*NURSING > EXAM REVIEW > NR 602 Week 6 Quiz With Answers Completed A (All)
NR 602 Week 6 Quiz With Answers Completed A
Document Content and Description Below
NR 602 Week 6 Quiz Anovulation Anovulation is the failure of the ovary to release ova over a period of time generally exceeding 3 months. The normal functioning ovary releases one ovum every 25–2... 8 days. This average time between ovulation events is variable, especially during puberty and the perimenopause period.1 For nonpregnant women aged 16–40 anovulation is considered abnormal and a cause of infertility in 30% of fertility patients.2 One of the cardinal signs of anovulation is irregular or absent menstrual periods. Oligomenorrhea is defined as more than 36 days between menstrual cycles or fewer than eight cycles per year.3 In the absence of pregnancy, menstruation follows ovulation by approximately 14 days. Because menstruation is linked to ovulation, the clinical finding of oligomenorrhea correlates with oligoovulation. This predictable pattern of ovulation and menstruation is regulated by a cyclic change in hormones. Consequently, the diagnosis of ovulation dysfunction includes the assessment of the hormones and systems involved in ovulation and not just the symptom of amenorrhea. The most important consideration in the workup of anovulation is to determine the patient’s goals. Treatment of the patient who wants to get pregnant differs from that of the patient who is concerned about the risks of early menopause. In patients who desire pregnancy, the clinician needs to determine if they are actively trying for pregnancy, or are planning for pregnancy several years in the future. The approach outlined below begins with the patient who is actively trying for pregnancy. History Many patients with anovulation will present with amenorrhea. Primary amenorrhea is failure to menstruate and no secondary sexual characteristics by age 14 or no menstruation by age 16 with normal sexual development.129 Secondary amenorrhea is the cessation of menstruation for more than 3 months.130 The etiologies of primary and secondary amenorrhea differ. Primary amenorrhea is often seen in congenital disorders.131 The most common cause of secondary amenorrhea in women of childbearing age is pregnancy, consequently the workup for anovulation should begin with a pregnancy test. Details of a patient’s previous medical history can direct the evaluation of anovulation. Chronic disease can affect ovulation and may increase risks during pregnancy.132 Psychiatric problems are also often associated with ovulation dysfunction. The use of any antipsychotic medications should be noted.40 Details of previous pregnancies are likewise important in the evaluation of ovulation and can help distinguish genetic disorders from later onset anovulation. Physical The physical exam should include an evaluation of vital signs, height, weight, BMI, and appearance. Obesity is commonly associated with anovulation and PCOS.77 Very thin patients may have anorexia or nutritional deficits. Hirsutism may suggest PCOS, CAH or an androgen secreting tumor. Visual field testing is useful in patients who report visual changes suggesting a pituitary tumor. Palpation of the thyroid and abdomen should also be performed to evaluate for masses. Evaluation of the patient with primary amenorrhea should include a bimanual exam to determine the presence of a patent outflow tract and uterus. Laboratory tests In patients with amenorrhea, pregnancy should be considered and a pregnancy test performed early in theworkup. Evaluation of the HPO axis should be performed in a stepwise fashion. Serum estradiol and gonadotropins determine ovarian function. FSH measurements have been standardized for day 3 of the menstrual cycle. However, in patients with amenorrhea a random FSH is appropriate. Measurement of LH has limited clinical use. The ratio of LH to FSH has been studied for PCOS but is not included in the definition of the syndrome and is therefore not necessary.77 Elevated FSH indicates an ovarian problem. In patients under 30 years old with an elevated FSH, a karyotype should be performed. An increased risk of ovarian cancer is seen in XY females with gonadal dysgenesis.133 Turner syndrome (45,XO) is associated with increased risk for cardiovascular, thyroid, and renal disease.134 For these patients, a karyotype is very useful in the workup particularly relating to future pregnancy and health. In patients with elevated FSH and a normal karyotype, ovarian resistance and POI are considered. A trial of ovulation induction may be performed using clomiphene citrate as described later. If there is no benefit of clomiphene, exogenous gonadotropins may be effective. Normal or decreased FSH values suggest dysfunction of the HPO axis. Subsequent testing includes prolactin, TSH, and T4. Thyroid abnormalities are very common and may be seen in up to 4% of patients with infertility.135 Treatment for thyroid disease often restores HPO axis function. Hyperprolactinemia should direct the clinician to obtain an MRI of the pituitary. Serum prolactin levels greater than 250 μg/L are seen in prolactin secreting macroadenomas.136 Macroadenomas may require surgery, while many microadenomas can be successfully treated with medical therapy.137 In patients with signs of hirsutism, serum androgens including testosterone and dehydroepiandrosterone (DHEAS) can be evaluated. A testosterone level is a useful androgen test in determining the cause of hirsutism in women.138 Elevated free testosterone is seen in 70% of women with PCOS. Due to technical limitations in testing for free testosterone, measurement of total testosterone can be used. DHEAS is produced primarily from the adrenal gland and elevated levels suggest an adrenal tumor. Many androgen-secreting tumors, however, cause severe signs of hyperandrogenism including virilization and clitoromegally.139 A normal DHEAS level should direct attention to the ovary as the origin of excess androgens. Another useful hormone test in hirsutism is 17-hydroxyprogesterone. This is produced in the adrenal gland and the ovary, and is elevated in CAH. Most patients with hirsutism and PCOS will have elevated testosterone levels, while only 25–35% will have elevated DHEAS.138 An additional laboratory test for patients with PCOS is a 2-hour GTT.85 This test involves examining insulin and glucose levels following administration of a 75 g glucose bolus.140 The glucose tolerance test is useful for determining insulin resistance. Additionally, obese PCOS patients are at increased risk for dyslipidemia and metabolic syndrome and a serum lipid profile is appropriate.141 Elevated lipid levels, particularly in young patients, may increase the risk of cardiovascular disease later in life. Diet, weight loss, and lifestyle modifications should be recommended to patients with metabolic syndrome risks. Imaging tests Ultrasound is an invaluable tool for the evaluation of gynecologic problems including the assessment of ovarian architecture, which is a criterion for the diagnosis of PCOS. Transvaginal ultrasound provides a reliable measurement of the thickness of the endometrial lining.142 A thickened endometrial lining suggesys the presence and effect of estrogen. Long term anovulation leads to chronic estrogen stimulation of the uterus and increases the risk of uterine cancer.143 Since there is not good correlation between thickness and absence of endometrial hyperlasia or cancer,144 it is justified to sample the endometrial lining in chronic anovulatory patients independent of the endometrial thickness. Ultrasound can also be used to evaluate the ovaries and measure the number antral follicles. Antral follicle count is a sensitive test for determining ovarian reserve and response to ovarian stimulation.145 A low number of antral follicles during the follicular phase of the menstrualcycle is an indication of poor ovarian reserve. Ultrasound evaluation of the ovary is useful in the diagnosis of PCOS. To satisfy the definition of polycystic ovaries, each ovary must contain more than 12 follicles 2–9 mm in size or a calculated ovarian volume more than 10 mL.146 Abnormal/Dysfunctional Uterine Bleeding Essentials of Diagnosis Abnormal uterine bleeding includes abnormal menstrual bleeding and bleeding due to other causes such as pregnancy, systemic disease, or cancer. In childbearing women, a complication of pregnancy must always be considered. Exclusion of all possible pathologic causes of abnormal bleeding establishes the diagnosis of dysfunctional uterine bleeding (nearly 60% of cases). General Considerations Abnormal uterine bleeding includes abnormal menstrual bleeding and bleeding due to other causes such as pregnancy, systemic disease, or cancer. The diagnosis and management of abnormal uterine bleeding present some of the most difficult problems in gynecology. Patients may not be able to localize the source of the bleeding from the vagina, urethra, or rectum. In childbearing women, a complication of pregnancy must always be considered, and one must always remember that more than 1 entity may be present, such as uterine myomas and cervical cancer. Patterns of Abnormal Uterine Bleeding The standard classification for patterns of abnormal bleeding recognizes 7 different patterns. Menorrhagia (hypermenorrhea) is heavy or prolonged menstrual flow. The presence of clots may not be abnormal but may signify excessive bleeding. “Gushing” or “open-faucet” bleeding is always abnormal. Submucous myomas, complications of pregnancy, adenomyosis, IUDs, endometrial hyperplasias, malignant tumors, and dysfunctional bleeding are causes of menorrhagia. Hypomenorrhea (cryptomenorrhea) is unusually light menstrual flow, sometimes only spotting. An obstruction such as hymenal or cervical stenosis may be the cause. Uterine synechiae (Asherman's syndrome) can be causative and are diagnosed by a hysterogram or hysteroscopy. Patients receiving oral contraceptives occasionally complain of light flow and can be reassured that this is not significant. Metrorrhagia (intermenstrual bleeding) is bleeding that occurs at any time between menstrual periods. Ovulatory bleeding occurs midcycle as spotting and can be documented with basal body temperatures. Endometrial polyps and endometrial and cervical carcinomas are pathologic causes. In recent years, exogenous estrogen administration has become a common cause of this type of bleeding. Polymenorrhea describes periods that occur too frequently. This usually is associated with anovulation and rarely with a shortened luteal phase in the menstrual cycle. Menometrorrhagia is bleeding that occurs at irregular intervals. The amount and duration of bleeding also vary. Any condition that causes intermenstrual bleeding can eventually lead to menometrorrhagia. Sudden onset of irregular bleeding episodes may be an indication of malignant tumors or complications of pregnancy. Oligomenorrhea describes menstrual periods that occur more than 35 days apart. Amenorrhea is diagnosed if no menstrual period occurs for more than 6 months. Bleeding usually is decreased in amount and associated with anovulation, either from endocrine causes (eg, pregnancy, pituitary-hypothalamic causes, menopause) or systemic causes (eg, excessive weight loss). Estrogen-secreting tumors produce oligomenorrhea prior to other patterns of abnormal bleeding.Contact bleeding (postcoital bleeding) is self-explanatory but must be considered a sign of cervical cancer until proved otherwise. Other causes of contact bleeding are much more common, including cervical eversion, cervical polyps, cervical or vaginal infection (eg, Trichomonas), or atrophic vaginitis. A negative cytologic smear does not rule out invasive cervical cancer, and colposcopy, biopsy, or both may be necessary. Evaluation of Abnormal Uterine Bleeding Detailed history, physical examination, cytologic examination, pelvic ultrasound, and blood tests are the first steps in the evaluation of abnormal uterine bleeding. The main aim of the blood tests is to exclude a systemic disease, pregnancy, or a trophoblastic disease. The blood tests usually include complete blood count, assay of the β subunit of human chorionic gonadotropin (hCG), and thyroid-stimulating hormone (TSH). History Many causes of bleeding are strongly suggested by the history alone. Note the amount of menstrual flow, the length of the menstrual cycle and menstrual period, the length and amount of episodes of intermenstrual bleeding, and any episodes of contact bleeding. Note also the last menstrual period, the last normal menstrual period, age at menarche and menopause, and any changes in general health. The patient must keep a record of bleeding patterns to determine whether bleeding is abnormal or only a variation of normal. However, most women have an occasional menstrual cycle that is not in their usual pattern. Depending on the patient's age and the pattern of the bleeding, observation may be all that is necessary. Physical Examination Abdominal masses and an enlarged, irregular uterus suggest myoma. A symmetrically enlarged uterus is more typical of adenomyosis or endometrial carcinoma. Atrophic and inflammatory vulvar and vaginal lesions can be visualized, and cervical polyps and invasive lesions of cervical carcinoma can be seen. Rectovaginal examination is especially important to identify lateral and posterior spread or the presence of a barrel-shaped cervix. In pregnancy, a decidual reaction of the cervix may be the source of bleeding. The appearance is a velvety, friable erythematous lesion on the ectocervix. Cytologic Examination Although most useful in diagnosing asymptomatic intraepithelial lesions of the cervix, cytologic smears can help screen for invasive cervical (particularly endocervical) lesions. Although cytology is not reliable for the diagnosis of endometrial abnormalities, the presence of endometrial cells in a postmenopausal woman is abnormal unless she is receiving exogenous estrogens. Likewise, women in the secretory phase of the menstrual cycle should not shed endometrial cells. Of course, a cytologic examination that is positive or suspicious for endometrial cancer demands further evaluation. Tubal or ovarian cancer can be suspected based on a cervical smear. The technique of obtaining a smear is important, because a tumor may be present only in the endocervical canal and may not shed cells to the ectocervix or vagina. Laboratories should report the presence or absence of endocervical cells. The current use of a spatula and endocervical brush has significantly increased the adequacy of cytologic smears from the cervix. Any abnormal smear requires further evaluation (see Chapter 48). Pelvic Ultrasound Scan Pelvic ultrasonography has become an integral part of the gynecologic pelvic examination. The scan can be performed either transvaginally or transabdominally. The transvaginal examination is performed with an empty bladder and enables a closer look with greater details at the pelvic organs. The transabdominal examination is performed with a full bladder and enables a wider, but less discriminative, examination of the pelvis. The ultrasound scan can add many details to the physical examination, such as a description of theuterine lining and its width and regularity (Fig. 38–1) and the presence of intramural or submucous fibroids (Fig.38–1), intrauterine polyps, and adnexal masses. Persistent thick and irregular endometrium is one of the preoperative predictors of endometrial pathology and demands further evaluation and tissue biopsy. All Menstrual Cycle Phases Uterine Cycle The events that occur in the uterus during the menstrual cycle terminate with the menstrual flow. By the end of each menstrual period, all but the deep layer of the endometrium has sloughed. Under the influence of estrogen secreted from the developing follicles, the endometrium regenerates from the deep layer and increases rapidly in thickness during the period from the fifth to 16th days of the menstrual cycle. As the thickness increases, the uterine glands are drawn out so that they lengthen (Fig. 4–6), but they do not become convoluted or secrete to any degree. These endometrial changes are called proliferative, and this part of the menstrual cycle is sometimes called the proliferative phase. It is also called the preovulatory or follicular phase of the cycle. After ovulation, the endometrium becomes more highly vascularized and slightly edematous under the influence of estrogen and progesterone from the corpus luteum. The glands become coiled and tortuous (Fig. 4–6), and they begin to secrete clear fluid. Consequently, this phase of the cycle is called the secretory or luteal phase. Late in the luteal phase, the endometrium, like the anterior pituitary, produces prolactin. The function of this endometrial prolactin has yet to be determined, though it has been suggested that prolactin may play a role in implantation. The endometrium is supplied by 2 types of arteries. The superficial two-thirds of the endometrium, the stratum functionale, is shed during menstruation and is supplied by the long, coiled spiral arteries. The deep layer, which is not shed, is called the stratum basale and is supplied by short, straight basilar arteries. When the corpus luteum regresses, hormonal support for the endometrium is withdrawn, causing vascular spasms in the spiral artery, ultimately leading to endometrial ischemia. The endometrium becomes thinner, which adds to the coiling of the spiral arteries. Leukocyte infiltration into the endometrial stroma initiates the breakdown of the extracellular matrix in the functionalis layer. Foci of necrosis appear in the endometrium and walls of the spiral arteries, which coalesce and lead to spotty hemorrhages that become confluent and ultimately produce menstrual flow. Spiral artery vasospasm serves to limit blood loss during menstruation and probably is produced by locally released prostaglandins. There are large quantities of prostaglandins in the secretory endometrium and in menstrual blood. Infusions of prostaglandin F2a (PGF2a) produce endometrial necrosis and bleeding. One theory of the onset of menstruation holds that in necrotic endometrial cells, lysosomal membranes break down and release proteolytic enzymes that foster the formation of prostaglandins from cellular phospholipids while promoting further local tissue destruction. From the point of view of endometrial function, the proliferative phase of the menstrual cycle represents the restoration of the epithelium from the preceding menstruation, while the secretory phase represents the preparation of the uterus for implantation of the fertilized ovum. The length of the secretory phase is remarkably constant, about 14 days. The variations seen in the length of the menstrual cycle are mostly due to variations in the length of the proliferative phase. When fertilization fails to occur during the secretory phase, the endometrium is shed, and a new cycle begins. Premenstrual Syndrome/ Premenstrual dysphoric disorder (PMDD) Essentials of DiagnosisSymptoms include mood symptoms (irritability, mood swings, depression, anxiety), physical symptoms (bloating, breast tenderness, insomnia, fatigue, hot flushes, appetite changes), and cognitive changes (confusion and poor concentration). Symptoms must occur in the second half of the menstrual cycle (luteal phase). There must be a symptom-free period of at least 7 days in the first half of the cycle. Symptoms must occur in at least 2 consecutive cycles. Symptoms must be severe enough to require medical advice or treatment. General Considerations Premenstrual syndrome (PMS) has been defined as “the cyclic occurrence of symptoms that are of sufficient severity to interfere with some aspects of life and that appear with consistent and predictable relationship to the menses.” Although the symptoms themselves are not unique, the restriction of the symptoms to the luteal phase of the menstrual cycle is pathognomonic of PMS. It is a psychoneuroendocrine disorder with biologic, psychological, and social parameters that is both difficult to define adequately and quite controversial. One major difficulty in detailing whether PMS is a disease or a description of physiologic changes is its extraordinary prevalence. Up to 75% of women experience some recurrent PMS symptoms; 20–40% are mentally or physically incapacitated to some degree, and 5% experience severe distress. The highest incidence occurs in women in their late 20s to early 30s. PMS is rarely encountered in adolescents and resolves after menopause. Evidence suggests that women who have suffered with PMS and premenstrual dysphoric disorder are more likely to suffer from perimenopausal symptoms. The symptoms of PMS may include headache, breast tenderness, pelvic pain, bloating, and premenstrual tension. More severe symptoms include irritability, dysphoria, and mood lability. When these symptoms disrupt daily functioning, they are clustered under the name premenstrual dysphoric disorder (PMDD). Other symptoms commonly included in PMS are abdominal discomfort, clumsiness, lack of energy, sleep changes, and mood swings. Behavioral changes include social withdrawal, altered daily activities, marked change in appetite, increased crying, and changes in sexual desire. In all, more than 150 symptoms have been related to PMS. Thus the symptom complex of PMS has not been clearly defined. Pathogenesis The etiology of the symptom complex of PMS is not known, although several theories have been proposed, including estrogen–progesterone imbalance, excess aldosterone, hypoglycemia, hyperprolactinemia, and psychogenic factors. A hormonal imbalance previously was thought to be related to the clinical manifestations of PMS/PMDD, but in the most recent consensus, physiologic ovarian function is believed to be the trigger. This is supported by the efficacy of ovarian cyclicity suppression, either medically or surgically, in eliminating premenstrual complaints. Further research has shown that serotonin (5-hydroxytryptamine [5-HT]), a neurotransmitter, is important in the pathogenesis of PMS/PMDD. Both estrogen and progesterone have been shown to influence the activity of serotonin and gamma-aminobutyric acid (GABA) centrally. Many of the symptoms of other mood disorders resembling the features of PMS/PMDD have been associated with serotonergic dysfunction. Disturbances in cortical GABA neuronal function and modulation by neuroactive steroids have been implicated as potentially important contributors to the pathogenesis of PMS/PMDD. GABA levels are decreased in women with PMS/PMDD during the late luteal phase compared with normal women. DiagnosisNo objective screening or diagnostic tests for PMS and PMDD are available; thus special attention must be paid to the patient's medical history. Certain medical conditions (eg, thyroid disease and anemia) with symptoms that can mimic those of PMS/PMDD must be ruled out. The patient is instructed to chart her symptoms during the month. According to the American College of Obstetricians and Gynecologists criteria, PMS can be diagnosed if the patient reports at least 1 affective symptom (depression, angry outbursts, irritability, anxiety, confusion, or social withdrawal) and somatic symptom (breast tenderness, abdominal bloating, headache, or swelling of extremities) during the 5 days before menses in each of the 3 prior menstrual cycles. These symptoms should be relieved within 4 days of the onset of menses, without recurrence until at least cycle day 13, and should be reproducible during 2 cycles of prospective recording. Clinical Findings A careful history and physical examination are most important to exclude organic causes of PMS localized to the reproductive, urinary, or gastrointestinal tracts. Most patients readily describe their symptoms, but careful questioning may be needed with some patients who may be reluctant to do so. Although it is important not to lead a patient to exaggerate her concerns, it is equally important not to minimize them. Symptoms of PMS may be specific, well localized, and recurrent. They may be exacerbated by emotional stress. Migraine-like headaches may occur, often preceded by visual scotomas and vomiting. Symptomatology varies among patients but often is consistent in the same patient. One of the most common symptoms of PMS is mastodynia, or mastalgia (pain, and usually swelling, of the breasts caused by edema and engorgement of the vascular and ductal systems). A positive correlation between degree of ductal dilatation and degree of breast pain has been documented. Mastodynia specifically refers to a cyclical occurrence of severe breast pain, usually in the luteal phase of the menstrual cycle, and it may be the primary symptom of this syndrome in some. It has been shown to be related to high gonadotropin levels. Estrogen stimulates the ductal elements, whereas progesterone stimulates the stroma. An augmented response to prolactin has also been suggested. Examination is always necessary to rule out neoplasm, although most malignant tumors are painless. The presence of solitary or multiple cystic areas suggests fibrocystic change. The diagnosis usually can be confirmed by aspiration, but excisional biopsy occasionally is necessary. Serial mammograms or ultrasound examinations can be used to help monitor these patients (see Chapter 5). A psychiatric history should be obtained, with special attention paid to a personal history of psychiatric problems or a family history of affective disorders. A mental status evaluation of affect, thinking, and behavior should be performed and recorded. A prospective diary correlating symptoms, daily activities, and menstrual flow can be useful to document changes and to encourage patient participation in her care. If underlying psychiatric illness is suspected, a psychiatric evaluation is indicated. The most common associated psychiatric illness is depression, which generally responds to antidepressant drugs and psychotherapy. Recall that psychiatric illnesses have premenstrual exacerbations, so medications should be altered accordingly. Treatment Treatment of PMS/PMDD depends on the severity of the symptoms. For some women, changes in eating habits—limiting caffeine, alcohol, tobacco, and chocolate intake, and eating small, frequent meals high in complex carbohydrates—may be sufficient. Decreasing sodium intake may alleviate edema. Stress management, cognitive behavioral therapy, and aerobic exercise have all been shown to improve symptoms.Low-risk pharmacologic interventions that may be effective include calcium carbonate (1000–1200 mg/d) for bloating, food cravings, and pain; magnesium (200–360 mg/d) for water retention; vitamin B6 (note that prolonged use of 200 mg/d may cause peripheral neurotoxicity) and vitamin E; nonsteroidal anti-inflammatory drugs (NSAIDs); spironolactone for cyclic edema; and bromocriptine for mastalgia. Traditional Chinese herbal medicines are frequently used to treat PMS in China. A recent well-designed study has reported on the effectiveness of Jingqianping in the treatment of PMS. However, currently there is insufficient evidence to support the use of Chinese herbal medicine for PMS. For symptoms of severe PMS and PMDD, further pharmacologic intervention may be necessary. Large, welldesigned, randomized, placebo-controlled trials of fluoxetine and sertraline and smaller trials of several other serotonin reuptake inhibitors have shown clear benefit compared with placebo for women diagnosed with PMDD, with at least moderately beneficial response rates in 50–60% of women taking active drug. This is not a generic antidepressant effect, because agents with different mechanisms are not effective. Treatment should be given 14 days prior to the onset of menstruation and continued through the end of the cycle. Anxiolytics such as alprazolam and buspirone also have been shown to be efficacious, but their side effects and potential for dependence must be seriously considered. Hormonal interventions have been shown to be effective. Use of selected oral contraceptives and transdermal estradiol patch has been suggested because they suppress ovulation. Recently, the US Food and Drug Administration approved the use of a pill containing drospirenone, which is a progestin derived from spironolactone rather than 19-nortestosterone, for treating PMDD. This approval permits the manufacturer to make claims about the drug's effectiveness in treating PMDD. However, the product label notes that effectiveness after 3 cycles is unknown. Use of gonadotropin-releasing hormone (GnRH) agonists leads to a temporary “medical menopause” and an improvement in symptoms. Their limitations lie in a hypoestrogenic state and a risk for osteoporosis, although “add-back” therapy with estrogen and progesterone may obviate these problems. There is no conclusive evidence that progesterone can help women with PMS. Danazol may improve mastalgia. Finally, bilateral oophorectomy is a definitive surgical treatment option; again, estrogen replacement would be recommended. Cervical Cancer Essentials of Diagnosis Early disease is frequently asymptomatic, underscoring the importance of cervical cytology screening. Abnormal uterine bleeding and vaginal discharge are the most common symptoms. A cervical lesion may be visible on inspection as a tumor or ulceration; cancer within the cervical canal may be occult. Diagnosis must be confirmed by biopsy. General Considerations In the United States, an estimated 12,710 new cases of invasive cervical cancer are diagnosed annually, and there are 4290 deaths from the disease. In contrast, with more than 529,000 new cases diagnosed annually and a >50% mortality rate, cervical cancer is the second most common cause of cancer-related morbidity and mortality among women in developing countries. This dichotomy is largely the result of a 75% decrease in the incidence of cervical cancer in developed countries following the implementation of population-based screening programs and treatment of preinvasive disease. The average age at diagnosis of patients with cervical cancer is 51 years. However, the disease can occur in the second decade of life and during pregnancy,and nearly 20% of cervical cancers are diagnosed in women age 65 or older. More than 95% of patients with early cancer of the cervix can be cured. Pathogenesis The major epidemiologic risk factors for cervical cancer are the same as those for CIN and were discussed earlier. HPV is central to the development of cervical neoplasia. HPV DNA is found in 99.7% of all cervical carcinomas. HPV-16 is the most prevalent HPV type in squamous cell carcinoma and adenocarcinoma, followed by HPV-18 and HPV-45. Other associated risk factors are tobacco use, immunosuppression, infection with HIV or a history of other STIs, high parity, and oral contraceptive use. HPV is epitheliotropic. Once the epithelium is acutely infected with HPV, 1 of 3 clinical scenarios ensues: Asymptomatic latent infection; Active infection in which HPV undergoes vegetative replication but not integration into the genome (eg, leading to condyloma or CIN I); or Neoplastic transformation following integration of oncogenic HPV DNA into the human genome. The virus infects a subset of primitive basal cells in the epithelium where it will undergo replication. The infected cell then enters the proliferating epithelial component. Active infection, in which HPV undergoes replication but remains episomal, is characterized by minimal viral oncogene expression. However, integration of HPV into the human genome is associated with cell immortalization, allowing for malignant transformation. This involves an upregulation of the viral oncogenes E6 and E7. These oncoproteins interfere with cell-cycle control in the human host cell. E6 and E7 have the ability to complex with the tumor suppressor genes p53 and Rb, respectively. The disabling of these 2 major tumor suppressor genes is thought to be central to host cell immortalization and transformation induced by HPV and the observed increased genetic instability. Incipient cancer of the cervix is generally a slowly developing process. Most cervical cancers probably begin as a high-grade dysplastic change (see previous section) or CIS with gradual progression over a period of several years. At least 90% of carcinomas of the cervix develop from the intraepithelial layers, almost always within 1 cm of the squamocolumnar junction of the cervix either on the portio vaginalis of the cervix or slightly higher in the endocervical canal. Early stromal invasion (stage IA1) up to a depth of 3 mm below the basement membrane is a localized process, provided there is no pathologic evidence of lymphovascular space involvement. Penetration of the stroma beyond this point carries an increased risk of lymphatic metastasis (Table 48–2). When the lymphatics are involved, tumor cells are carried to the regional pelvic lymph nodes (parametrial, hypogastric, obturator, external iliac, and sacral) (Fig. 48–6). The more pleomorphic or extensive the local disease, the greater is the likelihood of lymph node involvement. As the tumor grows, it also spreads by direct extension to the parametria. Prevention Until now, prevention of morbidity and death from cervical cancer largely involved recognition and treatment of preinvasive and early invasive disease. Over 60% of women who develop cervical cancer in developed countries either never have been screened or have not been screened in the preceding 5 years. Risk factors must be recognized, and screening, treatment intervention, and patient education must be modified.Universal cytologic screening of all women age 21 years or older must be continued on a regular basis until better, more sensitive and specific means of screening are found and outreach into underserved areas is improved. Women with preinvasive cervical neoplasia should be treated and followed up closely (Fig. 48–5). It is important to remember that cervical cytology smears are of limited value in detecting frankly invasive disease, with some studies finding false-negative rates up to 50%. Sexual abstinence is an effective but impractical prophylactic measure. Education of young women and men about risk factors and the necessity for regular screening, as well as information about the association of HIV infection and smoking with the development of cervical cancers, is crucial. The role of HPV vaccination has been discussed earlier. Clinical Findings Symptoms & Signs Abnormal vaginal bleeding is the most common symptom of invasive cancer and may take the form of a blood-stained leukorrheal discharge, scant spotting, or frank bleeding. Leukorrhea, usually sanguineous or purulent, odorous, and nonpruritic, is frequently present. A history of postcoital bleeding may be elicited on specific questioning. Pelvic pain, often unilateral and radiating to the hip or thigh, is a manifestation of advanced disease, as is the involuntary loss of urine or feces through the vagina, a sign of fistula formation. Weakness, weight loss, and anemia are characteristic of the late stages of the disease, although acute blood loss and anemia may occur in a bulky or ulcerating stage I lesion. Physical examination findings include a grossly normal-appearing cervix with preclinical disease. As the local disease progresses, physical signs appear. Infiltrative cancer produces enlargement, irregularity, and a firm consistency of the cervix and eventually of the adjacent parametria. The growth pattern can be endophytic, leading to a barrel-shaped enlargement of the cervix, or exophytic, where the lesion generally appears as a friable, bleeding, cauliflowerlike lesion of the portio vaginalis. Ulceration may be the primary manifestation of invasive carcinoma; in the early stages, the change often is superficial, so that it may resemble an ectropion or chronic cervicitis. With further progression of the disease, the ulcer becomes deeper and necrotic, with indurated edges and a friable, bleeding surface. The adjacent vaginal fornices may become involved next. Eventually, extensive parametrial involvement by the infiltrative process may produce a nodular thickening of the uterosacral and cardinal ligaments with resultant loss of mobility and fixation of the cervix. Biopsy Because of the failure of malignant cells to desquamate and the obscuring effect of inflammatory cells, it is not uncommon for an invasive carcinoma of the cervix to exist despite a negative cytologic smear. Any suspicious lesion of the cervix should be sampled by adequate biopsy, regardless of cytologic examination result. Biopsy of any Schiller-positive areas or of any ulcerative, granular, nodular, or papillary lesion provides the diagnosis in most cases. Colposcopically directed biopsies with endocervical sampling or conization of the cervix may be required when reports of suspicious or probable exfoliated carcinoma cells are made by the pathologist and a visible or palpable lesion of the cervix is not evident. Colposcopic warning signs of early invasive cancer in a field of CIN include capillaries that are markedly irregular, appearing as commas, corkscrews, and spaghettishaped vessels with great variation in caliber and abrupt changes in direction, often causing acute angles. Ulcerations or a markedly irregular appearance of the cervix with a waxy, yellowish surface and numerous bizarre, atypical blood vessels are common. Bleeding may occur also after slight irritation. Differential DiagnosisA variety of lesions of the cervix can be confused with cancer. Entities that must sometimes be ruled out include cervical ectropion, acute or chronic cervicitis, condyloma acuminata, cervical tuberculosis, ulceration secondary to STD (syphilis, granuloma inguinale, lymphogranuloma venereum, chancroid), abortion of a cervical pregnancy, metastatic choriocarcinoma or other cancers, and rare lesions such as those of actinomycosis or schistosomiasis. Histopathologic examination is usually definitive. Complications The complications of cervical cancer, for the most part, are those related to tumor size or invasion, necrosis of the tumor, infection, and metastatic disease. The natural history of the disease was outlined earlier. There are also problems pertaining to treatment of the disease (eg, radical surgery or radiation therapy; see next section, Treatment). Treatment Invasive carcinoma of the cervix spreads primarily by direct extension and lymphatic dissemination. The therapy of patients with cervical cancer needs to address not only the primary tumor site, but also the adjacent tissues and lymph nodes. This is generally accomplished by either radical hysterectomy and pelvic lymphadenectomy, radiation with concomitant chemotherapy, or a combination thereof. Endometrial Cancer Endometrial Carcinoma Endometrial cancer is characterized by obvious hyperplasia and anaplasia of the glandular elements, with invasion of underlying stroma, myometrium, and vascular spaces. Although atypical complex hyperplasia is thought to be a precursor lesion, only approximately 25% of patients with endometrial carcinoma have a history of hyperplasia. Important prognostic factors include stage, histologic grade and cell type, depth of myometrial invasion, presence of lymphovascular space involvement (LVSI), lymph node status, involvement of the lower uterine segment, and size of tumor. Endometrial cancers of endometrioid histology of any grade with no myometrial invasion are almost never associated with lymph node metastases. The depth of myometrial invasion and histologic grade are correlated with the incidence of pelvic and aortic lymph node metastases. In the surgical pathology study GOG-33, nodal disease was more frequent with increasing grade (3% grade 1, 9% grade 2, 18% grade 3), depth of invasion (1% endometrium only, 5% inner one-third, 6% middle one-third, 25% outer one-third myometrial invasion), and LVSI (27% with LVSI, 7% without LVSI). Patients with poorly differentiated deeply invasive cancers have about a 35% incidence of involved pelvic nodes and a 10–20% incidence of aortic node metastases. Because patients with lymph node metastases are at very high risk for recurrence, these pathologic features have serious implications for treatment planning. Endometrial cancer can spread by 4 possible routes: direct extension, lymphatic metastases, peritoneal implants after transtubal spread, and hematogenous spread. Undifferentiated lesions (grade 3) may spread to the pelvic and aortic nodes while still confined to the superficial myometrium. In serous and clear cell subtypes, the spread pattern is similar to that of ovarian cancer, and upper abdominal metastases are common. Hematogenous metastases to the lungs are uncommon with primary tumors limited to the uterus but do occur with recurrent or disseminated disease. Endometrial cancer spreads via a dual pathway to the pelvic and aortic lymph nodes (Fig. 49–1). The aortic nodes are rarely involved when the pelvic nodes are freeof metastases. The lymph nodes most commonly involved in endometrial cancer are found in the obturator space. Vaginal metastases occur by submucosal lymphatic or vascular metastases in approximately 3–8% of patients with clinical stage I disease. The concept that these metastases occur by spillage of tumor through the cervix at the time of surgery lacks convincing support. However, vaginal metastases are more common with higher histologic grade and with lower uterine segment or cervical involvement. Pathologists recognize various histologic types of endometrial carcinoma. Approximately 80% of all endometrial cancers are of the endometrioid type with several variants: villoglandular, secretory, with squamous differentiation, and with ciliated cells. These types have similar presenting symptoms and signs, patterns of spread, and general clinical behavior. For this reason, they can be considered collectively for purposes of clinical workup, differential diagnosis, and treatment. Endometrial adenocarcinomas of the nonendometrioid phenotype show mucinous, serous, clear cell, squamous, small cell, mixed, or transitional cell differentiation. Adenocarcinoma The most common type of endometrial carcinoma is adenocarcinoma, composed of malignant glands that range from well-differentiated (grade 1) to anaplastic carcinoma (grade 3). To determine stage and prognosis, the tumor is usually graded by the most undifferentiated area visible under the microscope (Fig. 49–2). In the United States, adenocarcinoma comprises 80% of endometrial carcinomas. Prevention A doubling of the incidence of endometrial cancer in the 1970s correlated with unopposed estrogen use in hormone replacement and sequential oral contraceptives over the previous 10 years. The declining incidence in the 1980s paralleled progesterone use in hormone replacement regimens and low-dose estrogen combination birth control pills. Estrogens are implicated as a causative factor in endometrial carcinoma based mainly on the high incidence of this disease in patients with presumed alterations in estrogen metabolism and in those who take exogenous estrogens. Furthermore, patients with anovulatory cycles are at higher risk of developing endometrial cancer because of prolonged periods of estrogenic stimulation of the endometrium without the opposing effects of progesterone. Progesterone has an antiproliferative effect on the endometrium and can induce apoptosis of endometrial cells. Classically, endometrial carcinoma affects the obese, nulliparous, infertile, hypertensive, and diabetic white woman, but it can occur in the absence of all these factors. Unlike cervical cancer, it is not related to sexual history. Prophylactic hysterectomy and bilateral salpingo-oophorectomy have been shown to be effective strategies for preventing endometrial and ovarian cancer in these high-risk patients. Several modifiable risk factors for endometrial carcinoma have been described, including obesity, diabetes, hypertension, and nulliparity. Prevention of endometrial cancer is primarily based on weight control, physical exercise, adequate control of diabetes and hypertension, and increased surveillance of women at high risk. In addition, a careful family history of each patient will help identify patients with a genetic predisposition for endometrial cancer, for example, as part of the HNPCC syndrome. If appropriate, these patients should undergo genetic counseling and genetic testing. A hysterectomy after the completion of childbearing is appropriate for patients with HNPCC syndrome given the lifetime risk for endometrial cancer of up to 70%. Hormone therapy in postmenopausal patients without hysterectomy should always include a progestationalagent to oppose the action of estrogens on the endometrium. Estrogens should be administered either continuously or cyclically using the lowest dose that controls symptoms. Progesterone (10 mg of medroxyprogesterone acetate or 200 mg of micronized progesterone) should be added for the last 10–14 days of the cycle to neutralize the risk of endometrial carcinoma. Alternatively, if estrogen and progesterone are administered continuously, 2.5 mg of medroxyprogesterone acetate is given daily. Clinical Findings The onset of endometrial bleeding facilitates detection in the earlier stages of disease. The most common presenting symptom is abnormal vaginal bleeding, particularly postmenopausal bleeding. Less frequently, severe cramps from hematometra or pyometra caused by an obliterated endocervical canal in elderly patients may be the presenting symptom. Symptoms & Signs Abnormal bleeding occurs in approximately 80% of patients and is the most important and early symptom of endometrial carcinoma. An abnormal vaginal discharge, especially after menopause or intermittent spotting, is reported by some patients. During the premenopausal years, the bleeding is usually described as excessive flow at the time of menstruation. However, bleeding may occur as intermenstrual spotting or premenstrual and postmenstrual bleeding. Approximately 5–10% of patients with postmenopausal bleeding have underlying cancer, but the probability increases with age and depends on underlying risk factors. Approximately 10% of patients complain of lower abdominal cramps and pain secondary to uterine contractions caused by detritus and blood trapped behind a stenotic cervical os (hematometra). If the uterine contents become infected, an abscess develops and sepsis may occur. Physical examination is usually unremarkable but may reveal medical problems associated with advanced age. Speculum examination may confirm the presence of bleeding, but because it may be minimal and intermittent, blood might not be present. Atrophic vaginitis is frequently identified in these elderly women, but postmenopausal bleeding should never be ascribed to atrophy without a histologic sampling of the endometrium to rule out endometrial carcinoma. Bimanual and rectovaginal examination of the uterus in the early stages of the disease will be normal unless hematometra or pyometra is present. If the cancer is extensive at the time of presentation, the uterus may be enlarged and may be misdiagnosed as a benign condition such as leiomyomata. In advanced cases, the uterus may be fixed and immobile from parametrial extension. Vaginal, vulvar, or inguinal–femoral lymph node metastases are rarely identified in early disease but are not uncommon in advanced cases or with recurrence following treatment. Ovarian metastases may cause marked enlargement of these organs. Laboratory Findings Routine laboratory findings are normal in most patients with endometrial carcinoma. If bleeding has been prolonged or profuse, anemia may be present. Cytologic study of specimens taken from the endocervix and posterior vaginal fornix can reveal adenocarcinoma in symptomatic patients. More important, endometrial carcinoma will be missed in 40% of symptomatic patients by routine cytologic examination. Accuracy has been greatly increased by aspiration cytologic study or biopsy (discussed under Special Examinations). Nevertheless, the Papanicolaou (Pap) smear is an integral part of the examination of all patients, because it identifies a small but definite percentage of patients with asymptomatic disease. Furthermore, the presence of benign endometrial cells in the cervical or vaginal smear of a menopausal or postmenopausal woman is associatedwith occult endometrial carcinoma in 2–6% of cases and in up to 25% with postmenopausal bleeding. Thus, any postmenopausal woman who shows endometrial cells on a routine cervical Pap smear requires evaluation for endometrial cancer, including endometrial sampling. Routine blood counts, urinalysis, endocervical and vaginal pool cytology, chest radiography, stool guaiac, and sigmoidoscopy are useful ancillary diagnostic tests in patients with endometrial carcinoma. Liver function tests, blood urea nitrogen, serum creatinine, and a blood glucose test (because of the known relationship to diabetes) are considered routine. Serum CA-125 (cancer antigen-125), a well-established tumor marker for epithelial ovarian cancer, might be useful for endometrial cancer. Approximately 20% of patients with clinical stage I disease (preoperatively, the tumor appears to be confined to the uterus) have an elevated CA-125. In cases with extensive intraperitoneal spread or enlarged uterus, the tumor marker CA-125 may be markedly elevated. However, in contrast to patients with ovarian cancer, the value of CA-125 in the management of patients with endometrial cancer is limited. Imaging Studies Chest radiography might reveal metastases in patients with advanced disease but is rarely positive in the early stages. Colonoscopy is usually unnecessary in a patient with a negative stool guaiac test and normal sigmoidoscopic examination but should always be performed in the patient with gross or occult gastrointestinal bleeding or symptoms. In patients from families with HNPCC, a colonoscopy should be performed preoperatively, particularly if the patient screens positive for the HNPCC-associated DNA mismatch repair gene mutations. Hysteroscopy can increase the diagnostic accuracy over office endometrial biopsy or dilatation and curettage. Hysteroscopy promotes the transtubal spread of tumor cells into the peritoneal cavity. However, the presence of a positive peritoneal cytology after hysteroscopy does not seem to alter the prognosis. Computed tomography is useful in assessing pelvic anatomy, visualizing enlarged lymph nodes in the pelvis and periaortic areas and diagnosing distant metastasis in the liver and lungs. Magnetic resonance imaging (MRI) is particularly helpful in identifying myometrial invasion and lower uterine segment or cervical involvement. Treatment The mainstay of treatment is surgery, including a total hysterectomy with bilateral salpingo-oophorectomy and staging with pelvic and periaortic lymphadenectomy. Further postoperative therapy depends on the particular histologic characteristics and the extent of the tumor. The majority of endometrial cancer cases are diagnosed at an early stage and can be treated with high cure rates. The most important treatment modality is surgery with total hysterectomy, bilateral salpingooophorectomy, and staging, including pelvic and periaortic lymphadenectomy. Primary radiation therapy is used only in patients with medical contraindications for surgery or advanced pelvic disease. It has been repeatedly demonstrated that radiation therapy can cure endometrial carcinoma in some patients. However, radiation therapy averages about a 20% lower cure rate compared to surgery in stage I disease. Primary chemotherapy is used infrequently and mostly in patients with metastatic disease. High-dose progesterone therapy, commonly with medroxyprogesterone acetate or megestrol acetate, may be used for patients who are inoperable or in younger patients who elect for fertility preservation. The overall response to high-dose progesterone therapy is up to 75% in grade 1 endometrial cancer cases limited to the endometrium. To verify that the patient is responding to therapy, regular endometrial sampling needs to be performed. Adjuvant treatment is dependent on the results of surgical staging and histology. For example, adjuvant radiation therapy is frequently used in high-risk endometrial cancers of endometrioid histology to prevent pelvic recurrences. Advanced pelvic disease may be treated with radiation followed by systemicchemotherapy. Serous cancers of the endometrium behave biologically similar to ovarian cancer and are treated with adjuvant platinum-based chemotherapy possibly in conjunction with radiation. Atrophic Vaginitis Clinical Findings Prepubertal, lactating, and postmenopausal women lack the vaginal effects of estrogen production. The pH of the vagina is abnormally high, and the normally acidogenic flora of the vagina may be replaced by mixed flora. The vaginal epithelium is thinned and more susceptible to infection and trauma. Although most patients are asymptomatic, many postmenopausal women report vaginal dryness, spotting, presence of a serosanguineous or watery discharge, and/or dyspareunia. Some of the symptoms of irritation are caused by a secondary infection. On examination, the vaginal mucosa is thin, with few or absent vaginal folds. The pH is 5.0–7.0. The wet mount shows small, rounded parabasal epithelial cells and an increased number of polymorphonuclear cells. Treatment Treatment includes intravaginal application of estrogen cream. Because approximately one-third of the vaginal estrogen is systemically absorbed, this treatment may be contraindicated in women with a history of breast or endometrial cancer. The estradiol vaginal ring, which is changed every 90 days, may provide a preferable route of administration for some women. Estradiol hemihydrate (Vagifem) 1 tablet intravaginally daily for 2 weeks and then twice a week for at least 3–6 months may be more convenient. Systemic estrogen therapy should be considered if there are no contraindications. Postcoital bleeding Postcoital bleeding mainly comes from surface lesions of the genital tract to include cervical polyps, cervicitis, ectropion, cervical intra-epithelial lesion (CIN), or carcinoma [7]. The prevalence of cervical cancer in women with postcoital bleeding is 3.0 to 5.5% and prevalence of CIN is 6.8% to 17.8% [6, 8–13]. The differential diagnosis for women who present with postcoital bleeding is broad. Most women with postcoital bleeding have benign disease, which is reassuring given that the initial concern for both patient and provider is the possibility of underlying malignancy. Table 1outlines some of the most common causes for postcoital bleeding. At this time, there are no established guidelines from the American College of Obstetricians and Gynecologists or the Royal College of Obstetricians and Gynaecologists or evidence from randomized clinical trials to base recommendations on diagnosis and treatment of postcoital bleeding. The following discussion provides various considerations to take into account when approaching a patient with postcoital bleeding. Figure 1 presents a diagnostic algorithm for women with postcoital bleeding. A thorough emphasis on patient history often leads to an accurate diagnosis of postcoital bleeding. With all gynecologic patients, it is important to obtain an accurate menstrual history. Factors which should be elicited from the patient include the frequency of the patient's menstrual cycle, days of menstruation, presence of heavy bleeding, presence of intermenstrual bleeding, and whether cycles are regular or irregular. The duration of normal menstrual flow is 5 days with cycles typically lasting between 21–35 days [43]. Clinicians should also evaluate if the patient is postmenopausal which is defined as 12 months of amenorrhea without any other physiologic or pathologic cause. Moreover, history should focus on whether the patient's postcoital bleeding is truly bleeding that occurs as a direct result of intercourse or if it is secondary to irregular menstrual bleeding. History may also help to differentiate between whether bleeding is originating from the uterus or cervix. Patients with abnormal uterine bleeding often report heavy periods, intermenstrual bleeding not related to intercourse, and irregular menstrual cycles.There are multiple considerations to take into account for patients past medical history. Screening should be performed as to whether the patient has been diagnosed or has any symptoms concerning a bleeding disorder. Regarding surgical history, determine whether there have been surgeries on the genital tract with focus on timing and indication for the surgery. A detailed sexual history should be obtained with focus on number of partners, new partners, and history of any sexually transmitted infections for either the patient or her partners. It is imperative to also screen patients for domestic abuse and/or sexual abuse as genital tract trauma can lead to postcoital bleeding. Patients may not be willing to volunteer this information for either embarrassment or fear of retaliation. Providers should attempt to establish rapport with the patient and create an environment in which patients may be willing to share this information. If the patient's partner is present, then strategies may be employed to have the partner step outside the exam room during the time of pelvic exam, at which point one may also evaluate the patient privately for concerns of abuse. Finally, providers should ensure cervical cancer screening is up-to-date. There are also multiple factors to ask on review of symptoms that can help establish a diagnosis. For example, one should inquire about pain with focus on pain during menstruation (dysmenorrhea) or with intercourse (dyspareunia). Regarding the latter, a detailed history should be obtained as to when the dyspareunia occurs: at all times, with deep penetration, or in certain positions. Patients should be asked if there has been any change in discharge, specifically color, consistency, frequency, and odor. Finally, patients should be screened for symptoms concerning for pelvic organ prolapse such as a feeling of heaviness in the vagina, sensation that things are dropping, need to splint in order to have bowel movement or urination, and visualization of organs prolapsing from the vagina. Every woman presenting with postcoital bleeding requires a thorough examination of the genital tract. A bivalve speculum exam should be performed to evaluate the vaginal rugae and cervix. Attention should be focused to determine if there are any lacerations or trauma to the vaginal walls. Upon examining the cervix, one should evaluate any obvious gross lesions on the cervix or lesions protruding through the cervical canal. Colposcopy may be considered if there are any suspicious lesions on the cervix to further evaluate the lesion under high power. In obtaining cultures or clearing mucus from the cervix, one should also determine whether gentle palpation alone of the cervix with a swab is able to recreate bleeding. Considerations may then be made to break down the bivalve speculum and perform an inspection of the vagina with one blade of the speculum. This may allow for a better visualization of the vaginal rugae as there is less risk of obstruction by the blades of the speculum. This technique may be used to evaluate signs of pelvic organ prolapse. A blade should be placed along the anterior vaginal wall, while having the patient Valsalva, to evaluate prolapse of the posterior structures. A bimanual exam is performed to evaluate the size and contour of the uterus as well as the presence of any adnexal masses. During this exam, one may delineate whether there is presence of cervical motion tenderness which may help with diagnosing an underlying infection. If the patient has complained of dyspareunia or pelvic pain, then it is also important to delineate the location of the pain. Most women will not find a bimanual exam comfortable, so it is important to specifically ask what on exam reproduces the patient's pain. Finally, if there is concern for underlying malignancy, then one should also evaluate the inguinal lymph nodes to determine if there is any lymphadenopathy. A rectovaginal exam should be performed to determine if there are any masses or nodularities located on the anterior surface of the rectum or extension of disease into the parametrium. On speculum exam, there are multiple cultures that may be obtained to further evaluate postcoital bleeding. Nucleic acid amplification testing (NAAT) for N. gonorrhoeae, C. trachomatis, and T. vaginalis should routinelybe obtained in women presenting with postcoital bleeding. Even though wet mount is the most cost-effective means of diagnosing Trichomonas, the overall sensitivity is low and is dependent on the inoculum size; thus, NAAT testing has become popular due to its relatively high sensitivity and specificity. Women who are not recent on cervical cancer screening may also undergo cervical cytology, with or without testing for high risk HPV. Nevertheless, it is important to note that the false negative rate for Pap smears in the presence of invasive cancer is 50%; thus, gynecologists must be cognizant that a normal smear does not rule out underlying malignancy in women presenting with postcoital bleeding [44]. There are multiple variations based on expert opinion on which patients with postcoital bleeding should be referred for colposcopy. There is little debate that women with an abnormal pap smear or a grossly visible lesion that is suspicious for an underlying malignancy should be referred for colposcopy. Nevertheless, there is controversy on whether colposcopy should be performed on women with no visible lesions and negative cervical cancer screening results on recently performed testing. One may argue that postcoital bleeding alone is not an absolute indication for colposcopy [12]. Providers should discuss with their patients that there are no guidelines or evidence to base recommendations in these scenarios [19]. One retrospective study of 314 women with postcoital bleeding seen by a gynecologic service found that 20% of women diagnosed with cervical cancer or vaginal cancer on colposcopy had a normal speculum exam with negative cytology prior to the procedure [11]. In short, there is limited evidence to base recommendations on colposcopy for women with negative Pap smears and no obvious lesion on exam. However, the Working Group of the Royal Australian College of General Practice and of Obstetrics and Gynecology [7] recommend that general practitioners refer women for colposcopy if they have one of the following qualifications; nevertheless, it is important to realize that these recommendations are not evidence based [15]:persistent postcoital bleeding, postcoital bleeding associated with a single smear suggestive of LGSIL or worse, postcoital bleeding associated with repeated smears with minor atypia or wart virus changes. Directed biopsy with colposcopy remains the standard for disease detection [43]. Recent studies, however, have compared directed biopsy to blind four-quadrant ectocervical biopsies or loop excision procedure as diagnostic criteria [45, 46]. These studies found that the presence of CIN 2 and higher was missed on directed biopsy but detected on random four-quadrant biopsies in 18.6–31.6% of times [46, 47]. Another study, however, demonstrated that diagnosis of CIN 2 and higher was found in 57.1% of women with colposcopy directed biopsy versus 37.4% with random biopsy [48]. Based on these studies, the American College of Obstetricians Gynecologists recommends that biopsies should be performed on all visible lesions [49]. These recommendations and studies pertain to patients with abnormal cytology. It is hard to interpret these recommendations in women with postcoital bleeding and no history of abnormal cytology. There are multiple ways to evaluate the endocervical and endometrial cavity for sources of postcoital bleeding. One option is to perform an office endometrial biopsy which can evaluate for the presence of endometrial hyperplasia, malignancy, and endometrial polyps. If the patient is not amenable to this procedure or if further imaging is indicated, then a saline infused sonohysterogram is another useful diagnostic technique to evaluate the contours of the uterine cavity. Finally, depending on the presence of other complaints, one may also consider diagnostic hysteroscopy to evaluate the cervical canal and uterine cavity; although this procedure should be reserved for patients with complaints of abnormal uterine bleeding which may suggest an endometrial source for the abnormal bleeding. The clinical approach to postmenopausal women presenting with postcoital bleeding warrants other considerations to exclude carcinoma of the endometrium. The American College of Obstetricians and Gynecologists reports that there are two acceptable methods for evaluating malignancy: endometrial biopsy or transvaginal ultrasonography. An endometrial thickness of greater than 4 mm in a patient with postmenopausal bleeding requires further evaluation with sonohysterography, office endometrial biopsy, orhysteroscopy. Alternatively, providers may also decide to initiate the evaluation of postmenopausal bleeding with performing an endometrial biopsy [50]. The majority of women presenting to their primary care physician with the complaints of postcoital bleeding will be found to have no obvious underlying cause for their bleeding based on history, exam, or laboratory investigation [11]. Nevertheless, the reassuring aspect is that 60% of naturally menstruating women with postcoital bleeding will have spontaneous resolution of symptoms within six months [4]. Half of these women will maintain resolution for two years [4]. Diagnostic Laboratory Procedures Vaginal Dryness VAGINAL DRYNESS OVERVIEW Vaginal dryness, also known as atrophic vaginitis, is a common condition in postmenopausal women. This condition is also common in women who have had both ovaries removed at the time of hysterectomy. Some women have uncomfortable symptoms of vaginal dryness, such as pain with sex, burning vaginal discomfort or itching, or abnormal vaginal discharge, while others have no symptoms at all. Fortunately, there are several effective treatments for vaginal dryness. If you think you have vaginal dryness, talk to your healthcare provider about which treatment is right for you. (See "Clinical manifestations and diagnosis of genitourinary syndrome of menopause (vulvovaginal atrophy)".) VAGINAL DRYNESS CAUSES Estrogen helps to keep the vagina moist and to maintain thickness of the vaginal lining. Vaginal dryness occurs when the ovaries produce a decreased amount of estrogen. This can occur at certain times in a woman's life, and may be permanent or temporary. Times when less estrogen is made include: ●At the time of menopause. ●After surgical removal of the ovaries, chemotherapy, or radiation therapy of the pelvis for cancer. ●After having a baby, particularly in women who breastfeed. ●While using certain medications, such as danazol, medroxyprogesterone (brand names: Provera or DepoProvera), leuprolide (brand name: Lupron), or nafarelin. When these medications are stopped, estrogen production resumes. Women who smoke cigarettes have been shown to have an increased risk of an earlier menopause transition as compared to non-smokers. Therefore, atrophic vaginitis symptoms may appear at a younger age in this population. VAGINAL DRYNESS TREATMENT There are several treatment options for women with vaginal dryness: vaginal moisturizers or lubricants, vaginal estrogen, a pill called ospemifene (brand name: Osphena), and a vaginal tablet called prasterone, or dehydroepiandrosterone (DHEA). All vaginal dryness treatments work temporarily. The vaginal dryness will return when the treatment is stopped unless the ovaries make more estrogen.Vaginal lubricants and moisturizers — Vaginal lubricants and moisturizers can be purchased without a prescription. These products do not contain any hormones and have virtually no side effects. Lubricants are designed to reduce friction and discomfort from dryness during sexual intercourse. The lubricant is applied inside the vagina or on the penis just before having sex. Products designed as vaginal lubricants (eg, Astroglide) are more effective than lubricants that are not designed for this purpose, such as petroleum jelly (Vaseline). Oil-based lubricants, such as petroleum jelly, baby oil, or mineral oil, may damage latex condoms and/or diaphragms and make them less effective in preventing pregnancy or sexually transmitted infections. Polyurethane condoms can be used with oil based products. Also, lubricants that are made with water or silicone can be used with latex condoms and diaphragms. Natural lubricants, such as olive, avocado or peanut oil, are easily available products that may be used as a lubricant with sex. Again, natural oils are not recommended for use with latex condoms or diaphragms; the oil can damage the latex, potentially making it less effective in preventing pregnancy or sexually transmitted infections. Vaginal moisturizes (eg, Replens, Moist Again, Vagisil, K-Y Silk-E, and Feminease) are formulated to allow water to be retained in the vaginal tissues. Moisturizers are applied into the vagina three times weekly to allow a continued moisturizing effect. These should not be used just before having sex, as they can be irritating. Hand and body lotions should not be used to relieve vaginal dryness since they can be irritating to the vaginal tissues. Vaginal estrogen — Vaginal estrogen is the most effective treatment option for women with vaginal dryness. Vaginal estrogen must be prescribed by a healthcare provider. Very low doses of vaginal estrogen can be used when it is put into the vagina to treat vaginal dryness. A small amount of estrogen is absorbed into the bloodstream, but only about 100 times less than when using estrogen pills or tablets. As a result, there is a much lower risk of side effects, such as blood clots, breast cancer, and heart attack, compared with other estrogen-containing products (birth control pills, menopausal hormone therapy). Several types of vaginal estrogen products are available: ●Estrogen cream (eg, Premarin, Estrace cream) is inserted into the vagina every day for two to three weeks, and then one or two times weekly. The cream can be difficult to measure accurately and insert into the vagina. ●The vaginal estrogen insert (Vagifem) looks like a small tablet but is inserted inside the vagina. The vaginal tablet is packaged in a disposable applicator. Vagifem is usually inserted every day for two weeks and then twice weekly. ●The vaginal estrogen ring, called Estring, is a flexible plastic ring that is worn inside the vagina all the time. It is replaced every three months by the woman or her healthcare provider. The ring does not need to be removed during sex or bathing. It cannot be felt by most women or their sexual partners. In women who have previously had a hysterectomy, the ring will sometimes fall out.Estring should not be confused with the estrogen replacement vaginal ring (Femring), which releases a much higher dose of estrogen and is intended to be absorbed into the body to relieve hot flashes. (See "Patient education: Menopausal hormone therapy (Beyond the Basics)".) How long can I use vaginal estrogen? — Vaginal estrogen is thought to be safe and can probably be used indefinitely, although there are no long-term studies confirming its safety. Is vaginal estrogen safe for women with a history of breast cancer? — The safety of vaginal estrogen in women who have a past history of breast cancer is unclear. A small amount of estrogen can be absorbed from the vagina into the bloodstream. If you have a history of breast cancer, talk to your healthcare provider or your oncologist about the potential risks and benefits of vaginal estrogen. Ospemifene — Ospemifene is a prescription medication that is similar to estrogen, but is not estrogen. In the vaginal tissue, it acts similarly to estrogen. In the breast tissue, it acts as an estrogen blocker. It comes in a pill, and is prescribed for women who want to use an estrogen-like medication for vaginal dryness or painful sex associated with vaginal dryness, but prefer not to use a vaginal medication. The medication may cause hot flashes as a side effect. This type of medication may increase the risk of blood clots or uterine cancer. Further study of ospemifene is needed to evaluate the risk of these complications. This medication has not been tested in women who have had breast cancer or are at a high risk of developing breast cancer. Prasterone (dehydroepiandrosterone) — Prasterone, also known as dehydroepiandrosterone (DHEA), is also an option for women with vaginal dryness due to menopause. It comes in the form of a suppository that is inserted into the vagina once a day. Vaginal estrogen therapy is more commonly used than prasterone, because vaginal estrogen has been studied more thoroughly and the twice-weekly dosing may be more convenient. However, prasterone is a reasonable option for women who can't take estrogen or prefer to avoid it, but who can use other vaginal hormones. Sexual activity — Vaginal estrogen improves vaginal dryness quickly, usually within a few weeks. You may continue to have sex as you treat vaginal dryness because sex itself can help to keep the vaginal tissues healthy. Vaginal intercourse may help the vaginal tissues by keeping them soft and stretchable and preventing the tissues from shrinking. Primary dysmenorrhea Dysmenorrhea, or painful menstruation, is one of the most common complaints of gynecologic patients. Many women experience mild discomfort during menstruation, but the term dysmenorrhea is reserved for women whose pain prevents normal activity and requires medication, whether an over-the-counter or a prescription drug. There are 3 types of dysmenorrhea: (1) primary (no organic cause), (2) secondary (pathologic cause), and (3) membranous (cast of endometrial cavity shed as a single entity). This discussion focuses mainly on primary dysmenorrhea. Secondary dysmenorrhea is discussed elsewhere in this book in association with specific diseases and disorders (eg, endometriosis, adenomyosis, pelvic inflammatory disease, cervical stenosis, fibroids, and endometrial polyps). Membranous dysmenorrhea is rare; it causes intense cramping pain due to passage of a cast of the endometrium through an undilated cervix. Another cause of dysmenorrhea that should be considered is cramping due to the presence of an intrauterine device (IUD). PathogenesisPain during menstruation has long been known to be associated with ovulatory cycles. The mechanism of pain has been attributed to prostaglandin activity. Advances in the last 3 decades and current understanding suggest that in primary dysmenorrheal there is abnormal and increased prostanoid and possibly eicosanoid secretion, which in turn induces abnormal uterine contractions. The contractions reduce uterine blood flow, leading to uterine hypoxia. Other studies have confirmed increased leukotriene levels as a contributing factor. Vasopressin was thought to be an aggravating agent, but atosiban, a vasopressin antagonist, has shown no effect on menstrual pain. Psychological factors may be involved, including attitudes passed from mother to daughter. Girls should receive accurate information about menstruation before menarche; this can be provided by parents, teachers, physicians, or counselors. Emotional anxiety due to academic or social demands may be a cofactor. Clinical Findings Reactions to pain are subjective, and questioning by the physician should not lead the patient to exaggerate or minimize her discomfort. History taking is most important and should include the following questions: When does the pain occur? What does the patient do about the pain? Are there other symptoms? Do oral contraceptives relieve or intensify the pain? Does the pain become more severe over time? Because dysmenorrhea almost always is associated with ovulatory cycles, it does not usually occur at menarche but rather later in adolescence. As many as 14–26% of adolescents miss school or work as a result of pain. Typically, pain occurs on the first day of the menses, usually about the time the flow begins, but it may not be present until the second day. Nausea and vomiting, diarrhea, and headache may occur. The specific symptoms associated with endometriosis are not present. The physical examination does not reveal any significant pelvic disease. When the patient is symptomatic, she has generalized pelvic tenderness, perhaps more so in the area of the uterus than in the adnexa. Occasionally, ultrasonography or laparoscopy is necessary to rule out pelvic abnormalities such as endometriosis, pelvic inflammatory disease, or an accident in an ovarian cyst. Differential Diagnosis The most common misdiagnosis of primary dysmenorrhea is secondary dysmenorrhea due to endometriosis. With endometriosis, the pain usually begins 1–2 weeks before the menses, reaches a peak 1–2 days before, and is relieved at the onset of flow or shortly thereafter. Severe pain during sexual intercourse or findings of adnexal tenderness or mass or cul-de-sac nodularity, particularly in the premenstrual interval, help to confirm the diagnosis (see Chapter 56). A similar pain pattern occurs with adenomyosis, although in an older age group and in the absence of extrauterine clinical findings. Treatment NSAIDs or acetaminophen may relieve mild discomfort. Addition of continuous heat to the abdomen in addition to NSAIDs decreases pain significantly. For severe pain, codeine or other stronger analgesics may be needed, and bed rest may be desirable. Occasionally, emergency treatment with parenteral medication is necessary. Analgesics may cause drowsiness at the dosages required. Antiprostaglandins Antiprostaglandins are now used for treatment of dysmenorrhea. The newer, stronger, faster-acting drugs appear to be more useful than aspirin. Ibuprofen and naproxen, NSAIDs that are available over the counter, have been extremely effective in reducing menstrual prostaglandin and relieving dysmenorrhea. More specific cyclooxygenase-2 (COX-2) inhibitors are now available, but concerns about their adverse effects have recentlyattracted attention. Rofecoxib, valdecoxib, and lumiracoxib are effective for treating primary dysmenorrhea. Thus far, COX-2 inhibitors are equally effective but not better than naproxen. Given the above considerations, concerns about safety of COX-2 inhibitors, the short duration of therapy for relieving primary dysmenorrhea, and the low costs of NSAIDs, it is prudent to recommend established NSAIDs with track records of long-term safety as the preferred pharmacologic agent. The drug must be used at the earliest onset of symptoms, usually at the onset of, and sometimes 1–2 days prior to, bleeding or cramping. Antiprostaglandins work by blocking prostaglandin synthesis and metabolism. Once the pain has been established, antiprostaglandins are not nearly as effective as with early use. Oral Contraceptives Cyclic administration of oral contraceptives, usually in the lowest dosage but occasionally with increased estrogen, prevents pain in most patients who do not obtain relief from antiprostaglandins or cannot tolerate them. The mechanism of pain relief may be related to absence of ovulation or to altered endometrium resulting in decreased prostaglandin production. In women who do not require contraception, oral contraceptives are given for 6–12 months. Many women continue to be free of pain after treatment has been discontinued. NSAIDs act synergistically with oral contraceptive pills to improve dysmenorrhea. Surgical Treatment In a few women, no medication controls dysmenorrhea. Cervical dilatation is of little use. Laparoscopic uterosacral ligament division and presacral neurectomy are infrequently performed, although some physicians consider these procedures to be important adjuncts to conservative operation for endometriosis. Adenomyosis, endometriosis, or residual pelvic infection unresponsive to medical therapy or conservative surgical therapy eventually may require hysterectomy with or without ovarian removal in extreme cases. Rarely, a patient with no organic source of pain eventually requires hysterectomy to relieve symptoms. Adjuvant Treatments Continuous low-level topical heat therapy has been shown to be as effective as ibuprofen in treating dysmenorrhea, although its practicality in daily life may be questionable. Many studies have indicated that exercise decreases the prevalence and/or improves the symptomatology of dysmenorrhea, although solid evidence is lacking. A recent Cochrane review analyzed 7 randomized controlled trials of transcutaneous electrical nerve stimulation (TENS) compared with placebo or no treatment. Overall, high-frequency TENS is more effective for pain relief in primary dysmenorrhea than placebo TENS. Currently, there is insufficient evidence to recommend the use of herbal and dietary therapies for dysmenorrhea. Vaginitis Vaginitis Candidiasis Essentials of Diagnosis Intense vulvar pruritus A white vaginal discharge Vulvar erythemaFilaments and spores in vaginal discharge can be seen in saline (“wet prep”) and KOH preparations The gold standard for diagnosis is a vaginal culture Pathogenesis Approximately 75% of women experience an episode of vulvovaginal candidiasis during their lifetime. Candida albicans, the most common Candida species, causes symptomatic vulvovaginitis in approximately 90% of the cases. C albicans frequently inhabits the mouth, throat, large intestine, and vagina. Clinical infection is dependent on considerable growth and colonization and may be associated with a systemic disorder (diabetes mellitus, HIV, obesity), pregnancy, medication (antibiotics, corticosteroids, oral contraceptives), and chronic debilitation. Prevention Nonabsorbent undergarments should be avoided. The vulva and vaginal area should be kept dry. Controlling any underlying metabolic illnesses, especially diabetes, can prevent candidal growth. Even when diabetes is not present, a low-sugar diet is recommended, as the glucose in a vaginal discharge may promote the growth of the yeast. Complicating medications, especially antibiotics, estrogen, or oral contraceptive, should be discontinued if possible. Some experts recommend administering a prophylactic dose of an antifungal medication simultaneous to every antibiotic administration. Clinical Findings SYMPTOMS & SIGNS Vulvovaginal candidiasis presents with intense vulvar pruritus; a white, cheesy vaginal discharge; and vulvar erythema. A burning sensation may follow urination, particularly if there is excoriation of the skin from scratching. Widespread involvement of the skin adjacent to the labia may suggest an underlying systemic illness. The labia minora may be erythematous and edematous. WET PREP EVALUATION Diagnosis is based on a normal vaginal pH ≤4.5 and microscopic evaluation of vaginal secretions both in a saline preparation (wet prep) and mixed with 10% KOH solution. Identification of C albicans requires detections of filamentous forms (pseudohyphae) of the organism (Fig. 39–5). Spores may be present as well, but the presence of spores alone may indicate a Candida glabrata infection. The gold standard for diagnosis is a vaginal culture. Differential Diagnosis Genital herpes and localized provoked vulvodynia should be included in the differential diagnosis. Other causes of vaginal discharge are discussed later in this chapter. Treatment The current medical treatment of candidal infection is by imidazoles, fungistatic agents that interfere with the production of the sterol of the cell wall (Table 39–11). These are available as topical creams, vaginal suppositories, and oral agents. Application of a topical steroid may be beneficial to the patient with severe vulvar itch or edema. In evaluating the patient with complicated candidal vulvovaginitis, underlying predisposing disease processes should be addressed. Additionally, cultures of the vagina should be taken to identify resistant strains. C glabrata and Candida tropicalis, which are detected with increasing frequency, require prolonged periods of treatment. Treatment regimens for complicated candidal vulvovaginitis include prolonging antifungal therapy for at least 2 weeks, consistent with the life cycle of yeast; self-medication for 3–5 days upon first evidence of symptoms; and prophylactic treatment for several days before menstruation or during antibiotic therapy. Oral administration of fluconazole 150 mg weekly for 6 months or itraconazole 100 mg daily for 6 months mayreduce the frequency of recurrence to 10% during maintenance therapy. Liver function should be monitored during prolonged oral therapy. Treatment of the partner may be considered in cases of symptomatic balanitis. Gentian violet 1%, an aniline dye, has demonstrated effectiveness against C albicans and C glabrata when painted over vaginal surfaces once weekly. Boric acid compounded in a 600-mg suppository form, administered daily for 6 weeks, is also effective treatment for candidiasis and yeast infestation. Polyenes, such as nystatin, which is not absorbed in the gastrointestinal tract, may be taken orally to reduce intestinal colonization. Flucytosine may be administered in resistant cases. [Show More]
Last updated: 1 year ago
Preview 1 out of 24 pages
Buy this document to get the full access instantly
Instant Download Access after purchase
Add to cartInstant download
We Accept:

Reviews( 0 )
$12.00
Document information
Connected school, study & course
About the document
Uploaded On
May 15, 2021
Number of pages
24
Written in
Additional information
This document has been written for:
Uploaded
May 15, 2021
Downloads
0
Views
41

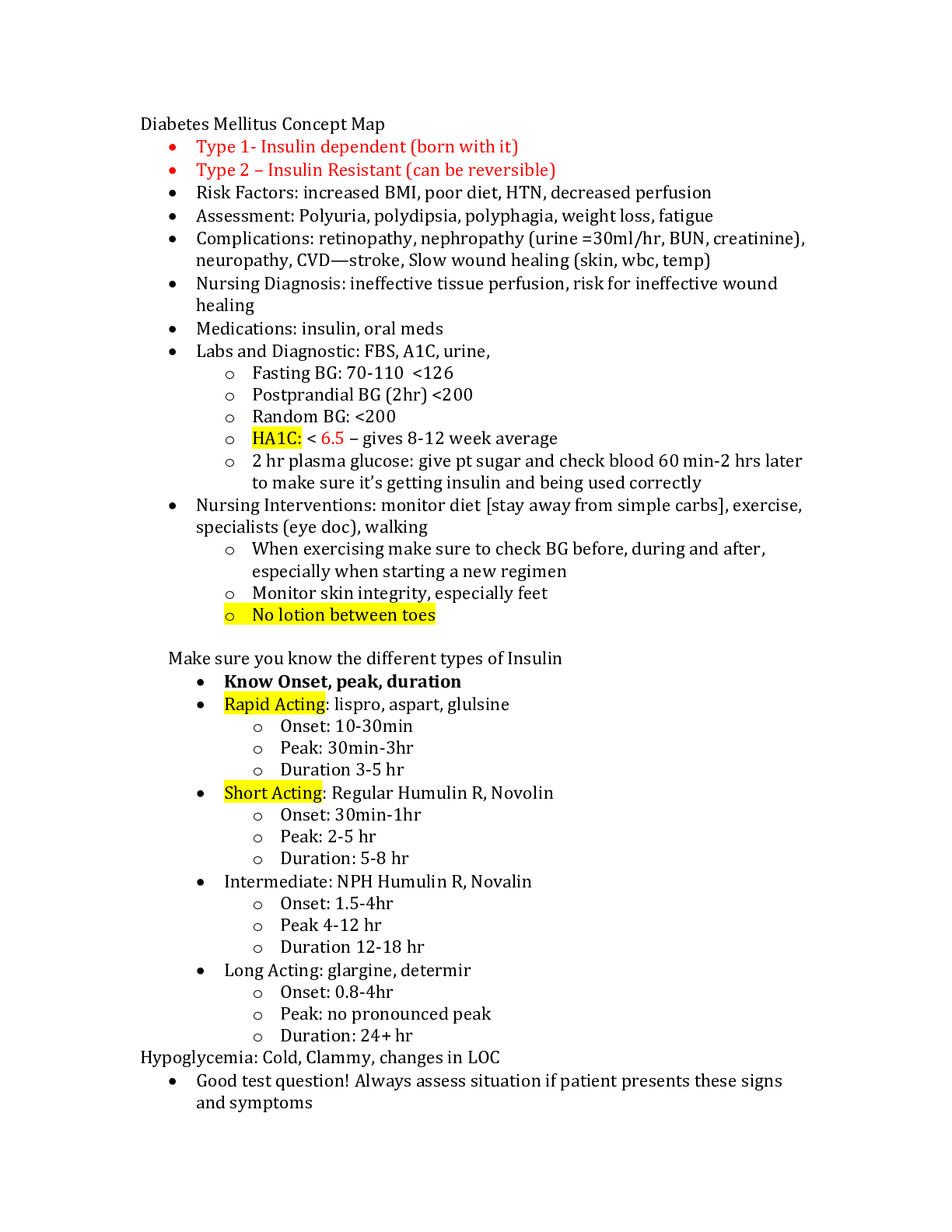
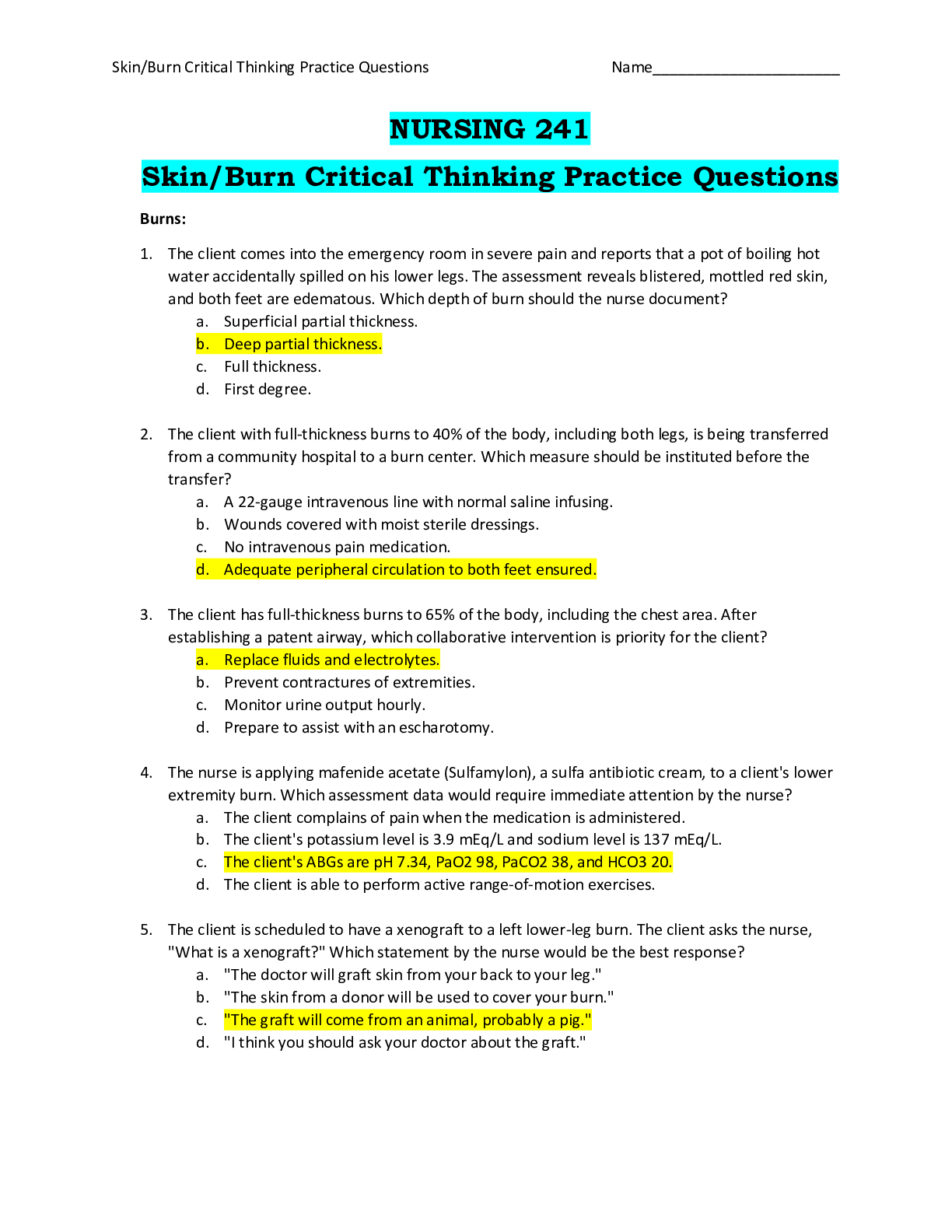
.png)
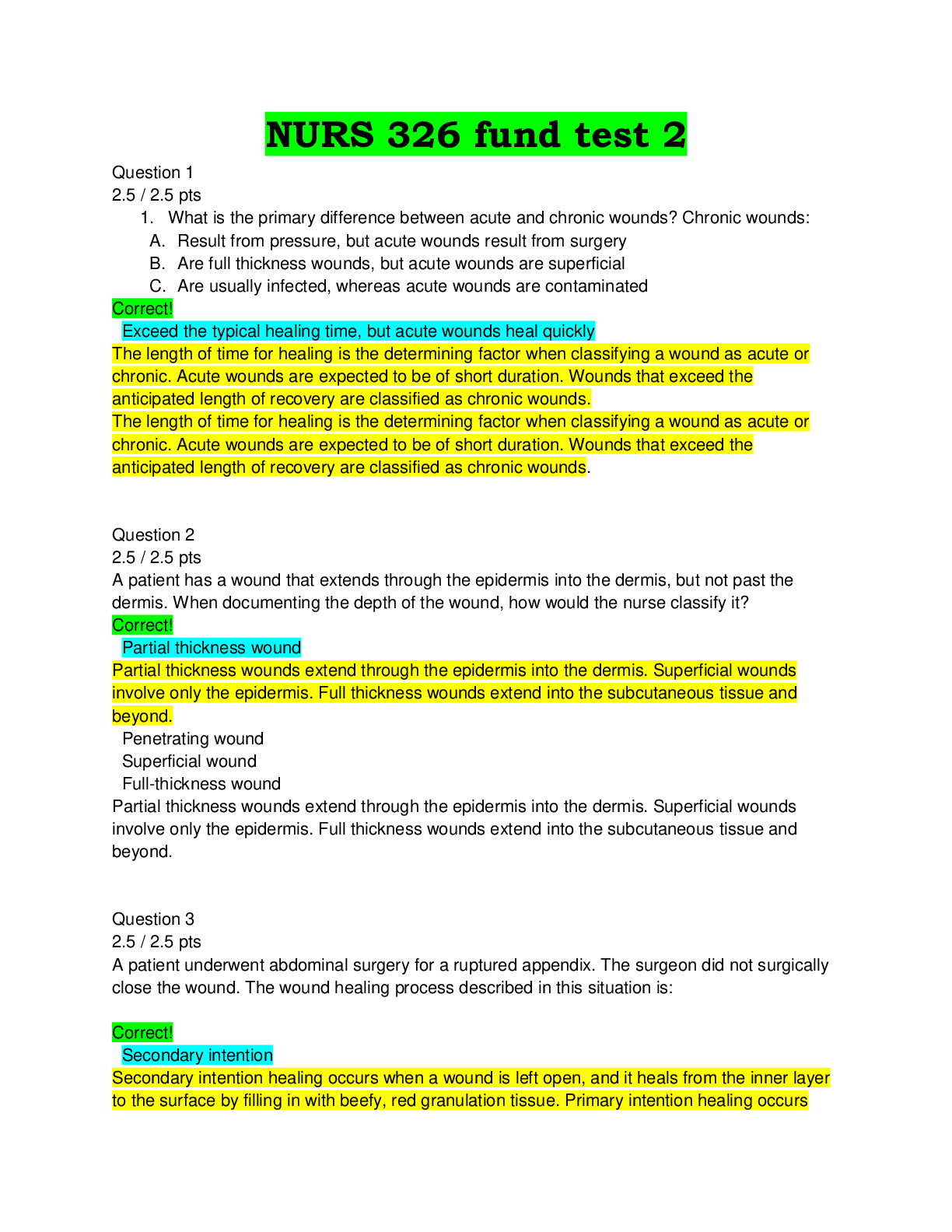
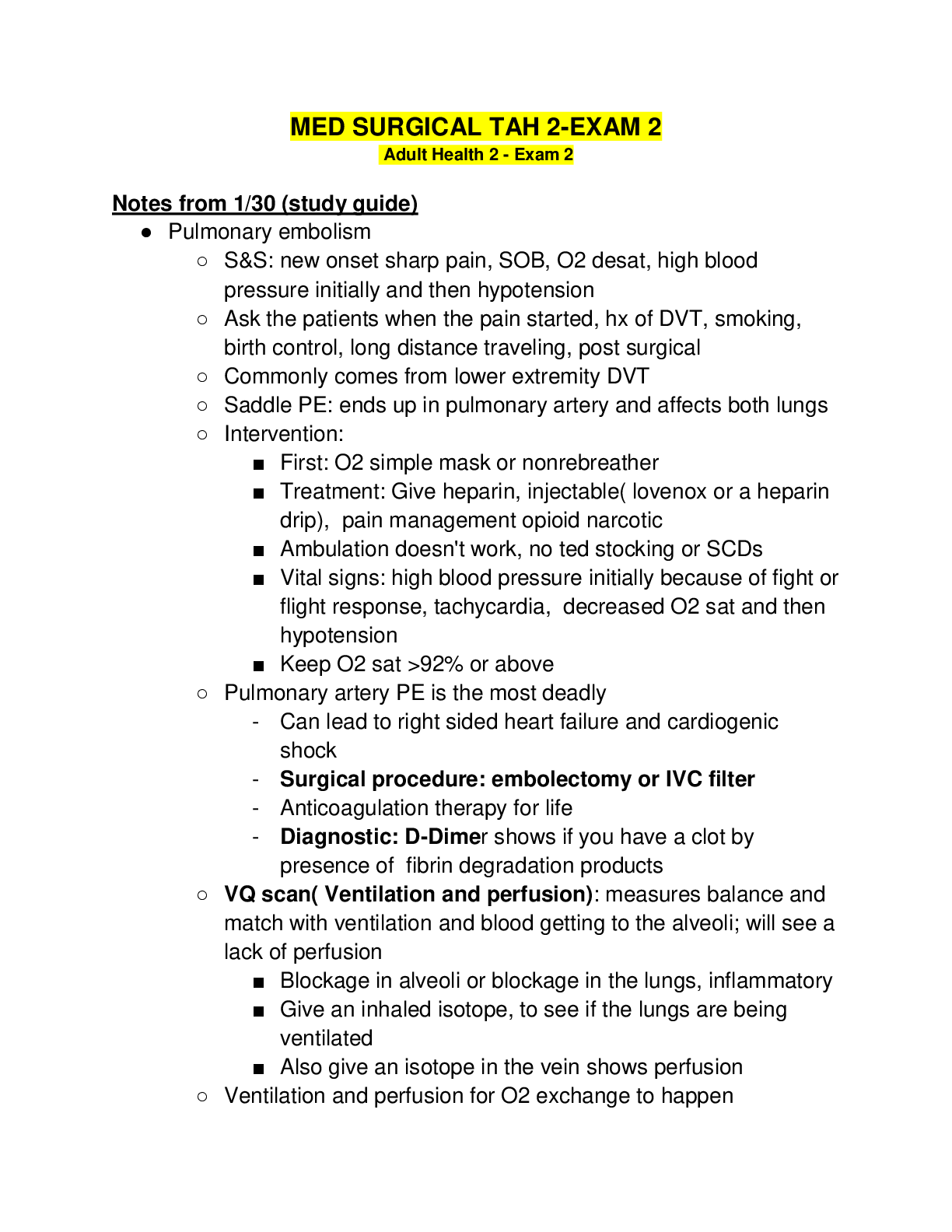
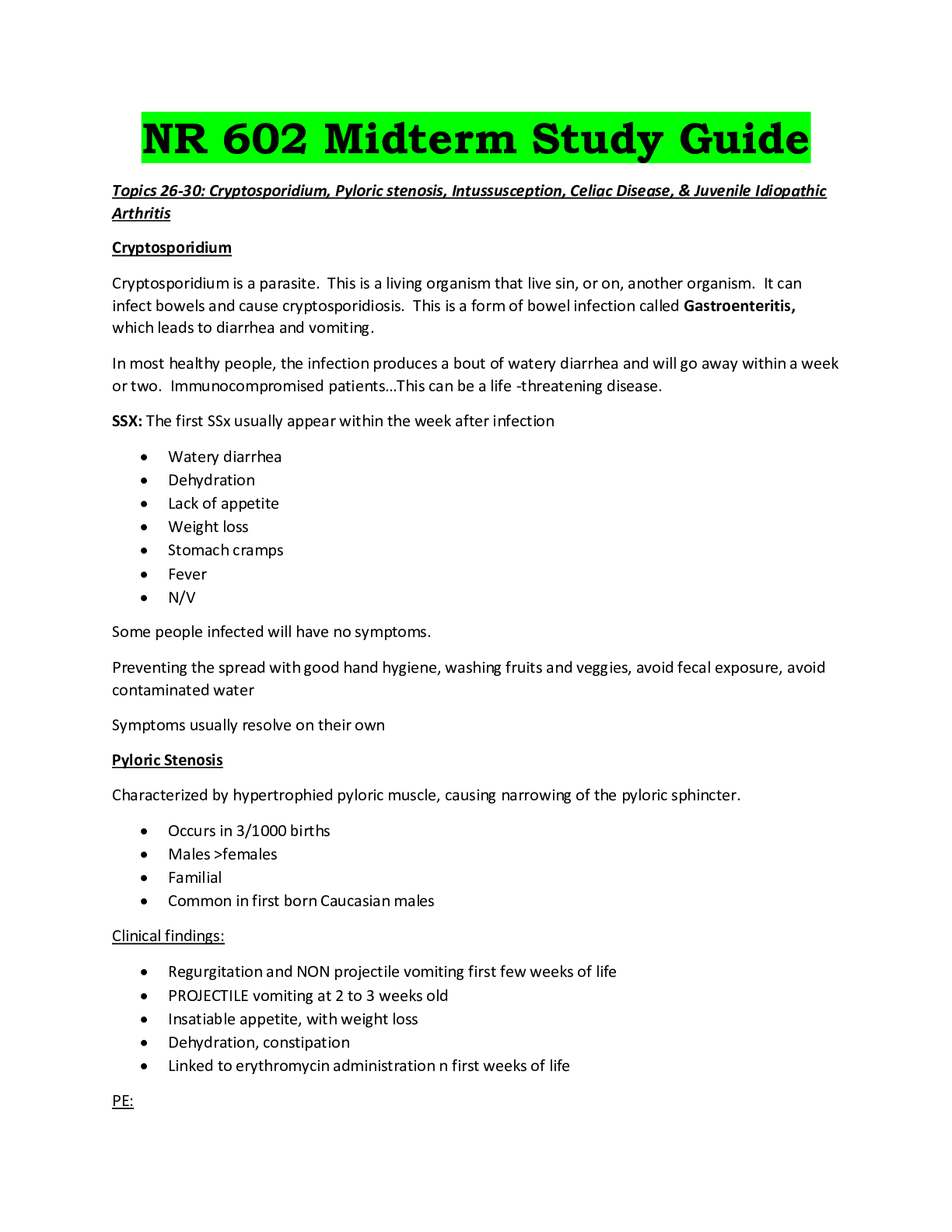
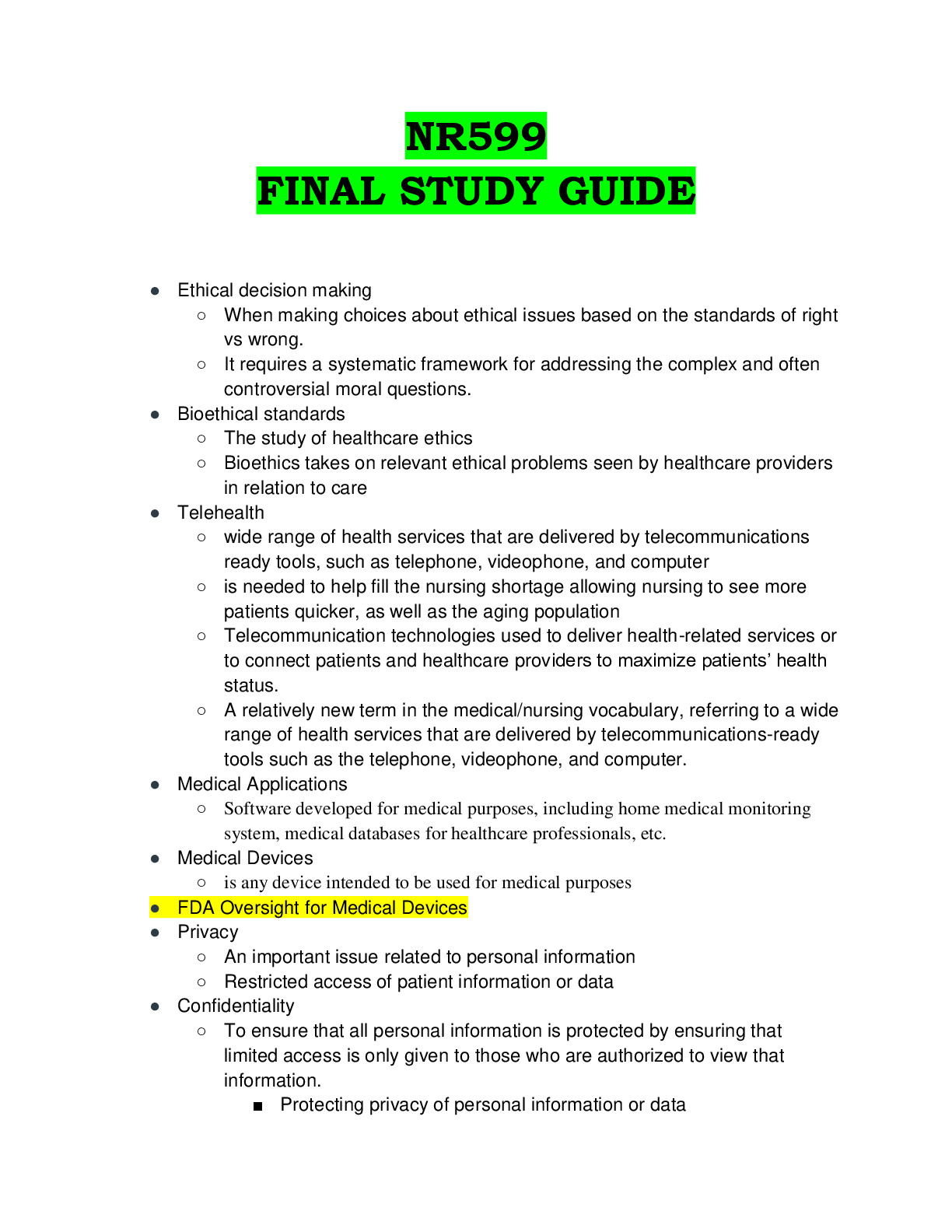
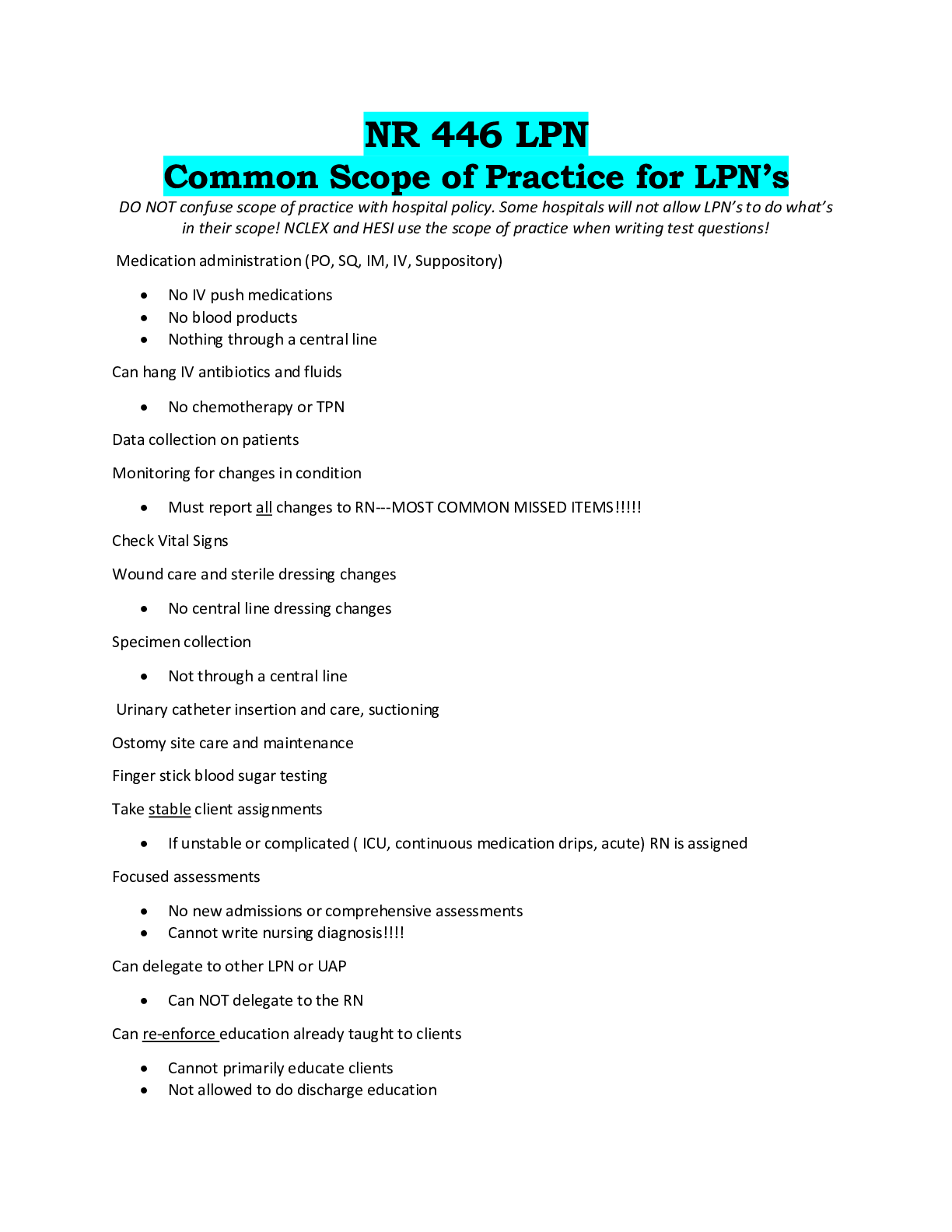
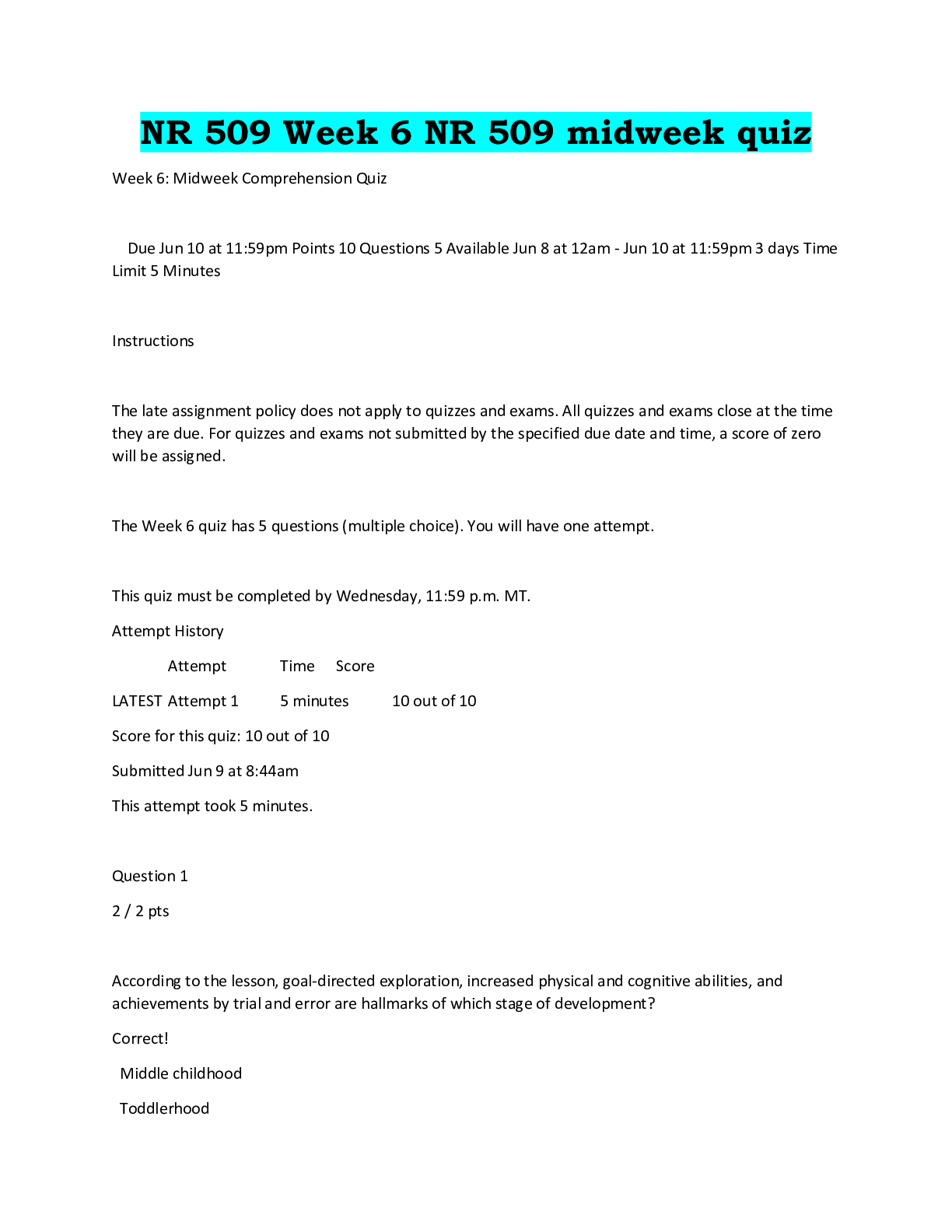
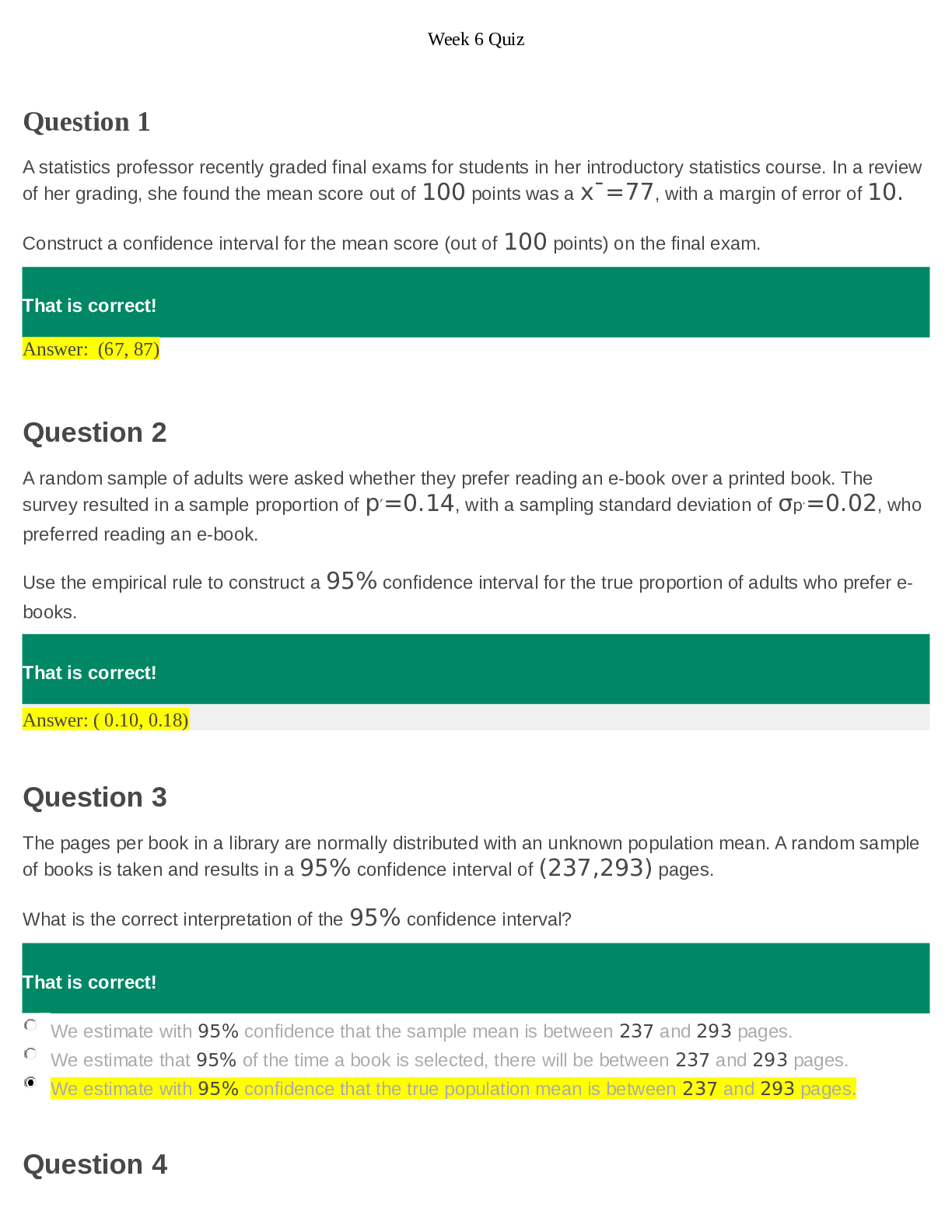

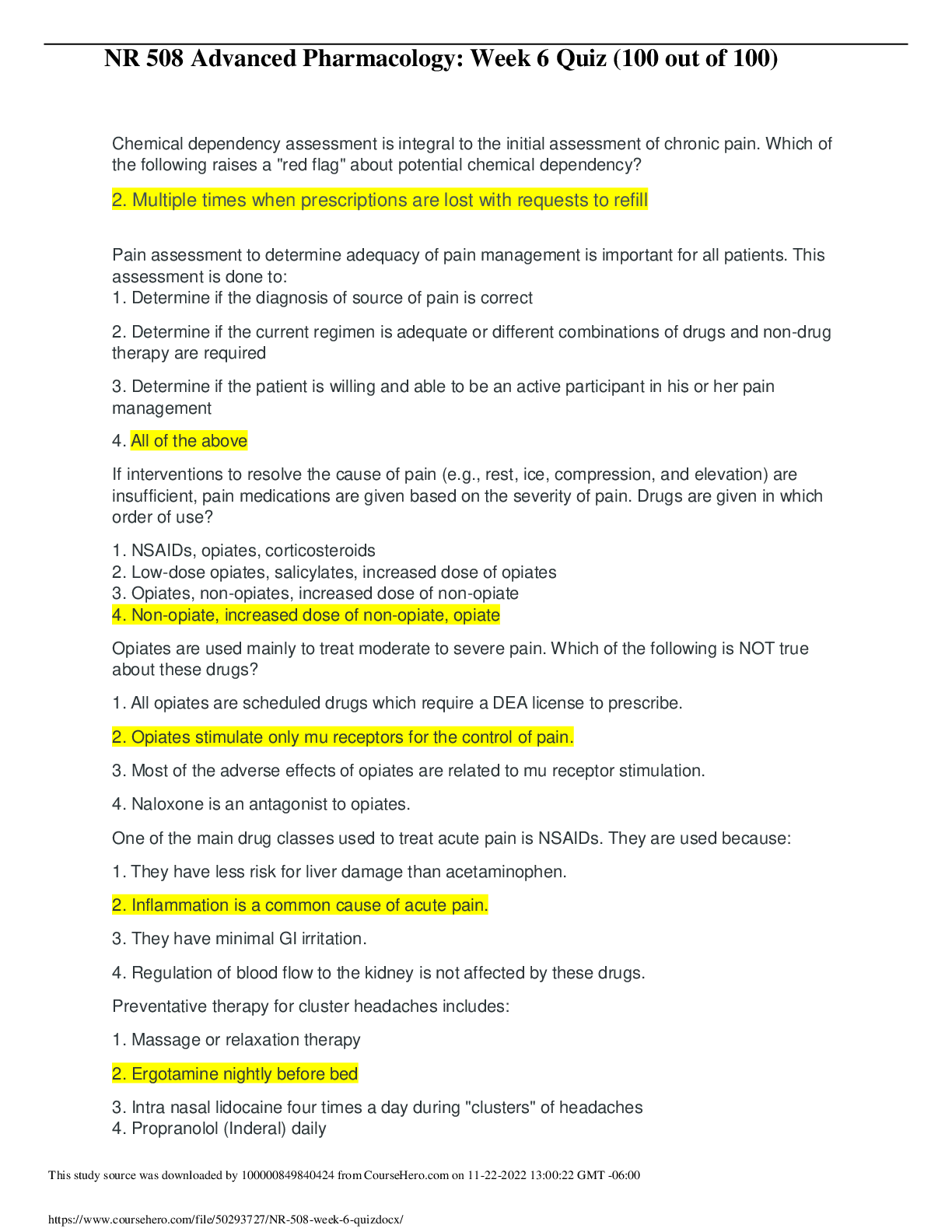
.png)