*NURSING > QUESTIONS and ANSWERS > NR 508 Final Exam study guide (All)
NR 508 Final Exam study guide
Document Content and Description Below
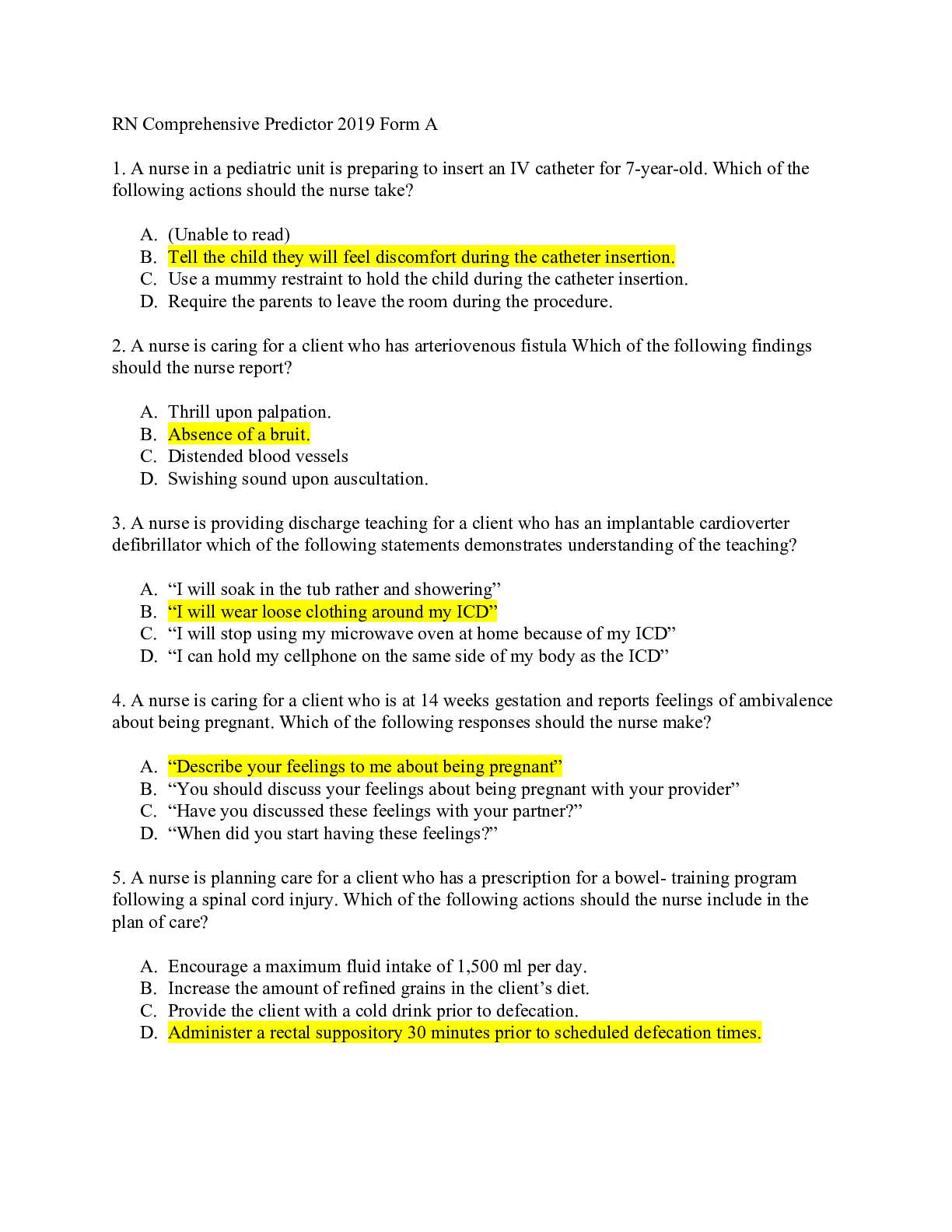
NR 508 Final Exam study guide Cardiovascular management: 1. Know Initial treatment choices for HTN AceI- sartans Arbs- ipine, verapamil & diltazem Thiazide- iaside, chlorthalidone, imdapamide, me... tolazone calcium channel blocker 2. Know first line treatment options for HTN for African Americans without renal impairment. Calcium channel blockers Thiazide 3. First line option for HTN for anyone with chronic kidney disease Ace inhibitors ARB’s Diuretics: 4. Types, Uses, Side effects Thiazides (HCTZ) Uses- HTN, CHF, edema, useful in decreases calcium stone formation Off label HCTZ- osteoporosis and diabetes AE- hypokalemia, hyperglycemia, arrhythmias, metabolic alkalosis, fatigue, postural Hypotension Loop diuretics (furosemide, torsemide, ethacrynic acid) *preferred diuretics for renal Impairment Uses- CFH, HTN, nephrotic syndrome, cirrhosis, pulmonary edema AE-hypocalcemia, hyponatremia, hypokalemia, ototoxicity Carbonic anhydrase inhibitors (acetazolamide) *weak diuretic Uses- edema, epilepsy, glaucoma, mountain sickeness AE- toxic epidermal necrolysis, agranulocytosis, aplastic anemia, thrombocytopenia, metabolic acidosis Potassium-sparing (spironolactone, eplerenone) Uses- CHF (in combo with thiazides or ACE and loop), HTN AE-gynomastia, n/v, erectile dysfuction, electrolyte imbalance, metabolic acidosis **postdiuretic sodium retention- It is important for pts to adhere to a low sodium diet. As drug concentrations fall, there is a period of positive sodium balance ** If a pt has a sulfa allergy= take ethacrynic acid 5. Preferred diuretic with renal impairment- Loop diuretics because they retain efficacy even with moderate renal insufficiency: such as furosemide, buetanide, torsemide, ethacrynic acid. Uses: Edematous states (HF, cirrhosis, pulmonary edema, nephrotic syndrome), hypercalcemia 6. Side effect of post diuretic sodium retention pg 374 As drug concentrations decrease, period of + Na balance, this is the post diuretic sodium retention If there is a high Na intake then Na lost with diuresis is offset.. diuretic resistance 7. Recognition that some diuretics are sulfa derivatives (carbonic anhydrase inhibitors, loop diuretics, thiazides, but NOT ethacrynic acid) Loops- Examples: furosemide, bumetanide, torsemide, ethacrynic acid "The Loop FURiously BUMmed my TORSo like ACID" Common side effects: orthostatic hypotension, excessive diuresis, tinnitus, vertigo, hyperuricemia note all these are precursors to toxicity Thiazides Hydrochlorothiazide, Chlorothoazide, , Chlorthalidone, Indapamide, Metolazone 1st line for HTN, Chronic Calcium Kidney Stones, HF, Idiopathic hypercalciuria, Nephrogenic diabetes insipidus, Osteoporosis. Other common side effects: orthostatic hypotension, dizzy, drowsy, syncope, weakness, nausea, GI irritation, elevated BUN, depressed respirations lethargy Carbonic anhydrase inhibitors- Acetazolamide N/V/D, Drowsy, Parathesis, confusion, tinnitus, myopia, anorexia, change in taste; polyuria, mild electrolyte changes Uses: Edematous states ( HF, cirrhosis, pulmonary edema, nephrotic syndrome), hypercalcemia Ethacrynic Acid Note it's the only diuretic with "acid" in its name 8. Management of edema Loops for volume excess 9. CHF drugs including diuretic choices 1- Loops -fluid 2- ACEIs or ARBs 3-BB - Diastolic after stable (B-Day) 4- Digoxin - Systolic , AFib, (Dig A Syst) 5- Spironolactone - if above not effective 6- Nitrates & Hydralazine *AA only* Think Michael Jordan goes Hy in his NIkes CCBs ( Amlodipine/Felodipine) only for angina or HTN if EF is preserved 2- Clinical pearls for CHF- Improve SX: ACEIs, ARBs, BBs (metoprolol, Bisoprolol, Carvedilol) , Dig ( only after diuretics & ACEIs) Prolong survival: ACEIs, ARBS, BB, Hydralazine/Nitrates(AA only) Aldosterone Antagonists BB NEVER IN ACTIVE FAILURE Dig does not improve mortality but improves SX decreases Hospitalization.. CAUTION:: Loops without Spironolactone **with hyperkalemia DIG CAN BECOME TOXIC" Neuro/Psych: 10. Know migraine management and prophylactics (see migraine lecture) dark, quiet room *NSAIDS or APAP *Triptans (sumatriptan/imitrex, zolmatriptan/zomig, rizatriptan/maxalt) -nasal, oral, subq -use no more than 2d/wk -CI-recent use of MAOIs, ergots, or SSRIs, CVD, CAD, TIA, HTN, pregnancy *Ergots (ergotamine tartrate/cafergot) not used often, expensive -nasal, oral, rectal, IM, IV, siblingual -CI-recent use of triptans, CVD, CAD, TIA, HTN, pregnancy *Caffeine (Excedrin) *antiemetics Migraine prevention *beta blockers (metoprolol, propranolol, timolol) -takes 2-3 months for full benefit- can decrease frequency and severity by 50% -AE- drowsiness, exercise intolerance, depression -CI-CHF, asthma *anticonvulsants (valproate, topiramate) effective but both have major AE -valproate AE- dizziness, platelet dysfunction, hair loss, hepatotoxic, teratogenic -topiramate AE- cognitive dysfunction, weight loss, renal stones *butterbur- PA free only, otherwise can cause liver damage and severe illness 11. Herbal migraine management Butter bur root. It should be PA free or could result in liver damage. Feverfew (Tanacetum parthenium) - Action: Antiinflammatory effects Uses: migraine prevention Interactions: Anticoagulants, antiplatelet drugs, aspirin (Pg. 99) 12. What drugs can cause serotonin syndrome? SSRIs and TRIPTANS 13. What migraine prophylactic medication class to avoid in patients with asthma. Beta Blockers such as Propranolol cyproheptadine (Periactin) - The drug may produce an atropine-like action, so it must be used with caution in patients treated for bronchial asthma (pg. 487) 14. Know the common side effects of methylphenidate Ritalin Most common: Nervousness & Insomnia Other common side effects: Decreased appetite Abdominal pain HA Depression Irritability Weight loss Rebound effect Side effects like if I don't have my stimulant COFFEE!! Page 453 Also: Temporary slowing of growth rate/Height and weight should be monitored with long term use ADHD management – 15. At what age can ADHD dx be made? DX typically before age 7 16. Stimulants including: Side effects -eg HA, tics, appetite suppression, elevated BP Stimulants: work by increasing “background” dopamine levels in the synapses. However, diagnostic trials of stimulant medications have failed to distinguish between children with and those without AD/HD. Amphetamine Like Drugs (Methylphenidate, ritalin, metadate, concerta) 1st LINE OF TREATMENT MOA: mild cortical stimulant with CNS actions similar to amphetamines. Inhibits reuptake of norepinephrine & dopamine Side effects: (may subside after a few weeks) common –These are drugs including methylphenidate and dexmethylphenidate Side effects Increased BP Exacerbation of behavior Agitation and aggression Watch for abuse Mania psychotic symptoms Blurred vision Temp stunting of growth Decreased appetite HA Depression Rebound SX NERVOUSNESS & INSOMNIA MOST COMMON monitor height weight and BP * Amphetamines - (Adderall, Vyvanse) MOA: Norepinephrine released from central noradrenergic neurons. Side effects: These drugs include dextroamphetamine Side effects Effects more severe initial days of TX Anorexia Weight loss Nausea Abdominal pain Diarrhea Xerostomia Constipation ** tics motor or phonetic May be unmasked* * Black Box warning sudden death with structural cardiac abnormalities*** Others- armodafinil (Nuvigil), modafinil (Provigil), Guanfacine (Intuniv), Clonidine (Kapvay) 17. At what age can medications for ADHD be prescribed? 6 YEARS AND UP Meds 6 and up RX of younger than 6 is off label 18. Which is the longest acting stimulant? Long Acting: methylphenidate (AMPHETAMINE LIKE DRUG) SR Concerta ( 12 HOURS), Metadate CD, Ritalin LA, Methylin, Daytrana Transdermal System, amphetamine/dextroamphetamine Adderall XR, clonidine Kapvay Atomoxetine is metabolized by the 2D6 enzyme system. Its half-life is 4 hours in most patients, although this may be prolonged to 30 to 40 hours in poor metabolizers (7% of population). Nonstimulant alternatives: 19. Strattera/ atomoxetine Norepinephrine reuptake inhibitor used to treat ADHD As effective as stimulants Low abuse potential Black box increased risk of suicide Preg C Causes more vomiting and insomnia Norepinephrine reuptake inhibitors (Strattera- atomoxetine) not a controlled substance and it is not a stimulant MOA: reuptake of presynaptic norepinephrine. It does not bind to monoamine receptors in the brain, thereby decreasing the risk of adverse reactions compared with older norepinephrine reuptake inhibitors. Side effects: “black box” warning increased suicide risk, vomiting, insomnia, headache, rhinitis, upper abdominal pain, decreased appetite, constipation, increased cough, flu syndrome Half-life - Atomoxetine is metabolized by the 2D6 enzyme system. Its half-life is 4 hours in most patients, although this may be prolonged to 30 to 40 hours in poor metabolizers (7% of population). 20. Clonidine derivatives eg guanfacine (intuniv)- these tend to be most effective in younger boys with hyperactivity symptoms and can be helpful with insomnia armodafinil (Nuvigil), modafinil (Provigil), Guanfacine (Intuniv), Clonidine (Kapvay) Use in children younger than 6 years of age is off-label. Most effective in younger boys Hyperactive SX and insomnia Stimulate alpha 2 adrenoreceptors, reduce sympathetic outflow 21. Buproprion (wellbutrin) (it is an off-label use) – consider in adolescent who also has depressive symptoms Off label for ADHD CONSIDER IN ADOLESCENT WHO HAD DEPRESSION SX NOTE WITH ANY ALPHA AGONISTS OR ANTIDEPRESSANTS RISK FOR ADVERSE CARDIAC EVENTS 22. Know the treatment of Alzheimer’s and the education behind the medication management of the disease. (When are each of them indicated? What is their benefit?) cholinesterase inhibitors. Cholinesterase inhibitors (ChE inhibitors (this abbreviation may be seen on the exam) eg donepezil: Can be used at any stage; Helps with functioning Donepezil SEVERE Rivastigmine MILD TO MOD Galantamine MILD TO MOD THIS CLASS IS CONSIDERED 1ST LINE SPECIFICALLY DONEPEZIL, GALANTAMINE ER , and RIVASTIGMINE DUE TO THEIR ONCE A DAY DOSING THESE DRUGS ARE SHOWN TO DELAY PROGRESSION OF DEMENTIA SX THUS IMPROVING FUNCTION DOES NOT HALTER DISEASE OR CURE NMDA Receptor Antagonists - Memantine for moderate to late stages; can be added to ChE inhibitors Memantine PREVENT COGNITIVE DAMAGE WIRH VASCULAR DEMENTIA MANAGEMENT MOD TO SEVERE DEMENTIA STAGES 5-7 Global Deterioration Scale = START MEMANTINE WITH DONEPEZIL Do not change doses Initial and long term term side effects GI SX common , sleep disturbances Explain purpose expectations time frame versus no cure Behavioral and environmental management Long term care May need to take Donepezil during day of sleep effected take fill or empty stomach Do not switch meds until after 6 months Only change meds if lack efficacy, initial response then fail, safety issues * increase or decrease dose before changing meds** Parkinson Disease: Drugs including 23. Levodopa/carbidopa – monotherapy or adjunctive; most effective therapy for slowness, stiffness, tremor; can cause dyskinesias (abnormal movements) Dopamine Precursors Carbidopa Carbidopa / Levodopa * 1st Line MOST EFFECTIVE* Effect of protein on absorption of levodopa-They compete for absorption. From what I can find on the internet eat carbs in the day (levodopa in the morning) and proteins at night DOPA all drugs have DOPA suffix- ** can cause dyskinesias (abnormal movements) monoamine oxidase B (MAO-B) inhibitors Selegiline - MAOI (eg selegiline) – monotherapy for slowness, stiffness therapy; adjunctive as well for motor fluctuations – wearing off phenomena Rasagiline *1st Line drug* Mono therapy for slowness stiffness Adjunct for motor fluctuations ** WEARING OFF PHENOMENA 3 glutamate Antagonists modulators Amantadine Amantadine – not the most effective but can be tried as adjunctive therapy for classic PD sx of slowness, stiffness and tremor Dopamine Agonists Apomorphine - . Apomorphine – ANTIVIRAL DOPAMINE AGONIST used for late stage PD as an adjunctive therapy for wearing off symptoms Pramipexole- Pramipexole – this is a dopamine agonist and can be used as mono or adjunctive therapy for classic PD sx Ropinirole Bromocriptine Canergoline 5- anticholinergic agents Benztropine- Benztropine – this is an anticholinergic that can be used to treat tremor in younger patients with PD; it can also be used to treat excessive drooling; anticholinergics can cause confusion, hallucinations, dry mouth, blurred vision and urinary retention (anticholinergic adverse effects more commonly a problem for older patients) Trinexphenidyl Diphenhydramine 6- catechol-O- methyl transferase COMT inhibitors Tolcapone Entacapone Depression medications including 24. SSRIs **1ST LINE DRUGS** Abrupt SSRI discontinuing = withdraw, flu like, rebound depression Except FLUOXETINE doesn't require taper Avoid SSRIs with linezolid, MAOIs, Lithium All have risk of SI until age 24 ⬆️ risk of SIADH, hyponatremia – WITH OLDER ADULTS Typically RX for elderly - Effective less toxic FLUOXETINE FOR ELDERLY *** SAFE IN OVERDOSE * Drugs: Fluoxetine ALOT of drug interactions Fluvoxamine Vilazodone Citalopram- avoid in renal, QT prolonged Escitalopram - avoid in Renal Sertraline Paroxetine - **weight gain, sexual dysfunction sedation, AVOID IN OLDER ADULTS DUE TO INCREASED RISK OF SEDATION AND DRUG INTERACTIONS 25. SNRIs Drugs Venlafaxine **1st Line increases BP 2nd lines Duloxetine Milnacipran Desvenlafaxine The DMD fights with the V for first place 26. Recognition that the SNRI duloxetine can be used for pain management as well It has official approval for both OA and fibromyalgia and neuropathic pain. Can be used for pain management Official use for OA Fibromyalgia Neuropathic Pain 27. Which SSRI is approved for use in children/teen? Fluoxetine 8 and up Others only 18 and up 28. Monitoring of depression. Monitor depression - labs etc All antidepressants- weight TCAs - ECG, CBC, LFTs, Glucose SSRIs - CBC, Electrolytes SNRIs - BP , Electrolytes Depression monitoring Most drugs are preg C or even D **Reserve for severe depression in pregnancy typically either fluoxetine or sertraline Acute TX phase- DX to 6/8 weeks Low dose and titrate up.. effects not seen until few weeks No response in 8-12 weeks slow titrate down and change drug Continuation phase - 16-20 weeks Preserve remission Maintenance phase - 4-9 months dose reduction not recommended Discuss plan to continue vs tapering off Depression monitoring Caution with MANY DRUG COMBINATIONS THAT ARE NOT COMPATIBLE ALSO ALL ANTIDEPRESSANTS MONITOR RISK OF SI ESP WITH TCAS PT MAY PLAN TO OD 29. Side effects of antipsychotics Extrapyramidal sx : acute / tardive SX ( dystonia, akathisia, tremor) More common in high potency drugs Monitor and assess at each encounter using the Use of the Abnormal Involuntary Movement Scale TD May be irreversible Clozapine has low rate of EPS and TD Acute phase of TX Begin antipsychotics dose low and titrate slow Several weeks Do not exceed dose that causes EPS Provide adjunct TX : BB, benzo, antidepressants, mood stabilizers Stable phase of TX Do not decrease dose to limit EPS it may also cause relapse of SX Once therapeutic effect is met, then attempt to decrease dose for long term maintenance Men younger than 40 and women at greater risk Remember TD is abnormal involuntary movements Progressive or irreversible Rhythmic movements of tongue, face, mouth Major limitation of 1st gen antipsychotics 2nd gen antipsychotics are used to decrease the risk of EPS : Dibenzepines, Benzisoxazoles, Quinolinones 30. What is the side effect of antipsychotics that can lead to abnormal rhythmic movements? How should this be managed? Acute phase of TX Begin antipsychotics dose low and titrate slow Several weeks Do not exceed dose that causes EPS Provide adjunct TX : BB, benzo, antidepressants, mood stabilizers Stable phase of TX Do not decrease dose to limit EPS it may also cause relapse of SX Once therapeutic effect is met, then attempt to decrease dose for long term maintenance 31. Serentil- Mesoridazine Phenothiazines- piperidines 1st generation antipsychotic Really not other info in book except dose.. Medscape doesn't even list it.. maybe off market? On lesson week 4 it's listed as a low potency 1st gen with high incidence of sedation, anticholinergic effects ,, 32. Lab monitoring required with Clozaril Clozapine: Monitor weekly CBC with differential, in keeping with the manufacturer's protocol. The manufacturer maintains a confidential register (800-448-5938); patients must be enrolled and have a baseline white blood cell (WBC) count and absolute neutrophil (ANC) count before initiation of therapy. Treatment should not be initiated if the baseline WBC is <3500/mm3 or ANC is <2000/mm3. Issue of weekly supplies of the drug is dependent on the results of the weekly white blood cell count; the results are sent to the national registry via forms supplied by the manufacturer. If after 6 months of weekly monitoring, the WBC has continuously remained ≥3500/mm3 and the ANC has remained ≥2000/mm3, the monitoring of blood counts through the registry may be reduced to every 2 weeks for 6 months. If acceptable WBC and ANC counts (WBC ≥3500/mm3 and ANC ≥2000/mm3) have been maintained during the second 6 months of continuous therapy, WBC and ANC may then be monitored every 4 weeks starting at the end of the 12 months and thereafter. page 557, Edmunds, M. W., & Mayhew, M. S. (2014). Pharmacology for the Primary Care Provider. Saint Louis: Elsevier Health Sciences. 33. Side effects of carbamazepine and lab monitoring 2nd gen antipsychotics *significant risk of agranulocytosis * Monitor leukocyte count (WBC) CBC with diff before, every week, and weekly 4 weeks after DC Aplastic anemia and agranulocytosis, although rare, have been reported in association with carbamazepine therapy. (Edmunds 500) Side effects: Rare but serious Aplastic anemia & agranulocytosis Benign leukopenia Mild anticholinergic— use caution with increased intraocular pressure, confusion/agitation elderly Exacerbated SZ in mixed SZ DO Ok for kids under 6 Preg D Monitor CBC before TX Repeat CBC q 3 months for first year Baseline and periodic liver function Baseline and periodic urinalysis- SIADH baseline and periodic eye exams 34. Know first line treatment for generalized seizure management (eg Dilantin) not adjunct therapies Generalized tonic clonic SZ Phenytoin - hydantoins Carbamazepine - misc drug Phenobarbital - barbiturates Valproic Acid - GABA analogs Topiramate - GABA analogs Generalized epilepsy : Beneficial Carbamazepine - misc Phenobarbital - barbiturates Phenytoin - hydantoins Valproate GABA analogs Note GABA drugs are newer drugs GU: 35. Be familiar with Beer’s Criteria Explicit not evidence based guidelines techniques for assessing appropriateness of drugs RX to elderly Many drugs that are high risk for ADRs and likely to produce ADRs are identified Topics include Decreased Renal clearance Decreased hepatic clearance Meds to avoid over 65 yrs the beers short list: sedating antihistamines, sedative hypnotics, sedating antidepressants, antispasmodic, Meds to avoid over 65 long list Anticholinergic Sedating antihistamines Ticlopidine Methyldopa Resperine Disopyramide Meperidine Propoxyphene Barbiturates Benzos Increased risk for physical performance decline Drugs on concern Analgesics Antibiotics Anticholinergics Antihistamines Antiparkinsons Benzos Barbituates Cardiovascular Muscle relaxants Proton pump inhibitors Psychotropics Remember drugs with strong anticholinergic properties Antihistamines Antidepressants *TCAs Antimuscarinics Antipsychotics Antispasmodics Skeletal muscle relaxers 36. Evaluation of incontinence – initial steps Initial steps Focused assessment Voiding diary UA / PVR TX based on type of incontinence Stress incontinence SNRIs, estrogen cream, ring, imipramine, pseudoephedrine Urge incontinence 1st line Oxybutynin, darifenacin, solifenacin, tolterodine, trospium 37. Meds for erectile dysfunction know which have a quick onset of action. – which has quickest onset: tadalafil (Cialis), sildenafil (Viagra), avanafil (Stendra) or vardenafil (Levitra)? PDE5 inhibitors sildenafil (Viagra), tadalfil (Cialis), vardenafil (Levitra), avanafil (Stendra) are the 1st line unless contraindicated. Vardenafil ( levitra) 60 mins prior Sildenafil (viagra) 30 mins to 4 hours prior Tadalafil (Cialis) 30-45 mins prior ** avanafil ( Stendra) newest drug shortest 1/2 life, 30 mins prior some have effect in 15 mins*** Lower dose of sildenafil with ritonavir, ketconaxole, itraconazole, erythromycin. Vardenafil may prolong QT. Other treatments- Hormone replacement therapy in cases of documented androgen deficiencies without contraindications. Alprostadil (MUSE)-intrathecal placement of pellet in urethra, initial dose must be done under healthcare supervision due to risk of syncome. Yohimbe (herbal) pg 389-391 38. Why should we avoid use of chronic nitrofurantoin in older adults? (See Geriatric lecture) Peripheral neuropathy, pulmonary & hepatic toxicity possible, avoid if CrCl less than 60 & neurotoxicity Endocrine: 39. Know the treatment and labs for Hyperthyroid and Hypothyroid (know normal TSH and T4 labs as well as pattern seen with hypo vs hyperthyroidism) Normal TSH. 0.3-5.5 Hyper TSH ⬇️ Hypo TSH ⬆️ Normal T4 5-12. Hyper T4 ⬆️. Hypo T4 ⬇️ Free T4 0.9-1.7. Hyper FreeT4 ⬆️. Hypo free T4 ⬇️ TX Hyperthyroidism Graves Disease 1st line Radioactive iodine - pretx in cardiovascular /elderly with anti-thyroid 2nd line surgery 3rd line anti thyroid meds: Methimazole perverted ***except 1st trimester than do propylthiouracil PTU tx hypothyroidism 1st line levothyroxine pure T4 safe in pregnancy L-thyronine pure T3 rarely used 40. What dose of levothyroxine should be started in a patient who has coronary artery disease? Start with 25mcg daily ***Note usual maintenance dose is 75-150 mcg daily 41. How often should one obtain a TSH when initially treating hypothyroidism? Monitor monthly until stable 42. Know what labs indicate Hypothyroid and which indicate Hyperthyroid Labs indicating hypothyroidism: Elevated ⬆️ TSH with low circulating levels of free (unbound) T3 & T4 Labs indicating hyperthyroidism: Low ⬇️ or undetectable TSH with high circulating levels of T3&T4 42. Know side effects of hyperthyroid medications For both PTU now with black box for liver damage & Methimazole ( preferred over PTU) potential agranulocytosis, thrombocytopenia, aplastic anemia ***monitor CBC Hepatotoxic *** AST, ALT, LDH, bilirubin, PT, alkaline phosphate GI irritation 43. How to monitor methimazole therapy- pg 587 Monitor every 3-6 weeks. Monitor for signs of infection and decreased pluse, BP, weight, elimination of nervousness and tremor. Potential for hepatoxicicity, AST, ALT, alkaline phosphatase, LDH, bilirubin, & PT. 44 . What is the typical course of congenital hypothyroidism – will the child always need thyroid replacement? Can possibly stop therapy at 3 years of age. Then recheck thyroid to see if it is still needed Child typically needs higher dose of meds until age 3 to meet metabolic demands TX may be stopped 2-8 weeks after child turns 3 If TSH levels remain normal the TX is DC permanently 45. Know how to prescribe oral diabetic medications and what labs to monitor. Mono therapy HbA1C < 7.5 Multiple agents A1C> 7.5 In order of recommendations Biguanides : Metformin MONITOR RENAL OBTAIN eGFR GLP-1 Receptor Agonists : Exenatide Liraglutide SGLT2 Inhibitors: canaglifozin empaglifozin DPP-4 inhibitors : Sitagliptin, saxagliptin, linagliptin TZDs: glitazone, ploglitazone, rosiglitazone Alpha glucosidase inhibitors : acarbose, miglitol MONITOR LFT Q 3 MONTH Amylin mimetic: pramlintide Amylin is a hormone Meglitinides : glinides, Sulfonylureas : Glipizide, Glyburide, Glimepiride MONITOR CBC, RENAL All start with G end in IDE REMEMBER DIET & EXERCISE ALWAYS FIRST 46. Know first line medication management in Type II Diabetes. 1. first line: Metformin If liver disease consider Sulfonylureas Per the textbook 2nd line agents include Sulfonylureas DPP-4 Meglintinides Alpha glucosidase inhibitors Pregnant use typically recommend changing to insulin Metformin, glyburide , glipizide used Metformin cat B Glyburide for gestational DM Type 2 DM with renal disease Non obese 2nd gen Sulfonylureas Obese Alpha glucosidase inhibitors Other choice for both: thiazolidinedione’s 47. Know first line oral diabetes management in a patient with and without renal disease. NORMAL RENAL FUNCTION NON-OBESE metformin Thiazolidinedione’s TZD 2nd gen Sulfonylureas Non-Sulfonylureas secretagogues (erratic meals) OBESE ELEVATED FASTING BLOOD SUGAR metformin TZD 2ng gen Sulfonylureas Incretins ELEVATED POSTPRANDIAL BLOOD SUGAR nonSulfonylureas secretagogues if erratic meals Alpha glucosidase inhibitors 2nd gen Sulfonylureas IMPAIRED RENAL FUNCTION NON-OBESE 2nd gen Sulfonylureas nonSulfonylureas secretagogues if erratic meals TZD OBESE Alpha glucosidase inhibitors TZD Sulfonylureas Incretins DM: 48. Preferred first line oral agent- Metformin 1st line- metformin, biguinide moa-decreases hepatic glucose production, ASSESS RENAL FUNCTION RISK FOR LACTIC ACIDOSIS 49. Vitamin deficiency associated with this drug (Metformin) B12 50. Side effects of this drug (Metformin) side effects- b12 deficiency, n/v/d, chills, rash, no wt. gain, dyspnea, lactic acidosis, hypoglycemia, metallic taste contraindicated- renal dysfunction, metabolic acidosis, dka, hold for iodine contrast imaging Vit B12 deficiency = Anemia & neuropathy LACTIC ACIDOSIS GI SX 51. MOA and side effects of acarbose pg 493 acarbose (precose)- alpha-glucosidace inhibitor (** hypoglycemia occurs less with this vs other drugs**) contraindicated- dka, cirrhosis, IBS, intestinal obstructions warning-carcinogenic x renal tumors MOA: it's an alpha glucosidase inhibitors, slows intestinal carb digestion and absorption Side effects : GI - flatulence diarrhea Elevate LFTs 52. MOA and side effects of canaglifozin canaglifozin SGLT-2 inhibitor MOA: inhibits SGLT2 in proximal nephron which blocks glucose reabsorption by kidney increasing glucosuria Side effects Yeast infection Polyuria Volume depletion Hypotension Dizzy Falls/FX Increased amputations Increased LDL Increase Cr DKA UTI Hyperkalemia reduced bone density From our discussion board gluscouria = Canaglifozin is working ENT: 53. Know the treatment for Otitis Media and Otitis Externa TX for Otitis Media Amoxicillin 80-90 mg/kg/day divide bid x 5-10 days Alternative Amoxicillin / Clavulanate (recent amox use ), cefuroxime, cefdinir, cefpodoxime, ceftriaxone IM Alternative TMP/SMX -s. Pneumoniae resistant to bactrim Azithromycin Clindamycin Tx failure Amox/clav Cetrixone IM x3 days Clindamycin Referal Hold antibiotics over 2, not severely ill, follow up ensured , tx can start if SX persists.. 60% will resolve without meds Otitis media with effusion Without evidence of infection Watch non high risk Persists 3 months hearing testing TX Otitis Externa Acetic acid, boric acid, benzalkonium chloride, aluminum acetate (burow's solution) antibacterial and antifungal properties Cipro otic solution Possibly add steroids: cortisporin otic solution 54. Preferred medication for impetigo (honey crusted skin lesions)? What are the recommended therapies if the impetigo is in a limited area vs more extensive? Oral dicloxacillin is the first choice. Bactroban may also be applied topically for mild lesions. First choice oral dicloxacillin Mupirocin- bactroban topical also effective cheaper Other alternatives Azithromycin Clarithromycin Erythromycin Cephalexin 55. Preferred first line antibiotic for acute OM including dose and management of otorrhea in a patient who has tympanostomy tubes per lecture slide: 1st line treatment-Amoxicillin 80-90mg/kg/day divided BID for 5-10 days. Alternative-Augmentin, cefuroxime, cefdinir, cefpodoximine, ceftriaxone IM. *if recent amoxicillin use, Augmentin is 1st line. If PCN allergy-TMP/SMX, axithromycin, clindamycin. If no improvement in 2-3 days, change to Amox/Clav, Ceftriaxone IM x 3 days, clindamycin and consider referral to specialist. Otorrhea with tympanostomy tubes-quinolone otic drops. check hearing if effusion persists for 3 months or longer or at any time if significant hearing/language problem. 56. How should you manage OME? When should you check hearing in a patient who has OME? Hydrocortisone, neomycin sulfate, polymyxin-cortisporin otic Cipro and hydrocortisone suspension Cipro HC otic Hearing test after 3 months if effusion persists or at any time if significant hearing/language problem 57. How should you treat resistant AOM? No SX improvement 2-3 days suggests bacterial resistance After changing meds also consider tympanocentesis with the referral (See lecture slides under Course Resources) 58. Tx of otitis externa floroquinolones (pg. 692) patho book says commonly caused by pseudomonas, staph, and ecoli. pg. 516 GI/nutrition: 59. Know evaluation and treatment of IBS including specific medications and their side effects, assessment of abdominal pain, evaluation and tx of IBS Alternating constipation/diarrhea: • Increased dietary fiber (25 g/day) Pain • Antispasmodic (anticholinergic) medication—short term • TCAs—long term DIarrhea • Loperamide—short term; often used for breakthrough diarrhea • Antidepressants (TCAs)—long term • Alosetron (ordered by GI specialists) if resistant to all other interventions Constipation • Fiber, Laxitives CRAMPING ABDOMINAL PAIN Antispasmodic (anticholinergic) PRN if SX present shortly after meal ABDOMINAL PAIN FREQUENT OR SEVERE TCAs PAIN SX WITH DIARRHEA TCAs PAIN SX WITH CONSTIPATION SSRIs conflicting efficacy SIMETHICONE Use for problems with gas, explosive BM, belching, flatus LUBIPROSTONE AND POLYETHYLENE GLYCOL also RX for IBS 60. Tx of infant with oral candidiasis/thrush 1st line treatment: fluconazole 6 mg/kg x1 then 3-12 mg/kg x 2 week minimum (pg. 723) 61. Vitamin deficiency questions (eg what the symptoms of various vitamin deficiencies are?) Vitamin A- Fat soluble (Retinol, beta carotenes, carotenoids) Blindness Vitamin D (Vitamin D2, Ergocalciferol, d3, Cholecalciferol) Rickets, bowlegged, contracted pelvis, skull malformation, dental eruption delay Vitamin E (Alpha-tocopherol) BILIARY OBSTRUCTION OR PANCREATICE INFUFFCIENCY Vitamin K- for those who take Coumadin be careful it’s a clotting factor. It interferes with metabolism and absorption Vitamin B12 – disruption in GI in habits absorption, peripheral nervous system changes, central nervous system changes Folic acid- fetal neural tube defects, spinal bifida, anencephaly Vitamin C- scurvy , lack of repair of collagenous tissue causing muscle weakness 62. What vitamin deficiency is common with chronic alcohol abuse? Vitamin B1 Thiamine 63. What iron deficiency is associated with overconsumption of milk in toddlers? What is the screening test that should be ordered? Iron Deficiency Anemia Check CBC to confirm 64. What side effect can occur with salt substitutes? Hyperkalemia Potassium toxicity Confusion, fatigue, intestinal tract changes, irregular rapid HR, dropping BP, paralysis arms legs, convulsions, coma, cardiac arrest 66. Vitamins a vegetarian may require Vitamin B12 pg 796, Cobalt, zinc 67. How to prevent osteoporosis Sufficient intake of calcium Ability to absorb calcium - fat intake vs fiber fat may increase absorption Vit D for calcium utilization Risks Inadequate calcium Vit D deficiency High phosphorus intake soda processed meats eggs peanut Excessive calcium use - multiple pregnancies Steroids during bone building years Smoking cessation: 68. How to taper nicotine nasal spray pg 786 useful for patients with severe cravings and wants immediate relief. Fastest nicotine delivery, most closely resembles nicotine effects of smoking. Each spray delivers 0.5 mg of nicotine Normal dose 1-2 sprays per waking hour for 3-6 months Taper period half number of doses used each week Also 1-2 0.5 mg sprays each nostril/hour. Do not exceed 5 sprays/ hour or 40/sprays day. gradually reduce rate over 6-8 weeks pg 785 ID: 69. Tx of Rocky Mountain Spotted Fever? What to do if patient fails oral therapy? Pg 660 Doxycycline 100mg po bid x 7 days Fail oral TX Chloramphenicol 50mg/kg/day IV q 6 hrs x7 days 70. Know the indications for the use of Vancomycin pg 668 Vancomycin IV is used most often in serious or life-threatening staphylococcal or streptococcal infections. Pseudomembranous colitis caused by C-Diff oral form when flagyl not effective The primary care use of vancomycin is for pseudomembranous colitis caused by C. difficile. It is given in oral form when treatment with metronidazole is contraindicated or ineffective Prevents synthesis of the bacterial cell wall by blocking peptidoglycan strand formation. 71. Know Vancomycin mechanism of action pg 668 preventing synthesis of the bacterial cell wall by blocking peptidoglycan strand formation. pg668 Prevents synthesis of the bacterial cell wall by blocking peptidoglycan strand formation. 72. Know the mechanism of action of Cephalosporinspg 678 Cephalosporins interferes with bacteria cell wall (Bacteriocidal) Beta lactame - antibodies interfere with cell wall synthesis through inhibition of synthesis of bacterial peptidoglycan in cell wall 73. What class is erythromycin? Macrolides Analgesia: 74. Know the side effects of Acetaminophen When acetaminophen is used as directed, adverse effects are rare. Skin eruptions, urticaria, erythematous skin reactions and fever, increases asthma in kids, Extremely rare hematologic reactions include hemolytic anemia, leukopenia, neutropenia, and pancytopenia. Other reactions are hypoglycemia and jaundice. Adverse effects are usually dose dependent. Hepatic toxicity may occur following intake of >7.5 g within 8 hours. Alcoholics and patients on hepatic metabolizing medications are more susceptible to hepatic toxicity. This is very important because hepatic toxicity can be caused by binge drinking. 75. Know the signs of Acetaminophen toxicity Symptoms that appear in the first 24 hours are o nausea, o vomiting o drowsiness o lethargy o malaise o confusion. 76. NSAID side effects; use of topical NSAIDs GI upset, dizziness, headaches, bleeding, fluid retention HA, increased sweating, photosensitive, rash, pruritus, urticaria, Steven Johnson's syndrome, toxic epidermal necrolysis, anaphylaxis pulmonary infiltrate, asthma, tachycardia, palpitation, HTN, MI, HF, arrhythmia, PE AFib, GI bleeding, N/V, constipation, dyspepsia. Flatulence, CVA, confusion, sedation, blurred vision, tinnitus, hearing loss, vertigo, increased LFTs low Cr hyperkalemia, renal, Use of topical NSAIDs o Capsaicin for OA 77. Know the difference between nonselective vs selective NSAIDs pg 407 Nonselective more GI issues COX1&COX2 COX 1 responsible for GI Selective are COX2 not as much GI issues 78. Know the Management of Osteoarthritis APAP 1st line long term - be effective in treating the pain of OA because many patients have minimal inflammation. If not effective then NSAIDS for flares o Intraarticular injection of steroids for knee hip mod to severe pain- NSAIDs can be used. NSAIDs are more effective than acetaminophen for OA of the knee or hip. They are also more effective in moderate to severe disease. Some patients’ conditions can be managed via long-term acetaminophen therapy with short-term use of NSAIDs for flare-ups. Because of the decreased risk of GI toxicity, Non pharm exercise with rest weight loss o A supervised walking program can improve functional status. Recommend weight loss to overweight patients to reduce strain on joints. The patient must be realistic about the limitations of medications and about his own prognosis. (Edmunds 409) COX-2 inhibitors are useful for long-term management of OA in elderly patients. Intraarticular injection of steroids can be provided on a limited basis. o Topical creams such as capsaicin can also help with the pain. Surgical measures such as hip or knee replacement may be necessary in joints that are seriously affected. (Edmunds 409) PPT= Aspirin and Celecoxib (cox-2) 79. Know acetaminophen toxicity, and indications in children Acetaminophen is used commonly for pain and fever in children and generally is well tolerated. Use caution to avoid over dosage. Acute over dosage of acetaminophen can result in hepatotoxicity and is life threatening. Toxicity is likely to occur if a patient takes more than 250 mg/kg in a single dose or greater than 12 g within a 24-hour period. After 24 hours up until 72 hours, symptoms abate and liver toxicity (AST/ALT elevation) normally occurs. An increase in liver enzymes within 24 hours is a sign of permanent injury. Liver enzyme elevation usually peaks at between 72 and 96 hours after ingestion, along with other markers of liver function such as the INR and a total bilirubin concentration above 4. The last stage, which consists of recovery, lasts anywhere from 4 days to 2 weeks; recovery is complete in many cases. The patient should immediately receive activated charcoal. Further treatment should take place in a hospital setting with the patient receiving N-acetylcysteine (NAC), the specific antidote for acetaminophen poisoning . Acetaminophen is metabolized in the liver. Toxic metabolite is detoxified with hepatic glutathione. Hepatic necrosis can occur if glutathione stores have been depleted by long-term or toxic doses of acetaminophen. Children at increased risk for acetaminophen toxicity include those with diabetes, concomitant viral infections, a family history of hepatotoxic reactions, obese children, and chronically malnourished children. More than 250 mg/kg in a single dose or More than 12 G in 24 hours 350mg/kg severe hepatotoxicity life threatening o N/V drowsy lethargy, malaise, confusion Elevated AST, ALT Tx activated charcoal and n-acetylcysteine IV o Children: High risk for APAP toxicity Failure to give correct dose, dose may be confusing Children with DM, viral infections, family history of hepatotoxic reactions, obese, chronically malnourished at greater risk for toxicity 10-15 mg/kg oral 10-2 mg/kg rectal o Do not exceed 2.6 grams day Give every 4-6 hours [Show More]
Last updated: 1 year ago
Preview 1 out of 10 pages
Reviews( 0 )
Document information
Connected school, study & course
About the document
Uploaded On
Apr 14, 2021
Number of pages
10
Written in
Additional information
This document has been written for:
Uploaded
Apr 14, 2021
Downloads
0
Views
58



.png)