*NURSING > QUESTIONS & ANSWERS > C475 – Care of the Older Adult – Study Plan #1 /(finished care of older adult study guide) | Wes (All)
C475 – Care of the Older Adult – Study Plan #1 /(finished care of older adult study guide) | Western Governors University
Document Content and Description Below
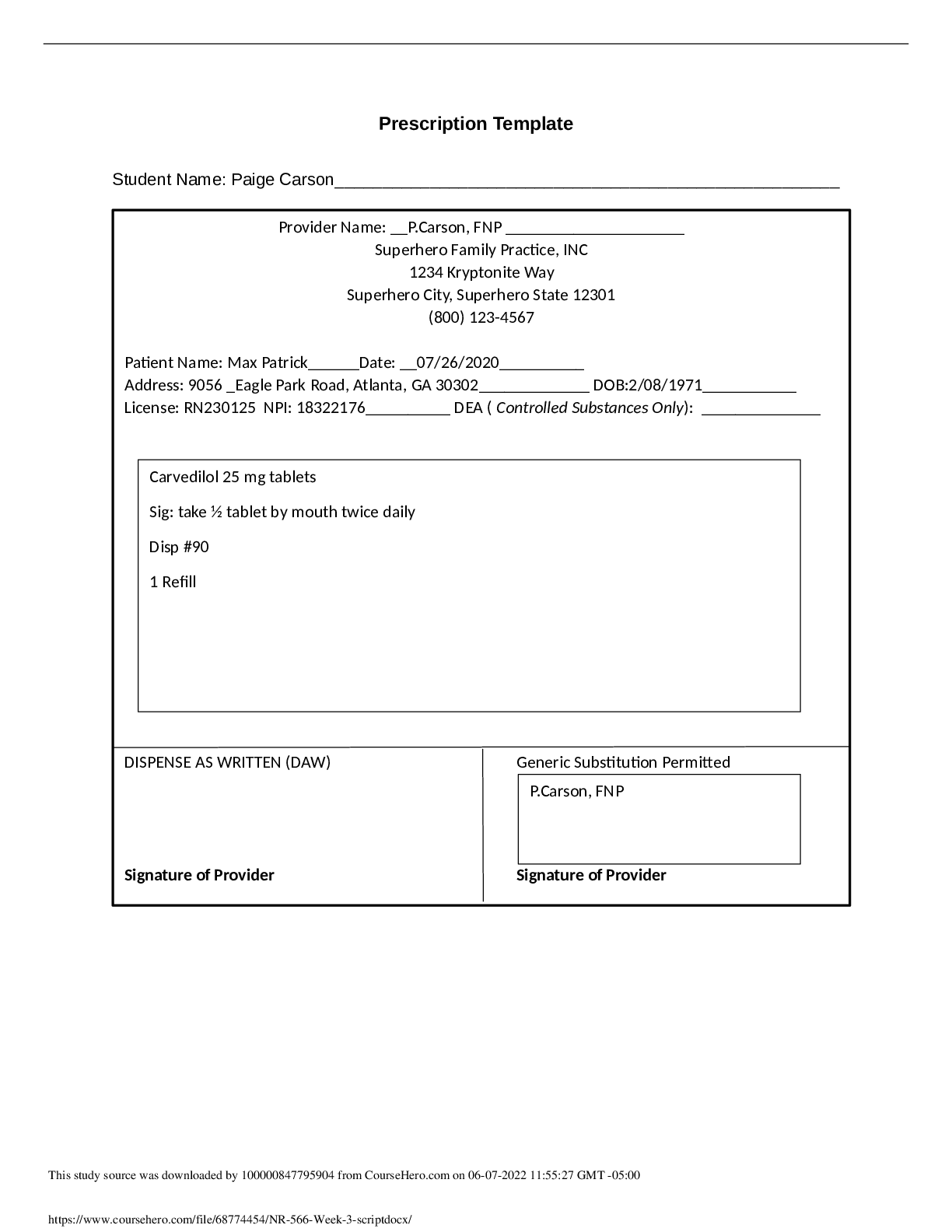
C475 – Care of the Older Adult – Study Plan #1 1- Compassionate and Respectful Care of Older Adults 1) How do the five senses help the older adult interpret various forms of communic... ation? Hearing- use repeat method, elimate backround noise, ask if volume of voice is approriate for pt, maintain direct line of vision so pt can see lips, provide time for pt to process and anwser, summarize, limit amount of spearks talking to the pt. Vision- maintain eye contact, visuals of teaching such as pictures/graphs. use large easy to read print for education, make sure glasses are present for pt. Touch- use touch to maintain attention/comfort Cognitive processes- include pt, if mentaly impaired have care giver present for education, summarize, provide written inforamtion, speak at a slower rate, avoid jargen 2) Explain how the aging of Baby Boomers has impacted the healthcare system in the United States? Over 75% of baby boomer population have atleast one chronic disease, now that peaople are living longer this requires use of goverment health assistance such as medicare,medicaid, social security and increased demand for nurses in the long term and cute care settings. Geriatric specialty needs has also increased. 3) Describe Miller’s Functional Consequences Theory of Aging? Environmental and biopsychosocial consequences impact functioning. Nursing’s role is risk reduction to minimize age-associated disability in order to enhance safety and quality of living. Miller’s theory has been used to create an assessment tool for the early detection of hospitalized elderly patients experiencing acute confusion. 4) List 4 health disparities seen among the African-American population in the US. Distrustful of the healthcare system, increased cases of heart disease, htn,stroke, 5) Describe effective communication techniques for patients who have cognitive impairment? Use repeat method/clarification, face pt, have caregiver present, use pts first language, determine level of compentcies/skills. 6) Which teaching preferences are desired by most older adults? Methods that enable them to keep up with what’s going on in the world,Methods that are direct, hands-on experiences,Methods that are easy to access, require small investments of time and money to get started,and allow learning to begin immediately. 7) Write two questions you could ask a patient to screen for spiritual needs. Do you consider yourself a spiritul person? do you need to see a chaplian? do you have any spiritual needs at this time? 2- Health Promotion/Maintenance and Living Environments of Older Adults 1) How does the heart of an older adult respond to exercise? With age, the increased heart rate and contractility usually associated with exercise become less pronounced; however, opposition to blood flow increases. With these changes, an overall decline in cardiac function and cardiac output is observed with initiation of exercise 2) Describe how changes in kidney function can contribute to ADRs (adverse drug reactions). A decline in GFR becomes significant as people age because elimination of waste andtoxins declines, causing an accumulation of harmful substances such as uric acid and medications in the body, causing an increased chance of adr. they cannot metabolize effictivley. 3) Explain “start low and go slow.” The key phrase in geriatric pharmacy remains “start low and go slow” because of renal changes that affect pharmacokinetics and pharmacodynamics with age Titration should be done cautiously, with close monitoring of the older adults response to the medication. 4) What are controllable risk factors for stroke? Prevention of afib rvr, htn, stress, dm, smoking, high choleterol 5) Which lifestyle modifications would you teach a patient with heart failure? Reduce stress, low fat diets, low ldl diet, dont smoke, control htn 6) Describe the Mini-Cog tool and how it is utilized. Screening consists of a three-item recall and a clock-drawing test. Assess language comprehension, visual—motor skills and executive function 7) How would you perform a functional assessment and what tools would you use? Assess ability to perform self-care, self-maintenance, and physical activities. There are two approaches: One approach is to ask questions about ability, and the other approach is to observe ability through evaluating task completion of ADLS. 8) Define frailty and interventions to prevent it. Fraility is the weakening of the pt and decrease of ability. To prevent we must identify early signs and keep the pt active and include them in the plan of care 9) What exercise recommendations would you offer an older adult? Brisk walking, tia chi, swimming 10) Describe nutrition bull’s-eye. People to consume the nutritious foods that are listed in the center of the bull’s-eye. These foods are low in saturated fat, sugar, and sodium, and high in fiber. They include skim milk, nonfat yogurt, most fruits and vegetables, whole grains, beans and legumes, and water-packed tuna. As you move to the foods listed in the rings farther away from the bull’s-eye, you eat more saturated fat, sugar, sodium, and low-fiber foods. In the outer ring of the bull’s-eye, therefore, are most cheeses, ice cream, butter, whole milk, beef, cake, cookies, potato chips, and mayonnaise. 11) What is the USPSFT recommendation regarding colorectal cancer screening for older adults? Screening recommendations are graded by expert panels according to the strength of the supporting evidence and the net benefit. The USPSTF uses the following rating scale: Level A: The USPSTF recommends the service. There is high certainty that the net benefit is substantial based on rigorous experimental research with consistent results. Level B: The USPSTF recommends the service. There is high certainty that the net benefit is moderate or there is moderate certainty that the net benefit is moderate to substantial. Level C: Clinicians may provide this service to selected patients depending on individual circumstances. However, for most individuals without signs or symptoms there is likely to be only a small benefit from this service. Level D: The USPSTF recommends against the service. There is moderate or high certainty that the service has no net benefit or that the harms outweigh the benefits. Level I: The USPSTF concludes that the current evidence is insufficient to assess the balance of benefits and harms of the service. Evidence is lacking, of poor quality, or conflicting, and the balance of benefits and harms cannot be determined. 12) Give an example of primary prevention. Vaccines 3- Health Needs of Older Adults 1) Which factors would you include in your assessment of sleep? What are your activities before sleeping? how long do you sleep? quality? how do you relax? schedule? routines? SPICES 2) Discuss risks of hypnotic drugs in older population Over sedation, bradycadia, hypotension, confusion, fall risk increase, decrease saliva production 3) Describe the physiological, psychological & social implications of dysphagia. Pts inability to comunicate properly declines social interaction which can lead to depression and low self esteem. Choking hazard from decreased muscle use to the mouth and throat. 4) Which 2 supplements may help prevent falls? Calcium and vit D3 for healthy bone production 5) Your patient has a 1 x 1 cm shallow ulcer on sacrum. The wound has a red base and minimal drainage. How would you treat this? What interventions would you recommend to off-load the area and protect from further injury? A Polyurethane Foam dressing would be the best for this ulcar. using positioning aids such as wedges and pillows as well as turning pts often and checking the skin with every assessment. nutrition also plays a huge role in ulcer prevention. underweight and malnutrition pts more at risk. 6) List 4 ways you might manage anxiety in your patient. Decrease environmental stimuli, Stay with the patient, Make no demands and do not ask the patient to make major decisions. 7) What are common causes of depression? Decline in health or new onset of illness, Exposure to multiple medications and their associated side effects, as well as drug–drug interactions, can cause elders to feel physically and mentally “down”, Having outlived spouses, loved ones, and friends and Having to move from private homes to assisted living or long-term care because of decreasing ability to live independently 8) Describe a brown bag assessment and the advantages of this. Patients bring in all of the medications they are currently taking, including OTCs, supplements, and herbals, to their clinic visits or hospitalizations for assessment. This method is far superior to relying on patient self-report, internal medical records, or transferred medical records from other providers. Even insurance claims data are not as accurate as face-to-face, brown bag medication assessment. This eliminates polypharmacy, repeat med orders and adverse reactions of meds 9) Give an example of how use of a “natural product” could cause harm to a patient. Interaction with oother meds pt is taking could have a harmful reaction. 4- Promoting Independence and Autonomy While Reducing Risk Factors in Older Adults 1) Describe the benefits of using an interdisciplinary team to plan care. Centers on the ability to deliver patient-centered care, which takes into account the whole person, the context in which they find themselves, and their presenting concerns 2) How does a leader foster a culture of safety? Create a blame-free culture, there is an assumption that errors spring up as a result of problems within a system. On the other end of the spectrum is a punitive culture, in which errors are blamed on individuals. When there is a culture of safety, there is middle ground between these two ends of the spectrum, with a balance between them. 3) List the 4 steps in the delegation process 1 assessment of the patient, the staff, and the context of the situation; 2 communication to provide direction and opportunity for interaction during the completion of the delegated task; 3 surveillance and monitoring to assure compliance with standards of practice, policies, and procedures; and 4 evaluation to consider the effectiveness of the delegation and whether the desired patient outcome was attained 4) How would you determine a patient’s decision-making capacity? Ability to appreciate the current situation and its consequences, Ability to reason or manipulate information rationally, Ability to communicate a choice 5) Describe ways to facilitate autonomy for a patient who lives in a long-term care facility. Encourage completion of advance directives Provide patient-centered care Provide appropriate education and training to patients and their family Ensure consents and refusals are truly informed Support and educate patients about their rights Stay informed of regulatory guidelines and laws related to the elderly Provide feedback to legislators developing laws that affect the elderly Know how to assist patients to access resources and navigate insurance and the healthcare system 6) Outline risk factors for a victim of elder abuse Psychiatric illness/psychological problems Poor physical health or frailty Behavior (provocative/aggressive/resists care) Cognitive impairment Older than 75 years Female Ethnicity Low Income Trauma or past abuse Personality trait 7) Discuss the 3 R’s in detecting & reporting elder abuse. Reconize the signs, assessment, and risk factors , Respond with a plan of action and look up state laws, Report to the approriate athorities 5- Promoting Health and Independence in Older Adults 1) Describe the differences between dementia and delirium. Demintia- Congnitive graduial detereation non reversable Delirium- Temporary cognitive impairment reversable 2) Which characteristics describe the “moderate” stage of Alzheimer’s disease? Behavioral and psychological symptoms of dementia (BPSD) are most commonly exhibited during the moderate stage- 24 hr supervision 3) What nursing interventions are appropriate for managing behavioral symptoms of dementia? Calm enviroment, Pharmacological therapy for AD would prevent beta-amyloid plaques and/or ameliorate the neuronal damage caused by the plaques and neurofibrillary tangles. Unfortunately, currently no medications are available that have this mechanism of action, although many new promising agents are being studied. Two classes of medications currently are approved for the treatment of Alzheimer’s dementia: cholinesterase inhibitors (CEIs) and N-methyl-d-aspartate (NMDA) receptor antagonists. 4) List 4 precipitating factors for delirium in the hospitalized patient. Hunger Thirst Toileting needs Feeling too hot or too cold Pain Boredom Overstimulation Certain people Certain activities (meals, baths) 5) Describe nursing interventions for the delirious patient who is agitated. Avoid provoking situations. Intervene early, before the behavior escalates. Remain calm; speak in a soft voice. Approach slowly from the front. 6) What nursing assessments will you perform to identify risk factors for falls? Pulse: Arrhythmias, bradycardia Orthostatic blood pressure: Postural hypotension (see Box 12-6) Oxygen saturation/pulse oxygen: Low oxygen saturation leads to confusion Vision screening deficits: Evaluate need to use glasses, visual acuity, depth perception, peripheral vision Muscle strength: Weakness in one or both sides Range of motion in neck, spine, and extremities: Limitations in range of motion Gait and balance 7) Outline 5 interventions you would implement to prevent falls in the acute care setting. Vitals, positioning of belongings, bathroom assistance, call bell in reach, bed alarm on, bed in low position. 8) Differentiate between stress incontinence and functional incontinence. Stress- Involuntary loss of urine during activities that increase intraabdominal pressure (e.g., lifting, coughing, sneezing, and laughing) Functional- Results from problems external to the lower urinary tract, such as cognitive impairment, physical disability, and environmental barriers. 6- Technology-Assisted Care of Older Adults 1) Describe how you would teach an elderly patient about a new assistive technology. Mnemonics and cues will favorably affect self-efficacy in handling new products. Training sessions should be held in the home or natural meeting places of the elderly. Instructor should be well known by the elderly or introduced well in advance of the training. The attitudes of the instructors toward the aged must be positive and realistic 2) What are the 7 common applications for assistive technology? Dragon Dictation: This voice-recognition application allows users to dictate text or email messages and see them instantly, including tweets or status updates for Facebook. Voice Reading: Excellent for those who get tired reading long emails or Web content; the application will read aloud any text shared from other applications, URLs, or even text files. EyeReader: This application acts as a magnifying glass. By holding their iPhone in front of a book or newspaper users get a clear picture of the text with a light to help brighten it. Vouchercloud: This application, from one of the original money-saving coupon Websites, offers on-the-go discount vouchers. Idealo: An application that allows cost-conscious shoppers to scan the barcode on a product and search for the cheapest place to buy it online. Mint Bills: Users can streamline their bill pay and view all of their accounts in one place with this mobile application. Pill Reminder Pro: Users can enter in the name of their pill, dosage, frequency, and what times of day it is taken, and PillReminder will alert them when it is time to take their pills. 3) Give an example of how nursing informatics can improve patient safety. Assitive technology such as EMR and barcode med scanners as well as CPOE are all systems in informatics that work as a safe garud for orders and med passes. 4) Describe ways robotic assistance might result in a patient remaining in their own home for a longer period of time. Robotics can help the patient achieve independence in medication taking, sosical interaction, tele visits with healthcare providers keeps the patient the center of care plan and included as well as "reminding systems" to help the patient not get confused or lost 7- Healthcare Systems and Health Policy 1) Describe a patient for whom an assisted living facility might be a good option. Provide assistance and monitoring of older residential adults for whom independent living is no longer appropriate but who do not need 24-hour skilled nursing home care. 2) Describe the Bismarck model of healthcare coverage. Employers and employees fund health insurance in this model – those who are employed have access to “sickness funds” created by compulsory payroll dedications 3) List the 3 Triple Aim goals. Better care, better health outcomes, and lower costs 4) Briefly outline what is covered by Part A, Part B and Part D of Medicare. Part A- Blood, home health services, hospice, inpatient hospital care, SNF care (for transitional care Part B- Doctor and other healthcare provider services, outpatient care, durable medical equipment, mental health services, some home care services, some screening and preventive services, laboratory services Part D- Multiple plans are offered from which a beneficiary can choose. Plans vary in prescriptions covered, deductible, premium, and copayment. 5) Outline the 7 components of the Affordable Care Act. Elimination of lifetime limits for health insurance coverage for essential services Elimination of the ability of insurance companies to rescind coverage Free preventive care Development of a prevention and public health fund Increased access to affordable care, including a provision for preexisting conditions Quality improvement and cost reduction programs Increased access to health care in the community or at home, which provides more options for care outside of institutional settings 6) Why do you think it is important for nurses to be familiar with healthcare delivery systems in other countries? Patient come from diverse backrounds and a patient may be headed back to that country after current care, or not know what there coverage covers. 8- Care Transitions 1) Describe the various duties a nurse might perform when working in transitional care. Contribute to the safety and continuity of care for their patients upon discharge to home or transfer to another care setting. 2) Explain how transitional care can prevent hospital re-admissions. Resources such as plan of care, dc plans starting as soon as pt is admitted and interplanary teams communicating and making the pt the center have been identified and projects have been proposed to discover appropriate interventions across the healthcare continuum. 3) List factors that can lead to poor outcomes in the transition of care. (1) inadequate education to patients and their families about care management, (2) poor communication between patients and care providers, (3) inadequate assessment at point of care, (4) medication discrepancies, (5) lack of follow-up care, (6) health literacy issues, (7) lack of support systems, and (8) cultural barriers. 4) Besides demographic data, describe the patient information that you would include on a transfer form. Detailed assessment Treatments Wounds Current medications Allergies Level of independence Recent diagnostic testing Primary care practitioner notification upon discharge and admission to the receiving facility 9- Palliative and End-of-life Care 1) List components of “Five Wishes” document. Five Wishes is a movement that encourages people to provide more specific instructions than those offered by a living will, including one’s wishes in five categories: The person chosen to make decisions when the individual can no longer make them for himself or herself—a durable power of attorney for health care The kind of treatment the person wants or does not want—a living will How comfortable the person wants to be How the person wants to be treated by others What the person wants his or her loved ones to know 2) How does “AND” differ from “DNR”? Allow natural death no life saving measures like cpr will be performed with a DNR with a AND promotes a more positive approach to consideration of a person’s wishes at end of life. 3) What is the major goal of palliative care? to make the patient comfortable as possible 4) Who would qualify for hospice? What are the benefits of referring a patient to hospice? Anyone with a serious illness whom doctors think has only a short time to live, often less than 6 months. Hospice provides comprehensive comfort care to the dying person as well as support to his or her family 5) Summarize treatment options for neuropathic pain and nocioceptive pain. For nociceptive pain, the first-line management is with pharmacological analgesic medication. For neuropathic pain, the aim of the treatment is to relieve the pain caused by damage to the nerves. In most cases, analgesic medications are unable to provide effective relief and, instead, the nerves themselves must be targeted. Neurostimulation therapy is used to excite the nervous tissue 6) How can you facilitate a “good death” for a patient? Instilling good memories Uniting with family and medical staff Avoiding suffering, with relief of pain and other symptoms Maintaining alertness, control, privacy, dignity, and support Becoming spiritually ready Saying goodbye Dying quietly [Show More]
Last updated: 1 year ago
Preview 1 out of 12 pages
Reviews( 0 )
Document information
Connected school, study & course
About the document
Uploaded On
May 25, 2021
Number of pages
12
Written in
Additional information
This document has been written for:
Uploaded
May 25, 2021
Downloads
0
Views
25

 And LETRS Unit 8 Final Assessment Test.png)