*NURSING > CASE STUDY > NR 504 Week 2 Paper| NR 504 Week 2: Role of Ethics Within Leadership (All)
NR 504 Week 2 Paper| NR 504 Week 2: Role of Ethics Within Leadership
Document Content and Description Below
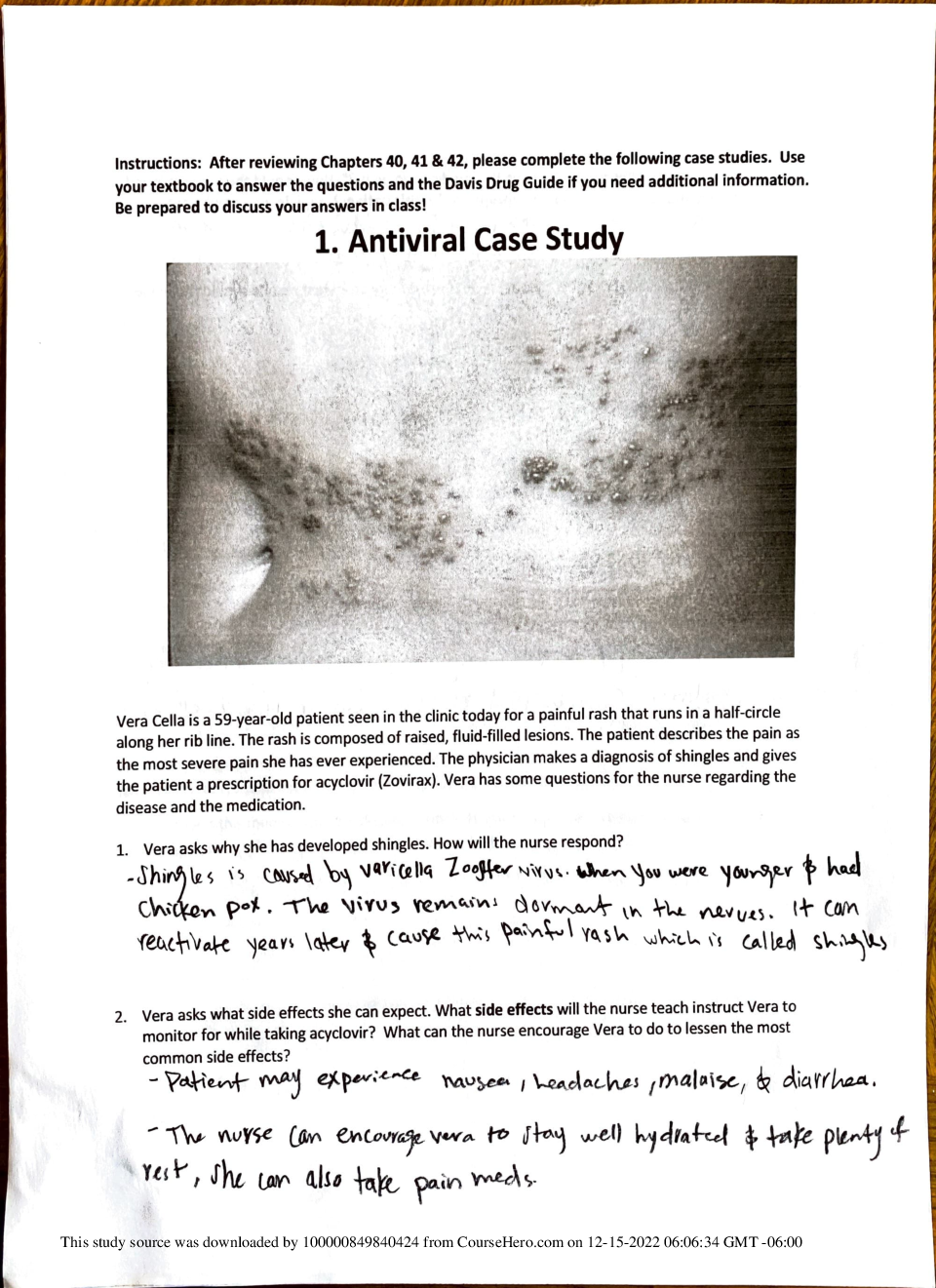
Week 2: Role of Ethics Within Leadership Chamberlain College of Nursing NR-504 Leadership and Nursing Practice: Role Development The Role of Ethics Within Leadership According to the Am... erican Nurses Association Code of Ethics (2015), the difference between morals and ethics is a matter of science. While morality commonly refers to an individual’s personal character, beliefs, values and conduct within a community, ethics is the formal study of morality and is considered a branch of philosophy or theology as a matter of theory. (ANA, 2015). In nursing, there are several ethical principles that guide nursing practice, including autonomy, beneficence, fidelity, justice, nonmaleficence, paternalism and respect. While there are a number of ethical theories that are applicable to nursing, Cammie Derr (2012) noted that there are two types of leadership styles that involve implementation of these ethical theories: transformational leadership and transactional leadership. In her article Ethics and Leadership, Derr set forth the simple principle that ethical leaders promote ethical employees. (Derr, 2012). This paper will identify how two of the ethical principles of nursing, specifically justice and autonomy, directly affect and can be applied to leadership in the field of nursing. Explanation and Application of Ethical Principles to Leadership The notion of justice as applied to nursing ethics simply means that all individuals are equally entitled to care. The ANA notes that health is considered by the nursing profession to be a “fundamental universal human right.” (ANA, 2015, p. 47). Principles of justice in the healthcare industry note that individuals have equal rights both when seeking healthcare and in participating in healthcare decisions. (Bhanji, 2013). The principle of autonomy in nursing dovetails with the principle of justice, describing the notion that nurses have the right to apply their professional knowledge and exercise professional judgment in the performance of their duties, and presupposes the concepts of knowledge and competence as well as an ability to engage in decision-making. (Mannella and Pilgrim, 2017). Just as it is necessary that nurses have autonomy in the performance of their duties, they must also recognize a patient’s autonomy and respect their healthcare decisions that are based upon accurate, complete and truthful information. (Bhanji, 2013). It is important for nurse leaders to promote these and other ethical principles among their staff. According to Derr, “ethical leadership is a style that strives to motivate ethical behavior in employees by the display of the thoughts, values, attitudes and good behavior of the leaders.” (Derr, 2012, p. 67). In their article Nursing Leadership: Ethical Aspects, Mennella and Smith noted that observing these ethical and moral principles can affect outcomes as the healthcare industry moves toward the notion of patient-directed and centered care. (Mannella & Smith, 2016). A good nurse leader will therefore exhibit the ethical principles of justice and autonomy in their own practice and, according to Derr, employees will likewise follow these principles in an effort to emulate their leaders. A nurse leader who consistently provides competent, fair and equal treatment to all patients regardless of race, religion or socioeconomic status will set the standard for their staff in that regard. Likewise, a nurse leader who makes it their practice to exercise their professional judgment in treating patients, based upon honest, complete and accurate information so that the patient can actively be involved in decisions about care, and who respects the decisions that patients make based upon that information, will be the example that staff should follow. Application of Ethical Principles to Leadership Issues Present-day healthcare is often affected by factors that are completely outside the control of medical professionals. According to the Henry J. Kaiser Foundation, uninsured individuals are not as likely to receive preventative care and medical services as those who are insured. (Kaiser, 2017). Access to healthcare insurance is not the only factor affecting disparities in care, though. According to McMorrow, Kenney and Goin (2014), “differences in insurance coverage explain 25% to 40% of the disparities in preventive service use by income, but education, age, and health status are also important drivers.” (McMorrow, et. al, 2014, p. 2392). By insisting on justice within their facilities, nurse leaders and other healthcare professionals can offer fair and impartial healthcare to all patients, regardless of their ability to pay for services provided. Just as patients may be treated differently based upon factors over which they have no control, so to the autonomy of various nursing professionals may be perceived differently depending upon factors that are outside the scope of their control. Ethical notions of autonomy are ideals to work toward, but reality is much different, as Mannella and Pilgrim (2016) noted, professional nurse autonomy is affected by factors such as education and social hierarchy in the workplace. (Mannella & Pilgrim, 2016). They warn that “a lack of professional autonomy can lead to physical and psychological distress. A 2014 study focused on psychiatric nurses found that lack of professional autonomy is associated with emotional exhaustion, depersonalization, and job ‘burnout’” (Mannella & Pilgrim, 2016, p. 1). Nurse leaders should recognize the importance of autonomy to a healthy workplace and to the improvement of patient outcomes, and exemplify it, leading by example to the rest of the staff. Application of Ethical Principles to Personal Leadership. As an employee of the Veterans Administration (VA), I am in a unique situation as far as the ethical principle of justice is concerned. The Veterans Administration is charged with the care of Veterans and, through the caregiver support program, their families. Therefore, we do not care for civilians of any kind. The principle of justice as applied to the Veterans Administration comes into play not with socioeconomic status, race or religion, but with service record. Not all of our Veterans are decorated war Veterans, nor did they have to fight in a combat theater. Indeed, any Veteran who received any discharge other than a dishonorable discharge will receive treatment at our facility. This has caused and unfortunately will continue to cause some stress among nursing and medical staff in general, because many of them are Veterans themselves. From time to time, employees question under their breath why they must provide care for someone who was in the military for a period of time less than a standard enlistment. Justice, in the case of the VA, dictates that length of service does not determine priority of care. As a nurse leader, it is important to constantly reinforce this principle so that those Veterans who are entitled to care receive that care from our staff, regardless of their service tenure, rank or decorations. Equally important is to ensure that that staff treat all Veterans equally regardless of whether the Veteran was drafted into service or chose to serve. In my practice, I treat all Veterans with respect and provide the best of care. It is important as a nurse leader to remind staff that seeing a patient and not a length of service is the best approach when providing care. I work diligently to keep the work place a place where employees want to come every day and want to give their all every day. I will continue to reinforce the fact that every Veteran that comes to us is just important as the one who just left. I will also be available for dialogue when my staff feels or acts contrary to this principle. Finally, I will remain an active listener to their concerns, but also remind them of our mission moving forward. The principle of autonomy is also important within the VA system. Allowing the nurses to not only have an opinion, but also to play an active role in caring for their patients independently without micro management will be another aspect of my leadership. I recognize that completing nursing school and passing the boards is no easy feat, and given the level of education and experience of staff, I as a leader must trust the judgment of the nursing staff. I will use horizontal communication to create a team approach when there is need. I will continue to lead by example, ethically and clinically showing the way while allowing for individual independent care within the guidelines of our facility. I will remain a part of the team helping where needed with the intention of exhibiting a united front with my staff. Leading by example while respecting the autonomy of individual nursing staff will promote a more positive work environment for staff and increasingly positive outcomes for our patients. Conclusion According to Mannella and Smith (2016), “ethical nursing leadership involves incorporating moral decision making in professional nursing practice in order to create a culture that promotes the values of individuals, groups, healthcare organizations, and society” (Mannella & Smith, 2016, p. 1). By promoting the ethical principles of justice and autonomy in a healthcare setting, a nurse leader can help to improve workplace satisfaction and positive patient outcomes. Nurses should be encouraged to become actively involved in decision making, and their autonomy should be respected by leaders. Acknowledging the autonomy of nursing professionals through the use of transformational leadership will foster a sense of team, while encouraging independent work and development. Patients must be treated equally and fairly with respect to care, and nurses and other medical personnel should respect their personal autonomy with regard to healthcare decisions. Ethical leadership is vital, because it can lead to staff satisfaction and enhance patient outcomes. (Mennella & Smith, 2016). References American Nurses Association, Inc. (2015, January). Code of Ethics for Nurses: With Interpretive Statements. Silver Spring, MD. Retrieved from: http://nursingworld.org/DocumentVault/Ethics-1/Code-of-Ethics-for-Nurses.html ANA Center for Ethics and Human Rights (2015, June). ANA position statement on privacy and confidentiality. American Nurses Association. Silver Spring, MD. Retrieved from: http://www.nursingworld.org/DocumentVault/Position-Statements/Ethics-and- Human-Rights/Position-Statement-Privacy-and-Confidentiality.pdf ANA Center for Ethics and Human Rights (2015, June). ANA position statement on risk and responsibility in providing nursing care. American Nurses Association. Silver Spring, MD. Retrieved from: http://www.nursingworld.org/DocumentVault/Position- Statements/Ethics-and-Human-Rights/RiskandResponsibility.pdf ANA Center for Ethics and Human Rights (2016). ANA position statement on the nurse’s role in ethics and human rights: Protecting and promoting individual worth, dignity and human rights in practice settings. American Nurses Association. Silver Spring, MD. Retrieved from: http://www.nursingworld.org/MainMenuCategories/EthicsStandards/Resources/E thics-Position-Statements/NursesRole-EthicsHumanRights-PositionStatement.pdf Auletto, K.T., & Miller, A.J. (2017) Developing more ethical leaders. Techniques: Connecting Education & Careers, 92(4), 16. Bhanji, S.M. (2013). Health care ethics. Journal of Clinical Research Bioethics, 2013, 4:1. DOI: 10.4172/2155-9627.1000142. Retrieved from: https://www.omicsonline.org/health-care-ethics-2155-9627.1000142.pdf Ciulla, J. B. (2014) Ethics: The Heart of Leadership. ABC-CLIO, LLC; Praeger, Santa Barbara. Retrieved from: https://books.google.com/books?hl=en&lr=&id=mw- 9BAAAQBAJ&oi=fnd&pg=PP1&dq=leadership+ethics+nursing&ots=gXLaS1llf2&sig= jULEPTy_k20Ixf7B1gsTxoXiIgs#v=onepage&q=leadership%20ethics %20nursing&f=false Derr, C.L. (2012). Ethics and leadership. Journal of Leadership, Accountability and Ethics, vol. 9(6) 2012. Retrieved from: http://www.na-businesspress.com/jlae/derrcl_web9_6_.pdf Henry J. Kaiser Foundation. (2017, Sept. 19). Key facts about the underinsured population. Kaiser Family Foundation. Retrieved from: https://www.kff.org/uninsured/fact- sheet/key-facts-about-the-uninsured-population/ McMorrow, S., Kenney, G.M., & Goin, D. (2014). Determinants of Receipt of Recommended Preventative Services: Implications for the Affordable Care Act. American Journal of Public Health, 104(12), 2392-2399. Mannella, H.A., & Pilgrim, J.M. (2016, December 2). Professional Nurse Autonomy. CINAHL Nursing Guide. Mennella, H.A., & Smith, N.C. (2016, October 7). Nursing leadership: Ethical aspects. CINAHL Nursing Guide. [Show More]
Last updated: 1 year ago
Preview 1 out of 9 pages
Buy this document to get the full access instantly
Instant Download Access after purchase
Add to cartInstant download
We Accept:

Reviews( 0 )
$7.50
Document information
Connected school, study & course
About the document
Uploaded On
Jun 26, 2021
Number of pages
9
Written in
Additional information
This document has been written for:
Uploaded
Jun 26, 2021
Downloads
0
Views
52
.png)