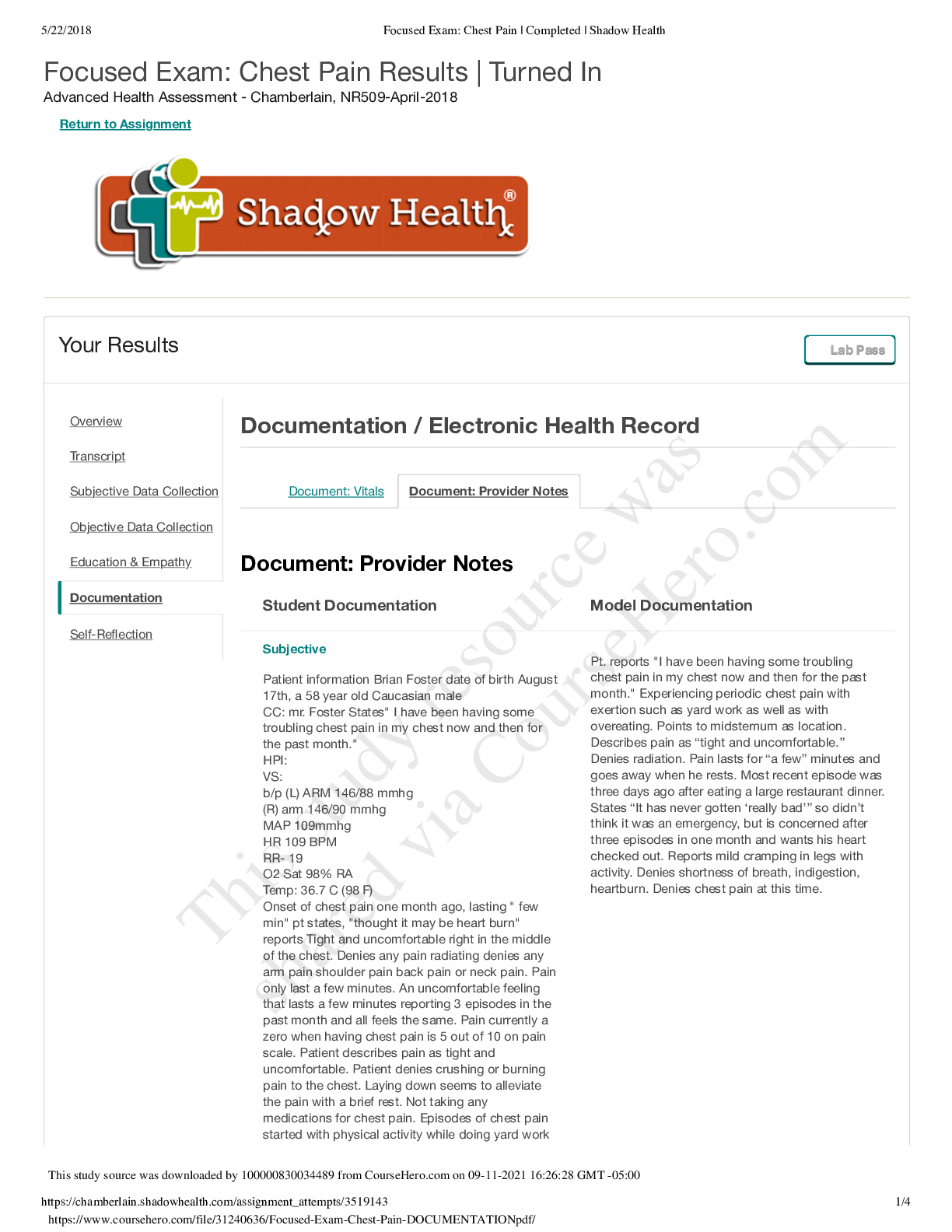
*NURSING > SOAP NOTE > NR509 Week_4_SOAP_Note - Chamberlain College of Nursing | NR 509 Week_4_SOAP_Note - CHEST PAIN (All)
NR509 Week_4_SOAP_Note - Chamberlain College of Nursing | NR 509 Week_4_SOAP_Note - CHEST PAIN
Document Content and Description Below
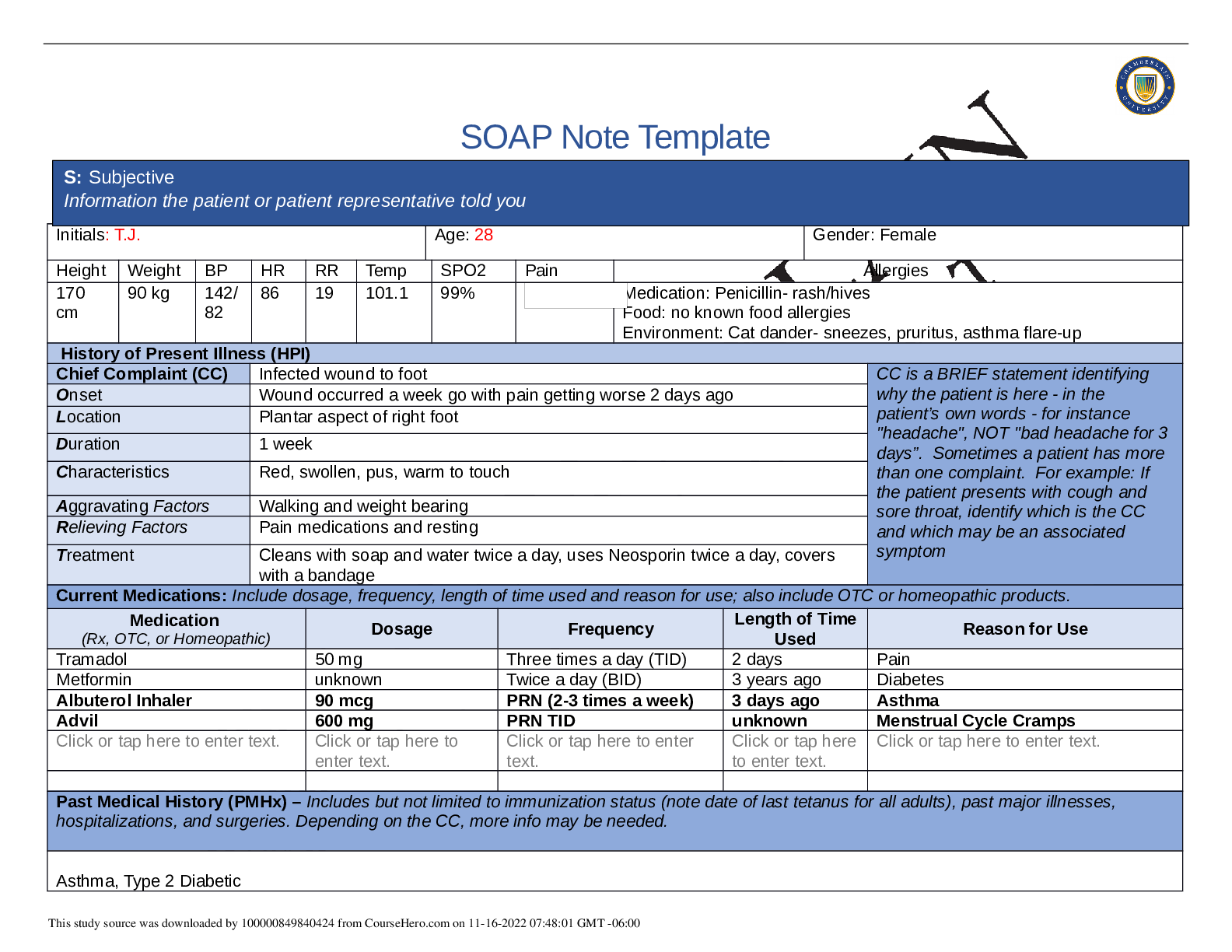
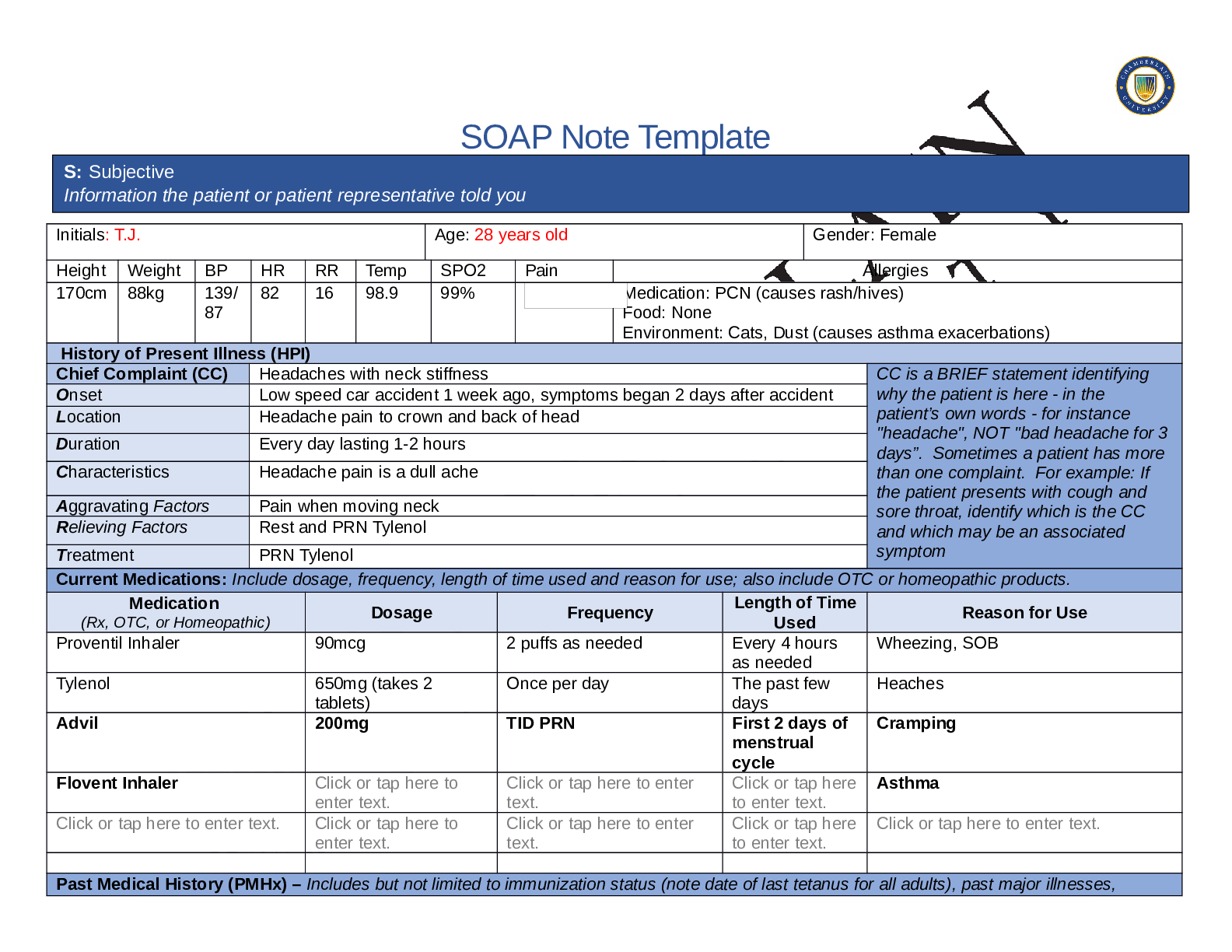
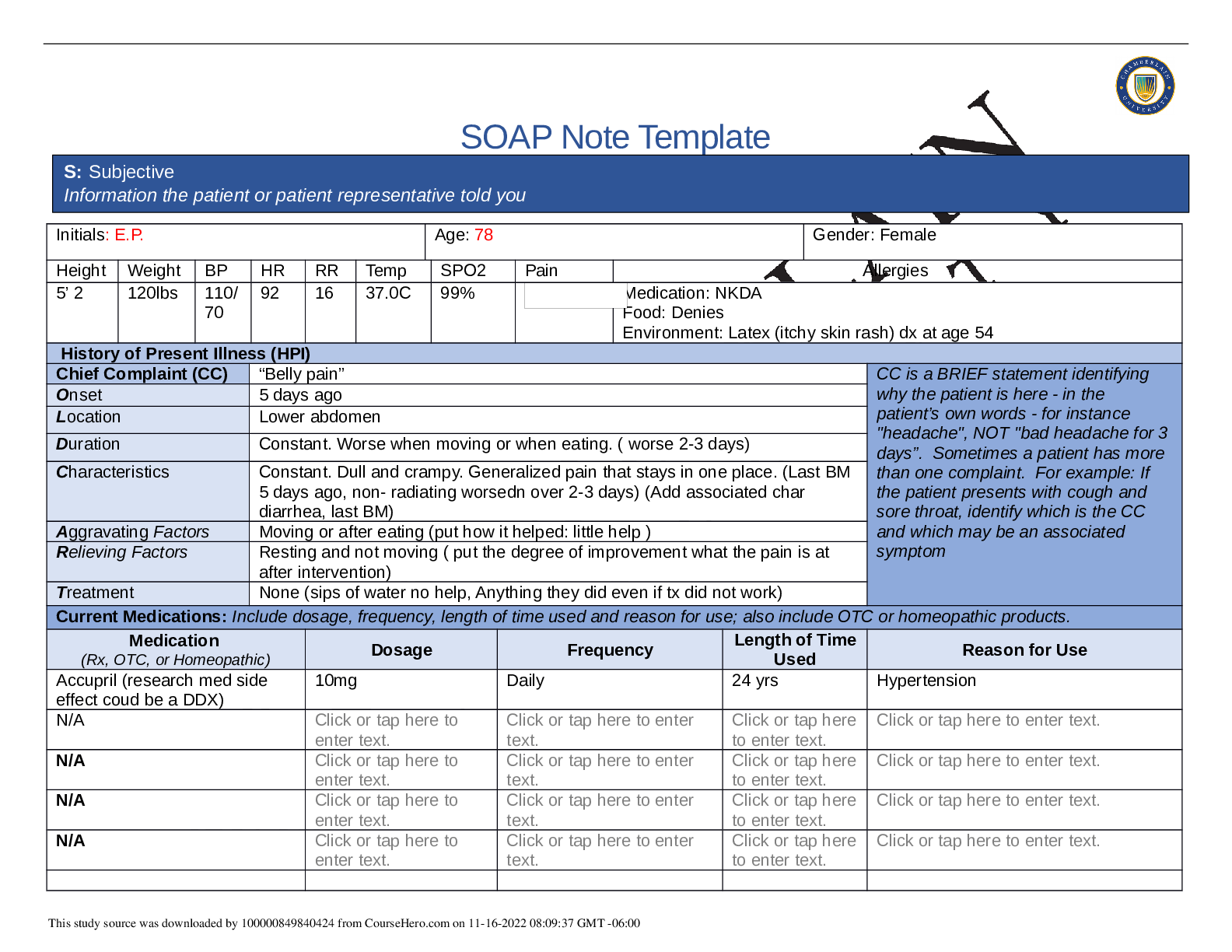
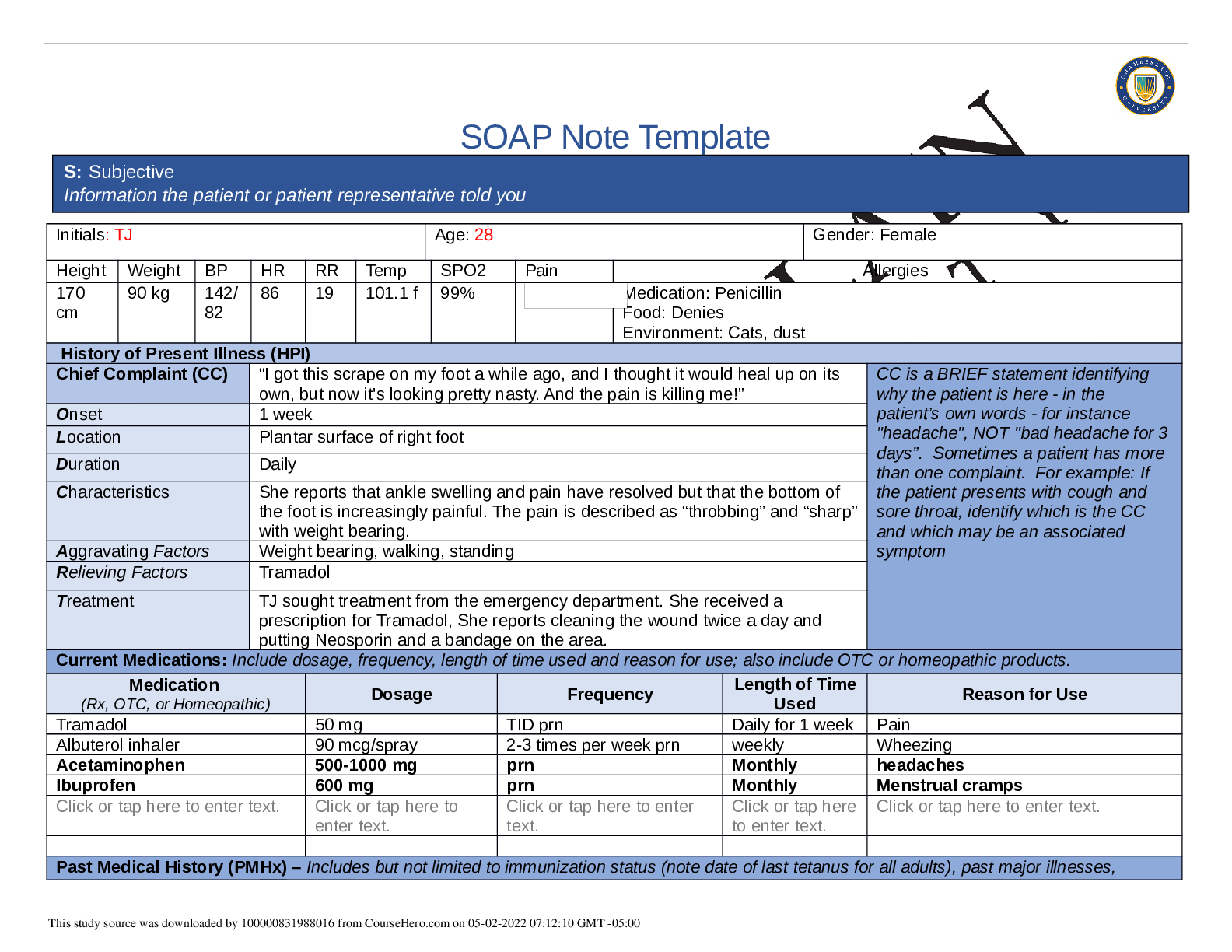
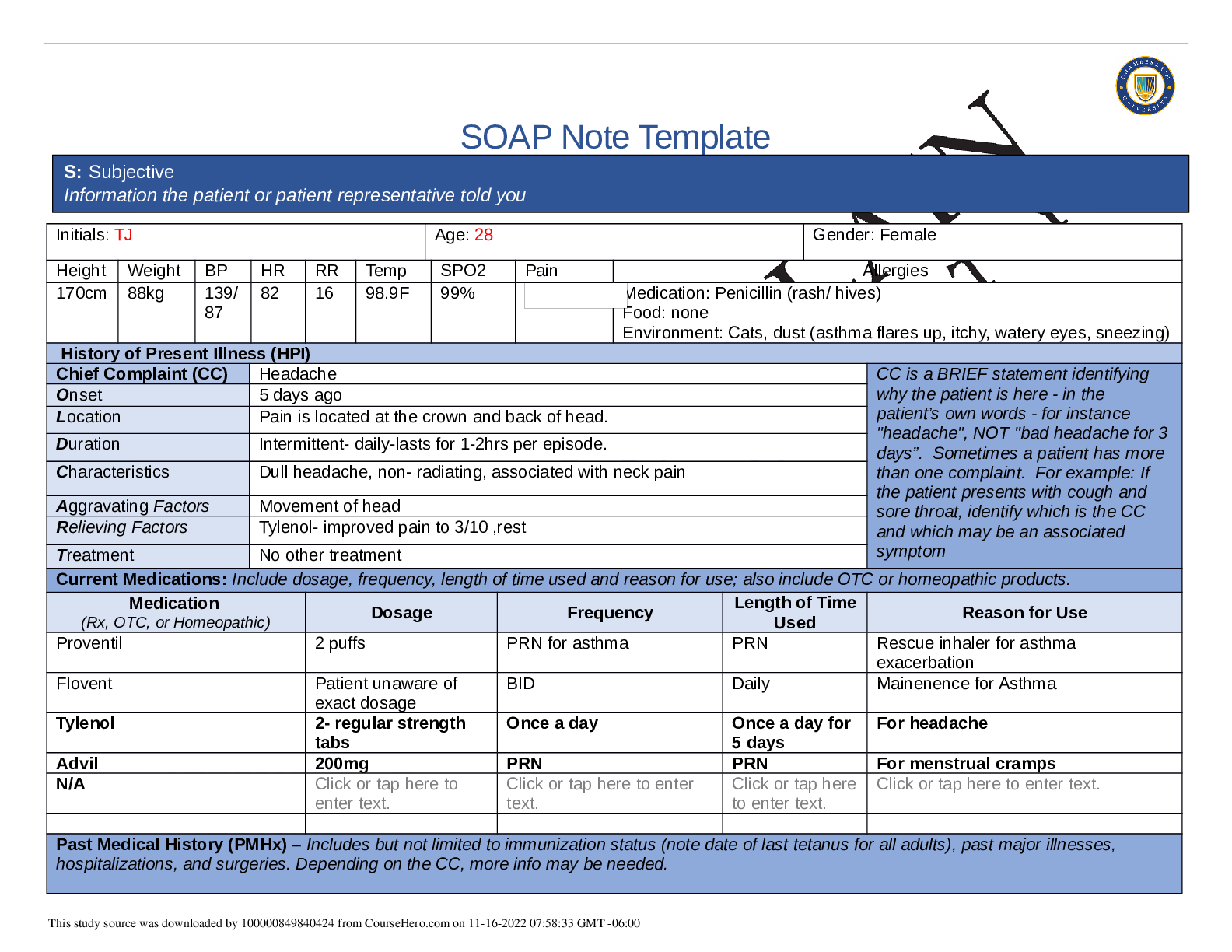
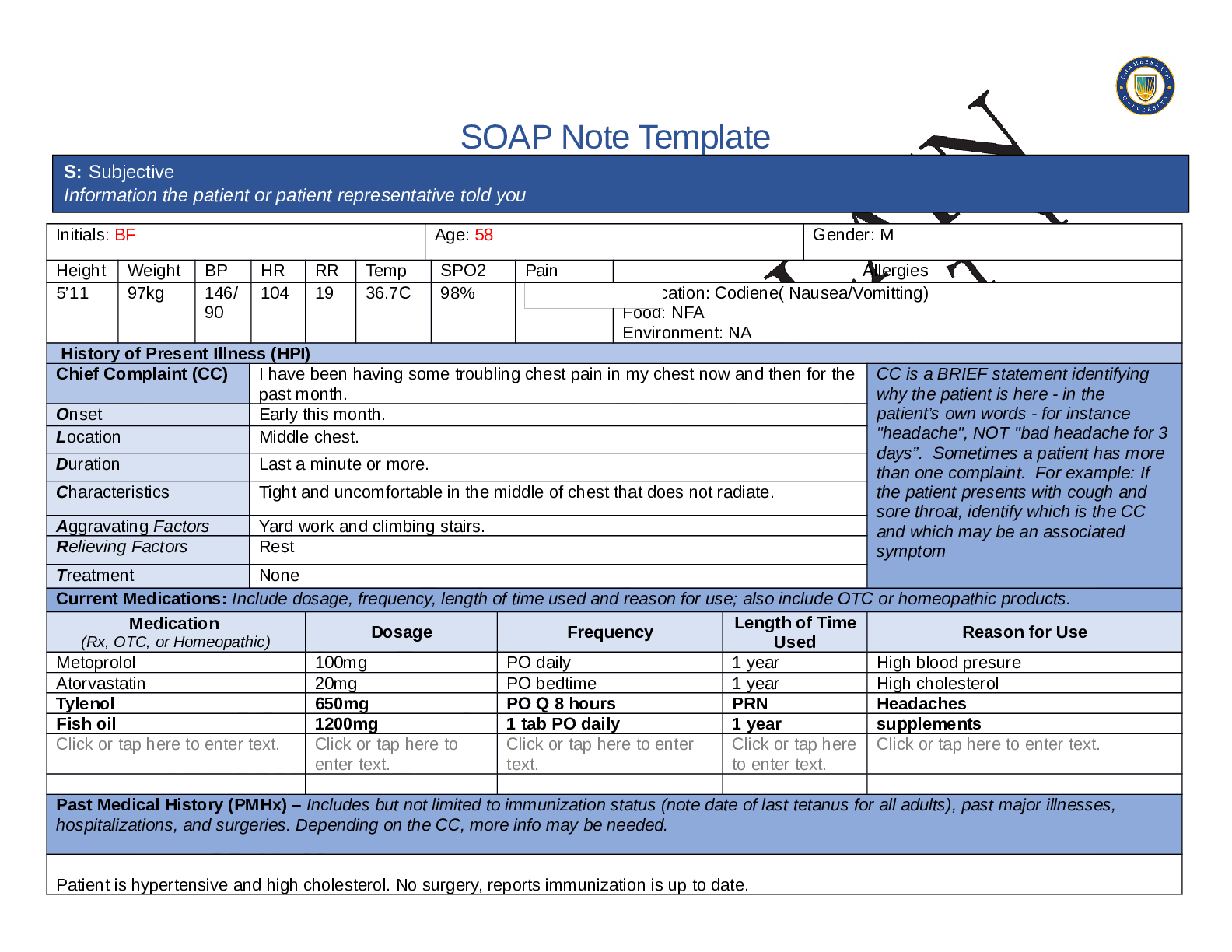
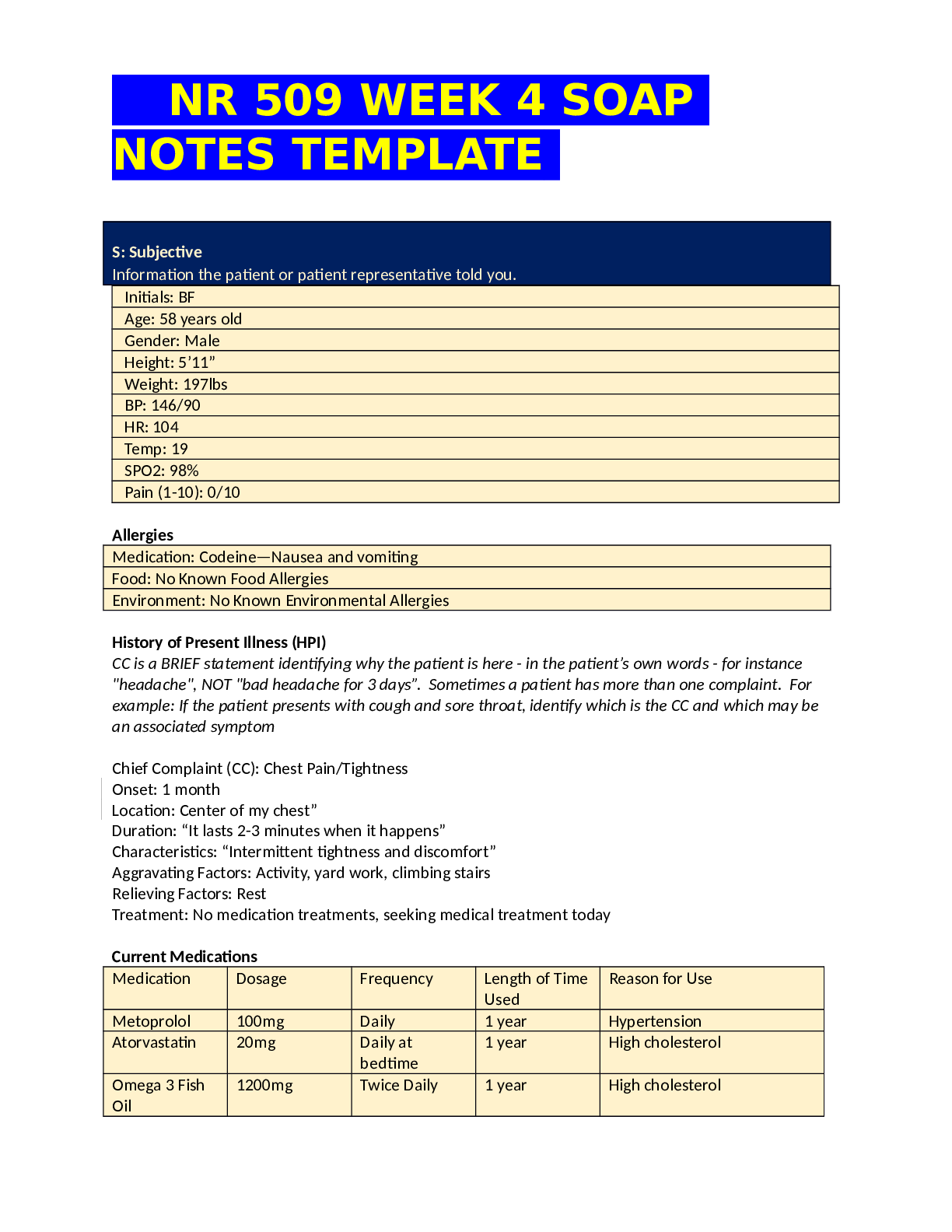
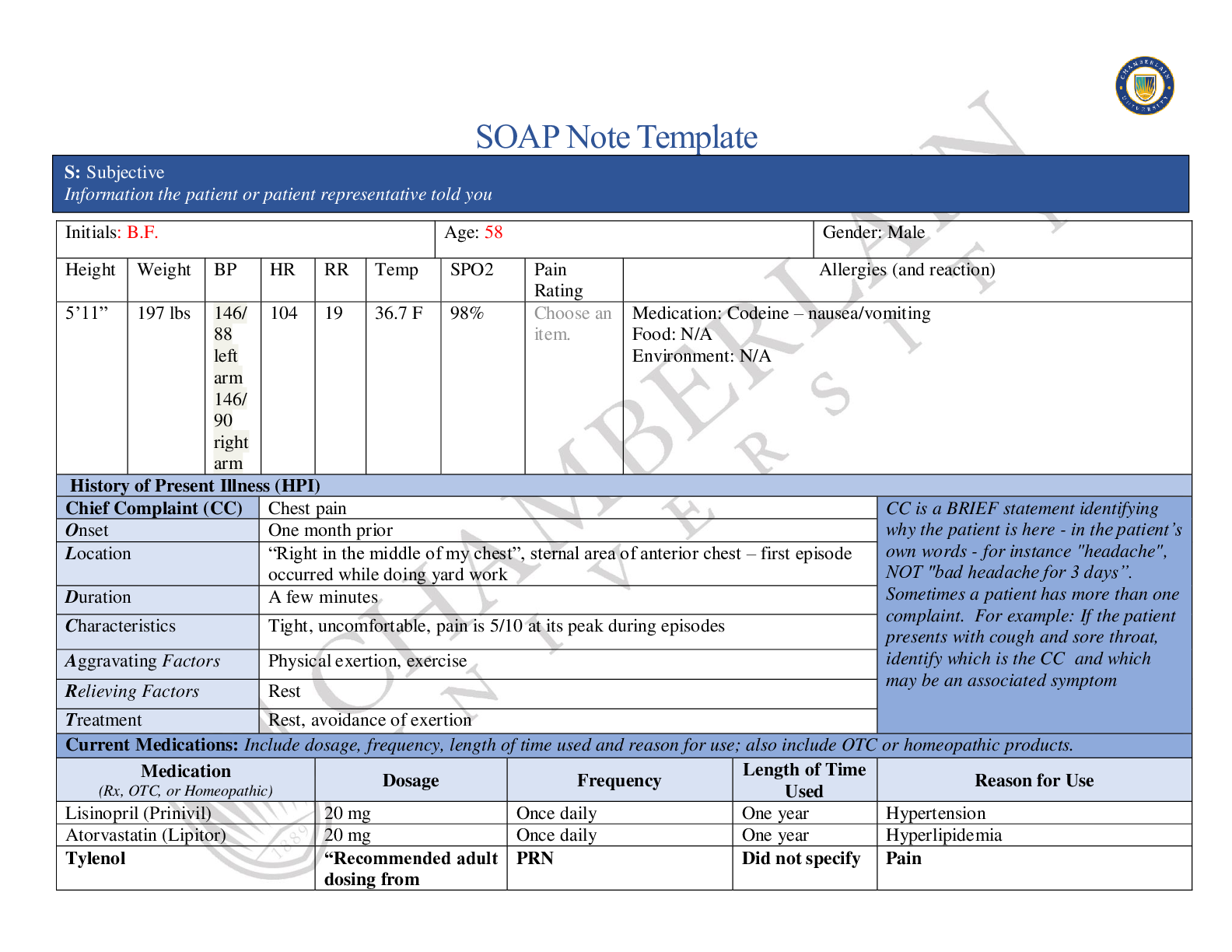
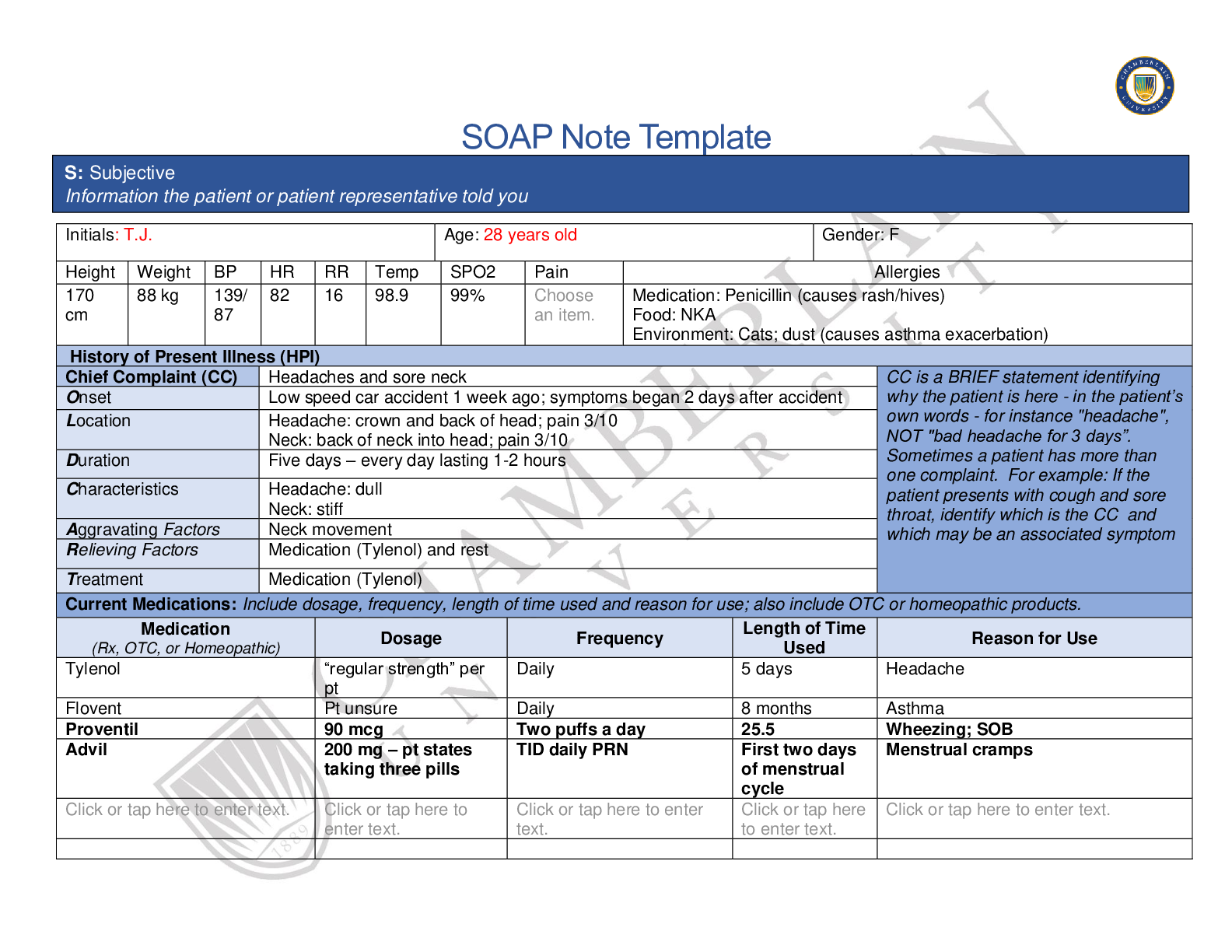
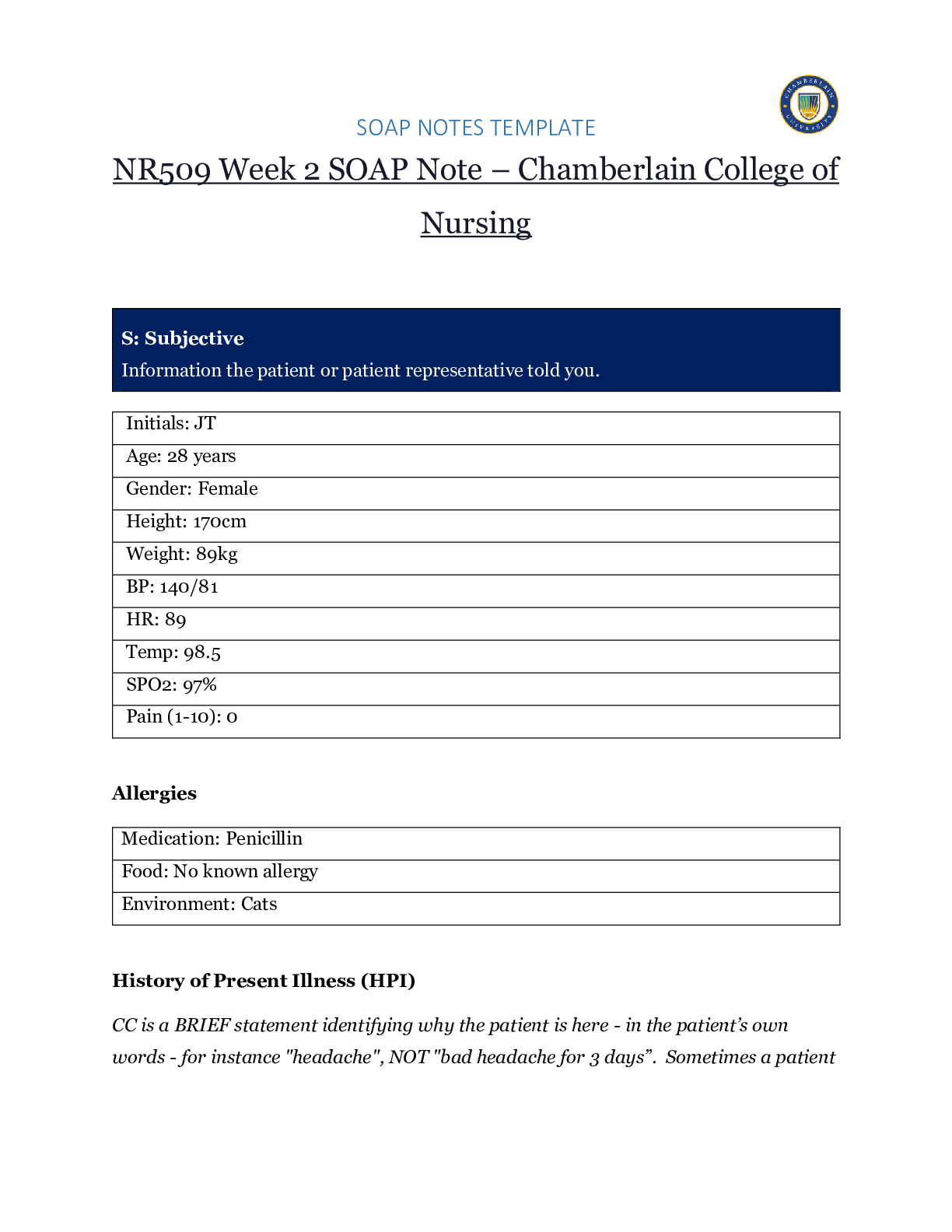
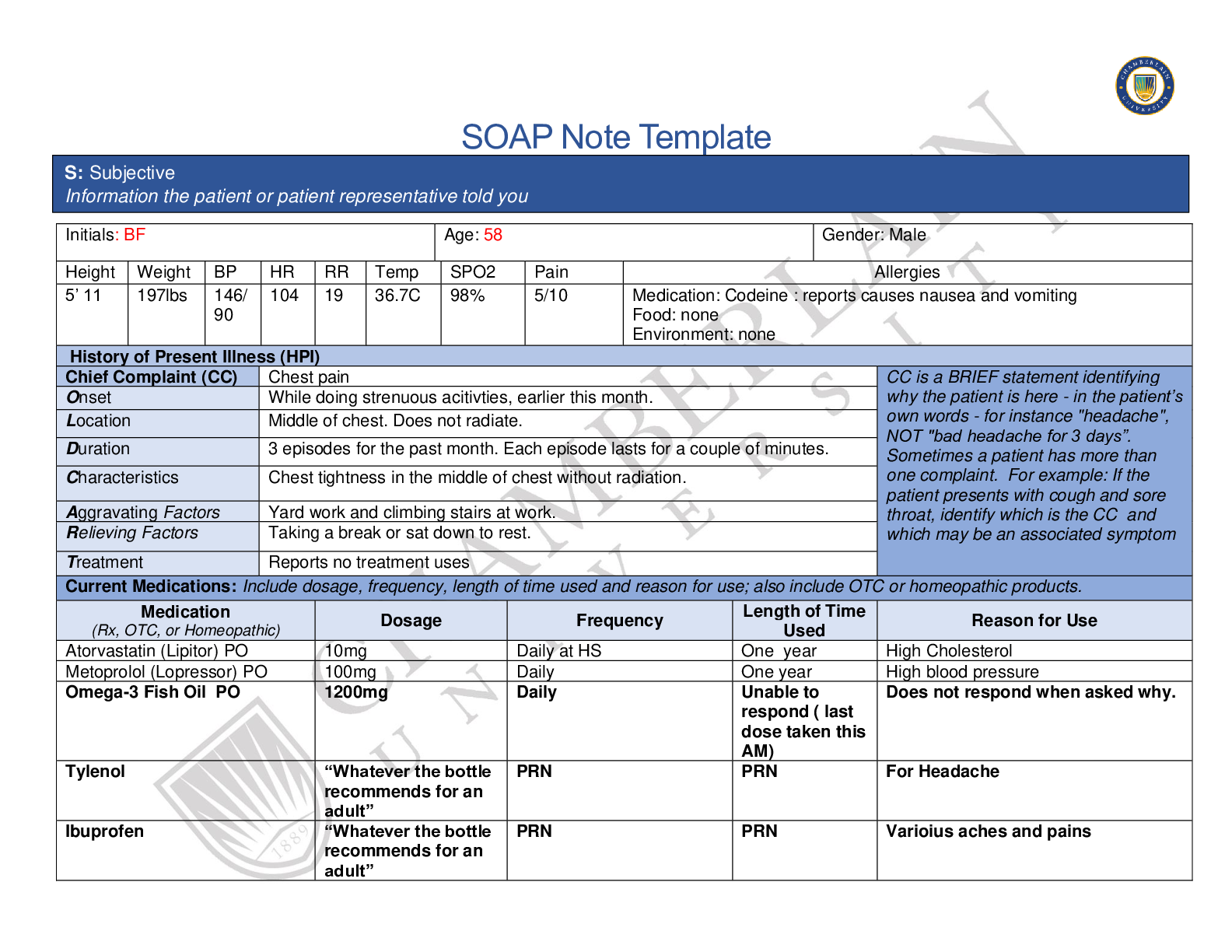
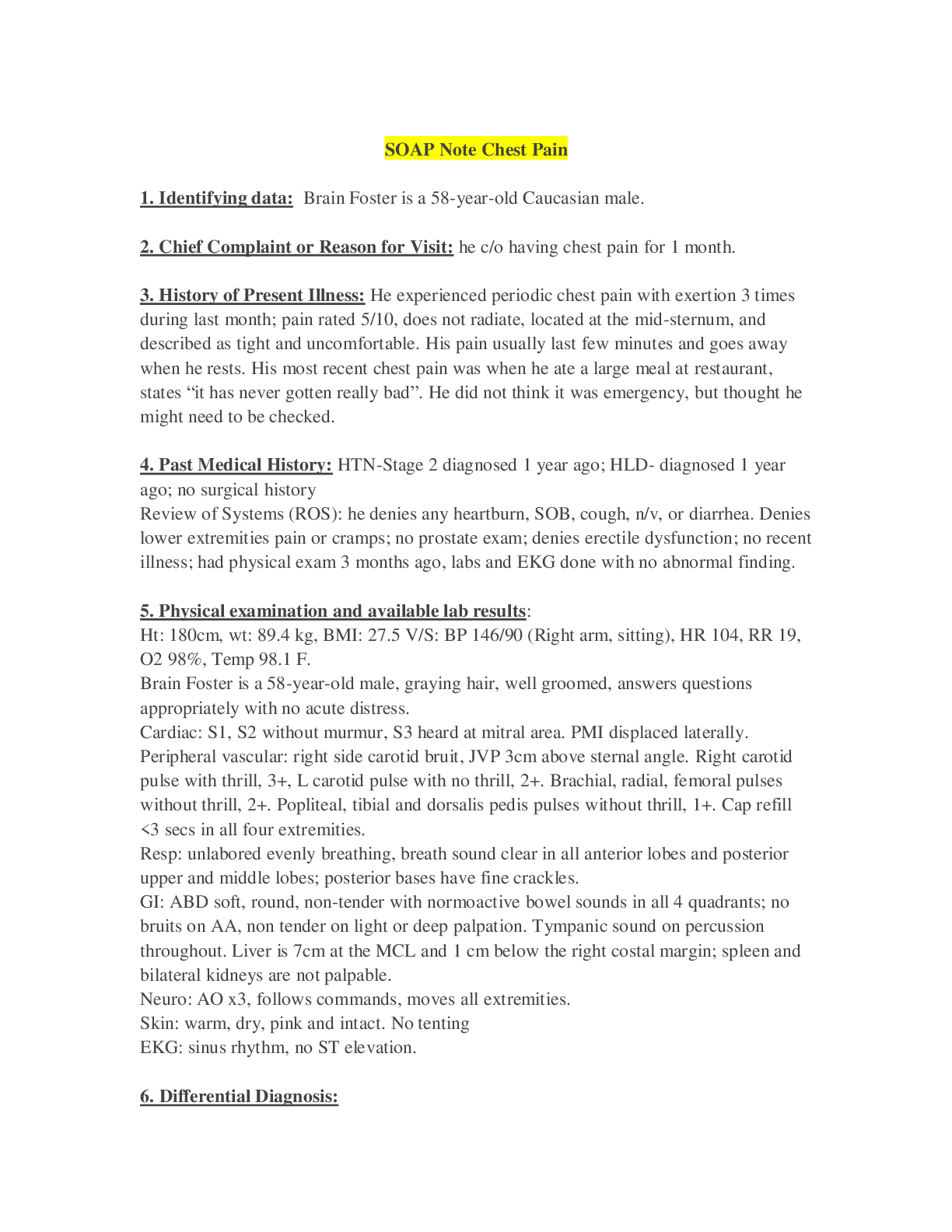
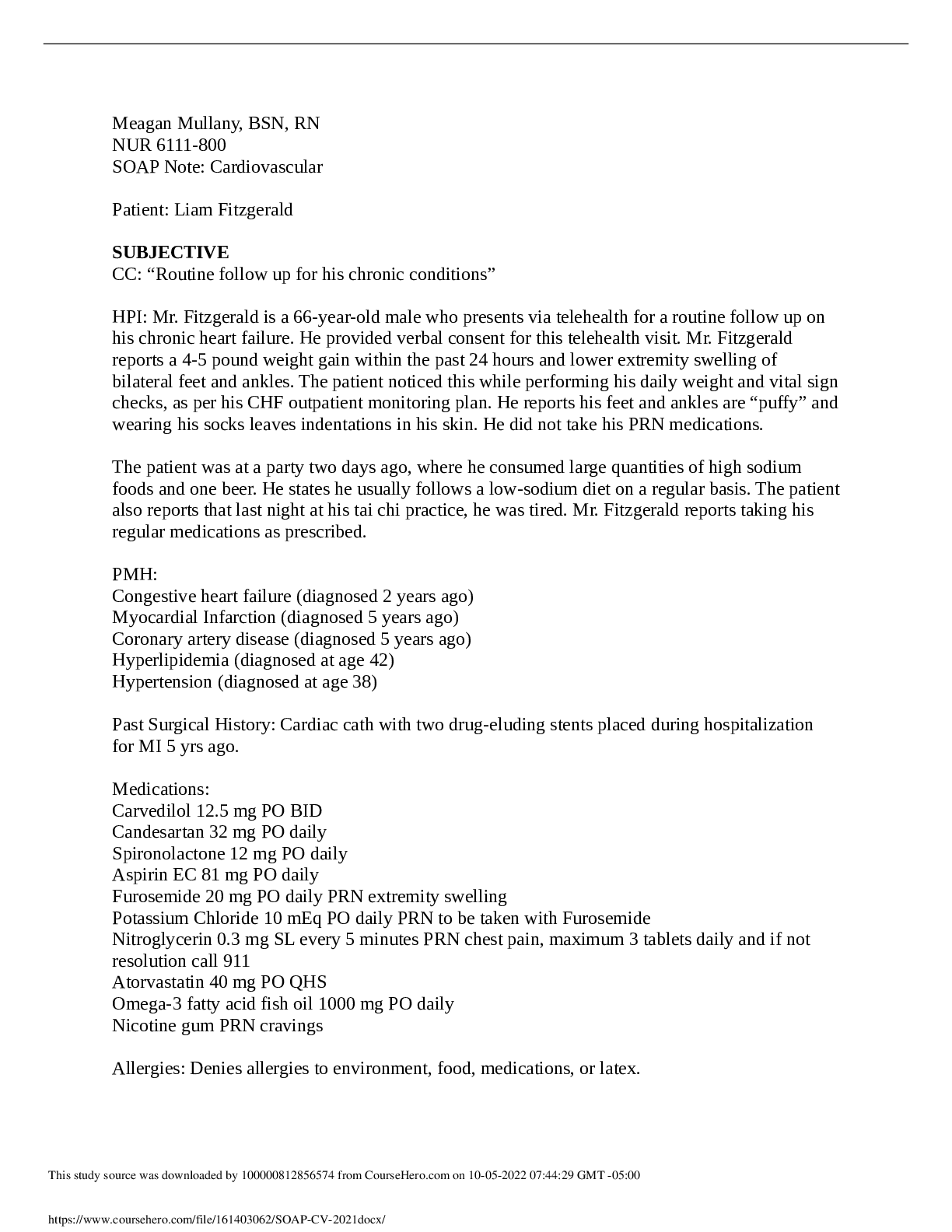
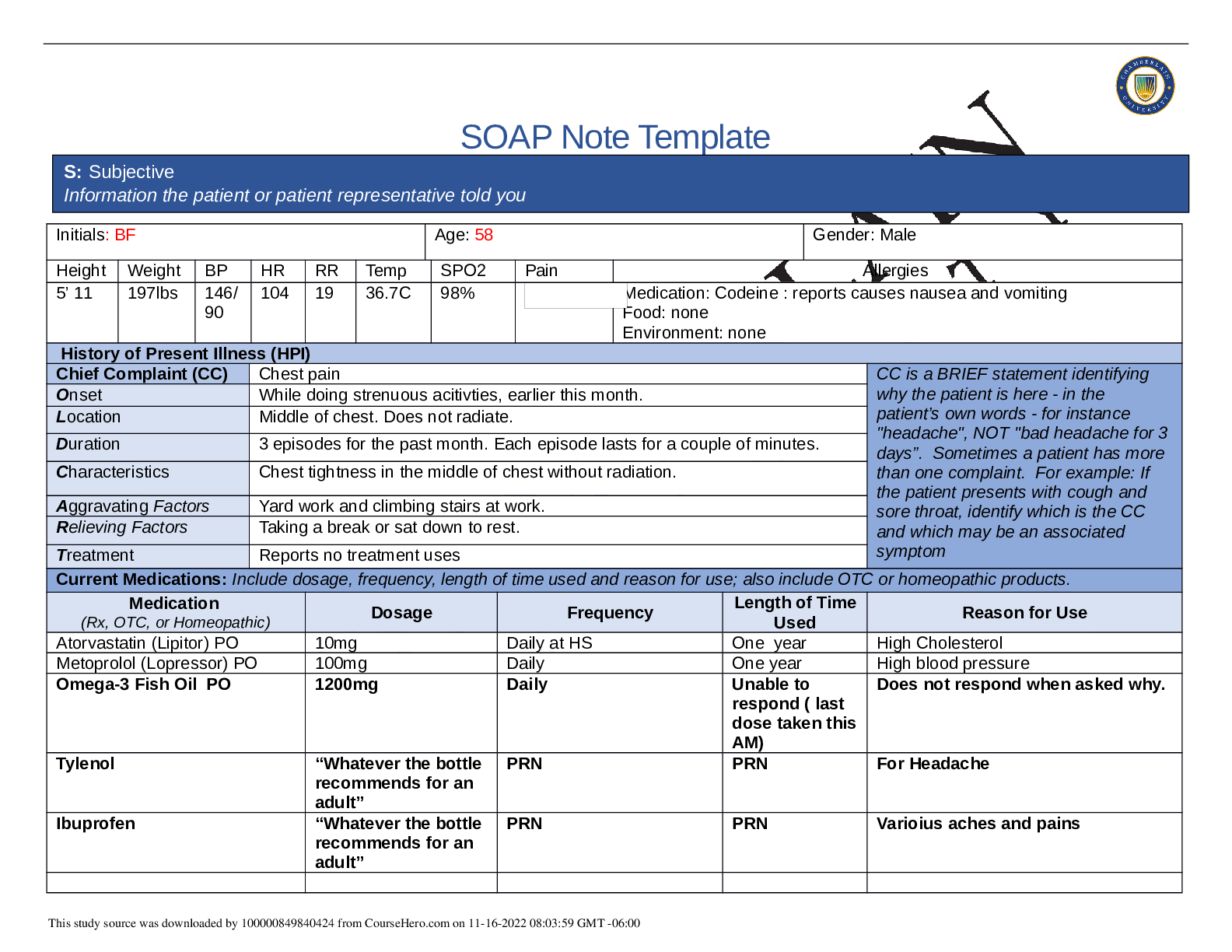
SOAP Note Template Initials: BF Age: 58 Gender: Male Height Weight BP HR RR Temp SPO2 Pain Allergies 5’ 11 197lbs 146/ 90 104 19 36.7C 98% Medication: Codeine : reports causes nausea and vomiti... ng Food: none Environment: none History of Present Illness (HPI) Chief Complaint (CC) Chest pain CC is a BRIEF statement identifying why the patient is here - in the patient’s own words - for instance "headache", NOT "bad headache for 3 days”. Sometimes a patient has more than one complaint. For example: If the patient presents with cough and sore throat, identify which is the CC and which may be an associated symptom Onset While doing strenuous acitivties, earlier this month. Location Middle of chest. Does not radiate. Duration 3 episodes for the past month. Each episode lasts for a couple of minutes. Characteristics Chest tightness in the middle of chest without radiation. Aggravating Factors Yard work and climbing stairs at work. Relieving Factors Taking a break or sat down to rest. Treatment Reports no treatment uses Current Medications: Include dosage, frequency, length of time used and reason for use; also include OTC or homeopathic products. Medication (Rx, OTC, or Homeopathic) Dosage Frequency Length of Time Used Reason for Use Atorvastatin (Lipitor) PO 10mg Daily at HS One year High Cholesterol Metoprolol (Lopressor) PO 100mg Daily One year High blood pressure Omega-3 Fish Oil PO 1200mg Daily Unable to respond ( last dose taken this AM) Does not respond when asked why. Tylenol “Whatever the bottle recommends for an adult” PRN PRN For Headache Ibuprofen “Whatever the bottle recommends for an adult” PRN PRN Varioius aches and pains S: Subjective Information the patient or patient representative told you This study source was downloaded by 100000831988016 from CourseHero.com on 04-11-2022 07:14:00 GMT -05:00 Past Medical History (PMHx) – Includes but not limited to immunization status (note date of last tetanus for all adults), past major illnesses, hospitalizations, and surgeries. Depending on the CC, more info may be needed. 3 episodes of 5/10 chest pain with physical activity, that resolved with rest after 2 min. Reports no shortness of breath. History of hypertension and hyperlipidemia. Reports Stress test 4 mo ago: normal. EKG: NSR with no ST changes. Last annual exam by PCP: 3 months ago. Reports never hospitalized. Reports no surgical history. Threw out back few years ago and took codeine, but reports allergy to codeine. Unable to recall last Pneumovax vaccine. Tdap: last on 10/2014. Influenza : received this flu season. Regular caffeine intake 1-2 cups daily. Social History (Soc Hx) - Includes but not limited to occupation and major hobbies, family status, tobacco and alcohol use, and any other pertinent data. Include health promotion such as use seat belts all the time or working smoke detectors in the house. Patient is married, lives with wife and daughter. Son lives in town. Patient is a Civil Engineer (denies working out in the field) Goes over work proposals. Denies chemical exposure. Hobbies include: fishing, sports, going to see son’s body building competitions. Family dynamic is great. Low stress. Denies cigarette smoking.Denies tobacco use. Denies current illicit drug use. Reports history of cocaine use 30 yrs ago. Reports drinking 1-2 cups coffee daily. Reports 2-3 alcohol drinks per weekend (typically drinks 2- 3beers in one sitting). Denies hx or current suicidal ideation. Denies Depression. Denies regular exercise. Family History (Fam Hx) - Includes but not limited to illnesses with possible genetic predisposition, contagious or chronic illnesses. Reason for death of any deceased first degree relatives should be included. Include parents, grandparents, siblings, and children. Include grandchildren if pertinent. Mother 80 y.o.(living)- Type 2 Diabetes and hypertension Father-Deceased at 75y.o. from colon cancer. Hx obesity, hypertention, and hyperlipidemia Spouse (Maria) 51 y.o. : Denies illnesses Son (Sam) 26y.o. : reports is healthy, is a competitive body builder Daughter(Allie) 19y.o. : Asthma Sister: 52 y.o.living- Type 2 Diabetes and hypertention Brother: deceased at 24y.o. from a car accident. Paternal grandpa- died at 85y.o. unknown Paternal grandma- died at 78 y.o from pneumonia. Maternal grandpa- died at 54 from a heart attack. Maternal grandma- died at 65 from breast cancer. Review of Systems (ROS): Address all body systems that may help rule in or out a differential diagnosis Check the box next to each positive symptom and provide additional details. Constitutional Skin HEENT This study source was downloaded by 100000831988016 from CourseHero.com on 04-11-2022 07:14:00 GMT -05:00 ☐Fatigue Denies ☐Weakness Denies ☐Fever/Chills Denies ☒Weight Gain reports 15- 20 lbs last 2 years. ☐Weight Loss Denies ☐Trouble Sleeping Denies ☐Night Sweats Denies ☐Other: Click or tap here to enter text. ☐Itching Denies ☐Rashes Denies ☐Nail Changes Denies ☐Skin Color Changes Denies ☐Other: Click or tap here to enter text. ☐Diplopia Denies ☐Eye Pain Denies ☐Eye redness Denies ☐Vision changes Denies ☐Photophobia Denies ☐Eye discharge Denies ☐Earache Denies ☐Tinnitus Denies ☐Epistaxis Denies ☐Vertigo Denies ☐Hearing Changes Denies ☐Hoarseness Denies ☐Oral Ulcers Denies ☐Sore Throat Denies ☐Congestion Denies ☐Rhinorrhea Denies ☐Other: Click or tap here to enter text. Respiratory Neuro Cardiovascular ☐Cough Denies ☐Hemoptysis Denies ☐Dyspnea Denies ☐Wheezing Denies ☐Pain on Inspiration Denies ☐Sputum Production ☒Other: Fine crackles in bilateral posterior, lower lobes ☐Syncope or Lightheadedness Denies ☐Headache Denies ☐Numbness Denies ☐Tingling Denies ☐Sensation Changes ☐Speech Deficits Denies ☐Other: Click or tap here to enter text. ☒Chest pain 3 episodes the last month, each episode last 1-2 minutes and resides with rest. ☐SOB Denies ☒Exercise Intolerance Reports unable to exercise because afraid of chest pain occurring again ☐Orthopnea Denies ☐Edema Denies ☐Murmurs Denies ☐Palpitations Denies ☐Faintness Denies ☐OC Changes Denies ☐Claudications Denies ☐PND Denies ☐Other: Click or tap here to enter text. MSK GI GU PSYCH ☐Pain chest pain ☐Stiffness Denies ☐Crepitus not assessed ☐Swelling Denies ☐Limited ROM ☐Redness Denies ☐Misalignment not assessed ☐Other: Click or tap here to enter ☐Nausea/Vomiting Denies ☐Dysphasia Denies ☐Diarrhea Denies ☐Appetite Change Denies ☐Heartburn Denies ☐Blood in Stool Denies ☐Abdominal Pain Denies ☐Excessive Flatus Denies ☐Food Intolerance Denies ☐Urgency Denies ☐Dysuria Denies ☐Burning Denies ☐Hematuria Denies ☐Polyuria Denies ☐Nocturia Denies ☐Incontinence Denies ☐Other: Click or tap here to enter text. ☒Stress low stress ☒Anxiety Little anxious about the chest pain ☐Depression Denies ☐Suicidal/Homicidal Ideation Denies ☐Memory Deficits Denies ☐Mood Changes Denies ☐Trouble Concentrating This study source was downloaded by 100000831988016 from CourseHero.com on 04-11-2022 07:14:00 GMT -05:00 text. ☐Rectal Bleeding Denies ☐Other: Click or tap here to enter text. Denies ☐Other: Click or tap here to enter text. GYN ☐Rash N/A ☐Discharge N/A ☐Itching N/A ☐Irregular Menses N/A ☐Dysmenorrhea N/A ☐Foul Odor N/A ☐Amenorrhea N/A ☐LMP: N/A ☐Contraception N/A ☐Other:Click or tap here to enter text. O: Objective Information gathered during the physical examination by inspection, palpation, auscultation, and palpation. If unable to assess a body system, write “Unable to assess”. Document pertinent positive and negative assessment findings. This study source was downloaded by 100000831988016 from CourseHero.com on 04-11-2022 07:14:00 GMT -05:00 Body System Positive Findings Negative Findings General N/A Pleasant 51 year old male sitting on exam table with normal stature. Alert and oriented x 4. Clear speech. No signs of current distress. No signs of pain or shortness of breath at this time. Able to follow commands and answer questions appropriately. Skin Inspected skin looks pale Inspected skin no scars, intact, no rash. Warm and dry. No tenting. Fingernails and toe nails inspected no abnormal color. HEENT N/A Inspected face: No visible abnormal findings. Respiratory Adventitious breath sound: Fine crackles heard in the posterior left and right lower lobes. Chest rise symmetrical. No visible abnormal findings. Neuro Click or tap here to enter text. Alert and oriented x 4, moves all extremities. Cardiovascular Auscultated extra heart sounds: Gallop, Auscultated carotid arteries: Right bruit present. Palpated Right carotid pulse: 3+ ,thrill. Palpated Right and Left popliteal, Tibial, dorsalis pedis pulses: no thrill at 1+ diminished pulses. Palpated PMI: displaced laterally < 3 cm brisk and tapping. Auscultation:Left side absent for Bruit. S1, S2,S3 audible. Auscultated abdominal aorta and lower extremity arteries: no bruit.Capillary refill < 3 seconds in all 4 extremities. Palpated Brachial, radial, femoral: no thrill and expected 2+. Kidneys are not palpable. EKG: Regular sinus rhythm, no ST changes. Musculoskeletal Click or tap here to enter text. Click or tap here to enter text. Gastrointestinal Liver Palpable at 1cm below right costal margin. Palpated: PMI displaced laterally. Inspected Abdome: symmetric, rounded, no abnormal visual findings. Bowel sounds: normoactive in all quadrants. Percussed Liver span at 7cm in the mid-clavicular line. Palpated Abdomen: no tenderness noted, No palpable mass. Spleen:not palpable Percussed abdomen and spleen: tympanic. Genitourinary Click or tap here to enter text. Click or tap here to enter text. Psychiatric ClickortapheretoentertextClickortapheretoentertextThis study source was downloaded by 100000831988016 from CourseHero.com on 04-11-2022 07:14:00 GMT -05:00 Problem List 1 Chest pain 6 Hypertension 11 N/A 2 Abnormal heart gallop 7 Hypercholesterolemia 12 N/A 3 Adventitious breath sounds (fine crackles) 8 weight gain 13 N/A 4 carotid bruit 9 Diminished pulses in the bilateral lower extremities 14 N/A 5 tachycardia 10 physical activity intolerance 15 N/A Diagnosis ICD-10 Code Pertinent Findings Stable Angina I20.9 Chest pain with physical activity, 5/10 pain at worst, c/o chest tightness in the middle of chest. Last 1-2min and resolves on it’s own with rest. Congestive heart failure I50.2 Fine crackles present in posterior left and right lower [Show More]
Last updated: 1 year ago
Preview 1 out of 8 pages
Reviews( 0 )
Document information
Connected school, study & course
About the document
Uploaded On
Apr 11, 2022
Number of pages
8
Written in
Additional information
This document has been written for:
Uploaded
Apr 11, 2022
Downloads
0
Views
129