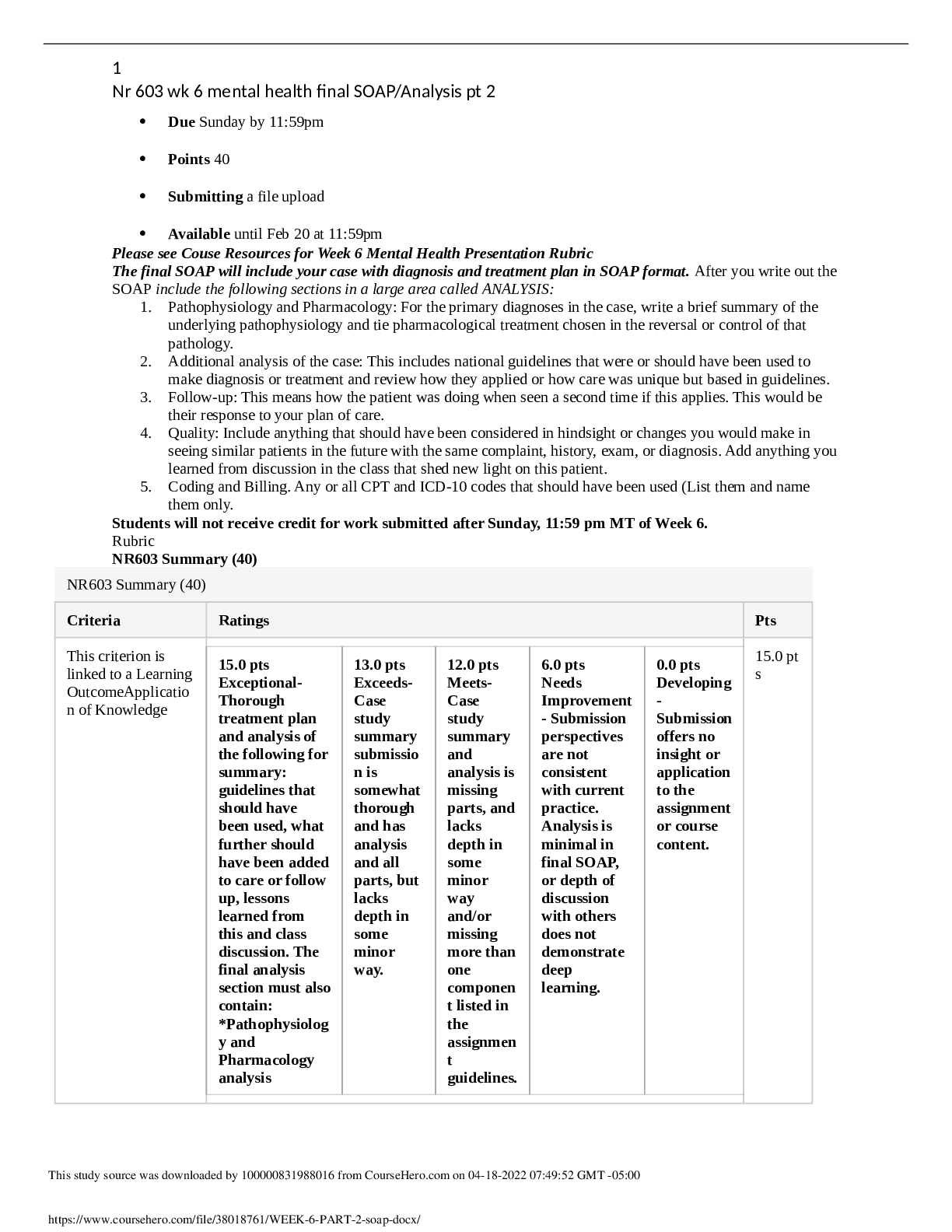
*NURSING > SOAP NOTE > NR509_SOAP_Note_Tina Jones Neuro | Chamberlain College of Nursing > DETAILED SOLUTION 100% (All)
NR509_SOAP_Note_Tina Jones Neuro | Chamberlain College of Nursing > DETAILED SOLUTION 100%
Document Content and Description Below
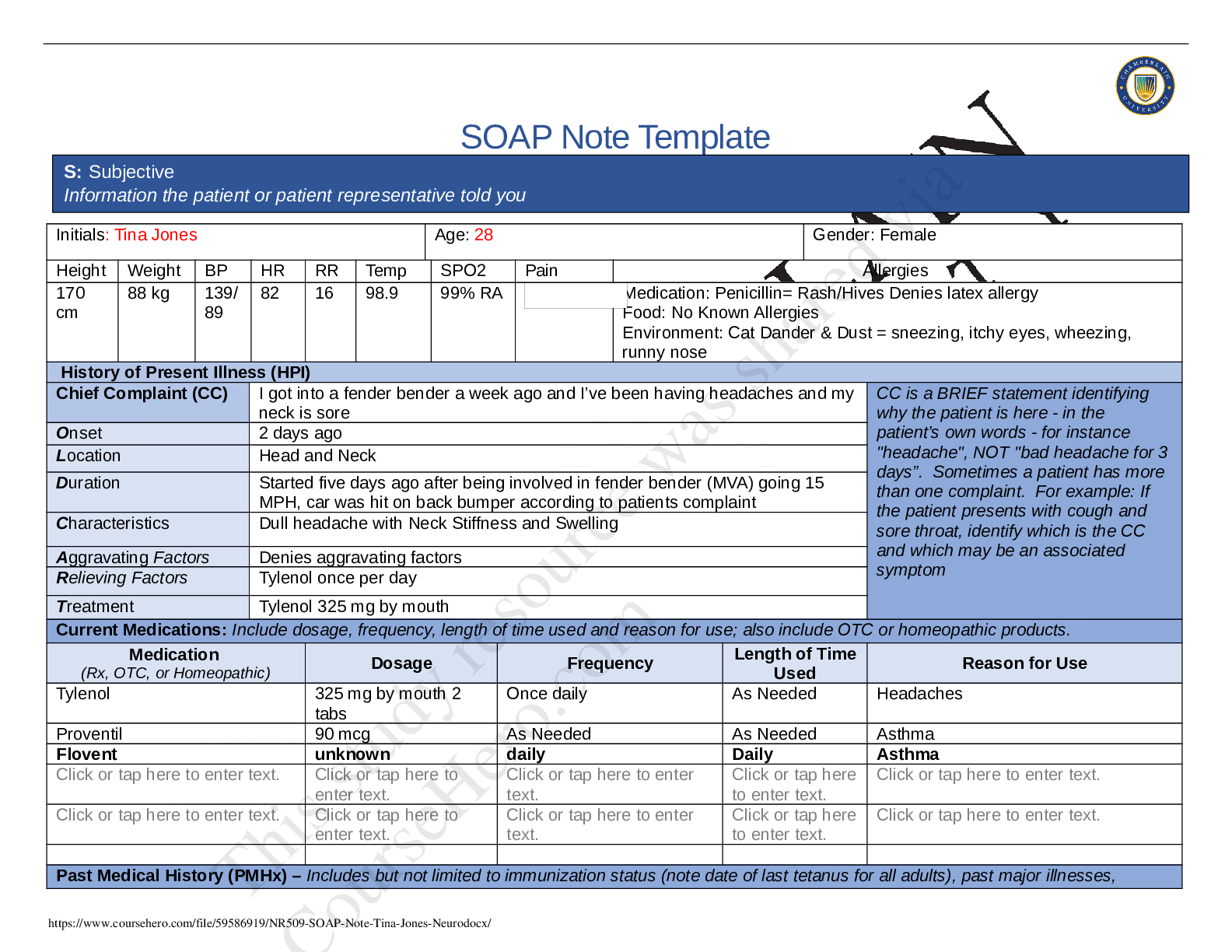
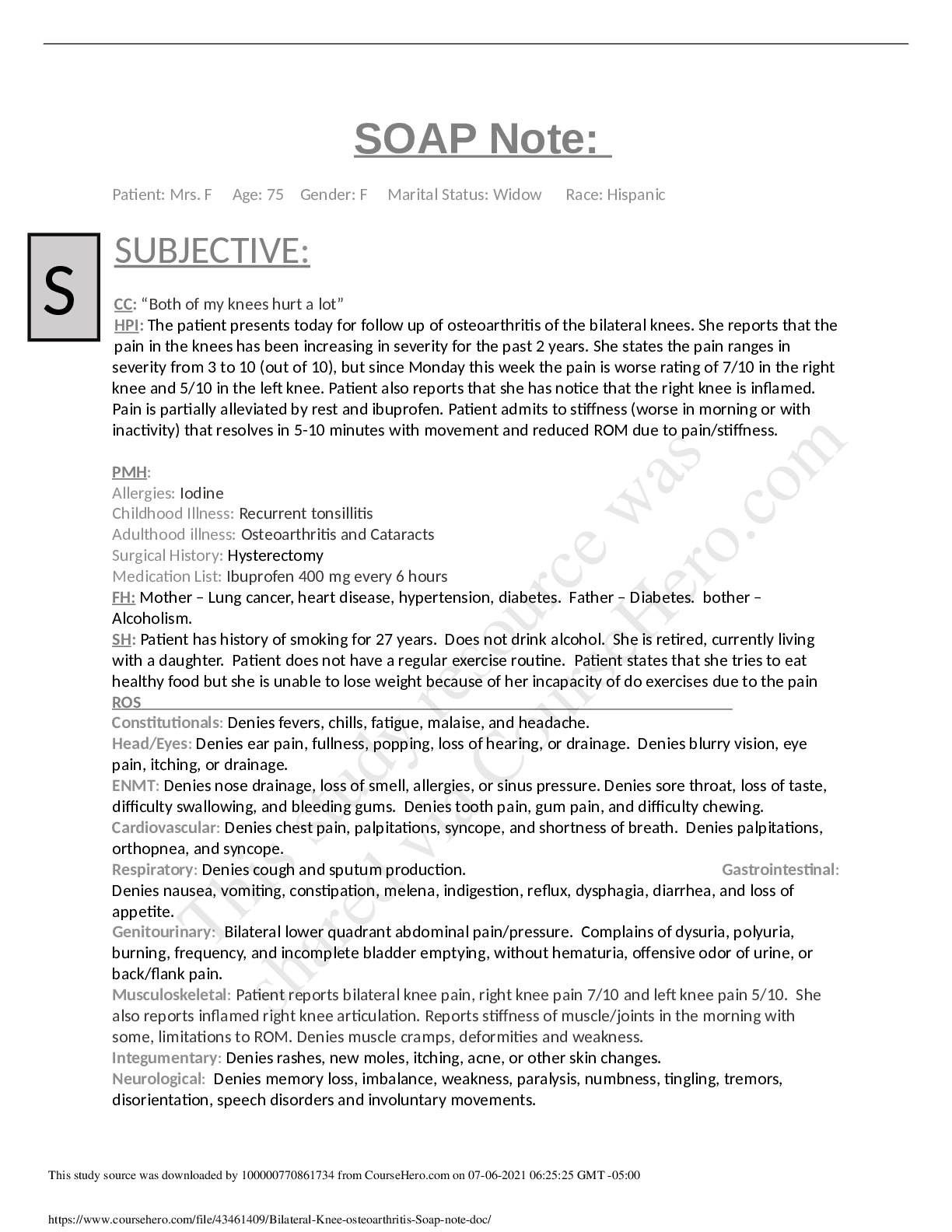
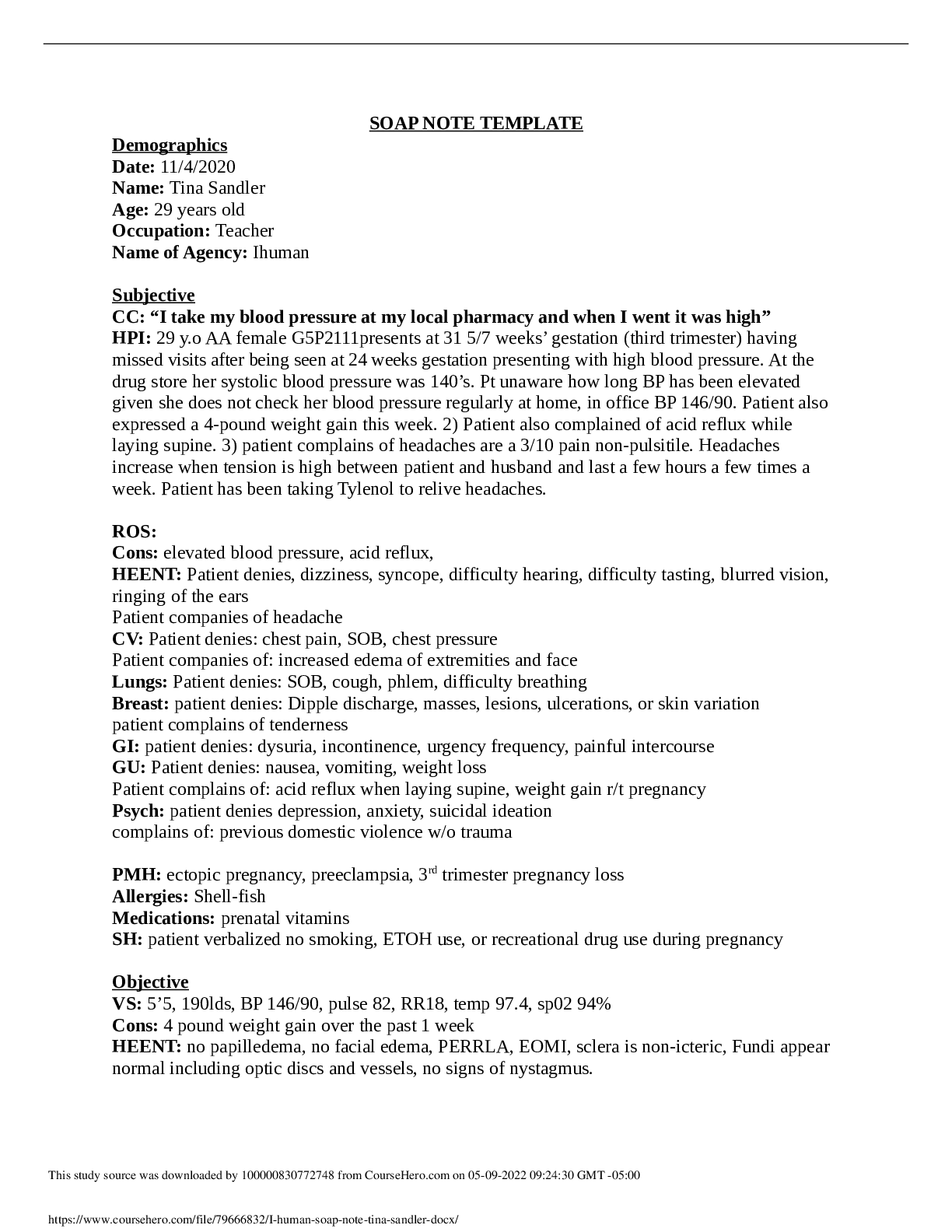
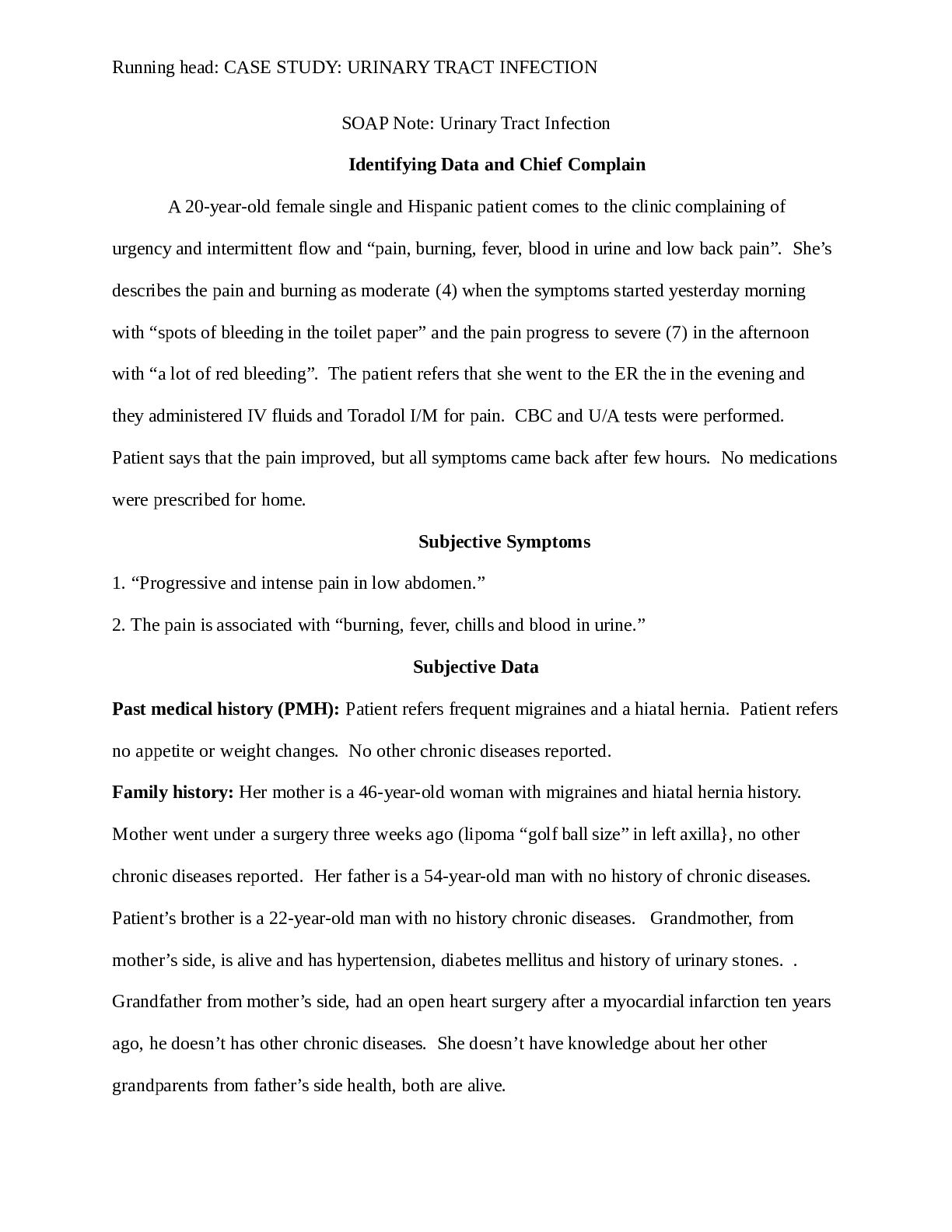
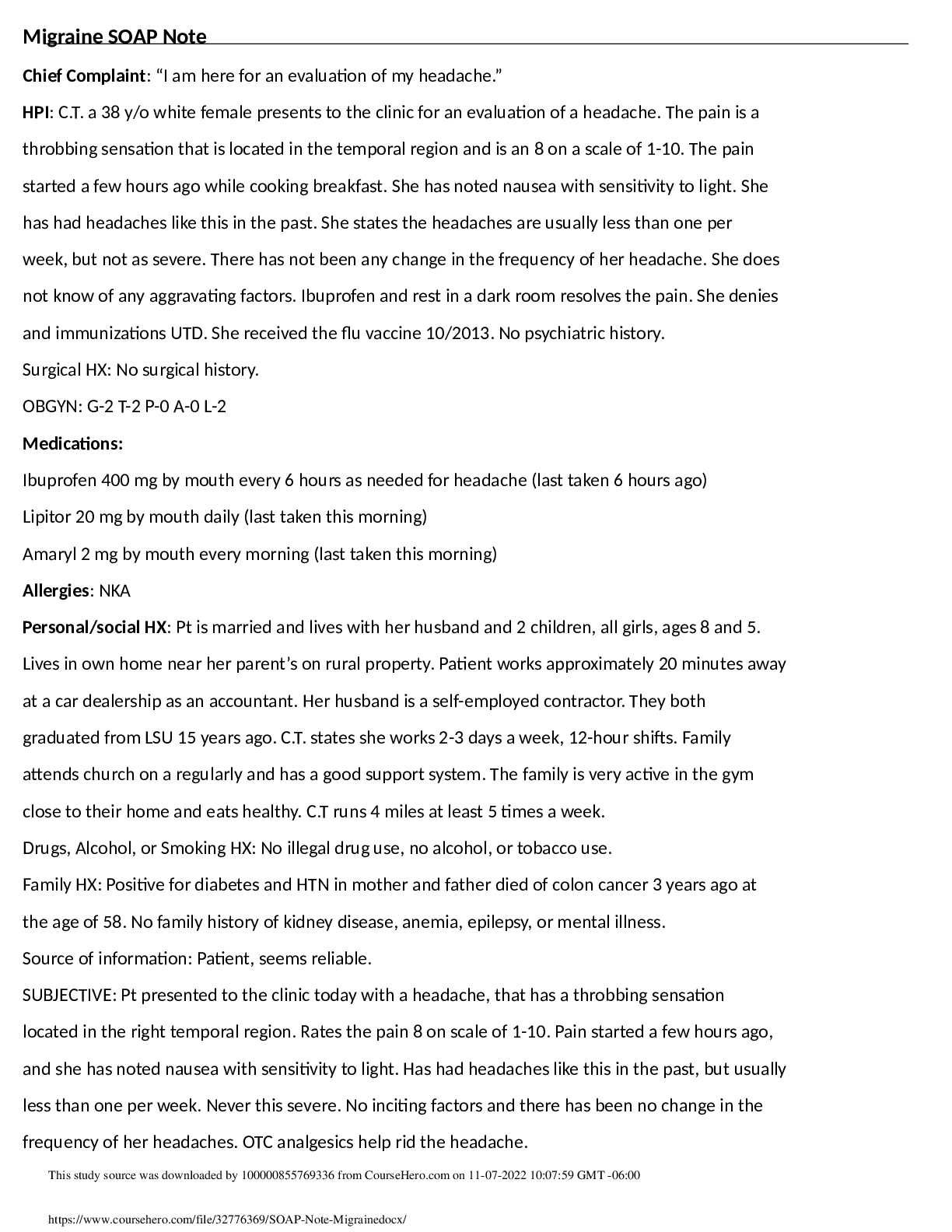
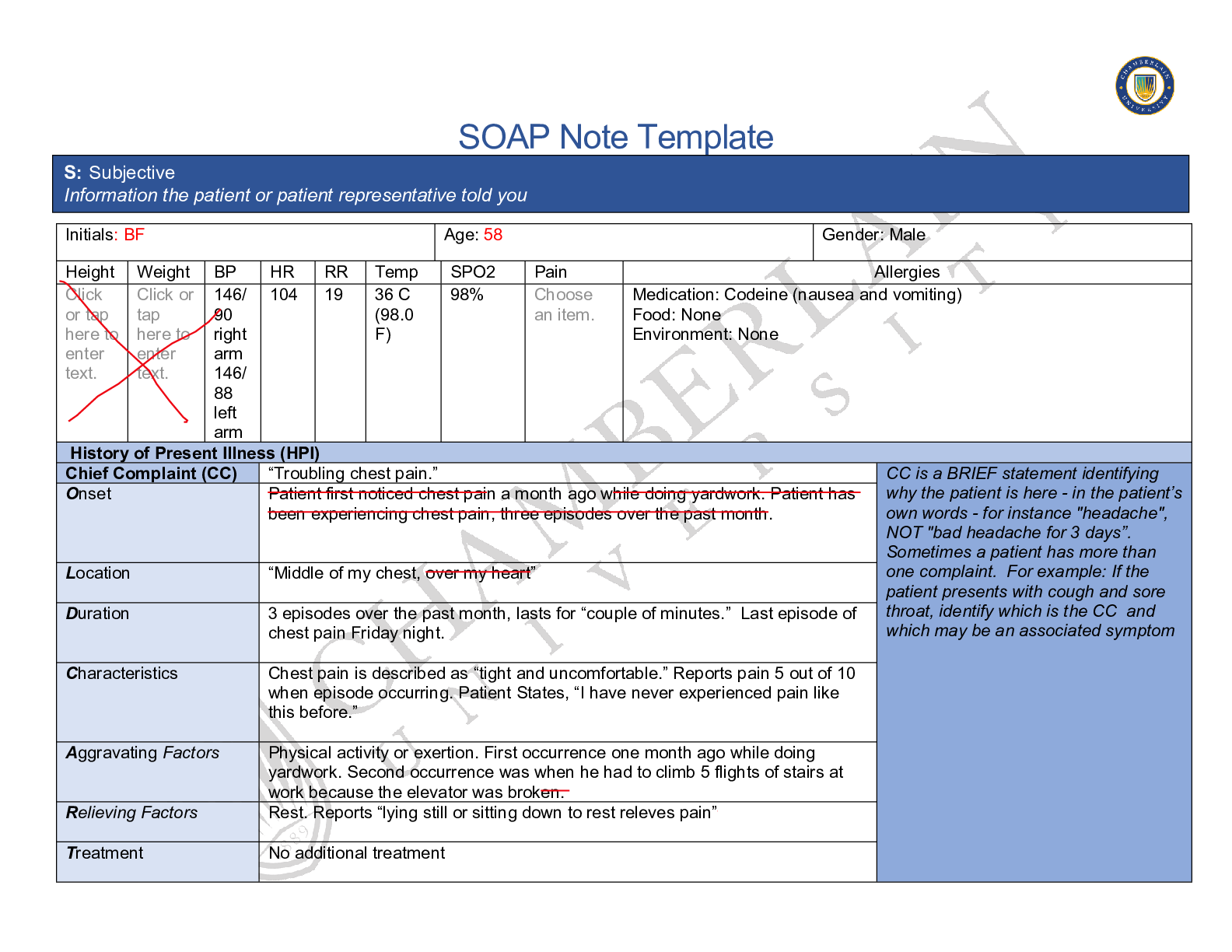
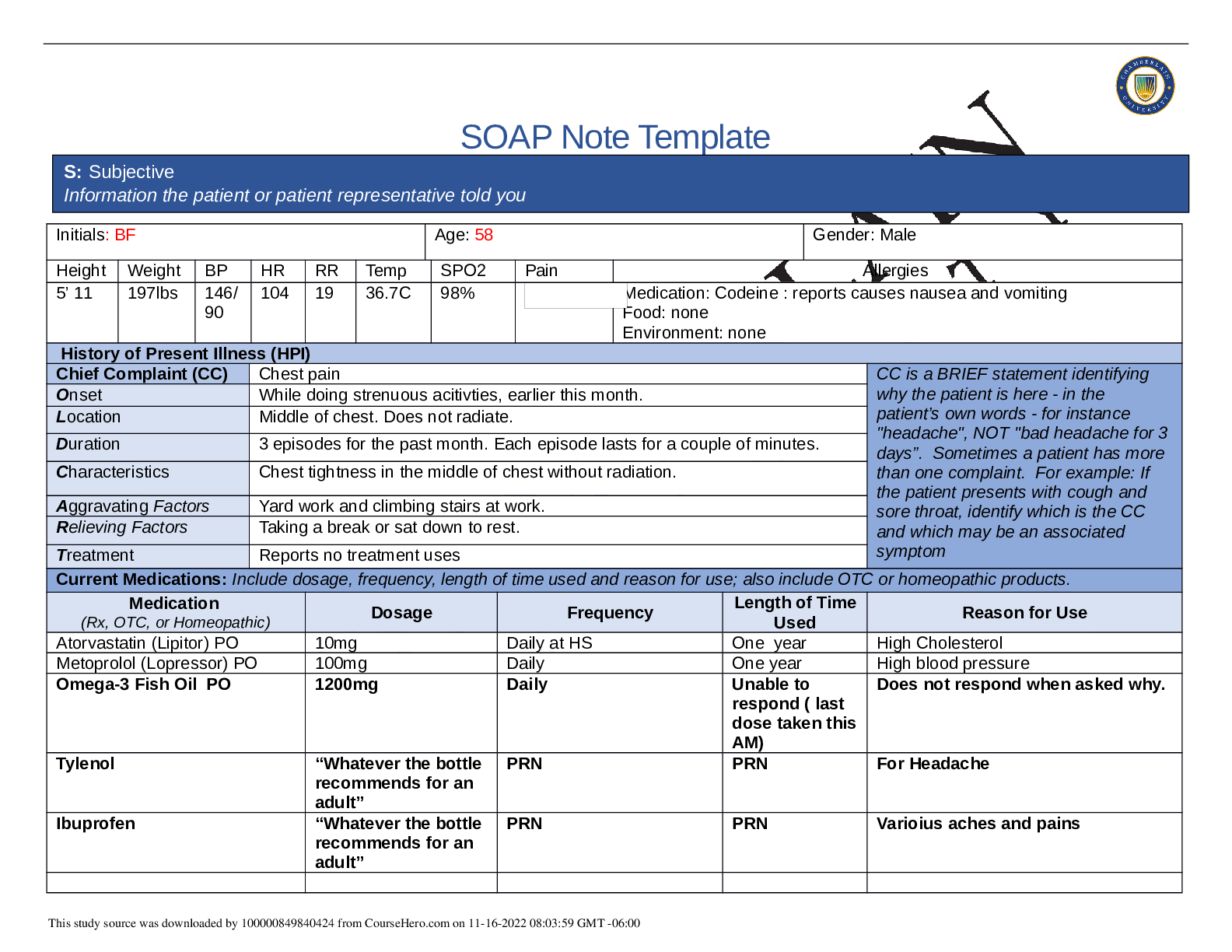
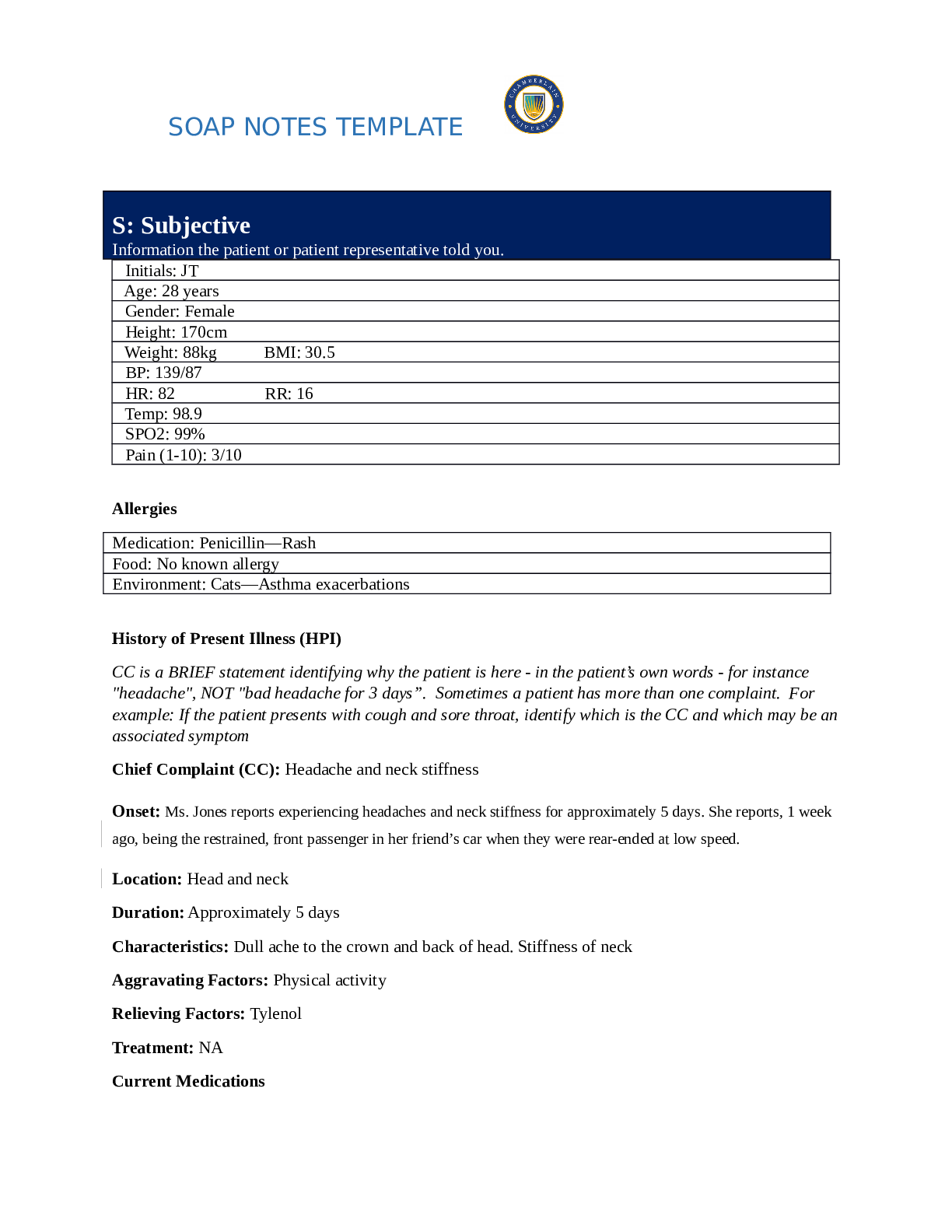
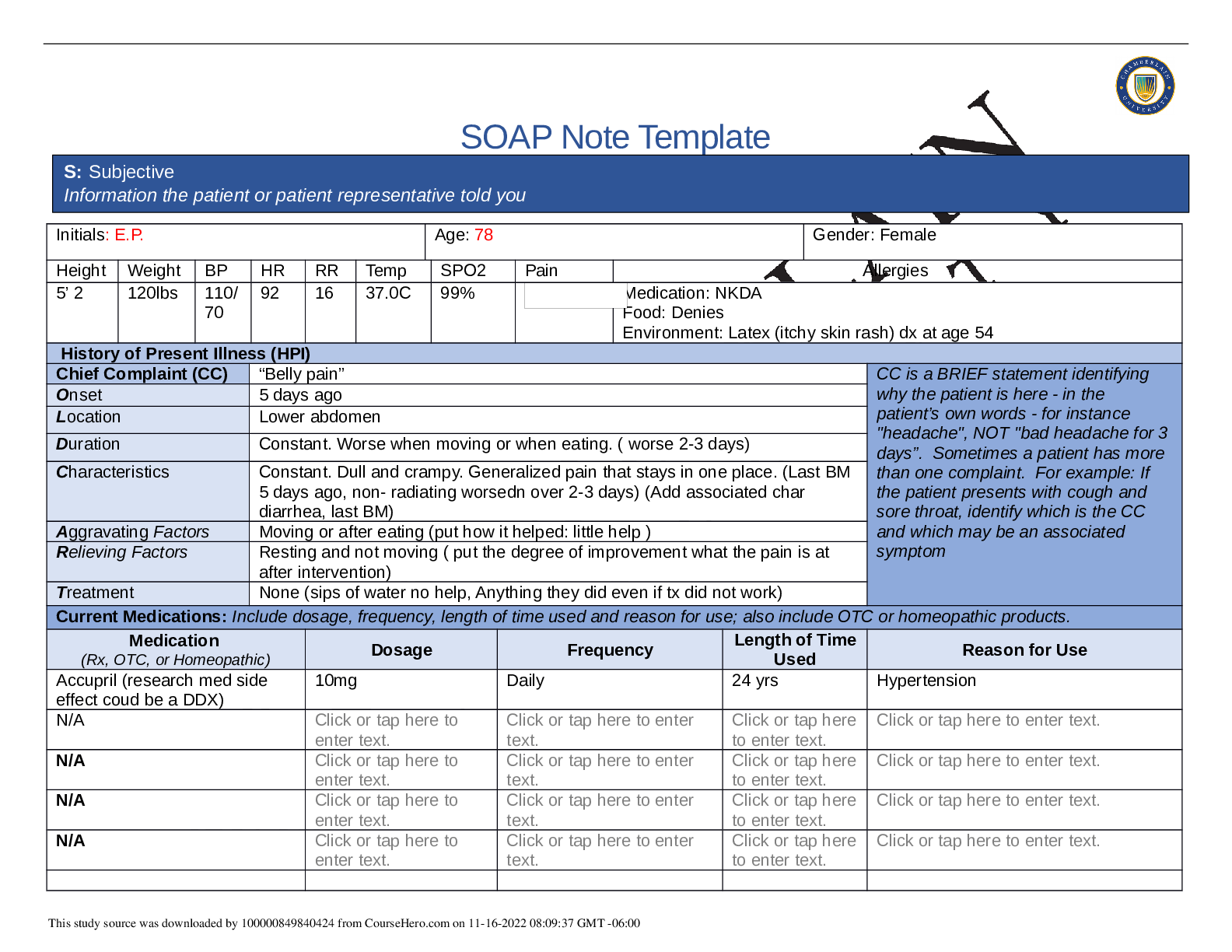
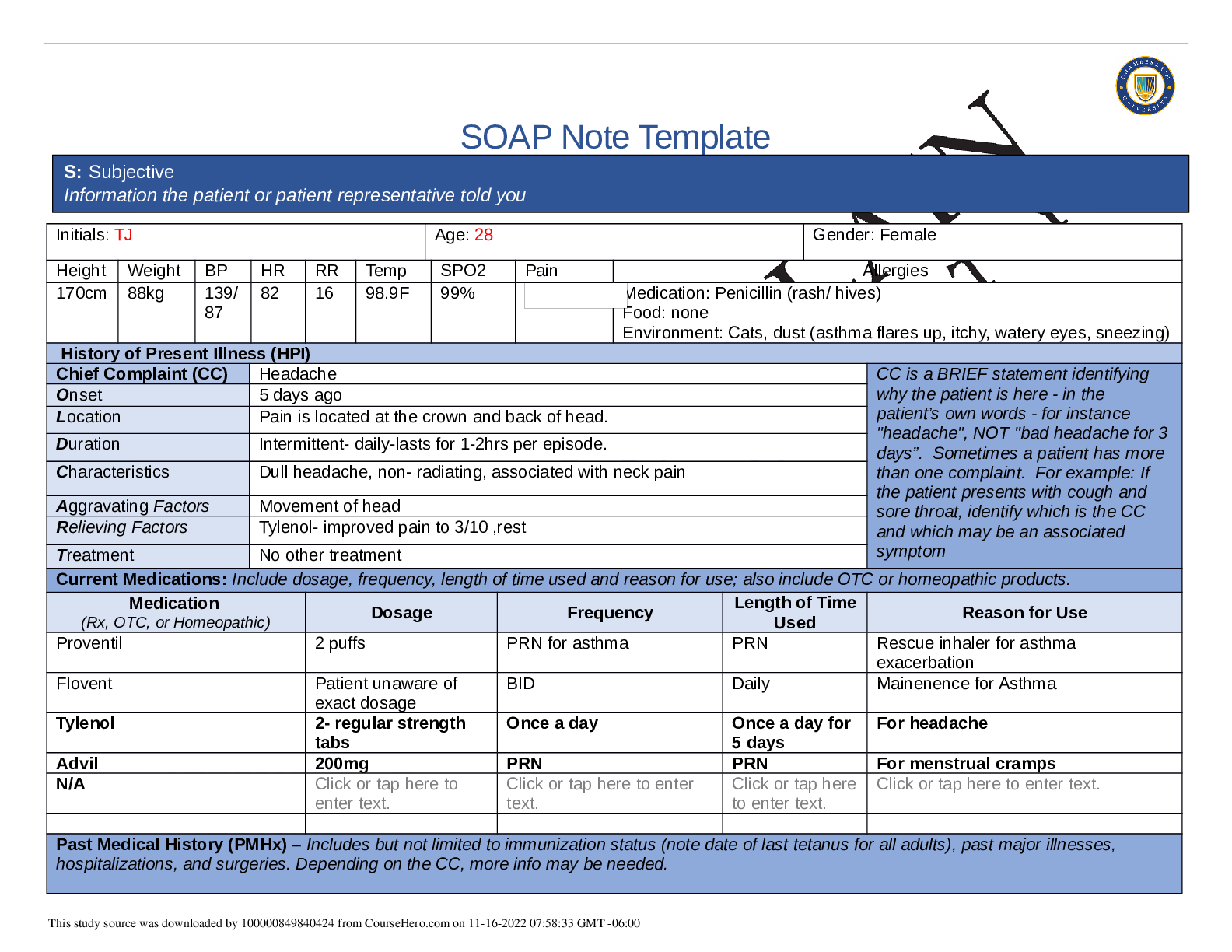
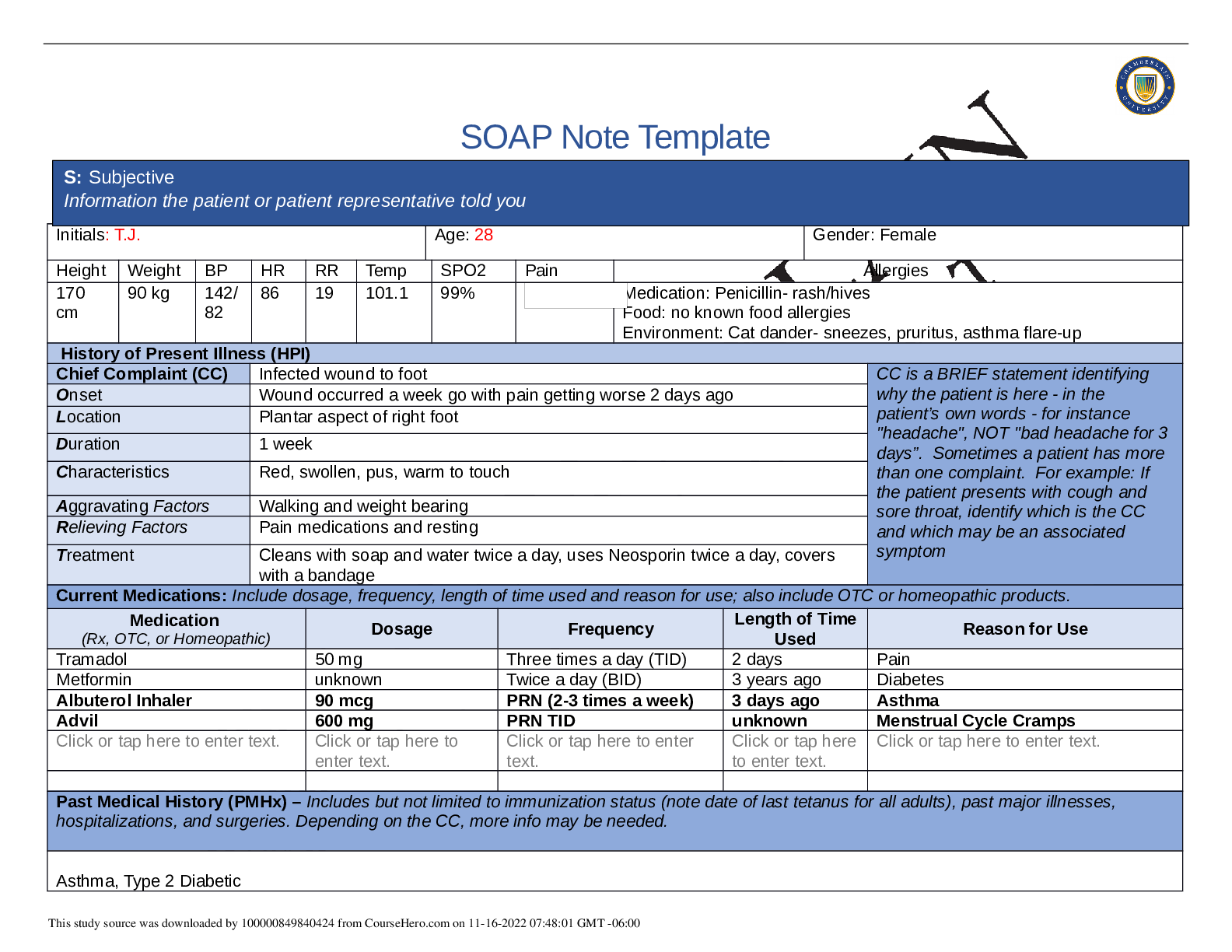
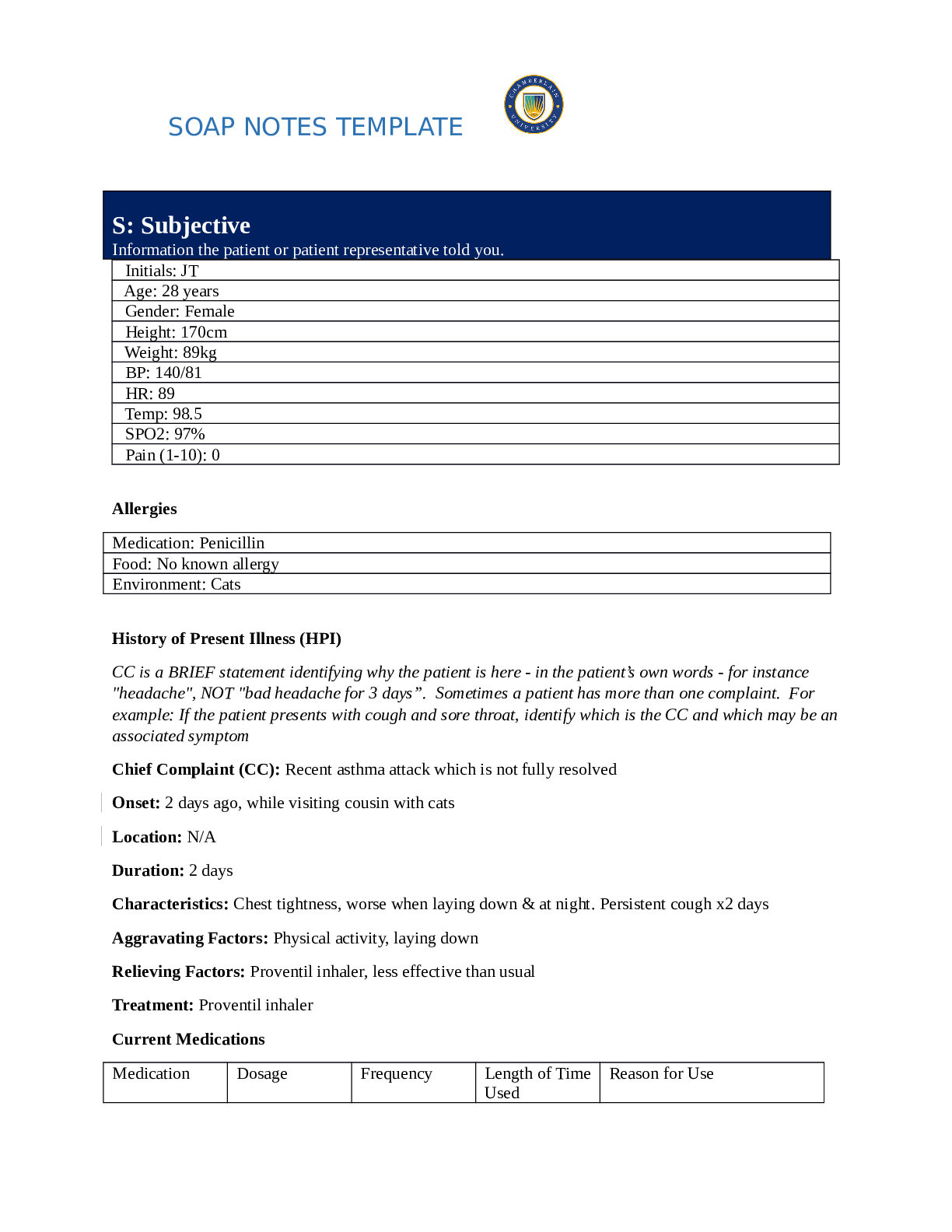
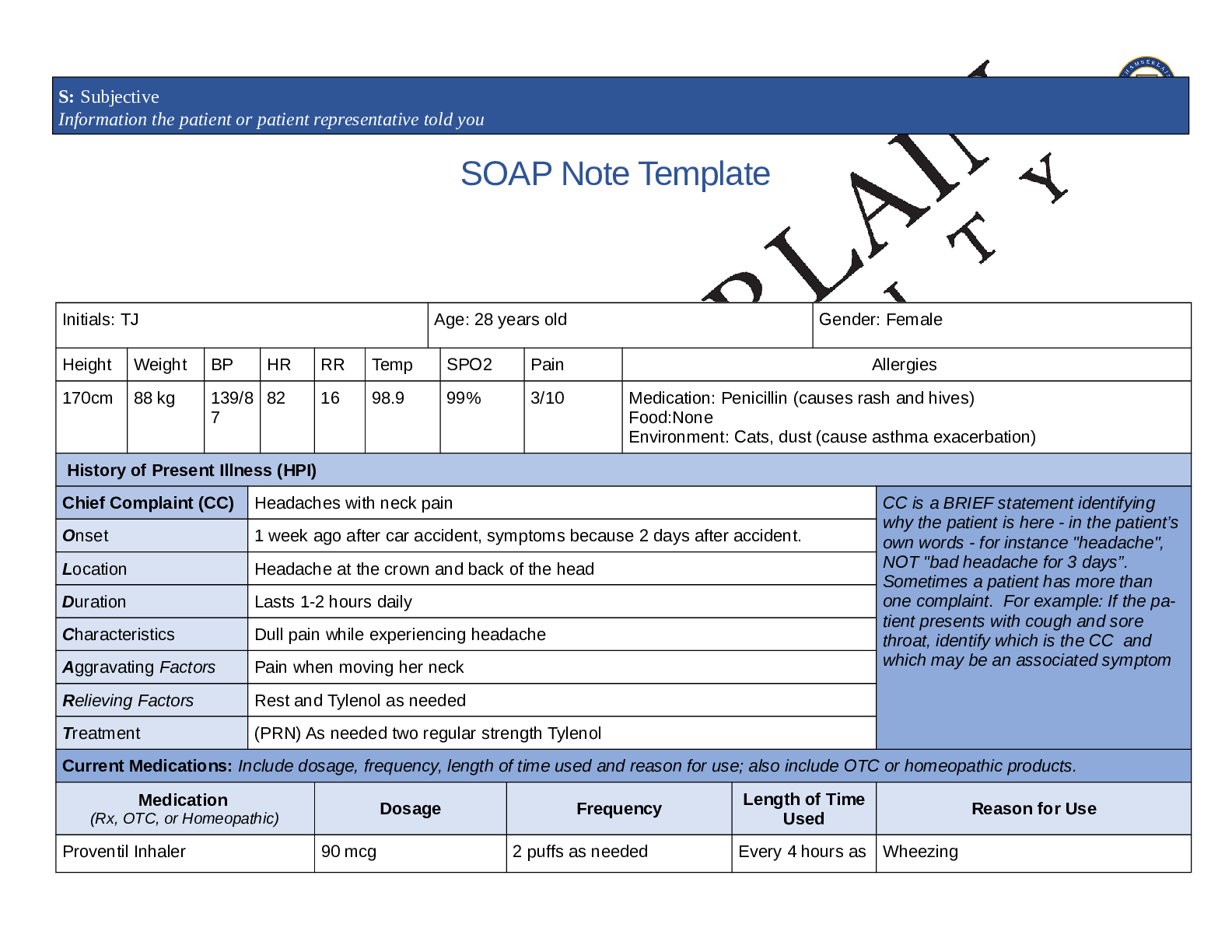
SOAP Note Template Initials: Tina Jones Age: 28 Gender: Female Height Weight BP HR RR Temp SPO2 Pain Allergies 170 cm 88 kg 139/ 89 82 16 98.9 99% RA Medication: Penicillin= Rash/Hives Den... ies latex allergy Food: No Known Allergies Environment: Cat Dander & Dust = sneezing, itchy eyes, wheezing, runny nose History of Present Illness (HPI) Chief Complaint (CC) I got into a fender bender a week ago and I’ve been having headaches and my neck is sore CC is a BRIEF statement identifying why the patient is here - in the patient’s own words - for instance "headache", NOT "bad headache for 3 days”. Sometimes a patient has more than one complaint. For example: If the patient presents with cough and sore throat, identify which is the CC and which may be an associated symptom Onset 2 days ago Location Head and Neck Duration Started five days ago after being involved in fender bender (MVA) going 15 MPH, car was hit on back bumper according to patients complaint Characteristics Dull headache with Neck Stiffness and Swelling Aggravating Factors Denies aggravating factors Relieving Factors Tylenol once per day Treatment Tylenol 325 mg by mouth Current Medications: Include dosage, frequency, length of time used and reason for use; also include OTC or homeopathic products. Medication (Rx, OTC, or Homeopathic) Dosage Frequency Length of Time Used Reason for Use Tylenol 325 mg by mouth 2 tabs Once daily As Needed Headaches Proventil 90 mcg As Needed As Needed Asthma Flovent unknown daily Daily Asthma Click or tap here to enter text. Click or tap here to enter text. Click or tap here to enter text. Click or tap here to enter text. Click or tap here to enter text. Click or tap here to enter text. Click or tap here to enter text. Click or tap here to enter text. Click or tap here to enter text. Click or tap here to enter text. Past Medical History (PMHx) – Includes but not limited to immunization status (note date of last tetanus for all adults), past major illnesses, hospitalizations, and surgeries. Depending on the CC, more info may be needed. Reports fender bender (MVA) five days ago with headache and neck pains beginning two days ago. Denies hitting head during accident. Describes headache as dull sensation behind eyes, bilaterally, that occurs once a day and lasts for approximately one hour. Pain severity of 4/10 during headache. Headache pain does not radiate. Reports headache is detracting but not incapacitating. Patient denies sharp pain associated with headaches. States headache does not occur as a rapid crescendo, in clusters nor occurs in cycles. Last headache was yesterday afternoon. Denies aura, nausea, vomiting, dizziness or photophobia associated with headache. Reports some increased pain to neck when headache is present. Patient describes neck pain as constant stiffness primarily located to the left side, with 3/10 in severity, which does not radiate. Patient has noted some swelling to neck. Denies nuchal rigidity.Patient denies dizziness, nausea, vomiting or changes in neurological functioning. Denies changes in vision, hearing or sense of smell since accident. Patient states she was in the passenger seat at the time of the accident and was wearing her seat belt. Patient reports she did not lose consciousness during or after accident. Patient reports no alcohol, drug or cell phone use at the time of the accident. Denies any recent or past surgeries or illness, last tetanus booster 1 year ago, Has had asthma since 2.5 years old, hospitalized at 16 years old for asthma had 5 prior hospitilizatons for asthma, denies being intubated during these hospitilizations. Up to date on all immunizations. Influenza not current. Last dental exam several years ago. Patient is non-compliant diabetic, states doesn’t take any medications. Last took metformin years ago because it was making her sick. Social History (Soc Hx) - Includes but not limited to occupation and major hobbies, family status, tobacco and alcohol use, and any other pertinent data. Include health promotion such as use seat belts all the time or working smoke detectors in the house. Denies smoking cigarettes and other illecit drugs Smoked Marijuana at 21 years old, does not currently use Drinks alcohol twice per week or less College Student majoring in accounting Lives in an old home with her mother. Enjoys watching tv, reading books, and going to talks at her church Non compliant with diabetic medications. Hasn’t used in 3 years. Doesn’t monitor blood glucose daily. Doesn’t check blood pressure regularly. Not currently sexually active, last used contraceptives 3 years ago. Family History (Fam Hx) - Includes but not limited to illnesses with possible genetic predisposition, contagious or chronic illnesses. Reason for death of any deceased first degree relatives should be included. Include parents, grandparents, siblings, and children. Include grandchildren if pertinent. Mother= Hypertension & High Cholesterol Father= died in car accident at 58 years old, Type II diabetes, Hypertension, High Cholesterol Paternal Grandfather= colon cancer, Hypertension, High Cholesterol, Type II diabetes Paternal Grandmother= Hypertension, High Cholesterol Maternal Grandfather= died of a heart attack, Hypertension, High Cholesterol Maternal Grandmother= died of a stroke, Hypertension, High Cholesterol Sister= Asthma Brother= Overweight Denies family history of Migranes symptom and provide additional details. Constitutional Skin HEENT ☐ Fatigue denies ☐ Weakness denies ☐ Fever/Chills denies ☐ Weight Gain denies ☐ Weight Loss denies ☐ Trouble Sleeping denies ☐ Night Sweats denies ☐ Other: denies ☐ Itching denies ☐ Rashes deneis ☐ Nail Changes denies ☐ Skin Color Changes denies ☐ Other: denies ☐ Diplopia denies ☐ Eye Pain denies ☐ Eye redness denies ☐ Vision changes denies ☐ Photophobia denies ☐ Eye discharge denies ☐ Earache denies ☐ Tinnitus denies ☐ Epistaxis denies ☐ Vertigo denies ☐ Hearing Changes denies ☐ Hoarseness denies ☐ Oral Ulcers denies ☐ Sore Throat denies ☐ Congestion denies ☐ Rhinorrhea denies ☐ Other: Complains of neck stiffness after MVA 1 week ago Respiratory Neuro Cardiovascular ☐ Cough denies ☐ Hemoptysis denies ☐ Dyspnea denies ☐ Wheezing denies ☐ Pain on Inspiration denis ☐ Sputum Production ☐ Other: denies ☐ Syncope or Lightheadedness denies ☒Headache worse after MVA 1 week ago ☐ Numbness denies ☐ Tingling denies ☐ Sensation Changes ☐ Speech Deficits denies ☐ Other: denies ☐ Chest pain denies ☐ SOB denies ☐ Exercise Intolerance denies ☐ Orthopnea denies ☐ Edema denies ☐ Murmurs denies ☐ Palpitations denies ☐ Faintness denies ☐ OC Changes denies ☐ Claudications denies ☐ PND denies ☐ Other: denies MSK GI GU PSYCH ☒Pain Complains of 3/10 headache ☒Stiffness Neck stiffness due to MVA occuring 1 week ago ☐ Crepitus denies ☐ Swelling denies ☐ Limited ROM ☐ Redness denies ☐ Misalignment denies ☐ Nausea/Vomiting denies ☐ Dysphasia denies ☐ Diarrhea denies ☐ Appetite Change denies ☐ Heartburn denies ☐ Blood in Stool denies ☐ Abdominal Pain denies ☐ Excessive Flatus denies ☐ Food Intolerance denies ☐ Urgency denies ☐ Dysuria denies ☐ Burning denies ☐ Hematuria denies ☐ Polyuria denies ☐ Nocturia denies ☐ Incontinence denies ☐ Other: denies ☐ Stress denies ☐ Anxiety denies ☐ Depression denies ☐ Suicidal/Homicidal Ideation denies ☐ Memory Deficits denies ☐ Mood Changes denies ☐ Trouble Concentrating denies ☐ Other: denies ☐ Rectal Bleeding denies ☐ Other: denies ☐ Other: denies GYN ☐ Rash denies ☐ Discharge denies ☐ Itching denies ☐ Irregular Menses denies ☐ Dysmenorrhea denies ☐ Foul Odor denies ☐ Amenorrhea denies ☐ LMP: denies ☐ Contraception denies ☐ Other:denies Body System Positive Findings Negative Findings General Skin Appears obese. Alert and Oriented, pleasant and cooperative 28 year old African American Female. Denies increased fatigue or changes in sleep pattern. Denies dizziness and chills. Click or tap here to enter text. HEENT Vision right eye 20/40 Head: Face symmetrical, no drooping noted. Normal hair growth to top of head. Eyes: No edema or ptosis bilaterally. Extraocular movements intact bilaterally with normal convergence. Pupils equal round and reactive to light bilaterally. Clear outline of disk to right and left fundus; no hemorrhages, optic disc pallor or papilledema. Vision left eye 20/20 Ears: Weber midline. No conductive hearing loss to left and right ears. Nose: Ability to discriminate between odors intact. Mouth: Moist buccal mucosa. Tongue midline with no wasting or fasciculations. Gag reflex intact. Neck: No swelling noted bilaterally. Sternocleidomastoid and trapezius strength normal against resistance. Respiratory Click or tap here to enter text. Click or tap here to enter text. Neuro Cranial nerve II Optic Nerve Visual Acuity right eye 20/40 Sensory: Decreased sensation in feet bilaterally. Mental Status: Alert and oriented to person, place and time. Normal attention function. Immediate and remote memory function normal. Normal learning function. Cranial Nerves: I: able to discriminate odors II: 20/20 in left eye III, IV, VI: Normal extraocular movements. V: Facial sensation intact with dull, sharp and soft sensation. VII: Symmetrical, no drooping. VIII: Lateralization normal, hearing intact bilaterally. IX, X: Gag intact XI: Strength of sternomastoid and trapezius muscles normal https://www.coursehero.com/file/59586919/NR509-SOAP-Note-Tina-Jones-Neurodocx/ against resistance. Problem List 1. Acute Pain 6 Concussion 11 Cervical spondylosis 2 Headache 7 Spinal Cord Injury 12 Cervical dislocation/fracture 3 Cervical strain/sprain 8 Neck Pain 13 Click or tap here to enter text. 4 Cluster headache 9 Whiplash trauma 14 Click or tap here to enter text. 5 Migraine 10 Tension headache 15 Click or tap here to enter text. A: Assessment Medical Diagnoses. Provide 3 differential diagnoses which may provide an etiology for the CC. The first diagnosis (presumptive diagnosis) is the diagnosis with the highest priority. Provide the ICD-10 code and pertinent findings to support each diagnosis. Diagnosis ICD-10 Code Pertinent Findings Cervical Strain S13.4XXA Complains of neck stiffness & swelling after MVA 1 week ago Acute Pain G89.11 Complains of 3/10 headache with neck stiffness after MVA 1 week ago R51 Complains 3/10 headache over last 5 days after MVA 1 week ago Headache X-Ray Cervical Spine AP, lateral, & Odontoid Click or tap here to enter text. Rule out fracture in cervical spine due to recent MVA causing trauma. (Freeman, 2019) Click or tap here to enter text. Tizanidine 2mg by mouth Take 1 tablet every 6-8 hours as needed Pain & Muscle Spasms (Freeman, 2019) Click or tap here to enter text. Click or tap here to enter text. Click or tap here to enter text. Click or tap here to enter text. Click or tap here to enter text. Click or tap here to enter text. Click or tap here to enter text. Click or tap here to enter text. Click or tap here to enter text. Click or tap here to enter text. Click or tap here to enter text. Referral/Consults: Physical Therapy Rationale/Citation Pain and Inflammation management due to recent cervical spine strain/sprain (Freeman, 2019) (Malanga, Mehnert, & Kim, 2016) Education: Alternate rest & Ice: Use Ice packs for 15-20 minutes every 1-2 hours for 7 days (1 week). This treatment aids in decreasing muscle spasms, decreasing pain, and promoting vasoconstriction. Theurapeutic exercises to include no repetitive or heavy lifting more than 10 pounds for 7 days (1 week),there should be no repetitive bending, upper extremeity twisting, over the head movement, or exaggerated neck movements. Active treatment refers to theurapeutic exercises that are aimed at improving strength, endurance, flexibility, posture, and body mechanics. Typical prescription for theurapeutic exercise is 3 times per week for 4-8 weeks. Patient will need to wear a soft neck collar because according to Freeman 2019 patients with whip-lash associated disorders caused by MVA require treatment with active submaximal movements combined with mechanical diagnosis and therapy is the standard program of initial rest, use of soft collar, and gradual self-mobilization. Rationale/Citation (Buttaro, Trybulski, Bailey, & Sandberg-Cook, 2013) (Freeman, 2019) (Malanga, Mehnert, & Kim, 2016) Follow Up: Indicate when patient should return to clinic and provide detailed instructions indicating if the patient should return sooner than scheduled or seek attention elsewhere. Patient will return to clinic in 1 week to follow up on treatment, medications, and physical therpay management. If patient’s symptoms worsen before the 1 week follow-up patient may return to clinic or seek emergency medical services at nearby Emergency Department. If patient has serious complications to include sudden or progressive Rationale/Citation (Buttaro, Trybulski, Bailey, & Sandberg-Cook, 2013) (Freeman, 2019) limb weakness, bowel or bladder changes and constituional symptoms seek emergency medical services immediately. (Malanga, Mehnert, & Kim, 2016) References Include at least one evidence-based peer-reviewed journal article which relates to this case. Use the correct APA 6th edition formatting. Buttaro, T. M., Trybulski, J., Bailey, P. P., & Sandberg-Cook, J. (2013). Neck pain. In Primary care a collaborative practice (4th ed., pp. 957-962). St. Louis, MO: Elsevier. Freeman, M. D. (2019, September 11). Cervical Sprain and Strain: Practice Essentials, Pathophysiology, Epidemiology. Retrieved from https://emedicine.medscape.com/article/306176-overview Malanga, G. A., Mehnert, M. J., & Kim, D. (2016, January 21). Cervical Spine Sprain/Strain Injuries: Background, Epidemiology, Functional Anatomy. Retrieved from https://emedicine.medscape.com/article/94387-overview [Show More]
Last updated: 1 year ago
Preview 1 out of 8 pages
Reviews( 0 )
Document information
Connected school, study & course
About the document
Uploaded On
Mar 21, 2021
Number of pages
8
Written in
Additional information
This document has been written for:
Uploaded
Mar 21, 2021
Downloads
0
Views
241

.png)


.png)
.png)
.png)
.png)

