*NURSING > QUESTIONS and ANSWERS > Maternal Newborn ATI (GRADED A+) Study Guide | Download To Score An A (All)
Maternal Newborn ATI (GRADED A+) Study Guide | Download To Score An A
Document Content and Description Below
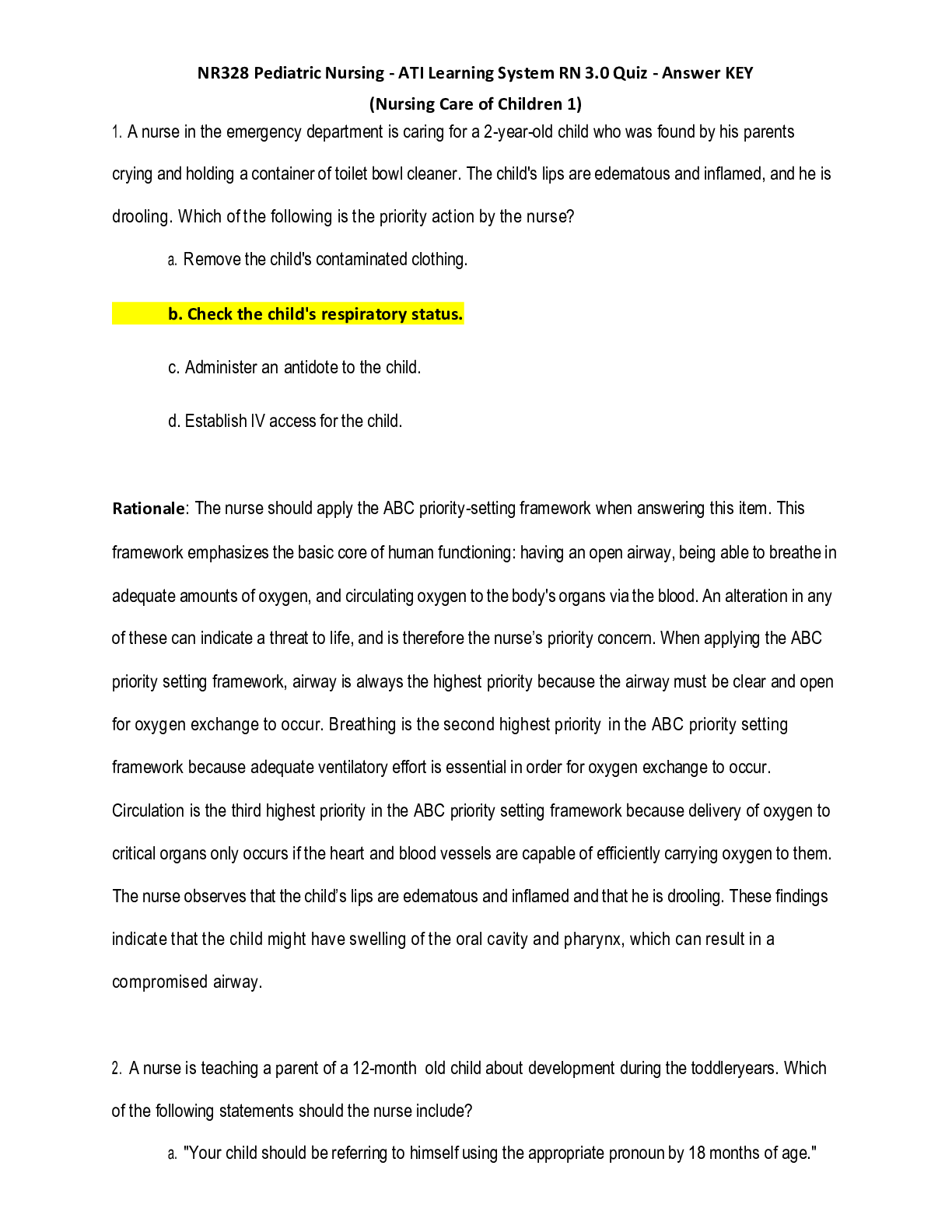
Maternal Newborn ATI A nurse on the postpartum unit is caring for a client following a cesarean birth. Which of the following assessments is the nurse’s priority? **Amount of lochia** - When usin... g the airway, breathing, circulation approach to client care, the nurse should place the priority in the immediate postpartum period on assessing the amount of postpartum lochia. The greatest risk to the client is bleeding and postpartum hemorrhage. A nurse is caring for a client who is in labor and whose fetus is in the right occiput posterior position. The client is dilated to 8 cm and reports back pain. Which of the following actions should the nurse take? **Apply sacral counterpressure** - Sacral counterpressure assists in relieving back labor pain related to fetal posterior position. A nurse is demonstrating to a client how to bathe her newborn. In which order should the nurse perform the following actions? **Wipe the newborn’s eyes from the inner canthus outward. Wash the newborn’s neck by lifting the newborn’s chin. Cleanse the skin around the newborn’s umbilical cord stump. Wash the newborn’s legs and feet. Clean the newborn’s diaper area.** - Use a head to toe, clean to dirty approach when washing a newborn. A nurse is caring for a client and her partner who have experienced a fetal death. Which of the following actions should the nurse take? **Take photos of the newborn to give to the parents.** - The nurse should create a memory box that includes mementos of the newborn (ex: photos, the newborn’s ID bands, the newborn’s hat, & the newborn’s blanket). A nurse is caring for a client who is at 36 weeks of gestation and has a positive contraction stress test. The nurse should plan to prepare the client for which of the following diagnostic tests? **Biophysical profile** - A positive contraction stress test indicates that further evaluation of the fetus is necessary (baby’s heart slowed or showed abnormality during contraction). A biophysical profile will provide further evaluation with real-time ultrasound. A nurse is reviewing the medical record of a client who is postpartum and has preeclampsia. Which of the following laboratory results should the nurse report to the provider? **Platelets 50,000/mm3** - A platelet count of 50,000/mm3 is below the expected reference range, which can indicate disseminated intravascular coagulation. The nurse should report this result to the provider. A nurse is assessing a newborn who was born at 26 weeks of gestation using the New Ballard Score. Which of the following findings should the nurse expect? **Minimal arm recoil** - The nurse should expect a newborn who was born at 26 weeks gestation to have decreased muscular tone, or minimal arm recoil. A nurse is assessing a newborn following circumcision. Which of the following findings should the nurse identify as an indication that the newborn is experiencing pain? **Chin quivering** - Behavioral responses to a newborn’s pain include facial expressions (ex: chin quivering, grimacing, & furrowing of the brow). A nurse is assessing the newborn of a client who took a selective serotonin reuptake inhibitor (SSRI) during pregnancy. Which of the following manifestations should the nurse identify as an indication of withdrawal from an SSRI? **Vomiting** - Expected clinical manifestations associated with fetal exposure to SSRIs include irritability, agitation, tremors, diarrhea, & vomiting. These usually last 2 days. A nurse is developing a plan of care for a newborn who is to undergo phototherapy for hyperbilirubinemia. Which of the following actions should the nurse include in the plan? **Remove all clothing from the newborn except the diaper.** - The nurse should remove all of the newborn’s clothing except the diaper while under phototherapy. Maximum skin exposure to the ultraviolet light is needed to break down the excess bilirubin. A nurse is creating a plan of care for a client who is postpartum and adheres to traditional Hispanic cultural beliefs. Which of the following cultural practices should the nurse include in the plan of care? **Protect the client’s head and feet from cold air.** - Protecting the client’s head and feet from cold air should be included in the plan of care because this is a traditional Hispanic practice during the postpartum period. Hispanic practices also include delaying bathing for 14 days, bed rest for 3 days, and drinking warm beverages following delivery. A nurse is caring for a client who is at 38 weeks of gestation. Which of the following actions should the nurse take prior to applying an external transducer for fetal monitoring? **Perform Leopold maneuvers.** - The nurse should perform Leopold maneuvers to assess the position of the fetus to best determine the optimal placement for the external fetal monitoring transducer. A nurse is caring for a client who is in active labor and has had no cervical change in the last 4 hours. Which of the following statements should the nurse make? **”Your provider will insert an intrauterine pressure catheter to monitor the strength of your contractions.”** - Insertion of an intrauterine pressure catheter is necessary to determine uterine contraction intensity, which will identify whether or not the contractions are adequate for the progression of labor. A nurse on a postpartum unit is caring for a client who is experiencing hypovolemic shock. After notifying the provider, which of the following actions should the nurse take next? **Massage the client’s fundus.** - The greatest risk to the client is hemorrhage. Therefore, the next action the nurse should take is to massage the client’s fundus to expel clots and promote contractions. A nurse is reviewing the medical record of a client who is one day postpartum. The client had a vaginal birth with a fourth-degree perineal laceration. The nurse should contact the provider regarding which of the following prescriptions? **Bisacodyl rectal suppository daily as needed for constipation** - The nurse should not administer a rectal suppository or enema to a client who has a fourth-degree perineal laceration. These can cause separation of the suture line, bleeding, or infection. A nurse is caring for a client who is at 26 weeks gestation and has epilepsy. The nurse enters the room and observes the client having a seizure. After turning the client’s head to one side, which of the following actions should the nurse take immediately after the seizure? **Administer oxygen via a nonrebreather mask.** - When using the airway, breathing, and circulation approach to client care, the nurse should place the priority on administering oxygen to the client via a nonrebreather mask to ensure adequate oxygenation to mother and fetus. A nurse in a prenatal clinic is caring for a client who reports that her menstrual period is 2 weeks late. The client appears anxious and asks the nurse if she is pregnant. Which of the following responses should the nurse make? **”You can miss your period for several other reasons. Describe your typical menstrual cycle.”** - Amenorrhea is a presumptive sign of pregnancy, not a positive sign. Therefore, the nurse should explore the client’s menstrual cycle to determine other necessary interventions. A nurse is providing discharge teaching to a client who is postpartum and was taking insulin for gestational diabetes mellitus. Which of the following instructions should the nurse include in the teaching? **”You should get a 2-hour oral glucose tolerance test in 6-12 weeks.”** - The nurse should instruct the client to get 2-hour oral glucose tolerance test 6-12 weeks postpartum and every 3 years to screen for type 2 diabetes. The nurse should instruct the client that blood glucose levels return to the expected reference range after childbirth. Therefore, the client does not need to monitor her blood glucose levels or continue the insulin at home. A nurse on an antepartum unit is caring for 4 clients. Which of the following clients should the nurse identify as the priority? **A client who is at 34 weeks gestation and reports epigastric pain** - Epigastric pain is a clinical manifestation of preeclampsia and indicates hepatic involvement, which is an urgent finding. Therefore, the nurse should identify this client as the priority. A nurse is preparing to administer oxytocin to a client who is postpartum. Which of the following findings is an indication for the administration of the medication? **Flaccid uterus and excessive vaginal bleeding** - Oxytocin increases the contractility of the uterus which decreases vaginal bleeding and promotes involution. A nurse is caring for a full-term newborn immediately following birth. Which of the following actions should the nurse take first? **Dry the newborn.** - When using the urgent vs. nonurgent approach to client care, the nurse should determine that the greatest risk to the newborn is cold stress. Therefore, the first action the nurse should take immediately after delivery is to dry the newborn. A nurse is performing a physical assessment of a newborn. Which of the following clinical findings should the nurse expect? **Heart rate of 154/min, respiratory rate of 58/min, and weight of 2.6kg** - The expected reference range for a newborn’s heart rate is 110-160/min. A healthy newborn’s temperature ranges between 36.5-37.5C (97.7-99.5F). The expected reference range for a newborn’s respiratory rate is 30-60/min. A newborn’s length should be between 45-55cm (17.7-21.7in) and weight between 2.5-4kg (5.5-8.8lb). A nurse in an Antepartal clinic is providing care for a client who is at 26 weeks gestation. Upon reviewing the client’s medical record, which of the following findings should the nurse report to the provider? **Fundal height measurement of 30cm** - A fundal height measurement of 30 should be reported to the provider. Fundal height should be measured in centimeters and should equal the number of gestational weeks +/- 2 weeks from 18-32 weeks gestation. Therefore, a fundal height of 30 at 26 weeks is greater than expected. 1-hour glucose tolerance test results should be less than 130-140mg/dL. Hematocrit should be greater than 33%, and FHR should be between 110-160/min. A nurse is performing a routine assessment on a client who is at 18 weeks gestation. Which of the following findings should the nurse expect? **FHR of 152/min** - The expected range of FHR is 110-160/min with rates at the higher end of range early in the pregnancy (<20 weeks). Deep tendon reflexes are an indication of the balance between the cerebral cortex and spinal cord. The nurse should expect the client’s deep tendon reflexes to be 2+. A deep tendon reflex of 4+ indicates hyperreflexia. The normal range for urine protein is less than 1+. A nurse is teaching a client who is Rh negative about Rh0(D) immune globulin. Which of the following statements by the client indicates an understanding of the teaching? **”I will need this medication if I have an amniocentesis.”** - Rh0(D) immune globulin is given to clients who are Rh negative following an amniocentesis because of the potential of fetal RBCs entering the maternal circulation. Rh0(D) immune globulin is administered at 28 weeks gestation to mothers who are Rh-negative and following the birth of a newborn who is Rh- positive. A nurse is caring for a client who is anemic at 32 weeks gestation and is in preterm labor. The provider prescribed betamethasone 12mg IM. Which of the following outcomes should the nurse expect? **A reduction in respiratory distress in the newborn** - Betamethasone is a glucocorticoid that is given to stimulate fetal lung maturity and prevent respiratory distress. A nurse is teaching a client who is at 8 weeks gestation about exercise. Which of the following instructions should the nurse include in the teaching? **”You should exercise for 30 minutes each day.”** - The nurse should instruct the client to engage in 30 minutes of moderate exercise every day to improve muscle tone throughout her pregnancy. The client should also take her pulse every 10-15 minutes during exercise, decrease weight-bearing exercises as the pregnancy progresses, and rest in a lateral position for 10 minutes following exercise. A nurse is assessing a newborn 12 hours after birth. Which of the following manifestations should the nurse report to the provider? **Jaundice** - Jaundice occurring within the first 24 hours of birth is associated with ABO incompatibility, hemolysis, or Rh-isoimmunization. Acrocyanosis is a bluish discoloration of the hands and feet and is expected in a newborn 12 hours after birth. Transient strabismus is a normal variation in the newborn’s eyes that can persist until 4 months of age. Caput succedaneum is a benign edematous area of the scalp that is commonly found on the occiput. A nurse is planning care for a client who is to undergo a nonstress test. Which of the following actions should the nurse include in the plan of care? **Instruct the client to press the provided button each time fetal movement is detected.** - Fetal movement may not be evident on the fetal monitor and tracing. Instructing the client to press the button when she detects fetal movement will ensure that the fetal movement is noted. Massaging the abdomen does not stimulate fetal movement. The client should be placed in a semi-Fowler’s or sitting position and tilted to the right or left to promote uterine perfusion and prevent supine hypotension. There is no indication for the client to be NPO, and sometimes clients are encouraged to drink liquids to promote adequate hydration. A nurse is teaching a client who is at 35 weeks gestation about clinical manifestations of potential pregnancy complications to report to the provider. Which of the following manifestations should the nurse include? **Headache that is unrelieved by analgesia** - A headache that is unrelieved by analgesia may indicate preeclampsia and should be reported. A nurse is planning care for a client who is in labor and is to have an amniotomy. Which of the following assessments should the nurse identify as the priority? **Temperature** - The greatest risk for a client following amniotomy is infection. Temperature is the greatest indication of infection and should be the priority assessment. A nurse is teaching a newly licensed nurse about collecting a specimen for the universal newborn screening. Which of the following statements should the nurse include in the teaching? **”Ensure that the newborn has been receiving feedings for 24 hours prior to obtaining the specimen.”** - The nurse should ensure that the newborn has been receiving regular feedings for at least 24 hours prior to testing. The universal newborn screening is mandated by law for all newborns. Therefore, informed consent is not needed or required. The test requires the nurse to collect a capillary blood sample via heel stick. Premature newborns have a delayed development of liver enzymes which can cause a false positive result. A client who is at 34 weeks gestation asks the nurse how she will know when she is in labor and should go to the hospital. Which of the following responses should the nurse make? **”You will notice blood-tinged discharge from your vagina.”** - The nurse should inform the client that a sign of true labor is the bloody show, which is a blood-tinged discharge from the vagina that occurs when the cervix begins to efface and dilate. This is an indication that the client should go to the hospital. A nurse is caring for a client who is at 35 weeks gestation and is undergoing a nonstress test that reveals a variable deceleration in the FHR. Which of the following actions should the nurse take? **Have the client change positions.** - Having the client change positions is the first intervention for a variable deceleration to relieve umbilical cord compression. A staff nurse on an obstetric unit is caring for a client who is scheduled for an induced abortion. The staff nurse informs the nurse manager that she has a moral issue with the client’s decision. Which of the following actions should the nurse manager take? **Reassign the client to another staff nurse.** - The nurse manager should take into account the staff nurse’s moral beliefs and recognize that she also has rights and responsibilities concerning the care of a client who is undergoing an induced abortion. A nurse in the antepartum clinic is assessing a client’s adaptation to pregnancy. The client states that she is, “happy one minute and crying the next.” The nurse should interpret the client’s statement as an indication of which of the following? **Emotional lability** - The nurse should recognize and interpret the client’s statement as an indication of emotional lability. Many women experience rapid and unpredictable changes in mood during pregnancy. Intense hormonal changes may be responsible for mood changes that occur during pregnancy. Tears and anger alternate with feelings of joy or cheerfulness for little or no reason. The focusing phase is the third phase of the father’s emotional response to the pregnancy. It is characterized by his active involvement in the pregnancy and his relationship with the child. Cognitive restructuring is accepting the idea of pregnancy and assimilating it into the woman’s life. The degree of acceptance is shown in the mother’s emotional responses. Couvade syndrome is pregnancy-life manifestations experienced by the expectant father. Manifestations may include nausea, weight gain, and other physical manifestations of pregnancy. A nurse is teaching a client who is at 10 weeks gestation about nutrition during pregnancy. Which of the following statements by the client indicates an understanding of the teaching? **”I should take 600 micrograms of folic acid each day.”** - A client who is pregnant should increase her folic acid intake to 600mcg daily. Folic acid assists with preventing neural tube birth defects. A client who is pregnant should also increase her protein intake to 71g daily, water intake to 3L daily, increase her caloric intake by 340 during the second trimester, and by 452 during the third trimester. A nurse is caring for a prenatal client who has parvovirus B19 (fifth disease). Which of the following actions should the nurse take? **Schedule an ultrasound examination.** - The nurse should schedule serial ultrasound examinations to monitor the fetus during the pregnancy to detect the possible development of fetal hydrops. A charge nurse on a labor and delivery unit is teaching a newly licensed nurse how to perform Leopold maneuvers. Which of the following images indicates the first step of Leopold maneuvers? ** ** - The first step of Leopold’s maneuvers is to palpate the abdomen with the palms to determine which fetal part is in the uterine fundus. A nurse is caring for a client who is pregnant and is at the end of her first trimester. The nurse should place the Doppler ultrasound stethoscope in which of the following locations to begin assessing for the fetal heart tones (FHT)? **Just above the symphysis pubis** - At the end of the first trimester of pregnancy, the client’s uterus is approximately the size of a grapefruit and is positioned low in the pelvis slightly above the symphysis pubis. Therefore, the nurse should assess for FHTs just above that. A nurse is preparing to administer hepatitis B immune globulin to a newborn. The prescription states, “Administer 5 mcg IM once today.” Available is a 5 mL vial with 10 mcg/mL. How many mL should the nurse administer (rounded to the nearest tenth)? **0.5 mL** A nurse is assessing a client who is in labor and notes early decelerations on the fetal monitor. Which of the following findings should the nurse identify as a possible cause of the early decelerations? **Fetal head compression** - The nurse should identify that early decelerations are an expected fetal pattern caused by fetal head compression due to uterine contractions, fundal pressure, and vaginal examinations. A nurse is providing teaching about family planning to a client who has a new prescription for a diaphragm. Which of the following statements should the nurse include in the teaching? **”You should leave the diaphragm in place for at least 6 hours after intercourse.”** - The client should be advised that the diaphragm must remain in place for at least 6 hours after intercourse to provide the most protection agains pregnancy. The diaphragm should be replaced every 2 years. The client should have an empty bladder prior to insertion and avoid using oil-based products because they weaken the rubber of the diaphragm. A nurse is caring for a client who is 36 weeks gestation and has a prescription for an amniocentesis. For which of the following reasons should the nurse prepare the client for an ultrasound? **To locate a pocket of fluid** - Locating a pocket of fluid using the ultrasound prior to the amniocentesis reduces the risk of injury to the fetus. A nurse is caring for a client who becomes unresponsive upon delivery of the placenta. Which of the following actions should the nurse take first? **Determine respiratory function.** - The priority using the airway, breathing, circulation approach is to determine the respiratory function and the need for cardiopulmonary resuscitation. A nurse is teaching a client who is pregnant about managing nausea and vomiting. Which of the following instructions should the nurse include in the teaching? **”Eat high carbohydrate foods.”** - The nurse should instruct the client to eat high carbohydrate foods such as toast, potatoes, and rice to decrease nausea and vomiting. The client should also be instructed to avoid spicy, fatty, or fried foods. A nurse is calculating a client’s expected date of birth using Naegele’s rule. The client tells the nurse that her last menstrual cycle started on November 27th. Which of the following dates is the clients expected date of birth? **September 3rd** - Naegele’s rule = first day of last cycle – 3 months + 7 days A nurse is observing a new mother caring for her crying newborn who is bottle feeding. Which of the following actions by the mother should the nurse recognize as positive parenting behavior? **Lays the newborn across her lap and gently sways** - This tactile stimulation promotes a sense of security for the new born and is a correct technique for quieting a newborn. A nurse is teaching a client who is in preterm labor about terbutaline. Which of the following statements by the client indicates an understanding of the teaching? **”I will have blood tests because my potassium might decrease.”** - Terbutaline is administered subcutaneously every 4 hours for no longer than 24 hours. The adverse effects are hyperglycemia, hypokalemia, and hypotension. A nurse is reviewing the laboratory report of a client who is 24 hours postpartum following a vaginal delivery. Which of the following laboratory results should the nurse identify as an indication of a postpartum infection? **Erythrocyte Sedimentation Rate (ESR) 26 mm/hr** - The nurse should recognize that this exceeds the expected reference range for a postpartum client and indicates infection. A nurse is planning discharge for a client who is 3 days postpartum. Which of the following nonpharmacological interventions should the nurse include in the plan of care for lactation suppression? **Apply cabbage leaves to the breasts** - Plant sterols and salicylates from cabbage leaves can help to relieve swelling and discomfort caused by breast engorgement A nurse is caring for a client following an amniocentesis at 18 weeks gestation. Which of the following findings should the nurse report to the provider as a potential complication? **Leakage of fluid from the vagina** - Leakage of fluid from the vagina could indicate premature leakage of amniotic fluid and should be reported to the provider. A nurse is teaching a new mother about newborn safety. Which of the following instructions should the nurse include in the teaching? **”You can share your room with your baby for the next few weeks.”** - Room-sharing is recommended during the first few weeks. This allows the parents to be readily available to the newborn and learn the newborn’s cues. However, the nurse should instruct the parents to avoid placing the newborn in their bed as it increases the risk for SIDS. A nurse is assessing a client who is at 30 weeks gestation during a routine prenatal visit. Which of the following findings should the nurse report to the provider? **Swelling of the face** - Swelling of the face, sacral area, and hands can indicate gestational HTN or preeclampsia. Reduction in renal perfusion leads to sodium and water retention. Fluid moves out of the intravascular compartment into the tissues, causing edema. Varicose veins in the calves, nonpitting 1+ ankle edema, and hyperpigmentation of the cheeks are expected findings in the third trimester. A nurse is caring for a client who has hyperemesis gravidarum and is receiving IV fluid replacement. Which of the following findings should the nurse report to the provider? **BUN 25mg/dL** - The nurse should report an elevated BUN to the provider since it can indicate dehydration. A nurse in a prenatal clinic is assessing a group of clients. Which of the following clients should the nurse request the provider see first? **A client who is at 11 weeks gestation and reports abdominal cramping** - When using the urgent vs. nonurgent approach to client care, the nurse should determine that the priority finding is a client who is at 11 weeks gestation and reports abdominal cramping. Abdominal cramping can indicate an ectopic pregnancy or manifestations of spontaneous abortion. The nurse should request that the provider see this client first. A nurse is assessing a client who gave birth vaginally 12 hours ago and palpates her uterus to the right above the umbilicus. Which of the following interventions should the nurse perform? **Assist the client to empty her bladder.** - The nurse should assist the client to empty her bladder because the assessment findings indicate that the bladder is distended. This can prevent the uterus from contracting, resulting in increased vaginal bleeding or postpartum hemorrhage. Simethicone should be administered to reduce bloating, discomfort, or pain caused by excessive gas. A nurse is caring for a postpartum client who is receiving heparin via a continuous IV infusion for thrombophlebitis in her left calf. Which of the following actions should the nurse take? **Maintain the client on bed rest.** - The client should remain on bed rest to decrease the risk of dislodging the clot, which could cause a pulmonary embolism. A client receiving anticoagulant therapy, such as heparin, should not receive aspirin due to the risk of bleeding. The nurse should avoid massaging the affected leg to decrease the risk of dislodging the clot, which could cause a pulmonary embolism. The nurse should apply warm compresses to the affected area to promote circulation and decrease edema. A nurse is providing teaching about comfort measures to a client who is breastfeeding and is experiencing engorgement. Which of the following nonpharmacological measures should the nurse include in the teaching? **”You should use cold compresses after each feeding.”** - The nurse should suggest applying cold compresses or ice packs to alleviate the discomforts of engorgement in the client who is breastfeeding. The client should avoid the use of breast binders because they can decrease the milk supply. Applying colostrum to the nipples helps with sore nipples, and breast shells may be worn to promote circulation of air and prevent clothing from touching sore nipples. A nurse is teaching a new mother about steps the nurses will take to promote the security and safety of the newborn. Which of the following statements should the nurse make? **”Staff members who take care of your baby will be wearing a photo identification badge.”** - The nurse should teach the client that all staff members that care for newborns are required to wear a photo identification badge so that the client will be reassured of her newborn’s safety. When entering the unit, visitors must only provide the name of the client they are visiting. Clients are allowed to have anyone visit them on the unit without documentation of the visitor’s relationship to the client. The nurse should teach the mother to place the baby in the bassinet on the side of the bed away from the door while she is sleeping. A nurse is assessing a late preterm newborn. Which of the following clinical manifestations is an indication of hypoglycemia? **Respiratory distress** - Late preterm newborns are at an increased risk for hypoglycemia due to decreased glycogen stores and immature insulin secretion. Respiratory distress is a clinical manifestation of hypoglycemia. Other manifestations include an abnormal cry, jitteriness, lethargy, poor feeding, apnea, and seizures. A nurse is providing teaching to a client about the physiological changes that occur during pregnancy. The client is at 10 weeks gestation and has a BMI within the expected reference range. Which of the following client statements indicates an understanding of the teaching? **”I will likely need to use alternative positions for sexual intercourse.”** - The weight gain of pregnancy will likely require alternative positions for sexual intercourse. The recommended weight gain for a woman with a normal BMI is 25-35lbs. The recommended weight gain for a woman who has a BMI above the expected range is 15-20lbs. A nurse is teaching about effective breastfeeding to a client who is 3 days postpartum. Which of the following information should the nurse include? **”Your newborn should appear content after each feeding.”** - A baby who continues to show indications of hunger such as rooting, sucking on the hands, or crying may not be effectively emptying the breasts during feedings. The client’s breasts should feel softer after feeding indicating that they were emptied during the session. Mature milk production occurs 3-4 days postpartum. The newborn should void 6-8 times per day with at least 3 stools per day. It is not uncommon for a breastfed newborn to have stools with each feeding. A nurse is teaching a client who is 36 weeks gestation and has a prescription for a nonstress test. Which of the following statements should the nurse include in the teaching? **”You will be offered orange juice to drink during the test.”** - Having the client drink orange juice or another beverage high in glucose will stimulate the fetus during the procedure, helping to obtain results of fetal activity. The procedure will take 20-40 minutes and is noninvasive. Noninvasive procedures do not require informed consent. A nurse is assessing a client who is postpartum and has idiopathic thrombocytopenia pupura (ITP). Which of the following findings should the nurse suspect? **Decreased platelet count** - A client who has ITP has an autoimmune response that results in a decreased platelet count. An increased ESR is an indication of chronic renal failure, and increased WBCs is an indication of infection. A nurse in a family planning clinic is caring for a client who requests an oral contraceptive. Which of the following findings in the client’s history should the nurse recognize as a contraindication to oral contraceptives? **Cholecystitis, HTN, and migraine headaches** - A history of gallbladder disease (cholecystitis), HTN, or migraines are all contraindications for oral contraceptives. A nurse is teaching a new mother how to use a bulb syringe to suction her newborn’s secretions. Which of the following instructions should the nurse include? **Stop suctioning when the newborn’s cry sounds clear.** - The client should stop suctioning when the newborn’s cry no longer sounds like ti is coming through a bubble of fluid or mucus. The client should compress the bulb before inserting the syringe tip to avoid pushing/blowing the secretions further inside. The newborn’s mouth should always be suctioned before the nose (Nobody wants to taste their own snot!), and the syringe should be inserted into the side of the mouth to avoid triggering the gag reflex. A nurse is assessing a client who is in active labor and notes early decelerations in the FHR on the monitor tracing. The client is 39 weeks gestation and is receiving a continuous IV infusion of oxytocin. Which of the following actions should the nurse take? **Continue monitoring the client.** - Early decelerations in the FHR are considered benign and occur due to compression of the fetal head during contractions, vaginal exams, and pushing during the second stage of labor. No interventions are necessary for early decelerations. A nurse is teaching a group of parents about newborn safety. Which of the following statements by a parent indicates an understanding of the teaching? **”I will dress my baby in flame-retardant clothing.”** - Flame-retardant clothing will help prevent injury to the baby. Parents should avoid using plastic in the crib or bibs around the newborn’s neck at night to avoid suffocation and choking. The parents should not heat formula in a microwave to prevent uneven warming. A nurse is assessing a client who is 1 day postpartum and has a vaginal hematoma. Which of the following manifestations should the nurse expect? **Vaginal pressure** - The nurse should expect a client with a vaginal hematoma to report pressure in the vagina due to the blood that leaked into the tissues and persistent vaginal or rectal pain. Lochia serosa vaginal drainage is a manifestation for a client who is 4-10 days postpartum. A charge nurse on the postpartum unit is observing a newly licensed nurse who is preparing to administer pain medication to a client. The charge nurse should intervene when the newly licensed nurse uses which of the following secondary identifiers to identify the client? **The client’s room number** - The client’s room number can change and places the client at risk for a medication error. A nurse is providing discharge teaching to a client who had a cesarean birth 3 days ago. Which of the following instructions should the nurse include? **”You can still become pregnant if you are breastfeeding.”** - The nurse should inform the client that breastfeeding does not prevent ovulation. Contraception that is safe during breastfeeding should be discussed with this client. It is recommended that the client wait until after the 6-week follow-up appointment to resume sexual activity. Kegel exercises are helpful to maintain tone of the pelvic muscles and ensure future urinary continence after any pregnancy. The client should avoid abdominal exercises for 4-6 weeks following a cesarean birth. A nurse is providing discharge teaching to a client who is postpartum. For which of the following clinical manifestations should the nurse instruct the client to monitor and report to the provider? **Unilateral breast pain** - Chills, fever, malaise, and unilateral breast pain can be indications of mastitis, an infection of the breast tissue that should be reported to the provider. Persistent abdominal striae are caused by the separation of the underlying connective tissue and are an expected postpartum finding. Temperatures of 100.4F or higher should be reported as an indication of infection. Brownish-red discharge is an expected manifestation for 3-10 days postpartum. The client should report a large amount of lochia or clots to the provider. A nurse is caring for a client who is 15 weeks gestation, Rh-negative, and has just had an amniocentesis. Which of the following interventions is the nurse’s priority following the procedure? **Monitor the FHR** - The greatest risk to this client and her fetus is fetal death. A nurse is admitting a client to the labor and delivery unit when the client states, “My water just broke.” Which of the following interventions is the nurse’s priority? **Begin FHR monitoring.** - The greatest risk to the client and her fetus following a rupture of membranes is umbilical cord prolapse. The nurse should monitor the fetus closely to ensure well-being. A nurse is caring for a client who has recently experienced a perinatal death. Which of the following statements should the nurse make to the client? **”I’m sad for you.”** - This statement shows empathy and encourages the client to communicate about the death. A nurse is assessing a client who is 38 weeks gestation during a weekly prenatal visit. Which of the following findings should the nurse report to the provider? **Weight gain of 2.2kg (4.8lb)** - This is greater than the expected weekly weight gain and could indicate complications. A nurse is caring for a client who has uterine hypotonicity and is experiencing postpartum hemorrhage. Which of the following actions is the nurse’s priority? **Massage the client’s fundus.** - The nurse’s priority is to massage the client’s fundus to minimize blood loss and help prevent hypovolemic shock. A nurse in a provider’s office is reviewing the medical record of a client who is in her first trimester. Which of the following findings should the nurse identify as a risk factor for the development of preeclampsia? **Pregestational diabetes** - Risk factors for the development of preeclampsia include pregestational diabetes, preexisting HTN, renal disease, systemic lupus erythematosus, BMI greater than 30, multifetal gestations, maternal age less than 19 or greater than 40, and rheumatoid arthritis. A nurse is planning care for a client who is in labor and is requesting epidural anesthesia for pain control. Which of the following actions should the nurse include in the plan of care? **Monitor the client’s blood pressure every 5 minutes following the first dose of anesthetic solution.** - The nurse should plan to obtain a baseline blood pressure prior to the initial dose of anesthetic solution and monitor every 5-10 minutes after to assess for maternal hypotension. The nurse should also plan to position the client upright to allow the solution to flow downward, administer 500-1000mL of lactated Ringer’s or normal saline 15-30 minutes prior to the first dose in order to reduce the risk of maternal hypotension. Dextrose should not be administered because it can cause maternal hyperglycemia and fetal hypoglycemia. A nurse is providing teaching about nonpharmacological pain management to a client who is breastfeeding and has engorgement. The nurse should recommend the application of which of the following items? **Cold cabbage leaves** A nurse is providing prenatal teaching to a client who is 26 weeks gestation. Which of the following positions should the nurse recommend for the client to increase circulation to the placenta? **Side-lying** - Side-lying avoids compression of the vena cava and promotes placental perfusion. A nurse is speaking with a client who is trying to make a decision about uterine tube occlusion. The client asks, “What effects will this procedure have on my sex life?” Which of the following responses should the nurse make? **”This process should have no effect on your sexual performance or adequacy.”** - Sexual function depends on various hormonal and psychological factors. Tubal occlusion should have no physiological effect on sexual performance or adequacy. Enjoyment of sex should increase due to the loss of fear of pregnancy. A nurse is discussing the differences between true labor and false labor with a group of expectant parents. Which of the following characteristics should the nurse include when discussing true labor? **Contractions become stronger with walking** - The contractions that occur during true labor increase in intensity and become more regular with a change in activity. True labor cannot be suppressed by using comfort measures, and the pain is felt in the lower back and lower abdomen. A nurse is teaching a client who has pregestational type 1 diabetes about management during pregnancy. Which of the following statements by the client indicates an understanding of the teaching? **”I will continue taking my insulin if I experience nausea and vomiting.”** - The client should continue taking her insulin as prescribed during illness to prevent hypoglycemia and hyperglycemia. Her fasting glucose goal should be 60-90mg/dL. The nurse should teach the client to avoid snacks and foods high in refined sugar and to not exercise during periods of hyperglycemia and when positive urine ketones are present. A nurse is assessing a newborn who was delivered vaginally and experienced a tight nuchal cord. Which of the following clinical manifestations should the nurse expect? **Petechiae over the head** - Nuchal cord, or the umbilical cord being wrapped tightly around the neck, can cause bruising and petechiae over the face, head, and neck. A nurse is teaching a client who is 24 weeks gestation regarding 1-hour glucose tolerance testing. Which of the following statements should the nurse include in her teaching? **”A blood glucose of 130-140 is considered a positive screening result.”** - The nurse should teach the client that a blood glucose level of 130-140 is considered a positive screening. If she receives a positive result, she will need to undergo a 3-hour glucose tolerance test to confirm gestational diabetes. A nurse is assessing a newborn who is 12 hours old. Which of the following clinical manifestations requires intervention by the nurse? **Substernal chest retractions while sleeping** - Substernal chest retractions can indicate respiratory distress syndrome in the newborn. This clinical manifestation requires further assessment and intervention by the nurse. An audible murmur at the left sternal border is an expected finding in newborns. Acrocyanosis is a bluish discoloration of the newborn’s hands and feet and is expected. Babinski reflex is a normal finding that is elicited when a newborn’s sole is stroked and the newborn’s toes hyperextend in response. A nurse is caring for a client who is 22 weeks gestation and reports concern about the blotchy hyperpigmentation on her forehead. Which of the following actions should the nurse take? **Explain to the client that this is an expected occurrence.** - Chloasma, the mask of pregnancy, is a blotchy brown hyperpigmentation of the skin over the cheeks, nose, and forehead. It is seen most often in dark-skinned women and is caused by an increase in melanotropin during pregnancy. It appears after 16 weeks gestation and increases gradually until deliver for 50- 70% of women. The nurse should reassure the client that this is expected and usually fades after delivery. A nurse is caring for a client who is to receive oxytocin to augment her labor. Which of the following findings contraindicates the initiation of the oxytocin infusion and should be reported to the provider? **Late decelerations** - Late decelerations are indicative of uteroplacental insufficiency and is a contraindication for the administration of oxytocin. A nurse is planning care for a client who is 24 weeks gestation and reports daily mild headaches. Which of the following instructions should the nurse include in the plan of care? **Recommend that the client perform conscious relaxation techniques daily.** - Conscious relaxation techniques are a way to relieve tension and reduce stress which can help to decrease and eliminate headaches. A nurse is providing discharge teaching to a parent whose newborn has just had a circumcision. Which of the following instructions should the nurse include? **Apply slight pressure with a sterile gauze pad for mild bleeding.** - The client should attempt to stop mild bleeding first with a sterile gauze pad, and if unsuccessful, the client should notify the provider. The client should change the newborn’s diaper and examine the circumcision site at least every 4 hours. Baby wipes containing alcohol can irritate the skin and should be avoided until the circumcision has healed, which usually takes 5-6 days. During each diaper change, the penis should be washed gently with warm water and have petroleum jelly applied to the glans. The client should not attempt to remove any yellow exude from the circumcision site because it is part of the healing process, which begins 24 hours post procedure and can last 2-3 days. Disrupting this process can cause pain and bleeding. A nurse is reviewing the medical record at 1800 for a client who is 34 weeks gestation. Based on the chart findings and documentation, the nursing plan of care should include which of the following actions? **Administer terbutaline.** - The nurse should administer terbutaline to stop contractions because the lab results indicate that the fetus’s lungs are not mature enough for delivery. A nurse is developing a plan of care for a client who has preeclampsia and is receiving magnesium sulfate via a continuous IV infusion. Which of the following interventions should the nurse include in the plan? **Monitor FHR continuously.** - Magnesium sulfate, which is used to prevent seizures in clients who have preeclampsia, is a high-alert medication that requires close monitoring. The FHR and uterine contractions should be monitored continuously while the client is treated with this medication. The vitals should be monitored every 15-30 minutes. Intake should be no more than 125mL/hr. Calcium gluconate should only be administered if the client shows signs of magnesium sulfate toxicity such as loss of deep tendon reflexes, respiratory depression, slurred speech, or cardiac arrest. A nurse is preparing to administer magnesium sulfate 2g/hr IV to a client who is in preterm labor. Available is 20g magnesium sulfate in 500mL dextrose 5% in water (D5W). The nurse should set the IV infusion pump to administer how many mL/hr? (Whole number) **50mL/hr** A nurse in a woman’s health clinic is providing teaching about nutritional intake to a client who is 8 weeks gestation. The nurse should instruct the client to increase her daily intake of which of the following nutrients? **Iron** - The recommendation for iron intake during pregnancy is 27mg/day. A nurse is teaching clients in a prenatal class about the importance of taking folic acid during pregnancy. The nurse should instruct the clients to consume an adequate amount of folic acid from various sources to prevent which of the following fetal abnormalities? **Neural tube defect** - The nurse should inform the clients that neural tube defects are more common in newborns born to mothers who had inadequate folic acid intake. Food sources of folic acid include fortified cereals and grain products, oranges, artichokes, liver, broccoli, and asparagus. A nurse is assessing a client who received carboprost for postpartum hemorrhage. Which of the following findings is an adverse effect of this medication? **Hypertension** - The nurse should recognize that carboprost is a vasoconstrictor that can cause HTN. A nurse is caring for a newborn who is undergoing phototherapy to treat hyperbilirubinemia. Which of the following actions should the nurse take? **Cover the newborn’s eyes while under the phototherapy light.** - Applying an opaque eye mask prevents damage to the newborn’s retinas and corneas from the phototherapy light. All of the newborn’s clothing should be removed except a diaper when undergoing phototherapy. All moisture or creams should be avoided because they can absorb heat and cause burns. The nurse should turn and reposition the newborn every 2-3 hours to allow for maximum exposure of body surfaces to the phototherapy light. A nurse is performing a newborn assessment. Which of the following images should the nurse identify as an indication of spina bifida occulta? ** ** - External indications of the neural tube defect spina bifida occulta include a dimpled area over the defect and the presence of a birthmark or hairy patch above the area. A nurse is providing teaching for a client who gave birth 2 hours ago about the facility policy for newborn safety. Which of the following client statements indicate an understanding of the teaching? **”The person who comes to take my baby’s pictures will be wearing a photo identification badge.”** - All personnel working on the unit should wear a photo identification badge. The nurse should teach the mother to never allow anyone who is not wearing an identification badge to come in contact with her newborn. The nurse will match the newborn’s identification number with the mother’s when she brings the baby to the mother’s room. Newborns should always be transported in a bassinet when outside the mother’s room and should always wear the electronic security bracelet because it will alarm if anyone removes it or if the infant is brought near an exit door. A nurse is preparing to perform Leopold maneuvers for a client. Identify the sequence the nurse should follow. **Palpate the fundus to identify the fetal part. Determine the location of the fetal back. Palpate for the fetal part presenting at the inlet. Identify the attitude of the head.** A nurse is assessing a full-term newborn 15 minutes after birth. Which of the following findings requires intervention by the nurse? **Respiratory rate 18/min** - During the first phase of a newborn’s transition, up to 30 minutes after birth, the respiratory rate can range 20-100/min, heart rate of 160-180, presence of tremors, crying, and startling motions, and fine crackles and nasal flaring are expected. A nurse is caring for a client who is 40 weeks gestation and in early labor. The client has a platelet count of 75,000/mm3 and is requesting pain relief. Which of the following treatment modalities should the nurse anticipate? **Attention-focusing** - The low platelet count places the client at a high risk for bleeding which contraindicates the placement of an epidural. A pudendal nerve block is administered during the third stage of labor for the repair of an episiotomy or laceration. Attention-focusing and distraction techniques are the safest types of care for this patient to effectively relieve her labor pain. A school nurse is providing teaching to an adolescent about levonorgestrel contraception. Which of the following information should the nurse include in the teaching? **”You should take the medication within 72 hours following unprotected sexual intercourse.”** - Levonorgestrel is an emergency contraceptive which inhibits ovulation to prevent conception. It has no effect on the other oral contraceptive the adolescent might be taken and should be taken if an adolescent misses a dose of her regular daily oral contraception and engages in unprotected sex. Levonorgestrel will not protect from future instances of unprotected sex after taking the medication. A nurse is caring for a client who is in labor and reports increasing rectal pressure. She is experiencing contractions 2-3 minutes apart, each lasting 80-90 seconds, and a vaginal exam reveals her cervix is dilated to 9cm. The nurse should identify that the client is in which of the following phases of labor? **Transition** - Latent phase is the first phase of labor characterized by cervical dilation of 0-3cm and contractions every 5-30 minutes each lasting 30-45 seconds. Active phase is the second phase of labor characterized by cervical dilation of 4-7cm and contractions every 3-5 minutes each lasting 40-70 seconds. Transition phase is the next phase of labor characterized by cervical dilation of 8-10cm and contractions every 2-3 minutes each lasting 45-90 seconds. Descent phase is the last phase of labor characterized by active pushing with contractions every 1-2 minutes each lasting 90 seconds each. A nurse is performing a vaginal exam on a client who is in labor and reports severe pressure and pain in the lower back. The nurse notes that the fetal head is in a posterior position. The nurse should identify that which of the following is the best nonpharmacological intervention to perform to relieve the client’s discomfort? **Counter-pressure** - Counter-pressure is the best nonpharmacological technique to use when relieving the client’s discomfort from the fetus being in a posterior position because this intervention lifts the fetal head off of the spinal nerve. A nurse is developing an educational program for adolescents about nutrition during the third trimester. Which of the following statements should the nurse include in the program? **”Consume 3-4 servings of dairy each day.”** - Calcium intake is important during an adolescent’s pregnancy because bone absorption of calcium is still occurring. Sodium supports the increase in blood volume that occurs during pregnancy. Adequate sodium intake is 1.5g/day. Adequate protein is necessary to support the rapid growth of the fetus, maternal tissues, increasing blood volume, and the formation of the amniotic fluid. Protein intake during the second and third trimester should be 71g daily. A nurse is planning care for a client who is 2 hours postpartum. Which of the following interventions should the nurse plan to implement during the taking-hold phase of postpartum behavioral adjustment? **Demonstrate to the client how to perform a newborn bath.** - During the taking-in phase, the client displays dependent and passive behaviors and due to excitement and fatigue is unable to retain information. During this phase, the nurse should repeat instructions to ensure client understanding and should allow the client and her partner to reflect on the birth experience. During the taking-hold phase, the mother begins taking a stronger interest in her role as mother and is focusing on the care of her newborn and acquiring new parenting skills. This is the perfect time to teach the client caregiving skills while offering positive reinforcement to promote maternal adjustment and confidence. The letting-go phase focuses on moving forward as a family with interchanging members. The discussion of contraceptive options should occur during this last phase. A nurse is preparing to collect a blood specimen from a newborn via a heel stick. Which of the following techniques should the nurse use to help minimize the pain of the procedure for the newborn? **Place the newborn skin to skin on the mother’s chest.** - Placing the newborn skin to skin on the mother’s chest is an effective technique to significantly decrease the newborn’s pain and anxiety levels. The nurse should implement this technique before, during, and after the procedure. A warm pack can also be applied prior to the puncture to help ensure an adequate specimen is obtained. A nurse is caring for a newborn who was transferred to the nursery 30 minutes after delivery. Which of the following actions should the nurse take first? **Verify the newborn’s identification.** - When using the safety/risk reduction approach to client care, the first action the nurse should take is to verify the newborn’s identity upon arrival to the nursery. IM vitamin K is administered soon after birth to increase clotting factors and prevent bleeding but can be delayed until after initial bonding time and the first breastfeeding. A nurse is performing a physical assessment of a newborn upon administration to the nursery. Which of the following clinical manifestations should the nurse expect? **Creases over 2/3 of the soles of the feet, molding of the head, and lanugo on the shoulders.** - Molding of the head occurs during the birth process as the newborn travels through the birth canal, resulting in compression of the soft bones of the skull. A nurse providing dietary teaching to a client who has hyperemesis gravidarum. Which of the following statements by the client indicates understanding of the teaching? **”I will eat foods that appeal to my taste instead of trying to balance my meals.”** - Clients who have hyperemesis gravidarum should eat to taste to avoid nausea, avoid going to bed with an empty stomach, alternate liquids and solids every 2-3 hours to avoid empty stomach or over-filling, and should eat protein following a sweet snack. A nurse is assessing fetal heart tones for a client who is pregnant. The nurse has determined the fetal position as left occipital anterior. To which of the following areas of the client’s abdomen should the nurse apply the ultrasound transducer in order to assess the point of maximum intensity of the fetal heart? **Left lower quadrant** - The fetal heart tones of a fetus in the left occipital anterior position are best heard in the left lower quadrant. The fetal heart tones of a fetus in the left sacrum anterior position are best heard in the left upper quadrant. The fetal heart tones of a fetus in the right sacrum anterior position are best heard in the right upper quadrant. The fetal heart tones of a fetus in the right occipital anterior position are best heard in the right lower quadrant. A nurse is providing discharge teaching to the parents of a newborn about using a car seat properly. Which of the following instructions should the nurse include? **Position the car seat rear-facing in the back seat of the vehicle.** - Infants and toddlers should remain rear-facing in the backseat until they are 2 years old or reach the height and weight requirements of the car seat manufacturer. The newborn should be placed at a 45 degree angle to minimize the risk of airway obstruction from leaning forward. The retainer clip should be at the level of the newborn’s axillae and the shoulder harness just below the newborn’s shoulders. A nurse is providing education about family bonding to parents who recently adopted a newborn. The nurse should make which of the following suggestions to aid the family’s 7 year old child in accepting the new family member? **Obtain a gift from the newborn to present to the sibling.** - Presenting a gift from the newborn to the sibling is a strategy to facilitate a school-age sibling’s acceptance of the new family member so that the new sibling doesn’t feel left out and understands his role in the family. A nurse is assessing 4 newborns. Which of the following findings should the nurse report to the provider? **A newborn who is 18 hours old and has an axillary temperature of 37.7C (99.9F)** - An axillary temperature greater than 37.5D (99.5F) is above the expected range and can be an indication of sepsis. Erythema toxicum is a transient rash that can occur anywhere on the newborn’s body during the first 24-72 hours following birth but requires no intervention. Meconium stool should be passed within the first 24-48 hours following birth. Pink tinged urine is an indication of uric acid crystals and an expected finding in a newborn for the first week following birth. A nurse is performing a vaginal exam for a client who is in active labor and reports back pain. The nurse determines that the client is 8cm dilated, 100% effaced, -2 station, and that the fetus is in the occiput posterior position. Which of the following actions should the nurse take? **Assist the client to the hands and knees position.** - The nurse should assist the client into the hands and knees position to help relieve the back pain and enable the rotation of the fetus from the posterior to an anterior occiput position. A nurse is assessing a client who is 12 hours postpartum. The client’s fundus is 2 fingerbreadths above the umbilicus, deviated to the right of midline, and less firm than previously noted. Which of the following actions should the nurse take? **Assist the client to the bathroom to void.** - A distended bladder inhibits the uterus from contracting normally and can cause uterine atony. A nurse is assessing a client who is 26 weeks gestation. Which of the following manifestations should the nurse report to the provider? **Decreased urine output** - Decreased urine output, increased blood pressure, proteinuria, and decreased fetal activity can be signs of preeclampsia and should be reported. [Show More]
Last updated: 1 year ago
Preview 1 out of 26 pages
Reviews( 0 )
Document information
Connected school, study & course
About the document
Uploaded On
Jul 02, 2021
Number of pages
26
Written in
Additional information
This document has been written for:
Uploaded
Jul 02, 2021
Downloads
0
Views
47






.png)

 Correct Study Guide, Download to Score A.png)