*NURSING > STUDY GUIDE > NURS 261_Health Assessment for Nursing Practice Midterm Study Guide Spring 2019/2020 – Virginia Co (All)
NURS 261_Health Assessment for Nursing Practice Midterm Study Guide Spring 2019/2020 – Virginia Commonwealth University | NURS261_Health Assessment for Nursing Practice Midterm Study Guide Spring 2019/2020
Document Content and Description Below
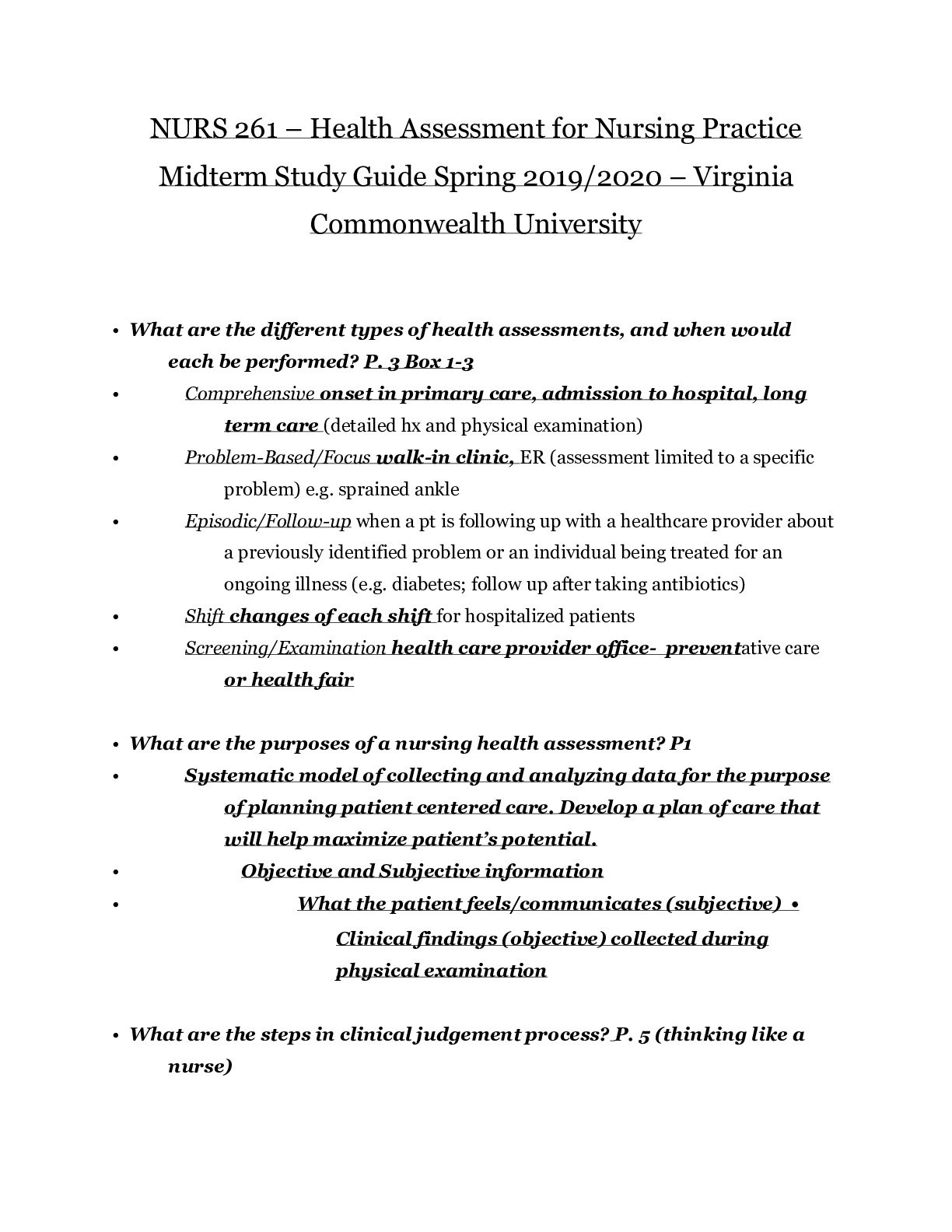
NURS 261_Health Assessment for Nursing Practice Midterm Study Guide Spring 2019/2020 – Virginia Commonwealth University NURS261_Health Assessment for Nursing Practice Midterm Study Guide Spring 201... 9/2020 • What are the different types of health assessments, and when would each be performed? P. 3 Box 1-3 • Comprehensive onset in primary care, admission to hospital, long term care (detailed hx and physical examination) • Problem-Based/Focus walk-in clinic, ER (assessment limited to a specific problem) e.g. sprained ankle • Episodic/Follow-up when a pt is following up with a healthcare provider about a previously identified problem or an individual being treated for an ongoing illness (e.g. diabetes; follow up after taking antibiotics) • Shift changes of each shift for hospitalized patients • Screening/Examination health care provider office- preventative care or health fair • What are the purposes of a nursing health assessment? P1 • Systematic model of collecting and analyzing data for the purpose of planning patient centered care. Develop a plan of care that will help maximize patient’s potential. • Objective and Subjective information • What the patient feels/communicates (subjective) • Clinical findings (objective) collected during physical examination • What are the steps in clinical judgement process? P. 5 (thinking like a nurse) • What are the factors in symptom analysis? P. 15 • Systematic method of collecting data about the history and status of symptoms • Onset, location, duration, characteristics, aggravating and alleviating factors, related symptoms, treatment, severity of symptoms • How does the nurse assess pain? • Collect subjective data, interviews patients about present health status, how they manage their pain. Use OLD CARTS • Rely on self-report of patient • Pain Scales • Numeric (NRS) 0-10 , 0 no pain 5 moderate 10 worst pain possible • Wong-Baker FACES, No Hurt-Hurts to Hurts Worst Alternative coding 0-10 (2) • Compare health promotion and health protection. P. 5 Table 1-1 • Health Promotion- desire to increase well-being (individual) • Primary- prevent a disease from developing (immunizations) • Secondary-screening effort (BP screening) • Tertiary-acute or chronic disease minimize, max health benefits (diabetes mgt) • Health Protection- desire to actively avoid illness (guidelines prevent spread of communicable diseases) • Detect illness early • Maintaining functioning within its constraints • Describe the differences between a screening assessment and a follow up assessment. P. 3 • Screening assessment- short exam focused on disease detection/prevention • Blood pressure, glucose, cholesterol, colorectal • Follow-up assessment- previously identified problem • Pneumonia after antibiotics • Diabetes follow ups • Identify infection control procedures to be used when conducting a health assessment. (i.e. when do you wear gloves, and when don’t you) Box 3-1 P. 22 • Gloves • To protect from bloodborne pathogens carried by patient • To protect patient from microorganism on the hands of the nurse • To reduce the potential of infection transmission from patient to patient via the nurse • giving an injection • emptying a urinary catheter drainage bag • giving a bed bath • inserting a peripheral IV (an IV in a smaller vein) • removing a peripheral IV • removing a urinary catheter • Mask, Eye/Face shield • During procedures that may result in splashes or sprays of blood, fluids, secretions • Not usually done during health assessment. • Gowns • To protect arms-exposed skin and prevent contamination of clothing with patients’ blood or fluids • What are the differences between subjective and objective data? See above • Symptoms are considered subjective data • data that is perceived and reported by the patient (e.g. pain, itching, nausea) • Signs are considered objective data • data that can observed, felt, heard, or measured (e.g. rash, swelling) • What assessment techniques are used to evaluate vital signs? P. 23 • BP • Pulse • RR • Pulse O2 • Temperature • Techniques of Physical Assessment: • Inspection- Pain, Respiration, Visual exam of body, movement and posture. • Palpation- HR hands to feel texture, size, shape, consistency, pulsation • Percussion-evaluate size, boarders, consistency of internal organs (fluid) • Auscultation- BP listening to sounds heat blood vessels, lungs, intestine. • Define orthostatic hypotension and describe how to assess for it. P. 42 • Series of BP measurements Lying, sitting and standing position • It is a 20 to 30 mm drop when patient goes from lying to sitting position to standing • State the rationale and technique for the two step blood pressure measurement. • requires that you take the blood pressure by feeling the brachial artery and then using a stethoscope. So, in a sense you will be taking the blood pressure twice using the same arm but with two methods. • Give an example of how each physical assessment technique is used: inspection, palpation, percussion, and auscultation. See Q19 • Inspection: e.g. using a penlight to inspect jugular vein pulsation • Palpation: e.g involves hands to feel • Percussion: • Auscultation: the use of the stethoscope • Identify the use of the bell and diaphragm of a stethoscope. 28 • Bell Low(soft) pitch sounds- extra heart sounds, vascular (bruit-whooshing) • Diaphragm high pitch sounds breath, bowel, normal heart • What is meant by “general survey”, and what are the elements included? P 483 • Collected during the history, Physical Exam LOC/ Mental Status Personal Hygiene Skin Color Posture/position Breathing effort Mobility Ability to hear and speak Example: Cooperative, oriented, alert women; sitting with erect position; maintains eye contact; appropriately groomed and dressed; Vital signs BP 110/7; P7; R14; T 98: Wt 137; Ht 5’3; BMI 24.3 - - - - - - - - - - - - - - - - - - - - - - • Describe the routine exam of the peripheral vascular system, including pulses that should be palpated. Palpate: femoral, popliteal, anterior tibial and dorsalis pedis pulses Temporal: lateral to each eyebrow- amplitude Carotid: lower 3rd of neck, one at a time-amplitude Inspect: Jugular- pulsations Measure Blood pressure Inspect and Palpate upper extremities, pulses Inspect and Palpate lower extremities, pulses Brachial- antecubital fossa Radial- on thumb side of forearm, same time both Ulnar- medial side of forearm For amplitude: Femoral Popliteal Tibial Dorsalis Pedis • Define the scale used to describe amplitude of peripheral pulses. 0+ absent 1+ diminished barely palpable 2+ normal 3+ Full Volume 4+ Full Volume bounding hyperkinetic • Differentiate between arterial and venous insufficiency. Arterial insufficiency: • Usually calf • Pain worse with activity – prolonged walking • If pain is relieved by rest it is called “intermittent claudication” (artery 50% occlusion), if not relieved by rest it is called “rest pain” • Worse with legs elevated, better when dependent • Venous insufficiency: • Intensifies with prolonged standing or sitting • Pain worse in dependent position • Pain is better when legs are elevated and worse at end of the day • Define the scale used to describe the level of pitting edema. P222 • 1+ barely perceptible pit • 2+ deeper pit in a few seconds • 3+ deep pit, rebounds in 10-20 seconds • 4+ deep pit, rebounds > 30 seconds [Show More]
Last updated: 1 year ago
Preview 1 out of 24 pages
Reviews( 0 )
Document information
Connected school, study & course
About the document
Uploaded On
Jul 14, 2020
Number of pages
24
Written in
Additional information
This document has been written for:
Uploaded
Jul 14, 2020
Downloads
0
Views
33




.png)