*NURSING > QUESTIONS & ANSWERS > Chapter 15: Structure and Function of the Neurologic System: Chapter 17: Alterations in Cognitive Sy (All)
Chapter 15: Structure and Function of the Neurologic System: Chapter 17: Alterations in Cognitive Systems, Cerebral Hemodynamics, and Motor Function: Chapter 18: Disorders of the Central and Peripheral Nervous Systems and the Neuromuscular Junction: Chapter 19: Neurobiology of Schizophrenia, Mood Disorders, and Anxiety Disorders : Chapter 20: Alterations of Neurologic Function in Children
Document Content and Description Below
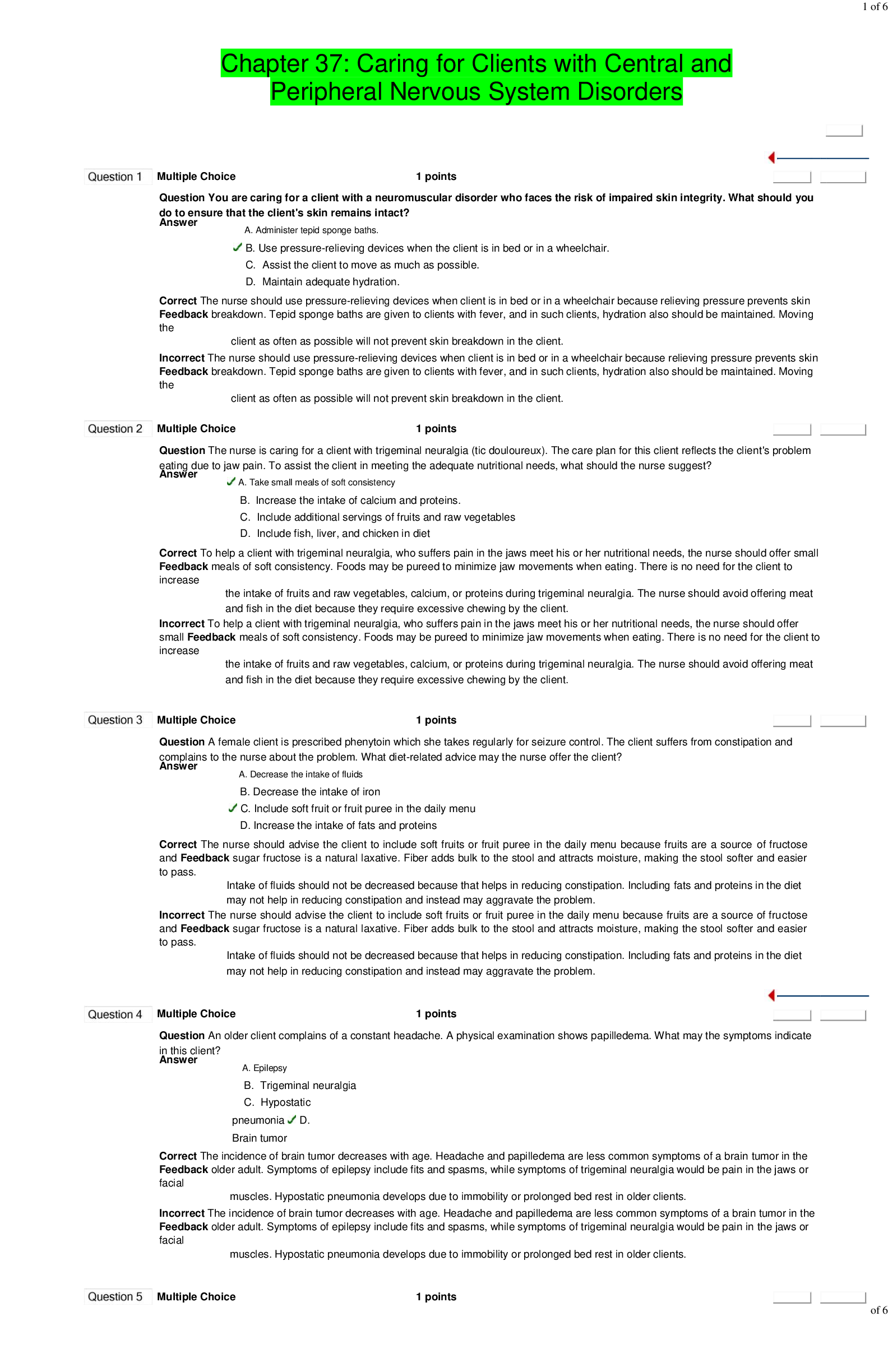
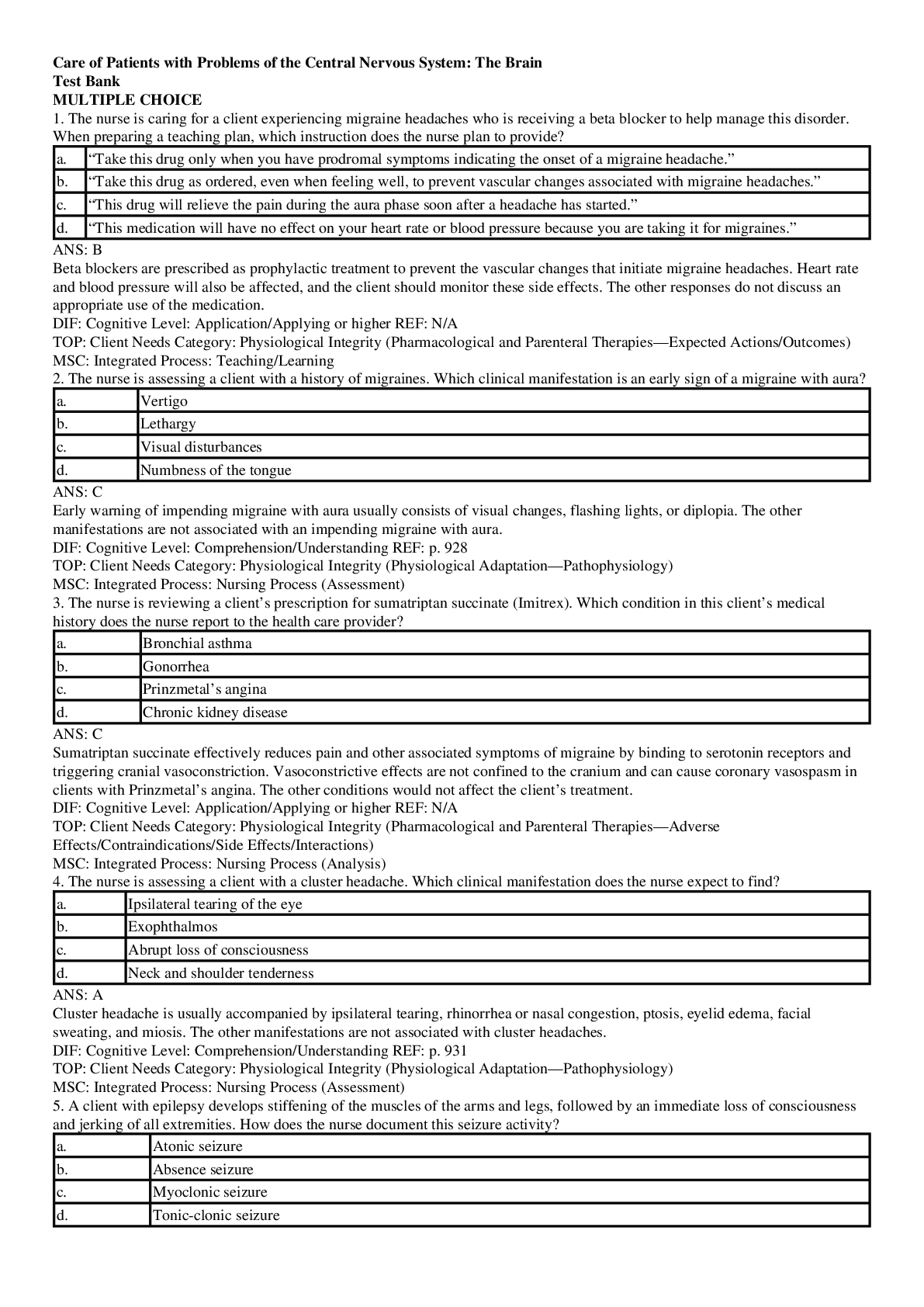
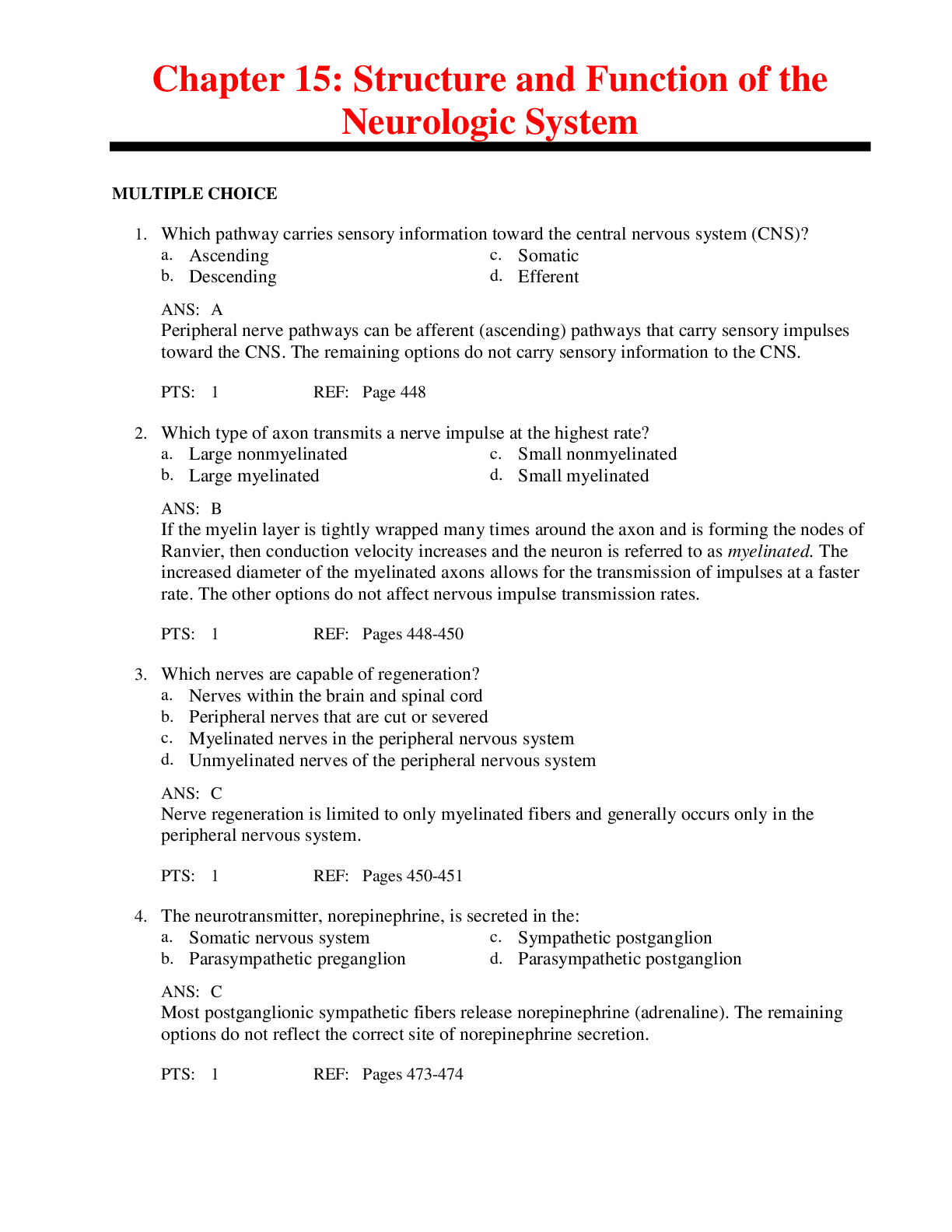
Chapter 15: Structure and Function of the Neurologic System MULTIPLE CHOICE 1. Which pathway carries sensory information toward the central nervous system (CNS)? a. Ascending c. Somatic b. De... scending d. Efferent 2. Which type of axon transmits a nerve impulse at the highest rate? a. Large nonmyelinated c. Small nonmyelinated b. Large myelinated d. Small myelinated 3. Which nerves are capable of regeneration? a. Nerves within the brain and spinal cord b. Peripheral nerves that are cut or severed c. Myelinated nerves in the peripheral nervous system d. Unmyelinated nerves of the peripheral nervous system 4. The neurotransmitter, norepinephrine, is secreted in the: a. Somatic nervous system c. Sympathetic postganglion b. Parasympathetic preganglion d. Parasympathetic postganglion 5. Both oligodendroglia and Schwann cells share the ability to: a. Form a myelin sheath c. Transport nutrients b. Remove cellular debris d. Line the ventricles 6. During a synapse, what change occurs after the neurotransmitter binds to the receptor? a. The permeability of the presynaptic neuron changes; consequently, its membrane potential is changed as well. b. The permeability of the postsynaptic neuron changes; consequently, its membrane potential is changed as well. c. The postsynaptic cell prevents any change in permeability and destroys the action potential. d. The presynaptic cell synthesizes and secretes additional neurotransmitters. 7. What name is given to a large network of neurons within the brainstem that is essential for maintaining wakefulness? a. Midbrain c. Medulla oblongata b. Reticular activating system d. Pons 8. Thought and goal-oriented behaviors are functions of which area of the brain? a. Cerebellum c. Prefrontal lobe b. Limbic system d. Occipital lobe 9. The region responsible for the motor aspects of speech is located in the: a. Wernicke area in the temporal lobe c. Wronka area in the parietal lobe b. Broca area in the frontal lobe d. Barlow area in the occipital lobe 10. Parkinson and Huntington diseases are associated with defects in which area of the brain? a. Thalamus c. Cerebellum b. Medulla oblongata d. Basal ganglia 11. Maintenance of a constant internal environment and the implementation of behavioral patterns are main functions of which area of the brain? a. Thalamus c. Subthalamus b. Epithalamus d. Hypothalamus 12. The ability of the eyes to track moving objects through a visual field is primarily a function of which colliculi? a. Inferior c. Mid b. Superior d. Posterior 13. What parts of the brain mediate the expression of affect, both emotional and behavioral states? a. Hypothalamus and subthalamus c. Limbic system and prefrontal cortex b. Parietal and frontal lobes d. Basal ganglia and medulla oblongata 14. Reflex activities concerned with heart rate, blood pressure, respirations, sneezing, swallowing, and coughing are controlled by which area of the brain? a. Pons c. Cerebellum b. Midbrain d. Medulla oblongata 15. From which part of the midbrain do cranial nerves V to VIII emerge? a. Midbrain c. Medulla oblongata b. Pons d. Lateral colliculi 16. From which part of the midbrain do cranial nerves IX to XII emerge? a. Midbrain c. Medulla oblongata b. Pons d. Lateral colliculi 17. Which area of the brain assumes the responsibility for conscious and unconscious muscle synergy and for maintaining balance and posture? a. Cerebrum c. Diencephalon b. Cerebellum d. Brainstem 18. Which statement is true regarding upper motor neurons? a. Upper motor neurons directly influence muscles. b. They modify spinal reflex arcs. c. Upper motor neurons are located in the gray matter of the spinal cord. d. They extend their dendritic processes out of the CNS. 19. The membrane that separates the brain’s cerebellum from its cerebrum is the: a. Tentorium cerebelli c. Arachnoid membrane b. Falx cerebri d. Falx cerebelli 20. The function of arachnoid villi is to: a. Produce cerebrospinal fluid b. Provide nutrients to the choroid plexuses c. Transmit impulses within the meninges d. Absorb cerebrospinal fluid into the cerebral venous sinuses 21. Where is the cerebrospinal fluid produced? a. Arachnoid villi c. Ependymal cells b. Choroid plexuses d. Pia mater 465-466 22. Which of the meninges closely adheres to the surface of the brain and spinal cord and follows the sulci and fissures? a. Dura mater c. Pia mater b. Arachnoid d. Inner dura 23. Norepinephrine produces what primary response? a. Increased contractility of the heart c. Vasoconstriction b. Release of renin from the kidney d. Pupillary dilation 24. What is an effect of the sympathetic nervous system? a. Stimulation of peristalsis c. Reduction in heart rate b. Increased blood sugar levels d. Pupillary constriction 25. The brain receives approximately what percentage of the cardiac output? a. 80% c. 20% b. 40% d. 10% 26. The collateral blood flow to the brain is provided by the: a. Carotid arteries c. Circle of Willis b. Basal artery d. Vertebral arteries 27. The nurse recognizes that a patient’s diagnosis of a viral infection of the brain’s meningeal layer is supported by which diagnostic laboratory result? a. Chloride <110 mEq/L c. Protein <10 mg/dl b. Leukocytes >10/mm3 d. Glucose <40 mg/dl MULTIPLE RESPONSE 28. Which cranial nerves contain parasympathetic nerves? (Select all that apply.) a. I (olfactory) d. IX (glossopharyngeal) b. III (oculomotor) e. X (vagus) c. VII (facial) 29. The sympathetic nervous system primarily serves to protect an individual by doing which of the following? (Select all that apply.) a. Decreasing mucous production d. Decreasing sweat excretion b. Increasing blood sugar levels e. Increasing blood pressure c. Increasing body temperature 30. The aging process brings about what changes to human cells? (Select all that apply.) a. Increased neurofibrillary tangles d. Decreased myelin presence b. Imbalance of neurotransmitters e. Altered dendrite structure c. Increased neuron production 5 31. Which statement is true regarding the blood-brain barrier (BBB)? (Select all that apply.) a. The BBB is dependent on astrocytes. b. It uses the meningeal layers of the brain. c. It restricts the flow of large molecules, such as potassium. d. Naturally occurring inflammatory mediators affect the BBB. e. The BBB appears to play a role in slowing down the onset of degenerative brain disease. 32. A nurse caring for an older adult patient would expect which functional changes to occur? (Select all that apply.) a. Increased risk for falls b. Increased risk for falls c. Loss of muscle in the arms and legs d. Decrease in the need for social interaction e. Increased agitation and frustration levels 33. What evidence does the nurse expect to see when a patient experiences trauma to the hypothalamus? (Select all that apply.) a. Uneven expression of mood b. Unstable blood glucose levels c. Poor regulation of body temperature d. Visual disturbances such as blurred vision e. Nausea, vomiting, and symptoms of gastroesophageal reflux disease 34. A Schwann cell: (Select all that apply.) a. Can form the myelin sheath. b. Is also referred to as a neurolemmocyte. c. Affects the function of the nodes of Ranvier. d. Is located in the peripheral nervous system. e. Is responsible of decreasing conduction velocity. MATCHING Match the function with the appropriate cranial nerve. ______ A. Fibers emerge from the posterior midbrain and exit from the skull to run to the eye. ______ B. Provides motor and sensory functions to the face, mouth, nose, and eyes. ______ C. Fibers emerge from the midbrain, exit from the skull, and extend to the eye. ______ D. Controls motor functions to the pharynx and salivary glands and sensory functions from the pharynx and tongue. ______ E. Innervates muscles that move the eye laterally. ______ F. Affects control over the motor fibers to the muscles of tongue and sensory impulses from the tongue to the brain. ______ G. Is purely sensory and carries impulses for the sense of smell. ______ H. Is made up of parasympathetic motor fibers that supply the smooth muscles of the abdominal organs. ______ I. Transmits impulses for the sense of hearing. ______ J. Carries sensory and motor fibers to the pharynx and larynx. 35. Glossopharyngeal nerve 36. Oculomotor nerve 37. Trochlear nerve 38. Abducens nerve 39. Trigeminal nerve 40. Hypoglossal nerve 41. Vagus nerve 42. Spinal accessory nerve 43. Olfactory nerve 44. Vestibulocochlear nerve 35. ANS: D PTS: 1 REF: Page 472 | Table 15-6 MSC: The glossopharyngeal nerve affects control over the motor fibers that serve the pharynx (throat) and salivary glands, as well as the sensory fibers that carry impulses from the pharynx, posterior tongue (taste buds), and pressure receptors of the carotid artery. 36. ANS: C PTS: 1 REF: Page 472 | Table 15-6 MSC: The oculomotor nerve fibers emerge from the midbrain, exit from the skull, and extend to the eye. These fibers control: (1) the motor fibers to the inferior oblique, superior, inferior, and medial rectus extraocular muscles that direct the eyeball; (2) the levator muscles of the eyelid; (1) the smooth muscles of the iris and ciliary body; and (4) proprioception (sensory) to brain from the extraocular muscles. 37. ANS: A PTS: 1 REF: Page 472 | Table 15-6 MSC: The trochlear nerve fibers emerge from posterior midbrain and exit from skull to affect control over the proprioceptor and motor fibers for the superior oblique muscle of eye (extraocular muscle). 38. ANS: E PTS: 1 REF: Page 472 | Table 15-6 MSC: The abducens nerve affects control over the motor fibers to the lateral rectus muscle and the proprioceptor fibers from the same muscle to the brain, allowing the eyes to move laterally. 39. ANS: B PTS: 1 REF: Page 472 | Table 15-6 MSC: The trigeminal nerve affects control over both the motor and sensory functions to the face; conducts sensory impulses from the mouth, nose, surface of eye, and dura mater; it also contains motor fibers that stimulate the chewing muscles. 40. ANS: F PTS: 1 REF: Page 472 | Table 15-6 MSC: The hypoglossal nerve affects control over the motor fibers to the muscles of tongue and sensory impulses from the tongue to the brain. 41. ANS: H PTS: 1 REF: Page 472 | Table 15-6 MSC: The vagus nerve affects control over the fibers that carry sensory and motor impulses for the pharynx. A large part of this nerve is parasympathetic motor fibers that supply smooth muscles of the abdominal organs and is capable of receiving sensory impulses from the viscera. 42. ANS: J PTS: 1 REF: Page 472 | Table 15-6 MSC: The spinal accessory nerve affects control over the sensory and motor fibers for the sternocleidomastoid and trapezius muscles and the muscles of the soft palate, pharynx, and larynx. 43. ANS: G PTS: 0 REF: Page 472 | Table 15-6 MSC: The olfactory nerve is purely sensory and carries impulses for the sense of smell. 44. ANS: I PTS: 0 REF: Page 472 | Table 15-6 MSC: The vestibulocochlear nerve is purely sensory; the vestibular branch transmits impulses for the sense of equilibrium; the cochlear branch transmits impulses for the sense of hearing. Chapter 17: Alterations in Cognitive Systems, Cerebral Hemodynamics, and Motor Function MULTIPLE CHOICE 1. Cognitive operations cannot occur without the effective functioning of the brain’s: a. Pons c. Reticular activating system b. Medulla oblongata d. Cingulate gyrus 2. Which intracerebral disease process is capable of producing diffuse dysfunction? a. Closed head trauma with bleeding c. Neoplasm b. Subdural pus collections d. Infarct emboli 3. What is the most common infratentorial brain disease process that results in the direct destruction of the reticulating activation system (RAS)? a. Cerebrovascular disease c. Neoplasms b. Demyelinating disease d. Abscesses 4. What stimulus causes posthyperventilation apnea (PHVA)? a. Changes in PCO2 levels c. Damage to the forebrain b. Changes in PaCO2 levels d. Any arrhythmic breathing pattern 5. Posthyperventilation apnea (PHVA) ceases and rhythmic breathing is resumed when levels of arterial: a. Carbon dioxide increase c. Oxygen increase b. Carbon dioxide become normal d. Oxygen decrease 6. Cheyne-Stokes respirations are described as a: a. Sustained deep rapid but regular pattern of breathing b. Crescendo-decrescendo pattern of breathing, followed by a period of apnea c. Prolonged inspiratory period, gradually followed by a short expiratory period d. Completely irregular breathing pattern with random shallow, deep breaths and irregular pauses 7. Vomiting is associated with central nervous system (CNS) injuries that compress which of the brain’s anatomic locations? a. Vestibular nuclei in the lower brainstem b. Floor of the third ventricle c. Any area in the midbrain d. Diencephalon 8. Which midbrain dysfunction causes pupils to be pinpoint size and fixed in position? a. Diencephalon dysfunction b. Oculomotor cranial nerve dysfunction c. Dysfunction of the tectum d. Pontine dysfunction 9. What characteristic is a medical criterion of brain death? a. Akinetic mutism c. Apnea b. Coma d. Locked-in syndrome 10. A clinical manifestation caused by damage to the lower pons includes an abnormal: a. Flexion with or without extensor response of the lower extremities b. Extension response of the upper and lower extremities c. Extension response of the upper extremities and flexion response of the lower extremities d. Flaccid response in the upper and lower extremities 11. Which person is at the greatest risk for developing delirium? a. An individual with diabetes celebrating a 70th birthday b. A depressed Hispanic woman c. An individual on the second day after hip replacement d. A man diagnosed with schizophrenia 12. A sudden, explosive, disorderly discharge of cerebral neurons is termed: a. Reflex c. Epilepsy b. Seizure d. Convulsion 13. A complex partial seizure is described as: a. Alternating of tonic and clonic movements b. Impairment of both consciousness and the ability to react to exogenous stimuli c. Focal motor movement without loss of consciousness d. One seizure followed by another in less than 1 minute 14. Status epilepticus is considered a medical emergency because of the: a. Loss of consciousness b. Development of cerebral hypoxia c. Possibility of a head injury during seizures d. Decrease in brain metabolism 15. The most critical aspect in correctly diagnosing a seizure disorder and establishing its cause is: a. Computed tomographic (CT) scan c. Skull x-ray studies b. Cerebrospinal fluid analysis d. Health history 16. What type of seizure starts in the fingers and progressively spreads up the arm and extends to the leg? a. Complex-psychomotor seizure c. Generalized seizures b. Focal (partial) Jacksonian seizure d. Atonic-drop seizure 17. What area of the brain mediates the executive attention functions? a. Limbic c. Parietal b. Prefrontal d. Occipital 18. What term describes the loss of the comprehension or production of language? a. Agnosia c. Akinesia b. Aphasia d. Dysphasia 19. With receptive dysphasia (fluent), the individual is able to: a. Respond in writing, but not in speech. b. Produce verbal speech, but not comprehend language. c. Comprehend speech, but not verbally respond. d. Neither respond verbally nor comprehend speech. 20. What is the normal intracranial pressure (in mm Hg)? a. 5 to 15 c. 12 to 14 b. 7 to 20 d. 80 to 120 21. Cerebral edema is an increase in the fluid content of the brain’s: a. Ventricles c. Neurons b. Tissue d. Meninges 22. What type of cerebral edema occurs when permeability of the capillary endothelium increases after injury to the vascular structure? a. Cytotoxic c. Vasogenic b. Interstitial d. Ischemic 23. A communicating hydrocephalus is caused by an impairment of the: a. Cerebrospinal fluid flow between the ventricles b. Cerebrospinal fluid flow into the subarachnoid space c. Blood flow to the arachnoid villi d. Absorption of cerebrospinal fluid 24. Which edema is most often observed with noncommunicating hydrocephalus? a. Metabolic c. Vasogenic b. Interstitial d. Ischemic 25. Which dyskinesia involves involuntary movements of the face, trunk, and extremities? a. Paroxysmal c. Hyperkinesia b. Tardive d. Cardive 26. Antipsychotic drugs cause tardive dyskinesia by mimicking the effects of increased: a. Dopamine c. Norepinephrine b. Gamma-aminobutyric acid d. Acetylcholine 27. The existence of regular, deep, and rapid respirations after a severe closed head injury is indicative of neurologic injury to the: a. Lower midbrain c. Supratentorial b. Pontine area d. Cerebral area 28. What type of posturing exists when a person with a severe closed head injury has all four extremities in rigid extension with the forearms in hyperpronation and the legs in plantar extension? a. Decorticate c. Spastic b. Decerebrate d. Cerebellar 29. Since his cerebrovascular accident, a man has been denying his left hemiplegia. What term is used to describe this finding? a. Visual agnosia c. Amusia agnosia b. Anosognosia d. Agraphia agnosia 30. After a cerebrovascular accident, a man is unable to either feel or identify a comb with his eyes closed. This is an example of: a. Agraphia c. Anosognosia b. Tactile agnosia d. Prosopagnosia 31. Most dysphasias are associated with cerebrovascular accidents involving which artery? a. Anterior communicating c. Circle of Willis b. Posterior communicating d. Middle cerebral 32. Tactile agnosia is related to injury of which area of the brain? a. Frontotemporal c. Temporal b. Parietal d. Broca area 33. Neurofibrillary tangles characterize which neurologic disorder? a. Dementia syndrome c. Alzheimer disease b. Delirium d. Parkinson disease 34. The body compensates for a rise in intracranial pressure by first displacing the: a. Cerebrospinal fluid c. Venous blood b. Arterial blood d. Cerebral cells 35. Stage 1 intracranial hypertension is caused by the: a. Loss of autoregulation that normally maintains constant blood flow during changes in cerebral perfusion pressure b. Displacement of cerebrospinal fluid, followed by compression of the cerebral venous system c. Vasoconstriction of the cerebral arterial system with reciprocal increase in systemic blood pressure d. Compression of the medulla oblongata in the brainstem by herniation of the cerebral cortex 36. Dilated and sluggish pupils, widening pulse pressure, and bradycardia are clinical findings evident of which stage of intracranial hypertension? a. 1 c. 3 b. 2 d. 4 37. Dilation of the ipsilateral pupil, following uncal herniation, is the result of pressure on which cranial nerve (CN)? a. Optic (CN I) c. Oculomotor (CN III) b. Abducens (CN VI) d. Trochlear (CN IV) 38. Which characteristic is the most critical index of nervous system dysfunction? a. Size and reactivity of pupils c. Motor response b. Pattern of breathing d. Level of consciousness 39. Diagnostic criteria for a persistent vegetative state include: a. Absence of eye opening b. Lack of subcortical responses to pain stimuli c. Roving eye movements with visual tracking d. Return of autonomic functions such as gastrointestinal function 40. Uncal herniation occurs when: a. The hippocampal gyrus shifts from the middle fossa through the tentorial notch into the posterior fossa. b. The diencephalon shifts from the middle fossa straight downward through the tentorial notch into the posterior fossa. c. The cingulate gyrus shifts under the falx cerebri. d. A cerebellar tonsil shifts through the foramen magnum. 41. Which assessment finding marks the end of spinal shock? a. Return of blood pressure and heart rate to normal b. Gradual return of spinal reflexes c. Return of bowel and bladder function d. Evidence of diminished deep tendon reflexes and flaccid paralysis 42. Characteristics of primary motor neuron atrophy include: a. Loss of sensation in distal, proximal, or midline muscles b. Fasciculations and muscle cramps c. Flaccid paralysis with paresthesia d. Spastic paralysis with increased deep tendon reflexes 43. The weakness resulting from the segmental paresis and paralysis characteristic of anterior horn cell injury is difficult to recognize because: a. Upper motor neurons are involved. b. The injury is microscopic. c. Two or more nerve roots supply each muscle. d. The person is unable to feel the involved muscles. 44. Parkinson disease is a degenerative disorder of the brain’s: a. Hypothalamus c. Frontal lobe b. Anterior pituitary d. Basal ganglia 45. Clinical manifestations of Parkinson disease are caused by a deficit in which of the brain’s neurotransmitters? a. Gamma-aminobutyric acid c. Norepinephrine b. Dopamine d. Acetylcholine 46. Tremors at rest, rigidity, akinesia, and postural abnormalities are a result of the atrophy of neurons in the brain’s: a. Caudate that produces serotonin b. Putamen that produces gamma-aminobutyric acid c. Substantia nigra that produces dopamine d. Hypothalamus that produces acetylcholine MULTIPLE RESPONSE 47. Dementia is commonly characterized by the deterioration in which abilities? (Select all that apply.) a. Sociability b. Balance c. Memory d. Speech e. Decision making 48. The clinical manifestations of Parkinson disease include: (Select all that apply.) a. Fragmented sleep b. Drooping eyelids c. Depression d. Muscle stiffness e. Bradykinesia 49. In Parkinson disease the basal ganglia influence the hypothalamic function to produce which clinical manifestations? (Select all that apply.) a. Inappropriate diaphoresis b. Gastric retention c. Vomiting d. Diarrhea e. Urinary retention Chapter 18: Disorders of the Central and Peripheral Nervous Systems and the Neuromuscular Junction MULTIPLE CHOICE 1. Diffuse axonal injuries (DAIs) of the brain often result in: a. Reduced levels of consciousness c. Fine motor tremors b. Mild but permanent dysfunction d. Visual disturbances 2. What event is most likely to occur to the brain in a classic cerebral concussion? a. Brief period of vital sign instability b. Cerebral edema throughout the cerebral cortex c. Cerebral edema throughout the diencephalon d. Disruption of axons extending from the diencephalon and brainstem 3. Which disorder has clinical manifestations that include decreased consciousness for up to 6 hours, as well as retrograde and posttraumatic amnesia? a. Mild concussion c. Cortical contusion b. Classic concussion d. Acute subdural hematoma 4. What group is most at risk of spinal cord injury from minor trauma? a. Children c. Adults b. Adolescents d. Older adults 5. The edema of the upper cervical cord after spinal cord injury is considered life threatening because of which possible outcome? a. Hypovolemic shock from blood lost during the injury b. Breathing difficulties from an impairment to the diaphragm c. Head injury that likely occurred during the injury d. Spinal shock immediately after the injury 6. What indicates that spinal shock is terminating? a. Voluntary movement below the level of injury b. Reflex emptying of the bladder c. Paresthesia below the level of injury d. Decreased deep tendon reflexes and flaccid paralysis 7. What term is used to describe the complication that can result from a spinal cord injury above T6 that is producing paroxysmal hypertension, as well as piloerection and sweating above the spinal cord lesion? a. Craniosacral dysreflexia c. Autonomic hyperreflexia b. Parasympathetic dysreflexia d. Retrograde hyperreflexia 8. Why does a person who has a spinal cord injury experience faulty control of sweating? a. The hypothalamus is unable to regulate body heat as a result of damage to the sympathetic nervous system. b. The thalamus is unable to regulate body heat as a result of damage to the sympathetic nervous system. c. The hypothalamus is unable to regulate body heat as a result of damage to the parasympathetic nervous system. d. The thalamus is unable to regulate body heat as a result of damage to spinal nerve roots. 9. Autonomic hyperreflexia–induced bradycardia is a result of stimulation of the: a. Sympathetic nervous system to ß-adrenergic receptors to the sinoatrial node b. Carotid sinus to the vagus nerve to the sinoatrial node c. Parasympathetic nervous system to the glossopharyngeal nerve to the atrioventricular node d. Bundle branches to the -adrenergic receptors to the sinoatrial node 10. A herniation of which disk will likely result in motor and sensory changes of the lateral lower legs and soles of the feet? a. L2-L3 c. L5-S1 b. L3-L5 d. S2-S3 11. Which condition poses the highest risk for a cerebrovascular accident (CVA)? a. Insulin-resistant diabetes mellitus c. Polycythemia b. Hypertension d. Smoking 12. A right hemisphere embolic CVA has resulted in left-sided paralysis and reduced sensation of the left foot and leg. Which cerebral artery is most likely affected by the emboli? a. Middle cerebral c. Posterior cerebral b. Vertebral d. Anterior cerebral 13. Atrial fibrillation, rheumatic heart disease, and valvular prosthetics are risk factors for which type of stroke? a. Hemorrhagic c. Embolic b. Thrombotic d. Lacunar 14. Microinfarcts resulting in pure motor or pure sensory deficits are the result of which type of stroke? a. Embolic c. Lacunar b. Hemorrhagic d. Thrombotic 15. Which vascular malformation is characterized by arteries that feed directly into veins through vascular tangles of abnormal vessels? a. Cavernous angioma c. Arteriovenous angioma b. Capillary telangiectasia d. Arteriovenous malformation 16. Which clinical finding is considered a diagnostic indicator for an arteriovenous malformation (AVM)? a. Systolic bruit over the carotid artery b. Decreased level of consciousness c. Hypertension with bradycardia d. Diastolic bruit over the temporal artery 17. Which cerebral vascular hemorrhage causes meningeal irritation, photophobia, and positive Kernig and Brudzinski signs? a. Intracranial c. Epidural b. Subarachnoid d. Subdural 18. In adults, most intracranial tumors are located: a. Infratentorially c. Laterally b. Supratentiorially d. Posterolaterally 19. In children, most intracranial tumors are located: a. Infratentorially c. Laterally b. Supratentiorially d. Posterolaterally 20. The most common primary central nervous system (CNS) tumor is the: a. Microglioma c. Astrocytoma b. Neuroblastoma d. Neuroma 21. Meningiomas characteristically compress from: a. Within neural tissues c. Outside the spinal cord b. Outside spinal nerve roots d. Within the subarachnoid space 22. What is the central component of the pathogenic model of multiple sclerosis? a. Myelination of nerve fibers in the peripheral nervous system (PNS) b. Demyelination of nerve fibers in the CNS c. Development of neurofibrillary tangles in the CNS d. Inherited autosomal dominant trait with high penetrance 23. A blunt force injury to the forehead would result in a coup injury to which region of the brain? a. Frontal c. Parietal b. Temporal d. Occipital 24. A blunt force injury to the forehead would result in a contrecoup injury to which region of the brain? a. Frontal c. Parietal b. Temporal d. Occipital 25. Spinal cord injuries most likely occur in which region? a. Cervical and thoracic c. Lumbar and sacral b. Thoracic and lumbar d. Cervical and thoracic-lumbar 26. The most likely rationale for body temperature fluctuations after cervical spinal cord injury is that the person has: a. Developed bilateral pneumonia or a urinary tract infection. b. Sustain sympathetic nervous system damage resulting in disturbed thermal control. c. Sustained a head injury that damaged the hypothalamus’s ability to regulate temperature. d. Developed septicemia from posttrauma infection. 27. A man who sustained a cervical spinal cord injury 2 days ago suddenly develops severe hypertension and bradycardia. He reports severe head pain and blurred vision. The most likely explanation for these clinical manifestations is that he is: a. Experiencing acute anxiety b. Developing spinal shock c. Developing autonomic hyperreflexia d. Experiencing parasympathetic areflexia 28. The type of vascular malformation that most often results in hemorrhage is: a. Cavernous angioma c. Capillary telangiectasia b. Venous angioma d. Arteriovenous malformation 29. Atheromatous plaques are most commonly found: a. In larger veins c. At branches of arteries b. Near capillary sphincters d. On the venous sinuses 30. Multiple sclerosis is best described as a(an): a. Central nervous system demyelination, possibly from an immunogenetic virus b. Inadequate supply of acetylcholine at the neurotransmitter junction as a result of an autoimmune disorder c. Depletion of dopamine in the central nervous system as a result of a virus d. Degenerative disorder of lower and upper motor neurons caused by viral-immune factors 31. What is the most common opportunistic infection associated with acquired immunodeficiency syndrome (AIDS)? a. Non-Hodgkin lymphoma c. Toxoplasmosis b. Kaposi sarcoma d. Cytomegalovirus 32. It is true that Guillain-Barré syndrome (GBS): a. Is preceded by a viral illness. c. Results in asymmetric paralysis. b. Involves a deficit in acetylcholine. d. Is an outcome of HIV. 33. It is true that myasthenia gravis: a. Is an acute autoimmune disease. c. May result in adrenergic crisis. b. Affects the nerve roots. d. Causes muscle weakness. 34. In which disorder are acetylcholine receptor antibodies (IgG antibodies) produced against acetylcholine receptors? a. Guillain-Barré syndrome c. Myasthenia gravis b. Multiple sclerosis d. Parkinson disease 35. Multiple sclerosis and Guillain-Barré syndrome are similar in that they both: a. Result from demyelination by an immune reaction. b. Cause permanent destruction of peripheral nerves. c. Result from inadequate production of neurotransmitters. d. Block acetylcholine receptor sites at the myoneuronal junction. MULTIPLE RESPONSE 36. Which clinical manifestation is characteristic of cluster headaches? (Select all that apply.) a. Preheadache aura b. Severe unilateral tearing c. Gradual onset of a tight band around the head d. Significant unilateral, temporal pain e. Pain lasting from 30 to 120 minutes 37. What are the initial clinical manifestations immediately noted after a spinal cord injury? (Select all that apply.) a. Headache b. Bladder incontinence c. Loss of deep tendon reflexes d. Hypertension e. Flaccid paralysis MATCHING Match the terms with the corresponding descriptions. ______ A. Complication of mastoiditis ______ B. Opportunistic infection ______ C. CNS manifestation of tuberculosis ______ D. Mosquito-borne viral infection ______ E. Tick-borne bacterial infection 38. Meningitis 39. Encephalitis 40. Cryptococcus neoformans 41. Brain abscess 42. Lyme disease 38. ANS: C PTS: 1 REF: Pages 611-612 MSC: Tubercular meningitis is the most common and serious form of central nervous system (CNS) tuberculosis. 39. ANS: D PTS: 1 REF: Page 614 MSC: Encephalitis is an acute febrile illness, usually of viral origin, with nervous system involvement. Arthropod-borne (mosquito-borne) viruses and herpes simplex cause the most common encephalitides. 40. ANS: B PTS: 1 REF: Page 617 MSC: Opportunistic infections may be bacterial, fungal, protozoal, or viral in origin and produce nervous system disease. Cryptococcus neoformans is an example of such an infection. 41. ANS: A PTS: 1 REF: Page 613 MSC: Abscesses may occur in association with a contiguous spread of infection, such as the middle ear, mastoid cells, nasal cavity, and nasal sinuses. 42. ANS: E PTS: 1 REF: Page 617 MSC: Lyme disease, a tick-borne spirochete bacterial infection, is a common arthropod-borne infection in the United States. Chapter 19: Neurobiology of Schizophrenia, Mood Disorders, and Anxiety Disorders MULTIPLE CHOICE 1. Which would be considered a positive symptom of schizophrenia? a. Blunted affect c. Poverty of speech b. Auditory hallucinations d. Lack of social interaction 2. The onset of schizophrenia can be triggered by which prenatal occurrence? a. Viral infection c. Maternal smoking b. Maternal depression d. Exposure to toxic waste 3. Which neurotransmitter is reduced in people with schizophrenia? a. Dopamine c. Acetylcholine b. Gamma-aminobutyric acid d. Serotonin 4. Alterations in which part of the brain are linked to hallucinations, delusions, and thought disorders associated with schizophrenia? a. Parietal lobe c. Temporal lobe b. Limbic system d. Hypothalamus 5. Antipsychotic drugs block which neurotransmitter receptor? a. Norepinephrine c. Serotonin b. Gamma-aminobutyric acid d. Dopamine 6. What data confer the link between bipolar disorders and schizophrenia? a. Individuals with bipolar disorder who exhibit psychotic behaviors have deficits in reelin expression linked to genetic loci located on chromosome 22. b. Individuals with schizophrenia who exhibit psychotic behaviors have deficits in serotonin linked to genetic loci located on chromosome 16. c. Individuals with bipolar disorder who exhibit psychotic behaviors have deficits in gamma-aminobutyric acid (GABA) linked to genetic loci located on chromosome 20. d. Individuals with schizophrenia who exhibit psychotic behaviors have deficits in reelin expression linked to genetic loci located on chromosome 18. 7. Hypothalamic-pituitary-adrenal (HPA) system abnormalities exist in a large percentage of individuals with: a. Schizophrenia c. Mania b. Major depression d. Panic disorder 8. The common property among the three types of medications used to treat depression is that they: a. Increase neurotransmitter levels within the synapse. b. Increase neurotransmitter levels in the presynapse. c. Decrease neurotransmitter levels in the postsynapse. d. Decrease neurotransmitter levels within the synapse. 9. The link between major depression and cortisol secretion is that individuals with depression: a. Show suppression of plasma cortisol when given dexamethasone. b. Have a decreased plasma cortisol level, despite the administration of exogenous corticosteroids. c. Show that persistently elevated plasma cortisol levels can result in inflammation that is believed to trigger depression. d. Have normal plasma cortisol levels throughout the day when they take antidepressant medication as prescribed. PTS: 1 REF: Page 648 10. A decrease in receptor binding for which neurotransmitter is found in individuals with depression? a. Norepinephrine c. Dopamine b. Serotonin d. Acetylcholine 11. When treating individuals with depression, the result produced by electroconvulsive therapy (ECT) is believed to be an alteration in: a. The monoamine systems c. Norepinephrine b. Serotonin d. The limbic system 12. Which electrolyte imbalance contributes to lithium toxicity? a. Hypernatremia c. Hyperkalemia b. Hyponatremia d. Hypokalemia 13. Which neurotransmitter is inhibited in panic disorders? a. Norepinephrine c. Dopamine b. Serotonin d. Gamma-aminobutyric acid (GABA) 14. A criterion for a diagnosis of generalized anxiety disorder (GAD) is a period of excessive worrying that lasts for at least how many months? a. 3 c. 9 b. 6 d. 12 15. Individuals who eat aged cheese and avocado when taking monoamine oxidase inhibitors (MAOIs) may experience: a. Kidney damage c. Orthostatic hypotension b. Hypertensive crisis d. Weight gain 16. Electroconvulsive therapy (ECT) is used to treat depression: a. In pregnant women b. By enhancing the effect of antidepressants c. As a first-line treatment before medications d. That is unipolar 17. A notable complication of panic disorder is: a. Avolition c. Alogia b. Anhedonia d. Agoraphobia 18. Persistent symptoms of posttraumatic stress disorder (PTSD) include: a. Depression c. Nightmares b. Hypertension d. Poor nutrition 19. Hallucinations, delusions, and thought disorders occur with alterations to which part of the brain? a. Temporal lobe c. Hypothalamus b. Parietal lobe d. Cerebral cortex MULTIPLE RESPONSE 20. Significant numbers of individuals with depression have problems related to: (Select all that apply.) a. Sleep cycles b. Weight stabilization c. Eating patterns d. Thyroid function e. Cognitive skills 21. Which neurotransmitter is inhibited in generalized anxiety disorder (GAD)? (Select all that apply.) a. Acetylcholine b. Serotonin c. Dopamine d. Norepinephrine e. Epinephrine 22. What are the most common side effects of selective serotonin reuptake inhibitors (SSRIs)? (Select all that apply.) a. Orthostatic hypotension b. Dry mouth c. Sleep disturbances d. Agitation e. Nausea MATCHING Match the terms with the corresponding descriptions. ______ A. Delusions ______ B. Formal thought disorder ______ C. Anhedonia ______ D. Hallucinations ______ E. Alogia ______ F. Avolition 23. Perceptions are experienced without external stimulation of the sense organs. 24. Persistent beliefs are contrary to the educational and cultural background of the individual. 25. Fluent speech is difficult to comprehend. 26. Spontaneous speech is absent. 27. Condition is characterized by an inability to have emotional experiences. 28. Condition is characterized by a deficit in spontaneous or goal-directed activities. 23. ANS: D PTS: 1 REF: Page 644 MSC: A hallucination is a perception experienced without external stimulation of the sense organs. 24. ANS: A PTS: 1 REF: Page 646 MSC: A delusion is a persistent belief contrary to the educational and cultural background of the individual. 25. ANS: B PTS: 1 REF: Page 646 MSC: A common form of disorganized speech is formal thought disorder, which involves fluent speech that is difficult to comprehend. 26. ANS: E PTS: 1 REF: Page 646 MSC: Alogia is the absence of spontaneous speech production for the purpose of answering questions or expressing oneself. 27. ANS: C PTS: 1 REF: Page 646 MSC: In anhedonia, individuals are unable to experience emotions such as pleasure or pain; they report a sense of detachment from the environment. 28. ANS: F PTS: 1 REF: Page 646 MSC: Avolition is a deficit in spontaneous or goal-directed behavior in which an individual may sit for prolonged periods and must be prodded into completing simple daily tasks. Chapter 20: Alterations of Neurologic Function in Children MULTIPLE CHOICE 1. The neural groove closes dorsally during which week of gestational life? a. Second c. Eighth b. Fourth d. Twelfth 2. Which nutritional deficiency in a pregnant woman is associated with neural tube defect (NTD)? a. Iron c. Zinc b. Vitamin C d. Folate 3. Which defect of neural tube closure is most common? a. Anterior c. Lateral b. Posterior d. Midline 4. What is the anomaly in which the soft bony component of the skull and much of the brain is missing? a. Anencephaly c. Cranial meningocele b. Myelodysplasia d. Hydrocephaly 5. The most common cause of obstructive hydrocephalus in infants is: a. Obstructed arachnoid villi b. Stenosis of the aqueduct of Sylvius c. Excessive production of cerebrospinal fluid d. Impaired cerebrospinal fluid circulation in the subarachnoid space 6. What is the term for a herniation or protrusion of brain and meninges through a defect in the skull? a. Encephalocele c. Arachnoidocele b. Meningocele d. Cephacephalocele 7. What is the result of a Chiari type II malformation associated with a myelomeningocele? a. Upward displacement of the cerebellum into the diencephalon b. Motor and sensory lesions below the level of the myelomeningocele c. Downward displacement of the cerebellum, brainstem, and fourth ventricle d. Generalized cerebral edema and hydrocephalus 8. Prompt surgical repair of a myelomeningocele is critical to best prevent: a. Infection c. Mental retardation b. Paralysis d. Additional nervous system damage 9. Which body system is the largest site for human immunodeficiency virus (HIV) infection in infants and children? a. Central nervous system c. Integumentary system b. Gastrointestinal system d. Musculoskeletal system 10. An infant diagnosed with hydrocephalus is observed to demonstrate: a. Shrunken ventricles b. Bulging fontanels c. Retarded head growth d. Decreased production of cerebrospinal fluid 11. Gait disturbances and instability are characteristic of which form of cerebral palsy? a. Spastic c. Ataxic b. Dyskinetic d. Biochemical 12. Children with phenylketonuria (PKU) are unable to synthesize: a. Essential amino acid, phenylalanine, to tyrosine b. Renin, erythropoietin, and antidiuretic hormone c. Aldosterone, cortisol, and androgens d. Neurotransmitters gamma-aminobutyric acid (GABA) and acetylcholine 13. Benign febrile seizures are characterized by: a. A temperature lower than 39° C b. Respiratory or ear infections c. Onset after the fifth year of life d. Episodes lasting 30 minutes or longer 14. What is the most common general symptom of a localized childhood brain tumor? a. Poor bonding b. Increased intracranial pressure c. Delayed extinction of newborn reflexes d. Failure to thrive 15. The tonic neck reflex observed in a newborn should no longer be obtainable by: a. 2 years c. 10 months b. 1 year d. 5 months 16. What term is used to describe a hernial protrusion of a saclike cyst that contains meninges, spinal fluid, and a portion of the spinal cord through a defect in a posterior arch of a vertebra? a. Encephalocele c. Spina bifida occulta b. Meningocele d. Myelomeningocele 17. What test is performed on amniotic fluid and maternal blood to test for neural tube defect? a. Total protein c. -fetoprotein b. Culture d. C-reactive protein 18. The clinical manifestations of dyskinetic cerebral palsy include: a. Increased muscle tone and prolonged primitive reflexes b. Exaggerated deep tendon reflexes, clonus, and rigidity of extremities c. Scoliosis, contractures, and stiffness of trunk muscles d. Jerky uncontrolled and abrupt fine musculoskeletal movements MULTIPLE RESPONSE 19. Which musculoskeletal deformities are associated with myelomeningocele? (Select all that apply.) a. Extra digits on feet b. Clubfoot c. Dislocation of the hips d. Scoliosis e. Kyphosis 20. True microcephaly can be caused by: (Select all that apply.) a. Autosomal gene alterations b. Prenatal physical abuse of the mother c. X-linked gene alterations d. Toxic-induced chromosomal defects e. Maternal anorexia 21. Which statements regarding the term myelodysplasia are true? (Select all that apply.) a. Myelodysplasia is used to define a defect in the formation of the spinal cord. b. It can be used to refer to brain anomalies involving missing brain tissue. c. Myelodysplasia correctly includes encephaloceles. d. It is used to describe a herniation of brain and meninges through a defect in the skull. e. Myelodysplasia can be used to refer to a form of spina bifida. MATCHING Match the tumor name with its site of development. ______ A. Medulloblastoma ______ B. Ependymoma ______ C. Cerebellar astrocytoma ______ D. Craniopharyngioma ______ E. Neuroblastoma 22. Originates in the neural crest that normally forms the sympathetic ganglia and adrenal medulla. 23. Develops in the fourth ventricle. 24. Develops in the vermis of the cerebellum and may extend to the fourth ventricle. 25. Originates from the pituitary or hypothalamus. 26. Causes unilateral symptoms such as nystagmus. 22. ANS: E PTS: 1 REF: Page 684 MSC: A neuroblastoma is an embryonal aggressive tumor that originates in the neural crest cells that normally give rise to the sympathetic nervous system (sympathetic ganglia and the adrenal medulla). 23. ANS: B PTS: 1 REF: Page 683 MSC: The ependymoma develops in the fourth ventricle and arises from the ependymal cells that line the ventricular system. 24. ANS: A PTS: 1 REF: Page 683 MSC: A medulloblastoma is an embryonal tumor and the most common childhood malignant tumor. It occurs as an invasive tumor that develops in the vermis of the cerebellum and may extend into the fourth ventricle. 25. ANS: D PTS: 1 REF: Page 683 MSC: The area of the sella turcica, the structure containing the pituitary gland, is the site of several childhood brain tumors, including craniopharyngioma (the most common). These tumors may originate from the pituitary gland or the hypothalamus. 26. ANS: C PTS: 1 REF: Page 683 MSC: Cerebellar astrocytomas are located on the surface of the right or left cerebellar hemisphere and cause unilateral symptoms (occurring on the same side of the tumor), such as head tilt, limb ataxia, and nystagmus when the eyes are turned toward the tumor. [Show More]
Last updated: 1 year ago
Preview 1 out of 45 pages
Instant download
Buy this document to get the full access instantly
Instant Download Access after purchase
Add to cartInstant download
Reviews( 0 )
Document information
Connected school, study & course
About the document
Uploaded On
Jul 14, 2020
Number of pages
45
Written in
Additional information
This document has been written for:
Uploaded
Jul 14, 2020
Downloads
0
Views
45