. 2. Malathion (Ovide) is used daily for a week until all lice are dead. 3. Rinse the malathion (Ovide) off and shampoo hair after 8 to 12 hours. 4. Use gloves to apply the malathion (Ovide). ____ 20. When writing a prescription of permethrin 5% cream (Elimite) for scabies, patient education would include: 1. All members of the household and personal contacts should also be treated. 2. Infants should have permethrin applied from the neck down. 3. The permethrin is washed off after 10 to 20 minutes. 4. Permethrin is flammable and to avoid open flame while the medication is applied. Chapter 24. Drugs Used in Treating Infectious Diseases Multiple Choice Identify the choice that best completes the statement or answers the question. ____ 1. Factors that place a patient at risk of developing an antimicrobial-resistant organism include: 1. Age over 50 years 2. School attendance 3. Travel within the U.S. 4. Inappropriate use of antimicrobials ____ 2. Infants and young children are at higher risk of developing antibiotic-resistant infections due to: 1. Developmental differences in pharmacokinetics of the antibiotics in children 2. The fact that children this age are more likely to be in daycare and exposed to pathogens from other children 3. Parents of young children insisting on preventive antibiotics so they don’t miss work when their child is sick 4. Immunosuppression from the multiple vaccines they receive in the first 2 years of life ____ 3. Providers should use an antibiogram when prescribing. An antibiogram is: 1. The other name for the Centers for Disease Control guidelines for prescribing antibiotics 2. An algorithm used for prescribing antibiotics for certain infections 3. The reference also known as the Pink Book, published by the Centers for Disease Control 4. A chart of the local resistance patterns to antibiotics developed by laboratories ____ 4. There is often cross-sensitivity and cross-resistance between penicillins and cephalosporins because: 1. Renal excretion is similar in both classes of drugs. 2. When these drug classes are metabolized in the liver they both produce resistant enzymes. 3. Both drug classes contain a beta-lactam ring that is vulnerable to beta-lactamase-producing organisms. 4. There is not an issue with cross-resistance between the penicillins and cephalosporins. ____ 5. Jonathan has been diagnosed with strep throat and needs a prescription for an antibiotic. He says the last time he had penicillin he developed a red, blotchy rash. An appropriate antibiotic to prescribe would be: 1. Penicillin VK, because his rash does not sound like a serious rash 2. Amoxicillin 3. Cefadroxil (Duricef) 4. Azithromycin ____ 6. Sarah is a 25-year-old female who is 8 weeks pregnant and has a urinary tract infection. What would be the appropriate antibiotic to prescribe for her? 1. Ciprofloxacin (Cipro) 2. Amoxicillin (Trimox) 3. Doxycycline 4. Trimethoprim-sulfamethoxazole (Septra) ____ 7. Pong-tai is a 12-month-old child who is being treated with amoxicillin for acute otitis media. His parents call the clinic and say he has developed diarrhea. The appropriate action would be to: 1. Advise the parents that some diarrhea is normal with amoxicillin and recommend probiotics daily. 2. Change the antibiotic to one that is less of a gastrointestinal irritant. 3. Order stool cultures for suspected viral pathogens not treated by the amoxicillin. 4. Recommend increased fluids and fiber in his diet. ____ 8. Lauren is a 13-year-old child who comes to clinic with a 4-day history of cough, low-grade fever, and rhinorrhea. When she blows her nose or coughs the mucous is greenish-yellow. The appropriate antibiotic to prescribe would be: 1. Amoxicillin 2. Amoxicillin/clavulanate 3. TMP/SMZ (Septra) 4. None ____ 9. Joanna had a small ventricle septal defect (VSD) repaired when she was 3 years old and has no residual cardiac problems. She is now 28 and is requesting prophylactic antibiotics for an upcoming dental visit. The appropriate antibiotic to prescribe according to current American College of Cardiology and American Heart Association guidelines is: 1. None, no antibiotic is required for dental procedures 2. Amoxicillin 2 grams 1 hour before the procedure 3. Ampicillin 2 grams IM or IV 30 minutes before the procedure 4. Azithromycin 1 gram 1 hour before the procedure ____ 10. To prevent further development of antibacterial resistance it is recommended that fluoroquinolones be reserved for treatment of: 1. Urinary tract infections in young women 2. Upper respiratory infections in adults 3. Skin and soft tissue infections in adults 4. Community-acquired pneumonia in patients with comorbidities ____ 11. Fluoroquinolones have a Black Box Warning regarding ________ even months after treatment. 1. Renal dysfunction 2. Hepatic toxicity 3. Tendon rupture 4. Development of glaucoma ____ 12. Janet was recently treated with clindamycin for an infection. She calls the advice nurse because she is having frequent diarrhea that she thinks may have blood in it. What would be the appropriate care for her? 1. Encourage increased fluids and fiber. 2. Assess her for pseudomembranous colitis. 3. Advise her to eat yogurt daily to help restore her gut bacteria. 4. Start her on an antidiarrheal medication. ____ 13. Keng has chronic hepatitis that has led to mildly impaired liver function. He has an infection that would be best treated by a macrolide. Which would be the best choice for a patient with liver dysfunction? 1. Azithromycin (Zithromax) 2. Clarithromycin (Biaxin) 3. Erythromycin (E-mycin) 4. None of the above ____ 14. Jamie has glucose-6-phosphate dehydrogenase deficiency (G6PD) and requires an antibiotic. Which class of antibiotics should be avoided in this patient? 1. Penicillins 2. Macrolides 3. Cephalosporins 4. Sulfonamides ____ 15. If a patient is allergic to sulfonamide antibiotics, he or she will most likely have cross-sensitivity to: 1. Loop diuretics 2. Sulfonylureas 3. Thiazide diuretics 4. All of the above ____ 16. Tetracyclines such as minocycline are safe to use in: 1. Pregnant women 2. Adolescents 3. Patients with renal dysfunction 4. Patients with hepatic dysfunction ____ 17. Tetracyclines should not be prescribed to children younger than 8 years due to: 1. Risk of developing cartilage problems 2. Development of significant diarrhea 3. Risk of kernicterus 4. Adverse effects on bone growth ____ 18. Nicole is a 16-year-old female who is taking minocycline for acne. She comes to the clinic complaining of a headache. What would be the plan of care? 1. Advise acetaminophen or ibuprofen as needed for headaches. 2. Prescribe sumatriptan (Imitrex) to be taken at the onset of the headache. 3. Evaluate her for pseudotremor cerebri. 4. Assess her caffeine intake and sleep patterns. ____ 19. Patricia has been prescribed doxycycline for a chlamydia infection. She is healthy and her only medication is an oral combined contraceptive. Patricia’s education would include: 1. Use a back-up method of birth control (condom) until her next menses. 2. Doxycycline may cause tendonitis and she should report any joint pain. 3. Her partner will need treatment if her infection doesn’t clear with the doxycycline. 4. Doxycycline is used for one-dose treatment of STIs; take the whole prescription at once. ____ 20. To prevent the development of peripheral neuropathy in patients taking isoniazid for tuberculosis the patient is also prescribed: 1. Niacin (vitamin B3) 2. Pyridoxine (vitamin B6) 3. Riboflavin (vitamin B2) 4. Thiamine (vitamin B1) ____ 21. Sadie is an 82-year-old patient who has herpes zoster (shingles) and would benefit from an antiviral such as valacyclovir. Prior to prescribing valacyclovir she will need an assessment of: 1. Complete blood count to rule out anemia 2. Liver function 3. Renal function 4. Immunocompetence ____ 22. When prescribing acyclovir, patients should be educated regarding the: 1. High risk of developing diarrhea 2. Need to drink lots of fluids during treatment 3. Risk for life-threatening rash such as Stevens-Johnson 4. Eccentric dosing schedule ____ 23. Nicholas has been diagnosed with type A influenza. Appropriate prescribing of oseltamivir (Tamiflu) would include: 1. Starting oseltamivir within the first 48 hours of influenza symptoms 2. Advising the patient he can stop the oseltamivir when his symptoms resolve 3. Educating the patient that oseltamivir will cure influenza 4. Prophylactic treatment of all family members ____ 24. Monitoring for patients who are on long-term antifungal therapy with ketoconazole includes: 1. Platelet count 2. BUN and creatinine 3. White blood cell count 4. AST, ALT, alkaline phosphatase, and bilirubin ____ 25. When prescribing metronidazole (Flagyl) to treat bacterial vaginosis, patient education would include: 1. Metronidazole is safe in the first trimester of pregnancy. 2. Consuming alcohol in any form may cause a severe reaction. 3. Sexual partners need concurrent therapy. 4. Headaches are a sign of a serious adverse reaction and need immediate evaluation. ____ 26. Every antibiotic drug class has resistant organisms that influence prescribing decisions. 1. True 2. False Chapter 25. Drugs Used in Treating Inflammatory Processes Multiple Choice Identify the choice that best completes the statement or answers the question. ____ 1. Henry presents to clinic with a significantly swollen, painful great toe and is diagnosed with gout. Of the following, which would be the best treatment for Henry? 1. High-dose colchicine 2. Low-dose colchicine 3. High-dose aspirin 4. Acetaminophen with codeine ____ 2. Patient education when prescribing colchicine includes: 1. Colchicine may be constipating. 2. Colchicine always causes some degree of diarrhea. 3. Mild muscle weakness is normal. 4. Moderate amounts of alcohol are safe with colchicine. ____ 3. Larry is taking allopurinol to prevent gout. Monitoring of a patient who is taking allopurinol includes: 1. Complete blood count 2. Blood glucose 3. C-reactive protein 4. BUN, creatinine, and creatinine clearance ____ 4. Phil is starting treatment with febuxostat (Uloric). Education of patients starting febuxostat includes: 1. Gout may worsen with therapy. 2. Febuxostat may cause severe diarrhea. 3. He should consume a high-calcium diet. 4. He will need frequent CBC monitoring. ____ 5. Sallie has been taking 10 mg per day of prednisone for the past 6 months. She should be assessed for: 1. Gout 2. Iron deficiency anemia 3. Osteoporosis 4. Renal dysfunction ____ 6. Patients whose total dose of prednisone will exceed 1 gram will most likely need a second prescription for: 1. Metformin, a biguanide to prevent diabetes 2. Omeprazole, a proton pump inhibitor to prevent peptic ulcer disease 3. Naproxen, an NSAID to treat joint pain 4. Furosemide, a diuretic to treat fluid retention ____ 7. Daniel has been on 60 mg of prednisone for 10 days to treat a severe asthma exacerbation. It is time to discontinue the prednisone. How is prednisone discontinued? 1. Patients with asthma are transitioned directly off the prednisone onto inhaled corticosteroids. 2. Prednisone can be abruptly discontinued with no adverse effects. 3. Develop a tapering schedule to slowly wean Daniel off the prednisone. 4. Substitute the prednisone with another anti-inflammatory such as ibuprofen. ____ 8. Patients with rheumatoid arthritis who are on chronic low-dose prednisone will need co-treatment with which medications to prevent further adverse effects? 1. A bisphosphonate 2. Calcium supplementation 3. Vitamin D 4. All of the above ____ 9. Patients who are on or who will be starting chronic corticosteroid therapy need monitoring of: 1. Serum glucose 2. Stool culture 3. Folate levels 4. Vitamin B12 ____ 10. Patients who are on chronic long-term corticosteroid therapy need education regarding: 1. Receiving all vaccinations, especially the live flu vaccine 2. Reporting black tarry stools or abdominal pain 3. Eating a high carbohydrate diet with plenty of fluids 4. Small amounts of alcohol are generally tolerated. ____ 11. All nonsteroidal anti-inflammatory drugs (NSAIDS) have an FDA Black Box Warning regarding: 1. Potential for causing life-threatening GI bleeds 2. Increased risk of developing systemic arthritis with prolonged use 3. Risk of life-threatening rashes, including Stevens-Johnson 4. Potential for transient changes in serum glucose ____ 12. Jamie has fractured his ankle and has received a prescription for acetaminophen and hydrocodone (Vicodin). Education when prescribing Vicodin includes: 1. It is okay to double the dose of Vicodin if the pain is severe. 2. Vicodin is not habit-forming. 3. He should not take any other acetaminophen-containing medications. 4. Vicodin may cause diarrhea; increase his fluid intake. ____ 13. When prescribing NSAIDS, a complete drug history should be conducted as NSAIDs interact with these drugs: 1. Omeprazole, a proton pump inhibitor 2. Combined oral contraceptives 3. Diphenhydramine, an antihistamine 4. Warfarin, an anticoagulant ____ 14. Josefina is a 2-year-old child with acute otitis media and an upper respiratory infection. Along with an antibiotic she receives a recommendation to treat the ear pain with ibuprofen. What education would her parent need regarding ibuprofen? 1. They can cut an adult ibuprofen tablet in half to give Josefina. 2. The ibuprofen dose can be doubled for severe pain. 3. Josefina needs to be well-hydrated while taking ibuprofen. 4. Ibuprofen is completely safe in children with no known adverse effects. ____ 15. Henry is 82 years old and takes two aspirin every morning to treat the arthritis pain in his back. He states the aspirin helps him to “get going” each day. Lately he has had some heartburn from the aspirin. After ruling out an acute GI bleed, what would be an appropriate course of treatment for Henry? 1. Add an H2 blocker such as ranitidine to his therapy. 2. Discontinue the aspirin and switch him to Vicodin for the pain. 3. Decrease the aspirin dose to one tablet daily. 4. Have Henry take an antacid 15 minutes before taking the aspirin each day. ____ 16. The trial period to determine effective anti-inflammatory activity aspirin for rheumatoid arthritis is: 1. 48 hours 2. 4 to 6 days 3. 4 weeks 4. 2 months ____ 17. Patients prescribed aspirin therapy require education regarding the signs of aspirin toxicity. An early sign of aspirin toxicity is: 1. Black tarry stools 2. Vomiting 3. Tremors 4. Tinnitus ____ 18. Monitoring a patient on a high-dose aspirin level includes: 1. Salicylate level 2. Complete blood count 3. Urine pH 4. All of the above ____ 19. Patients who are on long-term aspirin therapy should have ______ annually. 1. Complete blood count 2. Salicylate level 3. Amylase 4. Urine analysis Chapter 26. Drugs Used in Treating Eye and Ear Disorders Multiple Choice Identify the choice that best completes the statement or answers the question. ____ 1. The Centers for Disease Control recommends all newborn infants receive prophylactic administration of __________ within 1 hour of birth. 1. Gentamicin ophthalmic ointment 2. Ciprofloxacin ophthalmic drops 3. Erythromycin oral suspension 4. Erythromycin ophthalmic ointment ____ 2. Conjunctivitis in a child that is accompanied by acute otitis media is treated with: 1. Sulfacetamide 10% ophthalmic solution (Bleph-10) 2. Bacitracin/polymyxin B (Polysporin) ophthalmic drops 3. Ciprofloxacin (Ciloxan) ophthalmic drops 4. High-dose oral amoxicillin ____ 3. Twenty-year-old Annie comes to the clinic complaining of copious yellow-green eye discharge. Gram stain indicates she most likely has gonococcal conjunctivitis. While awaiting the culture results, the plan of care should be: 1. None, wait for the culture results to determine the course of treatment 2. Ciprofloxacin (Ciloxan) ophthalmic drops 3. IM ceftriaxone 4. High-dose oral amoxicillin ____ 4. Education of women who are being treated with ophthalmic antibiotics for conjunctivitis includes: 1. Throwing away eye makeup and purchasing new 2. Redness and intense burning is normal with ophthalmic antibiotics 3. When applying eye ointment, set the tip of the tube on the lower lid and squeeze in inch 4. Use a cotton swab to apply ointment, spreading the ointment all over the lid and in the conjunctival sac ____ 5. Sadie was prescribed betaxolol ophthalmic drops by her ophthalmologist to treat her glaucoma. Oral beta blockers should be avoided in patients who use ophthalmic beta blockers because: 1. There may be an antagonistic reaction between the two. 2. The additive effects may include bradycardia. 3. They may potentiate each other and cause respiratory depression. 4. The additive effects may cause metabolic acidosis. ____ 6. David presents to the clinic with symptoms of allergic conjunctivitis. He is prescribed cromolyn sodium (Opticrom) eye drops. The education regarding using cromolyn eye drops includes: 1. He should not wear his soft contacts while using the cromolyn eye drops. 2. Cromolyn drops are instilled once a day to prevent allergy symptoms. 3. Long-term use may cause glaucoma. 4. He may experience bradycardia as an adverse effect. ____ 7. Ciprofloxacin otic drops are contraindicated in: 1. Children 2. Patients with acute otitis externa 3. Patients with a perforated tympanic membrane 4. Swimmer’s ear ____ 8. __________ is / are prescribed to prevent swimmer’s ear. 1. Ciprofloxacin otic drops (Ciloxan) 2. Isopropyl ear drops (EarSol) 3. Colistin (Coly-Mycin S Otic) 4. Gentamicin otic drops ____ 9. Patient education regarding the use of ciprofloxacin-hydrocortisone (Cipro HC otic) ear drops includes: 1. Fill the canal with the drops with each dose. 2. Some redness and itching around the ear canal is normal. 3. Warm the bottle of ear drops in his or her hand before administering. 4. Cipro HC otic may cause ototoxicity. ____ 10. Janie presents to the clinic with hard ear wax in both ear canals. Instructions regarding home removal of hard cerumen include: 1. Moisten a cotton swab (Q-tip) and swab the ear canal twice daily. 2. Instill tap water in both ears while bathing. 3. Squirt hydrogen peroxide into ears with each bath. 4. Instill carbamide peroxide (Debrox) twice daily until canals are clear. Chapter 27. Anemia Multiple Choice Identify the choice that best completes the statement or answers the question. ____ 1. Pernicious anemia is treated with: 1. Folic acid supplements 2. Thiamine supplements 3. Vitamin B12 4. Iron ____ 2. Premature infants require iron supplementation with: 1. 10 mg/day of iron 2. 2 mg/kg per day until age 12 months 3. 7 mg/day in their diet 4. 1 mg/kg per day until they are receiving adequate intake of iron from foods ____ 3. Breastfed infants should receive iron supplementation of: 1. 3 mg/kg per day 2. 6 mg/kg per day 3. 1 mg/kg per day 4. Breastfed babies do not need iron supplementation ____ 4. Valerie presents to the clinic with menorrhagia. Her hemoglobin is 10.2 and her ferritin is 15 ng/mL. Initial treatment for her anemia would be: 1. 18 mg/day of iron supplementation 2. 6 mg/kg per day of iron supplementation 3. 325 mg ferrous sulfate per day 4. 325 mg ferrous sulfate tid ____ 5. Chee is a 15-month-old male whose screening hemoglobin is 10.4 g/dL. Treatment for his anemia would be: 1. 18 mg/day of iron supplementation 2. 6 mg/kg per day of elemental iron 3. 325 mg ferrous sulfate per day 4. 325 mg ferrous sulfate tid ____ 6. Monitoring for a patient taking iron to treat iron deficiency anemia is: 1. Hemoglobin, hematocrit, and ferritin 4 weeks after treatment is started 2. Complete blood count every 4 weeks throughout treatment 3. Annual complete blood count 4. Reticulocyte count in 4 weeks ____ 7. Valerie has been prescribed iron to treat her anemia. Education of patients prescribed iron would include: 1. Take the iron with milk if it upsets her stomach. 2. Antacids may help with the nausea and GI upset caused by iron. 3. Increase fluids and fiber to treat constipation. 4. Iron is best tolerated if it is taken at the same time as her other medications. ____ 8. Allie has just had her pregnancy confirmed and is asking about how to ensure a healthy baby. What is the folic acid requirement during pregnancy? 1. 40 mcg/day 2. 200 mcg/day 3. 800 mcg/day 4. 2 gm/day ____ 9. Kyle has Crohn’s disease and has a documented folate deficiency. Drug therapy for folate deficiency anemia is: 1. Oral folic acid 1 to 2 mg per day 2. Oral folic acid 1 gram per day 3. IM folate weekly for at least 6 months 4. Oral folic acid 400 mcg daily ____ 10. Patients who are being treated for folate deficiency require monitoring of: 1. Complete blood count every 4 weeks 2. Hematocrit and hemoglobin at 1 week and then at 8 weeks 3. Reticulocyte count at 1 week 4. Folate levels every 4 weeks until hemoglobin stabilizes ____ 11. The treatment of vitamin B12 deficiency is: 1. 1,000 mcg daily of oral cobalamin 2. 2 gm per day of oral cobalamin 3. Vitamin B12 100 mcg/day IM 4. 500 mcg/dose nasal cyanocobalamin 2 sprays once a week ____ 12. The dosage of Vitamin B12 to initially treat pernicious anemia is: 1. Nasal cyanocobalamin 1 gram spray in each nostril daily x 1 week then weekly x 1 month 2. Vitamin B12 IM monthly 3. Vitamin B12 1,000 mcg IM daily x 1 week then 1,000 mg IM weekly for a month 4. Oral cobalamin 1,000 mcg daily ____ 13. Before beginning IM vitamin B12 therapy, which laboratory values should be obtained? 1. Reticulocyte count, hemoglobin, and hematocrit 2. Iron 3. Vitamin B12 4. All of the above ____ 14. ________ should be monitored when vitamin B12 therapy is started. 1. Serum calcium 2. Serum potassium 3. Ferritin 4. C-reactive protein ____ 15. Anemia due to chronic renal failure is treated with: 1. Epoetin alfa (Epogen) 2. Ferrous sulfate 3. Vitamin B12 4. Hydroxyurea Chapter 28. Chronic Stable Angina and Low-Risk Unstable Angina Multiple Choice Identify the choice that best completes the statement or answers the question. ____ 1. Angina is produced by an imbalance between myocardial oxygen supply (MOS) and demand (MOD) in the myocardium. Which of the following drugs help to correct this imbalance by increasing MOS? 1. Calcium channel blockers 2. Beta blockers 3. Angiotensin-converting-enzyme (ACE) inhibitors 4. Aspirin ____ 2. Not all chest pain is caused by myocardial ischemia. Noncardiac causes of chest pain include: 1. Pulmonary embolism 2. Pneumonia 3. Gastroesophageal reflux 4. All of the above ____ 3. The New York Heart Association and the Canadian Cardiovascular Society have described grading criteria for levels of angina. Angina that occurs with unusually strenuous activity or on walking or climbing stair after meals is class: 1. I 2. II 3. III 4. IV ____ 4. Patients at high risk for developing significant coronary heart disease are those with: 1. LDL values between 100 and 130 2. Systolic blood pressure between 120 and 130 3. Class III angina 4. Obesity ____ 5. To reduce mortality, all patients with angina, regardless of class, should be on: 1. Aspirin 81 to 325 mg/d 2. Nitroglycerin sublingually for chest pain 3. ACE inhibitors or angiotensin receptor blockers 4. Digoxin ____ 6. Patients who have angina, regardless of class, who are also diabetic, should be on: 1. Nitrates 2. Beta blockers 3. ACE inhibitors 4. Calcium channel blockers ____ 7. Management of all types and grades of angina includes the use of lifestyle modification to reduce risk factors. Which of these modifications are appropriate for which reason? Both the modification and the reason for it must be true for the answer to be correct. 1. Lose at least 10 pounds of body weight. Excessive weight increases cardiac workload. 2. Reduce sodium intake to no more than 2,400 mg of sodium. Sodium increases blood volume and cardiac workload. 3. Increase potassium intake to at least 100 mEq/d. The heart needs higher levels of potassium to improve contractility and oxygen supply. 4. Intake a moderate amount of alcohol. Moderate intake has been shown by research to improve cardiac function. ____ 8. Nitrates are especially helpful for patients with angina who also have: 1. Heart failure 2. Hypertension 3. Both 1 and 2 4. Neither 1 nor 2 ____ 9. Beta blockers are especially helpful for patients with exertional angina who also have: 1. Arrhythmias 2. Hypothyroidism 3. Hyperlipidemia 4. Atherosclerosis ____ 10. Rapid-acting nitrates are important for all angina patients. Which of the following are true statements about their use? 1. These drugs are useful for immediate symptom relief when the patient is certain it is angina. 2. The dose is one sublingual tablet or spray every 5 minutes until the chest pain goes away. 3. Take one nitroglycerine tablet or spray at the first sign of angina; repeat every 5 minutes for no more than two doses. If chest pain is still not relieved, call 911. 4. All of the above ____ 11. Isosorbide dinitrate is a long-acting nitrate given twice daily. The schedule for administration is 7 a.m. and 2 p.m. because: 1. Long-acting forms have a higher risk for toxicity. 2. Orthostatic hypotension is a common adverse effect. 3. It must be taken with milk or food. 4. Nitrate tolerance can develop. ____ 12. Combinations of a long-acting nitrate and a beta blocker are especially effective in treating angina because: 1. Nitrates increase MOS and beta blockers increase MOD. 2. Their additive effects permit lower doses of both drugs and their adverse reactions cancel each other out. 3. They address the pathology of patients with exertional angina who have fixed atherosclerotic coronary heart disease. 4. All of the above ____ 13. Drug choices to treat angina in older adults differ from those of younger adults only in: 1. Consideration of risk factors for diseases associated with and increased in aging 2. The placement of drug therapy as a treatment choice before lifestyle changes are tried 3. The need for at least three drugs in the treatment regimen because of the complexity of angina in the older adult 4. Those with higher risk for silent myocardial infarction ____ 14. Which of the following drugs has been associated with increased risk for myocardial infarction in women? 1. Aspirin 2. Beta blockers 3. Estrogen replacement 4. Lipid-lowering agents ____ 15. Cost of antianginal drug therapy should be considered in drug selection because of all of the following EXCEPT: 1. Patients often require multiple drugs 2. A large number of angina patients are older adults on fixed incomes 3. Generic formulations may be cheaper but are rarely bioequivalent 4. Lack of drug selectivity may result in increased adverse reactions ____ 16. Situations that suggest referral to a specialist is appropriate include: 1. When chronic stable angina becomes unpredictable in its characteristics and precipitating factors 2. When a post-myocardial infarction patient develops new-onset angina 3. When standard therapy is not successful in improving exercise tolerance or reducing the incidence of angina 4. All of the above ____ 17. The rationale for prescribing calcium blockers for angina can be based on the need for: 1. Increased inotropic effect in the heart 2. Increasing peripheral perfusion 3. Keeping heart rates high enough to ensure perfusion of coronary arteries 4. Help with rate control ____ 18. Medications are typically started for angina patients when: 1. The first permanent EKG changes occur 2. The start of class I or II symptoms 3. The events trigger a trip to the emergency department 4. When troponin levels become altered ____ 19. The most common cause of angina is: 1. Vasospasm of the coronary arteries 2. Atherosclerosis 3. Platelet aggregation 4. Low systemic oxygen ____ 20. Ranolazine is used in angina patients to: 1. Dilate plaque-filled arteries 2. Inhibit platelet aggregation 3. Restrict late sodium flow in the myocytes 4. Induce vasoconstriction in the periphery to open coronary vessels ____ 21. When is aspirin (ASA) used in angina patients? 1. All angina patients should be taking ASA unless it is contraindicated for allergy or other medical reasons. 2. ASA should only be used in men. 3. ASA has no role in angina, but is useful in MI prevention. 4. The impact of ASA is best at the time of an angina attack. Chapter 29. Anxiety and Depression Multiple Choice Identify the choice that best completes the statement or answers the question. ____ 1. Common mistakes practitioners make in treating anxiety disorders include: 1. Switching medications after an 8- to 12-week trial 2. Maximizing dosing of antianxiety medications 3. Encouraging exercise and relaxation therapy before starting medication 4. Thinking a partial response to medication is acceptable ____ 2. An appropriate first-line drug to try for mild to moderate generalized anxiety disorder would be: 1. Alprazolam (Xanax) 2. Diazepam (Valium) 3. Buspirone (Buspar) 4. Amitriptyline (Elavil) ____ 3. An appropriate drug to initially treat panic disorder is: 1. Alprazolam (Xanax) 2. Diazepam (Valium) 3. Buspirone (Buspar) 4. Amitriptyline (Elavil) ____ 4. Prior to starting antidepressants, patients should have laboratory testing to rule out: 1. Hypothyroidism 2. Anemia 3. Diabetes mellitus 4. Low estrogen levels ____ 5. David is a 34-year-old patient who is starting on paroxetine (Paxil) for depression. David’s education regarding his medication would include: 1. Paroxetine may cause intermittent diarrhea. 2. He may experience sexual dysfunction beginning a month after he starts therapy. 3. He may have constipation and he should increase fluids and fiber. 4. Paroxetine has a long half-life so he may occasionally skip a dose. ____ 6. Jamison has been prescribed citalopram (Celexa) to treat his depression. Education regarding how quickly selective serotonin reuptake inhibitor (SSRI) antidepressants work would be: 1. Appetite and concentration improve in the first 1 to 2 weeks. 2. Sleep should improve almost immediately upon starting citalopram. 3. Full response to the SSRI may take 2 to 4 months after he reaches the full therapeutic dose. 4. His dysphoric mood will improve in 1 to 2 weeks. ____ 7. An appropriate drug for the treatment of depression with anxiety would be: 1. Alprazolam (Xanax) 2. Escitalopram (Lexapro) 3. Buspirone (Buspar) 4. Amitriptyline (Elavil) ____ 8. An appropriate first-line drug for the treatment of depression with fatigue and low energy would be: 1. Venlafaxine (Effexor) 2. Escitalopram (Lexapro) 3. Buspirone (Buspar) 4. Amitriptyline (Elavil) ____ 9. The laboratory monitoring required when a patient is on a selective serotonin reuptake inhibitor is: 1. Complete blood count every 3 to 4 months 2. Therapeutic blood levels every 6 months after a steady state is achieved 3. Blood glucose every 3 to 4 months 4. There is no laboratory monitoring required ____ 10. Jaycee has been on escitalopram (Lexapro) for a year and is willing to try tapering off of the selective serotonin reuptake inhibitor. What is the initial dosage adjustment when starting a taper off antidepressants? 1. Change dose to every other day dosing for a week 2. Reduce dose by 50% for 3 to 4 days 3. Reduce dose by 50% every other day 4. Escitalopram (Lexapro) can be stopped abruptly due to its long half-life ____ 11. The longer-term Xanax patient comes in and states they need a higher dose of the medication. They deny any additional, new, or accelerating triggers of their anxiety. What is the probable reason? 1. They have become tolerant of the medication, which is characterized by the need for higher and higher doses. 2. They are a drug seeker. 3. They are suicidal. 4. They only need additional counseling on lifestyle modification. ____ 12. What “onset of action” symptoms should be reviewed with patients who have been newly prescribed a selective serotonin reuptake inhibitor? 1. They will have insomnia for a week. 2. They can feel a bit of nausea, but this resolves in a week. 3. They will have an “onset seizure” but this is considered normal. 4. They will no longer dream. ____ 13. Which of the following should not be taken with a selective serotonin reuptake inhibitor? 1. Aged blue cheese 2. Grapefruit 3. Alcohol 4. Green leafy vegetables ____ 14. Why is the consistency of taking paroxetine (Paxil) and never running out of medication more important than with most other selective serotonin reuptake inhibitors (SSRIs)? 1. It has a shorter half-life and withdrawal syndrome has a faster onset without taper. 2. It has the longest half-life and the withdrawal syndrome has a faster onset. 3. It is quasi-addictive in the dopaminergic reward system. 4. It is the most activating of SSRI medications and will cause the person to have sudden deep sadness. ____ 15. The patient shares with the provider that he is taking his Prozac at night before going to bed. What is the best response? 1. This is a good idea because this class of medications generally makes people sleepy. 2. Have you noticed that you are having more sleep issues since you started that? 3. This a good way to remember to take your daily medications because it is near your toothbrush. 4. This is a good plan because you can eat grapefruit if there is 8–12 hours difference in the time each are ingested. Chapter 30. Asthma and Chronic Obstructive Pulmonary Disease Multiple Choice Identify the choice that best completes the statement or answers the question. ____ 1. Prior to developing a plan for the treatment of asthma, the patient’s asthma should be classified according to the NHLBI Expert Panel 3 guidelines. In adults mild-persistent asthma is classified as asthma symptoms that occur: 1. Daily 2. Daily and limit physical activity 3. Less than twice a week 4. More than twice a week and less than once a day ____ 2. In children age 5 to 11 years mild-persistent asthma is diagnosed when asthma symptoms occur: 1. At nighttime one to two times a month 2. At nighttime three to four times a month 3. Less than twice a week 4. Daily ____ 3. One goal of asthma therapy outlined by the NHLBI Expert Panel 3 guidelines is: 1. Ability to use albuterol daily to control symptoms 2. Minimize exacerbations to once a month 3. Keep nighttime symptoms at a maximum of twice a week 4. Require infrequent use of beta 2 agonists (albuterol) for relief of symptoms ____ 4. A stepwise approach to the pharmacologic management of asthma: 1. Begins with determining the severity of asthma and assessing asthma control 2. Is used when asthma is severe and requires daily steroids 3. Allows for each provider to determine their personal approach to the care of asthmatic patients 4. Provides a framework for the management of severe asthmatics, but is not as helpful when patients have intermittent asthma ____ 5. Treatment for mild intermittent asthma is: 1. Daily inhaled medium-dose corticosteroids 2. Short-acting beta-2-agonists (albuterol) as needed 3. Long-acting beta-2-agonists every morning as a preventative 4. Montelukast (Singulair) daily ____ 6. The first-line therapy for mild-persistent asthma is: 1. High-dose montelukast 2. Theophylline 3. Low-dose inhaled corticosteroids 4. Long-acting beta-2-agonists ____ 7. Monitoring a patient with persistent asthma includes: 1. Monitoring how frequently the patient has an upper respiratory infection (URI) during treatment 2. Monthly in-office spirometry testing 3. Determining if the patient has increased use of his or her long-acting beta-2-agonist due to exacerbations 4. Evaluating the patient every 1 to 6 months to determine if the patient needs to step up or down in their therapy ____ 8. Asthma exacerbations at home are managed by the patient by: 1. Increasing frequency of beta-2-agonists and contacting their provider 2. Doubling inhaled corticosteroid doses 3. Increasing frequency of beta-2-agonists 4. Starting montelukast (Singulair) ____ 9. Patients who are at risk of a fatal asthma attack include patients: 1. With moderate persistent asthma 2. With a history of requiring intubation or ICU admission for asthma 3. Who are on daily inhaled corticosteroid therapy 4. Who are pregnant ____ 10. Pregnant patients with asthma may safely use ________ throughout their pregnancy. 1. Oral terbutaline 2. Prednisone 3. Inhaled corticosteroids (budesonide) 4. Montelukast (Singulair) ____ 11. One goal of asthma management in children is: 1. They independently manage their asthma 2. Participation in school and sports activities 3. No exacerbations 4. Minimal use of inhaled corticosteroids ____ 12. Medications used in the management of patients with chronic obstructive pulmonary disease (COPD) include: 1. Inhaled beta-2-agonists 2. Inhaled anticholinergics (ipratropium) 3. Inhaled corticosteroids 4. All of the above ____ 13. Patients with a COPD exacerbation may require: 1. Doubling of inhaled corticosteroid dose 2. Systemic corticosteroid burst 3. Continuous inhaled beta-2-agonists 4. Leukotriene therapy ____ 14. Patients with COPD require monitoring of: 1. Beta-2-agonist use 2. Serum electrolytes 3. Blood pressure 4. Neuropsychiatric effects of montelukast ____ 15. Education of patients with COPD who use inhaled corticosteroids includes: 1. Doubling the dose at the first sign of a URI 2. Using their inhaled corticosteroid first and then their bronchodilator 3. Rinsing their mouth after use 4. Abstaining from smoking for at least 30 minutes after using ____ 16. Education for patients who use an inhaled beta-agonist and an inhaled corticosteroid includes: 1. Use the inhaled corticosteroid first, followed by the inhaled beta-agonists. 2. Use the inhaled beta-agonist first, followed by the inhaled corticosteroid. 3. Increase fluid intake to 3 liters per day. 4. Avoid use of aspirin or ibuprofen while using inhaled medications. Chapter 31. Contraception Multiple Choice Identify the choice that best completes the statement or answers the question. ____ 1. Women who are taking an oral contraceptive containing the progesterone drospirenone may require monitoring of: 1. Hemoglobin 2. Serum calcium 3. White blood count 4. Serum potassium ____ 2. The mechanism of action of oral combined contraceptives that prevents pregnancy is: 1. Estrogen prevents the luteinizing hormone surge necessary for ovulation. 2. Progestins thicken cervical mucus and slow tubal motility. 3. Estrogen thins the endometrium making implantation difficult. 4. Progestin suppresses follicle stimulating hormone release. ____ 3. To improve actual effectiveness of oral contraceptives women should be educated regarding: 1. Use of a back-up method if they have vomiting or diarrhea during a pill packet 2. Doubling pills if they have diarrhea during the middle of a pill pack 3. The fact that they will have a normal menstrual cycle if they miss two pills 4. The fact that mid-cycle spotting is not normal and the provider should be contacted immediately ____ 4. A contraindication to the use of combined contraceptives is: 1. Adolescence (not approved for this age) 2. A history of clotting disorder 3. Recent pregnancy 4. Being overweight ____ 5. Obese women may have increased risk of failure with which contraceptive method? 1. Combined oral contraceptives 2. Progestin-only oral contraceptive pill 3. Injectable progestin 4. Combined topical patch ____ 6. Ashley comes to the clinic with a request for oral contraceptives. She has successfully used oral contraceptives before and has recently started dating a new boyfriend so would like to restart contraception. She denies recent intercourse and has a negative urine pregnancy test in the clinic. An appropriate plan of care would be: 1. Recommend she return to the clinic at the start of her next menses to get a Depo Provera shot. 2. Prescribe oral combined contraceptives and recommend she start them at the beginning of her next period and use a back-up method for the first 7 days. 3. Prescribe oral contraceptives and have her start them the same day as the visit with a back-up method used for the first 7 days. 4. Discuss the advantages of using the topical birth control patch and recommend she consider using the patch. ____ 7. When discussing with a patient the different start methods used for oral combined contraceptives, the advantage of a Sunday start over the other start methods is: 1. Immediate protection against pregnancy the first week of using the pill 2. No back-up method is needed when starting 3. Menses occur during the week 4. They can start the pill on the Sunday after the office visit ____ 8. The topical patch combined contraceptive (Ortho Evra) is: 1. Started on the first day of the menstrual cycle 2. Recommended for women over 200 pounds 3. Not as effective as oral combined contraceptives 4. Known to have more adverse effects, such as nausea, than the oral combined contraceptives ____ 9. Progesterone-only pills are recommended for women who: 1. Are breastfeeding 2. Have a history of migraine 3. Have a medical history that contradicts the use of estrogen 4. All of the above ____ 10. Women who are prescribed progestin-only contraception need education regarding which common adverse drug effects? 1. Increased migraine headaches 2. Increased risk of developing blood clots 3. Irregular vaginal bleeding for the first few months 4. Increased risk for hypercalcemia ____ 11. An advantage of using the NuvaRing vaginal ring for contraception is: 1. It does not require fitting and is easy to insert. 2. It is inserted once a week, eliminating the need to remember to take a daily pill. 3. Patients get a level of estrogen and progestin equal to combined oral contraceptives. 4. It also provides protection against vaginal infections. ____ 12. Oral emergency contraception (Plan B) is contraindicated in women who: 1. Had intercourse within the past 72 hours 2. May be pregnant 3. Are taking combined oral contraceptives 4. Are using a diaphragm Chapter 32. Dermatologic Conditions Multiple Choice Identify the choice that best completes the statement or answers the question. ____ 1. When choosing a topical corticosteroid cream to treat diaper dermatitis, the ideal medication would be: 1. Intermediate potency corticosteroid ointment (Kenalog) 2. A combination of a corticosteroid and an antifungal (Lotrisone) 3. A low-potency corticosteroid cream applied sparingly (hydrocortisone 1%) 4. A high-potency corticosteroid cream (Diprolene AF) ____ 2. Topical immunomodulators such as pimecrolimus (Elidel) or tacrolimus (Protopic) are used for: 1. Short-term or intermittent treatment of atopic dermatitis 2. Topical treatment of fungal infections (Candida) 3. Chronic, inflammatory seborrheic dermatitis 4. Recalcitrant nodular acne ____ 3. Long-term treatment of moderate atopic dermatitis includes: 1. Topical corticosteroids and emollients 2. Topical corticosteroids alone 3. Topical antipruritics 4. Oral corticosteroids for exacerbations of atopic dermatitis ____ 4. Severe contact dermatitis caused by poison ivy or poison oak exposure often requires treatment with: 1. Topical antipruritics 2. Oral corticosteroids for 2 to 3 weeks 3. Thickly applied topical intermediate-dose corticosteroids 4. Isolation of the patient to prevent spread of the dermatitis ____ 5. When a patient has contact dermatitis, wet dressings with Domeboro solution are used for: 1. Cleaning the weeping area of dermatitis 2. Bathing the patient to prevent infection 3. Relief of inflammation 4. Providing a barrier layer to protect the surrounding skin ____ 6. Appropriate initial treatment for psoriasis would be: 1. An immunomodulator (Protopic or Elidel) 2. Wet soaks with Burrow’s or Domeboro solution 3. Intermittent therapy with intermediate potency topical corticosteroids 4. Anthralin (Drithocreme) ____ 7. Patient education when prescribing the vitamin D3 derivative calcipotriene for psoriasis includes: 1. Apply thickly to affected psoriatic areas two to three times a day. 2. A maximum of 100 grams per week may be applied. 3. Do not use calcipotriene in combination with their topical corticosteroids. 4. Calcipotriene may be augmented with the use of coal tar products. ____ 8. Mild acne may be initially treated with: 1. Topical combined antibiotic 2. Minocycline 3. Topical retinoid 4. OTC benzoyl peroxide ____ 9. Tobie presents to the clinic with moderate acne. He has been using OTC benzoyl peroxide at home with minimal improvement. A topical antibiotic (clindamycin) and a topical retinoid adapalene (Differin) are prescribed. Education of Tobie would include: 1. He should see an improvement in his acne within the first 2 weeks of treatment. 2. If there is no response in a week, double the daily application of adapalene (Differin). 3. He may see an initial worsening of his acne that will improve in 6 to 8 weeks. 4. Adapalene may cause bleaching of clothing. ____ 10. Josie has severe cystic acne and is requesting treatment with Accutane. The appropriate treatment for her would be: 1. Order a pregnancy test and if it is negative prescribe the isotretinoin (Accutane). 2. Order Accutane after educating her on the adverse effects. 3. Recommend she try oral antibiotics (minocycline). 4. Refer her to a dermatologist for treatment. ____ 11. The most cost-effective treatment for two or three impetigo lesions on the face is: 1. Mupirocin ointment 2. Retapamulin (Altabax) ointment 3. Topical clindamycin solution 4. Oral amoxicillin/clavulanate (Augmentin) ____ 12. Dwayne has classic tinea capitis. Treatment for tinea on the scalp is: 1. Miconazole cream rubbed in well for 4 weeks 2. Oral griseofulvin for 6 to 8 weeks 3. Ketoconazole shampoo daily for 6 weeks 4. Ciclopirox cream daily for 4 weeks ____ 13. Nicolas is a football player who presents to the clinic with athlete’s foot. Patients with tinea pedis may be treated with: 1. OTC miconazole cream for 4 weeks 2. Oral ketoconazole for 6 weeks 3. Mupirocin ointment for 2 weeks 4. Nystatin cream for 2 weeks ____ 14. Jim presents with fungal infection of two of his toenails (onychomycosis). Treatment for fungal infections of the nail includes: 1. Miconazole cream 2. Ketoconazole cream 3. Oral griseofulvin 4. Mupirocin cream ____ 15. Scabies treatment for a 4-year-old child includes a prescription for: 1. Permethrin 5% cream applied from the neck down 2. Pyrethrin lotion 3. Lindane 1% shampoo 4. All of the above ____ 16. Vanessa has been diagnosed with scabies. Her education would include: 1. She should apply the scabies treatment cream for an hour and wash it off. 2. Scabies may need to be retreated in a week after initial treatment. 3. All members of the household and close personal contacts should be treated. 4. Malathion is flammable and she should take care until the solution dries. ____ 17. Catherine has head lice and her mother is asking about what products are available that are not neurotoxic. The only non-neurotoxin head lice treatment is: 1. Permethrin 1% (Nix) 2. Lindane shampoo 3. Malathion (Ovide) 4. Benzoyl alcohol (Ulesfia) ____ 18. Rick has male pattern baldness on the vertex of his head and has been using Rogaine for 2 months. He asks how effective minoxidil (Rogaine) is. Minoxidil: 1. Provides a permanent solution to male pattern baldness if used for at least 4 months 2. Will show results after 4 months of twice-a-day use 3. May not work for Rick’s type of baldness 4. Works better if he also uses hydrocortisone cream daily on his scalp Chapter 33. Diabetes Mellitus Multiple Choice Identify the choice that best completes the statement or answers the question. ____ 1. Type 1 diabetes results from autoimmune destruction of the beta cells. Eighty-five to 90% of type 1 diabetics have: 1. Autoantibodies to two tyrosine phosphatases 2. Mutation of the hepatic transcription factor on chromosome 12 3. A defective glucokinase molecule due to a defective gene on chromosome 7p 4. Mutation of the insulin promoter factor ____ 2. Type 2 diabetes is a complex disorder involving: 1. Absence of insulin production by the beta cells 2. A suboptimal response of insulin-sensitive tissues in the liver 3. Increased levels of glucagon-like peptide in the postprandial period 4. Too much fat uptake in the intestine ____ 3. Diagnostic criteria for diabetes include: 1. Fasting blood glucose greater than 140 mg/dl on two occasions 2. Postprandial blood glucose greater than 140 mg/dl 3. Fasting blood glucose 100 to 125 mg/dl on two occasions 4. Symptoms of diabetes plus a casual blood glucose greater than 200 mg/dl ____ 4. Routine screening of asymptomatic adults for diabetes is appropriate for: 1. Individuals who are older than 45 and have a BMI of less than 25 kg/m2 2. Native Americans, African Americans, and Hispanics 3. Persons with HDL cholesterol greater than 100 mg/dl 4. Persons with prediabetes confirmed on at least two occasions ____ 5. Screening for children who meet the following criteria should begin at age 10 and occur every 3 years thereafter: 1. BMI above the 85th percentile for age and sex 2. Family history of diabetes in first- or second-degree relative 3. Hypertension based on criteria for children 4. Any of the above ____ 6. Insulin is used to treat both types of diabetes. It acts by: 1. Increasing beta cell response to low blood-glucose levels 2. Stimulating hepatic glucose production 3. Increasing peripheral glucose uptake by skeletal muscle and fat 4. Improving the circulation of free fatty acids ____ 7. Adam has type 1 diabetes and plays tennis for his university. He exhibits a knowledge deficit about his insulin and his diagnosis. He should be taught that: 1. He should increase his carbohydrate intake during times of exercise. 2. Each brand of insulin is equal in bioavailability, so buy the least expensive. 3. Alcohol produces hypoglycemia and can help control his diabetes when taken in small amounts. 4. If he does not want to learn to give himself injections, he may substitute an oral hypoglycemic to control his diabetes. ____ 8. Insulin preparations are divided into categories based on onset, duration, and intensity of action following subcutaneous injection. Which of the following insulin preparations has the shortest onset and duration of action? 1. Lispro 2. Glulisine 3. Glargine 4. Detemir ____ 9. The drug of choice for type 2 diabetics is metformin. Metformin: 1. Decreases glycogenolysis by the liver 2. Increases the release of insulin from beta cells 3. Increases intestinal uptake of glucose 4. Prevents weight gain associated with hyperglycemia ____ 10. Before prescribing metformin, the provider should: 1. Draw a serum creatinine level to assess renal function. 2. Try the patient on insulin. 3. Prescribe a thyroid preparation if the patient needs to lose weight. 4. All of the above ____ 11. Sulfonylureas may be added to a treatment regimen for type 2 diabetics when lifestyle modifications and metformin are insufficient to achieve target glucose levels. Sulfonylureas have been moved to Step 2 therapy because they: 1. Increase endogenous insulin secretion 2. Have a significant risk for hypoglycemia 3. Address the insulin resistance found in type 2 diabetics 4. Improve insulin binding to receptors ____ 12. Dipeptidyl peptidase-4 inhibitors (gliptins) act on the incretin system to improve glycemic control. Advantages of these drugs include: 1. Better reduction in glucose levels than other classes 2. Less weight gain than sulfonylureas 3. Low risk for hypoglycemia 4. Can be given twice daily ____ 13. Control targets for patients with diabetes include: 1. HbA1C between 7 and 8 2. Fasting blood glucose levels between 100 and 120 mg/dl 3. Blood pressure less than 130/80 mm Hg 4. LDL lipids less than 130 mg/dl ____ 14. Establishing glycemic targets is the first step in treatment of both types of diabetes. For type 1 diabetes: 1. Tight control/intensive therapy can be given to adults who are willing to test their blood glucose at least twice daily. 2. Tight control is acceptable for older adults if they are without complications. 3. Plasma glucose levels are the same for children as adults. 4. Conventional therapy has a fasting plasma glucose target between 120 and 150 mg/dl. ____ 15. Treatment with insulin for type 1 diabetics: 1. Starts with a total daily dose of 0.2 to 0.4 units per kg of body weight 2. Divides the total doses into three injections based on meal size 3. Uses a total daily dose of insulin glargine given once daily with no other insulin required 4. Is based on the level of blood glucose ____ 16. When the total daily insulin dose is split and given twice daily, which of the following rules may be followed? 1. Give two-thirds of the total dose in the morning and one-third in the evening. 2. Give 0.3 units per kg of premixed 70/30 insulin with one-third in the morning and two-thirds in the evening. 3. Give 50% of an insulin glargine dose in the morning and 50% in the evening. 4. Give long-acting insulin in the morning and short-acting insulin at bedtime. ____ 17. Studies have shown that control targets that reduce the HbA1C to less than 7% are associated with fewer long-term complications of diabetes. Patients who should have such a target include: 1. Those with long-standing diabetes 2. Older adults 3. Those with no significant cardiovascular disease 4. Young children who are early in their disease ____ 18. Prevention of conversion from prediabetes to diabetes in young children must take highest priority and should focus on: 1. Aggressive dietary manipulation to prevent obesity 2. Fostering LDL levels less than 100 mg/dl and total cholesterol less than 170 mg/dl to prevent cardiovascular disease 3. Maintaining a blood pressure that is less than 80% based on weight and height to prevent hypertension 4. All of the above ____ 19. The drugs recommended by the American Academy of Pediatrics for use in children with diabetes (depending upon type of diabetes) are: 1. Metformin and insulin 2. Sulfonylureas and insulin glargine 3. Split-mixed dose insulin and GPL-1 agonists 4. Biguanides and insulin lispro ____ 20. Unlike most type 2 diabetics where obesity is a major issue, older adults with low body weight have higher risks for morbidity and mortality. The most reliable indicator of poor nutritional status in older adults is: 1. Weight loss in previously overweight persons 2. Involuntary loss of 10% of body weight in less than 6 months 3. Decline in lean body mass over a 12-month period 4. Increase in central versus peripheral body adiposity ____ 21. The drugs recommended for older adults with type 2 diabetes include: 1. Second-generation sulfonylureas 2. Metformin 3. Pioglitazone 4. Third-generation sulfonylureas ____ 22. Ethnic groups differ in their risk for and presentation of diabetes. Hispanics: 1. Have a high incidence of obesity, elevated triglycerides, and hypertension 2. Do best with drugs that foster weight loss, such as metformin 3. Both 1 and 2 4. Neither 1 nor 2 ____ 23. The American Heart Association states that people with diabetes have a 2- to 4-fold increase in the risk of dying from cardiovascular disease. Treatments and targets that do not appear to decrease risk for micro- and macro-vascular complications include: 1. Glycemic targets between 7% and 7.5% 2. Use of insulin in type 2 diabetics 3. Control of hypertension and hyperlipidemia 4. Stopping smoking ____ 24. All diabetic patients with known cardiovascular disease should be treated with: 1. Beta blockers to prevent MIs 2. Angiotensin-converting enzyme inhibitors and aspirin to reduce risk of cardiovascular events 3. Sulfonylureas to decrease cardiovascular mortality 4. Pioglitazone to decrease atherosclerotic plaque buildup ____ 25. All diabetic patients with hyperlipidemia should be treated with: 1. HMG-CoA reductase inhibitors 2. Fibric acid derivatives 3. Nicotinic acid 4. Colestipol ____ 26. Both angiotensin converting enzyme inhibitors and some angiotensin II receptor blockers have been approved in treating: 1. Hypertension in diabetic patients 2. Diabetic nephropathy 3. Both 1 and 2 4. Neither 1 nor 2 ____ 27. Protein restriction helps slow the progression of albuminuria, glomerular filtration rate, decline, and end stage renal disease in some patients with diabetes. It is useful for patients who: 1. Cannot tolerate angiotensin converting enzyme inhibitors or angiotensin receptor blockers 2. Have uncontrolled hypertension 3. Have HbA1C levels above 7% 4. Show progression of diabetic nephropathy despite optimal glucose and blood pressure control ____ 28. Diabetic autonomic neuropathy (DAN) is the earliest and most common complication of diabetes. Symptoms associated with DAN include: 1. Resting tachycardia, exercise intolerance, and orthostatic hypotension 2. Gastroparesis, cold intolerance, and moist skin 3. Hyperglycemia, erectile dysfunction, and deficiency of free fatty acids 4. Pain, loss of sensation, and muscle weakness ____ 29. Drugs used to treat diabetic peripheral neuropathy include: 1. Metoclopramide 2. Cholinergic agonists 3. Cardioselective beta blockers 4. Gabapentin ____ 30. The American Diabetic Association has recommended which of the following tests for ongoing management of diabetes? 1. Fasting blood glucose 2. HbA1C 3. Thyroid function tests 4. Electrocardiograms ____ 31. Allison is an 18-year-old college student with type 1 diabetes. She is on NPH twice daily and Novolog before meals. She usually walks for 40 minutes each evening as part of her exercise regimen. She is beginning a 30-minute swimming class three times a week at 1 p.m. What is important for her to do with this change in routine? 1. Delay eating the midday meal until after the swimming class. 2. Increase the morning dose of NPH insulin on days of the swimming class. 3. Adjust the morning insulin injection so that the peak occurs while swimming. 4. Check glucose level before, during, and after swimming. ____ 32. Allison is an 18-year-old college student with type 1 diabetes. Allison’s pre-meal BG at 11:30 a.m. is 130. She eats an apple and has a sugar-free soft drink. At 1 p.m. before swimming her BG is 80. What should she do? 1. Proceed with the swimming class. 2. Recheck her BG immediately. 3. Eat a granola bar or other snack with CHO. 4. Take an additional dose of insulin. ____ 33. Bart is a patient is a 67-year-old male with T2 DM. He is on glipizide and metformin. He presents to the clinic with confusion, sluggishness, and extreme thirst. His wife tells you Bart does not follow his meal plan or exercise regularly, and hasn’t checked his BG for 1 week. A random glucose is drawn and it is 500. What is a likely diagnosis based on preliminary assessment? 1. Diabetic keto acidosis (DKA) 2. Hyperglycemic hyperosmolar syndrome (HHS) 3. Infection 4. Hypoglycemia ____ 34. What would one expected assessment finding be for hyperglycemic hyperosmolar syndrome? 1. Low hemoglobin 2. Ketones in the urine 3. Deep, labored breathing 4. pH of 7.35 ____ 35. A patient on metformin and glipizide arrives at her 11:30 a.m. clinic appointment diaphoretic and dizzy. She reports taking her medication this morning and ate a bagel and coffee for breakfast. BP is 110/70 and random finger-stick glucose is 64. How should this patient be treated? 1. 12 oz apple juice with 1 tsp sugar 2. 10 oz diet soda 3. 8 oz milk or 4 oz orange juice 4. 4 cookies and 8 oz chocolate milk Chapter 34. Gastroesophageal Reflux and Peptic Ulcer Disease Multiple Choice Identify the choice that best completes the statement or answers the question. ____ 1. Gastroesophageal reflux disease may be aggravated by the following medication that affects lower esophageal sphincter (LES) tone: 1. Calcium carbonate 2. Estrogen 3. Furosemide 4. Metoclopramide ____ 2. Lifestyle changes are the first step in treatment of gastroesophageal reflux disease (GERD). Food or drink that may aggravate GERD include: 1. Eggs 2. Caffeine 3. Chocolate 4. Soda pop ____ 3. Metoclopramide improves gastroesophageal reflux disease symptoms by: 1. Reducing acid secretion 2. Increasing gastric pH 3. Increasing lower esophageal tone 4. Decreasing lower esophageal tone ____ 4. Antacids treat gastroesophageal reflux disease by: 1. Increasing lower esophageal tone 2. Increasing gastric pH 3. Inhibiting gastric acid secretion 4. Increasing serum calcium level ____ 5. When treating patients using the “Step-Down” approach the patient with gastroesophageal reflux disease is started on _______ first. 1. Antacids 2. Histamine2 receptor antagonists 3. Prokinetics 4. Proton pump inhibitors ____ 6. If a patient with symptoms of gastroesophageal reflux disease states that he has been self-treating at home with OTC ranitidine daily, the appropriate treatment would be: 1. Prokinetic (metoclopramide) for 4 to 8 weeks 2. Proton pump inhibitor (omeprazole) for 12 weeks 3. Histamine2 receptor antagonist (ranitidine) for 4 to 8 weeks 4. Cytoprotective drug (misoprostol) for 2 weeks ____ 7. If a patient with gastroesophageal reflux disease who is taking a proton pump inhibitor daily is not improving, the plan of care would be: 1. Prokinetic (metoclopramide) for 8 to 12 weeks 2. Proton pump inhibitor (omeprazole) twice a day for 4 to 8 weeks 3. Histamine2 receptor antagonist (ranitidine) for 4 to 8 weeks 4. Cytoprotective drug (misoprostol) for 4 to 8 weeks ____ 8. The next step in treatment when a patient has been on proton pump inhibitors twice daily for 12 weeks and not improving is: 1. Add a prokinetic (metoclopramide) 2. Referral for endoscopy 3. Switch to another proton pump inhibitor 4. Add a cytoprotective drug ____ 9. Infants with reflux are initially treated with: 1. Histamine2 receptor antagonist (ranitidine) 2. Proton pump inhibitor (omeprazole) 3. Anti-reflux maneuvers (elevate head of bed) 4. Prokinetic (metoclopramide) ____ 10. Long-term use of proton pump inhibitors may lead to: 1. Hip fractures in at-risk persons 2. Vitamin B6 deficiency 3. Liver cancer 4. All of the above ____ 11. An acceptable first-line treatment for peptic ulcer disease with positive H. pylori test is: 1. Histamine2 receptor antagonists for 4 to 8 weeks 2. Proton pump inhibitor bid for 12 weeks until healing is complete 3. Proton pump inhibitor bid plus clarithromycin plus amoxicillin for 14 days 4. Proton pump inhibitor bid and levofloxacin for 14 days ____ 12. Treatment failure in patients with peptic ulcer disease associated with H. pylori may be because of: 1. Antimicrobial resistance 2. An ineffective antacid 3. Overuse of proton pump inhibitors 4. All of the above ____ 13. If a patient with H. pylori-positive peptic ulcer disease fails first-line therapy, the second-line treatment is: 1. Proton pump inhibitor bid plus metronidazole plus tetracycline plus bismuth subsalicylate for 14 days 2. Test H. pylori for resistance to common treatment regimens 3. Proton pump inhibitor plus clarithromycin plus amoxicillin for 14 days 4. Proton pump inhibitor and levofloxacin for 14 days ____ 14. After H. pylori treatment is completed, the next step in peptic ulcer disease therapy is: 1. Testing for H. pylori eradication with a serum ELISA test 2. Endoscopy by a specialist 3. A proton pump inhibitor for 8 to 12 weeks until healing is complete 4. All of the above Chapter 35. Headaches Multiple Choice Identify the choice that best completes the statement or answers the question. ____ 1. Paige has a history of chronic migraines and would benefit from preventative medication. Education regarding migraine preventive medication includes: 1. Medication is taken at the beginning of the headache to prevent it from getting worse. 2. Medication alone is the best preventative against migraines occurring. 3. Medication should not be used more than four times a month. 4. The goal of treatment is to reduce migraine occurrence by 50%. ____ 2. A first-line drug for abortive therapy in simple migraine is: 1. Sumatriptan (Imitrex) 2. Naproxen (Aleve) 3. Butorphanol nasal spray (Stadol NS) 4. Butalbital and acetaminophen (Fioricet) ____ 3. Vicky, age 56 years, comes to the clinic requesting a refill of her Fiorinal (aspirin and butalbital) that she takes for migraines. She has been taking this medication for over 2 years for migraines and states one dose usually works to abort her migraine. What is the best care for her? 1. Switch her to sumatriptan (Imitrex) to treat her migraines. 2. Assess how often she is using Fiorinal and refill her medication. 3. Switch her to a beta blocker such as propranolol to prevent her migraine. 4. Request she return to the original prescriber of Fiorinal as you do not prescribe butalbital for migraines. ____ 4. When prescribing ergotamine suppositories (Wigraine) to treat acute migraine, patient education would include: 1. Ergotamine will briefly make the migraine worse before the migraine resolves. 2. The patient may experience bradycardia and dizziness. 3. They may need premedication with an antinausea medication. 4. Ergotamine works best if the patient starts off with a full suppository to get the full effect. ____ 5. Migraines in pregnancy may be safely treated with: 1. Acetaminophen with codeine (Tylenol #3) 2. Sumatriptan (Imitrex) 3. Ergotamine tablets (Ergostat) 4. Dihydroergotamine (DHE) ____ 6. Xi, a 54-year-old female, has a history of migraines that do not respond well to OTC migraine medication. She is asking to try Maxalt (rizatriptan) because it works well for her friend. Appropriate decision making would be: 1. Prescribe the Maxalt, but only give her four tablets with no refills to monitor the use. 2. Prescribe Maxalt and arrange to have her observed in the clinic or urgent care with the first dose. 3. Explain that rizatriptan is not used for postmenopausal migraines and recommend Fiorinal (aspirin and butalbital). 4. Prescribe sumatriptan (Imitrex) with the explanation that it is the most effective triptan. ____ 7. Kelly is a 14-year-old patient who presents to the clinic with a classic migraine. She says she is having a headache two to three times a month. The initial plan would be: 1. Prescribe NSAIDs as abortive therapy and have her keep a headache diary to identify her triggers. 2. Prescribe zolmitriptan (Zomig) as abortive therapy and recommend relaxation therapy to reduce her stress. 3. Prescribe acetaminophen with codeine (Tylenol #3) for her to take at the first onset of her migraine. 4. Prescribe sumatriptan (Imitrex) nasal spray and arrange for her to receive the first dose in the clinic. ____ 8. Jayla is a 9-year-old patient who has been diagnosed with migraines for almost 2 years. She is missing up to a week of school each month. Her headache diary confirms she averages four or five migraines per month. Which of the following would be appropriate? 1. Prescribe amitriptyline (Elavil) daily, start at a low dose and increase dosage slowly every 2 weeks until it’s effective in eliminating migraines. 2. Encourage her mother to give her Excedrin Migraine (aspirin, acetaminophen, and caffeine) at the first sign of a headache to abort the headache. 3. Prescribe propranolol (Inderal) to be taken daily for at least 3 months. 4. Explain that it is rare for a 9-year-old child to get migraines and she needs an MRI to rule out a brain tumor. ____ 9. Amber is a 24-year-old patient who has had migraines for 10 years. She reports a migraine on average of once a month. The migraines are effectively aborted with naratriptan (Amerge). When refilling Amber’s naratriptan, education would include: 1. Naratriptan will interact with antidepressants, including selective serotonin reuptake inhibitors (SSRIs) and St John’s wort, and she should inform any providers she sees that she has migraines. 2. Continue to monitor her headaches, if the migraine is consistently happening around her menses there is preventive therapy available. 3. Pregnancy is contraindicated when taking a triptan. 4. All of the above ____ 10. When prescribing for migraines, patient education includes: 1. Triptans are safe to be used as often as needed as long as the patient is healthy. 2. Use triptan before trying OTC meds such as acetaminophen or naproxen. 3. Stress reduction and regular sleep are integral to migraine treatment. 4. If migraines worsen they are to increase their medication. ____ 11. Juanita presents to the clinic with a complaint of headaches off and on for months. She reports they feel like someone is “squeezing” her head. She occasionally takes Tylenol for the pain, but usually just “toughs it out.” Initial treatment for tension headache includes asking her to keep a headache diary and a prescription for: 1. Sumatriptan (Imitrex) 2. Naproxen (Aleve) 3. Ergotamine (Ergostat) 4. Tylenol with codeine (Tylenol #3) ____ 12. Nonpharmacologic therapy for tension headaches includes: 1. Biofeedback 2. Stress management 3. Massage therapy 4. All of the above ____ 13. James has been diagnosed with cluster headaches. Appropriate acute therapy would be: 1. Butalbital and aspirin (Fiorinal) 2. Meperidine IM (Demerol) 3. Oxygen 100% for 15 to 30 minutes 4. Indomethacin (Indocin) ____ 14. Preventative therapy for cluster headaches includes: 1. Massage or relaxation therapy 2. Ergotamine nightly before bed 3. Intranasal lidocaine four times a day during “clusters” of headaches 4. Propranolol (Inderal) daily ____ 15. When prescribing any headache therapy, appropriate use of medications needs to be discussed to prevent medication-overuse headaches. A clinical characteristic of medication-overuse headaches is that they: 1. Are increasing in frequency 2. Are increasing in intensity 3. Recur when medication wears off 4. Begin to “cluster” into a pattern Chapter 36. Heart Failure Multiple Choice Identify the choice that best completes the statement or answers the question. ____ 1. Angiotensin-converting-enzyme (ACE) inhibitors are a central part of the treatment of heart failure because they have more than one action to address the pathological changes in this disorder. Which of the following pathological changes in heart failure is NOT addressed by ACE inhibitors? 1. Changes in the structure of the left ventricle so that it dilates, hypertrophies, and uses energy less efficiently. 2. Reduced formation of cross-bridges so that contractile force decreases. 3. Activation of the sympathetic nervous system that increases heart rate and preload. 4. Decreased renal blood flow that decreases oxygen supply to the kidneys. ____ 2. One of the three types of heart failure involves systolic dysfunction. Potential causes of this most common form of heart failure include: 1. Myocardial ischemia and injury secondary to myocardial infarction 2. Inadequate relaxation and loss of muscle fiber secondary to valvular dysfunction 3. Increased demands of the heart beyond its ability to adapt secondary to anemia 4. Slower filling rate and elevated systolic pressures secondary to uncontrolled hypertension ____ 3. The American Heart Association and the American College of Cardiology have devised a classification system for heart failure that can be used to direct treatment. Patients with symptoms and underlying disease are classified as stage: 1. A 2. B 3. C 4. D ____ 4. Diagnosis of heart failure cannot be made by symptoms alone because many disorders share the same symptoms. The most specific and sensitive diagnostic test for heart failure is: 1. Chest x-rays that show cephalization and measure heart size 2. Two-dimensional echocardiograms that identify structural anomalies and cardiac dysfunction 3. Complete blood count, blood urea nitrogen, and serum electrolytes that facilitate staging for end-organ damage 4. Measurement of brain natriuretic peptide to distinguish between systolic and diastolic dysfunction ____ 5. Treatments for heart failure, including drug therapy, are based on the stages developed by the ACC/AHA. Stage A patients are treated with: 1. Drugs for hypertension and hyperlipidemia, if they exist 2. Lifestyle management including diet, exercise, and smoking cessation only 3. Angiotensin-converting enzyme (ACE) inhibitors to directly affect the heart failure only 4. No drugs are used in this early stage ____ 6. Class I recommendations for stage A heart failure include: 1. Aerobic exercise within tolerance levels to prevent the development of heart failure 2. Reduction of sodium intake to less than 2,000 mg/day to prevent fluid retention 3. Beta blockers for all patients regardless of cardiac history 4. Treatment of thyroid disorders, especially if they are associated with tachyarrhythmias ____ 7. Stage B patients should have beta blockers added to their heart failure treatment regimen when: 1. They have an ejection fraction less than 40% 2. They have had a recent MI 3. Both 1 and 2 4. Neither 1 nor 2 ____ 8. Increased life expectancy for patients with heart failure has been associated with the use of: 1. ACE inhibitors, especially when started early in the disease process 2. All beta blockers regardless of selectivity 3. Thiazide and loop diuretics 4. Cardiac glycosides ____ 9. Stage C patients usually require a combination of three to four drugs to manage their heart failure. In addition to ACE inhibitors and beta blockers, diuretics may be added. Which of the following statements about diuretics is NOT true? 1. Diuretics reduce preload associated with fluid retention. 2. Diuretics can be used earlier than stage C when the goal is control of hypertension. 3. Diuretics may produce problems with electrolyte imbalances and abnormal glucose and lipid metabolism. 4. Diuretics from the potassium-sparing class should be used when using an angiotensin receptor blocker (ARB). ____ 10. Digoxin has a very limited role in treatment of heart failure. It is used mainly for patients with: 1. Ejection fractions above 40% 2. An audible S3 3. Mitral stenosis as a primary cause for heart failure 4. Renal insufficiency ____ 11. Which of the following classes of drugs is contraindicated in heart failure? 1. Nitrates 2. Long-acting dihydropyridines 3. Calcium channel blockers 4. Alpha-beta blockers ____ 12. Heart failure is a leading cause of death and hospitalization in older adults (greater than 65 years old). The drug of choice for this population is: 1. Aldosterone antagonists 2. Eplerenone 3. ACE inhibitors 4. ARBs ____ 13. ACE inhibitors are contraindicated in pregnancy. While treatment of heart failure during pregnancy is best done by a specialist, which of the following drug classes is considered to be safe, at least in the later parts of pregnancy? 1. Diuretics 2. ARBs 3. Beta blockers 4. Nitrates ____ 14. Heart failure is a chronic condition that can be adequately managed in primary care. However, consultation with or referral to a cardiologist is appropriate when: 1. Symptoms markedly worsen or the patient becomes hypotensive and has syncope 2. There is evidence of progressive renal insufficiency or failure 3. The patient remains symptomatic on optimal doses of an ACE inhibitor, a beta blocker, and a diuretic 4. Any of the above ____ 15. ACE inhibitors are a foundational medication in HF. Which group of patients cannot take them safely? 1. Elderly patients with reduced renal clearance 2. Pregnant women 3. Women under age 30 4. 1 and 2 ____ 16. What assessment that can be done at home is the most reliable for making decisions to change HF medications? 1. Weight 2. BP 3. Heart rate 4. Serum Glucose ____ 17. Evidence is strong that the timing of HF interventions are best initiated when: 1. The person enters stage C 2. The person has functional disabilities 3. At the earliest indication 4. When stage IV is determined ____ 18. HF patients frequently take more than one drug. When are anticoagulants typically used? 1. When the patient enters stage III 2. Only in cases of diastolic failure 3. When there is concurrent A Fib 4. In all cases ____ 19. What can chest x-rays contribute to the diagnosis and management of HF? 1. They have no role. 2. They can give very precise pictures of pulmonary fluid status. 3. They provide an idea of general cardiac size and pulmonary great vessel distribution. 4. They can confirm the diagnosis. Chapter 38. Hormone Replacement Therapy and Osteoporosis Multiple Choice Identify the choice that best completes the statement or answers the question. ____ 1. The goals of therapy when prescribing hormone replacement therapy (HRT) include reducing: 1. Cardiovascular risk 2. Risk of stroke or other thromboembolic event 3. Breast cancer 4. Vasomotor symptoms ____ 2. The optimal maximum time frame for HRT or estrogen replacement therapy (ERT) is: 1. 2 years 2. 5 years 3. 10 years 4. 15 years ____ 3. Dosage changes of conjugated equine estrogen (Premarin) are made at _________ intervals. 1. 1 to 2 week 2. 2 to 4 week 3. 6 to 8 week 4. 12 week ____ 4. The advantage of vaginal estrogen preparations in the treatment of vulvovaginal atrophy and dryness is: 1. Ability to deliver higher doses of estrogen in a non-oral form 2. The vaginal cream formula provides moisture to the vaginal area 3. Relief of symptoms without increasing cardiovascular risk 4. All of the above ____ 5. Women with an intact uterus should be treated with both estrogen and progestin due to: 1. Increased risk for endometrial cancer if estrogen alone is used 2. Combination therapy provides the best relief of menopausal vasomotor symptoms 3. Reduced risk for colon cancer with combined therapy 4. Lower risk of developing blood clots with combined therapy ____ 6. Ongoing monitoring for women on ERT includes: 1. Lipid levels, repeated annually if abnormal 2. Annual health history and review of risk profile 3. Annual mammogram 4. All of the above ____ 7. Kristine would like to start HRT to treat the significant vasomotor symptoms she is experiencing during menopause. Education for a woman considering hormone replacement would include: 1. Explaining that HRT is totally safe if used short term 2. Telling her to ignore media hype regarding HRT 3. Discussing the advantages and risks of HRT 4. Encouraging the patient to use phytoestrogens with the HRT ____ 8. Angela is a black woman who has heard that women of African descent do not need to worry about osteoporosis. What education would you provide Angela about her risk? 1. She is correct, black women do not have much risk of developing osteoporosis due to their dark skin. 2. Black women are at risk of developing osteoporosis due to their lower calcium intake as a group. 3. If she doesn’t drink alcohol, her risk of developing osteoporosis is low. 4. If she has not lost more than 10% of her weight lately, her risk is low. ____ 9. Drugs that increase the risk of osteoporosis developing include: 1. Oral combined contraceptives 2. Carbamazepine 3. Calcium channel blockers 4. High doses of vitamin D ____ 10. Selective estrogen receptor modifiers (SERMs) treat osteoporosis by selectively: 1. Inhibiting magnesium resorption in the kidneys 2. Increasing calcium absorption from the GI tract 3. Acting on the bone to inhibit osteoblast activity 4. Selectively acting on the estrogen receptors in the bone ____ 11. Sallie has been diagnosed with osteoporosis and is asking about the “once a month” pill to treat her condition. How do bisphosphonates treat osteoporosis? 1. By selectively activating estrogen pathways in the bone 2. By reducing bone resorption by inhibiting parathyroid hormone (PTH) 3. By reducing bone resorption and inhibiting osteoclastic activity 4. By increasing PTH production ____ 12. Inadequate vitamin D intake can contribute to the development of osteoporosis by: 1. Increasing calcitonin production 2. Increasing calcium absorption from the intestine 3. Altering calcium metabolism 4. Stimulating bone formation ____ 13. The drug recommended as primary prevention of osteoporosis in women over age 70 years is: 1. Alendronate (Fosamax) 2. Ibandronate (Boniva) 3. Calcium carbonate 4. Raloxifene (Evista) ____ 14. The drug recommended as primary prevention of osteoporosis in men over age 70 years is: 1. Alendronate (Fosamax) 2. Ibandronate (Boniva) 3. Calcium carbonate 4. Raloxifene (Evista) ____ 15. The ongoing monitoring for patients over age 65 years taking alendronate (Fosamax) or any other bisphosphonate is: 1. Annual dual-energy x-ray absorptiometry (DEXA) scans 2. Annual vitamin D level 3. Annual renal function evaluation 4. Electrolytes every 3 months ____ 16. Bisphosphonate administration education includes: 1. Taking it on a full stomach 2. Requiring sitting erect for at least 30 minutes afterward 3. Drinking it with orange juice 4. Taking it with H2 blockers or proton pump inhibitors (PPI) to protect the stomach ____ 17. IV forms of bisphosphonates are used for all the following except: 1. Severe gastric irritation with oral forms 2. Known cancer mets into the bone 3. Persons with advancing renal dysfunction 4. Progression of bone loss on oral formulations ____ 18. What is the established frequency of repeating DEXA imaging after stating bisphosphonates? 1. Every 2 years 2. Every 5 years 3. There is no evidence-based time line for monitoring after the first 2 years 4. There need to be annual exams ____ 19. What is the duration of SERM use for menopausal issues? 1. It matches the 5 years for estrogen products 2. The bone health impact allows long-term use 3. The increased risk of breast cancer encourages tapering as soon as possible 4. The abnormal lipid profile contributes to an early termination as soon as hot flashes no longer occur ____ 20. Why are SERMS generally not ordered for women early into menopause? 1. The rapid onset of severe hot flashes can be unbearable. 2. The bone remodeling effect results in osteoporosis. 3. They tend to induce intermittent spotting. 4. They create more risk with breast cancer than they are worth. Chapter 39. Hyperlipidemia Multiple Choice Identify the choice that best completes the statement or answers the question. ____ 1. The overall goal of treating hyperlipidemia is: 1. Maintain an LDL level of less than 160 mg/dL 2. To reduce atherogenesis 3. Lowering apo B, one of the apoliproteins 4. All of the above ____ 2. When considering which cholesterol-lowering drug to prescribe, which factor determines the type and intensity of treatment? 1. Total LDL 2. Fasting HDL 3. Coronary artery disease risk level 4. Fasting total cholesterol ____ 3. First-line therapy for hyperlipidemia is: 1. Statins 2. Niacin 3. Lifestyle changes 4. Bile acid-binding resins ____ 4. James is a 45-year-old patient with an LDL level of 120 and normal triglycerides. Appropriate first-line therapy for James may include diet counseling, increased physical activity, and: 1. A statin 2. Niacin 3. Sterols 4. A fibric acid derivative ____ 5. Joanne is a 60-year-old patient with an LDL of 132 and a family history of coronary artery disease. She has already tried diet changes (increased fiber and plant sterols) to lower her LDL and after 6 months her LDL is slightly higher. The next step in her treatment would be: 1. A statin 2. Niacin 3. Sterols 4. A fibric acid derivative ____ 6. Sharlene is a 65-year-old patient who has been on a lipid-lowering diet and using plant sterol margarine daily for the past 3 months. Her LDL is 135 mg/dL. An appropriate treatment for her would be: 1. A statin 2. Niacin 3. A fibric acid derivative 4. Determined by her risk factors ____ 7. Phil is a 54-year-old male with multiple risk factors who has been on a high-dose statin for 3 months to treat his high LDL level. His LDL is 135 mg/dL and his triglycerides are elevated. A reasonable change in therapy would be to: 1. Discontinue the statin and change to a fibric acid derivative. 2. Discontinue the statin and change to ezetimibe. 3. Continue the statin and add in ezetimibe. 4. Refer him to a specialist in managing patients with recalcitrant hyperlipidemia. ____ 8. Jamie is a 34-year-old pregnant woman with familial hyperlipidemia and elevated LDL levels. What is the appropriate treatment for a pregnant woman? 1. A statin 2. Niacin 3. Fibric acid derivative 4. Bile acid-binding resins ____ 9. Han is a 48-year-old diabetic with hyperlipidemia and high triglycerides. His LDL is 112 mg/dL and he has not tolerated statins. He warrants a trial of a: 1. Sterol 2. Niacin 3. Fibric acid derivative 4. Bile acid-binding resin ____ 10. Jose is a 12-year-old overweight child with a total cholesterol of 180 mg/dL and LDL of 125 mg/dL. Along with diet education and recommending increased physical activity, a treatment plan for Jose would include ____________ with a reevaluation in 6 months. 1. Statins 2. Niacin 3. Sterols 4. Bile acid-binding resins ____ 11. Monitoring of a patient who is on a lipid-lowering drug includes: 1. Fasting total cholesterol every 6 months 2. Lipid profile with attention to serum LDL 6 to 8 weeks after starting therapy, then again in 6 weeks 3. Complete blood count, C-reactive protein, and erythrocyte sedimentation rate after 6 weeks of therapy 4. All of the above ____ 12. Before starting therapy with a statin, the following baseline laboratory values should be evaluated: 1. Complete blood count 2. Liver function (ALT/AST) and creatine kinase 3. C-reactive protein 4. All of the above ____ 13. When starting a patient on a statin, education would include: 1. If they stop the medication their lipid levels will return to pretreatment levels. 2. Medication is a supplement to diet therapy and exercise. 3. If they have any muscle aches or pain, they should contact their provider. 4. All of the above ____ 14. Omega 3 fatty acids are best used to help treat: 1. High HDL 2. Low LDL 3. High triglycerides 4. Any high lipid value ____ 15. When are statins traditionally ordered to be taken? 1. At bedtime 2. At noon 3. At breakfast 4. With the evening meal ____ 16. Which the following persons should not have a statin medication ordered? 1. Someone with 3 first- or second-degree family members with history of muscle issues when started on statins 2. Someone with high lipids, but low BMI 3. Premenopausal woman with recent history of hysterectomy 4. Prediabetic male with known metabolic syndrome ____ 17. Fiber supplements are great options for elderly patients who have the concurrent problem of: 1. End-stage renal failure on fluid restriction 2. Recurrent episodes of diarrhea several times a day 3. Long-term issues of constipation 4. Needing to take multiple medications around the clock every 2 hours ____ 18. What is considered the order of statin strength from lowest effect to highest? 1. Lovastatin, Simvastatin, Rosuvastatin 2. Rosuvastatin, Lovastatin, Atorvastatin 3. Atorvastatin, Rosuvastatin, Simvastatin 4. Simvastatin, Atorvastatin, Lovastatin Chapter 40. Hypertension Multiple Choice Identify the choice that best completes the statement or answers the question. ____ 1. Because primary hypertension has no identifiable cause, treatment is based on interfering with the physiological mechanisms that regulate blood pressure. Thiazide diuretics treat hypertension because they: 1. Increase renin secretion 2. Decrease the production of aldosterone 3. Deplete body sodium and reduce fluid volume 4. Decrease blood viscosity ____ 2. Because of its action on various body systems, the patient taking a thiazide or loop diuretic may also need to receive the following supplement: 1. Potassium 2. Calcium 3. Magnesium 4. Phosphates ____ 3. All patients with hypertension benefit from diuretic therapy, but those who benefit the most are: 1. Those with orthostatic hypertension 2. African Americans 3. Those with stable angina 4. Diabetics ____ 4. Beta blockers treat hypertension because they: 1. Reduce peripheral resistance 2. Vasoconstrict coronary arteries 3. Reduce norepinephrine 4. Reduce angiotensin II production ____ 5. Which of the following disease processes could be made worse by taking a nonselective beta blocker? 1. Asthma 2. Diabetes 3. Both might worsen 4. Beta blockade does not affect these disorders ____ 6. Disease states in addition to hypertension in which beta blockade is a compelling indication for the use of beta blockers include: 1. Heart failure 2. Angina 3. Myocardial infarction 4. Dyslipidemia ____ 7. Angiotensin-converting enzyme (ACE) inhibitors treat hypertension because they: 1. Reduce sodium and water retention 2. Decrease vasoconstriction 3. Increase vasodilation 4. All of the above ____ 8. Compelling indications for an ACE inhibitor as treatment for hypertension based on clinical trials includes: 1. Pregnancy 2. Renal parenchymal disease 3. Stable angina 4. Dyslipidemia ____ 9. An ACE inhibitor and what other class of drug may reduce proteinuria in patients with diabetes better than either drug alone? 1. Beta blockers 2. Diuretics 3. Nondihydropyridine calcium channel blockers 4. Angiotensin II receptor blockers ____ 10. If not chosen as the first drug in hypertension treatment, which drug class should be added as a second step because it will enhance the effects of most other agents? 1. ACE inhibitors 2. Beta blockers 3. Calcium channel blockers 4. Diuretics ____ 11. Treatment costs are important for patients with hypertension. Which of the following statements about cost is NOT true? 1. Hypertension is a chronic disease where patients may be taking drugs for a long time. 2. Most patients will require more than one drug to treat the hypertension. 3. The cost includes the price of any routine or special laboratory tests that a specific drug may require. 4. Few antihypertensive drugs come in generic formulations. ____ 12. Caffeine, exercise, and smoking should be avoided for at least how many minutes before blood pressure measurement? 1. 15 2. 30 3. 60 4. 90 ____ 13. Blood pressure checks in children: 1. Should occur with their annual physical examinations after 6 years of age 2. Require a blood pressure cuff that is one-third the diameter of the child’s arm 3. Should be done during every health-care visit after 3 years of age 4. Require additional laboratory tests such as serum creatinine ____ 14. Lack of adherence to blood pressure management is very common. Reasons for this lack of adherence include: 1. Lifestyle changes are difficult to achieve and maintain. 2. Adverse drug reactions are common and often fall into the categories more associated with nonadherence. 3. Costs of drugs and monitoring with laboratory tests can be expensive. 4. All of the above ____ 15. Lifestyle modifications for patients with prehypertension or hypertension include: 1. Diet and increase exercise to achieve a BMI greater than 25. 2. Drink 4 ounces of red wine at least once per week. 3. Adopt the dietary approaches to stop hypertension (DASH) diet. 4. Increase potassium intake. ____ 16. Which diuretic agents typically do not need potassium supplementation? 1. The loop diuretics 2. The thiazide diuretics 3. The aldosterone inhibitors 4. They all need supplementation ____ 17. Aldactone family medications are frequently used when the hypertensive patient also has: 1. Hyperkalemia 2. Advancing liver dysfunction 3. The need for birth control 4. Rheumatoid arthritis ____ 18. Hypertensive African Americans are typically listed as not being as responsive to which drug groups? 1. ACE inhibitors 2. Calcium channel blockers 3. Diuretics 4. Bidil (hydralazine family of medications) ____ 19. What educational points concerning fluid intake must be covered with diuretic prescriptions? 1. Fluid should be restricted when on them. 2. Fluids should contain at least one salty item daily. 3. Fluid intake should remain near normal for optimal performance. 4. Avoidance of potassium-rich fluids is encouraged. ____ 20. What is a common side effect concern with hypertensive medications and all individuals, but especially the elderly? 1. Risk of falls 2. Triggering of a hypertensive crisis 3. Erectile priapism 4. Risk for bladder cancer development Chapter 41. Hyperthyroidism and Hypothyroidism Multiple Choice Identify the choice that best completes the statement or answers the question. ____ 1. When methimazole is started for hyperthyroidism it may take ________ to see a total reversal of hyperthyroid symptoms. 1. 2 to 4 weeks 2. 1 to 2 months 3. 3 to 4 months 4. 6 to 12 months ____ 2. In addition to methimazole, a symptomatic patient with hyperthyroidism may need a prescription for: 1. A calcium channel blocker 2. A beta blocker 3. Liothyronine 4. An alpha blocker ____ 3. After starting a patient with Grave’s disease on an antithyroid agent such as methimazole, patient monitoring includes TSH and free T4 every: 1. 1 to 2 weeks 2. 3 to 4 weeks 3. 2 to 3 months 4. 6 to 9 months ____ 4. A woman who is pregnant and has hyperthyroidism is best managed by a specialty team who will most likely treat her with: 1. Methimazole 2. Propylthiouracil (PTU) 3. Radioactive iodine 4. Nothing, treatment is best delayed until after her pregnancy ends ____ 5. Goals when treating hypothyroidism with thyroid replacement include: 1. Normal TSH and free T4 levels 2. Resolution of fatigue 3. Weight loss to baseline 4. All of the above ____ 6. When starting a patient on levothyroxine for hypothyroidism the patient will need follow-up measurement of thyroid function in: 1. 2 weeks 2. 4 weeks 3. 2 months 4. 6 months ____ 7. Once a patient who is being treated for hypothyroidism returns to euthyroid with normal TSH levels, he or she should be monitored with TSH and free T4 levels every: 1. 2 weeks 2. 4 weeks 3. 2 months 4. 6 months ____ 8. Treatment of a patient with hypothyroidism and cardiovascular disease consists of: 1. Levothyroxine 2. Liothyronine 3. Liotrix 4. Methimazole ____ 9. Infants with congenital hypothyroidism are treated with: 1. Levothyroxine 2. Liothyronine 3. Liotrix 4. Methimazole ____ 10. When starting a patient with hypothyroidism on thyroid replacement hormones patient education would include: 1. They should feel symptomatic improvement in 1 to 2 weeks. 2. Drug adverse effects such as lethargy and dry skin may occur. 3. It may take 4 to 8 weeks to get to euthyroid symptomatically and by laboratory testing. 4. Because of its short half-life, levothyroxine doses should not be missed. ____ 11. In hyperthyroid states, what organ system other than CV must be evaluated to establish potential adverse issues? 1. The liver 2. The nails and skin 3. The eye 4. The ear ____ 12. Why are “natural” thyroid products not readily prescribed for most patients? 1. There is no reliability for the amount of hormone per dose. 2. There is higher incidence of allergic reactions. 3. There is a more reliable dose of T3 to T4 per batch. 4. All of the above ____ 13. What is the desired mixed of T3 to T4 drug levels in newly diagnosed endocrine patients? 1. 99% of T3 and the rest is T4 to get rapid resolution. 2. Most needs to be T4 to mimic natural ratios of hormone. 3. The ratio is unimportant. 4. The mix needs to be 50-50 at first. ____ 14. Laboratory values are actually different for TSH when screening for thyroid issues and when used for medication management. Which of the follow holds true? 1. Screening TSH has a wider range of normal values 0.02-5.0; therapeutic levels need to remain above 5.0. 2. Screening values are much narrower than the acceptable range used to keep a person stable on hormone replacement. 3. Therapeutic values are kept between 0.05 and 3.0 ideally. Screening values are considered acceptable up to 10. 4. Screening values are between 5 and 10, and therapeutic values are greater than 10. ____ 15. What happens to the typical hormone replacement dose when a woman becomes pregnant? 1. Most women need less medication. 2. Most women do not require a dose change. 3. The average woman needs more medication during pregnancy. 4. The average woman needs more medication only if carrying multiples. Chapter 42. Pneumonia Multiple Choice Identify the choice that best completes the statement or answers the question. ____ 1. The most common bacterial pathogen in community-acquired pneumonia is: 1. Haemophilus influenzae 2. Staphylococcus aureus 3. Mycoplasma pneumoniae 4. Streptococcus pneumoniae ____ 2. The first-line drug choice for a previously healthy adult patient diagnosed with community-acquired pneumonia would be: 1. Ciprofloxacin 2. Azithromycin 3. Amoxicillin 4. Doxycycline ____ 3. The first-line antibiotic choice for a patient with comorbidities or who is immunosuppressed who has pneumonia and can be treated as an outpatient would be: 1. Levofloxacin 2. Amoxicillin 3. Ciprofloxacin 4. Cephalexin ____ 4. If an adult patient with comorbidities cannot reliably take oral antibiotics to treat pneumonia, an appropriate initial treatment option would be: 1. IV or IM gentamicin 2. IV or IM ceftriaxone 3. IV amoxicillin 4. IV ciprofloxacin ____ 5. Samantha is 34 weeks pregnant and has been diagnosed with pneumonia. She is stable enough to be treated as an outpatient. What would be an appropriate antibiotic to prescribe? 1. Levofloxacin 2. Azithromycin 3. Amoxicillin 4. Doxycycline ____ 6. Adults with pneumonia who are responding to antimicrobial therapy should show improvement in their clinical status in: 1. 12 to 24 hours 2. 24 to 36 hours 3. 48 to 72 hours 4. 4 or 5 days ____ 7. Along with prescribing antibiotics, adults with pneumonia should be instructed on lifestyle modifications to improve outcomes, including: 1. Adequate fluid intake 2. Increased fiber intake 3. Bedrest for the first 24 hours 4. All of the above ____ 8. John is a 4-week-old infant who has been diagnosed with chlamydial pneumonia. An appropriate treatment for his pneumonia would be: 1. Levofloxacin 2. Amoxicillin 3. Erythromycin 4. Cephalexin ____ 9. Wing-Sing is a 4-year-old patient who has suspected bacterial pneumonia. He has a temperature of 102°F, oxygen saturation level of 95%, and is taking fluids adequately. What would be appropriate initial treatment for his pneumonia? 1. Ceftriaxone 2. Azithromycin 3. Cephalexin 4. Levofloxacin ____ 10. Giselle is a 14-year-old patient who presents to the clinic with symptoms consistent with mycoplasma pneumonia. What is the treatment for suspected mycoplasma pneumonia in an adolescent? 1. Ceftriaxone 2. Azithromycin 3. Ciprofloxacin 4. Levofloxacin Chapter 43. Smoking Cessation Multiple Choice Identify the choice that best completes the statement or answers the question. ____ 1. Nicotine withdrawal symptoms include: 1. Nervousness 2. Increased appetite 3. Difficulty concentrating 4. All of the above ____ 2. If a patient wants to quit smoking, nicotine replacement therapy is recommended if the patient: 1. Smokes more than 10 cigarettes a day 2. Smokes within 30 minutes of awakening in the morning 3. Smokes when drinking alcohol 4. All of the above ____ 3. Instructions for a patient who is starting nicotine replacement therapy include: 1. Smoke less than 10 cigarettes a day when starting nicotine replacement. 2. Nicotine replacement will help with the withdrawal cravings associated with quitting tobacco. 3. Nicotine replacement can be used indefinitely. 4. Nicotine replacement therapy is generally safe for all patients. ____ 4. Nicotine replacement therapy should not be used in which patients? 1. Pregnant women 2. Patients with worsening angina pectoris 3. Patients who have just suffered an acute myocardial infarction 4. All of the above ____ 5. Instructions for the use of nicotine gum include: 1. Chew the gum quickly to get a peak effect. 2. The gum should be “parked” in the buccal space between chewing. 3. Acidic drinks such as coffee help with the absorption of the nicotine. 4. The highest abstinence rates occur if the patient chews the gum when he or she is having cravings. ____ 6. Patients who choose the nicotine lozenge to assist in quitting tobacco should be instructed: 1. Chew the lozenge well. 2. Drink at least 8 ounces of water after the lozenge dissolves. 3. Use one lozenge every 1 to 2 hours (at least nine per day with a maximum of 20 per day). 4. A tingling sensation in the mouth should be reported to the provider. ____ 7. Transdermal nicotine replacement (the patch) is an effective choice in tobacco cessation because: 1. The patch provides a steady level of nicotine without reinforcing oral aspects of smoking. 2. There is the ability to “fine tune” the amount of nicotine that is delivered to the patient at any one time. 3. There is less of a problem with nicotine toxicity than other forms of nicotine replacement. 4. Transdermal nicotine is safer in pregnancy. ____ 8. The most common adverse effect of the transdermal nicotine replacement patch is: 1. Nicotine toxicity 2. Tingling at the site of patch application 3. Skin irritation under the patch site 4. Life-threatening dysrhythmias ____ 9. If a patient is exhibiting signs of nicotine toxicity when using transdermal nicotine, they should remove the patch and: 1. Wash the area thoroughly with soap and water. 2. Flush the area with clear water. 3. Reapply a new patch in 8 hours. 4. Take acetaminophen for the headache associated with toxicity. ____ 10. When a patient is prescribed nicotine nasal spray for tobacco cessation, instructions include: 1. Inhale deeply with each dose to ensure deposition in the lungs. 2. The dose is one to two sprays in each nostril per hour, not to exceed 40 sprays per day. 3. If they have a sensation of “head rush” this indicates the medication is working well. 4. Nicotine spray may be used for up to 12 continuous months. ____ 11. If prescribing bupropion (Zyban) for tobacco cessation, the instructions to the patient include: 1. Bupropion (Zyban) is started 1 to 2 weeks before the quit date. 2. Nicotine replacement products should not be used with bupropion. 3. If they smoke when taking bupropion they may have increased anxiety and insomnia. 4. Because they are not using bupropion as an antidepressant, they do not need to worry about increased suicide ideation when starting therapy. ____ 12. Varenicline (Chantix) may be prescribed for tobacco cessation. Instructions to the patient who is starting varenicline include: 1. The maximum time varenicline can be used is 12 weeks. 2. Nausea is a sign of varenicline toxicity and should be reported to the provider. 3. The starting regimen for varenicline is start taking 1 mg twice a day a week before the quit date. 4. Neuropsychiatric symptoms may occur. ____ 13. The most appropriate smoking cessation prescription for pregnant women is: 1. A nicotine replacement patch at the lowest dose available 2. Bupropion (Zyban) 3. Varenicline (Chantix) 4. Nonpharmacologic measures Chapter 44. Sexually Transmitted Infections and Vaginitis Multiple Choice Identify the choice that best completes the statement or answers the question. ____ 1. The goals of treatment when prescribing for sexually transmitted infections include: 1. Treatment of infection 2. Prevention of disease spread 3. Prevention of long-term sequelae from the infection 4. All of the above ____ 2. The drug of choice for treatment of primary or secondary syphilis is: 1. Ceftriaxone IM 2. Benzathine penicillin G IM 3. Oral azithromycin 4. Oral ciprofloxacin ____ 3. The drug of choice for treatment of early latent or tertiary syphilis is: 1. Ceftriaxone IM 2. Benzathine penicillin G IM 3. Oral azithromycin 4. Oral ciprofloxacin ____ 4. Demione is a 24-year-old patient who is 32 weeks pregnant and has tested positive for syphilis. The best treatment for her would be: 1. IM ceftriaxone 2. IM benzathine penicillin G 3. Oral azithromycin 4. Any of the above ____ 5. Treatment for suspected gonorrhea is: 1. Ceftriaxone 250 mg IM x 1 2. Ceftriaxone 2 grams IM x 1 3. Ciprofloxacin 500 mg PO x 1 4. Doxycycline 100 mg bid x 7 days ____ 6. When treating suspected gonorrhea in a nonpregnant patient, the patient should be concurrently treated for chlamydia with: 1. Azithromycin 1 gram PO x 1 2. Amoxicillin 500 mg PO x 1 3. Ciprofloxacin 500 mg PO x 1 4. Penicillin G 2.4 million units IM x 1 ____ 7. Ongoing monitoring is essential after treating for gonorrhea. The patient should be rescreened for gonorrhea and chlamydia in: 1. 4 weeks 2. 3 to 6 weeks 3. 3 to 6 months 4. 1 year ____ 8. A test of cure is recommended after treating chlamydia in which patient population? 1. Men who have sex with men 2. Adolescent females 3. Pregnant patients 4. All of the above ____ 9. Treatment for chancroid in a nonpregnant patient would be: 1. Oral azithromycin 2. IM ceftriaxone 3. Oral ciprofloxacin 4. Any of the above ____ 10. Jamie was treated for chancroid. Follow-up testing after treatment of chancroid would be: 1. Syphilis and HIV testing at 3-month intervals 2. Chancroid-specific antigen test every 3 months 3. Urine testing for Haemophilus ducreyi in 3 to 6 months for test of cure 4. Annual HIV testing if engaging in high-risk sexual behavior ____ 11. Helima presents with a complaint of vaginal discharge that when tested meets the criteria for bacterial vaginosis. Treatment of bacterial vaginosis in nonpregnant symptomatic women would be: 1. Metronidazole 500 mg PO bid x 7 days 2. Doxycycline 100 mg PO bid x 7 days 3. Intravaginal tinidazole daily x 5 days 4. Metronidazole 2 grams PO x 1 dose ____ 12. Besides prescribing antimicrobial therapy, patients with bacterial vaginosis require education regarding the fact that: 1. The most recent partners in the past 60 days should also be treated. 2. Alcohol should not be consumed during and for 1 day after metronidazole is taken. 3. Condoms should be used during intercourse if intravaginal clindamycin cream is used. 4. Co-treatment for chlamydia is necessary. ____ 13. Sydney presents to the clinic with vulvovaginal candidiasis. Appropriate treatment for her would be: 1. OTC intravaginal clotrimazole 2. OTC intravaginal miconazole 3. Oral fluconazole one-time dose 4. Any of the above ____ 14. If a woman presents with recurrent vulvovaginal candidiasis she may be treated with: 1. Weekly intravaginal butoconazole for 3 months 2. Fluconazole 150 mg PO daily x 7 doses then monthly for 6 months 3. Weekly fluconazole 150 mg PO x 6 months 4. Intravaginal tioconazole x 14 days ____ 15. Zoe presents with genital warts present on her labia. Patient-applied topical therapy for warts includes: 1. Podofilox 0.5% gel 2. Podophyllin 10% resin 3. Trichloracetic acid 4. Any of the above ____ 16. Sophie presents to the clinic with a malodorous vaginal discharge and is confirmed to have Trichomonas infection. Treatment for her would include: 1. Metronidazole 2 grams PO x 1 dose 2. Topical intravaginal metronidazole daily x 7 days 3. Intravaginal clindamycin daily x 7 days 4. Azithromycin 2 grams PO x 1 dose ____ 17. In addition to antimicrobial therapy, patients treated for Trichomonas infection should be educated regarding: 1. Necessity of treating sexual partner simultaneously 2. Abstaining from intercourse until both partners are treated 3. Need for retesting in 3 months due to high reinfection rate 4. All of the above Chapter 45. Tuberculosis Multiple Choice Identify the choice that best completes the statement or answers the question. ____ 1. Drug resistant tuberculosis (TB) is defined as TB that is resistant to: 1. Fluoroquinolones 2. Rifampin and isoniazid 3. Amoxicillin 4. Ceftriaxone ____ 2. Goals when treating tuberculosis include: 1. Completion of recommended therapy 2. Negative purified protein derivative at the end of therapy 3. Completely normal chest x-ray 4. All of the above ____ 3. The principles of drug therapy for the treatment of tuberculosis include: 1. Patients are treated with a drug to which M. tuberculosis is sensitive. 2. Drugs need to be taken on a regular basis for a sufficient amount of time. 3. Treatment continues until the patient’s purified protein derivative is negative. 4. All of the above ____ 4. Isabella has confirmed tuberculosis and is placed on a 6-month treatment regimen. The 6-month regimen consists of: 1. Two months of four-drug therapy (INH, rifampin, pyrazinamide, and ethambutol) followed by Four months of INH and rifampin 2. Six months of INH with daily pyridoxine throughout therapy 3. Six months of INH, rifampin, pyrazinamide, and ethambutol 4. Any of the above ____ 5. Kaleb has extensively resistant tuberculosis (TB). Treatment for extensively resistant TB would include: 1. INH, rifampin, pyrazinamide, and ethambutol for at least 12 months 2. INH, ethambutol, kanamycin, and rifampin 3. Treatment with at least two drugs to which the TB is susceptible 4. Levofloxacin ____ 6. Lila is 24 weeks pregnant and has been diagnosed with tuberculosis (TB). Treatment regimens for a pregnant patient with TB would include: 1. Streptomycin 2. Levofloxacin 3. Kanamycin 4. Pyridoxine ____ 7. Bilal is a 5-year-old patient who has been diagnosed with tuberculosis. His treatment would include: 1. Pyridoxine 2. Ethambutol 3. Levofloxacin 4. Rifabutin ____ 8. Ezekiel is a 9-year-old patient who lives in a household with a family member newly diagnosed with tuberculosis (TB). To prevent Ezekiel from developing TB he should be treated with: 1. 6 months of Isoniazid (INH) and rifampin 2. 2 months of INH, rifampin, pyrazinamide, and ethambutol, followed by 4 months of INH 3. 9 months of INH 4. 12 months of INH ____ 9. Leonard is completing a 6-month regimen to treat tuberculosis (TB). Monitoring of a patient on TB therapy includes: 1. Monthly sputum cultures 2. Monthly chest x-ray 3. Bronchoscopy every 3 months 4. All of the above ____ 10. Compliance with directly observed therapy can be increased by: 1. Convenient clinic times 2. Incentives such as food, clothing, and transportation costs 3. Offering gifts for compliance 4. All of the above Chapter 46. Upper Respiratory Infections, Otitis Media, and Otitis Externa Multiple Choice Identify the choice that best completes the statement or answers the question. ____ 1. Caleb is an adult with an upper respiratory infection (URI). Treatment for his URI would include: 1. Amoxicillin 2. Diphenhydramine 3. Phenylpropanolamine 4. Topical oxymetazoline ____ 2. Rose is a 3-year-old patient with an upper respiratory infection (URI). Treatment for her URI would include: 1. Amoxicillin 2. Diphenhydramine 3. Pseudoephedrine 4. Nasal saline spray ____ 3. Patients who should be cautious about using decongestants for an upper respiratory infection (URI) include: 1. School-age children 2. Patients with asthma 3. Patients with cardiac disease 4. Patients with allergies ____ 4. Jaheem is a 10-year-old low-risk patient with sinusitis. Treatment for a child with sinusitis is: 1. Amoxicillin 2. Azithromycin 3. Cephalexin 4. Levofloxacin ____ 5. Jacob has been diagnosed with sinusitis. He is the parent of a child in daycare. Treatment for sinusitis in an adult who has a child in daycare is: 1. Azithromycin 500 mg q day for 5 days 2. Amoxicillin-clavulanate 500 mg bid for 7 days 3. Ciprofloxacin 500 mg bid for 5 days 4. Cephalexin 500 mg qid for 5 days ____ 6. The length of treatment for sinusitis in a low-risk patient should be: 1. 5–7 days 2. 7–10 days 3. 14–21 days 4. 7 days beyond when symptoms cease ____ 7. Patient education for a patient who is prescribed antibiotics for sinusitis includes: 1. Use of nasal saline washes 2. Use of inhaled corticosteroids 3. Avoiding the use of ibuprofen while ill 4. Use of laxatives to treat constipation ____ 8. Myles is a 2-year-old patient who has been diagnosed with acute otitis media. He is afebrile and has not been treated with antibiotics recently. First-line treatment for his otitis media would include: 1. Azithromycin 2. Amoxicillin 3. Ceftriaxone 4. Trimethoprim/sulfamethoxazole ____ 9. Alyssa is a 15-month-old patient who has been on amoxicillin for 2 days for acute otitis media. She is still febrile and there is no change in her tympanic membrane examination. What would be the plan of care for her? 1. Continue the amoxicillin for the full 10 days. 2. Change the antibiotic to azithromycin. 3. Change the antibiotic to amoxicillin/clavulanate. 4. Change the antibiotic to trimethoprim/sulfamethoxazole. ____ 10. A child that may warrant “watchful waiting” instead of prescribing an antibiotic for acute otitis media includes patients who: 1. Are low risk with temperature of less than 39oC or 102.2oF 2. Have reliable parents with transportation 3. Are older than age 2 years 4. All of the above ____ 11. Whether prescribing an antibiotic for a child with acute otitis media or not, the parents should be educated about: 1. Using decongestants to provide faster symptom relief 2. Providing adequate pain relief for at least the first 24 hours 3. Using complementary treatments for acute otitis media, such as garlic oil 4. Administering an antihistamine/decongestant combination (Dimetapp) so the child can sleep better ____ 12. First-line therapy for a patient with acute otitis externa (swimmer’s ear) and an intact tympanic membrane includes: 1. Swim-Ear drops 2. Ciprofloxacin and hydrocortisone drops 3. Amoxicillin 4. Gentamicin ophthalmic drops Chapter 47. Urinary Tract Infections Multiple Choice Identify the choice that best completes the statement or answers the question. ____ 1. The treatment goals when treating urinary tract infection (UTI) include: 1. Eradication of infecting organism 2. Relief of symptoms 3. Prevention of recurrence of the UTI 4. All of the above ____ 2. Sally is a 16-year-old female with a urinary tract infection. She is healthy, afebrile, with no use of antibiotics in the previous 6 months and no drug allergies. An appropriate first-line antibiotic choice for her would be: 1. Azithromycin 2. Trimethoprim/sulfamethoxazole 3. Ceftriaxone 4. Levofloxacin ____ 3. Jamie is a 24-year-old female with a urinary tract infection. She is healthy, afebrile, and her only drug allergy is sulfa, which gives her a rash. An appropriate first-line antibiotic choice for her would be: 1. Azithromycin 2. Trimethoprim/sulfamethoxazole 3. Ceftriaxone 4. Ciprofloxacin ____ 4. Juanita is a 28-year-old pregnant woman at 38 weeks’ gestation who is diagnosed with a lower urinary tract infection (UTI). She is healthy with no drug allergies. Appropriate first-line therapy for her UTI would be: 1. Azithromycin 2. Trimethoprim/sulfamethoxazole 3. Amoxicillin 4. Ciprofloxacin ____ 5. Which of the following patients may be treated with a 3-day course of therapy for their urinary tract infection? 1. Juanita, a 28-year-old pregnant woman 2. Sally, a 16-year-old healthy adolescent 3. Jamie, a 24-year-old female 4. Suzie, a 26-year-old diabetic ____ 6. Nicole is a 4-year-old female with a febrile urinary tract infection (UTI). She is generally healthy and has no drug allergies. Appropriate initial therapy for her UTI would be: 1. Azithromycin 2. Trimethoprim/sulfamethoxazole 3. Ceftriaxone 4. Ciprofloxacin ____ 7. Monitoring for a healthy, nonpregnant adult patient being treated for a urinary tract infection is: 1. Symptom resolution in 48 hours 2. Follow-up urine culture at completion of therapy 3. “Test of cure” urinary analysis at completion of therapy 4. Follow-up urine culture 2 months after completion of therapy ____ 8. Monitoring for a child who has had a urinary tract infection is: 1. Symptom resolution in 48 hours 2. Follow-up urine culture at completion of therapy 3. “Test of cure” urinary analysis at completion of therapy 4. Follow-up urine culture 2 months after completion of therapy ____ 9. Monitoring for a pregnant woman who has had a urinary tract infection is: 1. Symptom resolution in 48 hours 2. Follow-up urine culture at completion of therapy 3. “Test of cure” urinary analysis at completion of therapy 4. Follow-up urine culture every 2 weeks until delivery ____ 10. Along with an antibiotic prescription, lifestyle education for a nonpregnant adult female who has had a urinary tract infection includes: 1. Increasing her intake of vitamin C-containing orange juice 2. Voiding 10 to 15 minutes after intercourse 3. Avoiding ingesting urinary irritants, such as asparagus 4. All of the above ____ 11. Lisa is a healthy nonpregnant adult woman who recently had a urinary tract infection (UTI). She is asking about drinking cranberry juice to prevent a recurrence of the UTI. The correct answer to give her would be: 1. Sixteen ounces per day of cranberry juice cocktail will prevent UTIs. 2. 100% cranberry juice or cranberry juice extract may decrease UTIs in some patients. 3. There is no evidence that cranberry juice helps prevent UTIs. 4. Cranberry juice only works to prevent UTIs in children. Chapter 48: Women as Patients Multiple Choice Identify the choice that best completes the statement or answers the question. ____ 1. Prescribing for women during their childbearing years requires constant awareness of the possibility of: 1. Pregnancy unless the women is on birth control 2. Risk for silent bacterial or viral infections of the genitalia 3. High risk for developmental disorders in their infants 4. Decreased risk for abuse during this time ____ 2. Intimate partner violence is a serious public health problem. It should be screened for: 1. At every encounter within the health-care system 2. When a women is being seen for symptoms of depression 3. Throughout pregnancy 4. If a sexually transmitted disease is diagnosed ____ 3. Because of their longer life expectancy, women are more likely than men to experience a disabling condition. Common conditions in older women that can produce disability include: 1. Depression 2. Panic disorders 3. Dementia 4. All of the above ____ 4. Gender differences between men and women in pharmacokinetics include: 1. More rapid gastric emptying so that drugs absorbed in the stomach have less exposure to absorption sites 2. Higher proportion of body fat so that lipophilic drugs have relatively greater volumes of distribution 3. Increased levels of bile acids so that drugs metabolized in the intestine have higher concentrations 4. Slower organ blood flow rates so drugs tend to take longer to be excreted ____ 5. Which of the following drug classes is associated with significant differences in metabolism based on gender? 1. Beta blockers 2. Antibiotics 3. Serotonin reuptake inhibitors 4. Angiotensin-converting-enzyme (ACE) inhibitors ____ 6. Since 40% of bone accrual occurs during adolescence, building bone during this time is critical. Ways to improve bone accrual in adolescents include: 1. Use of bisphosphonates early if dual energy X-ray absorptiometry (DEXA) scans show limited bone accrual 2. Encouraging a daily dietary intake of 1,300 mg of calcium and 400 IU of vitamin D 3. Avoiding all birth control methods that include progesterone 4. Fostering the intake of iron mainly in green and leafy vegetables ____ 7. Hot flashes are often a concern during menopause. Which of the following may help in reducing them? 1. Drink one caffeinated liquid per day 2. Take progesterone supplementation 3. Exercise 20-40 minutes/day 4. Increase intake of carrots, yams, and soy products ____ 8. Factors common in women that can affect adherence to a treatment regimen include all of the following EXCEPT: 1. Number of drugs taken: Women tend to take fewer drugs over longer periods of time 2. Fear that medications can cause disease: Information obtained from social networks may be inaccurate for a specific woman 3. Nutritional status: Worries about possible weight gain from a given drug may result in nonadherence 4. Religious differences: A patient’s belief system that is not congruent with the treatment regimen presents high risk for nonadherence ____ 9. Dysmenorrhea is one of the most common gynecological complaints in young women. The first line of drug treatment for this disorder is: 1. Oral contraceptive pills 2. Caffeine 3. NSAIDs 4. Aspirin ____ 10. Premenstrual dysphoric disorder (PMDD) occurs in a fairly small number of patients. Theories of the pathology behind PMDD that are supported in research include: 1. Altered sensitivity in the serontonic system 2. Inhibition of the cyclooxygenase system 3. Fluctuations of the gonadal hormones 4. All of these are theories supported by research ____ 11. Treatment of PMDD that affects all or most of the symptoms includes: 1. Tryptophan up to 6 g/d 2. Vitamin E 200-400 mg/d 3. Evening primrose oil 500 mg/d 4. Fluoxetine 20 mg/d ____ 12. Women are now the fastest growing population with HIV infection and AIDS. HIV-infected women: 1. Are less likely to become pregnant or to carry a pregnancy to term 2. Have higher rates of cervical dysplasia and HPV-concurrent infections 3. Are most often over 35 years of age 4. Most often come from Asian and Caucasian ethnic groups ____ 13. Maternal-to-child transmission of HIV infection during pregnancy may be prevented by: 1. Use of antiviral drugs such as zidovudine 2. Use of condoms during intercourse 3. Both 1 and 2 4. Neither 1 nor 2 ____ 14. Erroneous information about LGBTQ individuals can lead to failure to give accurate advice to them as patients. Which of the following statements is true about lesbians: 1. Lesbians cannot contract a sexually transmitted infection from their female partner. 2. Screening for cervical cancer is not required. 3. Lesbians as a group are less likely to have health-care insurance. 4. Like women in general, lesbians are more likely than gay men to seek care for health-related issues. ____ 15. Which of the following holds true for the pharmacokinetics of women? 1. Gastric emptying is faster than that of men. 2. Organ blood flow is the same as that of men. 3. Evidence is strong concerning renal differences in elimination. 4. Medications that involve binding globulins are impacted by estrogen levels. ____ 16. The metabolism of drugs in women is primarily impacted by: 1. Hepatic blow flow 2. Enzymes of the CYP450 system differences with men 3. The amount of gastric secretions 4. Whether they are pre- or postmenopausal ____ 17. The interpretation of DEXA scores in the rare cases of adolescent osteoporosis in teens: 1. Use the same T scores that are established for women 2. Cannot be done because of less-than-mature bones 3. Must use special Z-scores developed for this reason 4. Can only be done if bisphosphonates have already been started ____ 18. The timing of NSAIDS for best control of severe menstrual cramps includes: 1. Taking them for 2-3 days prior to the start of bleeding 2. Taking them 2-3 times a day during the first 2 days 3. Taking them every 2-3 hours 4. They have not been found to be helpful at all ____ 19. Which of the following is true concerning lesbian health concerns? 1. They cannot contract an STI from another woman. 2. Pap smears are not required to screen for cervical cancer. 3. Lesbian women have a tendency to be frequent clinic visitors. 4. The health risks associated with smoking, alcohol, and depression are higher than in the heterosexual population. Chapter 49. Men as Patients Multiple Choice Identify the choice that best completes the statement or answers the question. ____ 1. The factor that has the greatest effect on males developing male sexual characteristics is: 1. Cultural beliefs 2. Effective male role models 3. Adequate intake of testosterone in the diet 4. Androgen production ____ 2. When assessing a male for hypogonadism prior to prescribing testosterone replacement, serum testosterone levels are drawn: 1. Without regard to time of day 2. First thing in the morning 3. Late afternoon 4. In the evening ____ 3. Some research supports that testosterone replacement therapy may be indicated in which of the following diagnoses in men? 1. Age-related decrease in cognitive functioning 2. Metabolic syndrome 3. Decreased muscle mass in aging men 4. All of the above ____ 4. The goal of testosterone replacement therapy is: 1. Absence of all hypogonadism symptoms 2. Testosterone levels in the mid-normal range 1 week after an injection 3. Testosterone levels in the mid-normal range just prior to the next injection 4. Avoidance of high serum testosterone levels during therapy ____ 5. While on testosterone replacement, hemoglobin and hematocrit levels should be monitored. Levels suggestive of excessive erythrocytosis or abuse are: 1. Hemoglobin 14 g/dl or hematocrit 39% 2. Hemoglobin 11.5 g/dl or hematocrit 31% 3. Hemoglobin 13 g/dl or hematocrit 38% 4. Hemoglobin 17.5 g/dl or hematocrit 54% ____ 6. Monitoring of an older male patient on testosterone replacement includes: 1. Oxygen saturation levels at every visit 2. Serum cholesterol and lipid profile every 3 to 6 months 3. Digital rectal prostate screening exam at 3 and 6 months after starting therapy 4. Bone mineral density at 3 months and 6 months after starting therapy ____ 7. When prescribing phosphodiesterase type 5 (PDE-5) inhibitors such as sildenafil (Viagra) patients should be screened for use of: 1. Statins 2. Nitrates 3. Insulin 4. Opioids ____ 8. Men who are prescribed phosphodiesterase type 5 (PDE-5) inhibitors for erectile dysfunction should be educated regarding the adverse effects of the drug which include: 1. Hearing loss 2. Hypotension 3. Delayed ejaculation 4. Dizziness ____ 9. Male patients who should not be prescribed phosphodiesterase type 5 (PDE-5) inhibitors include: 1. Diabetics 2. Those who have had an acute myocardial infarction in the past 6 months 3. Patients who are deaf 4. Patients under age 60 years of age ____ 10. Monitoring of male patients who are using phosphodiesterase type 5 (PDE-5) inhibitors includes: 1. Serum fasting glucose levels 2. Cholesterol and lipid levels 3. Blood pressure 4. Complete blood count Chapter 50. Children as Patients Multiple Choice Identify the choice that best completes the statement or answers the question. ____ 1. The Pediatric Research Equity Acts requires: 1. All children be provided equal access to drug research trials 2. Children to be included in the planning phase of new drug development 3. That pediatric drug trials guarantee children of multiple ethnic groups are included 4. All applications for new active ingredients, new indications, new dosage forms, or new routes of administration require pediatric studies ____ 2. The Best Pharmaceuticals for Children Act: 1. Includes a pediatric exclusivity rule which extends the patent on drugs studied in children 2. Establishes a committee that writes guidelines for pediatric prescribing 3. Provides funding for new drug development aimed at children 4. Encourages manufacturers specifically to develop pediatric formulations ____ 3. The developmental variation in Phase I enzymes has what impact on pediatric prescribing? 1. None, Phase I enzymes are stable throughout childhood. 2. Children should always be prescribed lower than adult doses per weight due to low enzyme activity until puberty. 3. Children should always be prescribed higher than adult doses per weight due to high enzyme activity. 4. Prescribing dosages will vary based on the developmental activity of each enzyme, at times requiring lower than adult doses and other times higher than adult doses based on the age of the child. ____ 4. Developmental variation in renal function has what impact on prescribing for infants and children? 1. Lower doses of renally excreted drugs may be prescribed to infants younger than age 6 months. 2. Higher doses of water soluble drugs may need to be prescribed because of increased renal excretion. 3. Renal excretion rates have no impact on prescribing. 4. Parents need to be instructed on whether drugs are renally excreted or not. ____ 5. Topical corticosteroids are prescribed cautiously in young children because: 1. They may cause an intense hypersensitivity reaction 2. Of hypothalamic-pituitary-adrenal axis suppression 3. Corticosteroids are less effective in young children 4. Young children may accumulate corticosteroids, leading to toxic levels ____ 6. Liza is breastfeeding her 2-month-old son and has an infection that requires an antibiotic. What drug factors influence the effect of the drug on the infant? 1. Maternal drug levels 2. Half-life 3. Lipid-solubility 4. All of the above ____ 7. Drugs that are absolutely contraindicated in lactating women include: 1. Selective serotonin reuptake inhibitors 2. Antiepileptic drugs such as carbamazepine 3. Antineoplastic drugs such as methotrexate 4. All of the above ____ 8. Zia is a 4-month-old patient with otitis media. Education of his parents regarding administering oral antibiotics to an infant includes: 1. How to administer an oral drug using a medication syringe 2. Mixing the medication with a couple of ounces of formula and putting it in a bottle 3. Discontinuing the antibiotic if diarrhea occurs 4. Calling for an antibiotic change if the infant chokes and sputters during administration ____ 9. To increase adherence in pediatric patients a prescription medication should: 1. Have a short half-life 2. Be the best tasting of the effective drugs 3. Be the least concentrated form of the medication 4. Be administered 3 or 4 times a day ____ 10. Janie is a 5-month-old breastfed infant with a fever. Treatment for her fever may include: 1. “Baby” aspirin 2. Acetaminophen suppository 3. Ibuprofen suppository 4. Alternating acetaminophen and ibuprofen Chapter 51. Geriatric Patients Multiple Choice Identify the choice that best completes the statement or answers the question. ____ 1. Principles of prescribing for older adults include: 1. Avoiding prescribing any newer high-cost medications 2. Starting at a low dose and increasing the dose slowly 3. Keeping the total dose at a lower therapeutic range 4. All of the above ____ 2. Sadie is a 90-year-old patient who requires a new prescription. What changes in drug distribution with aging would influence prescribing for Sadie? 1. Increased volume of distribution 2. Decreased lipid solubility 3. Decreased plasma proteins 4. Increased muscle-to-fat ratio ____ 3. Glen is an 82-year-old patient who needs to be prescribed a new drug. What changes in elimination should be taken into consideration when prescribing for Glen? 1. Increased glomerular filtration rate (GFR) will require higher doses of some renally excreted drugs. 2. Decreased tubular secretion of medication will require dosage adjustments. 3. Thin skin will cause increased elimination via sweat. 4. Decreased lung capacity will lead to measurable decreases in lung excretion of drugs. ____ 4. A medication review of an elderly person’s medications involves: 1. Asking the patient to bring a list of current prescription medications to the visit 2. Having the patient bring all of their prescription, over-the-counter, and herbal medications to the visit 3. Asking what other providers are writing prescriptions for them 4. All of the above ____ 5. Steps to avoid polypharmacy include: 1. Prescribing two or fewer drugs from each drug class 2. Reviewing a complete drug history every 12 to 18 months 3. Encouraging the elderly patient to coordinate their care with all of their providers 4. Evaluating for duplications in drug therapy and discontinuing any duplications ____ 6. Robert is a 72-year-old patient who has hypertension and angina. He is at risk for common medication practices seen in the elderly including: 1. Use of another person’s medications 2. Hoarding medications 3. Changing his medication regimen without telling his provider 4. All of the above ____ 7. To improve positive outcomes when prescribing for the elderly the nurse practitioner should: 1. Assess cognitive functioning in the elder 2. Encourage the patient to take a weekly “drug holiday” to keep drug costs down 3. Encourage the patient to cut drugs in half with a knife to lower costs 4. All of the above ____ 8. When an elderly diabetic patient is constipated the best treatment options include: 1. Mineral oil 2. Bulk-forming laxatives such as psyllium 3. Stimulant laxatives such as senna 4. Stool softeners such as docusate ____ 9. Delta is an 88-year-old patient who has mild low-back pain. What guidelines should be followed when prescribing pain management for Delta? 1. Keep the dose of oxycodone low to prevent development of tolerance. 2. Acetaminophen is the first-line drug of choice. 3. Avoid prescribing NSAIDs. 4. Add in a short-acting benzodiazepine for a synergistic effect on pain. ____ 10. Robert is complaining of poor sleep. Medications that may contribute to sleep problems in the elderly include: 1. Diuretics 2. Trazodone 3. Clonazepam 4. Levodopa ____ 11. The GFRs for a 91-year-old woman who weighs 93 pounds and is 5'1" with a serum creatinine of 1.1, and for a 202-pound, 25-year-old male who is 5'9" with the same serum creatinine according to the Cockcroft Gault formula are: 1. 25ml/ min and 133 mL/min respectively 2. 25 mL/min and 103 mL/min respectively 3. 22 ml/min and 133 mL/min respectively 4. 22 ml/min and 103 mL/min respectively ____ 12. In geriatric patients, the percentage of body fat is increased. What are the pharmacologic implications of this physiologic change? 1. A lipid-soluble medication will be eliminated more quickly and not work as well. 2. A lipid-soluble medication will accumulate in fat tissue and its duration of action may be prolonged. 3. Absorption of lipid-soluble drugs is impaired in older adults. 4. The bioavailability of the lipid-soluble drug will be increased in older adults. ____ 13. All of the following statements about the Beer’s List are true except: 1. It is a list of medications or medication classes that should generally be avoided in persons 65 years or older because they are either ineffective or they pose unnecessarily high risk for older persons and a safer alternative is available. 2. It is derived from the expert opinion of one geriatrician and is not evidence-based. 3. These criteria have been adopted by the Centers for Medicare and Medicaid Services for regulation of long-term care facilities. 4. These criteria are directed at the general population of patients over 65 years of age and do not take disease states into consideration. ____ 14. You are reviewing the data from several meta-analyses that addressed the most common causes of adverse drug reactions in the older adult. Which of the following would you find to be decreased and the most common cause of these problems in older adults? 1. Body fat content 2. Liver function 3. Renal function/clearance 4. Plasma albumin levels ____ 15. Which of the following is not consistent with the rules for geriatric prescribing: 1. Half-life will be longer in older adults 2. Steady state is reached more quickly in the older adult 3. Reduce the number of drugs in the patient's regimen whenever possible 4. Adverse drug responses present atypically in the older adult Chapter 52. Pain Management: Acute and Chronic Pain Multiple Choice Identify the choice that best completes the statement or answers the question. ____ 1. Different areas of the brain are involved in specific aspects of pain. The reticular and limbic systems in the brain influence the: 1. Sensory aspects of pain 2. Discriminative aspects of pain 3. Motivational aspects of pain 4. Cognitive aspects of pain ____ 2. Patients need to be questioned about all pain sites because: 1. Patients tend to report the most severe or important in their perception. 2. Pain tolerance generally decreases with repeated exposure. 3. The reported pain site is usually the most important to treat. 4. Pain may be referred from a different site to the one reported. ____ 3. The chemicals that promote the spread of pain locally include: 1. Serotonin 2. Norepinephrine 3. Enkephalin 4. Neurokinin A ____ 4. Narcotics are exogenous opiates. They act by: 1. Inhibiting pain transmission in the spinal cord 2. Attaching to receptors in the afferent neuron to inhibit the release of substance P 3. Blocking neurotransmitters in the midbrain 4. Increasing beta-lipoprotein excretion from the pituitary gland ____ 5. Age is a factor in different responses to pain. Which of the following age-related statements about pain is NOT true? 1. Preterm and newborn infants do not yet have functional pain pathways. 2. Painful experiences and prolonged exposure to analgesic drugs during pregnancy may permanently alter neuronal organization in the child. 3. Increases in the pain threshold in older adults may be related to peripheral neuropathies and changes in skin thickness. 4. Decreases in pain tolerance are evident in older adults. ____ 6. Which of the following statements is true about acute pain? 1. Somatic pain comes from body surfaces and is only sharp and well-localized. 2. Visceral pain comes from the internal organs and is most responsive to acetaminophen and opiates. 3. Referred pain is present in a distant site for the pain source and is based on activation of the same spinal segment as the actual pain site. 4. Acute neuropathic pain is caused by lack of blood supply to the nerves in a given area. ____ 7. One of the main drug classes used to treat acute pain is NSAIDs. They are used because: 1. They have less risk for liver damage than acetaminophen. 2. Inflammation is a common cause of acute pain. 3. They have minimal GI irritation. 4. Regulation of blood flow to the kidney is not affected by these drugs. ____ 8. Opiates are used mainly to treat moderate to severe pain. Which of the following is NOT true about these drugs? 1. All opiates are scheduled drugs which require a DEA license to prescribe. 2. Opiates stimulate only mu receptors for the control of pain. 3. Most of the adverse effects of opiates are related to mu receptor stimulation. 4. Naloxone is an antagonist to opiates. ____ 9. If interventions to resolve the cause of pain (e.g., rest, ice, compression, and elevation) are insufficient, pain medications are given based on the severity of pain. Drugs are given in which order of use? 1. NSAIDs, opiates, corticosteroids 2. Low-dose opiates, salicylates, increased dose of opiates 3. Opiates, non-opiates, increased dose of non-opiate 4. Non-opiate, increased dose of non-opiate, opiate ____ 10. The goal of treatment of acute pain is: 1. Pain at a tolerable level where the patient may return to activities of daily living 2. Reduction of pain with a minimum of drug adverse effects 3. Reduction or elimination of pain with minimum adverse reactions 4. Adequate pain relief without constipation or nausea from the drugs ____ 11. Which of the following statements is true about age and pain? 1. Use of drugs that depend heavily on the renal system for excretion may require dosage adjustments in very young children. 2. Among the NSAIDs, indomethacin is the preferred drug because of lower adverse effects profiles than other NSAIDs. 3. Older adults who have dementia probably do not experience much pain due to loss of pain receptors in the brain. 4. Acetaminophen is especially useful in both children and adults because it has no effect on platelets and has fewer adverse effects than NSAIDs. ____ 12. Pain assessment to determine adequacy of pain management is important for all patients. This assessment is done to: 1. Determine if the diagnosis of source of pain is correct 2. Determine if the current regimen is adequate or different combinations of drugs and non-drug therapy are required 3. Determine if the patient is willing and able to be an active participant in his or her pain management 4. All of the above ____ 13. Pathological similarities and differences between acute pain and chronic pain include: 1. Both have decreased levels of endorphins. 2. Chronic pain has a predominance of C-neuron stimulation. 3. Acute pain is most commonly associated with irritation of peripheral nerves. 4. Acute pain is diffuse and hard to localize. ____ 14. A treatment plan for management of chronic pain should include: 1. Negotiation with the patient to set personal goals for pain management 2. Discussion of ways to improve sleep and stress 3. An exercise program to improve function and fitness 4. All of the above ____ 15. Chronic pain is a complex problem. Some specific strategies to deal with it include: 1. Telling the patient to “let pain be your guide” to using treatment therapies 2. Prescribing pain medication on a “PRN” basis to keep down the amount used 3. Scheduling return visits on a regular basis rather than waiting for poor pain control to drive the need for an appointment 4. All of the above ____ 16. Chemical dependency assessment is integral to the initial assessment of chronic pain. Which of the following raises a “red flag” about potential chemical dependency? 1. Use of more than one drug to treat the pain 2. Multiple times when prescriptions are lost with requests to refill 3. Preferences for treatments that include alternative medicines 4. Presence of a family member who has abused drugs ____ 17. The Pain Management Contract is appropriate for: 1. Patients with cancer who are taking morphine 2. Patients with chronic pain who will require long-term use of opiates 3. Patients who have a complex drug regimen 4. Patients who see multiple providers for pain control [Show More]
Last updated: 1 year ago
Preview 1 out of pages
Reviews( 0 )
Document information
Connected school, study & course
About the document
Uploaded On
May 25, 2020
Number of pages
Written in
Additional information
This document has been written for:
Uploaded
May 25, 2020
Downloads
0
Views
22

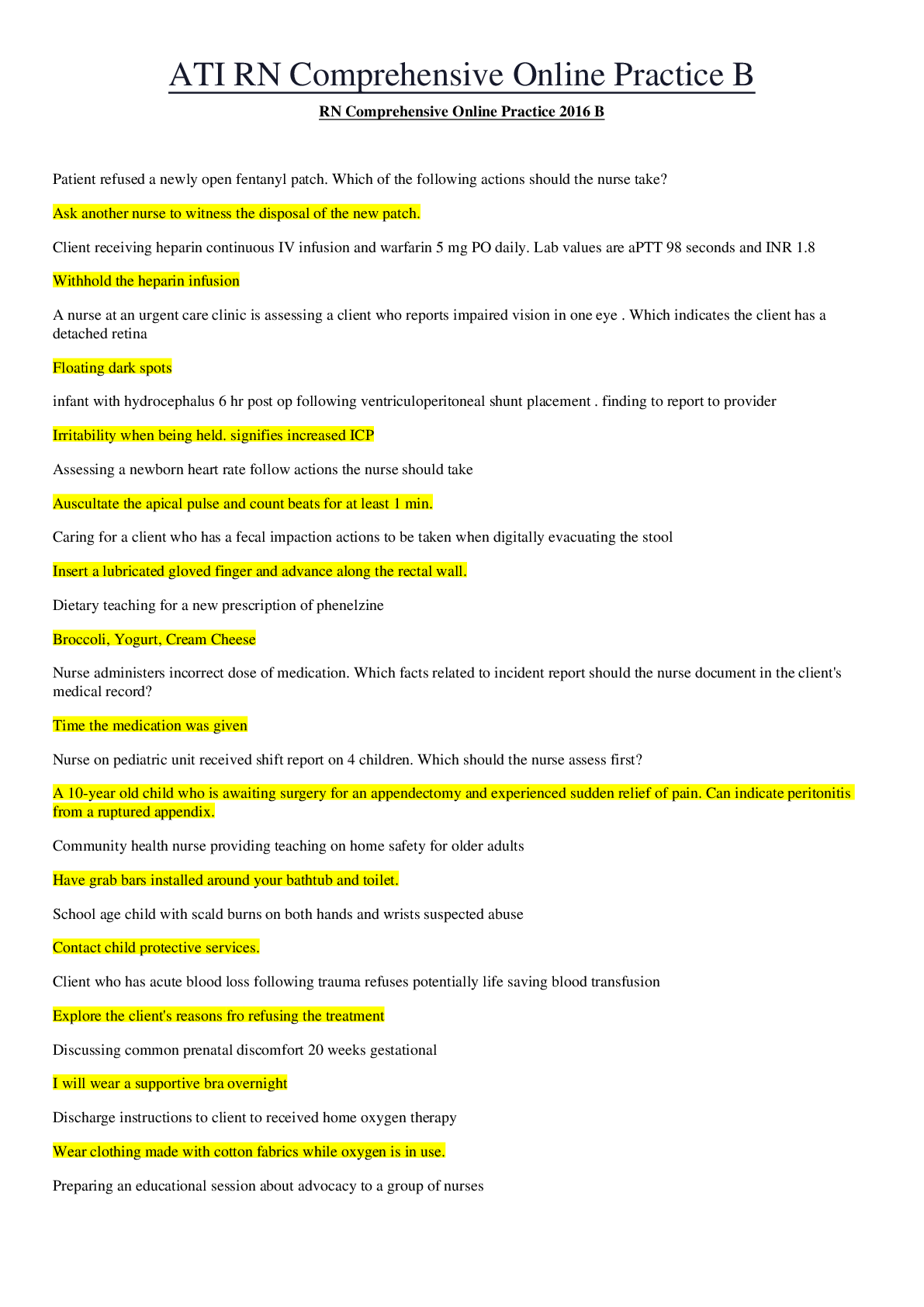
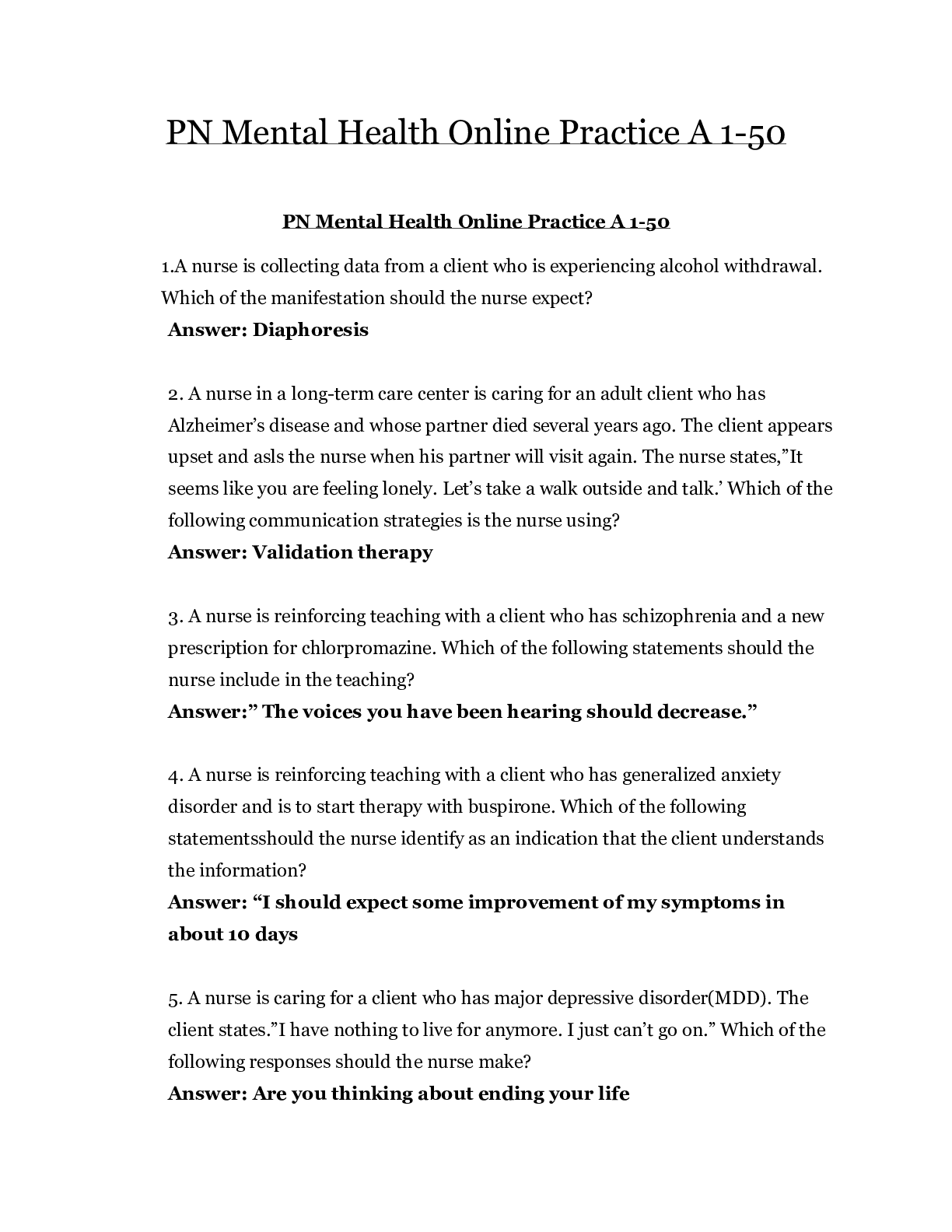
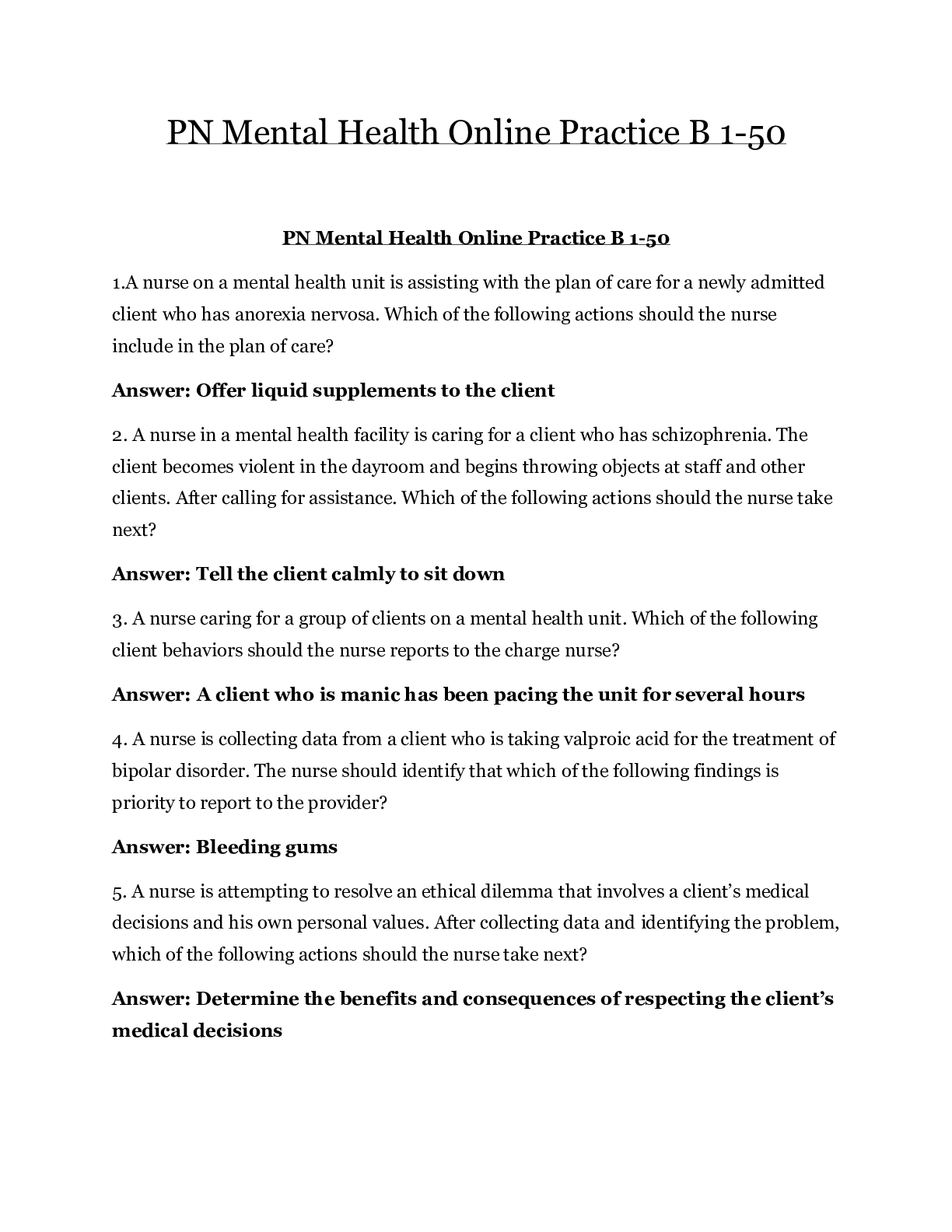
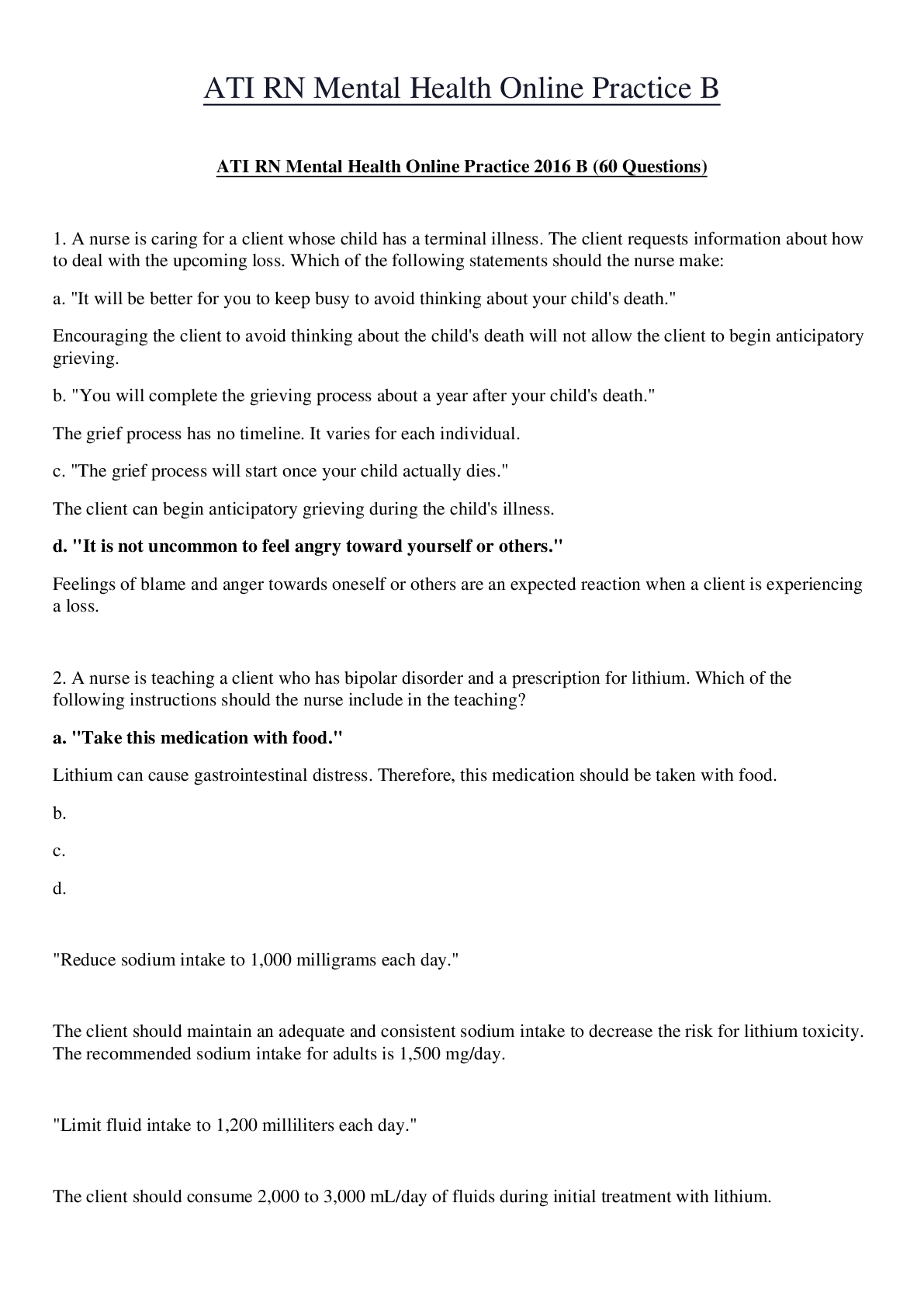
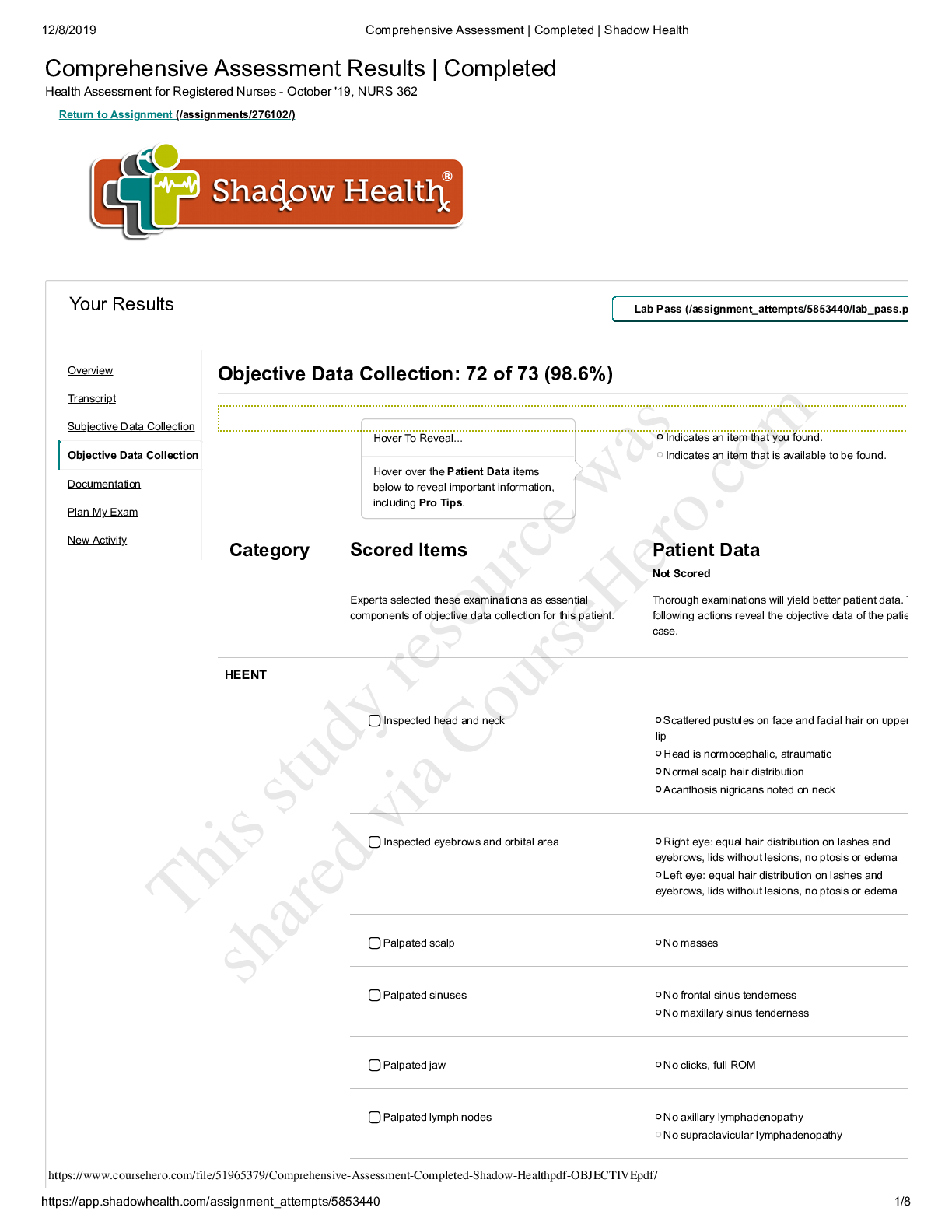

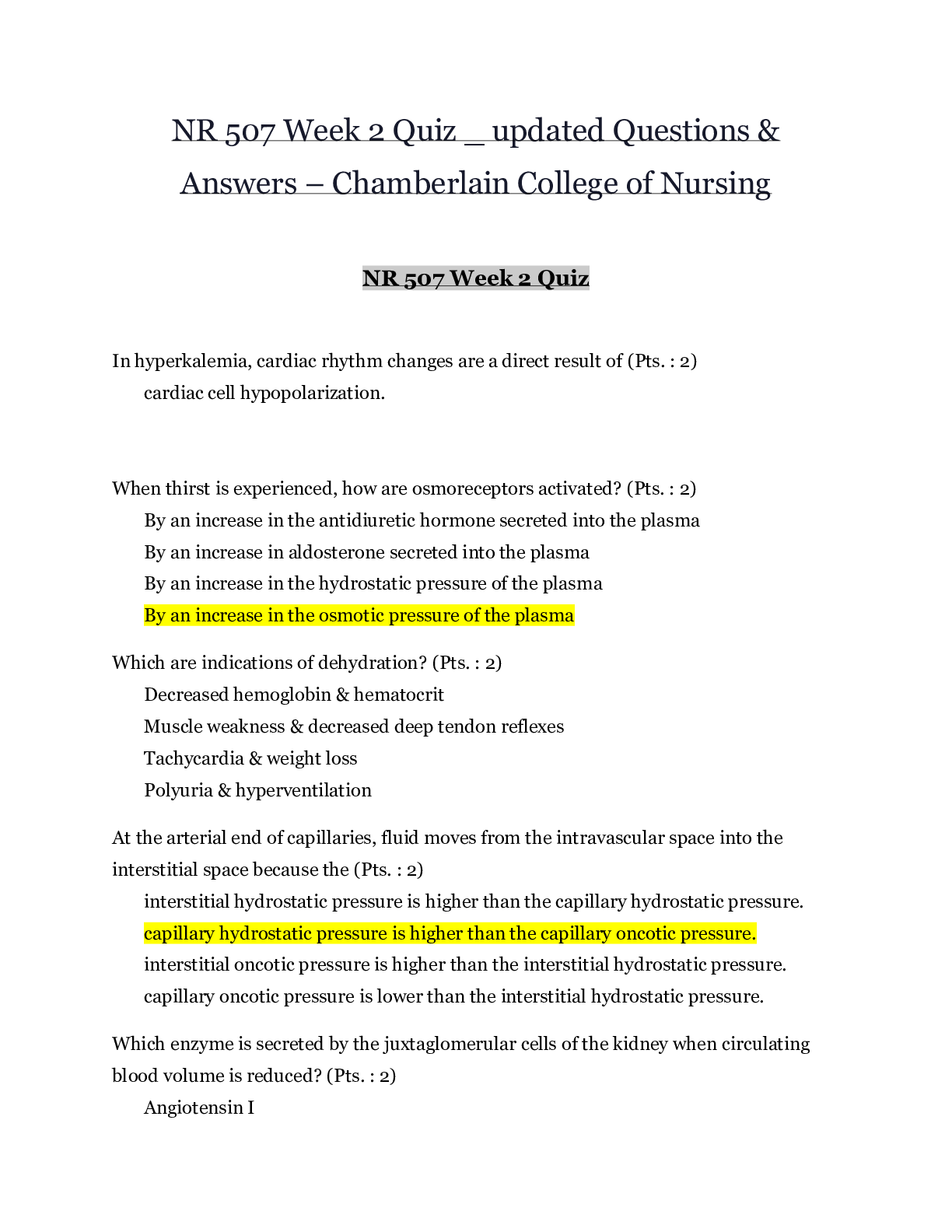
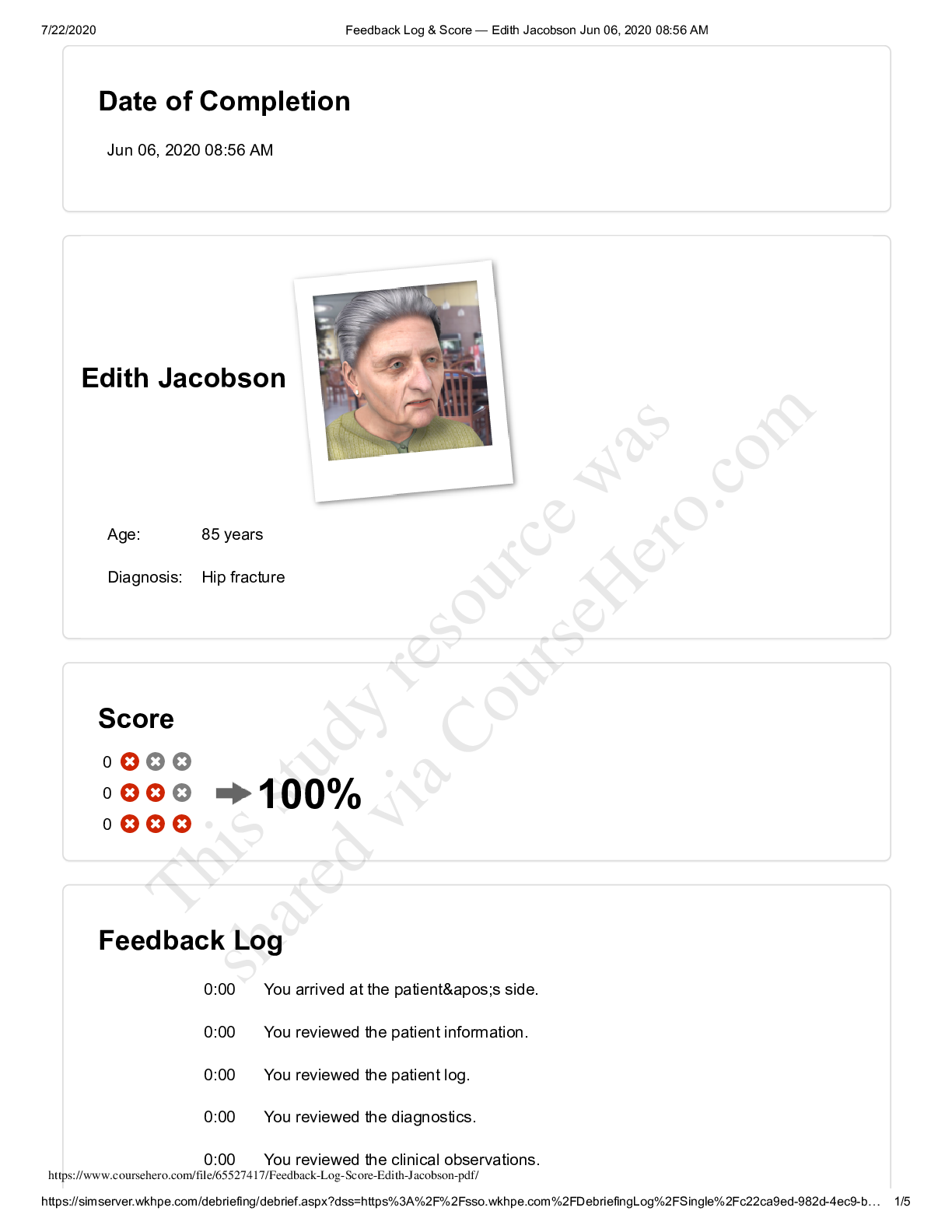


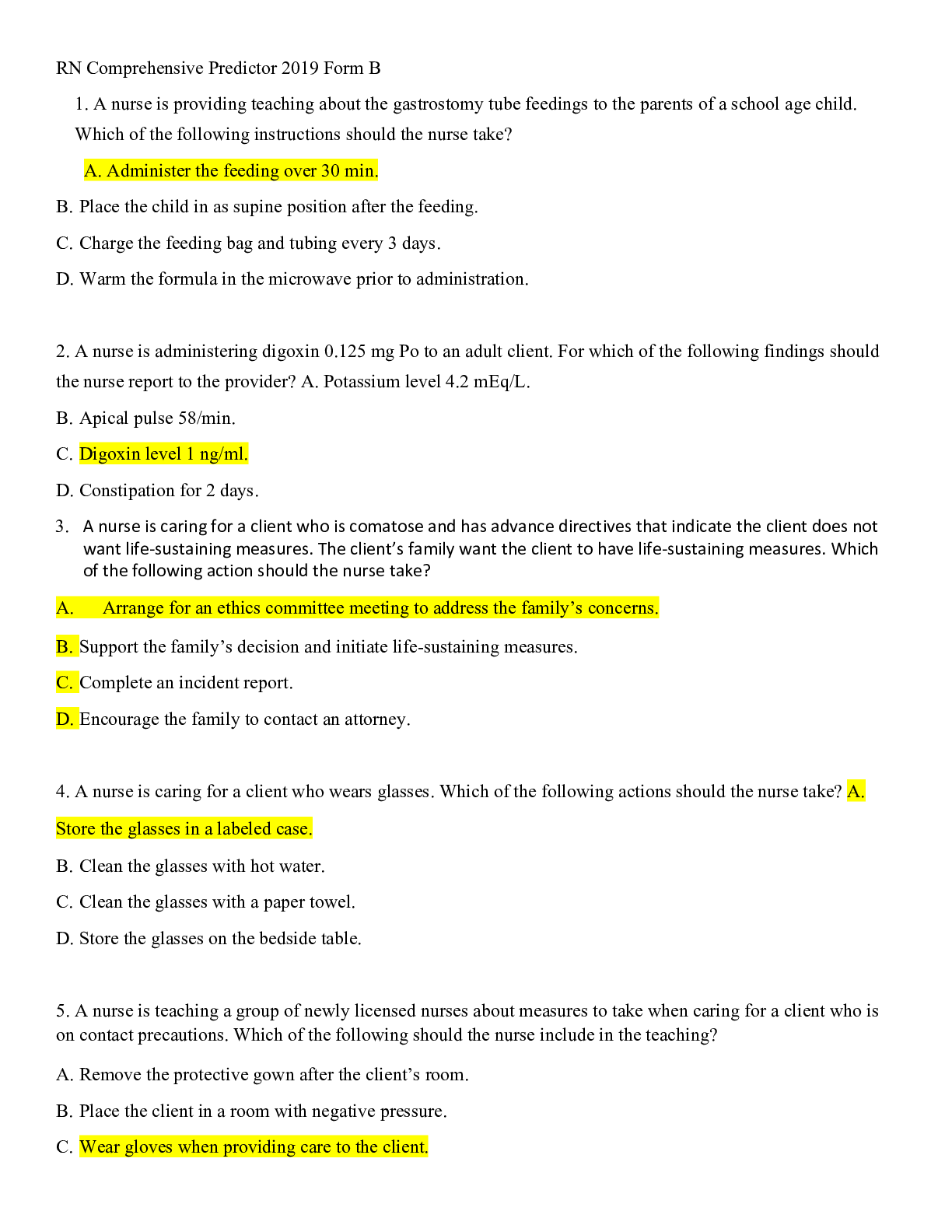
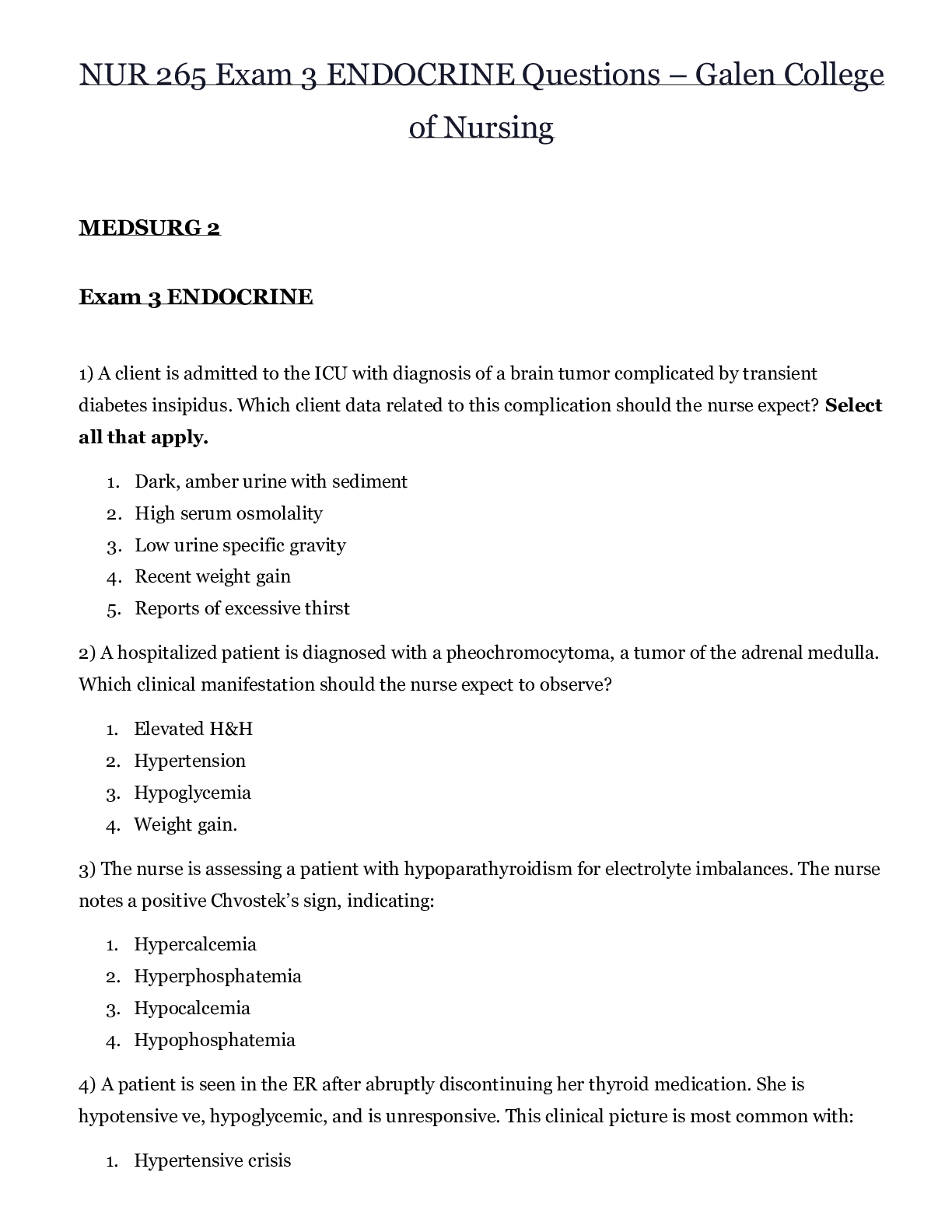
 – CHAMBERLAIN COLLEGE OF NURSING.png)