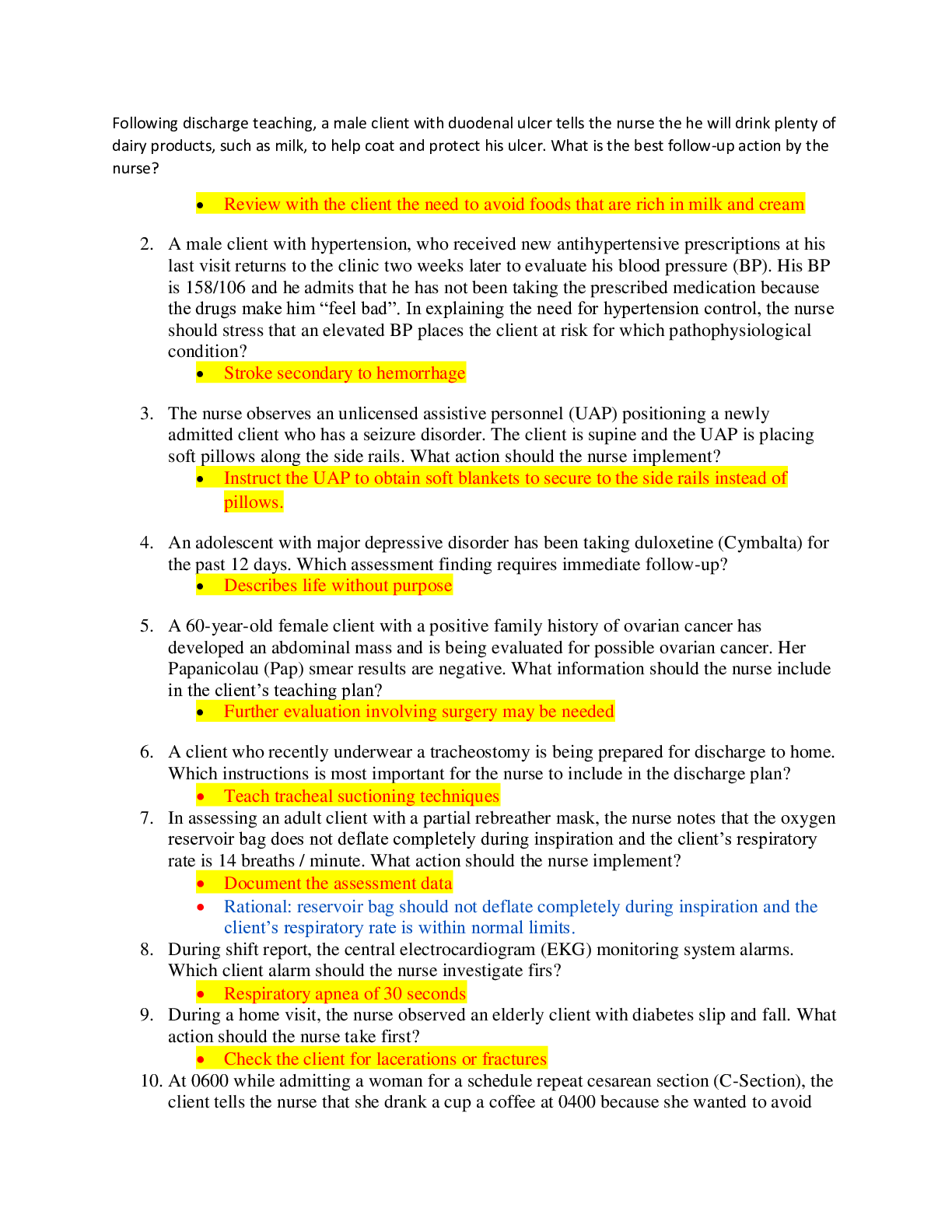
*NURSING > HESI MED SURG > HESI MED SURG Kelly study guide exam 1 NEW VERSION 2020 (All)
HESI MED SURG Kelly study guide exam 1 NEW VERSION 2020
Document Content and Description Below
Chapter 25 Assessment of Cardiovascular Function Cardiac Action Potential Depolarization: electrical activation of cell caused by influx of sodium into cell while potassium exits cell This exch... ange of ions creates a positively charged intracellular space and a negatively charged extracellular space. Repolarization: return of cell to resting state caused by re-entry of potassium into cell while sodium exits Refractory Periods Effective (absolute) refractory period: phase in which cells are incapable of depolarizing.( no desert no matter what you have no room) Cell is unresponsive to any electrical stimulus. Relative refractory period: phase in which cells require stronger-than-normal stimulus to depolarize ( EG you have room for desert so if stimulus is great enough) Cardiac Hemodynamics Cardiac Output Refers to the total amount of blood ejected by one of the ventricles in liters/minute. In a resting adult is 4 to 6 L/min normally Computed by multiplying the stroke volume by the heart rate. Stroke volume is the amount of blood ejected from one of the ventricles per heartbeat. Average resting stroke volume is about 60 to 130 mL. Preload: degree of stretch of the ventricular cardiac muscle fibers at end of diastole End of diastole is the period when filling volume in the ventricles is the highest and the degree of stretch of the muscle fibers is the greatest. Preload is referred to as left ventricular end-diastolic pressure. As the volume of blood returning to the heart increases, muscle fiber stretch also increases (increased preload), resulting in stronger contraction and a greater SV Preload is decreased by a reduction in the volume of blood returning to the ventricles. o Diuresis, venodilating agents (nitrates), excessive loss of blood, or dehydration (loss of body fluids from vomiting, diarrhea, or diaphoresis). Preload is increased by increasing the return of circulating blood volume to the ventricles. o Controlling the loss of blood or body fluids and replacing fluids (blood transfusions and IV fluid administration). Afterload: resistance to ejection of blood from ventricle Inverse relationship between afterload and stroke volume. Afterload is increased by arterial vasoconstriction leading to decreased stroke volume. Arterial vasodilation reduces afterload because there is less resistance to ejection, and stroke volume increases. Contractility: ability of cardiac muscle to shorten in response to electrical impulse Refers to the force generated by the contracting myocardium. Enhanced by circulating catecholamines, sympathetic neuronal activity, and certain meds (digoxin, dopamine, dobutamine). Increased contractility results in increased stroke volume. Depressed by hypoxemia, acidosis, and certain meds (beta blockers) Ejection fraction: percent of end diastolic volume ejected with each heart beat. Ejection fraction of the normal left ventricle is 55% to 65%. Used as a measure of myocardial contractility. An ejection fraction of less than 40% indicated decreased left ventricular function and patient may require treatment for HF. Assessment of the Cardiovascular System:Based on several factors: Severity of the patient’s symptoms, Presence of risk factors, Practice setting, Purpose of the assessment Health History Chief complaint, History of Present Illness, Past medical, surgical history, Past family history, Past social history, Home medications, Allergies Common Symptoms Chest pain or discomfort (angina pectoris, ACS, dysrhythmias, valvular heart disease) Shortness of breath or Dyspnea (ACS, cardiogenic shock, HF, valvular heart disease) Peripheral edema, weight gain, abdominal distention due to enlarged spleen and liver or ascites (HF) Palpitations (Tachycardia from a variety of causes, including ACS, caffeine or other stimulants, electrolyte imbalances, stress, valvular heart disease, ventricular aneurysms) Fatigue referred to as vital exhaustion (early warning symptom of ACS, HF, or valvular heart disease, characterized by feeling tired or fatigued, irritable, and dejected). Dizziness, syncope, changes in level of consciousness (Cardiogenic shock, cerebrovascular disorders, dysrhythmias, hypotension, postural hypotension, vasovagal episode) Chest Pain Identify quantity of pain (0-10 SCALE), Identify location of pain, Identify quality of pain, Radiation of pain Associated signs/symptoms (diaphoresis or nausea) Events that precipitate the onset of symptoms and duration of symptoms, and measures that aggravate or relieve symptoms, Duration of pain Assess for other cardiac conditions Assess for other significant conditions (see p. 663-664) o Pneumonia, pulmonary embolism, Hiatal hernia, GERD, Costochondritis, Vascular Assessment Medications- A careful med history often uncovers common medication errors and causes for non-adherence to the medication regimen. Nutrition o Dietary modifications, exercise, weight loss, and careful monitoring are important strategies for managing three major cardiovascular risk factors: hyperlipidemia, hypertension, and diabetes. Diets restricted in sodium, fat, cholesterol, or calories are common Elimination: o Nocturia (awakening at night to urinate) is common in patients with HF Sleep, rest o Orthopnea the need to sit upright or stand to avoid feeling short of breath. o Sudden awakening with shortness of breath, called paroxysmal nocturnal dyspnea, is a symptom of worsening HF. Caused by the reabsorption of fluid from dependent areas of the body (arms and legs) back into the circulatory system within hours of lying in bed. Fluid shift increases preload and places increased demand of the heart of patients with HF, causing sudden pulmonary congestion. Physical Assessment General assessment Any deviations from the normal? o Heart as a pump (reduced pulse pressure, displaced PMI from fifth intercostal space midclavicular line, gallop sounds, murmurs) o Atrial/ventricular filling volumes and pressures (elevated jugular venous distention, peripheral edema, ascites, crackles, postural changes in BP). o Cardiac output (reduced pulse pressure, hypotension, tachycardia, reduced urine output, lethargy, or disorientation) o Compensatory mechanisms (peripheral vasoconstriction, tachycardia) Cardiac Specific General appearance o Evaluates the patient’s LOC o Changes may be attributed to inadequate perfusion of the brain from a compromised cardiac output of thromboembolic event (stroke). o Observe for signs of distress (pain, discomfort, SOB, anxiety). o Measure height and weight Assessment of skin and extremities o Skin color, temp, and texture for problems with arterial or venous circulation. o S/S of acute obstruction of arterial blood flow in the extremities, referred to as the six P’s are pain, pallor, pulselessness, paresthesia, poikilothermia (coldness), and paralysis. Assess frequently o Hematoma, or a localized collection of clotted blood in the tissue. o Edema is an abnormal accumulation of fluid in dependent areas o Prolonged capillary refill time indicates inadequate arterial perfusion o Clubbing of the fingers and toes indicates chronic hemoglobin desaturation and is associated with congenital heart disease. o Hair loss, brittle nails, dry or scaling skin, atrophy of the skin, skin color changes, and ulcerations due to reduced oxygen and nutrient supply BP o Pulse pressure is the difference between the systolic and the diastolic pressure. It is a reflection of stroke volume, ejection velocity, and systemic vascular resistance. Normally 30 to 40 mm Hg, indicates how well the patient maintains cardiac output. o Postural blood pressure changes- normal postural responses that occur when a person moves from a lying to a standing position include: A heart rate increase of 5 to 20 bpm above the resting rate Unchanged systolic pressure, or a decrease of up to 10 mm Hg Slight increase of 5 mm Hg in diastolic pressure o Postural (orthostatic) hypotension is a sustained decrease of at least 20 mm Hg in systolic BP or 10 mm Hg in diastolic BP within 3 minutes of moving from a lying or sitting to a standing position. Accompanied by dizziness, lightheadedness, or syncope. Arterial pulses o Pulse rate Normal pulse rate varies from a low of 50 bpm in healthy, athletic young adults to rates well in excess of 100 bpm after exercise o Pulse rhythm Heart rate could be counted by auscultating the apical pulse located at the PMI, for a full minute while simultaneously palpating the radial pulse. Disturbances of rhythm (dysrhythmias) often result in a pulse deficit, which is a difference between the apical and radial pulse rates. Pulse deficits occur with atrial fibrillation, atrial flutter, and premature ventricular contractions. o Pulse amplitude- Used to assess peripheral arterial circulation. +1 diminished +2 normal +3 moderately increased +4 markedly increased Jugular venous distention o Right sided heart function can be estimated by observing the pulsations of the jugular veins of the neck, which reflects central venous pressure (CVP). CVP is the pressure in the right atria of the right ventricle at the end of diastole. o This abnormality is observed is patients with right-sided HF, due to hypervolemia, pulmonary hypertension, and pulmonary stenosis. Heart Inspection and Palpation Heart Auscultation o Normal heart sounds S1, S2 produced by closure of the AV valves and the semilunar valves. The period between S1 and S2 – systole Period between S2 and S1 – diastole Only sounds heard during the cardiac cycle. S1 - tricuspid and mitral valve closure creates the first heart sound. “Lub” heard the loudest at the apical area. S2 – closure of the pulmonic and aortic valves. “Dub” heard the loudest over the aortic and pulmonic areas. Abnormal heart sounds S3, S4 gallops, opening snaps, systolic clicks, and murmurs. S3 and S4 gallops are heard during diastole. S3 “Dub” is heard early in diastole immediately after S2. “Lub-dub-DUB” S4 “Lub” occurs late in diastole. Heard just before S1.. “LUB lub-dub” Assessment of Lungs: Hemoptysis: pink, froth sputum is indicative of acute pulmonary edema. Cough: a dry, hacking cough from irritation of small airways is common in patients with pulmonary congestion from HF. [Show More]
Last updated: 1 year ago
Preview 1 out of 31 pages
.png)
Reviews( 0 )
Document information
Connected school, study & course
About the document
Uploaded On
Apr 08, 2021
Number of pages
31
Written in
Additional information
This document has been written for:
Uploaded
Apr 08, 2021
Downloads
0
Views
44

 Test Bank.png)
.png)

 Correct Study Guide, Download to Score A.png)
.png)

 Correct Study Guide, Download to Score A.png)

