*NURSING > NCLEX-RN > Gastrointestinal System Disorders NCLEX 2021 Summer Final Practice Quiz #7 (35 Questions) (All)
Gastrointestinal System Disorders NCLEX 2021 Summer Final Practice Quiz #7 (35 Questions)
Document Content and Description Below
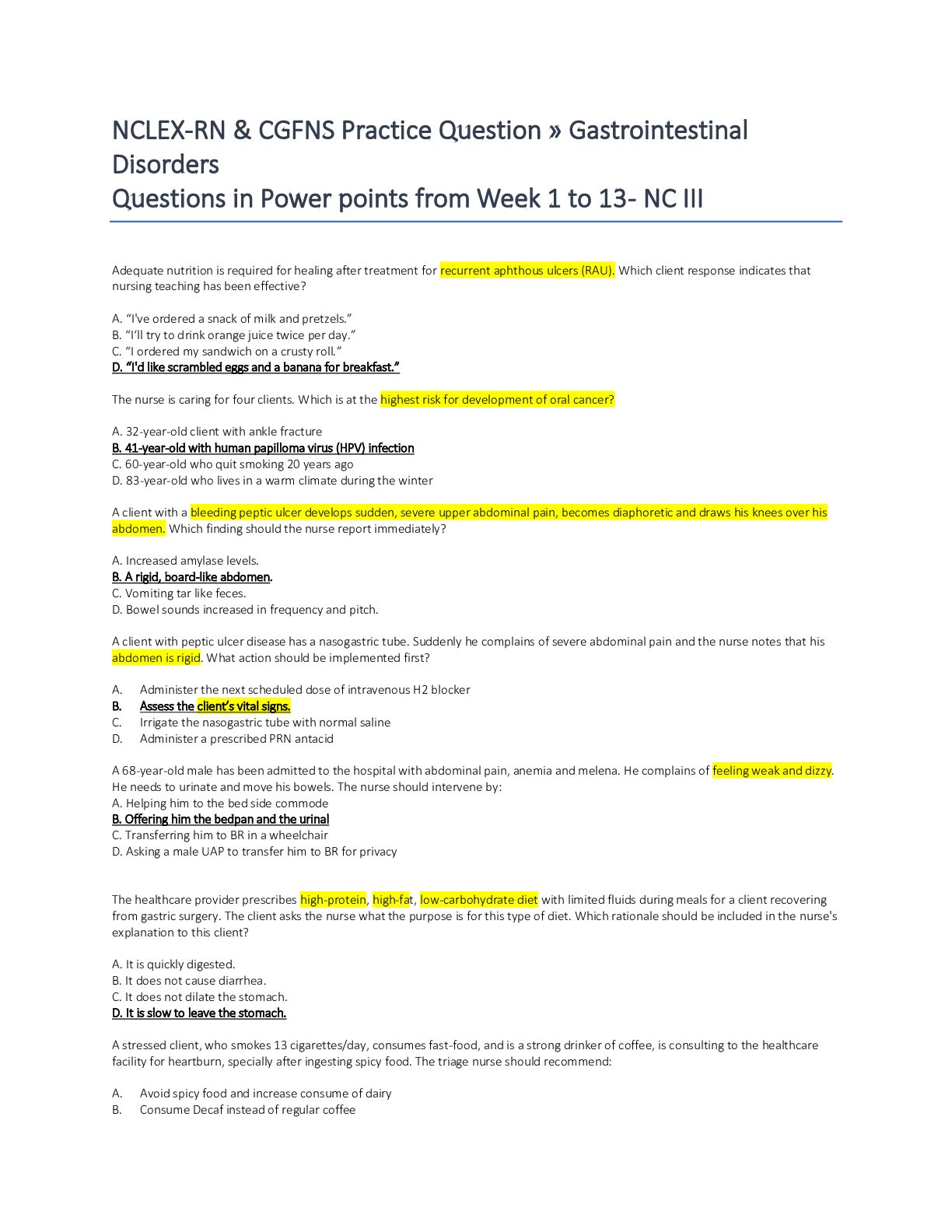
Gastrointestinal System Disorders NCLEX 2021 Summer Final Practice Quiz #7 (35 Questions) 1. Question Which of the following laboratory values would be the most important to monitor for a patient wi... th pancreatic cancer? • A. Serum glucose • B. Radioimmunoassay (RIA) • C. Creatine phosphokinase (CPK) • D. Carcinoembryonic antigen (CEA) Correct Answer: A. Serum glucose In pancreatitis, hypersecretion of the insulin from a tumor may affect the islets of Langerhans, resulting in hyperinsulinemia, a complication of pancreatic cancer. Pancreatitis damages the cells that produce insulin and glucagon, which are the hormones that control the amount of glucose in the blood. This can lead to an increase in blood glucose levels. • Option B: RIA should also be monitored to measure the effects of therapy, but hypoglycemia may be life-threatening. Determination of serum pancreatic enzymes remains the gold standard for the diagnosis of acute pancreatitis. More expensive and cumbersome methods such as RIA or ELISA for pancreatic elastase are useful only in special clinical circumstances. • Option C: Creatine phosphokinase is an enzyme that reflects normal tissue catabolism. Elevated serum levels indicate trauma to cells with high CPK content. CPK and CPK-isoenzymes are used to detect myocardial infarction. Serum CPK is elevated in most alcoholics including patients with delirium tremens (6, 9) or acute pancreatitis, a finding which possibly reflects a certain degree of myopathy known to occur in patients with acute alcohol intoxication as well as with chronic alcoholism • Option D: Carcinoembryonic antigen (CEA) is one of the most widely used tumor markers and is increased in 30%–60% of patients with pancreatic cancer. Although carbohydrate antigen 19-9 (CA19-9) is the most important serum biomarker in pancreatic cancer, the diagnostic and prognostic value of CEA is gradually being recognized. 2. Question You observe changes in mentation, irritability, restlessness, and decreased concentration in a patient with cancer of the liver. Hepatic encephalopathy is suspected and the patient is ordered neomycin enemas. Which of the following information in the patient’s history would be a contraindication of this order? • A. Left nephrectomy • B. Glaucoma in both eyes • C. Myocardial infarction • D. Peripheral neuropathy Correct Answer: A. Left nephrectomy Neomycin prevents the release of ammonia from the intestinal bacteria flora and from the breakdown of red blood cells. Common side-effects of this drug are nephrotoxicity and ototoxicity. Patients with renal disease or renal impairment should not take this drug. A baseline serum BUN/creatinine should be obtained with subsequent periodical follow-up blood tests during chronic therapy to monitor for effects on renal function. Prompt discontinuation of the drug should occur with any signs of renal or otologic damage. • Option B: Glaucoma is not affected by neomycin. Neomycin belongs to a group of antibiotics known as aminoglycosides. Like others in the aminoglycoside family, neomycin works by inhibiting bacterial protein synthesis leading to its bactericidal effect. This group of medications is particularly effective in killing gram-negative organisms allowing for good coverage of enteric organisms. • Option C: MI is not affected by neomycin. Neomycin’s mechanism of action is very similar to most aminoglycosides as it binds to the 30s ribosomal subunit interfering with bacterial protein synthesis. This action thereby disrupts the process of translation by bacteria leading to the medication’s bactericidal effects. • Option D: Peripheral neuropathy is a chronic complication of diabetes mellitus. Neomycin’s bactericidal effects decrease ammonia-producing bacteria residing in the GI tract, thereby decreasing the burden of ammonia on the patient. Neomycin is often reserved for patients that cannot tolerate rifaximin. 3. Question A nursing intervention for a patient with hepatitis B would include which of the following types of isolation. • A. Universal precautions • B. Blood transfusions • C. Enteric isolation • D. Strict isolation Correct Answer: A. Universal precautions Universal precautions are indicated for the patient with hepatitis B. Hepatitis B is contracted via blood and blood products, body secretions, and punctures from contaminated needles. Universal precautions apply to blood and to other body fluids containing visible blood. Occupational transmission of HIV and HBV to healthcare workers by blood is documented. Blood is the single most important source of HIV, HBV, and other bloodborne pathogens in the occupational setting. • Option B: Currently, guidelines for transfusion of red blood cells (RBC), generally follow a restrictive threshold. While there is some variation in the number for the threshold, 7 g/dL is an agreed-upon value for asymptomatic healthy patients. Transfusion may also be indicated in patients with active or acute bleeding as well as in patients with symptoms related to anemia (for example, tachycardia, weakness, dyspnea on exertion) and hemoglobin less than 8 g/dL. • Option C: Enteric precautions are taken to prevent infections that are transmitted primarily by direct or indirect contact with fecal material. They’re indicated for patients with known or suspected infectious diarrhea or gastroenteritis. Clostridium difficile is the most common cause of hospital-acquired infectious diarrhea. • Option D: Strict isolation includes suspected highly infectious and transmissible virulent and pathogenic microbes, highly resistant bacterial strains, and agents that are not accepted in any form of distribution in society or in the environment. Examples are completely resistant Mycobacterium tuberculosis, viral hemorrhagic fevers like Ebola and Lassa, pandemic severe influenza, and coronavirus like SARS, MERS, etc. 4. Question A patient is admitted with lacerated liver as a result of blunt abdominal trauma. Which of the following nursing interventions would not be appropriate for this patient? • A. Monitor for respiratory distress. • B. Monitor for coagulation studies. • C. Administer pain medications as ordered. • D. Administer normal saline, crystalloids as ordered. Correct Answer: C. Administer pain medications as ordered. Pain medication may mask signs and symptoms of hemorrhage, further decrease blood pressure, and interfere with assessment of neurologic status and additional abdominal injury. With the potential for hemorrhage, nonsteroidal anti-inflammatory drugs (NSAIDs) probably should be avoided. Acetaminophen with or without small quantities of mild narcotic analgesics may be all that should be prescribed initially. Minimize use of analgesics in patients who are admitted for observation. • Option A: The evaluation of any trauma patient begins with evaluating the airway, accessing the breathing, and managing the circulation. The diagnosis of intra-abdominal injury following blunt trauma depends primarily on the hemodynamic status of the patient. Once the airway is protected, it is mandatory to protect the cervical spine. • Option B: Because the presentation is often not straightforward, the diagnosis can be difficult and often time-consuming. Besides pain, the patient may present with bleeding per rectum, unstable vital signs, and the presence of peritonitis. The physical exam may reveal marks from a lap belt, ecchymosis, abdominal distention, absent bowel sounds, and tenderness to palpation. • Option D: After the primary survey is complete, patients who are hypotensive require aggressive fluid resuscitation. If hemodynamic instability persists, blood should be typed and crossed, but in the meantime, immediate transfusion with O negative blood can be done (O+ for males and women past childbearing years). All patients with blunt abdominal trauma who have signs of peritonitis, frank bleeding, or worsening of clinical signs require an immediate laparotomy. 5. Question A male client is recovering from a small bowel resection. To relieve pain, the physician prescribes meperidine (Demerol), 75 mg I.M. every 4 hours. How soon after administration should meperidine onset of action occur? • A. 5 to 10 minutes • B. 15 to 30 minutes • C. 30 to 60 minutes • D. 2 to 4 hours Correct Answer: B. 15 to 30 minutes Meperidine onset of action is 15 to 30 minutes. It peaks between 30 and 60 minutes and has a duration of action of 2 to 4 hours. Meperidine, also known as pethidine, is in the class of phenylpiperidine as a hydrochloride salt synthetic form of the opioid, which is a white crystalline with a melting point of 186°C. This medication has calcium sulfate, dibasic calcium phosphate, starch, stearic acid, and talc as inactive ingredients. Clinicians use meperidine for the treatment of moderate to severe pain. • Option A: Oral form is not recommended for acute pain control. Using Meperidine for pain control should be considered if no other options are available, in which case the duration of medication use should be limited to less than 48 hours, and the total dosage administered should not exceed 600 mg in 24 hours. • Option C: Meperidine has the same mechanism of action as morphine, which is acting as an agonist to the mu-opioid receptor. The anti-shivering effect may involve the stimulation of k-opioid receptors. • Option D: Meperidine also has some local anesthetic effects because of its interactions with sodium ion channels. Also, meperidine has stimulant effects by inhibition of the dopamine transporter (DAT) and norepinephrine transporter (NET). 6. Question Nathaniel has severe pruritus due to having hepatitis B. What is the best intervention for his comfort? • A. Give tepid baths. • B. Avoid lotions and creams. • C. Use hot water to increase vasodilation. • D. Use cold water to decrease the itching. Correct Answer: A. Give tepid baths. For pruritus, care should include tepid sponge baths and use of emollient creams and lotions. Bathe or shower using lukewarm water and mild soap or nonsoap cleansers. Long bathing or showering in hot water causes drying of the skin and can aggravate itching through vasodilation. • Option B: Lubrication with fragrance-free creams or ointments serves as a barrier to prevent further drying of the skin through evaporation. Moisturizing is the cornerstone of treatment. Over-the-counter moisturizing lotions include Eucerin, Lubriderm, and Nivea. Lotions are lighter and less emollient than creams. • Option C: Encourage the patient to adopt skincare routines to decrease skin irritation. After bathing, allow the skin to air dry or gently pat the skin dry. Avoid rubbing or brisk drying. Rubbing the skin with a towel can irritate the skin and exacerbate the itch-scratch cycle. • Option D: If more moisturizing is required than a lotion can provide, a cream is recommended. These include Keri cream, Cetaphil cream, Eucerin cream, and Neutrogena Norwegian formula. Ointments are the most emollient. Vaseline Pure Petroleum Jelly or Aquaphor Natural Healing Ointment may be beneficial. 7. Question Rob is a 46 y.o. admitted to the hospital with a suspected diagnosis of Hepatitis B. He’s jaundiced and reports weakness. Which intervention will you include in his care? • A. Regular exercise. • B. A low-protein diet. • C. Allow the patient to select his meals. • D. Rest period after small, frequent meals. Correct Answer: D. Rest period after small, frequent meals. Rest periods and small frequent meals are indicated during the acute phase of hepatitis B. Monitor dietary intake and caloric count. Suggest several small feedings and offer the “largest” meal at breakfast. Large meals are difficult to manage when a patient is anorexic. Anorexia may also worsen during the day, making intake of food difficult later in the day. • Option A: Institute bed red or chair rest during the toxic state. Provide a quiet environment; limit visitors as needed. This promotes rest and relaxation. Available energy is used for healing. Activity and an upright position are believed to decrease hepatic blood flow, which prevents optimal circulation to the liver cells. • Option B: If tolerated, a normal or increased protein intake helps with liver regeneration. Protein restriction may be indicated in severe disease (fulminant hepatitis) because the accumulation of the end products of protein metabolism can potentiate hepatic encephalopathy. • Option C: Consult with a dietitian, nutritional support team to provide diet according to patient’s needs, with fat and protein intake as tolerated. Useful in formulating dietary programs to meet individual needs. Fat metabolism varies according to bile production and excretion and may necessitate the restriction of fat intake if diarrhea develops. 8. Question You’re discharging Nathaniel with hepatitis B. Which statement suggests understanding by the patient? • A. “Now I can never get hepatitis again.” • B. “I can safely give blood after 3 months.” • C. “I’ll never have a problem with my liver again, even if I drink alcohol.” • D. “My family knows that if I get tired and start vomiting, I may be getting sick again.” Correct Answer: D. “My family knows that if I get tired and start vomiting, I may be getting sick again.” Hepatitis B can recur. Patients infected with HBV could be asymptomatic initially and, depending on the particular genotype, might not be symptomatic throughout the infected state. In these particular cases, careful history taking is important to establish a diagnosis. However, when symptomatic from acute HBV infection, patients can present with serum sickness-like syndrome manifested as fever, skin rash, arthralgia, and arthritis. This syndrome usually subsides with the onset of jaundice. Patients may also have fatigue, abdominal pain, nausea, and anorexia. • Option A: Unlike hepatitis A and hepatitis E, in which there is no chronic state, HBV infection has the potential for the development of a chronic state. Chronic hepatitis B predisposes a patient to the development of portal hypertension, cirrhosis, and its complications or hepatocellular carcinoma (HCC). • Option B: Patients who have had hepatitis are permanently barred from donating blood. HBsAg is transmitted via blood contact or body secretions, and the risk of acquiring hepatitis B is considerably higher in individuals with close contact with HBsAg-positive patients. • Option C: Alcohol is metabolized by the liver and should be avoided by those who have or had hepatitis B. As such, patients with HBV infection should be monitored closely, and a referral to a specialist is highly recommended. Fulminant liver failure from HBV infection requires an emergent liver transplant evaluation at a liver transplant center. 9. Question Gail is scheduled for a cholecystectomy. After completion of preoperative teaching, Gail states,” If I lie still and avoid turning after the operation, I’ll avoid pain. Do you think this is a good idea?” What is the best response? • A. “You’ll need to turn from side to side every 2 hours.” • B. “It’s always a good idea to rest quietly after surgery.” • C. “The doctor will probably order you to lie flat for 24 hours.” • D. “Why don’t you decide about activity after you return from the recovery room?” Correct Answer: A. “You’ll need to turn from side to side every 2 hours.” To prevent venous stasis and improve muscle tone, circulation, and respiratory function, encourage her to move after surgery. Insufflation of the abdominal cavity with carbon dioxide during laparoscopic surgery increases abdominal pressure, which may cause stasis of the blood flow in inferior vena cava and common iliac veins. Moreover, the reverse Trendelenburg position, in which laparoscopic cholecystectomy is performed, decreases venous return. • Option B: The patient may need to walk around the same day of surgery, or the day after. The movement will help prevent blood clots. She may also be given exercises to do in bed. The patient should not get out of bed on her own until the healthcare provider says you can. She should talk to healthcare providers before she gets up the first time. They may need to help the patient stand up safely. • Option C: The patient should take deep breaths and cough 10 times each hour. This will decrease the risk of a lung infection. She should take a deep breath and hold it for as long as she can. Let the air out and then cough strongly. Deep breaths help open the airway. The patient may be given an incentive spirometer to help take deep breaths. • Option D: The patient may be taken to a recovery room, where she will stay until she is fully awake. Healthcare providers will watch closely for problems. She should not attempt to get out of bed until the healthcare provider says it is okay. When healthcare providers see that she is okay, she will be taken back to a hospital room. 10. Question You’re caring for a 28 y.o. woman with hepatitis B. She’s concerned about the duration of her recovery. Which response isn’t appropriate? • A. Encourage her to not worry about the future. • B. Encourage her to express her feelings about the illness. • C. Discuss the effects of hepatitis B on future health problems. • D. Provide avenues for financial counseling if she expresses the need. Correct Answer: A. Encourage her to not worry about the future. Telling her not to worry minimizes her feelings. Contract with the patient regarding time for listening. Encourage discussion of feelings/concerns. Establishing time enhances trusting relationships. Providing an opportunity to express feelings allows the patient to feel more in control of the situation. Verbalization can decrease anxiety and depression and facilitate positive coping behaviors. • Option B: The patient may need to express feelings about being ill, length and cost of illness, possibility of infecting others, and (in severe illness) fear of death. She may have concerns regarding the stigma of the disease. The recovery period may be prolonged (up to 6 mo), potentiating family and/or situational stress and necessitating the need for planning, support, and follow-up. • Option C: Avoid making moral judgments regarding lifestyle. The patient may already feel upset and angry and condemn self; judgments from others will further damage self-esteem. This can also start distrust issues with care workers. • Option D: Assess the effect of illness on economic factors of the patient and SO. Financial problems may exist because of loss of the patient’s role functioning in the family and prolonged recovery. Make appropriate referrals for help as needed: case manager, discharge planner, social services, and/or other community agencies. 11. Question Elmer is scheduled for a proctoscopy and has an I.V. The doctor wrote an order for 5mg of I.V. diazepam(Valium). Which order is correct regarding diazepam? • A. Give diazepam in the I.V. port closest to the vein. • B. Mix diazepam with 50 ml of dextrose 5% in water and give it over 15 minutes. • C. Give diazepam rapidly I.V. to prevent the bloodstream from diluting the drug mixture. • D. Question the order because I.V. administration of diazepam is contraindicated. Correct Answer: A. Give diazepam in the I.V. port closest to the vein. Diazepam is absorbed by the plastic I.V. tubing and should be given in the port closest to the vein. Diazepam is a benzodiazepine medication that is FDA approved for the management of anxiety disorders, short-term relief of anxiety symptoms, spasticity associated with upper motor neuron disorders, adjunct therapy for muscle spasms, preoperative anxiety relief, management of certain refractory epilepsy patients and adjunct in severe recurrent convulsive seizures, and an adjunct in status epilepticus. • Option B: Diazepam is available in multiple formulations, including oral tablets, intramuscular injections (IM), intravenous injection (IV), or rectal gel. Of note, oral tablets have a more reliable absorption and controlled release when compared to IM. • Option C: Diazepam is highly lipophilic. While there is a moderately quick onset of action, the drug quickly redistributes. Once in the body, diazepam is mostly broken down by the CYP2C19 and CYP3A4 enzymes to several active metabolites, mainly desmethyldiazepam. Other minor active metabolites include oxazepam and temazepam. The average half-lives of oral diazepam and desmethyldiazepam are about 46 hours and 100 hours, respectively. • Option D: When administered intravenously, diazepam actS within 1 to 3 minutes, while oral dosing onset ranges between 15 to 60 minutes. Diazepam is long-lasting with a duration of action of more than 12 hours. 12. Question Annabelle is being discharged with a colostomy, and you’re teaching her about colostomy care. Which statement correctly describes a healthy stoma? • A. “At first, the stoma may bleed slightly when touched.” • B. “The stoma should appear dark and have a bluish hue.” • C. “A burning sensation under the stoma faceplate is normal.” • D. “The stoma should remain swollen away from the abdomen.” Correct Answer: A. “At first, the stoma may bleed slightly when touched.” For the first few days to a week, slight bleeding normally occurs when the stoma is touched because the surgical site is still new. She should report profuse bleeding immediately. A small amount of blood from the stoma itself is not unusual while it is healing. • Option B: A stoma should be a beefy red or pink color. The tissue that makes a stoma is the lining of the intestine and should be moist and shiny. It is very similar in appearance to the inside of the mouth along your cheek. • Option C: The skin may be tender initially during the healing process and may feel irritated by normal cleaning. The skin immediately surrounding the stoma and stoma can be irritated by the cleaning process. • Option D: A normal stoma in the days after surgery may be swollen and may also produce mucus. While the stoma itself should be moist, the skin around the stoma should be normal in appearance. 13. Question A patient who underwent abdominal surgery now has a gaping incision due to delayed wound healing. Which method is correct when you irrigate a gaping abdominal incision with sterile normal saline solution, using a piston syringe? • A. Rapidly instill a stream of irrigating solution into the wound. • B. Apply a wet-to-dry dressing to the wound after the irrigation. • C. Moisten the area around the wound with normal saline solution after the irrigation. • D. Irrigate continuously until the solution becomes clear or all of the solution is used. Correct Answer: D. Irrigate continuously until the solution becomes clear or all of the solution is used. To wash away tissue debris and drainage effectively, irrigate the wound until the solution becomes clear of all the solution is used. Irrigation helps the wound to heal properly from the inside out; it helps prevent surface healing over an abscess pocket or infected tract. Continue to irrigate the wound until you have administered the prescribed amount of solution or until the solution returned is clear. Note the amount of solution administered. Remove and discard the catheter and syringe in the appropriate container. • Option A: Gently instill a slow, steady stream of irrigating solution into the wound until the syringe empties. Make sure the solution flows from the clean tissue to the dirty area of the wound to prevent contamination of clean tissue by exudate. Be sure the solution reaches all areas of the wound. • Option B: Keep the patient positioned to allow further wound drainage into the basin. Cleanse the area around the wound to help prevent skin breakdown and infection. Gently pack the wound, if ordered, and/or apply dressing. • Option C: Observe for wound size including length, width, and depth; drainage characteristics including type, amount, color, and odor; wound bed tissue type/color including necrotic, slough, eschar, granulating, clean, non-granulating, epithelial; and symptoms of infection including redness, swelling, pain, discharge or increased temperature. 14. Question Hepatic encephalopathy develops when the blood level of which substance increases? • A. Ammonia • B. Amylase • C. Calcium • D. Potassium Correct Answer: A. Ammonia Ammonia levels increase d/t improper shunting of blood, causing ammonia to enter systemic circulation, which carries it to the brain. Under normal conditions, ammonia is produced by bacteria in the gastrointestinal tract (e.g., breakdown product of amines, amino acids, purines, and urea) followed by metabolism and clearance by the liver. In the case of cirrhosis or advanced liver dysfunction, however, there is either a decrease in the number of functioning hepatocytes, portosystemic shunting, or both, resulting in decreased ammonia clearance and hyperammonemia. • Option B: Amylase is indirectly affected in hepatic encephalopathy. Hepatic encephalopathy (HE) is a reversible syndrome observed in patients with advanced liver dysfunction. The syndrome is characterized by a spectrum of neuropsychiatric abnormalities resulting from the accumulation of neurotoxic substances in the bloodstream (and ultimately in the brain). • Option C: Elevated blood ammonia levels, not calcium levels, are often seen in patients with hepatic encephalopathy. It is more useful, however, to assess the clinical improvement or deterioration of a patient undergoing treatment rather than monitor serial arterial blood ammonia measurements. • Option D: Once ammonia crosses the blood-brain barrier, it has multiple neurotoxic effects. These include alterations in molecular transport (e.g., amino acids, electrolytes, water) in astrocytes and neurons, increased synthesis of glutamine from glutamate by astrocytes, inhibition of excitatory and inhibitory postsynaptic potential generation, impaired amino acid metabolism, and impaired energy utilization as a result of increased GABA activity. 15. Question Your patient recently had abdominal surgery and tells you that he feels a popping sensation in his incision during a coughing spell, followed by severe pain. You anticipate an evisceration. Which supplies should you take to his room? • A. A suture kit. • B. Sterile water and a suture kit. • C. Sterile water and sterile dressings. • D. Sterile saline solution and sterile dressings. Correct Answer: D. Sterile saline solution and sterile dressings. Saline solution is isotonic, or close to body fluids in content, and is used along with sterile dressings to cover an eviscerated wound and keep it moist. If the wound shows signs of evisceration, the wound can be covered with a sterile saline dressing until the herniating organs can be reduced back into the abdomen. • Option A: A suture kit would be needed later during closure of the wound. Dehiscence is a partial or total separation of previously approximated wound edges, due to a failure of proper wound healing. This scenario typically occurs 5 to 8 days following surgery when healing is still in the early stages. The causes of dehiscence are similar to the causes of poor wound healing and include ischemia, infection, increased abdominal pressure, diabetes, malnutrition, smoking, and obesity • Option B: When dehiscence is identified, it is crucial to determine the extent of wound failure. Superficial dehiscence can be managed with abdominal binders to reduce strain on the wound and prevent further dehiscence. The existing wound failure may be allowed to heal by secondary intention or can close secondarily. • Option C: Deep dehiscence of the underlying fascia is a surgical emergency and must be closed in the operating room, as this can lead to evisceration. Secondary closure is preferred to healing by secondary intention in patients with superficial dehiscence. Patients who underwent secondary closure experience a faster healing time and fewer postoperative visits than the healing by secondary intention group. 16. Question Findings during an endoscopic exam include a cobblestone appearance of the colon in your patient. The findings are characteristic of which disorder? • A. Ulcer • B. Crohn’s disease • C. Chronic gastritis • D. Ulcerative colitis Correct Answer: B. Crohn’s disease Crohn’s disease penetrates the mucosa of the colon through all layers and destroys the colon in patches, which creates a cobblestone appearance. As the inflammation progresses, non-caseating granulomas form involving all layers of the intestinal wall. It can develop into the classic cobblestone mucosal appearances and skip lesions along the length of the intestine sparing areas with normal mucosa. • Option A: In a gastric ulcer, on histopathology, one will see an ulcer base with clear margins that penetrate the muscularis propria and into the submucosa. Inflammatory debris on the epithelial surface is often present. In the submucosa, one will see fibrosis and thickened blood vessels. • Option C: H. pylori infection’s first appearance of gastritis tends to be antral. The inflammation, composing mainly of mononuclear inflammatory cells and plasma cells are superficial and mostly in the upper layers of the mucosa of the corpus (body of the stomach). The chronic inflammation of gastric mucosa is associated with neutrophilic inflammation; the effects are dependent on the cytotoxicity of the H. pylori strain. • Option D: Histologically, the mucosal layer of the colon in a patient with ulcerative colitis includes infiltrates of varying density and composition, depending on the stage of the disease. These infiltrates primarily consist of lymphocytes, plasma cells, and granulocytes, with the latter being more prominent during acute flares of the disease. 17. Question What information is correct about stomach cancer? • A. Stomach pain is often a late symptom. • B. Surgery is often a successful treatment. • C. Chemotherapy and radiation are often successful treatments. • D. The patient can survive for an extended time with TPN. Correct Answer: A. Stomach pain is often a late symptom. Stomach pain is often a late sign of stomach cancer; outcomes are particularly poor when cancer reaches that point. In the United States, most patients have symptoms of an advanced stage at the time of presentation. The most common presenting symptoms for gastric cancers are non-specific weight loss, persistent abdominal pain, dysphagia, hematemesis, anorexia, nausea, early satiety, and dyspepsia. • Option B: Surgery has minimal positive effects. Patients with localized, resectable gastric cancer have the best chance of long-term survival with surgery alone. The main goal of surgery is complete resection with adequate margins (more than 4 cm), and only 50% of patients will obtain R0. • Option C: Chemotherapy and radiation have minimal positive effects. Neoadjuvant chemotherapy has been shown to downstage primary tumors and regional lymph nodes to attempt higher long-term curative resections. Neoadjuvant therapy should be offered to patients at high risk of developing distant metastases (bulky T3/T4, perigastric nodes, linitis plastica, or positive peritoneal cytology), sparing unnecessary surgery in case an emerging metastasis appears. • Option D: TPN may enhance the growth of cancer. Total parenteral nutrition is known to be effective in cases of malnutrition in patients who do not have cancer. However, TPN has not been shown to positively affect the nutritional status in patients with cancer. This is due in part to the metabolic changes associated with cancer. 18. Question Dark, tarry stools indicate bleeding in which location of the GI tract? • A. Upper colon • B. Lower colon • C. Upper GI tract • D. Small intestine Correct Answer: C. Upper GI tract Melena is the passage of dark, tarry stools that contain a large amount of digested blood. It occurs with bleeding from the upper GI tract. The clinical presentation can vary but should be well-characterized. Hematemesis is the overt bleeding with vomiting of fresh blood or clots. Melena refers to dark and tarry-appearing stools with a distinctive smell. The term “coffee-grounds” describes gastric aspirate or vomitus that contains dark specks of old blood. • Option A: UGIB is described as blood loss from a gastrointestinal source above the ligament of Treitz. It can manifest as hematemesis, which can be bright red emesis or coffee-ground emesis, hematochezia, or melena. Patients may also present with symptoms secondary to blood loss, such as syncopal episodes, fatigue, and weakness. • Option B: Gastrointestinal bleeding can fall into two broad categories: upper and lower sources of bleeding. The anatomic landmark that separates upper and lower bleeds is the ligament of Treitz, also known as the suspensory ligament of the duodenum. This peritoneal structure suspends the duodenojejunal flexure from the retroperitoneum. • Option D: Bleeding that originates above the ligament of Treitz usually presents either as hematemesis or melena whereas bleeding that originates below most commonly presents as hematochezia. 19. Question A patient has an acute upper GI hemorrhage. Your interventions include: • A. Treating hypovolemia. • B. Treating hypervolemia. • C. Controlling the bleeding source. • D. Treating shock and diagnosing the bleeding source. Correct Answer: A. Treating hypovolemia. A patient with an acute upper GI hemorrhage must be treated for hypovolemic and hemorrhagic shock. Monitor patient’s vital signs, especially BP and HR. Look for signs of orthostatic hypotension. Hypotension and tachycardia are initial compensatory mechanisms usually noted with bleeding. Orthostasis (a drip of 20 mm Hg in systolic BP or 10 mm Hg in diastolic BP when changing from supine to sitting position) indicates reduced circulating fluids. • Option B: Educate the patient and family members about signs of bleeding that need to be reported to a health care provider. Early evaluation and treatment of bleeding by a health care provider reduce the risk for complications from blood loss. • Option C: Controlling the bleeding may require surgery or intensive medical treatment. Tell the family members to be active in decision-making about the treatment of the patient at risk for bleeding. Active participation encourages a fuller understanding of the rationale and compliance with the treatment. • Option D: Inform the patient to check the color and consistency of stools. Bright red blood in the stools is an indicator of lower gastrointestinal bleeding. A stool that has a dark greenish-black color and a tarry consistency is linked with upper gastrointestinal bleeding. 20. Question You promote hemodynamic stability in a patient with upper GI bleeding by: • A. Encouraging oral fluid intake. • B. Monitoring central venous pressure. • C. Monitoring laboratory test results and vital signs. • D. Giving blood, electrolyte, and fluid replacement. Correct Answer: D. Giving blood, electrolyte, and fluid replacement. To stabilize a patient with acute bleeding, NS or LR solution is given I.V. until BP rises and urine output returns to 30ml/hr. Two large-caliber (18-gauge or larger) peripheral I.V. catheters or a central venous catheter should be inserted. For patients who are hemodynamically unstable, two 16-gauge I.V. catheters should be inserted. • Option A: Nurses should expect to administer isotonic fluids, such as normal saline or lactated Ringer’s solution, as well as any necessary blood products. Coagulopathies should be corrected with fresh frozen plasma and vitamin K. If necessary, more rapid reversal of anticoagulation can be achieved via prothrombin complex concentrate infusions; this is the preferred approach for patients with serious or life-threatening bleeding. Platelets should be administered for patients with thrombocytopenia or a platelet count below 50,000/mcL (normal, 150,000 to 450,000/mcL). • Option B: Closely monitor the patient’s clinical status, including airway, vital signs, cardiac rhythm, urine output, and nasogastric output if a nasogastric tube is in place. Initial treatment goals are focused on airway maintenance and volume resuscitation. Endotracheal intubation should be considered for those with ongoing hematemesis or altered respiratory or mental status. • Option C: After initial fluid resuscitation, patients may require a blood transfusion, depending on their signs and symptoms and overall clinical presentation. A hemoglobin level maintained above 7 g/dL (normal, 13.5 to 17.5 g/dL in men) is recommended, but transfusions may be necessary for patients who are clinically unstable despite their hemoglobin levels. 21. Question You’re preparing a patient with a malignant tumor for colorectal surgery and subsequent colostomy. The patient tells you he’s anxious. What should your initial step be in working with this patient? • A. Determine what the patient already knows about colostomies. • B. Show the patient some pictures of colostomies. • C. Arrange for someone who has a colostomy to visit the patient. • D. Provide the patient with written material about colostomy care. Correct Answer: A. Determine what the patient already knows about colostomies. Initially, you should assess the patient’s knowledge about colostomies and how it will affect his lifestyle. Review anatomy, physiology, and implications of surgical intervention. Discuss future expectations, including anticipated changes in the character of effluent. Provides knowledge base from which the patient can make informed choices, and offers an opportunity to clarify misconceptions regarding an individual situation. • Option B: Include written, picture (photo, video, Internet) learning resources. This provides references for obtaining support, equipment, and additional information after discharge to support patient efforts for independence in self-care. • Option C: Ascertain whether support and counseling were initiated when the possibility and/or necessity of ostomy was first discussed. This provides information about the patient’s/SO’s level of knowledge and anxiety about an individual situation. • Option D: The patient may find it easier to accept or deal with an ostomy done to correct chronic or long-term disease than for traumatic injury, even if ostomy is only temporary. Also, patient who will be undergoing a second procedure (to convert ostomy to a continent or anal reservoir) may possibly encounter less severe self-image problems because body function eventually will be “more normal.” 22. Question Your patient, Christopher, has a diagnosis of ulcerative colitis and has severe abdominal pain aggravated by movement, rebound tenderness, fever, nausea, and decreased urine output. This may indicate which complication? • A. Fistula • B. Bowel perforation • C. Bowel obstruction • D. Abscess Correct Answer: B. Bowel perforation An inflammatory condition that affects the surface of the colon, ulcerative colitis causes friability and erosions with bleeding. Patients with ulcerative colitis are at increased risk for bowel perforation, toxic megacolon, hemorrhage, cancer, and other anorectal and systemic complications. Colonic perforations are usually a complication of a toxic megacolon. However, perforation can also present in severe ulcerative colitis even in the absence of toxic megacolon. Most perforations occur in the left colon, commonly in the sigmoid colon. • Option A: Fistulas can occur anywhere in the bowel. The longer the client has Crohn’s, the more likely he is to develop a fistula. In ulcerative colitis the inflammation doesn’t spread through the full thickness of the bowel wall, so fistulas are less likely to form. The symptoms the client experiences depend on where the fistula is. • Option C: Crohn’s disease affects the entire thickness of the bowel wall. This makes strictures more common in people who have ulcerative colitis, which typically affects only the inner lining of the bowel. Bowel obstructions with strictures may either be temporary or permanent. • Option D: The typical histological (microscopic) lesion of ulcerative colitis is the crypt abscess, in which the epithelium of the crypt breaks down and the lumen fills with polymorphonuclear cells. The lamina propria is infiltrated with leukocytes. 23. Question A patient has a severe exacerbation of ulcerative colitis. Long-term medications will probably include: • A. Antacids • B. Antibiotics • C. Corticosteroids • D. Histamine2-receptor blockers Correct Answer: C. Corticosteroids Medications to control inflammation such as corticosteroids are used for long-term treatment. First-line treatment is sulfasalazine and 5-aminosalicylates, given orally or rectally, which have a remission rate of about 50%. Glucocorticoids, orally or rectally, can be added for those who fail to achieve remission within two weeks. Except for glucocorticoids, all of these medications can be used in the maintenance of remission. • Option A: Antacids are a group of drugs that have been on the market for many years. They were initially first-line defense against peptic ulcer disease; however, the discovery of proton pump inhibitors revolutionized the treatment of peptic ulcer disease. Currently, antacid use is restricted to the relief of mild intermittent gastroesophageal reflux disease (GERD) associated with heartburn. • Option B: Antibiotic therapy is often initiated before an exact infectious disease diagnosis is made and microbiological results are available. Antibiotics used in this manner are referred to as empiric therapy. This approach attempts to cover all potential pathogens. When microbiology tests result and antibiotic susceptibilities are known, definitive antibiotic therapy can then be tailored to the specific infection etiology. • Option D: H2 receptor blockers, or H2 receptor antagonists (H2RAs), are a class of gastric acid-suppressing agents frequently used in various gastric conditions. They are FDA-approved for short-term use in treating uncomplicated gastroesophageal reflux disease (GERD), gastric or duodenal ulcers, gastric hypersecretion, and mild to infrequent heartburn or indigestion. 24. Question The student nurse is teaching the family of a patient with liver failure. You instruct them to limit which foods in the patient’s diet? • A. Meats and beans • B. Butter and gravies • C. Potatoes and pasta • D. Cakes and pastries Correct Answer: A. Meats and beans Meats and beans are high-protein foods. In liver failure, the liver is unable to metabolize protein adequately, causing protein by-products to build up in the body rather than be excreted. Have about 1.2 to 1.5 grams of protein per kilogram of body weight. This means that a 154-pound (70-kilogram) man should eat 84 to 105 grams of protein per day. Look for non-meat protein sources such as beans, tofu, and dairy products when you can. • Option B: Eat a moderate intake of fat, as prescribed by the provider. The increased carbohydrates and fat help prevent protein breakdown in the liver. Eat fruits and vegetables and lean protein such as legumes, poultry, and fish. Avoid uncooked shellfish. • Option C: Eat large amounts of carbohydrate foods. Carbohydrates should be the major source of calories in this diet. Increase the intake of carbohydrates to be in proportion with the amount of protein the client eats. • Option D: Liver disease can affect the absorption of food and the production of proteins and vitamins. Therefore, diet may influence the weight, appetite, and the amounts of vitamins in the body. Do not limit protein too much, because it can result in a lack of certain amino acids. 25. Question An intubated patient is receiving continuous enteral feedings through a Salem pump tube at a rate of 60ml/hr. Gastric residuals have been 30-40ml when monitored Q4H. You check the gastric residual and aspirate 220ml. What is your first response to this finding? • A. Notify the doctor immediately. • B. Stop the feeding, and clamp the NG tube. • C. Discard the 220ml and clamp the NG tube. • D. Give a prescribed GI stimulant such as metoclopramide (Reglan). Correct Answer: B. Stop the feeding, and clamp the NG tube. A gastric residual greater than 2 hours worth of feeding or 100-150ml is considered too high. The feeding should be stopped; the NG tube clamped, and then allowed time for the stomach to empty before additional feeding is added. Gastric residual volume is the amount of liquid drained from a stomach following administration of enteral feed; this liquid consists mainly of infused nutritional formula or water, and secreted GI juice. Gastric residual volume is measured either by aspiration using a syringe, or by gravity drainage to a reservoir. • Option A: It is unnecessary to notify the physician immediately. Monitoring GRV involves obtaining frequent GRV measurements and employing appropriate interventions in patients with large GRVs. Gastric residual volume monitoring (monitoring of residual volume of the enteral nutrients including digestive juices) is an essential component of EN patient care and aids in preventing complications due to EN. • Option C: Administering additional enteral nutrients in patients with increased GRVs may cause aspiration and an increase in intra?abdominal pressure, which increases the risk of respiratory and circulatory failure, and intestinal necrosis. For this reason, it is particularly important to monitor GRV in the early stages of administration of enteral nutrition, especially in critically ill patients. • Option D: Frequency of GRV measurement (e.g. every six hours) and the intervention strategy for large GRVs (e.g. if GRV is above 500 mL, hold feeding for two hours and re?check GRV) is usually decided as per institution?specific protocols and needs of the inpatient population. 26. Question Your patient with peritonitis is NPO and complaining of thirst. What is your priority? • A. Increase the I.V. infusion rate. • B. Use diversion activities. • C. Provide frequent mouth care. • D. Give ice chips every 15 minutes. Correct Answer: C. Provide frequent mouth care. Frequent mouth care helps relieve dry mouth. Maintain NPO with nasogastric or intestinal aspiration. This reduces hyperactivity of bowel and diarrhea losses. Observe skin or mucous membrane dryness, turgor. Note peripheral and sacral edema. Hypovolemia, fluid shifts, and nutritional deficits contribute to poor skin turgor, taut edematous tissues. • Option A: Administer plasma or blood, fluids, electrolytes, diuretics as indicated. Replenishes circulating volume and electrolyte balance. Colloids (plasma, blood) help move water back into the intravascular compartment by increasing the osmotic pressure gradient. Diuretics may be used to assist in the excretion of toxins and to enhance renal function. • Option B: Change position frequently, provide frequent skincare, and maintain dry or wrinkle-free bedding. Edematous tissue with compromised circulation is prone to breakdown. • Option D: Eliminate noxious sights and smells from the environment. Limit intake of ice chips. This reduces gastric stimulation and vomiting response. Excessive use of ice chips during gastric aspiration can increase gastric washout of electrolytes. 27. Question Kevin has a history of peptic ulcer disease and vomits coffee-ground emesis. What does this indicate? • A. He has fresh, active upper GI bleeding. • B. He needs immediate saline gastric lavage. • C. His gastric bleeding occurred 2 hours earlier. • D. He needs a transfusion of packed RBCs. Correct Answer: C. His gastric bleeding occurred 2 hours earlier. Coffee-ground emesis occurs when there is upper GI bleeding that has undergone gastric digestion. For blood to appear as coffee-ground emesis, it would have to be digested for approximately 2 hours. The term “coffee-grounds” describes gastric aspirate or vomitus that contains dark specks of old blood. UGIB is classified as any blood loss from a gastrointestinal source above the ligament of Treitz. • Option A: The clinical presentation can vary but should be well-characterized. Hematemesis is the overt bleeding with vomiting of fresh blood or clots. Patients may also present with syncope or orthostatic hypotension if bleeding is severe enough to cause hemodynamic instability. • Option B: Patients must have a minimum of two large-bore peripheral access catheters (at least 18-gauge). Intravenous fluids should be administered to maintain adequate blood pressure and hemodynamic stability. If patients are not able to protect their airways or have ongoing severe hematemesis, elective endotracheal intubation is advised. • Option D: Blood transfusions should be given to target a hematocrit above 20%, with a hematocrit above 30% targeted in high-risk patients, such as the elderly and patients with coronary artery disease. There is no evidence that higher targets for hematocrit goals should be sought as that higher targets can even be deleterious. 28. Question A 53 y.o. patient has undergone a partial gastrectomy for adenocarcinoma of the stomach. An NG tube is in place and is connected to low continuous suction. During the immediate postoperative period, you expect the gastric secretions to be which color? • A. Brown • B. Clear • C. Red • D. Yellow Correct Answer: C. Red Normally, drainage is bloody for the first 24 hours after a partial gastrectomy; then it changes to brown-tinged and then to yellow or clear. Drainage will be bloody for the first 12 hours, and then should clear and turn greenish. Continued or recurrent bleeding suggests complications. A decline in output may reflect the return of GI function. • Option A: This tube will be set to suction and will drain out brownish-colored stomach acid. When it runs from brown to light green to clear, this is an indication that things are moving through the stomach and feedings may be possible. • Option B: Gastric aspirate is usually cloudy and green, tan or off-white, or brown. Intestinal aspirate is generally clear and yellow to bile-colored. Pleural fluid is pale yellow and serous; tracheobronchial secretions are usually tan or off-white mucus. • Option D: Normal color of gastric drainage is light yellow to green in color due to the presence of bile. Bloody drainage may be expected after gastric surgery but must be monitored closely. The presence of coffee-ground type drainage may indicate bleeding. 29. Question Your patient has a retractable gastric peptic ulcer and has had a gastric vagotomy. Which factor increases as a result of vagotomy? • A. Peristalsis • B. Gastric acidity • C. Gastric motility • D. Gastric pH Correct Answer: D. Gastric pH If the vagus nerve is cut as it enters the stomach, gastric acid secretion is decreased, but intestinal motility is also decreased and gastric emptying is delayed. Because gastric acids are decreased, gastric pH increases. The postoperative complications of truncal vagotomy are well documented. Resection of the vagal nerve trunks above the celiac and hepatic branches (differentiates TV versus SV) leads to parasympathetic denervation of the pylorus, liver, biliary tree, pancreas, and small and large intestines. • Option A: The stomach loses the vagally mediated receptive relaxation. This leads to an increased intragastric pressure causing an increased emptying of liquids. The pylorus does not relax effectively, and a decrease in solid food emptying is seen. • Option B: Gastrin is secreted by the G cells that are mainly located in the stomach antrum and pylorus. Acetylcholine is released in response to parasympathetic stimulation, which travels in the fibers of the vagus nerves. Histamine is released by the enterochromaffin-like cells. • Option C: Gastric phase begins once food enters the stomach. It is stimulated by proximal stomach distension (vagally mediated). It is absent in patients with a vagotomy. The gastric phase is stimulated by amino acids and peptides, leading to G cell activation. It accounts for 60% of total acid production. 30. Question Christina is receiving an enteral feeding that requires a concentration of 80 ml of supplement mixed with 20 ml of water. How much water do you mix with an 8 oz (240ml) can of feeding? • A. 60 ml • B. 70 ml • C. 80 ml • D. 90 ml Correct Answer: A. 60 ml Dosage problem. It’s 80/20 = 240/X. X=60. There are many different formulas that are used for enteral nutrition, and each formula is specific to the medical condition. For example, there are formulas for relatively healthy people, and those with cancer, diabetes, and kidney or liver disease, among other medical conditions. Most formulas will provide between 1.0-2.0 calories per mL of formula. • Option B: On average, enteral formulas deliver between 1.0-2.0 calories/mL of formula. To calculate how much formula is needed, divide the total calorie needs by the amount of calories per mL of formula. The total calories a person needs over a 24-hr period is calculated by multiplying BMR by the activity factor. The activity factor is a number used to represent how many calories a person burns through physical activity. • Option C: Enteral nutrition involves supplying nutrients directly into the stomach or intestines (the word ‘enteral’ comes from the word ‘entrails’, which means ‘intestines’). Enteral nutrition is often referred to as ‘tube feeding’ because a tube is used to supply a liquid formula directly into the GI tract. This liquid formula contains calories, fats, vitamins, minerals, and other nutrients needed for proper health and survival. • Option D: Enteral formulas are composed of carbohydrates, fats, proteins, micronutrients, and free water. The majority of the formulation (60-85%) is free water and can be easily calculated. 31. Question Which stoma would you expect a malodorous, enzyme-rich, caustic liquid output that is yellow, green, or brown? • A. Ileostomy • B. Ascending colostomy • C. Transverse colostomy • D. Descending colostomy Correct Answer: A. Ileostomy The output from an Ileostomy is described. The consistency of the ileostomy output will be liquid to pasty, depending on one’s diet, medications, and other factors. Because the output is constant, the pouch will need to be emptied 5-8 times a day. Average ileostomy output ranges from 800 – 1,200 milliliters (mL) or 3 – 5 cups per day. Right after surgery, output may be watery. During the first few weeks after surgery, the output should thicken to the consistency of applesauce. • Option B: Ascending colostomy is made from the ascending part of the colon. The ascending colostomy is usually located in the low to the middle right side of the abdomen. The output is often liquid to semiliquid, and gas is common. • Option C: Transverse colostomy is made from the transverse part of the colon. The transverse colostomy is usually located in the center of the abdomen above the navel. The output often is liquid to pasty, and gas is common. • Option D: Descending colostomy is made from the descending part of the colon. The descending colostomy is typically located on the lower left-hand side of the abdomen. The output may be pasty to a formed consistency, and gas is common. 32. Question George has a T tube in place after gallbladder surgery. Before discharge, what information or instructions should be given regarding the T tube drainage? • A. “If there is any drainage, notify the surgeon immediately.” • B. “The drainage will decrease daily until the bile duct heals.” • C. “First, the drainage is dark green; then it becomes dark yellow.” • D. “If the drainage stops, milk the tube toward the puncture wound.” Correct Answer: B. “The drainage will decrease daily until the bile duct heals.” As healing occurs from the bile duct, bile drains from the tube; the amount of bile should decrease. Teach the patient to expect dark green drainage and to notify the doctor if drainage stops. Monitor intake and output (I&O) carefully, measure liquid stool. Weigh regularly. This provides direct indicators of fluid balance. Greatest fluid losses occur with an ileostomy, but they generally do not exceed 500–800 mL/day. • Option A: Monitor vital signs, noting postural hypotension, tachycardia. Evaluate skin turgor, capillary refill, and mucous membranes. Reflects hydration status and/or the possible need for increased fluid replacement. • Option C: Recommend foods used to manage constipation (bran, celery, raw fruits), and discuss the importance of increased fluid intake. Proper management can prevent or minimize problems of constipation. • Option D: Irrigations may be done on a daily basis if appropriate, although there are differing views on this practice. Many believe cleaning the bowel on a regular basis is helpful. Others believe that this interferes with normal functioning. 33. Question Your patient Maria takes NSAIDS for her degenerative joint disease, and has developed peptic ulcer disease. Which drug is useful in preventing NSAID-induced peptic ulcer disease? • A. calcium carbonate (Tums) • B. famotidine (Pepcid) • C. misoprostol (Cytotec) • D. sucralfate (Carafate) Correct Answer: C. misoprostol (Cytotec) Misoprostol restores prostaglandins that protect the stomach from NSAIDS, which diminish the prostaglandins. Currently, misoprostol is FDA-approved only for the prevention and treatment of NSAID-induced gastric ulcers in patients taking NSAIDs and at high risk for ulceration. It has an indication (but not FDA approved) in the short-term treatment of active duodenal or gastric ulcers with other etiologies. • Option A: Calcium carbonate is an inorganic salt primarily used in the management and treatment of low calcium conditions, GERD, CKD, and a variety of other indicated conditions. It is classified as a calcium supplement, antacid, and as a phosphate binder. • Option B: Famotidine is a competitive histamine H-receptor antagonist (H2RA) that binds to the H-receptors located on the basolateral membrane of the parietal cell in the stomach, effectively blocking histamine actions. Its pharmacologic activity results in the inhibition of gastric secretion by suppressing acid concentration and volume of gastric secretion. • Option D: Sucralfate is a medication used to treat duodenal ulcers, epithelial wounds, chemotherapy-induced mucositis, radiation proctitis, ulcers in Behcet disease, and burn wounds. Sucralfate exhibits its action by forming a protective layer, increasing bicarbonate production, exhibiting anti-peptic effects, promoting tissue growth, regeneration, and repair. 34. Question The student nurse is participating in a colorectal cancer screening program. Which patient has the fewest risk factors for colon cancer? • A. Janice, a 45 y.o. with a 25-year history of ulcerative colitis. • B. George, a 50 y.o. whose father died of colon cancer. • C. Herman, a 60 y.o. who follows a low-fat, high-fiber diet. • D. Sissy, a 72 y.o. with a history of breast cancer. Correct Answer: C. Herman, a 60 y.o. who follows a low-fat, high-fiber diet. Large population studies with variable strength evidence have found CRC protective factors such as physical activity, diet (fruits and vegetables, fiber, resistant starch, fish), vitamin supplements (folate, folic acid, pyridoxine B6, calcium, vitamin D, magnesium), garlic and coffee, and drugs [aspirin, non-steroidal anti-inflammatory drugs (NSAIDs), hormonal replacement therapy in postmenopausal, statins, bisphosphonate and angiotensin inhibitors]. • Option A: Inflammatory bowel disease (IBD), mainly ulcerative colitis, has a well-known association with Cca, with an estimated incidence 0.5% per year between 10 and 20 years after the time of IBD diagnosis and 1% per year after that reaching a 30% risk probability by the fourth decade of patients with pancolitis. • Option B: Personal or family history of CRC, adenomatous polyps, and polyps with villous or tubulovillous dysplasia indicate a high risk for synchronous and metachronous CRC primary cancer up to 3% to 5% at 5 years or even longer after resection requiring a closer screening interval. • Option D: Colon cancer (Cca) could present as sporadic (70%), familial clustering (20%), and inherited syndromes (10%). Sporadic Cca average age diagnosis is older than 50 years and mostly linked to environmental factors, different from a minority of patients with a true inherited pattern that carries a higher risk at a younger age (younger than 50 years), and the remaining 20% are familial clustering in the absence of identifiable inherited syndrome. 35. Question Your patient, post-op drainage of a pelvic abscess secondary to diverticulitis, begins to cough violently after drinking water. His wound has ruptured and a small segment of the bowel is protruding. What’s your priority? • A. Ask the patient what happened, call the doctor, and cover the area with a water-soaked bed sheet. • B. Obtain vital signs, call the doctor, and obtain emergency orders. • C. Have a CAN hold the wound together while you obtain vital signs, call the doctor and flex the patient’s knees. • D. Have the doctor called while you remain with the patient, flex the patient’s knees, and cover the wound with sterile towels soaked in sterile saline solution. Correct Answer: D. Have the doctor called while you remain with the patient, flex the patient’s knees, and cover the wound with sterile towels soaked in sterile saline solution. Call for help but stay with the patient. Tell the person who responds to notify the surgeon immediately. Lower the bed until it is flat or no steeper than 20 degrees. Have the patient bend his knees to reduce abdominal muscle tension. Soak sterile towels with sterile saline or use pre moistened sterile dressings. • Option A: Using a water-soaked bed sheet to cover the area may lead to severe infection. Preventive measures to avoid wound dehiscence and wound evisceration include client coaching and teaching the client how to splint their incisional area when coughing, sneezing, vomiting and when doing planned, routine coughing and deep breathing exercises postoperatively. • Option B: In some situations, a surgical incision may open during the recovery process, allowing organs to be visible or even spill out of the body. This is obviously a serious medical condition that should be treated as soon as possible. Vital signs may be taken after the surgeon has arrived or the patient’s wound has been securely covered. • Option C: It is not advisable to touch an evisceration. Covering the area with sterile, saline-soaked dressings could prevent an infection. Dehiscence and evisceration can be a life-threatening emergency; do not leave the client immediately call for help and, using a clean, sterile towel or sterile saline dampened dressing, cover the wound. Under no circumstance should reinserting the organs be attempted. Maintain light pressure on the wound and monitor the client for shock until help arrives. [Show More]
Last updated: 1 year ago
Preview 1 out of 37 pages
Reviews( 0 )
Document information
Connected school, study & course
About the document
Uploaded On
Jul 08, 2021
Number of pages
37
Written in
Additional information
This document has been written for:
Uploaded
Jul 08, 2021
Downloads
0
Views
59