*NURSING > EXAM > Fundamentals Final Reviewer, Fundamentals Final Reviewer Test bank - Questions and Answers (2021/202 (All)
Fundamentals Final Reviewer, Fundamentals Final Reviewer Test bank - Questions and Answers (2021/2022)
Document Content and Description Below
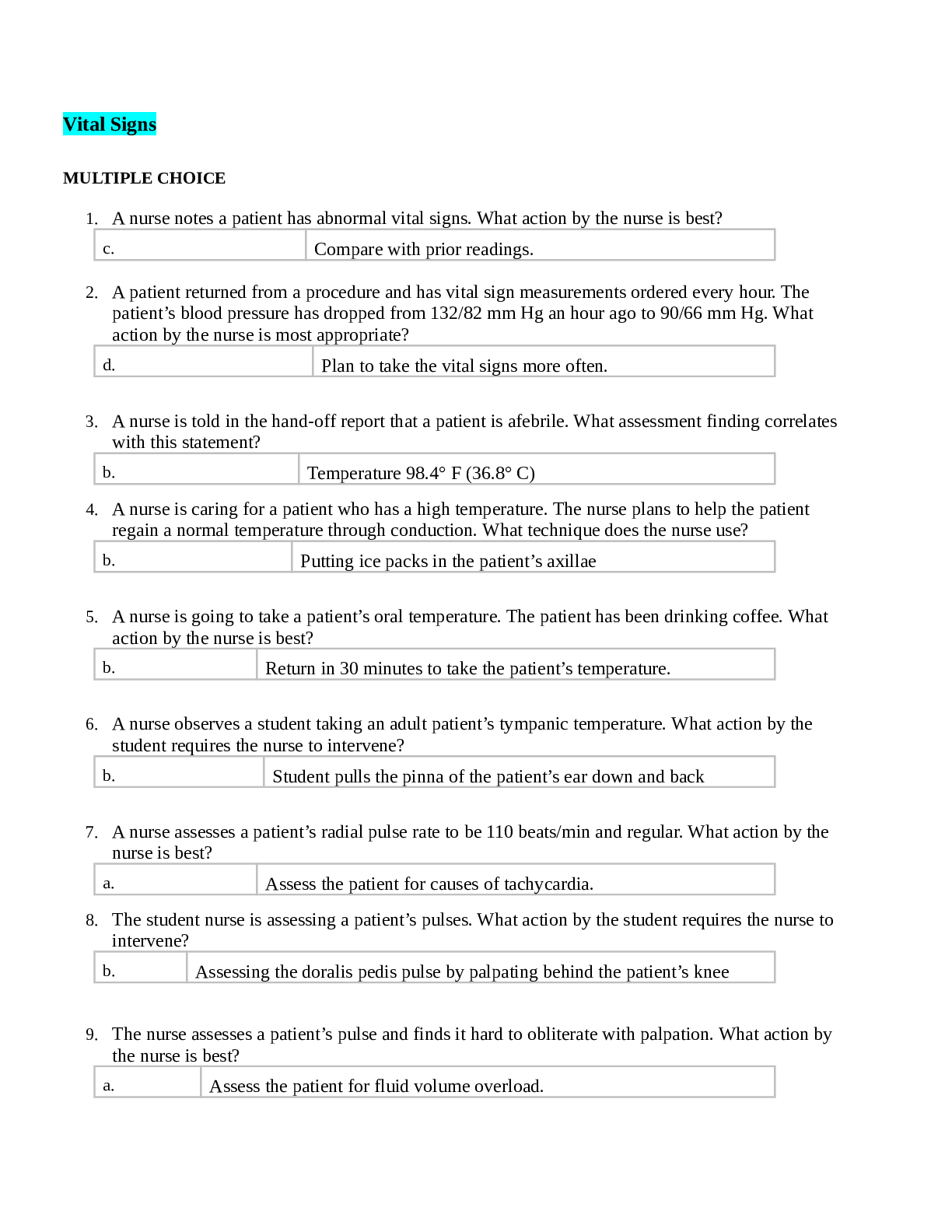
Fundamentals Final Reviewer Test bank - Questions and Answers Vital Signs MULTIPLE CHOICE 1. A nurse notes a patient has abnormal vital signs. What action by the nurse is best? 2. A patien... t returned from a procedure and has vital sign measurements ordered every hour. The patient’s blood pressure has dropped from 132/82 mm Hg an hour ago to 90/66 mm Hg. What action by the nurse is most appropriate? 3. A nurse is told in the hand-off report that a patient is afebrile. What assessment finding correlates with this statement? 4. A nurse is caring for a patient who has a high temperature. The nurse plans to help the patient regain a normal temperature through conduction. What technique does the nurse use? 5. A nurse is going to take a patient’s oral temperature. The patient has been drinking coffee. What action by the nurse is best? 6. A nurse observes a student taking an adult patient’s tympanic temperature. What action by the student requires the nurse to intervene? 7. A nurse assesses a patient’s radial pulse rate to be 110 beats/min and regular. What action by the nurse is best? 8. The student nurse is assessing a patient’s pulses. What action by the student requires the nurse to intervene? 9. The nurse assesses a patient’s pulse and finds it hard to obliterate with palpation. What action by the nurse is best? 10. The nursing faculty member is observing a student taking a patient’s carotid pulse. What action by the student requires intervention by the faculty member? 11. A nurse is caring for a patient who has orthopnea. What action by the nurse is most appropriate? 12. The nurse has applied a pulse oximeter to the finger of a patient who is hypothermic. The pulse oximeter does not provide a good reading. What action by the nurse is best? 13. A patient’s blood pressure is 142/76 mm Hg. What does the nurse chart as the pulse pressure? 14. A nurse performs orthostatic blood pressure readings on a patient with the following results: lying 148/76 mm Hg, standing 110/60 mm Hg. What action by the nurse is best? 15. The nurse is caring for a woman who had a right-sided mastectomy 2 years ago. What action by the nurse is most appropriate? 16. A nurse works on a postoperative care unit and sees many patients who have orthopedic surgery. One patient complains of significantly more pain than the other postoperative patients usually do. What action by the nurse is best? 17. The nurse receives a handoff report on four patients. Which patient should the nurse assess first? 18. A nursing student is caring for a patient with metabolic acidosis. The student asks the registered nurse why the patient’s respiratory rate is so high. What response by the nurse is best? 1. The nursing student learns that the purpose of measuring vital signs includes which rationale? (Select all that apply.) 2. The nurse is delegating taking vital signs to an unlicensed assistive personnel (UAP). What instructions does the nurse provide the UAP? (Select all that apply.) 3. The nurse understands that which factors can increase blood pressure? (Select all that apply.) 4. The nurse assessing respirations understands that problems in what organs can directly affect the process of respiration? (Select all that apply.) 5. A nurse is teaching a patient and the patient’s family about self-care measures for hypertension. Which topics does the nurse include? (Select all that apply.) 6. Which parameters does the nurse include when assessing pain? (Select all that apply.) 7. A nurse is caring for an unconscious patient. What objective assessments does the nurse use to help evaluate pain in this patient? (Select all that apply.) Health History and Physical Assessment 1. A nurse is conducting a physical assessment in a clinic with a partly undressed patient. What action by the nurse is most appropriate? 2. A patient wishes to review his medical record. What response by the nurse is best? 3. A clinic nurse is examining an older, confused patient on an examination table and realizes a piece of needed equipment was left outside in the hall. What action by the nurse is best? 4.A student nurse is preparing to auscultate a patient’s lungs. What action by the student leads the instructor to intervene? 5. The nurse is assessing a patient’s alcohol intake. What question is most appropriate? 6. The nurse is planning to educate four patients on preventing skin cancer and early warning signs. Which patient is the priority for this education? 7. A nurse has assessed a patient’s capillary refill, which was 5 seconds. What action by the nurse is most appropriate? 8. The student nurse asks if it matters whether a healthy eye or a diseased eye should be examined first. What response by the faculty is best? 9. A nurse observes a patient sitting up in bed, leaning forward with the arms braced against the over- the-bed table. What action by the nurse is best? and Maintenance NOT: Concepts: Gas Exchange 10. The nurse is assessing a patient whose chart indicates a Grade 3 heart murmur. What action is best in order to hear the murmur? 11. A nurse has conducted an Allen’s test on a patient and the result was 8 seconds. What action by the nurse is best? 12. A hospitalized patient complains of bilateral leg pain and asks the nurse to massage her legs. One calf is noticeably larger than the other and is warm and slightly reddened. What action by the nurse is best? 13. A nurse is told in handoff report that a patient opens eye spontaneously, is confused but able to answer questions, and demonstrates purposeful movement to painful stimuli. What does the nurse calculate the patient’s Glasgow Coma Scale to be? 14. A nurse is assessing a patient’s abdomen and hears bowel sounds every 20 to 25 seconds. What action by the nurse is best? 15. A nurse is assisting a patient who is having an examination of the female genitalia. What action by the nurse is best? 16. A nurse assesses a patient’s lungs and notes the presence of low-pitched snoring sounds that clear with coughing. What action by the nurse is best? 17. The nurse is assessing a patient’s cranial nerve III. What technique is best? 18. A nurse is assessing a patient’s cranial nerves and notes an abnormal response to testing cranial nerve VI. What action by the nurse is best? 19. The nurse reads in a chart that a patient has a paronychia. What assessment technique is most appropriate? 1. A new nurse is conducting a patient interview. What behaviors observed by the experienced nurse require education on this process? (Select all that apply.) 2. A nurse is conducting a physical examination using palpation. Which assessments might the nurse note? (Select all that apply.) 3. A nurse conducting the general survey of a patient includes which items? (Select all that apply.) 4. The nurse examining a patient’s skin correlates which conditions with which underlying pathology? (Select all that apply.) 5. A nurse is educating women on breast cancer risk reduction. What topics does the nurse include in the presentation? (Select all that apply.) 6. A nurse has finished examining a patient. What actions does the nurse take next? (Select all that apply.) Urinary Elimination 1. The nurse is caring for a patient who is recovering from septic shock. While in the ICU, the patient developed renal failure. Which type of renal failure did the patient most likely develop? a. Prerenal 2. The nurse is caring for a patient with diabetes insipidus. The patient has constant severe thirst, drinks fluids continuously, and voids 3 to 4 L of clear yellow urine daily. Which term will the nurse use in the record to describe this patient’s urinary output? 3. The nurse is caring for a patient who is experiencing stress incontinence. Which goal is the most important for this patient? 4. The nurse is caring for a postoperative patient whose urinary catheter was removed 8 hours previously. The patient has not been able to void since the catheter was removed and now reports suprapubic pain. What is the priority action of the nurse? 5. The nurse is caring for a patient who recently underwent ileal conduit surgery. Which nursing diagnosis is the highest priority for this patient? 6. The nurse is caring for a patient who reports an urgent need to urinate but is unable to pass more than a few drops of urine on the toilet. Which is the priority assessment to be performed by the nurse? 7. The nurse is caring for a seriously ill patient whose laboratory results show a serum creatinine level of 3.5 mg/dL and a serum BUN of 35 mg/dL. Which conclusion can the nurse draw from these test results? 8. The nurse is caring for a patient who has developed kidney failure. Which test finding leads the nurse to contact the nephrologist and arrange for emergency hemodialysis? 9. The nurse is caring for a patient who will undergo ultrasound testing of the bladder and kidneys the next morning. Which instruction will the nurse provide to the patient about the test? 10. The nurse is caring for a patient who has urinary retention resulting from benign prostatic hyperplasia (BPH). The patient requires catheterization in order to drain the urine from his bladder. Which action will the nurse take to facilitate this procedure? 11. The nurse is caring for an incontinent male patient who has a deep decubitus ulcer on his sacrum. Which intervention will best manage the patient’s urinary incontinence and facilitate healing of the ulcer? 12. The nurse is caring for a patient who has urinary frequency. Which nursing diagnosis is the highest priority for this patient? 13. The nurse is caring for a patient who has just had an intravenous pyelography (IVP) completed. Which assessment is the nurse’s highest priority after the patient returns from the test? 14. The nurse is caring for a patient with benign prostatic hypertrophy who states that he feels a constant urge to urinate but cannot pass more than 30 to 60 mL of urine into the toilet at a time. The nurse performs a bladder scan and finds that there are 1100 mL of urine in the patient’s bladder. What is the priority nursing diagnosis for this patient? 15. The nurse is caring for a patient who had prostate surgery the previous day. The patient has had significantly decreased urine output over the last shift despite ample oral and IV fluid intake. The patient’s urine from the indwelling catheter is cherry red with occasional small clots. What is the appropriate action of the nurse? 16. The nurse is caring for a patient with the nursing diagnosis of Urge urinary incontinence related to urinary tract infection. Which statement is appropriate for the “as evidenced by” portion of the patient’s diagnosis? 17. The nurse is caring for a patient with an indwelling urinary catheter caused by severe prostate enlargement. Which is the priority nursing diagnosis for this patient? 18. The preceptor is watching a nursing student care for a male patient who requires a condom catheter. Which action by the nursing student indicates that the procedure is performed correctly? 19. The nurse is caring for a patient with a history of type I diabetes. Which assessment finding indicates to the nurse that the patient may not be compliant with his diabetic treatment regimen? 20. The nurse is caring for a patient who is to undergo computed tomography (CT) of the kidneys and ureters. Which assessment finding by the nurse must be reported to the physician and radiologist before the patient has the procedure? 21. The nurse is caring for a patient with a history of incontinence and poor perineal hygiene practices. The patient has had four urinary tract infections in the past year. Which is the priority goal for the nursing diagnosis of Ineffective therapeutic regimen management? . 1. The nurse is caring for an elderly patient whose dementia has become worse over the last 24 hours. The nurse suspects that the patient may have developed a urinary tract infection and obtains a urine sample. Which assessment findings prompt the nurse to contact the physician to obtain an order for urine culture and sensitivity testing? (Select all that apply.) 2. The nurse is caring for a male patient who will be performing intermittent self-catheterization at home. Which actions by the patient indicate the need for additional teaching about this procedure? (Select all that apply.) 3. The nurse is working with a new nursing assistant who is providing care to patients with urinary difficulties. Which action by the nursing assistant indicates that additional teaching is required so that the assistant will learn to care for patients correctly? (Select all that apply.) the : Potential for Complications from Procedures NOT: Concepts: Elimination 4. The nurse is caring for a patient who is to complete a 24-hour urine collection to measure creatinine clearance. Which tasks related to this test may be delegated to the nursing assistant? (Select all that apply.) Bowel Elimination 1. The nurse is caring for a patient who periodically has small streaks of fresh red blood in his stool. The patient denies abdominal pain or loss of appetite. What is the most likely cause of this patient’s bleeding? 2. The nurse is caring for a patient who has diarrhea. What is the priority nursing diagnosis for this patient? 3. The nurse is caring for a patient who is prescribed diphenoxylate-atropine (Lomotil). Which assessment finding by the nurse indicates a need to contact the prescriber and question the order? 4. The nurse is caring for an immobile patient who has abdominal pain and frequent small, liquid stools. The patient vomited his breakfast and is still nauseated. Which action by the nurse is the highest priority? 5. The nurse is caring for a patient who is recovering from bowel surgery. Which assessment finding best indicates that the bowel is starting to resume function and the patient will be able to resume oral intake soon? 6. The nurse is caring for a patient who has an ileostomy. Which nursing diagnosis has the highest priority for the patient? 7. The nurse is caring for a patient who is taking narcotic pain medication after surgery. Which breakfast choices will help prevent constipation and promote return to regular bowel function? 8. The nurse is caring for a patient who has not had a bowel movement for 2 days. Which is the priority nursing intervention for this patient? 9. The nurse is caring for a patient who will be undergoing upper GI series testing the next day. Which instruction will the nurse provide to the patient about the upcoming exam? 10. The nurse is caring for a patient who will undergo colonoscopy testing. Which intervention will the nurse include in the patient’s plan of care for the day before the test? 11. The nurse is caring for a patient who is to have testing for fecal occult blood. What step will the nurse perform during this testing? 12. The nurse is caring for a patient who is to have a cleansing enema. Which assessment finding by the nurse indicates a need to contact the prescriber and question the order? 13. The nurse is caring for a postoperative patient who underwent bowel resection surgery that morning. The nurse assesses the patient’s abdomen and notes that there are hypoactive bowel sounds. The patient is resting quietly without nausea or vomiting. What is the appropriate action of the nurse? 14. The nurse is caring for a patient who is constipated and has not had a bowel movement for 3 days. The nurse performs a rectal examination and finds hard dry stool in the rectum. What is the best option to help the patient have a bowel movement? 15. The nurse is caring for a patient who has just completed 2 weeks of IV antibiotics for a severe infection. The patient now has frequent loose watery stools and a low-grade temperature. What is the most likely cause of the patient’s new symptoms? 16. The nurse is caring for a patient who takes laxatives and enemas regularly to ensure that he has a large daily bowel movement. The patient states that he feels constipated if he does not defecate every day. Which nursing diagnosis is most appropriate for this patient? 17. The nurse is caring for a patient who had a colonoscopy earlier that day. The patient states that he still feels very bloated after the procedure. What is the best action of the nurse? 18. The nurse is caring for a patient with a history of dementia who is incontinent of stool because she cannot communicate the need to defecate. What is the priority action of the nurse? 19. The nurse is caring for a patient who is recovering after hip surgery. The patient requires assistance to use the bathroom because no weight bearing is allowed on the right leg. Which goal is most important for the nurse to include for the diagnosis of toileting self-care deficit? 20. The nurse is caring for a patient who is recovering from gastroenteritis. The nurse teaches the patient about dietary recommendations as the digestive system recovers. Which menu selection by the patient indicates that additional teaching is needed? 21. The nurse is caring for a patient who has had a severe stroke and requires assistance to use the toilet. Which goal is the highest priority for this patient? 22. A student nurse is working with a preceptor to administer an enema to the patient. Which action by the student prompts intervention and redirection by the preceptor? 1. The nurse is caring for a postoperative patient who had a colostomy placed 2 days ago. The appliance needs to be changed for the first time. Which ostomy care actions may the nurse delegate to the nursing assistant? (Select all that apply.) 2. The nurse is caring for a patient who will be having a colonoscopy the following morning. Which items must be removed from the patient’s dinner tray since they are not allowed prior to the test? (Select all that apply.) Fluid, Electrolytes, and Acid-Base Balance 1. The nurse will be caring for a patient who is severely malnourished. Laboratory test results show that the patient’s albumin level is critically low. What assessment finding will the nurse expect to note when meeting with the patient? 2. The nurse is reviewing the patient’s laboratory results. Which result must be communicated to the physician immediately? 3. The nurse is caring for a patient who is at risk for fluid overload as a result of a history of congestive heart failure. Which intervention will the nurse teach the patient to perform at home to monitor fluid balance? 4. The nurse is caring for a patient who is admitted to the hospital with diabetic ketoacidosis. Which assessment finding indicates an attempt made by the patient’s body to correct the pH? 5. The nurse is caring for a patient who takes furosemide (Lasix) daily to treat congestive heart failure. The nurse will watch for which electrolyte imbalance that may occur as a result of this therapy? 6. The nurse is caring for a patient who was brought to the ER after overdosing on narcotic pain medication. The patient was found unresponsive with no respirations. Arterial blood gases were drawn shortly after the patient’s arrival to the hospital. Which results will the nurse expect to see? 7. The nurse is caring for a patient who is admitted to the hospital with dehydration and gastroenteritis. The patient attempted to walk to the bathroom and fainted right after getting out of bed. Which is the most likely cause of the patient’s collapse? 8. The nurse is caring for a patient whose ABG results reveal the following: pH 7.56, PaCO2 32 mm Hg, HCO3 42 mEq/L, PaO2 90 mm Hg. Which condition will the nurse expect to see in the patient’s chart as the underlying cause of these results? Potential: Laboratory Values 9. The nurse is caring for a patient who has a 1200 mL daily fluid restriction. The patient has consumed 250 mL with each of her three meals and had another 150 mL with her medications. The patient has received 150 mL of IV fluids during the day. How many mL of fluid may the patient still consume in order to stay within the prescribed fluid restriction? 10. The nurse is caring for a patient who has a history of congestive heart failure. The nurse includes the diagnosis fluid volume excess in the patient’s care plan. Which goal statement has the highest priority for the patient and nurse? 11. The nurse is caring for a patient with syndrome of inappropriate antidiuretic hormone secretion (SIADH) who has a serum sodium level of 118 mEq/dL and symptoms of fluid overload. Which IV fluid will the nurse expect to administer to this patient in order to correct the patient’s fluid imbalance? 12. The nurse is caring for a patient with congestive heart failure who requires intermittent IV bolus doses of furosemide (Lasix) for a few days to correct fluid volume overload. No continuous IV fluids are ordered. Which type of IV will the nurse insert in order to administer the patient’s medication? 13. The nurse is caring for a patient who has a central venous catheter (CVC). Which nursing intervention is the most important for the nurse to include in the patient’s plan of care? 14. The nurse is caring for a patient with a peripheral IV who tells the nurse that the IV site is painful and puffy. What is the nurse’s best action? 15. The nurse is caring for a patient who is to receive intermittent bolus doses of phenytoin (Dilantin) through the IV line. Which intervention has the highest priority when administering this medication? 16. The nurse is caring for a patient who is to receive a transfusion of packed red blood cells. The patient has a 22-gauge IV in his arm with 0.9% normal saline infusing. What intervention will the nurse perform before obtaining the packed red blood cells from the blood bank? 17. The nurse is caring for a patient who is receiving a blood transfusion. One hour into the transfusion, the patient’s blood pressure decreases significantly and the patient complains of a severe headache. What is the priority action of the nurse? 18. The nurse is caring for a patient who is very dehydrated. Which goal best indicates that the nursing diagnosis of Deficient fluid volume has been corrected and that the patient’s fluid balance has been restored? 19. The nurse is caring for a patient who is admitted with a serum sodium level of 120 mEq/L. Which is the most important intervention for the nurse to perform? 20. The nurse is caring for a patient who has a history of congestive heart failure and takes once- daily furosemide (Lasix) in order to prevent fluid overload and pulmonary edema. The patient tells the nurse that she has stopped taking the medication because she has to urinate frequently during the night. What is the nurse’s best response? 21. The nurse is caring for a patient with renal failure who has a serum potassium level of 7.1 mEq/L and serum magnesium level of 3.5 mEq/L. The nurse prepares to administer 10 units of insulin and an ampule of 50% dextrose to the patient. The patient asks why he will be receiving insulin when he is not diabetic. What is the nurse’s best answer? 22. The nurse is caring for a patient with a history of hyperparathyroidism who presents with a serum calcium level of 14.5 mg/dL. What is the highest priority nursing diagnosis for this patient? 23. The nurse is caring for a patient who has a serum magnesium level of 0.8 mEq/L. Which is the highest priority goal to include in the patient’s plan of care? 24. The nurse is caring for a hospitalized patient with hyperparathyroid disease and a serum calcium level of 14.2 mg/dL. What is the priority intervention of the nurse? 1. The nurse is caring for a patient who has B-positive blood. The patient is severely anemic and requires a blood transfusion. Which types of blood can the patient receive? (Select all that apply.) Oxygenation and Tissue Perfusion 1. The nurse finds the patient in cardiopulmonary arrest with no pulse or respirations. Which oxygen delivery device will the nurse use for this patient? 2. The nurse is caring for a patient who is slow to awaken following general anesthesia. The patient is breathing spontaneously but is minimally responsive and having difficulty maintaining a patent airway. Which intervention is the most appropriate for the patient to improve oxygenation? 3. The nurse is caring for a patient with a history of left-sided congestive heart failure who is acutely short of breath. The nurse hears fine crackles throughout both lung fields and notes that the patient’s pulse oximetry is only 88% on 4 L of oxygen. What is the priority intervention of the nurse? 4. The nurse is caring for a patient who has been intubated with an oral endotracheal tube for several weeks. The physicians predict that the patient will need to remain on a ventilator for at least several more weeks before he will be able to maintain his airway and breathe on his own. What procedure does the nurse anticipate will be planned for the patient to facilitate his recovery? 5. The nurse is caring for a patient with a chest tube who was transported to radiology for testing. When the patient returns to the nursing unit, the transporter shows the nurse the patient’s chest tube collection device, which was badly damaged after being caught in the elevator door. What is the priority action of the nurse? 6. The nurse is caring for a patient who is hospitalized for pneumonia. Which nursing diagnosis has the highest priority? 7. The nurse is caring for a patient who developed a pulmonary embolism after surgery. Which goal statement is the highest priority for the nurse to include in the patient’s care plan for the diagnosis Impaired gas exchange r/t impaired pulmonary blood flow from embolus? 8. The nurse is caring for a patient with severe COPD who is becoming increasingly confused and disoriented. What is the priority action of the nurse? 9. The nurse is caring for a patient who has been prescribed warfarin (Coumadin) therapy after being diagnosed with atrial fibrillation. The patient tells the nurse that he doesn’t want to take any more pills and asks what could happen if he doesn’t fill the prescription. What is the nurse’s best response? 10. The preceptor is working with a new nurse to provide care for a patient with a chest tube to relieve a pneumothorax. Which action by the new nurse indicates need for additional teaching about chest tube care? 11. The nurse is caring for a postoperative patient who has just been diagnosed with a deep vein thrombosis (DVT) in the right leg. Which focused assessment question has the highest priority for this patient? 12. Which of the following patients would benefit from postural drainage? 13. The nurse is caring for a patient who has a history of congestive heart failure with generalized pitting edema. Which of the following laboratory results will the nurse expect to find in the patient’s chart? 14. The nurse is caring for a patient with high cholesterol who has been prescribed atorvastatin (Lipitor). Which laboratory result indicates that the patient has been taking the medication as ordered and following the physician’s dietary recommendations? Potential: Laboratory Values NOT: Concepts: Nutrition 15. The nurse is caring for a patient who has just had a massive myocardial infarction. Which is the priority nursing diagnosis for this patient? 16. The nurse is caring for a patient who has presented to the ER with chest pain. Which diagnostic test will best indicate if there is significant blockage of certain important blood vessels that provide oxygen to the heart muscle? 17. The nurse hears a loud murmur when listening to the patient’s heart. Which diagnostic test will best display the condition of the valves and structures within the patient’s heart that could be causing the murmur? 18. The nurse is caring for a patient who will be returning to the nursing unit following a cardiac catheterization via the right femoral artery. Which assessment is the highest priority for the nurse to perform when the patient arrives on the unit? 19. The home care nurse is caring for a patient who has severe COPD and home oxygen therapy. The patient tells the nurse that she feels much better after increasing the oxygen flowmeter from 2 L to 5 L/min. The patient’s pulse oximetry is 98%. What is the priority action of the nurse? 1. The nurse is caring for a patient with advanced COPD who reports feeling short of breath. The nurse notes that the patient’s lung sounds are diminished bilaterally and the patient’s pulse oximetry is 91% on 2 L/min oxygen via nasal cannula. What actions will the nurse take to make the patient more comfortable? (Select all that apply.) 2. The nurse is performing a respiratory assessment on a patient. Which assessment findings indicate to the nurse that the patient has a history of long-standing chronic respiratory disease? (Select all that apply.) 3. The nurse notes the following findings when assessing a patient with COPD. Which require prompt nursing intervention? (Select all that apply.) 4. The nurse is working with a nursing assistant to care for a patient with a new tracheostomy. Which tasks may the nurse delegate to the assistant? (Select all that apply.) 5. The preceptor is working with a new nurse to provide care for a patient with a new tracheostomy. Which actions by the new nurse indicate need for additional teaching about the procedure? (Select all that apply.) 6. The preceptor is working with a new nurse to suction a patient through his new tracheostomy. Which actions by the new nurse indicate need for additional teaching about the procedure? (Select all that apply.) Hygiene and Personal Care 1. The nurse knows that which of the following statements is true regarding the importance of hygiene? 2. Excessively dry skin can lead to cracks and openings in the integumentary system. Based on this, what is the most applicable nursing diagnosis for a patient with excessively dry skin? 3. The nurse correctly identifies which patient as having the highest risk for injury related to temperature of water when bathing? MSC: NCLEX Client Needs Category: Physiological Integrity NOT: Concepts: Caregiving 4. Which tool is used to determine risk for impaired skin integrity? 5. The patient expresses a desire to learn methods to be independent regarding self-care. Based on this, the most appropriate nursing diagnosis would be: 6. The nurse is providing care to a post-stroke patient on the rehabilitation floor with a nursing diagnosis of hygiene self-care deficit. Which goal is most appropriate on day one? 7. The nurse is preparing to give a patient a complete bed bath. What area of the body should be bathed first? 8. The UAP asks why the arms are washed from distal to proximal. Which response by the nurse is appropriate? 9. The nurse has assisted the patient to wash his hands, face, axillae, and perineal area. What type of bath should the nurse chart? 10. The nurse is performing perineal care for the uncircumcised patient. Which of the following is true? 11. Which member of the collaborative team is most appropriate to cut the toenails of a diabetic patient? 12. The nurse knows that routine hygienic care does not include: 13. The nurse is caring for a patient with swallowing concerns and decreased level of consciousness. The nurse knows to put the patient in what position for oral care? 14. Regarding denture care, what action by the nurse is inappropriate? 15. What statement is true regarding oral care of patients on anticoagulants? 16. The nurse is assisting a patient to insert contacts and a contact is dropped. What action should occur next? 17. Which statement by the patient indicates a teaching need? 18. The nurse is asked to shave a patient that is taking Coumadin. What is the most appropriate action? 19. The nurse and UAP are making an occupied bed together. Which action by the nurse is incorrect? 1. The nurse knows that which areas are at increased risk of excoriation? (Select all that apply.) 2. The nurse is demonstrating cultural sensitivity in performing perineal care when he/she does the following: (Select all that apply.) 3. The nurse is assisting her patients with hygiene care. She knows that this includes the following: (Select all that apply.) ANS: A, B, C, D, E 4. The nurse is bathing a patient and notes reddened skin above the coccyx. Which action by the nurse is appropriate? (Select all that apply.) 5. Regarding perineal care, which nursing action is appropriate? (Select all that apply.) 6. The nurse should avoid soaking the feet of which patient population? (Select all that apply.) 7. The nurse notes that a trauma patient has multiple tangles in the hair. Which of the following actions taken by the nurse is appropriate? (Select all that apply.) Medication Administration 1. Which medication has the highest potential for abuse? 2. The nurse is caring for a patient who will give himself medication injections at home after discharge. How can the nurse best determine that the patient understands the technique and can administer the injections correctly? 3. The nurse is caring for a patient who is in agonizing pain. All of the following options are listed on the patient’s medication order sheet to relive pain. Which will provide the most rapid pain relief for the patient? 4. The nurse administers a medication to a patient. Shortly afterward, the patient develops an itchy rash all of his body and reports feeling very unwell. What is the priority action of the nurse? 5. Which of the following medication orders is to be administered PRN? 6. After administering an antibiotic to the patient, the patient complains of feeling very ill. The nurse notes that the patient is scratching and has hives. The patient soon starts having difficulty breathing and his blood pressure drops. What is the nurse’s assessment of the situation? red 7. The nurse makes a medication error. Which action will the nurse take first? 8. The nurse prepares to administer the following medication to the patient. Which instruction will the nurse be sure to give before the patient takes the medication? 9. The nurse begins a shift on a busy medical-surgical unit. The nurse will be caring for multiple patients. Which patient will the nurse assess first? 10. The nurse carefully reviews the patient’s medication list. Which observation about the list indicates the highest risk for serious drug-drug interactions? 11. The nurse is caring for a patient who is taking many prescription medications for various health problems. Which direction from the nurse will help the patient avoid dangerous drug interactions? 12. During discharge teaching, the nurse is to give the patient a signed, dated, and timed prescription from the physician for medications to be taken at home. Which prescription drug order needs to be corrected before it is given to the patient? 13. The nurse administers a medication to the patient. Which symptoms indicate that the patient is having an allergic reaction rather than a side effect? 14. The nurse suspects that the patient is experiencing a drug toxicity rather than a side effect. Which question will the nurse ask to help confirm this suspicion? 15. The nurse is caring for a patient who is receiving vancomycin (Vancocin) to treat a severe infection. The next vancomycin dose is due to be administered at 10:00 A.M. What time will the nurse draw the vancomycin serum trough level? 16. When administering phenytoin (Dilantin) through the patient’s IV line, the nurse carefully flushes the IV with normal saline before and afterward to avoid crystal formation of the medication that occurs when it mixes with dextrose in water (D5W) solution. Which type of drug interaction is the nurse being careful to avoid? 17. The nurse is noting an order for a medication to be given TID. Which times will the nurse plan to administer the medication to the patient? 18. The nurse is caring for a patient who was just made NPO. The nurse is to administer carvedilol (Coreg) 25 mg PO to the patient for control of high blood pressure. What is the best action of the nurse? 19. The nurse is to administer 1 mL of prochlorperazine (Compazine) 10 mg IM to an adult patient. Which syringe will the nurse select to administer the medication? 20. The nurse is to administer 15 mg of morphine liquid to the patient. How much morphine liquid will the nurse draw up to administer to the patient? 21. The nurse is caring for a patient with multiple chronic illnesses who is having difficulty remembering to take all of her many medications at the correct times. Which is the appropriate nursing diagnosis for this patient? 22. The nurse is caring for a patient who takes 6 tablets of methotrexate once every week on Fridays. How many mg of methotrexate does the patient take per dose? 23. The nurse is to administer 45 mg of phenobarbital to the patient. How many tablets will the patient receive? 1. The nurse is caring for a patient who is NPO with a new PEG (percutaneous endoscopic gastrostomy) tube. Which of the patient’s medications can the nurse administer through the tube? (Select all that apply.) 2. Which medications are to be administered via parenteral routes? (Select all that apply.) ANS: B, F Cognitive and Sensory Alterations 1. A nurse is caring for a patient with a stroke that has impacted her ability to see. Which area of the brain was likely impacted by the stroke that is responsible for visual function? 2. The family of a patient who was in a motor vehicle accident tells you he “just isn’t the same person before the crash.” You know this is likely because of the injury to what area of his brain? 3. The nurse is educating the family of a patient in the intensive care unit about the patient’s cognitive status, including her current problem of delirium. Which statement by the family indicates a need for further education? 4. The nurse is caring for a patient with depression. Which statement by the patient indicates a need for further education? 5. The nurse is caring for a patient who is complaining of tingling in her hands and fingers. The nurse knows this is a sign of what electrolyte imbalance? 6. The nurse is providing discharge instructions to an older adult who is being discharged with orthostatic hypotension. Which of the following responses by the patient indicates a need for further education? 7. The nurse is assessing the patient’s ability to hear. Which is the correct procedure for the doing this? 8. The nurse notices her 50-year-old patient is holding his lunch menu at arm’s length while trying to read his choices. This is an indication of: 9. The nurse is providing discharge education to her patient with diabetes regarding foot care. Which of the following statements by the patient indicates a need for further education? ] 10. An appropriate goal for a patient with the diagnosis of acute confusion is: NOT: Concepts: Cognitive and Sensory Perception 11. An appropriate goal for a patient with a diagnosis of social isolation is: 12. The nurse is educating the family to care for a patient at home with cognitive alterations. Which statement by the family indicates a need for further education? 13. The nurse is delegating care to an unlicensed assistive personnel (UAP) to a patient who has sensory overload. Which statement by the UAP indicates a need for further orientation? 14. The nurse is providing discharge instructions to a patient with visual alterations. Which statement by the patient indicates a need for further education? 1. The nurse is completing her assessment of an older adult and notices some cognitive impairment not normally associated with aging. Which of these alterations would prompt further follow-up? (Select all that apply.) 2. You are providing education to the family of a patient being discharged with dementia. Which statement by the family indicates a good level of understanding of dementia? (Select all that apply.) 3. The nurse is caring for a patient who suffered a stroke on the right side of the brain. The nurse is careful to implement what safety measures? (Select all that apply.) 4. The nurse is performing a health history to determine the patient’s cognitive status. Which questions will be best suited to elicit the information needed? (Select all that apply.) 5. The nurse is performing a health history to determine the patient’s sensory status. Which questions will be best suited to elicit the information needed? (Select all that apply.) 6. The nurse is caring for a diabetic patient who has had a long history of poor glucose control. For what complications is the patient at risk? (Select all that apply.) 7. The nurse is caring for a patient who is hospitalized with cognitive impairment. The following interventions will assist the patient in orientation: (Select all that apply.) 8. The nurse is caring for a patient with expressive aphasia. Which interventions will assist the nurse in communicating with the patient? (Select all that apply.) 9. The nurse is caring for a patient with receptive aphasia. Which interventions will assist the nurse in communicating with the patient? (Select all that apply.) 10. The nurse is preparing discharge instructions for a patient who has tactile alterations in his legs. Which instructions should be included? (Select all that apply.) 11. The nurse is preparing discharge instructions for a patient who has equilibrium alterations. Which instructions should be included? (Select all that apply.) Skin Integrity and Wound Care 1. The nurse knows the following wound would be classified as a closed wound: 2. The nurse is educating the patient about the signs and symptoms of a wound infection. Which statement indicates a need for further education? 3. The nurse knows the following types of wounds heal by tertiary intention: 4. The nurse is caring for a patient who is postoperative day one from an abdominal surgery. The patient complains of a “popping sensation” and a wetness in her dressing. The nurse immediately suspects: 5. The nurse is caring for a postoperative patient who has had abdominal surgery and whose wound has completely eviscerated when she walks into the room. In addition to notifying the physician, what should the nurse do? 6. The nurse knows the most appropriate goal for a patient with a stage III pressure ulcer who has a nursing diagnosis of Impaired skin integrity is: 7. The nurse is delegating care of a patient with a chronic nonsterile wound to a UAP. The delegation is inappropriate if: 8. The nurse is repositioning her patient in the side-lying position. To avoid putting the patient at risk for pressure ulcers, the HOB should be placed at: 9. The nurse knows that mechanical debridement involves all of the following except: 10. The nurse is explaining to the student nurse the purpose of occlusive dressings. Which statement by the student nurse indicates a lack of understanding? 11. The nurse knows that a hydrocolloid dressing is appropriate for the following type of wound: 12. The nurse is caring for a patient with a Penrose drain. She knows the patient will require the following care: 13. The nurse is educating the patient about the use of heat/cold therapy at home. The following statement by the patient indicates the need for further education? 14. The nurse knows to irrigate a deep wound with: 15. The nurse understands the rationale for drying a wound after irrigation is: 16. The nurse is performing a wet/damp to dry dressing change when the patient begins to complain of severe pain. What should the nurse do first? 17. The nurse knows an appropriate goal for a patient with a stage III pressure ulcer with the nursing diagnosis Impaired physical mobility is: 18. The nurse knows a stage III pressure ulcer is: 19. The nurse knows the layer that delivers the blood supply to the dermis, provides insulation, and has a cushioning effect is: 1. The nurse knows that the following factors contribute to the development of wounds and lead to delays in wound healing: (Select all that apply.) 2. The nurse knows that the cause of pressure ulcers includes the following factors: (Select all that apply.) 3. The nurse is performing a focused wound assessment on a patient. The following should be included in the documentation: (Select all that apply.) 4. The nurse is using the Braden scale to assess the patient’s risk for a pressure ulcer. Which risk categories are associated with the Braden scale? (Select all that apply.) 5. The nurse is caring for a postoperative orthopedic patient who has two Hemovac drains in place. Which interventions should the nurse perform? (Select all that apply.) 6. The nurse knows that cold therapy is contraindicated in the following conditions: (Select all that apply.) Asepsis and Infection Control 1. The second line of defense that leads to local capillary dilation and leukocyte infiltration is known as: 2. The antigen-antibody reaction is an example of what type of immunity? 3. The nurse administers an immunization consisting of antibodies against hepatitis B. The nurse knows this is a form of what type of immunity? 4. A disease-causing organism is known as: 5. The nurse is explaining to the patient why she is receiving antibiotics. Her answer would be correct if she stated antibiotics are effective against which microorganism? 6. The nurse anticipates correctly that what type of medication would be ordered to treat athlete’s foot? MSC: NCLEX Client Needs Category: Safe and Effective Care NOT: Concepts: Infection 7. The nurse’s stethoscope most correctly represents which possible link in the chain of infection? 8. The nurse is teaching a group of patient about diseases such as Rocky Mountain Spotted Fever that are transmitted by ticks. The nurse’s explanation would be correct if she states that the tick functions as: 9. The nurse correctly identifies that the most effective method to prevent hospital-acquired infections is: 10. The nurse correctly identifies which patient as having the greatest risk for infection? 11. The nurse understands that which set of vitals most likely indicates infection? 12. The nurse notes that a patient’s albumin is low and is concerned about the patient’s ability to fight infection related to antibodies being made from what? 13. A patient admitted after abdominal surgery has a nursing diagnosis of risk for infection. Which is the most appropriate goal? 14. The nurse is caring for a patient who is comatose. Her intervention is appropriate when she performs oral care: 15. The nurse knows that which of the following skills does not require the use of sterile technique? 16. For which situation is it inappropriate to use alcohol-based hand sanitizer? 17. The nurse is preparing to perform suctioning on a new tracheostomy with the potential for forceful expulsion of secretions. What PPE should be worn? 18. The patient has hepatitis A. Which isolation precaution is correctly implemented? 19. The patient has pertussis. What isolation precaution is correctly implemented? 20. The nurse recognizes the correct order to remove PPE as: 21. The nurse has placed her sterile gloved hands below her waist. Her hands are now considered: 1. The nurse is planning care for an elderly patient. The nurse recognizes the patient is at risk for respiratory infections based on which factors? (Select all that apply.) 2. The nurse is providing education to a patient who is being discharged home on antibiotic therapy. Which of the following statement(s) by the patient indicates further education is needed? (Select all that apply.) 3. Which statement regarding handwashing indicates a need for further education? (Select all that apply.) 4. The nurse knows that standard precautions are indicated for: (Select all that apply.) 5. The patient is on protective precautions. Which is true regarding these precautions? (Select all that apply.) Safety 1. The increase focus in nursing on patient safety has resulted in a project funded by the Robert Wood Johnson Foundation called: 2. Individual factors affecting safety include those that are related to the functioning of body systems and those that are directly associated with a person’s particular lifestyle. Changes in which body system affect overall mobility increasing the propensity of falling? 3. The nurse is visiting a patient with cardiac disease who has been experiencing increased episodes of shortness of breath when she tries to exercise. The nurse is concerned that her decrease in activity may lead to: 4. Conversations about safe sexual practices, including the consequences of unprotected sex such as pregnancy and sexually transmitted infections, are important to begin in what patient population? 5. The nurse manager is developing a training guide. Which is the best organization to help her develop guidelines she can use to help her to prevent exposure to hazardous situations and decrease the risk of injury in the work place? 6. The nurse is educating parents about firearm safety. Which of the following statements indicates a need for further education? 7. The nurse recognizes that a patient is using a portable generator in the house as a power source. What source of poisoning does the nurse appropriately identify? 8. The nurse is educating the patient about the proper disposal of medications in the home. Which statement by the patient indicates she has a good understanding of the information? 9. The nurse knows that which of the following patients has a teaching need based on statements by the patient or the patient’s parents? 10. The nurse is working with a student nurse to teach her about restraint use in patients. Which statement by the student nurse indicates a learning need regarding restraints? 11. The nurse displays an understanding of high-risk populations for MRSA when identifying which group as the lowest risk? 12. The nurse knows that which of the following is not used to assess fall risk? 13. The patient has a nursing diagnosis of risk for falls. Which goal is most important? 14. Which collaborative team member would be most effective in assisting the nurse to identify medication alternatives that are less likely to cause drowsiness and dizziness to reduce the risk of falls in the elderly patient? 15. The nurse is concerned about helping the patient find resources to obtain assistive equipment to be used in the home. Which team member should the nurse contact first? 16. Which statement by the patient indicates a teaching need regarding safety in the home? 17. The ER nurse is triaging a patient with suspected poisoning. Who should the nurse anticipate contacting first? 18. Many health care facilities use the fire emergency response defined by the acronym: 19. The nurse is ambulating her patient back from the bath when the patient begins to have a seizure. Which of the following actions should the nurse do first? 20. The nurse is caring for a confused, combative patient. Which action would be considered last by the nurse to control behavior of the client? 21. The nurse knows that which of the following is an appropriate way to tie restraints? 22. Which statement by the nurse correctly identifies the UAP role in patient restraint use? 1. The nurse is explaining the National Patient Safety Goals (NPSG) to the student nurse. Which of the following answers indicates that the student has a good understanding of these goals? (Select all that apply.) 2. The nurse is providing education to a cardiac patient who has multiple life stressors that are impacting the patient’s health. Which of the following statements by the patient indicate he has a good understanding of actions he can take to reduce his stressors? (Select all that apply.) 3. The nurse is providing some education to a community group on environmental safety. Which of the following safety measures are effective in improving their environmental safety? (Select all that apply.) Perioperative Nursing Care 1. The nurse is caring for a patient who is about to have surgery. Which intervention will be included in the patient’s care to meet the goals for Risk for perioperative positioning injury r/t immobilization during surgical procedure? 2. The nurse is caring for a male patient who will soon have open heart surgery. The patient’s chest is covered with thick hair so the surgical technician comes in to shave the patient’s skin near the operative site. Which action by the technician requires intervention by the nurse to correct the technique? 3. The nurse is caring for a patient who has just been brought to the postoperative unit following major surgery. The patient has many tubes and monitors in place. Which will the nurse assess first? 4. The nurse is caring for a patient who has a family history of reactions to general anesthesia. Which medication will the anesthesiologist have ready as a precautionary measure before the patient’s surgery is started? 5. Which action by the nurse best demonstrates accountability in the operating room? 6. The nurse is caring for a patient who will be having surgery. The patient has just signed the consent form for the operation. What does the patient’s signature indicate? 7. The nurse is caring for a postoperative patient who is very sleepy following general anesthesia and administration of pain medication. The nurse notes that the patient is making snoring sounds and his pulse oximetry has dropped to 88%. What is the best action of the nurse? 8. The nurse is caring for a postoperative patient on his first day after surgery. The nurse informs the patient that the plan is to sit in the chair and ambulate in the hallway. The patient states that he is in pain and he has no intention of getting out of bed. What is the nurse’s best response? 9. The nurse is walking a postoperative patient in the hallway when she notices a large red stain of fresh blood on the patient’s gown over the abdominal incision. The patient states, “I felt something just ripped open.” What is the priority action of the nurse? 10. The nurse is caring for a patient with advanced colon cancer. The patient is to have surgery to relieve a bowel obstruction that has been causing unrelenting vomiting and abdominal pain. What type of surgery will this patient undergo? 11. After general anesthesia is administered, the patient is carefully placed in the prone position. What is the primary consideration of the nursing staff as the patient is positioned? 12. The nurse is caring for a preoperative patient who has just received sedation prior to general anesthesia in the OR. What is the priority action of the nurse? 13. The nurse is caring for a postoperative patient who is recovering from abdominal surgery. The nurse notes that the patient’s breath sounds are clear but diminished, shallow, and slightly labored. The patient’s pulse oximetry is 96% on room air. What is the priority action of the nurse? 14. The nurse will be caring for a patient who has just arrived on the medical-surgical unit following surgical repair of his fractured right ankle. Which is the priority action of the nurse when the patient arrives on the unit? 15. The nurse is caring for a patient who is recovering from chest surgery. Which action by the patient indicates that additional teaching is needed about how to use the ordered incentive spirometer correctly? 16. The nurse is caring for a patient who is headed to the operating room for abdominal surgery. Which goal is appropriate for the nursing diagnosis risk for Perioperative positioning injury? 17. The nurse is caring for a patient who requires emergency surgery for injuries sustained in a motor vehicle accident. The patient was on his way back to work after having lunch with colleagues when the accident happened. What is the highest priority nursing diagnosis for this patient? 18. The nurse is caring for a postoperative patient who has a history of COPD. What is the priority nursing diagnosis for this patient? 19. The nurse is assigned to care for several patients on the surgical unit. Which patient need will the nurse address first? MULTIPLE RESPONSE 1. The nurse is obtaining preoperative information for a patient who will be having emergency surgery shortly for a ruptured appendix. Which information is crucial for the nurse to assess? (Select all that apply.) 2. The nurse is working with a nursing assistant to care for several postoperative patients. Which interventions can the nurse delegate to the assistant for completion? (Select all that apply.) 3. Which of the following patients would benefit from preoperative teaching about splinting of incisions to minimize discomfort? (Select all that apply.) 4. The nurse is caring for a patient who is recovering from bowel resection surgery. Which assessment findings indicate to the nurse that the patient no longer needs to remain NPO and may progress to oral intake of food and fluids? (Select all that apply.) 5. The nurse is caring for a patient who underwent abdominal surgery the previous day. Which assessment findings indicate to the nurse that the patient may be experiencing serious internal bleeding? (Select all that apply.) Diagnostic Testing 1. The nurse is caring for a patient who states that he has been taking his medications and following his diabetic diet carefully. Which test result indicates to the nurse that the patient has not been compliant with the treatment plan? 2. The nurse is caring for an elderly patient with dementia. Which laboratory finding indicates to the nurse that that patient is often forgetting to eat meals? 3. The nurse is caring for a patient who has a deep leg wound that is badly infected. Which laboratory test results will the nurse expect to find in the patient’s chart? 4. The nurse is caring for a patient who has a bleeding gastric ulcer. How will the nurse expect the patient’s stool to appear? 5. The nurse is caring for a patient who is to have a noncontrast MRI scan performed. Which assessment finding leads the nurse to report that the patient may not be able to have the test? 6. The nurse is caring for a patient who has had severe acid reflux. Which test will allow the physician to directly check for damage to the esophagus? 7. The nurse is caring for a woman who has a cyst in her breast that was found at her recent mammogram. The physician wants to make sure that the cyst is not malignant. Which test will be used to determine this? 8. The nurse is caring for a patient who is scheduled for a needle aspiration and biopsy to rule out cancer. Which nursing diagnosis is appropriate and important for this patient? 9. The nurse is caring for a patient who will be undergoing flexible sigmoidoscopy testing to screen for colon cancer. What goal will the nurse include in the patient’s plan of care? 10. The nurse is caring for a patient who will be receiving iodine-based contrast medium for a CT scan. Which allergy should be reported to the technician and radiologist before the test is performed? 11. The nurse is caring for a patient who has just undergone bronchoscopy. The patient states that she is thirsty and requests a drink of water. What is the nurse’s best action? 12. The nurse is caring for a patient who will be undergoing bone marrow biopsy. Which statement by the patient indicates that additional teaching is needed? 13. The nurse is caring for a patient who is sedated following a colonoscopy. Which is the priority action of the nurse? 14. The nurse is caring for a patient who recently had a liver biopsy. To whom must the nurse give the results? 15. The nurse is caring for a patient who is to collect a 24-hour urine specimen. Which statement by the patient indicates that additional teaching is required? 16. The nurse is caring for a patient whose immune system is destroying red blood cells at a very rapid rate. Which test result will the nurse expect to see in the patient’s chart as a result? 17. The nurse is caring for a patient with a urinary tract infection. Which test will indicate which antibiotics will be effective to treat the infection? 18. The nurse is caring for a patient who has just undergone paracentesis. For which complication will the nurse carefully monitor? 19. The nurse is caring for a patient who is having blood drawn as part of preoperative testing. Which step is the most important to ensure the safety of the patient and the nurse? 20. The nurse is caring for a diabetic patient who will be doing fingerstick blood glucose testing at home. What is the best way for the nurse to ensure that the patient can perform the procedure correctly? 1. The nurse is caring for a patient who is anemic. Which CBC test results demonstrate that the patient’s treatment plan is effective and the anemia is resolving? (Select all that apply.) 2. The nurse is caring for a patient who has been having abdominal pain. The doctor suspects that the patient may have an abdominal aortic aneurysm. Which tests would confirm the doctor’s suspicion? (Select all that apply.) 3. The nurse is caring for a patient who is undergoing a liver biopsy. Which interventions will be included in the patient’s care plan for the diagnosis of Risk for infection: r/t invasive diagnostic procedure? (Select all that apply.) 4. The nurse is caring for a patient who needs to collect a 24-hour urine specimen at home. Which steps of specimen collection may be delegated to the assistant? (Select all that apply.) 5. The nurse is caring for a patient who is taking medication that is toxic to the liver. Which laboratory test results will be reviewed by the nurse to ensure that the patient’s liver is tolerating the medication without damage to the organ? (Select all that apply.) Activity, Immobility, and Safe Movement 1. The nurse knows rheumatoid arthritis affects the musculoskeletal system by causing: 2. The nurse is implementing generalized falls precautions for his patients who are at risk for falls. Which intervention indicates a lack of understanding of these precautions? 3. The nurse is educating the family of a patient on falls risk precautions. Which of the following statements by the family indicates a need for further education? 4. The nurse is performing passive range-of-motion exercises on his patient when the patient begins to complain of pain. What is the first thing the nurse should do? 5. An appropriate goal for the patient who is postoperative day one from a hip fracture with the nursing diagnosis Impaired physical mobility is: 6. An appropriate goal for the patient who is postoperative day one from abdominal surgery and on bed rest with the nursing diagnosis Impaired skin integrity is: 7. The nurse is providing education to the patient about isometric exercises. Which statement by the patient indicates a good understanding? 8. The nurse is preparing to assist her patient to walk to the bathroom after medicating her with a narcotic for pain management. Of what possible adverse effect should the nurse be immediately aware? 9. The nurse correctly selects which intervention to avoid causing shear or friction when moving a patient in bed? 10. The nurse knows active assistive range of motion is: 11. The nurse appropriately delegates care to the UAP when she: 12. The nurse knows that manual lifting should only be done in the following situations: 13. The nurse is preparing to reposition the patient in bed. What is the first step in this process? 14. The nurse has delegated to the UAP to assist a patient with ambulating in the hallway with a cane. Which statement by the UAP indicates a need for further education? 15. The nurse correctly teaches the patient to rise from a chair using crutches when the following interventions are used: 1. The nurse is teaching a patient about ways to decrease her risk of bone fractures. The following statements by the patient indicate a good understanding. (Select all that apply.) 2. The nurse knows that a patient with a compromised cardiopulmonary system has a diminished capacity for exercise because of the following: (Select all that apply.) 3. The nurse is educating the patient about the effects of immobility on the body. The following statements by the patient indicate a need for further education: (Select all that apply.) 4. The nurse knows the following items should be included in the documentation of the patient on falls precautions: (Select all that apply.) 5. The nurse knows the following indicates orthostatic hypotension: (Select all that apply.) 6. The nurse appropriately delegates care of her patient to the properly trained UAP when she: (Select all that apply.) 7. The nurse is correctly demonstrating the use of a transfer belt when engaging in the following: (Select all that apply.) NOT: Concepts: Mobility 8. The nurse is correctly assisting the patient in using a cane when the patient demonstrates the following: (Select all that apply.) 9. The nurse is providing discharge education for her patient who is going home with a walker. Which statement by the patient indicates a good level of understanding of safety in the home? (Select all that apply.) 10. The nurse knows the knee-high SCD sleeves are correctly placed on the patient when the following conditions are met: (Select all that apply.) Sleep 1. The nurse knows that with the onset of darkness and in preparation for sleep: 2. The nurse knows the reticular activating system (RAS): 3. The nurse is educating a patient about taking measures to help avoid disruption to the circadian rhythm. The following statement by the patient indicates a need for further education: 4. The nurse knows that polysomnograpy is: 5. The nurse knows the usual progression of sleep is: 6. The nurse is providing discharge instructions to the parents of a toddler about sleeping habits. Which of the following statements indicates further education is needed? 7. The nurse knows that cataplexy includes: 8. The nurse is providing discharge instructions to a patient who has had sleep alterations. The following statements by the patient indicate further education is needed. 9. The nurse is performing an assessment of the patient’s sleep patterns. Which question will elicit the best response? 10. The nurse knows an appropriate goal for the nursing diagnosis Sleep deprivation is: 11. The nurse knows an appropriate goal for the nursing diagnosis Disturbed sleep pattern during hospitalization is: NOT: Concepts: Caring Interventions 12. The nurse knows an appropriate goal for the nursing diagnosis Insomnia is: 13. The nurse is providing discharge education for a patient with narcolepsy. The following statement by the patient indicates a need for further education: 14. The nurse is providing discharge education for a patient with restless leg syndrome. The following statement by the patient indicates a need for further education: 15. Which of the following is inappropriate to delegate to the unlicensed assistive personnel (UAP)? 16. The nurse is providing discharge instructions for the patient with sleep pattern disturbances. Which statement by the patient indicates a need for further education? 1. The nurse knows that during rapid eye movement (REM) sleep, the following occur: (Select all that apply.) 2. The nurse knows that during non-rapid eye movement (NREM) sleep, the following occur: (Select all that apply.) 3. The nurse knows the following changes in sleep patterns occur in the older adult: (Select all that apply.) 4. The nurse knows the following information about sudden infant death syndrome (SIDS): (Select all that apply.) 5. The nurse knows that dyssomnias are: (Select all that apply.) 6. The nurse manager is concerned about her staff who are working the night shift. What interventions can she suggest to assist nurses in overcoming shift related sleep disturbances? (Select all that apply.) Integrity 7. The nurse knows the following risk factors are associated with obstructive sleep apnea (OSA): (Select all that apply.) 8. The nurse is admitting a patient to the general medical-surgical unit. What should the nurse assess as part of a routine sleep assessment? (Select all that apply.) 9. The nurse knows the following interventions will help improve sleep quality during hospitalization: (Select all that apply.) Activity, Immobility, and Safe Movement 1. The nurse knows rheumatoid arthritis affects the musculoskeletal system by causing: 2. The nurse is implementing generalized falls precautions for his patients who are at risk for falls. Which intervention indicates a lack of understanding of these precautions? 3. The nurse is educating the family of a patient on falls risk precautions. Which of the following statements by the family indicates a need for further education? 4. The nurse is performing passive range-of-motion exercises on his patient when the patient begins to complain of pain. What is the first thing the nurse should do? 5. An appropriate goal for the patient who is postoperative day one from a hip fracture with the nursing diagnosis Impaired physical mobility is: 6. An appropriate goal for the patient who is postoperative day one from abdominal surgery and on bed rest with the nursing diagnosis Impaired skin integrity is: 7. The nurse is providing education to the patient about isometric exercises. Which statement by the patient indicates a good understanding? 8. The nurse is preparing to assist her patient to walk to the bathroom after medicating her with a narcotic for pain management. Of what possible adverse effect should the nurse be immediately aware? 9. The nurse correctly selects which intervention to avoid causing shear or friction when moving a patient in bed? 10. The nurse knows active assistive range of motion is: 11. The nurse appropriately delegates care to the UAP when she: 12. The nurse knows that manual lifting should only be done in the following situations: 13. The nurse is preparing to reposition the patient in bed. What is the first step in this process? 14. The nurse has delegated to the UAP to assist a patient with ambulating in the hallway with a cane. Which statement by the UAP indicates a need for further education? 15. The nurse correctly teaches the patient to rise from a chair using crutches when the following interventions are used: 1. The nurse is teaching a patient about ways to decrease her risk of bone fractures. The following statements by the patient indicate a good understanding. (Select all that apply.) 2. The nurse knows that a patient with a compromised cardiopulmonary system has a diminished capacity for exercise because of the following: (Select all that apply.) 3. The nurse is educating the patient about the effects of immobility on the body. The following statements by the patient indicate a need for further education: (Select all that apply.) 4. The nurse knows the following items should be included in the documentation of the patient on falls precautions: (Select all that apply.) 5. The nurse knows the following indicates orthostatic hypotension: (Select all that apply.) 6. The nurse appropriately delegates care of her patient to the properly trained UAP when she: (Select all that apply.) 7. The nurse is correctly demonstrating the use of a transfer belt when engaging in the following: (Select all that apply.) 8. The nurse is correctly assisting the patient in using a cane when the patient demonstrates the following: (Select all that apply.) 9. The nurse is providing discharge education for her patient who is going home with a walker. Which statement by the patient indicates a good level of understanding of safety in the home? (Select all that apply.) 10. The nurse knows the knee-high SCD sleeves are correctly placed on the patient when the following conditions are met: (Select all that apply.) [Show More]
Last updated: 1 year ago
Preview 1 out of 55 pages
Buy this document to get the full access instantly
Instant Download Access after purchase
Add to cartInstant download
We Accept:

Reviews( 0 )
$18.00
Document information
Connected school, study & course
About the document
Uploaded On
Jul 23, 2021
Number of pages
55
Written in
Additional information
This document has been written for:
Uploaded
Jul 23, 2021
Downloads
0
Views
44