HESI PEDIATRIC NURSING QUESTIONS AND ANSWERS | 100% GUARANTEED PASS.
Document Content and Description Below
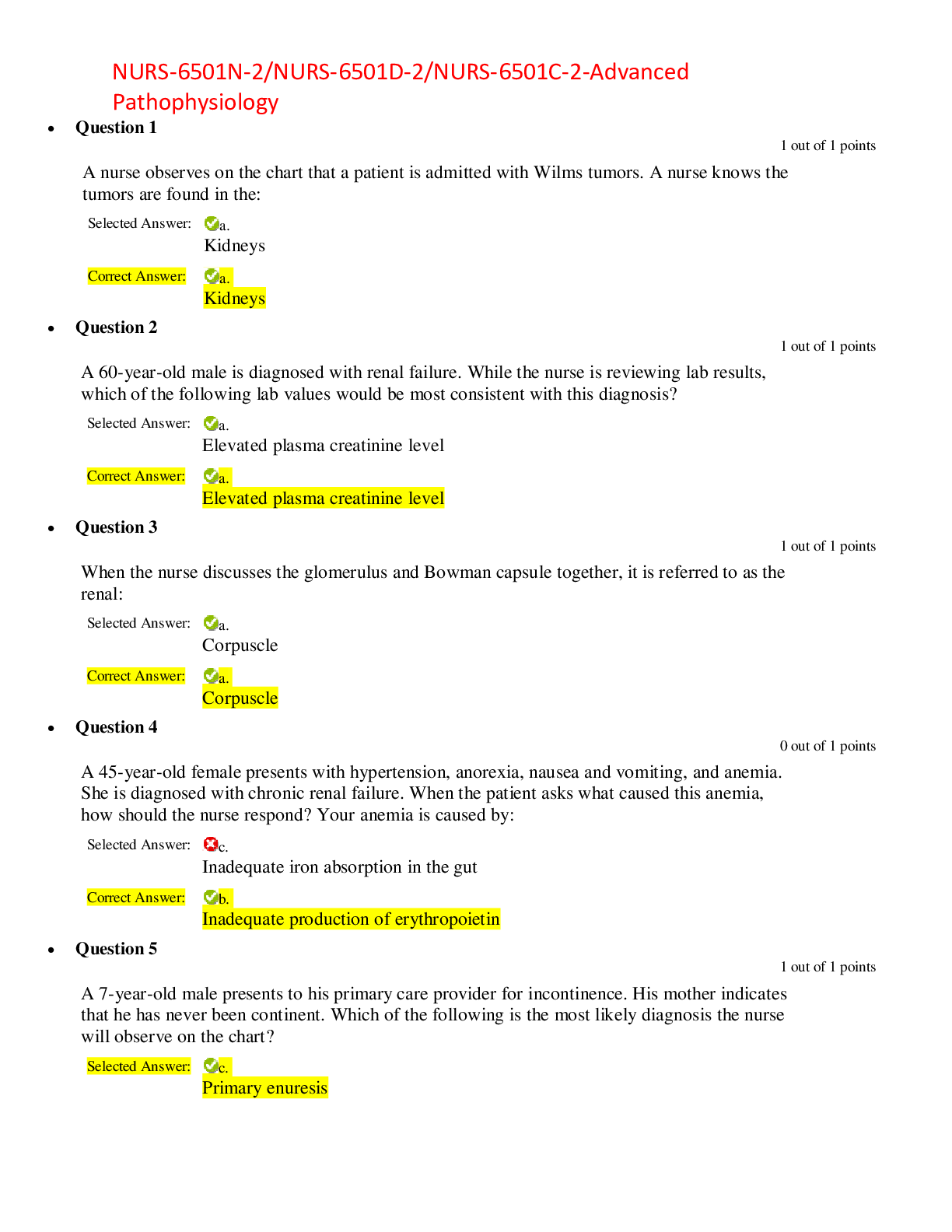
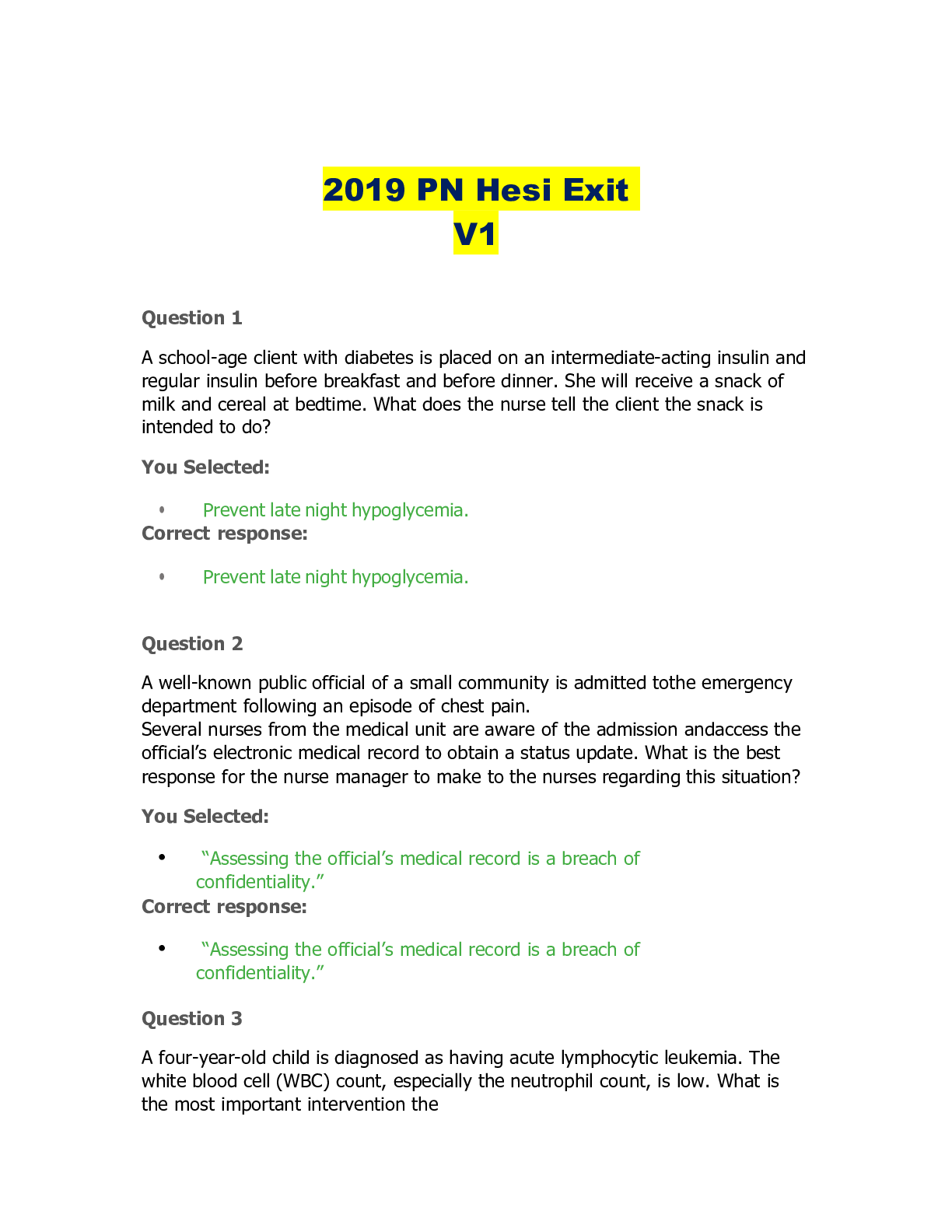
HESI PEDIATRIC NURSING QUESTIONS Child Health Promotion 1. List two contraindications to live virus immunization. • Immunocompromised child or a child in a household with an immunocompromised... individual. 2. List three classic signs and symptoms of measles. • Photophobia, confluent rash that begins on the face and spreads downward, and Koplik spots on the buccal mucosa. 3. List the signs and symptoms of iron deficiency. • Anemia, pale conjunctiva, pale skin color, atrophy of papillae on tongue, brittle, ridged or spoon-shaped nails, and thyroid edema. 4. Identify food sources of vitamin A. • Liver, sweet potatoes, carrots, spinach, peaches, and apricots. 5. What disease occurs with vitamin C deficiency? • Scurvy. 6. What measurements reflect present nutritional status? • Weight, skinfold thickness, and arm circumference. 7. List the signs and symptoms of dehydration in an infant. • Poor skin turgor, absence of tears, dry mucous membranes, weight loss, depressed fontanel, and decreased urinary output. 8. List the laboratory findings that can be expected in a dehydrate child. • Loss of bicarbonate/decreased serum pH, loss of sodium (hyponatremia), loss of potassium (hypokalemia), elevated Hct, and elevated BUN. 9. How should burns in children be assessed? • By using the Lund-Browder chart, which takes into account the changing proportions of the child’s body. 10. How can the nurse best evaluate the adequacy of fluid replacement in children? • By monitoring urine output. 11. How should a parent be instructed to childproof a house? • By being taught to lock all cabinets, to safely store all toxic household items in locked cabinets, and to examine the house from the child’s point of view. 12. What interventions should the nurse perform first in caring for a child who has ingested a poison? • Assessment of the child’s respiratory, cardiac, and neurologic status. 13. What early signs should the nurse assess for if lead poisoning is suspected? • Anemia, acute cramping, abdominal pain, vomiting, constipation, anorexia, headache, lethargy, hyperactivity, aggression, impulsiveness, decreased interest in play, irritability, short attention span. Respiratory Disorders 1. Describe the purpose of bronchodilators. • To help open airways by relaxing the bronchial muscles. 2. What are the physical assessment findings for a child with asthma? • Expiratory wheezing, rales, tight cough, and signs of altered blood gases. 3. What nutritional support should be provided for a child with cystic fibrosis? • Pancreatic enzyme replacement; fat-soluble vitamins; and a moderate- to low-carbohydrate, high-protein, moderate- to high-fat diet. 4. Why is genetic counseling important for the family of a child with cystic fibrosis? • Because the disease is autosomal recessive in its genetic pattern. 5. List seven signs of respiratory stress in a pediatric patient. • Restlessness, tachycardia, tachypnea, diaphoresis, flaring nostrils, retractions and grunting. 6. Describe the care of a child in a mist tent. • Monitor child’s temperature, keep tent edges tucked in, keep clothing dry, assess respiratory status, and look at child inside tent. 7. What position does a child with epiglottitis assume? • Upright sitting, with chin out and tongue protruding (“tripod position”). 8. Why are IV fluids important for a child with an increased respiratory rate? • The child is at risk for dehydration and acid-base imbalance. 9. Children with chronic otitis media are at risk for developing what problem? • Hearing loss. 10. What is the most common postoperative complication after a tonsillectomy? Describe the signs and symptoms of this complication. • Hemorrhage; frequent swallowing, vomiting fresh blood, and clearing throat. Cardiovascular Disorders 1. Differentiate between a right-to-left and a left-to-right shunt in cardiac disease. • A right-to-left shunt bypasses the lungs and delivers unoxygenated blood to the systemic circulation, causing cyanosis. A left-to-right shunt moves oxygenated blood back through the pulmonary circulation. 2. List the four defects associated with tetralogy of Fallot. • VSD, overriding aorta, pulmonary stenosis, and right ventricular hypertrophy. 3. List the common signs of cardiac problems in an infant. • Poor feeding, poor weight gain, respiratory distress and infections, edema, and cyanosis. 4. What are the two objectives in treating CHF? • Reduce the workload of the heart and increase cardiac output. 5. Describe nursing interventions to reduce the workload of the heart. • Give small, frequent feedings or gavage feedings. Plan frequent rest periods. Maintain a neutral thermal environment. Organize activities to disturb child only as indicated. 6. What position would best relieve the child experiencing a tet spell? • Knee-chest position or squatting. 7. What are the common signs of digoxin toxicity? • Diarrhea, fatigue, weakness, nausea, and vomiting; the nurse should check for bradycardia before administration. 8. List five risks in cardiac catheterization. • Arrhythmia, bleeding, perforation, phlebitis, and obstruction of the arterial entry site. 9. What cardiac complications are associated with rheumatic fever? • Aortic valve stenosis and mitral valve stenosis. 10. What medications are used to treat rheumatic fever? • Penicillin, erythromycin, and aspirin. Neuromuscular Disorders 1. What are the physical features of a child with Down syndrome? • Simian creased in palms, hypotonia, protruding tongue, and upward-outward slant of eyes. 2. Describe Scissoring. • A common characteristic of spastic CP in infants; legs are extended and crossed over each other; feet are plantar flexed. 3. What are two nursing priorities for a newborn with myelomeningocele? • Prevention of infection of the sac and monitoring for hydrocephalus (measure head circumference, check fontanel, assess neurologic functioning.). 4. List the signs and symptoms of increased ICP in older children. • Irritability, change in LOC, motor dysfunction, headache, vomiting, unequal pupil response, and seizures. 5. What teaching should parents of a newly shunted child receive? • Information about signs of infection and increased ICP; understanding that shunt should not be pumped and that child will need revisions with growth; guidance concerning growth and development. 6. State the three main goals in providing nursing care for a child experiencing a seizure. • Maintain patent airway, protect from injury, and observe carefully. 7. What are the side effects of Dilantin? • Gingival hyperplasia, dermatitis, ataxia, GI distress. 8. Describe the signs and symptoms of a child with meningitis. • Fever, irritability, vomiting, neck stiffness, opisthotonos, positive Kernig sign, positive Brudzinski sign; infant may not show all classic signs even though very ill. 9. What antibiotics are usually prescribed for bacterial meningitis? • Ampicillin, ceftriaxone, or chloramphenicol. 10. How is a child usually positioned after brain tumor surgery? • Flat or on either side. 11. Describe the function of an osmotic diuretic. • Osmotic diuretics remove water from the CNS to reduce cerebral edema. 12. What nursing interventions increase intracranial pressure? • Suctioning and positioning, turning. 13. Describe the mechanism of inheritance of Duchenne muscular dystrophy. • Duchenne muscular dystrophy is inherited as an X-linked recessive trait. 14. What is the Gowers sign? • Gowers sign is an indicator of muscular dystrophy; to stand, the child has to “walk” hands up legs. Renal Disorders 1. Compare the signs and symptoms of AGN with those of nephrosis. • AGN: gross hematuria, recent strep infection, hypertension, and mild edema; nephrosis: severe edema, massive proteinuria, frothy-appearing urine, and anorexia. 2. What antecedent event occurs with AGN? • Beta-hemolytic streptococcal infection. 3. Compare the dietary interventions for AGN and nephrosis. • AGN: low-sodium diet with no added salt; nephrosis: high-protein, low-salt diet. 4. What is the physiologic reason for the laboratory finding of hypoproteinemia in nephrosis? • Hypoproteinemia occurs because the glomeruli are permeable to serum proteins. 5. Describe safe monitoring of prednisone administration and withdrawal. • Long-term prednisone should be given every other day. Signs of edema, mood changes, and GI distress should be noted and reported. The drug should be tapered, not discontinued suddenly. 6. What interventions can be taught to prevent urinary tract infections in children? • Avoid bubble baths; void frequently; drink adequate fluids, especially acidic fluids such as apple or cranberry juice; and clean genital area from front to back. 7. Describe the pathophysiology of vesicoureteral reflux. • A malfunction of the valves at the end of the ureters, allowing urine to reflux out of the bladder into the ureters and possibly into the kidneys. 8. What are the priorities for a client with a Wilms tumor? • Protect the child from injury to the encapsulated tumor. Prepare the family and child for surgery. 9. Explain why hypospadias correction is performed before the child reaches preschool age. • Preschoolers fear castration, achieving sexual identity, and acquiring independent toileting skills. Gastrointestinal Disorders 1. Describe feeding techniques for a child with cleft lip or palate. • Use lamb’s nipple or prosthesis. Feed child upright, with frequent bubbling. 2. List the signs and symptoms of esophageal atresia with TEF. • Choking, coughing, cyanosis, and excess salivation. 3. What nursing actions are initiated for the newborn with suspected esophageal atresia with TEF? • Maintain NPO immediately, and suction secretions. 4. Describe the postoperative nursing care for an infant with pyloric stenosis. • Maintain IV hydration, and provide small, frequent oral feedings of glucose or electrolyte solutions or both within 4 to 6 hours. Gradually increase to full- strength formula. Position infant on right side in semi-Fowler position after feeding. 5. Describe why a barium enema is used to treat intussusception. • A barium enema reduces the telescoping of the intestine through hydrostatic pressure without surgical intervention. 6. Describe the preoperative nursing care for a child with Hirschsprung disease. • Check vital signs at take axillary temperatures. Provide bowel-cleansing program, and teach about colostomy. Observe for bowel perforation; measure abdominal girth. 7. What care is needed for a child with a temporary colostomy? • Family needs education about skin care and appliances. Referral to an enterostomal therapist is appropriate. 8. What are the signs of anorectal malformation? • A newborn that does not pass meconium within 24 hours; meconium appearing through a fistula or in the urine; an unusual-appearing anal dimple. 9. What are the priorities for a child undergoing abdominal surgery? • Maintain fluid balance (I&O, nasogastric suction, monitor electrolytes); monitor vital signs; care for drains, if present; assess bowel function; prevent infection of incisional area and other postoperative complications; and support child and family with appropriate teaching. Hematologic Disorders 1. Describe the information families should be given when a child is receiving oral iron preparations. • Give oral iron on an empty stomach and with vitamin C. Use straws to avoid discoloring teeth. Tarry stools are normal. Increase dietary sources of iron. 2. List dietary sources of iron. • Meat, green leafy vegetables, fish, liver, whole grains, legumes. 3. What is the genetic transmission pattern of hemophilia? • It is an X-linked recessive chromosomal disorder transmitted by the mother and expressed in mal children. 4. Describe the sequence of events in a vasoocclusive crisis in sickle cell anemia. • A vasoocclusive crisis is caused by the clumping of RBC’s, which blocks small blood vessels; therefore the cells cannot get through the capillaries, causing pain and tissue and organ ischemia. Lowered oxygen tension affects HgbS, which causes sickling of the cells. 5. Explain why hydration is a priority in treating sickle cell disease. • Hydration promotes hemodilution and circulation of the RBC’s through the blood vessels. 6. What should families and clients do to avoid triggering sickling episodes? • Keep child well hydrated. Avoid known sources of infections. Avoid high altitudes. Avoid strenuous exercise. 7. Nursing interventions and medical treatments for a child with leukemia are based on what three physiologic problems? • Anemia (decreased erythrocytes); infection (neutropenia); bleeding thrombocytopenia (decreased platelets). 8. Nursing interventions and medical treatments for a child with retinoblastoma are based on what type of treatment and if inherited? • The nursing interventions and medical treatment are dependent on the type of treatment. Children with inherited blastoma need to be screened throughout their lives for development of other forms of cancer. Metabolic and Endocrine Disorders 1. How is congenital hypothyroidism diagnosed? • Newborn screening revealing a low T4 and a high TSH. 2. What are the symptoms of congenital hypothyroidism in early infancy? • Large, protruding tongue; coarse hair; lethargy; sleepiness; and constipation. 3. What are the outcomes of untreated congenital hypothyroidism? • Mental retardation and growth failure. 4. What are the metabolic effects of PKU? • CNS damage, mental retardation, and decreased melanin. 5. What two formulas are prescribed for infants with PKU? • Lofenalac and Phenex-1 6. List foods high in phenylalanine. • Meat, milk, dairy products, and eggs. 7. What are the three classic signs of diabetes? • Polydipsia, polyphagia, and polyuria. 8. Differentiate the signs of hypoglycemia and hyperglycemia. • Hypoglycemia: tremors, sweating, headache, hunger, nausea, lethargy, confusion, slurred speech, anxiety, tingling around mouth, nightmares. Hyperglycemia: polydipsia, polyuria, polyphagia, blurred vision, weakness, weight loss, and syncope. 9. Describe the nursing care of a child with ketoacidosis. • Provide care for an unconscious child, administer regular insulin IV in normal saline, monitor blood gas values, and maintain strict I&O. 10. Describe developmental factors that would affect the school-age child with diabetes. • Need to be like peers; assuming responsibility for own care; modification of diet; snacks and exercise in school. 11. What is the relationship between hypoglycemia and exercise? • During exercise, insulin uptake is increased and the risk for hypoglycemia occurs. Skeletal Disorders 1. List normal findings in a neurovascular assessment. • Warm extremity, brisk capillary refill, free movement, normal sensation of the affected extremity, and equal pulses. 2. What is compartment syndrome? • Damage to nerves and vasculature of an extremity due to compression. 3. What are the signs and symptoms of compartment syndrome? • Abnormal neurovascular assessment: cold extremity, severe pain, inability to move the extremity, and poor capillary refill. 4. Why are fractures of the epiphyseal plate a special concern? • Fractures of the epiphyseal plate (growth plate) may affect the growth of the limb. 5. How is skeletal traction applied? • Skeletal traction is maintained by pins or wires applied to the distal fragment of the fracture. 6. What discharge instructions should be included concerning a child with a Spica cast? • Check child’s circulation. Keep cast dry. Do not place anything under cast. Prevent cast soilage during toileting or diapering. Do not turn child using an abductor bar. 7. What are the signs and symptoms of congenital dislocated hip in infants? • Unequal skin folds of the buttocks, Ortolani sign, limited abduction of the affected hip, and unequal leg lengths. 8. How would the nurse conduct a scoliosis screening? • Ask the child to bend forward from the hips, with arms hanging free. Examine the child for a curve in the spine, a rib hump, and hip asymmetry. 9. What instructions should a child with scoliosis receive about a skeletal brace? • The child should be instructed to wear the brace 23 hours per day; wear a t- shirt under brace; check skin for irritation; perform back and abdominal exercises; and modify clothing. The child should be encouraged to maintain normal activities as able. 10. What car is indicated for a child with juvenile rheumatoid arthritis? • Prescribed exercise to maintain mobility; splinting of affected joints; and teaching about medication management and side effects of drugs. [Show More]
Last updated: 1 year ago
Preview 1 out of 11 pages
Instant download
Buy this document to get the full access instantly
Instant Download Access after purchase
Add to cartInstant download
Reviews( 0 )
Document information
Connected school, study & course
About the document
Uploaded On
Apr 13, 2021
Number of pages
11
Written in
Additional information
This document has been written for:
Uploaded
Apr 13, 2021
Downloads
0
Views
38


.png)