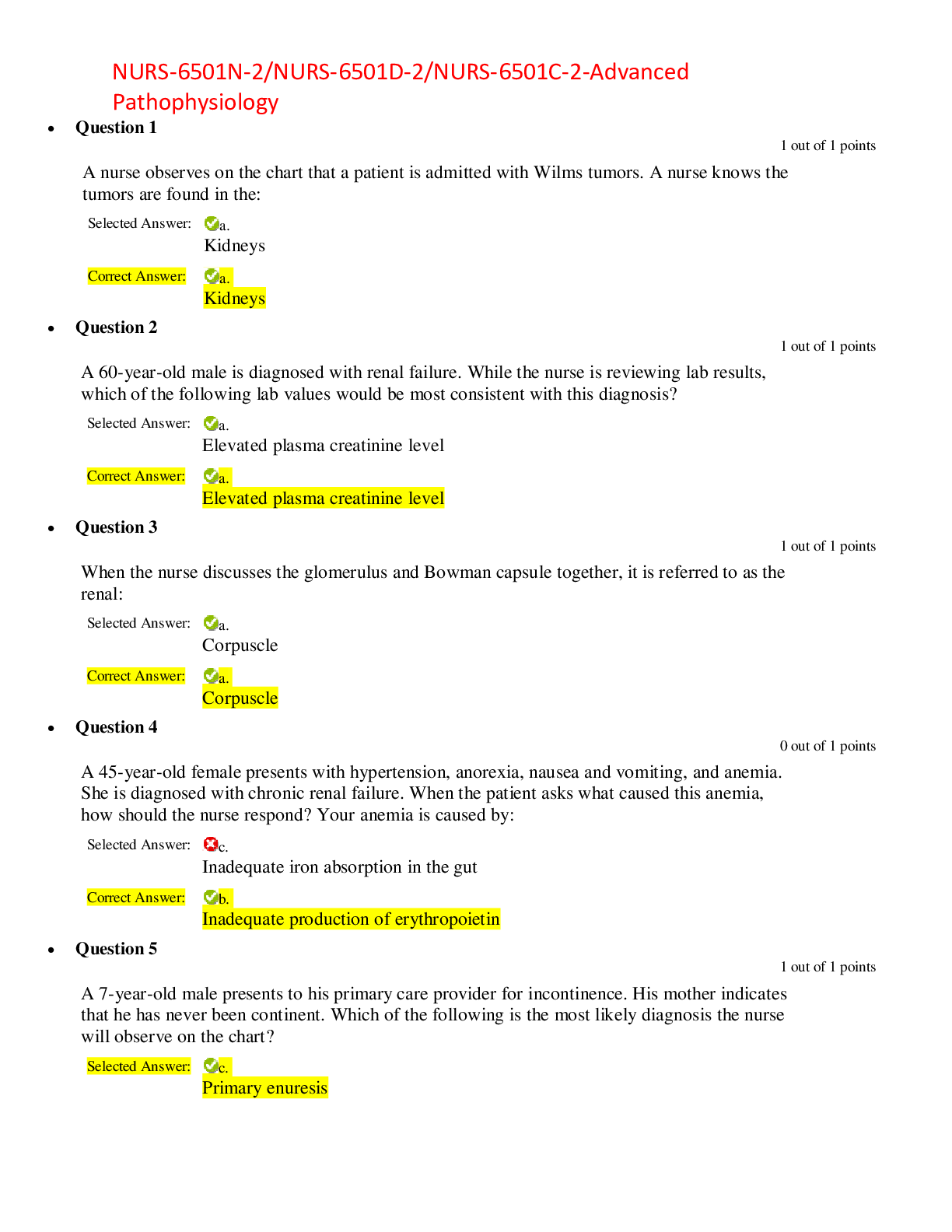
*NURSING > EXAM > NURS 6512N | NURS 6512N Week 6 Midterm Exam Review Week 1 to 6 | COMPLETE DETAILED REVIEW EXAM NURS (All)
NURS 6512N | NURS 6512N Week 6 Midterm Exam Review Week 1 to 6 | COMPLETE DETAILED REVIEW EXAM NURS 6512N
Document Content and Description Below
NURS 6512 Midterm Exam Review (Week 1-6) Building A Complete Health History 1. Communication techniques used to obtain a patient’s health history Courtesy, Comfort, Connection, Confirmation (i... .e. knock on door before entering, learn their names, ensure confidentiality, ensure good lighting & temperature, don't overtire patient, maintain good eye contact, watch your language, avoid being judgemental, conduct a CPE, avoid leading or directing an answer, ask the patient to summarize discussion, allow time for questions, be honest if you do not know the answer) 2. Recording and documenting patient information Documentation is most important: • Chronologically documents the care of the patient & contributes to high-quality care • Primary means of communication between healthcare team members which facilitates continuity care & communication among those involved with the patient's care • Establishes your credibility as a healthcare provider (i.e., use professional language, include appropriate content) • Legal implications: • Provides evidence that appropriate care was given & how the patient responded to the care provided • "If it was not documented, it was not done" - quote is important with considerable time-lapse that in a event where you may have to recall the events that occurred in court • The Centers for Medicare and Medicaid Services (CMS) requires: (Sullivan, 2012, p. 2) 1. The medical record should be complete and legible 2. The documentation of each patient encounter should include the following: • Reason for the encounter and relevant history, physical exam findings, and diagnostic test results • Assessment, clinical impression, or diagnosis • Plan for care • Date and legible identity of the observer 3. If not documented, the rationale for ordering diagnostic and other ancillary services should be easily inferred 4. Past and present diagnoses should be accessible to the treating and consulting providers 5. Appropriate health risk factors should be identified. 6. The patient's progress, response to and changes in treatment, and revision of diagnoses should be documented 7. The Current Procedural Terminology (CPT) and ICD-9 codes reported on the health insurance claim form or billing statement should be documentation. (Examples of how to document ICD code are on page 5 of Sullivan's). • Maintain patient confidentiality (HIPPA) • Patients and their respected parties have the right to view medical records with limitations (i.e., psychiatric patients cannot view provider's notes) The Comprehensive History & Physical Exam • Documents the patient's medical history, physical exam findings, diagnoses or medical problems, diagnostic studies to be performed, and initial plan of care implemented to address any problems identified. • Do not copy another provider's H&P- always perform your own and if unable to then give credit to the provider responsible • History includes: patient's personal identification • Chief Complaint (CC)- why is the patient there? (Best stated in the patient's own words) • History of the Present Illness or History of the CC: the chronological description of the development of the patient's present illness from the first sign or symptom of the presenting problems. Include identifying elements such as location, quality, severity, duration, timing, content, modifying factors, & associated sign and symptoms. • Past Medical History: documents the patient's past and current health. Includes: Past medical history, past surgical history or other hospitalizations (provide dates if possible), medications, drug allergies, and health maintenance and immunizations. • Family History: first-degree relatives includes parents, grandparents, and siblings with the age their age and status. If deceased, include the age at time of death and cause of death. Psychosocial History: Identify factors that may influence the patient's overall health or behaviors that places the patient at risk for specific conditions. Includes patient's sexual orientation, marital status, children, occupation status, environmental risks, language preference (if interpreter required, it must be documented), religion/ cultural beliefs, tobacco/etoh/illicit drug use, diet, etc. • Review of Systems (ROS): an inventory of specific body systems designed to document any symptoms the patient may be experiencing or has experienced. Includes positive and negative responses from patient • Physical Examination: may confirm or refute a diagnosis suspected from the history and provide a more accurate problem list. • Laboratory & Diagnostic Studies: laboratory tests, radiographs, or other imaging studies with specific values/results which allows readers to formulate their own conclusions, documents baseline values, and saves time for other readers to look values. • Problem List, Assessment, and Differential Diagnosis: provider evaluates all the info to identify the patient's problems in a numbered list (includes date of onset and whether active/inactive) with the most severe problems listed first. • Plan of Care: document any additional studies or workup needed, referrals or consults needed, pharmacological management, nonpharm.or other management patient education, and disposition (i.e., "return to clinic" or "admit to the hospital" 3. SOAP note documentation SOAP note documentation is the comprehensive history and physical examination documented in a format. S – Subjective: includes chief complaint (CC), history of present illness (HPI), Pertinent past medical history (PMH), Pertinent family history (FH), Pertinent psychosocial history (SH), any specialized history related to the chief complaint, and Pertinent review of systems (ROS) (Sullivan, pp.91-92). O – Objective: includes the vital signs, a general assessment of the patient, physical examination findings, results from laboratory or diagnostic tests (Sullivan, p. 93) A – Assessment: is an analysis and interpretation of the subjective and objective data to provide a diagnosis or a list of differential diagnoses (Sullivan, pp. 96-97). P – Plan: this area includes diagnostic studies that will be obtained, referrals, therapeutic interventions, educational material, disposition of the patient, next visit (Sullivan, p. 99). 4. Subjective vs objective information when documenting Subjective is the history given by the patient that guides the physical objective examination (Sullivan, p. 91). Subjective information is based on personal opinions, interpretations, points of view, emotions and judgment. Objective information or analysis is fact-based, measurable and observable. 5. Ethical decision-making and beneficence • Beneficence: "The principle of acting with the best interest of the other in mind. It is the basic premise that healthcare providers have a duty to be of a benefit to the patient as well as to take positive steps to prevent harm from the patient." (Levitt, 2014). • "Practitioners need to be aware and make practice decisions from good quality scientific evidence as well as clinical judgment considerations with individual patients" (Dains, Baumann, & Scheibel, 2016, p. 10). • "Not all diseases or conditions are appropriate for screening. The purposes of screening must be ethically acceptable, information must be used for appropriate purposes, tests must be of high quality, individuals should know what is taking place and informed of their results, counseling must be available to interpret results, and results must be kept confidential" (Dains et al., 2016, p. 8). • Guidelines to determine if appropriate to screen: 1. Is the condition significant in the community? -Morbidity and mortality data must justify if the condition has a significant impact on quality and quantity of life. Does it justify the cost to screen? 2. Can the condition be screened? -Tests must be at a reasonable cost and is determined by the sensitivity (ability to provide a true positive), specificity (ability to provide a true negative), reliability (reproducibility), and validity (does it measure what you think it measures?). 3. Should the conditions be screened? -"Before screening can be recommended, acceptable treatments must be available." Once the condition is detected, will the treatment have a significant impact to improve the health outcomes? • The United States Preventive Services Task Force (USPSTF): independent group of experts in prevention and evidence-based medicine; Makes recommendations about clinical preventive services such as screenings, counseling, and preventive medications. -Works with the Evidence-Based Practice Centers (EPCs) to conduct in-depth systematic reviews of available evidence and develop a analytic framework Diversity and Health Assessments 6. Cultural awareness and diversity *Cultural reflects the whole of human behavior including ideas and attitudes; ways of relating, speaking manners, products of physical effort, ingenuity and imagination. *Cultural awareness- being knowledgeable of one’s thoughts, feelings, sensation and how these things affect interactions Crossing the cultural divide helps, but skepticism is a barrier. *Cultural humility- recognizing one’s limitation in knowledge and cultural perspective to be open to new perspectives; view each patient individually *Seeleman et al framework- emphasizes on awareness of social context which specific ethnic groups live Social context in minority group means assessing stressors and support networks, sense of life control and literacy *Campinha- Bacote’s process of Cultural Competence Model- includes (cultural competence dimensions): Awareness- self- examination and in -depth exploration of your biases, stereotypes, prejudices, and assumption Knowledge- seeking and obtaining education Skill- collecting culturally relevant data assessing in a cultural manner Encounter- patient interactions used to validate, redefine or modify existing beliefs and practices and develop cultural desire or modify existing beliefs and practices and develop cultural desire awareness, skill, and knowledge Desire- motivation to want engagement in being culturally competent Siedel- pp. 22- 23 7. Socioeconomic, spiritual, and lifestyle factors affecting diverse populations Culturally competent care requires that health care providers be sensitive to patients’ heritage, sexual orientation, socioeconomic situation, ethnicity, and cultural background. Cultural encounters: the continuous process of interacting with patients from culturally diverse backgrounds in order to validate, refine, or modify existing values, beliefs, and practices about a cultural group and to develop cultural desire, cultural awareness, cultural skill, and cultural knowledge. Cultural Desire: the motivation of the health care professional to “want to” engage in the process of becoming culturally competent, not the “have to”. Cultural Awareness: the deliberate self-examination and in-depth exploration of one’s biases, stereotypes, prejudices, assumptions and “isms” that one holds about individuals and groups who are different from them. Cultural Knowledge: the process of seeking and obtaining a sound educational base about culturally and ethnically diverse groups. Cultural Skill: the ability to collect culturally relevant data regarding the patient’s presenting problem, as well as accurately performing a culturally-based physical assessment in a culturally sensitive manner. Poverty and inadequate education disproportionately affects various cultural groups; socioeconomic disparities negatively affect the health and medical care of individuals belonging to these groups. The health care provider must be open and willing to understand individual’s different spiritual rituals. When cultural differences exist, be certain that you grasp exactly what the patient means and know exactly what the patient thinks you mean in words and actions. 8. Functional assessments Functional assessment is an attempt to understand a patient’s ability to achieve the basic activities of daily living. This assessment should be made for all older adults and for any person limited by disease or disability, acute or chronic. A well-taken history and a meticulous physical examination can bring out subtle influences, such as tobacco and alcohol use, sedentary habits, poor food selection, overuse of medications (prescribed and non-prescribed), and less than obvious emotional distress. Even some physical limitations may not be readily apparent. Keep in mind that patients tend to overstate their abilities and, quite often, to obscure reality. When performing a functional assessment consider a variety of disabilities: physical, cognitive, psychologic, social, and sexual. An individual’s social and spiritual support system must be as clearly understood as the physical disabilities. There are a variety of physical disabilities, including: mobility, upper extremity function, housework, and instrumental activities of daily living. Assessment Tools and Diagnostic Tests in Adults and Children 9. Growth, Development, and Measurements in children and adults Assessment tools: Body Mass Index (BMI): weight in pounds/height in inchesx703=BMI Adults: Children over age 2: (same calculation with the result plotted on a curve) Underweight= <18.5 Underweight: under the 5th percentile Appropriate weight= 18.5-24.9 At risk for overweight: >85th percentile Overweight= 25-29.9 Overweight: >95th percentile Obese=30-39.9 Extremely obese= >40 Measurements for children: Use WHO growth curve for age and gender to identify percentile growth Birth-24 months, over the age of 2 years use CDC growth curve for gender. Recumbent length: while child is laying flat with legs straight measure from head to bottom of feet Standing height obtained beginning at 2 years of age-done without child wearing shoes and when placed back against the wall looking straight forward. Device mounted on wall then placed flat on the top of the head. Weight: most accurate measurement is in grams Newborns lose up to 10% of weight and regain within 2 weeks of life. Then gain 1 oz/day until 3 months when gain slows. Double birth weight by 4-5 months, and triple by 1 year Head circumference: completed from birth through age 2-3 years. Wrap tape around head at occipital protuberance and the supraorbital prominence At 2 years of age the head circumference is 2/3 of its adult size Chest circumference: measure around chest at nipple line Head circumference equals or exceeds chest circumference until 5 months of age, then both measurements are about equal until age 2, after age 2 the chest circumference exceeds the head circumference Upper-to-Lower Segment Ratio: Only used if child has inappropriate proportions between the head and trunk compared to lower extremities Measure from symphysis pubis to the floor while child standing to obtain lower segment. Subtract this number from the total height to obtain upper body segment. Then divide the upper body segment by the lower body segment to obtain ratio. Gestational Age: indicator of newborn’s maturity Determined by calculating the number of completed weeks between the first day of the mother’s last menstrual period and the date of birth Ballard Gestational Tool: evaluates 6 physical and 6 neuromuscular characteristics within 36 hours of birth to establish/confirm newborn’s gestational age Intrauterine growth curve: used to classify fetus as small (<10th percentile), appropriate (10th- 90th percentile) or large (>90th percentile) for gestational age. Weight is the used measurement Sexual Maturation: Secondary sexual characteristics include breast (5 stages) and pubic hair (6 stages) development in girls, and genital (5 stages) and pubic hair (6 stages) development in boys. Onset of puberty for girls is stage 2 of breast development or stage 2 of pubic hair development. Completion is when stage 4 of breast development or stage 5 of pubic hair development is reached. Puberty often begins between 9-12 years of age in girls, and 10-13 years of age in boys Sexual Maturity Rating (SMR): average of girl’s stages of pubic hair and breast development, or average of boy’s stages of pubic hair and genital development. Menarche usually begins in SMR 4 or breast stage 3 or 4. Pregnancy: Recommended weight gain based on prepregnancy BMI. First trimester weight gain is variable. Second and third trimesters ½-1 pound/week. Normal BMI: gain 25-35 pounds Underweight BMI: gain 28-40 pounds Overweight BMI: gain 15-25 pounds Obese: gain no more than 11-20 pounds 10. Nutritional assessment to include recommended water intake and energy requirements ****Nutrients necessary to the body are macronutrients, micronutrients and water**** -A nutritional assessment is an analysis of an individual’s approximate nutrient intake and related it to the history, physical exam findings, body size measurements, and biochemical measures. -Provides a guide for assessing an individual’s intake. For H & P: assess nutritional status by reviewing: 1) recent growth 2) Wight loss or weight gain 3) Chronic illnesses affecting nutritional status or intake 4) Med and supplement use 5) Nutritional screen 6) Assessment of nutrient intake 7) s/s of nutrient or energy deficiency 8) lab values -Comparing anthropometric measurements and compare to standardized tables. 1) standing height 2) weight 3). BMI 4). Waist circumference 5). Waist-height ration and waist-hip circumference ration 6). Triceps skinfold. -Water is the most vital nutrient. An individual can exist without food for several weeks but without water for only a few days. The body of a human adult is made of about 55-65% of water. Approximately 2-2.5 liters of water is lost from the body per day. There is no recommended daily allowance for water since individual water needs vary by activity and exposure to heat and stress. 11. Macronutrients vs Micronutrients Macronutrients: -Are fats, proteins and carbohydrates. -Are main sources of calories in the diet. -Purpose is to deliver energy and important material to ensure the entire body composition. -They have the potential to alter cognitive function by exerting effects on neuronal cell structure, neurotransmission, energy supply to the brain and metabolism. • Carbs: found in plants and in milk. Main source of energy for the body. Recommend no less than 130 grams per day. • Protein: found in animals and plant products. Broken down into amino acids during digestion. Recommend 46 grams daily in adult woman and 56 grams daily in adult men. • Fat: Present in fatty fish, animal, and plant products. Classified as saturated trans, monounsaturated, and polyunsaturated. Recommended intake is 20-35% of daily total calories. Micronutrients: -Vitamins, minerals (elements), and electrolytes. -Stored in very small (micro) amounts in the body. -Are not a source of energy..BUT are essential for growth, development, and hundreds of metabolic processes that occur in the body daily. -Vitamin D, Vitamin K, and biotin are metabolized by the body. Other minerals and vitamins are not. 12. Significance of a food diary -Tracks meals, snacks and beverages -Provides retrospective view of an individual’s eating habits and dietary intake. -Tracks what you eat and drink -Can keep you focused on your diet, provide motivation, increase your efficacy, and help maintain goals. 13. BMI measurements for normal, overweight, obesity, morbid obesity Undernutrition- under 18.5 Normal: 18.5-24.9 Overweight: 25-29.9 Obese: 30-39.9 Extremely obese: 40 and higher 14. Pernicious Anemia Pernicious Anemia: the body can’t make enough healthy RBC because it doesn’t have enough b12. Can’t absorb the b12 because of the lack of intrinsic factor, which is a protein made in the stomach. 15. Examination techniques and equipment Inspection • Inspection is the process of observation it continues through the history taking process and during the physical examination. Pay attention to detail and note your findings. •Observe critically. Do not let modesty stop you from inspecting what is necessary. Palpation • Palpation is the use of your hands and fingers to gather information through the sense of touch (be gently and use warm hands). • Palmar surfaces of fingers and finger pads are more sensitive than the finger tips *use for discriminatory touch: determining position, texture, size, consistency, masses, fluid , and crepitus • Ulnar Surface of the hands and fingers *most sensitive for distinguishing vibration • Dorsal surface of the hands *best for determining temperature Percussion (must be performed against bare skin) • Percussion involves striking one object against another to produce vibration and subsequent sound waves. *The density of the medium through which the sound waves travel determines the degree of percussion tone. The more dense the medium, the quitter the percussion tone. •The percussion tone over air is loud, over fluid less loud, and over solid areas soft. (See table 3-3, pg 35, Ball) *Proceed with percussion from areas of resonance to areas of dullness *Immediate/Direct percussion: strike the finger or hand directly against the body *Mediate/Indirect percussion: Place the distal phalanx of the middle finger firmly on the body surface with the other fingers slightly elevated off the surface. Snap the wrist of your other hand downward, and with the tip of the middle finger, sharply tap the interphalangeal joint of the finger that is on the body surface (see figure 3-1, pg 35, Ball). *Use your fist to percuss to elicit tenderness arising from liver, gallbladder, or kidneys. Use the ulnar aspect of the fist to deliver a firm blow to the area. Auscultation • Auscultation involves listening to sounds produced by the body. *Sounds you hear with or without a stethoscope *Quiet environment, place stethoscope on naked skin *listen for characteristics of the sound: intensity, pitch, duration, and quality *Auscultation should be carried out last, except the abdominal examination. 16. Diagnostic Assessment tools and tests to include tuning forks, BP monitoring, use of stethoscope, otoscope, ophthalmoscope Tuning Forks • Used for screening tests in auditory function and for vibratory sensation or as part of the neurologic examination. As tuning forks are activated, vibrations are created that produce a particular frequency of sound wave, expressed as cycles per second (cps) or Hertz (Hz). Thus, a fork of 512 Hz vibrates at 512 cycles per second. • For auditory evaluation use a fork with a frequency of 500-1000 Hz, as it estimates hearing loss in the range of normal speech, approximately 300 to 3000 Hz. • Activate the fork by gently squeezing and stroking the prongs or by tapping them against the knuckles of our hand so that they ring softly-you must hold by the handle. • For vibratory sensation use a for of lower frequency with greatest sensitivity to vibration occurs when the fork is vibrating between 100-400 Hz. Activate the tuning fork by tapping it against the heel of your hand, then apply the base of the fork to a bony prominence. The patient feels the vibration as a buzzing or tingling sensation. BP monitoring • Measured indirectly with a stethoscope and either an aneroid or mercury sphygmomanometer. The electronic sphygmomanometers senses vibrations and converts them into electric impulses. The impulses are transmitted to a device that translates them into a digital readout, also capable of measuring pulse rate simultaneously. Stethoscope (3 kinds) 1. Acoustic Stethoscope: *Diaphragm has natural frequency of around 300 Hz and screens OUT low-pitched sounds and BEST transmits high-pitched sounds like the second heart sound. *Bell end piece has a natural frequency which varies with amount of pressure exerted. It transmits low-pitched sounds when very light pressure is used and with firm pressure, the skin converts it to a diaphragm end piece. *Stereophonic is a type of acoustic stethoscope which differentiates between the right and left auscultatory sounds using a two-channel design. 2. Magnetic Stethoscope: *Single end piece is the diaphragm, contains an iron disk on the interior surface behind this is a permanent magnet and a strong spring keeps the diaphragm bowed outward when it is not compressed against a body surface. Compression of the diaphragm activates the air column as magnetic attraction is established between the iron and the magnet, rotations of a dial adjusts for high, low, and full-frequency sounds. 3. Electronic Stethoscope: *Picks up vibrations transmitted to the surface of the body and converts them into electrical impulses. The impulses are amplified and transmitted to a speaker, where they are reconverted to sound. Newer devices have extended listening ranges, digital readout, sound recording and storage, playback, and electronic device linkage. Otoscope • Provides illumination for examining the external auditory canal and the tympanic membrane. An attached speculum narrows and directs the beam of light. Select the larges size of speculum that will fit comfortably into the patient’s ear canal. • Can be used for nasal examination if nasal speculum not available. • The pneumatic attachment for the otoscope is used to evaluate the fluctuating capacity of the tympanic membrane. Ophthalmoscope • The ophthalmoscope has a system of lenses and mirrors that enables visualization of the interior structures of the eye. The instrument has a light source that projects through various apertures while you focus on the inner eye. The large aperture, the one used most often, produces a large round beam. The various apertures are selected by rotating aperture selection dial. • The lenses in varying powers of magnification are used to bring the structure under examination into focus by converging or diverging light. An illuminating lens indicator displays the lens number positioned in the viewing aperture. The number correspond to the magnification power of the lens. The positive numbers are shown in black with the negative numbers are shown in red (just remember when your negative $ you’re in the red). The system of plus and minus lenses can compensate for myopia or hyperopia in both the examiner and the patient, there is no compensation for astigmatism. • PanOptic Ophthalmoscope: The panoramic ophthalmoscope head uses an optimal design that allows a larger field of view and increases magnification. Fundus view is 5 times larger than a standard ophthalmoscope. • StrabismoScope: Used for detecting strabismus (eye misalignment) and can be used as part of eye testing in children. *Instruct the child to focus on an accommodative target, such as the wall poster that comes with the instrument. Turn on the StrabismoScope and place it over the patient’s eye. Because of a one-way mirror, you are able to see in but the patient is not able to see out. As a result, subtle eye movements associated with strabismus are more easily detected. With the StrabismoScope in place, watch for movement in both the covered and uncovered eye. Repeat with the other eye. Assessment of the Skin, Hair, and Nails 17. Skin lesion characteristics Skin lesion can describe any pathologic skin changes and can be primary or secondary. Characteristics • Size • Shape • Color • Texture • Elevation or depression • Attachment at base: pedunculated (having a stalk) or sessile (without a stalk) • Exudates • Color • Odor • Amount • Consistency • Configuration • Annular (rings) • Grouped • Linear • Arciform (bow-shaped) • Diffuse • Location and distribution • Generalized or localized • Region of the body • Patterns • Discrete or confluent 18. Documenting skin lesions using “ABCD” rule ABCDE Changes in Moles • A = Asymmetry of lesion. Divide the lesion in ½ with each side not lining up evenly • B = Borders. The edges of the lesions are irregular, blurry, notched and pigment may overlap the edges of the lesion • C = Color. The color of the lesion may have varying shades of brown or black sometimes patchy red, white or blue throughout • D = Diameter. The diameter is less than the size of a pencil eraser or is growing larger in size • E = Evolution. Existing lesions begin a process of change in pigmentation especially evolving in a nonuniform manner 19. Anatomy and physiology of skin layers (pg 114- Physiologic processes of the Skin: • Functions: o Protect from invasion and trauma o Restrict body fluid loss by providing a mechanical barrier o Regulate Body: radiation, conduction, convection, and evaporation o Sensory Perception via nerves and receptors o Produce Vit D o Contribute BP regulation through constriction of skin blood vessels o Repair surface wounds by exaggerating the normal process of cell replacement o Excrete sweat, urea, & lactic acid o Express Emotions • Anatomy o Epidermis: Outer Most layer (made of 2 layers) ▪ Stratum Corneum (protects, restricts H20 loss) • Dead squamous cells that Contain waterproofing protein keratin ▪ Cellular Stratum: keratin cells are synthesized here in the deepest layer called the stratum germinativum (also where melanocytes (gives skin color) are • Additional sublayer of cellular stratum: stratum lucidum (only in the thicker skin of the palms and soles o Dermis: vascular connective tissue layer, that supports and separates the epidermis from the cutaneous adipose tissue ▪ Sensory nerve fibers: pain, touch, and temp felt ▪ Autonomic motor nerves: innervate blood vessels, glands, and the arrectores pilorum muscles ▪ Elastin, collagen, and reticulum fibers o Hypodermis: connects the dermis to underlying organs, it’s the subQ layer that consists of loose connective tissue filled with fatty cells. ▪ Adipose layer: generates heat and provides insulation, shock absorption, and reserve of calories 20. Abnormal nail findings in older adults Nail changes associated with aging are common in the elderly and include characteristic modifications of color, contour, growth, surface, thickness, and histology. The calcium content of the aging nail increases and iron decreases. • Keratinocytes of the nail plate are increased in size with an increased number of ‘pertinax bodies’ (remnants of keratinocyte nuclei) • nail bed dermis also shows thickening of the blood vessels and elastic tissue, especially beneath the pink part of the nail. • Nail growth decreases by approximately 0.5% per year between 20 and 100 years of age. • Prominent longitudinal ridges were the most common change • Brittleness of the nail is a common condition related to aging. • Onychauxis which is an age-associated thickening of the nail plate • changes in nail contour, increased transverse curvature https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2965930/ • White banding (Terry Nails) is a nail disorder that is specifically linked to age – p. 158. Pathophysiology: associated with cirrhosis, CHF, adult-onset diabetes mellitus, and age. Appearance: transverse white bands cover the nail except for narrow zone at the distal tip • Onychomycosis is a fungal infection that causes the nail plate to crumble – p. 156. Pathophysiology: this is not specifically related to older adults but is associated with loss of manual dexterity (interfere with exercise or walking). Appearance: distal nail plate turns yellow or white as hyperkeratotic debris accumulates, causing the nail to separate from the nail bed 21. Psoriatic skin lesions • Discrete, polycyclic, regional, erythematous or salmon in color, considered a plaque. (Pg. 147 or 126) 22. Vesicular skin characteristics • Small fluid filled sacs (fluid can be clear, white, yellow or mixed with blood). AKA as a blister or bullae. Conditions that cause vesicular skin characteristics > boils,burns,frostbite, staph infections, skin nodules, neurofibromas, or tumors that develop on the nerves, infected hair follicles. 23. Normal vs abnormal hair distribution during aging Normal • The quality and distribution of hair vary according to individual genetic makeup. • Hair is commonly present on the scalp, lower face, neck, nares, ears, chest, axillae, back and shoulders, arms, legs, toes, pubic area, and around the nipples. • Color will vary from very light blond to black to gray and may show alterations with rinses, dyes, or permanents. • Hair shedding is common and considered part of the normal hair cycle that changes with internal and external factors. Abnormal • Hair loss to the extremities may indicate poor circulation or nutritional deficient. • Look for any inflammation or scarring that accompanies hair loss, particularly localized. Diffuse hair loss usually occurs without inflammation and scarring. Scarring is helpful with diagnosis. Aging & Hair Changes • Hair color change. This is one of the clearest signs of aging. Hair color is due to a pigment called melanin, which hair follicles produce. Follicles are structures in the skin that make and grow hair. With aging, the follicles make less melanin, and this causes gray hair. Graying often begins in the 30s. Scalp hair often starts graying at the temples and extends to the top of the scalp. Hair color becomes lighter, eventually turning white. Body and facial hair also turn gray, but most often, this happens later than scalp hair. Hair in the armpit, chest, and pubic area may gray less or not at all. Graying is largely determined by your genes. Gray hair tends to occur earlier in white people and later in Asians. Nutritional supplements, vitamins, and other products will not stop or decrease the rate of graying. • Hair thickness change. Hair is made of many protein strands. A single hair has a normal life between 2 and 7 years. That hair then falls out and is replaced with a new hair. How much hair you have on your body and head is also determined by your genes. Nearly everyone has some hair loss with aging. The rate of hair growth also slows. Hair strands become smaller and have less pigment. So the thick, coarse hair of a young adult eventually becomes thin, fine, light-colored hair. Many hair follicles stop producing new hairs. Men may start showing signs of baldness by the time they are 30 years old. Many men are nearly bald by age 60. A type of baldness related to the male hormone testosterone is called male-pattern baldness. Hair loss may be at the temples or at the top of the head. Women can develop a similar type of baldness as they age. This is called female-pattern baldness. Hair becomes less dense and the scalp may become visible. As you age, your body and face also lose hair. Women's remaining facial hair may get coarser, most often on the chin and around the lips. Men may grow longer and coarser eyebrow, ear, and nose hair. 24. Characteristics of hair distribution 1) Palpate hair for texture while simultaneously inspecting color, distribution, and quantity a. Note- coarse, fine, curly, straight b. Note- shiny, smooth, resilient 2) Palpate scalp for dryness and brittleness a. Could indicate a systemic disorder 3) Color of hair a. Light blonde – gray b. Note- rinse, dyes, or permanents 4) Quantity and distribution of hair vary depending on genetic makeup a. Hair is present on scalp, lower face, neck, nares, ears, chest, axillae, back, shoulders, arms, legs, toes, pubic area, around nipples i. Fine vellus hair = body ii. Coarse terminal hair = scalp, pubic, axillae, arms, legs, beards b. Note hair loss i. Poor circulation vs nutritional deficit ii. Assess for inflammation or scarring (particularly localized) iii. Note whether hair shafts are broken off or absent 5) Genetically predisposed men = gradual, symmetric hair loss on scalp during adulthood a. Response to androgens 6) Asymmetric hair loss = ?pathologic condition 7) Women in 20s and 30s can develop adrenal androgenic alopecia a. Gradual loss of hair from central scalp 8) Male pubic hair configuration – upright triangle, extends midline to umbilicus 9) Female pubic hair configuration – inverted triangle, may extend midline to umbilicus 10) Assess for hirsutism in women (growth of terminal hair in a male distribution pattern on face, body, pubic) a. Hirsutism may be a sign of an endocrine disorder Assessment of Head, Neck, Eyes, Ears, Nose, and Throat 25. Cranial Nerves associated with the HEENT system • God gave you 1 nose (Olfactory) and 2 eyes (Optic). Nerves 3,4, and 6 make your eyes do tricks (3 Occularmotar, 4 Trochlear, and 6 Abducens). FIVE rhymes with TRI (5 Trigeminal). 7 is like an "F" backwards (F for Facial). 8 looks like earrings (8 Vestibulocochlear (Auditory)). "9 and10, under my chin" (IX Glossopharyngeal (Swallowing, saliva, taste), X Vagus (Control of PNS e.g. smooth muscles of GI tract) (just check gag reflex), 12 for swallowing (XII Hypoglossal (Tongue muscles - speech & swallowing)), and the number 11 looks like the neck (XI Accessory (Moving head & shoulders). • In the pic of the face attached, each part of the number 5 the crosses the face (3 lines) corresponds with the first, second, and third segments of the Trigeminal nerve (Forhead, maxila and mandible). • Here is a quick, meat and potatoes crainial nerve assessment video that is to point: https://www.youtube.com/watch?v=t5dolQ-Pzdw As the video suggests, the 1st crainial nerve is not tested during routine exam, but you could blindfold the patient and hold coffee, alchohol, etc under the nose and test like you would a taste for sugar and salt. Now, to remember the order, a "clean" acronym for remembering the crainial nerve order would be, "Oh Oh Oh To Touch And Feel Very Good Velvet, Such Heaven." Take the first letter of this acronym for the order of the nerves. There is another acronym that helps you determine whether the nerve is sensory, motor, or both. This acronym is, "Some Say Marry Money But My Brother Says Big Brains Matter Most." Where S=Sensory, M=Motor, and B=Both. I. Olfactory Smell, sensory II. Optic Vision, sensory III. Oculomotor Pupil, motor IV. Trochlear Lateral/inferior eye movement, motor V. Trigeminal Face feeling, chewing, sensory/motor VI. Abducent Lateral eye movement, motor VII. Facial Expressions (motor), taste (sensory) VIII. Vestibulocochlear Hearing and balance, sensory IX. Glossopharyngeal Swallowing (motor), taste (posterior/sensory) X. Vagus Heart, dig, respiratory (motor) / respiratory, voice, dig, (sensory) XI. Spinal Accessory Sternocleidomastoid, trapezius (motor) XII. Hypoglossal Muscle of tongue (motor) No automatic alt text available. No automatic alt text available. 26. Normal assessment findings of an adolescent’s nose and throat Assessment findings of adolescent’s nose and throat are pretty much the same as an adult. What makes them interesting and likely a test question is that the frontal sinus is not fully developed until adulthood and the sphenoid sinus develops during adolescence. It is not present for younger children. Here are some normal assessment findings in the nose and throat of adults. Throat • Tonsils, graded 1-4 depending on size, color and presence of exudate should be noted, tonsils should be symmetric • The mouth is separated from the oropharynx by tonsillar pillars • Soft palate should move symmetrically otherwise this indicates lesions on cranial nerves IX or X Normal assessment would read like this, clear without erythema, tonsils 1+ without exudate, Uvula rises evenly and gag reflex is intact, no hoarseness Nose • Nasal septum divides nose into two anterior cavities • Turbinates form the lateral wall of the nose there are three pairs, inferior, superior, and middle • Assessment should look for redness, swelling, or bleeding, nostrils should be patent Normal assessment – No discharge or polyps, mucosa pink and moist, septum midline, patent bilaterally. No edema over frontal or maxillary sinuses, no sinus tenderness to palpation 27. Normal examination findings of an infant’s fontanelles • Anterior fontanel (soft spot)- the junction where the frontal and parietal bones meet, described as a 5cm diamond shape. They remain soft up to 12 months to 15 months • Posterior fontanel- the junction of the parietal and the occipital bones. Closes before the anterior fontanelle during the first several months of life (around 6ths) • The third fontanel (mastoid)-located between anterior and posterior fontanelles common in infants with down syndrome • Depressed fontanelles are due to dehydration; bulging fontanelles are due to increased intracranial pressure, hemorrhage, infection or tumor • Large flat and soft fontanels are caused by hydrocephaly, hypothyroidism, or malnutrition • Palpable ridges indicate skull fractures 28. Examination findings of a patient with hypothyroid and hyperthyroid Hypothyroid • Weight gain • Constipation • Fatigue • Cold intolerance • Normal size thyroid, goiter or nodules Hyperthyroid • Weight loss • Tachycardia • Diarrhea • Heat sensitivity • Fine hair, bridle nails, proptosis. • Normal size thyroid, goiter or nodules 29. Techniques for examining the HEENT systems • Before the exam, gather all the necessary equipment: Tape measure (primarily for infants), stethoscope, cup of water, an otoscope with a pneumatic attachment, nasal sepeculum, tongue blades, tuning fork, Snellen chart or Lea Cards, Rosenbaum or Jaeger near vision card, gauze, gloves, penlight or similar, cotton wisps, and vials with different odors. • Review with patient: chief complaint, history of present illness, past medical history, family history, and personal/social history. • Physical exam with explanation of patient what you'll be doing 2 Options for physical exam review: 1. Des Moines University's PDF (condensed version) 2. Seidel's Guide to Physical Examination (8th ed.) -Head & Neck (p. 184) -Eyes (p. 204) -Ears, Nose, Throat (p.231) **Or Seidel's Printable Exam Summaries** 30. Examination findings for a patient with sinus symptoms (See "Health Assessment Midterm Study Guide 30 and 33" in Files for full info & sample questions) • Skin colour and texture and scars or wounds should be assessed. • Nasal deformities of the dorsum, tip or columellae may indicate internal alterations. • Unilateral rhinorrhea would indicate a choanal atresia or a foreign body in the nostril. Anterior Rhinoscopy • Rhinoscopy allows examination of the nasal vestibulum, septum, inferior turbinate and meatus and the floor of the nasal cavity. • Vasoconstrictor sprays or topical anaesthetics with epinephrine can be used in selected patients. • Small children are better examined in the supine position, with the examiner holding the head with one hand while an assistant immobilises the child. 1. The appearance of the mucosa (e. g. colour, humidity) 2. The situation and deformities of the nasal septum 3. Characteristics of nasal secretions (e. g. type, appearance, localization) 4. Turbinate congestion and meatal patency 5. Presence of tumours, foreign bodies or nasal polyps 6. Bleeding points Posterior Rhinoscopy • The posterior part of the nasal cavity are the choanae, tail of the turbinates, posterior end of the septum, rhinopharynx and torus tubarius. • What is needed to examine the posterior nasal cavity? A headlight, a small laryngeal mirror and a tongue depressor. • What to look for: 1. The size and shape of the choanae 2. Blockage of the nasopharynx, e. g. tumours, adenoid hypertrophy, polyps, cysts, angiofibromas, etc. 3. Nasal secretions: type, appearance 4. Size and shape of the tails of inferior and middle turbinates 5. Morphology of the torus tubarius and Rossenmüller’s fossae • Sinusitis is a common inflammation of the paranasal sinuses, the cavities that produce the mucus necessary for the nasal passages to work effectively. • Sinusitis can be caused by viruses, bacteria, fungi, allergies, or even an autoimmune reaction. • People have four pairs of sinuses, hollow spaces behind the bones of the face. • Chronic sinusitis can lasts more than 12 weeks. • Acute sinusitis is a temporary infection of the sinuses often associated with a cold. • Fever is more associated with acute sinusitis. • Chronic rhinosinusitis, this condition interferes with drainage and causes mucus buildup. • Chronic sinusitis can be brought on by an infection, by growths in the sinuses (nasal polyps) or by a deviated nasal septum. Primary signs and symptoms of chronic sinusitis: • Thick, discolored discharge from the nose or drainage down the back of the throat (postnasal drainage) • Nasal obstruction or congestion, causing difficulty breathing through your nose • Pain, tenderness and swelling around your eyes, cheeks, nose or forehead • Reduced sense of smell and taste in adults or cough in children Continued or untreated chronic rhinosinusitis are: • Ear pain • Aching in your upper jaw and teeth • Cough that might worsen at night • Sore throat • Bad breath (halitosis) • Fatigue or irritability • Nausea Steps to reduce risk of getting chronic sinusitis: • Avoid upper respiratory infections. • Manage your allergies. • Avoid cigarette smoke and polluted air. • Use a humidifier. • Chronic sinusitis is not usually bacterial in nature. • Functional endoscopic sinus surgery (FESS) is the main procedure used for treatment of sinuses. • A septoplasty will be used to straighten out this bone and cartilage a deviated septum is causing as a result of recurrent infections. 31. Appropriate tuning fork frequencies to approximate vocal frequencies Appropriate tuning fork frequencies to approximate vocal frequencies Normal speech has a range of 300 to 3000 Hz; therefore, the 500- to 1000-Hz fork is most often used because it can estimate hearing loss in the range of normal speech 32. Examining the oral mucosa The oral mucosa is examined using a tongue blade and bright light. The oral mucosa is expected to be pinkish red, smooth and moist. The Stensen duct is expected to be whitish-yellow or whitish-pink and produce a small amount of saliva. Possible abnormalities include: • Small stones or exudate from the Stensen duct. • Fordyce spots – small yellow-white ectopic sebaceous glands on the buccal mucosa and lips. • Parotitis – red spots on the Stensen duct. • Aphthous ulcers – white round or oval ulcerative lesions with a red halo. • Leukoplakia – white patch lesion that cannot be wiped away. 33. Hearing loss findings when examining the elderly patient (See "Health Assessment Midterm Study Guide 30 and 33" in Files for full info & sample questions) • Hearing loss is a sudden or gradual decrease in how well you can hear. • Earring loss is one of the most common conditions affecting older and elderly adults. • Hearing depends on a series of events that change sound waves in the air into electrical signals. Your auditory nerve then carries these signals to your brain through a complex series of steps. 1. Sound waves enter the outer ear and travel through a narrow passageway called the ear canal, which leads to the eardrum. 2. The eardrum vibrates from the incoming sound waves and sends these vibrations to three tiny bones in the middle ear. These bones are called the malleus, incus, and stapes. 3. The bones in the middle ear couple the sound vibrations from the air to fluid vibrations in the cochlea of the inner ear, which is shaped like a snail and filled with fluid. An elastic partition runs from the beginning to the end of the cochlea, splitting it into an upper and lower part. This partition is called the basilar membrane because it serves as the base, or ground floor, on which key hearing structures sit. 4. Once the vibrations cause the fluid inside the cochlea to ripple, a traveling wave forms along the basilar membrane. Hair cells-sensory cells sitting on top of the basilar membrane-ride the wave. 5. As the hair cells move up and down, microscopic hair-like projections (known as stereocilia) that perch on top of the hair cells bump against an overlying structure and bend. Bending causes pore-like channels, which are at the tips of the stereocilia, to open up. When that happens, chemicals rush into the cells, creating an electrical signal. 6. The auditory nerve carries this electrical signal to the brain, which turns it into a sound that we recognize and understand. • Men usually experience greater hearing loss and have earlier onset compared with women. • The most common type is age-related hearing loss; however, many conditions can interfere with the conduction of sound vibrations to the inner ear and their conversion to electrical impulses for conduction to the brain. • Examination of the auditory canal and tympanic membrane can identify causes of conductive hearing loss. • Audiometric testing is required to confirm hearing loss. • Major barriers to improved hearing in older adults include lack of recognition of hearing loss; perception that hearing loss is a normal part of aging or is not amenable to treatment; and patient nonadherence with hearing aids because of stigma, cost, inconvenience, disappointing initial results, or other factors. 34. Examination techniques used to examine the trachea and thyroid Please refer to pages in Siedel pp. 185-188, pp. 194-195, Hyper and Hypothyroidism (pp 200-201) and pg. 273 View video on YouTube demo: The Thyroid Exam (Stanford Medicine 25) on YouTube: https://www.youtube.com/watch?v=lmEus_ZDipg View Video: Thyroid Status Examination - OSCE Guide: https://www.youtube.com/watch? v=ziaYBkgEZNU View Video: Examination of the Trachea https://www.youtube.com/watch?v=RBVBnG35q04 Thyroid Anatomy: One gland two lobes, butterfly-shaped and joined by an isthmus at their lowest aspect (Seidel, p.185). Thyroid Gland that straddles the trachea in the middle of the neck. Secretes T4 and T3. Has two lobes. Thyroid is the largest endocrine gland in the body producing two hormones Thyroxine (T4) and Triiodothyronine (T3). Thyroid feels: Rubbery and easier to feel on a long slender neck What do you do if the thyroid is enlarged?: Listen over lateral lobes w/ bell and listen for thyroid bruit Inspect Neck for range of motion, strength, trachea, thyroid, and lymph nodes. Trachea: The trachea, colloquially called the windpipe, is a cartilaginous tube that connects the pharynx and larynx to the lungs, allowing the passage of air, and so is present in almost all air-breathing animals with lungs What techniques do you use to examine the neck? 1. inspection: inspect the neck in the usual anatomic position, in slight hyperextension as the patient swallows ( Seidel p. 193 see pictures). 2. palpation: palpate the trachea for midline position (Seidel p.192, see picture) 3. auscultation: when checking for bruits often noted in children and uncommon in neonates (Seidel p. 192). Refer to Website: https://depts.washington.edu/physdx/thyroid/tech.html Techniques: Thyroid Exam There are several physical examination maneuvers described for examination of the thyroid described below that are at least moderately sensitive and specific. Much of the exam is based on physiological reasoning and tradition rather than on studies of reliability or precision. Combining the examination and association signs and symptoms increases the accuracy of the physical examination of the thyroid. euthyroid, hypo- or hyperthyroid. Goiter: Examination of the thyroid for size Note: An enlarged thyroid is referred to as a goiter. There is no direct correlation between size and function- a person with a goiter can be A normal thyroid is estimated to be 10 grams with an upper limit of 20 grams or 2 to 4 teaspoons. Examination for goiter can increase the possibility of thyroid disease in patients with symptoms of hypo- or hyperthyroidism, in determining the choice of treatment in hyperthyroidism and monitoring the response to therapy directed at decreasing the size of the thyroid in cases of symptomatic goiter. The examination consists of three portions: • Inspection, • Palpation, and • Synthesis of data from these techniques In addition to palpating for size, also note the gland texture, mobility, tenderness and the presence of nodules. Inspection Inspection: Anterior Approach 1. The patient should be seated or standing in a comfortable position with the neck in a neutral or slightly extended position. 2. Cross-lighting increases shadows, improving the detection of masses. 3. To enhance visualization of the thyroid, you can: 1. Extending the neck, which stretches overlying tissues 2. Have the patient swallow a sip of water, watching for the upward movement of the thyroid gland. 4. 251KB video demo from Return to the Bedside Inspection: Lateral Approach 1. After completing anterior inspection of the thyroid, observe the neck from the side. 2. Estimate the smooth, straight contour from the cricoid cartilage to the suprasternal notch. 3. Measure any prominence beyond this imagined contour, using a ruler placed in the area of prominence. Palpation Note: There is no data comparing palpation using the anterior approach to the posterior approach so examiners should use the approach that they find most comfortable. Palpation: Anterior Approach 1. The patient is examined in the seated or standing position. 2. Attempt to locate the thyroid isthmus by palpating between the cricoid cartilage and the suprasternal notch. 3. Use one hand to slightly retract the sternocleidomastoid muscle while using the other to palpate the thyroid. 4. Have the patient swallow a sip of water as you palpate, feeling for the upward movement of the thyroid gland. 5. 454KB video demo from Return to the Bedside. Palpation: Posterior Approach 1. The patient is examined in the seated or standing position. 2. Standing behind the patient, attempt to locate the thyroid isthmus by palpating between the cricoid cartilage and the suprasternal notch. 3. Move your hands laterally to try to feel under the sternocleidomstoids for the fullness of the thyroid. 4. Have the patient swallow a sip of water as you palpate, feeling for the upward movement of the thyroid gland. Note: This traditional technique is based on physiological reasoning; data of effectiveness is lacking. Synthesis of data from these techniques Using the data from anterior and lateral inspection and from palpation, categorize the gland as: a. goiter ruled out [normal or small (1 to 2 times normal) with lateral prominence <2 mm ], b. goiter ruled in [large (& 2 times normal) or lateral prominence >2 mm] or c. inconclusive. See Evidence Base and Differential Diagnosis. Nodules: Examination of the thyroid for nodularity Thyroid nodules are common (prevalence 4%). Half of the thyroids glands examined by ultrasound or direct visualization (surgery or autopsy) have nodules. Physical examination detects approximately 10% of the nodules found by these methods. Nodules increase in frequency with age and are four times more likely in women than men. Less than 5% of all nodules are cancerous. Technique 1. The location of the thyroid is identified by inspection. 2. Using the anterior or posterior approach, palpate the thyroid to identify nodules 3. Note the size and number of nodules. 4. Note the consistency of the nodule. 5. Palpate regional lymph nodes for consistency and mobility. 6. Take a look at a teaching demo video. Assessment of the Abdomen and Gastrointestinal System 35. Organs involved in the alimentary tract • Also called the digestive tract, the alimentary tract is composed of the following hollow organs: the mouth, the esophagus, stomach, small intestines, large intestines, and the anus. The solid organs of the tract include the liver, pancreas, and gallbladder. 36. Correct assessment order for examining the abdomen • The correct assessment order for examining the abdomen is: 1) Inspect 2) Auscultate 3) Percuss 4) Palpate • Inspect the skin characteristics, contour, pulsations, and movement • Auscultate all 4 quadrants for bowel sounds. Auscultate the aorta and renal, iliac, and femoral arteries for bruits or venous hums. • Percuss all quadrants for tone. Percuss liver borders and estimate spans. Percuss left midaxillary line for splenic dullness. • Lightly palpate quadrants x4. Deeply palpate quadrants x4. Palpate right costal margin for liver border. palpate left costal margin for spleen. Palpate laterally at the flanks for left and right kidneys. • Palpate midline for aortic pulsation. Test abdominal reflexes. Finally, have the patient raise the head as you inspect the abdominal muscles. 37. Examination technique and findings of the liver • Inspection: skin of the abdomen should be the same color as the rest of the body. Abnormal findings include jaundice or cyanosis. • Percussion: Percussion is used to map the size and location of the liver. To measure the span of the liver, delineate the upper and lower borders by percussion of the right chest and abdomen in the midclavicular line, with breath‐holding and with breathing, as movement with respiration helps to confirm the dullness as hepatic and show whether the diaphragm can contract. Percussion of liver dullness in the midsternal line, where the finding that the span may be the same or greater than in the midclavicular line detects left lobe enlargement that is typical of cirrhosis, and which also may be felt as a firm mass in the epigastrium. • Palpation: The lower border of the liver is identified by palpating progressively upward from the right lower quadrant toward the right costal margin, from which the enlarging organ emerges; its uppermost surface/margin cannot be reached. The liver moves downwards with inspiration, its consistency, any irregularity of its edge, tenderness, and pulsatility. If right subcostal tenderness limits or arrests deep respiration, this is termed a positive Murphy sign of acute cholecystitis. A palpable structure below the right costal margin may simply be the normal variant tongue‐like inferior projection of the right or Riedel lobe of the liver. A globular subcostal mass may be gallbladder cancer, or painless gallbladder distension in the patient with jaundice caused by malignant biliary obstruction that is located below the insertion of the cystic duct (Courvoisier sign). On rare occasions, the gallbladder is palpable in acute cholecystitis, which is known as Cope sign. 38. Examination findings associated with appendicitis An accurate diagnosis of appendicitis is based on history and physical examination. • In adults with appendicitis: symptoms may present as right lower quadrant (RLQ) pain, initial periumbilical pain with migration to the RLQ, and the presence of pain before vomiting. Physical exam will reveal the presence of rigidity (a positive psoas sign), fever, and/or rebound tenderness. If patients do not present with these signs/symptoms, diagnosis of appendicitis is unlikely. "No finding effectively rules out appendicitis" (Ball et al., 2015, p. 390). • Usually pain characteristics: Initial periumbilical or epigastric; colickly; later becomes localized to RLQ, often at McBurney's point. Possible associated S/S: Guarding, tenderness; + iliopsoas and +obturator signs, RLQ skin hyperesthesia; anorexia, nausea, or vomiting after onset of pain; low-grade fever; + Aaron, Rovsing, Markle, and McBurney signs. [From Table 17-2 in Ball et al., p. 390, 2015] • In children with appendicitis: more helpful- vomiting, rebound tenderness, rectal tenderness, and fever. Less helpful- RLQ tenderness 39. Examining McBurney’s sign • McBurney's sign: Rebound tenderness and sharp pain when McBurney's point is palpated. A positive McBurney's sign is associated with appendicitis. (Ball, J. W., Dains, J. E., Flynn, J. A., Solomon, B. S., & Stewart, R. W. (2015). Seidel's guide to physical examination (8th ed.). St. Louis, MO: Elsevier Mosby) • The McBurney's point is the point over the right side of the abdomen that is one-third of the distance from the anterior superior iliac spine to the umbilicus. 40. Assessment of abdominal pain in women *Key Points • Auscultation should be done last when examining the abdomen • Example question found through Elsevier online: Your patient is complaining of acute, intense sharp epigastric pain that radiates to the back and left scapula with nausea and vomiting. Based on this history, your prioritized physical examination should be to: inspect for ecchymosis of the flank. • When assessing abdominal pain in college-aged women always ask when the first day of their last menstrual period was!!! • Before performing an abdominal exam have the patient empty their bladder! • After abdominal inspection then AUSCULTATE • Inspection of the abdomen should begin with the patient SUPINE Advanced Health Assessment and Clinical Diagnosis in Primary Care (Dains, Baumann, & Scheibel: Chapter 3 pg. 11 • Pg. 20: Perform a pelvic exam in women to rule out STI, PID, ovarian pain, ectopic pregnancy, and uterine fibroids. Cervical motion tenderness (CMT) is the hallmark of PID. • Pg. 28-32 table with common causes of acute abdominal pain Examples for women: 1. Ectopic Pregnancy: women of childbearing age, sudden onset of spotting and persistent cramping in lower quadrant that begins shortly after missed period. Physical findings: hemorrhage, shock, and lower abdominal peritoneal irritation, enlarged uterus, CMT, tender adnexal mass. (SURGICAL EMERGENCY) (Dains pg. 28) (Seidel pg. .391- Table 17.2) 2. Dysmenorrhea: typical premenstrual pain onset soon after menarche, gradually diminishes with age. Gynecology consult is needed with pelvic ultrasound. (pg. 30) 3. Uterine Fibroids: pain related to menses or intercourse. ( Physical Findings: Palpable myomas. Pelvic ultrasound is needed with gynecology consult (pg. 27, 31) 4. Ovarian Cyst: common with younger women. (pg. 27, 31) Physical Findings: adnexal pain and palpable ovarian cysts especially later in cycle 5. Cholecystitis: more common in women. Pain located in RUQ and radiates to right scapular area, dark urine, N/V, light stools, and may be aggravated by certain foods. (pg. 29) 6. Pelvic Inflammatory Disease (PID): common in women younger than 35 who are sexually active usually with more than one partner. Often caused by chlamydia trachomatis and Neisseria gonorrhoeae with onset occurring after menses. Patients present with lower abdominal pain that progressively becomes severe. Upon examination: tender abdomen, CMT, and adnexal tenderness. Patients may guard and have rebound tenderness, fever, irregular bleeding, vaginal discharge, and vomiting, WBC and ESR are usually elevated. (pg. 25) Causes of lower abdominal or pelvic pain • Lower abdominal or pelvic pain, refers to discomfort that occurs at or below your belly button. Most women will experience pain in the lower abdomen from time to time. More often than not this is due to menstruation. • The bladder and reproductive organs are often where pelvic pain occurs. In many cases it is difficult to diagnose the exact cause of the pain, but noting certain symptoms will help come to a diagnosis. The most common lower abdominal pain causes are: • A urinary disorder, such as bladder or kidney problems. • A bowel problem. • A problem with the reproductive system – the uterus, fallopian tubes and ovaries. Abdominal pain arising from the urinary system • Urine infections are common and present symptoms, such as burning when you pass urine and going to the toilet more often. • Infection can spread to the kidneys (pyelonephritis) and can make you feel unwell with a high temperature and back pain. • If you have pain that spreads from your back down to your groin and is severe – your doctor may be more concerned that you have kidney stones. The doctor will test your urine if you have any of the above symptoms. Abdominal pain arising from the digestive system • Pain arising from the large intestine is a particularly common cause of lower abdominal pain in both men and women. Features suggesting your pain may be to do with the bowel are: Pain associated with bowel movement • A change in bowel habit • Blood with bowel movement • Bloating • Both constipation and diarrhea can give you pain. The pain they are often associated with is described as crampy or 'colicky.' This means that it comes and goes in waves. Large bowel pain is characteristically relieved on opening the bowels. • Potential causes of pain arising from the bowel include irritable bowel syndrome (IBS), which can give you alternating diarrhea, constipation and bloating. • Other conditions include diverticular disease and its complications which are more frequent in older patients. Inflammatory bowel disease (ulcerative colitis or Crohn's). A rare but important diagnosis is colorectal cancer. • Bloating and swelling is also a common symptom that people report and can be due to a problem affecting the bowels. Abdominal pain arising from the reproductive organs • Pain can originate from your uterus (womb), fallopian tubes or ovaries. It's usually felt in the middle of the lower abdomen. • Pain that is felt more to the side can be more typical of a pain coming from the ovary. • Pain coming from the uterus is often worse during your period and is called dysmenorrhea. • Some conditions affecting the reproductive system can also cause pain during intercourse. This is called dyspareunia and it is important to let your doctor know if you are concerned. Examples of conditions of the reproductive organs include: • Endometriosis • Fibroids • Pelvic inflammatory disease • Ovarian cysts • Problems related to the early stage of pregnancy, such as a miscarriage or ectopic pregnancy. *Seek immediate medical assistance if your symptoms include a fever, vomiting blood, passing dark or bloody stools or acute and worsening pain. • Questions about a person's emotional life-family, home, work and sex life are appropriate. Further abdominal pain investigations • Depending on the exact symptoms and duration, referral to the appropriate specialist is often required. These may include: • Gynecological causes may require vaginal swabs, cervical smears or pelvic ultrasound examination. Ultrasound may also be performed from within the vagina. Specialized blood test for ovarian cancer, CA-125, are usually performed. More invasive tests will depend upon the doctor's suspicion of the cause of the pain. • Urinary causes can be investigated by urine culture, ultrasound or CT scan. • Colonic causes may require internal endoscopic examination of the bowel by Flexible Sigmoidoscopy or Colonoscopy. • A CT (Computerized Tomography Scan) may be appropriate for all three major sites of pain. 41. Landmarks for abdominal examination Anatomic correlates of Nine regions of abdomen. Seidel p. 378-379 Right Hypochondriac Epigastric Left hypochondriac Right lobe of liver Pylorus Stomach Gallbladder Duodenum Spleen Portion of duodenum Pancreas Tail of pancreas Hepatic flexure of colon Portion of the liver Splenic flexure of colon Portion of right kidney Upper pole of left kidney Right adrenal gland Left adrenal gland Right Lumbar UMBILICAL Left lumbar Ascending colon Omentum Descending colon Lower half of right kidney Mesentery Lower half of left kidney Portion of duodenum and jejunum Lower part of duodenum Portions of jejunum and ileum Jejunum and ileum Right Inguinal Hypogastric (pubic) Left inguinal Cecum Ileum Sigmoid colon Appendix Bladder Left ureter Lower end of ileum Uterus (if enlarged) Left spermatic cord Right ureter Left ovary Right spermatic cord Right ovary 42. Characteristics of bowel sounds heard during auscultation (Seidel p. 381) • Range from 5 to 35 per minute • Borborygmi: loud prolonged gurgles o Increased bowel sounds may occur with gastroenteritis, early intestinal obstruction, or hunger. • High-pitched tinkling suggest intestinal fluid or air under pressure (in early obstruction) • Decreased bowel sounds occur with peritonitis and paralytic ileus. *MUST auscultate in all four quadrants if there are any major concern and the absence of bowel sounds is the inability to hear ANY bowel sounds after 5 minutes of continuous listening; typically associated with abdominal pain and rigidity and is considered an EMERGENCY. [Show More]
Last updated: 1 year ago
Preview 1 out of 30 pages
Instant download

Buy this document to get the full access instantly
Instant Download Access after purchase
Add to cartInstant download
Reviews( 0 )
Document information
Connected school, study & course
About the document
Uploaded On
Apr 03, 2021
Number of pages
30
Written in
Additional information
This document has been written for:
Uploaded
Apr 03, 2021
Downloads
0
Views
24


.png)