Pharmacology > QUESTIONS & ANSWERS > NURS 531 PHARMACOTHERAPEUTICS NOTES; Module/Exam 2 DOWNLOAD TO GET A HIGH SCORE (All)
NURS 531 PHARMACOTHERAPEUTICS NOTES; Module/Exam 2 DOWNLOAD TO GET A HIGH SCORE
Document Content and Description Below
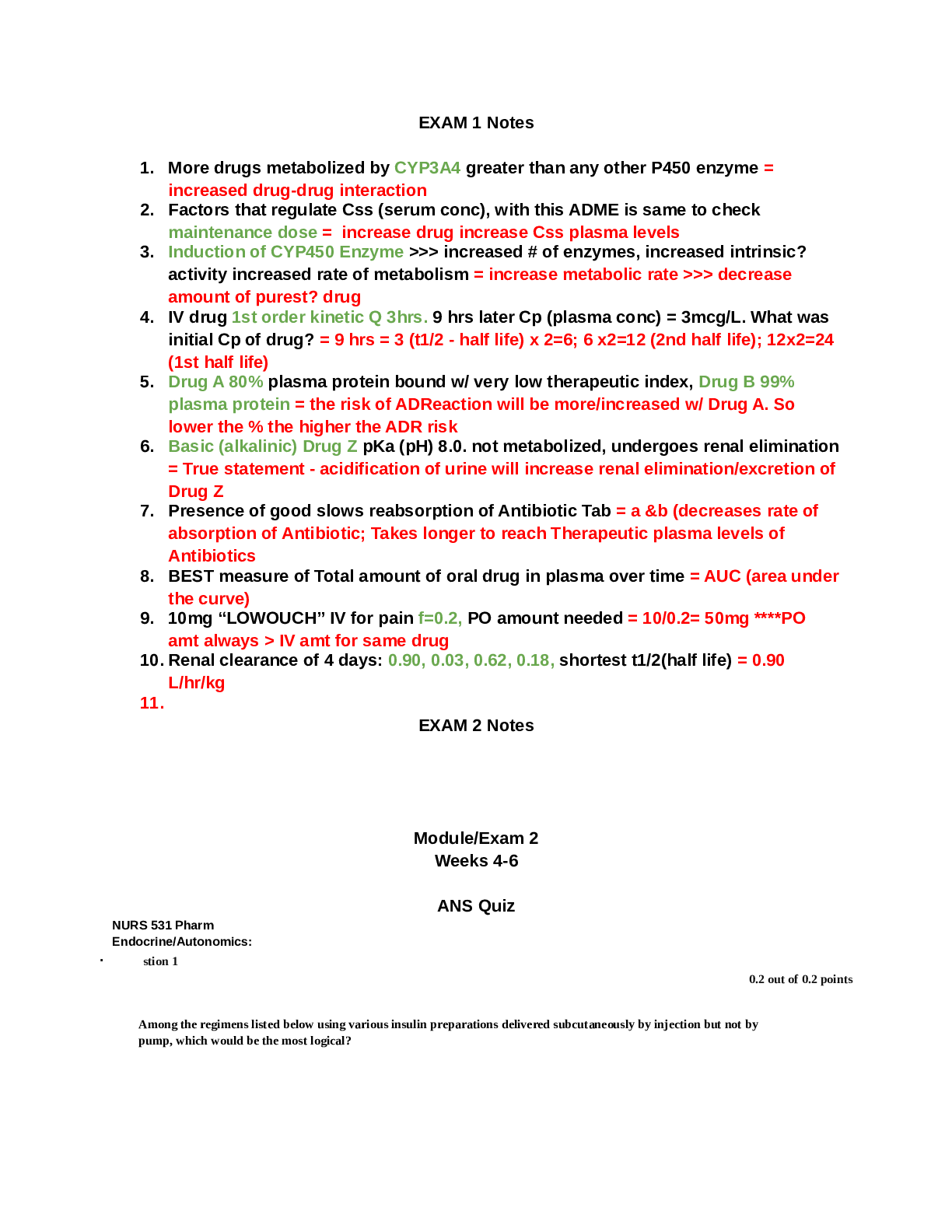
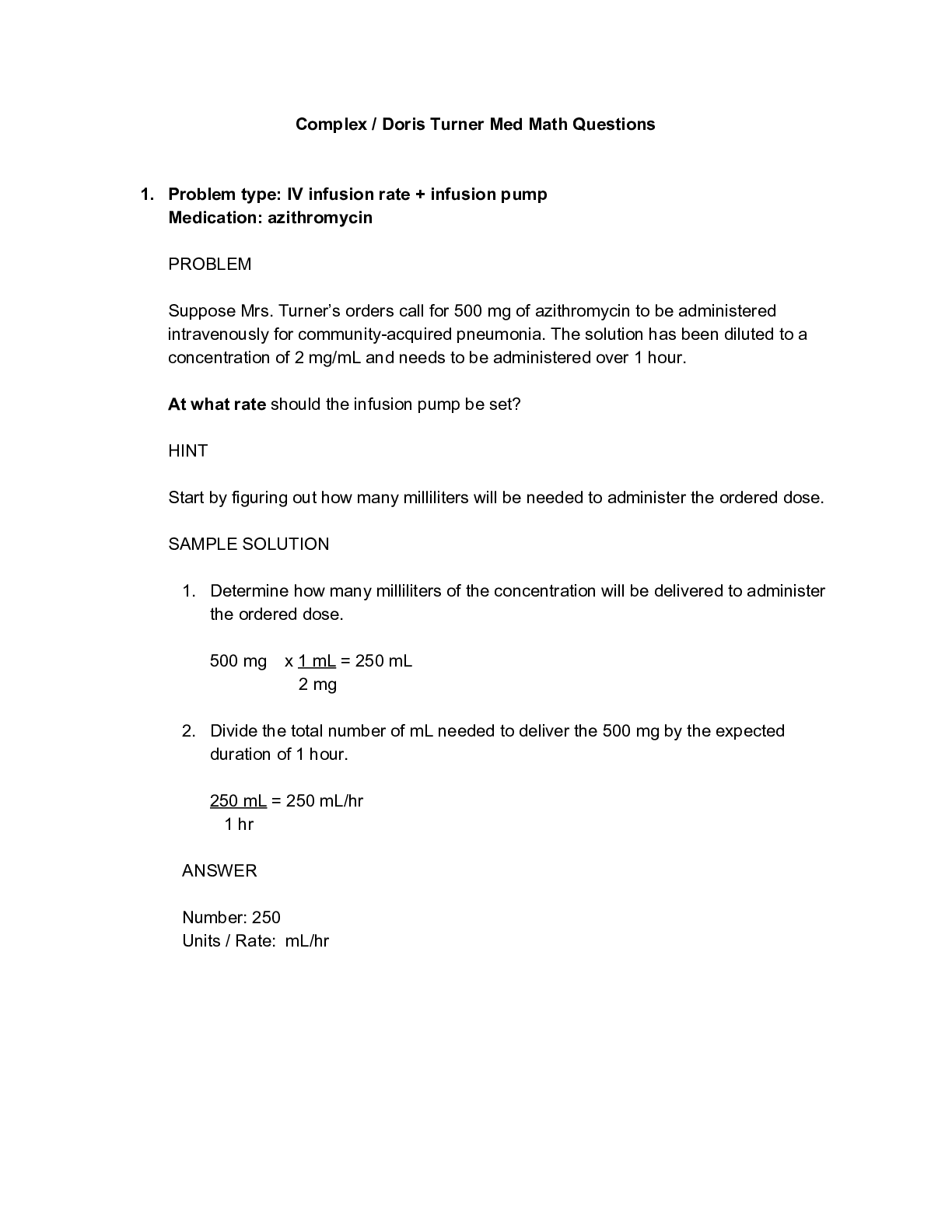
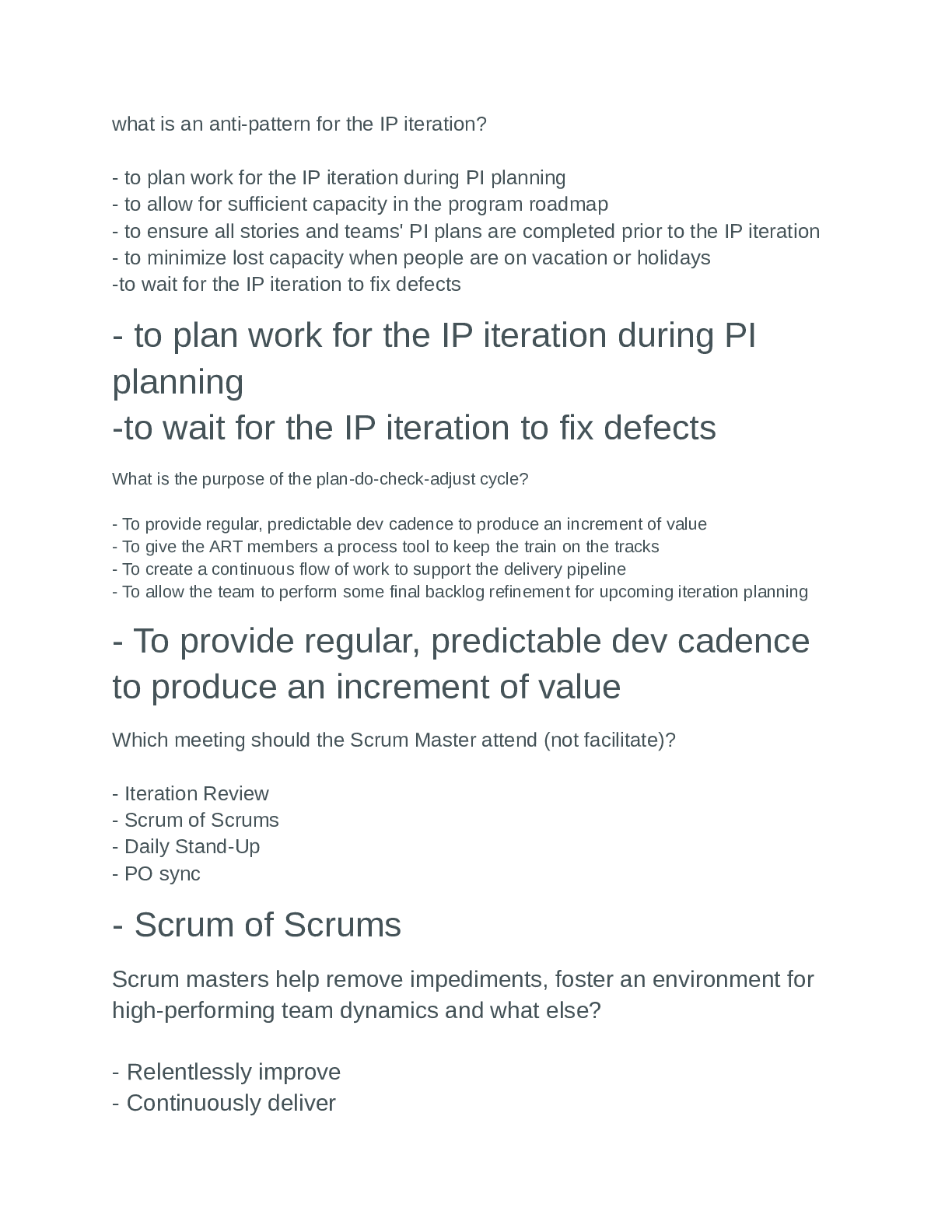
NURS 531EXAM 1 Notes 1. More drugs metabolized by CYP3A4 greater than any other P450 enzyme = increased drug-drug interaction 2. Factors that regulate Css (serum conc), with this ADME is same to c hec... k maintenance dose = increase drug increase Css plasma levels 3. Induction of CYP450 Enzyme > >> increased # of enzymes, increased intrinsic? activity increased rate of metabolism = increase metabolic rate >>> decrease amount of purest? drug 4. IV drug 1st order kinetic Q 3hrs. 9 hrs later Cp (plasma conc) = 3mcg/L. What was initial Cp of drug? = 9 hrs = 3 (t1/2 - half life) x 2=6; 6 x2=12 (2nd half life); 12x2=24 (1st half life) 5. Drug A 80% plasma protein bound w/ very low therapeutic index, Drug B 99% plasma protein = the risk of ADReaction will be more/increased w/ Drug A. So lower the % the higher the ADR risk 6. Basic (alkalinic) Drug Z pKa (pH) 8.0. not metabolized, undergoes renal elimination = True statement - acidification of urine will increase renal elimination/excretion of Drug Z 7. Presence of good slows reabsorption of Antibiotic Tab = a &b (decreases rate of absorption of Antibiotic; Takes longer to reach Therapeutic plasma levels of Antibiotics 8. BEST measure of Total amount of oral drug in plasma over time = AUC (area under the curve) 9. 10mg “LOWOUCH” IV for pain f=0.2, PO amount needed = 10/0.2= 50mg ****PO amt always > IV amt for same drug 10. Renal clearance of 4 days: 0.90, 0.03, 0.62, 0.18, shortest t1/2(half life) = 0.90 L/hr/kg 11. EXAM 2 Notes Module/Exam 2 Weeks 4-6 ANS Quiz NURS 531 Pharm Endocrine/Autonomics: · stion 1 0.2 out of 0.2 points Among the regimens listed below using various insulin preparations delivered subcutaneously by injection but not by pump, which would be the most logical? Selected Answer: b. Glargine to provide basal insulin coverage and aspart given before each meal. Answers: a. Lispro to provide basal insulin coverage and detimir given before each meal. b. Glargine to provide basal insulin coverage and aspart given before each meal. c. Detemir to provide basal insulin coverage and NPH insulin before each meal. d. Lispro or glargine injected every 3 hours and NPH given at bedtime. · Question 2 0.2 out of 0.2 points Mr. P self-medicates with an aluminum hydroxide antacid before every meal to reduce symptoms of hyperacidity. However he tends to overeat and drink. As a result, he ends up taking a couple of aspirin every day. Which of the following is likely to be TRUE with regard to Mr. P’s self-medication with these over-the-counter medications? Selected Answer: c. Mr. P. will experience reduced therapeutic effects from the antacid because he is not taking it at the optimal time. Answers: a. More aspirin will be absorbed in the presence of the antacid. b. Mr P. is likely to experience diarrhea. c. Mr. P. will experience reduced therapeutic effects from the antacid because he is not taking it at the optimal time. d. Mr. P. sometimes takes other types of antacids because one antacid is the same as another with regard to adverse effects. · Question 3 0.2 out of 0.2 points Which of the following statement(s) is/are TRUE about treatment of erectile dysfunction with a phosphodiesterase type 5 inhibitors? (Hint:You may choose more than one answer.) b. Phosphodiesterase type 5 inhibitors decrease the degradation of cyclicGMP. c. Among the phosphodiesterase type 5 inhibitors, tadalafil has the longest half-life. d. Use of phosphodiesterase type 5 inhibitors can result in visual disturbances and hypotension because these inhibitors are not absolutely selective for the phosphodiesterase type 5 isoform. Answers: a. Phosphodiesterase type 5 inhibitors stimulate nitric oxide synthase. b. Phosphodiesterase type 5 inhibitors decrease the degradation of cyclicGMP. c. Among the phosphodiesterase type 5 inhibitors, tadalafil has the longest half-life. d. Use of phosphodiesterase type 5 inhibitors can result in visual disturbances and hypotension because these inhibitors are not absolutely selective for the phosphodiesterase type 5 isoform. e. Only sildenafil can be taken with an organic nitrate. · Question 4 0.2 out of 0.2 points Anna is an APN is treating a 58 year-old postmenopausal patient for severe osteoporosis. Consider the following and select one answer. e. All of the above actions are incorrect. Answers: a. Anna prescribes 2 drugs. She prescribes alendronate and raloxifene because the mechanism of alendronate is anabolic and the mechanism of raloxifene is anti-resorptive. b. Anna suggests that her patient should eat a large meal before taking alendronate to reduce potential gastrointestinal side effects of the drug. c. Anna orders liver function test for 6 months and 12 months after initiating therapy to treat osteoporosis because bisphosphonates are metabolized in the liver where they form a reactive metabolite that can injure liver cells. d. Because bisphosphonates can cause hypercalcemia, Anna suggests that her patient should refrain from drinking milk or eating foods like yogurt and ice cream. e. All of the above actions are incorrect. · Question 5 0.2 out of 0.2 points Match the mechanism of action with the drug o Question Correct Match Selected Match Glyburide e. Stimulates insulin secretion by binding to beta-cell sulfonylurea receptor e. Stimulates insulin secretion by binding to beta-cell sulfonylurea receptor Pioglitazone a. Act as a PPAR-gamma agonists to reduce insulin resistance a. Act as a PPAR-gamma agonists to reduce insulin resistance Metformin d. Delays glucose absorption from gut, reduces gluconeogenesis, reduces glycogenolysis, facilitates insulin-mediated glucose utilization d. Delays glucose absorption from gut, reduces gluconeogenesis, reduces glycogenolysis, facilitates insulin-mediated glucose utilization Exenatide b. Synthetic GLP-1 mimetic - enhances glucose-dependent insulin secretion, suppresses inappropriately elevated serum glucose concentrations, and delays gastric emptying b. Synthetic GLP-1 mimetic - enhances glucose-dependent insulin secretion, suppresses inappropriately elevated serum glucose concentrations, and delays gastric emptying Acarbose c. Delays the absorption of glucose from the intestines by inhibiting glucosidase in the wall of the intestines c. Delays the absorption of glucose from the intestines by inhibiting glucosidase in the wall of the intestines o o All Answer Choices a. Act as a PPAR-gamma agonists to reduce insulin resistance b. Synthetic GLP-1 mimetic - enhances glucose-dependent insulin secretion, suppresses inappropriately elevated serum glucose concentrations, and delays gastric emptying c. Delays the absorption of glucose from the intestines by inhibiting glucosidase in the wall of the intestines d. Delays glucose absorption from gut, reduces gluconeogenesis, reduces glycogenolysis, facilitates insulin-mediated glucose utilization e. Stimulates insulin secretion by binding to beta-cell sulfonylurea receptor · Question 6 0.2 out of 0.2 points Which of the following statements are TRUE about histamine2-receptor antagonists in the treatment of hyperactivity and uncomplicated gastroesophageal reflux disease (GERD)? Selected Answer: c. For optimal response, H2 antagonists should be taken in the evening. Answers: a. Blocking the H2 receptor blocks the final common pathway of acid production in parietal cells. b. H2 receptor antagonists protect the stomach lining by increasing mucus production. c. For optimal response, H2 antagonists should be taken in the evening. d. Among the H2 antagonists, cimetidine has the least number of adverse effects. · Question 7 0.2 out of 0.2 points Which of the following statements is TRUE with regard the ideal anti-muscarinic drug to treating overactive bladder (OAB)? Selected Answer: d. The ideal anti-muscarinic drug would be highly selective for the M3 receptor and would not cross the blood brain barrier. Answers: a. The ideal anti-muscarinic drug would be highly selective for the M2 receptor subtype. b. The ideal anti-muscarinic drug would be a tertiary amine. c. The ideal drug already exists. Current anti-muscarinics on the market are very effective. d. The ideal anti-muscarinic drug would be highly selective for the M3 receptor and would not cross the blood brain barrier. · Question 8 0.2 out of 0.2 points Methimazole and propylthiouracil (PTU) are two drugs that are used to treat patients with Grave’s disease. What extra mechanism of action of PTU (compared to methimazole) explains the beneficial effects of PTU on patients who are experiencing severe hyperthyroidism or thyroid storm? Selected Answer: c. Only PTU inhibits conversion of T4 to T3 in periphery Answers: a. Only PTU inhibits peroxidase (oxidation of iodide to iodine) b. Only PTU inhibits coupling of iodine to tyrosine c. Only PTU inhibits conversion of T4 to T3 in periphery · Question 9 0.2 out of 0.2 points RANKL (receptor activator of nuclear factor KappaB ligand) is a cell-attached ligand that is important in regulating bone remodeling. Which of the following statement is TRUE about drugs used to treat osteoporosis by decreasing RANKL action? Selected Answers: a. Osteoblasts-associated RANKL binds to the RANK receptor on osteoclasts. Answers: a. Osteoblasts-associated RANKL binds to the RANK receptor on osteoclasts. b. Bisphosphonates act as a transcription factor to increase the expression of RANKL. c. r-OPG (recombinant osterprotegrin) and denosumab bind to RANK and inhibit maturation of osteoclasts and thereby inhibit degradation of bone. d. Based on the mechanism of action of denosumab, a predicted effect of this drug would be an increase in serum calcium · Question 10 0.2 out of 0.2 points Your patient is complaining that she has frequent spotting or break through bleeding since she started an oral contraceptive (OC). A common reason for this occurrence is related to: Selected Answer: taking an OC pill at different times. Answers: having multiple sexual partners. taking an OC pill at different times. the clinical and therapeutic efficacy of the drug. taking an OC pill with food. ANS Quiz module 2 · ion 1 0.2 out of 0.2 points Nerve pathways from the autonomic nervous system (ANS) normally have a preganglionic and a postganglionic fiber. Which of the following properties is characteristic of ONLY the parasympathetic nervous system (PNS) but not the sympathetic nervous system (SNS)? Selected Answer: c. Acetylcholine is the primary neurotransmitter at the postganglionic fiber. Answers: a. Acetylcholine is the neurotransmitter of the preganglionic fiber. b. ATP and neuropeptide Y are co-transmitters at the postganglionic fiber. c. Acetylcholine is the primary neurotransmitter at the postganglionic fiber. d. Stimulation mediates stress, fright, flight and fright. e. Innervation of the eye, heart and lungs. Response Feedback: a) Acetylcholine is the neurotransmitter at the ganglion of both the PNS and SNS. b) ATP and neuropeptide Y are co-transmitters at adrenergic nerve terminals in the SNS. Co-transmitters ofcholinergic nerves are nitric oxide and vasoactive intestinal peptide. c) Acetylcholine is the primary neurotransmitter of PNS postganglionic fibers. Norepinephrine is the primary neurotransmitter of the ANS postganglionic fiber. d) Stimulation of the SNS mediates stress, fright, flight and fight. PNS stimulation is usually associated with relaxing or moderating activity e) Both the PNS and the SNS innervate the eye, heart and lungs. · Question 2 0.2 out of 0.2 points What would be the outcome of blocking depolarization-induced influx of calcium through calcium channels in a preganglionic nerve terminal of the parasympathetic or sympathetic nervous system? Selected Answer: b. Release of neurotransmitter from the nerve terminal would be inhibited. Answers: a. Uptake of neurotransmitter from the synapse would be inhibited. b. Release of neurotransmitter from the nerve terminal would be inhibited. c. Synthesis of neurotransmitter in the nerve terminal would be inhibited. d. Binding of the neurotransmitter on the target cell/organ receptor would be facilitated. e. Neurotransmitter would be released from the presynaptic terminal by exocytosis. Response Feedback: a) Uptake may require ions to facilitate uptake but calcium is not one of the ions. * Note that inhibited does not necessarily infer that a process is totally reduced to zero or ablated. It means that the process is reduced or decreased to a varying degree. b) Release of neurotransmitter would be inhibited because depolarization induced opening of calcium channels mediates calcium influx. The influx of calcium mediates fusion of vesicles containing neurotransmitter (NT) to the cell surface membrane and exocytosis of the NT into the synapse. Without the Ca influx the NT would not be released. c) Calcium is not involved in synthesis of neurotransmitter in these nerve terminals d) Decreased calcium influx into the presynaptic membrane would have no effect on target organ receptor binding. e) If the influx of calcium were interrupted exocytosis of neurotransmitter would be inhibited. · Question 3 0.2 out of 0.2 points Binding of acetylcholine to nicotinic receptors: Selected Answer: e. Results in the opening of sodium channels and the influx of sodium into the cell. Answers: a. Stimulates totally different signal transduction mechanisms at neuronal and skeletal muscle receptor sites b. Results in the inhibition of adenylate cyclase with subsequent decreased production of cAMP. c. Results in the activation of phospholipase C (PLC) with the subsequent production of inositol trisphosphate(IP3) and diacylglycerol (DAG). d. Leads to hyperpolarization of the cell membrane potential. e. Results in the opening of sodium channels and the influx of sodium into the cell. Response Feedback: a) Regardless of the location of the nicotinic receptor, binding of acetylcholine results in opening of sodium channels b) Neither activation or inhibition of adenylate cyclase is the signal transduction mechanism associated with nicotinic receptors. c) The contribution of PLC activation to nicotinic receptor signal transduction is very minimal if at all and certainly not the rule. d) Binding of acetylcholine to nicotinic receptors will result in depolarization of the cell membrane. e) Binding of acetylcholine to nicotinic receptors results in opening of Na+ channels and the influx of Na+ into the cell. · Question 4 0.2 out of 0.2 points Which of the following statements best describes the consequence of norepinephrine (NE) binding to alpha2-adrenergic receptors (alpha2-AR) in the autonomic nervous system? Selected Answer: d. NE binds to presynaptic alpha2-AR, inhibits adenylase cyclase activity and diminishes the release of NE from the nerve terminal. Answers: a. NE binds to post-synaptic alpha2-AR, stimulates activation of adenylate cyclase and elicits a response in the target cell b. NE binds to post-synaptic alpha2-AR, inhibits activation of adenylate cyclase and mitigates the target cell response to other adrenergic agonists. c. NE binds to presynaptic alpha2-AR, stimulates adenylase cyclase activity and facilitates further release of NE from the nerve terminal. d. NE binds to presynaptic alpha2-AR, inhibits adenylase cyclase activity and diminishes the release of NE from the nerve terminal. e. NE binds to presynaptic alpha2-AR and stimulates the release of co-transmitters Response Feedback: It is true that NE binds to alpha2-AR. However, alpha2-AR are located on the pre-synaptic nerve terminal, inhibitsadenylate cyclase and diminishes the release of NE from the nerve terminal. This is a feedback mechanism. · Question 5 0.2 out of 0.2 points Fill in the blanks of the following statements with either the word “increase” or “decrease”. Blocking reuptake of NE in an adrenergic nerve terminal would (1) ___________ the response to NE. Inhibiting acetylcholinesterase activity in cholinergic nerve terminals would (2) __________ the response to acetylcholine. Selected Answer: c. 1 = increase 2 = increase Answers: a. 1 = increase 2 = decrease b. 1 = decrease 2 = increase c. 1 = increase 2 = increase d. 1 = decrease 2 = decrease Response Feedback: Adrenergic: The main mechanism for termination of NE neurotransmission is reuptake of the neurotransmitter into the presynaptic nerve cell (reuptake 1). Blocking the reuptake of NE at the nerve terminal will result in a higher concentration of NE to bind to receptors. Therefore, the response to stimulation of an adrenergic neuron would be greater because more receptors would be bound in the target cell. Cholinergic : The main mechanism by which cholinergic transmission is terminated is by degradation ofacetylcholine into acetate and choline by acetylcholinesterase that is found in the cleft. If acetylcholinesterase were inhibited, the rate of acetylcholine degradation would be slower. Because of the slower degradation of acetylcholine, the neurotransmitter would accumulate and there would be more to bind to receptors. The greater the fraction of receptors bound the greater the response. · Question 6 0.08 out of 0.2 points Match the response with stimulation of the appropriate receptor. Choose the best match. o Question Correct Match Selected Match Positive chronotropic effect on the heart b. Beta1-AR b. Beta1-AR Endothelial cell-mediated vasodilation of healthy, intact vascular a. Muscarinic (M3) e. Muscarinic (M2) Vasoconstriction of healthy, intact vasculature d. Alpha1-AR b. Beta1-AR Relaxation of bronchial smooth muscle c. Beta2-AR c. Beta2-AR Negative chronotropic effect on the heart e. Muscarinic (M2) a. Muscarinic (M3) o o All Answer Choices a. Muscarinic (M3) b. Beta1-AR c. Beta2-AR d. Alpha1-AR e. Muscarinic (M2) Response Feedback: It's necessary to know the location and normal physiologic anticipated response when a receptor is activated. B1 + chrontropic effect on Heart; M3 Endothelial cell-mediated vasodilation of healthy, intact vascular; Alpha1-AR Vasoconstriction of healthy, intact vasculature; Beta2-AR Relaxation of bronchial smooth muscle; M2 Negative chronotropic effect on the heart. I want to point out that if the endothelium in an arteriole is injured or ablated then direct muscarinic stimulation of a vascular smooth muscle cell will cause contraction (vasoconstriction). It is also important to point out that beta2-adrenergic stimulation (by epinephrine) in skeletal muscle arterioles will cause vascular smooth muscle relaxation and vasodilation. · Question 7 0.2 out of 0.2 points Early symptoms of nerve gas exposure include excessive salivation, lacrimation, urination, diarrhea/defecation, miosis (small pupil size), and fasciculation or tremors. Which of the following would best explain these symptoms? Selected Answer: b. Inhibition of degradation of acetylcholine released from cholinergic nerve terminals. Answers: a. Increased release of norepinephrine (NE) from adrenergic nerve terminals. b. Inhibition of degradation of acetylcholine released from cholinergic nerve terminals. c. Decreased depolarization of postsynaptic parasympathetic nerve fibers. d. Decreased reuptake of NE into presynaptic adrenergic nerve terminals. e. Increased acetylcholinesterase activity. Response Feedback: a) If you increase the release of NE you would be likely to observe symptoms that are the opposite of those described. b) Inhibition of degradation of acetylcholine that has been released from cholinergic nerves would result in increased Acetylcholine levels and increased occupancy of muscarinic receptors mediating symptoms characteristic of activations of the parasympathetic nervous system similar to those described in the question. In addition there would be more acetylcholine to bind to nicotinic receptors in skeletal muscle motor end plates leading to fasciculation and/or tremors. c) If depolarization of postsynaptic parasympathetic cholinergic nerves were decreased – less acetylcholine neurotransmitter would be released and receptors that mediate the symptoms described in the question would not be observed. d) Decreased uptake into presynaptic adrenergic nerve terminals would result in more NE-induced stimulation of alpha- and beta-adrenergic receptors on target organs/cell. Norepinephrine does not mediate the described symptoms. e) Increased acetylcholinesterase activity would result in increased degradation of acetylcholine and thereby less acetylcholine to bind muscarinic and nicotinic receptors (see answer b) · Question 8 0.2 out of 0.2 points Some target organs or cells are more influenced by either the sympathetic or parasympathetic nervous system (i.e., the target organ receives higher sympathetic or parasympathetic tone). Given this fact, if transmission at all autonomic nervous system ganglion were blocked, what change would you expect to see on the production of saliva by salivary glands? Selected Answer: c. A decrease in salivation Answers: a. No change in salivation b. An increase in salivation c. A decrease in salivation Response Feedback: General rationale: Most organs controlled by the autonomic nervous system have input from both the parasympathetic nervous system (PNS) and the sympathetic nervous system (SNS).Because ganglionic blockers block the PNS and the SNS, the effect of these drugs is influenced by the dominant tone in the organ system. Salivary glands have higher parasympathetic tone (or input) than sympathetic tone. Therefore if you blocked stimulation of both divisions of the ANS, the greatest effect you will observe will be the loss of PNS stimulation. PNS stimulation mediates increased salivation. Thus you would observe this loss or a decrease in salivation or dry mouth. · Question 9 0.2 out of 0.2 points Binding of acetylcholine to muscarinic receptors on the adrenal gland results in the release of epinephrine into the bloodstream. Select the statement which correctly identifies a way in which epinephrine differs from norepinephrine. Selected Answer: e. Epinephrine has a higher affinity for the beta2-adrenergic receptor subtype than norepinephrine. Answers: a. Epinephrine has higher affinity for alpha1-adrenergic receptors than norepinephrine. b. Epinephrine is lacking a methyl group on its amine (nitrogen molecule) whereas norepinephrine has a methyl group at this position. c. Epinephrine is degraded by catechol-O-methyltransferase and monoamine oxidase whereas these enzymes do not degrade norepinephrine. d. Epinephrine crosses the blood-brain barrier whereas norepinephrine does not. e. Epinephrine has a higher affinity for the beta2-adrenergic receptor subtype than norepinephrine. Response Feedback: This is essentially a true/false question. Of the 5 statements e is true. a. Epinephrine has higher affinity for alpha 1-adrenergic receptors than norepinephrine. b. These catecholamines are structurally similar with the exception that epinephrine has a methyl group on itsamine side (nitrogen molecule) whereas norepinephrine has a hydrogen ion at this position. c. Epinephrine is degraded by catechol-O-methyltransferase and monoamine oxidase. The same enzymes degradenorepinephrine. d. Epinephrine does not cross the blood-brain barrier whereas norepinephrine acts as a neurotransmitter in the brain (important at the end of the course too). e. Epinephrine has a higher affinity for the beta2-adrenergic receptor subtype than norepinephrine. The ranked order of the drug affinity for the beta2-adrenergic receptor is Isoprotenol>Epinephrine>Norepinephrine. See the dose response curve for B2 receptor. · Question 10 0.2 out of 0.2 points Which of the following statements correctly describes the circulatory reflex initiated by the baroreceptors in response to an episodic elevation in blood pressure? Selected Answer: c. Excitation of the baroreceptors causes a drop in blood pressure because of a decrease in peripheral vascular resistance and a decrease in cardiac output. Answers: a. Increased sympathetic stimulation causes vasodilation bringing elevated blood pressure back to normal. b. Stimulating the vagal parasympathetic center in the medulla causes an increased heart rate and strength of contraction. c. Excitation of the baroreceptors causes a drop in blood pressure because of a decrease in peripheral vascular resistance and a decrease in cardiac output. d. Heart rate increases and stroke volume increases resulting in a higher cardiac output. Response Feedback: Increased blood pressure in the carotid and aortic artery stretches the baroreceptors and initiates an increased rate of depolarization of the vagal and glossopharyngeal nerves that synapse in the cardiovascular center of the medulla. This results in activation of nerves that inhibit the vasoconstrictor center of the medulla and excite thevagal parasympathetic center. In turn this causes: (1) vasodilation of the veins and arterioles in the periphery (2) decrease in heart rate and (3) decreased strength of contraction. As a result arterial pressure is reduced by decreasing heart rate, stroke volume (thereby cardiac output) and peripheral resistance. a) Increased sympathetic stimulation would cause vasoconstriction and increase blood pressure. b) Parasympathetic stimulation decreases heart rate and strength of contraction via the vagus nerve. c) Excitation of the baroreceptors causes a drop in blood pressure because of a decrease in peripheral vascular resistance and a decrease in cardiac output. d) Heart rate increases and stroke volume increases resulting in a higher cardiac output. This sequence describes what happens with a drop in blood pressure. Quiz 1 9/18/17 This is a multiple choice quiz with 10 questions. Each correct answer is worth 1 point. This is an open book quiz with forced completion (must answer all questions at one time). You may use any resources to help you answer the questions. You may take 2 attempts to take the quiz. However, you must submit your final answers before the deadline. The submission site for this quiz will close at that time. After the deadline passes, you will have no other opportunity to submit your quiz. · Question 1 0.2 out of 0.2 points An identical dose of medication was administered to a patient. The first time it was administered orally and the second time it was given intravenously. Plasma drug concentrations were measured at the same time intervals after administration of each drug. In the following Figure, the results were graphed as log of the plasma drug concentration (Cp) versus time after administration. AUCIV is the area under the curve when the drug was given intravenously and AUCPO is the area under the curve when the drug was given orally. What information can you obtain based on the Figure? Selected Answer: e. a and c Answers: a. oral bioavailability b. potency of the drug c. extent and rate of oral absorption the drug d. efficacy of the drug e. a and c Response Feedback: Bioavailability is defined as the fraction of the administered dose of a drug that reaches the systemic circulation in an active form. We define the bioavailability of a drug given intravenously as 1.0 (100%), because medications given via intravenously can avoid barriers which affect absorption. However, drugs given by routes other than IV must be absorbed and might undergo hepatic first-pass metabolism. Thus, they have a bioavailability of less than 1.0. The calculation of bioavailability is based on the ratio of the area under the concentration-time curve (AUC) for the administration route being considered (oral, IM, etc.) and the AUC obtained with IV administration. In other words - in this case the bioavailability would be AUCPO divided by AUCIV. The area under the curve also defines the extent of absorption. · Question 2 0.2 out of 0.2 points A 55 year old female who has chronic renal failure due to a history of poorly controlled diabetes has a estimated glomerular filtration rate (eGFR) = 28 ml/min/ 1.73m2. Which of the following statement(s) describe pharmacokinetic issue(s) of special concern for this patient? Selected Answer: e. b and d Answers: a. The half-life of drugs cleared by glomerular filtration would be shorter. b. Plasma concentration of drugs eliminated by the kidney may be higher in this individual than those without chronic renal failure. c. Drugs cleared by biliary excretion will have a longer half-life. d. Drugs with a narrow therapeutic window that are eliminated by the kidney are more likely to cause adverse effects in this individual than in those without chronic renal failure. e. b and d Response Feedback: The clearance of drugs eliminated by the kidney are likely to be lower in a person with chronic renal failure. The glomerular filtration rate is very low as indicated by her creatinine clearance value. Half-life is the time it takes for half of the drug to be cleared from the body. Therefore if a drug is eliminated by the kidney - particularly by glomerular filtration - then the half-life will be longer. If a drug has a narrow therapeutic window then decreased elimination of the drug can result in higher plasma levels for a longer period of time and a higher probability of an adverse effect. If the drug is given chronically at a given dose and maintenance interval - it is likely that the drug will accumulate in the plasma and be even more likely to result in an adverse effect. · Question 3 0.2 out of 0.2 points Ten (10) mg of Drug B is given to Mr. Anderson. Every hour, 0.5 mg of Drug B is eliminated. Therefore, drug B is eliminated by (1)_____order kinetics. However, if a constant proportion of Drug B were eliminated every hour, then Drug B would be eliminated by (2)_____order kinetics. Selected Answer: a. (1) zero; (2) first Answers: a. (1) zero; (2) first b. (1) first; (2) zero Response Feedback: In first order kinetics, the elimination of the drug is proportional to the plasma concentration. After one half-life, 50% of the drug will be eliminated. For example, if 100 mg of a drug is given, following one half-life, 50% of the drug will be eliminated, decreasing the plasma concentation to 50 mg. If 200 mg of the same drug is given, after one half-life, 50% of the drug will be eliminated, resulting in a plasma concentration of 100 mg. Regardless of the amount of drug given, after one half-life, 50% of the drug will be eliminated. In zero order kinetics, the amount of drug eliminated is the same and is independent of the drug concentration. For example, 0.5 mg of Drug B is eliminated every hour. If 10 mg of Drug B is given, after one hour, 9.5 mg of Drug B will remain in the body. If the dose is tripled and 30 mg of Drug B is given, the body still only eliminates 0.5 mg every hour. Therefore, after one hour, 29.5 mg of Drug B will remain in the body. You can see how this could lead to toxic drug levels since the body does not eliminate more of the drug when a larger dose is given. · Question 4 0 out of 0.2 points Which of the following statements are FALSE regarding P-glycoprotein? Selected Answer: a. P-glycoprotein reduces transport of drugs from one side of a membrane to the other. Answers: a. P-glycoprotein reduces transport of drugs from one side of a membrane to the other. b. P-glycoprotein can be found in the brain and intestines. c. Increasing or decreasing the expression of P-glycoprotein can affect the absorption and plasma levels of drugs. d. P-glycoprotein allows for increased transportation of drugs across the intestines and blood brain barrier. Response Feedback: Recall that P-glycoproteins are efflux proteins and function as a protective barrier, which decrease transportation of drugs into intestinal cells and across blood brain barrier. They are found in multiple sites throughout the body. Changing the expression of theses transport proteins affects drugs levels. · Question 5 0.2 out of 0.2 points Which are TRUE about cytochrome p450 (CYP450) enzymes? Selected Answer: e. All of the above. Answers: a. They are important for phase 1 drug metabolism. b. There is more than one isoform (isozyme) of CYP450 metabolizing enzymes and CYP3A4 & CYP2D6 are two examples CYP450 isoforms. c. CYP450 enzymes are found throughout the body, but are predominantly found in the liver and small intestine. d. CYP450 enzymes can activate pro-drugs. e. All of the above. Response Feedback: All are true statements. Pro-drugs need to be metabolized in order to be altered to their active form. · Question 6 0.2 out of 0.2 points If Drug X is metabolized by the CYP3A4 enzyme and Drug Y inhibits the CYP3A4 enzyme, concomitant administration of drugs X and Y would likely cause which result? Selected Answer: a. Increase in Drug X plasma levels. Answers: a. Increase in Drug X plasma levels. b. Decrease in Drug X plasma levels. c. No change in Drug X or Drug Y plasma levels. Response Feedback: If Drug Y inhibits the enzyme required to metabolize Drug X, metabolism of Drug X will be hindered. Metabolism usually makes a drug more polar and more easily cleared from the body. If this process is inhibited the drug will be cleared more slowly resulting in an increase in plasma levels of Drug X. Importantly try to visualize that an enzyme like the CYP450 enzymes have an active site where the drug must bind to be metabolized (i.e., to be converted to a metabolite). You can think of this active site somewhat like a receptor. There are a limited number of enzymes and thereby a limited number of active sites. If there are enough enzymes to metabolize a certain amount of drug then the drug metabolism will be at a maximum rate. However, it more of that drug is in the system than there active sites, the drug can not be metabolized any faster. Or - if a drug is being metabolized at a maximum rate and then another drug is added that is metabolized by the same isoform of CYP450, then the 2 drugs will compete for the active site on the limited number of enzymes and the rate of metabolism of both drugs will be less than optimum. The affinity of the drug for the active site of the enzyme comes into play. If the second drug (Y) has a very high affinity for the active site of the enzyme, it may have a fast on rate and a very slow off rate. As a result the second drug will inhibit the ability of the first drug (X) to compete for the active site and get metabolized. Thus - the rate of metabolism of the first drug (X) will be reduced, the rate of clearance will be reduced, and the plasma levels will be elevated. · Question 7 0.2 out of 0.2 points Drug Z has a half-life of 2 hours. One hundred (100) mg of Drug Z is given at 9 am. At 11 am, the plasma level of Drug Z is 50 mg. At 1 pm, the plasma level of Drug Z is 25 mg. What will the plasma level of Drug Z be at 5 pm? Selected Answer: b. 6.25 mg Answers: a. 12.5 mg b. 6.25 mg c. 10 mg d. 3.1 mg Response Feedback: Drug Z is eliminated by first order kinetics, with a half-life of 2 hours. This means that every 2 hours, 50% of Drug Z will be eliminated from the body. If Drug Z was given at 9 am, after one half-life (2 hours), 50% of the drug would be eliminated. After the next half-life, which would be at 11 am, another 50% of Drug Z would be eliminated, and at 1 pm, another 50% eliminated. At 9 am, 100 mg of Drug Z was given, so at 11 am, 50 mg of Drug Z would be eliminated, since 50% of 100 mg is 50 mg. At 1 pm, another 50% of Drug Z would be eliminated, so 50% of 50 mg is 25 mg. At 3 pm, 50% of 25 mg would be eliminated, so 12.5 mg of Drug Z would remain in the body. At 5 pm, another 50% of Drug Z would be eliminated, so 50% of 12.5 mg is 6.25 mg. Therefore, at 5 pm, the plasma level of Drug Z would be 6.25 mg. · Question 8 0.2 out of 0.2 points Drug A is a substrate for P-glycoprotein. Drug B inhibits P-glycoprotein. Which of the following could happen if Drug A and Drug B are given together? Selected Answer: e. a and c Answers: a. Increased transport of Drug A into the brain. b. Decreased transport of Drug B into the brain. c. Increased transport of Drug A across the intestinal cells into the blood. d. Decreased transport of Drug B across the intestinal cells into the blood. e. a and c Response Feedback: If Drug A is a substrate of P-glycoprotein, P-glycoprotein will transport Drug A out of the brain and intestines. If Drug B is given at the same time though, it prevents P-glycoprotein from "kicking out" Drug A from the brain and intestinal cells. With the action of P-glycoprotein (P-gp) being inhibited by Drug B, Drug A will then be able to cross into the brain (drug moves from blood to brain) and across the intestinal cells into the blood (drug does not cross into the intestinal lumen but remains in intestinal cells and moves into blood). In the gut, the P-gp action takes place on the membrane between the intestinal cells and the intestinal lumen. · Question 9 0.2 out of 0.2 points Sam is taking 100 mg of Drug X that is eliminated by first order kinetics, with a half-life of 3 hours. Sam is also taking 100 mg of Drug Y that is eliminated by zero order kinetics. Ten (10) mg of Drug Y is eliminated every hour. At 10 am, Sam accidentally takes 300 mg of Drug X and 300 mg of Drug Y, instead of taking 100 mg of each. Given the elimination patterns of each of these drugs, plasma levels of which drug (X or Y) will be higher at 1 pm, and could lead to a greater risk of adverse effects? Selected Answer: b. Drug Y Answers: a. Drug X b. Drug Y Response Feedback: Drug X is eliminated by first order kinetics. Even though Sam tripled his dose, after one half-life, or at 1 pm, 50% of the drug will be eliminated. Therefore, at 1 pm, Sam's plasma levels of Drug X will be 150 mg. Drug Y is eliminated by zero order kinetics (same amount of drug is eliminated). Even though Sam took 300 mg of Drug Y instead of 100 mg, 10 mg of Drug Y will still be eliminated every hour. Therefore, at 1 pm, Sam's plasma levels of Drug Y will be 270 mg (290 mg at 11 am, 280 mg at 12 pm, & 270 mg at 1 pm). If Drug Y has adverse effects, the risk of adverse effects will be greatly increased, since it will take several hours to get the plasma levels down to therapeutic levels given that only 10 mg of Drug Y are eliminated every hour. · Question 10 0 out of 0.2 points John is a 70 kg man. He needs an oral dose of the drug kinetico. Kinetico has a bioavailability of 0.4. It has a volume of distribution (Vd) of 0.5 L/kg (liters per kilogram). He needs to take a dose of kinetico that will give him a plasma level of 2 ug/L (2 micrograms per liter). What dose of kinetico will you give him? Selected Answer: c. 70 micrograms Answers: a. 112 micrograms b. 175 micrograms c. 70 micrograms d. 350 micrograms Response Feedback: If the Vd is 0.5 L/kg, John weighs 70 kg - so for every Kg of body weight there is a potential volume of 0.5 L that the drug can be distributed in. Calculate apparent- Vd 70 kg x 0.5 L/kg = 35 L You want the plasma concentration to be 2 ug/L, meaning you want 2 ug in each of those liters. So 2 ug/L x 35 L = 70 ug total drug However, bioavailability of kinetico is 0.4 or 40% so for every ug of kinetico you give, only 0.4 ug will make it into the systemic circulation. So you will have to give more drug to achieve the desired concentration. You want to know 40% of what dose (x) will give you 70 ug... 0.4 x = 70 ug or x = 70/0.4 x = 175 ug You will have to give 175 ug You can set this up as using the formula from the Katzung video series: mass (dose) = plasma concentration x apparent Vd. Don't forget this is an oral dose so divide by F. ANS QUIZ Module 2 Anti-Diabetic Drugs: Part 1 : Insulin Therapy Hormones of endocrine: pancreas & insulin 1. Pancreas - (alpha, Beta , Delta, F cells) *alpha cells > glucagon -glucagon secreated by pancreas, works in liver -thru glycogenolysis converts glycogen to glucose in liver > released to blood. - *****controls glucose level in the body *****prevents blood glucose levels from dropping too low) *Beta cells *Delta cells: *F cells 2. INSULIN - secreted in Response to: *glucose *amino acids *some GI hormones Primary Action: ● Maintains blood glucose within narrow range ● Promotes formation of: - Part 2: Insulin Secretagogues Drugs to treat Diabetes Overview Control of Plasma Glucose: Pancreatic axix: *Insulin ● Secreted by Beta - B cells dt High BG levels ● Suppresses glycogenolysis > increase glucose uptake into tissue *Glucagon ● Secreted by Alpha - a cells when BG is Low ● Induces glycogenolysis > release of glucose into blood MOA: Indicated: Contraindicated: AEs: Clinical Efficacy (ability to reduce HbA1C Part 3: Biguanides (Metformin) MOA: ● decrease hepatic production of GLUCOSE ● Reduce insulin resistance ● Increase insulin sensitivity Indicated: ● T2D ● overweight, ● obese w/ insulin resistance Contraindicated/cautions: pt w/ ● Liver disease, ● Decreased GFR ● Decreased Cardiorespiratory perfusion AEs: lactic acidosis, GI discomfort Clinical Efficacy (ability to reduce HbA1C): ● 1 - 1.4% *****muscle stimulates glucose utilization *****liver decreases gluconeogenesis & glycogenolysis. Part 4: Thiazolidinediones MOA: Indicated: Contraindicated: AEs: Clinical Efficacy (ability to reduce HbA1C Part 5: Incretins Part 6: Alpha-glucosidase Inhibitors Part 7: Sodium Glucose Co-transporters 2 inhibitors Part 8: updates on DM drugs Module/Exam 1 Week 1-2 Objectives ------------->Common routes of drug admin & excretion VIDEO 2 *oral - swallowed (max convenience, slower absorption, subject to first-pass effect = agent/med is metabolized in gut wall, portal circulation, & liver b4 it reaches systemic circulation. *buccal/sublingual - not swallowed) (Direct absorption into venous circulation, bypasses hepatic portal circuit & first-pass metabolism *IV (Instant, complete absorption, 100% bioavailability but potentially more dangerous) *IM (Faster & more complete, higher bioavailability than oral; if drug not irritating it can be given in large amt, first-pass metabolism avoided) *SQ (slower absorption than IM; first-pass metabolism avoided) *Rectal (Suppository; ***best for bad tasting drugs, & large amt; partial avoidance of first-pass metabolism) 2 concepts to differentiate common drug admin routes: 1. Absorption rate - **** depends on blood flow of that site *IV>IM>SQ *benefit of faster absorption = rapid onset Slow absorption = longer duration of action ******pt w/ compliance issue -”give birth control SQ than oral daily 2. First pass effect & bioavailability *goal = eliminate DRUG A before it reaches systemic circulation *first pass effect = occurs mostly w/ oral & rectal (partial) admin ******1st pass effect = decrease bioavailability because LIVER HAS 2 BLOOD SUPPLY Q MATH: PCN bioavailability of 25%. Dose of 10mg given pt PO, how much drug gets in systemic circulation? A******* (Mass/drug admin) x f = Mass(Total mass/drug absorbed) Mass (total mass/drug admin 10mg) × f (bioavailability .25) = Mass (total mass/drug absorbed) = 2.5mg Liver= metabolizing organ of body Liver= first pass effect organ b4 drug reaches systemic circulation ORAL > stomach > Intestines > portal vein > LIVER > IVC-Inferior vena cava > aorta > celiac artery > common hepatic artery > liver (cycle of metabolism) > kidney - for excretion RECTAL > inferior rectum > space btwn IR & superior rectum (from IR 50% of drug admin skips liver > IVC; from SR 50% drug admin goes to portal vein RECTAL admin only PARTIAL FIRST PASS EFFECT, this a higherer BIOAVAILABILITY IV - NO FIRST PASS EFFECT has (f) = 1 or in other words 100% BIOAVAILABILITY IM/SQ (Diffusion to capillaries) ***FIXED LAW = absorption is proportional to concentration gradient CG & surface area. So good blood flow maintains high CG, poor blood flow leads to decreased diffusion & absorption of drug. E.g. give pt insulin shot in leg & arm & pt goes running. The insulin in leg has higher diffusion/absorption rate -------------->Define: *Therapeutic index = space between the efficacy of a drug & its toxicity. -drugs w/ high therapeutic index are safe over a wide range of concentration encompassing the variations caused by genetics then it's not necessary to consider polymorphisms in the context of therapeutics -drugs w/ low therapeutic index (warfarin) it has minor variations in concentration causes by polymorphism *half life = time to metabolize 50% of drug *if half life of drug is 1 hour then 50% of the drug is eliminated after every 1 hour. *If 100mg administered after 1 hour amt in body will be 50mg bcuz the rate is not constant but constant proportion of drug is eliminated after 2 hours (another 1 hour) the rate will be 25mg (see table below) 1. you will be asked to solve for it in 2 ways: Graph ( Co) or Table (½ Co) Co=concentration 2. 95% of drug always eliminated after ~4.5 half LIVES! Assuming the drug is undergoing 1st order elimination = a constant proportion of drug eliminated per unit time 3. Half life equation w/ variables t ½ = (half life) = 0.693 x Vd (vol of dist) / CL (clearance) **** see book notes on how to solve for half life (t ½) using *Table *Gragh *Equation *clearance 1. Defination the vol of plasma cleared of drug per unit time (unit = Vol/Time) *how clearance affect half life or rate of drug elimination *****Increase CL > decrease t ½ (thus we eliminate drug quicker) ***** if half life (t ½) = 0.693 * Vd / CL (clearance) 2. Ability of how drug clears from body? By equation below: *****CL total = CL renal + CL hepatic *Renal clearance of drug (check GFR) 3. Clearance is the proportionality factor used to determine rate of elimination ******Rate of elimination = CL x Concernt ******CL =Rate of elimination / Concerntn (answer will always be a constant bcuz clearnce is always a constant). Clearance has nothing to do with amount of the drug, just the rate at which drug from plasma goes out & into liver and kidneys *****Renal clearance = drugs going into kidneys - urine (most drugs) ***** hepatic clearance = drugs going into liver - bile (some drugs) *********************pt has kidney disease give drug that is cleared mostly by liver not by kidneys *elimination Elimination rate = mass or amt of drug cleared from blood per unit time ***** when solving for elimination rate we assume that we are solving for first order elimination = elimination rate is proportional to plasma drug concentration up to certain point. ---------------->Graph to show drug elimination : (see book notes) *first order elimination *zero-order elimination 1 __Increase__ plasma drug concentration > __Increase___ rate of drug elimination ___Increase__ plasma drug concentration > __No increase_ rate of drug elimination 2 Rate of elimination is proportional to drug concentration 0 hour = 100mg, 1 hour = 50mg, 2 hours = 25mg, 3 hours = 12.5mg Rate of elimination is independent of drug concentration 0 hour = 100mg, 1 hour = 75mg, 2 hours = 50mg, 3 hours = 25mg (Rate is constant, the proportion is not constant) 3 Constant Half life Constant rate of drug elimination 4 Ex. Most drugs at most doses Ex. High doses aspirin, phenytoin & alcohol 5 ------>clinical implications of changes in half life ------>Process of drug (ADME) * absorption * distribution *metabolism *excretion ------>concepts of Bioavailability & Vol of distribution *bioavailability(f) = fraction of admin’d dose that reaches systemic circulation f = [Mass (total Mass absorbed) = Mass (total Mass Admin) Concentration vs Time Graph (VIDEO 3) Concentration = plasma drug concentration Plasma = blood w/o the cells Blood vol = 5L Plasma Vol = 2.5L Q MATH: 10mg dose, drug x, 100% absorbed. What is approx plasma drug concentration shortly after admin? M (Mass) = 10mg V (vol) = 2.5L bcuz blood staying in plasma C (concentration) ? C= M/V = 10/2.5 = 4mg/L See book note for graphs: Pay attn to area under the curve - the larger the area the more drug absorbed ******Bioavailability route = AUC (route)/AUC (IV) ********by definition the bioavailability of any drug given IV = 100% Mass = dose of drug which reaches systemic circulation (units = mg) - dose that gets absorbed Volume = plasma volume (units = L, mL) *volume of distribution (VIDEO 4 - apparent vol of distribution) *When the drug leaves the vascular space(plasma 2.5L) = systemic circulation & it's distributed to extravascular space (7.5L)= target tissue(heart, muscle, fat, brain…. w/ their individual vol) * Admin 10mg drug C (plasma concentration b4 distribution @ t=0) = 10mg/2.5L = 4mg/L C (plasma concentration after distribution @ t=1 hour) = 10mg/2.5L+7.5L = 10mg/10mg = 1mg/L *****C=M/V Why is drug distribution important? Bcuz drugs don't distribute equally in the vascular space we can't assume the Vol *****Vd (vol of dist) = M/C (M= amt of drug in the body, C in the blood/plasma concentration) High Vd > Low C (concentration) - widely distributed, will not stay in plasma ( less in vascular space, more in extravascular space) Vd=20/2= 10) e.g. widely distributed drugs don't stay in plasma :* lipophilic (fat), * binds to extravascular tissue (muscle), small Molecular wt (MW) Low Vd > High C ( more in vascular space, less in extracellular space) Vd=20/18=1.1 bcuz 18 units stayed in plasma E.g. drugs not widely distributed, stay in plasma: H2O soluble, plasma protein bound, large ME What determines the Vol of distribution/vol you are going to solve for? 2 determinants of Vd: 1. Properties of drug 2. Size of extravascular space - size/pt’s vol estimated from pt’s wt. E.g. obese ot vs child *****Vd recorded as L/Kg ; or ****** low Vd = high degree plasma protein binding (stays in blood) How would a very high vol of dist affect the limitation of a drug? Takes longer to eliminate the drug bcuz of their higher vol of dist ------>relevance of Hepatic first pass effect ------>application of these principal in clinical situations *Pharmacokinetics Dr. V Metabolism/Biotransfornation Def: transforming active compounds into “metabolites” (have pharmaceutical properties) -by deactivating parent compound into excretable form or both - occurs mostly in liver (& plasma, kidney, intestines & brain) - liver enzymes convert lipid soluble drugs > more polar compounds w/ smaller Vd > inactive parent compound > elimination IV drug metabolizes by moving back & forth into central & peripheral compartments. The drug is metabolized in liver. *****Liver & kidney in Central Compartment highly vascularized. Factors that influence metabolism: *age - kids <1 yo & elderly have ****decreased metabolic capacity in liver *pregnancy - here some metabolic pathways increase or decrease capacities *liver disease - decrease metabolic capacity *genetics - CYP enzyme some pop have variations in metabolic capacity to certain drugs e.g. *****warfarin, SSRIs 2 Types of metabolism 1. Phase I (ORH) -oxidation - Reduction - hydrolysis 2. Phase II (CAAM) - conjugation - Alkylation -Acetylation -Methylation Phase I Reactions of Metabolism *mediated by large family group of enzymes called *****Cytochrome p450 enzymes *******5 substrates of cytochrome p450 family that undefined Phase I biotransformation:(95% of drugs) *1A2 *2C9 *2D6 *2E1 *3A4 *******majority of drugs are metabolized through CYP3A subfamily, followed by CYP2D6 CYP2C Types of CYP P450 drug interactions: *inhibition *induction *Inhibition = when 1 compound competes w/ the other for CYP P450 enzyme binding site (drugs drug interactions ) ********most common type of pharmacokinetics drug interactions = CYP P450 ********drugs w/ CYP P450 inhibition capability/most common types of pharmacokinetics drug interactions involve: *warfarin *HIV drugs *Antibiotic *Antiarrhythmics *******CYP p450 metabolism is (or enzymes are) saturable = when all enzyme binding sites are filled, the system is saturated. *********Drug accumulation = 2 drugs, same substrate to same enzyme are given together. 1 blocks metabolism of the other causing blocked drug to accumulate. Diagram: Red discs = CYP2C19 enzymes, blue discs = drug -drug binds to CYP then it's metabolized, but if enzymes are blocked the drug cannot be metabolized Clinical application of drug-drug interaction Q: 55 yo female Hx DVT/PE. ℅ weakness, black tarry stool. INR 9.2. On Warfarin. Completed ABT bactrim 4 UTI yesterday. What Happened? A: Bactrim blocked absorption/metabolism of warfarin > warfarin not metabolized > warfarin accumulates > INR goes up > pt experiences bleeding. *Induction - when some compounds increase the activity of CYP P450 enzymes > increase metabolism of meds > Tx failures dt subtherapeutic concentration of drugs Some people w/ a genetic variant that can metabolize some drugs rapidly. So clinically it's important to consider when titrating drugs and pt is still in subtherapeutic level. Consider maybe pt is a Rapid Metabolizer- UM Clinical application of enzyme induction Q&A Q: Public advisory in risk of drug interaction w/ St. John's Wort & HIV meds. What happened? A: st. John's wort induces/increases the CYP enzymes available so the HIV drugs were rapidly metabolized > pts getting Hiv Enzyme inhibitor + liver disease > toxicity level of drugs increase Enzyme inducer added > Tx failure occurs ******pts should be kept at MINIMALLY EFFECTIVE CONCENTRATION level or steady state… think of therapeutics index. *Excretion of drugs: * occurs mainly in kidneys * also thru urine, feces, lungs, skin, sweat, breast milk * excreted in their active state or undergo metabolism in the liver to convert them into excretable form = more hydrophilic/more polar Factors that influence kidneys ability to excrete drugs: *kidney disease - decrease excretive capacity *age - excretion capacity reduced in newborns & elders *heart disease - dt decrease perfusion esp in pt w/ heart failure > decreases kidneys ability to excrete drugs dt impaired heart's ability to deliver fluids to kidneys *urinary pH - plays a big role in drug excretion. Has to do with ****ionization of the drug. Manipulating urinary pH is one way to manipulate drug levels *plasma protein binding - **** only unbound, “free drugs” that can bind to receptors & can be excreted via kidneys Renal physiology: 3 ways drugs can be excreted: 1. Drug is filtered > glomerulus apparatus then excreted 2. Drug goes thru glomerulus is filtered > capillaries & reabsorbed 3. Drug goes thru glomerulus to capillaries & thru circulation system & excreted thru the tubular system w/o being filtered Renal Excretion: - estimating renal function is paramount ● Highly influenced by renal function ● Renal function is defined by *****GFR glomerular filtration rate ● *****Most clinically useful tool to estimate GFR is by calculating Creatinine Clearance = CrCi ● Most widely used CrCi estimator = Cockcroft-Gault equation then adjust meds to avoid ADRs/Events *******Male 140 - age x ideal body wt (IBW) / serum creatinine x 72 (For female correction factor multiply male fraction above x 0.87) ******IBW female (kg) = 45.5kg + (2.3x inches > 5’ feet) *IBW male (kg)= 50 kg + (2.3x inches > 5’) (See more book for equation) *Pharmacokinetics in infants & Children - ADME factors differ across age within the Peds age category - *****ADE-ffects in infants & children are usually similar to adults but there are some unusual or unique toxicity in this age group. - Know dosing intervals to calculate amt of drug to admin @ each interval - Dosing for some less frequently used drugs may be based on Age, WT, and/or BSA (Body surface Area) Weight-based dosing: *****Know the WT of Peds pt in Kg (1kg=2.2Lbs) *****mg/kg/day OR mg/BSA/day *****BSA = (are notebook) Considerations in peds dosing: - She, disease, pharmacokinetics differences in age group (ADME) 1. Change across the age range 2. Mediate plasma drug levels & time course of drug on the body. ******use of theophylline has increased in peds Absorption: *Oral absorption depends on: - Gastric/intestinal pg - Bike formation - Gastric emptying time - Intestinal motility - bowel length & effective absorption surface - Activity of intestinal wall drug metabolizing enzymes (CYP450) & drug protein - GASTRIC pH varies w/ age: - Acid labile drugs in acidic environment = increase absorption & bioavailability - ***** basic/alkaline drugs in basic environment = increase absorption - LIKE GOES WITH LIKE - *****Phenobarbital (weak acid)= decreased bioavailability in neonate/infants/children - Bile formation: - Low bile formation low/decreased absorption of lipophilic drugs/vits - *****incomplete absorption = when reduced gastric emptying & intestinal motility > increased time to reach Therapeutic concentration - Variable microbial colonization of gut: - *****gut is sterile at birth - *****amt & type of bacteria influences intestinal metabolism of drugs Distribution : *depends on: - SIze (of drug molecules esp lipid or water soluble - Membrane permeability - Water partitioning - Protein binding - Blood flow to tissue - Physicochemical properties of drug ionized - ***** compared to adults children have a higher Vd of water soluble drugs & lower Vd of lipid soluble drugs except at age around 1yo. - Distribution into brain: ● *****increased permeability across BBB (blood brain barrier) bc it's not well established ● *****CNS vol is disproportionate bigger compares to rest of body for Neonates, Infants & children (NIC). - Plasma protein binding: - Neonates - ● Qualitatively different binding proteins which drugs may have LOW affinity to ● Higher blood concentration of bilirubin & non-esterified fatty acids - these compete w/ drugs for plasma protein binding sites ● Neonate & infants: Albumin & alpha1-acidic glycoprotein concentration are lower but reach adult values @ 1yo ● *****highly plasma protein bound drug w/ higher levels of free drugs > greater response & toxicity (e.g. PCN, phenytoin, sulfa drugs, lidocaine & propranolol) ● *****high affinity drugs for plasma protein displacement bilirubin > Kernicterus (e.g. Ceftriaxone) ● *****only free drugs can exert an effect or be metabolized Metabolism: -primarily hepatic - liver -depends on: ****hepatic blood flow; amt & activity of drug metabolizing enzymes ● Up to 1 yo - reduced hepatic blood flow ● Infants/children - liver size to body WT ratio is higher than adults ● In NIC - phase 1 metabolism is generally reduced & dependent on CYP450 isoforms ● In children - phase 1 metabolism may be increased in some CYP450 enzymes ● Phase II metabolism decreased > CONJUGATION ● *****drug metabolism > more polar, water soluble metabolite that's more easily eliminated ● *****metabolism is required for activation of a prodrug ● *****some metabolites are active & potentially more active than parent drug ● *****lower drug metabolism > decreased clearance > increased accumulation > increased toxicity risk ● *****lower metabolism of prodrug > decreased active drug > decreased response First Pass Metabolism ● Drugs can be metabolized by metabolic enzymes in the intestinal wall - esp CYP450 ● In NIC - reduced CYP450 > increased BIOAVAILABILITY = less drug metabolized > more absorped ● Inpremies & neonates decreased metabolism of Midazolam by CYP3A4 > increased plasma levels > increased risk of over sedation ● Zidovudine (ARV) metabolized by glucuronidation & several CYP450 isoforms has lower first pass metabolism > lower clearance > higher plasma drug concentration Elimination/ Total Body Clearance ● *****Renal excretion = primary route of drug elimination - Other routes (biliary, lungs, skin, breastmilk) - *****involves: - * glomerular filtration - * renal secretion - * renal reabsorption - *****measure of drug elimination = clearance = vol of plasma cleared of drug per unit time (ml/min) - *****half life (t ½) = amt of time required for concentration of drug to reduce by 50% - *****consider renal function alterations & dose modifications in pt w/ renal disease Glandular filtration - *****GFR measured by creatinine clearance (CrCl) which is reduced but reaches adult function at 6months - 1 year (infants) - *****CrCl in infants is 3x that of adults (40-120) - *****Schwartz equation = 1wk old - 18yo CrCl = (ml/min/1.73m2) = [Length (cm) x k] / Scr *****Scr in mg/DL Renal Secretion ● Rate lower but reach adult rate by 7 months ● E.g. of drugs w/ reduced renal secretion: PCN, furosemide, sulfonamides, cephalosporins ● Higher renal elimination in late infancy w/ some drugs w/ rapid tubular secretions & lower plasma protein binding (e.g. digoxin, carbamazepine, clindamycin, cimetidine, chlorpheniramine) Renal Reabsorption ● Rates lower but reach adult rates btwn 1-3 years ● In Neonates & infant lower urinary pH > altered reabsorption rate Implications: *****lower rate renal elimination > slower clearance > increased plasma levels > increased drug response > higher potential for ADRs *****with decreased clearance just decrease dose OR increase dosing intervals *****examine each drug individually ***** follow normal pharmacokinetic principles to predict implications with differences btwn age groups. *****CLEARANCE = parameter importance w/ kids. Pharmacological considerations Elderly Part 1: *eldely > 65 *older elderly >85 > 100 Reasons for concern: ● *****disproportionately higher incidence of ADRs ● More diseases, chronic conditions, polypharmacy ● Elderly severely underrepresented in clinical trials on pharmacotherapeutic response (benefits) & risks (ADRs) ● *****ACE inhibitors in those > 75 are not effective What is ADR? ● Side effect - expect it may happen, unnecessarily unavoidable ● Toxicity - Inability to maintain steady state ● Allergic reaction ● Drug-drug interaction ● Drug-food interaction ● Sub-optimal drug treatment - drug not suitable What is optimal drug therapy? (True for gen. pop. not just elderly) ● *****maximizing therapeutic effect while minimizing risks (ADRs) ● Drug selection for overall greatest advantage ● Selection of pharmacotherapeutic interventions whereby potential benefit outweigh potential risk Factors influencing ADR: ● ***** impaired homeostasis (homeostatic reserve) ● *****altered Pharmacodynamics & pharmacokinetics ● *****polypharmacy Primary reasons for ADRs in elderly: ● *****Absolute age is less important than # of diagnoses (diseases) & # of drugs consumed ● So CHRONIC COMORBIDITIES & POLYPHARMACY Factors contributing to polypharmacy: ● # of diseases ● Multiple Rx (ing) HCPs & multiple filling pharmacies ● Use of drugs to Tx symptoms vs underlying disease ● Tx (ing) AEs of one drug w/ another ● ***** Propensity of HCPs to Rx ● Expectations of pts to receive a Rx ● Reluctance to D/C old meds ● *****Automatic refill mechanisms ● *****multiple OTC meds ● Lack of compliance/adherence ● Borrowing meds from family/friends ● *****inadequate clinical assessment = lack of systematic eval of pharmacotherapeutic intervention ● ************studies - NPs w/ prescription authority order fewer drugs than physician & Rx were appropriate for the medical Dxs Age-related changes that affect pharmacokinetics: ● ADME Dose Response Relationship: ● Response to drug depends on drug concentration at receptor site (amt of drug available) ● *****concentration of drug at receptor site = steady state plasma concentration (Css) of the drug ● *****ideally Css > therapeutic level & < toxic level (within therapeutic Window) Physiologic changes from 20-80 years: ● +35 - body fat / total body WT ● -17 - total body water ● ***** 50 - monitor GFR ● *****40 - renal & splanchnic blood flow Age/disease/drug-related Changes in Absorption: ● Age > decreased splanchnic blood flow, gastric acidity, motility & absorption surface ● Absorption Slows down in elderly use non oral route if you need rapid response of drug ● ***** are factors may delay absorption but overall have minimal clinical significant effect ● *****Ask about use of OCTs (antacids, laxatives, bile acid binders, drug that alter gastric emptying) ● *****drug-drug interaction & disease states can increase or decrease absorption Alterations in Vd change Css: Vd = ***** extent of drug distribution throughout the body *****Related to : compartment of body water in which the drug is dissolved *****Change in Vd (drug dist) alters t ½ & Css (are Equations for Exam 1 for Css & t ½ formula Distribution: Age: ● Decrease in TBM (total body mass), lean body mass, body water & *****ALBUMIN (10-20%) ● Increase or decrease of Css ● Hydrophilic drugs - decreased Vd But Increased Css & response, ● Lipophilic drug - increase Vd, t 1/2 , duration of action > risk of toxicity ------>effects of drug binding ON volume of distribution when a drug *stays in the plasma *binds to plasma protein * binds to peripheral tissue (elderly) (See diagram in lecture Handout pg 8) Fig A Plasma Protein Binding: Drug D Alone ● When Drug D alone binds to plasma protein in vascular compartment > decrease its intensity & prolongs its action. So the ratio of bound-to-free drug remains constant regardless total amt of drug in the plasma. ratio represents free drug/total drug D 4/16, 3/12 , 1/4 (25% of total drug = free drug) ● *****Albumin - most abundant Cat-ion Fig B Plasma Protein Binding: When Drug A added t [Show More]
Last updated: 1 year ago
Preview 1 out of 68 pages
Instant download
Buy this document to get the full access instantly
Instant Download Access after purchase
Add to cartInstant download
Reviews( 0 )
Document information
Connected school, study & course
About the document
Uploaded On
Apr 05, 2021
Number of pages
68
Written in
Additional information
This document has been written for:
Uploaded
Apr 05, 2021
Downloads
0
Views
43




 (1).png)
.png)

