*NURSING > EXAM > TESTBANK Primary Care, A Collaborative Practice, 5th Ed. by Buttaro. (Chapter 1 to Chapter 250). Ve (All)
TESTBANK Primary Care, A Collaborative Practice, 5th Ed. by Buttaro. (Chapter 1 to Chapter 250). Verified A+ Answers
Document Content and Description Below
Primary Care, A Collaborative Practice, 5th Ed. Chapter 1: The Evolving Landscape of Collaborative Practice Test Bank Multiple Choice 1. Which assessments of care providers are performed as par... t of the Value Based Purchasing initiative? Select all that apply. a. Appraising costs per case of care for Medicare patients b. Assessing patients’ satisfaction with hospital care c. Evaluating available evidence to guide clinical care guidelines d. Monitoring mortality rates of all patients with pneumonia e. Requiring advanced IT standards and minimum cash reserves Value Based Purchasing looks at five domain areas of processes of care, including efficiency of care (cost per case), experience of care (patient satisfaction measures), and outcomes of care (mortality rates for certain conditions. Evaluation of evidence to guide clinical care is part of evidence-based practice. The requirements for IT standards and financial status are part of Accountable Care Organization standards. REF: Value Based Purchasing 2. What was an important finding of the Advisory Board survey of 2014 about primary care preferences of patients? a. Associations with area hospitals b. Costs of ambulatory care c. Ease of access to care d. The ratio of providers to patients As part of the 2014 survey, the Advisory Board learned that patients desired 24/7 access to care, walk-in settings and the ability to be seen within 30 minutes, and care that is close to home. Associations with hospitals, costs of care, and the ratio of providers to patients were not part of these results. REF: The New Look of Primary Care 3. A small, rural hospital is part of an Accountable Care Organization (ACO) and is designated as a Level 1 ACO. What is part of this designation? a. Bonuses based on achievement of benchmarks b. Care coordination for chronic diseases c. Standards for minimum cash reserves d. Strict requirements for financial reporting A Level 1 ACO has the least amount of financial risk and requirements, but receives shared savings bonuses based on achievement of benchmarks for quality measures and expenditures. Care coordination and minimum cash reserves standards are part of Level 2 ACO requirements. Level 3 ACOs have strict requirements for financial reporting. REF: Accountable Care Organizations Chapter 2: Transitional Care Test Bank Multiple Choice 1. To reduce adverse events associated with care transitions, the Centers for Medicare and Medicaid Service have implemented which policy? a. Mandates for communication among primary caregivers and hospitalists b. Penalties for failure to perform medication reconciliations at time of discharge c. Reduction of payments for patients readmitted within 30 days after discharge d. Requirements for written discharge instructions for patients and caregivers As a component of the Affordable Care Act, the Centers for Medicare and Medicaid Service developed the Readmissions Reduction Program reducing payments for certain patients readmitted within 30 days of discharge. The CMS did not mandate communication, institute penalties for failure to perform medication reconciliations, or require written discharge instructions. REF: Transitional Care 2. According to Naylor’s transitional care model, which intervention has resulted in lower costs and fewer rehospitalizations in high-risk older patients? a. Coordination of post-hospital care by advanced practice nurses b. Frequent post-hospital clinic visits with a primary care provider c. Inclusion of extended family members in the outpatient plan of care d. Telephone follow up by the pharmacist to assess medication compliance Naylor’s transitional care model provided evidence that high risk older patients who had post- hospital care coordinated by an APN had reduced rehospitalization rates. It did not include clinic visits with a primary care provider, inclusion of extended family members in the plan of care, or telephone follow up by a pharmacist. REF: Transitional Care 3. Which approaches are among those recommended by the Agency for Healthcare Research and Quality to improve health literacy in patients? Select all that apply. a. Empowering patients and families b. Giving written handouts for all teaching c. Highlighting no more than 7 key points d. Repeating the instructions e. Supplementing teaching with visual aids , D, E AHRQ recommends using clear, simple language, highlighting 3 to 5 key points, using pictures or visual aids, repeating the instructions, using Teach Back, and empowering patients. Written communication is not part of the recommendations. REF: Health Literacy Chapter 3: Translating Research Into Clinical Practice Test Bank Multiple Choice 1. Which is the most appropriate research design for a Level III research study? a. Epidemiological studies b. Experimental design c. Qualitative studies d. Randomized clinical trials The experimental design is the most appropriate design for a Level III study. Epidemiological studies are appropriate for Level II studies. Qualitative designs are useful for Level I studies. Randomized clinical trials are used for Level IV studies. REF: Level III Research/Experimental Design 2. What is the purpose of clinical research trials in the spectrum of translational research? a. Adoption of interventions and clinical practices into routine clinical care b. Determination of the basis of disease and various treatment options c. Examination of safety and effectiveness of various interventions d. Exploration of fundamental mechanisms of biology, disease, or behavior Clinical research trials are concerned with determining the safety and effectiveness of interventions. Adoption of interventions and practices is part of clinical implementation. Determination of the basis of disease and treatment options is part of the pre-clinical research phase. Exploration of the fundamental mechanisms of biology, disease, or behavior is part of the basic research stage. REF: Translational Science Spectrum 3. What is the purpose of Level II research? a. To define characteristics of interest of groups of patients b. To demonstrate the effectiveness of an intervention or treatment c. To describe relationships among characteristics or variables d. To evaluate the nature of relationships between two variables Level II research is concerned with describing the relationships among characteristics or variables. Level I research is conducted to define the characteristics of groups of patients. Level II research evaluates the nature of the relationships between variables. Level IV research is conducted to demonstrate the effectiveness of interventions or treatments. REF: Level II Research Chapter 4: The Patient, the Provider, and Primary Care: An Integrated Perspective Test Bank Multiple Choice 1. A patient takes glucosamine chondroitin to help control osteoarthritis pain. Which medications, taken in conjunction with this medication, are of concern? a. Anticholinergic drugs b. Beta blocker medications c. Blood-thinning agents d. Narcotic analgesics Glucosamine chondroitin can prolong bleeding if taken with other blood-thinning agents. It does not have anticholinergic effects, cardiac effects or analgesic effects. REF: Alternative Therapies for Common Chronic Conditions/Joint Pain 2. The provider learns that a patient is taking herbal supplements for a variety of reasons. What is an important point to discuss with this patient about taking such supplements? a. Because they are not FDA approved, they are not safe b. Dietary supplements are safer than most prescription medications c. Many supplements lack clear clinical evidence of efficacy d. Supplements should not be taken with prescription medications Many dietary supplements lack clinical evidence to support their use. Even though they are not FDA approved, federal law mandates that the products are safe and cannot make misleading claims about use. Supplements are not necessarily safer than prescription drugs. Supplements may be taken with prescription medications as long as the effects, side effects, and drug interactions are known. REF: Alternative Therapies for Common Chronic Conditions 3. Which dietary supplements have shown some effectiveness in reducing blood pressure in patients with hypertension? Select all that apply. a. Chromium picolinate b. Cinnamon c. CoQ10 d. Garlic extract e. L-arginine CoQ10, garlic extract, and L-arginine have demonstrated effectiveness in reducing blood pressure in some studies. Chromium picolinate and cinnamon have been studied for effects on glucose tolerance and fasting glucose. REF: Alternative Therapies for Common Chronic Conditions/Prehypertension and Hypertension Chapter 5: Population-Based Care for Primary Care Providers Test Bank Multiple Choice 1. Which are key components of the Patient-Centered Medical Home? Select all that apply. a. Access to care b. Comprehensive care c. Coordination of care d. Provision of care by a single provider e. Storage of medical records The Patient-Centered Medical Home is a team-based approach to providing care that is accessible, comprehensive, coordinated, longitudinal and high quality. It is not provided by a single provider, but is managed as a team. The original concept had to do with where medical records are stored, but this is not the working definition today. REF: The Patient-Centered Medical Home 2. The chronic care model (CCM) was developed to manage patients with complicated chronic conditions because the traditional acute care model a. could not provide efficient and cost-effective chronic care. b. did not meet longitudinal health care needs for this population. c. did not offer ambulatory care services for these patients. d. put patients and families at the center of care. The chronic care model was developed based on the recognition that the traditional acute care model did not meet longitudinal health care needs of patients with chronic and complicated conditions, not because of inefficiencies or costs. The traditional model does include ambulatory care, but that is not the focus. The traditional model does not typically place patients at the center of care. REF: Chronic Care Model 3. What are functions of patient registries in the chronic care model? Select all that apply. a. Alerting providers to medication interactions b. Identifying appropriate specialists for referral c. Recommending routine screenings d. Reminding providers about immunizations e. Transmitting clinical data about patients Patient registries are used to help manage patients at risk and include alerting providers about medication interactions, recommending routine screenings, reminders for immunizations, and transmitting clinical data. They are not used to identify or recommend providers or specialists. REF: Chronic Care Model/Clinical Information Systems Chapter 6: Health Literacy, Health Care Disparities, and Culturally Responsive Primary Care Test Bank Multiple Choice 1. A primary care provider administers the “Newest Vital Sign” health literacy test to a patient newly diagnosed with a chronic disease. What information is gained by administering this test? a. Ability to calculate data, along with general knowledge about health b. Ease of using technology and understanding of graphic data c. Reading comprehension and reception of oral communication d. Understanding of and ability to discuss health care concerns The “Newest Vital Sign” tests asks patients to look at information on an ice cream container label and answer questions that evaluate ability to calculate caloric data and to grasp general knowledge about food allergies. It does not test understanding of technology or directly measure reading comprehension. It does not assess oral communication. The “Ask Me 3” tool teaches patients to ask three primary questions about their health care and management. REF: Health Literacy Assessment 2. A female patient who is from the Middle East schedules an appointment in a primary care office. To provide culturally responsive care, what will the clinic personnel do when meeting this patient for the first time? a. Ensure that she is seen by a female provider b. Include a male family member in discussions about health care c. Inquire about the patient’s beliefs about health and treatment d. Research middle eastern cultural beliefs about health care It is important not to make assumptions about beliefs and practices associated with health care and to ask the patient about these. While certain practices are common in some cultural and ethnic groups, assuming that all members of those groups follow those norms is not culturally responsive. REF: Address Cultural Variations Among Diverse Patient Groups 3. What is the main reason for using the REALM-SF instrument to evaluate health literacy? a. It assesses numeracy skills. b. It enhances patient-provider communication. c. It evaluates medical word recognition. d. It measures technology knowledge. The REALM-SF is an easy and fast tool that measures medical word recognition. It does not evaluate numeracy. The “Ask Me 3” tool enhances patient-provider communication. This tool does not evaluate understanding of technology. REF: Health Literacy Assessment Chapter 7: Genetic Considerations in Primary Care Test Bank Multiple Choice 1. A patient expresses concern that she is at risk for breast cancer. To best assess the risk for this patient, what is the best initial action? a. Ask if there is a family history of breast cancer b. Gather and record a three-generation pedigree c. Order a genetic test for the breast cancer gene d. Recommend direct-to-consumer genetic testing The three-generation pedigree is the best way to evaluate genetic risk. Asking about a family history is not a systematic risk assessment and doesn’t specify who in the family has the history or whether there is a pattern. Genetic testing and DTC genetic testing are not the initial actions when assessing genetic risk. REF: Gathering a Family History 2. A patient asks about direct-to-consumer (DTC) genetic testing. What will the provider tell the patient? a. It is not useful for identifying genetic diseases. b. Much of the information does not predict disease risk. c. The results are shared with the patient’s insurance company. d. The results must be interpreted by a provider. DTC testing gives a lot of information, but much of it does not contribute to disease prediction, since mutations are not necessarily related to specific diseases. The tests are useful, but must be interpreted accurately. The results are confidential and do not have to be interpreted by a provider. REF: Direct-to-Consumer (DTC) Genetic Testing Chapter 8: Risk Management Test Bank Multiple Choice 1. What are some causes for failures or delays in diagnosing patients resulting in malpractice claims? Select all that apply. a. Failing to recognize a medication complication b. Failing to request appropriate consultations c. Improper performance of a treatment d. Not acting on diagnostic test results e. Ordering a wrong medication , D Failing to obtain consultations when indicated or not acting on diagnostic test results can lead to diagnosis-related failures. Failing to recognize medication complications and ordering a wrong medication lead to medication prescribing allegations. Improper performance of a treatment can lead to treatment related malpractice claims. REF: Nurse Practitioner Malpractice Claims 2. What is an important part of patient care that can minimize the risk of a formal patient complaint even when a mistake is made? a. Ensuring informed consent for all procedures b. Maintaining effective patient communication c. Monitoring patient compliance and adherence d. Providing complete documentation of visits Effective patient communication is key to building trust and rapport and ineffective communication is a predictor for malpractice claims. The other items are important aspects of care and may help the provider during the investigation of a claim, but do not minimize the risk. REF: Communication Issues Chapter 9: Adolescent Issues Test Bank Multiple Choice 1. Which behavior is most characteristic of early adolescence? a. Arguing with parents and teachers b. Assimilating adult roles and thinking c. Exhibiting fatigue more frequently d. Experimenting with sex and risky behaviors Early adolescents challenge authority, experience wide mood swings, reject the ideation of childhood, and can be argumentative and disobedient. Middle adolescents experience fatigue and begin experimenting with sex and risky behaviors. Late adolescents begin to assimilate adult roles. REF: Introduction 2. What is the initial sign of puberty in the adolescent male? a. Deepening of the voice b. Elongation of the penis c. Nocturnal emissions d. Testicular enlargement Testicular enlargement is the initial sign of puberty in adolescent males. Penile growth and nocturnal emissions occur later as does deepening of the voice. REF: Physical Development 3. A parent reports that an adolescent child does well in school but seems to consistently make poor decisions about activities with friends. What will the practitioner recommend as an approach to help the adolescent make better decisions? a. Correcting the adolescent’s decisions and judgments b. Listening without making suggestions about choices c. Making decisions for the adolescent to provide guidance d. Providing factual information about appropriate behavior Test Bank 2 Listening without correcting is the best approach to help adolescents learn to make good decisions. Correcting the decisions, making decisions for the adolescent, or giving information that is unsolicited are not recommended. REF: Cognitive Development Chapter 10: LGBTQ Patient Care Test Bank Multiple Choice 1. Which is the most important factor limiting access to health care for sexual and gender minorities? a. Lack of familial support for SGM members b. Laws prohibiting full marriage equality c. Risky coping behaviors among SGM members d. Social stigma about being in this population Since most people get health insurance through their employer or their spouse s employer, states which do not allow full marriage equality limit access to health care for LGBTQ people. The other causes are important, but this is the leading cause. REF: Introduction 2. What is the medical diagnostic term used to identify transgender patients? a. Gender dysphoria b. Gender expression disorder c. Gender identity disorder d. Gender role unconformity Gender dysphoria is the term used to identify transgender patients in order to justify the medical necessity of treatments for transgender patients. It replaces the previous “gender identity disorder” designation. REF: Access to Care Chapter 11: Pregnancy and Prenatal Care Test Bank Multiple Choice 1. A woman who is currently pregnant reports that she has had three previous pregnancies: twins delivered at 35 weeks gestation (both living), one at 38 weeks gestation (living), and one miscarriage at 16 weeks gestation. How will this be recorded as her G/TPAL in her electronic medical record? a. G4P:1113 b. G4P:1213 c. G5P:1113 d. G5P:1213 Using the notation G (number of pregnancies), T (term deliveries), P (preterm deliveries), A (abortions – elective or spontaneous), L (living children), this patient is G4P:1113. She is in her fourth pregnancy, so is G4. She has had one delivery at 38 weeks or more, one delivery (of twins) at less than 36 weeks gestation, one spontaneous abortion, and has three living children. REF: Gravidity and Parity 2. A pregnant woman reports not having had any vaccinations as a child but requests vaccines during her pregnancy. Which vaccines may be given? Select all that apply. a. HPV b. Inactivated influenza c. Live, attenuated influenza d. MMR e. Tdap f. Varicella , B, E Tdap is recommended to pregnant woman, optimally between 27 and 36 weeks gestation. Inactivated is strongly recommended and may be given at any point in the pregnancy. Hepatitis B is given to women at risk if needed. Live, attenuated influenza vaccine, MMR, and varicella vaccines are not recommended during pregnancy. REF: Health History 3. A pregnant woman who is overweight has no previous history of hypertension or diabetes. Her initial screening exam reveals a blood pressure of 140/90 and a fasting blood glucose of 128 mg/dL. What will the practitioner do? a. Initiate insulin therapy b. Monitor blood pressure and fasting blood glucose closely c. Prescribe an antihypertensive medication d. Refer the patient to a high-risk pregnancy specialist This woman, although she has no previous history of HTN or DM, is at elevated risk because of obesity. Her initial screening lab values are at the high end of normal, indicating potential development of gestational HTN and gestational DM. The initial response of the practitioner should be to monitor the patient closely and consider treatment at the first signs of development of these complications. Referral is warranted when these conditions become severe. REF: Hypertension/Diabetes Chapter 12: Lactation Guidance Test Bank Multiple Choice 1. An infant who has just begun nursing develops hyperbilirubinemia. What will the provider tell the mother? a. To decrease the frequency of breastfeeding b. To supplement feedings with extra water c. To switch to formula until the bilirubin level drops d. To use a breast pump to increase her milk supply Infants with suboptimal breastfeeding can have starvation jaundice and mothers should be encouraged to increase the frequency of breastfeeding and should be offered a breast pump to increase milk supply. It is not recommended to supplement with water or sugar water or to switch to formula. REF: Physiologic Jaundice 2. The mother of a 3-day-old newborn reports that her infant nurses every 4 hours during the day and sleeps 6 hours at night. What will the provider recommend? a. Awakening the baby every 3 hours to nurse b. Continuing this schedule until the infant is 6 months old c. Ensuring that her infant nurses for 15 to 20 minutes each time d. Pumping her breasts to maintain her milk supply Newborn infants should nurse 8 to 12 times daily and mothers should be encouraged to awaken a sleepy baby to nurse every 3 hours or more often. The feedings will gradually space out as the infant is older. REF: The First Few Days 3. A mother who has been breastfeeding her infant for several weeks develops a fever, breast warmth, and breast tenderness. What will the provider recommend? a. Ice packs and decreased frequency of nursing b. Ice packs and increased frequency of nursing c. Warm packs and decreased frequency of nursing d. Warm packs and increased frequency of nursing This mother has symptoms of mastitis. She should be encouraged to use warm packs for comfort and to increase the frequency of nursing to relieve the pressure. REF: Mastitis Chapter 13: Aging and Common Geriatric Syndromes Test Bank Multiple Choice 1. When prescribing medications to an 80-year-old patient, the provider will a. begin with higher doses and decrease according to the patient’s response. b. consult the Beers list to help identify potentially problematic drugs. c. ensure that the patient does not take more than five concurrent medications. d. review all patient medications at the annual health maintenance visit. The Beers list provides a list of potentially inappropriate medications in all patients age 65 and older and helps minimize drug-related problems in this age group. Older patients should be started on lower doses with gradual increase of doses depending on response and side effects. Patients who take five or more drugs are at increased risk for problems of polypharmacy, but many will need to take more than five drugs; providers must monitor their response more closely. Medications should be reviewed at all visits, not just annually. REF: Polypharmacy/Consequences of Polypharmacy/Management 2. An 80-year-old woman who lives alone is noted to have a recent weight loss of 5 pounds. She appears somewhat confused, according to her daughter, who is concerned that she is developing dementia. The provider learns that the woman still drives, volunteers at the local hospital, and attends a book club with several friends once a month. What is the initial step in evaluating this patient? a. Obtain a CBC, serum electrolytes, BUN, and glucose b. Ordering a CBC, serum ferritin, and TIBC c. Referring the patient to a dietician for nutritional evaluation d. Referring the patient to a neurologist for evaluation for AD Patients with weight loss, confusion, and lethargy are often dehydrated and this should be evaluated by looking at Hgb and Hct, electrolytes, and BUN. This patient is currently leading an active life, so the likelihood that recent symptoms are related to AD, although this may be evaluated if dehydration is ruled out. Anemia would be a consideration when dehydration is ruled out. Referrals are not necessary unless initial evaluations suggest that malnutrition or AD is present. REF: Dehydration/Pathophysiology/Clinical Presentation/Physical Examination 3. The practitioner is establishing a plan for routine health maintenance for a new female client who is 80 years old. The client has never smoked and has been in good health. What will the practitioner include in routine care for this patient? Select all that apply. a. Annual hypertension screening b. Baseline abdominal aorta ultrasound c. Colonoscopy every 10 years d. One-time hepatitis B vaccine e. Pneumovax vaccine if not previously given f. Yearly influenza vaccine For older clients a one-time pneumovax is given after age 65. Influenza vaccine should be given every year. Hypertension screening should be performed at each office visit, not just annually. An abdominal aorta US is performed once for every smoking male. Colonoscopy is performed every 10 years after age 50, but not after age 74. REF: Table 13-1: Recommended Screening and Immunizations Chapter 14: Palliative and End-of Life Care Test Bank Multiple Choice 1. A patient who is near death is exhibiting signs of agitation, anxiety, and intractable pain. When discussing palliative sedation with this patient’s family, what will be discussed? Select all that apply. a. The chance that refractory symptoms will be alleviated b. The fact that this is an intervention of last resort c. The likelihood that the patient will develop dependence on the drugs d. The need for informed consent from the patient and family e. The possibility that this measure may hasten death , D, E Palliative sedation is used as a treatment of last resort for patients whose symptoms are intolerable or refractory. Patients, if possible, and family members must give informed consent. This treatment has the possibility of hastening death by inhibiting respirations. Symptoms will not be alleviated by using the measure. The chance of drug dependence is irrelevant in this situation. REF: Palliative Sedation for Management of Intractable Symptoms in Patients Near Death 2. When should palliative care be initiated by a primary care provider? a. After an ill patient asks for Hospice services b. As part of routine health maintenance c. When a patient is diagnosed with a serious disease d. When an interdisciplinary team is formed to manage a disease Palliative care support begins with an understanding of a patient’s preferences and helping the patient to identify goals of care. Health care providers should initiate such discussions as a component of the initial history of adults regardless of age or health status. Palliative care services may be ordered when a patient is diagnosed with a serious disease; waiting until the patient asks for Hospice services or when an interdisciplinary team is formed increases the chances of providing end-of-life care that does not meet the patient’s needs. REF: Palliative Care/Advance Care Planning 3. When using the “Five Wishes” approach to documenting patient preferences for end-of-life care, the provider will document which types of preferences? Select all that apply. a. A directive to avoid calling 911 at the time of death b. A specific list of treatments the patient does not want c. How much information to give various family members d. The level of sedation versus alertness the patient desires e. The people designated to make care decisions for the patient , D, E The Five Wishes approach addresses the type of care a patient wants as a disease progresses and is less defensive than the traditional advance directive which indicates the type of care a patient does not want. Calling 911 may be done without requiring resuscitation if the patient has an appropriate advanced directive in place. REF: Advance Care Planning Chapter 15: Obesity and Weight Management Test Bank Multiple Choice 1. A woman who is obese has a neck circumference of 16.5 cm. Which test is necessary to assess for complications of obesity in this patient based on this finding? a. Electrocardiography b. Gallbladder ultrasonography c. Mammography d. Polysomnography Women with a neck circumference greater than 16 cm have an increased risk of obstructive sleep apnea and should have polysomnography to assess for this complication. The other tests may be necessary for obese patients, but are not specific to this finding. REF: Physical Examination/Diagnostics 2. Which medications are associated with weight gain? Select all that apply. a. Antibiotics b. Antidepressants c. Antihistamines d. Insulin analogs e. Seizure medications Antidepressants, antihistamines, insulin and insulin analogs, and seizure medications are all associated with weight gain. Antibiotics are not associated with weight gain. REF: Pharmaceuticals Associated with Weight Gain Chapter 16: Lifestyle Management Test Bank Multiple Choice 1. A 60-year-old patient who leads a sedentary lifestyle has expressed an interest in beginning an aerobic exercise program. What will the provider include when counseling this patient about this program? a. Begin with a 45 to 60 minute workout b. Include a 1 to 2 minute warm up before exercise c. Maintain a heart rate between 80 and 128 beats per minute d. Stretching should be performed prior to activity The heart rate should be kept between 50% and 80% of the maximum heart rate (220 minus the patient’s age = 160), which is 80 to 128 beats per minute. Patients who are not conditioned should begin with a 20 minute workout; conditioned individuals may increase up to 60 minutes. The warm up should be 3 to 5 minutes and longer if it is cold. Stretching is performed after the activity when the muscles are warm. REF: Exercise 2. Routine screening blood tests at an annual physical exam reveal a fasting glucose level of 125 mg/dL and a hemoglobin A1C of 6.2%. What will the provider do, based on these results? a. Evaluate the patient for impaired glucose tolerance b. Reassure the patient that these are normal values c. Suggest that the patient begin an exercise program d. Tell the patient that these results indicate diabetes The fasting blood glucose level is normal, but the HgA1C indicates impaired glucose tolerance. If the HgA1C were greater than 6.4%, the patient would be diagnosed with diabetes. Until the results are evaluated, suggestions for treatment are not indicated. REF: Diabetes 3. The primary care provider is screening a patient using the CAGE criteria. What will the provider include in this assessment? Select all that apply. a. Number of times per week eaten in restaurants b. Sodium and sugar intake c. Sources of daily dairy intake d. Total number of servings of fruits and vegetables e. Types of meats and proteins The CAGE questionnaire is designed to evaluate the intake of saturated fat and cholesterol, so the provider will ask about sources of dairy, the number of times eating foods not made at home, and the types of meats and proteins eaten. The questionnaire does not evaluate for sodium, sugar, fruits, or vegetables. REF: Box 16-1: Dietary CAGE Questions for Assessment of Intake of Saturated Fat and Cholesterol Chapter 17: Routine Health Screening and Immunizations Test Bank Multiple Choice 1. A 50-year-old female patient has a blood pressure of 118/72 mm Hg, a negative family history for breast and ovarian cancer, a normal Pap smear 2 years prior, and a Framingham risk screening within normal limits. Which should be part of this patient’s routine annual well-patient exams? a. Bone mineral density screening b. Breast cancer screening and mammogram c. Cervical cancer screening with a Pap test d. Lipid screening and cholesterol tests The American Cancer Society recommends yearly mammogram at age 40. Bone mineral density screening begins at age 50 to 64, based on risk. Cervical cancer screening should be performed every 3 years unless there is increased risk. Lipid screening and cholesterol is performed annually if there is increased risk according to the Framingham guidelines. REF: Table 17-1: Screening Tests for Women/Table 17-4: Comparison of American Cancer Society and USPSTF Screening Guidelines for the Early Detection of Cancer in Asymptomatic Individuals 2. A 55-year-old patient who had influenza in the previous influenza season asks about the flu vaccine. What will the provider tell the patient? a. Having influenza vaccine confers lifetime immunity b. The FluMist vaccine may be used each year c. The Fluzone High-Dose vaccine is recommended d. The trivalent influenza vaccine is indicated annually Because the strains of influenza vary from year to year, annual immunization with TIV is indicated for all persons. Lifetime immunity is not conferred with infection. The Flu Mist is used in persons 50 years of age and younger. The Fluzone High-Dose vaccine is used in patients older than 65 year. REF: Influenza Vaccine 3. A 60-year-old patient with a previous history of shingles asks about the herpes zoster vaccine. What will the provider recommend? a. A series of two herpes zoster vaccinations b. A single dose of herpes zoster vaccine c. No herpes zoster vaccine is necessary d. Prophylactic vaccination if exposed to chicken pox All patients 50 years and older should have a single dose of herpes zoster vaccine regardless of previous herpes zoster infection. REF: Herpes Zoster Vaccine Chapter 18: Principles of Occupational and Environmental Health in Primary Care Test Bank Multiple Choice 1. A patient who has a history of working around asbestos and silica fibers is concerned about developing lung disease. The primary care provider determines that the patient has a previous history of asthma as a child and currently has frequent episodes of bronchitis. A physical examination is normal and pulmonary function tests and radiographs are negative. What action is correct? a. Reassure the patient about the normal findings b. Refer the patient to an occupational health specialist c. Request a workplace environmental assessment d. Suggest that the patient follow up with a pulmonologist Patients with environmental exposure may not have symptoms or positive findings. Because this patient reports frequent bronchitis, this should be followed up with an occupational health specialist who can evaluate the degree of exposure and perform further testing. Normal findings are not necessarily reassuring. The occupational specialist may request an environmental assessment. Pulmonologists are not trained in occupational health. REF: Occupational Respiratory Diseases 2. During a pre-placement screening for a person hired for a job requiring heavy lifting, a primary care provider notes that the new employee has environmental allergies, a history of GERD, recurrent eczema, a previous history of an ankle fracture, and normal lower back strength and flexibility. A urine drug screen is negative. What will be included in the report to the employer? Select all that apply. a. GERD history b. History of allergies and eczema c. History of ankle fracture d. Lower back screening results e. Urine drug screening results , E Only findings related to the ability of the individual to perform position requirements for the job are included in the report. Other findings should not be included, even though they may need to be addressed. REF: Pre-Placement Health Evaluation Chapter 19: College Health Test Bank Multiple Choice 1. A female freshman college student tells the primary care provider at the student health center that she has a history of anorexia nervosa that has been well-controlled for several years. What will the provider recommend for this student? a. Dietary counseling b. Participation in sports c. Regular weight assessments d. Stress management strategies Students with previous eating disorders may regress when stressed, so stress management is essential. Unless she begins to regress, dietary counseling is not indicated. Many who participate in sports will develop eating disorders in order to control weight. It is not necessary to evaluate weight regularly. REF: Eating Disorders and Weight Management 2. A female college student seeks information about emergency contraception. What is the most important part of the assessment of this patient? a. Cultural considerations for use of contraception b. Feelings of guilt about a possible pregnancy c. Possible concerns about confidentiality d. The female’s sense of control in sexual situations Because college women are at greater risk for sexual violence and assault, a request for emergency contraception must be followed by an evaluation of possible rape or assault. The other considerations may be part of the assessment, but are not as important as determining whether a rape has occurred. REF: Reproductive, Substance, and Safety Issues Chapter 20: Health Care of the International Traveler Test Bank Multiple Choice 1. An international traveler plans to travel to Kenya in sub-Saharan Africa. Which is an important disease precaution for this person? a. Carrying chloroquine to take as needed b. Starting prophylactic doxycycline before travel c. Taking precautions against Chikungunya fever d. Understanding how Ebola virus is transmitted Malaria is a greater concern worldwide than Ebola virus and Chikungunya fever, although both are emerging diseases. Travelers should take antimalarial medications and, in this part of Africa, where there is widespread resistance to chloroquine, doxycycline is a better choice as prophylaxis. Even when chloroquine is appropriate, it must be taken prior to travel and not as needed. Chikungunya fever is a disease of the Western Hemisphere, especially in the Caribbean. Ebola virus is epidemic in western Africa and not in Kenya. REF: Introduction/Medications and Prescriptions/Malaria/4: Provider Toolbox for Travelers: Brochures, Vaccines, and Medications 2. A patient returns home from travel in Africa and experiences chronic, non-bloody diarrhea. The patient reports frequent bloating and flatulence with a “rotten egg” smell. What is the treatment for this type of diarrhea? a. Azithromycin b. Ciprofloxacin c. Metronidazole d. Rifampin This patient has symptoms characteristic of Giardia lamblia and should be treated with metronidazole. Azithromycin is given for Campylobacter infection, which is a bacterial cause. Ciprofloxacin is used for bacterial infections such as Salmonella or Shigella, which cause bloody diarrhea. Rifampin is used for non-invasive strains of E. coli. REF: Food and Water Precautions and Traveler’s Diarrhea 3. A patient who is planning international travel to a developing country asks the provider about vaccinations. Which is true about pre-travel vaccines? Test Bank 2 a. Country-specific guidelines are provided by individual embassies. b. Malaria vaccine is the most important vaccine for worldwide travel. c. Requirements should be reviewed at least 6 to 8 weeks prior to travel. d. There are at least five required vaccines for entry into certain countries. Patients seeking immunizations prior to international travel should have these reviewed at least 6 to 8 weeks prior so that antibody responses and completion of vaccine series may occur. Country-specific guidelines may be found on the CDC website. Malaria is not prevented by vaccine, but by prophylactic antimalarial drugs. There are only two vaccines that are required. REF: Immunizations/Medications and Prescriptions/Malaria Chapter 21: Presurgical Clearance Test Bank Multiple Choice 1. Which factors determine which diagnostic tests should be performed in a presurgical clearance evaluation? Select all that apply. a. Patient’s age b. Patient’s comorbidities c. Previous surgeries d. Surgeon’s preference e. Type of anesthetic agent planned The patient’s age and comorbidities, surgeon preference, and the type of anesthetic planned all determine which presurgical diagnostic tests will be performed. The patient’s previous surgeries do not determine presurgical testing. REF: Diagnostics 2. Which patient should have pulmonary function testing as part of the presurgical exam? a. A patient older than 60 years of age b. A patient undergoing major intra-thoracic surgery c. A patient with a history of pneumonia in the last 2 years d. A patient with diabetes and morbid obesity Any patient undergoing major thoracic surgery should have pulmonary function testing. Age over 60 years, a history of pneumonia, and diabetes and obesity do not require pulmonary function testing unless there is comorbid COPD. REF: Table 21-1: Tests for Presurgical Clearance Chapter 22: Preparticipation Sports Physical Test Bank Multiple Choice 1. During a pre-participation sports physical, the examiner notes a difference in strength of the patient’s radial and femoral pulses with the femoral pulses being weaker. What will the provider do? a. Evaluate for orthostatic hypotension b. Obtain Doppler studies of lower extremity circulation c. Reassure the patient that this is a normal finding d. Refer the patient for a cardiologic exam Differences in strength between radial and femoral pulses may indicate coarctation of the aorta and should be evaluated by a cardiologist. This finding does not indicate orthostatic hypotension. The likelihood of decreased circulation is low in a young athlete. REF: Physical Examination 2. An overweight adolescent who takes metformin has type 2 diabetes with a HgA1c of 8.5% and asks about sports participation. What will the provider recommend? a. Losing weight prior to initiating sports participation b. Participation in strenuous sports to help with weight loss c. Referral to the endocrinologist for sports clearance d. Switching to insulin therapy prior to participation Patients with poorly controlled diabetes should be referred to a specialist prior to clearance for sports participation. This patient has an elevated HgA1C, indicating poor control. The endocrinologist may suggest the other options, but the primary care provider should not clear this patient for participation in sports. REF: Medical Clearance 3. A high-school adolescent is being screened for fitness before participating in sports. The adolescent has a normal examination and the examiner notes S1 and S2 heart sounds without murmur, normal blood pressure, and equal pulses. The parent reports that the adolescent’s father has a history or Wolff-Parkinson-White syndrome, which has been treated. What will the provider do? a. Clear the adolescent to play sports Test Bank 2 b. Perform an electrocardiogram c. Refer the adolescent to a cardiologist d. Tell the adolescent that sports are not allowed A positive family history of Wolff-Parkinson-White syndrome requires physician consultation or referral before medical clearance can be given. The adolescent has a normal heart rate and physical exam, so the ECG may not yield significant or useful results. The examiner cannot clear the adolescent without consulting with a specialist. The adolescent may be cleared for sports by the specialist. REF: Medical Clearance Chapter 23: Disaster/Emergency Preparedness and Response in Primary Care Test Bank Multiple Choice 1. What is included in the mitigation phase of emergency management? a. Debriefing and review b. Drills and exercises c. Identification of risks d. Use of Incident Command System The mitigation phase involves identification of risks. Debriefing and review occurs during the recovery phase. Drills and exercises are part of the preparedness phase. Use of an Incident Command System is part of the response phase. REF: Preparing the Primary Care Office for Small-Scale Emergencies/Disasters 2. A primary care office develops a plan for what to do in case of a fire in the building. As part of the plan, two people are to take charge in case of this emergency. Which phase of emergency planning does this represent? a. Mitigation b. Preparedness c. Response d. Recovery The response phase involves identification of those who will be in command in case of an emergency and identification of the roles of other personnel. The mitigation phase involves identification of risks. Debriefing and review occurs during the recovery phase. Drills and exercises are part of the preparedness phase. REF: Preparing the Primary Care Office for Small- Scale Emergencies/Disasters Chapter 24: Acute Bronchospasm Test Bank Multiple Choice 1. A patient with asthma has been given three bronchodilator treatments but continues to have wheezing and shortness of breath. The nurse caring for the patient notes an oxygen saturation of 90% on room air. What action is indicated? a. Administer oxygen and continue to monitor the patient b. Contact the respiratory therapist to administer another treatment c. Notify the patient’s physician immediately d. Reassure the patient that the treatments will take effect soon Patients with bronchospasm who have oxygen saturations less than 92% on room air and who fail to improve with nebulizer treatment given three times, need physician consultation. While oxygen administration and further nebulizer treatments may be indicated, it is incorrect to continue to monitor the patient without notifying the physician. REF: Acute Bronchospasm/Physician Consultation 2. Which clinical findings are worrisome in a patient experiencing acute bronchospasm, requiring immediate treatment? Select all that apply. a. A silent chest after previously wheezing b. Decreasing blood pressure c. Presence of an urticarial rash d. Pulsus paradoxus of 10 mm Hg e. Wheezing on both inspiration and expiration A silent chest indicates severe spasm and is an ominous sign. Decreasing blood pressure and urticarial rash are present with anaphylaxis, which is a respiratory emergency requiring oxygen, diphenhydramine or epinephrine. A pulsus paradoxus greater than 25 mm Hg is worrisome. Wheezing on inspiration and expiration is a common finding and not necessarily an emergency. REF: Acute Bronchospasm/Physical Examination/Differential Diagnosis 3. Which symptom in a patient with asthma indicates severe bronchospasm? Test Bank 2 a. Breathlessness with minimal activity or eating b. Pausing to breathe while attempting to talk c. Repetitive, spasmodic coughing at night d. Wheezing after exposure to a trigger Inability to speak a full sentence without pausing to breathe indicates severe bronchospasm. Breathlessness, repetitive and spasmodic coughing, and wheezing are all common signs of bronchospasm and do not necessarily indicate severe bronchospasm. REF: Acute Bronchospasm/Clinical Presentation Chapter 25: Anaphylaxis Test Bank Multiple Choice 1. A child with no previous history of asthma is brought to the emergency department with wheezing, stridor, and shortness of breath. When the child is started on oxygen and given a nebulized bronchodilator treatment, the treatment team notes a wheal and flare rash on the child’s trunk. What medication will be given immediately? a. Inhaled racemic epinephrine b. Intramuscular epinephrine c. Intravenous diphenhydramine d. Intravenous ranitidine The patient has signs of anaphylaxis and should be given IM or SC epinephrine immediately as first-line therapy, with this repeated every 5 to 20 minutes as needed to prevent cardiovascular shock. Inhaled epinephrine is used for acute upper airway bronchospasm. Diphenhydramine and ranitidine are given as second-line treatment after epinephrine is administered or for mild, non- life-threatening allergic reactions. REF: Anaphylaxis/Management 2. A man self-administers epinephrine using an Epi-Pen after experiencing a bee sting and developing angioedema and wheezing. What should the man do next? a. Obtain transport to an emergency department immediately b. Repeat the epinephrine dose if needed and notify a physician of the episode c. Resume normal activity if symptom free after 30 to 60 minutes d. Take oral diphenhydramine and report any symptoms to a provider The man has a history of anaphylaxis and experienced symptoms after contact with a trigger. The Epi-Pen should be used immediately, but does not prevent the need for follow up in an emergency department for close observation, since continued reaction to the allergen can occur for 6 to 8 hours. The epinephrine dose may be given if needed before emergency personnel arrive, but a second dose is not sufficient to prevent ongoing reaction to the allergen. REF: Anaphylaxis/Management/Education and Health Promotion Chapter 26: Bites and Stings Test Bank Multiple Choice 1. A patient is seen in the emergency department after experiencing a spider bite. The spider is in a jar and is less than one inch in size, yellow-brown, and has a violin-shaped marking on its back. Depending on the patient’s symptoms, which treatments and diagnostic evaluations may be ordered? Select all that apply. a. Airway management b. An acute abdominal series c. Antivenom therapy d. CBC, BUN, electrolytes, and creatinine e. Coagulation studies f. Tetanus prophylaxis The spider is a brown recluse. If the patient exhibits systemic symptoms, laboratory workup, including CBC, BUN, creatinine, electrolytes, and coagulation studies should be performed. Tetanus prophylaxis is given. Airway management, an acute abdominal series, and antivenom therapy are used for black widow spider bites. REF: Spider Bites/Definition and Epidemiology/Diagnostics/Initial Stabilization and Management 2. A child experiences a snake bite while camping and is seen in the emergency department. The child’s parents are not able to identify the type of snake. An inspection of the site reveals two puncture wounds on the child’s arm with no swelling or erythema at the site. The child has normal vital signs. Which treatment is indicated? a. Administering antivenom and observing the child for 24 to 48 hours b. Cleaning the wound, giving tetanus prophylaxis, and observing for 12 hours c. Performing a type and cross match of the child’s blood d. Referral to a surgeon for incision and suction of the wound The child does not have immediate symptoms of envenomation, since there is no swelling or erythema. Because symptoms may be delayed, and the type of snake is unknown, the child should be observed in an ED or hospital for 12 hours after providing wound care and tetanus prophylaxis. Antivenom is not indicated unless envenomation occurs. Type and cross match is done if envenomation is severe. Incision and suction of the sound is not recommended. REF: Reptile Bites and Scorpion Stings/Physical Examination/Diagnostics/Initial Stabilization and Management Chapter 27: Bradycardia and Tachycardia Test Bank Multiple Choice 1. A patient reports heart palpitations but no other symptoms and has no prior history of cardiovascular disease. The clinic provider performs an electrocardiogram and notes atrial fibrillation and a heart rate of 120 beats per minute. Which is the initial course of action in treating this patient? a. Administer atenolol intravenously b. Admit to the hospital for urgent cardioversion c. Refer the patient to a cardiologist d. Transport the patient to the ED by ambulance This patient has no history of serious heart disease and does not have symptoms of chest pressure, acute MI, or congestive heart failure and may be referred to a cardiologist for evaluation and treatment. Atenolol is given IV for patients who are unstable; the advanced life support treatment guidelines do not recommend treatment of tachycardia if the patient is stable. Urgent cardioversion is rarely needed if the heart rate is less than 150 beats per minute unless there are underlying heart conditions. It is not necessary to transport a stable patient to the ED. REF: Tachycardia/Initial Stabilization and Management 2. A patient who takes a beta blocker medication is in the emergency department with syncope, shortness of breath, and hypotension. A cardiac monitor reveals a heart rate of 35 beats per minute. Which medication may be used to stabilize this patient? a. Adenosine b. Amiodarone c. Atropine d. Epinephrine Epinephrine is indicated if unstable bradycardia is caused by beta blockers. This patient is symptomatic and unstable and should be treated. Adenosine and amiodarone are used to treat tachycardia. Atropine is used for some types of bradycardia, but not when induced by beta blockers. REF: Bradycardia/Initial Stabilization and Management 3. Which cardiac arrhythmia in an unstable patient requires unsynchronized shocks, or defibrillation? a. Atrial fibrillation b. Atrial flutter c. Monomorphic ventricular tachycardia d. Polymorphic ventricular tachycardia Polymorphic ventricular tachycardia should be treated as ventricular fibrillation with unsynchronized shocks. The other arrhythmias are treated with synchronized cardioversion. REF: Box 27-1: Cardioversion and defibrillation of unstable patients with tachycardia Chapter 28: Cardiac Arrest Test Bank Multiple Choice 1. Current American Heart Association (AHA) recommendations include: Select all that apply. a. A compression depth of 1½ inches or more on an adult b. A rate of 100 compressions per minute at a minimum c. Rescue breaths given during 2 seconds to allow full chest rise d. Untrained rescuers giving compressions without breaths e. Using a ratio of 2 rescue breaths to 30 compressions , D, E The AHA recommends compression rates of at least 100 compressions per minute at a ratio of 2 breaths for every 30 compressions. Untrained rescuers are encouraged to provide chest compressions only. The depth of compressions in adults should be at least 2 inches. Rescue breaths are given over 1 second with full chest rise. REF: Cardiac Arrest/Physical Examination 2. The AHA recommends early CPR and AED use for adult victims of cardiac arrest outside of a hospital setting because most victims have which arrhythmia? a. Atrial fibrillation b. Atrial flutter c. Ventricular fibrillation d. Ventricular tachycardia Most victims of cardiac arrest are in ventricular fibrillation, so the AHA considers early defibrillation the most effective treatment for adult victims of cardiac arrest. The other arrhythmias are not usually present in cardiac arrest and are treated with synchronized cardioversion REF: Cardiac Arrest/Initial Stabilization and Management 3. A health care provider in a clinic finds a patient in a room, unresponsive and pale. Which sign should be used to identify the need to initiate cardiopulmonary resuscitation (CPR)? a. Assessment of gasping breaths or not breathing b. Determination of pulselessness or bradycardia c. Evaluation of peripheral perfusion and level of consciousness d. Obtaining a history of previous myocardial infarction The AHA recommends initiating CPR if the victim in not breathing or has gasping breaths. Determination of a pulse in an arrest situation can be problematic and the search for a pulse should not delay chest compressions if the patient is gasping for breath or not breathing. Evaluation of peripheral perfusion and LOC is not part of the initial assessment and not used to indicate the need for CPR. A medical history may be obtained after resuscitation is in progress. REF: Cardiac Arrest/Physical Examination Chapter 29: Chemical Exposure Test Bank Multiple Choice 1. What is true when considering activated charcoal for gastrointestinal decontamination to treat a toxic substance ingestion? a. It acts by enhancing gastric motility to reduce absorption. b. It is administered only through a nasogastric tube. c. It may be used when petroleum distillates are ingested. d. It must be administered within 60 minutes of ingestion. Activated charcoal must be given within an hour after ingestion of the toxin. It absorbs ingested substances and reduces absorption and may cause bowel obstruction; it does not increase bowel motility. It may be given orally or by nasogastric tube. Because it is associated with vomiting, it should not be used when caustic substances, alcohols, and petroleum distillates are ingested. REF: Initial Stabilization and Management/Ingestions 2. A lawn maintenance worker is brought to the emergency department after an accident in which a large amount of pesticide was sprayed all over his clothing. He is able to relate the details of the accident to the emergency department personnel. What is the priority treatment on admission? a. Administer intravenous diphenhydramine and possibly epinephrine b. Contact the Poison Control center to ask about appropriate antidotes c. Place on a cardiorespiratory monitor and establish intravenous access d. Remove the patient’s clothing and irrigate the skin for 15 to 30 minutes Most skin exposure to chemicals must be treated immediately with copious irrigation with water, so this is the initial priority in a stable patient. Since he is able to converse with staff, he is likely to be stable. If signs of anaphylaxis occur, diphenhydramine and epinephrine are indicated. The Poison Control center should be contacted, but this is not the priority. After irrigation to minimize exposure, other interventions, such as cardiorespiratory monitoring and IV access may be necessary. REF: Initial Stabilization and Management/Skin Exposure 3. A child is brought to the emergency department because a grandparent suspects ingestion of a tricyclic antidepressant medication found in the bathroom. What symptoms will the ED professionals expect to observe if this is the case? Select all that apply. a. Excessive salivation b. Flushed skin c. Hallucinations d. Hypothermia e. Mydriasis f. Urinary frequency Tricyclic antidepressants will cause anticholinergic effects, including flushing of the skin, hallucinations or psychosis, and mydriasis. These medications also cause dry mucous membranes, hyperthermia, and urinary retention. REF: Chemical Exposure/Clinical Presentation Chapter 30: Electrical Injuries Test Bank Multiple Choice 1. What is true about electrical injuries? Select all that apply. a. Alternating current causes tetanic skeletal muscle contractions. b. Direct current is more dangerous than alternating current. c. Electrical injury causes more tissue necrosis in nerves than other tissues. d. Lightning is less lethal because the duration of electrical strike is short. e. Low-voltage contact has no potential to be lethal. Alternating current tends to be more lethal than direct current because it causes tetanic muscle contractions. Electrical injury affects nerves more than other tissues because nerve tissue has the least resistance to direct flow and is most easily damaged. Lightning, although it has a voltage of 10 million to 2 billion volts, has a short duration of contact. Alternating current is more dangerous than direct current. Low-voltage contact has the potential to be lethal. REF: Pathophysiology 2. An adolescent male has an electrical injury from a high-voltage wire after climbing a tree. Which initial diagnostic test is necessary? a. 12-lead electrocardiogram b. Cervical spine radiography c. Complete blood count and electrolytes d. Creatine kinase and myoglobin level An early essential assessment in all patients with electrical injury is a 12-lead ECG to assess arrhythmias and conduction disturbances. The other labs are part of the initial workup, but not a priority over the ECG. A C-spine radiograph is done if cervical injury is suspected. REF: Physical Examination/Diagnostics Chapter 31: Environmental Allergies Test Bank Multiple Choice 1. When performing diagnostic tests to determine which environmental allergens cause symptoms in an atopic patient, which aspects of scratch testing are preferable to other methods? Select all that apply. a. It has a lower potential for anaphylaxis. b. It is more sensitive. c. It is safer. d. It produces more rapid results. e. It requires a stepwise approach. Scratch testing involves scratching the surface of the skin. This method has a lower potential for anaphylaxis, is safer, and has more rapid results. It is not as sensitive as the intradermal method, which requires a stepwise approach. REF: Environmental Allergies/Diagnostics 2. Which immunoglobulin is responsible for initiating the allergic cascade in susceptible individuals who are exposed to allergens? a. IgG b. IgA c. IgM d. IgE While IgA, IgG, and IgM are produced to appropriately protect the body, circulating levels of IgE are responsible for the atopic reaction. REF: Environmental Allergies/Pathophysiology 3. Which food allergies in children may be outgrown in the first decade of life? Select all that apply. a. Egg allergy b. Fish allergy c. Milk allergy d. Nut allergy e. Shell fish allergy , C Both egg and milk allergy may be outgrown within the first decade of life. Fish, nut, and shell fish allergies are more common in adults and have a higher incidence of lifetime allergy. REF: Food Allergies/Definition and Epidemiology Chapter 32: Head Trauma Test Bank Multiple Choice 1. A patient is in the emergency department after sustaining a blow to the head in a motor vehicle accident. The patient’s Glasgow Coma score is 14 and the patient is drowsy. The patient has a small amount of blood in one external auditory canal. Which is a priority in diagnosing the extent of injury in this patient? a. Close monitoring of pulse, respiration, and oxygenation b. Continued assessment of neurological status c. Magnetic resonance imaging of the head d. Non-enhanced computed tomography of the head Although this patient’s GCS is non-concerning, the type of injury and the sign of blood in the external auditory canal put this patient at high risk for skull fracture, so a head CT is indicated immediately. Close monitoring of vital signs and neurological status should be continuously performed, the CT is a priority to help determine the treatment needed. MRI is not especially useful, but may be performed after CT if more detail of structures is needed. REF: Head Trauma/Diagnostics 2. A patient who sustained a head injury has a Glasgow Coma score of 14. The patient’s spouse reported that the patient lost consciousness for approximately 7 minutes after falling down the stairs. A head CT does not reveal brain lesions. Which treatment is indicated? a. Admission to the hospital with a neurosurgical evaluation b. Continued observation in the emergency department until stability is ensured c. Discharge to home with close observation by the patient’s spouse for 24 hours d. Dismissal to home with a referral for follow up with a neurologist This patient had loss of consciousness longer than 5 minutes and has a GCS of 14; both of these are indications for admission to the hospital with a neurosurgery consult, even though the CT is currently normal. REF: Head Trauma/Disposition and Referral 3. A patient is brought to the emergency department after being hit in the head with a baseball. The patient is awake and talking, but is confused and disoriented and does not obey simple commands. The patient is able to point to the area of pain and opens eyes only when commanded to do so. Bystanders report a period of unconsciousness lasting almost 5 minutes. Which severity of traumatic brain injury is likely? a. Normal b. Mild c. Moderate d. Severe This patient’s Glasgow Coma score is 11, based on eye opening to verbal command (3), ability to localize pain (4), and conversing while confused (4). The patient was unconscious less than 10 minutes, which usually indicates less severe injury. A patient with a GCS between 9 and 12 with or without loss of consciousness is considered to have a moderate head injury. REF: Head Trauma/Definition and Epidemiology/Table 32-1: Glasgow Coma Scale Chapter 33: Hypotension Test Bank Multiple Choice 1. A young adult patient is being treated for hypertension and is noted to have a resting blood pressure of 135/88 mm Hg just after finishing a meal. After standing, the patient has a blood pressure of 115/70 mm Hg. What is the likely cause of this change in blood pressure? a. A hyperglycemic episode b. Antihypertensive medications c. Neurogenic orthostatic hypotension d. Postpriandal hypotension Medications to treat hypertension may cause orthostatic hypotension. Hypoglycemia may cause hypotension. Neurogenic orthostatic hypotension is less likely. Postpriandal hypotension occurs in elderly patients. REF: Pathophysiology 2. An elderly patient who has orthostatic hypotension secondary to antihypertensive medications is noted to have a drop in systolic blood pressure of 25 mm Hg. Which intervention is important for this patient? a. Administration of intravenous fluids b. Close monitoring cardiorespiratory status c. Initiation of a fall risk protocol d. Withholding antihypertensive medications A reduction of systolic blood pressure >20 mm Hg is a risk factor for falls in the elderly, so a fall risk protocol should be initiated. Unless the patient is dehydrated, IV fluids are not recommended. Close monitoring of CR status will not prevent falls. Withholding antihypertensive medications often worsens orthostatic hypotension. REF: Diagnostics/Management 3. An older patient develops orthostatic hypotension secondary to an antihypertensive medication and asks what measures can be taken to minimize this condition. What will the provider recommend? Select all that apply. a. Crossing the legs when standing up b. Custom-fitted elastic stockings c. Discontinuation of the medication d. Increased physical activity e. Performing the Valsalva maneuver Measures such as crossing the legs when standing, wearing custom-fitted elastic stockings, and increasing physical activity may all help prevent orthostatic hypotension symptoms. Discontinuation of the medication may make the condition worse. Performing the Valsalva maneuver will increase intrathoracic pressure and should be avoided. REF: Management Chapter 34: Poisoning Test Bank Multiple Choice 1. A patient who ingested a bottle of acetaminophen tablets is brought to the emergency department. Which treatment is indicated? a. Flumazenil b. N-acetylcysteine c. Naloxone d. Supportive care only N-acetylcysteine is used as an antidote for acetaminophen overdose. Flumazenil is used to treat benzodiazepine overdose. Naloxone is given for opioid overdose. REF: Poisoning/Initial Stabilization and Management 2. Several groups of college students arrive in the emergency department reporting severe gastrointestinal symptoms after leaving a fraternity party. After stabilizing these patients, a priority for the emergency department personnel is to a. contact the fraternity to determine whether others are affected. b. isolate the patients to prevent spread of infection. c. notify the local health department about this outbreak. d. obtain histories from the patients about illicit drug use. Providers must be alert to situations in which a number of people present with similar symptoms within a short time, suggesting a common source of poisoning. This lowered threshold of suspicion requires action to prevent additional casualties, so the providers should contact the fraternity. If an infectious cause is determined, isolation may be required, but an investigation of the common source is paramount. After the situation is stabilized, the health department should be notified. Because the symptoms appeared in a cluster of patients who all attended the same party, questioning them about illicit drug use is a lower priority than determining risk to others. REF: Poisoning/Clinical Presentation 3. What is the first priority in emergency management of a biological terrorism attack? a. Basic life support b. Communication with authorities c. Containing the exposures d. Informing the public of the risk In a bioterrorism attack, the initial priority is to contain the exposures and prevent expansion of the event to others. Basic life support is the second priority and close communication with authorities is the third priority. Informing the public is a later priority after the situation has been stabilized. REF: Terrorism Chapter 35: Sexual Assault Test Bank Multiple Choice 1. A patient who was sexually assaulted one month prior tells her provider that she is concerned about contracting HIV. When is it appropriate to perform testing? a. Immediately and then every 6 months for the first year b. Immediately with definitive results c. In two weeks and then 3 to 6 months after the assault d. Three to 6 months after the assault Because of the length of time for seroconversion to occur, patients concerned about HIV exposure should be tested 6 weeks after and then 3 to 6 months after the assault. Immediate results will not provide accurate information. The initial testing should be 6 weeks after potential exposure. REF: Sexual Assault/Diagnostics 2. During a health maintenance examination, 17-year-old female reports having been raped repeatedly at a college party during the previous semester and tells the practitioner that she did not seek help at the time. Which action is a priority for the primary care provider? a. Recommending counseling at a local mental health center b. Referring the patient to the emergency department for STI testing c. Reporting the alleged assault to law enforcement d. Suggesting that the patient report the incident to the school Any sexual assault perpetrated on a victim younger than 18 years must be reported to the local child or adult protective agency as well as to law enforcement, regardless of whether the patient reports that sexual assault occurred. Counseling, STI testing, and reporting the incident to the school are important, but are not the priority. REF: Sexual Assault/Indications for Referral or Hospitalization 3. When beginning a health maintenance exam, the health care provider learns that an adult patient has been sexually assaulted the previous day. What is the initial responsibility of the provider? a. Notify the police and encourage the patient to press criminal charges b. Perform a thorough gynecological exam and obtain cultures c. Question the patient about the events surrounding the assault d. Refer the patient to the emergency department for a forensic examination If a patient has been sexually assaulted within the past 5 days, and especially if within the previous 72 hours, the provider should defer a physical examination and refer the patient to the ED for a forensic examination. It is not necessary to notify the police unless the victim is a child, elderly, or disabled. The provider should not perform the exam – a forensic exam ensures that standard protocol is followed and appropriate evidence is obtained. Retelling the story of the assault may be traumatizing to the patient, so this should be left to providers performing the forensic exam. REF: Sexual Assault/Physical Examination Chapter 36: Syncope Test Bank Multiple Choice 1. Which tests are indicated as part of the initial evaluation for women of childbearing age who report syncope? Select all that apply. a. 12-lead electrocardiogram b. Cardiac enzyme levels c. Complete blood count d. Electroencephalogram e. Serum glucose testing Initial evaluation for all patients reporting syncope should include a standard 12-lead ECG. Women of childbearing age should have a CBC, serum pregnancy test, and serum glucose testing. Cardiac enzyme levels are obtained if the patient has cardiac risk factors. EEG is performed only if there is a concern for seizure disorder. REF: Syncope/Diagnostics 2. A healthy 20-year-old patient reports having had 1 or 2 episodes of syncope without loss of consciousness. Which is the most likely type of syncope in this patient? a. Cardiac b. Neurogenic c. Orthostatic hypotensive d. Reflex syncope Neurally mediated or reflex syncope is the most common cause of syncope and is primarily seen in young adults. Cardiac, neurogenic, and orthostatic syncope are generally seen in older adults. REF: Syncope/Pathophysiology 3. An elderly patient reports experiencing syncope each morning when getting out of bed. Which assessment will the health care provider perform first to evaluate this patient’s symptoms? a. Cardiac enzyme levels b. Electroencephalogram c. Fasting blood glucose d. Orthostatic blood pressures Orthostatic blood pressures should be measured first since this patient reports problems associated with rising from a supine position. The other tests are performed as part of the diagnostic workup only if indicated by associated symptoms or suspected causes. REF: Syncope/Physical Examination Chapter 37: Thermal Injuries Test Bank Multiple Choice 1. A child is brought to the emergency department after getting lost while camping on a cold, rainy day. The child is lethargic on admission. The cardiorespiratory monitor shows a normal heart rate and rhythm, a respiratory rate of 8 to 10 breaths per minute, and a normal blood pressure. The assessment reveals erythema and edema of the child’s hands and feet. What treatments are indicated? Select all that apply. a. Administer antibiotics b. Apply warmed blankets c. Elevate the child’s extremities d. Massage the hands and feet e. Remove all clothing The child has signs of frostbite without other systemic signs. Warming with warm blankets is indicated. The affected areas should be elevated, but not massaged or rubbed. The providers should remove the child’s clothing which may be restrictive or wet and examine the child’s entire skin surface for other signs of frostbite. Antibiotics are not given unless signs of infection are present. REF: Frostbite/Management 2. A patient is brought to a clinic after fainting while working outdoors on a hot day. The patient has slurred speech and headache and has a temperature of 104° F. What will the provider do? a. Administer antipyretic medications to reduce the temperature b. Administer intravenous fluids in the clinic and monitoring response c. Rehydrate the patient with oral fluids containing electrolytes d. Transport the patient to the emergency department This patient has CNS signs and an elevated temperature with a history consistent with heat stroke. This patient should be immediately transported to an emergency department. Antipyretic medications are not useful for treating thermal injury. The patient will be given IV fluids and electrolytes in the ED. Oral rehydration is not indicated. REF: Clinical Presentation/Management 3. A provider attending a soccer match on a hot day is assisting a player who feels hot and appears dehydrated, but who is alert and oriented. What does the provider suspect? a. Heat cramps b. Heat exhaustion c. Heat stroke d. Heat syncope Heat exhaustion is present when patients have excessive sweating accompanied by sodium and water loss. Heat cramps involve muscle pains or spasms. Heat stroke causes a core body temperature of >106° F. Heat syncope causes fainting or dizziness. REF: Definition and Epidemiology Chapter 38: Examination of the Skin and Approach to Diagnosis of Skin Disorders Test Bank Multiple Choice 1. When examining a patient’s skin, a practitioner uses dermoscopy in order to Select all that apply. a. accentuate changes in color of pathologic lesions by fluorescence. b. assess changes in pigmentation throughout various lesions. c. determine whether lesion borders are regular or irregular. d. differentiate fluid masses from cystic masses in the epidermis. e. visualize skin fissures, hair follicles, and pores in lesions. Dermoscopy is used to visualize the epidermis and superficial dermis and can reveal changes in pigmentation throughout lesions, whether borders are regular or irregular, and the various fissures, follicles, and pores present in lesions. The Wood’s light, or black light, is used to fluoresce lesions to accentuate changes in color. A direct light source is useful for differentiating fluid masses from cystic masses. REF: Physical Examination 2. A primary care provider is performing a Tzanck test to evaluate possible herpes simplex lesions. To attain accurate results, the provider will a. blanch the lesions while examining them with a magnifying glass. b. gently scrape the lesions with a scalpel onto a slide. c. perform a gram stain of exudate from the lesions. d. remove the top of the vesicles and obtain fluid from the lesions. The Tzanck test requires removing the tops from vesicular lesions in order to obtain fresh fluid from the base of the lesions. Blanching of blue to red lesions under a microscope helps to evaluate whether blood is in the capillaries of the lesions. Scraping lesions onto a slide is done to evaluate the presence of hyphae and spores common with candidiasis or fungal infections. Gram staining is performed to distinguish gram-positive from gram-negative organisms in suspected bacterial infections. REF: Box 38-1: Skin Examination Technique Chapter 39: Surgical Office Procedures Test Bank Multiple Choice 1. A provider is preparing to administer electrocautery to a patient who has several seborrheic keratoses. The patient tells the provider that he has a pacemaker. Which action is correct? a. Administer the electrocautery per the usual protocol b. Apply electrocautery in short burst at low voltage c. Refer the patient to a dermatologist for removal d. Suggest another method for removal of the lesions Patients with pacemakers or implantable cardioverter-defibrillators may receive electrocautery if appropriate precautions, such as lower voltage and shorter bursts are taken. It is not necessary to suggest another method or to refer to a dermatologist. REF: Electrocautery 2. A patient has molluscum contagiosum and the provider elects to use cryosurgery to remove the lesions. How will the provider administer this procedure? a. Apply one freeze-thaw cycle to each lesion b. Apply two or more freeze-thaw cycles to each lesion c. Apply until the freeze spreads laterally 1 mm from the lesion edges d. Apply until the freeze spreads laterally 4 mm from the lesion edges For molluscum contagiosum, one freeze-thaw cycle is usually sufficient. Two freeze-thaw cycles are generally required for thicker, more keratotic lesions. The freeze should spread laterally 3 to 4 mm from the edge of the lesions. REF: Cryosurgery 3. Which type of office surgical procedure warrants sterile technique? a. Curettage b. Punch biopsy c. Scissor excision d. Shave biopsy Punch biopsy requires sterile technique. The other procedures require cleaning with alcohol and clean technique with universal precautions. REF: Biopsy Chapter 40: Principles of Dermatologic Therapy Test Bank Multiple Choice 1. An infant has atopic dermatitis and seborrheic dermatitis with lesions on the forehead and along the scalp line. Which is correct when prescribing a corticosteroid medication to treat this condition? a. Initiate treatment with 0.1% triamcinolone acetonide (Kenalog lotion) b. Monitor the infant closely for systemic adverse effects during use c. Place an occlusive dressing over the medication after application d. Prescribe 0.05% fluocinonide (Lidex-E Cream) to apply liberally Treatment with 0.1% triamcinolone acetonide is appropriate in this case, because it is a class V corticosteroid and may be used on the face and is suggested for use for these conditions. Systemic side effects are rare when topical corticosteroids are used appropriately. Occlusive dressings increase the risk of adverse effects and are not recommended. 0.05% fluocinonide is a class III corticosteroid and should not be used on the face. REF: Topical Corticosteroids/Table 40-3: Topical Corticosteroids Ranked by Potency/Table 40-4: Suggested Strength of Topical Steroids to Initiate Treatment 2. When recommending an over-the-counter topical medication to treat a dermatologic condition, which instruction to the patient is important to enhance absorption of the drug? a. Apply a thick layer of medication over the affected area b. Place an occlusive dressing over the medication c. Put cool compresses over the affected area after application d. Use a lotion or cream instead of an ointment preparation Drug absorption may be enhanced up to 10 times with application of occlusive dressings. Applying a thicker layer does not increase skin penetration or effectiveness of a medication. Warm or inflamed skin absorbs medications more readily; cool compresses will decrease absorption. Lotions and creams are not as readily absorbed as ointments, which have occlusive properties. REF: Dermatologic Vehicles 3. A provider is prescribing a topical dermatologic medication for a patient who has open lesions on a hairy area of the body. Which vehicle type will the provider choose when prescribing this medication? a. Cream b. Gel c. Ointment d. Powder Gels are an excellent vehicle for use on hairy areas of the body. Creams and ointments are not recommended for hairy areas. Powders should be avoided in open wounds. REF: Dermatologic Vehicles/Table 40-2: Common Vehicles for Topical Pharmacotherapeutic Preparations Chapter 41: Screening for Skin Cancer Test Bank Multiple Choice 1. Curing a total body skin examination for skin cancer, the provider notes a raised, shiny, slightly pigmented lesion on the patient’s nose. What will the provider do? a. Consult with a dermatologist about possible melanoma b. Reassure the patient that this is a benign lesion c. Refer the patient for possible electrodessication and curettage d. Tell the patient this is likely a squamous cell carcinoma This lesion is characteristic of basal cell carcinoma, which is treated with electrodessication and curettage. Melanoma lesions are usually asymmetric lesions with irregular borders, variable coloration, >6 mm diameter, which are elevated; these should be referred immediately. All suspicious lesions should be biopsied; until the results are known, the provider should not reassure the patient that the lesion is benign. Squamous cell carcinoma is roughened, scaling, and bleeds easily. REF: Physical Examination/Management 2. What is the initial approach when obtaining a biopsy of a potential malignant melanoma lesion? a. Excisional biopsy b. Punch biopsy c. Shave biopsy d. Wide excision A suspected malignant melanoma lesion should be biopsied with excisional biopsy; if diagnosed, a wide excision should follow. Punch and shave biopsy procedures are appropriate for diagnostic evaluation of NMSC lesions. REF: Diagnostics Chapter 42: Acne Vulgaris Test Bank Multiple Choice 1. A patient has acne and the provider notes lesions on half of the face, some nodules, and two scarred areas. Which treatment will be prescribed? a. Oral clindamycin for 6 to 8 weeks b. Oral isotretinoin c. Topical benzoyl peroxide and clindamycin d. Topical erythromycin This patient has moderate acne, based on symptoms of lesions on half of the face with nodules and a few scars. A combination of topical benzoyl peroxide and clindamycin is recommended. Oral antibiotics are reserved for severe cases. Oral isotretinoin is used only for recalcitrant cases which are severe and have not responded to other treatments. Topical antibiotics should be used as monotherapy. REF: Acne Vulgaris/Pathophysiology/Management 2. When counseling a patient with rosacea about management of this condition, the provider may recommend Select all that apply. a. applying a topical steroid. b. avoiding makeup. c. avoiding oil-based products. d. eliminating spicy foods. e. exposing the skin to sun. f. using topical antibiotics. Patients with rosacea should avoid oil-based products and eliminate spicy foods, alcohol, and hot fluids. Topical antibiotics may be used if pustules are present. Topical steroids are not recommended. Patients do not need to avoid makeup and should avoid the sun. REF: Rosacea 3. A provider is considering an oral contraceptive medication to treat acne in an adolescent female. Which is an important consideration when prescribing this drug? a. A progesterone-only contraceptive is most beneficial for treating acne. b. Combined oral contraceptives are effective for non-inflammatory acne only. c. Oral contraceptives are effective because of their androgen enhancing effects. d. Yaz, Ortho Tri-Cyclen, and Estrostep are approved for acne treatment. Three oral contraceptives have a labeled use for acne treatment: Yaz, Ortho Tri-Cyclen, and Estrostep. Progesterone-only contraceptives may worsen acne. Combined oral contraceptives are effective in reducing inflammatory and non-inflammatory acne. Oral contraceptives are effective because of their antiandrogen effects, since androgen induces sebum production. REF: Acne Vulgaris/Management Chapter 43: Alopecia Test Bank Multiple Choice 1. A patient is in the clinic with patches of hair loss. The provider notes several well- demarcated patches on the scalp and eyebrows without areas of inflammation and several hairs within the patch with thinner shafts near the scalp. Based on these findings, which type of alopecia is most likely? a. Alopecia areata b. Anagen effluvium c. Cicatricial alopecia d. Telogen effluvium These findings are characteristic of alopecia areata. Anagen effluvium and telogen effluvium both result in diffuse hair loss and not discrete patches. Cicatricial alopecia involves inflammation. REF: Physical Examination 2. A patient with alopecia is noted to have scaling on the affected areas of the scalp. Which confirmatory test(s) will the provider order? a. Examination of scalp scrapings with potassium hydroxide b. Grasping and pulling on a few dozen hairs c. Serum iron studies and a complete blood count d. Venereal Disease Research Laboratory (VDRL) test Scaling on the scalp is suggestive of tinea capitis. To confirm this, the provider will perform scalp scraping or test hair samples with KOH preparation to look for hyphae. Grasping and pulling on hairs is used to identify anagen or telogen hairs by appearance. Serum iron and a CBC are used if anemia is suspected as a cause. VDRL is performed if syphilis is suspected. REF: Diagnostics 3. A female patient is diagnosed with androgenetic alopecia. Which medication will the provider order? a. Anthralin b. Cyclosporine c. Finasteride d. Minoxidil Either minoxidil or finasteride are used for androgenetic alopecia, but finasteride is Pregnancy Category X, so minoxidil is the only medication approved by the FDA for use in women. Anthralin and cyclosporine are used to treat alopecia areata. REF: Management Chapter 44: Animal and Human Bites Test Bank Multiple Choice 1. Which type of bite is generally closed by delayed primary closure? Select all that apply. a. Bites to the face b. Bites to the hand c. Deep puncture wounds d. Dog bites on an arm e. Wounds 8 hours old Cat and human bites, deep puncture wounds, clinically infected wounds, wounds more than 6 to 12 hours old, and bites to the hand should be left open and closed by delayed primary closure. A bite to the face is closed by primary closure. Dog bites do not require delayed or secondary closure. REF: Management 2. A patient has been bitten by a dog and has sustained several puncture wounds near the thumb of one hand. The patient is able to move all fingers and the bleeding has stopped. What is the correct treatment for this patient? a. Begin rabies and tetanus prophylaxis and bandage the wound b. Clean the wound thoroughly and order a topical antibiotic c. Obtain a physician consultation for evaluation and treatment d. Prescribe oral antibiotics and have the patient follow up in a few days Any animal bites on the face or hand require physician consultation because of the increased risk for osteomyelitis, tendinitis, and septic arthritis. The other interventions may or may not be appropriate, but must be decided by the consulting physician. REF: Definition and Epidemiology/Physician Consultation 3. A patient has sustained a human bite on his hand during a fist fight. Which is especially concerning with this type of bite injury? a. Possible exposure to rabies virus b. Potential septic arthritis or osteomyelitis c. Sepsis from Capnocytophaga canimorsus infection d. Transmission of human immunodeficiency virus Clenched-fist injury, or “fight bite,” has a high complication rate from the high penetrating force with the potential for osteomyelitis, tendinitis, and septic arthritis. Humans do not transmit rabies unless infected, which is highly unlikely. Humans do not transmit C. canimorsus. HIV transmission is potential, but the risk is extremely low. REF: Definition and Epidemiology/Pathophysiology Chapter 45: Bullous Pemphigoid Test Bank Multiple Choice 1. An elderly adult patient with bullous pemphigoid is prescribed oral prednisone and hydroxyzine to manage symptoms. Which medication side effect is of immediate concern for this patient? a. Osteoporosis b. Pruritis c. Sedation d. Weight gain Older patients should take hydroxyzine cautiously because of the risks of sedation. Osteoporosis and weight gain are long-term effects of prednisone and not of immediate concern. Hydroxyzine is given to treat pruritus. REF: Management 2. A patient is newly diagnosed with bullous pemphigoid and has moderate to severe itching. The provider orders a topical corticosteroid will discuss which potential complication with this patient? a. Bone marrow suppression b. Developing systemic lesions c. Secondary infection d. Spread of disease to others Topical corticosteroids and excessive rubbing and trauma to skin increase the risk of secondary infections. Bone marrow suppression is a side effect of immunosuppressive therapy. Systemic lesions are not likely; patients may develop systemic infection if secondary infection occurs. The disease is not contagious. REF: Patient and Family Education 3. When assisting with a skin biopsy of a patient suspected of having bullous pemphigoid lesions, the practitioner will a. avoid contact with the infected lesions. b. elicit a positive Nikolsky sign to confirm the diagnosis. c. perform direct immunofluorescence microscopy. d. prevent spread of the lesions to other areas of the skin. Direct immunofluorescence microscopy is the gold standard for diagnosis of BP. The lesions are not infected. The Nikolsky sign will be negative in patients with BP. The lesions do not spread by this manner. REF: Clinical Presentation and Physical Examination/Diagnostics Chapter 46: Burns (Minor) Test Bank Multiple Choice 1. A patient comes to the clinic after being splashed by boiling water while cooking. The patient has partial thickness burns on both forearms, the neck, and the chin. What will the provider do? a. Clean and dress the burn wounds b. Order a CBC, glucose, and electrolytes c. Perform a chest radiograph d. Refer the patient to the emergency department Patients with burns on the face, potential circumferential burns, and any patient at risk of airway compromise should be referred to the ED for evaluation and treatment. The provider should do this urgently and not clean and dress the wounds or order diagnostic tests. REF: Definition and Epidemiology 2. A patient suffers chemical burns on both arms after a spill at work. What is the initial action by the providers in the emergency department? a. Begin aggressive irrigation of the site b. Contact the poison control center c. Remove the offending chemical and garments d. Request the Material Safety Data information The initial response to a chemical burn is to remove the patient’s clothing and the offending chemical. Aggressive irrigation is usually recommended next, but providers should first determine the source to make sure that it is safe to use water. Contacting Poison Control and getting MSDS information are useful measures after the clothing and chemical is removed. REF: Chemical Burns/Management Chapter 47: Cellulitis Test Bank Multiple Choice 1. A patient with a purulent skin and soft tissue infection (SSTI). A history reveals a previous MRSA infection in a family member. The clinician performs an incision and drainage of the lesion and sends a sample to the lab for culture. What is the next step in treating this patient? a. Apply moist heat until symptoms resolve b. Begin treatment with amoxicillin-clavulanate c. Prescribe oral clindamycin d. Wait for culture results before ordering an antibiotic Because of a history of exposure to MRSA, the patient is likely to be colonized and should be treated accordingly. Small lesions may be treated with moist heat, but the likelihood of MRSA requires treatment. Amoxicillin-clavulanate is not effective for MRSA. Treatment should be started empirically. REF: Clinical Presentation/Management 2. A previously healthy patient has an area of inflammation on one leg which has well- demarcated borders and the presence of lymphangitic streaking. Based on these symptoms, what is the initial treatment for this infection? a. Amoxicillin-clavulanate b. Clindamycin c. Doxycycline d. Sulfamethoxazole-trimethoprim This patient has symptoms consistent with erysipelas, which is commonly caused by staphylococcal or streptococcal bacteria. These may be treated empirically with a penicillinase- resistant penicillin. Clindamycin, doxycycline, and sulfamethoxazole-trimethoprim are used for methicillin-resistant staphylococcus aureus infections. REF: Clinical Presentation/Management 3. A child has vesiculopustular lesions around the nose and mouth with areas of honey-colored crusts. The provider notes a few similar lesions on the child’s hands and legs. Which treatment is appropriate for this child? a. Amoxicillin-clavulanate Test Bank 2 b. Culture and sensitivity of the lesions c. Sulfamethoxazole-trimethoprim d. Topical antiseptic ointment This child has symptoms of impetigo which has spread to the hands and legs. A systemic penicillinase-resistant penicillin is recommended. It is not necessary to obtain a culture since this can be treated empirically in most cases. MRSA is unlikely, so sulfamethoxazole-trimethoprim is not indicated. Oral antibiotics, not topical antiseptics, are the treatment of choice. REF: Clinical Presentation/Management Chapter 48: Contact Dermatitis Test Bank Multiple Choice 1. A child has irritant contact dermatitis with lesions on the extremities and face. Which treatment is recommended for this patient? a. Antihistamines b. Medium- to high-potency topical corticosteroids c. Oral corticosteroids d. Topical calcineurin inhibitors When periorbital regions or more than 20% of the body surface area is involved, the use of an oral steroid is appropriate. Antihistamines produce relaxation and improve sleep, but do not reduce the pruritus associated with contact dermatitis. Topical calcineurin inhibitors may be used in place of topical steroids, but oral steroids are indicated in this instance. REF: Management 2. A patient who has been exposed to poison ivy presents with inflammation and a vesicular rash on one arm. The provider recommends a topical steroid, but the next day the patient calls to report similar lesions appearing on the face. What will the provider tell this patient? a. The rash is spreading through self-inoculation. b. The vesicles may continue to develop for up to 2 weeks. c. The rash may spread over the next 8 weeks. d. The patient must have been re-exposed to the irritant. Exposure to poison ivy resin results in vesicles and bullae that develop for up to 2 weeks. Once the resin is washed off, no further spread occurs. With insufficient treatment, the rash may persist, but not spread, for up to 8 weeks. REF: Clinical Presentation and Physical Examination Chapter 49: Corns and Calluses Test Bank Multiple Choice 1. A patient develops a corn on the dorsolateral aspect of the fifth toe on one foot. What will the practitioner do initially to treat this condition? a. Apply a 40% salicylic acid plaster over the lesion for 48 to 72 hours b. Gently pare the lesion with a No. 15 scalpel blade c. Obtain a foot radiograph to assess underlying bone structures d. Recommend trying an over-the-counter corn solution Treatment for corns begins by decreasing the size of the callus or corns using a No. 15 scalpel blade. After decreasing the size, salicylic acid is applied for 48 to 72 hours before paring the remaining tissue. Foot radiographs may be performed if treatment fails. OTC solutions are not generally recommended. REF: Management 2. A patient with a soft corn develops an infection without surrounding erythema or edema. Which treatments are recommended? Select all that apply. a. Oral erythromycin b. Salicylic acid patch c. Sanding with a pumice stone d. Topical mupirocin e. Twice-daily warm soaks , E Soft corn infections are treated with twice-daily warm soaks and application of topical mupirocin. If signs of cellulitis are present, an oral antibiotic may be added. Salicylic acid patches are used as part of corn removal. Pumice stones are used to reduce the size of calluses. REF: Management Chapter 50: Cutaneous Herpes Test Bank Multiple Choice 1. A patient who has recurrent, frequent genital herpes outbreaks asks about therapy to minimize the episodes. What will the provider recommend as first-line treatment? a. Acyclovir b. Famciclovir c. Topical medications d. Valacyclovir All three oral antiviral medications help reduce the number of occurrences and the frequency of asymptomatic shedding. Famciclovir and valacyclovir are more costly and no more effective, so should not be first-line therapy. Topical medications are not useful with recurrent, frequent genital herpes. REF: Suppression of Frequent Recurrences 2. A patient who has never had an outbreak of oral lesions reports a burning sensation on the oral mucosa and then develops multiple painful round vesicles at the site. A Tzanck culture confirms HSV-1 infection. What will the provider tell the patient about this condition? a. Antiviral medications are curative for oral herpes. b. The initial episode is usually the most severe. c. There are no specific triggers for this type of herpesvirus. d. Transmission to others occurs only when lesions are present. In herpesvirus outbreaks, the initial episode is generally the most severe. Antiviral medications may prevent outbreaks, but do not cure the disease. HSV-1 has several specific triggers. Transmission to others may occur even when lesions are not present. REF: Cutaneous Herpes/Pathophysiology/Clinical Presentation/Management/Patient and Family Education 3. A patient who has had lesions for several days is diagnosed with primary herpes labialis and asks about using a topical medication. What will the provider tell this patient? a. Oral antivirals are necessary to treat this type of herpes. b. Preparations containing salicylic acid are most helpful. c. Topical medications can have an impact on pain and discomfort. d. Topical medications will significantly shorten the healing time. Topical medications may alleviate discomfort, but do not shorten healing time. Oral antivirals may help shorten healing, but are not necessary as treatment, since the disease is usually self- limiting. Salicylic acid should not be used because it can erode the skin. REF: Primary Herpes Labialis Chapter 51: Dermatitis Medicamentosa Test Bank Multiple Choice 1. A patient is taking a sulfonamide antibiotic and develops a rash that begins peeling. Which type of rash is suspected? a. Erythema multiforme b. Stevens-Johnson c. Urticaria d. Wheal and flare The Stevens-Johnson syndrome rash typically peels in sheets. Erythema multiforme, urticaria, and wheal and flare rashes do not peel. REF: Complications 2. A child is brought to a clinic with a sudden onset of rash after taking an antibiotic for 2 days. The provider notes all over wheals with pruritis, which the parent reports seem to come and go. Which action is correct? a. Admit the child to the hospital for treatment and observation b. Prescribe an oral antihistamine and follow up in 1 to 2 days c. Reassure the parent that the rash will eventually subside d. Suggest trying cool compresses and tepid baths at home Urticarial lesions are pruritic and often “move.” The more sudden and explosive the appearance of the urticaria, the more likely that anaphylaxis may occur, so the child should be hospitalized for treatment and observation. Oral antihistamines, cool compresses, and tepid baths may be used, but the child should not be sent home. REF: Differential Diagnosis 3. Which types of medications are associated with urticarial type rashes? Select all that apply. a. ACE inhibitors b. Erythromycin c. NSAIDs d. Penicillins e. Phenothiazines Erythromycin, NSAIDs, and cillins are associated with urticaria. ACE inhibitors tend to cause angioedema. Phenothiazines are associated with photosensitivity. REF: Table 51-1: Skin Reactions Chapter 52: Dry Skin Test Bank Multiple Choice 1. A patient who has chronically dry skin who has been using emollients and moisturizers reports an uneven diamond pattern and redness on the lower legs and arms. What will the provider recommend? a. A topical antibiotic ointment b. Increasing sodium consumption c. Referral to a dermatologist d. Using antihistamines at night This patient exhibits symptoms of eczema craquele, which is a more severe type of dry skin. Because the patient has been treated without success, referral to a dermatologist is recommended. Topical antibiotics are used only if signs of infection are present. Patients should limit sodium intake. Antihistamines are not indicated. REF: Clinical Presentation and Physical Examination/Management 2. When counseling a patient who has dry skin about ways to minimize exacerbations, what will the provider include? Select all that apply. a. Cleanse the skin frequently b. Eat soups and stews frequently c. Take tepid-water baths d. Use topical corticosteroids regularly e. Use fragrance-free detergents Providers should recommend eating foods high in fluids, such as soups and stews. Bath water should be tepid. Patients should use products that are fragrance free. Cleansing the skin frequently increases drying. Topical corticosteroids should be used only for flare ups; too frequent use causes atrophy of the skin. REF: Patient Education and Health Promotion Chapter 53: Eczematous Dermatitis (Atopic Dermatitis) Test Bank Multiple Choice 1. Which is the primary symptom causing discomfort in patients with atopic dermatitis? a. Dryness b. Erythema c. Lichenification d. Pruritis Itching is incessant and patients usually develop other signs at the site of itching. REF: Definition and Epidemiology 2. The parent of a 10-month-old child with atopic dermatitis asks what can be done to minimize the recurrence of symptoms in the child. What will the provider recommend? a. Calcineurin inhibitors b. Lubricants and emollients c. Oral diphenhydramine d. Prophylactic topical steroids Emollients and lubricants are used long-term to reduce flare-ups. Cacineurin inhibitors are not recommended for children under 2 years. Oral diphenhydramine helps with symptoms of itching, but is not used to prevent symptoms. Corticosteroids should be used sparingly to treat symptoms and stopped once the inflammation has subsided. REF: Management 3. A child who has atopic dermatitis has recurrent secondary bacterial skin infections. What will the provider recommend to help prevent these infections? a. Bleach baths twice weekly b. Frequent bathing with soap and water c. Low-dose oral antibiotics d. Topical antibiotic ointments Bleach baths and intranasal mupirocin have been shown to reduce bacterial superinfections of the skin. Frequent bathing with soap and water may increase flare-ups and increase the risk for superinfections. Oral and topical antibiotic prophylaxis are not recommended. REF: Complications Chapter 54: Fungal Infections (Superficial) Test Bank Multiple Choice 1. Which medication will the provider prescribe as first-line therapy to treat tinea capitis? a. Oral griseofulvin b. Oral ketoconazol c. Topical clotrimazole d. Topical tolnaftate Systemic antifungal medications are used for widespread tinea and always with infections that involve the nails or scalp. Oral ketoconazole should be avoided due to risks of hepatotoxicity and serious drug interactions. REF: Dermatophyte Infections/Management 2. When collecting a specimen to determine a diagnosis of tinea corporis, the provider will scrape which portion of the lesion? a. The active, leading border b. The area of central clearing c. The erythematous plaque d. The papular lesions The key to a reliable KOH preparation is properly obtaining an adequate specimen by scraping the active, leading border of a lesion. The other areas do not yield a reliable specimen. REF: Dermatophyte Infections/Diagnostics 3. When evaluating scalp lesions in a patient suspected of having tinea capitis, the provider uses a Wood’s lamp and is unable to elicit fluorescence. What is the significance of this finding? a. The patient does not have tinea capitis. b. The patient is less likely to have tinea capitis. c. The patient is positive for tinea capitis. d. The patient may have tinea capitis. Although some fungal species causing tinea capitis fluoresce with a Wood’s lamp, Trichophyton tonsurans, the most common cause or tinea capitis, does not fluoresce, so lack of fluorescence does not rule out the infection, make it less likely, or diagnose it. REF: Dermatophyte Infections/Diagnostics Chapter 55: Herpes Zoster (Shingles) Test Bank Multiple Choice 1. A patient who has had a previous herpes zoster outbreak experiences a second outbreak and asks the provider about treatment to reduce the duration and severity of symptoms. What will the provider recommend? a. Acyclovir b. Lidocaine patch c. Oral corticosteroids d. Topical corticosteroids Acyclovir, given within 72 hours of onset of rash, has been shown to reduce the duration and severity of the rash and pain and to reduce the risk for PHN and disseminated disease. Lidocaine patches help with pain, but do not reduce the duration of the symptoms. Corticosteroids have not been shown to prevent development of PHN, but have shown modest reduction in duration and severity. REF: Management 2. An older patient experiences a herpes zoster outbreak and asks the provider if she is contagious because she is going to be around her grandchild who is too young to be immunized for varicella. What will the provider tell her? a. An antiviral medication will prevent transmission to others. b. As long as her lesions are covered, there is no risk of transmission. c. Contagion is possible until all of her lesions are crusted. d. Varicella zoster and herpes zoster are different infections. Herpes zoster lesions contain high concentrations of virus that can be spread by contact and by air; although they are less contagious than primary infections, contagion is possible until all lesions are crusted. Antiviral medications shorten the course, but do not reduce transmission. Covering the lesions does not prevent transmission. Herpes zoster and varicella zoster are the same. REF: Pathophysiology 3. A patient has a unilateral vesicular eruption which is described as burning and stabbing in intensity. To differentiate between herpes simplex and herpes zoster, which test will the provider order? a. Polymerase chain reaction analysis b. Serum immunoglobulins c. Tzanck test d. Viral culture The PCR is a rapid and sensitive test that can differentiate between the two. Serum Ig levels are not diagnostic. The Tzanck test identifies the presence of a herpes virus, but does not differentiate between the two types. Viral culture will differentiate, but is not rapid. REF: Diagnostics Chapter 56: Hidradenitis Suppurativa (Acne Inversa) Test Bank Multiple Choice 1. Which medications may be used as part of the treatment for a patient with hidradenitis suppurativa? Select all that apply. a. Chemotherapy b. Erythromycin c. Infliximab d. Isotretinoin e. Prednisone Hidradenitis suppurativa is not malignant and chemotherapy is not used. Erythromycin, infliximab, isotretinoin, and prednisone are all used. REF: Hidradenitis Suppurativa/Management 2. A female patient is diagnosed with hidradenitis suppurativa and has multiple areas of swelling, pain, and erythema, along with several abscesses in the right femoral area. When counseling the patient about this disorder, the practitioner will include which information? a. Antibiotic therapy is effective in clearing up the lesions. b. It is often progressive with relapses and permanent scarring. c. The condition is precipitated by depilatories and deodorants. d. The lesions are infective and the disease may be transmitted to others. Although lesions may be treated with antibiotics, other medications, and drainage, the disease is often progressive, with relapses and permanent scarring. Deodorants and depilatories are not implicated as a cause. The disease is not transmitted to others, although the organisms may cause other infections in other people. REF: Hidradenitis Suppurativa/Management/Patient Education Chapter 57: Hyperhidrosis Test Bank Multiple Choice 1. A patient is newly diagnosed with hyperhidrosis with excessive sweating on the palms and soles. What will the provider recommend to treat this condition? a. Aluminum chloride hexahydrate b. Liposuction of sweat glands c. Oral anticholinergic agents d. Thoracic endoscopic surgery Topical aluminum chloride hexahydrate is used initially for excessive perspiration on hands, feet, and in the axillae. Liposuction is performed on axillary glands. Oral anticholinergics may be used, but the initial treatment is the topical preparation. Thoracic endoscopic surgery may be used if other treatments fail. REF: Management 2. A patient has excessive sweating of the palms, soles, and axillae. The provider understands that this presentation is often due to which cause? a. Anxiety b. Hormones c. Hypoglycemia d. Medications Localized excessive sweating is usually due to anxiety, heat, or is idiopathic, while more generalized excessive sweating may be due to underlying conditions. REF: Clinical Presentation 3. A patient reports generalized excessive sweating and states that night sweats are present. Which diagnostic test is a priority for this patient to determine the underlying cause? a. Blood pressure evaluation b. Fasting blood glucose c. Purified protein derivative test d. Thyroid function tests When night sweats are present, a PPD is done to exclude tuberculosis. Blood pressure evaluation is performed if pheochromocytoma is suspected. Fasting blood glucose and thyroid testing will be performed to exclude thyroid disease and diabetes. Since night sweats are common with TB, this test has priority. REF: Physical Examination/Diagnostics and Differential Diagnosis Chapter 58: Intertrigo Test Bank Multiple Choice 1. A patient with intertrigo shows no improvement and persistent redness after treatment with drying agents and antifungal medications. The patient reports an onset of odor associated with a low-grade fever. What will the provider do next to manage this condition? a. Culture the lesions to determine the cause b. Evaluate the patient for HIV infection c. Order topical nystatin cream d. Prescribe a cephalosporin antibiotic This patient has symptoms of a secondary bacterial infection. The lesions should be cultured and the results used to determine the appropriate antibiotic. Patients with recurrent candida infections should be evaluated for underlying HIV infection, diabetes, and other immunocompromised states. Topical nystatin cream is used for candida infection and these symptoms are consistent with bacterial infection. Antibiotics should be chosen based on culture results. REF: Management 2. When recommending ongoing treatment for a patient who has recurrent intertrigo, what will the provider suggest? Select all that apply. a. Aluminum sulfate solution b. Burow’s solution compresses c. Cornstarch application d. Nystatin cream e. Topical steroid cream , B Aluminum sulfate solution and other drying agents are recommended and Burow’s solution compresses may be soothing. Cornstarch is ineffective and may result in fungal growth. Nystatin cream is used only for candida intertrigo. Topical steroids may promote infection. REF: Management 3. An overweight patient has intertrigo, with recurrent fungal infections. In addition to medication therapy, what will the provider recommend to treat the condition? Select all that apply. a. Apply moisturizer to affected areas b. Expose areas to light and air c. Use a hand-held dryer to dry the area d. Use powder containing cornstarch e. Wear natural-fiber clothing , C, E Affected areas should be kept clean and dry to reduce the incidence of recurrence. Exposing skin to light and air several times daily, using a hair dryer on low setting, and wearing natural-fiber clothing are all recommended. Applying moisturizer and using cornstarch are not recommended. REF: Patient and Family Education and Health Promotion Chapter 59: Nail Disorders Test Bank Multiple Choice 1. A patient with recurrent herpetic whitlow is counseled about management of symptoms and prevention of complications. What will be included in this teaching? Select all that apply. a. Begin antiviral medications within 3 days of onset of symptoms b. Contact the provider if symptoms persist longer than 3 weeks c. Cool compresses may help with comfort and decrease erythema d. Keep hands away from the mouth and eyes to prevent inoculation e. Wear gloves when preparing foods to prevent spread to others , C, D Patients with herpetic whitlow should be seen by a physician if symptoms are recalcitrant to treatment after 3 weeks. Cool compresses may help with symptomatic relief. Patients should avoid touching the mouth and eyes to prevent spread of lesions to these tissues. Antiviral medications should be given within 48 hours of onset of symptoms to be effective. Wearing gloves during food preparation is not necessary. REF: Herpetic Whitlow/Management/Education and Health Promotion 2. A patient is diagnosed with herpetic whitlow and in a follow-up evaluation, is noted to have paronychial inflammation of the tendon sheath in one finger. What is a priority treatment for this patient? a. Begin therapy with an oral antiviral medication b. Obtain a consult for incision and drainage of the lesion c. Order a creatinine clearance test to evaluate renal function d. Refer the patient to the emergency department When paronychial infection of the tendon sheath is suspected in patients with herpetic whitlow, they should be immediately referred to the emergency department for a surgical referral. Oral antiviral medications are given for severe cases and recurrences, but the emergent situation is a priority. Incision and drainage may lead to superinfection of longer healing. Creatinine clearance is ordered when beginning oral antiviral therapy. REF: Herpetic Whitlow/Management 3. A female patient who works with caustic chemicals has developed acute paronychia. What will he provider include when teaching this patient about her condition? Select all that apply. a. Analgesics may be necessary for comfort b. Apply clear nail polish to protect her nails c. Avoid trimming the nails until the infection clears d. Use protective gloves while working e. Wear waterproof gloves when washing dishes , D, E Patients with paronychia may require analgesics for comfort. They should be instructed to wear protective gloves while working, if the condition is work-related and to wear waterproof gloves while washing dishes. Nail polish should be avoided and nails should be kept trimmed and clean REF: Paronychia/Management/Education and Health Promotion Chapter 60: Pigmentation Changes (Vitiligo) Test Bank Multiple Choice 1. A patient with well-localized vitiligo is referred to a dermatologist for treatment. What will the initial treatment be? a. Chemical depigmentation with mequinol b. Narrow-band ultraviolet B light therapy c. Psoralens plus ultraviolet A light d. Twice-daily application of a mid-potency steroid cream The initial treatment for vitiligo is twice-daily mid-potency steroids. UVA and UVB therapy with psoralens may be used if this isn’t effective and must be performed by a qualified specialist. Patients with widespread areas of vitiligo may be treated with depigmentation therapy. REF: Management 2. A parent reports the appearance of areas of depigmented skin on a child which has spread rapidly. The provider notes asymmetrically patterned tri-colored, macules in a dermatomal distribution. What type of vitiligo does the provider suspect? a. Inflammatory vitiligo b. Segmented vitiligo c. Type A vitiligo d. Vitiligo with poliosis Segmented, or dermatomal vitiligo, spreads rapidly, is usually asymmetrical, and tends to occur in children. Inflammatory vitiligo occurs after inflammation of the skin. Type A vitiligo is non- dermatomal and is generally symmetric. Poliosis occurs when well-defined areas of white hair occur. REF: Clinical Presentation 3. A patient who is diagnosed with vitiligo asks the provider what can be done to minimize the contrast between depigmented and normal skin. What will the provider recommend? a. Applying a cosmetic cover-up or tanning cream b. Lightening the dark skin areas with hydrogen peroxide c. Tanning for limited periods in a tanning booth d. Waiting for all skin to become depigmented Cosmetic cover-ups or tanning creams are useful to help darken affected areas. Hydrogen peroxide is not recommended. Tanning is contraindicated; excessive sunburn can stimulate depigmentation. Waiting for widespread depigmentation is unpredictable. REF: Management Chapter 61: Pruritus Test Bank Multiple Choice 1. A patient has pruritis related to use of fabric softeners in clothing and reports all-over itching. A physical examination reveals no areas of inflammation. Besides stopping the use of this product, what is an initial intervention to stop the pruritis? a. Application of capsaicin b. Cooling the skin c. Topical antihistamines d. Topical corticosteroids Cooling of the skin by wearing light clothing or using a fan can help stop pruritis and should be initiated first. Capsaicin is used for localized pruritis. Topical antihistamines are sensitizers and should be discouraged. Topical corticosteroids are reserved for cases of cutaneous inflammation. REF: Management 2. A patient undergoing renal dialysis has extensive pruritis. Which medication will the provider order? a. Cholestyramine (Questran) b. Cyproheptadine (Periactin) c. Doxepin (Sinequan) d. Gabapentin (Neurontin) Gabapentin is useful for patients who experience pruritis as a result of dialysis. Cholestyramine is used for pruritis caused by cholestasis. Cyproheptadine is used for patient with pruritis resulting from polycythemia vera. Doxepin is used for its anxiolytic effects. REF: Systemic Therapy 3. A patient complains of persistent pruritis of the extremities. A history is negative for medical and psychiatric causes and the patient has not had significant exposures. The physical examination of the affected skin is negative, except for marks made by scratching. What will the provider order to evaluate the cause of this itching? Select all that apply. a. A skin biopsy specimen b. Blood urea nitrogen and serum creatinine c. Complete blood count with differential d. Referral for psychiatric evaluation e. Thyroid panel and blood glucose , C, E Initial laboratory tests should include a CBC with differential, BUN and creatinine, a thyroid panel, and a blood glucose. Skin biopsy may be done if lesions are present. If other causes are ruled out, a psychiatric evaluation may be ordered. REF: Diagnostics Chapter 62: Psoriasis Test Bank Multiple Choice 1. A child has plaques on the extensor surfaces of both elbows and on the face with minimal scaling and pruritis. What is the likely cause of these lesions? a. Atopic dermatitis b. Guttate psoriasis c. Psoriasis d. Seborrhea Children with psoriasis often have lesions on the face and have less scaling than adults. Psoriasis tends to present on extensor surfaces, while atopic dermatitis occurs on flexor surfaces. Guttate psoriasis appears as teardrop-shaped lesions that appear on the trunk and spread to the extremities and are occasionally seen after streptococcal infections in adolescents. Seborrhea usually occurs on the scalp. REF: Definition and Epidemiology/Differential Diagnosis 2. A patient with psoriasis develops lesions on the intertriginous areas of the skin. Which treatment is recommended? a. High-potency topical steroids b. Oral corticosteroid injections c. Topical steroids with vitamin D d. Topical, low-potency steroids Patients with intertriginous psoriasis should be treated with low-potency topical steroids. High- potency steroids usually produce maximum benefit in 2 to 3 weeks and research suggests combining high-potency steroids with vitamin D analog is best. Oral corticosteroids are used for recalcitrant symptoms. REF: Management/Topical Therapy 3. A patient with severe, recalcitrant psoriasis has tried topical medications, intralesional steroid injections, and phototherapy with ultraviolet B light without consistent improvement in symptoms. What is the next step in treating this patient? a. Cyclosporine b. Etanercept c. Methotrexate d. Oral retinoids Methotrexate has shown good efficacy in treating recalcitrant psoriasis. Cyclosporine and oral retinoids are effective, but have serious side effects. Etanercept and other biologic agents are effective but expensive and should be tried after all other treatments have failed. REF: Management/Systemic Medications/Biologic Agents Chapter 63: Purpura Test Bank Multiple Choice 1. A patient has a purpural rash with flat, non-palpable lesions. Which laboratory tests will be most helpful in the initial diagnosis? a. Blood urea nitrogen and liver function studies b. Complete blood count with platelets c. Erythrocyte sedimentation rate or C-reactive protein d. Prothrombin time, partial thromboplastin time, and international normalized ratio The initial diagnostic workup should include a CBC and platelet count and is most helpful in the initial diagnosis. BUN and LFTs are used to exclude organ disease and may be performed as part of the differential diagnosis. The ESR and CRP are used if the lesions are thought to be related to an inflammatory cause. The PT, PTT, and INR are used to determine the presence of coagulopathies. REF: Diagnostics 2. A pediatric patient has immune thrombocytopenic purpura and has a platelet count of 60,000/mm3. What is the recommended treatment based on this laboratory value? a. Close observation b. High-dose steroids c. Intravenous immunoglobulin d. Possible splenectomy Immune thrombocytopenic purpura (ITP) may have mild to severe symptoms. Treatment is usually reserved for those with a platelet count less than 50,000/mm3 and may include steroids, immunoglobulin, and possible splenectomy. This child has levels high enough to warrant observation without treatment. REF: Differential Diagnosis 3. A patient presents with a purpural rash. The provider notes localized swelling and palpable lesion. What underlying condition may be the cause of this rash? a. A bleeding disorder b. A medication hypersensitivity c. A vasculitis disorder d. An infectious disease Inflammatory purpura is most often palpable and is associated with the vasculitides. Non- inflammatory purpura may be caused by infectious disease, medication hypersensitivity, and bleeding disorders. REF: Differential Diagnosis Chapter 64: Scabies Test Bank Multiple Choice 1. An adult patient has greasy, scaling patches on the forehead and eyebrows suggestive of seborrheic dermatitis. What is included in assessment and management of this condition? Select all that apply. a. Begin first-line treatment with a topical antifungal medication b. Evaluate the scalp for dry, flaky scales and treat with selenium sulfide shampoo c. Teach the patient that proper treatment is curative in most instances d. Topical antibacterial medications may be used to prevent Malassezia proliferation e. Use topical steroids for several weeks to prevent recurrence of symptoms , B First-line therapy may include topical antifungals or corticosteroids. Adults with symptoms on the face or eyebrows are likely to have scalp lesions, since this is usually a “top-down” disorder. The condition is chronic and recurrent. Antibacterial medications are used for secondary bacterial infections but do not treat Malazessia, which is a fungus. Topical steroids should be used on a short-term basis. REF: Management/Patient and Family Education 2. The provider is prescribing 5% permethrin cream for an adolescent patient who has scabies. What will the provider include in education for this patient? a. All household contacts will be treated only if symptomatic. b. Itching 2 weeks after treatment indicates treatment failure. c. Stuffed animals and pillows should be placed in plastic bags for 1 week. d. The adolescent’s school friends should be treated. Bedding and clothing of persons with scabies should be washed in hot water and dried on hot dryer settings. Items that cannot be washed should be put in plastic bags for 1 week. All household contacts should be treated. Itching may persist as a result of the secondary dermatitis for up to 2 weeks and does not represent treatment failure. Casual contacts do not require treatment. REF: Management/Patient and Family Education 3. A patient has a pruritic eczematous dermatitis which has been present for one week and reports similar symptoms in other family members. What will the practitioner look for to help determine a diagnosis of scabies? a. Bullous lesions on the soles of the feet and palms of the hands b. Intra-epidermal burrows on the interdigital spaces of the hands c. Nits and small bugs along the scalp line at the back of the neck d. Pustular lesions in clusters on the trunk and extremities The scabies mite typically burrows no deeper than the stratus corneum and burrows may be found in the interdigital spaces of the hands, among other places. Bullous lesions may occur with impetigo. Nits and small bugs are characteristic findings with pediculosis. Pustular lesions represent superficial skin infections. REF: Clinical Presentation and Physical Examination Chapter 65: Seborrheic Dermatitis Test Bank Multiple Choice 1. An adult patient has greasy, scaling patches on the forehead and eyebrows suggestive of seborrheic dermatitis. What is included in assessment and management of this condition? Select all that apply. a. Begin first-line treatment with a topical antifungal medication b. Evaluate the scalp for dry, flaky scales and treat with selenium sulfide shampoo c. Teach the patient that proper treatment is curative in most instances d. Topical antibacterial medications may be used to prevent Malassezia proliferation e. Use topical steroids for several weeks to prevent recurrence of symptoms , B First-line therapy may include topical antifungals or corticosteroids. Adults with symptoms on the face or eyebrows are likely to have scalp lesions, since this is usually a “top-down” disorder. The condition is chronic and recurrent. Antibacterial medications are used for secondary bacterial infections but do not treat Malazessia, which is a fungus. Topical steroids should be used on a short-term basis. REF: Management/Patient and Family Education 2. A patient with chronic seborrheic dermatitis reports having difficulty remembering to use the twice daily ketoconazole cream prescribed by the provider. What will the provider order for this patient? a. Burow’s solution soaks once daily b. Oral corticosteroids c. Oral itraconazole (Sporanox) d. Selenium sulfide shampoo 2.5% as a daily rinse Itraconazole is effective for moderate to severe symptoms and is an alternative for those who do not wish to use topical treatment. Burow’s solution and selenium shampoo rinses are not indicated. Oral corticosteroids are usually not given. REF: Management Chapter 66: Stasis Dermatitis Test Bank Multiple Choice 1. Which treatment is most important in long-term management of stasis dermatitis? a. “Active” dressing application b. Compression therapy c. Massage therapy d. Systemic antibiotics Compression therapy is considered the gold standard of treatment for stasis dermatitis. “Active” dressings are used when ulcerations occur to help with wound healing. Massage therapy is not recommended. Systemic antibiotics are used only when secondary infections occur. REF: Management 2. A patient who has stasis dermatitis is instructed to apply an emollient to the skin around the ankles. What is the reason for this recommendation? a. To encourage formulation of granulation tissue b. To maintain optimum skin integrity c. To minimize the risk of allergic contact dermatitis d. To prevent itching and inflammation Emollients are used to maintain skin integrity. When ulcerations form, topically applied growth factor is used to help with granulation tissue formation. Using plain petrolatum as an emollient, rather than a product with potentially irritating chemicals, will help prevent allergic contact dermatitis. Corticosteroids are used for itching and inflammation. REF: Management 3. Which are elements of patient education when counseling a client who has stasis dermatitis about preventing complications associated with this disease? Select all that apply. a. Applying emollients daily b. Keeping legs elevated when seated c. Minimizing exercise and ambulation d. Reducing fluid intake Test Bank 2 e. Weight reduction , B, E Patients should be encouraged to apply emollients daily, to keep legs elevated when seated as much as possible, and to lose weight if needed. Exercise and ambulation should be encouraged. Reducing fluids is not recommended because this will reduce circulating blood volume. REF: Patient and Family Education Chapter 67: Urticaria Test Bank Multiple Choice 1. A patient describes a wheal and flare type rash that recurs frequently with hives that appear and then fade within an hour. The provider notes that the patient demonstrates a wheal and flare reaction when the skin is stroked with a pen. What will the provider ask the patient to help determine the cause of this rash? a. If the patient takes any medications, such as NSAIDs regularly b. If there is a family history of thyroid autoimmunity disease c. Whether the patient is experiencing gastrointestinal discomfort d. Whether the patient is exposed to cold or water prior to the rash Urticaria caused by physical triggers, such as cold or water, tends to develop quickly and then fade within an hour and will also exhibit dermatographism, which is a wheal and flare reaction to physical stimuli. The other factors tend to cause more typical urticaria that develops more slowly and lasts longer. REF: Definition and Epidemiology 2. A patient with chronic urticaria is taking a high dose non-sedating H1 blocker medication but reports minimal relief from itching. What will the provider prescribe to help alleviate this symptom? a. A corticosteroid b. A leukotriene inhibitor c. A sedating antihistamine d. An H2 blocker For urticaria refractory to H1 blockade, evidence exists for clinical benefit when an H2 blocker is added. Corticosteroids are useful for acute urticaria. Leukotriene inhibitors may be useful in some, but clinical trials are inconclusive. Addition of a sedating antihistamine at bedtime will help patients sleep, but does not add much to symptom control. REF: Management Chapter 68: Warts Test Bank Multiple Choice 1. A pregnant woman has a history of human papillomavirus (HPV) and asks what she should do to prevent spread of this disease to her newborn. What will the provider recommend? a. Administration of the HPV vaccine b. Elective caesarean section c. No precautions are necessary d. Referral for cryotherapy Infants born to mothers with HPV infection may contract the virus during passage through the birth canal, so elective caesarean section may be performed to prevent this exposure. HPV vaccine is not given once infection has occurred. Cryotherapy is not indicated. REF: Pathophysiology/Management 2. An adolescent patient has several warts on one hand. Which action by the provider is indicated? a. Evaluate the patient’s HPV immunization status b. Reassure the patient that these lesions will regress spontaneously c. Remind the patient not to touch the genitals to prevent self-inoculation d. Treat the patient with either chemical agents or cryotherapy Most warts are benign and will regress spontaneously over time. Warts on the hands and feet do not have an affinity for anogenital areas, so HPV immunization is not considered when evaluating these warts and patients do not have to be taught to avoid touching these areas. Chemical agents or cryotherapy may be used for wart that are painful or for cosmetic reasons. REF: Management Chapter 69: Wound Management Test Bank Multiple Choice 1. A patient has a pressure ulcer that has been treated with topical medications. During a follow-up visit, the provider notes an area of red bumps in the lesion. What does this indicate? a. Healing tissue b. Poor perfusion c. Secondary infection d. Tunneling lesions Wounds that are healing of have the potential to heel will demonstrate pink or red tissue and the absence of exudate, infection, or debris and will have bumpy granulation tissue. Perfusion is assessed by pulse assessment and localized capillary refill. Secondary infection is characterized by exudate and cellular debris. Tunneling is a secondary wound. REF: Physical Examination 2. A patient has an ulcer on one lower leg just above the medial malleolus. The provider notes irregular wound edges with granulation tissue and moderate exudate, with ankle edema in that leg. What is the initial treatment to help treat this wound? a. Compression therapy b. Hyperbaric oxygen therapy c. Revascularization procedures d. Skin grafting This patient has symptoms consistent with venous ulcers, which are characterized by irregular borders and granulation tissue. Compression therapy is the initial treatment of choice to reduce edema and promote venous return. Hyperbaric oxygen therapy, revascularization procedures, and skin grafting are generally used to treat arterial ulcers. REF: Ulcers: Venous and Arterial/Management 3. A patient with a wound containing necrotic tissue requires debridement. The practitioner notes an area of erythema and exudate in the wound. Which type of debridement will most likely be used? a. Autolytic debridement b. Biologic debridement c. Chemical debridement d. Mechanical debridement Mechanical debridement may be performed using a syringe with an 18-gauge needle to remove hyperkeratotic or necrotic tissue. Autolytic and chemical debridement methods require dressings that retain moisture and are contraindicated in the presence of infection. Biologic debridement uses maggots and is not widely used in the U.S. REF: Debridement Chapter 70: Evaluation of the Eyes Test Bank Multiple Choice 1. During an eye examination, the provider notes a red light reflex in one eye but not the other. What is the significance of this finding? a. Normal physiologic variant b. Ocular disease requiring referral c. Potential infection in the “red” eye d. Potential vision loss in one eye The red reflex should be elicited in normal eyes. Any asymmetry or opacity suggests ocular disease, potentially retinoblastoma, and should be evaluated immediately. REF: Posterior Segment 2. A patient comes to clinic with diffuse erythema in one eye without pain or history of trauma. The examination reveals a deep red, confluent hemorrhage in the conjunctiva of that eye. What is the most likely treatment for this condition? a. Order lubricating drops or ointments b. Prescribe ophthalmic antibiotic drops c. Reassure the patient that this will resolve d. Refer to an ophthalmologist Most subconjunctival hemorrhage, occurring with trauma or Valsalva maneuvers, will self- resolve and are benign. Lubricating drops are used for chemosis. Antibiotic eye drops are not indicated. Referral is not indicated. REF: Anterior Segment 3. A provider performs an eye examination during a health maintenance visit and notes a difference of 0.5 mm in size between the patient’s pupils. What does this finding indicate? a. A relative afferent pupillary defect b. Indication of a difference in intraocular pressure c. Likely underlying neurological abnormality d. Probable benign, physiologic anisocoria A difference in diameter of less than 1 mm is usually benign. Afferent pupillary defects are paradoxical dilations of pupils in response to light. This does not indicate differences in intraocular pressure. A difference of more than 1 mm is more likely to represent an underlying neurological abnormality. REF: Pupil Response Chapter 71: Cataracts Test Bank Multiple Choice 1. A primary care provider may suspect cataract formation in a patient with which finding? a. Asymmetric red reflex b. Corneal opacification c. Excessive tearing d. Injection of conjunctiva An asymmetric red reflex may be a finding in a patient with cataracts. Corneal opacification, excessive tearing, and corneal injection are not symptoms of cataracts. REF: Physical Examination 2. Which are risk factors for development of cataracts? Select all that apply. a. Advancing age b. Cholesterol c. Conjunctivitis d. Smoking e. Ultraviolet light , D, E Most older adults will develop cataracts. Smoking and UV light exposure hasten the development of cataracts. Cholesterol and conjunctivitis are not risk factors. REF: Pathophysiology Chapter 72: Blepharitis, Hordeolum, and Chalazion Test Bank Multiple Choice 1. A child has a localized nodule on one eyelid which is warm, tender, and erythematous. On examination, the provider notes clear conjunctivae and no discharge. What is the recommended treatment? a. Referral to an ophthalmologist b. Surgical incision and drainage c. Systemic antibiotics d. Warm compresses and massage of the lesion This child has a hordeolum, which is generally self-limited and usually spontaneously improves with conservative treatment. Warm compresses and massage of the lesion are recommended. Referral is not necessary unless a secondary infection occurs. Surgical intervention is not indicated. Systemic antibiotics are used to treat secondary cellulitis. REF: Management 2. A patient has a gradually enlarging nodule on one upper eyelid and reports that the lesion is painful. On examination, the lesion appears warm and erythematous. The provider knows that this is likely to be which type of lesion? a. Blepharitis b. Chalazion c. Hordeolum d. Meibomian Although hordeolum and chalazion lesions both present as gradually enlarging nodules, a hordeolum is usually painful, while a chalazion generally is not. Blepharitis refers to generalized inflammation of the eyelids. Meibomian is a type of gland near the eye. REF: Clinical Presentation 3. A patient reports has been using artificial tears for comfort because of burning and itching in both eyes, but reports worsening symptoms. The provider notes redness and discharge along the eyelid margins with clear conjunctivae. What is the recommended treatment? a. Antibiotic solution drops four times daily b. Compresses, lid scrubs, and antibiotic ointment c. Oral antibiotics given prophylactically for several months d. Reassurance that this is a self-limiting condition This patient has symptoms of blepharitis without conjunctivitis. Initial treatment involves lid hygiene and antibiotic ointment may be applied after lid scrubs. Antibiotic solution is used if conjunctivitis is present. Oral antibiotics are used for severe cases. This disorder is generally chronic. REF: Clinical Presentation/Management Chapter 73: Conjunctivitis Test Bank Multiple Choice 1. A patient who has a cold develops conjunctivitis. The provider notes erythema of one eye with profuse, watery discharge and enlarged anterior cervical lymph nodes, along with a fever. Which treatment is indicated? a. Antihistamine-vasoconstrictor drops b. Artificial tears and cool compresses c. Topical antibiotic eye drops d. Topical corticosteroid drops Viral conjunctivitis accompanies URI and is generally self-limited, lasting 5 to 14 days. Symptomatic treatment is recommended. Antihistamine-vasoconstrictor drops are used for allergic conjunctivitis. Topical antibiotic drops are sometimes used for bacterial conjunctivitis. Topical corticosteroid drops are used for severe inflammation. REF: Management/Viral Conjunctivitis 2. A patient reports bilateral reports burning and itching eyes for several days. The provider notes a boggy appearance to the conjunctivae, along with clear, watery discharge. The patient’s eyelids are thickened and discolored. There are no other symptoms. Which type of conjunctivitis is most likely? a. Allergic b. Bacterial c. Chemical d. Viral Allergic conjunctivitis generally presents simultaneously in both eyes with itching as a predominant feature. Discharge is generally clear or stringy and white and the patient will have lid discoloration, thickening, and erythema. Bacterial conjunctivitis is characterized by acute inflammation of the conjunctivae along with purulent discharge. Chemical conjunctivitis will not have purulent discharge. Viral conjunctivitis is usually in association with a URI. REF: Clinical Presentation/Acute Allergic Conjunctivitis 3. A patient with allergic conjunctivitis who has been using a topical antihistamine- vasoconstrictor medication reports worsening symptoms. What is the provider’s next step in managing this patient’s symptoms? a. Consider prescribing a topical mast cell stabilizer b. Determine the duration of treatment with this medication c. Prescribe a non-sedating oral antihistamine d. Refer the patient to an ophthalmologist for further care Antibiotic-vasoconstrictor agents can have a rebound effect with worsening symptoms if used longer than 3 to 7 days, so the provider should determine whether this is the cause. Topical mast cell stabilizers are useful as prophylaxis for recurrent or persistent allergic conjunctivitis and results do not occur for several weeks. Oral antihistamines may be the next step if it is determined that the cause of worsening symptoms is related to the allergy. It is not necessary to refer to ophthalmology at this time. REF: Management Chapter 74: Corneal Surface Defects and Ocular Surface Foreign Bodies Test Bank Multiple Choice 1. Which patients should be referred immediately to an ophthalmologist after eye injury and initial treatment? Select all that apply. a. A patient who was sprayed by lawn chemicals b. A patient who works in a metal fabrication shop c. A patient with a corneal abrasion d. A patient with a full-thickness corneal laceration e. A patient with irritation secondary to wood dust , B, D Patients with chemical eye injuries, any with possible metallic foreign bodies, and those with full-thickness corneal lacerations must have immediate referral. Corneal abrasions and irritation from wood dust may be managed by primary care providers. REF: Management/Box 74-2: Indications for Immediate Ophthalmology Referral 2. A patient who works in a furniture manufacturing shop reports a sudden onset of severe eye pain while sanding a piece of wood and now has copious tearing, redness, and light sensitivity in the affected eye. On examination, the conjunctiva appears injected, but no foreign body is visualized. What is the practitioner’s next step? a. Administration of antibiotic eye drops b. Application of topical fluorescein dye c. Instillation of cyclopegic eye drops d. Irrigation of the eye with normal saline The practitioner must determine if there is a corneal abrasion and will instill fluorescein dye in order to examine the cornea under a Wood’s lamp. Antibiotic eye drops are not indicated as initial treatment. Cyclopegic drops are used occasionally for pain control, but should be used with caution. Irrigation of the eye is indicated for chemical burns. REF: Management Chapter 75: Dry Eye Syndrome Test Bank Multiple Choice 1. A patient has evaporative dry eye syndrome with eyelid inflammation. What are some pharmacologic and non-pharmacologic measures the provider can recommend? Select all that apply. a. Apply over-the-counter artificial tears as needed b. Avoid direct exposure to air conditioning c. Topical steroid eye drops as a maintenance medication d. Use non-tearing baby shampoo to gently scrub the eyelids e. Use tetrahydrozoline drops for discomfort , B, D Patients with dry eye are encouraged to use OTC artificial tears to help moisten the eyes. Avoiding exposure to fans, air conditioning, and wind is recommended. Non-tearing baby shampoo may be used to cleanse the lids in patients with eyelid inflammation. Topical steroid eye drops should be used sparingly and for short periods of time. Tetrahydozoline drops constrict blood vessels and may dry eyes further. REF: Management 2. A patient has chronically dry eyes, sometimes with a foreign body sensation, burning, and itching. A Schirmer test is abnormal. What is the suspected cause of this patient’s symptoms based on this test finding? a. Aqueous-deficiency b. Corneal abrasion c. Evaporative disorder d. Poor eyelid closure An abnormal Schirmer test, which assesses aqueous production, indicates aqueous-deficient dry eye. A corneal abrasion usually causes excessive tearing. An evaporative disorder is determined by an evaluation of tear breakup time. Poor eyelid closure causes increased corneal exposure and increased evaporation of tears. REF: Diagnostics Chapter 76: Nasolacrimal Duct Obstruction and Dacryocystitis Test Bank Multiple Choice 1. A patient has dacryocystitis. The provider notes a painful lacrimal sac abscess that appears to be coming to a head. Which treatment will be useful initially? a. Eyelid scrubs with baby shampoo b. Incision and drainage c. Lacrimal bypass surgery d. Topical antibiotic ointment When an abscess is present and coming to a head, incision and drainage may be useful. Definitive treatment with lacrimal bypass surgery will be performed once the acute episode has resolved. Eyelid scrubs and topical ointments are not effective. REF: Management 2. An adult patient with a history of recurrent sinusitis and allergic rhinitis reports chronic tearing in one eye, ocular discharge, and eyelid crusting. The provider suspects nasolacrimal duct obstruction. Which initial treatment will the provider recommend? a. Antibiotic eye drops b. Nasolacrimal duct probing c. Systemic antibiotics d. Warm compresses This is most likely acquired nasolacrimal duct obstruction. Initial treatment should include warm compresses. Antibiotics are only used if infection is present. Nasolacrimal duct probing is not useful for acquired conditions; definitive treatment usually requires surgery. REF: Clinical Presentation/Management Chapter 77: Preseptal and Orbital Cellulitis Test Bank Multiple Choice 1. A patient has eyelid swelling with erythema and warmth and reports pain with eye movement. Which diagnostic tests will be performed to confirm a diagnosis of orbital cellulitis? Select all that apply. a. Blood cultures b. Complete blood count c. CT scan of orbits d. Lumbar puncture e. Visual acuity testing , C A complete blood count will help distinguish infectious from non-infectious orbital cellulitis. A CT scan or the orbits is necessary to confirm the diagnosis. Blood cultures do not confirm the diagnosis of orbital cellulitis, but may be used to evaluate whether septicemia is occurring. Lumbar puncture is indicated if meningitis is suspected. Visual acuity testing may be used to monitor recovery. REF: Diagnostics 2. Which is the most common cause of orbital cellulitis in all age groups? a. Bacteremic spread from remote infections b. Inoculation from local trauma or bug bites c. Local spread from the ethmoid sinus d. Paranasal sinus inoculation Because the membrane separating the ethmoid sinus from the orbit is literally paper-thin, this is the most common source of orbital infection in all age groups. Bacteremic spread, inoculation from localized trauma, and paranasal sinus spread all may occur, but are less common. REF: Pathophysiology 3. A child has unilateral eyelid edema, warmth and erythema and does not exhibit pain with ocular movement. Which is most likely true about this child’s infection? a. Decreased visual acuity may occur Test Bank 2 b. Increased intraocular pressure will be present c. Optic nerve compromise is a complication d. The eye is typically spared without conjunctivitis This child has symptoms of preseptal cellulitis in which the eye is typically spared. The other findings are consistent with orbital cellulitis. REF: Clinical Presentation and Physical Examination Chapter 78: Pinguecula and Pterygium Test Bank Multiple Choice 1. A patient has an elevated, yellowish-white lesion adjacent to the cornea at the 3 o’clock position of the right eye. The provider notes pinkish inflammation with dilated blood vessels surrounding the lesion. What will the provider tell the patient about this lesion? a. Artificial tear drops are contraindicated b. Spontaneous bleeding is likely c. UVB eye protection is especially important d. Visine may be used for symptomatic relief This patient has a pinguecula which has become inflamed. Wide-brimmed hats and sunglasses with UVB protection should be advised since UVB light will make this worse. Artificial tear drops are recommended to reduce irritation. These types of lesions typically do not bleed spontaneously. Visine is contraindicated because chronic vasoconstriction may lead to rebound inflammation. REF: Clinical Presentation/Management 2. A patient who has an inflamed pterygia lesion has been using loteprednol topical steroid drops for 7 days. The patient shows no improvement in symptoms. What is the next course of action? a. Consult with an ophthalmologist b. Continue the medication for 7 more days c. Prescribe a systemic corticosteroid d. Refer the patient to the emergency department Topical steroid medications are used to treat pterygia, but should not be used longer than 7 days without ophthalmic consultation. Systemic corticosteroids are not indicated and an emergent referral is not necessary. REF: Management Chapter 79: Traumatic Ocular Disorders Test Bank Multiple Choice 1. A child sustains an ocular injury in which a shard of glass from a bottle penetrated into the eye wall. The emergency department provider notes that the shard has remained in the eye. Which best describes this type of injury? a. Intraocular foreign body b. Penetrating eye injury c. Perforating eye injury d. Ruptured globe injury When a portion of the insulting object enters and remains in the eye, the injury is correctly referred to as an intraocular foreign body. A penetrating injury occurs when something penetrates through the eye wall without an exit wound. A perforating injury occurs when the object has both an entry and an exit wound. A ruptured globe injury occurs when blunt force causes the eye wall to rupture. REF: Definition 2. A patient suffers a penetrating injury to one eye caused by scissors. The provider notes a single laceration away from the iris that involves the anterior but not the posterior segment. What is the prognosis for this injury? a. Because the posterior segment is not involved, the prognosis is good b. Blindness is likely with this type of eye injury c. Massive hemorrhage and loss of intraocular contents is likely d. Retinal detachment is almost certain to occur Mechanical energy imparted from sharp objects generally results in lacerations, with disruption that is more localized. The prognosis is better if the posterior segment is not involved. The other complications are more common with globe ruptures. REF: Mechanical Injuries 3. Which is an important protective precaution in a metal fabrication workshop? a. 2 mm polycarbonate safety glasses b. Eyewash stations c. Glasses with UVB protection Test Bank 2 d. Polycarbonate goggles Polycarbonate goggles, which have better side protection, will protect from foreign bodies that can reach around other lenses and should be used in very high risk activities, such as hammering metal on metal or grinding. 2 mm polycarbonate safety glasses are a minimum safety precaution. Glasses with UVB protection are used in occupations where sunlight exposure is high. Eyewash stations are necessary where splash injuries or chemical exposures are possible. REF: Education and Health Promotion Chapter 80: Auricular Disorders Test Bank Multiple Choice 1. During a routine physical examination, a provider notes a shiny, irregular, painless lesion on the top of one ear auricle and suspects skin cancer. What will the provider tell the patient about this lesion? a. A biopsy should be performed. b. Immediate surgery is recommended. c. It is benign and will not need intervention. d. This is most likely malignant. This lesion is characteristic of basal cell carcinoma, which is a slow-growing cancer least likely to metastasize. A biopsy should be performed to evaluate this. Immediate surgery is not necessary. Until a biopsy is performed, the provider cannot determine whether it is benign. REF: Definition and Epidemiology/Management 2. A primary care provider notes painless, hard lesions on a patient’s external ears that expel a white crystalline substance when pressed. What diagnostic test is indicated? a. Biopsy of the lesions b. Endocrine studies c. Rheumatoid factor d. Uric acid chemical profile These lesions are consistent with gout and uric acid deposits. The provider should evaluate this by ordering a uric acid chemical profile. Biopsy is indicated for any small, crusted, ulcerated, or indurated lesion that doesn’t heal. Rheumatoid nodules indicate a need for rheumatoid profiles. Endocrine studies are ordered for patients with calcification nodules. REF: Definition and Epidemiology/Diagnostics Chapter 81: Cerumen Impaction Test Bank Multiple Choice 1. A provider is recommending a cerumenolytic for a patient who has chronic cerumen buildup. The provider notes that the patient has dry skin in the ear canal. Which preparation is FDA approved for this use? a. Carbamide peroxide b. Hydrogen peroxide c. Liquid docusate sodium d. Mineral oil Any preparation with carbamide peroxide is FDA approved as a cerumenolytic. Patients with dry skin in the ear canal should not use any product containing hydrogen peroxide. Liquid docusate sodium and mineral oil are often used, but do not have specific FDA approval. REF: Management 2. A patient complains of otalgia and difficulty hearing from one ear. The provider performs an otoscopic exam and notes a dark brown mass in the lower portion of the external canal blocking the patient’s tympanic membrane. What is the initial action? a. Ask the patient about previous problems with that ear b. Irrigate the canal with normal saline c. Prescribe a ceruminolytic agent for that ear d. Use a curette to attempt to dislodge the mass Before attempting to remove impacted cerumen, the provider must determine whether the TM is intact and should ask about pressure equalizing ear tubes, a history of ruptured TM, and previous ear surgeries. Once the TM is determined to be intact, the other methods may be attempted, although the curette should only be used if the mass is in the lateral third of the ear canal. REF: Management 3. A child has recurrent impaction of cerumen in both ears and the parent asks what can be done to help prevent this. What will the provider recommend? a. Clean the outer ear and canal with a soft cloth Test Bank 2 b. Removing cerumen with a cotton-tipped swab c. Try thermal-auricular therapy when needed d. Use an oral irrigation tool to remove cerumen Parents should be instructed to use a soft cloth to clean the outer ear and canal only. Use of a cotton-tipped swab or any other implement may push cerumen deeper into the canal and risk damaging the tympanic membrane. Thermal-auricular therapy is not recommended. Oral irrigation tools have high pressure and a risk of damage to the tympanic membrane. REF: Education and Health Promotion Chapter 82: Cholesteatoma Test Bank Multiple Choice 1. A child is diagnosed as having a congenital cholesteatoma. What is included in management of this condition? Select all that apply. a. Antibacterial treatment b. Insertion of pressure equalizing tubes c. Irrigation of the ear canal d. Removal of debris from the ear canal e. Surgery to remove the lesion , D, E Cholesteatoma is treated with antibiotics, removal of debris from the ear canal, and possibly surgery. PETs and irrigation of the ear canal are not part of treatment for cholesteatoma. REF: Management 2. A young child has a pale, whitish discoloration behind the tympanic membrane ™. The provider notes no scarring on the TM and no retraction of the pars flaccida. The parent states that the child has never had an ear infection. What do these findings most likely represent? a. Chronic cholesteatoma b. Congenital cholesteatoma c. Primary acquired cholesteatoma d. Secondary acquired cholesteatoma Patients without history of otitis media or perforation of the TM most likely have congenital cholesteatoma. Primary acquired cholesteatoma will include retraction of the pars flaccida. Secondary acquired cholesteatoma has findings associated with the underlying etiology. REF: Physical Examination Chapter 83: Impaired Hearing Test Bank Multiple Choice 1. Which are risk factors for developing hearing loss caused by presbycusis? Select all that apply. a. Diabetes b. GERD c. High blood pressure d. Liver disease e. Smoking , C, E Presbycus is a gradual degeneration within the cochlea that accompanies aging. Diabetes, high blood pressure, and smoking may hasten these changes. GERD and liver disease are not associated with an increased rate of changes. REF: Pathophysiology 2. A child who has recurrent otitis media fails a hearing screen at school. The provider suspects which type of hearing loss in this child? a. Central b. Conductive c. Mixed type d. Sensorineural A common cause of conductive loss is fluid in the middle ear as a result of chronic otitis media with effusion. Central hearing loss is related to CNS disorders. Mixed type hearing loss is related to causes of both conductive and sensorineural hearing loss. Sensorineural hearing loss is caused by damage to the structures in the inner ear, usually caused by infection, barotrauma, or trauma. REF: Pathophysiology 3. A screening audiogram on a patient is abnormal. Which test may the primary provider perform next to further evaluate the cause of this finding? a. Impedance audiometry b. Pure tone audiogram c. Speech reception test d. Tympanogram A screening tympanogram may be performed by a primary provider to determine tympanic membrane mobility and may help in identifying the presence of infection, fluid, or changes in middle ear pressure. The other tests are performed by audiologists, not primary care providers. REF: Diagnostics Chapter 84: Inner Ear Disturbances Test Bank Multiple Choice 1. A patient is suspected of having vestibular neuritis. Which finding on physical examination is consistent with this diagnosis? a. Facial palsy and vertigo b. Fluctuating hearing loss and tinnitus c. Spontaneous horizontal nystagmus d. Vertigo with changes in head position Many patients with vestibular neuritis will exhibit spontaneous horizontal or rotary nystagmus, away from the affected ear. Facial palsy with vertigo occurs with Ramsay Hunt syndrome, caused by herpes zoster. Fluctuating hearing loss with tinnitus is common in Meniere’s disease. Tinnitus may occur with vestibular neuritis, but hearing loss does not occur. Patients with benign paroxysmal positional vertigo will exhibit vertigo associated with changes in head position. REF: Vestibular Neuritis/Physical Examination/Differential Diagnosis 2. Which symptoms may occur with vestibular neuritis? Select all that apply. a. Disequilibrium b. Fever c. Hearing loss d. Nausea and vomiting e. Tinnitus , D, E Vestibular neuritis can cause severe vertigo, disequilibrium, nausea, vomiting, and tinnitus, but not fever or hearing loss. REF: Vestibular Neuritis/Clinical Presentation/Physical Examination 3. A patient reports several episodes of acute vertigo, some lasting up to an hour, associated with nausea and vomiting. What is part of the initial diagnostic workup for this patient? a. Audiogram and MRI b. Auditory brainstem testing c. Electrocochleography d. Vestibular testing An audiogram and MRI are part of basic testing for Meniere’s disease. The other testing may be performed by an otolaryngologist after referral. REF: Meniere’s Disease/Diagnostics Chapter 85: Otitis Externa Test Bank Multiple Choice 1. A patient reports a feeling of fullness and pain in both ears and the practitioner elicits exquisite pain when manipulating the external ear structures. What is the likely diagnosis? a. Acute otitis externa b. Acute otitis media c. Chronic otitis externa d. Otitis media with effusion This patient’s symptoms are classic for acute otitis externa. Chronic otitis externa more commonly presents with itching. Acute otitis media is accompanied by fever and tympanic membrane inflammation, but not external canal inflammation. Otitis media with effusion causes a sense of fullness but not pain. REF: Clinical Presentation/Box 85-1: Differential Diagnosis 2. Which are risk factors for developing otitis externa? Select all that apply. a. Cooler, low-humidity environments b. Exposure to someone with otitis externa c. Having underlying diabetes mellitus d. Use of ear plugs and hearing aids e. Vigorous external canal hygiene , D, E Otitis externa is a cellulitis of the external canal that develops when the integrity of the skin is compromised. Diabetes mellitus predisposes patients to skin disorders. Using devices that cause moisture retention and irritation will increase the risk. Vigorous cleansing removes protective cerumen. Warm, high-humidity environments increase risk. The disease is not contagious. REF: Definition and Epidemiology/Pathophysiology 3. A patient has an initial episode otitis external associated with swimming. The patient’s ear canal is mildly inflamed and the tympanic membrane is not involved. Which medication will be ordered? a. Cipro HC b. Fluconazole c. Neomycin d. Vinegar and alcohol In the absence of a culture, the provider should choose a medication that is effective against both P. aeruginosa and S. aureus. Cipro HC covers both organisms and also contains a corticosteroid for inflammation. Fluconazole is an oral anti-fungal medication used when fungal infection is present. Neomycin alone does not cover these organisms. Vinegar and alcohol is used to treat mild fungal infections. REF: Management Chapter 86: Otitis Media Test Bank Multiple Choice 1. Which symptoms in children are evaluated using a parent-reported scoring system to determine the severity of pain in children with otitis media? Select all that apply. a. Appetite b. Difficulty sleeping c. Level of cooperation d. Poor hearing e. Tugging on ears , B, E Decreased appetite, difficulty sleeping, and tugging on ears are part of the Acute Otitis Media Severity of Symptom Scale used to evaluate pediatric pain. Children may refuse to cooperate for reasons other than pain. Poor hearing is not part of the pain assessment. REF: Clinical Presentation and Physical Examination 2. Which patient may be given symptomatic treatment with 24 hours follow-up assessment without initial antibiotic therapy? a. A 36 month old with fever of 38.5° C, mild otalgia, and red, non-bulging TM b. A 4 year old, afebrile child with bilateral otorrhea c. A 5 year old with fever of 38.0° C, severe otalgia, and red, bulging TM d. A 6 month old with fever of 39.2° C, poor sleep and appetite and bulging TM Children older than 24 months with fever less than 39° C and non-severe symptoms may be watched for 24 hours with symptomatic treatment. Children with otorrhea, those with severe AOM, and any children with fever greater than 39° C should be given antibiotics. REF: Management 3. A pediatric patient has otalgia, fever of 38.8° C, and a recent history of upper respiratory examination. The examiner is unable to visualize the tympanic membranes in the right ear because of the presence of cerumen in the ear canal. The left tympanic membrane is dull gray with fluid levels present. What is the correct action? a. Perform a tympanogram on the right ear b. Recommend symptomatic treatment for fever and pain c. Remove the cerumen and visualize the tympanic membrane d. Treat empirically with amoxicillin 80 to 90 mg/kg/day The AAP 2013 guidelines strongly recommend visualization of the tympanic membrane to accurately diagnose otitis media and not to treat based on symptoms alone. The practitioner should attempt to remove the cerumen in order to visualize the tympanic membrane. A tympanogram cannot be performed when cerumen is blocking the canal. Because the child may have an acute ear infection, antibiotics may be necessary. REF: Clinical Presentation and Physical Examination Chapter 87: Tympanic Membrane Perforation Test Bank Multiple Choice 1. A patient reports ear pain and difficulty hearing. An otoscopic examination reveals a small tear in the tympanic membrane of the affected ear with purulent discharge. What is the initial treatment for this patient? a. Insert a wick into the ear canal b. Irrigate the ear canal to remove the discharge c. Prescribe antibiotic ear drops d. Refer the patient to an otolaryngologist This perforation is most likely due to infection and should be treated with antibiotic ear drops. Wicks are used for otitis externa. The ear canal should not be irrigated to avoid introducing fluid into the middle ear. It is not necessary to refer unless the perforation does not heal. REF: Clinical Presentation and Physical Examination/Management 2. A patient reports ear pain after being hit in the head with a baseball. The provider notes a perforated tympanic membrane. What is the recommended treatment? a. Order antibiotic ear drops if signs of infection occur b. Prescribe analgesics and follow up in 1 to 2 days c. Reassure the patient that this will heal without problems d. Refer the patient to an otolaryngologist for evaluation Patients with traumatic or blast injuries causing perforations of the tympanic membranes should be referred to specialists to determine whether damage to inner ear structures has occurred. For an uncomplicated perforation, the other interventions are all appropriate. REF: Complications and Indications for Referral Chapter 88: Chronic Nasal Congestion and Discharge Test Bank Multiple Choice 1. A patient reports persistent nasal blockage, nasal discharge, and facial pain lasting on the right side for the past 4 months. There is no history of sneezing or eye involvement. The patient has a history of seasonal allergies and takes a non-sedating antihistamine. What does the provider suspect is the cause of these symptoms? a. Allergic rhinitis b. Autoimmune vasculitides c. Chronic rhinosinusitis d. Rhinitis medicamentosa Chronic rhinosinusitis is present when symptoms occur longer than 3 months. Sneezing and itchy, watery eyes tend to occur with allergic rhinitis. Autoimmune vasculitides affects upper and lower respiratory tracts as well as the kidneys. Rhinitis medicamentosa occurs with use of nasal decongestants and not oral antihistamines. REF: Clinical Presentation/Differential Diagnosis/Table 88-1: Comparison of Clinical Presentations of Chronic Rhinosinusitis and Allergic Rhinitis 2. A provider determines that a patient has chronic rhinosinusitis without nasal polyps. What is the first-line treatment for this condition? a. Intranasal corticosteroids b. Oral decongestants c. Systemic corticosteroids d. Topical decongestants Intranasal corticosteroids are the mainstay of treatment for CRS. Oral decongestants should be used sparingly, only when symptoms are intolerable. Topical decongestants can cause rebound symptoms. Systemic steroids are not indicated. REF: Management 3. A pregnant woman develops nasal congestion with chronic nasal discharge. What is the recommended treatment for this patient? a. Intranasal corticosteroids b. Prophylactic antibiotics c. Saline lavage d. Topical decongestants Saline lavage is recommended for pregnancy rhinitis; the condition will resolve after delivery. There is no human data on the safety of intranasal corticosteroids during pregnancy. Prophylactic antibiotics are not indicated; this is not an infectious condition. Topical decongestants can cause rebound symptoms. REF: Management Chapter 89: Epistaxis Test Bank Multiple Choice 1. A patient has recurrent epistaxis without localized signs of irritation. Which laboratory tests may be performed to evaluate this condition? Select all that apply. a. BUN and creatinine b. CBC with platelets c. Liver function tests d. PT and PTT e. PT/INR , D, E A CBC with platelets is part of the diagnostic workup along with coagulation studies. LFTs and renal function tests aren’t used to evaluate recurrent epistaxis. REF: Diagnostics 2. A patient is in the emergency department with unilateral epistaxis that continues to bleed after 15 minutes of pressure on the anterior septum and application of a topical nasal decongestant. The provider is unable to visualize the site of the bleeding. What is the next measure for this patient? a. Chemical cautery b. Electrocautery c. Nasal packing d. Petrolatum ointment Nasal packing is used if bleeding continues after initial measures. Chemical cautery and electrocautery are used only if the site of bleeding is visualized. Petrolatum ointment is applied once the bleeding is stopped. REF: Management/Anterior Epistaxis 3. A patient has bilateral bleeding from the nose with bleeding into the pharynx. What is the initial intervention for this patient? a. Apply firm, continuous pressure to the nostrils b. Assess airway safety and vital signs c. Clear the blood with suction to identify site of bleeding d. Have the patient sit up straight and tilt the head forward Bilateral epistaxis into the pharynx is more indicative of a posterior bleed which is more likely to be severe. The most important intervention is to ensure airway safety and determine stability of vital signs. Other measures are taken as needed. REF: Physical Examination Chapter 90: Nasal Trauma Test Bank Multiple Choice 1. A provider performs a nasal speculum examination on a patient who sustained nasal trauma in a motor vehicle accident. The provider notes marked swelling of the nose, instability and crepitus of the nasal septum with no other facial bony abnormalities and observes a rounded bluish mass against the nasal septum. Which action is necessary at this time? a. CT scan of facial structures b. Ice packs to reduce facial swelling c. Surgery to reduce the nasal fracture d. Urgent drainage of the mass A rounded bluish or purplish mass indicates a septal hematoma and must be drained urgently for cosmetic purposes to prevent loss of nasal cartilage caused by loss of blood supply to this area. This patient has no signs of facial fractures, so this exam may be deferred. Ice packs are part of ongoing management, but not a priority. The nasal fracture may be reduces within the first 3 to 5 days after injury. REF: Physical Examination/Management/Complications 2. An alert, irritable 12-month-old child is brought to the emergency department by a parent who reports that the child fell into a coffee table. The child has epistaxis, periorbital ecchymosis, and nasal edema. Nares are patent and the examiner palpates instability and point tenderness of the nasal septum. The orbital structures appear intact. What is an urgent action for this patient? a. Assessment of tetanus vaccination b. Ice, head elevation, and analgesia c. Immediate nasal reduction surgery d. Involvement of social services Young children and infants generally do not engage in activities that cause the high impact needed to cause a nasal fracture and nasal structures, which have more cartilage than adults, are at much lower risk of fracture. Child abuse must be suspected in this case. Assessment of tetanus status and application of symptomatic treatment may be ongoing, but are not urgent. Nasal reduction surgery may be deferred for several days. REF: Physical Examination/Management/Lifespan Considerations/Pediatric 3. A child is hit with a baseball bat during a game and sustains an injury to the nose, along with a transient loss of consciousness. A health care provider at the game notes bleeding from the child’s nose and displacement of the septum. What is the most important intervention at this time? a. Apply ice to the injured site to prevent airway occlusion b. Immobilize the child’s head and neck and call 911 c. Place nasal packing in both nares to stop the bleeding d. Turn the child’s head to the side to prevent aspiration of blood Nasal trauma resulting in loss of consciousness and possible neck injury are emergencies. The provider should take cervical spine precautions and call 911 for transport to an emergency room. The other interventions may be performed once the child’s head and neck are stable. REF: Clinical Presentation Chapter 91: Rhinitis Test Bank Multiple Choice 1. A patient has recurrent sneezing, alterations in taste and smell, watery, itchy eyes, and thin, clear nasal secretions. The provider notes puffiness around the eyes. The patient’s vital signs are normal. What is the most likely diagnosis for this patient? a. Acute sinusitis b. Allergic rhinitis c. Chronic sinusitis d. Viral rhinitis Patients with symptoms described above typically have allergic rhinitis. Sinusitis causes facial pain, fever, and purulent discharge. Viral rhinitis will also cause purulent discharge and other symptoms of URI. REF: Allergic Rhinitis/Clinical Presentation 2. A patient has seasonal rhinitis symptoms and allergy testing reveals sensitivity to various trees and grasses. What is the first-line treatment for this patient? a. Antihistamine spray b. Intranasal cromolyn c. Intranasal steroids d. Oral antihistamines Intranasal steroids are the mainstay of treatment and are the most effective medication for preventing symptoms. Antihistamine sprays are helpful, but are not first-line treatments. Intranasal cromolyn can be effective, but must be used four times daily. Oral antihistamines are used in conjunction with intranasal steroids, but are less effective than the steroids. REF: Allergic Rhinitis/Medications 3. A patient is concerned about frequent nasal stuffiness and congestion that begins shortly after getting out of bed in the morning. The patient denies itching and sneezing. A physical examination reveals erythematous nasal mucosa with scant watery discharge. What treatment will the provider recommend for this patient? a. Consultation for immunotherapy b. Daily intranasal steroids c. Oral antihistamines each morning d. Oral decongestants as needed This patient has symptoms of vasomotor or idiopathic rhinitis. Intranasal steroids are an effective treatment. Immunotherapy is not effective. This type of rhinitis typically does not respond to antihistamines. Oral decongestants are effective, but are best used around the clock, not just prn. REF: Vasomotor Rhinitis/Management Chapter 92: Sinusitis Test Bank Multiple Choice 1. A patient is concerned about frequent nasal stuffiness and congestion that begins shortly after getting out of bed in the morning. The patient denies itching and sneezing. A physical examination reveals erythematous nasal mucosa with scant watery discharge. What treatment will the provider recommend for this patient? a. Consultation for immunotherapy b. Daily intranasal steroids c. Oral antihistamines each morning d. Oral decongestants as needed Intranasal steroids should be considered for symptomatic relief for patients with sinusitis, especially those with allergic rhinitis. Oral mucolytics have little support in efficacy. Saline solution rinses may provide some relief, but there is no evidence to support their usefulness. Topical decongestants do decrease nasal congestion and edema, but the potential harm of rebound congestion requires recommendation with caution. REF: Management 2. Which are potential complications of chronic or recurrent sinusitis? Select all that apply. a. Allergic rhinitis b. Asthma c. Meningitis d. Orbital infection e. Osteomyelitis , D, E Complications of chronic or recurrent sinusitis include spread of infection to other tissues and may cause meningitis, orbital cellulitis, and osteomyelitis. Allergic rhinitis and asthma are associated with chronic sinusitis, but not complications of this condition. REF: Complications 3. A patient has nasal congestion, fever, purulent nasal discharge, headache, and facial pain and begins treatment with amoxicillin-clavulanate. At a follow-up visit 10 days after initiation of treatment, the patient continues to have purulent discharge, congestion, and facial pain without fever. What is the next course of action for this patient? a. A CT scan of the paranasal sinuses b. A referral to an otolaryngologist c. A second course of amoxicillin-clavulanate d. A trial of azithromycin This patient may have subacute sinusitis and may benefit from a second course of the antibiotic. The lack of fever shows improvement, so this antibiotic may be used. CT scan is usually not performed in adults unless other complications are present or suspected. Referral to an otolaryngologist is necessary if no improvement after the second course of antibiotics. Azithromycin is not used in adults unless pregnant, due to resistance patterns. REF: Clinical Presentation/Diagnostics/Management Chapter 93: Smell and Taste Disturbances Test Bank Multiple Choice 1. An elderly patient has a permanent loss of the sense of smell and diminished taste. What will be included in teaching this patient about managing these symptoms? Select all that apply. a. Avoiding perfumes and perfumed soaps b. Eating regular meals at scheduled times c. Putting dates on food in the refrigerator d. The importance of installing smoke detectors e. Using gas rather than electrical appliances , C, D Patients with diminished or absent smell or taste are at risk because of the inability to detect spoiled foods or gas stoves and a tendency to lose interest in eating. It is not necessary to avoid perfumes, but patients should be counseled to eat regular meals, put dates on foods in the refrigerator, and install smoke detectors. They should avoid gas stoves. REF: Geriatrics/Patient and Family Education and Health Promotion 2. A patient reports that meat smells different than it used to. What word describes this dysfunction? a. Aliageusia b. Anosmia c. Dysgeusia d. Parosmia Parosmia refers to smell distortion. Aliageusia is unpleasant taste. Anosmia is a loss of the sense of smell. Dysgeusia is persistent taste. REF: Definition and Epidemiology Chapter 94: Tumors and Polyps of the Nose Test Bank Multiple Choice 1. A provider examines a patient who has chronic nasal obstruction, respiratory tract symptoms, and generalized malaise. An examination of the nasal mucosa reveals ulceration of the nasal septum. What is the most important action when caring for this patient? a. Administering prednisone b. Obtaining a chest radiograph c. Performing laboratory tests d. Referring to a specialist This patient has symptoms of granulomatosis with polyangitis (GPA) and should be referred as soon as the disease is suspected. The other actions will be taken, but referral is the most important. REF: Granulomatosis with Polyangitis/Clinical Presentation/Management and Indications for Referral or Hospitalization 2. A patient reports chronic nasal obstruction and difficulty distinguishing smells. The provider examines the nares with a nasal speculum and observes several grapelike lesions in both nostrils. What is the likely cause of this patient’s symptoms? a. Chronic sinusitis b. Nasal polyps c. Squamous cell carcinoma d. Vascular benign tumor Polyps cause obstruction and olfactory dysfunction and appear as grapelike lesions on the nasal mucosa. Most malignant neoplasms are asymptomatic until late in the course. Chronic sinusitis characteristically produces inflammation and purulent discharge. REF: Clinical Presentation 3. A patient reports chronic nasal obstruction and recurrent epistaxis. Which type of nasal mass is likely? a. Inverted papilloma b. Nasal polyp c. Paranasal lymphoma Test Bank 2 d. Squamous cell carcinoma Inverted papillomas are benign tumors of the nasal mucosa and are highly vascular with frequent bleeding. Nasal polyps typically do not bleed and are associated with allergies. Paranasal lymphoma and squamous cell carcinoma are not initially associated with bleeding. REF: Pathophysiology Chapter 95: Dental Abscess Test Bank Multiple Choice 1. A patient has been taking amoxicillin for treatment of a dental abscess. In a follow-up visit, the provider notes edema of the eyelids and conjunctivae. What is the next action? a. Hospitalize the patient for an endodontist consultation b. Prescribe amoxicillin clavulanate for 10 to 14 days c. Recommend follow up with a dentist in 2 to 3 days d. Suggest using warm compresses to the eyes for comfort This patient has signs of complications and requires hospitalization with management by a dentist or endodontist. Changing the antibiotic without consultation is not recommended. Prompt hospitalization is required. REF: Indications for Referral or Hospitalization 2. A patient reports tooth pain in a lower molar and the provider notes a mobile tooth with erythema and edema of the surrounding tissues without discharge. Which is the initial course of action by the provider? a. Perform an incision and drainage of the edematous tissue b. Prescribe amoxicillin and refer to a dentist in 2 to 3 days c. Recommend oral antiseptic rinses and follow up in one week d. Refer to an oral surgeon for emergency surgery The primary provider may prescribe antibiotics, especially if the surrounding tissues are infected. Patients should follow up with a dentist in 2 to 3 days. The primary provider generally does not perform I&D; this should be done by the dentist. Follow up should be with a dentist in 2 to 3 days, not one week. Emergency surgery is indicated if there is a question of airway compromise. REF: Management Chapter 96: Diseases of the Salivary Glands Test Bank Multiple Choice 1. A patient has a chronic swelling of the parotid gland that is unresponsive to antibiotics and which has not increased in size. Which diagnostic test is indicated? a. Computed tomography b. Fine needle aspiration c. Magnetic resonance imaging d. Plain film radiography Chronic lesions may represent tuberculosis or malignancies, so fine needle aspiration is indicated to rule out these diseases. Radiological studies are used to identify the extent of disease, but are usually not diagnostic. REF: Diagnostics 2. A patient reports painful swelling in the mouth with increased pain at mealtimes. The provider notes a mass in the salivary gland region. What is the likely cause of these symptoms? a. Basal cell adenoma b. Sialolithiasis c. Sjogren syndrome d. Warthin’s tumor Sialolithiasis is a non-infectious salivary gland disorder characterized by pain at mealtimes caused by blockage of the salivary duct by stones. Basal cell adenoma is a noninfectious cause of salivary gland inflammation that is generally painless. Sjogren syndrome manifests with xerostomia and abnormal taste. Warthin’s tumor causes a painless, unilateral mass. REF: Clinical Presentation 3. A patient has parotitis and cultures are positive for actinomycosis. What is the initial treatment for this condition? a. Intravenous penicillin b. Oral clindamycin c. Oral erythromycin d. Topical antibiotics IV penicillin, followed by oral PCN for several months is indicated for actinomycosis. Clindamycin and erythromycin are used for PCN allergy. Topical antibiotics are not effective. REF: Management Chapter 97: Epiglottitis Test Bank Multiple Choice 1. An adult patient has epiglottitis secondary to a chemical burn. Which medication will be given initially to prevent complications? a. Chloramphenicol b. Clindamycin c. Dexamethasone d. Metronidazole This case of epiglottitis does not have an infectious cause, so antibiotics are not given unless there are symptoms of infection. A corticosteroid can decrease the need for intubation. REF: Management 2. An adult patient is seen in clinic with fever, sore throat, and dysphagia. Which diagnostic test will the provider order to confirm a diagnosis of epiglottitis? a. Blood cultures b. Complete blood count c. Fiberoptic nasopharyngoscopy d. Lateral neck film Fiberoptic nasopharyngoscopy allows direct visualization of the epiglottis and is used increasingly with adult patients suspected of having epiglottitis. Blood cultures and a CBC may be drawn as part of the workup to help guide antimicrobial therapy, but are not diagnostic. A lateral neck film is not always diagnostic with adults. REF: Diagnostics 3. The provider sees a child with a history of high fever and sore throat. When entering the exam room, the provider finds the child sitting in the tripod position and notes stridor, drooling, and anxiety. What is the initial action for this patient? a. Administer empiric intravenous antibiotics and steroids b. Have the child lie down and administer high-flow, humidified oxygen c. Obtain an immediate consultation with an otolaryngologist d. Perform a thorough examination of the oropharynx Patients with suspected epiglottitis, with high fever, sore throat, stridor, drooling, and respiratory distress, should be referred immediately to otolaryngology. Starting an IV or having the child lie down will increase distress and may precipitate laryngospasm. The throat should not be examined because it may cause laryngospasm REF: Diagnostics/Management Chapter 98: Oral Infections Test Bank Multiple Choice 1. A patient reports painful oral lesions 3 days after feeling pain and tingling in the mouth. The provider notes vesicles and ulcerative lesions on the buccal mucosa. What is the most likely cause of these symptoms? a. Bacterial infection b. Candida albicans c. Herpes simplex virus d. Human papilloma virus HSV infections generally start with a prodrome of tingling, pain, and burning followed by vesicular and ulcerative lesions. Bacterial infection presents with inflammation of the gingiva, bleeding, and ulceration with or without purulent discharge. Candida albicans appear as white, cottage cheese-like lesions that may be removed, but may cause bleeding when removed. HPV manifests as white, verrucous lesions individually or in clusters. REF: Clinical Presentation 2. A patient has gingival inflammation with several areas of ulceration and a small amount of purulent discharge. What is required to diagnose this condition? a. Culture and sensitivity b. Microscopic exam of oral scrapings c. Physical examination d. Tzanck smear This patient has symptoms consistent with gingivitis, which may be diagnosed by physical examination alone. Cultures are not necessary unless systemic disease is present. A microscopic exam of oral scrapings to look for hyphae may be performed to diagnose candida infections. A Tzanck smear is performed to confirm a diagnosis of herpes simplex. REF: Clinical Presentation/Diagnostics 3. A patient has painful oral lesions and the provider notes several white, verrucous lesions in clusters throughout the mouth. What is the recommended treatment for this patient? a. Nystatin oral suspension b. Oral acyclovir c. Oral hygiene measures d. Surgical excision White, verrucous lesions in clusters are diagnostic for HPV infection which is treated with surgical excision. Nystatin suspension is given for candida infection. Oral acyclovir is used for HSV infection. Oral hygiene measures are used for gingivitis. REF: Clinical Presentation/Management Chapter 99: Parotitis Test Bank Multiple Choice 1. Which physical examination finding suggests viral rather than bacterial parotitis? a. Clear discharge from Stensen’s duct b. Enlargement and pain of affected glands c. Gradual reduction in saliva production d. Unilateral edema of parotid glands Viral parotitis generally produces clear discharge. Enlargement and pain of affected glands may be non-specific or is associated with TB infection. A gradual reduction in saliva, resulting in xerostomia, is characteristic of HIV infection. Unilateral edema is more often bacterial. REF: Clinical Presentation 2. A patient who has acute suppurative parotitis has been taking amoxicillin-clavulanate for 4 days without improvement in symptoms. The provider will order an antibiotic for Methicillin-resistant S. aureus. Which other measure may be helpful? a. Cool compresses b. Discouraging chewing gum c. Surgical drainage d. Topical corticosteroids If improvement does not occur after 3 to 4 days of antibiotics, surgical drainage is appropriate. Warm compresses are recommended for comfort. Chewing gum and other sialogogues to stimulate the production of saliva are recommended. Steroids are questionable and topical steroids will have little effect. REF: Management 3. What are factors associated with acute suppurative parotitis? Select all that apply. a. Allergies b. Anticholinergic medications c. Diabetes mellitus d. Hypervolemia e. Radiotherapy , C, E Anticholinergic medications decrease salivary flow and increase the risk for parotitis. Chronic diseases, including diabetes mellitus, can increase the risk. Radiotherapy and other procedures may increase the risk. Allergies and hypervolemia do not increase the risk. REF: Definitions and Epidemiology Chapter 100: Peritonsillar Abscess Test Bank Multiple Choice 1. An adolescent has fever, chills, and a severe sore throat. On exam, the provider notes foul- smelling breath and a muffled voice with marked edema and erythema of the peritonsillar tissue. What will the primary care provider do? a. Evaluate for possible epiglottitis b. Perform a rapid strep and throat culture c. Prescribe empiric oral antibiotics d. Refer the patient to an otolaryngologist This patient has clinical signs of peritonsillar abscess, which may be diagnosed on clinical signs alone. Patients with peritonsillar abscess should be referred to an otolaryngologist for possible I&D of the abscess and hospitalization for IV antibiotics. A rapid strep and culture are not indicated. Oral antibiotics generally do not work. REF: Clinical Presentation/Management 2. A patient is diagnoses with peritonsillar abscess and will be hospitalized for intravenous antibiotics. What additional treatment will be required? a. Intubation to protect the airway b. Needle aspiration of the abscess c. Systemic corticosteroid administration d. Tonsillectomy and adenoidectomy Needle aspiration, antibiotics, pain medication, and hydration can effectively treat peritonsillar abscess. Intubation is not performed unless the airway is compromised. Systemic corticosteroid administration is useful, but not required in all cases. Tonsillectomy alone is sometimes performed if recurrent tonsillitis or peritonsillar abscess is present. REF: Management Chapter 101: Pharyngitis and Tonsillitis Test Bank Multiple Choice 1. A patient has sore throat, a temperature of 38.5° C, tonsillar exudates, and cervical lymphadenopathy. What will the provider do next to manage this patient’s symptoms? a. Order an antistreptolysin O titer b. Perform a rapid antigen detection test c. Prescribe empiric penicillin d. Refer to an otolaryngologist The RADT is performed initially to determine whether GAS is present. The ASO titer is not used during initial diagnostic screening. Penicillin should not be given empirically. A referral to a specialist is not required for GAS infection. REF: Diagnostics 2. A patient reports a sudden onset of sore throat, fever, malaise, and cough. The provider notes mild erythema of the pharynx and clear rhinorrhea without cervical lymphadenopathy. What is the most likely cause of these symptoms? a. Allergic pharyngitis b. Group A streptococcus c. Infectious mononucleosis d. Viral pharyngitis Viral pharyngitis will cause sore throat, fever, and malaise and is often accompanied by URI symptoms of cough and runny nose. Allergic pharyngitis usually also causes dryness. GAS causes high fever, cervical adenopathy, and marked erythema with exudate. Infectious mononucleosis will cause an exudate along with cervical adenopathy. REF: Clinical Presentation/Physical Examination 3. A school-age child has had 5 episodes of tonsillitis in the past year and 2 episodes the previous year. The child’s parent asks the provider if the child needs a tonsillectomy. What will the provider tell this parent? a. Current recommendations do not support tonsillectomy for this child. b. If there is one more episode in the next 6 months, a tonsillectomy is necessary. c. The child should have radiographic studies to evaluate the need for tonsillectomy. d. Tonsillectomy is recommended based on this child’s history. Recommendations suggest 6 to 7 documented episodes of GAS within 1 year, 5/year for 2 consecutive years, or 3/year for 3 years. Radiographic studies are not indicated. REF: Management Chapter 102: Acute Bronchitis Test Bank Multiple Choice 1. An adult patient who had pertussis immunizations as a child is exposed to pertussis and develops a runny nose, low-grade fever, and upper respiratory illness symptoms without a paroxysmal cough. What is recommended for this patient? a. Azithromycin daily for 5 days b. Isolation if paroxysmal cough develops c. Pertussis vaccine booster d. Symptomatic care only Adults previously immunized against pertussis may still get the disease without the classic whooping cough sign seen in children and are contagious from the beginning of the catarrhal stage of runny nose and common cold symptoms. Azithromycin or other macrolide antibiotics are useful for reducing symptoms and for decreasing shedding of bacteria to limit spread of the disease. Patients should be isolated for 5 days from the start of treatment. Pertussis vaccine booster will not alter the course of the disease once exposed. Symptomatic care only will not reduce symptoms or decrease disease spread. REF: ManagementQ uestion 2 of 3 2. A patient develops a dry, non-productive cough and is diagnosed with bronchitis. Several days later, the cough becomes productive with mucoid sputum. What may be prescribed to help with symptoms? a. Antibiotic therapy b. Antitussive medication c. Bronchodilator treatment d. Mucokinetic agents Antitussive medications are occasionally useful for short-term relief of coughing. Antibiotic therapy is generally not needed and should be avoided unless a bacterial cause is likely. Bronchodilator medications show no demonstrated reduction in symptoms and are not recommended. Mucokinetic agents have no evidence to support their use. REF: Communication and Language Development 3. A patient develops acute bronchitis and is diagnosed as having influenza. Which medication will help reduce the duration of symptoms in this patient? a. Azithromycin b. Clindamycin c. Oseltamivir d. Trimethoprim-sulfamethoxazole Oseltamivir is an antiviral medication used to reduce the severity and duration of symptoms of influenza. The other medications are antibacterial medications and not effective to treat influenza. REF: Management Chapter 103: Asthma Test Bank Multiple Choice 1. A patient who has asthma calls the provider to report having a peak flow measure of 75%, shortness of breath, wheezing, and cough, and tells the provider that the symptoms have not improved significantly after a dose of albuterol. The patient uses an inhaled corticosteroid medication twice daily. What will the provider recommend? a. Administering two more doses of albuterol b. Coming to the clinic for evaluation c. Going to the emergency department d. Taking an oral corticosteroid The patient is experiencing an asthma exacerbation and should follow the asthma action plan (AAP) which recommends three doses of albuterol before reassessing. The peak flow is above 70%, so ED admission is not indicated. The patient may be instructed to come to the clinic for oxygen saturation and spirometry evaluation after administering the albuterol. An oral corticosteroid may be prescribed if the patient will be treated as an outpatient after following the AAP. REF: Management 2. An adult develops chronic cough with episodes of wheezing and shortness of breath. The provider performs chest radiography and other tests and rules out infection, upper respiratory, and gastroesophageal causes. Which test will the provider order initially to evaluate the possibility of asthma as the cause of these symptoms? a. Allergy testing b. Methacholine challenge test c. Peak expiratory flow rate d. Spirometry Spirometry is recommended at the time of initial assessment to confirm the diagnosis of asthma. Allergy testing is performed only if allergies are a possible trigger. The methacholine challenge test is performed if spirometry is inconclusive. PEFR is generally used to monitor asthma symptoms. REF: Diagnostics 3. A patient is seen in clinic for an asthma exacerbation. The provider administers three nebulizer treatments with little improvement, noting a pulse oximetry reading of 90% with 2 L of oxygen. A peak flow assessment is 70%. What is the next step in treating this patient? a. Administer three more nebulizer treatments and reassess b. Admit to the hospital with specialist consultation c. Give epinephrine injections and monitor response d. Prescribe an oral corticosteroid medication Patients having an asthma exacerbation should be referred if they fail to improve after three nebulizer treatments or three epinephrine injections, have a peak flow less than 70% and a pulse oximetry reading less than 90% on room air. Giving more nebulizer treatments or administering epinephrine are not indicated. The patient will most likely be given IV corticosteroids; oral corticosteroids would be given if the patient is managed as an outpatient. REF: Definition and Epidemiology Chapter 104: Chest Pain (Noncardiac) Test Bank Multiple Choice 1. A patient comes to an emergency department with chest pain. The patient describes the pain is sharp and stabbing and reports that it has been present for several weeks. Upon questioning, the examiner determines that the pain is worse after eating. The patient reports getting relief after taking a friend’s nitroglycerin during one episode. What is the most likely cause of this chest pain? a. Aortic dissection pain b. Cardiac pain c. Esophageal pain d. Pleural pain Pain that is constant for weeks or is sharp and stabbing is not likely to be cardiac in origin. Both esophageal and cardiac causes will be attenuated with sublingual nitroglycerin. Aortic dissection will cause an abrupt onset with the greatest intensity at the beginning of the pain. Pleural pain is usually related to deep breathing or cough.REF: Clinical Presentation 2. A patient has chronic chest pain that occurs after meals and the provider suspects gastroesophageal reflux disease (GERD). The provider prescribes a proton pump inhibitor and after 2 months the patient reports improvement in symptoms. What is the next action in treating this patient? a. Continue the proton pump inhibitor b. Order esophageal pH monitoring c. Refer the patient to a gastroenterologist d. Schedule an upper endoscopy Often the effectiveness of treatment with a PPI is diagnostic in itself and is equal to or better than more invasive and expensive testing. As long as the patient continues to show improvement, there is no need to order tests or refer for evaluation.REF: Diagnostics 3. A high school athlete reports recent onset of chest pain that is aggravated by deep breathing and lifting. A 12-lead electrocardiogram in the clinic is normal. The examiner notes localized pain near the sternum that increases with pressure. What will the provider do next? a. Order a chest radiograph b. Prescribe an antibiotic c. Recommend an NSAID d. Refer to a cardiologist This patient has symptoms consistent with chest wall pain because the chest pain occurs with specific movement and is easily localized. Since the ECG is normal, there is no need to refer to a cardiologist. The patient does not have symptoms of pneumonia so a radiograph or antibiotic is not needed. NSAIDs are recommended for comfort.REF: Management Chapter 105: Chronic Cough Test Bank Multiple Choice 1. A young adult patient develops a cough persisting longer than 2 months. The provider orders pulmonary function tests and a chest radiograph, which are normal. The patient denies abdominal complaints. There are no signs of rhinitis or sinusitis and the patient does not take any medications. What will the provider evaluate next to help determine the cause of this cough? a. 24-hour esophageal pH monitoring b. Methacholine challenge test c. Sputum culture d. Tuberculosis testing Chronic cough without other symptoms may indicate asthma. If PFTs are normal, a methacholine challenge test may be performed. 24-hour esophageal pH monitoring is sometimes performed to evaluate for GERD, but this patient does not have abdominal symptoms and this test is usually not performed because it is inconvenient. Sputum culture is not indicated. TB is less likely.REF: Diagnostics 2. A patient is recovering from Mycoplasma pneumoniae infection and has a persistent cough 6 weeks after the infection. What will the provider do? a. Perform chest radiography to assess for secondary infection b. Perform pulmonary function and asthma challenge testing c. Prescribe a second round of azithromycin to treat the persistent infection d. Reassure the patient that this is common after M. pneumoniae infection Post-infection cough is common after M. pneumoniae infection and may persist up to 8 weeks after the infection; this type of cough generally needs no intervention. It is not necessary to perform chest radiography unless secondary infection is suspected. Antibiotics are not indicated. Unless the cough persists after 8 weeks, asthma testing is not indicated.REF: Definition and Epidemiology 3. A non-smoking adult with a history of cardiovascular disease reports having a chronic cough without fever or upper airway symptoms. A chest radiograph is normal. What will the provider consider initially as the cause of this patient’s cough? a. ACE inhibitor medication use b. Chronic obstructive pulmonary disease c. Gastroesophageal reflux disease d. Psychogenic cough About 10% of patients taking ACE inhibitors will develop chronic cough. COPD, GERD, and psychogenic causes are possible, but given this patient’s cardiovascular history, the possibility of ACE inhibitor- induced cough should be investigated initially.REF: Differential Diagnosis Chapter 106: Chronic Obstructive Pulmonary Disease Test Bank Multiple Choice 1. Which is characteristic of chronic bronchitis and not emphysema? a. Damage to the alveolar wall b. Destruction of alveolar architecture c. Mild alteration in lung tissue compliance d. Mismatch of ventilation and perfusion Chronic bronchitis causes much less parenchymal damage than emphysema does, so there is milder alteration in lung tissue compliance. The other symptoms are characteristic of emphysema.REF: Pathophysiology 2. A patient with chronic obstructive pulmonary disease and reports daily symptoms of dyspnea and cough. Which medication will the prescriber order? a. Ipratropium bromide b. Pirbuterol acetate c. Salmeterol xinafoate d. Theophylline Ipratropium bromide is an anticholinergic medication and is used as first-line therapy in patients with daily symptoms. Pirbuterol acetate and salmeterol xinafoate are both beta2-adrenergics and are used to relieve bronchospasm; pirbuterol is a short-term medication used for symptomatic relief and salmeterol is a long-term medication useful for reducing nocturnal symptoms. Theophylline is a third-line agent.REF: Management 3. Which test is most diagnostic for chronic obstructive pulmonary disease? a. COPD Assessment Test b. Forced expiratory time maneuver c. Lung radiograph d. Spirometry for FVC and FEV1 Spirometry testing is the gold standard for diagnosis and assessment of COPD because it is reproducible and objective. The forced expiratory time maneuver is easy to perform in a clinic setting and is a good screening to indicate a need for confirmatory spirometry. Lung radiographs are non-specific, but may indicate hyperexpansion of lungs. The COPD assessment test helps measure health status impairment in persons already diagnosed with COPD.REF: Diagnostics Chapter 107: Dyspnea Test Bank Multiple Choice 1. A young adult patient without a previous history of lung disease has an increased respiratory rate and reports a feeling of “not getting enough air.” The provider auscultates clear breath sounds and notes no signs of increased respiratory effort. Which diagnostic test will the provider perform initially? a. Chest radiograph b. Complete blood count c. Computerized tomography d. Spirometry This patient has no signs indicating lung disease, but does exhibit signs of hypoxia. A CBC would evaluate for anemia, which is a more common cause of hypoxia in otherwise healthy adults. Chest radiography is used to evaluate infectious causes. CT is used if interstitial lung disease is suspected. Spirometry is useful to diagnose asthma and COPD.REF: Clinical Presentation/Diagnostics 2. A patient reports shortness of breath with activity and exhibits increased work of breathing with prolonged expirations. Which diagnostic test will the provider order to confirm a diagnosis in this patient? a. Arterial blood gases b. Blood cultures c. Spirometry d. Ventilation/perfusion scan The patient has signs of either asthma or COPD. Spirometry is essential to both the diagnosis and management of these diseases. ABGs are useful when evaluating severity of exacerbations, but are not specific to these diseases. Blood cultures are drawn if pneumonia is suspected. A ventilation/perfusion scan is performed to evaluate for pulmonary thromboembolic disease. REF: Diagnostics 3. An older patient with COPD is experiencing dyspnea and has an oxygen saturation of 89% on room air. The patient has no history of pulmonary hypertension or congestive heart failure. What will the provider order to help manage this patient’s dyspnea? a. Anxiolytic drugs b. Breathing exercises c. Opioid medications d. Supplemental oxygen Formal pulmonary rehabilitation programs, including breathing exercises, are used to manage long-term disease such as COPD. Anxiolytics and opioids must be used cautiously because of respiratory depression side effects. Medicare does not approve oxygen supplementation unless saturations are less than 88% on room air or for patients who have pulmonary hypertension or CHF who have saturations 89%.REF: Management Chapter 108: Hemoptysis Test Bank Multiple Choice 1. A patient with hemoptysis and no other symptoms has a normal chest radiograph, CT, and fiberoptic bronchoscopy studies. What is the next action in managing this patient? a. Observation b. Prophylactic antibiotics c. Specialist consultation d. Surgical intervention Patients with negative findings on CXR, CT, and bronchoscopy, with no risk factors may be observed for 3 years. Antibiotics are not indicated, since signs of infection are not present. Specialty consultation and surgery are not indicated.REF: Management 2. A patient reports coughing up a small amount of blood after a week of cough and fever. The patient has been previously healthy and does not smoke or work around pollutants or irritants. What will the provider suspect as the most likely cause of this patient’s symptoms? a. Infection b. Lung abscess c. Malignancy d. Thromboembolism In a healthy patient without risk factors who has a cough and fever, infection is the most likely cause. Lung abscess may occur, but is less likely. Malignancy is also less likely. Thromboembolism is more likely after surgery or with trauma.REF: Differential Diagnosis 3. A patient with a smoking history of 35 pack years reports having a chronic cough with recent symptoms of pink, frothy blood on a tissue. The chest radiograph shows a possible nodule in the right upper lobe. Which diagnostic test is indicated? a. Coagulation studies b. Computerized tomography c. Fiberoptic bronchoscopy d. Needle biopsy CT is suggested for initial evaluation of patients at high risk of malignancy, such as a smoker with >30 pack years, who have suspicious findings on chest radiography. Coagulation studies are performed for patients taking anticoagulants or a history of coagulopathy. Fiberoptic bronchoscopy is used with CT, but is not the initial test. Needle biopsy is performed if other tests indicate a tumor.REF: Diagnostics Chapter 109: Lung Cancer Test Bank Multiple Choice 1. A patient with small cell lung cancer (SCLC) has undergone chemotherapy with a good initial response to therapy. What will the provider tell this patient about the prognosis for treating this disease? a. Surgical resection will improve survival chances. b. That relapse is likely with a poor prognosis. c. There is an 80% chance of 5-year survival. d. Treatment will proceed with curative intent. Although SCLC often responds very well initially to chemotherapy, the majority of patients will relapse and the 5-year survival rates are approximately 10%. Surgical resection does not play a significant role in the management of SCLC because the majority of patients have metastatic disease at diagnosis. Treatment is generally palliative.REF: Small Cell Lung Cancer 2. When screening for metastatic cancer in a patient with lung cancer, the provider will assess for Select all that apply. a. complaints of headache. b. increased cough. c. low hematocrit. d. lymph nodes greater than 1 cm. e. unexplained weight gain. , C, D Headaches may indicate brain metastases. Low hematocrit and lymphadenopathy with nodes greater than 1 cm also indicate metastasis. Increased cough is a sign of lung cancer itself, not metastasis. Patients with metastatic cancer have unexplained weight loss of more than 10 pounds.REF: Clinical Presentation and Physical Examination 3. A patient with a cough has a suspicious lung lesion, a mediastinal lymph mass, and several bone lesions. What test is indicated to determine histology and staging of this cancer? a. Biopsy of a bone lesion b. Bone marrow aspiration and biopsy c. Bronchoscopy with lung biopsy d. Thoracentesis and pleural fluid cytology The diagnosis and stage should be determined in the least invasive manner possible. A single biopsy of the bone lesion can determine histology and staging. The other procedures are more invasive and not necessary.REF: Diagnostics Chapter 110: Pleural Effusions and Pleurisy Test Bank Multiple Choice 1. Which are causes of pleural effusions? Select all that apply. a. Allergies b. Breast cancer c. Bronchiectasis d. Congestive heart failure e. Dehydration , C, D Breast cancer, bronchiectasis, and CHF can all cause pleural effusions. Allergies and dehydration do not.REF: Pathophysiology 2. A patient complains of shortness of breath when in a recumbent position and reports coughing and pain associated with inspiration. The provider notes distended neck veins during the exam. What is the likely cause of these findings? a. Congestive heart failure b. Hepatic disease c. Pulmonary embolus d. Pulmonary infection CHF causes the symptoms described above, with distended neck veins being a significant finding. Hepatic disease would also cause abdominal distention with ascites and hepatomegaly. Pulmonary embolus has marked shortness of breath. Pulmonary infection causes inflammation and a friction rub.REF: Clinical Presentation/Differential Diagnosis Chapter 111: Pneumonia Test Bank Multiple Choice 1. A patient has a cough and fever and the provider auscultates rales in both lungs that do not clear with cough. The patient reports having a headache and sore throat prior to the onset of coughing. A chest radiograph shows patchy, nonhomogeneous infiltrates. Based on these findings, which organism is the most likely cause of this patient’s pneumonia? a. A virus b. Mycoplasma c. S. pneumoniae d. Tuberculosis Atypical pneumonias, such as those caused by mycoplasma often present with headache and sore throat and will have larger areas of infiltrate on chest radiograph. Viral pneumonias show more diffuse radiographic findings. S. pneumonia will have high fever and cough and distinct areas of infiltration.REF: Pathophysiology/Clinical Presentation 2. A young adult, previously healthy clinic patient has symptoms of pneumonia including high fever and cough. Auscultation reveals rales in the left lower lobe. A chest radiograph is normal. The patient is unable to expectorate sputum. Which treatment is recommended for this patient? a. A B-lactam antibiotic plus a fluoroquinolone b. A respiratory fluoroquinolone antibiotic c. Empiric treatment with a macrolide antibiotic d. Hospitalization for intravenous antibiotics This patient likely has community-acquired pneumonia. The patient has typical symptoms and, even though the chest radiograph is normal, will require outpatient treatment. For community- acquired pneumonia in a previously healthy individual, treatment with a macrolide antibiotic is the recommended first-line therapy. B-lactam plus fluoroquinolone therapy is used for patients in the ICU. Respiratory fluoroquinolones are used for patients with underlying disorders who develop pneumonia. Hospitalization is not necessary.REF: Management Test Bank 2 3. A patient who was initially treated as an outpatient for pneumonia and then hospitalized for two weeks after no improvement continues to show no improvement after several antibiotic regimens have been attempted. What is the next step in managing this patient? a. Administration of the pneumonia vaccine b. Increasing the dose of the antibiotics c. Open lung biopsy d. Performing diagnostic bronchoscopy Patients who do not respond to antibiotic therapy may have opportunistic fungal or other infections, bronchogenic carcinoma, or other diseases. Bronchoscopy can exclude or confirm these. The pneumonia vaccine is preventative for pneumococcal causes and will not help this patient. Increasing the dose of the antibiotics is not recommended. Open lung biopsy may be performed if a bronchoscopy is inconclusive.REF: Complications Chapter 112: Pneumothorax Test Bank Multiple Choice 1. A patient who has a central line develops respiratory compromise. What is the initial intervention for this patient? a. Lung ultrasonography to determine the cause b. Obtaining cultures and starting antibiotics c. Prompt removal of the central line d. Rapid assessment and resuscitation Patients with central lines are at increased risk for pneumothorax. Acute respiratory distress is a medical emergency and assessment and resuscitation should begin immediately. Lung US, cultures and antibiotics, and removal of the central line may be performed if indicated when the patient is stabilized.REF: Physical Examination 2. Which method of treatment is used for traumatic pneumothorax? a. Needle aspiration of the pneumothorax b. Observation for spontaneous resolution c. Placement of a small-bore catheter d. Tube thoracostomy Traumatic pneumothorax requires tube thoracostomy because of its ability to drain larger volumes of air along with blood and fluids. Needle aspiration is safe for primary pneumothorax. Observation for spontaneous resolution is indicated for small pneumothoraxes.REF: Management Chapter 113: Pulmonary Embolism Test Bank Multiple Choice 1. Which clinical sign is especially worrisome in a patient with a pulmonary embolism? a. Abnormal lung sounds b. Dyspnea c. Hypotension d. Tachycardia Hypotension in a patient with PE has a high correlation with acute right ventricular failure and subsequent death. The other signs are common with PE.REF: Diagnosis 2. A patient who has undergone surgical immobilization for a femur fracture reports dyspnea and chest pain associated with inspiration. The patient has a heart rate of 120 beats per minute. Which diagnostic test will confirm the presence of a pulmonary embolism? a. Arterial blood gases b. CT angiography c. D-dimer d. Electrocardiogram Ct angiography is used to diagnose PE. D-dimer assays have good negative predictive value but have poor positive predictive value, making it useful for excluding but not confirming the presence of PE. An ECG does not confirm PE but is used to demonstrate comorbid conditions. Arterial blood gases do not confirm PE and are used to identify the degree of respiratory compromise.REF: Diagnostics 3. A patient develops a pulmonary embolism after surgery and shows signs of right-sided heart failure. Which drug will be administered to this patient? a. Low molecular heparin b. Tissue plasminogen activator c. Unfractionated heparin d. Warfarin Fibrinolytic therapy with recombinant tissue plasminogen activator is given to patients with hypotension and right-sided heart failure. Heparin is used for its anticoagulant properties in all patients with PE. Warfarin is not indicated.REF: Management Chapter 114: Pulmonary Hypertension Test Bank Multiple Choice 1. A patient with increased left-sided heart pressure will have which type of pulmonary hypertension? a. Group 2 b. Group 3 c. Group 4 d. Group 5 Group 2 pulmonary hypertension is associated with increased left-sided heart pressure.REF: Definition and Epidemiology 2. A patient who has had mild pulmonary hypertension with a previous symptom of a loud second heart sound on exam now has edema and jugular vein distension. This indicates which complication? a. Left ventricular dysfunction b. Right ventricular dysfunction c. Tricuspid valve involvement d. Mitral valve involvement Right ventricular dysfunction occurs as the disease worsens with manifestations that include jugular vein distension, edema, and increased liver size. These symptoms do not indicate left ventricular dysfunction or valvular involvement.REF: Physical Examination 3. A patient with pulmonary arterial hypertension (PAH) has increased dyspnea with activity. Which drug may be prescribed to manage this on an outpatient basis? a. An inhaled prostanoid b. Bosentan c. Epoprostenol d. Trepostinil Bosentan helps promote pulmonary artery smooth muscle cell proliferation and improves exercise capacity. It is also given PO, so is easy to give on an outpatient basis. Inhaled prostanoids have a short half-life and must be given 6 to 9 times daily. Epoprostenol has a short half-life and must be given IV. Trepostinil is given IV.REF: Management/Table 114—1: Therapies for Pulmonary Arterial Hypertension Chapter 115: Sarcoidosis Test Bank Multiple Choice 1. A patient who has dyspnea and chest pain along with occasional chills and night sweats has a chest radiograph that shows bilateral hilar lymphadenopathy and pulmonary infiltrates. The provider suspects which classification of sarcoidosis? a. Stage 1 b. Stage 2 c. Stage 3 d. Stage 4 Stage 1 sarcoidosis is classified based on bilateral hilar lymphadenopathy (BHL) only. Stage 2 presents with BHL and pulmonary infiltrates, Stage 3 with pulmonary infiltrates without BHL, and stage 4 with pulmonary fibrosis.REF: Diagnostics 2. A patient with stage 1 sarcoidosis who is taking a nonsteroidal anti-inflammatory medication to treat joint discomfort develops mild dyspnea and cough. Which medication will be added to treat this symptom? a. A beta-adrenergic medication b. An antimalarial agent c. An immunosuppressant drug d. An oral corticosteroid Corticosteroids are begun when pulmonary symptoms develop. Beta-adrenergics are not used. Antimalarial agents are used to treat chronic skin lesions. Immunosuppressants are used when corticosteroids are no longer effective or when the disease progresses.REF: Management 3. When following a patient with sarcoidosis over time, which diagnostic test is useful to help monitor the progression of the disease? a. Chest radiographs b. Erythrocyte sedimentation rate c. Pulmonary function test d. Radionucleotide scanning Pulmonary function tests may be normal or may demonstrate a restrictive pattern and may be of most value in monitoring the course of the disease in individual cases. Chest radiographs may help with staging the disease initially. The ESR may be elevated with sarcoidosis, but is a non- specific finding. Radionucleotide scanning is non-specific, although it can be used to locate the presence of pulmonary lesions.REF: Diagnostics Chapter 116: Cardiac Diagnostic Testing: Noninvasive Assessment of Coronary Artery Disease Test Bank Multiple Choice 1. An asymptomatic 63-year-old female has a low-density lipoprotein level of 135 mg/dL. Which test is beneficial to assess this patient’s coronary artery disease risk? a. Coronary artery calcium score b. C-reactive protein c. Exercise echocardiography d. Myocardial perfusion imaging The CRP is useful in asymptomatic women >60 years who have LDL <160 mg/dL to predict CAD risk. Although the CACS has shown some benefit in patients with moderate risk, the role for this diagnostic test is unclear. Exercise echocardiography and myocardial perfusion imaging are not performed initially.REF: Overview of Cardiac Diagnostic Testing 2. Which risk assessment for coronary artery disease is recommended for all female patients? a. Coronary artery calcium score b. Electrocardiogram c. Exercise stress test d. Framingham risk score The Framingham risk score is a quick method for identifying potential risk for CAD and can guide providers in choosing subsequent tests based on risk level. The ECG is performed on women with risk factors. The exercise stress test is useful in symptomatic women who have a normal ECG. The CACS may be used if moderate risk is present.REF: Diagnostic Testing for Cardiovascular Disease in Women Chapter 117: Abdominal Aortic Aneurysm Test Bank Multiple Choice 1. A patient reports abdominal and back pain with anorexia and nausea. During an exam, the provider notes a pulsatile abdominal mass. What is the initial action? a. Immediate referral to a thoracic surgeon b. Ordering computerized tomography angiography c. Scheduling an MRI to evaluate for aortic disease d. Ultrasound of the mass to determine size This patient has symptoms consistent with an aortic aneurysm. The initial step is to determine the size of the aneurysm; this can be done by US. Immediate referral is not necessary. MRI and CT diagnostic tests are ordered before surgery to evaluate the characteristics of the aneurysm.REF: Pathophysiology 2. A 70-year-old male patient has an aortic aneurysm measuring 5.0 cm. The patient has poorly- controlled hypertension, and decompensated heart failure. What is the recommendation for treatment for this patient? a. Endovascular stent grafting of the aneurysm b. Immediate open surgical repair of the aneurysm c. No intervention is necessary for this patient d. Serial ultrasonographic surveillance of the aneurysm This patient’s aneurysm is less than 5.5 cm and repair is not necessary at this time. Serial US surveillance is necessary to continue to evaluate size. Repair is risky in patients with hypertension and heart failure, so avoiding procedures if possible is recommended.REF: Management Chapter 118: Cardiac Arrhythmias Test Bank Multiple Choice 1. A patient reports sustained, irregular heart palpitations. What is the most likely cause of these symptoms? a. Anemia b. Atrial fibrillation c. Extrasystole d. Paroxysmal attacks Atrial fibrillation causes palpitations that are irregular and tend to be sustained. Anemia will cause rapid palpitations that are regular. Extrasystole causes palpitations or an awareness of isolated extra beats with a pause. Paroxysmal attacks start and terminate abruptly and are usually rapid and regular.REF: Tachyarrhythmias 2. An adult patient reports frequent episodes of syncope and lightheadedness. The provider notes a heart rate of 70 beats per minutes. What will the provider do next? a. Evaluate the patient’s orthostatic vital signs b. Monitor the patient’s heart rate while the patient is bearing down c. Order an electrocardiogram and exercise stress test d. Reassure the patient that the symptoms are non-cardiac in origin Orthostatic vital signs are helpful to exclude orthostatic hypotension as a cause of syncope and is easily performed in the clinic. Assessment for vagal bradycardia may be performed next. ECG and ETT are not recommended as an initial evaluation in a healthy patient, unless other causes are not determined. Without assessment of the cause of the syncope, cardiac causes cannot be excluded.REF: Physical Examination 3. A child with a history of asthma is brought to the clinic with a rapid heart rate. A cardiac monitor shows a heart rate of 225 beats per minute. The provider notifies transport to take the child to the emergency department. What initial intervention may be attempted in the clinic? a. Administration of intravenous adenosine b. Giving a beta blocker Test Bank 2 c. Providing a loading dose of digoxin d. Using a vagal maneuver or carotid massage This child has paroxysmal supraventricular tachycardia. Vagal maneuvers or carotid massage may be attempted to slow the ventricular rate. Adenosine is contraindicated in patients with asthma. Medications such as beta blockers and digoxin are not used in emergency treatment of PSVT.REF: Paroxysmal Supraventricular Tachycardia Chapter 119: Carotid Artery Disease Test Bank Multiple Choice 1. According to current research, which are associated with a decreased incidence of stroke? a. ≧7 servings of fruits and vegetables per day b. B-complex vitamin supplements c. Intensive insulin therapy in type 1 diabetes d. Low-sugar soda e. Mediterranean diet , C, E Individuals without hypertension in Sweden who consumed ≧7 servings of fruits and vegetables per day had a 19% lower risk of stroke than those consuming only one serving per day. Intensive insulin therapy in patients with type 1 diabetes was shown to lower the risk of stroke. Consuming a Mediterranean diet is associated with a reduced stroke risk. B-complex vitamins and low-sugar soda have not shown a decreased risk.REF: Definition and Epidemiology 2. During a routine health maintenance examination, the provider auscultates a cervical bruit. The patient denies syncope, weakness, or headache. What will the provider do, based on this finding? a. Order a carotid duplex ultrasound b. Order catheter-based angiography c. Refer the patient to a neurosurgeon d. Schedule a computed tomography angiography Carotid duplex ultrasound is the primary diagnostic tool for carotid stenosis. A cervical bruit in an asymptomatic patient is an indication for this test. Catheter-based angiography is the criterion- based standard, but has inherent costs and risks. A neurosurgery referral is not indicated without further testing. CTA is used instead of duplex US if the test is not available, if US results are inconclusive, or further evaluation is needed based on US results.REF: Diagnostics Chapter 120: Chest Pain and Coronary Artery Disease Test Bank Multiple Choice 1. A patient reports recurrent chest pain that occurs regardless of activity and is not relieved by rest. The provider administers a nitroglycerin tablet which does not relieve the discomfort. What is the next action? a. Administer a second nitroglycerin tablet b. Give the patient a beta blocker medication c. Prescribe a calcium channel blocker mediation d. Start aspirin therapy and refer the patient to a cardiologist Patient with these symptoms who do not respond to nitroglycerin is likely to have microvascular angina. Treatment is effective with beta blockers. These symptoms are not characteristic of acute MI, so aspirin is not given. A second nitroglycerin tablet is used for classic angina. Calcium channel blockers are not indicated.REF: Microvascular Angina 2. A patient is brought to an emergency department with symptoms of acute ST-segment elevation MI (STEMI). The nearest hospital that can perform percutaneous coronary intervention (PCI) is 3 hours away. What is the initial treatment for this patient? a. Administer heparin b. Give the patient an oral beta blocker c. Initiate fibrinolytic treatment d. Transfer to the PCI-capable institution Fibrinolytic therapy should be administered to any patient with evolving STEMI within 30 minutes of the time of first medical contact. Patients more than 120 minutes away from a PCI- capable hospital should be given fibrinolytic therapy since PCI should be performed within 90 minutes if possible. Giving heparin or beta blockers is not helpful.REF: Acute St-Segment Elevation Myocardial Infarction 3. Patients who meet the criteria for statin therapy to help prevent atherosclerotic cardiovascular disease are those with a history of a. a 10 year risk score of 5% and an LDL of 165 mg/dL. b. a 10 year risk score of 8% with an LDL of 80 mg/dL. c. a low-density lipoprotein (LDL) level >190 mg/dL. d. diabetes and an LDL between 40 and 70 mg/dL. e. previous myocardial infarction. , C, E Patients with previous MI, those with risk scores >8% and an LDL >70 mg/dL, and those with LDL levels >190 mg/dL are candidates for statin therapy. Patients with a risk score <7.5% with LDL levels between 75 and 190 mg/dL are not candidates and patients who have diabetes with LDL levels <75 mg/dL are not candidates.REF: Lipid Guidelines Chapter 121: Heart Failure Test Bank Multiple Choice 1. A patient who has heart failure with reduced ejection fraction will have which symptoms? a. Dyspnea and fatigue without volume overload b. Impairment of ventricular filling and relaxation c. Mild, exertionally related dyspnea d. Pump failure from left ventricular systolic dysfunction Heart failure with reduced ejection fraction results in pump failure from ventricular systolic dysfunction. Heart failure with preserved ejection fraction may have milder symptoms and is associated with impairment of ventricular filling and relaxation.REF: Definition and Epidemiology 2. A patient who has been diagnosed with heart failure for over a year reports being comfortable while at rest and experiences palpitations and dyspnea when walking to the bathroom. Which classification of heart failure is appropriate based on these symptoms? a. Class I b. Class II c. Class III d. Class IV Patients with Class II heart failure (HF) will have slight limitation of activity and will be comfortable at rest with symptoms occurring with ordinary physical activity. Patients with Class I HF do not have limitations and ordinary physical activity does not produce symptoms. With Class III HF, less than usual activity will produce symptoms. With Class IV HF, symptoms are present even at rest and all physical activity worsens symptoms.REF: Table 121-7: Classification of Heart Failure 3. A patient who has Class II heart failure is taking an ACE inhibitor and reports a recurrent cough that does not interfere with sleep or activity. What will the provider do initially to manage this patient? a. Assess serum potassium and sodium immediately b. Discontinue the ACE inhibitor and prescribe an ARB c. Provide reassurance that this is a benign side effect d. Withhold the drug and evaluate renal and pulmonary function Cough occurs in about 20% of patients who take ACE inhibitors and is not dangerous. The patient should be reassured that this is the case. If the cough is annoying, alternate therapy with an ARB may be considered. It is not necessary to evaluate electrolytes, renal function, or pulmonary function.REF: Pharmacologic Therapy Overview/ACE Inhibitors Chapter 122: Hypertension Test Bank Multiple Choice 1. Which are causes of secondary hypertension? a. Increased salt intake b. Isometric exercises c. Nonsteroidal anti-inflammatory drugs d. Oral contraceptives e. Sleep apnea , D, E NSAIDs and OCPs can both increase the risk of hypertension. Sleep apnea causes secondary hypertension. Increased salt intake does not cause HTN, but those with HTN are more sensitive to sale. Regular isometric exercise can decrease blood pressure. REF: Primary Hypertension/Secondary Hypertension 2. A 55-year-old patient has a blood pressure of 138/85 on three occasions. The patient denies headaches, palpitations, snoring, muscle weakness, and nocturia and does not take any medications. What will the provider do next to evaluate this patient? a. Assess serum cortisol levels b. Continue to monitor blood pressure at each health maintenance visit c. Order urinalysis, CBC, BUN, and creatinine d. Refer to a specialist for a sleep study This patient has pre-hypertension levels and should be evaluated. UA, CBC, BUN, and creatinine help to evaluate renal function and are in the initial workup. Serum cortisol levels are performed if pheochromocytoma is suspected, which would cause headache. The patient does not have snoring, so a sleep study is not indicated at this time. It is not correct to continue to monitor without assessing possible causes of early hypertension. REF: Differential Diagnosis/Diagnostics 3. An African-American patient who is being treated with a thiazide diuretic for chronic hypertension reports blurred vision and shortness of breath. The provider notes a blood pressure of 185/115. What is the recommended action for this patient? a. Add a beta blocker to the patient’s regimen b. Admit to the hospital for evaluation and treatment c. Increase the dose of the thiazide medication d. Prescribe a calcium channel blocker Patients with a blood pressure >180/120 or those with signs of target organ symptoms should be admitted to inpatient treatment with specialist consultation. Changing the medications may be done with consultation, but a hospitalization and stabilization must be done initially. REF: Management Chapter 123: Infective Endocarditis Test Bank Multiple Choice 1. A patient has infective endocarditis and is being treated with empiric antibiotics after blood cultures are inconclusive. The patient develops a severe headache along with transient neurologic changes. What is the likely cause of these symptoms? a. Extra-cardiac abscess formation b. Haemophilus infection c. Mycotic aneurysm d. Rheumatic heart fever Patients with mycotic aneurysms will present with symptoms of severe unrelenting headache, neurological changes, and signs of cranial nerve involvement. Extracardiac abscess formation depends on the organ involved. Haemophilus infections cause larger vegetations in the heart. Rheumatic heart fever has a classic group of symptoms involving the skin. REF: Clinical Presentation and Physical Examination/Neuro logic Findings 2. A patient has native valve endocarditis. While blood cultures are pending, which antibiotics will be ordered as empiric treatment? a. A beta-lactamase resistant penicillin and an antifungal drug b. Imipenem-cilastin and ampicillin c. Penicillin and an aminoglycoside antibiotic d. Vancomycin and quinupristin-dalfopristin The most common organism in NVE is S. aureus; until resistance is known, treatment with penicillin and an aminoglycoside is needed, although most strains causing NVE are not penicillin-resistant. Antifungal infections are rare and antifungal medications are not part of empiric therapy. Imipenem-cilcastin plus ampicillin is given for identified Enterococcus faecalis infection. Vancomycin and quinupristin-dalfopristin is used, with limited evidence for benefit, for Enterococcus faecium infection. REF: Management/Table 123-1: Some Suggested Antibiotic Regimens 3. A patient who is on renal dialysis is diagnosed with infective endocarditis. What causative organisms are more likely in this patient? a. Enterococcal organisms b. Neisseria gonorrhea c. Pseudomonas aeruginosa d. Staphylococcus aureus This patient is more likely to have a health care associated endocarditis; most of these are caused by S. aureus. Enterococcal organisms are the second highest cause in this population. REF: Health Care-Associated Endocarditis Chapter 124: Myocarditis Test Bank Multiple Choice 1. A patient who is a runner is diagnosed with viral myocarditis and asks when he may begin exercising again. What will the provider tell this patient? a. Exercise is contraindicated for life b. Exercise may resume when symptoms subside c. He may resume exercise in 6 months d. He must be symptom-free for 1 year Patients with myocarditis should not exercise for 6 months after the onset of symptoms. REF: Management 2. Which test is diagnostic for diagnosing myocarditis? a. Echocardiogram b. Electrocardiogram c. Endomyocardial biopsy d. Magnetic resonance imaging Endomyocardial biopsy is the only definitive test to diagnose myocarditis. Other tests are useful in determining symptoms, but are not specific to this diagnosis. REF: Diagnostics 3. A previously healthy patient develops myocarditis and presents with sudden onset of dyspnea, fatigue, and orthopnea. A family history is negative. The provider suspects myocarditis. What is the most likely etiology for this patient? a. Autoimmune disorder b. Bacterial infection c. Protozoal infection d. Viral infection Viral infection is the most common cause of myocarditis. Other infections are less likely. Although this patient may have an autoimmune disorder, the absence of family history makes this somewhat less likely. REF: Pathophysiology Chapter 125: Peripheral Arterial and Venous Insufficiency Test Bank Multiple Choice 1. An elderly female without prior history of cardiovascular disease reports lower leg soreness and fatigue when shopping or walking in the neighborhood. The primary care provider notes decreased pedal pulses bilaterally. Which test will the provider order initially to evaluate for peripheral arterial disease based on these symptoms? a. Digital subtraction angiography b. Doppler ankle, arm index c. Magnetic resonance angiography d. Segmental limb pressure measurement The Doppler study may be performed easily to indicate the likelihood of PAD. Other tests are performed only if indicated. REF: Diagnostics 2. A 75-year-old patient reports pain and a feeling of tiredness in both legs that only relieves after sitting for 30 minutes or more. What the does provider suspect as the cause for these symptoms? a. Buerger’s disease b. Cauda equina syndrome c. Diabetic neuropathy d. Peripheral arterial disease Patients with cauda equina syndrome, which causes spinal stenosis, will often not get relief until they sit down for a period of time. Buerger’s disease involves both the upper and lower extremities. Diabetic neuropathy may mask pain. PAD involves these symptoms that stop with rest. REF: Differential Diagnosis 3. A patient is diagnosed with PAD and elects not to have angioplasty after an angiogram reveals partial obstruction in lower extremity arteries. What will the provider recommend to help with relief of symptoms in this patient? a. Daily aspirin therapy to prevent clotting b. Statin therapy with clopidogrel c. Walking slowly for 15 to 20 minutes twice daily d. Walking to the point of pain each day Studies have demonstrated that an exercise program involving walking to the point of pain is as effective as angioplasty. Medications are useful to prevent progression of plaque formation and to prevent MI. REF: Management Chapter 126: Valvular Heart Disease and Cardiac Murmurs Test Bank Multiple Choice 1. Which are factors can cause a heart murmur? a. Backward flow through a septal defect b. Backward flow into a normal vessel c. Forward flow into a dilated vessel d. High rates of flow through a normal valve e. Low rates of flow into a cardiac chamber , C, D High rates of flow into either normal or abnormal vessels can cause murmurs. Backward flow into septal defects, regurgitant valves, or PDAs can cause murmurs. Forward flow into constricted or irregular valves or into a dilated vessel can cause murmur. Backward flow into a normal vessel or low flow rates are not responsible for murmurs. REF: Definition 2. A young female patient has known mitral valve prolapse. During a routine health maintenance exam, the provider notes an apical systolic murmur and a midsystolic click on auscultation. The patient denies chest pain, syncope, or palpitations. What will the provider do? a. Admit the patient to the hospital for evaluation and treatment b. Consult with the cardiologist to determine appropriate diagnostic tests c. Continue to monitor the patient every 3 years d. Reassure the patient that these findings are expected Most patients with mitral valve prolapse are monitored every 3 years unless they have a systolic murmur. The provider should consult with the cardiologist. Hospital admission is not necessary since the patient is asymptomatic. REF: Mitral Valve Prolapse 3. A patient has a cardiac murmur that peaks in midsystole and is best heard along the left sternal border. The provider determines that the murmur decreases in intensity when the patient changes from standing to squatting and increases in intensity with the Valsalva maneuver. Which cause will the provider suspect for this murmur? a. Aortic stenosis b. Hypertrophic cardiomyopathy c. Mitral valve prolapse d. Tricuspid regurgitation These findings occur with hypertrophic cardiomyopathy. With aortic stenosis, the murmur is a harsh crescendo-decrescendo heard best at the right sternal border that decreases in intensity with the Valsalva maneuver. With mitral valve prolapse, the murmur is heard in mid- to late systole, is heard best at the left lower sternal border, and may have a click that moves to later systole or disappear with the Valsalva maneuver. With tricuspid regurgitation, the murmur may occur at early, mid, or late systole, is heard at the left lower sternal border, and decreases with the Valsalva maneuver. REF: Table 126-1: Murmurs Chapter 127: Abdominal Pain and Infections Test Bank Multiple Choice 1. A patient is in clinic for evaluation of sudden onset of abdominal pain. The provider palpates a pulsatile, painful mass between the xiphoid process and the umbilicus. What is the initial action? a. Order a CBC, type and crossmatch, electrolytes, and renal function tests b. Perform an ultrasound examination to evaluate the cause c. Schedule the patient for an aortic angiogram d. Transfer the patient to the emergency department for a surgical consult This patient has symptoms and physical findings consistent with a ruptured aortic aneurysm and should have an immediate surgical consult. Ordering other tests is not necessary by the primary provider. REF: Ruptured Aortic Aneurysm 2. Which symptoms in a patient with abdominal pain are suggestive of appendicitis? a. Abdominal rigidity along with pain b. Pain accompanied by low-grade fever c. Pain occurring prior to nausea and vomiting d. Pain that begins in the left lower quadrant e. Prolonged duration of right lower quadrant pain , B, C Patients with appendicitis typically have pain that begins in the epigastric or periumbilical area and migrates to the left lower quadrant. Abdominal rigidity is common, as is low-grade fever. Pain precedes other symptoms and when the symptoms occur in any other order, the diagnosis of appendicitis should be questioned. Pain is usually of short duration. REF: Appendicitis/Clinical Presentation 3. An adult patient has intermittent, crampy abdominal pain with vomiting. The provider notes marked abdominal distention and hyperactive bowel sounds. What will the provider do initially? a. Admit the patient to the hospital for consultation with a surgeon b. Obtain upright and supine radiologic views of the abdomen c. Prescribe an antiemetic and recommend a clear liquid diet for 24 hours d. Schedule the patient for a barium swallow and enema If available, the primary care provider can order radiographic studies of the abdomen and chest. Once small bowel obstruction is confirmed or suspected, immediate hospitalization with surgeon referral is necessary. Because small bowel obstruction can have potentially serious or life- threatening consequences, waiting 24 hours is not recommended. REF: Small Bowel Obstruction/Clinical Presentation/Diagnostics Chapter 128: Anorectal Complaints Test Bank Multiple Choice 1. What are recommendations for patients with chronic pruritis ani? a. Application of a topical antihistamine b. Applying a of 1% hydrocortisone cream for several months c. Avoid tight-fitting or non-breathable clothing d. Avoiding perfumed soaps and toilet papers e. Using a hair dryer on the cool setting to control itching , D, E Measures to control itching include avoiding tight-fitting clothing as well as perfumed products and keeping the area clean and dry and using a cool hair dryer to dry the skin. Topical antihistamines are not used. Using a topical steroid longer than 2 weeks causes thinning of the skin. REF: Pruritis Ani/Management 2. A patient reports anal pruritis and occasional bleeding with defecation. An examination of the perianal area reveals external hemorrhoids around the anal orifice as the patient is bearing down. The provider orders a colonoscopy to further evaluate this patient. What is the treatment for this patient’s symptoms? a. A high-fiber diet and increased fluid intake b. Daily laxatives to prevent straining with stools c. Infiltration of a local anesthetic into the hemorrhoid d. Referral for possible surgical intervention Most hemorrhoids, unless incarcerated or painful, are treated conservatively. A high-fiber diet and increased fluid intake are recommended first. Daily laxatives are not recommended because the variation in stool consistency makes hemorrhoid management more difficult. Infiltration of a local anesthetic is performed for thrombosed external hemorrhoid prior to removing the clot. Hemorrhoidectomy is performed for severe or very painful hemorrhoids. REF: Management Chapter 129: Cholelithiasis and Cholecystitis Test Bank Multiple Choice 1. A patient has sudden onset of right upper quadrant and epigastric abdominal pain with fever, nausea, and vomiting. The emergency department provider notes yellowing of the sclerae. What is the probable cause of these findings? a. Acute acalculous cholecystitis b. Chronic cholelithiasis c. Common bile duct obstruction d. Infectious cholecystitis This patient has symptoms of cholecystitis with bile duct obstruction, which causes jaundice. The common triad of RUQ pain, fever, and jaundice occurs when a stone in lodged in the common bile duct. Acute acalculous cholecystitis is inflammation without stones. Chronic cholelithiasis doesn’t cause acute symptoms; jaundice occurs with obstruction. Infectious cholecystitis may occur without obstruction. REF: Clinical Presentation 2. A patient with a previous history of liver disease has bile duct obstruction. Which procedure will be used for this patient? a. Chemical dissolution of the gallstone b. Lithotripsy c. Open cholecystectomy d. Laparoscopic cholecystectomy Patients with possible liver disease should have open cholecystectomy. The other procedures are contraindicated. Chemical dissolution is not reliable and may take some time. REF: Management 3. A 30-year-old woman has right upper quadrant abdominal pain, nausea, and vomiting. Which diagnostic test will the provider order? a. Abdominal CT with contrast b. Abdominal ultrasound c. MRI of the abdomen d. Plain abdominal radiographs Women of childbearing age may safely have ultrasound. Until pregnancy is ruled out, the other studies may be harmful to a developing fetus and should be avoided. REF: Diagnostics 4. A patient has fever, nausea, vomiting, anorexia, and right upper quadrant abdominal pain. An ultrasound is negative for gallstones. Which action is necessary to treat this patient’s symptoms? a. Empiric treatment with antibiotics b. Hospitalization for emergent treatment c. Prescribing ursodeoxycholic acid d. Supportive care with close follow-up This patient has symptoms of acute acalculous cholecystitis, and is critically ill. Hospitalization is required. Empiric treatment with antibiotics and supportive care with follow-up do not address critical care needs. Ursodeoxycholic acid is a medication that helps with gallstone dissolution; this patient does not have gallstones. REF: Clinical Presentation/Physical Examination Chapter 130: Cirrhosis Test Bank Multiple Choice 1. A patient who is a chronic alcoholic reports weight loss, pruritis, and fatigue and the provider suspects cirrhosis of the liver. The patient’s urine and stools appear normal. What do these findings indicate? a. Early liver cirrhosis b. Late liver cirrhosis c. Liver failure and ascites d. Probably viral hepatitis Early symptoms of cirrhosis are characterized by this patient’s symptoms. As the condition worsens, stools and urine change color and the patient develops anorexia, nausea, and vomiting. Liver failure and ascites are late and will include abdominal pain. Viral hepatitis is a less likely diagnosis in the patient with a history of alcoholism. REF: Clinical Presentation 2. A patient with cirrhosis develops ascites. Which medication will be ordered initially to improve symptoms? a. Cephalosporin b. Furosemide c. Lactulose d. Spironolactone Spironolactone is the initial diuretic used to improve fluid diuresis in patients with ascites. Furosemide may be used as adjunctive therapy. Cephalosporin is used when infections occurs. Lactulose is used to increase stools and reduce encephalopathy. REF: Management 3. A patient has fibrotic liver disease and a liver biopsy shows micronodular cirrhosis. What is the most common cause of this form of cirrhosis? a. Alcoholism b. Hepatitis C c. Hepatocellular carcinoma d. Right-sided heart failure Micronodular cirrhosis is often associated with alcoholic liver disease. Viral causes and carcinoma usually cause macronodular cirrhosis. Right-sided heart failure occurs with many other causes as part of the disease development. REF: Definition and Epidemiology Chapter 131: Constipation Test Bank Multiple Choice 1. A patient is diagnosed with chronic constipation who uses polyethylene glycol, reports increased abdominal discomfort with nausea and vomiting. What is the initial action by the provider? a. Increase the dose of polyethylene glycol b. Obtain radiographic abdominal studies c. Perform a stool culture and occult blood d. Refer to a specialist for colonoscopy Patients with abdominal pain, nausea, and vomiting should have radiologic studies to exclude obstruction, ileus, megacolon, or volvulus. If those are ruled out, increasing the laxative may be warranted. Stool culture is indicated if the parasite ascariasis is suspected. Referral for colonoscopy is needed if alarm symptoms for neoplasm are present. REF: Diagnostics 2. A patient reports a decrease in the frequency of stools and asks about treatment for constipation. Which findings are part of the Rome III criteria for diagnosing constipation? a. Feeling of incomplete evacuation b. Fewer than 5 stools per week c. Lumpy stools d. Presence of irritable bowel syndrome e. Symptoms present for 3 months , C, E According to the Rome III criteria, symptoms must have begun 6 months prior and persisted for at least 3 months and include a feeling of incomplete evacuation, lumpy or hard stools, fewer than 3 stools per week, and not meeting criteria for irritable bowel syndrome. REF: Definition and Epidemiology 3. A patient has recurrent constipation which improves with laxative use but returns when laxatives are discontinued. Which pharmacologic treatment will the provider recommend for long-term management? a. Bisacodyl b. Docusate sodium c. Methylcellulose d. Mineral oil Methylcellulose is a bulk-forming product and is used initially. The other medications are used for more severe constipation and not recommended for long-term use. REF: Management Chapter 132: Diarrhea, Noninfectious Test Bank Multiple Choice 1. Which types of chronic noninfectious diarrhea will cause fatty stools? a. Celiac disease b. Cystic fibrosis c. Diabetes mellitus d. Lactose intolerance e. Pancreatic insufficiency , B, E Celiac disease, cystic fibrosis, and pancreatic insufficiency all produce malabsorption of fats and will result in fatty stools. Diabetes results in glucose malabsorption, while lactose intolerance causes lactose malabsorption. REF: Differential Diagnosis/Chronic Noninfectious Diarrhea 2. A patient develops acute diarrhea and then comes to clinic two weeks later reporting profuse watery, bloody diarrheal stools 6 to 8 times daily. The provider notes a toxic appearance with moderate dehydration. Which test is indicated to diagnose this cause? a. Qualitative and quantitative fecal fat b. Stool collection for 24-hour stool pH c. Stool sample for C. difficile toxin d. Wright stain of stool for white blood cells Patients with acute onset diarrhea lasting more than 2 weeks with profuse, watery, bloody stools of more than 6 times in a 24-hour period warrants testing for C. difficile toxin. Qualitative and quantitative fecal fat, 24-hour pH studies, and Wright stain for WBCs are performed when chronic diarrhea are present. REF: Diagnostics/Acute Diarrhea/Chronic Diarrhea 3. A patient who developed chronic diarrhea after gastric surgery asks what can be done to mitigate symptoms. What will the provider recommend initially? a. A diet high in carbohydrates b. Avoiding liquids with meals c. Empiric antibiotic therapy d. Probiotic supplements Initial suggestions for treating postoperative diarrhea will include avoiding fluids during meals and lying down after meals. Concentrated carbohydrates may trigger symptoms. Empiric antibiotic therapy is indicated for small intestinal bacterial overgrowth syndrome with specific symptoms and an association with an elevated folate level. Probiotic supplements may be used as adjunctive therapy. REF: Management Chapter 133: Diverticular Disease Test Bank Multiple Choice 1. A patient has intermittent left-sided lower abdominal pain and fever associated with bloating and constipation alternating with diarrhea. The provider suspects acute diverticulitis. Which tests will the provider order? a. Barium enema examination b. CT scan of abdomen and pelvis c. Plain abdominal radiographs d. Rigid sigmoidoscopy e. Stool for occult blood , E A CT scan of the abdomen and pelvis is the preferred imaging study if acute diverticulitis is suspected with diverticular abscess. Occult blood tests are necessary because uncomplicated diverticulosis is not known to cause occult rectal bleeding. Barium enema should be avoided in acute diverticulitis because of the risk of extravasation of barium into the peritoneal cavity, causing chemical peritonitis. Plain radiographs are not useful because they will appear normal. Rigid sigmoidoscopy usually cannot be performed beyond the recto-sigmoid junction, so is not useful. REF: Diagnostics 2. A patient has a history of diverticular disease and asks what can be done to minimize acute symptoms. What will the practitioner recommend to this patient? a. Avoiding saturated fats and red meat b. Consuming a diet high in fiber c. Taking an anticholinergic medication d. Using bran to replace high-fiber foods Increasing dietary fiber reduces constipation and reduces the incidence of acute symptoms. Avoiding saturated fats and red meats does not reduce the risk of diverticulitis, but does decrease the risk of colon cancer. Anticholinergics and antispasmodics do not prevent attacks, but may help with symptoms. Bran may be used as an adjunct to high-fiber foods, but should not replace other high-fiber sources. REF: Management 3. A patient who has a history of diverticular disease has left-sided pain and reports seeing blood in the stool. What is an important intervention for these symptoms? a. Ordering a CBC and stool for occult blood b. Prescribing an antispasmodic medication c. Referring the patient for a lower endoscopy d. Reminding the patient to eat a high- fiber diet Patients with suspected diverticular abscess of rectal bleeding need further evaluation and a referral for lower endoscopy is warranted. Hemorrhage is more common from the right colon. The other actions do not have priority over the need to evaluate the cause of the bleeding. REF: Complications/Indications for Referral or Hospitalization Chapter 134: Dysphagia Test Bank Multiple Choice 1. Which diagnostic study is best to evaluate a swallowing disorder? a. CT of the head and neck b. Electroglottography c. Electromyoscopy d. Videofluoroscopy Videofluoroscopy is the most appropriate because it visualizes the actual swallow. Electroglottography and electromyoscopy may be appropriate, but are more limited. CT evaluation may aid in diagnosis, but does not describe the actual swallow mechanism. REF: Diagnostics 2. A patient has a feeding disorder after a stroke that causes disordered tongue function and impaired laryngeal closure. What intervention will be helpful to reduce complications in this patient? a. Surface electrical stimulation b. Teaching head rotation c. Thickened liquids d. Thinning liquids Thickening liquids is helpful for patients with disordered tongue function and impaired laryngeal closure, because there is a reduced tendency for liquids to spill over the tongue base and cause aspiration. Surface electrical stimulation helps improve strength of muscles, but does not address the problem of aspiration. Teaching head rotation is used for patients with unilateral laryngeal dysfunction. Thinning liquids is used for patients with weak pharyngeal contraction. REF: Table 134-1: Swallowing Therapy Techniques, Rationales, and Indications 3. An elderly patient has recent weight loss and the patient’s spouse reports noticing coughing and choking when eating. What is the likely cause of this presentation? a. Esophageal dysphagia b. Oral stage dysphagia c. Pharyngeal dysphagia d. Xerostomia causing dysphagia Pharyngeal dysphagia often results from weakness or poor coordination of the pharyngeal muscles which can cause delayed swallow and failure of airway protection, leading to coughing and choking. Esophageal dysphagia is associated with pain after swallowing. Oral stage disorders are related to poor bolus control and result in drooling or spilling. Xerostomia is when oral mucous membranes are dry. REF: Clinical Presentation Chapter 135: Gastroesophageal Reflux Disease Test Bank Multiple Choice 1. Which medications may increase the prevalence of GERD? a. Aspirin b. Benzodiazepines c. Calcium antagonists d. Hormone replacements e. Oral contraceptives , B, C Aspirin, benzodiazepines, and calcium antagonists all increase the likelihood of GERD, while hormone replacement therapy and OCPs are associated with a lower incidence. REF: Clinical Presentation 2. A patient has been taking a proton pump inhibitor (PPI) for several months to treat GERD with rebound symptoms when discontinuing the medication. To minimize long-term side effects of the PPI, what regimen may be ordered? a. Alternate-day dosing of the PPI b. Switching to a histamine-2 receptor antagonist (H2RA) c. Taking a PPI and H2RA at different times a day d. Twice daily dosing of the PPI Taking a PPI and an H2RA at different times a day is an alternate to high-dose PPI therapy. Alternate-day dosing of PPIs is not an effective long-term regimen. PPIs are superior to H2RAs. Twice daily dosing of the PPI will not minimize side effects. REF: Management 3. A patient experiences a sharp pain with swallowing just under the sternum. This is more commonly associated with which condition? a. Hiatal hernia b. Infectious esophagitis c. Peptic stricture d. Schatzki ring A sharp, substernal pain with swallowing is most commonly associated with infectious esophagitis. Esophageal strictures are highly correlated with hiatal hernia and patients with stricture will report a feeling of food becoming stuck. A Schatzki ring and peptic stricture are types of strictures. REF: Clinical Presentation Chapter 136: Gastrointestinal Hemorrhage Test Bank Multiple Choice 1. A patient has both occasional “coffee ground” emesis and melena stools. What is the most probably source of bleeding in this patient? a. Hepatic b. Lower GI c. Rectal d. Upper GI Coffee ground emesis is usually old blood from an upper GI source and melena is black, shiny, foul-smelling as a result of blood degradation and is usually upper GI in origin. Lower GI and rectal bleeding will cause bright red blood in stools. Hepatic bleeding usually does not affect the GI tract. REF: Clinical Presentation 2. What is an initial action when admitting a patient to the hospital who has a GI bleed, hypotension, and a hematocrit decrease of 6% from baseline? a. Administer packed red blood cells b. Place a Foley catheter to monitor output c. Place two large-bore intravenous lines d. Prepare for surgical repair of the bleed The first interventions should involve restoring circulatory status to normal in patients with hypotension and low hematocrit. Placement of two large-bore intravenous lines or a central line is essential to allow transfusions of PRCs and fluids. The other interventions will be carried out, but are not the initial action. REF: Management 3. A 50-year-old, previously healthy patient has developed chronic gastritis. What is the most likely cause of this condition? a. H. pylori infection b. NSAID use c. Parasite infestation d. Viral gastroenteritis H. pylori accounts for approximately 100% of chronic superficial gastritis, 90% to 95% of duodenal ulcers, and 89% of gastric ulcers. NSAID use is an important cause, but not likely in a previously healthy individual. Parasites are the leading cause worldwide, but not in the U. S. Viral gastroenteritis usually does not cause chronic gastritis and usually has lower GI symptoms. REF: Pathophysiology Chapter 137: Hepatitis Test Bank Multiple Choice 1. A patient who is asymptomatic tests positive for the hepatitis C virus. What will the provider tell the patient about managing this illness? a. A rapidly fulminant disease ending with cirrhosis is likely b. Administering immunoglobulins helps shorten the course c. Pegylated interferon is given for 6 to 12 months d. Treatment is supportive since the infection is self-limiting Pegylated interferon is used for HCV to reduce the viral load of this chronic disease. HCV rarely has a rapidly fulminant course, although cirrhosis is likely after years of infection. Immunoglobulin therapy is given for HBV. The disease is not self-limiting.REF: Management 2. Which form of hepatitis virus is rapidly spread via the fecal-oral route? a. Hepatitis A b. Hepatitis B c. Hepatitis C d. Hepatitis D HAV is rapidly spread, usually through contaminated food, through the fecal-oral route. The other types have a parenteral transmission via blood and other body fluids.REF: Pathophysiology 3. A recovering chronic alcoholic reports nausea, vomiting, diarrhea, and abdominal discomfort. A physical examination is negative for jaundice or ascites. What will the provider do initially? a. Obtain a bilirubin level and prothrombin time b. Order a complete blood count and liver function tests c. Reassure the patient that this is likely a viral gastroenteritis d. Refer the patient to a specialist for evaluation and treatment Patients with alcoholic hepatitis may present initially with signs of gastroenteritis. Based on the history, even without jaundice and ascites, the provider should order a CBC and LFTs. Bilirubin and PT levels are performed when a diagnosis is made to determine prognosis and course of the disease. Reassuring the patient without confirmation of disease is not recommended. Referral is made if hepatitis is diagnosed.REF: Clinical Presentation/Diagnostics Chapter 138: Inflammatory Bowel Disease Test Bank Multiple Choice 1. A patient is diagnosed with ulcerative colitis. Which medication will be prescribed initially to establish remission? a. Azathioprine b. Budesonide c. Infliximab d. Sulfasalazine Sulfasalazine is a 5-aminosalicyclic acid used to induce remission in UC and is a first-line medication. Budesonide is a synthetic corticosteroid used for moderate to severe disease, but not as a first-line agent. Azathioprine is an immunomodulator used to minimize the need for corticosteroids. Infliximab is a biologic medication and is more useful for treating Crohn’s disease.REF: Management/Pharmacotherapy 2. A patient reports lower abdominal cramping and occasional blood in stools. The provider suspects inflammatory bowel disease. Which test will the provider order to determine whether the patient has ulcerative colitis or Crohn’s disease? a. Barium enema b. Colonoscopy c. Genetic testing d. Small bowel series Colonoscopy is useful in differentiating UC from CD. Barium enema has limited use in diagnosis, but is used to detect distension, strictures, tumors, fistulas, or obstructions. Genetic testing may be helpful in the future with further advances. Small bowel series are used infrequently to determine small bowel involvement.REF: Diagnostics 3. Which are characteristic of Crohn’s disease? Select all that apply. a. Fistulous tracts may occur as disease complications. b. Half of patients will not have significant remission of symptoms. c. Inflammation affects all layers of the intestinal tract wall. d. The disease may be limited to the small intestine. e. The inflammation is diffuse and continuous. , C, D CD may be complicated by fistulous tracts. Inflammation affects all layers of the intestinal wall tract. The disease may be limited to the small intestine. UC causes inflammation that is diffuse and continuous and about 50% of patients with UC may never have significant remission of symptoms.REF: Definition and Epidemiology Chapter 139: Irritable Bowel Syndrome Test Bank Multiple Choice 1. A patient has irritable bowel syndrome with alternating diarrhea and constipation and asks the provider about dietary changes that may help with symptoms. What will the provider recommend? a. Avoiding all beverages containing caffeine b. Consuming a high fiber diet c. Eliminating all foods containing dairy products d. Keeping a food and symptom diary Because all patients with IBS are different and there are no specific foods that cause symptoms, each patient should keep a diary to determine which foods may trigger symptoms before adding or eliminating foods.REF: Dietary Modification 2. Which symptom must be present for a diagnosis of irritable bowel syndrome? a. Abdominal pain b. Bloating c. Constipation d. Diarrhea Abdominal pain must be present to diagnose IBS. The other symptoms may or may not occur.REF: Clinical Presentation 3. What is the probable underlying pathology of irritable bowel syndrome, according to research over the last decade? a. Alteration in processing of sensory information b. Changes in intestinal secretory mucosa c. Intestinal tissue disease d. Malabsorption of specific nutrients Recent research has yielded information about alterations in sensory processing that are different in persons with IBS. Changes in intestinal mucosa, intestinal tissue disease, and malabsorption syndromes are structural disorders and this is a functional disease.REF: Pathophysio logy Chapter 140: Jaundice Test Bank Multiple Choice 1. A patient has an elevated indirect bilirubin. Which condition may be causing this symptom? a. Alcoholic cirrhosis b. Cholelithiasis c. Hemolytic anemia d. Viral hepatitis Indirect, or unconjugated bilirubin is often associated with an increase in the destruction of RBCs, as with hemolytic anemia. Direct, or conjugated bilirubin, is elevated when there is liver dysfunction or obstruction.REF: Pathophysiology 2. A patient who has jaundice has bright orange urine. What is a likely cause of this jaundice? a. Bile duct obstruction b. Blood transfusion reaction c. Defective erythropoiesis d. Sickle cell anemia Conjugated bilirubin, which is in excess with liver disease, is excreted in the urine, causing a characteristic orange color. Unconjugated bilirubin is elevated with increased destruction of RBCs, which occurs with transfusion reactions, defective erythropoiesis, and sickle cell anemia.REF: Pathophysiology 3. A patient has jaundice and bilirubin testing reveals elevated direct bilirubin. Which subsequent testing may help determine the cause of these findings? Select all that apply. a. Complete blood count b. Liver function tests c. Renal function tests d. Serologic viral tests e. Serum iron and ferritin , D, E Since the direct bilirubin is elevated, hepatic causes should be evaluated. These tests will include liver function tests, viral tests for hepatitis, and serum iron and ferritin. CBC and renal function tests evaluate the presence of hemolytic disease.REF: Diagnostics Chapter 141: Nausea and Vomiting Test Bank Multiple Choice 1. A patient has a recent episode of vomiting and describes the vomitus as containing mostly gastric juice. What does this symptom suggest? a. Bile duct obstruction b. Gastritis c. Peptic ulcer d. Small bowel obstruction The vomitus with peptic ulcer disease contains mostly gastric juice. Bile duct obstruction will result in bilious vomitus. Gastritis vomitus contains blood and will have a coffee-ground appearance. Small bowel obstruction produces vomitus that is feculent.REF: History 2. A patient has nausea associated with chemotherapy. Which agent will be prescribed? a. Diphenhydramine b. Meclizine c. Ondansetron d. Scopolamine Ondansetron is used to treat chemotherapy-induced nausea and vomiting. The other medications are used for nausea associated with motion sickness, migraines, and vertigo.REF: Management Chapter 142: Pancreatitis Test Bank Multiple Choice 1. Which is the most common cause of pancreatitis in the United States? a. Ethyl alcohol b. Gallstones c. Hyperlipidemia d. Trauma Gallstones are the most common cause of pancreatitis in the US.REF: Definition and Epidemiology 2. A patient reports a sudden onset of constant, sharp abdominal pain radiating to the back. The examiner notes both direct and rebound tenderness with palpation of the abdomen. What is the significance of this finding? a. Compression of the common bile duct b. Presence of a pancreatic pseudocyst c. Retroperitoneal hemorrhage d. Severe acute pancreatitis with peritonitis Direct and rebound tenderness is an ominous sign suggesting severe peritonitis. Jaundice is present with compression of the common bile duct. Palpation of a mass suggests the presence of a pancreatic pseudocyst. Bruising of the periumbilicus or flank suggests retroperitoneal hemorrhage.REF: Acute Pancreatitis/Physical Examination 3. The provider suspects that a patient has chronic pancreatitis. Which diagnostic tests will be most helpful to confirm this diagnosis? a. Blood glucose and fecal fat b. Complete blood count c. Liver function tests d. Serum amylase and lipase levels Patients with pancreatic insufficiency will have elevated blood glucose levels and steatorrhea. The CBC, LFTs, and serum amylase and lipase are typically normal with chronic pancreatitis.REF: Chronic Pancreatitis/Diagnostics Chapter 143: Tumors of the Gastrointestinal Tract Test Bank Multiple Choice 1. A patient with a history of esophageal reflux reports difficulty swallowing. The provider notes fixed cervical and axillary lymphadenopathy on exam. What is the significance of these findings if esophageal carcinoma is suspected? a. A tumor is likely confined to the upper esophagus. b. Lymphadenopathy indicates advanced disease. c. The prognosis for cure is poor. d. This type of cancer responds well to radiation. Supraclavicular, cervical, and axillary lymphadenopathy are signs of advanced disease. Hepatomegaly and superior vena cava syndrome indicate a poor prognosis. Esophageal cancer usually has a high mortality rate.REF: Esophageal Cancer/Physical Examination 2. A patient is diagnosed with cancer of the colon and is scheduled for surgical resection. A carcinoembryonic antigen (CEA) test prior to surgery is not elevated. What is the significance of this finding? a. A negative CEA indicates a reduced need for surgery. b. The CEA should be repeated every 3 months. c. The test is not informative and will not be repeated. d. This result indicates a better prognosis for cure. A negative CEA indicates that this test is not informative and will not be useful postoperatively. A positive CEA indicates the usefulness of this test and the measurement should be repeated every 3 months after surgery to detect tumor recurrence. It does not indicate whether surgery should be performed and does not predict cure rates.REF: Tumors of the Colon/Management 3. A patient is diagnosed with gastric cancer after presenting with cachexia, small bowel obstruction, hepatomegaly, and ascites. What will the provider tell this patient about treatment and possible cure? a. A complete resection will be curative. b. Chemotherapy is the only option. c. Palliative resection may be performed. d. Radiation therapy is preferred for metastasis. This patient presented with signs of advanced disease, which has a poor prognosis. Palliative resection may be performed. Curative treatment involves surgery, chemotherapy, and radiation. Chemotherapy is not the only option and is usually combined with other therapies. Chemotherapy is preferred for metastatic disease.REF: Tumors of the Stomach/Management Chapter 144: Peptic Ulcer Disease Test Bank Multiple Choice 1. A patient has persistent epigastric pain occurring 2 to 3 hours after a meal. Which test is definitive for diagnosis peptic ulcer in this patient? a. Barium swallow with radiography b. Breath test or stool antigen testing for H. pylori c. Endoscopy with biopsy of gastric mucosa d. Physical exam with percussion of the upper abdomen Endoscopy provides the most accurate diagnosis of PUD and allows biopsy of multiple areas to exclude malignancy. Barium swallow may still be performed in patients unwilling to undergo endoscopy. Breath tests and stool antigen testing for H. pylori can confirm a bacterial cause. Physical exam generally yields negative findings.REF: Physical Examination/Diagnostics 2. What is the best treatment for H. pylori-related peptic ulcer disease? a. H2RA and clarithromycin for 14 days b. H2RA, bismuth, metronidazole, and tetracycline for 10 to 14 days c. PPI and clarithromycin for 14 days d. PPI, amoxicillin, and clarithromycin for 10 days A PPI and clarithromycin for 14 days has documented improved effectiveness over other regimens. Use of an H2RA is cheaper.REF: Management/Table 144-1: Treatment of H. pylori infection 3. A patient who has been taking an NSAID for osteoarthritis pain has peptic ulcer disease. What is the initial step in treating this patient? a. Discontinue the NSAID b. Order prostaglandin therapy c. Prescribe a proton pump inhibitor d. Recommend an H2 receptor antagonist The first step in treating medication-induced peptic ulcer is to discontinue the medication. H2 receptor antagonists are the first anti-secretory medications prescribed. Proton pump inhibitors are more expensive and are used as second-line treatment. Prostaglandin therapy helps protect the gastric and duodenal mucosa and is used if NSAIDS cannot be discontinued.REF: Management Chapter 145: Incontinence Test Bank Multiple Choice 1. The provider is evaluating a patient for potential causes of urinary incontinence and performs a postvoid residual (PVR) test which yields 30 mL of urine. What is the interpretation of this result? a. The patient may have overflow incontinence. b. The patient probably has a UTI. c. This is a normal result. d. This represents incomplete emptying. A PVR less than 50 mL is considered normal and this result does not indicate any abnormality.REF: Diagnostics 2. The provider is counseling a patient who has stress incontinence about ways to minimize accidents. What will the provider suggest initially? a. Increasing fluid intake to dilute the urine b. Referral to a physical therapist c. Taking pseudoephedrine daily d. Voiding every 2 hours during the day Timed voiding is useful to help minimize stress incontinence and is used initially. Increasing fluid intake will increase symptoms. PT referral may be done if other measures fail to help with exercises to strengthen the pelvic floor muscles. Pseudoephedrine is useful, but not an initial therapy.REF: Stress Incontinence/Behavioral Therapies 3. The daughter of an elderly, confused female patient reports that her mother is having urinary incontinence several times each day. What will the provider do initially? a. Obtain a urine sample for urinalysis and possible culture b. Order serum creatinine and blood urea nitrogen tests c. Perform a bladder scan to determine distention and retention d. Tell the daughter that this is expected given her mother’s age and confusion When incontinence occurs, UA is performed initially to exclude hematuria, pyuria, glucosuria, or proteinuria and possible infection. Serum creatinine and BUN may be performed if renal disease is suspected. Bladder scans may be performed if the UA is normal to evaluate physiologic causes. It is not correct to offer reassurance without ruling out other causes.REF: Diagnostics Chapter 146: Prostate Cancer Test Bank Multiple Choice 1. An older male patient reports urinary frequency, back pain, and nocturia. A dipstick urinalysis reveals hematuria. What will the provider do next to evaluate this condition? a. Order a PSA and perform a digital rectal exam b. Refer for a biopsy c. Refer the patient to a urologist d. Schedule a transurethral ultrasound Patients with symptoms of potential prostate cancer should be screened with PSA and DRE. Referral to a urologist is the next step even with normal findings, since PSA is occasionally normal. The urologist may order TRUS or biopsy.REF: Clinical Presentation/Diagnostics 2. An older male patient has a screening PSA which is 12 ng/mL. What does this value indicate? a. A normal result b. Benign prostatic hypertrophy c. Early prostate cancer d. Prostate cancer A PSA greater than 10 ng/mL suggests prostate cancer. A level between 4 and 10 ng/mL may be early prostate cancer or a benign condition. A level less than 4 ng/mL is normal.REF: Diagnostics 3. A patient is diagnosed with prostate cancer and diagnostic testing reveals disease that has gone past the prostatic capsule without evidence of metastasis. The patient does not wish to undergo treatment. What will the provider tell this patient? a. Chemotherapy is indicated to provide cure for this cancer. b. Monitoring PSA with regular DSE is an acceptable option. c. Palliative radiation therapy is necessary to improve quality of life. d. This level of disease requires intervention with hormonal therapy. This patient has stage T2 prostate cancer which may be managed with watchful waiting which includes PSA and DRE evaluation. Chemotherapy, palliative radiation therapy, and hormonal therapy are not required.REF: Management Chapter 147: Prostatic Hyperplasia (Benign) Test Bank Multiple Choice 1. A male patient reports nocturia and daytime urinary frequency and urgency without changes in the force of the urine stream. What is the likely cause of this? a. Bladder outlet obstruction b. Lower urinary tract symptoms c. Prostate cancer d. Urinary tract infection Lower urinary tract symptoms (LUTS) result from irritative changes in the lower tract. Bladder outlet obstruction causes hesitancy, decreased caliber and force of the urine stream, and post- void dribbling. Diagnosis of prostate cancer and UTI require further testing and are less likely causes.REF: Clinical Presentation 2. A 70-year-old male reports urinary hesitancy, post-void dribbling, and a diminished urine stream. A digital rectal exam reveals an enlarged prostate gland that feels rubbery and smooth. Which tests will the primary care provider order based on these findings? a. Bladder scan for post-void residual b. PSA and bladder imaging c. Urinalysis and serum creatinine d. Urine culture and CBC with differential The DRE reveals a prostate gland consistent with BPH. The primary provider should order a urinalysis and creatinine to evaluate possible infection and renal function. A bladder scan is ordered at the discretion of the urologist. The prostate exam isn’t consistent with prostate cancer, so PSA and bladder imaging are not necessary. Symptoms of prostatitis would indicate a need for evaluation of possible infection.REF: Diagnostics/Box 147-1: Diagnostics 3. A patient has been taking terazosin daily at bedtime to treat BPH and reports persistent daytime dizziness. What will the provider do? a. Prescribe finasteride instead of terazosin b. Recommend taking the medication in the morning c. Suggest using herbal preparations d. Switch the prescription to doxazosin Patients who cannot tolerate the side effect of alpha-adrenergic antagonists, the provider may initiate therapy with a 5a-reductase inhibitor such as finasteride. Terazosin should be given at bedtime to minimize these adverse effects. Herbal preparations have not been proven to be safe or effective. Doxazosin is in the same drug class as terazosin.REF: Management Chapter 148: Proteinura and Hematuria Test Bank Multiple Choice 1. An older male patient reports gross hematuria but denies flank pain and fever. What will the provider do to manage this patient? a. Monitor blood pressure closely b. Obtain a urine culture c. Perform a 24-hour urine collection d. Refer for cystoscopy and imaging Gross hematuria in older men denotes a significant risk of malignant disease, so cystoscopy and imaging are indicated. Proteinuria is concerning for hypertension. The patient does not have flank pain or fever, so the likelihood of infection is lower. A 24-hour urine collection is not indicated.REF: Hematuria/Clinical Presentation/Diagnostics and Differential Diagnosis a. A pregnant woman at 30 weeks gestation has proteinuria. What will the provider do next? b. Evaluate her blood pressure c. Monitor serum glucose for gestational diabetes d. Perform a 24-hour urine collection Reassure her that this normal at this stage of pregnancy Proteinuria after 24 weeks gestation is usually a sign of preeclampsia, so her blood pressure should be evaluated. Serum glucose evaluation for gestational diabetes is performed as part of routine screening, but is not related to the finding of proteinuria. A 24-hour urine collection is not indicated.REF: Proteinuria/Clinical Presentation 2. A female patient reports hematuria and a urine dipstick and culture indicate a urinary tract infection. After treatment for the UTI, what testing is indicated for this patient? a. 24-hour urine collection to evaluate for glomerulonephritis b. Bladder scan c. No testing if hematuria is resolved d. Voiding cystourethrogram If hematuria resolves after treatment for UTI, no further testing is indicated, especially in women who are at increased risk for UTI.REF: Hematuria/ Diagnostics and Differential Diagnosis Chapter 149: Renal Failure Test Bank Multiple Choice 1. A primary care provider sees a new patient who reports having a diagnosis of chronic kidney disease for several years. The patient is taking one medication for hypertension which has been prescribed since the diagnosis was made. The provider orders laboratory tests to evaluate the status of this patient. Which laboratory finding indicates a need to refer the patient to a nephrologist? a. ACR of 325 mg/g b. Blood pressure of 145/85 mm Hg c. GFR of 35 d. Urine RBC of 15/hpf An albumin/creatinine ratio greater than 300 mg/g warrants referral. A specialist is necessary for persistent hypertension refractory to treatment with four or more agents, a GFR of less than 30, and urine RBC greater than 20/hpf.REF: Specialist Referral 2. Which tests should be monitored regularly in order to monitor for complications of chronic renal disease? Select all that apply. a. Liver enzymes b. Parathyroid hormone levels c. Serum glucose d. Serum lipids e. Vitamin D levels , D, E CKD can cause hyperparathyroidism, hyperlipidemia, and alterations in vitamin D, calcium, and phosphorus metabolism, so these should be monitored. Liver function and serum glucose are not affected by CKD.REF: Box 149-1: Major Complications of Stage 4-5 CKD 3. Which is a pre-renal cause of acute kidney injury? a. Anaphylactic shock b. Hydronephrosis c. Hypertension d. Renal calculi Anaphylactic shock interferes with perfusion of the kidney, which is a pre-renal cause of AKI. Hydronephrosis and renal calculi are post-renal causes leading to obstruction to renal pelvis, ureters, bladder, or urethra. Hypertension is an intrinsic cause.REF: Pathophysiology Chapter 150: Sexual Dysfunction (Male) Test Bank Multiple Choice 1. The provider orders the oral phosphodiesterase type 5 inhibitor sildenafil to treat erectile dysfunction in a 65-year-old male patient. What will be included when teaching this patient about taking this medication? Select all that apply. a. The medication is best taken on an empty stomach. b. The medication should be taken with a fatty food or meal. c. The medication’s effects may last for 24 to 36 hours. d. This medication has a rapid onset and short duration of action. e. This medication may be taken once daily. , D Sildenafil has a rapid onset and short duration of action and should be taken on an empty stomach. Fatty foods may delay or interfere with absorption. This medication is given when sexual activity is desired and not once daily.REF: Management 2. A 50-year-old man reports having erectile dysfunction. What is an important response by the provider when developing a plan of care for this patient? a. Considering testosterone hormone replacement therapy b. Evaluating the patient for cardiovascular disease c. Prescribing an oral phosphodiesterase type 5 inhibitor d. Referring the patient for psychotherapy and counseling Men under age 60 years with ED are at higher risk for cardiovascular disease, so this patient should be evaluated for this condition. Until the underlying cause is found, prescribing medications or hormones is not indicated. Psychotherapy and counseling are used when psychogenic ED is present.REF: Management 3. Which is true about hypoactive sexual desire in older men? a. Hypoactive sexual desire in older men is related to sexual aversion. b. Hypoactive sexual desire is a conscious choice to avoid sexual relations. c. Men with hypoactive sexual desire may have normal excitement and orgasm. d. The most common type of sexual dysfunction is hypoactive sexual desire. Men with hypoactive sexual desire have diminished response in the desire phase of the sexual response cycle but may still experience normal excitement and orgasm. Sexual aversion and hypoactive desire are not related. Many people with normal sexual desires choose not to have sexual relations; hypoactive desire is a physiological condition. Only 16% of men have hypoactive desire.REF: Introduction Chapter 151: Testicular Disorders Test Bank Multiple Choice 1. A young adult male reports a dull pain in the right scrotum and the provider notes a bluish color showing through the skin on the affected side. Palpation reveals a bag of worms on the proximal spermatic cord. What is an important next step in managing this patient? a. Anti-infective therapy with ceftriaxone or doxycycline b. Consideration of underlying causes of this finding c. Reassurance that this is benign and may resolve spontaneously d. Referral to an emergency department for surgical consultation This patient has symptoms of varicocele. Because varicocele is rare on the right side, the provider should look for underlying causes of these findings. Anti-infective therapy is indicated for epididymitis. Varicocele requires surgical intervention or ablation to resolve. Testicular torsion is an emergency. 2. An adolescent male reports severe pain in one testicle. The examiner notes edema and erythema of the scrotum on that side with a swollen, tender spermatic cord and absence of the cremasteric reflex. What is the most important intervention? a. Doppler ultrasound to assess testicular blood flow b. Immediate referral to the emergency department c. Prescribing anti-infective agents to treat the infection d. Transillumination to assess for a “blue dot” sign This patient has symptoms of testicular torsion, which is a surgical emergency. An immediate referral is warranted. Doppler US and transillumination are useful in establishing a diagnosis, but the referral is the most important. Anti-infective agents are used if epididymitis is suspected. 3. A 3-month-old male infant has edema and painless swelling of the scrotum. On physical examination, the provider is able to transilluminate the scrotum. What will the provider recommend? a. A Doppler ultrasound to evaluate the scrotal structures b. A short course of empiric antibiotic therapy c. Immediate referral to a genitourinary surgeon for repair d. Observation and reassurance that spontaneous resolution may occur This infant has symptoms of hydrocele; these disorders often resolve spontaneously during infancy and do not require treatment unless symptoms, such as pain, occur. It is not necessary to perform other studies or refer to a surgeon. Antibiotics are not indicated, since this is not infectious. Chapter 152: Urinary Calculi Test Bank Multiple Choice 1. A patient who has diabetes has symptoms consistent with renal stones. Which type of stone is most likely in this patient? a. Citrate b. Cysteine c. Oxalate d. Uric acid Uric acid stones are more prevalent in diabetics. Citrate, cysteine, and oxalate are less common in all patients.REF: Pathophysiology 2. Which factors increase the risk of renal stones? Select all that apply. a. Excess antacid use b. Snow skiing c. Strenuous exercise d. Surgical menopause e. Vitamin D excess , C, D Excess antacids, strenuous exercise, and surgical menopause are all linked to renal stone risk. Tropical vacations are also linked to renal stone development. Vitamin D excess is not a risk factor.REF: Definition and Epidemiology 3. A patient has acute renal colic, nausea, and vomiting and a urinalysis reveals hematuria, but is otherwise normal. A radiographic exam shows several radiopaque stones in the ureter which are less than 1 mm in diameter. What will the primary provider do initially to manage this patient? a. Obtain a consultation with a urology specialist b. Order a narcotic pain medication and increased oral fluids c. Prescribe desmopressin and a corticosteroid medication d. Prescribe nifedipine and hospitalize for intravenous antibiotics Stones that are less than 1 mm in diameter will usually pass spontaneously. The provider should counsel the patient to increase fluid intake and should prescribe adequate pain medication. A consultation is not necessary unless initial measures fail. Desmopressin and corticosteroids have not been shown to be effective. Nifedipine and IV fluids may be used as a secondary option.REF: Management Chapter 153: Urinary Tract Infections and Sexually Transmitted Infections Test Bank Multiple Choice 1. A 30-year-old male patient has a positive leukocyte esterase and nitrites on a random urine dipstick during a well patient exam. What type of urinary tract infection does this represent? a. Complicated b. Isolation c. Uncomplicated d. Unresolved All UTIs in males are considered complicated, because the infection source is not secondary to ascending infection.REF: Definition and Epidemiology 2. An asymptomatic pregnant woman has a positive leukocyte esterase and positive nitrites on a urine dipstick screening. What will the provider do next? a. Admit to the hospital b. Obtain a urine culture c. Order a renal ultrasound d. Prescribe trimethoprim-sulfamethoxazole Urine culture is the definitive test and should be obtained in all pregnant women. Admission to the hospital is usually not necessary. Renal ultrasound is used to identify abnormalities or obstructions that may be causing recurrent symptoms. TMP-SMZ is contraindicated in pregnant women.REF: Diagnostics/Management 3. An asymptomatic female learns that her boyfriend has gonorrhea and asks about antibiotics. What will the provider recommend? a. Amoxicillin-clavulanate for 10 days b. Cultures and treatment if symptoms appear c. Empiric ceftriaxone and azithromycin d. Trimethoprim-sulfamethoxazole Patients with gonorrhea usually have chlamydia as well, so treatment with both ceftriaxone and azithromycin are given. Amoxicillin-clavulanate and TMP-SMZ are used for UTIs. The patient should be treated empirically. Females are often asymptomatic.REF: Gonorrhea/Management Chapter 154: Uropathies (Obstructive) and Tumors of the Genitourinary Tract (Kidneys, Ureters, and Bladder) Test Bank Multiple Choice 1. A patient has a partial urinary tract obstruction caused by benign prostatic hypertrophy. The patient reports increasing difficulty initiating a urine stream and occasional incontinence, but has not experienced a urinary tract infection. Which initial treatment will be ordered? a. A 5a-reductase inhibitor b. Surgical intervention c. Urinary catheterization d. Urinary diversion procedure Patients with BPH may not require treatment unless there is retention, recurrent infection, or unacceptable symptoms. This patient has symptoms, but no retention or infection. The obstruction is not always progressive, so surgery may be delayed until more severe symptoms occur. 5a-Reductase inhibitors help reduce the prostate size and may be used initially to see if there is symptomatic relief. Urinary catheterization is used for an acute obstruction. Urinary diversion is used when bladder cancer is present.REF: Management 2. A patient reports right sided flank pain and hematuria and the provider palpates a renal mass on the affected side. What is the probable treatment for this patient’s condition? a. Biologic response modifiers, including interleukin b. Ileal conduit urinary diversion surgery c. Nephron-sparing nephrectomy and chemotherapy d. Radiotherapy for palliation of metastatic lesions This patient has the classic triad of symptoms for renal cell carcinoma, which usually do not present until metastasis has occurred, with poor prognosis for survival. Palliative radiotherapy is often used to treat metastatic lesions. RCC does not respond well to biologic response modifiers. Ileal conduit diversion is used for bladder carcinoma. Nephron-sparing nephrectomy may be used if there is a better chance of survival.REF: Clinical Presentation/Renal Cell Carcinoma/Management Chapter 155: Amenorrhea Test Bank Multiple Choice 1. A 16-year-old female has primary amenorrhea. A pregnancy test is negative. Further testing reveals a normal TSH and an elevated prolactin level. Which test will the provider order next? a. Clomiphene challenge test b. Magnetic resonance imaging c. Progesterone challenge test d. Serum dehydroepiandrosterone In patients with primary amenorrhea who have a negative pregnancy test, normal TSH, and elevated prolactin, the provider may order MRI or CT of the sella turcica to identify microadenomas and macroadenomas. If that is normal, a progesterone challenge test will be ordered to evaluate estrogen status. Clomiphene challenge is ordered to evaluate hypergonadotropic amenorrhea. Serum DHEA, if increased, indicates an adrenal origin for androgen in women with hirsutism.REF: Diagnostics 2. An adolescent female has amenorrhea. The provider notes short stature, neck webbing, and a pigeon chest deformity. Based on these symptoms, what is the underlying disorder causing this patient’s amenorrhea? a. Androgen insensitivity b. Hypothyroidism c. Polycystic ovarian disease d. Turner’s syndrome Turner’s syndrome is characterized by congenital short stature, neck webbing, and a pigeon chest. Androgen insensitivity is characterized by a complete absence of axillary and pubic hair. Hypothyroidism will cause changes in vital signs, weight gain, and fatigue. Polycystic ovarian disease causes metabolic syndrome.REF: Clinical Presentation 3. A 15-year-old female who participates in high school track and gymnastics is experiencing amenorrhea after having eight normal periods. A pregnancy test is negative. What may be included in management of this patient’s amenorrhea to restore normal periods? Test Bank 2 Select all that apply. a. Calcium and vitamin D supplementation b. Clomiphene administration c. Combination oral contraceptives d. Dietician consultation e. Estriol therapy , D, E To help maintain bone density, vitamin D and calcium should be given to any women who have amenorrhea. A dietician should be consulted to assist with healthy weight gain. Estriol, a weak estrogen, is used to help restore normal endocrine function.REF: Management Chapter 156: Bartholin's Gland Cysts and Abscesses Test Bank Multiple Choice 1. An adolescent female reports a mass on her genitalia which is becoming increasingly painful. On exam, the provider notes an erythematous, edematous, tender mass lateral to the vestibule without discharge. What will the provider do initially? a. Obtain a consultation for biopsy of the lesion b. Perform a speculum examination of the vagina c. Prescribe empiric metronidazole twice daily d. Refer the patient for an incision and drainage and culture Empiric administration of antibiotics, if done early, can be helpful. Metronidazole is a first-line antibiotic. Biopsy is performed if the mass is suspected as being cancerous. Speculum examination is deferred until pain is relieved. I&D has risks and often results in recurrence.REF: Management 2. A patient has undergone surgical incision and drainage of a Bartholin’s cyst with insertion of a drain. What is an important aspect of care for this patient? a. Administration of antibiotics b. Education about long-term dyspareunia c. Teaching about reproductive sequelae d. Weekly follow-up monitoring Patients with surgical I&D who have a drain should be monitored weekly. If adequately treated, long-term function should be normal.REF: Incision and Drainage/Life Span Considerations Chapter 157: Breast Disorders Test Bank Multiple Choice 1. A woman who has just weaned her infant from breastfeeding develops signs of mastitis and is treated with antibiotics. At a follow up visit, the provider notes marked breast edema and erythema of the affected breast. What will the provider do next? a. Consult with a surgeon for I&D of the breast b. Counsel the patient to apply warm compresses c. Prescribe antibiotics to treat MRSA infection d. Refer the patient for an immediate biopsy Patients treated for mastitis who do not respond to antibiotics and who have persistent erythema and edema are likely to have inflammatory breast carcinoma and should be referred for a biopsy immediately. MRSA infection is possible, but these symptoms are severe and the patient needs immediate evaluation. Warm compresses and surgical K&D are not indicated.REF: Mastitis/Clinical Presentation 2. A postmenopausal woman reports unilateral breast pain that she describes as sharp and burning and localized to one area. A breast examination reveals no dimpling, discharge, or masses. Which diagnostic test will the provider order? a. Bilateral mammography b. Focused ultrasound c. Hormone levels d. Needle biopsy Bilateral mammography is usually performed in postmenopausal women with noncyclic breast pain, although the likelihood of abnormal findings is low. Focused ultrasound may be performed in addition to mammography if indicated. Hormone levels are generally normal. Needle biopsy is performed if a suspicious mass is identified.REF: Breast Pain/Clinical Presentation/Diagnostics 3. A female patient is identified as having the BRCA mutation and she asks which intervention will reduce her risk of breast cancer the most? What will the provider tell her? a. Breast magnetic resonance imaging Test Bank 2 b. Clinical breast examination every 6 months c. Early childbearing and breastfeeding d. Prophylactic mastectomy and oophorectomy Although all of the options help to reduce breast cancer risk, patients with BRCA mutation are at extremely high risk and will benefit most from prophylactic mastectomy and oophorectomy. MRI can help detect invasive cancers earlier.REF: Risk Reduction Chapter 158: Chronic Pelvic Pain Test Bank Multiple Choice 1. A woman with chronic pelvic pain most likely has a gynecological cause for her symptoms. Which treatment will the provider recommend initially? a. Counseling and support b. Hysterectomy c. Neurostimulation d. Oral contraceptives Oral contraceptives may be helpful and are a good initial choice. Counseling and support are necessary throughout management, but do not help with symptom relief. Hysterectomy may be indicated if there are more severe structural problems, but does not always alleviate symptoms. Neurostimulation is used when neuropathic pain is present.REF: Management 2. Which underlying causes are related to chronic pelvic pain in women? Select all that apply. a. Faulty posture b. Hepatitis c. Interstitial cystitis d. Physical abuse e. Recurrent pneumonia , C, D Problems with posture can cause inflammation in the lower spinal column, leading to chronic pelvic pain. Interstitial cystitis and physical or sexual abuse are related to CPP. Hepatitis and recurrent pneumonia are not linked to CPP.REF: Definition and Epidemiology Chapter 159: Dysmenorrhea Test Bank Multiple Choice 1. A patient with primary dysmenorrhea has taken NSAIDs and COX-2 inhibitors without getting relief from symptoms. What will the provider suggest? a. A combined oral contraceptive b. Complementary therapies c. Intrauterine device implantation d. Narcotic analgesics as needed OCPs have demonstrated some effectiveness and should be tried in this instance. IUDs are used in Europe, but have not been approved for this use in the US. Complementary therapies have not been sufficiently studied. Narcotic analgesics are not recommended for this level of pain.REF: Management 2. A 35-year-old woman without a previous history of dysmenorrhea reports lower pelvic pain and irregular bleeding between periods. What is the initial action in managing this patient? a. Obtaining a pelvic transvaginal ultrasound with saline infusion b. Ordering a CBC, erythrocyte sedimentation rate, and cultures c. Performing an abdominal, pelvic, and rectovaginal examination d. Prescribing a trial of nonsteroidal anti-inflammatory medications Symptoms that occur later in life are more likely to be secondary dysmenorrhea and must be investigated, beginning with a thorough abdominal, pelvic, and rectovaginal exam. Other tests may be performed if indicated by findings on the physical exam. NSAIDs are first-line therapy for primary dysmenorrhea.REF: Clinical Presentation/Diagnostics 3. An adolescent female reports crampy pelvic pain radiating to the back, sacrum, and inner thighs during the first 2 days of each menstrual period, associated with nausea and loose tools. She asks about what causes these symptoms. What will the provider tell her? a. Excess prostaglandins, vasopressin will cause these symptoms b. Mechanical cervical obstruction or severe uterine flexion are likely causes c. Nulliparity and her young age are correlated with these symptoms Test Bank 2 d. The most likely cause at her age is anovulatory menstrual cycles Chemical mediators, including prostaglandins, vasopressin, and other substances originating from phospholipids have been shown to produce the symptoms and associated symptoms of dysmenorrhea. Mechanical obstruction or severe cervical flexion have no substantial evidence to support their role in causing these symptoms. Nulliparity and age have not shown correlation with dysmenorrhea. Ovulation causes increased release of chemical mediators, so anovulatory cycles will result in fewer symptoms.REF: Pathophysio logy/Clinical Presentation Chapter 160: Dyspareunia Test Bank Multiple Choice 1. A previously healthy 22-year-old female reports pain in the rectovaginal area that occurs with sexual intercourse. What is the most likely cause of this patient’s discomfort? a. Atherosclerosis b. Endometriosis c. Inadequate lubrication d. Psychologic issues In the premenopausal woman, endometriosis is the most common cause of dyspareunia, especially when it involves the rectovaginal area. Atherosclerosis and inadequate lubrication may occur in older women. Psychological issues are less common.REF: Pathophysiology 2. A perimenopausal woman reports a recent onset of moderate to severe pain with sexual intercourse. Which treatment will the provider prescribe initially to treat this pain? a. Botulism injections b. Topical corticosteroids c. Topical estrogen d. Water-based lubrication If the problem is estrogen-insufficient dryness, which occurs during menopause, topical estrogen is effective for moderate to severe pain. Botulism injections are useful when spasms are the cause of pain. Topical corticosteroids are not indicated. Water-based lubrication may be effective for mild symptoms.REF: Management and Health Promotion Chapter 161: Ectopic Pregnancy Test Bank Multiple Choice 1. A female patient has lower abdominal pain, nausea, and vomiting and reports missing a period 3 weeks prior. The patient reports using an intrauterine device for contraception. A serum B-hCG is 1500 mIU/mL. What will the provider do, based on these findings? a. Perform a transvaginal ultrasound b. Recheck the B-hCG level in 4 to 6 weeks c. Refer for a diagnostic laparoscopy d. Tell the patient that a viable pregnancy is likely With elevations in serum B-hCG greater than 1000 mIU/mL, transvaginal US can usually detect both viable and non-viable ectopic pregnancies without subjecting women to the risks of an invasive procedure. A diagnostic laparoscopy is the definitive test for ectopic pregnancy and should be performed if the US is indeterminate. The level is already high enough that a fetus would be detectable on US, so rechecking this level is not indicated. Patients who use IUDs are at higher risk for ectopic pregnancy; telling this woman that a viable pregnancy is likely should not occur until diagnostic tests are performed.REF: Diagnostics 2. A patient is determined to have a non-ruptured ectopic pregnancy within 1 week of a missed period. Which treatment will the specialist order? a. Laparoscopy b. Leucovorin rescue c. Methotrexate d. Mifepristone In an early non-ruptured ectopic pregnancy, methotrexate is widely used. Leucovorin rescue and mifepristone are used as adjunctive medications with methotrexate. Laparoscopy is performed when a ruptured ectopic pregnancy is present.REF: Management 3. A patient has received methotrexate therapy for treatment of an ectopic pregnancy. What will the provider include when teaching this patient about this therapy? Select all that apply. a. Avoid sexual intercourse for 3 months b. Do not consume alcohol for at least 3 months c. Long-term effects include lower fertility d. Pregnancy should be avoided in the future e. Refrain from taking vitamins containing folic acid , B, E Patients who have been given methotrexate for an ectopic pregnancy should refrain from sexual intercourse and consumption of alcohol and vitamins containing folic acid for 3 months. Good subsequent fertility rates have been demonstrated, so women do not need to avoid pregnancy or expect poor pregnancy outcomes.REF: Patient and Family Education Chapter 162: Fertility Control Test Bank Multiple Choice 1. A female calls the provider to report having unprotected sexual intercourse approximately 4 days prior. Which regimen will the provider recommend? a. Plan-B One-Step twice daily for 5 days b. Plan-B One-Step daily for 5 days c. Ulipristal Acetate taken one time d. Ulipristal Acetate twice daily for 3 days Although the OTC product Plan B is effective, its efficacy drops significantly after 72 hours. The prescription product Ulipristal Acetate is prescribed as a single dose taken within 120 hours after intercourse, but studies have shown greater efficacy for this product than Plan-B from 72 to 120 hours after unprotected sexual intercourse.REF: Postcoital Contraception 2. A woman has a history of migraines with aura and request oral contraceptives to prevent pregnancy. Which type of contraceptive will the provider recommend? a. Combination oral contraceptive b. Contraceptive implant c. Progestin-only contraception d. Transdermal combination product Women with migraine with aura are at increased risk for stroke and should avoid estrogen- containing contraceptives. The progestin-only pill is recommended. The other products all contain estrogen. Altering the method of administration does not alter the estrogen dose.REF: Hormonal Contraception/Oral Contraceptives 3. A woman who is taking oral contraceptive pills (OCPs) to prevent pregnancy calls the provider to report forgetting to take the pills for 4 days. She has not had sexual intercourse during that time. What will the provider recommend? a. Resume the pills and use a backup method the remainder of the cycle b. Stop the OCP, use an alternative method, and resume OCPs at the next cycle c. Take 2 pills daily for 4 days and use an alternative method for 4 days d. Use a morning after pill today and resume the OCPs now When OCPs are missed longer than 2 days, women should use an alternative method of fertility control until the end of the cycle and resume taking the pills as prescribed. It is not recommended that the pills be stopped until a new cycle begins. When pills are missed for 2 or fewer days, women should take 2 pills daily and use a backup method until the end of the cycle. The morning after pill is used when pregnancy may have occurred.REF: Hormonal Contraception/Oral Contraceptives Chapter 163: Genital Tract Cancers Test Bank Multiple Choice 1. A woman asks about her risk of ovarian cancer. To best assess risk in this patient, what will the provider do first? a. Ask about parity and age of menarche b. Evaluate age of menopause c. Obtain a 3-generation family history d. Order testing for the BRCA gene The family history is the best predictor of ovarian cancer risk. The other factors contribute, but not as significantly as family history. If there is a strong family history, testing for the BRCA gene is indicated.REF: Ovarian Cancer/Pathophysiology 2. A postmenopausal woman who is overweight and who has hyperlipidemia and a history of infertility develops vaginal bleeding and reports a feeling of pelvic pressure. The provider suspects a genital tract cancer and refers the patient for diagnostic evaluation. What is the likely cause of this woman’s symptoms? a. Cervical cancer b. Endometrial cancer c. Ovarian cancer d. Vaginal cancer This woman has symptoms characteristic of type I endometrial cancer, including her health history, bleeding, and pelvic pressure. Cervical cancer, ovarian cancer, and vaginal cancer typically do not have symptoms.REF: Endometrial Cancer/Clinical Presentation 3. A woman who has had routine Pap tests all of her adult life has an abnormal Pap. What will the provider tell her about this result? a. Colposcopy with biopsy is necessary b. She may have vaginal cancer c. She most likely has early cervical cancer d. The result most likely indicates HPV infection The Pap test is a screen and should be followed by colposcopy with biopsy. Women who have had Pap tests routinely are less likely to have cervical cancer.REF: Cervical Cancer/Diagnostics Chapter 164: Infertility Test Bank Multiple Choice 1. A couple who has been trying to conceive for over 9 months asks the provider about artificial reproductive therapy. When discussing risks and benefits associated with these methods, what will the provider include? Select all that apply. a. Higher rates of pregnancy-induced hypertension b. Increased premature births c. Likelihood of increased infant birth weight d. More frequent multiple gestations e. Reduced risk of ovarian and breast cancers , B, D ART methods often produce multiple gestation births and increase the likelihood of premature births, along with higher rates of PIH. Infants born via ART methods more often have lower birth weights. There is an association between higher rates of ovarian cancer and use of ART.REF: Complications 2. A provider is caring for a couple who are trying to conceive. To most accurately evaluate ovulation and luteal surge in the woman, what test will the provider recommend or perform? a. Basal body temperature b. Maintaining a menstrual calendar c. Plasma midluteal progesterone concentration level d. Urinary luteal hormone home kit A home kit to assess urinary luteal hormone can identify the surge that precedes ovulation by 1 or 2 days; these kits, when done with an afternoon or evening urine sample, correlate well with peak serum LH. Basal body temperature is easy, convenient, and inexpensive methods to assess ovulatory function, but the resultant curves may be difficult to interpret. Menstrual calendars are less accurate. Plasma midluteal progesterone concentration levels are presumptive of ovulation but cannot assess the quality of the luteal phase.REF: Diagnostics Chapter 165: Menopause Test Bank Multiple Choice 1. A 45-year-old woman has gone 120 days without a menstrual period. A pregnancy test is negative. What will the provider do, based on this symptom? a. Evaluate for various causes of amenorrhea b. Reassure her that this can be normal c. Tell her she has developed early menopause d. Tell her that this is likely perimenopause Women who have prolonged episodes of amenorrhea, even with FSH levels in menopausal range, may resume normal menstruation. Other causes of amenorrhea should be evaluated.REF: Physiology 2. A woman who has stopped having menstrual periods has vasomotor symptoms, but does not want to use hormone replacement therapy. What measures will the provider recommend? Select all that apply. a. Avoiding caffeine b. Engaging in regular exercise c. Having a glass of wine each evening d. Keeping the house cool e. Trying herbal remedies , B, D Women with vasomotor symptoms should be counseled to avoid caffeine and alcohol, to engage in regular exercise, and to lower the thermostat. Consuming alcohol is not recommended to reduce symptoms. Herbal remedies are frequently used but have not been shown to be beneficial and many may be harmful.REF: Vasomotor Symptoms 3. Shortly after the onset of menopause, a woman begins to show signs of osteopenia. The provider orders oral Bazedoxifene combined with conjugated estrogen (BZA/CE). What will the provider tell her about the purpose of this treatment? a. It will improve calcium absorption. b. It will prevent further bone loss. c. It will reduce the incidence of fractures. d. It will reverse bone loss. HT therapy is given to reduce bone loss, reduce the incidence of osteoporotic fractures, and reduce height loss. It does not improve calcium absorption and will not prevent further bone loss or reverse bone loss.REF: Osteoporosis Chapter 166: Pap Test Abnormalities Test Bank Multiple Choice 1. What is the benefit of using a liquid-based medium when performing a Pap test? a. It allows HPV, gonorrhea, and chlamydia testing with the same specimen. b. It is a more accurate test than the slide method of Pap testing. c. It is not necessary to use endocervical cells to obtain results. d. It is predictive of the later development of cervical cancer. The liquid-based medium method allows testing of HPV, gonorrhea, and chlamydia using the same specimen. It is not necessarily more accurate. It requires use of endocervical cells. It does not predict the development of cancer.REF: Diagnostics: Cervical Cancer Screening 2. A young female has a Pap test which reveals atypical squamous cells of undetermined significance. What will the next step be in managing this patient? a. Colposcopy with biopsy b. Endometrial sampling c. Reflex HPV DNA test d. Repeat cytology in 12 months Young women with ASC-US may have repeat cytology testing in 12 months. Colposcopy with biopsy is performed if low-grade intraepithelial lesions or high-grade squamous intraepithelial lesions are present. Reflex HPV DNA testing is not indicated. Endometrial sampling is performed with low- or high-grade lesions who are older than 35 years.REF: Indications for Referral 3. What is true about HPV infection in women? a. A single, isolated HPV infection will lead to cervical cancer. b. HPV subtypes causing genital warts indicate the likelihood of cancer. c. Most HPV lesions will resolve spontaneously without causing cancer. d. Most women with HPV infection will develop cervical cancer. Most HPV infections resolve spontaneously, especially in younger women. It is the persistence of HPV infection and not a single infection that increases the risk. The subtypes causing genital warts are not implicated in the etiology of cervical cancer. Most women with HPV infection will not develop cancer.REF: Definition and Epidemiology Chapter 167: Pelvic Inflammatory Disease Test Bank Multiple Choice 1. Which are risk factors for pelvic inflammatory disease? Select all that apply. a. Age under 25 years b. Cigarette smoking c. Tubal sterilization d. Using barrier methods of contraception e. Vaginal douching , B, E Age under 25 years, cigarette smoking, and vaginal douching all increase the risk for PID. Tubal sterilization and barrier contraceptive methods decrease the risk.REF: Definition and Epidemiology 2. A sexually active female has symptoms of PID with fever. Cultures are pending. For outpatient treatment, what will the provider order? a. Ampicillin and doxycycline b. Cefotetan and doxycycline c. Clindamycin and gentamicin d. Rocephin, doxycycline, and metronidazole For outpatient management, Rocephin is given once IM and then doxycycline and metronidazole are given for 14 days.REF: Management 3. A female patient reports cramping, dysuria, low back pain, and nausea. A dipstick urinalysis is normal and a pregnancy test is negative. What will the provider do next? a. Obtain vaginal secretions for testing b. Refer for radiological studies c. Schedule for an endometrial biopsy d. Treat with empiric antibiotics The provider should continue to evaluate by getting specimens for testing to rule out active infection. Radiological studies and endometrial biopsy may be necessary if other tests are not conclusive. Empiric antibiotics should not be given until other causes are ruled out.REF: Management Chapter 168: Sexual Dysfunction (Female) Test Bank Multiple Choice 1. A female patient with vaginal atrophy is prescribed a local estrogen therapy product with conjugated equine estrogen cream. What will the provider recommend as adjunctive therapy for this patient? a. Adding progesterone to the regimen b. Pelvic floor physical therapy c. Treatment with a testosterone patch d. Trigger point injections Conjugated equine estrogen is absorbed systemically, so the patient will need progesterone to prevent unopposed estrogen stimulation of the endometrium. Pelvic floor PT and trigger point injections are used for dyspareunia. Testosterone patches are used for decreased arousal and desire.REF: Management 2. What is a possible cause of decreased arousal, libido, and orgasm in a postmenopausal woman? a. Diminished testosterone b. Endometriosis c. Low estrogen levels d. Uterine prolapse Diminished testosterone has been implicated in deceased arousal, libido, and orgasm in women. Endometriosis is a common cause of deep dyspareunia. Low estrogen causes vaginal dryness, coital pain, and decreased desire. Uterine prolapse causes deep dyspareunia.REF: Pathophysiology Chapter 169: Unplanned Pregnancy Test Bank Multiple Choice 1. In order to help prevent unplanned pregnancies, which group of providers may make the most impact by providing contraceptive counseling to women? a. Counselors in STI clinics b. Gynecologists c. Practitioners in walk-in clinics d. Primary care providers Women receive most of their preventive care from non-gynecologic providers, so PCPs have a unique opportunity to provide contraceptive counseling to women. Women seek care in STI clinics and gynecology clinics for specific reasons, often after contraceptive counseling is no longer preventive.REF: Definition and Epidemiology 2. An adolescent female calls a primary care clinic to report that she has missed two periods and is having morning nausea and vomiting. What will the provider suggest? a. Coming to the clinic for pregnancy testing b. Making an appointment with a gynecologist c. Purchasing a home pregnancy test kit d. Referral to a community health clinic Patients who feel especially vulnerable and are in denial about a pregnancy may not want to take a test at home, desiring immediate guidance when a result is discovered. Referring to another provider will only alienate this adolescent further.REF: Clinical Presentation 3. A provider sees a woman who has just learned she is pregnant with an unplanned pregnancy. What is an initial step in helping this woman make decisions about his pregnancy? a. Actively listen to the woman’s concerns and questions b. Ask the mother if the father of the baby will be involved c. Make a referral to an obstetrician for more informatio d. Offer information about both adoption and abortion The initial step is to actively listen to the woman to determine what her concerns and needs are. The provider should give unbiased information and answer any questions the woman has. Asking her about the father’s involvement puts an emphasis on other concerns. Referring her to an obstetrician conveys a desire to avoid helping her with her problems. Giving information that she has not asked for conveys a judgment about what she should do.REF: Management and Counseling Chapter 170: Vulvar and Vaginal Disorders Test Bank Multiple Choice 1. A female patient reports vulvar pruritus and dyspareunia. The provider notes white papules on the vulva with thinning of the epithelium. What condition does the provider suspect? a. Bartholin’s duct cyst b. Lichen sclerosis c. Sexually transmitted infection d. Vulvar psoriasis These symptoms are consistent with lichen sclerosis, with white papules and epithelial thinning being diagnostic. The other conditions may cause pruritus, but not the skin lesions.REF: Lichen Sclerosis 2. A sexually active young female reports vaginal discharge and moderate vulvovaginal irritation. The examination reveals a white, non-inflammatory discharge adhering to the vaginal walls, clue cells on microscopic examination and a positive KOH whiff test. What will the provider do next? a. Obtain cultures of the vaginal discharge b. Order a gynecologic referral for evaluation and treatment c. Prescribe metronidazole 500 mg for 7 days d. Screen the patient for gonorrhea and chlamydia Bacterial vaginosis may be treated empirically based on the symptoms this woman has and on the three criteria noted in clinic. Metronidazole is the first-line treatment. It is not necessary to obtain cultures or to refer to a specialist.REF: Bacterial Vaginosis/Clinical Presentation/Diagnostics/Management 3. A postmenopausal woman is diagnosed with lichen planus. After several weeks of treatment with a potent corticosteroid ointment, the woman reports improvement in itching, but states that she has extreme vaginal dryness. What will the provider recommend? a. Increasing the frequency of the corticosteroid application b. Taking diphenhydramine daily at bedtime c. Using a topical estrogen cream along with the steroid d. Using petrolatum ointment to minimize drying Patient with concomitant vulvovaginal atrophy related to menopause may need to use topical estrogen cream to treat those symptoms. After several weeks, the corticosteroid is tapered to a lower dose, not increased. Diphenhydramine is given for itching. Petrolatum ointment is useful for external skin as a barrier, but is not used internally.REF: Lichen Planus/Management Chapter 171: Ankle and Foot Pain Test Bank Multiple Choice 1. A patient has pain on the plantar aspect of the heel with weight bearing after rest. The pain is worsened with dorsiflexion of the foot. What is the initial treatment for this patient? a. A series of steroid injections b. Avoiding all high- impact activities c. Night splints d. Wearing flat shoes only This patient has signs of plantar fasciitis. The initial treatment includes avoiding all high-impact activities. A single steroid injection may be given with subsequent injections if no improvement. Night splints are part of second-tier treatment. Flat shoes should be avoided.REF: Plantar Fasciitis/Management 2. A patient injures an ankle while playing soccer and reports rolling the foot inward while falling with immediate pain and swelling of the lateral part of the joint. The patient is able to bear weight and denies hearing an audible sound at the time of injury. What does this history indicate? a. Likely ankle sprain with a possible fracture b. Mild ankle injury without fracture c. Mild soft tissue injury only d. Serious ankle injury with certain fracture Immediate swelling of the joint raises the index of suspicion for a fracture or a substantial amount of joint involvement. Without radiographs, none of these possibilities can be confirmed.REF: Clinical Presentation 3. A patient who is a distance runner reports pain in one heel that is worse in the morning and seems to improve with exercise. The provider notes localized swelling and a bony prominence at the heel. What is the initial treatment for this condition? a. Cessation of all sports activities and exercise b. Crutches and partial weight bearing c. Physical therapy for ultrasound therapy d. Referral to an orthopedist for MRI and evaluation This patient has symptoms consistent with Achilles tendonitis. Immediate cessation of sports and exercise is the first step in management. Crutches and partial weight bearing may be indicated if symptoms do not improve with rest and NSAIDs. Physical therapy is used as adjunctive therapy. Symptoms that do not improve require referral.REF: Achilles Tendonitis/Management Chapter 172: Bone Tumors Test Bank Multiple Choice 1. Which treatments may be used to manage bone pain in patients with bone tumors? Select all that apply. a. Bisphosphonates b. Exercise c. External beam radiation d. Massage e. Vertebralplasty , B, C, E Bisphosphonates can decrease pain by preventing growth and development of existing and new bone lesions. Exercise is useful to maintain function and reduce pain. External beam radiation is useful in the majority of patients. Vertebralplasty involves injecting bone cement to stabilize bone. Massage is not recommended.REF: Pain Management 2. A patient reports persistent lower back pain and constipation. A digital rectal examination reveals a mass at the sacrum. What will the primary care provider do to manage this patient? a. Order spinal radiographs in 3 months b. Perform an MRI of the sacrum c. Refer the patient to an oncologist d. Schedule the patient for a biopsy Patients with chordoma, which is a type of sarcoma with a predilection for the sacrum will have these symptoms and a palpable mass coming out of the sacrum. A referral to an oncologist is necessary. These tumors have a significant risk for malignancy, so waiting 3 months is not an option. The oncologist will order a CT and body scan and possibly biopsy or surgery.REF: Clinical Presentation 3. A provider discovers a bone tumor as an incidental finding on a radiograph in a patient who has sustained an injury to a ligament. The patient has not had pain prior to the injury. What will the provider do next? a. Consult with an orthopedic specialist b. Order a chest CT and full body scan c. Refer the patient to for a bone biopsy d. Repeat the radiograph in 6 to 12 months Latent bone tumors are usually discovered as incidental findings during evaluation for musculoskeletal injury. If the injury is the source of pain, the radiograph may be repeated in 6 to 12 months to determine whether it is increasing in size. Consultation with an orthopedic specialist, referral for a biopsy, and further testing with chest CT or full body scanning are done if there is suspicion of an active tumor.REF: Clinical Presentation Chapter 173: Bursitis Test Bank Multiple Choice 1. A patient with shoulder pain is seen by an orthopedic specialist who notes erythema, warmth, and fluctuance of the shoulder joint. What is the next step in treatment for this patient? a. Admit to the hospital for intravenous antibiotics b. Inject lidocaine into the joint and reassess in 5 to 10 minutes c. Order a plain radiograph of the shoulder to identify possible fracture d. Perform a shoulder ultrasound to further evaluate the cause Immediate referral is indicated for patients who present with symptoms consistent with septic bursitis, such as with the symptoms above. Lidocaine is injected into a painful joint to evaluate for improvement to determine whether bursitis or tendonitis is present as a result of impingement. This exam is not consistent with fracture. An ultrasound is not indicated.REF: Shoulder Bursitis/Management 2. A patient with elbow pain without localized erythema or warmth is diagnosed with bursitis of the elbow and serum laboratory results are pending. What is the initial treatment while waiting for these results? a. Aspiration of the bursal sac for culture b. Corticosteroid injection into the bursal sac c. Elbow pads, NSAIDs, rest, and ice d. Physical and occupational therapy Initial therapy includes conservative measures for comfort. Until infection is suspected, based on the white blood count and inflammatory markers, and without localized signs of infection, aspiration of the bursal sac is not indicated. Corticosteroids should not be injected into the bursal sac until infection has been excluded. Physical and occupational therapy should not precede comfort measures.REF: Elbow Bursitis/Management 3. What are included in the initial management of bursitis of the heel? Select all that apply. a. Activity modification and bracing b. Closed heel shoes to prevent further injury c. Corticosteroid injections d. Nonsteroidal anti-inflammatory medications e. Rest, ice, compression, and elevation , D, E Activity modification and bracing, NSAIDs, and RICE are all used initially to treat heel bursitis. Patients should wear open-heeled shoes. Corticosteroid injections should be used cautiously to prevent rupture of the Achilles tendon.REF: Heel Bursitis/Management Chapter 174: Elbow Pain Test Bank Multiple Choice 1. A patient has chronic elbow pain associated with arthritis. What is included in management of this condition? Select all that apply. a. Avoidance of certain activities b. Balanced rest and exercise c. Long-term NSAIDs d. Occupational therapy e. Splinting of the elbow , B, D Patients with arthritis may be managed by avoiding pain-causing activities, a program of balanced rest and exercise, and occupational therapy to improve function. NSAIDs are used for short periods. Splinting is not recommended.REF: Management 2. A patient reports elbow pain and the examiner elicits pain with resisted wrist flexion, forearm pronation, and passive wrist extension on the affected side. What is a likely cause of this pain? a. Lateral epicondylitis b. Medial collateral ligament instability c. Medial epicondylitis d. Ulnar neuritis Medial epicondylitis will produce pain as described above. Lateral epicondylitis may result in pain with passive wrist flexion and active wrist extension.REF: Physical Examination Chapter 175: Fibromyalgia and Myofascial Pain Syndrome Test Bank Multiple Choice 1. When counseling a patient about the long-term effects of fibromyalgia syndrome, what is important to include in teaching? a. A multidisciplinary approach to treatment is most effective. b. Eventual damage to muscles and joints will occur. c. Exercise may cause discomfort and damage to muscles. d. Medications are useful for controlling and preventing symptoms. A multidisciplinary approach to FMS management can help with pain management, stress, and exercise. Although patients experience pain, damage to tissues does not occur. Exercise may be painful, but does not cause damage. Medications help alleviate some, but not all symptoms.REF: Multidisciplinary Approach/Complications 2. Which are symptoms associated with fibromyalgia? Select all that apply. a. Gastrointestinal complaints b. Hepatosplenomegaly c. Musculoskeletal pain d. Non-restorative sleep e. Renal complications , C, D Fibromyalgia may cause GI complaints, musculoskeletal pain, and non-restorative sleep. Hepatosplenomegaly and renal complications are not associated with fibromyalgia.REF: Definition and Epidemiology 3. Which cause is implicated in patients with fibromyalgia syndrome (FMS)? a. Autoimmune disease b. Central nervous system dysfunction c. Muscle dysfunction d. Viral disease Although the cause of FMS is unclear, current research suggests a CNS cause and not muscle, autoimmune, or viral causes.REF: Pathophysiology Chapter 176: Gout Test Bank Multiple Choice 1. A patient with gout and impaired renal function who uses urate-lowering therapy (ULT) is experiencing an acute gout flare involving one joint. What is the recommended treatment? a. Administration of intra-articular corticosteroid b. Discontinuing ULT while treating the flare c. Oral colchicine for 5 days d. Therapy with NSAIDs begun within 24 hours Intra-articular steroids are practical and beneficial when only one or two joints are involved and are safe for patients who cannot use NSAIDs or colchicine. NSIADs are contraindicated in patients with renal disease and colchicine should not be used in those with low glomerular filtration rates. It is not necessary to discontinue urate-lowering therapy during an acute attack.REF: Management/Pharmacological Management/Treatment of Acute Gout 2. A patient experiences a second gouty flare and the provider decides to begin urate-lowering therapy (ULT). How should this be prescribed? a. Begin with a high loading dose and gradually decrease b. Start ULT during the current flare for best results c. Start ULT in 5 weeks along with an anti-inflammatory drug d. ULT should be suspended during future gouty flares Beginning therapy with a urate-lowering drug during an acute flare will prolong the flare. Typically, ULT is begun 5 to 6 weeks after a flare and should be given with an anti- inflammatory drug, since the initial period of ULT administration is associated with flares. ULT dosing should start low and gradually increase. It is not recommended to stop ULT during future flares, but to treat those flares while continuing the ULT.REF: Management/Pharmacological Management/Treatment of Chronic Gout 3. A post-menopausal female patient has a blood test that reveals hyperuricemia, although the patient has no symptoms of gout. What will the provider do? a. Ask the patient about medications and medical history b. Begin therapy with colchicine and an NSAID c. Recommend a low-purine, alcohol-restricted diet d. Treat for gout prophylactically to prevent a flare Patients without symptoms of gout but with hyperuricemia do not need treatment, since most of these patients will never have a gout flare. It is important, however, to determine the cause of this finding and correct it if possible, since it is a risk factor for gout. Certain medications and medical conditions can predispose patients to gout. Colchicine and NSAIDs are used to treat symptoms of gout. Dietary changes are not necessary and are difficult to follow. Prophylaxis for prevention of flares is for patients who have gout and who are between flares.REF: Pathophysiology/Management/Non-Pharmacologic Treatment Chapter 177: Hand and Wrist Pain Test Bank Multiple Choice 1. A patient has pain at the base of one thumb and reports frequently dropping things because of pain and weakness in that joint. During physical examination, what will the examiner do to help diagnose this condition? a. Adduct the first metacarpal and hyperextend the metacarpal phalanx b. Flex the thumb while placing a finger on the metacarpophalangeal joint c. Passively extend the thumb and observe for puckering of the skin d. Place the thumb on the palm while deviating the hand toward the ulna Adduction of the first metacarpal with hyperextension of the first metacarpal phalanx will elicit pain in patients with trapeziometacarpal arthritis which has symptoms described above. Flexing the thumb while the examiner places a finger on the metacarpophalangeal joint will elicit a pop when the digit is extended in patients with trigger finger. Puckering of the skin occurs with palmar fibrosis. Placing the patient’s thumb on the palm while deviating the hand toward the ulna will elicit pain in patients with tenosynovitis. REF: Physical Examination / Trapeziometacarpal Arthritis 2. A patient has symptoms of carpal tunnel syndrome. Which diagnostic tests will help confirm this disorder? Select all that apply. a. Anti-nuclear antibody b. Electromyography c. Erythrocyte sedimentation rate d. Nerve conduction studies e. Plain radiographs , D While diagnosis may be made on history and physical findings, electromyography and nerve conduction studies can be helpful to confirm or exclude carpal tunnel syndrome. ANA and ESR testing is useful when rheumatoid arthritis is suspected. Plain radiographs are not useful.REF: Diagnostics/Carpal Tunnel Syndrome 3. A 40-year-old woman reports pain at the thumb base in one hand radiating to the distal radius. The provider learns that the woman knits for a hobby and is able to elicit the pain by asking the patient to pour water from a pitcher. Which condition is suspected in this patient? a. Carpal tunnel syndrome b. Palmar fibrosis c. Tenosynovitis d. Trigger finger Tenosynovitis causes pain as described and occurs more in women between 30 and 59 years who engage in activities requiring excessive repetitive motions, such as knitting. Carpal tunnel syndrome presents with intermittent wrist pain, numbness, and tingling radiating from the palm to the thumb, index finger, middle finger, and medial aspect of the ring finger. Palmar fibrosis causes contractures, usually of the ring finger. Trigger finger causes nodules in tendons that catch on the finger pulley and impede movement.REF: Clinical Presentation/Tenosynovitis Chapter 178: Hip Pain Test Bank Multiple Choice 1. A patient with chronic hip pain cannot take NSAIDs and tells the provider that acetaminophen is minimally helpful. What might the provider recommend initially to improve pain relief? a. A fentanyl patch b. Capsaicin c. Glucosamine d. Lidocaine patches Topical capsaicin has been shown to provide short-term pain relief and has fewer side effects than oral agents. It is an appropriate initial therapy. Fentanyl is a narcotic analgesic and should be reserved for more severe pain. Glucosamine and lidocaine may be helpful for some patients.REF: Pain Management 2. An adult patient who has been taking high-dose corticosteroids reports a dull, aching pain in the groin and presents with a limp. What condition does the provider suspect, based on this history? a. Avascular necrosis of the femoral head b. Infectious arthritis of the hip c. Osteoarthritis of the hip d. Slipped capital femoral epiphysis Avascular necrosis has the symptoms listed above and is common among patients who have been taking corticosteroids. Infectious arthritis will typically be accompanied by fever and intense pain. Osteoarthritis causes progressively worsening pain with activity and improvement with rest. SCFE is common in adolescents.REF: Clinical Presentation Chapter 179: Infectious Arthritis Test Bank Multiple Choice 1. A patient reports the sudden onset of pain, redness, and swelling in one knee joint along with a no fever. The provider elicits exquisite pain with manipulation of the joint and notes no decrease in pain when the joint is at rest. Which is the likely cause of this arthritis? a. Bacterial infection b. Gout c. Lyme disease d. Rheumatoid arthritis Septic arthritis is usually painful both with movement and at rest and is accompanied by swelling and erythema. Fever is not always present. The other causes of arthritis are not painful at rest.REF: Clinical Presentation 2. An adolescent patient reports pain and swelling in various joints on the right side that comes and goes and occurs in the knee, elbow, wrist, and ankle. A physical examination reveals tenosynovitis and a maculopapular rash. Which diagnostic tests will be most helpful in determining a diagnosis in this patient? a. Blood cultures and a complete blood count b. Cultures of the urethra, pharynx, cervix, and rectum c. Skin lesion scrapings and cultures d. Urine cultures and renal function studies This patient has signs of gonococcal arthritis. Cultures of the urethra, pharynx, cervix, and rectum will be positive in 80% of patients with this infection. Blood cultures are likely to be negative. Culturing skin lesions is not helpful. Renal involvement is not part of this infection.REF: Gonococcal Arthritis 3. A patient has marked swelling of a shoulder joint with erythema and severe pain. The provider suspects a bacterial cause. Which culture will be most helpful to determine the cause of these symptoms? a. Blood culture b. Synovial fluid culture c. Urethral culture d. Urine culture Synovial fluid culture is the most important exam for diagnosis of septic arthritis. Blood culture may be positive in only 10% of cases. Urethral culture is performed if gonococcal arthritis is suspected. Urine culture is not helpful.REF: Diagnostics Chapter 180: Knee Pain Test Bank Multiple Choice 1. Which maneuver during a physical examination is used to assess the anterior cruciate ligament? a. Anterior drawer test b. Posterior drawer test c. Valgus stress on knee joint d. Varus stress on knee joint The anterior drawer test, in which the examiner pulls the tibia forward while the knee is flexed, is used to assess anterior cruciate ligament laxity. The posterior drawer test is used to determine posterior cruciate ligament laxity. The valgus stress test assesses MCL laxity and the varus stress test assesses LCL laxity.REF: Cruciate Ligament Injuries/Physical Examination 2. A previously healthy patient reports a sensation of one knee locking or feeling like it will give way when descending stairs. The patient has no recollection of injury to the knee and denies pain. What is the most likely treatment for this disorder? a. Conservative management with RICE and activity modification b. Immediate referral to an orthopedic surgeon for possible repair c. Intra-articular injections of corticosteroids three times yearly d. Restricting participation in sports and strenuous workouts indefinitely This patient has symptoms consistent with chronic degenerative meniscal injury and is without pain or significant disability. Conservative management is indicated. Immediate referral is indicated for severe pain or disability. Intra-articular injections of corticosteroids are used for patients with concomitant osteoarthritis. Patients should be encouraged to continue sports and exercise to improve overall muscle tone and minimize disability.REF: Meniscal Injury/Management 3. A high school soccer player sustains a knee injury when kicked on the lateral side of the knee by another player. The provider notes significant swelling of the knee, with pain at the joint line on the medial aspect of the knee. What will the provider do to treat this injury? a. Instruct about RICE management and follow up in 1 week b. Refer for a same-day orthopedic consultation c. Schedule a magnetic resonance imaging (MRI) exam d. Splint the knee and refer for orthopedic consultation in 1 to 2 weeks This patient has an injury caused by a traumatic event associated with swelling and should have a same-day orthopedic consultation. Simple sprains may be managed with RICE. MRI may be ordered by the orthopedist.REF: Definition and Epidemiology/Collateral Ligament Sprains Chapter 181: Low Back Pain Test Bank Multiple Choice 1. A patient has recurrent lumbar pain which is sometimes severe. The patient reports that prescription NSAIDs are no longer effective for pain relief. What will the provider recommend? a. Adjunctive treatment with physical therapy b. Beginning treatment with opioid analgesics c. Complementary and alternative therapies d. Referral to an interventional spine physician Patients with recurrent or chronic lower back pain may benefit from lumbar epidural corticosteroid injection performed by an interventional spine physician. Physical therapy is often used for acute injury if no improvement in 4 to 6 weeks. Opioid analgesics are not usually effective.REF: Spinal Interventional Procedures 2. A patient reports severe back pain located in the lumbar spine. To evaluate whether the patient has axial pain or radicular pain, which assessment is necessary? a. Asking the patient to perform the Valsalva maneuver b. Assessing reflexes and asking about tingling or numbness c. Determining whether the pain is present with prolonged sitting d. Noting whether pain is mitigated with frequent position shifts Associated neurological signs are present with radicular pain and include numbness, tingling, weakness, and reflex changes. The other symptoms occur with both axial and radicular pain.REF: Clinical Presentation 3. A patient has an acute onset of lower back pain associated with lifting heavy objects at work. A physical examination reveals no loss of lower extremity function or neurological symptoms. What is the initial intervention for this patient? a. MRI to evaluate soft tissue involvement b. Plain radiographs to evaluate the extent of the injury c. Traction therapy to minimize complications d. Treatment with a nonsteroidal anti-inflammatory drug NSAIDs are appropriate as first-line treatment in patients without potential complications. Radiologic studies are performed if improvement does not occur in 4 to 6 weeks. Traction may be used for patients with radicular symptoms to help resolve neurological deficits, although systematic review of research has not clearly identified a benefit to this therapy.REF: Management Chapter 182: Metabolic Bone Disease: Osteoporosis and Paget's Disease of the Bone Test Bank Multiple Choice 1. A patient is diagnosed with osteoporosis. What is the recommended treatment once the diagnosis is made? a. Biphosphonate therapy b. Calcium and vitamin D c. Estrogen replacement d. Yoga and weight-bearing exercises Biphosphenates are the only FDA-approved treatment for osteoporosis and will help improve bone density and reduce the risk of fractures. Calcium and vitamin D may help prevent osteoporosis, but must be taken from an early age. Estrogen replacement is used to prevent osteoporosis. Yoga and exercise help with balance and muscle strength to help prevent falls.REF: Management 2. A patient has bone pain and laboratory testing reveals an elevated serum alkaline phosphatase (SAP). Which test can help distinguish Paget’s from malignant bone disease? a. Bone densitometry b. Bone marrow biopsy c. Bone radiograph d. Bone scan A plain bone radiograph will show changes pathognomonic of Paget’s disease. The other tests are not necessary.REF: Paget’s Disease/Differential Diagnosis 3. The primary care provider is assessing a 45-year-old postmenopausal woman who has a family history of osteoporosis. Which test will be most useful to screen for this disease in this patient? a. Biochemical markers of bone resorption and bone formation b. Bone densitometry of the hip and posteroanterior lumbar spine c. Plain radiographs of the hips and lumbar and thoracic spine d. Serum calcium and serum 25-hydroxyvitamin D Postmenopausal women are candidates for bone densitometry to assess for osteopenia and osteoporosis. Biochemical markers are generally ordered by specialists; their role in primary care is uncertain. Plain radiographs are used to determine fracture. Serum calcium and vitamin D levels are useful in the general population as a preventive measure.REF: Diagnostics/Box 182-2: Indications for Bone Densitometry Chapter 183: Neck Pain Test Bank Multiple Choice 1. A patient comes to a provider with reports of unilateral arm pain and weakness with mild neck pain. The provider notes that the patient prefers holding the affected arm crossed in front of the throat. A history reveals a recent onset of sexual dysfunction. What does the provider suspect based on this history? a. Axial neck pain b. Cervical myelopathy c. Diabetic neuropathy d. Facet joint pain Patients with neurological symptoms have radicular neck pain, which is usually greater in one arm and involves neurological findings. Patients with concurrent lower extremity findings may have cervical myelopathy and should be evaluated immediately. Axial neck pain does not involve neurological findings. Diabetic neuropathy typically does not include neck pain. Facet joint pain is a cause of axial neck pain, associated with injuries and headaches.REF: Clinical Presentation 2. A patient has chronic radicular neck pain that no longer responds to over-the-counter NSAIDs and physical therapy measures and reports having difficulty sleeping. Which medication will the provider order? a. A skeletal muscle relaxant b. A tricyclic antidepressant c. An opioid analgesic d. Gabapentin Gabapentin is useful for central pain syndromes and radiculopathy and can help to restore sleep. Skeletal muscle relaxants are useful for muscle spasms. A tricyclic antidepressant is useful for some chronic neck pain, although gabapentin is more specific to this patient’s symptoms. Opioid analgesics should be used cautiously.REF: Medications 3. A provider suspects degenerative disk disease in a patient with chronic neck pain. Which diagnostic test will be performed? a. Computerized tomography b. Magnetic resonance imaging c. Plain radiograph d. Radionucleotide bone scintigraphy MRI is usually performed to diagnose degenerative disk disease. CT testing is used to identify bone and degenerative changes, but the exposure to radiation is high. Plain radiographs are used to identify fractures or when trauma or cancer is present. Radionucleotide bone scintigraphy is used for osteomyelitis, metastatic disease, or occult fracture.REF: Diagnostics Chapter 184: Osteoarthritis Test Bank Multiple Choice 1. A 45-year-old patient has mild osteoarthritis in both knees and asks about non-pharmacologic therapies. What will the provider recommend? a. Aerobic exercise b. Glucosamine with chondroitin c. Therapeutic magnets or copper bracelets d. Using a cane or walker Aerobic exercise helps with cardiovascular conditioning and weight reduction as well as improved range of motion, decreased pain, and strengthening of supporting structures. Randomized controlled studies have failed to demonstrate significant pain relief with glucosamine. Therapeutic magnets and copper have not been proven to be effective. A young patient with mild symptoms will not need assistive devices and should focus on conditioning.REF: Non-Pharmacologic Management/Complementary Approaches 2. A patient who has osteoarthritis in the carpometacarpal joints of both thumbs asks about corticosteroid injections to treat symptoms. What will the provider tell this patient about this therapy? a. Corticosteroid therapy reduces inflammation and improves joint mobility b. Injections may be administered as needed up to 6 times per year c. Intra-articular injections provide significant pain relief for 3 to 4 months d. This treatment may cause a temporary increase in pain, warmth, and redness Intra-articular injections of corticosteroids are helpful in decreasing pain, but may cause a transient increase in pain, warmth, and redness. This therapy does not improve inflammation and joint mobility. Injections are not recommended more than 3 to 4 times per year. The duration of pain relief is variable.REF: Intra-Articular Corticosteroid Injections 3. A 50-year-old woman reports pain in one knee upon awakening each morning that goes away later in the morning. A knee radiograph is negative for pathology and serum inflammatory markers are normal. What will the provider tell this patient? a. A magnetic resonance imaging study is necessary for diagnosis b. That the lack of findings indicates no disease process c. To take acetaminophen 1 gram three times daily for pain d. To use a cyclooxygenase 2-selective NSAIDs to reduce inflammation Acetaminophen is the mainstay for initial treatment of osteoarthritis. Radiologic findings are often negative in the early stages of the disease. There are no serologic markers for OA. A COX2-selective inhibitor has cardiovascular side effects and should not be used unless necessary. These agents are used more for pain than for inflammation.REF: Diagnostics/Management Chapter 185: Osteomyelitis Test Bank Multiple Choice 1. A 3-year-old child has marked pain in one leg localized to the upper tibia with refusal to bear weight. The child has a high fever and a toxic appearance. Which type of osteomyelitis is most likely? a. Chronic osteomyelitis b. Hematogenous osteomyelitis c. Osteomyelitis from a contiguous focus d. Peripheral vascular disease osteomyelitis Young children are more likely to have hematogenous osteomyelitis, especially with acute symptoms. Chronic osteomyelitis is more common with underlying diseases such as diabetes. Contiguous focus osteomyelitis occurs when organisms are introduced from a puncture wound, foreign body, or adjoining soft tissue infection. Peripheral vascular causes are more common in chronically ill patients.REF: Definition and Epidemiology 2. A 50-year-old patient with diabetes mellitus has a low-grade fever and pain on one foot. The provider notes erythema and swelling at the site along with several superficial skin ulcers without necrosis and suspects osteomyelitis. Which type of diagnostic study will the provider order? a. Biopsy of bone or debridement cultures b. Blood cultures and serologic markers of inflammation c. Magnetic resonance imaging of the foot d. Plain radiograph of the foot A patient with diabetic foot infection suspected of having osteomyelitis should have a plain radiograph to identify bony abnormality or soft tissue changes. MRI may be performed if more specific evaluation is needed or if abscess is suspected. Blood cultures are not diagnostic of osteomyelitis. Biopsy and debridement cultures increase the risk of further infection if poor healing at the site occurs.REF: Diabetic Foot 3. A patient has osteomyelitis related to vascular insufficiency. Which initial consultation is necessary? a. Infectious disease consultation b. Neurosurgical consultation c. Surgical consultation d. Wound care specialist consultation Because patients with vascular insufficiency who develop osteomyelitis may need debridement or draining of lesions, a surgical consult is necessary. Infectious disease consults are obtained for patients with resistant organisms or complex wounds. Neurosurgical consults are needed for patients with epidural abscess. Wound care consults are needed for patients with progressive or chronic wounds.REF: Management/Specialist Consultation Chapter 186: Shoulder Pain Test Bank Multiple Choice 1. A 45-year-old patient reports a recent onset of unilateral shoulder pain which is described as diffuse and is associated with weakness of the shoulder but no loss of passive range of motion. What does the provider suspect as the cause of these symptoms? a. Acromioclavicular joint disease b. Cervical radicular pain c. Glenohumeral arthritis d. Rotator cuff injury Rotator cuff injury is usually characterized by diffuse pain, weakness of the joint, but no change in range of motion. Acromioclavicular joint disease is associated with anterior-superior shoulder pain. Glenohumeral arthritis has similar symptoms, but with loss of range of motion. Cervical radicular pain is characterized by pain distal to the elbow.REF: Clinical Presentation 2. A patient reports a deep ache in one shoulder and the provider suspects tendonitis secondary to repetitive activity. To determine whether the pain is caused by impingement on the acromion, the provider will ask the patient to a. abduct the arm. b. adduct the arm. c. internally rotate the shoulder. d. shrug the shoulders. If pain is caused by impingement on the acromion, the patient will reflexively shrug when asked to abduct the arm to reduce the pain. Adduction of the arm does not elicit this response. The shrug elicited is reflexive and not intentional. Internal rotation may be performed to evaluate generalized muscle weakness.REF: Tendonitis 3. An examiner is evaluating a patient who reports unilateral shoulder pain and notes limited active and passive range of motion in the affected shoulder along with erythema and bulging on the anterior shoulder. What diagnosis is likely with this presentation? a. Acromioclavicular joint disease b. Adhesive capsulitis c. Inflammatory bursitis d. Rotator cuff tear Both bursitis and adhesive capsulitis will present with decreased active and passive range of motion, but patients with inflammatory bursitis will exhibit erythema and bulging of the anterior shoulder. Acromioclavicular joint disease does not cause erythema or bulging of the joint.REF: Physical Examination Chapter 187: Sprains, Strains, and Fractures Test Bank Multiple Choice 1. An emergency department provider is giving instructions for rest, ice, compression, and elevation (RICE) treatment in a patient with a sprain. What is included in teaching about this home care? Select all that apply. a. An elastic bandage is sufficient for compression b. Apply ice packs for 20 minutes three times daily c. Proximal joints should be elevated higher than distal joints d. Moist heat therapy may be applied if muscle spasm occurs e. Place a cloth between the ice pack and the skin , D, E There is good evidence supporting use of an economical elastic bandage for support and compression. Moist heat therapy may be administered if muscle spasm occurs with ice therapy. If using an ice pack, a cloth should be placed between the ice pack and skin to prevent cold burn. Ice packs should be applied at 20 minute intervals, allowing the skin to return to normal temperature before each application. Distal joints should be higher than proximal joints.REF: Management 2. A soccer player is brought to the emergency department after twisting an ankle during a game. An examination of the affected joint reveals ecchymosis and edema of the ankle and limited joint laxity along with pain on weight-bearing, although movement with pain is intact. Which grade sprain is likely? a. Grade I b. Grade II c. Grade III d. Grade IV This patient probably has a grade II sprain, which involves incomplete tear of a ligament with some functional impairment, ecchymosis, and pain with weight-bearing. A grade I sprain causes only pain and edema. A grade III sprain is a full or complete tear of the ligament with loss of ligament integrity. A grade IV sprain results in severe weakness with loss of function.REF: Pathophysiology 3. A school-age child falls off a swing and fractures the humerus close to the elbow joint. What is the most important assessment for this patient to evaluate possible complications of this injury? a. Evaluation of pain with extension b. Palpation for joint laxity c. Salter-Harris classification d. The presence of a spiral fracture Salter-Harris classification identifies the degree of epiphyseal, or growth plate involvement and is important to evaluate in children and adolescents, since damage to the growth plate can result in shortening of the long bone. The other assessments are part of the exam, but have less importance than assessment of growth plate involvement.REF: Physical Assessment Chapter 188: Neuropsychological Evaluation Test Bank Multiple Choice 1. What are some common goals of neuropsychiatric evaluation? Select all that apply. a. To definitively diagnose neurobehavioral disorders b. To determine the need for neurosurgical procedures c. To evaluate cognition when neuro-diagnostic tests are normal d. To help identify rehabilitation goals in brain-injured patients e. To monitor changes in symptoms over time , D, E Neuropsychological testing is performed to evaluate cognition when other diagnostic tests may be normal, to help identify rehabilitation goals for brain-injured patients, and to monitor changes in patients over time. Because they are one piece of the diagnostic workup, they do not definitively diagnose disorders or determine the need for surgical procedures.REF: Box 188-2: Neuropsychological Assessment Goals 2. What is an important purpose of conducting an interview prior to beginning neuropsychological testing on an older adult suspected of having dementia? a. To assess the patient’s ability to cooperate with the testing b. To determine the patient’s degree of dementia c. To evaluate the patient’s feelings about family members’ concerns d. To find out whether a referral to a specialist is needed The pre-testing interview may be conducted to determine whether a patient may need assistance or accommodations when being tested. The test itself will measure the degree of cognitive impairment. The interview may include the patient’s feelings, but the ability to cooperate with testing is a more important part of the interview. The testing will identify the need for referral.REF: Overview of the Assessment Process Chapter 189: Amyotrophic Lateral Sclerosis Test Bank Multiple Choice 1. A patient with a family history of amyotrophic lateral sclerosis (ALS) begins to have symptoms that include asymmetric weakness in the arms and difficulty walking. The neurologist recognizes these symptoms as characteristic of involvement of which portion of the nervous system? a. Lower motor neurons b. Upper motor neurons c. Corticospinal tracts d. Corticobulbar tracts Lower motor neuron involvement and early LMN cell death leads to an insidious onset of asymmetric weakness that is evident initially in the limbs, usually in the arms. Upper motor neuron cell death may result in hyperreflexia, spasticity, incoordination, and weakness. bulbar signs include dysarthria, dysphagia, and tongue fasiculations. The corticospinal tracts are part of the UMN cells.REF: Clinical Presentation and Physical Examination 2. The spouse of a patient newly-diagnosed with amyotrophic lateral sclerosis (ALS) asks about long-term care. What will the provider include when teaching the family about this disease? a. Bowel and bladder function will eventually be lost. b. Positive-pressure ventilation can prolong life. c. Preventing malnutrition is a key element in care. d. The nerves affecting sensation will die initially. Prevention of malnutrition may improve both the quality and length of life. Bowel and bladder function and sensation remain intact. Positive-pressure ventilation helps to relieve sleep disturbance.REF: Complications Chapter 190: Bell's Palsy Test Bank Multiple Choice 1. Which symptoms may occur with Bell’s palsy? Select all that apply. a. Alteration in taste b. Decreased hearing c. Drooling d. Inability to open the eye e. Tinnitus , C, E Bell’s palsy may cause altered taste, drooling, and tinnitus. It causes increased sensitivity to noises and an inability to close the eye.REF: Clinical Presentation 2. A 35-year-old patient reports suddenly experiencing an asymmetric smile along with drooping and tearing in one eye. The patient has a history of a recent viral illness, but is otherwise healthy. During the exam, the provider notes that there is unilateral full face paralysis on the right side. What is the initial intervention for this patient? a. Perform confirmatory diagnostic tests b. Prescribe oral prednisolone c. Recommend wearing an eye patch d. Refer the patient to a neurologist Steroids are highly effective and increase the probability of complete nerve recovery and should be started within 72 hours of onset. There are no confirmatory diagnostic tests, but other tests may be performed to rule out certain causes. Patients may be instructed to tape the eye closed at night, but eye patches are not recommended. A neurology referral is needed only if patients have an atypical presentation or other comorbid conditions.REF: Management 3. What is recommended to prevent ophthalmic complications in patients with Bell’s palsy? a. Acupuncture b. Lubricating eye drops c. Patching of the eye d. Sunglasses Exposure keratitis from drying of the eye can result in blindness. Lubricating eye drops should be used every 2 hours. Acupuncture has not been sufficiently studied. Patching is not recommended. Protective eyewear to prevent moisture loss is recommended.REF: Management Chapter 191: Cerebrovascular Events Test Bank Multiple Choice 1. A previously healthy 30-year-old patient is brought to the emergency department with signs of stroke. Diagnostic testing determines an ongoing ischemic cause. The patient’s spouse reports that symptoms began approximately 2 hours prior to transport. What is the recommended treatment? a. Administration of low-molecular-weight heparin b. Neurosurgical consultation for possible surgery c. Observation for complications prior to initiating tPA d. Tissue plasminogen activator (tPA) administration This patient meets the criteria for tPA administration and it should be begun within 3 hours after onset of symptoms. This patient has had symptoms for over 2 hours, so tPA should begin immediately. LMW heparin is not indicated. Neurosurgical intervention is recommended for patients with hemorrhagic stroke.REF: Thrombolytic Therapy 2. An elderly patient is brought to the emergency department after being found on the floor after a fall. The patient has unilateral sagging of the face, marked slurring of the speech, and paralysis on one side of the body. The patient’s blood pressure is 220/190 mm Hg. What is the likely treatment for this patient? a. Carotid endarterectomy b. Close observation until symptoms resolve c. Neurosurgical consultation d. Thrombolytic therapy This patient has signs consistent with hemorrhagic stroke and will need consultation with a neurosurgeon to determine whether surgical intervention will be beneficial. Carotid endarterectomy is performed in patients with carotid stenosis and is used in patients with hemispheric ACVS (TIA). Patients with TIA may be observed to monitor symptoms. Thrombolytic therapy is given to patients with ischemic stroke.REF: Management/Surgery 3. A patient exhibits visual field defect, ataxia, and dysarthria and complains of a mild headache. A family member reports that the symptoms began several hours prior. An examination reveals normal range of motion of the neck. What type of cerebrovascular event is most likely? a. Hemorrhagic stroke b. Hypertensive intracerebral hemorrhage c. Ischemic stroke d. Transient ischemic attack Patients with ischemic stroke typically do not have headache; if they do, it is milder than with hemorrhagic stroke. A TIA resolves within minutes.REF: Clinical Presentation Chapter 192: Delirium Test Bank Multiple Choice 1. What are initial approaches when managing delirium in a hospitalized patient who is agitated and confused? Select all that apply. a. Administer medications for sleep b. Apply physical restraints c. Attend to hydration and toileting needs d. Decrease stimulation e. Discontinue any non-essential medications , D, E Patients with delirium should be assisted with hydration and toileting needs. Stimulation should be decreased. Any non-essential medications should be discontinued. Giving medications for sleep may exacerbate the delirium. Physical restraints should be avoided unless necessary for safety.REF: Management 2. A previously lucid patient with early-stage Alzheimer’s disease is hospitalized after a surgical procedure and exhibits distractibility and perceptual disturbances that occur only in the late afternoon. The patient has difficulty sleeping at night and instead sleeps much of the morning. What is the likely cause of these symptoms? a. Hyperactive delirium b. Hypoactive delirium c. Sundowner syndrome d. Worsening dementia Patients with dementia are at increased risk of sundowner syndrome, characterized by the symptoms above and which typically appear in late afternoon and early evening. Hyperactive delirium is manifested by agitation and restlessness. Hypoactive delirium includes patients with decreased alertness, lethargy, and slowed speech. Delirium and worsening of dementia would cause symptoms around the clock, not just in the late afternoon or evening.REF: Clinical Presentation 3. An 80-year-old patient becomes apathetic, with decreased alertness and a slowing of speech several days after hip replacement surgery alternating with long periods of lucidity. What is the most likely cause of these symptoms? a. Anesthesia effects b. Delirium c. Pain medications d. Stroke An acute presentation of these symptoms is most likely delirium since they alternate with lucid periods. The other causes may contribute to delirium by intensifying it.REF: Clinical Presentation Chapter 193: Dementia Test Bank Multiple Choice 1. A patient with dementia experiences agitation and visual hallucinations and is given haloperidol with a subsequent worsening of symptoms. Based on this response, what is the likely cause of this patient’s symptoms? a. Alzheimer’s disease b. Lewy body dementia c. Pseudodementia d. Vascular neurocognitive disorder Patients with Lewy body dementia may present with these symptoms and will have an increased sensitivity to neuroleptics; when given haloperidol for agitation, will actually get worse. The other causes do not have these characteristic symptoms and are not sensitive to neuroleptics in this manner.REF: Clinical Presentation 2. A patient with Alzheimer’s disease (AD) is taking donepezil to treat cognitive symptoms. The patient’s son reports noting increased social withdrawal and sleep impairment. What is the initial step to manage these symptoms? a. Encourage activity and exercise b. Prescribe a selective serotonin reuptake inhibitor c. Recommend risperidone d. Referral to a neurologist for evaluation Patients with AD may have improvement in depression with nonpharmacologic management, including exercise and increased activity. If this is not effective, an SSRI may be prescribed. Risperidone, and other antipsychotics should not be prescribed.REF: Management 3. An elderly patient has symptoms of depression and the patient’s daughter asks about possible Alzheimer’s disease since there is a family history of this disease. A screening evaluation shows no memory loss. What is the initial step in managing this patient? a. Order brain imaging studies such as CT or MRI b. Perform genetic testing to identify true risk c. Prescribe a trial of an antidepressant medication d. Recommend a trial of a cholinesterase inhibitor drug Elderly patients with depression who do not have other signs of AD may be given a trial of antidepressant medications initially in order to evaluate these symptoms. Brain imaging studies are not indicated initially. Genetic testing is not indicated. Once the degree of depression is determined and if other symptoms appear, an anticholinesterase inhibitor may be ordered.REF: Clinical Presentation/Diagnostics Chapter 194: Dizziness and Vertigo Test Bank Multiple Choice 1. A patient reports a recurrent sensation of spinning associated with nausea and vomiting. Which test will the provider order to confirm a diagnosis for this patient? a. Electroencephalogram b. Holter monitoring and electrocardiogram c. Neuroimaging with computerized tomography d. The Hallpike-Dix positioning maneuver This patient has symptoms consistent with a vestibular lesion, so the provider will order a Hallpike-Dix positioning maneuver to evaluate vestibular function. If seizure activity is suspected, an electroencephalogram will be ordered. Holter monitoring and ECG are used if patients report syncope or lightheadedness. Neuroimaging with CT is used when patients possibly have a central lesion which would present with difficulty balancing.REF: Clinical Presentation/Diagnostics 2. An elderly patient reports sensations of being off balance when walking, but does not experience dizziness. The provider will refer this patient to which specialist for further evaluation? a. Audiologist b. Cardiologist c. Neurologist d. Otolaryngologist This patient has problems of balance without dizziness, suggestive of a central neural lesion and should be referred to a neurologist. Patients with vertigo are likely to have vestibular dysfunction and would be referred to an otolaryngologist and possibly an audiologist if hearing is affected. Patients with syncope or lightheadedness are more likely to have an underlying cardiac disorder and would be referred to a cardiologist.REF: Clinical Presentation/Management Chapter 195: Guillain-Barré Syndrome Test Bank Multiple Choice 1. Which diagnostic test helps confirm a diagnosis of Guillain-Barre syndrome in a patient who is developing muscle weakness and paresthesias? a. Lumbar puncture b. MRI imaging c. Nerve conduction studies d. Screening for systemic infection A lumbar puncture is the most important confirmatory test showing albuminocytologic disassociation. MRI imaging typically is not necessary unless there is concern for spine pathology, but does not diagnose GBS. Nerve conduction studies are not necessary for the diagnosis. Screening for systemic infection is based on history and does not diagnose GBS.REF: Diagnostics 2. Which monitoring parameters are necessary when caring for a patient with Guillain-Barre syndrome? Select all that apply. a. Bladder scans b. Cardiac telemetry c. Imaging studies d. Fever e. Vital capacity measures , B, D, E Urinary retention can cause discomfort and infection, so assessment of urinary retention is necessary. Cardiac telemetry is essential, as are measures of pulmonary function. Imaging studies are not essential.REF: Management 3. Following an upper respiratory infection, a patient begins to develop ataxia and distal paresthesias, along with oculomotor symptoms and double vision. Based on these presenting symptoms which type of GBS does this patient have? a. Acute inflammatory demyelinating polyradiculoneuropathy (AIDP) b. Acute motor axonal neuropathy (AMAN) c. Classic Guillain-Barre syndrome d. Miller Fisher syndrome (MFS) Miller Fisher syndrome has oculomotor symptoms. Patients with this type tend to peak sooner and recover more completely and quickly.REF: Clinical Presentation Chapter 196: Headache Test Bank Multiple Choice 1. A patient has recurrent cluster headaches and asks about abortive therapy. Which therapy is effective for a majority of patients with cluster headaches? a. Lithium b. NSAIDs c. Oxygen d. Verapamil Oxygen works as abortive therapy for cluster headaches in 75% of patients and should be inhaled at the start of an attack. Lithium and verapamil work well as preventive medications for cluster headaches, but are not given for abortive treatment. NSAIDs are not useful.REF: Management 2. A patient reports recurrent headaches occurring 1 or 2 times per month that generally occur with weather changes or when sleep patterns are disrupted and describes them as severe, with throbbing on one side of the head and sometimes accompanied by nausea. What is the recommended treatment for this type of headache? a. Gabapentin b. Propranolol c. Rizatriptan d. Topiramate This patient describes migraine headache without aura and has fewer than 4 per month. An abortive medication, such as rizatriptan is recommended. The other medications are preventive medications and are used for patients having more than 4 per month.REF: Clinical Presentation/Management 3. Which medications may be useful in treating tension-type headache? Select all that apply. a. Antiemetics b. Lithium c. Muscle relaxants d. NSAIDs e. Oxygen , C, D Antiemetics, muscle relaxants, and NSAIDs may all be used to treat tension-type headaches. Lithium and oxygen are not used.REF: Management Chapter 197: Infections of the Central Nervous System Test Bank Multiple Choice 1. A provider suspects that a patient has bacterial meningitis. When should antibiotics be given? a. If the serum C-reactive protein is greater than 10 mg/L b. Immediately after blood and spinal cultures are obtained c. Prior to obtaining a CT scan or lumbar puncture d. When initial spinal fluid gram stain results are available In all cases of suspected meningitis, the first dose of antimicrobials should be administered as soon as possible and prior to the CT and LP to avoid critical delays in treatment. The CSF culture will still yield bacteria for 1-2 hours after the first dose. Waiting for any laboratory results may delay effective treatment.REF: Management 2. A patient is brought to the emergency department with fever, lethargy, and headache without meningeal signs. The examination reveals hypotension and lethargy and the examiner notes petechiae on the patient’s trunk. What do these findings indicate? a. A poor prognosis b. Encephalitis c. Increased intracranial pressure d. Probable viral infection Petechiae are an ominous sign, indicating a rapidly progressing meningococcemia. Patients with encephalitis or other viral infection will not usually have petechiae and severe symptoms. Increased ICP will present with hypertension.REF: Clinical Presentation/Physical Examination Chapter 198: Movement Disorders and Essential Tremor Test Bank Multiple Choice 1. Which are common hyperkinetic movement disorders? Select all that apply. a. Dystonia b. Essential tremor c. Parkinson’s disease d. Progressive supranuclear palsy e. Tourette’s syndrome , B, E Dystonia, essential tremor, and Tourette’s are hyperkinetic disorders. Parkinson’s disease, and progressive supranuclear palsy are hypokinetic disorders.REF: Definition and Epidemiology 2. A patient reports trembling of both hands causing difficulty performing tasks with the hands. The provider notes symmetric, rhythmic movements which are present at rest and no other neurological findings. A history reveals that the trembling decreases when the patient has a glass of wine with dinner. What is the initial action? a. Evaluation in an emergency department b. Prescribing a beta blocker medication c. Reassurance that these will subside d. Referral to a neurologist This patient has symptoms consistent with essential tremors. Reassurance may be the first action, but the symptoms will not subside. Beta blockers are used when the tremor is functionally or socially problematic. It is not necessary to refer to an ED or a specialist.REF: Essential Tremors/Clinical Presentation/Management Chapter 199: Multiple Sclerosis Test Bank Multiple Choice 1. A patient reports two episodes of visual disturbances and eye pain that lasted 1 to 2 days each about 2 months apart. Which diagnostic testing will the provider order initially? a. Lumbar puncture b. Magnetic resonance imaging c. Optical Coherence Tomography d. Visual evoked potential Visual disturbances and eye pain may be the only presenting symptoms and should be investigated. The MRI is the gold standard for diagnosis of MS. The other tests may be performed if the diagnosis is unclear or if MRI is not readily available.REF: Diagnostics 2. A patient diagnosed with multiple sclerosis and begins disease modulating therapy drugs. As part of the counseling about this therapy, the provider will tell the patient that this regimen will a. decrease the need for other medications. b. induce long-term remission. c. reduce the exacerbation rate. d. stop progression of the disability. Disease modulating therapy will reduce the rate of exacerbations of symptoms. It does not decrease the need for other medications, induce long-term remission, or stop the progression of the disease.REF: Management Chapter 200: Parkinson's Disease Test Bank Multiple Choice 1. A patient with Parkinson’s disease (PD) has been taking carbidopa-levodopa (Sinemet) with good results, but develops increased dyskinesia. Which drug will be added to this patient’s regimen to help control this symptom? a. Amantadine b. Benztropine c. Ropinirole d. Tolcapone Amantadine is an antiviral agent that has antiparkinsonian activity. It is useful for controlling dyskinesia as adjunctive therapy to levodopa and is more effective than anticholinergic drugs. Benztropine is an anticholinergic drug that may be used for this purpose, but is less effective and is more commonly used to treat antipsychotic-induced parkinsonism. Ropinirole is used as a first-line agent in patients with young-onset PD. Tolcapone is a COMT agent to prolong and potentiate the effects of levodopa to help prevent “wearing off” periods.REF: Management 2. A primary care provider suspects Parkinson’s disease (PD) in a patient. Which tests may be performed to diagnose this disorder? a. Neuroimaging to identify specific midbrain lesion b. Neuromuscular studies to identify reflex function c. Presence of 2 cardinal signs which improve with levodopa d. Serum creatine phosphokinase levels The diagnosis of idiopathic PD is made based on clinical presentation and examination findings with 2 of 3 cardinal manifestations present which respond to dopaminergic therapy. Neuroimaging that identifies Lewy bodies is the gold standard, but is performed post-mortem. Neuromuscular studies and serum laboratory studies are not useful unless excluding other causes of symptoms.REF: Diagnostics 3. What are common symptoms seen in patients with Parkinson’s disease? Select all that apply. a. Bradykinesia b. Festination c. Hyperphonia d. Rigidity e. Symmetric tremor , B, D Symptoms of Parkinson’s disease include bradykinesia, or loss of automatic movement, festination, or an impulse to take much quicker and shorter steps, and rigidity. Hypophonia, not hyperphonia occurs. Tremors are unilateral or asymmetric.REF: Clinical Presentation Chapter 201: Seizure Disorder Test Bank Multiple Choice 1. A patient who has a seizure disorder and who takes levetiracetam is brought to an emergency department with a seizure which has persisted for15 minutes and which immediately followed another 15 minute seizure. What is the priority action for this patient? a. Administer a dose of levetiracetam now and repeat in 10 minutes b. Administer lorazepam and monitor cardiorespiratory status c. Administer phenytoin and phenobarbital along with oxygen d. Admit the patient to the hospital for a diagnostic work up This patient has status epilepticus, which should be treated with benzodiazepines and close monitoring of airway, breathing, and circulation. The other interventions are not appropriate for acute seizure management.REF: Initial Stabilization and Management of Acute Seizures 2. A patient with a seizure disorder has seizures which begin with eye twitching and occasionally visual hallucinations. Which site in the brain is the seizure focus? a. Frontal b. Occipital c. Parietal d. Temporal Occipital sites causing complex partial seizures will have visual auras that may begin with eye twitching and visual hallucinations. Frontal sites cause dizziness or fear. Parietal sites cause sensory changes, such as numbness, tingling, or pain. Temporal sites cause epigastric and déjà vu sensations.REF: Table 201-1: Clinical Manifestations of Complex Partial Seizures 3. Which drug is used to treat patients with focal epilepsy and complex partial seizures? a. Carbamazepine b. Ethosuximide c. Lamotrigine d. Topiramate Carbamazepine is used for focal and complex partial seizures. Ethosuximide is useful for petit mal seizures in children. Lamotrigine has a wide range of effectiveness, but has an increased risk for Stevens-Johnson syndrome. Topiramate is not a first-line drug because of cognitive side effects.REF: Pharmacologic Management Chapter 202: Trigeminal Neuralgia Test Bank Multiple Choice 1. A patient reports paroxysms of burning, shock-like pain on both sides of the face usually triggered by chewing or talking. The provider suspects trigeminal neuralgia. Based on these presenting symptoms, what testing is indicated? a. Autoimmune laboratory panel b. Inflammatory markers c. Magnetic resonance imaging d. Plain radiographs Trigeminal neuralgia is a clinical diagnosis. Pain on both sides of the face raises a suspicion for multiple sclerosis and MRI is done to corroborate the presence of MS. Autoimmune laboratory pane is performed if alternative diagnoses are suspected. Inflammatory markers are not diagnostic. Plain radiographs are not indicated.REF: Clinical Presentation/Diagnostics 2. A patient with trigeminal neuralgia has tried several medication regimens to control pain without success. What is the next step in management for this condition? a. Consultation with a psychiatrist b. Education about alternative treatments c. Recommending a pain center d. Referral to a neurosurgeon Referral to a neurosurgeon is indicated after medical therapies have been exhausted. The other options may be included in long-term care, but a neurosurgery referral is warranted.REF: Indications for Referral or Hospitalization 3. A patient is diagnosed with trigeminal neuralgia and reports having paroxysms several times each day. What is the initial treatment for this patient? a. A combination of baclofen, lamotrigine, and phenytoin b. A high dose of carbamazepine with subsequent titration downward c. Botox injections or intranasal lidocaine as needed d. Low doses of anticonvulsants with gradual increase as needed Anticonvulsants are first-line treatments for trigeminal neuralgia – carbamazepine is started at the maximum therapeutic dose and titrated down to the lowest effective dose. Combination drug therapy is begun if the initial treatment is not effective or if the single drug regimen has intolerable side effects. Botox injections and intranasal lidocaine are used as adjuncts to anticonvulsants for acute pain relief.REF: Management Chapter 203: Intracranial Tumors Test Bank Multiple Choice 1. A patient develops a gait disorder and the patient’s spouse reports noticing recent personality changes. The provider suspects a brain lesion. Which evaluation is especially important in the initial physical examination? a. Assessment of peripheral reflexes b. Evaluation of speech c. Examination of the optic fundi d. Testing for memory loss Gait disorders and personality changes are more typical presentations with non-focal lesions. Examination of the optic fundi for papilledema may be the only finding to indicate increased intracranial pressure. The other assessments help determine focal involvement.REF: Clinical Presentation/Physical Examination 2. Which is the preferred treatment for primary brain tumors? a. Chemotherapy b. Palliative care c. Radiation therapy d. Surgical resection Surgical resection is the most effective treatment for brain tumors. Chemotherapy is limited in effectiveness because of difficulty crossing the blood-brain barrier. Radiation therapy is used as a primary, adjuvant, or palliative therapy. Palliative care is not the preferred treatment; many patients with brain tumors live for many years.REF: Management Chapter 204: Acromegaly Test Bank Multiple Choice 1. A patient has IGF-1 screening showing age- and gender-matched elevation and the provider orders a fasting oral glucose tolerance test (OGTT). The patient’s GH level drops to 1.1 ng/mL 120 minutes after the oral glucose is given. What will the provider conclude about these results? a. Acromegaly is certain b. Acromegaly is excluded c. Acromegaly is likely d. Acromegaly is possible Acromegaly may be diagnosed when an OGTT suppresses GH to less than 1.0 mg/mL, but studies have shown that failure to suppress GH in the presence of elevated IGF-1 does not rule out acromegaly, so the diagnosis is still possible.REF: Diagnostics 2. A patient with sleep apnea is noted to have a large tongue and uvula along with deepening of the voice. What will the primary care provider do initially to evaluate these findings? a. Obtain an insulin- like growth factor-1 level b. Order a random serum growth hormone level c. Recommend an orthopedic consult for bone age evaluation d. Refer the patient to an otolaryngologist The IGF-1 level is a good screening test when acromegaly is suspected. This patient has symptoms characteristic of acromegaly. Referral to an ENT is not the first step in evaluation of symptoms. Random serum GH levels are not useful in diagnosis because of the pulsatile nature of GH secretion. Bone age evaluation is not indicated.REF: Clinical Presentation/Diagnostics Chapter 205: Adrenal Gland Disorders Test Bank Multiple Choice 1. A patient has rapid weight gain, amenorrhea without pregnancy, and mild hypertension. Once confirmatory tests are performed, what is a possible treatment for this patient? a. Antihypertensive therapy b. Mineralocorticoid replacement c. Oral hydrocortisone d. Pituitary tumor resection This patient has symptoms of Cushing’s syndrome. When indicated, pituitary tumor resection is performed as the first choice. Antihypertensive therapy is initiated in patients with pheochromocytoma. Mineralocorticoids and glucocorticoids are given to patients with Addison’s disease.REF: Physical Examination/Management 2. A patient has new-onset hypertension with a systolic blood pressure of 180 mm Hg. Which test will the provider order to diagnose this patient? a. ACTH suppression testing b. Adrenal antibody tests c. Cortisol excretion studies d. Fractionated metanephrine levels Patients with pheochromocytoma may present with new-onset hypertension with systolic pressure >170 mm Hg. Fractionated metanephrine will be elevated when the diagnosis is confirmed. ACTH suppression testing and cortisol excretion studies are performed to diagnose Cushing’s syndrome. Adrenal antibody tests are performed as part of the evaluation for Addison’s disease.REF: Physical Examination/Diagnostics 3. A patient has unexplained weight loss and the provider notes increased skin pigmentation on light-exposed skin folds along with darkened palmar creases. Which laboratory tests will the provider order? Select all that apply. a. Serum ACTH b. Serum cortisol c. Serum electrolytes d. TB skin testing e. Urine cortisol , C, D This patient has symptoms of Addison’s disease. Serum ACTH will be elevated in patients with Addison’s disease. Hyponatremia and hyperkalemia may occur and are sometimes the initial finding. TB skin testing is done to exclude tuberculosis. Serum and urine cortisol levels are evaluated with Cushing’s syndrome is suspected.REF: Physical Examination/Diagnostics Chapter 206: Diabetes Mellitus Test Bank Multiple Choice 1. A patient who has diabetes has a blood pressure of 140/90 mm Hg and albuminuria. Which initial action by the primary care provider is indicated for management of this patient? a. Consulting with a nephrologist b. Limiting protein intake c. Prescribing an antihypertensive medication d. Referring to an ophthalmologist Patients with diabetes who have elevated blood pressure and reduced renal function should be referred to a nephrologist. Limiting protein intake and giving an antihypertensive medication may be recommended, but evaluation by a nephrologist is essential. Ophthalmology referral will be made as well to assess concurrent ocular damage.REF: Management/Microvascular Complications 2. A patient who is obese has recurrent urinary tract infections and reports feeling tired most of the time. What initial diagnostic test will the provider order in the clinic at this visit? a. C-peptide level b. Hemoglobin A1C c. Random serum glucose d. Thyroid studies HbA1C, along with fasting plasma glucose or a 2-hour plasma glucose during an OGTT are diagnostic of diabetes. This patient is probably not fasting, so a glucose level will not be helpful. C-peptide levels help to distinguish type 1 from type 2 diabetes and may be performed after a diagnosis of diabetes is made and if there is uncertainty about the cause. Thyroid studies are helpful in evaluating comorbidity.REF: Clinical Presentation/Diagnostics 3. A patient recently diagnosed with type 1 diabetes mellitus is in clinic for a follow-up evaluation. The provider notes that the patient appears confused and irritable and is sweating and shaking. What intervention will the provider expect to perform once the point of care blood glucose level is known? a. Dipstick urinalysis for ketones b. Giving a rapid-acting carbohydrate c. Injection of rapid-acting insulin d. Performing a hemoglobin A1C This patient has signs of hypoglycemia, so a rapid-acting carbohydrate should be given once this is confirmed. Assessing for ketones is done if the patient is hyperglycemic, as is insulin administration. Hemoglobin A1C gives information about long-term and not immediate glucose control.REF: Table 206-5: Hypoglycemia 4. A patient with type 2 diabetes mellitus becomes insulin dependent after a year of therapy with oral diabetes medications. When explaining this change in therapy, the provider will tell the patient: a. it is necessary because the patient cannot comply with the previous regimen. b. that strict diet and exercise measures may be relaxed with insulin therapy. c. the use of insulin therapy may be temporary. d. this is because of the natural progression of the disease. Even after several years of therapy for type 2 DM well controlled with oral diabetic medications, diet, and exercise, the natural progression of the disease may require patients to become insulin dependent. Patients must understand that this does not represent failure on their part. Adding insulin may cause weight gain, so continuing lifestyle measures is essential. The addition of insulin is not temporary.REF: Management/Type 2 Diabetes Chapter 207: Hirsutism Test Bank Multiple Choice 1. A young adult woman is unable to conceive after trying to get pregnant for over 6 months. The woman reports having had irregular periods since the onset of menarche. The provider notes that the woman is overweight, has acanthosis nigricans, and an excess hair distribution. What does the provider suspect as the most likely primary cause of these symptoms? a. Congenital adrenal hyperplasia b. Cushing’s syndrome c. Polycystic ovarian syndrome d. Type 2 diabetes PCOS is the most likely cause of oligo- or amenorrhea, so this is the most likely cause. The other conditions are possible, but less likely.REF: Polycystic Ovarian Syndrome 2. A woman who has hirsutism with acne, and oligomenorrhea will most likely be treated with which medication to control these symptoms? a. Finasteride b. Levonorgestrel c. Norgestimate d. Spironolactone Norgestimate is a progestin with low androgenic activity and is used to suppress testosterone and control symptoms. Finasteride, which decreases the peripheral conversion of testosterone to DHT is not approved for this use. Levonorgestrel is an androgenic OCP and should be avoided. Spironolactone is a second-line medication approved for this purpose.REF: Management 3. An obese adolescent female patient reports irregular periods and excessive acne. The provider notes an increased amount of hair on her upper back, shoulders, and upper abdomen. What will the provider do, based on these findings? a. Consider treatment with oral contraceptive pills b. Counsel her about diet, exercise, and weight loss c. Recommend cosmetic laser hair removal d. Refer to an endocrinologist for evaluation All patients with suspected hirsutism should be referred to a specialist to determine the cause. OCPs, lifestyle changes, and cosmetic treatments may be part of the treatment, but the underlying causes must be determined first to ensure that a life-threatening condition is not present.REF: Polycystic Ovarian Syndrome Chapter 208: Hypercalcemia and Hypocalcemia Test Bank Multiple Choice 1. A patient is in the emergency department with confusion and fatigue and a corrected serum calcium concentration is 10.8 mg/dL. What is the initial treatment for this patient prior to admission to the inpatient unit? a. Administration of furosemide b. Correction of potassium and magnesium levels c. Parenteral salmon calcitonin d. Rapid administration of intravenous normal saline To help the kidneys excrete calcium, intravenous normal saline should be given initially. Furosemide may not be effective as once thought and is used less often today. Correction of other electrolytes may be done when these imbalances are assessed. Parenteral salmon calcitonin may be used later to enhance calcium losses.REF: Hypercalcemia/Management 2. A patient carpal spasm when a blood pressure cuff is inflated. Which diagnostic testing will the provider consider to evaluate the cause of this finding? a. Calcitriol level b. C-reactive protein c. Magnesium and vitamin D d. Protein electrophoresis The Trousseau’s sign indicates neuromuscular irritability, which occurs with hypocalcemia. Because hypomagnesemia and vitamin D deficiency may cause hypocalcemia, these should be evaluated to help determine a cause. Calcitriol levels are used to assess hypercalcemia. Inflammatory markers are not indicated. Protein electrophoresis is used in the evaluation of hypercalcemia.REF: Hypocalcemia/Physical Examination/Diagnostics Hypercalcemia/Management 3. A patient has low serum calcium associated with low serum albumin. What is the recommended treatment for this patient? a. Calcium supplementation only b. Correction of other serum electrolytes c. Thiazide diuretics and sodium restriction d. Vitamin D and calcium supplementation Patients with hypocalcemia associated with hypoalbuminemia do not require calcium replacement. Serum pH, potassium, magnesium, and phosphorus levels should be monitored and corrected if needed. Thiazide diuretics with sodium restriction may be used to lower urinary calcium excretion to allow lower dosing of calcium and vitamin D when these are given.REF: Hypocalcemia/Management Chapter 209: Hyperkalemia and Hypokalemia Test Bank Multiple Choice 1. A patient with normal renal function has a potassium level of 6.0 mEq/L. Which underlying cause is possible in this patient? a. Adrenocortical deficiency b. Alcoholism c. Hypertension d. Malabsorption syndrome Hyperkalemia without underlying renal disorder may be caused by Addison’s disease, which is an adrenocortical deficiency. Alcoholism, hypertension, and malabsorption syndromes all contribute to hypokalemia.REF: Hyperkalemia 2. A hospitalized patient with renal failure is accidently given parenteral potassium and has a potassium level of 7.0 mEq/L. An ECG reveals a normal QRS interval. What is the initial recommended treatment for this patient? a. Calcium chloride b. Insulin and glucose infusion c. Sodium bicarbonate d. Sodium polystyrene sulfate Patients with severe hyperkalemia should have IV administration of glucose and insulin to lower potassium levels quickly. If life-threatening sequelae, such as a widening QRS interval, are present, calcium chloride is given. Sodium bicarbonate is occasionally used, but should be used cautiously to prevent metabolic alkalosis. Sodium polystyrene sulfate is used when oral medications may be given.REF: Acute Hyperkalemia 3. A patient has a serum potassium level of 3 mEq/L and a normal blood pressure. Which test should be performed initially to assist with the differential diagnosis? a. Plasma aldosterone b. Plasma renin activity c. Serum bicarbonate d. Serum magnesium In patients with hypokalemia with normal blood pressure, serum bicarbonate should be assessed to evaluate for diabetic ketoacidosis, metabolic acidosis, or renal tubular acidosis. If bicarbonate is normal, the magnesium level may be assessed. Plasma aldosterone and renin activity are assessed in patients with hypokalemia who are hypertensive.REF: Hypokalemia Chapter 210: Hypernatremia and Hyponatremia Test Bank Multiple Choice 1. A patient has euvolemic hyponatremia secondary to chronic syndrome of inappropriate antidiuretic hormone (SIADH) and is hospitalized for fluid replacement. When preparing to discharge the patient home, what will be included in teaching? a. Limiting dietary protein intake b. Limiting fluids to 500 mL/day for several days c. Restriction of sodium intake d. The importance of adherence to vaptan therapy Patients with chronic hypovolemia secondary to SIADH require fluid restriction for several days. Sodium and protein are not restricted. Vaptan therapy is started for those whose serum sodium fails to normalize in 24 to 48 hours.REF: Euvolemic Hyponatremia/Syndrome of Inappropriate Antidiuretic Hormone 2. An elderly patient who is taking a thiazide diuretic has been ill with nausea and vomiting and is brought to the emergency department for evaluation. An assessment reveals oliguria, hypotension, and tachycardia and serum sodium is 118 mEq/L. What is the treatment? a. A single infusion of hypertonic saline b. Addition of spironolactone c. Emergency volume repletion with 3% NaCl. d. Fluid and dietary sodium restriction This patient has hypovolemic hyponatremia with a sodium less than 120 mEq/L and requires fluid resuscitation with 3% NaCl. Diuretics and fluid restriction are part of treatment for hypervolemic hyponatremia.REF: Hyponatremia/Management 3. A high school athlete is brought to the emergency department after collapsing during outdoor practice on a hot day. The patient is weak, irritable, and confused. Serum sodium is 152 mEq/L and has dry mucous membranes and tachycardia. What is the initial approach to rehydration in this patient? a. Hypotonic intravenous fluid replacement b. Intravenous fluid resuscitation with an isotonic solution c. Loop diuretics and hypotonic intravenous fluids d. Oral water replacement This patient is dehydrated and has hypernatremia because of heat exposure and sweating. Because the patient is confused, oral fluid replacement is not recommended, although it is the safest in cognitively intact patients who are able to swallow safely. The initial fluids should correct the hypovolemia and isotonic solutions such as normal saline (0.9%) or Ringer’s lactate are given. Hypotonic fluids are then given once vital signs and urine output have normalized in patients with hypernatremia caused by fluid loss. Loop diuretics are added for patients who have hypernatremia caused by sodium gain.REF: Hypernatremia/Management Chapter 211: Lipid Disorders Test Bank Multiple Choice 1. A patient with type 2 diabetes has a low-density lipoprotein (LDL) level of 110 gm/dL. What is recommended to manage this patient? a. Dietary and lifestyle changes to modify risk b. Initial treatment with a low intensity statin medication c. Prescription of a moderate or high intensity statin d. Statin therapy until the LDL level is below 75 mg/dL This patient is in one of the four groups of patients identified in current guidelines as one who would benefit from statin therapy because of type 2 diabetes. A moderate to high intensity statin should be prescribed. Statins will be used in conjunction with dietary and lifestyle changes, but these treatments alone do not reduce risk in this patient. Titration of statins is not recommended and goal levels are no longer part of the protocol.REF: Definition and Epidemiology 2. When using the 2013 ACC/AHA “Guideline on the Assessment of Cardiovascular Risk” to treat patients with hyperlipidemia, the practitioner understands that it provides information about: a. goals for treatment for low-density lipoprotein levels. b. how to titrate statin drugs to achieve goal levels. c. use of non-statin therapy for primary prevention. d. which patients will benefit from statin therapy. The 2013 guidelines identify four groups of patients who will benefit from statin therapy to lower LDL. The guidelines do not identify goal levels for treatment, do not recommend titration of statin drugs to achieve results, and do not recommend non-statin therapies for primary prevention.REF: Definition and Epidemiology/Management 3. A patient who is taking a statin drug to treat dyslipidemia has begun a diet and exercise program. The patient reports new onset of muscle pain several weeks after beginning therapy. What is the initial action by the provider? a. Discontinue the statin drug immediately b. Obtain a creatine kinase level c. Prescribe acetaminophen or ibuprofen d. Recommend reducing exercise intensity A potential serious side effect of statin drugs is drug-induced myopathy. Patients who report new-onset muscle pain should have creatine kinase levels evaluated. If this is elevated, the drug should be stopped and renal function should be evaluated. It is not safe to assume that the muscle pain is related to the exercise until CK levels are determined.REF: Pharmacotherapy Chapter 212: Metabolic Syndrome Test Bank Multiple Choice 1. What is important about increased PAI-1 levels in patients with metabolic syndrome? a. They cause increased insulin resistance. b. They increase the risk of arterial thrombosis. c. They lower the risk of hypertension. d. They predispose patients to dyslipidemia. Increased PAI-1 levels increase the risk of thrombosis. They are correlated, but do not cause, insulin resistance and do not affect the relative risk of hypertension or dyslipidemia.REF: Pathophysiology/Prothrombotic State 2. Which medication given for patients with metabolic syndrome helps to lower PAI-1 levels? a. Aspirin b. Atorvastatin c. Metformin d. Niacin Metformin is given to reduce hyperinsulinemia and lower insulin resistance, but also lowers plasma PAI-1 levels. Aspirin is given to reduce MI risk. Atorvastatin helps with dyslipidemia. Niacin may be given to lower triglycerides.REF: Management 3. Which findings are part of the 2009 diagnostic criteria for metabolic syndrome? Select all that apply. a. Decreased plasminogen activator inhibitor 1 levels b. Elevated waist circumference c. Fasting plasma glucose ≧100 mg/dL d. HDL cholesterol ≧45 mg/dL e. Triglycerides ≧150 mg/dL , D, E The current criteria for diagnosing metabolic syndrome includes increased waist circumference, elevated fasting plasma glucose, and elevated triglycerides. According to these criteria, patients will have HDL levels <40 mg/dL. The old criteria included elevated plasminogen activator inhibitor 1 levels.REF: Definition and Epidemiology Chapter 213: Parathyroid Gland Disorders Test Bank Multiple Choice 1. A 40-year-old patient with primary hyperparathyroidism has increased serum calcium 0.5 mg/dL above normal without signs of nephrolithiasis. What is the recommended treatment for this patient? a. Annual monitoring of calcium, creatinine, and bone density b. Avoidance of weight-bearing exercises c. Decreasing calcium and vitamin D intake until values normal d. Parathyroidectomy Medical management of primary hyperparathyroidism involves close monitoring of serum calcium and creatinine and bone density screenings. Weight-bearing exercises should be encouraged and vitamin D and calcium intake should be adequate, not decreased. This patient does not meet criteria for parathyroidectomy because of age less than 50 years and serum calcium less than 1 mg/dL above the upper limit of normal.REF: Management 2. Which laboratory values representing parathyroid hormone (PTH) and serum calcium are consistent with a diagnosis of primary hyperparathyroidism? a. Appropriately high PTH along with hypocalcemia b. Appropriately increased PTH and low or normal serum calcium c. Inappropriate secretion of PTH along with hypercalcemia d. Prolonged inappropriate secretion of PTH with subsequent hypercalcemia Primary hyperparathyroidism is characterized by the inappropriate secretion of PTH in the setting of hypercalcemia. Appropriately high PTH with hypocalcemia characterizes hypoparathyroidism. An appropriately increased secretion of PTH with low or normal serum calcium is characteristic of secondary hyperparathyroidism. Prolonged inappropriate secretion of PTH in which hypercalcemia develops is tertiary hyperparathyroidism.REF: Definition and Epidemiology 3. Which findings are symptoms of hyperparathyroidism? Select all that apply. a. Chvostek’s sign b. Cognitive impairment c. Left ventricular hypertrophy d. Perioral paresthesias e. Renal calculi , C, E Cognitive impairment, left ventricular hypertrophy, and renal calculi all occur with hyperparathyroidism. Chvostek’s sign and perioral paresthesias occur with hypoparathyroidism.REF: Clinical Presentation Chapter 214: Thyroid Disorders Test Bank Multiple Choice 1. Which thyroid stimulating hormone (TSH) level indicates hyperthyroidism? a. 0.2 uIU/L b. 0.4 uIU/L c. 2.4 uIU/L d. 4.2 uIU/L A TSH less than 0.3 uIU/L indicates hyperthyroid; greater than 4.0 uIU/L indicates hypothyroid, and between 0.3 to 4.0 uIU/L indicates euthyroid.REF : Thyroid Function Tests 2. A 20-year-old female patient with tachycardia and weight loss but no optic symptoms has the following laboratory values: decreased TSH, increased T3, and increased T4 and free T4. A pregnancy test is negative. What is the initial treatment for this patient? a. Beta blocker medications b. Radioiodine therapy c. Surgical resection of the thyroid gland d. Thionamide therapy Beta blockers should be initiated for patients with Graves’ disease to alleviate the alpha- adrenergic symptoms of the hyperthyroidism. Radioiodine therapy is used for patients with Graves’ ophthalmopathy. Surgical resection is performed for pregnant women who cannot be managed with thioamides or for patients who refuse radioiodine therapy. Thioamide therapy is recommended for patients younger than 20 years old, pregnant women, those with a high likelihood of remission, and those with active Graves’ Orbitopathy.REF: Management/Graves’ Disease 3. A postpartum woman develops fatigue, weight gain, and constipation. Laboratory values reveal elevated TSH and decreased T3 and T4 levels. What will the provider tell this patient? a. A thyroidectomy will be necessary. b. She should be referred to an endocrinologist. c. She will need lifelong medication. d. This condition may be transient. Postpartum hypothyroidism may be a transient condition and does not require surgical intervention, referral to a specialist, or lifelong medication unless it proves to be long-standing or refractory to treatment.REF: Hypothyroidism/Management 4. A patient has thyroid nodules and the provider suspects thyroid cancer. To evaluate thyroid nodules for potential malignancy, which test is performed? a. Radionucleotide imaging b. Serum calcitonin c. Serum TSH level d. Thyroid ultrasound Thyroid ultrasound evaluation should be performed for all patients with known thyroid nodules; high-resolution sonography can clearly distinguish between solid and cystic components. Radionucleotide imaging is not specific; many cold nodules are benign. The routine measurement of serum calcitonin levels is not useful or cost-effective. TSH levels are not specific to malignancy.REF: Diagnostics and Differential Diagnosis Chapter 215: Ankylosing Spondylitis and Related Disorders Test Bank Multiple Choice 1. A patient is treated for a urinary tract infection and, 3 weeks later, presents with pain and swelling of one knee and in one hand, along with inflammation in both eyes. What will the provider suspect as the cause of these symptoms? a. Ankylosing spondylitis b. Infectious arthritis c. Psoriatic arthritis d. Reactive arthritis Reactive arthritis can cause arthritis, urethritis, and inflammation of the eyes 1 to 4 weeks after a prior infection. Ankylosing spondylitis generally presents with lower back inflammation. Psoriatic arthritis is associated with psoriasis. Reactive arthritis is not related to infection in the involved joints.REF: Reactive Arthritis/Clinical Presentation and Physical Examination 2. A patient is diagnosed with ankylosing spondylitis and begins taking a COX-2 inhibitor with minimal pain and inflammation relief. What will the provider order initially to manage this patient’s symptoms? a. A trial of sulfasalazine and methotrexate b. Biologic anti-tumor necrosis factor agents c. Changing to a COX-1 inhibitor medication d. Corticosteroid injections every three months NSAIDs have been shown to reduce pain and stiffness and reduce progression of structural damage if administered continuously. Patients should try at least two NSAIDs before other medications are attempted. Sulfasalazine and methotrexate have not been shown to be significantly effective for axial disease. Biologic anti-tumor necrosis factor medications are given only after failure of two NSAIDs. Corticosteroid injections are not indicated.REF: Management 3. A patient reports a history of recurrent lower back pain for 6 months. The patient describes the pain as a deep ache and stiffness that is worse upon awakening and improves after walking. Which findings will the examiner elicit to help make a clinical diagnosis of ankylosing spondylitis? Select all that apply. a. Assessment of the degree of lumbar lordosis b. Evaluation of lateral thoracic spine flexion c. Measurement of chest expansion d. Noting the degree of cervical kyphosis e. Observation for scapular asymmetry , B, C Examination of the spine will show loss of the normal lumbar lordosis, decreased thoracic spine flexion, and diminished chest expansion. Cervical kyphosis is not assessed. Scapular asymmetry evaluates for scoliosis.REF: Clinical Presentation/Physical Examination Chapter 216: Polymyalgia Rheumatica and Giant Cell Arteritis Test Bank Multiple Choice 1. A 60-year-old patient reports new onset of bilateral shoulder pain with morning stiffness lasting approximately one hour. Which will be included in initial diagnostic testing for this patient? Select all that apply. a. Antinuclear antibodies b. ESR and CRP c. Liver function tests d. Protein electrophoresis e. Serum calcitonin , C, D ESR, CRP, and protein electrophoresis are included in the initial diagnostic workup when polymyalgia rheumatica is suspected. ANA testing is not specific for this disorder. Serum calcitonin is not indicated.REF: Diagnostics 2. A patient who is taking prednisolone 20 mg daily to treat polymyalgia rheumatica, reports blurred vision. What will the provider do? a. Discontinue the medication b. Increase the prednisolone dose to 60 mg daily c. Prescribe NSAIDs to treat the inflammation d. Refer to a rheumatologist immediately Sudden vision loss, diplopia, and other visual disturbances may indicate GCA and requires immediate referral to rheumatology. The primary provider should not change the medication regimen without a consult.REF: Giant Cell Arteritis/Clinical Presentation 3. A patient is diagnosed with polymyalgia rheumatica with giant cell arteritis. Which dose of prednisolone will be given initially? a. 15 mg daily b. 20 mg daily c. 30 mg daily d. 60 mg daily Although the usual starting dose to treat PMR is 15 to 20 mg daily, a higher dose of 60 mg daily is used when there is evidence of concomitant giant cell arteritis.REF: Management Chapter 217: Raynaud's Phenomenon Test Bank Multiple Choice 1. A provider performs a nail fold capillaroscopy on a patient who reports marked color changes of both hands with cold exposure and notes tortuous and dilated capillary loops. This finding is consistent with a. polymyositis. b. primary Raynaud’s phenomena. c. scleroderma. d. secondary Raynaud’s phenomena. Microvascular abnormalities like tortuous of dilated capillary loops are observed in secondary Raynaud’s phenomena and capillaroscopy is used to differentiate primary from secondary Raynaud’s. These findings are not present with polymyositis or scleroderma.REF: Clinical Presentation/Physical Examination 2. A patient who has secondary Raynaud’s phenomena with severe digital ischemia. Which treatment is indicated for this patient? a. Ginkgo biloba b. Intravenous prostaglandin E1 c. Oral nifedipine d. Sildenafil as needed Intravenous prostaglandin E1 is reserved for patients with secondary Raynaud’s phenomenon who have severe digital ischemia. Ginkgo biloba is associated with adverse effects and has not been shown to be effective. Nifedipine is used to prevent vasospasm in milder cases. Sildenafil may be used as a vasodilator in milder cases.REF: Management Chapter 218: Rheumatoid Arthritis Test Bank Multiple Choice 1. Which are symptoms of rheumatoid arthritis that distinguish it from osteoarthritis? Select all that apply. a. Extra-articular inflammatory signs b. History of injury to affected joints c. Morning stiffness of at least one hour d. Symmetric tender, swollen joints e. Unilateral joint involvement , C, D The clinical presentation of RA includes extra-articular symptoms, morning stiffness lasting at least one hour, and symmetric, bilateral joint involvement. OA often has a history of previous injury and is usually asymmetric and may be unilateral.REF: Clinical Presentation/Differential Diagnosis 2. A patient is diagnosed with rheumatoid arthritis after a review of systems, confirmatory lab tests, and synovial fluid analysis. What will the provide order initially to treat this patient? a. Disease-modifying anti-rheumatic drugs b. Long-term glucocorticoid therapy c. Non-pharmacological treatments d. Nonsteroidal anti-inflammatory drugs Treatment with DMARDs should be initiated as soon as the diagnosis of RA is established in order to achieve disease modification. Long-term glucocorticoid therapy is not recommended because of adverse effects. NSAIDs are not first-line drugs and increase the risk of cardiac and renal complications. Non-pharmacological treatments are used as adjunctive and not first-line therapy.REF: Management 3. A patient has swelling and tenderness in the small joints of both hands and reports several weeks of malaise and fatigue. A RF test is negative. What will the primary care provider do next? a. Begin treatment with a biologic disease-modifying anti-rheumatic drug b. Order radiographic tests, a CBC, and acute-phase reactant levels c. Reassure the patient that the likelihood of rheumatoid arthritis is low d. Refer the patient to an orthopedic specialist for evaluation and treatment The patient has signs of RA; the RF test may be negative initially, but will become positive in 70% to 80% of patients. The provider’s next step is to order tests to confirm the diagnosis and to provide a baseline to monitor disease progress and response to treatment. DMARDs may be ordered when the disease is confirmed. The PCP may treat in consultation with a rheumatologist who will order medications and will refer the patient for physical therapy, occupational therapy and psychotherapy.REF: Diagnostics/Management Chapter 219: Systemic Lupus Erythematosus Test Bank Multiple Choice 1. A patient with systemic lupus erythematosus (SLE) has frequent symptoms and has been taking prednisone for each episode. The provider plans to start hydroxychloroquine and the patient asks why this medication is necessary. What will the provider tell this patient about this medication? a. It is effective in reducing disease flares and for tapering steroids. b. It is given in conjunction with steroids to improve outcomes. c. It lowers blood pressure and decreases the risk for renal disease. d. It prevents the need for biphosphenate therapy. Hydroxychloroquine is effective in managing musculoskeletal, cutaneous, and serosal manifestations of SLE and allows tapering of steroids and reduces disease flares. Cyclophosphamide is given with prednisone to improve renal outcomes. Hydroxychloroquine is not given for effects on blood pressure and kidneys. Calcium and vitamin D are given to prevent the need for biphosphenates.REF: Management/Table 219-1: Drugs Used in Treatment of Systemic Lupus Erythematosus 2. A patient with systemic lupus erythematosus (SLE) develops end-stage renal disease. Because of the underlying SLE, what treatment is recommended for this patient? a. Dialysis only b. Immunosuppressant therapy c. Kidney transplantation d. Palliative care Patients with SLE who develop renal failure may require dialysis and then kidney transplantation; most who undergo transplant do relatively well because of the immunosuppression given to prevent graft rejection. Immunosuppressant therapy is given for graft rejection and does not treat end-stage renal failure. Palliative care is not the only option for this patient.REF: Clinical Presentation and Physical Examination 3. Which laboratory tests may help distinguish systemic lupus erythematosus (SLE) from other systemic rheumatologic disorders? a. Antinuclear antibody titer b. C-reactive protein c. Rheumatoid factor d. Serum complement levels With SLE, complement levels may decrease because of the activation and deposition of immune complexes in tissues. The other tests are non-specific tests for inflammation and rheumatologic disorders.REF: Diagnostics Chapter 220: Vasculitis Test Bank Multiple Choice 1. Which is a distinctive finding in patients who have Churg-Strauss syndrome (CSS)? a. Elevated ESR and CRP b. HBV surface antigen c. Increased eosinophils d. Positive antinuclear antibodies Unique to CSS are large numbers of circulating and tissue-based eosinophils. ESR and CRP are non-specific markers of inflammation HBV surface antigen is often present in polyarteritis nodosa. ANA levels are present in many autoimmune diseases.REF: Classification of Vasculitic Syndromes 2. A patient has a palpable purpural rash. This finding is most consistent with a. small-vessel vasculitis. b. medium- vessel vasculitis. c. large-vessel vasculitis. d. central-vessel vasculitis. A palpable purpural rash is the most helpful physical examination finding of a small-vessel vasculitis.REF: Clinical Presentation and Physical Examination 3. A child has a high fever, bilateral conjunctivitis, and a desquamating rash and is presumed to have a vasculitic disease. What is the likely treatment for this child? a. Antibiotic therapy for 10 to 14 days b. Aspirin and intravenous immunoglobulin c. High-dose prednisolone therapy d. Immunosuppressant medications This patient has symptoms of Kawasaki disease. Because of the risk for coronary aneurysms and death, ASA and IVIG are indicated. Antibiotics, prednisolone, and immunosuppressants are not useful.REF: Clinical Presentation and Physical Examination Chapter 221: Barotrauma and Other Diving Injuries Test Bank Multiple Choice 1. A scuba diver reports persistent nosebleeds after a diving trip. What is the treatment for this condition based on this history? a. A period of bedrest b. Decongestant medications c. Recompression therapy d. Referral to an otolaryngologist Topical and systemic nasal decongestants may provide both relief and prophylaxis for divers predisposed to epistaxis. Bedrest is not indicated. Recompression therapy is not used for sinus barotrauma. Referral to an otolaryngologist is necessary when conservative treatments are not effective.REF: Sinus Barotrauma/Management 2. A patient is brought to an emergency department after a diving accident and is receiving inhaled 100% oxygen. This is given in order to a. enhance oxygen delivery to ischemic tissues. b. improve oxygen saturations. c. prevent the need for recompression therapy. d. reduce the risk of neurological symptoms. Breathing 100% oxygen increases the extraction of nitrogen from tissues and can enhance oxygen delivery to ischemic tissues. It is not given to improve oxygen saturations, because the oxygen level is not of concern. Patients will still need recompression therapy. Oxygen is not given to minimize neurological symptoms.REF: Barotrauma/Management 3. When evaluating a person who is interested in taking a scuba diving class, the practitioner will screen for which conditions? Select all that apply. a. Chronic sinusitis b. Diabetes mellitus c. Peptic ulcer disease d. Pressure equalizing ear tubes e. Recurrent urinary tract infections , B, D Diving is relatively contraindicated in any patient with a history of frequent ear infections or chronic sinus infections. Diabetes, if unstable, is a contraindication. Pressure equalizing tubes are absolute contraindications. Peptic ulcer disease and recurrent UTI are not contraindications.REF: Pre-dive Physical Examination and Diagnostics Chapter 222: Chronic Pain Test Bank Multiple Choice 1. A patient with chronic leg pain describes the pain as “stabbing” and “throbbing.” This is characteristic of which type of pain? a. Neuropathic pain b. Referred pain c. Somatic pain d. Visceral pain Somatic pain is caused by the activation of nociceptors in the peripheral tissues, including skin, bones, muscles, and soft tissue and is usually well-localized and characterized as stabbing, aching, or throbbing. Neuropathic pain occurs from injury to or disease of the nervous system and is described as burning, shooting, or tingling. Referred pain is a kind of visceral pain that is localized, but not attributable to the involved organ. Visceral pain is related to an organ and is often referred and poorly localized.REF: Pathophysiology 2. A patient is beginning treatment for chronic pain and is unable to tolerate nonsteroidal anti- inflammatory drugs. What will the provider prescribe for this patient? a. A mixed opiate product b. A pure opioid compound c. A referral for a nerve block procedure d. A selective serotonin reuptake inhibitor Using the three-step analgesic ladder, the provider should use step 1 medications that include NSAIDs, tricyclic antidepressants, selective serotonin reuptake inhibitors, or anticonvulsants. Since the patient cannot tolerate NSAIDs, an SSRI is an appropriate choice. The next step if these fail, is a mixed opioid product. The third step is a pure opioid product. If medication therapy fails, a referral for nerve block may be necessary.REF: Three-Step Analgesic Ladder 3. A patient who has chronic lower back pain reports increased difficulty sleeping unrelated to discomfort, along with a desire to quit working. What will the provider do? a. Ask the patient about addiction issues b. Consult with a social worker c. Increase the dosage of prescribed pain medications d. Order radiographic studies of the lower spine Patients who exhibit poor sleep and poor coping may be developing mental defeat as a result of chronic pain and should be evaluated and treated early for this to prevent further disability and improve functionality. Substance abuse may be a part of mental defeat and should be evaluated based on assessment findings. Unless the symptoms are related to pain, increasing the dose of analgesics and ordering diagnostic studies are not indicated.REF: Definition and Epidemiology/Management and Interdisciplinary Management Chapter 223: Fatigue Test Bank Multiple Choice 1. A patient is seen in the clinic with complaints of constant fatigue. The patient’s spouse reports that the patient moves and kicks the legs frequently during sleep. What treatment will the provider anticipate once a diagnosis of the underlying cause is confirmed? a. An anti-oxidant diet b. Cognitive behavioral therapy c. Iron and vitamin C supplements d. Melatonin daily at bedtime This patient most likely has restless leg syndrome which may result from low ferritin levels and which is treated with vitamin C and iron. Anti-oxidant diets and cognitive behavioral therapy are sometimes used to treat non-specific CFS. Melatonin has not been shown to be effective.REF: Management 2. Which are causes of physiologic fatigue? Select all that apply. a. Acute and chronic illness b. Excessive alcohol use c. Irregular sleep habits d. Medication side effects e. Morbid obesity , C, D Physiologic causes are those resulting from external influences and include poor sleep hygiene, substance abuse, and medication effects. Physical causes are those where fatigue is secondary to diseases or conditions.REF: Differential Diagnosis 3. A patient with poorly controlled diabetes mellitus has chronic fatigue symptoms. What is the most likely underlying cause of this patient’s fatigue? a. Calorie depletion b. Decreased metabolism c. Psychological distress d. Sleep apnea Patients with poorly controlled DM have significant fluid and calorie depletion causing fatigue. Patients with hypothyroidism have decreased metabolism leading to fatigue. Psychological distress causing fatigue is associated with malignant neoplasms of the blood. Sleep apnea causing fatigue is associated with morbid obesity.REF: Differential Diagnosis Chapter 224: Fever Test Bank Multiple Choice 1. A patient has a fever of unknown etiology and blood tests reveal elevated eosinophils. The patient has no history of asthma or allergies. What may be the cause of this fever? a. Animal bite b. Endocarditis c. Lymphoma d. Parasites Eosinophils classically suggest a parasitic infection, asthma, or allergy. They are not present with other conditions unless there is concurrent parasitic infection or underlying asthma or allergies.REF: Diagnostic Evaluation for a Patient with Fever without Clear Etiology 2. Which patients with fever should generally be treated with antipyretics? Select all that apply. a. Children under the age of 5 years b. Patients taking antibiotics to treat infection c. Patients with temperature greater than 41° C d. Patients with urinary tract infection e. Those with underlying cardiovascular disease , C, E Children under 5 years are more prone to febrile seizures. Patients with very high temperatures should be treated to prevent CNS damage. Patients with underlying cardiovascular disease should be treated to avoid excessive metabolic demands. It is not especially necessary to treat fever in patients with UTI or for those taking antibiotics.REF: Management 3. A patient reports daily, recurrent fever associated with sweating, chills, and facial flushing, along with recent weight loss. What may this type of fever indicate? a. An underlying disease caused by animal bites b. Fever related to an immunocompromised state c. Possible exposure to tropical diseases d. Tuberculosis or lymphoma Hectic fever, or recurring fever associated with weight loss, sweating, chills, and facial flushing is concerning for tuberculosis or lymphoma. Fever from animal bites or travel to tropical areas is diagnosed after a history of exposure.REF: Evaluation of a Patient with Fever without Clear Etiology Chapter 225: Immunodeficiency Test Bank Multiple Choice 1. A 6-month-old infant is suspected of having an immune deficiency disorder. Which diagnostic tests may be included to evaluate this patient? Select all that apply. a. Blood, urine, sputum, and wound cultures b. Delayed-type hypersensitivity skin testing c. ESR and CRP d. Metabolic profiles e. Serum electrolytes , C, D Cultures are obtained to determine causative organisms in patients with frequent infections. ESR and CRP are performed to assess whether an inflammatory response is present. Metabolic profiles are useful to identify underlying metabolic disease that may cause immunodeficiency. Delayed-type hypersensitivity skin testing is not useful in children under 1 year of age because even unaffected children this age have not developed an exposure history adequate enough to have a positive result. Serum electrolytes are not indicated.REF: Diagnostics 2. A patient who has recurrent pneumococcal pneumonia and exhibits prolonged bleeding, easy bruising, and eczema. Which immunodeficiency disorder is likely in this patient? a. DiGeorge syndrome b. Hyperimmunoglobulinemia E syndrome c. Severe combined immunodeficiency disease (SCID) d. Wiskott-Aldrich syndrome (WAS) Patients with WAS also have platelet maturation abnormalities, so will have signs associated thrombocytopenia. Patients with DiGeorge syndrome have dysmorphic facial features. Hyperimmunoglobulinemia E syndrome also has dysmorphic features. Children with SCID have devastating infections, since they have a completely non-functioning immune system.REF: Clinical Presentation 3. A child has a primary immunodeficiency and the parent asks the provider about vaccines. What will the provider tell this patient? a. Avoid all vaccines since immunizations can cause disease in this child b. Immunized with all recommended childhood vaccines to prevent serious disease c. Some vaccines are contraindicated in those with T-cell involvement only d. The child may need more vaccine boosters than other children Children with T-cell disorders should not receive live-virus vaccines, but children with humoral deficiency may be given the vaccine. Vaccines are important to help prevent disease and children with immunodeficiency should receive any vaccines that are safe for them. Not all vaccines are recommended, since live-virus vaccines can cause disease in certain children.REF: Indications for Referral Chapter 226: Lymphadenopathy Test Bank Multiple Choice 1. A child developed cervical lymphadenopathy after a scabies infestation. One node remains enlarged 6 months after the infestation, but has not increased in size. The physical examination reveals a non-tender, non-erythematous node. What will the provider tell the child’s parents? a. The child may need surgical intervention. b. The child should see a pediatric oncologist. c. The node will need to be biopsied. d. This node is most likely benign. A nodule lasting up to a year without change in size is likely to be benign, especially since the cause is known. Unless there is enlargement or infection, surgical intervention and biopsy are not indicated and the child does not need to be evaluated by an oncologist.REF: Differential Diagnosis 2. An adolescent patient comes to the primary care provider because of a swollen lymph node which is warm, tender, and rapidly enlarging. Which initial action will the provider take? a. Observe the node over a period of 3 to 4 weeks b. Obtain a complete blood count with differential c. Prescribe empiric antibiotics for 10 to 14 days d. Refer for an ultrasound and possible biopsy Because this patient has symptoms consistent with infection, a CBC should be ordered to evaluate this potential cause. Nodes without evident cause may be observed over a period of 3 to 4 weeks. Empiric antibiotics are not recommended. Unless the node is suspicious, a referral for US and biopsy should not be considered until the lymphadenopathy has persisted for more than one month.REF: Diagnostics 3. A 50-year-old patient presents with supraclavicular lymphadenopathy. Which action is correct? a. Consult with an oncologist for evaluation b. Perform testing for sexually transmitted infections c. Reassure the patient that this will resolve d. Treat empirically with an antibiotic In patients over 40 years old, supraclavicular lymphadenopathy is likely to be cancerous in 90% of cases, so an oncologist should be consulted. STI causes are not associated with supraclavicular lymphadenopathy. Because this is likely to be cancer, reassuring the patient is not appropriate. Empiric antibiotic therapy is not indicated.REF: Differential Diagnosis Chapter 227: Sleep Disorders Test Bank Multiple Choice 1. A patient is diagnosed with mild restless leg syndrome which occasionally interferes with sleep. Which initial treatment will be helpful? a. A CPAP devices b. A dopaminergic agonist c. Hot baths and exercise d. Supplemental iron Patients with mild restless leg syndrome (RLS) may benefit from massage, hot baths, exercise, and good sleep hygiene. CPAP is used for obstructive sleep apnea. Dopaminergic agonists are useful medications, but have a risk of rebound or augmentation of effects. Supplemental iron is used in patients with low ferritin levels.REF: Restless Leg Syndrome/Management 2. Which patient would benefit from a polysomnography evaluation to assess a potential sleep disorder? a. A child with enlarged tonsils who has daytime sleepiness b. A patient with GERD who has difficulty falling asleep c. A shift worker who has trouble adjusting to new schedules d. An elderly woman with osteoarthritis who has difficulty staying asleep The child with enlarged tonsils is likely to have obstructive sleep apnea and would benefit from polysomnography (PSG) to help diagnose this problem. The other patients have sleep disorders related to other conditions that interfere with comfort or circadian rhythms and would not benefit from PSG/REF: Diagnostics 3. A patient who has excessive daytime sleepiness tells the practitioner that he goes to bed and gets up at the same times each day but still wakes up tired. The spouse reports that the patient snores so much she has had to move to another bedroom. The patient is otherwise healthy and does not take any medications or drink alcohol. Which diagnostic test may be performed for this patient? a. Full overnight polysomnography (PSG) b. Multiple sleep latency test (MSLT) c. Overnight pulse oximetry d. Unattended out of center sleep testing (OCST) This patient has a high probability of OSA without significant comorbidities or use of medications that may cause central sleep apnea, so this test, which has more limited measures than a full PSG, may be performed. Full overnight PSG is used when the cause of sleep apnea is less certain to help determine whether there is a central cause. The multiple sleep latency test is used to test EDS symptoms. Overnight pulse oximetry is not sufficiently sensitive to be a reliable screening for sleep apnea.REF: Obstructive Sleep Apnea/Diagnostics Chapter 228: Unintended Weight Loss Test Bank Multiple Choice 1. What factors may contribute to weight loss from functional anorexia in older women? Select all that apply. a. Apathy b. Delayed gastric emptying c. Malabsorption d. Pain with elimination e. Urinary frequency , B, D Weight loss from functional anorexia may occur because of apathy, delayed gastric emptying, and pain with elimination, which are behavioral adaptations to unsatisfactory eating experiences. Decreased calorie absorption causing weight loss may be due to malabsorption and urinary frequency.REF: Pathophysiology 2. Which non-pharmacologic intervention may be of most benefit in frail elders to restore physical function and improve appetite? a. Calorie dense foods b. Exercise c. Increased protein d. Nutritional drinks Exercise may be the most beneficial intervention in frail elders because nutritional interventions are less reliable.REF: Management 3. An elderly woman has marked decrease in muscle strength without weight loss. Which condition does the provider suspect in this patient? a. Cachexia b. Kwashiorkor c. Marasmus d. Sarcopenia Sarcopenia is reduced muscle mass. Cachexia includes muscle wasting following weight and fat loss. Kwashiorkor is due to protein deficiency and marasmus is insufficient calories.REF: Pathophysiology Chapter 229: Emerging and Reemerging Infectious Diseases Test Bank Multiple Choice 1. Using molecular polymerase chain reaction (PCR) techniques, a hospitalist identifies the presence of human metapneumovirus in a child who has bronchiolitis. This disease is considered an emerging disease because a. it has become more virulent. b. it has lately been reactivated. c. it is becoming pandemic. d. it is only recently recognized. This virus has only recently been identified as being present in children with lower respiratory tract infections because of techniques allowing it to be identified and isolated. It is not considered emerging because of increased virulence, reactivation after a period of dormancy, or because it is becoming pandemic.REF: Human Metapneumovirus 2. What are risk factors for the increase in emerging and re-emerging infectious diseases? Select all that apply. a. Antibiotic use in animal feeds b. Counterfeit drug sales c. Decreased antibiotic use d. Exotic pet ownership e. Reforestation of farmlands , B, D, E Using antibiotics in animal feed has increased the incidence of drug-resistant organisms. Counterfeit drug sales in Southeast Asia have contributed to the emergence of malaria species resistant to certain therapies. Exotic pet ownership has introduced new pathogens to some parts of the world. Reforestation of farmlands has led to the re-emergence of deer herds and a subsequent increase in Lyme disease. A decrease in antibiotic use will lower the risk of antibiotic resistance.REF: Risk Factors Favoring Emergence of Pathogens 3. A patient plans to travel to western Africa and is concerned about contracting Ebola. What will the provider suggest to this patient? a. Avoid contact with infectious body fluids b. Obtain the vaccine prior to travel c. Wear a mask when venturing outdoors d. Wear clothing that covers the skin Ebola is transmitted from human to human via contact with infectious body fluids. There currently is no approved vaccine for persons traveling to Ebola regions. The disease is not transmitted by respiratory droplets, so wearing a mask while outdoors is not indicated. The disease is not spread by vectors such as mosquitoes, so protective clothing is not indicated.REF: Zoonosis Chapter 230: HIV Infection Test Bank Multiple Choice 1. A pregnant woman tests positive for HIV infection. What will the provider recommend? a. Consideration of termination of the pregnancy b. No treatment and caesarian section for delivery c. Treatment with highly active antiretroviral therapy d. Treatment with standard antiretroviral therapy An absolute indication for treatment with highly active antiretroviral therapy (HAART) is the treatment of a pregnant woman to prevent mother-to-child transmission. Recommended regimens have no known significant fetal toxicity and can reduce the risk of vertical transmission from approximately 25% to less than 2%, making elective caesarean section no longer indicated in treated pregnant women.REF: Management 2. A homeless patient who has HIV infection has been on antiretroviral therapy (ART) for 18 months and has had normal CD4 counts and viral loads for past year. What will the provider recommend? a. Allow for periods of time off from ART medications b. Begin monitoring viral load and CD4 counts every 6 to 12 months c. Consider beginning highly active antiretroviral therapy (HAART) d. Continue monitoring viral load and CD4 counts every 3 to 4 months In patients who are clinically well and highly adherent who have normal CD4 counts and viral loads, monitoring may begin at 6 month intervals and sometimes annually. Those with risk factors such as homelessness, however, must continue to be monitored every 3 to 4 months. ART medications should never be interrupted unless there are medical reasons for doing so. HAART is given only by clinicians with significant training and experience in its use to patients who meet specific criteria.REF: Management 3. Which patients with documented HIV infection may be classified has having acquired immunodeficiency syndrome (AIDS)? Select all that apply. a. A patient with a CD4 cell count of 150/mm3 b. A patient with a CD4 cell count of 400/mm3 c. A patient with contact with a partner who has AIDS d. A patient with esophageal candidiasis e. A patient with tuberculosis , D, E Patient with HIV infection are classified as having AIDS either when the CD4 cell count is <200/mm3, or if they have one of a broad spectrum of opportunistic infections, malignant neoplasms, and nonspecific syndromes. Patients with CD4 cell counts >200/mm3 and those living with partners who have AIDS are not classified as having AIDS.REF: Definition and Pathophysiology Chapter 231: Influenza Test Bank Multiple Choice 1. A 65-year-old patient who has not had an influenza vaccine is exposed to influenza and comes to the clinic the following day with fever and watery, red eyes. What will the provider do initially? a. Administer LAIV influenza vaccine b. Begin treatment with an antiviral medication c. Observe for improvement or worsening for 24 hours d. Perform a nasal swab for RT-PCR assay Samples to isolate the virus should be collected within 12 to 36 hours of onset of illness and this should be performed to confirm the disease. Administration of the LAIV influenza vaccine will not prevent symptoms in this patient, is not recommended in persons over 59 years of age, and is contraindicated when also giving antiviral medications. Antiviral drugs should be started within 48 hours of onset of illness and may be started empirically while waiting on cultures because this patient is higher risk than younger patients. Because identification of the virus and effectiveness of treatment are time-limited, it is not correct to watch and wait for symptoms to worsen.REF: Diagnostics/Management 2. The parent of a 4-month-old infant who has had an episode of bronchiolitis asks the provider if the infant may have an influenza vaccine. What will the provider tell this parent? a. The infant should be given prophylactic antiviral medications. b. The infant should have an influenza vaccine now with a booster in 1 month. c. The infant should have the live attenuated influenza vaccine (LAIV). d. The rest of the family and all close contacts should have the influenza vaccine. Infants are not given influenza vaccine until age 6 months. To protect infants younger than 6 months, it is important for other family members and close contacts to be vaccinated. LAIV is approved for use in children over age 2 years. Antiviral prophylaxis is not recommended.REF: Health Promotion and Prevention 3. A previously healthy patient develops influenza which is confirmed by RT-PCR testing and begins taking an antiviral medication. The next day, the patient reports increased fever and cough without respiratory distress. The patient’s lungs are clear and oxygen saturations are 97% on room air. What will the provider recommend? a. Admission to the hospital for treatment of complications b. Empiric antibiotics to treat a possible secondary infection c. Referral to a specialist for evaluation and treatment d. Symptomatic treatment with close follow up in clinic This patient does not have risk factors for serious complications and may be managed as an outpatient. Symptoms should begin to gradually improve a few days after the onset of symptoms. Because this patient is stable, watchful waiting with symptomatic care and close follow up is acceptable. It is not necessary to admit to the hospital, refer to a specialist, or begin antibiotic therapy at this time.REF: Indications for Referral or Hospitalization Chapter 232: Infectious Diarrhea Test Bank Multiple Choice 1. A patient has had mild acute diarrhea for 8 days. The patient is alert with normal vital signs and no abdominal discomfort, but appears mildly dehydrated. Which tests will the provider perform? Select all that apply. a. BUN and creatinine b. Complete blood count c. Serum electrolytes d. Stool for fecal leukocytes e. Stool for occult blood , B, C A CBC, serum electrolytes, BUN, and creatinine are standard tests for evaluation of electrolyte derangement and dehydration and should be performed in patients who appear dehydrated. Stool samples for fecal leukocytes and occult blood are taken for patients with high temperatures, bloody diarrhea, and abdominal pain.REF: Diagnostics 2. A patient who has recently traveled has acute diarrhea which began the day after returning home. What are recommended treatments for this type of diarrhea? Select all that apply. a. Ciprofloxacin for 3 days, twice daily b. Loperamide at bedtime and after each stool c. Oral fluid replacement d. Quinolones daily for 2 to 4 weeks e. Sulfamethoxazole twice daily for 5 days , B, C Ciprofloxacin may be given for 3 days for traveler’s diarrhea, as well as loperamide. Oral fluid replacement is recommended. Because of widespread antibiotic resistance to sulfamethoxazole and quinolones, these drugs are not recommended.REF: Traveler’s Diarrhea 3. A patient is experiencing small-volume, non-inflammatory stools. Which organisms may be suspected in this case? Select all that apply. a. Clostridium difficile b. Cryptosporidium c. Escherichia coli d. Giardia e. Shigella . C, D Small-volume, non-inflammatory stools occur with infections of the small intestine and are due to enteric viruses, enterotoxic bacteria, such as E. coli, and noninvasive parasites, such as Giardia and Cryptosporidium. Infections of the lower intestine are characterized by frequent, large- volume inflammatory diarrhea and C. difficile and Shigella are among the likely pathogens.REF: Definition Chapter 233: Infectious Mononucleosis Test Bank Multiple Choice 1. A patient with EBV-IM also has group A beta-hemolytic streptococcal pharyngitis and is being treated with amoxicillin. On the third day of treatment, the patient develops a rash. A urinalysis is normal. What does this indicate? a. A reaction to the amoxicillin b. A streptococcal rash c. Hematologic complications d. Hemolytic-uremic syndrome 80% to 100% of patients with IM who are taking amoxicillin will develop a rash. A streptococcal rash appears at the onset of symptoms, not 3 days after initiation of antibiotics. This rash does not indicate hematologic complications or hemolytic- uremic syndrome.REF: Complications 2. An adolescent patient who plays football in high school is diagnosed with EBV infectious mononucleosis and is noted to have splenomegaly. What will the provider recommend to this patient about returning to sports? a. Abdominal ultrasounds are recommended to determine safety. b. Corticosteroid therapy may help shorten the course of the disease. c. He may return to minimal contact practice in 2 to 3 weeks. d. It will be safe to play football in 3 to 4 weeks. Patients with splenomegaly should be encouraged to refrain from strenuous activity for 3 to 4 weeks to avoid the risk of splenic rupture. Serial US studies beginning at week 2 to 3 may be helpful in determining the risk of rupture. Corticosteroids have not been shown to reduce the severity or duration of symptoms. Strenuous activity is not recommended until 3 to 4 weeks; without an US, it is not possible to ensure absolute safety for sports.REF: Management 3. An adolescent patient has fever, pharyngitis, and cervical lymphadenopathy and has a negative group A beta-hemolytic throat culture. A complete blood count shows absolute lymphocytosis, but a heterophil antibody test is negative for Epstein-Barr virus (EBV). What will the provider tell the patient about the likelihood of infectious mononucleosis (IM)? a. It will be necessary to repeat the heterophil antibody test in a few weeks. b. Liver function tests will help to confirm a diagnosis of EBV-IM. c. The likelihood of EBV infectious mononucleosis is still high. d. This IM is most likely caused by a virus other than Epstein-Barr virus. Because heterophil antibodies may not reach detectable levels early in the disease, it is possible to have a negative result. This patient has symptoms and the suspicion for disease remains high. Repeat testing in 7 to 10 days will help confirm the diagnosis. A positive heterophil antibody test with absolute lymphocytosis is diagnostic of acute IM. Epstein-Barr nuclear antigen is measured 6 to 8 weeks after onset of symptoms to distinguish between acute and previous infection. LFTs may be elevated in patients with IM, but this is not diagnostic.REF: Diagnostics Chapter 234: Tick-Borne Illnesses Test Bank Multiple Choice 1. A patient presents with fever, severe headache, and rash and has a history of tick bite. Which tick-borne illness is suspected? a. Babesiosis b. Erlichiosis c. Lyme disease d. Rocky Mountain spotted fever The classic triad of fever, severe headache, and rash is consistent with Rocky Mountain spotted fever.REF: Rocky Mountain Spotted Fever/Clinical Presentation 2. A patient with mild symptoms of babesiosis is diagnosed with a positive PCR assay. What is the recommended treatment for this patient? a. Atovaquone and azithromycin for 7 to 10 days b. Clindamycin and quinine for 10 to 14 days c. Intravenous clindamycin and hospitalization d. Symptomatic therapy with observation Patients with mild to moderate symptoms and a positive PCR assay should be treated. Atovaquone plus azithromycin is the treatment of choice. Clindamycin and quinine are effective, but have more adverse effects. IV clindamycin is given for severe symptoms. Patients without positive assays who have mild symptoms may be observed.REF: Babesiosis/Management 3. A parent brings a child to clinic and reports pulling a tick off of the child after being outdoors that day. The parent is concerned that the child may have Lyme disease. What will the provider tell this parent? a. A laboratory test today will help identify the presence of the disease. b. Antibiotic prophylaxis is necessary to prevent development of symptoms. c. Transmission of the organism only occurs with prolonged attachment of the tick. d. Unless the child develops systemic symptoms, treatment is not indicated. To transmit the spirochete to humans, the tick must be attached for an extended period of time of 36 to 72 hours. Serologic testing early in the disease may not be helpful. Antibiotic prophylaxis is not recommended. Treatment may begin with the presence of a localized rash.REF: Lyme Disease/Clinical Presentation/Diagnostics/Management Chapter 235: Tuberculosis Test Bank Multiple Choice 1. A 25-year-old patient has a tuberculosis skin test which reveals an area of induration of 12 mm. The patient is a recent immigrant from Mexico and lives in a homeless shelter. What is the recommended treatment for this patient? a. Administer the BCG vaccine b. Begin INH preventive therapy c. Order INH and Rifampin d. Perform regular TB skin testing every few months Patients younger than 35 who have any risk factors for TB and with an area of induration ≥10 mm should be considered for INH preventive therapy. This patient is an immigrant from Mexico and lives in a homeless shelter, so TB preventive therapy is acceptable. BCG vaccine is not helpful. INH and Rifampin are used if patients develop symptoms or if there is antibiotic resistance.REF: Management 2. A provider is concerned that a young child may have latent tuberculosis infection (LTBI). Which test will be performed initially to screen for this infection? a. Chest radiograph b. Interferon gamma release assay c. Mantoux test d. Two-step TST The Mantoux test is the most cost-effective test to administer as an initial screen. Chest radiograph is not used to detect LTBI because there is no radiographic evidence with latent infection. The IGRA may be used, but is more costly and the sensitivity in young children has not been established. The two-step TST is not indicated.REF: Latent Tuberculosis Infection/Diagnostics 3. A patient who has HIV infection has a negative tuberculosis skin test with induration less than 10 mm. The provider learns that the patient lives with a person who has active tuberculosis. What is the next step in managing this patient? a. Begin empiric antibiotic therapy b. Order a chest radiograph c. Perform an interferon gamma release assay d. Refer to an infectious disease specialist Patients who are immunocompromised who have had contact with a person with infectious TB should have a chest radiograph. Until infection is established, empiric antibiotic therapy is not indicated in order to reduce the risk of antibiotic resistance. IGRA is not indicated. If radiograph results are positive, or if the diagnosis remains unclear, referral is indicated.REF: Management Chapter 236: West Nile Virus Test Bank Multiple Choice 1. A patient who reports traveling to an area where West Nile virus (WNV) is endemic presents with fever, arthralgia, and rash for the last 7 days. What initial testing is recommended to confirm a diagnosis of WNV? a. ELISA for CSF antibodies b. ELISA for serum IgM c. PCR assays of CSF d. PCR assays of serum Serologic testing is the most effective method to confirm clinical suspicion of WNV infection and ELISA for detection of IgM in serum at 6 to 8 days indicates recent infection. CSF may be tested, but is more invasive. PCR assays are low yield because of the transient nature of viremia in humans.REF: Diagnostics 2. A patient expresses concern about contracting West Nile virus (WNV) infection after a family member becomes ill with the disease. What will the provider tell this patient? a. Human hosts may become reservoirs for infection for WNV. b. Humans may transmit the virus to mosquitoes after a bite. c. Humans must be bitten by a mosquito infected by a bird. d. Human-to-human transmission is possible with this disease. Birds are reservoir hosts for the virus and avian-mosquito-human transmission is how the disease is contracted. Humans do not sustain high-level viremias long enough to become reservoir or amplifying hosts. Human-to-human transmission does not occur.REF: Definitions Chapter 237: Anemia Test Bank Multiple Choice 1. A 20 kg child has iron-deficiency anemia and will begin taking an oral iron preparation. What will the provider teach the child’s parents about administration of this medication? a. Iron supplements should be given with food. b. The child must take the iron for 3 months. c. The correct dose is 30 mg twice daily. d. The iron is stopped when the hemoglobin increases. The dose for children is 3 mg/kg/day in divided doses. This child should get 60 mg/day, which is 30 mg/dose twice daily. Iron supplements are best absorbed on an empty stomach. Iron is given for at least 4 to 6 months. Hemoglobin levels will begin to increase in 1 to 2 weeks, but the iron is given until the serum ferritin increases sufficiently in 4 to 6 months.REF: Iron-Deficiency Anemia/Management 2. A 60-year-old female patient has recently lost weight and a physical examination reveals a beefy-red, sore tongue, with no neurological findings. Based on these clinical findings, what will the provider anticipate finding in the laboratory data? a. Decreased homocysteine levels b. Leukopenia and thrombocytopenia c. Low hemoglobin and elevated MCV d. Normal methylmalonic acid level Macrocytic anemia caused by vitamin B12 deficiency will have symptoms described above. Although folate acid deficiency causes macrocytic anemia, there are rarely any symptoms. Hemoglobin will be decreased and MCV will increase. Homocysteine levels will be increased. The patient with B12 deficiency will have leukopenia and thrombocytopenia with severe deficiency, characterized by neurologic findings, which this patient does not have. Methylmalonic acid level will decrease.REF: Macrocytic Anemia/Diagnostics 3. A patient reports recent mild fatigue and palpitations. A complete blood count reveals a decreased hemoglobin level and a normal ferritin level. What other findings are likely to be present? a. Decreased hematocrit b. Decreased MCV, MCH, and MCHC c. Elevated total iron-binding capacity d. Paresthesias, koilonychia, and pica This patient has signs of milder iron-deficiency anemia and will also have a low hematocrit level. The RBC indexes are the last to change as the anemia becomes more severe. When the ferritin level drops, the TIBC will become elevated. Paresthesias, koilonychia, and pica occur with more severe anemia.REF: Pathophysiology/Clinical Presentation Chapter 238: Blood Coagulation Disorders Test Bank Multiple Choice 1. A male patient has a history of recurrent epistaxis. Prior to a scheduled surgery, the provider asks about a family history of bleeding disorders. The patient reports no female relatives who had excessive bleeding episodes, but states that a maternal uncle and his maternal grandfather both had post-surgical complications related to bleeding. Based on this history, which diagnosis is possible? a. Hemophilia b. Thrombocytopenia c. Thrombophilia d. Von Willebrand disease Hemophilia is an X-linked recessive disorder affecting only males and carried by females. A family history of maternal males with bleeding disorders should clue the provider that this disorder is likely. Thrombocytopenia is usually an acquired disorder. Thrombophilia causes clots and thrombi, not bleeding. Von Willebrand disease is an autosomal genetic disorder affecting both males and females.REF: Pathophysiology and Clinical Presentation 2. A patient is noted to have prolonged bleeding after an intravenous needle is removed. A subsequent laboratory test reveals a prolonged activated partial thromboplastin (aPTT) time with a normal prothrombin time (PT). Based on this result, the provider may suspect alteration in function of which factor? a. Factor V b. Factor VII c. Factor VIII d. Factor X Factor VIII is part of the intrinsic system, which aPTT measures. The other factors are part of the extrinsic system, which is measured by PT.REF: Pathophysiology 3. A patient has type 1 Von Willebrand disease (vWD). What treatment is generally effective to prevent and treat bleeding episodes in this patient? a. Coagulation factor b. Desmopressin c. Heparin d. Vitamin K Desmopressin may be useful in patients with type 1 vWD. Coagulation factor is used in most patients with hemophilia. Heparin is an anticoagulant. Vitamin K is used to counter warfarin overdose.REF: Von Willebrand Disease Chapter 239: Leukemias Test Bank Multiple Choice 1. A patient is suspected of having leukemia and the provider orders biochemical studies and a bone marrow aspirate and biopsy. The results include WBCs greater than 200,000 cells/mm3 normal RBCs, hyperplastic myeloid cells, and the absence of serum leukocyte alkaline phosphatase. Which test will the provider order to confirm a diagnosis in this patient? a. Chest radiograph b. Coagulation studies c. Philadelphia chromosome test d. Serum protein electrophoresis The findings from the CBC and bone marrow biopsy, along with a positive Philadelphia chromosome test, confirm the diagnosis of chronic myelogenous leukemia. A chest radiograph and serum protein electrophoresis may be performed to evaluate for associated symptoms. Coagulation studies are usually performed as part of the diagnostic workup for ALL.REF: Clinical Presentation/Chronic Leukemias/Diagnostics and Differential Diagnosis 2. A child has a recent history of leg pain, unexplained bruising, and nosebleeds. The provider notes petechiae and diffuse lymphadenopathy. A complete blood count reveals a WBC of 30,000 cells/mm3 and near normal RBC and platelet counts. What will the provider do next to manage this patient? a. Order coagulation studies to evaluate for coagulopathies b. Perform biochemical studies to look for hyperuricemia c. Refer to a specialist for a bone marrow aspirate and biopsy d. Repeat the complete blood count in two weeks Patients with ALL may have normal blood counts even when the marrow has been replaced with leukemic cells, so a bone marrow aspirate and biopsy is required for the definitive diagnosis. Coagulation and biochemical studies may be performed after the diagnosis is known to evaluate for complications. Waiting and repeating the CBC in 2 weeks is not recommended since the definitive diagnosis is made by bone marrow biopsy.REF: Clinical Presentation/Acute Leukemias/Diagnostics and Differential Diagnosis 3. A patient with acute myelogenous leukemia (AML) who has a high white blood cell count and diffuse lymphadenopathy is hospitalized during the induction phase of chemotherapy. What monitoring and interventions are critical to assess for complications during this phase of care for this patient? Select all that apply. a. Administration of sodium bicarbonate and allopurinol b. Assessment for bruising and petechiae c. Close monitoring of absolute neutrophil counts d. Daily renal function and chemistry values e. Meticulous assessment of hydration status , D, E This patient has a high WBC load and diffuse lymphadenopathy, so is at increased risk for acute tumor lysis syndrome (ATLS). Close monitoring of renal function, serum renal chemistry values, and hydration status is essential. Adding sodium bicarbonate and allopurinol help to minimize risk. Thrombocytopenia causing bruising and petechiae, along with neutropenia, are common complications of chemotherapy but these symptoms generally occur 7 to 10 days after initiation of therapy.REF: Tumor Lysis Syndrome Chapter 240: Lymphomas Test Bank Multiple Choice 1. A patient reports a neck mass that has been present off and on for 5 or 6 weeks which varies in size. The provider palpates a lymph node measuring 1.25 cm. Which test will provide proper histologic diagnosis for this patient? a. Bone marrow aspirate b. CT scan with IV contrast c. Lymph node biopsy d. Positron emission tomography scan The lymph node biopsy is used to provide proper histologic diagnosis and precise classification. Bone marrow aspirate identifies the presence of dysplasic cells. PET and CT scans will identify the presence of other lesions.REF: Initial Evaluation/Making the Diagnosis 2. Which types of lymphomas typically have an aggressive presentation? Select all that apply. a. Adult T cell leukemia- lymphoma b. Burkitt lymphoma c. Diffuse large B cell lymphoma d. Follicular lymphoma e. Splenic marginal zone lymphoma , B, C Adult T cell leukemia-lymphoma, Burkitt lymphoma, and diffuse large B cell lymphoma are all aggressive lymphomas. Follicular lymphoma and splenic marginal zone lymphomas are indolent lymphomas.REF: Non-Hodgkin’s Lymphoma/Clinical Presentation 3. A 30-year-old male patient is diagnosed with Hodgkin lymphoma. Initial lab work reveals a WBC of 20 × 109/L, hemoglobin of 10.1 gm/dL, a serum albumin of 45 gm/dL, and lymphopenia of 0.5 × 109/L. Staging studies identify stage III disease. What is this patient’s prognostic score? a. 2 b. 3 c. 4 d. 5 Risk factors for lymphoma include age >45 years, male gender, serum albumin <40, Hb <10.5, stage IV disease, WBC >15, and lymphopenia <0.6. This patient has 4 risk factors.REF: Prognosis Chapter 241: Myelodysplastic Syndromes Test Bank Multiple Choice 1. A 70-year-old patient reports frequent infections, shortness of breath, fatigue, and palpitations. An exam reveals pallor and petechiae. The provider orders a peripheral blood smear and bone marrow biopsy. Which findings are consistent with a diagnosis of myelodysplasia? Select all that apply. a. Anisocytosis and poikilocytosis of erythrocytes on peripheral smear b. Defects in cellular maturation in all cell lines in bone marrow aspirate c. Hypercellular bone marrow with peripheral cytopenia d. Larger than normal megakaryocytes in bone marrow e. Smaller than normal granulocytes in the peripheral blood smear , B, C, D The key finding in MDS is packed, hypercellular bone marrow with peripheral cytopenia. Erythrocytes in peripheral blood will show anisocytosis, poikilocytosis, or basophilic stippling. The bone marrow will have defects in all cellular maturation. Megakaryocytes in bone marrow will be smaller than normal. Granulocytes in peripheral blood will be larger than normal.REF: Diagnostics 2. A patient with myelodysplastic syndrome (MDS) has severe neutropenia and anemia is given erythropoietin (EPO) with improvement in hemoglobin. Which intervention has been shown to prevent infection in patients with MDS who have severe neutropenia? a. Antithymocyte globulin and cyclosporine b. Granulocyte- macrophage colony-stimulating factor (GM-CSF) c. Intravenous immunoglobulin infusions d. Prophylactic treatment with floroquinolones Prophylactic antibiotic therapy with floroquinolones in neutropenic patients has been shown in a large meta-analysis to decrease the incidence of serious infections and reduce all-cause mortality. Antithymocyte globulin and cyclosporine is immune suppression treatment used to reduce the need for transfusions. GM-CSF is given when there is active infection, but does not decrease the actual number of infections. IVIG is not used for these patients and is not a prophylactic measure.REF: Management Chapter 242: Collaborative Management of the Oncology Patient Test Bank Multiple Choice 1. A patient being treated for cancer has had chemotherapy within the past two weeks and comes to the primary care clinic with a fever of 38.5° C. What is the initial action? a. Obtain a STAT CBC with differential b. Order a chest radiograph c. Order blood and urine cultures d. Prescribe empiric antibiotics Patients receiving chemotherapy who have a temperature >38° C and an ANC of less than 500/mm3 require immediate hospitalization and treatment. The primary provider should order a CBC to determine this risk and plan immediate hospitalization and referral to the oncologist. Once hospitalized, the patient will have further workup to determine the cause of the infection and then antibiotics to treat the infection.REF: Management 2. What is the most important role of the primary care provider in cancer management? a. Counseling about healthy practices to reduce risk factors b. Performing regular screenings to detect cancer c. Referring patients for genetic testing to identify those at risk d. Teaching patients about cancer management once diagnosed About three-fourths of cancer risks are related to elements that patients can control themselves and include diet, tobacco, alcohol, sun exposure, physical activity, and risky sexual behaviors. Emphasizing healthy lifestyle practices is a principle component of primary care. Screenings are next in importance and should be performed according to guidelines based on risk and age. Genetic testing is useful in a small percentage of patients; a good family history is important before referral for testing. The primary care provider may assist oncology specialists in teaching patients about cancer management.REF: Cancer Risks/Screening for Cancer/Patient Management Issues Chapter 243: Basic Principles of Oncology Treatment Test Bank Multiple Choice 1. An oncology specialist recommends placement of radioactive isotopes in capsules near a patient’s tumor. What is this form of radiation therapy called? a. Brachytherapy b. CT simulation c. External beam d. Fractionation Brachytherapy involves insertion of radioactive isotopes in a vehicle that can be implanted in the body to deliver radiation directly to a tumor. CT simulation is a method of delineating a radiation field prior to radiation therapy. External beam radiation is the use of linear accelerators to generate high-energy rays that penetrate the body to the tumor. Fractionation is used to minimize the harmful effects while maximizing the therapeutic benefit.REF: Radiation Therapy 2. Which chemotherapeutic agent classes are S-phase specific agents? Select all that apply. a. Asparaginase b. Bleomycin c. Fluorouracil d. Mercaptopurine e. Methotrexate , D, E Fluorouracil, mercaptopurine, and methotrexate are all S-phase specific. Asparaginase is a G1- phase specific chemotherapeutic agent and bleomycin is a G2-phase specific chemotherapeutic agent.REF: Chemotherapy 3. What is the purpose of radiation treatment prior to surgical resection of a tumor? a. To debulk the tumor mass b. To minimize local recurrence c. To prevent metastases d. To reduce pain and bleeding Preoperatively, radiation therapy may be used to debulk a tumor mass. It is used postoperatively to minimize local recurrence or when the resection margin remains suspicious for disease. It is used palliatively to address pain, bleeding, or brain metastases.REF: Radiation Therapy Chapter 244: Oncology Complications and Paraneoplastic Syndromes Test Bank Multiple Choice 1. A patient who has non-Hodgkin’s lymphoma reports a dull, aching back pain in the thoracic region for several weeks along with difficulty walking. The provider notes an ataxic gait. What is the immediate treatment for this condition? a. Chemotherapy b. Radiation therapy c. Steroid therapy d. Surgical decompression Dexamethasone is the immediate therapy for spinal cord compression to reduce vasogenic edema. The other options may be used depending on the type of cancer and the degree of neurologic deterioration.REF: Spinal Cord Compression/Management 2. Which are considered oncologic emergencies in a patient with cancer requiring urgent referral to an oncologist? Select all that apply. a. Bone marrow suppression b. Metastasis of cancer cells c. Superior vena cava syndrome d. Syndrome of inappropriate antidiuretic hormone e. Tumor lysis syndrome , D, E Superior vena cava syndrome, SIADH, and tumor lysis syndrome are all oncologic emergencies requiring urgent referral to the oncologist. Bone marrow suppression and metastasis occur with cancer, but are not emergencies.REF: Introduction 3. A patient is in the induction phase of chemotherapy just after diagnosis of cancer. Which prophylactic measures will help prevent tumor lysis syndrome? Select all that apply. a. Acidifying the urine b. Initiation of allopurinol c. Intravenous fluids of 3000 mL/day d. Rasburicase administration e. Sodium polystyrene sulfonate , C, D To help prevent the effects of tumor lysis syndrome, allopurinol is given when chemotherapy is initiated. IV fluids of 3000 mL/day are recommended. Rasburicase may be used instead of allopurinol. Alkalinization of the urine is recommended. Sodium polystyrene sulfonate is used to lower potassium, but is not a prophylactic measure.REF: Tumor Lysis Syndrome/Management and Complications Chapter 245: Oncology Pain and Symptom Management in Primary Care Test Bank Multiple Choice 1. A patient with cancer is expected to require long-term pain medication to manage cancer pain. Which agent will be best for this patient? a. Ibuprofen b. Meperidine c. Morphine d. Naloxone Pure opioid agonists do not have a ceiling dose and may be continually titrated as tolerance occurs, based on the patient’s need. Ibuprofen is not useful for severe pain. Meperidine has CNS side effects that may be fatal. Naloxone is an opioid antagonist.REF: Management of Oncology Pain 2. A patient with breast cancer has been symptom-free for 6 months and reports a new onset of lower back pain rated as an 8 on a 1 to 10 pain rating scale to the primary provider. What is most important when evaluating this patient’s pain? a. Evaluating the possibility of drug-seeking behavior b. Obtaining an MRI of the spinal cord c. Prescribing a trial of oral opioid medication d. Referring the patient to the oncologist Patients with cancers that tend to metastasize to the bone should have an MRI of the spine if they report back pain since early identification and treatment of spinal cord compression is essential to preserving neurologic function. If this is negative, the other measures may be taken if indicated.REF: Diagnostics of Oncology Pain 3. A patient with cancer is reluctant to take an opioid agonist medication because of the side effects. What will the primary care provider recommend? a. Adding an NSAID to the pain regimen b. Taking a stool softener with the opioid c. Using diphenhydramine to prevent itching d. Using opioids on an as needed basis only Almost all patients taking an opioid will experience constipation and do not develop tolerance to this effect. Giving a stool softener from the beginning may help alleviate this problem. Long- term use of NSAIDS increases the risk of GI bleeding and upset. Diphenhydramine may be given if itching occurs or is likely, but should not be used prophylactically. Opioids, when given, should be used around the clock and not as needed to best control pain.REF: Complications of Oncology Pain Chapter 246: Unknown Primary Carcinoma Test Bank Multiple Choice 1. A patient is determined to have an unknown primary carcinoma after a metastatic lesion is found in the lymph nodes. A blood test reveals that the patient has microcytic anemia. Which diagnostic test will the provider consider next to help determine the primary tumor? a. Alpha-fetoprotein and human chorionic gonadotropin levels b. Endoscopic evaluation of the upper and lower GI tract c. Positron emission tomography-computed tomography scan d. Prostate specific antigens Patients who are anemic may have a primary tumor in the GI tract, so initial diagnostic testing should focus on this. AFP and hCG levels help identify hepatocellular and germ cell tumors and midline tumors respectively. PET-CT helps rule out other sites of disease. PSA testing is useful if the UPC is an adenocarcinoma with dominant metastatic bone disease.REF: Diagnostics 2. A female patient is diagnosed with unknown primary carcinoma (UPC) after a metastatic squamous cell carcinoma is found. She asks the provider for an estimate about survival. What is the median survival rate for this type of UPC? a. 9 months b. 12 months c. 24 months d. 33 months Patients with squamous cell carcinoma have median survival times of 24 months. Patients with adenocarcinomas have a 9 month median survival, those with carcinoma have a 12 month median survival, and those with neuroendocrine carcinoma have a 33 month median survival.REF: Clinical Presentation 3. A woman has carcinomas confined to axillary nodes. A mammogram is normal. What is the next step in managing this patient? a. Begin treatment for primary breast tumor b. Evaluate HER-2 and estrogen and progesterone receptors c. Order an MRI of the breasts d. Reassure the patient that she probably does not have cancer Women with UPC confined to axillary lymph nodes are more likely to have occult breast cancer. Immunohistochemistry testing is indicated. If these findings are positive, treatment for breast cancer should begin. Even though some patients with UPC do not have cancer, in this case, she should be evaluated and treated if indicated.REF: Management Chapter 247: Anxiety Disorders Test Bank Multiple Choice 1. A patient is diagnosed with panic disorder and begins taking a selective serotonin reuptake inhibitor medication. Six weeks later, the patient reports little relief from symptoms. What will the provider do next to manage this patient? a. Change the medication to buspirone b. Discontinue the medication c. Increase the medication dose d. Refer to a mental health provider Patients taking SSRIs for anxiety disorders should see effects within 2 to 4 weeks. If patients have not had good results in 4 to 6 weeks, the provider should change the medication or refer to a mental health provider. Discontinuing an SSRI abruptly can cause withdrawal symptoms. Increasing the medication dose will not improve the effects. Buspirone is somewhat useful only for GAD.REF: Management 2. Which medication are useful in treating both obsessive-compulsive disorder and PTSD? Select all that apply. a. Benzodiazepines b. Buspirone c. Selective serotonin reuptake inhibitors d. Serotonin-norepinephrine reuptake inhibitors e. Tricyclic antidepressants , D, E SSRIs, SNRIs, and TCAs are useful in treating both OCD and PTSD. Benzodiazepines and buspirone are not indicated for either disorder.REF: Table 247-1: Pharmacologic Management of Anxiety Disorders: Indications and Considerations 3. A patient reports symptoms of restlessness, fatigue, and difficulty concentrating. The provider determines that these symptoms occur in relation to many events and concerns. What other things will the provider question this patient about? a. Ability to manage social situations b. Body image and eating habits c. Headaches and bowel habits d. Occupational performance This patient has symptoms consistent with generalized anxiety disorder (GAD) in which feelings occur in relation to many events. Patients with GAD often have headaches and irritable bowel syndrome. Phobias are linked to particular events and often include social situations. Patients with OCD tend to have eating disorders and difficulty with occupational and academic performance.REF: Clinical Presentation Chapter 248: Mood Disorders Test Bank Multiple Choice 1. A patient is seen in clinic 2 weeks after the death of a parent. The patient reports feelings of sadness and hopelessness and a feeling that the parent is still present, even to the point of hearing the parent’s voice at times. What will the provider determine from these findings? a. There is a concern for hypermania. b. There is a possibility of manic episodes. c. These are concerning for depression. d. These are normal grief responses. These are short-lived symptoms at this point, lasting less than 2 months. Auditory and sensory hallucinations only in relation to the deceased are normal during intense grief. Hypermania is an acute, short-lived manic episode. Mania involves abnormal elevation of a person’s mood. Depression is present when symptoms of grief are more severe and more prolonged.REF: Introduction/Table 248-1: Assessing Symptoms of Grief and a Depressive Mood Episode 2. A college student is brought to clinic by a parent who is concerned about increasingly bizarre behavior and poor school performance. The provider notes difficulty engaging the patient in an organized conversation. The patient denies any concerns about behavior. What will the provider do initially to manage this patient’s symptoms? a. Admit the patient for inpatient treatment b. Begin treatment with lithium or lamotrigine c. Counsel the parent to report any symptoms of depression d. Schedule an appointment with a psychiatrist Patients with symptoms of mania should begin treatment with a mood stabilizer and the primary care provider should initiate treatment for an acute episode. It is not necessary to admit as an inpatient unless there is indication of harm to the self or others. The primary provider should refer for psychiatric evaluation, but should begin medications as soon as possible.REF: Bipolar Disorder/Management 3. A patient is seen frequently over a 9-month period with somatic complaints that are not related to physical disease. The primary provider notes that the patient has had a 15% weight loss in the previous 2 months and the patient reports difficulty sleeping. The spouse tells the provider that the patient seems tired all the time and is irritable with other family members. What will the provider do initially? a. Perform a suicide risk assessment b. Prescribe a selective serotonin reuptake inhibitor c. Refer the patient for psychotherapy d. Suggest cognitive-behavioral therapy For any patients with symptoms of depression, the initial action is to perform a thorough assessment and evaluate potential suicide risk. SSRIs can be prescribed once a diagnosis is determined according to diagnostic criteria. Psychotherapy and cognitive-behavioral therapy may also be prescribed.REF: Depression/Clinical Presentation/Management Chapter 249: Substance Use Disorders Test Bank Multiple Choice 1. A patient is brought to the emergency department who is experiencing disorientation, confusion, and fever. The patient describes visual and auditory hallucinations. The patient’s spouse states that the patient had several drinks 12 hours prior to passing out. A blood alcohol level is 0.2%. What is the recommended treatment? a. Benzodiazepines b. Intravenous fluids and rest c. Naloxone d. Phenobarbital This patient is showing symptoms of major alcohol withdrawal and should be treated with a benzodiazepine, which is the safest, most effective drug to treat alcohol detoxification. Without medications, the patient may develop seizures and delirium tremens or may die. Naloxone is used for narcotics. Phenobarbital is used to treat seizures.REF: Alcohol Abuse/Management 2. A college student is brought to the emergency department by a roommate who is concerned about symptoms of extreme restlessness, nausea, and vomiting. The provider notes elevations of the pulse and blood pressure and pupillary dilation, along with hyperactive bowel sounds. The provider suspects withdrawal from which substance? a. Alcohol b. Cocaine c. LSD d. Opioids This patient has symptoms consistent with opioid withdrawal, which causes restlessness, hyperactive bowel sounds, pupillary dilation, and changes in vital signs. Alcohol withdrawal involves tremors, confusion, and hallucinations. Cocaine withdrawal causes muscle tension, teeth clenching, and blurred vision. LSD symptoms cause hallucinations.REF: Opioids Chapter 250: Other Mental Health Disorders Test Bank Multiple Choice 1. A 17-year-old male is brought to the clinic by a parent who is concerned that the patient has become more isolated and withdrawn and expresses suspicions that his teachers hate him and want him to fail. What will the provider tell this parent? a. The adolescent should be evaluated by a psychiatrist. b. The adolescent should be given a trial of antipsychotic medications. c. These are common adolescent behaviors and will eventually go away. d. These signs are diagnostic for schizophrenia. These signs, along with a family history of psychosis can be predictive of schizophrenia, so referral for psychiatric evaluation should be made. Unless symptoms are present longer than a month and the patient is diagnosed, antipsychotic medications are not indicated. Without evaluation, these behaviors should not be dismissed as normal. While these signs may raise concerns for schizophrenia, they are not diagnostic. REF: Clinical Presentation 2. A young male patient is reported to be more withdrawn from his peers than usual and has dropped out of college and quit his job within the last 5 months. The parent is concerned that the patient may have schizophrenia because a maternal uncle has the disease. What will the provider do next? a. Ask about the patient’s speech and thinking patterns b. Consider treatment with antipsychotic medications c. Reassure that classic symptoms of schizophrenia are not present d. Refer the patient for inpatient psychiatric treatment In order to diagnose schizophrenia, one or more of the positive signs of delusions, hallucinations, or disorganized speech must be present. Unless there is a definitive diagnosis, hospitalization and treatment are not indicated. The patient has some signs of schizophrenia, so further evaluation is necessary before reassurance can be made. REF: Box 250-1: Diagnostic Criteria for Schizophrenia 3. Which are considered “negative” symptoms of schizophrenia? Test Bank 2 Select all that apply. a. Auditory hallucinations b. Delusions of persecution c. Impaired self care d. Poor school performance e. Withdrawing from peers , D, E Negative symptoms are those related to decrease or loss of normal functions and may include social withdrawal, impaired self care, and poor school performance. Hallucinations and delusional beliefs are things added to normal behaviors and are considered positive symptoms of schizophrenia. REF: Clinical Presentation/Positive Symptoms/Negative Symptoms [Show More]
Last updated: 1 year ago
Preview 1 out of 441 pages
Instant download
Buy this document to get the full access instantly
Instant Download Access after purchase
Add to cartInstant download
Reviews( 0 )
Document information
Connected school, study & course
About the document
Uploaded On
Apr 09, 2021
Number of pages
441
Written in
Additional information
This document has been written for:
Uploaded
Apr 09, 2021
Downloads
1
Views
140

 HESI VI EXIT EXAM.png)
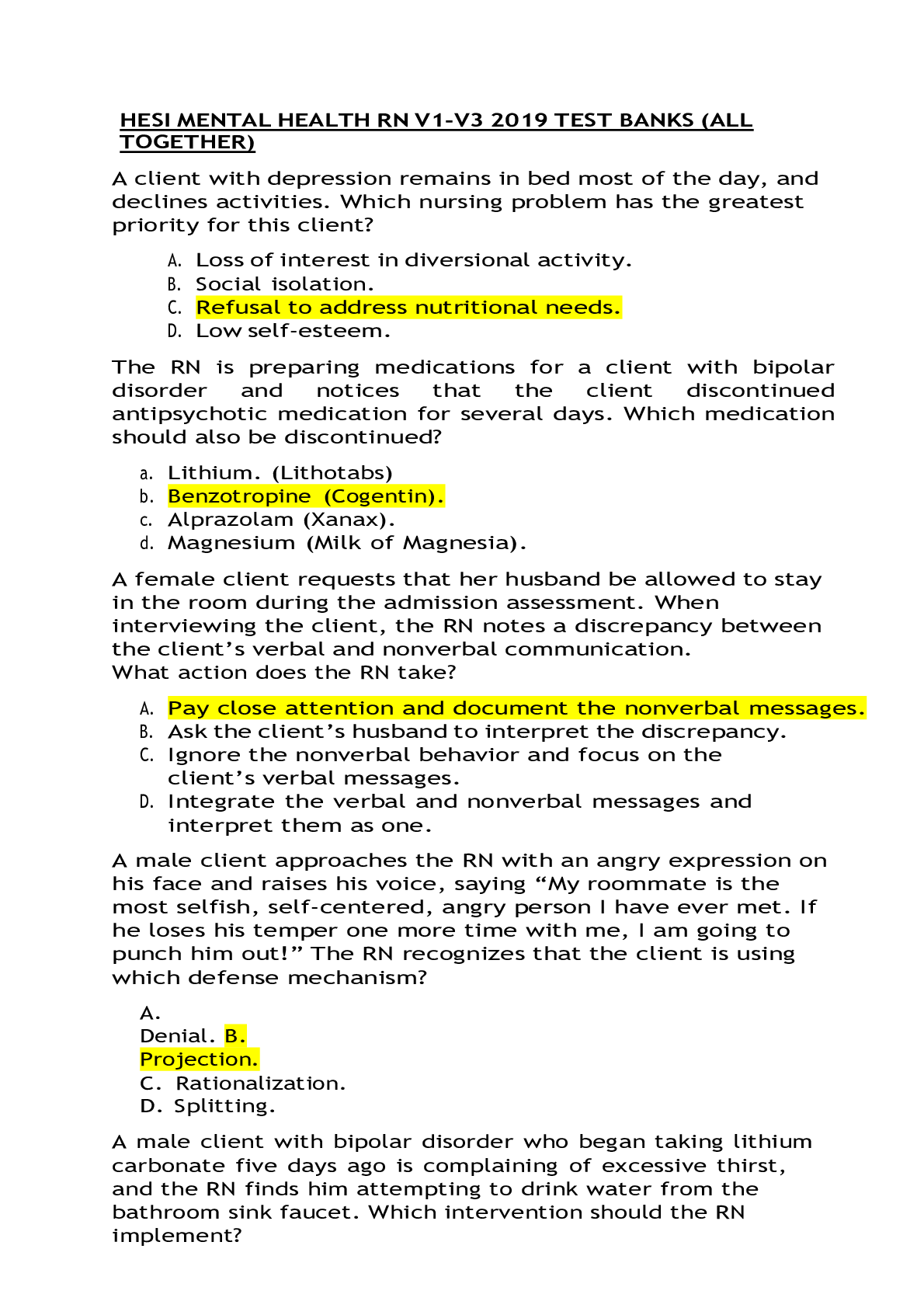
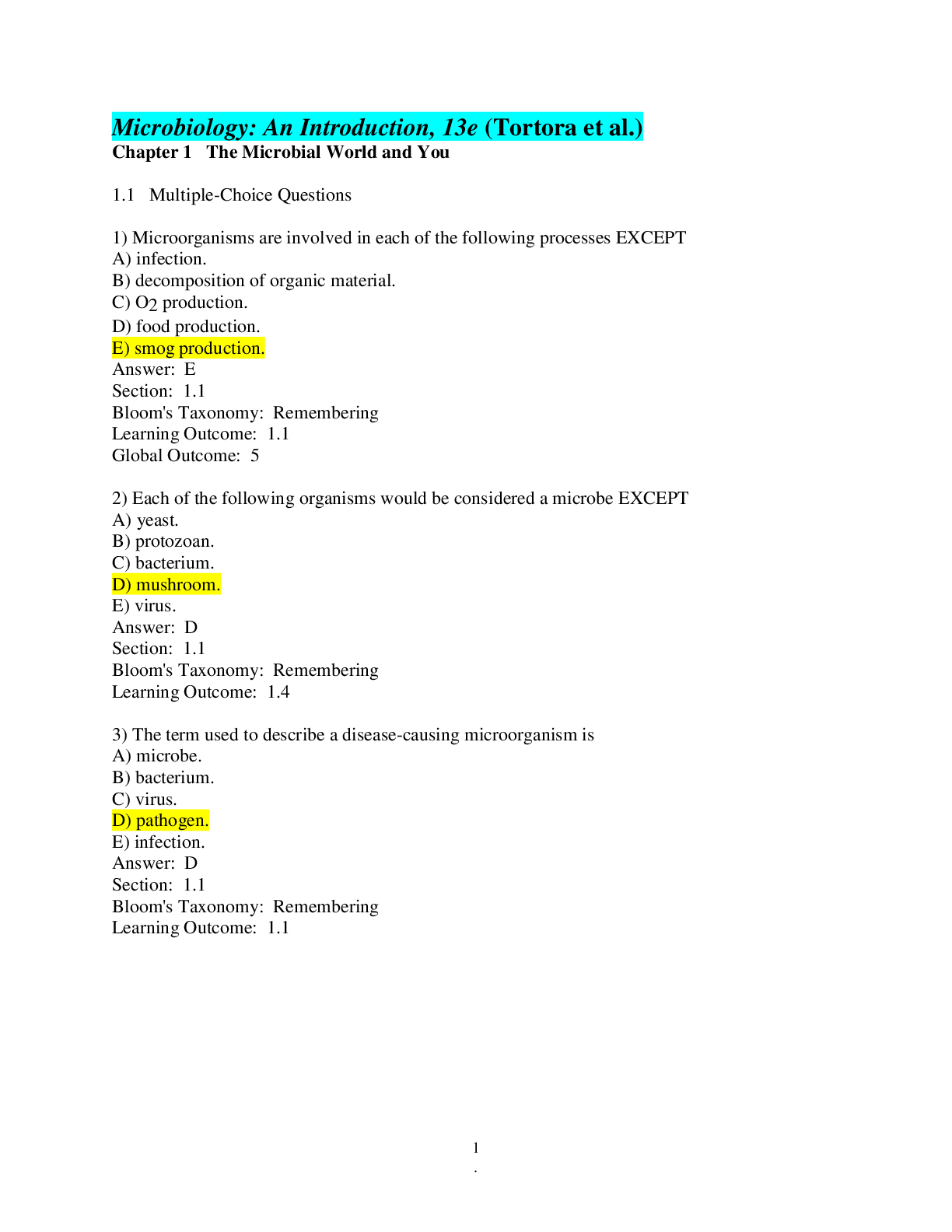
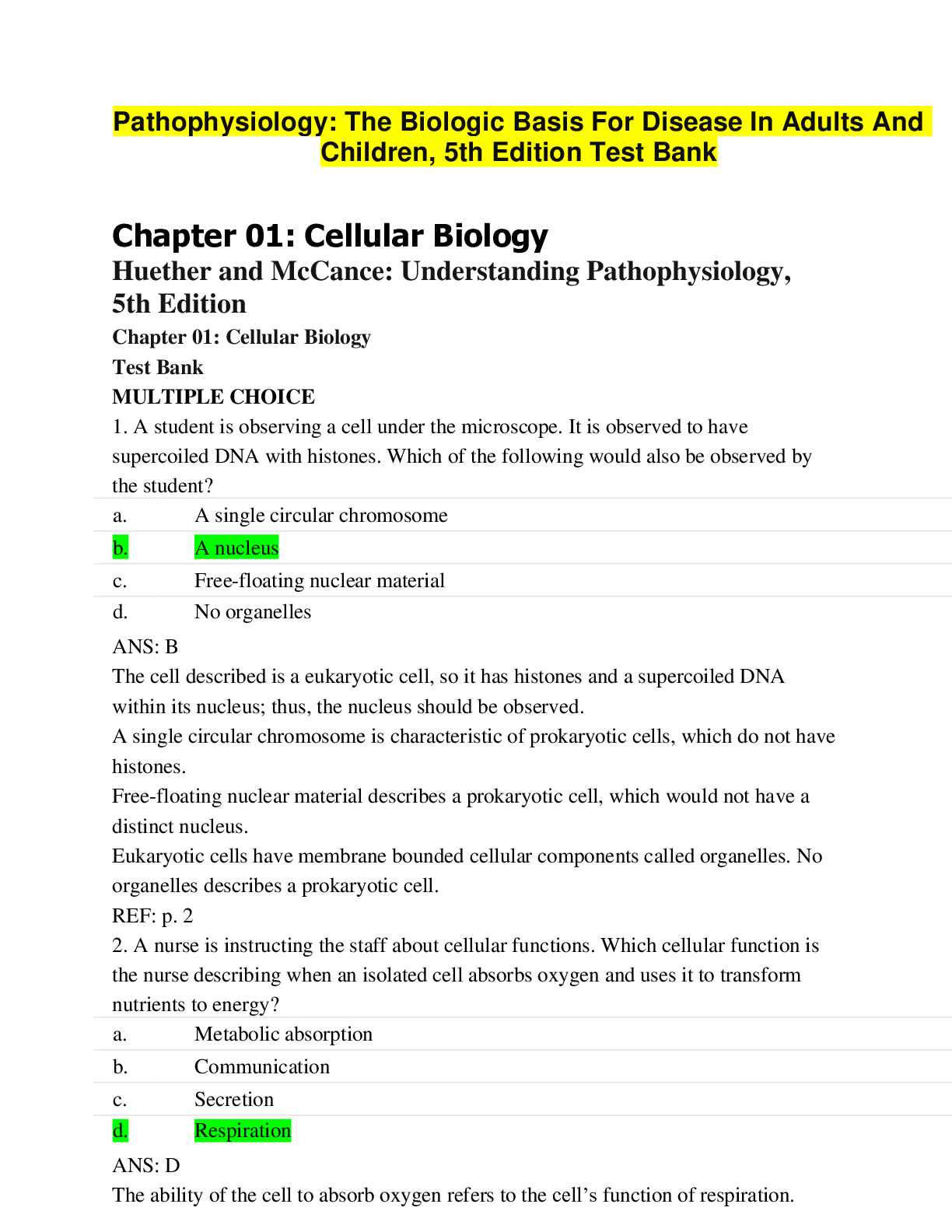

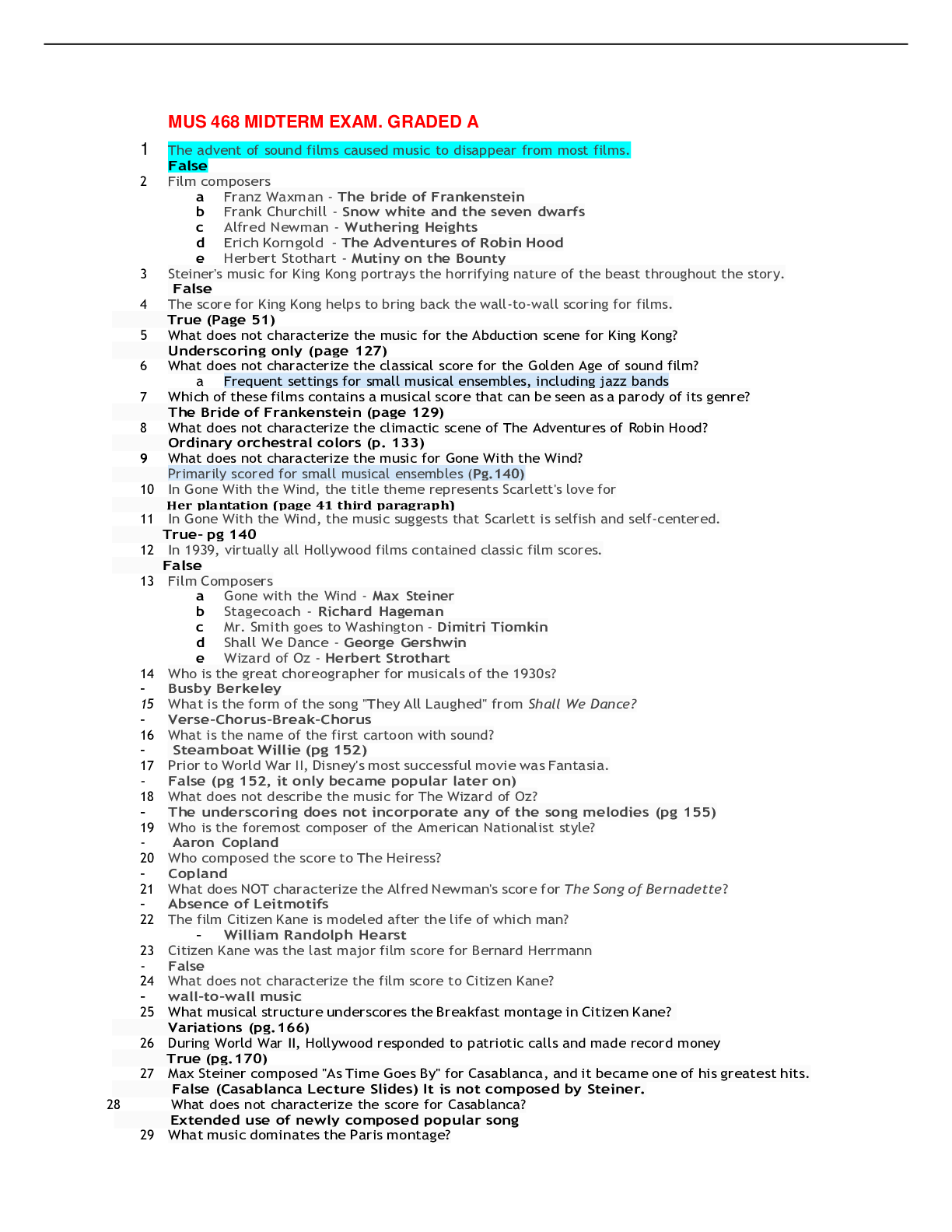
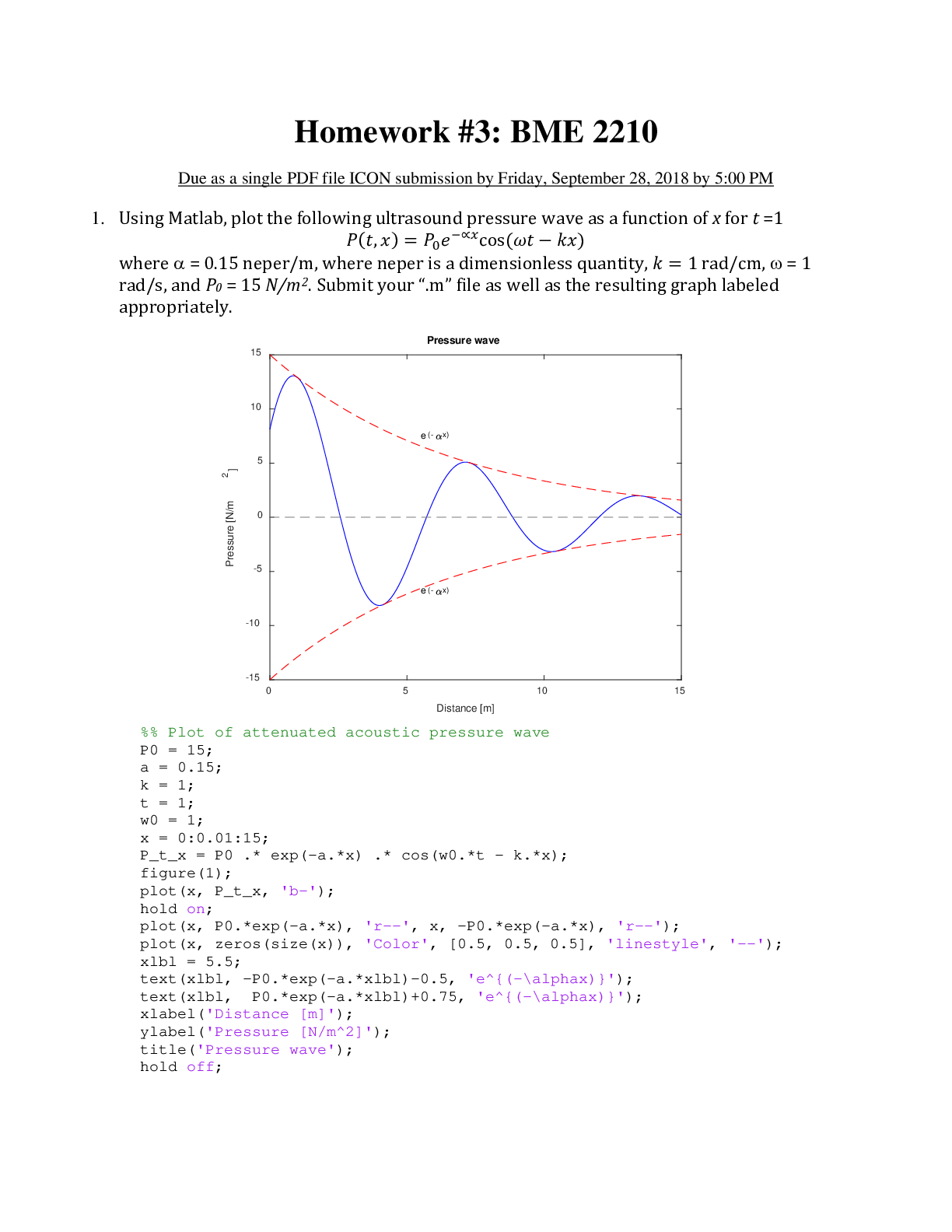
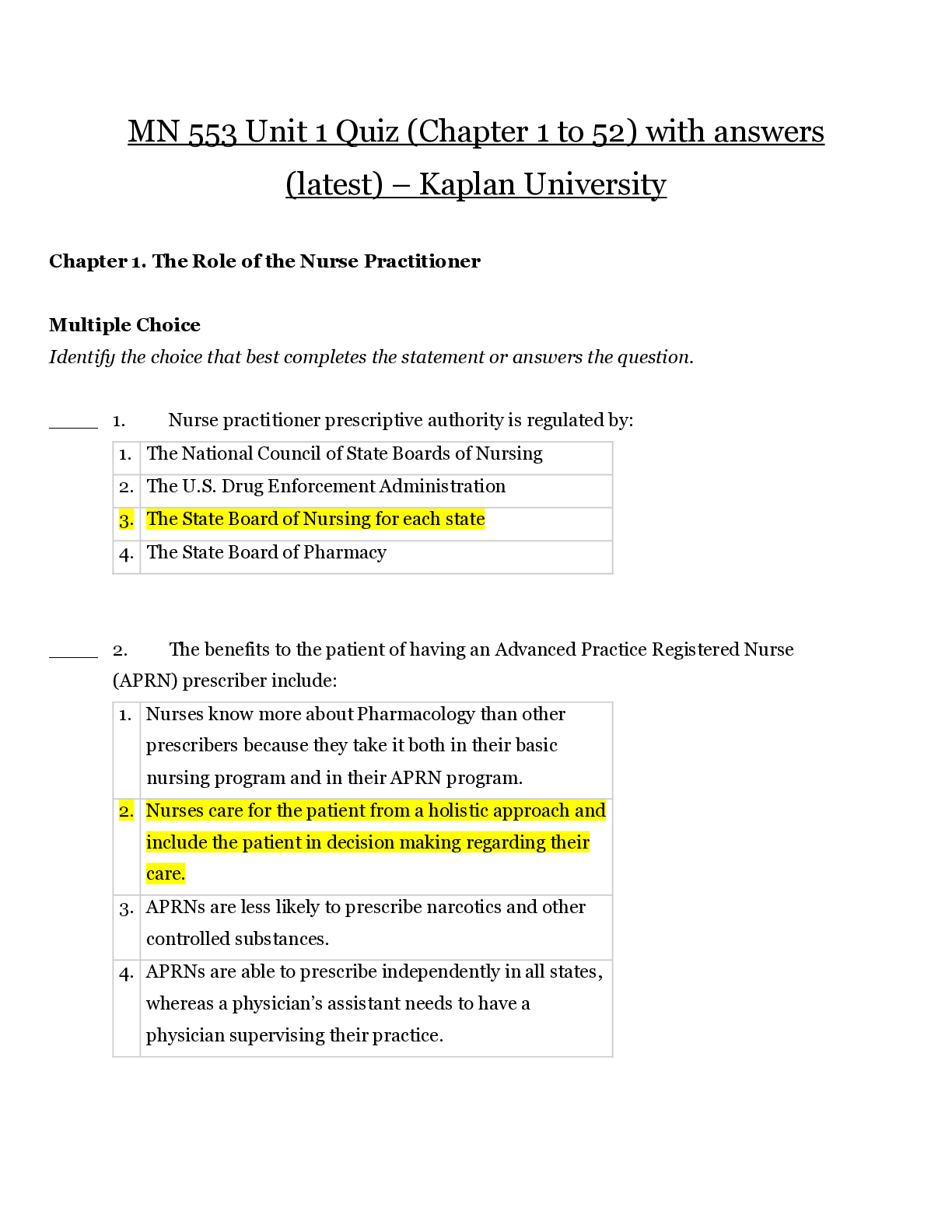


 (Test Bank) Questions and Answers (latest Update), 100% Correct, Download to Score A.png)